요통에 대한 필라테스
초록
배경
비특이적 요통은 세계적인 건강문제이다. 본 질환을 가진 환자를 대상으로 가장 일반적인 치료법으로 운동에 의한 중재가 실시되어왔다. 지난 몇년간 임상 진료에서 필라테스 요법이 가장 일반적인 운동 치료 요법으로 이용되어 왔다.
목적
비 특이적인 급성, 아급성 또는 만성 요통 환자의 필라테스 치료 효과를 검토한다.
검색 전략
CENTRAL, MEDLINE, EMBASE, CINAHL, PEDro 및 SPORTDiscus를 초판부터 2014년 3월까지 검색했다. 2015년 6월 검토를 업데이트 했지만 이 결과는 아직 포함되지 않았다. 또한 연구 등록 6개 사이트 및 해당하는 논문의 참고 문헌 목록도 조사했다. 언어 또는 출판의 제한은 없었다.
선정 기준
비특이적인 급성, 준급성 또는 만성 요통을 가진 환자에 대한 필라테스 요법의 효과를 검증하는 무작위 비교 연구만을 선택했다. 주요 결과는 통증, 장애, 전반적인 회복감 및 삶의 질이었다.
자료 수집 및 분석
코크란 권장 "비뚤림 위험도" 평가 방법을 이용해서 선택한 연구의 비뚤림 위험도 평가를 2명이 각각 실시하였다. 또한 본 영역에 관련된 5문항의 질문에 대한 답변 ("예" "아니오" "어느 쪽도 아니다")을 근거로 임상적 관련성도 평가했다. GRADE 법을 이용해서 총체적인 증거의 질을 평가하고 효과크기에 관해서는 3단계로 표기했다: 소(평균 차이(MD)가 스케일의 10% 미만), 중 (평균 차이(MD)가 스케일 10%에서 20%), 대 (평균 차이(MD)가 규모의 20% 이상). 다른 척도를 사용할경우 결과 판정법을 일반적인 0‐100 기준으로 변환했다.
주요 결과
총 126건의 연구를 발견했다. 10건의 연구가 선택 기준을 충족했기 때문에 그들을 본 리뷰에 선택했다 (총 샘플 510명). 10건 중 7건은 비뚤림 위험도가 낮았고, 나머지 3건은 높은 것으로 간주했다.
6건의 연구가 필라테스와 최소중재를 비교했다. 단기 추적 조사 (무작위 후 3개월 미만)에서 필라테스가 최소중재와 비교시 통증을 감소시켰다는 중간 효과 크기의 낮은 품질의 증거를 찾았다 (MD ‐14.05, 95% 신뢰 구간(CI) ‐18.91˜‐9.19). 중기 추적 조사 2건에서 (무작위 후 3개월에서 12개월 미만)에서 필라테스를 최소중재와 비교시 통증의 감소를 나타내는 중간 효과 크기의 중간수준의 증거를 나타냈다 (MD ‐10.54, 95% CI‐18.46˜‐2.62). 5건의 연구에서 필라테스가 최소중재대비 장애 개선에 효과적이라는 질 낮은 증거를 확보했는데 단기의 경우 작은 효과 크기 (MD ‐7.95, 95% CI ‐13.23˜‐2.67), 중기 추적조사의 경우 중간 효과크기의 중간수준의 질을 얻었다(MD ‐11.17, 95% CI ‐18.41˜‐3.92). 증거의 질이 낮은 1건의 연구에서 기능(MD 1.10, 95% CI 0.23˜1.97) 및 전반적인 회복감(MD 1.50, 95 % CI 0.70˜2.30) 에서 작은 효과크기의 상당한 효과를 보였지만, 중기 추적조사시 똑같은 결과가 나오진 않았다.
4건의 연구에서 필라테스와 다른 운동을 비교했다. 통증 결과에서의 높은 이질성 때문에 묘사형태로 결과를 통합했다. 단기 추적 조사에서는 낮은 질의 2건의 연구에서 필라테스를 지지하는 상당한 효과가 입증 되었지만, 1건의 연구에서 유의한 차이가 보고되지 않았다. 중기 추적 조사에서는 낮은 증거의 1건의 연구에서 필라테스 지지의 유의한 효과를 보였고 다른 1건의 연구에서 유의한 차이를 보고하지 않았다. 장애에 관한 결과에서 각각을 비교한 두 연구에 따르면 필라테스와 다른 운동은 단기간(MD ‐3.29, 95% CI ‐6.82˜0.24) 또는 중기간(MD‐0.91, 95% CI ‐5.02˜3.20) 에 유의한 차이가 없다는 중간 수준의 증거가 있다. 1건의 낮은 질의 연구에서는 단기 추적 조사에서 필라테스가 타 운동에 비해 상당한 수준의 기능차이를 일으킨다고 했지만 (MD 0.10, 95% CI ‐2.44˜2.64)중기추적 결과에서는 타 운동이 더 나은 것으로 나타났다 (MD ‐3.60, 95% CI ‐7.00˜‐0.20). 회복감이나 삶의 질을 보고한 연구는 없었다. 2건의 연구에서 부작용을 평가했고, 1건은 부작용을 찾지 못했고 나머지 1건은 경미한 사건들을 보고했다.
연구진 결론
어떠한 연구에서도 질 높은 증거를 찾지 못했다. 그러나 통증 및 장애에 최소 중재보다 필라테스가 효과적이라는 낮은˜중간 수준의 증거를 확보했다. 중기 추적 조사결과에 따르면 필라테스는 다른 운동과 비교시 고통과 장애에 대한 약간의 효과를 보였다. 요통에 대한 필라테스가 효과적이라는 증거가 적지 않게 존재하지만, 다른 운동 요법보다 필라테스가 효과적이라는 확실한 증거는 없다. 필라테스의 허리 통증 치료에 대한 이용 여부는 환자 또는 의료 제공자의 취향과 비용에 의하여 결정함이 바람직하다.
PICOs
쉬운 말 요약
요통에 대한 필라테스
연구의 질문
비 특이적인 급성, 아급성 또는 만성 요통 환자의 필라테스 치료 효과를 검토한다.
배경
요통은 전세계적으로 중요한 건강 문제이다. 요통에 가장 일반적인 치료는 운동이며 최근 몇 년간 필라테스 요법은 요통을 치료하는 흔한 방법 중 한가지가 되었다.
검색 날짜
2014년 3월까지 근거를 확인했다. 2015년 6월 검토를 업데이트 했지만 이 결과는 아직 포함되지 않았다.
연구 특징
본 고찰은 510명이 참여한 10건의 시험을 포함한다. 모든 시험이 비슷한 규모였으며, 비 특이적인 요통 환자를 대상으로 했다. 일부 시험은 만성 요통 환자만 대상으로 했다. 포함된 연구의 치료 프로그램 기간은 10일 부터 90일까지 였다. 후속 추적 기간은 4주 에서 6개월로 다양했다. 포함된 연구 중 6개월 넘는 추척 기간을 가진 연구는 없었다. 연구의 규모는 17˜87명이였다.
주요 결과
포함 된 연구를 통해 단기적 또는 중기적으로 봤을 때 필라테스는 통증 및 장애에 최소한의 중재보다 효과적이며 단기적 기능 향상 또는 전반적 회복을 보이는 것에 최소한의 중재보다 효과적인 것을 확인했다. 필라테스는 다른 운동과 비교하여 단기적 또는 중기적인 통증 및 장애의 개선에 특별한 우위를 보이지 않을 것이다. 중기 추적기간에는 다른 운동이 필라테스와 비교하여 기능적 향상에 더 우월하였으나 단기적 추적기간에는 그렇지 않았다. 따라서 필라테스가 요통에 효과가 있다는 근거가 있음에도 이것이 다른 운동 방법에 비해 월등히 효과적이라는 것에 대한 확증이 없다. 본 고찰의 중재에서 부작용은 경미했거나 없다고 보고했다.
근거의 질
전반적인 근거의 질은 낮음에서 중간 정도였다.
Authors' conclusions
Summary of findings
| Pilates compared with minimal intervention for low back pain | ||||||
| Patient or population: patients with low back pain Settings: primary or tertiary care Intervention: Pilates Comparison: minimal intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Minimal intervention | Pilates | |||||
| Pain NRS: scale from 0 to 100 (worse pain) Follow‐up: short‐term (less than 3 months from randomisation) | The mean pain at short‐term follow‐up ranged across control groups from 33.9 to 52 points | The mean pain at short‐term follow‐up in the intervention groups was (18.9 to 9.2 lower) | Mean difference ‐14.05 (‐18.91 to ‐9.19) | 265 participants | ⊕⊕⊝⊝ | This is a moderate effect that is clinically relevant in this patient group |
| Pain NRS: scale from 0 to 100 (worse pain) Follow‐up: intermediate‐term (more than 3 months and less than 12 months) | The mean pain at intermediate‐term follow‐up ranged across control groups from 53 to 58.3 points | The mean pain at intermediate‐term follow‐up in the intervention group was 10.5 lower (18.5 to 2.6 lower) | Mean difference ‐10.54 (‐18.46 to ‐2.62) | 146 participants (2 studies) | ⊕⊕⊕⊝ | This is a moderate effect that is clinically relevant in this patient group |
| Disability Multiple scales: scale from 0 to 100 (worse disability) Follow‐up: short‐term (less than 3 months from randomisation) | The mean disability at short‐term follow‐up ranged across control groups from 13.3 to 44.1 points | The mean disability at short‐term follow‐up in the intervention groups was 7.95 lower (13.2 to 2.7 lower) | Mean difference ‐7.95 (‐13.23 to ‐2.67) | 248 participants (5 studies) | ⊕⊕⊝⊝ | This is a small effect that may be clinically relevant in this patient group |
| Disability Multiple scales: scale from 0 to 100 (worse disability) Follow‐up: intermediate‐term (more than 3 months and less than 12 months) | The mean disability at intermediate‐term follow‐up ranged across control groups from 27.9 to 44.4 points | The mean disability at intermediate‐term follow‐up in the intervention groups was (18.4 to 3.9 lower) | Mean difference ‐11.17 (‐18.41 to ‐3.92) | 146 participants (2 study) | ⊕⊕⊕⊝ | This is a moderate effect that is clinically relevant in this patient group |
| Function Patient Specific Functional Scale: used in a 11‐point scale from 0 to 10 (greater functional ability) Follow‐up: short‐term (less than 3 months from randomisation) | The mean function at short‐term follow‐up in the control group was 6.4 points | The mean function at short‐term follow‐up in the intervention group was 1.1 higher (0.2 to 2.0 higher) | Mean difference 1.10 (0.23 to 1.97) | 86 participants (1 study) | ⊕⊕⊝⊝ | This is a small effect that may be clinically relevant in this patient group (results from 1 single study) |
| Function Patient Specific Functional Scale: used in a 11‐point scale from 0 to 10 (greater functional ability) Follow‐up: intermediate‐term (more than 3 months and less than 12 months) | The mean function at intermediate‐term follow‐up in the control group was 6.1 points | The mean function at intermediate‐term follow‐up in the intervention group was 0.8 higher (0.0 lower to 1.6 higher) | Mean difference 0.80 (‐0.00 to 1.60) | 86 participants (1 study) | ⊕⊕⊝⊝ | The difference is not statistically or clinically significant (results from 1 single study) |
| Global impression of recovery Global Perceived Effect Scale: scale from ‐5 to +5 (greater recovery) Follow‐up: short‐term (less than 3 months from randomisation) | The mean global impression of recovery at short‐term follow‐up in the control group was 1.7 points | The mean global impression of recovery at short‐term follow‐up in the intervention group was 1.5 higher (0.7 to 2.3 higher) | Mean difference 1.50 (0.70 to 2.30) | 86 participants (1 study) | ⊕⊕⊝⊝ | This is a small effect that may be clinically relevant in this patient group (results from 1 single study) |
| Global impression of recovery Global Perceived Effect Scale: scale from ‐5 to +5 (greater recovery) Follow‐up: intermediate‐term (more than 3 months and less than 12 months) | The mean global impression of recovery at intermediate‐term follow‐up in the control group was 1.7 points | The mean global impression of recovery at intermediate‐term follow‐up in the intervention group was 0.7 higher (0.1 lower to 1.5 higher) | Mean difference 0.70 (‐0.11 to 1.51) | 86 participants (1 study) | ⊕⊕⊝⊝ | The difference is not statistically or clinically significant (results from 1 single study) |
| Adverse events | See comment | See comment | Not estimable | See comment | Only 1 included trial assessed adverse events and none were reported | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one level due to imprecision (fewer than 400 participants, total). 2 Downgraded one level due to risk of bias (> 25% of the participants were from studies with a high risk of bias). 3Downgraded one level due to clear inconsistency of results. 4Downgraded one level due to inconsistency (I² > 50%). | ||||||
| Pilates compared with other exercises for low back pain | ||||||
| Patient or population: participants with low back pain Settings: primary and tertiary care Intervention: Pilates Comparison: other exercises | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Other exercises | Pilates | |||||
| Pain NRS: scale from 0 to 100 (worse pain) Follow‐up: short‐term (less than 3 months from randomisation) | Not estimated | Not estimated | Not estimated | 181 participants (3 studies) | ⊕⊕⊝⊝ | Pooled results not estimated due to high heterogeneity |
| Pain NRS: scale from 0 to 100 (worse pain) Follow‐up: intermediate‐term (more than 3 months and less than 12 months) | Not estimated | Not estimated | Not estimated | 151 participants (2 studies) | ⊕⊕⊝⊝ | Pooled results not estimated due to high heterogeneity |
| Disability Multiple scales: scale from 0 to 100 (worse disability) Follow‐up: short‐term (less than 3 months from randomisation) | The mean disability at short‐term follow‐up ranged across control groups from 17.1 to 20 points | The mean disability at short‐term follow‐up in the intervention groups was (6.8 lower to 0.2 higher) | Mean difference ‐3.29 (‐6.82 to 0.24) | 149 participants (2 studies) | ⊕⊕⊕⊝ | The difference is not statistically or clinically significant |
| Disability Multiple scales: scale from 0 to 100 (worse disability) Follow‐up: intermediate‐term (more than 3 months and less than 12 months) | The mean disability at intermediate‐term follow‐up ranged across control groups from 13 to 18.1 points | The mean disability at intermediate‐term follow‐up in the intervention groups was (5.0 lower to 3.2 higher) | Mean difference ‐0.91 (‐5.02 to 3.20) | 151 participants (2 studies) | ⊕⊕⊕⊝ | The difference is not statistically or clinically significant |
| Function Patient Specific Functional Scale: scale from 0 to 30 (greater functional ability) Follow‐up: short‐term (less than 3 months from randomisation) | The mean function at short‐term follow‐up in the control group was 18.9 points | The mean function at short‐term follow‐up in the intervention group was 0.1 lower (2.4 lower to 2.6 higher) | Mean difference 0.10 (‐2.44 to 2.64) | 87 participants (1 study) | ⊕⊕⊝⊝ | The difference is not statistically or clinically significant (results from 1 single study) |
| Function Patient Specific Functional Scale: scale from 0 to 30 (greater functional ability) Follow‐up: intermediate‐term (more than 3 months and less than 12 months) | The mean function at intermediate‐term follow‐up in the control group was 22.8 points | The mean function at intermediate‐term follow‐up in the intervention group was 3.6 lower (7 to 0.2 lower) | Mean difference ‐3.60 (‐7.00 to ‐0.20) | 87 participants (1 study) | ⊕⊕⊝⊝ | This is a small effect that may be clinically relevant in this patient group (results from 1 single study) |
| Adverse events | See comment | See comment | Not estimable | See comment | 1 trial assessed adverse events and reported minor events | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one level due to imprecision (fewer than 400 participants, total). 2Downgraded one level due to inconsistency (I² > 50%). 3Downgraded one level due to clear inconsistency of results. | ||||||
Background
Non‐specific low back pain (LBP) is a highly prevalent condition (Hoy 2012), which is associated with disability and work absenteeism worldwide (Waddell 2004). Recent prognostic studies have concluded that around 40% of patients with acute LBP will not recover within three months (Costa 2012; Henschke 2008), and of these only 40% will recover during the following 12 months (Costa 2009; Costa 2012). Not surprisingly, the costs associated with LBP and related disability are enormous, causing a major economic burden for patients, governments and health insurance companies (Dagenais 2008).
Exercise therapy is probably the most commonly used intervention for the treatment of patients with chronic non‐specific LBP. Exercise has a plausible biological rationale and low cost, and it has been recommended in most of the clinical practice guidelines for chronic LBP (Chou 2007; Delitto 2012; European Guidelines 2006), as well as by important systematic reviews on this topic (Hayden 2005; Hayden 2007). These reviews and guidelines have typically reported the effects of exercise in general, but not separately the effects of different approaches to exercise. However, the exercise programmes now used for low back pain vary enormously, for example hydrotherapy, walking programmes, behavioural approaches such as graded activity and graded exposure, and mind‐body exercises such as yoga and Tai Chi. To guide the treatment choice of both the clinician and patient it would be useful to have separate evidence on the effectiveness of the most popular approaches to exercise.
One type of exercise programme that has been increasingly used for patients with LBP over the last decade is the Pilates method (Musculino 2004; Queiroz 2005; Rydeard 2006). Pilates exercises were developed by Joseph Pilates in the 1920s and this method was originally named 'centrology' (Anderson 2000). These exercises can be performed with or without specialised equipment following six basic principles: centering, concentration, control, precision, flow and breathing (Wells 2012). The effectiveness of the Pilates approach has been tested in a few randomised controlled trials (Curnow 2009; Fonseca 2009; Gladwell 2006; Rydeard 2006; Wajswelner 2012). Our aim was to perform the first Cochrane systematic review on this topic in order to provide accurate and robust information on the effectiveness of the Pilates approach for low back pain, compared to no intervention, placebo or other types of interventions.
Description of the condition
Low back pain is defined as pain or discomfort localised below the ribs and above the gluteal crease (where the upper leg meets the buttock), with or without referred leg pain (European Guidelines 2006). Non‐specific LBP is the most common and can be defined as LBP without any known specific cause or pathology, such as nerve root compromise or serious spinal pathology (i.e. fracture, cancer and inflammatory diseases). Low back pain is often classified in three stages (acute, subacute and chronic) according to its duration and this provides some information to the clinician with regards to treatment and prognosis. Acute LBP is usually defined as an episode persisting for less than six weeks; subacute as LBP persisting for between six and 12 weeks, and chronic as LBP persisting for 12 weeks or longer (European Guidelines 2006). For the purposes of this review, we included studies that recruited patients with non‐specific LBP of any duration, but we analysed them separately (if applicable).
Description of the intervention
The Pilates method was developed by Joseph Hubertus Pilates and consists of comprehensive body conditioning, which aims to develop better body awareness and improved posture (Queiroz 2005; Rydeard 2006). Pilates exercises mainly involve isometric contractions (i.e. contraction without joint movement) of the core muscles, which make up the muscular centre responsible for the stabilisation of the body, both while it is moving or at rest. Pilates became popular as a treatment for low back pain long after Joseph Pilates died. Traditional Pilates exercises follow six basic principles: centering (i.e. tightening the 'powerhouse' (trunk muscles)), concentration (i.e. cognitive attention while performing the exercises), control (i.e. postural management while performing the exercises), precision (i.e. accuracy of exercise technique), flow (i.e. smooth transition of movements within the exercise sequence) and breathing in co‐ordination with the exercises (Wells 2012). A recent systematic review of Pilates exercises concluded that another principle should be added whenever these exercises are used in the treatment of LBP, which is posture (Wells 2012). Pilates exercises are usually prescribed by certified instructors. The exercises are considered to be similar to spinal stabilisation exercises (also known as motor control exercises); however, they do not involve conscious activation of specific muscles in the manner often used in spinal stabilisation exercises. During dynamic exercises in Pilates, co‐contraction of the multifidus (a deep back muscle), transversus abdominis (a deep abdominal muscle), pelvic floor and diaphragm muscles is observed. The goal of the co‐contraction of these muscles is to reduce joint compression and alter pelvic tilt (Bryan 2003; Gladwell 2006).
The Pilates method includes several stretching and strengthening exercises, which can be divided into two categories: mat Pilates (exercises performed on the ground, without any specific equipment) and exercises with the Pilates apparatus. The first exercises developed by Pilates were performed on the ground; he then created a series of apparatus on which to perform exercises against resistance provided by springs and pulleys (Musculino 2004; Queiroz 2005). The reported benefits of Pilates exercises include improvements in strength, range of motion, co‐ordination, balance, muscle symmetry, flexibility, proprioception (awareness of posture), body definition and general health (Bryan 2003; Gladwell 2006). The exercises are adapted to the condition of the patient and difficulty is gradually increased while respecting individual abilities and characteristics. The springs and pulleys of each apparatus can be used to make the exercises easier or more difficult to perform.
How the intervention might work
One biological rationale for how Pilates exercises might work is based upon the idea that stability and control of spinal muscles are altered in people with LBP (Hodges 1996). Two motor control impairments are proposed to occur in people with LBP: first the onset of activity of deep muscles such as the multifidus and transversus abdominis is delayed when the stability of the spine is challenged in dynamic tasks (Rackwitz 2006). Second, patients with LBP tend to compensate for this lack of stability by increasing the activity of superficial muscles (Hodges 1996; Rackwitz 2006), which increases the stiffness of the spine. The exercises advocated by the Pilates approach aim to target these two factors (i.e. improving the stability of the spine by improving the motor control of the deep muscles and reducing the activity of superficial muscles), as well as to improve posture and body awareness. These factors have the potential to improve pain, disability and quality of life in patients with LBP.
Why it is important to do this review
Over the last decade, the popularity of the Pilates method as an intervention for patients with LBP and other musculoskeletal conditions has steadily increased worldwide. There are published trials (Curnow 2009; Fonseca 2009; Gladwell 2006; Rajpal 2008; Rydeard 2006) and systematic reviews (Lim 2011; Miyamoto 2013; Posadzki 2011; Wells 2014) available on this topic. However, we are aware of new existing trials on this topic. Therefore, a well‐conducted systematic review is needed to better inform clinicians, patients and policy‐makers about the effectiveness of this intervention in patients with non‐specific LBP.
Objectives
To determine the effects of the Pilates method for patients with non‐specific acute, subacute or chronic low back pain.
Methods
Criteria for considering studies for this review
Types of studies
We only included randomised controlled trials in this review. We did not consider trials that used quasi‐random allocation procedures in this review to avoid biased estimates of treatment effects across the included studies (Higgins 2011).
Types of participants
Inclusion criteria:
-
Adult participants aged 16 or older with acute, subacute or chronic non‐specific LBP.
-
Patients recruited from primary, secondary or tertiary care; these patients could be either seeking care for back pain or recruited from the community.
Exclusion criteria:
-
Patients with any contraindication to exercise therapy.
-
Pregnancy.
-
Patients with serious spinal pathology (i.e. cancer, fracture, cauda equina syndrome and inflammatory diseases).
-
Trials that included more than 5% of participants with evidence of nerve root compromise.
Types of interventions
We considered any type of exercise therapy that followed the Pilates method. We judged trials to have evaluated Pilates when at least one of the following criteria was met:
-
The study explicitly stated that the intervention was based upon the Pilates principles (i.e. centering, concentration, control, precision, flow, breathing and posture) or at least three of these elements (Wells 2012).
-
The therapists who provided the interventions had previous training in Pilates exercises or the therapists were described as certified Pilates instructors.
Types of outcome measures
We included any type of clinically relevant measure that could be considered patient‐centred. We did not consider physiological and biomechanical variables (e.g. range of motion, motor control, muscle endurance) for this review.
Primary outcomes
-
Pain intensity measured by any reliable and valid self report outcome measure.
-
Disability measured by any reliable and valid self report outcome measure.
-
Global impression of recovery measured by any reliable and valid type of Global Perceived Effect Scale.
-
Quality of life (measured by any reliable and valid instrument).
Secondary outcomes
-
Return to work (measured by any reliable and valid instrument).
-
Adverse effects.
Search methods for identification of studies
Electronic searches
We searched for randomised controlled trials from the following electronic databases without restrictions on language or date of publication. We used the search strategies developed by the Cochrane Back Review Group. We searched all databases from the date of their inception to March 2014.
-
CENTRAL (Cochrane Central Register of Controlled Trials, The Cochrane Library, which contains the Back Group Trials Register) (Appendix 1).
-
MEDLINE (OvidSP, 1946 to March Week 2 2014) and MEDLINE In‐Process & Other Non‐Indexed Citations (OvidSP, March 24, 2014) (Appendix 2).
-
EMBASE (OvidSP, 1980 to 2014 Week 12) (Appendix 3).
-
CINAHL (Cumulative Index to Nursing and Allied Health Literature, EBSCO) (Appendix 4).
-
PEDro (Physiotherapy Evidence Database) (Appendix 5).
-
SPORTDiscus (EBSCO) (Appendix 6).
All databases were previously searched in March 2013. For the March 2014 search, we added MEDLINE In‐Process and Other Non‐Indexed Citations, we updated the EMBASE study design filter, we added a new term to the CINAHL strategy and we searched new fields in PEDro. Details can be found in the Appendices.
We performed an updated search in June 2015. We added one eligible study to the awaiting classification section and we will incorporate this in the next review update.
Searching other resources
We also searched the reference lists of eligible papers as well as trial registry websites: Australian and New Zealand Clinical Trials Registry (ANZCTR), National Research Registry, ClinicalTrials.gov, metaRegister of Controlled Trials (mRCT), Brazilian Registry of Clinical Trials (ReBEC) and the World Health Organization International Clinical Trials Registry Platform (WHO ICTRP). The search strategies for ClinicalTrials.gov and WHO ICTRP are described in Appendix 7.
