Intervenciones quirúrgicas para el tratamiento de la fractura del olécranon en adultos
Appendices
Appendix 1. Search strategies
Cochrane Central Register of Controlled Trials (CENTRAL)
#1 MeSH descriptor: [Olecranon Process] explode all trees (3)
#2 olecranon*:ti,ab,kw (25)
#3 #1 or #2 (25)
#4 MeSH descriptor: [Fractures, Bone] this term only (1196)
#5 MeSH descriptor: [Fracture Fixation] explode all trees (1248)
#6 MeSH descriptor: [Fracture Healing] this term only (402)
#7 fractur*:ti,ab,kw (9806)
#8 #4 or #5 or #6 or #7 (9810)
#9 #3 and #8 (14) [trials]
MEDLINE (Ovid Online)
1 Olecranon Process/ (154)
2 olecranon*.tw. (1517)
3 or/1‐2 (1536)
4 Fractures, Bone/ or exp Fracture Fixation/ or Fracture Healing/ (89,293)
5 fractur*.tw. (178,797)
6 or/4‐5 (203,618)
7 and/3,6 (890)
8 Randomized controlled trial.pt. (388,776)
9 Controlled clinical trial.pt. (89,842)
10 randomized.ab. (308,669)
11 placebo.ab. (159,706)
12 Drug therapy.fs. (1,744,944)
13 randomly.ab. (222,781)
14 trial.ab. (321,451)
15 groups.ab. (1,405,245)
16 or/8‐15 (3,447,063)
17 exp Animals/ not Humans/ (4,011,377)
18 16 not 17 (2,960,678)
19 and/7,18 (62)
EMBASE (Ovid Online)
1 Olecranon Fracture/ (598)
2 Olecranon/ (356)
3 olecranon*.tw. (1744)
4 or/2‐3 (1826)
5 exp Fracture Treatment/ or exp Fracture/ (234,864)
6 fractur*.tw. (210,718)
7 or/5‐6 (293,596)
8 and/4,7 (1038)
9 or/1,8 (1216)
10 Randomized controlled trial/ (352,502)
11 Clinical trial/ (838,245)
12 Controlled clinical trial/ (387,095)
13 Randomization/ (63,274)
14 Single blind procedure/ (18,833)
15 Double blind procedure/ (117,924)
16 Crossover procedure/ (40,233)
17 Placebo/ (258,577)
18 Prospective study/ (261,871)
19 ((clinical or controlled or comparative or placebo or prospective* or randomi#ed) adj3 (trial or study)).tw. (784,191)
20 (random* adj7 (allocat* or allot* or assign* or basis* or divid* or order*)).tw. (190,578)
21 ((singl* or doubl* or trebl* or tripl*) adj7 (blind* or mask*)).tw. (169,613)
22 (cross?over* or (cross adj1 over*)).tw. (72,540)
23 ((allocat* or allot* or assign* or divid*) adj3 (condition* or experiment* or intervention* or treatment* or therap* or control* or group*)).tw. (251,675)
24 RCT.tw. (14,794)
25 or/10‐24 (1,956,486)
26 Case Study/ or Abstract Report/ or Letter/ (948,253)
27 25 not 26 (1,917,135)
28 and/9,27 (94)
Current Controlled Trials
Search: olecranon
Total = (9)
ClinicalTrials.gov
Search: olecranon
Total = 9
World Health Organization (WHO) International Clinical Trials Registry platform
Search: olecranon
Total = 8
Appendix 2. Cable pin system (CPS)
Cable pin system Zimmer®: 2 x 4.0‐mm diameter, specially sharpened, partially threaded cancellous lag screws (pin length 35‐60 mm). The tail of the pin is connected to a stainless steel multi‐filament cable (diameter 1.3 mm, length 448 mm) and the other end of the cable is attached to a smooth shank end, which is used as a leader needle.
Operative technique: 2.5‐mm‐diameter drill bit was used to drill the holes, the first hole was drilled from the proximal end of the olecranon across the fracture site. The hole depth was measured and a pin of appropriate length was chosen. Next, the threaded portion of the pin was drilled across the fracture site through the hole until the tail was slightly countersunk into the bone. A second 2.5‐mm‐diameter hole was drilled parallel to the first, and the second pin was drilled across the fracture site in a similar manner to the first. The third drill hole was created perpendicular to the long axis of the ulna and posterior to the pins, at the same or slightly longer distance from the fracture site as the tip of the olecranon (usually 3‐4 cm distal to the fracture site). The 2 cables connecting the pins were crossed in a figure of 8 over the posterior surface of the olecranon. The leader needle of 1 cable was passed through the perpendicular drill hole (the third hole) in the ulna and pulled out. The free ends of the 2 cables were passed in opposite directions through a crimp, and the cables were adjusted by turning the button on the crimper tensioning handle. When the appropriate tension was achieved, the arms of the crimper tensioning handle were squeezed to secure the crimp.
Appendix 3. Disabilities of the Arm, Shoulder, and Hand Score (DASH)
The DASH questionnaire is a regional outcome measure suitable for people with musculoskeletal conditions of the upper limb and consists of 30 items (Hudak 1996).
DASH score assesses 6 domains: daily activities, symptoms, social function, work function, sleep and confidence. Each item in the daily activities domain is scored on a 5‐point scale, from 'no difficulty' to 'unable to do'. The other domains are also scored on a 5‐point scale.
The total score ranges from 0 (no disability) to 100 (severe disability).
Appendix 4. Mayo Elbow Performance Score (MEPS)
Pain: scale with a maximum of 45 points (Morrey 1995): 45 = no pain; 30 = mild pain; 15 = moderate pain; 0 = severe pain
Movement scale: maximum 20 points: 30 = arc > 100°; 15 = arc 50‐100°; 5 = arc < 50°
Stability scale: maximum of 10 points: 10 = stable; 5 = moderately unstable; 0 = grossly unstable
Functions of daily living: scale with a maximum of 25 points: 5 points each for being able to comb hair, feed oneself, perform personal hygiene, put on a shirt and put on shoes
MEPS total score is graded as: ≥ 90 points = excellent; 75‐89 points = good; 60‐74 points = fair; < 60 point = poor.
Appendix 5. Modified Murphy Scoring System
Modified Murphy Scoring System consists of 4 domains ‐ pain, function, range of movement and joint space ‐ with a total score of 4‐19 points: 18‐19 points = excellent; 17 points = good; 16 points = fair; < 16 points = poor (Murphy 1987).
Appendix 6. Helm criteria
The Helm criteria include pain, range of movement and revision surgery for operative failure (Helm 1987). No more than slight or occasional pain, loss of movement of < 15° at the elbow = good; occasional to moderate pain, loss of movement 15‐30° at the elbow = fair; constant pain, loss of movement > 30° at the elbow or operative failure needing revision surgery ‐ poor.
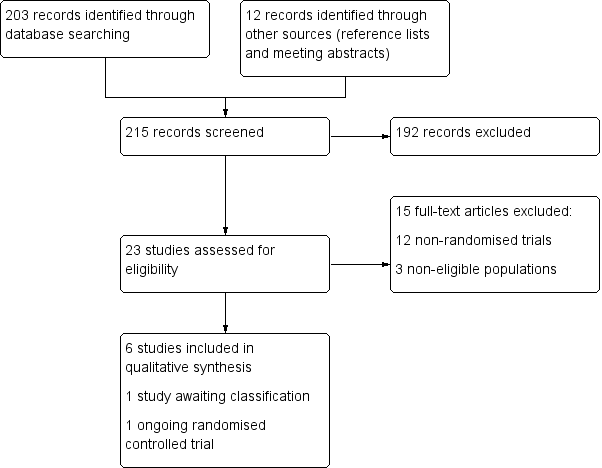
Flow diagram of search results.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Comparison 1 Plate fixation versus tension band wiring, Outcome 1 Good clinical outcome (little pain or loss of elbow motion: Helm criteria) 16‐86 weeks follow‐up.

Comparison 1 Plate fixation versus tension band wiring, Outcome 2 Adverse events.
