Intervenciones no farmacológicas para la prevención de la pérdida de puestos de trabajo en trabajadores con artritis inflamatoria
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT | |
| Participants | Participants were employed people with a rheumatic disease who were at risk for job loss and resided in eastern Massachusetts. Participants were recruited through letters from rheumatologists. Randomized: 242 participants, 122 in experimental group (I) and 120 in control group (C). Baseline characteristics: female 81.2% vs 81.7%, overall 81%; age 50 (9.4) vs 49 (9.8), overall 49 (range 24 to 66); education beyond high school 39.2% vs 31.2%, overall 35% (n = 85); work type professional/managerial 35.2% vs 30.8%, overall 33% (n = 80); HAQ score functional limitation, mean 0.51(0.4) vs 0.57 (0.4), overall 0.54 (range 0‐1.7) judged as 'mild limitation' in patients with RA; IA 63.9% vs 62.5%. Type of rheumatic disease not provided, overall (in experimental and control group): RA (n = 142), OA (n = 53), SLE (n = 36), AS (n = 8), PsA (n = 3). Duration arthritis: unknown. All participants were either full time or part time employed and at 'work' at baseline, i.e. none were on either short term or long term disability leave (personal communication with first author). Previous job loss: unknown; previous sick leave: unknown. | |
| Interventions | Intervention group: Job retention vocational rehabilitation provided by one of two rehabilitation counsellors during two 1.5‐hour sessions (or more) over a five‐month period. Intervention development was based on previous research findings and experience from rehabilitation counsellors. The intervention consisted of three components: (1) job accommodation, (2) vocational counselling and guidance, and (3) education and self‐advocacy.
The counsellors also gave the participants in the experimental group copies of pamphlets and flyers about how to manage health‐related employment problems and about other available resources. Training professionals: The job retention vocational rehabilitation intervention was developed and delivered by one of two experienced rehabilitation counsellors employed by the study; both counsellors had several years of experience, but no particular expertise in job retention vocational rehabilitation. Control group: Written information: Participants were given copies of the same pamphlets and flyers about how to manage health related employment problems and available resources that the experimental group participants received. These materials were mailed to the home addresses of the control group participants within one month after randomisation. | |
| Outcomes | 1) Job loss: follow‐up at 6 months intervals up to 48 months:
Job loss could be due to all health or arthritis related reasons. 2) Sickness absenteeism: not reported 3) Work functioning: not reported | |
| Notes | This study was run in a community setting. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Strata allocation lists were generated by the statistician and included in an Access database in such a way that treatment assignment was revealed only after a participant's characteristics were entered into the database." No further information regarding random sequence generation. |
| Allocation concealment (selection bias) | Low risk | See above: Using Access database, treatment assignment was revealed only after participants characteristics were entered in database. |
| Prognostic comparability baseline | Unclear risk | Baseline differences were minimal, though baseline information on sickness absenteeism was absent. HAQ scores were in same range (Table 1, Allaire 2003). |
| Blinding of participants and personnel (performance bias) | Low risk | Personal communication with first author: 16 August2013: "Patients were not told whether they had received either the experimental or control intervention; in enrolling subjects, patients were told we were testing two different ways of helping people stay employed. The counsellors provided intervention to experimental group subjects only and did not know or have any contact with control group subjects. Whether subjects told their work colleagues about their study participation remains doubtful." Employers were not involved in any way in Allaire's trial. |
| Blinding of outcome assessment (detection bias) | Low risk | Personal communication with first author: 16 August 2013: "The researcher was blinded as to which subjects were in each group (she had little contact with any subjects – only brief contact with a few who called with a question when the research assistant was away)". Allaire 2005: "A professional data collector hired for the study collected the data by telephone." Overall the assessment of job loss was assessed by patients self report and judged low risk of bias. |
| Incomplete outcome data (attrition bias) | Low risk | Allaire originally had a 36‐month follow‐up which was extended with an additional year of follow‐up. The main findings of this review are based on the outcomes of 12 and 24 months: in this time frame attrition was low. Recruitment was staggered and as a consequence not all participants were able to complete the 36 or 48 month follow‐up. During the original 36 months follow‐up 4 participants dropped out of the intervention group and 6 from the control group, and one patient died in each group. The total reported attrition rate one year later, at 48 months, by Allaire was 18% in the intervention and 20% in the control groups. Allaire reported that most of the drop outs were participants who choose not to participate in the additional year of follow‐up (up to 48 months). |
| Selective reporting (reporting bias) | Low risk | Study protocol is not available but given target of intervention ('job retention') and the primary outcome 'job loss' we consider reporting bias not likely. |
| Compliance | Unclear risk | Not documented in the trial text. |
| Methods | RCT | |
| Participants | Participants were people with a paid job (full time or part time, on sick leave, or with partial disability pension) with chronic rheumatic disease (RA, AS, PA, other) with a self‐perceived disease‐related work problem threatening their ability to work. Participants were recruited at 11 hospital outpatient rheumatology departments near Leiden, The Netherlands. Randomized: 140 participants, 74 in experimental group (I) and 66 in control group (C). Baseline characteristics were: female 41 (55%) vs 38 (58%), age 43 (21 to 57) vs 44 (24 to 58); educational level High 15 (20%) Medium 37 (50%) Low 22 (30%) vs 10 (15%), 39 (59%) and 17 (26%); work type ‐ occupational category ‐ mental demands 20 (28%), mixed mental/physical demands 15 (20%), light physical demands 20 (27%), heavy physical demands 19 (25%) vs 24 (36%), 13 (20%), 19 (29%), 10 (15%); HAQ score (0‐3): 0.76 (0.50) vs 0.83 (0.55); type of rheumatic disease, RA 34 (46%) vs 36 (55%), AS PA or reactive arthritis 17(23) vs 12 (18), SLE or scleroderma 23 (31%) vs 18 (27%). Duration disease: median (range) 11.0(0‐158) vs 19.5(0‐174). Full time or part time employment: unknown; previous job loss: unknown; sick leave: 42(57%) vs 35 (53%), duration sick leave median weeks (range) 16 (1‐52) vs 18 (3‐48); partial work disability benefit 12 (16%) vs 11 (17%). Adaptation at work due to rheumatic disease 22(29%) vs 15 (23%). | |
| Interventions | Experimental group: Hospital‐based multidisciplinary vocational rehabilitation programme ran by a multi‐disciplinary team (rheumatologist, social worker, physical therapist, occupational therapist and psychologist) during 4 to 12 weeks. During the intervention period participants visited Leiden University Medical Center, the Netherlands at least twice in connection with the rehabilitation program, which always consisted of a systematic assessment and a discussion with the team coordinator:
The final report was then sent to the rheumatologist who referred the patient and was sent to the participants' (company) occupational physician, but only if the patient had given written informed consent. Control group: Usual outpatient care: participants were treated and referred to other health professionals in relation to their working problem if regarded necessary by their rheumatologist. In addition, all participants received the same written information about the Dutch social security system regarding sick leave and work disability as participants in the experimental group. In both experimental and control groups, physicians had free choice with respect to their medical prescriptions and other treatment strategies. All medical treatment and the use of health services during the intervention period and two‐year follow‐up were recorded in both groups. | |
| Outcomes | 1) Job loss:
2) Sickness absenteeism: not reported 3) Work functioning: not reported | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization was done with stratification for center (academic hospital versus nonacademic hospital) and 3 diagnosis groups (RA; AS, psoriatic arthritis, or reactive arthritis; and SLE or scleroderma), according to a randomisation list that was created by a random digit generator." |
| Allocation concealment (selection bias) | Unclear risk | Not clearly documented in the text of the study. |
| Prognostic comparability baseline | Low risk | Some imbalance in number of participants with long sick leave > 40 weeks: n = 6 (8%) in the intervention group, and n = 2 (3%) in the control group (difference p = 0.17). Other sick leave variables measured at baseline were similar. Overall we judged differences to have a low risk of bias. |
| Blinding of participants and personnel (performance bias) | High risk | "To maintain allocation concealment, patients were instructed not to inform the principal investigator or the research nurse about the type of care they received." However, participants received many interventions in the control group as prescribed by the participating rheumatologists who were not blinded. de Buck 2005: "Moreover, the rheumatologist was informed about the treatment allocation in a later stage, another factor that could have induced enhanced treatment or referrals in connection with the work problem in the usual care (UC) group. Indeed, participants in the UC group initially paid more visits to the rheumatologist than participants in the Vocational Rehabilitation (VR) group. The participants' participation in the trial could have made rheumatologists aware of their participants' problems at work, and if a patient was allocated to the UC group rheumatologists might have thought they needed to act on account of their patients. In addition, it is possible that participants who were allocated to the control group made an extra appointment with their rheumatologist to discuss their working problem and potential solutions." Considering the high referral rate in the control group we think the contrast between treatment groups diminished (towards no effect), hence we judged high risk of bias. |
| Blinding of outcome assessment (detection bias) | Low risk | See above. The assessment of job loss was assessed by participants' self report and judged low risk of bias. |
| Incomplete outcome data (attrition bias) | Low risk | Loss to follow‐up accounted for (total 25/140: 13/74 in intervention group and 12/66 in control group) 18% at 24 months and was fairly evenly distributed between experimental and control group. In addition, baseline characteristics distribution of non‐completers were similar. |
| Selective reporting (reporting bias) | Low risk | Study protocol is not available but given target of intervention ('vocational rehabilitation'), primary outcome 'job loss' and the non‐significant results we consider reporting bias not likely. |
| Compliance | Low risk | We judged compliance as low risk of bias even though few participants were seen by their companies' occupational physician and did not receive additional guidance. |
| Methods | RCT | |
| Participants | Participants were employed patients with RA and medium to high work disability risk (assessed by RA WIS) who were recruited from RA Centre clinics in London, UK. Randomized: 32 participants, 16 in experimental group (I) and 16 in control group (C). Baseline characteristics: female 15 vs 15; age 49 (12) vs 53 (8); educational level college/university 10 vs 8, postgraduate 2 vs 0; work type: occupational category ‐ managers and professionals 11 vs 10, administrative and skilled trades 5 vs 4, customer service and sales 0 vs 2. Full time work 15 (94%) vs 9 (56%); Job duration < 1 year 3 vs 2, 1 to 3 years 4 vs 1, 3 to 5 years 1 vs 1, > 5 years 8 vs 12; HAQ DI score 1.36 (0.84) vs 1.39 (0.46); Duration disease: median (range) 11.6 (9.9) vs 8.4(6.2). Previous job loss: unknown; days (in month) missed from work, 3.3 (6.2) vs 2.1 (5.0). Biologic agents 2 vs 3 (all other on DMARDs). | |
| Interventions | Experimental group: Comprehensive occupational therapy provided by one occupational therapist (OT) specialized in rheumatology and vocational rehabilitation for a maximum duration of 6 months for 6 to 8 individualized treatment sessions lasting 30 minutes to 2 hours either in groups or individually, including work visits. Usual rheumatology care was provided as well. The case management role of the OT incorporated a biopsychosocial model stemming from the Canadian Occupational Performance Measure (COPM).
Control group: Usual care in the RA Centre clinics involved routine reviews by the rheumatologist. The focus of treatment was on early, aggressive medical management with a goal of achievement of remission (DAS28 score 2.6). There was no OT involvement with these participants. Medical management and rheumatology clinic visit schedules were not changed from normal practice for either group. | |
| Outcomes | 1) Job loss: None reported 2) Sickness absenteeism due to illness/RA:
The instrument was a self‐developed Modified Health Economics Questionnaire combined measures of presenteeism and absenteeism. This is a written self‐report questionnaire that includes the number of days/hours spent at work per week, the number of days missed from work in the past month due to RA. 3) Work functioning:
| |
| Notes | See text publication: under "occupational therapy received" page 1525: the COPM was used as an outcome measure but its outcomes were also used to direct the intervention. It's unclear whether this could bias participants in the intervention group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information on random sequence generation. |
| Allocation concealment (selection bias) | Low risk | "Patients were stratified into medium‐risk (RA WIS score 10 and 17) or high‐risk (RA WIS score 17) groups. Then within these strata, patients were randomly allocated in equal numbers to the occupational therapy or usual care group. The allocation procedure was completed in a blinded manner by an independent research nurse, using a sealed envelope method." |
| Prognostic comparability baseline | High risk | Some questions can be made about the prognostic comparability of both groups. As the group size is small with only 16 participants per group, little differences in prognosis can have substantial influence on outcome. Differences that may count are: longer disease duration in experimental group; more workers with full time employment in the experimental group; more university postgraduates in experimental group; younger people in experimental group. Regardless of whether these differences are significant or not, these factors could have a relationship with both the intervention and the outcome 'work days missed'. The analyses do not account for differences in prognostic imbalances (other outcomes did, but not workdays missed): independent samples T‐tests have been done for the work related outcomes. In addition, using T‐tests for skewed data like work absenteeism (workdays missed) is probably not adequate as well, especially if sample size is small. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Potentially personnel, the participants or the participants work colleagues were more aware or willing to support or influence the participants' work status, as a consequence of belonging to the experimental group or control group but for this trial we have no information that this happened. The extent of this effect remains unclear. |
| Blinding of outcome assessment (detection bias) | High risk | "self‐report questionnaire that includes the number of days/hours spent at work per week, the number of days missed from work in the past month due to RA." We consider these self report data to have a high risk of bias, and not be an objective measure. The intervention was quite intensive with 6 months of comprehensive OT including workplace visits which may have influenced patients recall at the six‐month follow‐up. Certainly there would be more emphasis on the importance of job loss or taking sick leave, although it is not clear how big this effect would be in either group. |
| Blinding of outcome assessment (detection bias) | Low risk | The outcome used, the RA WIS is a "self‐administered, written, validated questionnaire used to screen for work disability" and was assessed by patients' self report and judged low risk of bias. |
| Incomplete outcome data (attrition bias) | Low risk | Macedo reports the same number of participants at baseline and 6 months, and reports no job loss during the 6 months follow‐up. |
| Selective reporting (reporting bias) | Low risk | Study protocol is not available but given target of intervention ('targeted comprehensive Occupational Therapy" and participants with "with perceived work disability risk" ) and the primary outcome work productivity we consider reporting bias not likely. |
| Compliance | Unclear risk | No information is provided on the control group. Little information is provided for experimental group on the number of sessions of OT sessions. Not all attended group sessions or received work visits, and the type of interventions was highly variable. We considered the risk (and direction) of bias unclear. Macedo 2009: "half had a work visit completed and recommendations provided to their employer" and "Most patients (n=15) had approximately 6–8 occupational therapy sessions (30–120 minutes) to review work, home, and social needs on a one‐to‐one basis or in a group format. The remaining patient had a single consultation session due to poor attendance. Six patients attended the group education program run by the OT." |
RA: rheumatoid arthritis, AS: ankylosing spondylitis, OA: osteoarthritis, PsA: psoriatic arthritis, SLE: systemic lupus erythematosus
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Not sufficient participants with IA. Intervention does not fulfill all criteria. | |
| Not sufficient participants with IA. | |
| Intervention does not fulfill all criteria. No work‐related outcome. Sub‐population not working (some retired). | |
| Intervention does not fulfill all criteria. No work‐related outcome. | |
| Not sufficient participants with IA. Intervention does not fulfill all criteria. | |
| Intervention does not fulfill all criteria. No work‐related outcome. | |
| Intervention does not fulfill all criteria. | |
| Not sufficient participants with IA. |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | “Employment and arthritis: making it work”‐ a randomized controlled trial evaluating an online program to help people with inflammatory arthritis maintain employment |
| Methods | RCT of the making it work program compared to usual care and receiving printed information about arthritis and employment |
| Participants | Employed people, aged 18‐59, with inflammatory arthritis (RA, AS,PsA or SLE with arthritis) , at risk of job loss |
| Interventions | The intervention consists of a) 5 online group sessions; b) 5 web‐based e‐learning modules; c) consultations with an occupational therapist for an ergonomic assessment of their work and with a vocational rehabilitation counselor for job retention vocational counselling. |
| Outcomes | Primary outcomes include at‐work productivity (presenteeism)and work cessation (define as stopping work for > 6 months for any reason). Secondary outcomes include temporary work cessation, number of days missed from work per year, reduction in hours worked per week. A cost‐utility analysis of the intervention will also be performed, from a societal perspective |
| Starting date | September 2013 |
| Contact information | Diane Lacaille: [email protected] |
| Notes | Trial registration NCT01852851 |
| Trial name or title | Efficacy of a Modified Vocational Rehabilitation Intervention for Work Disability |
| Methods | RCT |
| Participants | Employed persons with rheumatoid and other forms of arthritis, as well as other rheumatic conditions |
| Interventions | Job retention delivered by physical and occupational therapists. Intervention has similarity to that in Allaire 2003. Control group: printed materials concerning working with a disability and relevant resources. |
| Outcomes | Ability to work, satisfaction with ability to work, job loss. |
| Starting date | Ongoing |
| Contact information | Julie Keysor: [email protected] |
| Notes | US |
| Trial name or title | "Care for Work" study |
| Methods | RCT |
| Participants | The population consists of RA patients (18 to 64 years of age) who have visited a rheumatologist of one of the participating hospitals during the last year. Eligible patients are diagnosed with RA, and have a paid job (paid‐employment or self‐employed) for at least 8 hours per week. Furthermore, eligible patients experience difficulties in functioning at work. |
| Interventions | The intervention program consists of two components which complement each other; integrated care including a participatory workplace intervention. |
| Outcomes | The primary outcome measure is work productivity, measured by hours lost from work due to presenteeism. Secondary outcome measures include sick leave, quality of life, pain and fatigue. Cost‐effectiveness of the intervention program will be evaluated from the societal perspective. |
| Starting date | 2012, first results 2015 |
| Contact information | Myrthe van Vilsteren: [email protected] |
| Notes | Trial registration NTR2886 |
RA: rheumatoid arthritis, AS: ankylosing spondilitis, OA: osteoarthritis, PsA: psoriatic arthritis, SLE: systemic lupus erythematosus
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Job loss counts (workers) cumulative 12, 24, 30, 48 months Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 1.1  Comparison 1 job loss prevention vs control intervention, Outcome 1 Job loss counts (workers) cumulative 12, 24, 30, 48 months. | ||||
| 1.1 Follow‐up 12 months | 2 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Follow‐up 24 months | 2 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Follow‐up 30 months | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Follow‐up 48 months | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Sickness absenteeism ‐ work days missed per month ‐ six months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.2  Comparison 1 job loss prevention vs control intervention, Outcome 2 Sickness absenteeism ‐ work days missed per month ‐ six months. | ||||
| 3 Work functioning ‐ RA WIS ‐ six months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.3  Comparison 1 job loss prevention vs control intervention, Outcome 3 Work functioning ‐ RA WIS ‐ six months. | ||||
| 4 Extra: Job loss or increase in disability pension: counts (participants) ‐ 24 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.4  Comparison 1 job loss prevention vs control intervention, Outcome 4 Extra: Job loss or increase in disability pension: counts (participants) ‐ 24 months. | ||||
| 5 Extra: Job loss events ‐ permanent and temporary ‐ 48 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.5  Comparison 1 job loss prevention vs control intervention, Outcome 5 Extra: Job loss events ‐ permanent and temporary ‐ 48 months. | ||||
| 6 Extra: Sickness absenteeism ‐ Workdays missed as proportion of days worked over the past month ‐ six months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.6  Comparison 1 job loss prevention vs control intervention, Outcome 6 Extra: Sickness absenteeism ‐ Workdays missed as proportion of days worked over the past month ‐ six months. | ||||
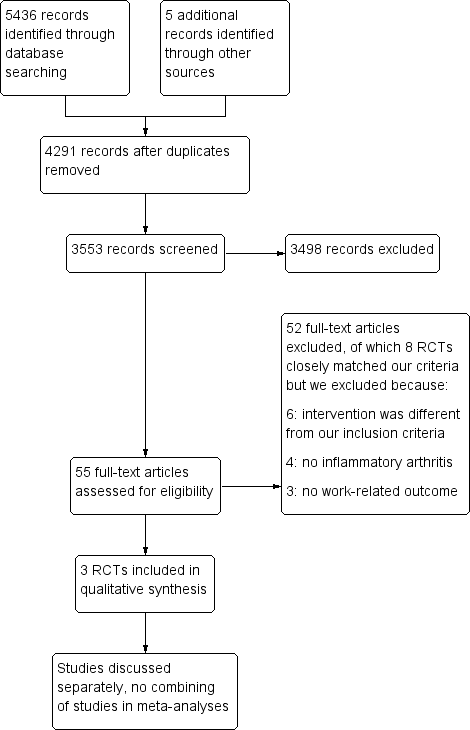
Study flow diagram.