Data collection and analysis
Selection of studies
Two pairs of review authors (CMNC and LCMC, BTS and TPY) independently screened titles and abstracts for potentially eligible studies. We used full‐text papers to determine the final inclusion in the review. We resolved disagreements between review authors through discussion or by the arbitration of a third review author (LOPC or CM) when consensus could not be reached. We included only full‐text papers, written in any language, regardless of the date of publication. We included papers written in English, Portuguese, Spanish, Italian and Dutch as the review team includes authors who are able to read these languages. We sent all remaining papers that were written in languages other than these to translators. We also scanned the reference lists from previous published reviews on Pilates as well as the reference lists from the eligible randomised trials.
Data extraction and management
Two independent review authors (TPY and BTS) extracted the following data from each of the eligible papers using a standardised data extraction form (Appendix 8). We resolved disagreements between review authors through discussion or by the arbitration of a third review author (CM).
-
Bibliometric data (authors, year of publication, language).
-
Study characteristics (study design, sample size, description of the sample, country, recruitment modality, funding).
-
Characteristics of the participants (gender, age, duration of symptoms, severity of the condition at baseline).
-
Description of the interventions (both experimental and control interventions), including dose (number of sessions, duration of each session of treatment, etc) and co‐interventions.
-
Duration of follow‐up assessments.
-
Outcomes assessed (converted to a common 0 to 100 scale when different scales were used).
-
Study results.
-
Time periods for outcome assessment: short‐term (less than three months after randomisation), intermediate‐term (at least three months but less than 12 months after randomisation) and long‐term (12 months or more after randomisation) follow‐up. When there were multiple time points that fell within the same category we used the one that was closer to the end of the treatment, six months and 12 months.
We pilot tested the data extraction form using two RCTs on back pain.
Assessment of risk of bias in included studies
We assessed the risk of bias in the included studies using the 'Risk of bias' assessment tool as recommended by The Cochrane Collaboration (Higgins 2011) and the Cochrane Back Review Group (Furlan 2009) (Appendix 9).
Two review authors (BTS and TPY) independently performed this 'Risk of bias' assessment and resolved possible disagreements between review authors by discussion, or arbitration by a third review author (CM) when consensus could not be reached. We scored each of the 12 items of the 'Risk of bias' assessment as 'high', 'low' or 'unclear' risk. We defined a study with an overall low risk of bias as having low risk of bias on six or more of these items.
We assessed clinical relevance by scoring five questions related to this domain as 'yes', 'no' or 'unclear' (Appendix 10). Two independent authors performed this and resolved possible disagreements by discussion, or arbitration by a third review author when consensus could not be reached.
Measures of treatment effect
We expected to deal mostly with continuous outcome measures to determine the treatment effect, such as pain intensity, disability or quality of life scales. For all continuous outcomes we quantified the treatment effects with the mean difference (MD). To accommodate the different scales used for these outcomes, we converted outcomes to a common 0 to 100 scale. We also expected to encounter dichotomous outcomes such as recovery or return to work and in such cases we calculated the risk ratios (RR) for experiencing the positive outcome. We used effect sizes and 95% confidence intervals (CI) as a measure of treatment effect. We considered between‐group differences of at least 20% as clinically important (Ostelo 2008). We used Review Manager 5 for all analyses. For effect sizes, we defined three levels as: small (MD < 10% of the scale), medium (MD 10% to 20% of the scale) or large (MD > 20% of the scale) (Rubinstein 2011) (Appendix 10).
Unit of analysis issues
We did not encounter any cross‐over or cluster‐randomised trials. To deal with repeated observations on participants we followed the advocated strategy of defining the outcomes (already stated previously) as well as the time points a priori (Higgins 2011). The time points were short‐term (less than three months after randomisation), intermediate‐term (at least three months but less than 12 months after randomisation) and long‐term (12 months or more after randomisation) follow‐up. When there were multiple time points that fell within the same category we used the one that was closer to the end of the treatment (short‐term), six months (intermediate‐term) and 12 months (long‐term). If studies included multiple treatment arms, we formed multiple treatment comparisons but if there was a shared group we split this in order to be able to include two (reasonably independent) comparisons.
Dealing with missing data
Firstly, review authors emailed the authors of each study requesting any necessary data that was not comprehensively reported in the manuscript. In cases where data were reported as a median and interquartile range (IQR), we assumed that the median is equivalent to the mean and the width of the IQR is equivalent to 1.35 times the standard deviation (Higgins 2011). We also estimated data from graphs in cases where this information was not presented in tables or text. If any information regarding standard deviations was missing, we calculated these from confidence intervals or standard errors (if available) of the same study. Finally, if no measure of variability was presented anywhere in the text, we estimated the standard deviation from the most similar trial in the review, taking the risk of bias of individual studies into consideration.
Assessment of heterogeneity
The assessment of heterogeneity was based upon visual inspections of the forest plots (e.g. overlapping confidence intervals) and more formally by the Chi2 test and the I2 statistic as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We combined results in a meta‐analysis using a random‐effects model if I2 < 50%. If substantial heterogeneity was present, we did not combine the results but instead presented them as a narrative synthesis. If I2 values were slightly higher than 50% but we identified no clear heterogeneity by visual inspection, we combined the results into a meta‐analysis.
Assessment of reporting biases
We performed comprehensive searches in order to reduce the possibility of reporting biases. We also planned to generate funnel plots (if we retrieved at least 10 trials) in order to determine possible reporting biases.
Data synthesis
We combined the results from individual trials through meta‐analysis. This pooling of the data was dependent on the level of statistical heterogeneity of the retrieved studies. We combined results in a meta‐analysis using a random‐effects model if the I2 value was less than 50%. If substantial statistical heterogeneity was present, we did not quantitatively pool the results but presented them as a narrative synthesis. If the I2 value was slightly higher than 50% but no clear clinical heterogeneity was detected by visual inspection we combined the results in a meta‐analysis.
Regardless of whether there were sufficient data available to use quantitative analyses to summarise the data, we assessed the overall quality of the evidence for each outcome. To accomplish this, we used the GRADE approach, as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) and adapted in the updated Cochrane Back Review Group method guidelines (Furlan 2009). Factors that may decrease the quality of the evidence are: study design and risk of bias (downgraded if more than 25% of the participants were from studies with a high risk of bias); inconsistency of results (downgraded if significant heterogeneity was present by visual inspection or if the I² value was greater than 50%); indirectness (generalisability of the findings; downgraded if more than 50% of the participants were outside the target group); imprecision (downgraded if fewer than 400 participants were included in the comparison for continuous data and there were fewer than 300 events for dichotomous data (Mueller 2007)) and other factors (e.g. reporting bias, publication bias). We considered single studies with fewer than 400 participants for continuous or dichotomous outcomes inconsistent and imprecise, providing 'low quality evidence', which could be downgraded to 'very low quality evidence' if there were further limitations on the quality of evidence (Rubinstein 2012). We reduced the quality of the evidence for a specific outcome by a level, according to the performance of the studies against these five factors and we described them as follows.
High quality evidence: there are consistent findings among at least 75% of RCTs with low risk of bias, consistent, direct and precise data and no known or suspected publication biases. Further research is unlikely to change either the estimate or our confidence in the results.
Moderate quality evidence: one of the domains is not met. Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low quality evidence: two of the domains are not met. Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low quality evidence: three of the domains are not met. We are very uncertain about the results.
No evidence: no RCTs were identified that addressed this outcome.
Subgroup analysis and investigation of heterogeneity
We stratified some of the analyses based upon a number of factors when necessary (Higgins 2011):
-
types of control groups (e.g. minimal intervention, placebo, another type of treatment, wait‐and‐see groups);
-
duration of follow‐up (i.e. short‐term, intermediate‐term and long‐term);
-
risk of bias (i.e. low and high risk of bias studies.
Sensitivity analysis
We did not plan to perform any sensitivity analyses as we anticipated that the number of studies and comparisons would be low. This turned out to be the case.
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of studies awaiting classification; Characteristics of ongoing studies.
Results of the search
The search retrieved 126 trials, of which nine fulfilled the inclusion criteria and were included in the review (a total pooled sample of 510 participants) (Figure 1).
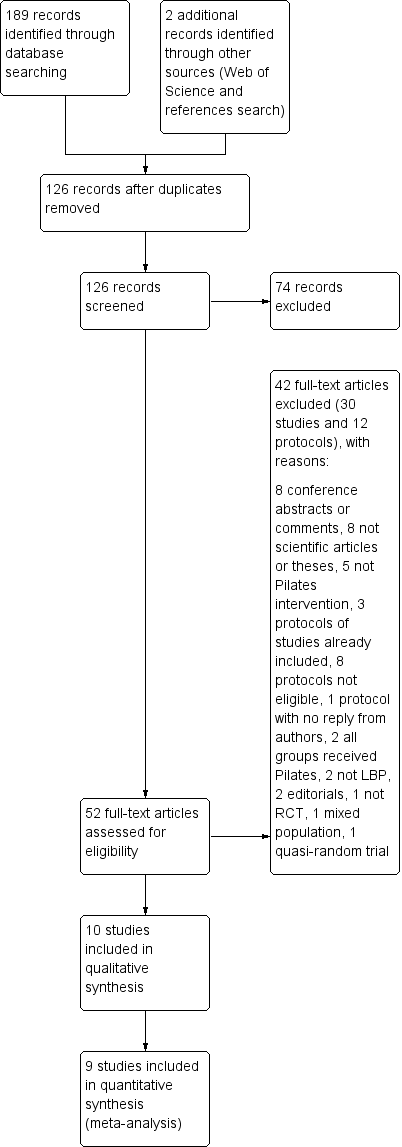
Study flow diagram.
A search for unpublished trials in ClinicalTrials.gov and the World Health Organization International Clinical Trials Registry Platform (WHO ICTRP) search portal revealed 13 records of trials evaluating Pilates for low back pain (LBP). Three records were for studies already included in this review (Marshall 2013; Miyamoto 2013; Wajswelner 2012) and eight were ineligible (three compared different forms of Pilates (NCT01533805, PACTR201211000443397, RBR‐7tyg5j), two were from populations not included in this review (e.g. military settings, children) (ACTRN12607000471482, NCT01711203), one included both groups performing Pilates exercise (NCT01919268), one included cervical pain (NCT01999283) and one is not a RCT (ACTRN12609000927224). Two registered trials appeared potentially eligible for this review (NCT01502059 and RBR‐7yhzym). We were able to find the published study for one of these records (NCT01502059) and we included the study in the review (Natour 2014). We did not find any publicly available report for the other record (RBR‐7yhzym), and the authors did not reply to our email contact attempts. For the additional updated search, one study fulfilled the inclusion criteria (Anand 2014) and we added it to the awaiting classification section to be incorporated in the next review update.
The 10 trials included in the review were conducted in five different countries: three were conducted in Australia (Brooks 2012; Marshall 2013; Wajswelner 2012), three in Brazil (Fonseca 2009; Miyamoto 2013; Natour 2014), two in the United Kingdom (Gladwell 2006; Quinn 2011), and one in each of Hong Kong (Rydeard 2006), and India (Rajpal 2008). All trials were published in English.
Included studies
A total of 510 participants were enrolled in the 10 included trials, of which we included data from 478 participants in the meta‐analyses. The study sample sizes ranged from 17 to 87 participants (median (IQR) = 41 (31.5)). One study was not included in the meta‐analysis because we found substantial heterogeneity in the comparison in which this study was included (Rajpal 2008).
The assessment of clinical relevance for each study is described in Table 1.
| Studies/criteria | Are the patients described in detail so that you can decide whether they are comparable to those that you see in your practice? | Are the interventions and treatment settings described well enough so that you can provide the same for your patients? | Were all clinically relevant outcomes measured and reported? | Is the size of the effect clinically important?* | Are the likely treatment benefits worth the potential harms? |
| Yes | Yes | Yes | No | Yes | |
| Yes | Yes | No | No | Yes | |
| Yes | Yes | Yes | No | Yes | |
| Yes | Yes | Yes | No | Yes | |
| Yes | Yes | Yes | Yes1 | Yes | |
| Yes | Yes | Yes | Yes1 | Yes | |
| Yes | Yes | Yes | Yes2 | Yes | |
| No | Yes | No | No | Yes | |
| Yes | Yes | Yes | No | Yes | |
| Yes | Yes | Yes | No | Yes |
*Clinical importance: consider 30% on VAS/NRS for pain intensity as clinically significant, and 2 to 3 points (or 8% to 12%) on the Roland‐Morris Disability Questionnaire for disability.
1Disability (short and intermediate‐term).
2Disability (short‐term).
Types of studies
We identified the following comparisons in this review: (i) six trials compared the Pilates method with minimal intervention or no intervention (Fonseca 2009; Gladwell 2006; Miyamoto 2013; Quinn 2011; Rydeard 2006; Natour 2014), and (ii) four trials compared the Pilates method with other types of exercises, including general exercise (Brooks 2012; Marshall 2013; Wajswelner 2012), and the McKenzie method (Rajpal 2008). We did not include studies evaluating two types of Pilates (e.g. mat Pilates versus equipment‐based Pilates) as the aim of this review was to provide evidence on the effectiveness of the Pilates method for low back pain; thereby we focused our comparisons on no intervention, placebo or other interventions.
Study population
Most participants in the included trials were middle‐aged (mean: 38 years), ranging from 22 to 50 years of age. Two trials included only women participants (Quinn 2011; Rajpal 2008), and all the other trials included both men and women. All trials included exclusively chronic participants (low back pain persisting for 12 weeks or more), except for one trial that included participants with LBP for at least six weeks (Rydeard 2006).
Technique: number and duration of treatments
The duration of the treatment programmes in the included trials ranged from 10 days to 90 days. One trial provided treatment twice a week for a total of 90 days (Natour 2014). In four trials, the participants received an eight‐week programme. In two of the four trials the frequency of treatment was three times per week (Brooks 2012; Marshall 2013), one trial provided treatment twice a week (Fonseca 2009), and the other one provided treatment once a week (Quinn 2011). In three trials the treatment duration was six weeks, with two trials evaluating treatment provided twice a week (Miyamoto 2013; Wajswelner 2012), and one trial evaluating treatment delivered once a week (Gladwell 2006). Two trials performed the treatment for four weeks, one included daily sessions (Rajpal 2008), and the other provided treatment three times per week (Rydeard 2006). The duration of all sessions was approximately one hour for all included studies. The mean number of sessions in the included studies was 15.3, ranging from six to 30 sessions.
Primary outcomes
Pain intensity
All studies measured pain intensity. In most cases, pain intensity was measured with a visual analogue scale (VAS) or numerical rating scale (NRS), and one study used the 0 to 5 point Roland Morris pain rating visual analogue scale (RMVAS) (Gladwell 2006). We converted all scales to a 0 to 100‐point scale.
Disability
Seven studies measured disability (Brooks 2012; Gladwell 2006; Marshall 2013; Miyamoto 2013; Quinn 2011; Rydeard 2006; Wajswelner 2012). Four studies measured disability with the Roland Morris Disability Questionnaire (Miyamoto 2013; Quinn 2011; Rydeard 2006, Natour 2014). Three studies used the Oswestry Disability Index for measuring disability (Brooks 2012; Gladwell 2006; Marshall 2013), and one study used the Quebec Disability scale (Wajswelner 2012). We converted all scales to a 0 to 100‐point scale.
Global impression of recovery
One study measured global impression of recovery using a Global Perceived Effect Scale (Miyamoto 2013).
Quality of life
Two studies measured quality of life, but the data from the physical and mental components were not available in the text and the authors did not provide this information on request (Natour 2014; Wajswelner 2012).
Secondary outcomes
We considered return to work and adverse effects as secondary outcomes in this review; however, none of the included studies reported these outcomes.
Other outcomes
Function
Two studies measured function using the Patient Specific Functional Scale (Miyamoto 2013; Wajswelner 2012).
Follow‐up
All studies measured short‐term follow‐up, which varied from four to eight weeks. Three studies measured intermediate follow‐up, from three to six months (Marshall 2013; Miyamoto 2013; Wajswelner 2012). None of the included studies measured follow‐up beyond six months.
Excluded studies
We excluded 42 studies in the full‐text assessment for eligibility (30 full text articles and 12 protocols). Of the 30 full text articles excluded, eight were conference abstracts, presentations or comments (Anderson 2006; Boden 2010; Cámara 2011; Kennedy 2012; Natour 2011; O'Brien 2006; SeQueira 2010; Xue‐Qiang 2013); five were magazine articles (Jaecks 2004; Kagan 2008; Parker 2010; Robinson 2007; Sparrowe 2007), two were theses (Anderson 2005; Gagnon 2005), and one was an opinion piece (Ickes 2007). In five studies, the intervention was not Pilates exercise (Mehling 2005; Rasmussen‐Barr 2003; Sherman 2010; Tekur 2008; Tilbrook 2011). In two studies both groups received Pilates or different forms of Pilates were tested (Curnow 2009; da Luz 2014). Two studies did not recruit LBP patients (Alves 2012; Phrompaet 2011), and two were editorials (McNeill 2009; McNeill 2010). One study included a mixed population of healthy participants and those who had LBP (Hides 2012), one study used a quasi‐random allocation procedure (Donzelli 2006), and one was a case report study (Blum 2002). Of the 12 protocols excluded, three records were for studies already included in this review (Marshall 2013; Miyamoto 2013; Wajswelner 2012) and eight were ineligible (NCT01533805;PACTR201211000443397;RBR‐7tyg5j; ACTRN12607000471482; NCT01711203; NCT01919268; NCT01999283; ACTRN12609000927224), and for one report we did not find any publicly available report (RBR‐7yhzym) and the authors did not reply to our email contact attempts.
