Intervenciones no farmacológicas para la prevención de la pérdida de puestos de trabajo en trabajadores con artritis inflamatoria
Resumen
Antecedentes
La participación en el trabajo por parte de los pacientes con artritis inflamatoria (AI) es importante no sólo económicamente sino también para la salud física y psicológica. Hasta la fecha no hay ninguna Revisión Cochrane sobre los estudios de las intervenciones no farmacológicas específicamente dirigidas a la prevención de la pérdida de puestos de trabajo en pacientes con AI.
Objetivos
Evaluar los efectos de las intervenciones no farmacológicas para prevenir la pérdida del empleo y el ausentismo laboral o mejorar el funcionamiento en el trabajo para los empleados con AI (artritis reumatoide [AR], espondilitis anquilosante [EA], artritis psoriásica [APs], otra espondilartritis [EpA] o AI asociada con enfermedades del tejido conjuntivo, como el lupus eritematoso sistémico [LES]).
Métodos de búsqueda
Se hicieron búsquedas en las siguientes bases de datos, desde su inicio hasta el 30 de abril 2014; The Cochrane Library (incluyendo el Registro Cochrane Central de Ensayos Controlados [Cochrane Central Register of Controlled Trials], es decir, CENTRAL y DARE), MEDLINE (PubMed), EMBASE (Embase.com), CINAHL (EbSCOhost), ClinicalTrials.gov y PsycINFO (ProQuest). No se impuso ninguna restricción de idioma en las búsquedas.
Criterios de selección
Se incluyeron ensayos controlados aleatorios (ECA) que evaluaron las intervenciones para prevenir la pérdida del empleo en adultos en edad activa (18 a 65 años de edad) con diagnóstico de AI, incluida la AR, la EA, la APs, la EpA u otros tipos de AI. Los resultados primarios fueron la pérdida del empleo y el ausentismo por enfermedad, y el resultado secundario fue el funcionamiento en el trabajo.
Obtención y análisis de los datos
Dos autores de la revisión seleccionaron de forma independiente los ensayos para la inclusión, extrajeron los datos y evaluaron el riesgo de sesgo en los ECA incluidos.
Resultados principales
Se incluyeron tres ECA con un total de 414 participantes en riesgo de perder el empleo. La mayoría de los participantes presentaba AI, principalmente AR y EA en un grado menor. Las intervenciones procuraron prevenir la pérdida delempleo y mejorar el funcionamiento en el trabajo de varias maneras: en primer lugar al evaluar los cambios o las adaptaciones en el trabajo y en segundo lugar al proporcionar cualquier intervención dirigida a la persona incluida la orientación vocacional, el asesoramiento o la educación. Las intervenciones directamente dirigidas al ambiente de trabajo fueron mínimas e incluyeron visitas al lugar de trabajo (un ensayo) o cualquier acción realizada por un médico ocupacional (un ensayo). La duración o la dosis de las intervenciones varió de dos sesiones de 1,5 horas (un ECA) durante cinco meses, dos consultas y tratamientos multidisciplinarios durante tres meses (un ECA), hasta seis a ocho sesiones individuales o grupales durante seis meses (también un ECA). Todos los participantes fueron reclutados por consultorios de reumatología, tanto dentro como fuera de los hospitales. Los ensayos incluidos investigaron la pérdida del empleo (n = dos ECA; 382 participantes), el ausentismo laboral y el funcionamiento en el trabajo (n = un ECA; 32 participantes). En general, se evaluaron los dos ensayos más pequeños como de alto riesgo de sesgo y el ensayo más amplio como de bajo riesgo de sesgo. Los ensayos mostraron diferencias marcadas en cuanto a cómo manejaron los ítems del riesgo de sesgo, en particular el sesgo de realización.
La calidad de las pruebas se evaluó mediante el enfoque GRADE y se consideró que había pruebas de calidad muy baja entre los tres resultados informados. De los dos ECA que investigaban la pérdida del puesto de trabajo, el más amplio (n = 242 participantes) informó una reducción grande estadísticamente significativa en la pérdida del puesto de trabajo (riesgo relativo [RR] = 0,35, intervalo de confianza [IC] del 95%: 0,18 a 0,68) y el otro ECA (n = 140) informó efectos similares en ambos grupos, aunque el IC fue muy amplio (RR = 1,05; IC del 95%: 0,53 a 2,06). El último probablemente presentó un sesgo de realización y se juzgó como en alto riesgo de sesgo. El único ensayo pequeño que investigó el ausentismo por enfermedad encontró resultados inciertos a los seis meses de seguimiento (DM = ‐2,42 días, IC del 95%: ‐5,03 a 0,19). Finalmente, en el mismo ensayo pequeño que investigó el funcionamiento en el trabajo mediante la Rheumatoid Arthritis‐Work Instability Scale (RA‐WIS), hubo una mejoría moderada en el funcionamiento en el trabajo a plazo intermedio (seis meses; rango de la escala 0 a 23; mejoría media ‐4,67 puntos, IC del 95%: ‐8,43 a ‐0,91). No se identificaron efectos adversos en las publicaciones de los tres ensayos.
Conclusiones de los autores
Esta revisión Cochrane de tres ECA halló pruebas de muy baja calidad en general sobre el efecto de las intervenciones para la prevención de la pérdida del empleo sobre la pérdida del empleo, el ausentismo laboral y el funcionamiento en el trabajo en los trabajadores con artritis inflamatoria. Aunque esta revisión destaca la necesidad de ECA adicionales de alta calidad, los resultados sugieren que estas estrategias tienen el potencial de ser efectivas.
PICO
Resumen en términos sencillos
Intervenciones no farmacológicas para ayudar a los trabajadores con artritis inflamatoria a mantener el puesto de trabajo
Antecedentes
La artritis inflamatoria (AI), también llamada reumatismo, es un grupo de enfermedades que causan dolor prolongado, rigidez e inflamación en las articulaciones. Estos síntomas dificultan la movilidad y causan sensación de cansancio, que a su vez pueden dificultar la actividad laboral. Los tipos más frecuentes de AI son: la artritis reumatoide, la artritis psoriásica y la espondilitis anquilosante. En todo el mundo alrededor del 3% de las personas tienen AI. La enfermedad generalmente comienza cuando los pacientes tienen entre 30 y 40 años de edad, en un momento en que todavía les quedan muchos años de vida laboral. Por lo tanto, es importante saber si hay formas efectivas para ayudar a los pacientes con AI a mantener el puesto de trabajo. Esta Revisión Cochrane se centra en las intervenciones no farmacológicas.
Ensayos encontrados
Se realizaron búsquedas en la literatura disponible hasta el 30 de abril de 2014. Se incluyeron tres ensayos controlados aleatorios con 414 participantes con AI que estaban en riesgo de perder su puesto de trabajo. Estos ensayos evaluaron en primer lugar la forma en que podría adaptarse el ambiente laboral y luego proporcionaron orientación, asesoramiento o educación relacionados con los problemas laborales. Un ensayo administró dos sesiones de 1,5 horas durante cinco meses. Otro ensayo proporcionó dos consultas y tratamientos multidisciplinarios durante tres meses. El tercer ensayo proporcionó seis a ocho sesiones individuales o grupales durante seis meses. Los ensayos incluidos compararon los efectos de las intervenciones con atención habitual (dos ensayos) o con información escrita solamente (un ensayo). Dos de los ensayos incluidos midieron el efecto de la intervención en la pérdida del empleo (382 participantes) y el tercero midió el efecto sobre el ausentismo laboral y el funcionamiento en el trabajo (32 participantes).
Lo que dice la investigación
Cuando se consideraron en conjunto, las pruebas de los tres ensayos fueron de muy baja calidad. Dos ensayos encontraron diferentes resultados en la pérdida del puesto de trabajo medida a los dos años de seguimiento: un ensayo sobre la orientación relacionada con el trabajo encontró una reducción grande en los pacientes que perdieron el empleo y el otro ensayo encontró efectos similares en ambos grupos. Otro ensayo no encontró un efecto considerable sobre el ausentismo a los seis meses de seguimiento aunque encontró una mejoría moderada en el funcionamiento en el trabajo.
Conclusiones
Debido a los resultados positivos de un ECA con un seguimiento a largo plazo, se observa el potencial de las intervenciones de prevención de la pérdida del empleo para ayudar a los trabajadores con artritis inflamatoria a mantener el puesto de trabajo. La certeza de estos resultados se ve limitada en general por las pruebas de calidad muy baja de los tres ECA.
Authors' conclusions
Summary of findings
| Job loss prevention compared to control intervention in people with IA | ||||||
| Patient or population: people with IA | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control intervention 7 | Job loss prevention | |||||
| Job loss | See comment | See comment | Not estimable | 340 | ⊕⊝⊝⊝ | Due to inconsistency in the trials we did not pool these two trials |
| Sickness absenteeism | The mean sickness absenteeism in the control groups was | The mean sickness absenteeism in the intervention groups was | ‐ | 32 | ⊕⊝⊝⊝ | ‐ |
| Work functioning | The mean work functioning in the control groups was | The mean work functioning in the intervention groups was | ‐ | 32 | ⊕⊝⊝⊝ | ‐ |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 We judged the RCTs by de Buck 2005 and Macedo 2009 to have an overall high risk of bias and the RCT by Allaire 2003 to have an overall low risk of bias. Overall, we judged serious risk of bias to be present and therefore we downgraded the quality of the evidence by one level (‐1). 7 All control groups received either usual care or a minimal intervention such as written information in Allaire 2003. | ||||||
Background
For any working age adult, the ability to participate in working life is important not only economically but also for physical and psychological health (Fifield 1991; Hoving 2013; MacKinnon 1992; Mehnert 1990). This is equally true for people with inflammatory arthritis (IA) who, in qualitative studies, have identified employment as an important problem and lack of employment services as a significant unmet need (Hoving 2009; Lacaille 2007; Mancuso 2000; Nilsson 2007). Although this importance has been recognised, the topic receives little attention in most clinical guidelines and evidence summaries. However, over the past decade work participation has received more attention, as shown by the growing number of both prognostic and intervention employment studies in rheumatic diseases (Lacaille 2005). Although work participation as an outcome has been included in recent reviews of pharmacological interventions (ter Wee 2012), to date no Cochrane Reviews of rheumatic diseases have reviewed studies of non‐pharmacological interventions specifically aimed at improving work participation. A systematic review of non‐randomised studies on this topic dates back to 2002 (de Buck 2002) and anon‐systematic overview was published in 2009 (Vliet Vlieland 2009). The overview published by Vliet Vlieland 2009 on vocational rehabilitation concluded that the effects of vocational rehabilitation interventions in people with chronic arthritis is "scanty" and work disability among individuals with chronic arthritis is substantial. In this Cochrane Review we study participation in paid work, and review the impact of job loss prevention interventions encompassing not only employment status (i.e. existence or degree of work disability) but also absences from paid work, and work functioning or presenteeism as per Outcome Measures in Rheumatology Clinical Trials (OMERACT) recommendations (Escorpizo 2007).
Description of the condition
IA, including its most common types: rheumatoid arthritis (RA), psoriatic arthritis (PsA), ankylosing spondylitis (AS) and undifferentiated spondyloarthritis (SpA), place a person at increased risk of work disability. IA is characterized by its chronic, progressive nature. Inflammation causes pain, stiffness and swelling in the joints, leading to restricted range of motion, decreased strength and reduced physical function, as well as general fatigue. Worldwide, IA prevalence is estimated to be around 3%, including a prevalence of 1% for RA (Gabriel 2001) and 1.9% for SpA (including AS and PsA) (Braun 1998). IA typically begins at a younger age, often in people aged between 30 and 40 years, at a time when they still have many years of potential active workforce participation. In the past, people who stopped working due to IA were not likely to return to work or gain employment elsewhere. This is not surprising, as IA is progressively disabling, with potential long‐term complications and it is difficult for people to return to active employment after prolonged absences from work. However, it seems that the prognosis for people with certain types of IA is improving (ter Wee 2012). The emergence of new disease‐modifying antirheumatic drugs (DMARDs) has renewed research interest in the relationship between IA and work functioning. DMARDs are now provided at an earlier stage of the disease to eradicate inflammation and thereby prevent radiological damage. It has been suggested that new biological agents, such as tumour necrosis factor (TNF) inhibitors, also have a beneficial effect on work participation and work functioning, although the magnitude of the effect is unclear and warrants further research (Allaire 2008; Hoving 2009; Verstappen 2007; Yelin 2003).
Description of the intervention
In this Cochrane Review, we are interested in interventions primarily targeted towards the consequences of IA on work participation. Earlier studies aimed at improving employment outcomes for people with IA have attempted to help people disabled by IA return to work. However, in general, once people are unable to work they are unlikely to re‐enter the workforce. For example, data from the USA show that people with arthritis infrequently utilized vocational rehabilitation services aiming to return them to work (Straaton 1997), and success was generally low. Recently, emphasis has shifted towards tertiary prevention, which helps people cope with impairments in their work, and primary prevention of work disability. Thus the focus is shifting from return to work towards job retention.
This review focuses on non‐pharmacological interventions aimed directly at addressing work participation in one or more ways. Firstly, there should be an analysis of a person's work activities, work functioning, ergonomic needs or communication at work to identify those features of working life that are placing the person at risk of having to stop working. Secondly, interventions should include some form of consultation, such as advice on job accommodations, vocational counselling or work rehabilitation strategies to deal with challenges in relation to work. Both components include the context of work directly. To our knowledge, a few intervention studies conducted in the past decade have looked at ways to implement and evaluate interventions directed at improving work participation for people with inflammatory rheumatic diseases (de Buck 2002; Vliet Vlieland 2009).
Other types of interventions not included in this review can also have an impact on work participation in people with IA. Pharmacological interventions for IA aiming to decrease the inflammatory process may have an impact on work participation. This may be through their effect on disease activity, pain or physical function, which are all known predictors of work disability. In this category we also place interventions that aim to improve the delivery of medical services, such as starting pharmacological treatment early or multidisciplinary interventions for the treatment of arthritis not including specific work‐related interventions. Both pharmacological interventions and interventions that promote the delivery of medical services are excluded from this review and have already been addressed in several Cochrane Reviews (Colebatch 2011; Radner 2012; Ramiro 2011).
There are also interventions, such as physical therapy or exercise therapy on the one hand, and psychological interventions or behavioral counselling on the other, that try respectively to improve physical functioning and fatigue, or coping and problem‐solving skills, for example, but weren't designed to change work participation. This enables people with IA to have more energy, have better joint function and strength, or be better able to cope with everyday stressors. These interventions do not target the disease but rather the disease symptoms and consequences. A benefit of these physical and psychosocial therapies, sometimes offered as part of a multi‐disciplinary rehabilitation program, may be that they also have an effect on work participation, through physical, physiological or psychological pathways. These therapies are not as commonly prescribed as medical (pharmacological) treatment, but are available to many people with IA, either by referral or direct access. We have also excluded these types of interventions from this Cochrane Review because they do not specifically target employment. They have also been addressed in previous reviews including several Cochrane Reviews (Dagfinrud 2008; Hurkmans 2009; Riemsma 2003; Silva 2010; Steultjens 2004).
How the intervention might work
As shown in several studies (de Croon 2004; de Croon 2005; Hoving 2013; Lacaille 2007; Van der Meer 2011), people with arthritis struggle to find a balance between work and home demands, medical appointments, work issues, communication with co‐workers and transportation, while coping with decreasing energy levels and pain. Work disability in people with RA has also been described as a: "...biopsychosocially determined misfit between individual capability and work demands" (de Croon 2004). This relationship is influenced by contextual factors. Interventions that target an individual's capability for work, or that target work demands by changing work routines or provide accommodations, enable people with IA to have fewer difficulties in functioning at work and thereby improves work participation.
Why it is important to do this review
Work participation is important to people with IA. Although medical treatment is improving, many continue to experience challenges in maintaining employment over time (Hoving 2009; Hoving 2013). The effectiveness of mono‐therapies and multidisciplinary programmes in people with IA has been evaluated, though not on work participation, in several Cochrane Reviews including physiotherapy (Dagfinrud 2008), dynamic exercise therapy (Hurkmans 2009), occupational therapy (Steultjens 2004), patient education (Riemsma 2003) and balance training (Silva 2010). Other reviews on interventions for people with rheumatic diseases that focus on work participation have either not included RCTs (de Buck 2002; Mahalik 2006) or have used a non‐systematic review process (Mahalik 2006; Vliet Vlieland 2009). For example, a systematic review on vocational rehabilitation in people with chronic rheumatic diseases reported only five studies published up to May 2001, and none were controlled (de Buck 2002). In their review of work site interventions for people with RA and osteoarthritis (OA), Mahalik 2006 indicated a need for "randomised, comparative studies, measuring multiple outcome measures". On the other hand, Vliet Vlieland 2009 looked at vocational rehabilitation programs for people with chronic arthritis and identified only two RCTs on vocational rehabilitation up to 2005. In addition, the importance of work participation as a topic is clear from the increasing number of Cochrane Reviews on other chronic diseases such as cancer (de Boer 2011) and multiple sclerosis (Khan 2009). All these reviews suggest that more research is warranted to study the effects of interventions that promote work participation for people with IA.
Objectives
To assess the effectiveness of non‐pharmacological interventions that aim to prevent job loss for employees with IA.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs).
Types of participants
We included trials in which the population was limited to adults of working age (18 to 65 years) of which at least half of all workers (>50%) had been diagnosed with IA, including RA, AS, PsA or SpA, or IA associated with connective tissue diseases such as Systemic Lupus Erythematosus (SLE). We included trials conducted with participants from hospital settings, occupational settings, primary care or community settings, or outpatient care settings.
Types of interventions
We included intervention where the focus was on job loss prevention or improving work function. To fulfil this criteria, we included interventions that fulfilled at least two of the following three components:
a) An evaluation of the work challenges or work adaptations as a step in the main intervention of the study;
b) Interventions directed at the person, meaning:
-
job coaching, job or vocational training, vocational counselling; or
-
empowerment for work; or
-
self‐management, including support or information regarding work or both;
c) Interventions directed at the work environment, meaning:
-
work adaptations, ergonomic measures, job accommodations; or
-
interventions targeted directly at the employer, supervisor or co‐workers.
We have named interventions that fulfil the above criteria job loss prevention interventions in this systematic review. The above includes interventions such as vocational rehabilitation, occupational rehabilitation or ergonomic interventions, but are not exclusive to these terms. These interventions include some kind of information or communication about work participation as part of the intervention directed to the worker or to the work environment. Included in the above are also multi‐disciplinary interventions as long as they include, or are part of, a), b) or c).
Types of outcome measures
Primary outcomes
As interventions should aim to prevent job loss, we judged the following outcomes to be important:
1. Job loss measured as:
-
the number of people that become unemployed at some stage following diagnosis, regardless of disability pension status; or
-
the time to job loss.
2. Sickness absenteeism measured as:
-
time lost from work (number of work days or hours missed at work due to sick leave, or absenteeism); or
-
time to return to work; or
-
the proportion of workers on sick leave at a certain moment of follow‐up.
Secondary outcomes
Work functioning measured using any at‐work productivity, work functioning or presenteeism questionnaire: including but not limited to the work limitations questionnaire, the work instability scale or the work role functioning questionnaire.
We categorised trials according to these follow‐up times:
-
short term (more than one day, up to three months);
-
intermediate term (more than three and less than 12 months); or
-
long term (one year or longer).
Search methods for identification of studies
We have listed the search strategies we used to search the different medical databases in Appendix 1, Appendix 2 , Appendix 3, Appendix 4 and Appendix 5. We devised and conducted the systematic search in collaboration with Leena Isotalo, the Trials Search Coordinator of the Cochrane Occupational Safety and Health Review Group.
Electronic searches
We searched the following electronic databases from inception up to 30 April 2014:
-
The Cochrane Library (including Cochrane Central Register of Controlled Trials, i.e. CENTRAL and the Database of Reviews of Effectiveness, i.e. DARE);
-
MEDLINE (PubMed);
-
EMBASE (Embase.com);
-
CINAHL (EbSCOhost);
-
ClinicalTrials.gov:
-
PsycINFO (ProQuest).
We ran the searches without language restrictions, using the Cochrane Collaboration highly‐sensitive search strategy to identify all RCTs (Lefebre 2011). We used specific MeSH headings and additional keywords to identify all RCTs on rheumatic diseases and different types of arthritis. The strategy combines disease terms as listed above and a controlled vocabulary for describing interventions to prevent job loss and improve work participation, including search terms such as work participation, work rehabilitation and vocational rehabilitation, for which we included search terms from a search string for identifying studies on work‐related outcomes and interventions (Haafkens 2006; Verbeek 2005).
Searching other resources
We retrieved additional references in several ways. We screened the reference lists of relevant systematic reviews from the Cochrane Database of Systematic Reviews (CDSR, The Cochrane Library). We also screened references from included RCTs and other reviews on work participation rehabilitation in rheumatic diseases. Finally, we asked experts in the field to identify any published or unpublished studies that may be relevant to this Cochrane Review.
Data collection and analysis
Selection of studies
We divided the identified trials between pairs of review authors (including JH in each pair) in order to examine each reference twice. To determine whether a study should be included, we read the title and abstract of all identified hits from the electronic database searches. We then decided independently of each other the article eligibility according to the predetermined selection criteria (see Criteria for considering studies for this review). If there was any doubt, the review authors retrieved and read the full text article. We resolved any disagreements about the eligibility of a trial in a consensus meeting or by email.
Data extraction and management
JH, and MF or JS independently extracted information regarding study design, interventions, patient population, outcome measures and timing of outcome assessment, co‐interventions, adverse effects, loss to follow‐up and results data for outcomes of interest using a standardised data extraction form.
Assessment of risk of bias in included studies
We evaluated the validity of the RCTs using the Cochrane Collaboration’s tool for assessing risk of bias as described in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We assessed each study for risk of bias in each of the following seven domains, with ratings of low risk of bias, high risk of bias or unclear risk of bias:
-
Random sequence generation;
-
Allocation concealment;
-
Blinding of participants and personnel;
-
Blinding of outcome assessment (per outcome); and attrition
-
Incomplete outcome data;
-
Selective reporting;
-
Other sources of bias including prognostic comparability at baseline, and compliance.
JH, and MF or JS independently assessed the risk of bias of each included trial. To determine the risk of bias of a trial, each criterion was evaluated for the presence of sufficient information and the likelihood of potential bias. We discussed any disagreements between the review authors and resolved them in a consensus meeting. We sought expert advice from the Cochrane OSH Review Group (Jos Verbeek) in a number of cases to facilitate decision making. Given the low number of included trials, we did not calculate agreement statistics as proposed by Brennan 1992 and Cohen 1960.
Measures of treatment effect
We expressed the results of each RCT as RRs with corresponding 95% confidence intervals (CI) for dichotomous data (job loss), and mean differences (MDs) or standardised mean differences (SMDs) for continuous data (sickness absenteeism and work functioning), depending on the similarity of outcome measurement scale (i.e. MDs were used when all trials used the same outcome measurement scale and SMDs when trials used different outcome measurement scales). RR smaller than 1.0 indicates a beneficial effect of the experimental intervention i.e. fewer job losses or days lost from work (Deeks 2008). RRs are considered clinically relevant if the RR is smaller than 0.7 or larger than 1.5, in favour of the intervention or control group, respectively.
Unit of analysis issues
We searched for all RCTs but did not find any trials that employed a cluster‐randomised design. Therefore we did not have to make an allowance for the design effect by assuming intra‐cluster correlations following methods stated in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). If when we update this review we should identify studies that contain more than two intervention groups, we will divide the number of participants in the control group with the number of interventions so as not to count the same control participants several times in the meta‐analysis.
Dealing with missing data
We contacted one trial author (Allaire 2003) to clarify data reported in their publication, which we could possibly use for meta‐analysis, but used no other unpublished data. In the absence of missing data, we had no need of calculating them from other available statistics such as P values according to the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Assessment of heterogeneity
We assessed clinical homogeneity based on similarity of population, intervention, outcome and follow‐up. We considered populations as similar when they fell into the specified diagnosis types. We considered interventions as similar when they fell into the pre‐defined interventions (see Types of interventions). We considered the work participation outcome categories similar within each of the three categories. We regarded follow‐up times of less than three months, three months to one year and more than one year as different. We tested for statistical heterogeneity using the I2 statistic (Higgins 2011), using the following as a rough guide for interpretation: 0% to 40% might not be important; 30% to 60% may represent moderate heterogeneity; 50% to 90% may represent substantial heterogeneity; and 75% to 100% considerable heterogeneity. In the absence of homogeneous comparisons we did not further explore heterogeneity (defined as I2 ≥ 75%) or include subgroup analyses.
Assessment of reporting biases
We reduced the effect of reporting bias by including trials rather than publications in order to avoid the introduction of duplicate data, as was present in two trials. We extracted data only once. We prevented location bias by searching across multiple databases. Language bias was prevented by not excluding any article based on language. Given the low number of included trials, we did not further explore publication bias using a funnel plot.
Data synthesis
If more than one trial reported on the same outcome, we planned to calculate the SMD and corresponding 95% confidence interval (CI). However, as we did not identify multiple trials per outcome, we reported the original scale scores at follow‐up, the mean difference and its 95% CI. In future review updates with more included trials, we plan to use the following formula to calculate SMD = (Or‐Ot/ PSD) where Or is mean improvement in the reference group, Ot is mean improvement in the treatment group and PSD is the pooled standard deviation (Deeks 2008). Interpretation of the SMD as described by Cohen 1988 is as follows: for example, an SMD of 0.2 is considered to indicate a small beneficial effect, 0.5 a medium effect, and 0.8 a large effect. The SMD is considered to indicate a clinically relevant effect when it is larger than 0.5. The calculation of SMDs is only useful if the outcome measures use different scales but measure the same concept.
In the current review we identified no more than two intervention groups (job loss prevention versus control intervention consisting of usual care or advice or both), enabling just one pair‐wise comparison. For future updates, we plan to include multiple pair‐wise comparisons between all possible pairs of intervention groups, but using the same group of participants only once in the meta‐analysis.
Similarly, in the absence of homogeneous comparisons we did not perform meta‐analyses in this review. If future updates can incorporate meta‐analyses and the results show statistically significant overall estimates we will transform these back (pooled estimate of RR, MD or SMD) into measures that are clinically useful in daily practice, such as the number needed to treat (NNT) and the absolute or relative improvement, or both, on the original units to express the final results of the review. In this case we will only pool data from trials judged to be clinically homogeneous using Review Manager 5.2 software (RevMan 2011). Likewise, if future review updates include trials that are statistically heterogeneous, we will use a random‐effects model; otherwise we will use a fixed‐effect model.
Regarding the primary outcome, we combined the following outcomes:
-
Number of people employed before and after intervention, number of people or percentages, either defined as job loss or otherwise;
-
Time lost from work and time to return to work were combined if necessary and analysed as continuous outcomes. We used the mean number of time lost from work to calculate the effect size using days on sick leave with the following formula: mean change difference over standard deviation (SD);
-
Time to job loss was analysed as a continuous outcome.
We used the GRADE approach as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) and as implemented in the GRADEPro 3.2 software (GRADE 2008) to present the quality of evidence and 'Summary of Findings' tables.
The downgrading of the quality of a body of evidence for a specific outcome was based on five factors:
-
Limitations in the design and implementation of available studies suggesting high likelihood of bias;
-
Indirectness of evidence (indirect population, intervention, control, outcomes);
-
Unexplained heterogeneity or inconsistency of results (including problems with subgroup analyses);
-
Imprecision of results (wide CIs);
-
High probability of publication bias.
The GRADE approach specifies four levels of quality (high, moderate, low and very low).
Subgroup analysis and investigation of heterogeneity
We intended to do subgroup analyses based on the most prevalent diagnosis categories, including RA, AS and remaining categories (other arthritis types). Similarly, we planned this in case job loss prevention (person‐directed or work environment‐directed) was given exclusively or as part of a multidisciplinary intervention that includes other interventions. As we didn't find a sufficient number of trials that met our inclusion criteria, we may plan to do these in future review updates.
Sensitivity analysis
We planned to conduct a sensitivity analysis to test the robustness of our meta‐analysis results by omitting trials we judged to have a high risk of bias. Given the low number of included trials we may do so in future updates. In that case we will use a random‐effects model to combine data and perform a sensitivity analysis by using the fixed‐effect model to reveal differences in results.
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of studies awaiting classification; and Characteristics of ongoing studies.
Results of the search
We conducted electronic and manual literature searches on April 30th 2014 and identified 5436 titles. This number was reduced to 4291 titles and abstracts after duplicate removal. We identified five additional studies through additional handsearches. Of these 3553 studies, 55 passed the title and abstract screening and were selected for further full text review (see Figure 1). From these, we identified 11 trials that dealt with the topic of this review. Of these, three original RCTs fulfilled all inclusion criteria (Allaire 2003; de Buck 2005; Macedo 2009). We also included multiple publications of the same research groups on the same trials (Allaire 2005; de Buck 2004).
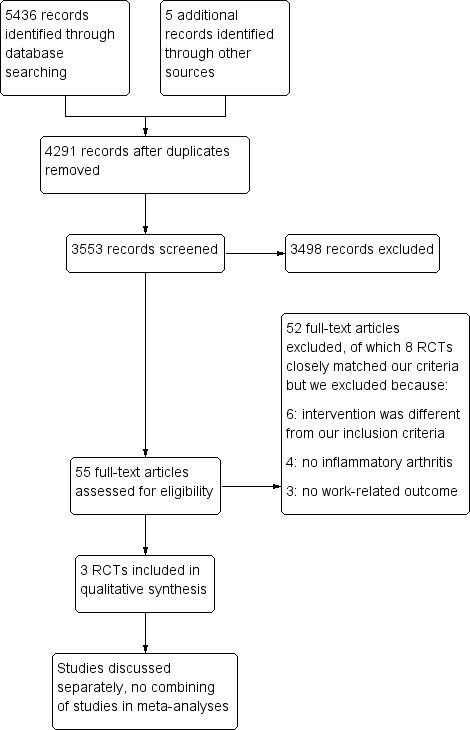
Study flow diagram.
Included studies
see Characteristics of included studies for details of all three RCTs.
Characteristics of included studies and participants
The trials by Allaire 2003 (USA), de Buck 2005 (Netherlands) and Macedo 2009 (UK) included a total of 414 participants, with 242, 140 and 32 participants, respectively. Participants in all three RCTs were recruited from rheumatology practices, inside or outside the hospital. The majority of participants had IA but the case mix varied: Allaire 2003 included participants with IA (RA, AS, PsA, SLE) but also a proportion with OA (36%), de Buck 2005 included participants with a mix of IA (RA, AS, PA or reactive arthritis) and Macedo 2009 included participants with RA. In all three RCTs, participants had a paid job and were considered at risk of losing their job or of work disability; in the de Buck 2005 trial some participants were already on extended sick leave (between 3% to 8% had sick leave> 40 weeks) at the start of the trial. Sick leave occurred before the start of the trial or at baseline, as in Macedo 2009 and de Buck 2005. de Buck 2005 reported between 39% to 42% of participants having more than six weeks of sick leave, and participants in Macedo 2009 had missed between two to three days in the past month. Data from the Allaire 2003 trial shows that all participants were 'at work' at baseline.
Intervention characteristics
The interventions reported in the three included RCTs aimed to prevent job loss and improve work functioning in several ways: firstly by a systematic assessment of work challenges or work adaptations, or both; and secondly by providing several person‐directed interventions including vocational counselling, advice or education. Interventions directly targeted at the work environment were minimal, and included workplace visits (Macedo 2009) or any actions by an occupational physician (de Buck 2005). The duration or dose of the interventions varied from two 1.5‐hour sessions over five months (Allaire 2003), two consultation and multidisciplinary treatments during three months (de Buck 2005), to six to eight individual or group sessions for six months (Macedo 2009).
In Allaire 2003, experimental group participants received a job retention vocational rehabilitation intervention designed for the trial; its focus was on job accomodation, vocational counselling, education and self‐advocacy. It was provided by one of two rehabilitation counsellors hired for the study in a community setting. Training on how to provide the intervention was provided to the counsellors. The experimental intervention was provided in two 1.5‐hour sessions over a five‐month period.This intervention may have had some similarity to services that could be provided to employed persons through the US public vocational rehabilitation program; the self‐advocacy component in particular was used (on disability rights etc.). Control group participants were sent printed information about disability‐related employment issues and resources in the postal mail; this was considered a minimal intervention, but more than the employment‐related care usually provided.
The multi‐disciplinary intervention described by de Buck 2005 was conducted in a hospital setting and care was provided by several hospital professionals (rheumatologist, social worker, physical therapy, occupational therapist and psychologist) with consultation by an occupational physician. de Buck 2005 provided multi‐disciplinary treatment over four to 12 weeks, including a discussion between the patient and a team coordinator and a report to the occupational physician. The control group were treated and referred to other health professionals in relation to their working problem if regarded necessary by their rheumatologist. Participants in both groups received written information about the Dutch social security system regarding sick leave and work disability.
The intervention by Macedo 2009 was provided by an occupational therapist experienced in vocational rehabilitation and rheumatology. The number of sessions varied. Macedo provided six to eight group sessions and individual sessions by the occupational therapist over six months lasting between 30 minutes and two hours, including a workplace visit for seven participants. The control group received usual care, which involved routine reviews by the rheumatologist, but no occupational therapy involvement.
In all interventions the start point included an assessment of workplace barriers, job or task evaluation, assessment of work problems or work challenges, along with subsequent analyses and treatment strategy to overcome these. For the assessment, Allaire 2003 used a screening tool called the augmented Work Experience Survey tool, and Macedo 2009 used a biopsychosocial model stemming from the Canadian Occupational Performance Measure (COPM). In de Buck 2005, a rheumatologist and a coordinator performed a systematic assessment, of medical and work‐related issues, using a list of potential challenges and psychosocial situations.
In all three RCTs, participant were recruited from rheumatology practices. Only de Buck 2005 clearly indicated that medical care was included in the intervention. Macedo 2009 stated that medical management and rheumatology clinic visit schedules were not changed from normal practice for either group and the participating clinics focused on early aggressive medical management with a goal of achieving remission. In contrast, standard medical treatment in Allaire 2003 was assumed as participants were recruited from rheumatologist's practices.
Outcome characteristics
Job loss was the only outcome reported in the RCTs by Allaire 2003 and de Buck 2005, and measured in various ways and at different time points. Both trials measured job loss counts (job losses were described as events in Allaire's trial). Allaire also makes a distinction between temporary and permanent job loss events. The outcomes sickness absenteeism and work functioning were only measured in the RCT by Macedo 2009.
Follow‐up times also varied: Macedo 2009 had a follow‐up of six months (i.e. intermediate term outcome), data on sickness absenteeism (cumulative work days missed) and work functioning (RA WIS: RA work instability scale), whereas both de Buck 2005 and Allaire 2003 reported job loss at six‐month intervals up to 24 and 48 months, respectively. In other words, de Buck 2005 and Allaire 2003 employed both intermediate (3‐12 months) and long term (>12 months) follow‐up. The Allaire 2003 trial originally had a follow‐up of 36 months with 80% of participants, but follow‐up was continued for a smaller proportion of participants (66%) up to 48 months. In addition, recruitment was staggered over time so that during the trial period not all participants completed the 36‐ or 48‐month follow‐up. Mainly because of this reason, the Allaire 2003 job loss counts were based on 12 and 24 months' follow‐up data.
Ongoing studies
We have identified three ongoing RCTs, which are listed in the Ongoing studies section. We obtained these through electronic database searching, i.e. published protocols (van Vilsteren 2012 and Carruthers 2014), or through our rheumatology experts on the review team (Keysor 2013). Updates of the current review should provide more evidence in coming years (see Characteristics of ongoing studies).
Excluded studies
Of the 11 studies that dealt with the topic of this review, we excluded eight studies for the following reasons (multiple reasons apply); 1) Intervention did not fulfill all criteria (six studies); 2) not sufficient workers with IA (four studies); and no work‐related outcome as specified in protocol (three studies). See Characteristics of excluded studies.
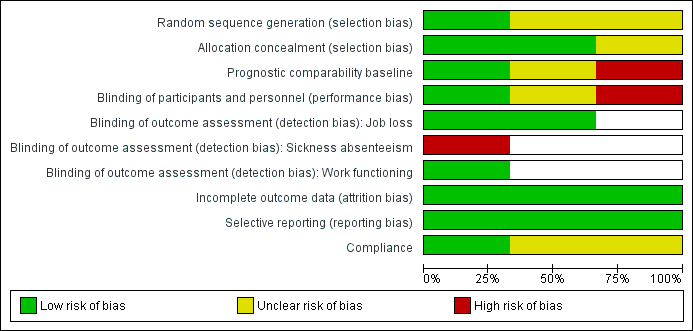
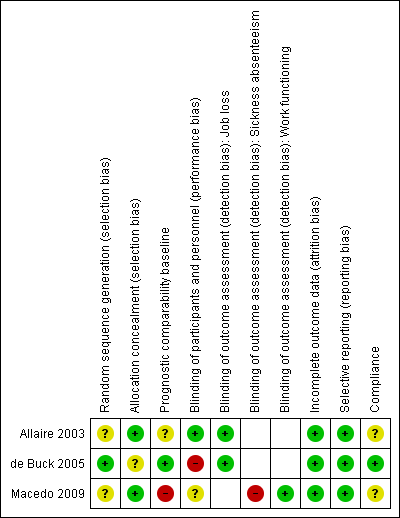
Risk of bias in included studies
For results of risk of bias assessment of RCTs, see the Characteristics of included studies section. We summarised the results in the risk of bias graph in Figure 2, which is an overview of the review authors' judgements about each risk of bias item presented as percentages across all included trials. Figure 3 shows the risk of bias summary of each risk of bias item for each included trial.
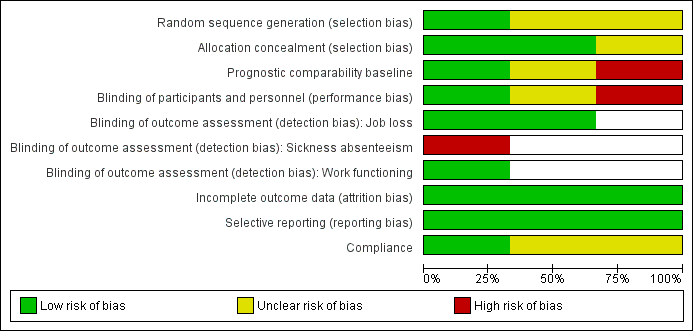
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included trials.
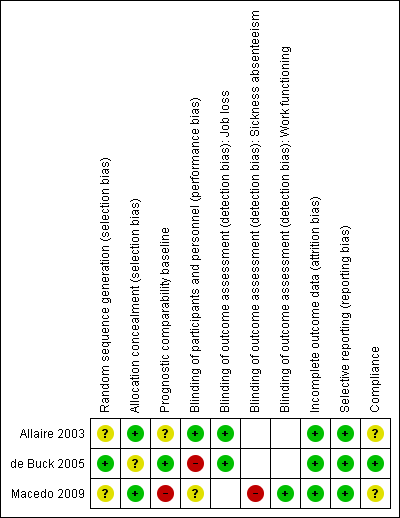
Risk of bias summary: review authors' judgements about each risk of bias item for each included trial.
Allocation
Allaire 2003 and Macedo 2009 provided insufficient information about sequence generation to permit judgement. Only de Buck 2005 adequately described sequence generation, using a randomisation list created by a random digit generator. de Buck 2005 provided insufficient information about allocation concealment. Allaire 2003 and Macedo 2009 used a statistician or independent research nurse to respectively create an access database requiring every participant to be entered before the randomisation code was provided, or perform sealed envelop randomisation respectively. We judged the risk of bias to be low for both RCTs.
Blinding
None of the three RCTs provided information about whether workers or the people performing the intervention were blinded. However, given the nature of the intervention provided (assessment, information, advice or counselling), it would have been impossible to blind the workers or at least some people performing the intervention to the allocation. de Buck 2005 asked workers not to inform the principal investigator or the research nurse about the type of care they received. All three outcomes in this review (job loss, sickness absenteeism or work functioning) were assessed through participant self‐report.
Performance bias (blinding of participants and intervention providers)
We judged the risk of bias to be unclear for performance bias (blinding participants and personnel) in the trial of Macedo 2009. Potentially personnel, the participants or the participants work colleagues were more aware or willing to support or influence the participants' work status, as a consequence of belonging to the experimental group or control group but for this trial we have no information that this happened. The extent of this effect remains unclear.
Allaire 2003 reported that participants were not told whether they had received either the experimental or control intervention. When enrolling subjects, participants were told they were testing two different ways of helping people stay employed. The counsellors provided intervention to experimental group participants only and did not know or have any contact with control group participants. Whether participants told their work colleagues about their trial participation is doubtful. Employers were not involved in any way in Allaire 2003. The researcher was blinded as to which participants were in each group (she had little contact with any participants – only brief contact with a few who called with a question when the research assistant was away). For this reason we judged the risk of bias to be low.
In the case of de Buck 2005, there are indications that participants and rheumatologists took extra effort providing care to the control group, as discussed by the trial authors. The experimental intervention consisted of at least two visits: a systematic (vocational) assessment and discussion of a multi‐disciplinary (vocational) report/plan. In addition, referral to education, counselling and different therapies (occupational therapist, physical therapist, exercise therapist, psychologist, rheumatology nurse, social worker) was provided based on the specific problems that were encountered in the (vocational) systematic assessment. It seems likely that participants and hospital personnel in the control group put extra effort into getting similar treatments as the experimental group. The number of referrals to the rheumatologist rose during the intervention period, and the control group received an equivalent number of therapies which were part of the experimental group intervention. As the control group received similar therapies, this affected the contrast between the experimental and control intervention. For this reason the RCT by de Buck 2005 was considered to have high risk of bias.
Detection bias (blinding of outcome assessors)
We considered the influence of detection bias to be potentially different across the three pre‐specified outcome measures of job loss (Allaire 2003; de Buck 2005), sickness absenteeism (Macedo 2009) and work functioning (Macedo 2009). We therefore evaluated the presence of detection bias separately for each outcome.
-
Job loss: in an older validation study, it was shown that self‐reported unemployment was in close agreement with the company administration of unemployment (Duncan 1985). We judged job loss a relative robust and objective measure given this information, even when it was self assessed as in Allaire 2003 and de Buck 2005. We therefore judged the risk of bias to be low.
-
Sickness absenteeism: we considered the self report data as reported by Macedo 2009 to have a high risk of bias, and not an objective measure. Participants had to remember how many days they missed from work and whether this was due to RA. The intervention was quite intensive with six months of comprehensive OT including workplace visits which may have influenced participants recall at the six month follow‐up. Certainly there would be more emphasis on the importance of job loss or taking sick leave, although it is not clear how big this effect would be in either group.
-
Job functioning: Macedo 2009 used the Rheumatoid Arthritis‐Work Instability Scale (RA‐WIS) which is a validated questionnaire with discrete items, judged to have a low risk of bias.
Incomplete outcome data
Allaire 2003 and de de Buck 2005 reported reasons for drop‐out of participants and had incomplete outcome data addressed. Macedo 2009 reported the same number of participants at baseline and six months, and stated no job loss during the six month follow‐up. Loss to follow‐up accounted for (total 25/140: 13/74 in I and 12/66 in C) 18% at 24 months for de Buck 2005 and was quite evenly distributed between experimental and control group, and baseline characteristics distribution of non‐completers were similar. Allaire 2003 originally had a 36‐month follow‐up, which was extended with an additional year of follow‐up. Recruitment was staggered and as a consequence not all participants were able to complete the 36‐month or 48‐month follow‐up. During the original 36‐month follow‐up, four participants dropped out of the intervention group and six from the control group, and one participant died in each group. The total reported attrition rate one year later, at 48 months, by Allaire 2003 was 18% in the intervention and 20% in the control. Allaire 2003 reported that most of the drop‐outs were participants who chose not to participate in the additional year of follow‐up (up to 48 months). For all three trials, the risk of bias was considered to be low.
Selective reporting
All included RCTs were judged to be free of selective reporting of the outcomes because all outcomes described in the methods were reported.
Other potential sources of bias
Prognostic comparability
For two out of the three included RCTs we raised some questions about baseline comparability. Allaire 2003 showed that baseline factors were comparable between groups on all variables presented, but did not assess the extent of previous work absenteeism, job or disease duration. For de Buck 2005, the effect of some baseline differences is unclear: there was a difference in the number of participants with a sick leave of > 40 weeks (8% in the intervention group and 3% in the control group). Though not statistically significant, sick leave is likely to influence the likelihood of job loss, as it is more difficult to return to work after prolonged sick leave.
As Macedo 2009 only had 32 participants in their RCT, any differences in prognostic factors will have a larger impact on the results. We judged the risk of bias higher in this trial for several reasons. Baseline imbalances, with reference to the experimental group, included longer disease duration, more workers with full time employment, more university postgraduates and younger people. All these factors favour a better prognosis with regard to the outcome 'work days missed' in the experimental group.
Compliance
We judged compliance in de Buck 2005 trial at low risk of bias even though few participants were seen by their companies' occupational physician and did not receive additional guidance. We judged unclear risk of bias due to the absence of information in Macedo 2009 and Allaire 2003.
Overall judgement of risk of bias
We judged overall risk of bias for each study. We judged Allaire 2003 to have an overall low risk of bias, de Buck 2005 trial to have an overall high risk of bias due to performance bias and Macedo 2009 to have an overall high risk of bias due to detection bias and baseline imbalances.
Effects of interventions
All three included RCTs evaluated the effects of job loss prevention (see Types of interventions) in workers at risk of job loss with IA compared to a control intervention consisting of usual care or information, or both. To establish the effectiveness of job loss prevention versus control intervention we looked at three outcomes: job loss and sickness absenteeism as primary outcomes, and work functioning as a secondary outcome. See summary of findings Table for the main comparison for details.
1. Job loss prevention versus control
1.1 Job loss
1.1.1 to 1.1.4 Long term effects
A priori we defined the number of participants with a job loss as the most relevant job loss outcome, based on the goal of the intervention (i.e. job retention). The number of participants with a job loss (Analysis 1.1) was the only outcome reported by more than one trial (Allaire 2003; de Buck 2005). We retrieved data from two RCT publications by Allaire (Allaire 2003; Allaire 2005) and only one for De Buck (de Buck 2005). Short term data were not provided by both RCTs, unsurprisingly as the intervention period took between three and five months to complete on average, and job loss would take time to occur. Therefore, we only present long term data of one year or more. The main comparison for job loss reported by both Allaire 2003 and de Buck 2005 was long term job loss measured at 12 and 24 months, which were considered relevant and reliable. Allaire 2003 reports a long term statistically significant reduction in the number of participants with a job loss in the experimental group compared to the control group, represented by a 12‐month relative risk of 0.32 (95% CI 0.11 to 0.97) and a 24‐month relative risk of 0.35 (95% CI 0.18 to 0.68) (see Analysis 1.1). This represents an absolute difference of ‐7.0% (95% CI 13.2% to ‐0.6%) at 12 months and a ‐16.0% (95% CI ‐25.4% to ‐6.6%) absolute difference at 24 months. Similarly, the number needed to treat was 14.4 at 12 months and 6.2 at 24 months in favour of the job loss prevention intervention. Though the magnitude of this effects is quite large, it is only reported in one RCT (Allaire 2003).
In contrast, de Buck 2005 reported no difference in job losses in favour of any group, neither at 12 months or at 24 months, as represented by a RR of 0.99 (95% CI 0.47 to 2.07) at 12 months and a RR of 1.05 (95% CI 0.53 to 2.06) at 24 months. Absolute differences are respectively ‐0.2% (95% CI ‐14.1% to 13.7%) at 12 months and 1.1% (95% CI ‐14.6% to 16.7%) at 24 months.
We did not pool the data for job loss reported above as statistical heterogeneity (I² > 80%) was considerable and would lead to non‐informative pooled estimates (see Analysis 1.1). Follow‐up times in the Allaire 2003 extended beyond 24 months up to 48 months but as stated previously, recruitment was staggered in Allaire 2003 and follow‐up data after 30 months were considered unreliable when reporting count data in calculation of RRs. Using a pooled logistic model, analyses reported by Allaire 2003 for time to any type of job loss over 48 months, adjusting for confounders, showed an overall odds ratio of 0.58 (95% CI 0.34 to 0.99), in line with individual previous results at 12, 24 and 30 months.
1.2 Sickness absenteeism
Macedo 2009 only reported sickness absenteeism at six months (Analysis 1.2), which is an intermediate term follow‐up. The results show a reduction of 2.4 sick days in the experimental group (MD ‐2.42, 95% CI ‐5.03 to 0.19) compared to the control group, measured over the past month but the CI around the estimated reduction is wide and also includes a possible small increase.
1.3 Work functioning
Macedo 2009 reported work functioning at six months using the RA‐WIS which ranges from 0 to 28 points, a higher score reflecting more risk of work disability. At six months the mean difference between the RA‐WIS score in the control and the RA‐WIS score in the experimental group was ‐4.67 points (‐8.43 to ‐0.91), in favour of the experimental group (Analysis 1.3).
Adverse effects
None of the included trials reported any adverse effects as a result of the intervention.
Other outcome data
We present effects of other supporting job loss outcome data that were reported in the trials including data on job loss events over 48 months, combined job loss or increase of disability pension data, or sickness absenteeism defined as workdays missed as proportion of days worked for informative purposes in Table 1. These results (Analysis 1.4; Analysis 1.5; Analysis 1.6) do not contribute to the conclusions.
| Outcome measures | Follow‐up times | Trials | Extra analyses |
| Combined job loss or increase of disability pension | 24 months | ||
| Job loss events | 48 months | ||
| Sickness absenteeism defined as workdays missed in proportion to days worked |
In this table we present other supporting job loss outcome data reported in the trials for informative purposes only. These data do not contribute to our conclusions.
Sensitivity analyses
We did not perform sensitivity analyses by omitting trials judged to be at high risk of bias, or using a random‐effects model for pooling data due to a lack of data in any one category and the absence of pooling.
Subgroup analyses and analyses of heterogeneity
Although we had planned subgroup analyses to assess the influence of the most prevalent diagnosis categories, the inclusion of vocational intervention with or without additional (multi‐disciplinary) interventions, these were not possible.
Discussion
Summary of main results
Overall we found very low quality evidence for a reduction of job loss in the long term in participants with IA for job loss prevention compared to a control intervention consisting of usual care or information. We downgraded the quality of evidence because of differences in findings between two trials: one large RCT (Allaire 2003) reported a large statistically significant reduction in job loss (RR 0.35, 95% CI 0.18 to 0.68) while the other (de Buck 2005) reported no effect (RR 1.05, 95% CI 0.53 to 2.06). We judged the first RCT (Allaire 2003) on vocational counselling as having an overall low risk of bias. We evaluated the second RCT (de Buck 2005) that used a mix of multi‐disciplinary and vocational elements to have an overall high risk of bias, and it probably suffered substantially from performance bias.
We also found very low quality evidence for a small non‐significant reduction (MD ‐2.42, 95% CI ‐5.03 to 0.19) of intermediate term sickness absenteeism (six months) in participants with IA, reported by one small underpowered RCT (Macedo 2009). This trial provided occupational therapy in group and individual sessions with vocational elements and was evaluated as having an overall high risk of bias. In addition, there was very low quality evidence for a moderate improvement of intermediate term work functioning (six months) ‐4.67 points (‐8.43 to ‐0.91) in participants with RA, reported by Macedo 2009.
Overall completeness and applicability of evidence
As presented in the Characteristics of included studies, one could question whether the three included RCTs were similar enough to be combined. A priori, the selection criteria for the interventions and outcomes in this review were considered quite strict and excluded a number of RCTs. In this sense, we combined specific types of interventions that primarily aim to reduce sickness absenteeism and prevent job loss, referred to by us as 'job loss prevention'. Nonetheless, the three trial interventions show differences regarding the duration of the intervention period and number of contact moments, the professionals involved, the setting or in the way the content of the job loss prevention components were delivered (see Types of interventions). We found that the trial authors provided little information on the hypothesized working mechanism of the interventions, making it harder to base the combining of studies on any solid theory (Verbeek 2012) through the descriptions of the interventions. Likewise, it was unclear how the optimal dosage or delivery (sessions, duration, etc.) was determined. It is clear that all three trial interventions focus around coaching, advising and the provision of information to the participant. With the exception of some workplace visits (Macedo 2009) and a few contacts with the participants' occupational physicians (de Buck 2005), the workplace was not directly involved.
We acknowledge that variation in effectiveness may exist between these trial interventions which should be investigated if more trials allow for subgroup analyses in future updates of this review. Control interventions included medical treatment but also included other co‐interventions described in a superficial manner in Allaire 2003, de Buck 2005 and Macedo 2009. It could be argued that given the available resources in the community, health care and increasingly on the internet, people can manage their work‐related challenges in many ways (Hoving 2013). This may require more understanding of how we interpret control interventions labelled as 'care‐as‐usual' or 'provision of pamphlets', and allow for better descriptions of these control interventions.
In the US trial, Allaire 2003 shows that more than one out of six job losses (risk difference 16%) can be prevented using vocational counselling in contrast to the absence of any job loss reduction for multi‐disciplinary vocational rehabilitation in the Dutch trial by de Buck 2005. The marked differences in effect on the outcome job loss begs the question if other variables than intervention characteristics could explain this difference. Over half of all trial participants in de Buck 2005 were on sick leave at baseline, and about 40% for longer than six weeks. Return to work after long sick leave may require more motivation and effort compared to keeping one's job while working. Given this long‐term sick leave, workers in de Buck 2005 possibly had more severe limitations in work capacity making reintegration more difficult and permanent work disability more unavoidable compared to the workers in Allaire 2003.
Socioeconomic differences are also believed to explain differences in effect of job loss prevention efforts between countries (Anema 2009). Paid sick leave for up to one year, possibly followed by long term disability benefits was customary for Dutch employees in 2001 during the trial period of de Buck 2005. Permanent work disability thus may have been easier to accept by Dutch trial participants. Whereas incentives in the US were different, with workers having a greater at risk of income loss if they choose to stop work permanently, and having less compensation for the initial days of sickness absence, and having a greater risk of dismissal after long‐term incapacitation (Anema 2009). However, the extent to which these differences in incentives explain the differences in effect between de Buck 2005 and Allaire 2003 remains uncertain.
All three trials included participants with IA, but Allaire 2003 also included participants with OA and Macedo 2009 only included participants with RA. We consider the interventions provided to be broadly applicable in the sense that they may be applied to many persons with progressive joint disorders who are at risk of job loss, but more trials are needed. The interventions in our review target the consequences of the disease and we believe that the intervention components in the review are potentially beneficial across many types of IA. However, the low number of included trials precludes any subgroup analyses at this point. Adverse effects were not reported in any of the RCTs. Given our extensive search and the low number of studies, we believe we have included all RCTs.
Quality of the evidence
Following the results for the GRADE assessment (see summary of findings Table for the main comparison) we found the following results for (1) risk of bias, (2) inconsistency, (3) indirectness, (4) imprecision and (5) publication bias.
-
Risk of bias: we judged this as serious (‐1) for each of the three outcomes, based on the assessment of the risk of bias across all RCTs where several items scored unclear or high risk of bias. Therefore we downgraded the quality of the evidence by one level (‐1).
-
Inconsistency: we considered inconsistency to be very serious for the outcome job loss, suggesting true differences in underlying treatment effect, with almost no overlap in the CIs of the relative risks of two RCTs. As we failed to identify a plausible explanation for the inconsistency, we downgraded the quality of the evidence by two levels (‐2). For the outcomes sickness absenteeism and work functioning we only had one RCT, hence we judged inconsistency to be not serious and thus we did not downgrade the quality of the evidence.
-
Indirectness: we judged it to be a minor issue in all comparisons as we could not detect any. We did not downgrade the quality of the evidence for this reason.
-
Imprecision: results are imprecise when studies include relatively few participants or events and thus have wide CIs around the estimate of effect (RR or MD). For job loss we included two RCTs but the heterogeneity prevented us from pooling these trials. Hence we looked at individual RCTs. The 'threshold rule of thumb value' states there should be at least 300 events for job loss (dichotomous outcome), and for the continuous outcomes there should be at least 400 participants (Higgins 2011). None of the included trials fulfilled this criterion, and neither did any of the comparisons, for any of the outcomes. Macedo 2009 had only 32 participants and we considered it to have very serious imprecision for the outcomes sickness absenteeism and work functioning. Thus, we downgraded the quality of the evidence by two levels (‐2). The other two RCTs reporting on job loss were larger and we judged them to have serious imprecision, and we downgraded the quality of the evidence by just one level (‐1).
-
Publication bias: given the low number of included trials we were not able to analyse publication bias with funnel plots or tests.
The quality of the evidence was variable across the three included RCTs. On the level of outcomes, the investigation of sickness absenteeism could be improved by using sickness registries or employer databases, and as such use more objective outcomes. However, confidentiality issues and availability of such registries might limit the feasibility of using such data sources.
As in the de Buck 2005 trial, contrast between interventions was a major issue and this may have been present in the other studies, especially in the Macedo 2009 trial where there were few participants. This may be particularly problematic if participants perceive that they have received the 'non‐effective' treatment, which can create biased outcome assessments and bias whereby workers assigned to the control group might seek other interventions (see de Buck 2005). Allaire 2003 provided written information in the control group (and experimental group) but this may not have been perceived as sufficiently valuable to prevent participants in the control group from seeking additional resources. Providing participants with a reasonable alternative intervention may therefore be considered if blinding cannot be guaranteed, as is the case in these types of interventions.
Potential biases in the review process
The primary investigator of the Allaire 2003 trial, Saralynn Allaire , helped us with study screening and by commenting drafts of text. However, she did not participate in data extraction, GRADE assessment or risk of bias assessment of any of the included studies, including Allaire 2003. Similarly we strived to minimise the possible effects of our personal views by having every single step in the review process performed independently by at least two review authors.
We identified some publications in languages other than English during study screening stage but none of them fulfilled our inclusion criteria.
We included only three trials, of which two were essentially positive and the other showed no difference. Although we had an extensive search strategy in several electronic databases we cannot exclude the possibility of publication bias, i.e. that we missed negative trials that did not reach the published literature. For this reason we welcome contact from any readers who are aware of any important trials that would meet the inclusion criteria of this review but are not included so far.
Agreements and disagreements with other studies or reviews
We only know of two other systematic reviews, one by de Buck 2002 and the other by Vliet Vlieland 2009. The review by de Buck 2002 was based on six non‐controlled studies and reported that five of six studied vocational rehabilitation programs consisted of multidisciplinary intervention and 15% to 69% of the participants successfully returned to work. Vliet Vlieland 2009 performed a narrative review of a range of vocational rehabilitation studies on chronic arthritis including the studies by de Buck 2005 and Allaire 2003. Vliet Vlieland 2009 also included studies that did not fulfil our selection criteria regarding disease types, interventions or outcomes. We present our reasons for excluding all these studies in the Characteristics of excluded studies. The conclusion by Vliet Vlieland 2009 was that "results of studies on interventions employed in the early phases of sick leave are promising". Their findings stress the need for early identification of persons at risk for work disability in stages when an intervention would be most effective. We agree with this, but we think this is not enough. We think additional efforts should be taken to come up with a sound theory or working mechanism for interventions that try to prevent job loss, i.e. what works for whom and for what reason?
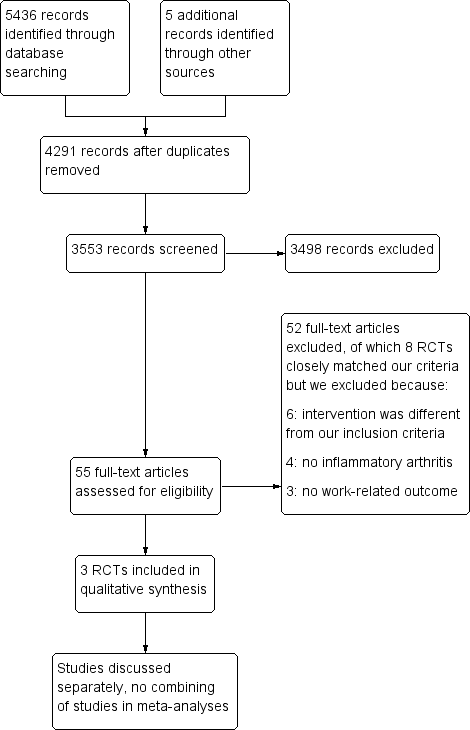
Study flow diagram.
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included trials.
Risk of bias summary: review authors' judgements about each risk of bias item for each included trial.
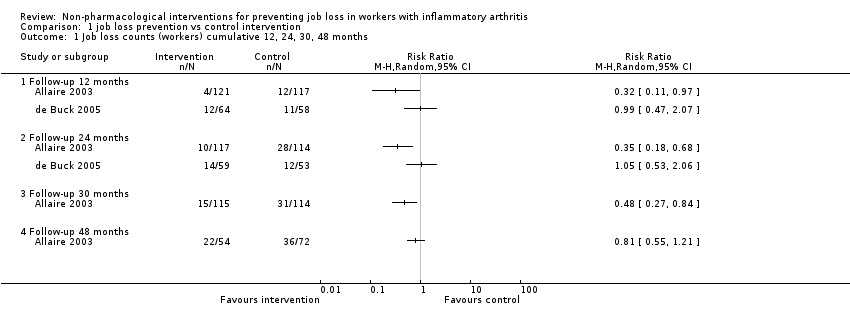
Comparison 1 job loss prevention vs control intervention, Outcome 1 Job loss counts (workers) cumulative 12, 24, 30, 48 months.
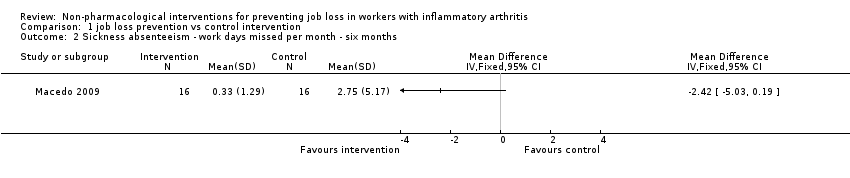
Comparison 1 job loss prevention vs control intervention, Outcome 2 Sickness absenteeism ‐ work days missed per month ‐ six months.
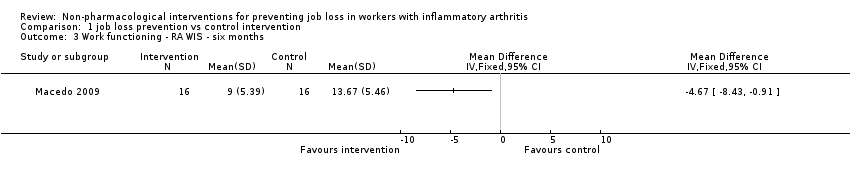
Comparison 1 job loss prevention vs control intervention, Outcome 3 Work functioning ‐ RA WIS ‐ six months.
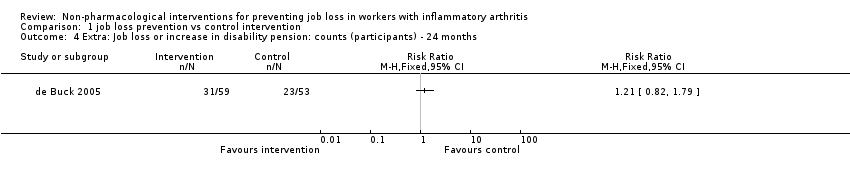
Comparison 1 job loss prevention vs control intervention, Outcome 4 Extra: Job loss or increase in disability pension: counts (participants) ‐ 24 months.
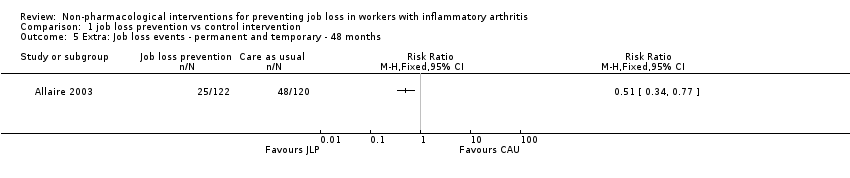
Comparison 1 job loss prevention vs control intervention, Outcome 5 Extra: Job loss events ‐ permanent and temporary ‐ 48 months.
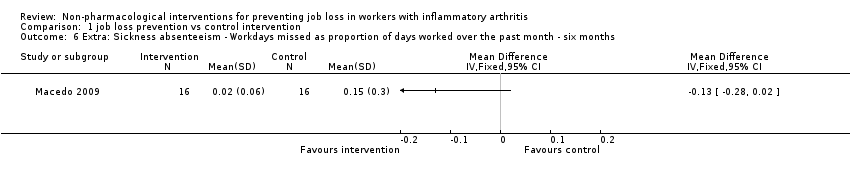
Comparison 1 job loss prevention vs control intervention, Outcome 6 Extra: Sickness absenteeism ‐ Workdays missed as proportion of days worked over the past month ‐ six months.
| Job loss prevention compared to control intervention in people with IA | ||||||
| Patient or population: people with IA | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control intervention 7 | Job loss prevention | |||||
| Job loss | See comment | See comment | Not estimable | 340 | ⊕⊝⊝⊝ | Due to inconsistency in the trials we did not pool these two trials |
| Sickness absenteeism | The mean sickness absenteeism in the control groups was | The mean sickness absenteeism in the intervention groups was | ‐ | 32 | ⊕⊝⊝⊝ | ‐ |
| Work functioning | The mean work functioning in the control groups was | The mean work functioning in the intervention groups was | ‐ | 32 | ⊕⊝⊝⊝ | ‐ |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 We judged the RCTs by de Buck 2005 and Macedo 2009 to have an overall high risk of bias and the RCT by Allaire 2003 to have an overall low risk of bias. Overall, we judged serious risk of bias to be present and therefore we downgraded the quality of the evidence by one level (‐1). 7 All control groups received either usual care or a minimal intervention such as written information in Allaire 2003. | ||||||
| Outcome measures | Follow‐up times | Trials | Extra analyses |
| Combined job loss or increase of disability pension | 24 months | ||
| Job loss events | 48 months | ||
| Sickness absenteeism defined as workdays missed in proportion to days worked | |||
| In this table we present other supporting job loss outcome data reported in the trials for informative purposes only. These data do not contribute to our conclusions. | |||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Job loss counts (workers) cumulative 12, 24, 30, 48 months Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Follow‐up 12 months | 2 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Follow‐up 24 months | 2 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Follow‐up 30 months | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Follow‐up 48 months | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Sickness absenteeism ‐ work days missed per month ‐ six months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Work functioning ‐ RA WIS ‐ six months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Extra: Job loss or increase in disability pension: counts (participants) ‐ 24 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Extra: Job loss events ‐ permanent and temporary ‐ 48 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Extra: Sickness absenteeism ‐ Workdays missed as proportion of days worked over the past month ‐ six months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |