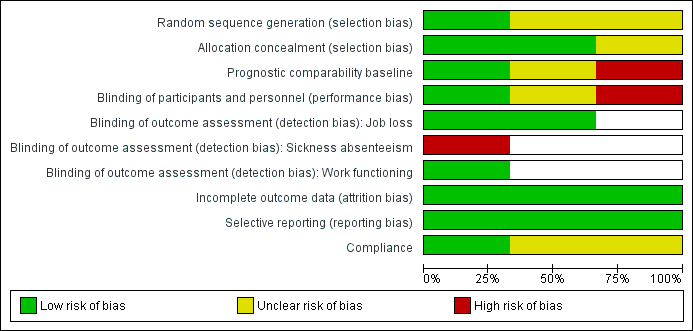
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included trials.
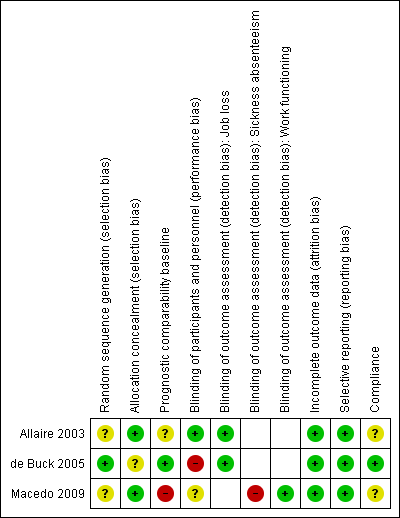
Risk of bias summary: review authors' judgements about each risk of bias item for each included trial.
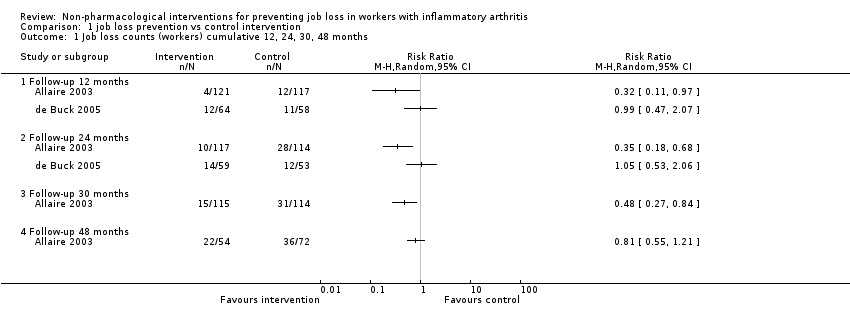
Comparison 1 job loss prevention vs control intervention, Outcome 1 Job loss counts (workers) cumulative 12, 24, 30, 48 months.
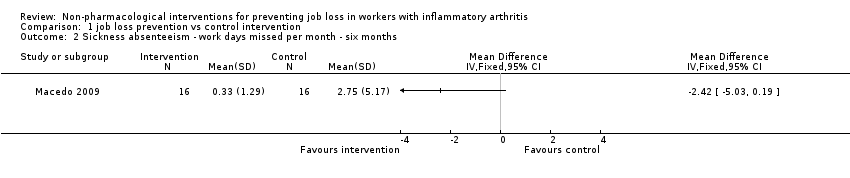
Comparison 1 job loss prevention vs control intervention, Outcome 2 Sickness absenteeism ‐ work days missed per month ‐ six months.
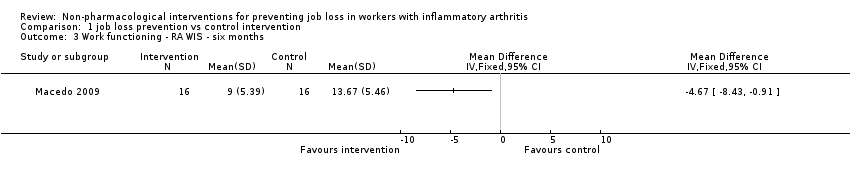
Comparison 1 job loss prevention vs control intervention, Outcome 3 Work functioning ‐ RA WIS ‐ six months.