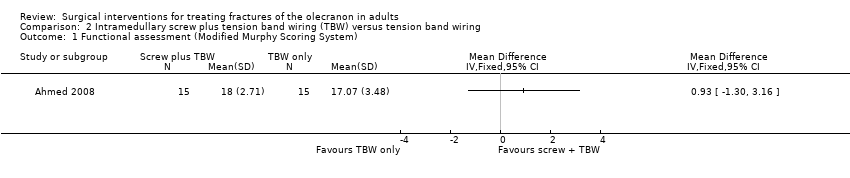
Comparison 2 Intramedullary screw plus tension band wiring (TBW) versus tension band wiring, Outcome 1 Functional assessment (Modified Murphy Scoring System).

Comparison 2 Intramedullary screw plus tension band wiring (TBW) versus tension band wiring, Outcome 2 Murphy score (including function, pain, loss of movement, joint space): excellent or good result.
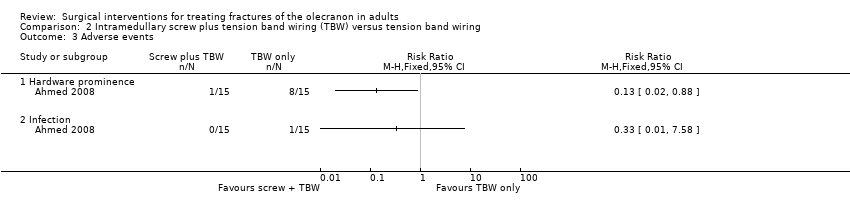
Comparison 2 Intramedullary screw plus tension band wiring (TBW) versus tension band wiring, Outcome 3 Adverse events.

Comparison 2 Intramedullary screw plus tension band wiring (TBW) versus tension band wiring, Outcome 4 Loss in flexion > 20°.
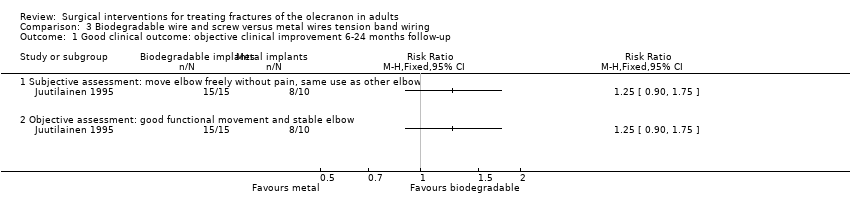
Comparison 3 Biodegradable wire and screw versus metal wires tension band wiring, Outcome 1 Good clinical outcome: objective clinical improvement 6‐24 months follow‐up.

Comparison 3 Biodegradable wire and screw versus metal wires tension band wiring, Outcome 2 Painless elbow joint.

Comparison 3 Biodegradable wire and screw versus metal wires tension band wiring, Outcome 3 Normal range of movement.

Comparison 4 Netz pins versus K‐wires tension band wiring (TBW), Outcome 1 Adverse events (4‐54 weeks follow‐up).
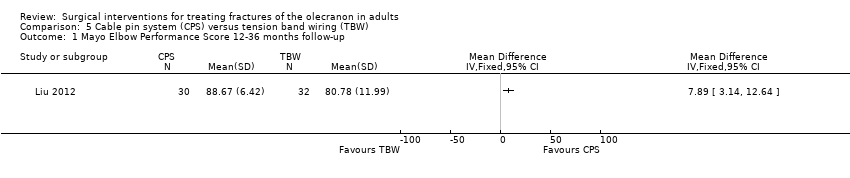
Comparison 5 Cable pin system (CPS) versus tension band wiring (TBW), Outcome 1 Mayo Elbow Performance Score 12‐36 months follow‐up.
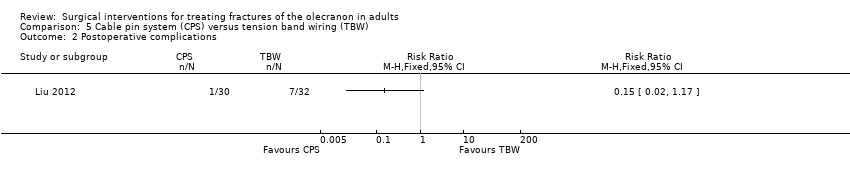
Comparison 5 Cable pin system (CPS) versus tension band wiring (TBW), Outcome 2 Postoperative complications.

Comparison 5 Cable pin system (CPS) versus tension band wiring (TBW), Outcome 3 Operation time and blood loss.
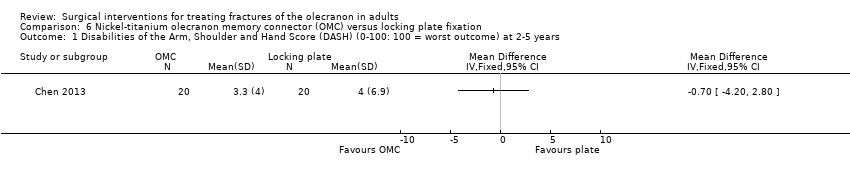
Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 1 Disabilities of the Arm, Shoulder and Hand Score (DASH) (0‐100: 100 = worst outcome) at 2‐5 years.
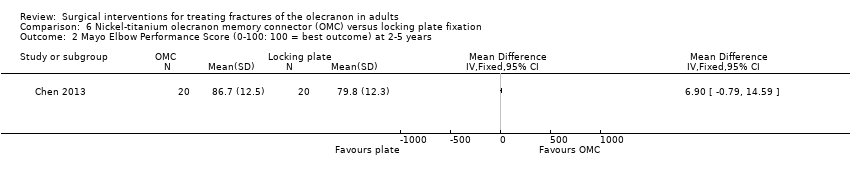
Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 2 Mayo Elbow Performance Score (0‐100: 100 = best outcome) at 2‐5 years.
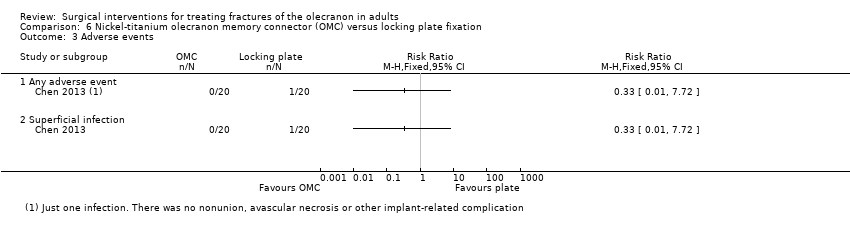
Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 3 Adverse events.
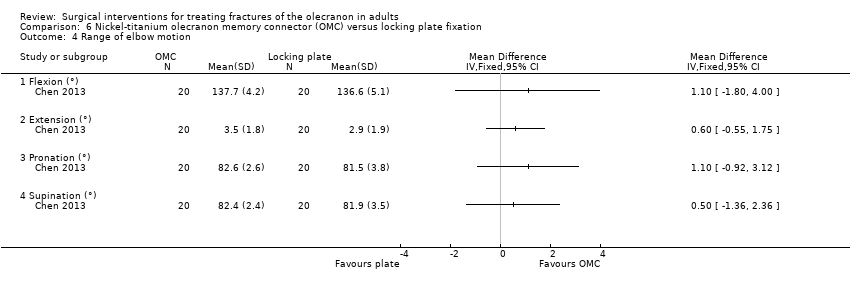
Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 4 Range of elbow motion.
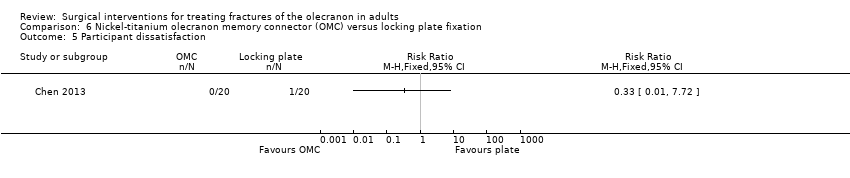
Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 5 Participant dissatisfaction.
| Plate fixation compared with tension band wiring for treating olecranon fractures in adults | ||||||
| Patient or population: adults with olecranon fractures Settings: hospital Intervention: plate fixation (using 1/3 tubular plates) Comparison: tension band wiring fixation | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk1 | Corresponding risk | |||||
| Tension band wiring | Plate fixation | |||||
| Functional assessment (e.g. via patient‐reported outcome measures of elbow function) | see Comments | see Comments | ‐ | ‐ | ‐ | Not reported. 1 ongoing trial (67 participants) testing this comparison will be reporting DASH (Disabilities of the Arm, Shoulder and Hand) scores at 1 year (NCT01391936) |
| Good clinical outcome (little pain or loss of elbow motion: Helm criteria) Follow‐up: mean 28.5 weeks, range 16‐86 weeks | Study population | RR 1.82 (1.10 to 3.01) | 41 participants | ⊕⊝⊝⊝ | Results were rated 'good' if there was no more than slight or occasional pain, loss of movement was less than 15° at the elbow and no revision surgery for operative failure | |
| 474 per 1000 | 863 per 1000 | |||||
| Pain | see Comments | see Comments | ‐ | 41 participants | ‐ | Separate pain data were not available; these should be in the 1 ongoing trial (67 participants) testing this comparison (NCT01391936) |
| Adverse events ‐ overall | see Comments | see Comments | ‐ | 41 participants | ‐ | Incomplete reporting and discrepancies in the reporting of infection meant that numbers of participants with ≥ 1 adverse events data could not be reported here |
| Adverse events ‐ symptomatic metal prominence Follow‐up: mean 28.5 weeks, range 16‐86 weeks | Study population | RR 0.11 (0.01 to 0.79) | 41 participants | ⊕⊝⊝⊝ | Metalwork prominence is a well‐known problem of tension band wiring. Symptoms were local discomfort or pain over the implant. There was no record of implant removal surgery in either group | |
| 421 per 1000 | 46 per 1000 | |||||
| Adverse events ‐ delayed or non‐union Follow‐up: 6 months | Study population | RR 0.17 [0.01 to 3.41] | 41 participants | ⊕⊝⊝⊝ | Surgical treated (debridement) infection preceded both cases in the tension band wiring group | |
| 106 per 1000 | 18 per 1000 | |||||
| Adverse events ‐ heterotopic ossification (bone formation) Follow‐up: mean 28.5 weeks, range 16‐86 weeks | Study population | RR 0.29 [0.01 to 6.72] | 41 participants | ⊕⊝⊝⊝ | The single participant with heterotopic ossification in the tension band wiring group developed ulnar neuropathy | |
| 53 per 1000 | 16 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1. The basis of the assumed risk is that for control group (tension band wiring) in the study population. 2. The evidence was downgraded 2 levels for limitations in design and implementation (including lack of blinding and spread of timing of outcome measurement) and 1 level for indirectness (the Herm criteria were not validated and could be considered surrogate to functional outcome). 3. The evidence was downgraded 2 levels for limitations in design and implementation (including lack of blinding and spread of timing of outcome measurement) and 1 level for imprecision. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Good clinical outcome (little pain or loss of elbow motion: Helm criteria) 16‐86 weeks follow‐up Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Metal prominence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Delayed or non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Heterotopic ossification | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Functional assessment (Modified Murphy Scoring System) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Murphy score (including function, pain, loss of movement, joint space): excellent or good result Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Hardware prominence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Loss in flexion > 20° Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Good clinical outcome: objective clinical improvement 6‐24 months follow‐up Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Subjective assessment: move elbow freely without pain, same use as other elbow | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Objective assessment: good functional movement and stable elbow | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Painless elbow joint Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Normal range of movement Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Adverse events (4‐54 weeks follow‐up) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Metalwork removed (all reasons, including 'routine') | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Metalwork removed because of symptoms (pin/cerclage affecting skin; pain) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Superficial infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Intraoperative complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mayo Elbow Performance Score 12‐36 months follow‐up Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Postoperative complications Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Operation time and blood loss Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Operation time (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Intraoperative blood loss (mL) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Disabilities of the Arm, Shoulder and Hand Score (DASH) (0‐100: 100 = worst outcome) at 2‐5 years Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Mayo Elbow Performance Score (0‐100: 100 = best outcome) at 2‐5 years Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Any adverse event | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Superficial infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Range of elbow motion Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Flexion (°) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Extension (°) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Pronation (°) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Supination (°) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Participant dissatisfaction Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |

