Intervenciones quirúrgicas para el tratamiento de la fractura del olécranon en adultos
Information
- DOI:
- https://doi.org/10.1002/14651858.CD010144.pub2Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 26 November 2014see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Bone, Joint and Muscle Trauma Group
- Copyright:
-
- Copyright © 2014 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
HM: conceived the review, designed and wrote the protocol, assessed studies, extracted and analysed data, wrote the review. HM is also the guarantor of the review.
AA: provided general advice on drafts of the protocol and review.
SB: provided general advice on drafts of the protocol and review.
NG: provided general advice on drafts of the protocol and review.
HA: conceived the review, designed and wrote the protocol, assessed studies, extracted and analysed data, helped in writing the review.
Declarations of interest
Hosam E Matar: none known.
Amjid A Ali: none known.
Simon Buckley: none known.
Nicholas I Garlick: none known.
Henry D Atkinson: none known.
Acknowledgements
We would like to thank Andrew Duckworth, Joanne Elliott, Lindsey Elstub, Xavier Griffin, Helen Handoll and Laura MacDonald for their helpful feedback and support at the review stage.
We are grateful to Andrew Duckworth, Helen Handoll and Lindsey Elstub for their help on the protocol and to Joanne Elliott and Catherine Deering for developing the search strategies.
Version history
| Published | Title | Stage | Authors | Version |
| 2014 Nov 26 | Surgical interventions for treating fractures of the olecranon in adults | Review | Hosam E Matar, Amjid A Ali, Simon Buckley, Nicholas I Garlick, Henry D Atkinson | |
| 2012 Oct 17 | Surgical interventions for treating fractures of the olecranon in adults | Protocol | Hosam E Matar, Amjid A Ali, Simon Buckley, Nicholas I Garlick, Henry D Atkinson | |
Differences between protocol and review
There were no differences between the protocol and the review.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Adolescent; Adult; Aged; Aged, 80 and over; Female; Humans; Male; Middle Aged;
PICOs

Flow diagram of search results.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Comparison 1 Plate fixation versus tension band wiring, Outcome 1 Good clinical outcome (little pain or loss of elbow motion: Helm criteria) 16‐86 weeks follow‐up.

Comparison 1 Plate fixation versus tension band wiring, Outcome 2 Adverse events.

Comparison 2 Intramedullary screw plus tension band wiring (TBW) versus tension band wiring, Outcome 1 Functional assessment (Modified Murphy Scoring System).

Comparison 2 Intramedullary screw plus tension band wiring (TBW) versus tension band wiring, Outcome 2 Murphy score (including function, pain, loss of movement, joint space): excellent or good result.

Comparison 2 Intramedullary screw plus tension band wiring (TBW) versus tension band wiring, Outcome 3 Adverse events.

Comparison 2 Intramedullary screw plus tension band wiring (TBW) versus tension band wiring, Outcome 4 Loss in flexion > 20°.

Comparison 3 Biodegradable wire and screw versus metal wires tension band wiring, Outcome 1 Good clinical outcome: objective clinical improvement 6‐24 months follow‐up.

Comparison 3 Biodegradable wire and screw versus metal wires tension band wiring, Outcome 2 Painless elbow joint.

Comparison 3 Biodegradable wire and screw versus metal wires tension band wiring, Outcome 3 Normal range of movement.
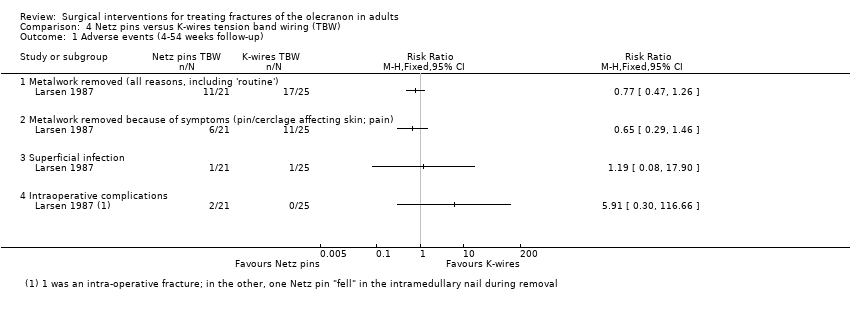
Comparison 4 Netz pins versus K‐wires tension band wiring (TBW), Outcome 1 Adverse events (4‐54 weeks follow‐up).

Comparison 5 Cable pin system (CPS) versus tension band wiring (TBW), Outcome 1 Mayo Elbow Performance Score 12‐36 months follow‐up.
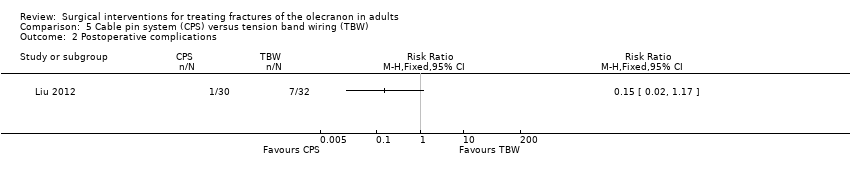
Comparison 5 Cable pin system (CPS) versus tension band wiring (TBW), Outcome 2 Postoperative complications.

Comparison 5 Cable pin system (CPS) versus tension band wiring (TBW), Outcome 3 Operation time and blood loss.
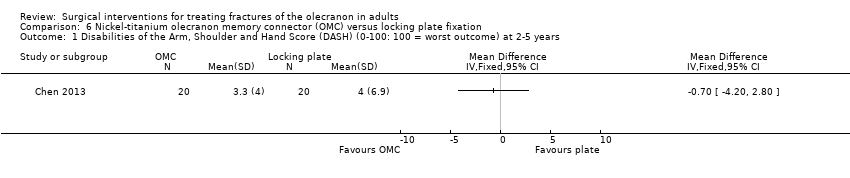
Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 1 Disabilities of the Arm, Shoulder and Hand Score (DASH) (0‐100: 100 = worst outcome) at 2‐5 years.

Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 2 Mayo Elbow Performance Score (0‐100: 100 = best outcome) at 2‐5 years.
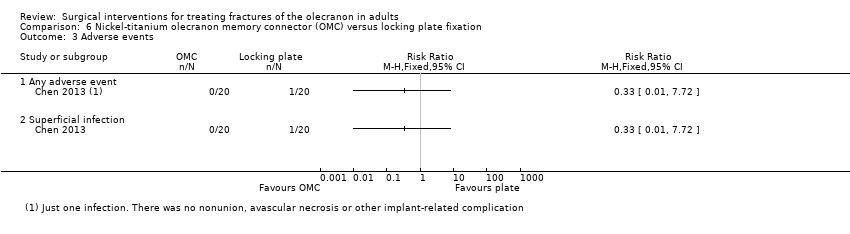
Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 3 Adverse events.

Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 4 Range of elbow motion.

Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 5 Participant dissatisfaction.
| Plate fixation compared with tension band wiring for treating olecranon fractures in adults | ||||||
| Patient or population: adults with olecranon fractures Settings: hospital Intervention: plate fixation (using 1/3 tubular plates) Comparison: tension band wiring fixation | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk1 | Corresponding risk | |||||
| Tension band wiring | Plate fixation | |||||
| Functional assessment (e.g. via patient‐reported outcome measures of elbow function) | see Comments | see Comments | ‐ | ‐ | ‐ | Not reported. 1 ongoing trial (67 participants) testing this comparison will be reporting DASH (Disabilities of the Arm, Shoulder and Hand) scores at 1 year (NCT01391936) |
| Good clinical outcome (little pain or loss of elbow motion: Helm criteria) Follow‐up: mean 28.5 weeks, range 16‐86 weeks | Study population | RR 1.82 (1.10 to 3.01) | 41 participants | ⊕⊝⊝⊝ | Results were rated 'good' if there was no more than slight or occasional pain, loss of movement was less than 15° at the elbow and no revision surgery for operative failure | |
| 474 per 1000 | 863 per 1000 | |||||
| Pain | see Comments | see Comments | ‐ | 41 participants | ‐ | Separate pain data were not available; these should be in the 1 ongoing trial (67 participants) testing this comparison (NCT01391936) |
| Adverse events ‐ overall | see Comments | see Comments | ‐ | 41 participants | ‐ | Incomplete reporting and discrepancies in the reporting of infection meant that numbers of participants with ≥ 1 adverse events data could not be reported here |
| Adverse events ‐ symptomatic metal prominence Follow‐up: mean 28.5 weeks, range 16‐86 weeks | Study population | RR 0.11 (0.01 to 0.79) | 41 participants | ⊕⊝⊝⊝ | Metalwork prominence is a well‐known problem of tension band wiring. Symptoms were local discomfort or pain over the implant. There was no record of implant removal surgery in either group | |
| 421 per 1000 | 46 per 1000 | |||||
| Adverse events ‐ delayed or non‐union Follow‐up: 6 months | Study population | RR 0.17 [0.01 to 3.41] | 41 participants | ⊕⊝⊝⊝ | Surgical treated (debridement) infection preceded both cases in the tension band wiring group | |
| 106 per 1000 | 18 per 1000 | |||||
| Adverse events ‐ heterotopic ossification (bone formation) Follow‐up: mean 28.5 weeks, range 16‐86 weeks | Study population | RR 0.29 [0.01 to 6.72] | 41 participants | ⊕⊝⊝⊝ | The single participant with heterotopic ossification in the tension band wiring group developed ulnar neuropathy | |
| 53 per 1000 | 16 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1. The basis of the assumed risk is that for control group (tension band wiring) in the study population. 2. The evidence was downgraded 2 levels for limitations in design and implementation (including lack of blinding and spread of timing of outcome measurement) and 1 level for indirectness (the Herm criteria were not validated and could be considered surrogate to functional outcome). 3. The evidence was downgraded 2 levels for limitations in design and implementation (including lack of blinding and spread of timing of outcome measurement) and 1 level for imprecision. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Good clinical outcome (little pain or loss of elbow motion: Helm criteria) 16‐86 weeks follow‐up Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Metal prominence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Delayed or non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Heterotopic ossification | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Functional assessment (Modified Murphy Scoring System) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Murphy score (including function, pain, loss of movement, joint space): excellent or good result Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Hardware prominence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Loss in flexion > 20° Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Good clinical outcome: objective clinical improvement 6‐24 months follow‐up Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Subjective assessment: move elbow freely without pain, same use as other elbow | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Objective assessment: good functional movement and stable elbow | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Painless elbow joint Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Normal range of movement Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Adverse events (4‐54 weeks follow‐up) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Metalwork removed (all reasons, including 'routine') | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Metalwork removed because of symptoms (pin/cerclage affecting skin; pain) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Superficial infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Intraoperative complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mayo Elbow Performance Score 12‐36 months follow‐up Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Postoperative complications Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Operation time and blood loss Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Operation time (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Intraoperative blood loss (mL) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Disabilities of the Arm, Shoulder and Hand Score (DASH) (0‐100: 100 = worst outcome) at 2‐5 years Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Mayo Elbow Performance Score (0‐100: 100 = best outcome) at 2‐5 years Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Any adverse event | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Superficial infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Range of elbow motion Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Flexion (°) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Extension (°) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Pronation (°) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Supination (°) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Participant dissatisfaction Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |