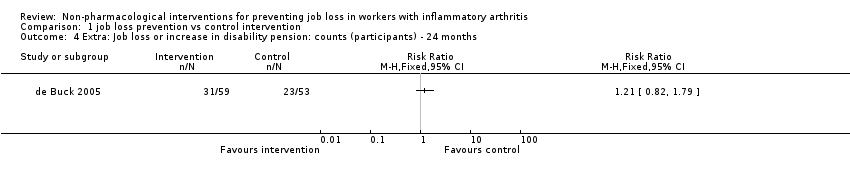
Comparison 1 job loss prevention vs control intervention, Outcome 4 Extra: Job loss or increase in disability pension: counts (participants) ‐ 24 months.
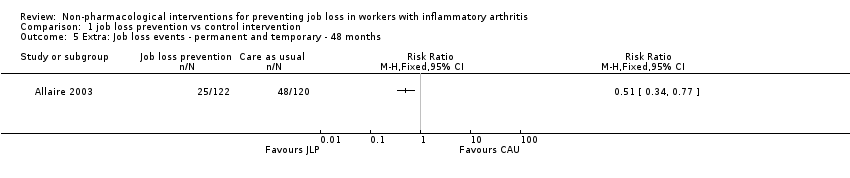
Comparison 1 job loss prevention vs control intervention, Outcome 5 Extra: Job loss events ‐ permanent and temporary ‐ 48 months.
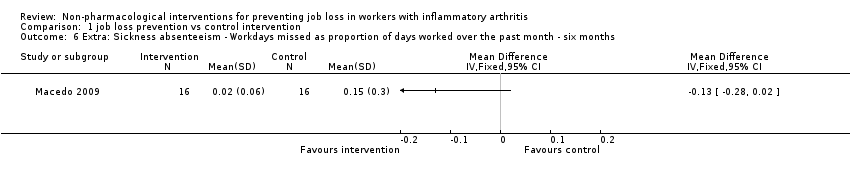
Comparison 1 job loss prevention vs control intervention, Outcome 6 Extra: Sickness absenteeism ‐ Workdays missed as proportion of days worked over the past month ‐ six months.
| Job loss prevention compared to control intervention in people with IA | ||||||
| Patient or population: people with IA | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control intervention 7 | Job loss prevention | |||||
| Job loss | See comment | See comment | Not estimable | 340 | ⊕⊝⊝⊝ | Due to inconsistency in the trials we did not pool these two trials |
| Sickness absenteeism | The mean sickness absenteeism in the control groups was | The mean sickness absenteeism in the intervention groups was | ‐ | 32 | ⊕⊝⊝⊝ | ‐ |
| Work functioning | The mean work functioning in the control groups was | The mean work functioning in the intervention groups was | ‐ | 32 | ⊕⊝⊝⊝ | ‐ |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 We judged the RCTs by de Buck 2005 and Macedo 2009 to have an overall high risk of bias and the RCT by Allaire 2003 to have an overall low risk of bias. Overall, we judged serious risk of bias to be present and therefore we downgraded the quality of the evidence by one level (‐1). 7 All control groups received either usual care or a minimal intervention such as written information in Allaire 2003. | ||||||
| Outcome measures | Follow‐up times | Trials | Extra analyses |
| Combined job loss or increase of disability pension | 24 months | ||
| Job loss events | 48 months | ||
| Sickness absenteeism defined as workdays missed in proportion to days worked | |||
| In this table we present other supporting job loss outcome data reported in the trials for informative purposes only. These data do not contribute to our conclusions. | |||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Job loss counts (workers) cumulative 12, 24, 30, 48 months Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Follow‐up 12 months | 2 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Follow‐up 24 months | 2 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Follow‐up 30 months | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Follow‐up 48 months | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Sickness absenteeism ‐ work days missed per month ‐ six months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Work functioning ‐ RA WIS ‐ six months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Extra: Job loss or increase in disability pension: counts (participants) ‐ 24 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Extra: Job loss events ‐ permanent and temporary ‐ 48 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Extra: Sickness absenteeism ‐ Workdays missed as proportion of days worked over the past month ‐ six months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |

