Intervenciones quirúrgicas para el tratamiento de la fractura del olécranon en adultos
Resumen
Antecedentes
Las fracturas del olécranon (el extremo óseo del codo) representan aproximadamente un 1% de todas las fracturas de las extremidades superiores. A menudo se necesita intervención quirúrgica para restaurar la función del codo. Dos métodos clave de intervención quirúrgica son la fijación con bandas de tensión de alambre y la fijación con placas.
Objetivos
Evaluar los efectos (beneficiosos y perjudiciales) de diferentes intervenciones quirúrgicas para el tratamiento de las fracturas del olécranon en adultos.
Métodos de búsqueda
Se hicieron búsquedas en el registro especializado del Grupo Cochrane de Lesiones Óseas, Articulares y Musculares (Cochrane Bone, Joint and Muscle Trauma Group) (22 septiembre 2014), Registro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials) (CENTRAL, 2014, número 8), MEDLINE (1946 hasta septiembre, semana, 2, 2014), EMBASE (1980 hasta 19 septiembre 2014), registros de ensayos, actas de congresos y listas de referencias de artículos.
Criterios de selección
Ensayos controlados aleatorios (ECA) y ensayos controlados cuasialeatorios que compararan diferentes intervenciones quirúrgicas para el tratamiento de las fracturas del olécranon en adultos.
Obtención y análisis de los datos
Dos autores de la revisión, de forma independiente, seleccionaron los estudios, evaluaron el riesgo de sesgo y extrajeron los datos. Los resultados primarios de esta revisión fueron la función, el dolor y los eventos adversos.
Resultados principales
Se incluyeron seis ensayos pequeños con 244 adultos que presentaban fracturas del olécranon. De los mismos, cuatro eran ECA y dos eran ensayos controlados cuasialeatorios; ambos estuvieron en riesgo alto de sesgo de selección. Los seis ensayos estuvieron en riesgo alto de sesgo de realización, lo cual refleja la falta de cegamiento, y cuatro ensayos estuvieron en riesgo alto de sesgo de detección. La calidad de las pruebas para la mayoría de los resultados en general fue muy baja debido a las limitaciones en el diseño y la ejecución del estudio, y a la imprecisión de los resultados o a las medidas de resultado inadecuadas. Por lo tanto, existen muchas dudas acerca de las estimaciones del efecto.
Un ensayo (41 participantes) que comparó la fijación con placas con la colocación de bandas de tensión de alambre estándar proporcionó pruebas de calidad muy baja entre las 16 a 86 semanas de seguimiento de un mejor resultado clínico después de la fijación con placas (buen resultado [poco dolor o pérdida del movimiento del codo]: 19/22 versus 9/19, cociente de riesgos [CR] 1,82 a favor de la fijación con placas, intervalo de confianza [IC] del 95%: 1,10 a 3,01). Hubo pruebas de muy baja calidad de menos prominencia sintomática de las piezas de metal después de la fijación con placas (1/22 versus 8/19; CR 0,11; IC del 95%: 0,01 a 0,79). Los resultados para otros efectos adversos (infección y consolidación retardada o viciosa) fueron no concluyentes. Hay pruebas pendientes de un ensayo recientemente completado (setiembre de 2014) (67 participantes) que realiza la misma comparación.
Cuatro ensayos compararon cuatro técnicas modificadas diferentes de colocación de bandas de tensión de alambre (es decir fijación adicional con tornillos intramedulares, clavos biodegradables, clavos Netz y sistema de clavos con cables) versus colocación de bandas de tensión de alambre estándar. Hubo pruebas de calidad muy baja de poca diferencia entre los seis a 14 meses en la función evaluada con una herramienta de calificación no validada a partir del agregado de un tornillo intramedular. Sin embargo, hubo menos casos de prominencia de la pieza de metal en el grupo de tornillo intramedular (1/15 versus 8/15; CR 2,00; IC del 95%: 1,15 a 3,49; un ensayo; 30 participantes). Hubo pruebas de muy baja calidad de un ensayo (25 participantes) de poca diferencia en el buen resultado evaluado subjetivamente u objetivamente a una media de 20 meses entre la colocación de bandas de tensión de alambre con implantes biodegradables versus implantes de metal. No hubo ningún evento adverso, ni se informaron casos de consolidación viciosa o de acumulación de líquido o en el seno. Los diez participantes del grupo de piezas de metal fueron sometidos a una cirugía adicional para retirar la pieza de metal un año más tarde. Un ensayo, que no informó la función ni el dolor, proporcionó pruebas de calidad muy baja de tasas inferiores de extracción de piezas de metal por cualquier motivo o por síntomas tras la colocación de bandas de tensión de alambre con clavos Netz en comparación con colocación de bandas de tensión de alambre estándar (11/21 con clavos Netz versus 17/25 con colocación de bandas de tensión de alambre estándar; CR 0,77; IC del 95%: 0,47 a 1,26; 46 participantes); estas pruebas también apoyan la posibilidad de tasas mayores de extracción de la pieza de metal para los clavos Netz. Se observaron dos complicaciones intraoperatorias en el grupo de clavos Netz. El cuarto ensayo, que comparó el sistema de clavos con cables con el procedimiento estándar, halló pruebas de muy baja calidad de que los clavos con cables mejoraron el resultado funcional a una media de 21 meses (Mayo Elbow Performance Score [MEPS], rango 0 a 100: mejor resultado: diferencia de medias [DM] 7,89 a favor de los clavos con cables, IC del 95%: 3,14 a 12,64; un ensayo; 62 participantes). También se encontraron pruebas de baja calidad de menos complicaciones posoperatorias en el grupo de clavos con cables (1/30 con el sistema de clavos con cables versus 7/32 colocación de bandas de tensión de alambre estándar; CR 0,15; IC del 95%: 0,02 a 1,17), aunque las pruebas no descartaron lo contrario.
Un ensayo aportó pruebas de muy baja calidad de una función similar informada por el paciente mediante el cuestionario Disabilities of the Arm, Shoulder and Hand (0 a 100: peor función) a los dos años o más tras la fijación con un conector con memoria del olécranon (OMC, por sus siglas en inglés) nuevo en comparación con la fijación con placas de inmovilización (DM ‐0,70 a favor del OMC, IC del 95%: ‐4,20 a 2,80; 40 participantes). El único evento adverso fue una infección superficial en el grupo de placas de inmovilización.
Conclusiones de los autores
Hay pruebas insuficientes para establecer conclusiones consistentes sobre los efectos relativos de las intervenciones quirúrgicas evaluadas por los ensayos incluidos. Ya existen pruebas pendientes de un ECA completado recientemente sobre los efectos relativos de la colocación de placas versus de bandas de tensión de alambre que incluyen datos informados por los pacientes. Se necesitan ECA adicionales, que utilicen métodos de buena calidad e informen medidas validadas informadas por los pacientes sobre la función, el dolor y las actividades cotidianas en seguimientos establecidos, e incluyan la evaluación de los resultados positivos como los relacionados con el uso de un tornillo intramedular y el sistema de clavos con cables. Dichos ensayos también deben incluir la evaluación sistemática de las complicaciones, el tratamiento adicional incluida la extracción habitual de la pieza de metal y el uso de los recursos.
PICOs
Resumen en términos sencillos
Intervenciones quirúrgicas para el tratamiento de las fracturas del olécranon (un hueso del codo) en adultos
Tratamiento quirúrgico de la fractura del olécranon
El extremo óseo del codo se llama olécranon. Su forma permite que el brazo se doble y se enderece a la altura del codo. El olécranon se sitúa directamente bajo la piel del codo, lo cual lo hace vulnerable a lesiones y fracturas después de una caída. Cuando esto sucede, los pacientes a veces son incapaces de enderezar el brazo. El tratamiento de esta fractura generalmente incluye una cirugía para colocar nuevamente en su posición las partes fracturadas del hueso y luego fijarlas en su lugar con alambres, clavos, placas, tornillos y otros dispositivos.
Descripción de los estudios incluidos en la revisión
Se realizaron búsquedas en la literatura médica hasta septiembre de 2014 y se encontraron seis ensayos, con 244 adultos con fracturas de olécranon. Cada ensayo tuvo una comparación diferente. La colocación de bandas de tensión de alambre, que es una técnica usada comúnmente para la fijación de estas fracturas, fue la intervención de “control” en cinco ensayos.
Calidad de la evidencia
Los seis ensayos eran pequeños y tenían debilidades que podían afectar a la fiabilidad de sus resultados. Se consideró la calidad general de las pruebas disponibles para cada comparación baja o muy baja.
Resumen de las pruebas
Un ensayo comparó el uso de fijación con placas con la colocación de bandas de tensión de alambre. Halló que más pacientes podían mover el codo sin dolor después de la fijación con placas y menos pacientes presentaban malestar causado por la prominencia de la pieza de metal (es un problema conocido de la fijación con alambres en que los alambres metálicos de la superficie del hueso justo debajo la piel causan dolor, malestar y otros problemas).
Cuatro ensayos compararon diferentes formas de colocar alambres en la fractura. Dos ensayos encontraron muy pocas pruebas claras de diferencias entre las mismas. Un ensayo halló que agregar un tornillo intramedular (es decir un tornillo que se inserta a través del hueso y a lo largo del canal óseo central) a la colocación de bandas de tensión de alambre estándar redujo el riesgo de prominencia de la pieza de metal bajo la piel. Otro ensayo halló que el sistema de clavos con cables mejoró la función y dio lugar a menos complicaciones en comparación con la colocación de bandas de tensión de alambre estándar.
Finalmente, un ensayo comparó un método nuevo de fijación mediante un dispositivo de titanio y níquel que una vez implantado adopta la forma del olécranon versus la fijación con placas de inmovilización. No encontró pruebas claras de diferencias entre las técnicas en la función y las complicaciones informadas por los pacientes (la única complicación fue una infección superficial).
Conclusiones
Actualmente, no hay pruebas suficientes para determinar de manera fiable el mejor tratamiento para estas fracturas. Se necesita investigación adicional de alta calidad, la cual probablemente tenga un impacto importante sobre la confianza en los cálculos de los efectos y posiblemente cambie los cálculos.
Authors' conclusions
Summary of findings
| Plate fixation compared with tension band wiring for treating olecranon fractures in adults | ||||||
| Patient or population: adults with olecranon fractures Settings: hospital Intervention: plate fixation (using 1/3 tubular plates) Comparison: tension band wiring fixation | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk1 | Corresponding risk | |||||
| Tension band wiring | Plate fixation | |||||
| Functional assessment (e.g. via patient‐reported outcome measures of elbow function) | see Comments | see Comments | ‐ | ‐ | ‐ | Not reported. 1 ongoing trial (67 participants) testing this comparison will be reporting DASH (Disabilities of the Arm, Shoulder and Hand) scores at 1 year (NCT01391936) |
| Good clinical outcome (little pain or loss of elbow motion: Helm criteria) Follow‐up: mean 28.5 weeks, range 16‐86 weeks | Study population | RR 1.82 (1.10 to 3.01) | 41 participants | ⊕⊝⊝⊝ | Results were rated 'good' if there was no more than slight or occasional pain, loss of movement was less than 15° at the elbow and no revision surgery for operative failure | |
| 474 per 1000 | 863 per 1000 | |||||
| Pain | see Comments | see Comments | ‐ | 41 participants | ‐ | Separate pain data were not available; these should be in the 1 ongoing trial (67 participants) testing this comparison (NCT01391936) |
| Adverse events ‐ overall | see Comments | see Comments | ‐ | 41 participants | ‐ | Incomplete reporting and discrepancies in the reporting of infection meant that numbers of participants with ≥ 1 adverse events data could not be reported here |
| Adverse events ‐ symptomatic metal prominence Follow‐up: mean 28.5 weeks, range 16‐86 weeks | Study population | RR 0.11 (0.01 to 0.79) | 41 participants | ⊕⊝⊝⊝ | Metalwork prominence is a well‐known problem of tension band wiring. Symptoms were local discomfort or pain over the implant. There was no record of implant removal surgery in either group | |
| 421 per 1000 | 46 per 1000 | |||||
| Adverse events ‐ delayed or non‐union Follow‐up: 6 months | Study population | RR 0.17 [0.01 to 3.41] | 41 participants | ⊕⊝⊝⊝ | Surgical treated (debridement) infection preceded both cases in the tension band wiring group | |
| 106 per 1000 | 18 per 1000 | |||||
| Adverse events ‐ heterotopic ossification (bone formation) Follow‐up: mean 28.5 weeks, range 16‐86 weeks | Study population | RR 0.29 [0.01 to 6.72] | 41 participants | ⊕⊝⊝⊝ | The single participant with heterotopic ossification in the tension band wiring group developed ulnar neuropathy | |
| 53 per 1000 | 16 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1. The basis of the assumed risk is that for control group (tension band wiring) in the study population. 2. The evidence was downgraded 2 levels for limitations in design and implementation (including lack of blinding and spread of timing of outcome measurement) and 1 level for indirectness (the Herm criteria were not validated and could be considered surrogate to functional outcome). 3. The evidence was downgraded 2 levels for limitations in design and implementation (including lack of blinding and spread of timing of outcome measurement) and 1 level for imprecision. | ||||||
Background
Description of the condition
At the elbow, the proximal (or upper) ends of the two forearm bones (the radius and ulna) and the distal (lower) end of the humerus (the upper arm bone) come together. The olecranon, which is the name for the proximal part of the ulna, forms the bony point or 'tip' of the elbow when the elbow is bent. The top side of the olecranon and the lower end of the humerus are shaped such that they act as a hinge joint, which allows bending (flexion) and straightening out (extension) of the arm at the elbow. The upper and posterior surface of the olecranon forms the insertion site for the triceps muscle, which is the main muscle used for straightening the arm. The olecranon is situated directly under the skin of the elbow, which makes it vulnerable to injury.
Olecranon fractures account for approximately 1% of all upper extremity fractures (Duckworth 2012), with an annual incidence of 11.5 to 12 per 100,000 population (Duckworth 2012; Karlsson 2002). These fractures are caused by either direct or indirect trauma (Bailey 2001; MacDermid 2001; Newman 2009; Veillette 2008). With direct trauma, people commonly present following a direct fall onto the elbow. A direct blow to the olecranon will force it into the distal end of the humerus, causing comminuted fractures (where the bone is broken into more than two fragments) (Hotchkiss 1996). In indirect trauma, which is more common in older people, people present following a fall onto an outstretched arm. This causes fractures of the olecranon as a result of forceful contraction or sudden pull of the powerful triceps muscle through its insertion point onto the olecranon. This often produces transverse (crosswise) or short oblique (slanting) fractures (Newman 2009).
Many classification systems describe olecranon fractures, most notably the AO classification system (Muller 1991), the Mayo Classification System (Morrey 1995), and the Schatzker‐Schmeling Classification System (Schatzker 1987). All are descriptive and classify fractures based on pattern and morphological appearance of fractures. Currently, there is no consensus in favour of any one system.
The aim of fracture treatment is to achieve anatomical reduction of the fracture and provide stable fixation that allows early mobilisation and restores function (Veillette 2008). Non‐surgical or conservative treatment of olecranon fractures usually involves plaster immobilisation. It is generally considered for non‐displaced or minimally displaced fractures, where the gap or step‐off between fracture fragments is less than two millimetres, the extensor mechanism is intact and there is no displacement with elbow flexion (Newman 2009; Schatzker 1987). Fractures meeting all these criteria can be successfully treated without surgery (Hak 2000).
Description of the intervention
Conventional indications for surgical treatment include open fractures, displaced fractures and fractures causing disruption to the extensor mechanism affecting the insertion of triceps muscle into the olecranon. There are four common methods in the surgical management of olecranon fractures: tension band wiring, plate fixation, intramedullary fixation and excision of the proximal fractured fragment with re‐attachment of triceps tendon.
Tension band wiring
The principle of tension band wiring, which was first described in 1883 (Lister 1883), utilises a 'figure of 8' loop and two parallel pins. The aim of this method is to convert the extensor forces of the triceps muscle into compressive forces along the articular surface to cause compression of the fracture. Tension band wiring with Kirschner wires (K wires) has become a well‐considered standard, especially in non‐comminuted transverse fractures (Newman 2009; Wolfgang 1987).
Plate fixation
Plate fixation uses a metallic plate attached to the fracture fragments with screws to bridge the fracture gap and facilitate fracture healing. It can be used for any type of olecranon fracture but is particularly recommended for the following indications: comminuted fractures, Monteggia fracture dislocations, oblique fractures (particularly those distal to midpoint of the trochlear notch) and fractures that involve the coronoid process (Hak 2000). One‐third tubular, 3.5‐mm contoured limited contact dynamic compression, 3.5‐mm reconstruction, hook plates and pre‐contoured locking plates are frequently used (Lavigne 2004).
Intramedullary fixation
Nailing systems and intramedullary screws are used to align and stabilise fractures, including olecranon fractures. The screws and nails are usually inserted into the bone marrow canal of long bones. In oblique or simple transverse olecranon fractures, a single intramedullary cancellous screw can be used with or without tension band wiring. More complex forms of intramedullary fixation with interlocking intramedullary nailing devices have been used for more complex injuries.
Olecranon excision and triceps advancement
Olecranon excision and triceps advancement has been adopted by many clinicians, particularly in older people with osteoporotic bone, extensive comminution or a fragment too small for internal fixation. This technique involves excision of fracture fragments with triceps tendon advancement or re‐attachment to restore the extensor mechanism.
Less commonly used surgical options include closed reduction and external fixation, and 'total elbow replacement' for complex elbow fractures including the olecranon.
How the intervention might work
Fractures of the olecranon represent a wide spectrum of injuries with multiple management options available. Anatomic reduction through surgical fixation ensures fracture stability and reconstruction of the articular surface to speed recovery. This also allows return to previous activities. This aim has been achieved with plate fixation and tension band wiring (Bailey 2001; Holdsworth 1984; Romero 2000; Veillette 2008), and to a lesser extent with olecranon excision and triceps advancement (Hak 2000; Hotchkiss 1996; Lavigne 2004; Newman 2009).
However, the subcutaneous location of the olecranon makes it prone to complications from metal implants used in surgical interventions, which can lead to pain and skin breakdown. Metalwork prominence is the most common complication of tension band wiring (Romero 2000) and plate fixation (Bailey 2001), often requiring removal of metal implants through a second operation (Rommens 2004).
Why it is important to do this review
Olecranon fractures vary in their severity and can have poor outcomes. There are several different surgical interventions available and in current use. Thus, there is a need to inform practice by systematically reviewing the evidence for the use of these different surgical interventions. To our knowledge, there is no recent systematic review that focuses on the surgical treatment of olecranon fractures in adults.
Objectives
To assess the effects (benefits and harms) of different surgical interventions in the treatment of olecranon fractures in adults.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) and quasi‐RCTs (where the method of allocating participants to a treatment was not strictly random and where allocation could be predicted, e.g. by date of birth, hospital record number, alternation) controlled trials that compared different surgical interventions for the treatment of olecranon fractures in adults.
Types of participants
We included adults with unilateral or bilateral olecranon fracture. We included all severities of fracture, both open and closed. We included trials containing participants with other elbow injuries provided the primary focus was on the treatment of the olecranon fracture.
We excluded trials that specifically focused on treating people with a primary bone disease (e.g. fibrous dysplasia), pathological fractures (from metastatic cancer) or periprosthetic fractures. We also excluded trials including children or people with primary bone diseases or pathological fractures unless separate data could be provided for adults with non‐pathological fractures or the proportion of children or adults with primary bone diseases or pathological fractures was small (less than 5%).
Types of interventions
We included trials comparing different surgical interventions for the treatment of olecranon fractures. As described in the Description of the intervention, the main interventions under consideration were tension band wiring, plate fixation, intramedullary fixation and olecranon excision with triceps advancement. The tension band wiring technique is considered the standard intervention and, hence, we considered this the control group against which the other interventions were compared. The selection of the experimental and control groups in trials evaluating other comparisons was based on an assessment of the relative novelty of the interventions being compared. We also included trials making other comparisons, including of different surgical techniques for the same intervention. We excluded trials comparing surgical with non‐surgical interventions.
Types of outcome measures
Primary outcomes
-
Functional assessment, including generic and upper‐limb‐specific validated clinical scores (e.g. Mayo Elbow Performance Score (MEPS; Morrey 1993), Broberg and Morrey rating system (Broberg 1987), and patient‐reported outcomes measures (e.g. participant‐rated elbow evaluation score (MacDermid 2001)).
-
Adverse events (e.g. surgical complications, non‐union, malunion, painful stiff elbow, persistent instability of the elbow, post‐traumatic arthritis, heterotopic ossification and problematic prominent hardware), generally requiring secondary procedures (e.g. further surgery).
-
Long‐term or persistent pain (assessed using self reported scales, e.g. visual analogue scale).
Secondary outcomes
-
Reduced range of elbow movements.
-
Patient‐reported health‐related quality of life measures (e.g. 36‐item Short Form (SF‐36)).
-
Return to work and former activities, such as sport.
-
Participant satisfaction, including the cosmetic result.
-
Operation time, blood loss.
-
Resource use and other costs (e.g. hospital stay, number of outpatient attendances, physiotherapy and other costs).
-
Others (as detailed in each individual study).
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group's Specialised Register (22 September 2014), the Cochrane Central Register of Controlled Trials (CENTRAL, 2014, Issue 8), MEDLINE (1946 to September week 2 2014), MEDLINE In‐Process & Other Non‐Indexed Citations (19 September 2014) and EMBASE (1980 to 19 September 2014). We also searched Current Controlled Trials, ClinicalTrials.gov, and the World Health Organization (WHO) International Clinical Trials Registry platform for ongoing and recently completed trials (22 September 2014). We did not restrict the inclusion of reports based on publication language.
In MEDLINE, we combined the subject‐specific search strategy with the sensitivity‐maximising version of the Cochrane Highly Sensitive Search Strategy for identifying randomised trials (Lefebvre 2011). Appendix 1 shows the search strategies for CENTRAL, MEDLINE and EMBASE.
Searching other resources
We checked reference lists of articles. We also attempted to contact researchers in the field for information on existing or ongoing trials. We searched the specific proceedings of shoulder and elbow surgery meetings and conferences from the following organisations: British Elbow & Shoulder Society (BESS) (2008 to 2013), American Orthopedic Trauma Association annual meetings (1996 to 2013) and American Academy of Orthopedic Surgeons annual meetings (2010 to 2013).
Data collection and analysis
Selection of studies
Two review authors (HM and HA) independently examined the titles and abstracts of articles identified in the search as potentially relevant trials. We obtained the full texts of trials that fulfilled our inclusion criteria and those that were unclear from perusal of the abstracts. We resolved any disagreements by discussion and, if necessary, arbitration by a third review author (NG). The review authors were not blinded to the journal or study authors.
Data extraction and management
For each included trial, two review authors (HM and HA) independently extracted data using a pre‐piloted form. We resolved any differences in data extraction by consensus, and by referring back to the original article. We resolved any disagreements by discussion and, where necessary, by consultation with a third review author (NG, AA).
Assessment of risk of bias in included studies
Two review authors (HM and HA) independently assessed risk of bias of the included studies using The Cochrane Collaboration's 'Risk of bias' tool (Higgins 2011). We assessed the following domains:
-
random sequence generation;
-
allocation concealment;
-
blinding of participants and personnel;
-
blinding of outcome assessment;
-
completeness of outcome data;
-
selective reporting;
-
other bias (e.g. major baseline imbalance; and risk of bias associated with inexperience of surgeons and other care providers with the interventions, and differences in rehabilitation).
We judged each of these domains as being at low risk of bias, high risk of bias or unclear risk of bias (either lack of information or uncertainty over the potential for bias). We resolved disagreements between authors regarding the risk of bias for domains by consensus.
Measures of treatment effect
For dichotomous outcomes, we expressed the treatment effects as risk ratios (RR) with 95% confidence intervals (CI). For continuous outcomes, we expressed treatment effects as mean differences (MD) and 95% CI. Had there been sufficient data to pool data from different outcome measures, we would have used standardised mean differences (SMD) and 95% CI.
Unit of analysis issues
All included trials were parallel‐group trials; there were no cross‐over trials. The units of randomisation and analysis were clearly individual participants in five of the included trials; however, there was a lack of information on one participant with bilateral fractures in one trial (Hume 1992). It was unclear how the study authors dealt with the issues around this participant but it is clear that the disparity between the units of analysis and randomisation would have been small (Hume 1992).
Dealing with missing data
Participants of all included trials completed the follow‐up and there were no missing data. If there had been missing data, we would have tried to contact the authors of primary studies to request missing data, such as number of participants, details of drop‐outs, means, measures of uncertainty (standard deviation or error) or number of events. In the event, the available data allowed an intention‐to‐treat analysis in which all randomised participants were analysed in the groups to which they had been originally assigned. For continuous outcomes with no standard deviations reported, we calculated standard deviations if possible from standard errors, P values or CIs using the methods outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We did not impute data.
Assessment of heterogeneity
We planned to judge clinical heterogeneity within all comparisons between included trials, and visually inspect forest plots in order to investigate the possibility of statistical heterogeneity. This was to have been supplemented using the I² statistic, which provides an estimate of the percentage of variability due to heterogeneity rather than to chance alone. An I² estimate of 75% or greater indicates the presence of high levels of heterogeneity (Higgins 2003).
Assessment of reporting biases
For future updates of the review, we will explore the possibility of publication bias using a funnel plot if we find data from over 10 trials for pooling.
Data synthesis
For each comparison, we calculated a summary estimate of treatment effect together with 95% CIs for individual outcomes. We had planned to use the fixed‐effect model and to consider using the random‐effects model, especially where there was unexplained and substantial heterogeneity. However, we were unable to perform meta‐analyses giving the included trials tested different comparisons. Instead, we presented results using a narrative approach and in table format.
Subgroup analysis and investigation of heterogeneity
We performed no meta‐analyses because of the heterogeneity of the included trials. We had planned, where relevant, to perform the following subgroup analyses:
-
polytrauma versus isolated injuries;
-
open versus closed injuries;
-
fracture pattern: comminuted versus non‐comminuted;
-
young adults versus older adults (generally over 65 years of age).
Should subgroup analyses be possible in future, we will investigate whether the results of subgroups are significantly different by inspecting the overlap of CIs and performing the test for subgroup differences available in Review Manager 5 (RevMan 2012).
We had also planned, for multiple trial comparisons with substantial heterogeneity, to perform sensitivity analyses to explore the effects on heterogeneity and outcome of the removal of outliers.
Sensitivity analysis
We performed no sensitivity analyses. We had planned sensitivity analyses to examine the effect of missing data, of excluding trials at high or unclear risk of bias (such as selection bias arising from the lack of allocation concealment) and of excluding trials only reported in conference abstracts.
Quality of the evidence and 'Summary of findings' tables
We used the GRADE approach to assess the quality of evidence related to each of the primary outcomes listed in Types of outcome measures (Higgins 2011; see Chapter 12.2). We prepared a 'Summary of findings' table for the key comparison of plate versus tension band wiring.
Results
Description of studies
SeeCharacteristics of included studies; Characteristics of excluded studies; Characteristics of studies awaiting classification; Characteristics of ongoing studies.
Results of the search
The search was completed in October 2013. We screened 203 records from the following databases: Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (seven records); CENTRAL (14 records), MEDLINE (62 records), EMBASE (94 records), Current Controlled Trials (nine records), ClinicalTrials.gov (nine records) and the WHO International Clinical Trials Registry platform (eight trials). We also identified one potentially eligible study from reference lists of included studies and 11 abstracts from meetings and conferences.
The search resulted in the identification of 23 potentially eligible studies (seeFigure 1). Upon study selection, we included six studies (Ahmed 2008; Chen 2013; Hume 1992; Juutilainen 1995; Larsen 1987; Liu 2012), excluded 15 studies (Frankle 1996; Gartsman 1981; Hamid 2010; Hope 1991; Jaskulka 1991; Karlsson 2002; Lan 2013; Ma 2012; Miyagi 1985; Mullett 2000a; Mullett 2000b; Murphy 1987; Partio 1992; Schliemann 2014; Teasdall 1993), and listed one study as awaiting classification (Sui 2008). We also identified one ongoing study (NCT01391936).

Flow diagram of search results.
We attempted to contact the corresponding author of one trial for further information and clarification about study design, but unfortunately, these attempts were unsuccessful (Sui 2008).
Included studies
The six included trials involved 244 participants (Ahmed 2008; Chen 2013; Hume 1992; Juutilainen 1995; Larsen 1987; Liu 2012). Full details of these trials are in the Characteristics of included studies.
Design
Four included trials were RCTs (Hume 1992; Chen 2013; Juutilainen 1995; Liu 2012), and two were quasi‐RCTs (Ahmed 2008; Larsen 1987).
Sample sizes
The populations of included trials were all small: 30 participants (Ahmed 2008), 40 participants (Chen 2013), 41 participants (Hume 1992), 25 participants (Juutilainen 1995), 46 participants (Larsen 1987), and 62 participants (Liu 2012).
Settings
All trials were hospital based. One trial was conducted in two hospitals in China (Liu 2012). The remaining five trials were single centre and were carried out in Egypt (Ahmed 2008), China (Chen 2013), the USA (Hume 1992), Sweden (Juutilainen 1995), and Denmark (Larsen 1987).
Participants
In total, there were 244 participants, comprising 125 men and 119 women: Ahmed 2008 (21 men, nine women), Chen 2013 (22 men, 18 women), Hume 1992 (30 men, 11 women), Juutilainen 1995 (eight men, 17 women), Larsen 1987 (14 men, 32 women) and Liu 2012 (30 men, 32 women). Participants' ages ranged from 16 to 87 years; mean ages were 33.4 years (Ahmed 2008), 48.4 years (Chen 2013), 30.9 years (Hume 1992), 49.8 years (Juutilainen 1995), and 47.1 years (Liu 2012); the median ages of the two groups in Larsen 1987 were 60 and 67 years. Most participants had displaced transverse or oblique olecranon fractures requiring surgical fixation. Three trials excluded comminuted fractures (Ahmed 2008; Juutilainen 1995; Liu 2012). The percentage of comminuted fractures in the other three trials were: 32.5% (Chen 2013), 29.3% (Hume 1992), and 32.6% (Larsen 1987). Three trials explicitly excluded participants with open fractures (Chen 2013; Juutilainen 1995; Liu 2012). One trial included four participants with open fractures (two in each group) (Hume 1992), of which one participant had bilateral fractures but it was not clear to what group this participant belonged.
Interventions
Each trial made a different comparison.
In five trials, the standard tension band wiring fixation technique was the control group (Ahmed 2008; Hume 1992; Juutilainen 1995; Larsen 1987; Liu 2012). One trial compared plate fixation with tension band wiring (Hume 1992). The other four trials evaluated the use of modified techniques or additional interventions. Ahmed 2008 compared intramedullary screw plus tension band wiring versus tension band wiring. Juutilainen 1995 compared biodegradable pins and screw versus metal wires for tension band wiring. Larsen 1987 compared the use of Netz pins versus standard K‐wires. Liu 2012 compared the cable pin system (see Appendix 2) versus standard tension band wiring. The sixth trial compared a novel olecranon memory connector (OMC) fixation technique versus locking plate fixation (Chen 2013).
Outcomes
Duration of follow‐up ranged from an endpoint of fracture healing (Larsen 1987) to 36 months (Liu 2012). We summarised only the primary outcomes below.
Only Chen 2013 reported a patient‐reported outcome measure; this was the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire (Appendix 3). Both Chen 2013 and Liu 2012 used the MEPS (Morrey 1993; Appendix 4), which includes assessment of pain, movement, stability and activities of daily living. Ahmed 2008 used the Modified Murphy Scoring System (Appendix 5), which is a composite score based on pain, function, range of movement and radiologically assessed joint space. Hume 1992 used the Helm criteria (Helm 1987; Appendix 6), based on assessment of pain, range of movement and revision surgery for operative failure. Juutilainen 1995 used a non‐validated outcome measure of clinical improvement. Larsen 1987 did not report on function.
All trials reported on adverse events or complications, which always included metalwork prominence. Larsen 1987 reported in full on reasons for metalwork removal, which included routine removal as well as removal because of symptoms.
No trial reported separately on pain.
Excluded studies
We excluded 15 studies: 12 clinical or comparative studies and three RCTs (Frankle 1996; Hamid 2010; Hope 1991). Of these, no isolated olecranon fractures were included in Frankle 1996, which compared total elbow replacements with open reduction and internal fixation for the treatment of complex elbow fractures in older women; there was no comparison of surgical interventions in Hamid 2010, which evaluated single‐fraction radiotherapy for prevention of heterotopic ossification in elbow fractures including the olecranon; and Hope 1991 included only children, which examined biodegradable pins fixation in children with elbow fractures (see the Characteristics of excluded studies).
Studies awaiting classification
There is one study awaiting classification (Sui 2008). This article, reported in Chinese, is of a comparative study of plate fixation versus tension band wiring in 63 participants with olecranon fractures. The English abstract contains numeral inconsistencies and did not describe the study design, including whether there was randomisation (see the Characteristics of studies awaiting classification).
Ongoing studies
We identified one ongoing trial (NCT01391936). This is an RCT involving 67 participants who were allocated either plate fixation or tension band wiring for olecranon fractures in older people. The one year follow‐up is now complete (September 2014) and the trial analysis and report underway. This study is likely to be included in future updates of this review and data pooled, where possible, with Hume 1992. See further details in the Characteristics of ongoing studies.
Risk of bias in included studies
Figure 2 and Figure 3 and the 'Risk of bias' tables in the Characteristics of included studies summarise the risk of bias judgements on all six trials.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
We assessed both quasi‐RCTs at high risk of bias for selection bias, reflecting non‐random sequence generation and lack of allocation concealment (Ahmed 2008; Larsen 1987). Three trials provided no details of their methods of sequence generation or allocation concealment and we judged them to be at unclear risk of selection bias (Chen 2013; Hume 1992; Juutilainen 1995). We attempted to contact the trial authors for further details but were unsuccessful. We judged one trial at low risk for random sequence generation (an adaptive biased coin design was used for sequence generation to protect against prognostic imbalance between the groups) and allocation concealment (sealed envelopes were opened after the consent form was signed) (Liu 2012).
Blinding
We judged all six trials at high risk of performance bias, reflecting the inevitable lack of blinding of surgeons and the lack of mention of blinding of trial participants. Two trials blinded outcome assessors of clinical outcomes and we judged them at low risk of detection bias (Chen 2013; Liu 2012). We judged the other four trials at high risk of detection bias, as they appeared not to have taken measures to blind outcome assessment.
Incomplete outcome data
There was no loss to follow‐up in any of the included trials. However, while we judged three trials at low risk of attrition bias, we judged Chen 2013 and Larsen 1987 at unclear risk and Hume 1992 at high risk. The judgements reflected some small discrepancies between text and tables in Chen 2013, the variation in length of follow‐up and lack of clarity on the criteria used to determine the time of follow‐up in Larsen 1987, and because follow‐up spanned several years and no information was given on one participant with bilateral fractures in Hume 1992.
Selective reporting
We did not have access to any of the included trial protocols; hence, we judged the risk of reporting bias as unclear.
Other potential sources of bias
We considered two trials at low risk of other bias reflecting lack of major differences in baseline characteristics and similar care programmes (Hume 1992; Liu 2012). We judged the risk of other bias as unclear in the other four trials; this reflected uncertainty in terms of potential confounding from between‐group differences in baseline characteristics in Ahmed 2008, and lack of information on baseline characteristics in Juutilainen 1995 and Larsen 1987. We judged one trial at unclear risk of other bias because the novel device being tested was designed by the trial authors (Chen 2013). Although no trial mentioned surgeon experience with the devices under test, we felt this would not be an important source of bias for any of the comparisons.
Effects of interventions
Each of the six included trials made a difference comparison.
Plate fixation versus tension band wiring
Hume 1992 compared one‐third tubular plate fixation with tension band wiring for displaced olecranon fractures in 41 adults who were followed up for a mean of 28.5 weeks (range 16 to 86 weeks).
Primary outcomes
Hume 1992, which did not report on function or provide separate data on pain, rated clinical results as good, fair or poor using the Helm criteria (Helm 1987; Appendix 6), which are based on pain, loss of movement and operative failure requiring revision surgery. Results were rated 'good' if there was no more than slight or occasional pain, loss of movement was less than 15° at the elbow and no revision surgery. There were twice as many participants with a 'good' outcome after plate fixation than tension band wiring (19/22 with plate fixation versus 9/19 with tension band wiring, RR 1.82 favouring plate fixation, 95% CI 1.10 to 3.01; P value = 0.02; Analysis 1.1).
There was incomplete information on the number of participants incurring an adverse event and contradictory statements in the trial report in terms of the number of participants developing an infection. One participant in the plate fixation group compared with eight participants in the tension band group developed symptomatic metalwork prominence (1/22 with plate fixation versus 8/19 with tension band wiring; RR 0.11 favouring plate fixation, 95% CI 0.01 to 0.79; P value = 0.03; Analysis 1.2). Two participants in the tension band group with non‐union at six months had had surgically treated infections. Another participant in the tension band group developed heterotopic ossification and subsequently ulnar neuropathy (seeAnalysis 1.2).
Secondary outcomes
Hume 1992 reported an absence of a statistically significant difference in elbow range of motion between the two groups at final follow‐up. The mean loss in elbow extension was 7° in the plate group and 10° in the tension band wiring group. The mean operation time was 120 minutes (range 85 to 120 minutes) in the plate fixation group and 94.5 minutes (range 75 to 120 minutes) in the tension band wiring group.
Intramedullary screw plus tension band wiring versus tension band wiring
Ahmed 2008 compared intramedullary screw plus tension band wiring fixation with standard tension band wiring for displaced olecranon fractures in 30 adults, who were followed up for a mean of 8.2 months (range six to 14 months).
Primary outcomes
Using the Modified Murphy Scoring System (Murphy 1987; Appendix 5), a composite score rating pain, activity restriction, loss of range of motion and joint space (0 to 19, where 19 = best outcome), Ahmed 2008 found little difference between the two groups at final follow‐up (mean score: 18 with screw plus tension band wiring versus 17.07 with tension band wiring; MD 0.93, 95% CI ‐1.30 to 3.16; P value = 0.41; Analysis 2.1). All 15 participants in the screw plus tension band wiring group had an excellent or good result based on scores of 17 or over; this applied to 11 of the 15 participants in the tension band group (RR 1.35, 95% CI 0.98 to 1.85; P value = 0.07; Analysis 2.2).
Hardware prominence was reported in one of the 15 participants in the screw plus tension band wiring group and eight of the 15 participants in the tension band wiring group (RR 0.13, 95% CI 0.02 to 0.88; P value = 0.04; Analysis 2.3). Hardware removal in the eight of the 15 participants in the tension band group was after fracture union; prior to metalwork removal, one participant had plaster cast immobilisation for two months. There was one infection in the tension band wiring group that resolved only upon metalwork removal.
Secondary outcomes
None of the trial participants had loss of forearm rotation. Substantial loss of range of motion (flexion contracture or limitation) occurred in one participant of the screw plus tension band wiring group and five participants in the tension band wiring group (RR 0.20, 95% CI 0.03 to 1.51; Analysis 2.4).
Biodegradable wire plus screw versus metal wire and two K‐wire tension band wiring
Juutilainen 1995 compared biodegradable materials (wire and screw) versus metal wire for olecranon fractures in 25 adults, who were followed up for a mean of 19.7 months (range six to 24 months).
Primary outcomes
Functional assessment was carried out using a binary scale of 'good' or 'poor'. Subjective outcome was considered 'good' if the participants could move the fractured side without pain six months after operation and if the use of the injured elbow was similar to the use of their other elbow. A 'good' objective outcome was when participants had good functional movement and their elbow joint was stable. Good results, whether assessed using 'subjective' or 'objective' criteria, were reported in all 15 (100%) participants who had biodegradable fixation compared with eight of the 10 (80%) of participants in the metal wire fixation group (RR 1.25, 95% CI 0.90 to 1.75; P value = 0.18; Analysis 3.1). Fourteen of the 15 participants in the biodegradable fixation group and eight of the 10 participants in the metal wire fixation group had a painless elbow joint at final follow‐up (RR 1.17, 95% CI 0.83 to 1.64; P value = 0.37; Analysis 3.2). There were no cases of non‐union in either group and no sinus or fluid accumulation in participants treated with biodegradable implants. Notably all metal implants were routinely removed one year post fixation surgery.
Secondary outcomes
More participants of the biodegradable group had normal range of elbow movement at final follow‐up (12/15 with biodegradable fixation versus 5/10 with metal wire fixation; RR 1.60 favouring biodegradable fixation, 95% CI 0.82 to 3.13; P value = 0.17; Analysis 3.3).
Netz pins versus K‐wires tension band wiring
Larsen 1987 compared Netz pins versus K‐wires for tension band wiring for displaced olecranon fractures in 46 adults, who were followed up to fracture healing (median 13 weeks, range four to 54 weeks).
Primary outcomes
Larsen 1987 did not report on function or pain, other than stating that pain was a reason for implant removal.
Removal of metalwork for any reason ('routine', young age, symptoms) occurred less often in the Netz pins group (11/21 with Netz pins versus 17/25 with K‐wires tension band wiring; RR 0.77, 95% CI 0.47 to 1.26; P value = 0.30; Analysis 4.1). The removal of metalwork because of symptoms (pin affecting skin, cerclage affecting skin or pain) was also less common in the Netz pins group (6/21 with Netz pins versus 11/25 with K‐wires tension band wiring; RR 0.65, 95% CI 0.29 to 1.46; P value = 0.29; Analysis 4.1). There were no deep infections but one participant in each group had a superficial infection. Two of 21 participants in the Netz pins group incurred intraoperative complications: these were an intra‐articular fracture in one participant with a comminuted fracture and dropping of a Netz pin into the intramedullary canal during metalwork removal.
Secondary outcomes
The median time to fracture healing and attainment of final range of elbow motion was 13 weeks in both groups.
Cable pin system versus tension band wiring
Liu 2012 compared the cable pin system, a modified tension band wiring technique, with the standard tension band wiring in 62 adults with olecranon fractures, who were followed up on average 21 months (range 12 to 36 months).
Primary outcomes
The MEPS (range 0 to 100: 100 = best outcome; Appendix 4) results were higher in the cable pin system group (mean: 88.67 with cable pin versus 80.78 with tension band wiring; MD 6.90 favouring cable pin, 95% CI 7.89, 95% CI 3.14 to 12.64; P value = 0.001; Analysis 5.1). There was also a lower rate of postoperative complications in the cable pin system group (1/30 with cable pin versus 7/32 tension band wiring; RR 0.15, 95% CI 0.02 to 1.17; P value = 0.07; Analysis 5.2). The only complication in the cable pin group was skin irritation from raised metalwork, which did not require treatment or implant removal. Five of the seven complications (two implant loosening, four metalwork prominence and one pain due to fracture of the steel wire) in the tension band wiring group required removal of metalwork. All fractures united.
Secondary outcomes
There was little difference between the two groups in operation time (MD ‐0.73 minutes, 95% CI ‐2.84 to 1.38; Analysis 5.3) or intraoperative blood loss (MD ‐1.19 mL, 95% CI ‐6.23 to 3.85; Analysis 5.3).
Nickel‐titanium olecranon memory connector versus locking plate fixation
Chen 2013 compared a novel OMC versus locking plate fixation for displaced olecranon fracture in 40 adults, who were followed for a mean of 37 months (range 24 to 56 months). The OMC, which was designed by the trial authors, conformed to the anatomical structure of the olecranon and was manufactured from nickel‐titanium shape memory alloy plate.
Primary outcomes
There was no clinically important difference between the two groups in the DASH scores (range 0 to 100: 100 = worst outcome; Appendix 3) at two or more years' follow‐up (mean: 3.3 with PMC versus 4.0 with locking plate fixation; MD ‐0.70 favouring OMC, 95% CI ‐4.20 to 2.80; P value = 0.69; Analysis 6.1). The MEPS (range 0 to 100: 100 = best outcome; Appendix 4) results were higher in the OMC group (mean: 86.7 with PMC versus 79.8 with locking plate fixation; MD 6.90 favouring OMC, 95% CI ‐0.79 to 14.59; P value = 0.08; Analysis 6.2).
All fractures healed. The only recorded adverse event was a superficial infection, which occurred in one participant in the locking plate fixation group (Analysis 6.3).
Secondary outcomes
There were no clinically significant differences between the two groups in range of motion (Analysis 6.4).
Seventeen (85%) participants in each group stated that they were very satisfied with their outcome. The only person expressing dissatisfaction was the same person in the locking plate fixation group who had had a superficial infection after surgery and pain during rehabilitation (Analysis 6.5).
Discussion
Summary of main results
We included only four RCTs and two quasi‐RCTs involving 244 participants. Each trial tested a different comparison, although tension band wiring, which is a standard surgical treatment for olecranon fracture, acted as the control group in five of these trials. Of these five trials, one compared plate versus tension band wiring, and the other four essentially compared modified techniques of tension band wiring with the established standard tension band wiring. The sixth trial compared a novel OMC fixation technique with locking plate fixation. There was little consistency in the clinical outcome measures used and presentation of data.
One trial (41 participants; 22 in plate fixation group, 19 in tension banding wiring group), which did not report participant‐assessed function, provided very low quality evidence of a better clinical outcome, based on an assessment of pain and loss of elbow range of motion, at a mean of six months' follow‐up after plate fixation compared with tension band wiring (Hume 1992; seesummary of findings Table for the main comparison). There was very low quality evidence that plate fixation resulted in fewer cases of symptomatic hardware prominence. Although the two cases of non‐union and the one case of heterotopic ossification occurred in the tension band wiring group, the very quality of the evidence for these and all outcomes of this trial means that we are very uncertain about the findings of this trial. Evidence from one ongoing trial (67 participants) is pending (NCT01391936).
One trial (30 participants; 15 in each group) provided very low quality evidence of little difference at a mean of 8.2 months between intramedullary screw plus tension band wiring fixation versus standard tension band wiring using the mean Modified Murphy Scoring System, which assessed function, pain, range of motion and joint space (Ahmed 2008). Although when presented in terms of excellent or good scores, the results favoured the screw group, where all had such scores, the arbitrary nature of the categorisation means that this result was insecure. There was very low quality evidence that hardware prominence was lower in the screw group. One infection occurred in the tension band wiring group.
One trial (25 participants; 15 in biodegradable group, 10 in metal wire fixation group) provided very low quality evidence of little difference in subjectively or objectively assessed good outcome at a mean of 20 months between tension band wiring with biodegradable implants versus metal wire fixation implants (Juutilainen 1995). One (6.6%) participant in the biodegradable group versus two (20%) participants in the metal wire fixation group had a painful elbow joint at final follow‐up. There were no adverse events reported. It was noted that all 10 participants in the metal wire fixation group had another routine operation to remove the metalwork at one year.
One trial (46 participants; 21 in Netz pin group, 25 in K‐wires tension binding group), which did not report on function or pain, provided very low quality evidence of lower rates of metalwork for any reason or for symptoms after Netz pin fixation compared with K‐wire tension band wiring (Larsen 1987). However, the evidence also supported the possibility of higher rates of metalwork removal in the Netz pins group. Two intraoperative complications (intraoperative fracture; a dropped Netz pin into the intramedullary canal during metalwork removal) occurred in the Netz pin group.
One trial (62 participants) provided low quality evidence of better objectively rated function based on MEPS with the cable pin system compared with standard tension band wiring (Liu 2012). It also found low quality evidence of a lower rate (1/30 with cable pin versus 7/32 with tension band wiring) of postoperative complications in the cable pin group; five of the tension band wiring group required removal of metalwork. All fractures united.
One trial (40 participants; 20 in each group) provided low quality evidence of similar patient‐reported function using DASH at two or more years after fixation using a novel OMC compared with locking plate fixation (Chen 2013). Although there was very low quality evidence of better objectively rated function based on MEPS in the OMC group, the wide CI values did not rule out the converse for locking plate fixation. The only adverse event was one of superficial infection in the locking plate group.
Overall completeness and applicability of evidence
This review included data from only six small trials with 244 participants. The available data for each comparison were from studies with only 25 to 62 participants.
The trial populations were representative of the populations generally treated by tension band wiring. The treated fractures were predominantly transverse or oblique fractures; and three trials excluded comminuted fractures. Around one‐third of participants had comminuted fractures in the other three trials (Chen 2013; Hume 1992; Larsen 1987). Only Hume 1992 included open fractures; there were two in each group. The mechanisms of injury in most participants were direct falls or road traffic accidents. In all trials, the evidence mainly focused on a cohort of participants with isolated transverse or oblique olecranon fractures amenable to surgical interventions. While this cohort was not fully representative of all people with olecranon fractures, it was representative of most people presenting to clinicians with olecranon fractures for whom surgery would be considered. Furthermore, trials were conducted in different geographical and healthcare settings spanning the globe (USA, Finland, Denmark, Egypt and China), thus providing good representation of people with olecranon fractures.
The tension band wiring technique is the most commonly used surgical intervention for the treatment of transverse and oblique olecranon fractures and five trials used it as the control group. The use of plate fixation, especially locking plate fixation, is growing for the treatment of several fractures and, thus, appropriate interventions for comparison in Chen 2013 and Hume 1992. However, the novelty of the nickel‐titanium OMC means that the applicability of this device is questionable. Other interventions, such as olecranon excision and triceps advancement, which is mainly used in older people with osteoporotic bone or extensive comminution, have not been investigated in controlled clinical trials.
Most participants with simple transverse or oblique olecranon fractures are expected to have good functional outcomes irrespective of the type of surgical intervention (Flinterman 2014). Our included trials all reported good outcomes in relation to fracture healing and return to near normal function. While there was some low or very low quality evidence of better clinical or functional outcome of the plate fixation or the cable pin system when compared with standard tension band wiring, the key difference was the rate of adverse effects and, on occasion, the need for further surgery. This pertains mainly to hardware prominence, which is the most commonly reported adverse effect of tension band wiring (Duckworth 2012; Newman 2009; Rommens 2004), and in our review. As emphasised in Juutilainen 1995, early or routine metalwork removal both incur further costs and risks of surgery.
Quality of the evidence
This review included only six small trials with 244 participants with olecranon fractures. There were four RCTs (Chen 2013; Hume 1992; Juutilainen 1995; Liu 2012) and two quasi‐RCTs (Ahmed 2008; Larsen 1987), both of which we judged to be at high risk of selection bias. We judged all six trials to be at high risk of performance bias, reflecting lack of blinding, and four trials at high risk of detection bias. Most judgements for the other domains were unclear, reflecting uncertainty and lack of information. There was little consistency in the clinical outcome measures used and presentation of data. Although final follow‐up was usually spread over several months or years in the individual trials, all participants were included in the final analyses.
We used the GRADE approach to assess the quality of the evidence and help interpret the findings (Schünemann 2008). When examining the outcome‐specific information concerning the overall quality of evidence from each included trial for every comparison, the evidence was of low quality for all included trials. For each comparison, there was only one study with few participants. We double‐downgraded each outcome in each comparison because of limitations in the study designs as stated above and imprecision in the results with wide CI values.
We downgraded the evidence from Hume 1992 (plate fixation versus tension band wiring), two levels for limitations in study design and implementation (reflecting lack of blinding and the spread of follow‐up of several years) and one level for either indirectness (reflecting the unsatisfactory nature of the clinical assessment tool) or imprecision (reflecting the wide CI values (adverse events)).
We downgraded the evidence from Ahmed 2008 (intramedullary screw plus tension band wiring versus tension band wiring) two levels for limitations in study design and implementation (reflecting selection bias and lack of blinding) and one level for either indirectness (reflecting the unsatisfactory nature of the composite assessment tool for assessing outcome) or imprecision (reflecting the wide CI values (adverse events)).
We downgraded the evidence from Juutilainen 1995 (biodegradable wire plus screw versus two K‐wire tension band wiring) two levels for limitations in study design and implementation (reflecting lack of blinding and overall uncertainties about study methods) and one level for either indirectness (reflecting the unsatisfactory nature of the assessing clinical outcome) or imprecision (reflecting the absence of data on adverse events).
We downgraded the evidence from Larsen 1987 (Netz pins versus K‐wires tension band wiring) two levels for limitations in study design and implementation (reflecting selection bias and lack of blinding) and one level for imprecision (reflecting the wide CI values (adverse events)).
We downgraded the evidence from Liu 2012 (cable pin system versus K‐wires tension band wiring), one level for limitations in study design and implementation (reflecting performance bias, related to unavoidable lack of blinding), and one level for either indirectness (reflecting the non‐validated and non‐subjective nature of the measurement of function) or imprecision (reflecting the wide CI values (adverse events)). Although we have no evidence for publication bias and could not test for it, we emphasise that it is inappropriate to rely on the evidence from one small trial, however well run.
We downgraded the evidence from Chen 2013 (a novel nickel‐titanium OMC versus locking plate fixation) two levels for limitations in study design and implementation (reflecting uncertainties relating to lack on reporting on methods, discrepancies in reporting, and lack of clinician and participant blinding), and one further level for imprecision reflecting broad CI values for objective outcomes. The novel nature of the intervention designed by the trial authors should also be noted.
Potential biases in the review process
The review was conducted as per the published protocol with no changes. We tried to minimise publication bias by undertaking a comprehensive search strategy and checking non‐English language citations. However, one Chinese comparative study identified in the search is awaiting classification (Sui 2008). Our search also included ongoing trials and we identified one RCT comparing tension band wiring with plate fixation, which has now completed follow‐up (NCT01391936). This will be added to the review in any future update. None of the review authors have conflicts of interest regarding this review.
Agreements and disagreements with other studies or reviews
To the best of our knowledge, this is the first systematic review of RCTs and quasi‐RCTs of surgical interventions for olecranon fractures. However, our findings are in line with other reviews of case‐series, non‐randomised controlled trials and current concept reviews, particularly in terms of the hardware prominence in tension band wiring (Duckworth 2012; Karlsson 2002; Newman 2009; Romero 2000; Veillette 2008).

Flow diagram of search results.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Comparison 1 Plate fixation versus tension band wiring, Outcome 1 Good clinical outcome (little pain or loss of elbow motion: Helm criteria) 16‐86 weeks follow‐up.

Comparison 1 Plate fixation versus tension band wiring, Outcome 2 Adverse events.

Comparison 2 Intramedullary screw plus tension band wiring (TBW) versus tension band wiring, Outcome 1 Functional assessment (Modified Murphy Scoring System).

Comparison 2 Intramedullary screw plus tension band wiring (TBW) versus tension band wiring, Outcome 2 Murphy score (including function, pain, loss of movement, joint space): excellent or good result.

Comparison 2 Intramedullary screw plus tension band wiring (TBW) versus tension band wiring, Outcome 3 Adverse events.

Comparison 2 Intramedullary screw plus tension band wiring (TBW) versus tension band wiring, Outcome 4 Loss in flexion > 20°.

Comparison 3 Biodegradable wire and screw versus metal wires tension band wiring, Outcome 1 Good clinical outcome: objective clinical improvement 6‐24 months follow‐up.

Comparison 3 Biodegradable wire and screw versus metal wires tension band wiring, Outcome 2 Painless elbow joint.

Comparison 3 Biodegradable wire and screw versus metal wires tension band wiring, Outcome 3 Normal range of movement.
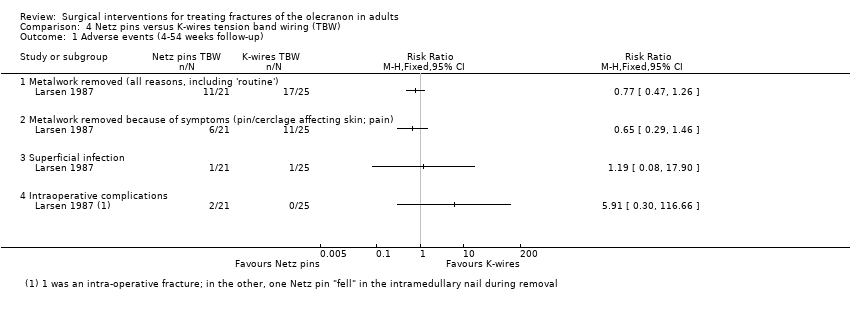
Comparison 4 Netz pins versus K‐wires tension band wiring (TBW), Outcome 1 Adverse events (4‐54 weeks follow‐up).

Comparison 5 Cable pin system (CPS) versus tension band wiring (TBW), Outcome 1 Mayo Elbow Performance Score 12‐36 months follow‐up.
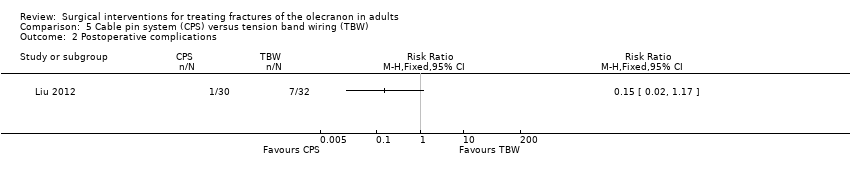
Comparison 5 Cable pin system (CPS) versus tension band wiring (TBW), Outcome 2 Postoperative complications.

Comparison 5 Cable pin system (CPS) versus tension band wiring (TBW), Outcome 3 Operation time and blood loss.
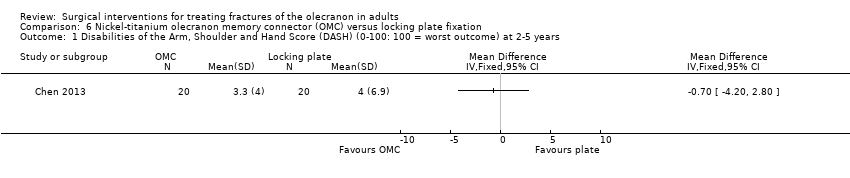
Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 1 Disabilities of the Arm, Shoulder and Hand Score (DASH) (0‐100: 100 = worst outcome) at 2‐5 years.

Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 2 Mayo Elbow Performance Score (0‐100: 100 = best outcome) at 2‐5 years.
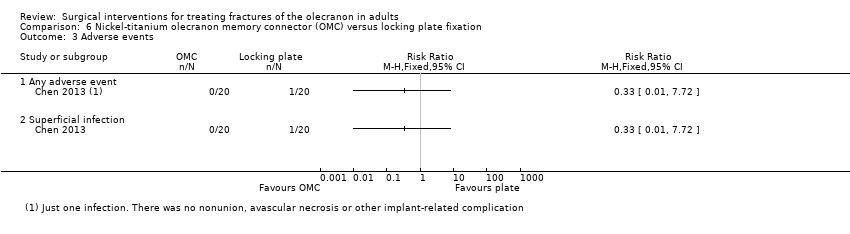
Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 3 Adverse events.

Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 4 Range of elbow motion.

Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 5 Participant dissatisfaction.
| Plate fixation compared with tension band wiring for treating olecranon fractures in adults | ||||||
| Patient or population: adults with olecranon fractures Settings: hospital Intervention: plate fixation (using 1/3 tubular plates) Comparison: tension band wiring fixation | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk1 | Corresponding risk | |||||
| Tension band wiring | Plate fixation | |||||
| Functional assessment (e.g. via patient‐reported outcome measures of elbow function) | see Comments | see Comments | ‐ | ‐ | ‐ | Not reported. 1 ongoing trial (67 participants) testing this comparison will be reporting DASH (Disabilities of the Arm, Shoulder and Hand) scores at 1 year (NCT01391936) |
| Good clinical outcome (little pain or loss of elbow motion: Helm criteria) Follow‐up: mean 28.5 weeks, range 16‐86 weeks | Study population | RR 1.82 (1.10 to 3.01) | 41 participants | ⊕⊝⊝⊝ | Results were rated 'good' if there was no more than slight or occasional pain, loss of movement was less than 15° at the elbow and no revision surgery for operative failure | |
| 474 per 1000 | 863 per 1000 | |||||
| Pain | see Comments | see Comments | ‐ | 41 participants | ‐ | Separate pain data were not available; these should be in the 1 ongoing trial (67 participants) testing this comparison (NCT01391936) |
| Adverse events ‐ overall | see Comments | see Comments | ‐ | 41 participants | ‐ | Incomplete reporting and discrepancies in the reporting of infection meant that numbers of participants with ≥ 1 adverse events data could not be reported here |
| Adverse events ‐ symptomatic metal prominence Follow‐up: mean 28.5 weeks, range 16‐86 weeks | Study population | RR 0.11 (0.01 to 0.79) | 41 participants | ⊕⊝⊝⊝ | Metalwork prominence is a well‐known problem of tension band wiring. Symptoms were local discomfort or pain over the implant. There was no record of implant removal surgery in either group | |
| 421 per 1000 | 46 per 1000 | |||||
| Adverse events ‐ delayed or non‐union Follow‐up: 6 months | Study population | RR 0.17 [0.01 to 3.41] | 41 participants | ⊕⊝⊝⊝ | Surgical treated (debridement) infection preceded both cases in the tension band wiring group | |
| 106 per 1000 | 18 per 1000 | |||||
| Adverse events ‐ heterotopic ossification (bone formation) Follow‐up: mean 28.5 weeks, range 16‐86 weeks | Study population | RR 0.29 [0.01 to 6.72] | 41 participants | ⊕⊝⊝⊝ | The single participant with heterotopic ossification in the tension band wiring group developed ulnar neuropathy | |
| 53 per 1000 | 16 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1. The basis of the assumed risk is that for control group (tension band wiring) in the study population. 2. The evidence was downgraded 2 levels for limitations in design and implementation (including lack of blinding and spread of timing of outcome measurement) and 1 level for indirectness (the Herm criteria were not validated and could be considered surrogate to functional outcome). 3. The evidence was downgraded 2 levels for limitations in design and implementation (including lack of blinding and spread of timing of outcome measurement) and 1 level for imprecision. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Good clinical outcome (little pain or loss of elbow motion: Helm criteria) 16‐86 weeks follow‐up Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Metal prominence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Delayed or non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Heterotopic ossification | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Functional assessment (Modified Murphy Scoring System) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Murphy score (including function, pain, loss of movement, joint space): excellent or good result Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Hardware prominence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Loss in flexion > 20° Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Good clinical outcome: objective clinical improvement 6‐24 months follow‐up Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Subjective assessment: move elbow freely without pain, same use as other elbow | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Objective assessment: good functional movement and stable elbow | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Painless elbow joint Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Normal range of movement Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Adverse events (4‐54 weeks follow‐up) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Metalwork removed (all reasons, including 'routine') | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Metalwork removed because of symptoms (pin/cerclage affecting skin; pain) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Superficial infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Intraoperative complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mayo Elbow Performance Score 12‐36 months follow‐up Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Postoperative complications Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Operation time and blood loss Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Operation time (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Intraoperative blood loss (mL) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Disabilities of the Arm, Shoulder and Hand Score (DASH) (0‐100: 100 = worst outcome) at 2‐5 years Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Mayo Elbow Performance Score (0‐100: 100 = best outcome) at 2‐5 years Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Any adverse event | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Superficial infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Range of elbow motion Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Flexion (°) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Extension (°) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Pronation (°) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Supination (°) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Participant dissatisfaction Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |