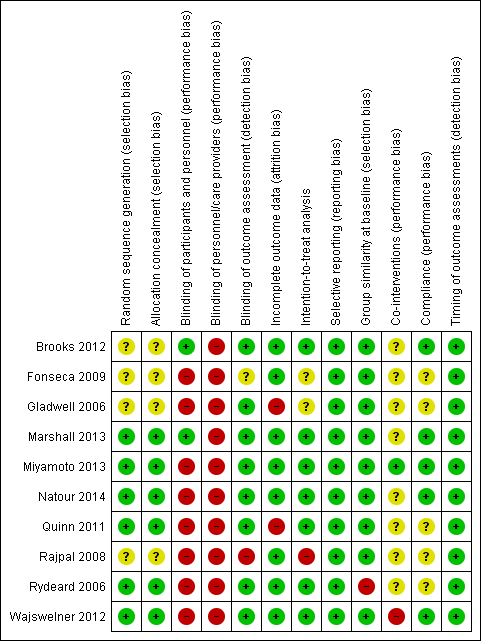
Risk of bias in included studies
The results from the 'Risk of bias' assessment for the individual studies are summarised in Figure 2. In total, we considered 70% of the studies to have a low risk of bias, which represents 83.7% of all participants.
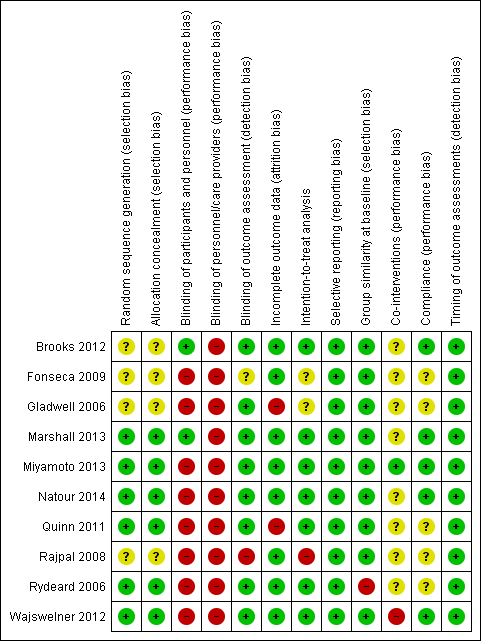
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
More than half of the included trials met the criteria for allocation (Marshall 2013; Miyamoto 2013; Natour 2014; Quinn 2011; Rydeard 2006; Wajswelner 2012). In four trials there was no information about the randomisation and allocation procedures (Brooks 2012; Fonseca 2009; Gladwell 2006; Rajpal 2008).
Blinding
One trial blinded both participants and assessors (Brooks 2012). One trial blinded only the participants (Marshall 2013), and seven trials blinded only the assessor (Gladwell 2006; Miyamoto 2013; Natour 2014; Quinn 2011; Rydeard 2006; Wajswelner 2012). In one trial the information about blinding was unclear (Fonseca 2009), and one trial did not blind both the assessor and patients (Rajpal 2008). Presumably, blinding of therapists was not possible for the intervention proposed.
Incomplete outcome data
A total of eight trials provided adequate information about missing data and were able to keep these below 20% for short and intermediate‐term outcomes, though none of the trials report long‐term follow‐up (Brooks 2012; Fonseca 2009; Marshall 2013; Miyamoto 2013; Natour 2014; Rajpal 2008; Rydeard 2006; Wajswelner 2012). Two trials exceeded the maximum of 20% withdrawals, with about 30% for both trials (Gladwell 2006; Quinn 2011).
Selective reporting
Published or registered protocols were available for four trials (Marshall 2013; Miyamoto 2013; Natour 2014; Wajswelner 2012); all were registered at the Australian and New Zealand Clinical Trials Registry. For one trial the protocol was also published (Miyamoto 2013). Trials for which it was not possible to find the protocols, but it was clear that all expected outcomes were included or were reported in a pre‐specified way, fulfilled this criterion. We considered all included studies at low risk of bias for this criterion.
Other potential sources of bias
Publication bias
We did not assess publication bias with funnel plots because too few studies were included in the meta‐analysis.
Effects of interventions
See: Summary of findings for the main comparison ; Summary of findings 2
See: summary of findings Table for the main comparison for the effect of Pilates versus minimal intervention, and summary of findings Table 2 for the effect of Pilates versus other exercises.
Effect of Pilates versus minimal intervention
We included a total of six trials in the meta‐analysis (Fonseca 2009; Gladwell 2006; Miyamoto 2013; Natour 2014; Quinn 2011; Rydeard 2006); four trials with low risk of bias (Miyamoto 2013; Natour 2014; Quinn 2011; Rydeard 2006) and two with high risk of bias (Fonseca 2009; Gladwell 2006). Most of the trials included in the comparison of Pilates with minimal intervention had small sample sizes (ranging from 17 to 86 participants).
Primary outcomes
For pain intensity, based on six trials, there is low quality evidence (downgraded due to imprecision and risk of bias) that Pilates reduces pain compared with minimal intervention at short‐term follow‐up, with a medium effect size (mean difference (MD) –14.05, 95% confidence interval (CI) –18.91 to –9.19; P value < 0.001) (Analysis 1.1). At intermediate‐term follow‐up, two trials, Miyamoto 2013 and Natour 2014, provided moderate quality evidence (downgraded due to imprecision) that Pilates reduces pain compared with minimal intervention, with a medium effect size (MD –10.54, 95% CI –18.54 to –2.62) (Analysis 1.1; Figure 3).

Forest plot of comparison: 1 Pilates versus minimal intervention, outcome: 1.1 Pain.
We considered disability for the meta‐analysis as we did not find considerable heterogeneity (I2 = 56%), but we downgraded the quality of the evidence due to inconsistency (Borenstein 2009; Higgins 2011). Based on five trials, there is low quality evidence (downgraded due to imprecision and inconsistency) that Pilates improves disability at short‐term follow‐up compared with minimal intervention, with a small effect size (MD –7.95, 95% CI –13.23 to –2.67; P value = 0.003) (Analysis 1.2). At intermediate‐term follow‐up, two trials, Miyamoto 2013 and Natour 2014, provided moderate quality evidence (downgraded due to imprecision) of a significant effect in favour of Pilates, with a medium effect size (MD –11.17, 95% CI –18.41 to –3.92) (Analysis 1.2).
Based on one trial, Miyamoto 2013, and low quality evidence (downgraded due to imprecision and inconsistency), we found a significant short‐term effect, with a small effect size for global impression of recovery (MD 1.50, 95% CI 0.70 to 2.30) (Analysis 1.4), but not for intermediate‐term follow‐up. One trial (Natour 2014) evaluated quality of life but the estimates for the physical and mental components were not available in the publication and the authors did not provide this information on request.
Secondary outcomes
Only one trial assessed adverse events, but none were reported (Miyamoto 2013). None of the included trials evaluated return to work.
Other outcomes
Based on one trial, Miyamoto 2013, and low quality evidence (downgraded due to imprecision and inconsistency), there is a significant short‐term effect, with a small effect size, for function (MD 1.10, 95% CI 0.23 to 1.97) (Analysis 1.3). No differences was found for an intermediate‐term follow‐up.
Effect of Pilates versus other exercises
Four trials were included in this comparison (Brooks 2012; Marshall 2013; Rajpal 2008; Wajswelner 2012), and three were included in the meta‐analysis (Brooks 2012; Marshall 2013; Wajswelner 2012). Two trials compared Pilates with general exercise (Brooks 2012; Wajswelner 2012), and one trial compared Pilates with stationary cycling exercise (Marshall 2013). Most of the trials included in the comparisons between Pilates and other exercises had small sample sizes (ranging from 32 to 87 participants).
Primary outcomes
Due to the high level of heterogeneity, we did not combine the results for pain intensity at short‐term and intermediate‐term follow‐up in a meta‐analysis (I2 = 74% for short‐term and I2 = 86% for intermediate‐term follow‐up), but we report these descriptively. For pain intensity, based on low quality evidence (downgraded due to imprecision and inconsistency), at short‐term follow‐up two trials demonstrated significant effect in favour of Pilates (Brooks 2012; Rajpal 2008), and one trial did not find significant difference (Wajswelner 2012). At intermediate‐term follow‐up, based on low quality evidence (downgraded due to imprecision and inconsistency), one trial reported a significant effect in favour of Pilates (Marshall 2013), and one trial reported a non‐significant difference in pain intensity (Wajswelner 2012).
In the meta‐analysis for disability there is moderate quality evidence (downgraded due to imprecision) that there is no significant difference between Pilates and other exercise at short‐term (MD –3.29, 95% CI –6.82 to 0.24) or intermediate‐term follow‐up (MD –0.91, 95% CI –5.02 to 3.20), based on two studies for each comparison (Analysis 2.2; Figure 4). One trial (Wajswelner 2012) evaluated quality of life but the estimates for the physical and mental components were not available in the publication and the authors did not provide this information on request.

Forest plot of comparison: 2 Pilates versus other exercises, outcome: 2.2 Disability.
Secondary outcomes
One trial reported minor adverse events in both groups (Wajswelner 2012). In the Pilates group two participants reported minor shoulder pain and one reported knee pain, but they were all able to continue the exercises. In the general exercise group, two participants reported back spasms but were able to continue the programme, and two reported worsening back pain causing them to cease the exercise. None of the included trials evaluated return to work.
Other outcomes
Based on low quality evidence (downgraded due to imprecision and inconsistency) from one trial (Wajswelner 2012), there was no significant difference between Pilates and other exercises in function at short‐term follow‐up (MD 0.10, 95% CI ‐2.44 to 2.64). However, there was a significant effect in favour of other exercises (general exercise) in intermediate‐term function, with a small effect size (MD ‐3.60, 95% CI ‐7.00 to ‐0.20) (Analysis 2.3).
Discussion
Summary of main results
The evidence on the effectiveness of Pilates for chronic non‐specific low back pain (LBP) is of low to moderate quality primarily because there are only a few small studies (range 17 to 87 participants). Of the 15 estimates of treatment effect we provide in this review, only eight are based on more than one study. None of the trials reported long‐term outcomes, which would be important to consider for patients with chronic LBP. In addition, we did not find any studies that investigated the effectiveness of Pilates for acute and subacute LBP.
A total of six trials (n = 265 participants) compared Pilates to minimal intervention. At short‐term follow‐up Pilates is more effective than minimal intervention for improvement in pain intensity, disability, function and global impression of recovery. At intermediate‐term follow‐up Pilates led to better pain intensity and disability outcomes, but was not superior to minimal intervention in terms of function and global impression of recovery. The effect sizes varied from small to medium for this comparison.
Four trials (n = 245 participants) compared Pilates to other exercises. Pilates appears not to be more effective than other exercises for pain intensity and disability outcomes. For function, one study found a small significant effect at intermediate‐term, but not at short‐term follow‐up.
Pilates appears to be an effective treatment compared to minimal intervention, but when compared to other types of exercises the effect sizes tend to be smaller or no difference in effectiveness is observed. This is in accordance with clinical practice guidelines (European Guidelines 2006) and previous reviews of exercise for low back pain (Hayden 2005), which recommend exercise therapy for patients with low back pain but note that there seems to be no clear difference in effectiveness between the various forms of exercise. We did not find any studies that reported return to work. Only two trials assessed adverse events: one trial found minor adverse effects in the Pilates group (shoulder and knee pain) (Wajswelner 2012); another trial did not find any adverse events (Miyamoto 2013).
Overall completeness and applicability of evidence
The trials included in this review were conducted in Australia, South America, Europe or Asia, with adult participants from primary or tertiary care with non‐specific low back pain for at least 12 weeks in most trials. The care providers were all experienced instructors or physiotherapists trained in the Pilates method, except for one trial that did not provide information about the care provider (Rajpal 2008). Therefore, we can generalise the results of this review to a range of settings. Regarding our clinical relevance assessment, most trials included provided a clear description of the patients, outcomes and interventions used. However, none of the trials found a clinically important effect size for pain intensity and only three reported a clinically important effect for disability (Miyamoto 2013; Natour 2014; Quinn 2011).
Quality of the evidence
In general, most included trials demonstrated a low risk of bias (427 participants were from studies with low risk of bias out of 510 participants in total). The most affected items were blinding of participants and care providers, which is understandable for exercise intervention trials. However, only 10 trials could be included in this review, which compromises the quality of the evidence provided. Also, the sample sizes in general were small (ranging from 17 to 87 participants); therefore, our results cannot be considered robust.
Potential biases in the review process
The main limitation of this review is the low number of trials and small sample sizes per comparison, outcome and follow‐up period, which prevented us from conducting a sensitivity analyses. An additional limitation is the potential for publication bias in the trials included. In this review, it was not possible to assess publication bias using funnel plots as too few studies were included. However, by inspecting registries we found one completed trial (from 2011) that was not yet published, which may indicate potential publication bias. Moreover, the source of funding should be considered due to potential financial conflicts from industry‐sponsored research (Bekelman 2003; Okike 2008). One trial received funding from a Pilates clinic to conduct the study (Wajswelner 2012). The remaining trials were not funded.
Finally, we found eight conference abstracts and for these we could not find a full publication. They were therefore not included in the analysis. We also did not include two theses. As unpublished studies are more likely to report negative findings, it is possible that the review's conclusions are overly optimistic.
Agreements and disagreements with other studies or reviews
In general, the results of this review are reasonably consistent with previous reviews regarding pain intensity and disability outcomes (Lim 2011; Miyamoto 2013; Wells 2014). In the most recent review, the authors reported a statistically significant short‐term effect for pain intensity and disability compared to usual care and/or physical activity (Wells 2014). For the comparison with other forms of exercises, the results were conflicting. The results of this review are partially consistent with our findings. The key limitation of this review is that the authors did not perform a meta‐analysis, limiting the comparison with our review.
In the 2013 review of Miyamoto et al the authors found a small short‐term effect on pain intensity and disability when compared to minimal intervention but not compared to other types of exercises (Miyamoto 2013). This is consistent with our review although we mostly found medium effect sizes for the comparison with minimal intervention and we considered the results for pain intensity compared to other exercises too heterogeneous to be combined in a meta‐analysis. The 2011 review of Lim et al only found a small significant effect on pain intensity in the short term compared to minimal intervention but not on disability (Lim 2011). This previous review did not find any significant effect for the comparison with other exercises; however, the authors included only one trial (Donzelli 2006) and one thesis (Gagnon 2005) in this comparison. Another systematic review concluded that no definite conclusions can be drawn except that further better quality research is needed (Posadzki 2011). The authors only had four trials available in their review, each one with a different control group, making any comparison or conclusions difficult.
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: 1 Pilates versus minimal intervention, outcome: 1.1 Pain.

Forest plot of comparison: 2 Pilates versus other exercises, outcome: 2.2 Disability.

Comparison 1 Pilates versus minimal intervention, Outcome 1 Pain.

Comparison 1 Pilates versus minimal intervention, Outcome 2 Disability.

Comparison 1 Pilates versus minimal intervention, Outcome 3 Function.

Comparison 1 Pilates versus minimal intervention, Outcome 4 Global impression of recovery.

Comparison 2 Pilates versus other exercises, Outcome 1 Pain.

Comparison 2 Pilates versus other exercises, Outcome 2 Disability.

Comparison 2 Pilates versus other exercises, Outcome 3 Function.
| Pilates compared with minimal intervention for low back pain | ||||||
| Patient or population: patients with low back pain Settings: primary or tertiary care Intervention: Pilates Comparison: minimal intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Minimal intervention | Pilates | |||||
| Pain NRS: scale from 0 to 100 (worse pain) Follow‐up: short‐term (less than 3 months from randomisation) | The mean pain at short‐term follow‐up ranged across control groups from 33.9 to 52 points | The mean pain at short‐term follow‐up in the intervention groups was (18.9 to 9.2 lower) | Mean difference ‐14.05 (‐18.91 to ‐9.19) | 265 participants | ⊕⊕⊝⊝ | This is a moderate effect that is clinically relevant in this patient group |
| Pain NRS: scale from 0 to 100 (worse pain) Follow‐up: intermediate‐term (more than 3 months and less than 12 months) | The mean pain at intermediate‐term follow‐up ranged across control groups from 53 to 58.3 points | The mean pain at intermediate‐term follow‐up in the intervention group was 10.5 lower (18.5 to 2.6 lower) | Mean difference ‐10.54 (‐18.46 to ‐2.62) | 146 participants (2 studies) | ⊕⊕⊕⊝ | This is a moderate effect that is clinically relevant in this patient group |
| Disability Multiple scales: scale from 0 to 100 (worse disability) Follow‐up: short‐term (less than 3 months from randomisation) | The mean disability at short‐term follow‐up ranged across control groups from 13.3 to 44.1 points | The mean disability at short‐term follow‐up in the intervention groups was 7.95 lower (13.2 to 2.7 lower) | Mean difference ‐7.95 (‐13.23 to ‐2.67) | 248 participants (5 studies) | ⊕⊕⊝⊝ | This is a small effect that may be clinically relevant in this patient group |
| Disability Multiple scales: scale from 0 to 100 (worse disability) Follow‐up: intermediate‐term (more than 3 months and less than 12 months) | The mean disability at intermediate‐term follow‐up ranged across control groups from 27.9 to 44.4 points | The mean disability at intermediate‐term follow‐up in the intervention groups was (18.4 to 3.9 lower) | Mean difference ‐11.17 (‐18.41 to ‐3.92) | 146 participants (2 study) | ⊕⊕⊕⊝ | This is a moderate effect that is clinically relevant in this patient group |
| Function Patient Specific Functional Scale: used in a 11‐point scale from 0 to 10 (greater functional ability) Follow‐up: short‐term (less than 3 months from randomisation) | The mean function at short‐term follow‐up in the control group was 6.4 points | The mean function at short‐term follow‐up in the intervention group was 1.1 higher (0.2 to 2.0 higher) | Mean difference 1.10 (0.23 to 1.97) | 86 participants (1 study) | ⊕⊕⊝⊝ | This is a small effect that may be clinically relevant in this patient group (results from 1 single study) |
| Function Patient Specific Functional Scale: used in a 11‐point scale from 0 to 10 (greater functional ability) Follow‐up: intermediate‐term (more than 3 months and less than 12 months) | The mean function at intermediate‐term follow‐up in the control group was 6.1 points | The mean function at intermediate‐term follow‐up in the intervention group was 0.8 higher (0.0 lower to 1.6 higher) | Mean difference 0.80 (‐0.00 to 1.60) | 86 participants (1 study) | ⊕⊕⊝⊝ | The difference is not statistically or clinically significant (results from 1 single study) |
| Global impression of recovery Global Perceived Effect Scale: scale from ‐5 to +5 (greater recovery) Follow‐up: short‐term (less than 3 months from randomisation) | The mean global impression of recovery at short‐term follow‐up in the control group was 1.7 points | The mean global impression of recovery at short‐term follow‐up in the intervention group was 1.5 higher (0.7 to 2.3 higher) | Mean difference 1.50 (0.70 to 2.30) | 86 participants (1 study) | ⊕⊕⊝⊝ | This is a small effect that may be clinically relevant in this patient group (results from 1 single study) |
| Global impression of recovery Global Perceived Effect Scale: scale from ‐5 to +5 (greater recovery) Follow‐up: intermediate‐term (more than 3 months and less than 12 months) | The mean global impression of recovery at intermediate‐term follow‐up in the control group was 1.7 points | The mean global impression of recovery at intermediate‐term follow‐up in the intervention group was 0.7 higher (0.1 lower to 1.5 higher) | Mean difference 0.70 (‐0.11 to 1.51) | 86 participants (1 study) | ⊕⊕⊝⊝ | The difference is not statistically or clinically significant (results from 1 single study) |
| Adverse events | See comment | See comment | Not estimable | See comment | Only 1 included trial assessed adverse events and none were reported | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one level due to imprecision (fewer than 400 participants, total). 2 Downgraded one level due to risk of bias (> 25% of the participants were from studies with a high risk of bias). 3Downgraded one level due to clear inconsistency of results. 4Downgraded one level due to inconsistency (I² > 50%). | ||||||
| Pilates compared with other exercises for low back pain | ||||||
| Patient or population: participants with low back pain Settings: primary and tertiary care Intervention: Pilates Comparison: other exercises | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Other exercises | Pilates | |||||
| Pain NRS: scale from 0 to 100 (worse pain) Follow‐up: short‐term (less than 3 months from randomisation) | Not estimated | Not estimated | Not estimated | 181 participants (3 studies) | ⊕⊕⊝⊝ | Pooled results not estimated due to high heterogeneity |
| Pain NRS: scale from 0 to 100 (worse pain) Follow‐up: intermediate‐term (more than 3 months and less than 12 months) | Not estimated | Not estimated | Not estimated | 151 participants (2 studies) | ⊕⊕⊝⊝ | Pooled results not estimated due to high heterogeneity |
| Disability Multiple scales: scale from 0 to 100 (worse disability) Follow‐up: short‐term (less than 3 months from randomisation) | The mean disability at short‐term follow‐up ranged across control groups from 17.1 to 20 points | The mean disability at short‐term follow‐up in the intervention groups was (6.8 lower to 0.2 higher) | Mean difference ‐3.29 (‐6.82 to 0.24) | 149 participants (2 studies) | ⊕⊕⊕⊝ | The difference is not statistically or clinically significant |
| Disability Multiple scales: scale from 0 to 100 (worse disability) Follow‐up: intermediate‐term (more than 3 months and less than 12 months) | The mean disability at intermediate‐term follow‐up ranged across control groups from 13 to 18.1 points | The mean disability at intermediate‐term follow‐up in the intervention groups was (5.0 lower to 3.2 higher) | Mean difference ‐0.91 (‐5.02 to 3.20) | 151 participants (2 studies) | ⊕⊕⊕⊝ | The difference is not statistically or clinically significant |
| Function Patient Specific Functional Scale: scale from 0 to 30 (greater functional ability) Follow‐up: short‐term (less than 3 months from randomisation) | The mean function at short‐term follow‐up in the control group was 18.9 points | The mean function at short‐term follow‐up in the intervention group was 0.1 lower (2.4 lower to 2.6 higher) | Mean difference 0.10 (‐2.44 to 2.64) | 87 participants (1 study) | ⊕⊕⊝⊝ | The difference is not statistically or clinically significant (results from 1 single study) |
| Function Patient Specific Functional Scale: scale from 0 to 30 (greater functional ability) Follow‐up: intermediate‐term (more than 3 months and less than 12 months) | The mean function at intermediate‐term follow‐up in the control group was 22.8 points | The mean function at intermediate‐term follow‐up in the intervention group was 3.6 lower (7 to 0.2 lower) | Mean difference ‐3.60 (‐7.00 to ‐0.20) | 87 participants (1 study) | ⊕⊕⊝⊝ | This is a small effect that may be clinically relevant in this patient group (results from 1 single study) |
| Adverse events | See comment | See comment | Not estimable | See comment | 1 trial assessed adverse events and reported minor events | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one level due to imprecision (fewer than 400 participants, total). 2Downgraded one level due to inconsistency (I² > 50%). 3Downgraded one level due to clear inconsistency of results. | ||||||
| Studies/criteria | Are the patients described in detail so that you can decide whether they are comparable to those that you see in your practice? | Are the interventions and treatment settings described well enough so that you can provide the same for your patients? | Were all clinically relevant outcomes measured and reported? | Is the size of the effect clinically important?* | Are the likely treatment benefits worth the potential harms? |
| Yes | Yes | Yes | No | Yes | |
| Yes | Yes | No | No | Yes | |
| Yes | Yes | Yes | No | Yes | |
| Yes | Yes | Yes | No | Yes | |
| Yes | Yes | Yes | Yes1 | Yes | |
| Yes | Yes | Yes | Yes1 | Yes | |
| Yes | Yes | Yes | Yes2 | Yes | |
| No | Yes | No | No | Yes | |
| Yes | Yes | Yes | No | Yes | |
| Yes | Yes | Yes | No | Yes | |
| *Clinical importance: consider 30% on VAS/NRS for pain intensity as clinically significant, and 2 to 3 points (or 8% to 12%) on the Roland‐Morris Disability Questionnaire for disability. 1Disability (short and intermediate‐term). 2Disability (short‐term). | |||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain Show forest plot | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Short‐term (< 3/12 months from randomisation) | 6 | 265 | Mean Difference (IV, Random, 95% CI) | ‐14.05 [‐18.91, ‐9.19] |
| 1.2 Intermediate‐term (more than 3/12 months, less than 12/12 months) | 2 | 146 | Mean Difference (IV, Random, 95% CI) | ‐10.54 [‐18.46, ‐2.62] |
| 2 Disability Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Short‐term (< 3/12 months from randomisation) | 5 | 248 | Mean Difference (IV, Random, 95% CI) | ‐7.95 [‐13.23, ‐2.67] |
| 2.2 Intermediate‐term (more than 3/12 months, less than 12/12 months) | 2 | 146 | Mean Difference (IV, Random, 95% CI) | ‐11.17 [‐18.41, ‐3.92] |
| 3 Function Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Short‐term (< 3/12 months from randomisation) | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Intermediate‐term (more than 3/12 months, less than 12/12 months) | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Global impression of recovery Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Short‐term (< 3/12 months from randomisation) | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Intermediate‐term (more than 3/12, less than 12/12 months) | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Short‐term (< 3/12 months from randomisation) | 3 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Intermediate‐term (more than 3/12, less than 12/12 months) | 2 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Disability Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Short‐term (< 3/12 months from randomisation) | 2 | 149 | Mean Difference (IV, Random, 95% CI) | ‐3.29 [‐6.82, 0.24] |
| 2.2 Intermediate‐term (more than 3/12, less than 12/12 months) | 2 | 151 | Mean Difference (IV, Random, 95% CI) | ‐0.91 [‐5.02, 3.20] |
| 3 Function Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Short‐term (< 3/12 months from randomisation) | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Intermediate‐term (more than 3/12, less than 12/12 months) | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |

