Intervenciones quirúrgicas para el tratamiento de la fractura del olécranon en adultos
References
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Study design: quasi‐RCT Method of randomisation: based on odd or even participant [record?] numbers Setting: Elhadara University Hospital, Alexandri, Egypt Study period: December 2004 to July 2005 | |
| Participants | 30 adults with displaced transverse or oblique fracture of the olecranon Mean age: 33.4 years (range 17‐70 years) Mechanism of injury: direct blow 26.7%, fall on elbow 40%, fall from height 10%, road traffic accident 23.3% Side: 15 right side, 15 left side Fracture population: 16 (53.3%) transverse fractures, 14 (46.7%) oblique fractures Inclusion criteria: displaced transverse or oblique fracture of the olecranon Exclusion criteria: people with comminuted, avulsion fractures or fracture dislocations All participants were included in the final analysis | |
| Interventions | 1. Intervention group: intramedullary screw plus tension band fixation (n = 15) 2. Control group: standard AO tension band wiring (n = 15) All participants had their arms put in an arm sling except those with less rigid intraoperative fixation who were put in a back slab. Gentle active exercises were started gradually after removal of stitches | |
| Outcomes | Mean follow‐up: 8.2 months (range 6‐14 months) 1. Modified Murphy scoring system 2. Adverse events: hardware prominence and infection 3. Loss of range of motion | |
| Notes | The following description was largely copied from Ahmed 2008 Operative technique for the intervention group: using a dorsal longitudinal incision and exposure of the fracture site, reduction was done using 2 reduction forceps. A small stab was made in the triceps aponeurosis then a drill hole was made in the olecranon passing towards the medullary canal of the ulna, tapping was done through the drill hole; the tap was used to determine the screw length at which the tap got 2 or 3 turns of solid cortical contact in the distal medullary canal. A 6.5‐mm cancellous screw with a washer was inserted through the drill hole leaving about 1 cm outside to pass the stainless steel wire around it. A 2.5‐mm transverse hole was drilled in the posterior cortex of the distal fragment about 2 cm from the fracture site, then a figure of 8 loop was applied deep to the triceps aponeurosis and around remaining part of the screw | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Participants were randomly divided into 2 groups of equal number where participants with odd numbers were allocated to the control group and participants with even numbers allocated to the intervention group |
| Allocation concealment (selection bias) | High risk | Quasi‐randomised: hence, allocation was not concealed |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was practical for surgeons. There was no mention of blinding for the participants |
| Blinding of outcome assessment (detection bias) | High risk | Unclear whether outcome assessors were blinded to treatment allocation |
| Incomplete outcome data (attrition bias) | Low risk | All participants were included in the final analysis |
| Selective reporting (reporting bias) | Unclear risk | No access to trial protocol |
| Other bias | Unclear risk | There were potentially important imbalances in the baseline characteristics. Similar care programmes were applied although varied according to perceived postoperative fracture stability |
| Methods | Study design: RCT Method of randomisation: participants were randomised to intervention groups (no further details) Setting: Changhai Hospital, Shanghi, China Study period: May 2004 to December 2009 | |
| Participants | 40 adults with olecranon fractures requiring surgical fixation Mean age: 48.4 years (range 21‐77 years) (or 49.4 years if using data in text rather than table 2 in trial report) Sex: 22 men, 18 women Mechanism of injury: fall 57.5%, road traffic accident 32.5%, sports injury 5%, falling objects 5% Fracture type: 19 Mayo type IIA, 10 Mayo type IIB, 8 Mayo type IIIA, 3 Mayo type IIIB (data from text) (see footnote for explanation) Inclusion criteria: closed Mayo classification type II/III olecranon fractures, transverse or slight oblique fracture, no neurovascular compromise, stable vital signs, written consent Exclusion criteria: Mayo type I fracture, non‐traumatic fractures, severe comminution, old fractures, or participants with psychological and social conditions with poor compliance All participants were included in the final analysis | |
| Interventions | 1. Intervention group: OMC fixation (see Notes section below) (n = 20) 2. Control group: locking plate fixation (n = 20) Postoperatively: all participants were given antibiotics after surgery as per local protocol. Cast immobilisation applied for 2 weeks followed by rehabilitation with gentle elbow flexion and extension started | |
| Outcomes | Mean follow‐up: 36.65 months (range 24‐56) (taken from text of report)
| |
| Notes | The following description was largely copied from Chen 2013. OMC: the OMC was designed on the basis of the anatomical structure of the olecranon and manufactured from 1.8‐2.5 mm thick Ni‐Ti shape memory alloy plate. It was composed of an intramedullary fixing lock, a base arc and 2 compression fixing arms. Depending on material properties, the memory direction of OMC is set as a 1‐way memory in order to obtain the largest memory kinetic energy. The transition temperature was set between 28 °C and 33 °C, so that memory kinetic energy and elastic force were produced during transition from plastic deformation phase in low temperature (martensite phase) to previous shape in high temperature (austenite phase), which can continuously provide lateral compressive force. The OMC was cooled with ice for 2‐4 minutes before implantation. A hole was drilled at the tip of olecranon, where the intramedullary fixing lock was inserted parallel to the ulnar. Then 2 holes were drilled at the ulnar diaphysis with a hole on each side, consistent with the head hook of the compression fixing arm. The OMC was fixed to the olecranon automatically with warm water after inserting the head hooks into the ulnar diaphysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were "randomly divided" into treatment groups ‐ no further details |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether the allocation was concealed |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was practical for surgeons. There was no mention of blinding for the participants |
| Blinding of outcome assessment (detection bias) | Low risk | All clinical assessment in this research was done by independent observers. "All assessors who evaluated the postoperative function were blinded by means of a randomised block design" |
| Incomplete outcome data (attrition bias) | Unclear risk | All participants were included in the final analysis and completed the follow‐up. However, there were some small discrepancies in the reporting of baseline characteristics, timing of follow‐up and MEPS |
| Selective reporting (reporting bias) | Unclear risk | None noted. No access to trial protocol |
| Other bias | Unclear risk | Both groups were similar at baseline and were provided with similar rehabilitation. However, the OMC was designed by the study authors and, while they claim no conflict of interest, it is uncertain whether this could be a source of bias |
| Methods | Study design: RCT Method of randomisation: no details Setting: Los Angeles Medical Centre, California, US Study period: 1 January 1986 to 1 January 1987 | |
| Participants | 41 participants with displaced olecranon fractures requiring surgical fixation Mean age: 30.9 years (range 18‐67 years) Sex: 30 men, 11 women Mechanism of injury: fall 35%, direct blow 47%, road traffic accident 18% Side: 25 non‐dominant side, 16 dominant side; 1 participant had bilateral olecranon fractures Fracture population: 3 simple reverse oblique, 11 simple transverse, 15 simple oblique and 12 comminuted; 4 participants had open fractures; 2 in each group Inclusion criteria: involvement of at least 1 cm of the olecranon, fracture extension into the semilunar notch, and articular displacement of at least 1 mm Exclusion criteria: small avulsion fractures not amenable to internal fixation, fractures associated with injury to the radial head or distal humerus All participants were included in the final analysis | |
| Interventions | 1. Intervention group: plate fixation (n = 22). Plate fixation: 1/3 tubular plate with 3.5‐mm screws used, plate contoured along the posterior surface of the proximal ulna and olecranon. Lag screws were used when possible across the fracture line to obtain interfragmentary compression 2. Control group: standard tension band wiring (n = 19). After reduction, 2 parallel 1.5 mm K‐wires were introduced; 18‐gauge wire was used to form a figure of 8 loop. After tightening, the protruding wire ends were bent at least 90° Postoperative care: long arm cast splint used for 2‐3 days then active flexion and extension were encouraged for all participants | |
| Outcomes | Mean follow‐up: 28.5 weeks (range 16‐86 weeks)
| |
| Notes | All procedures performed according the standard techniques | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomised to treatment groups, no further details |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether the allocation was concealed |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was practical for surgeons. There was no mention of blinding for the participants |
| Blinding of outcome assessment (detection bias) | High risk | There was no report of measures taken to blind outcome assessment |
| Incomplete outcome data (attrition bias) | High risk | All participants completed the follow‐up. However, follow‐up spanned several years, which could have been a source of bias. In addition, no information was given on participant with bilateral fractures. There was also some discrepancies in the reporting of infection |
| Selective reporting (reporting bias) | Unclear risk | None noted. No access to trial protocol |
| Other bias | Low risk | It was reported that the groups were similar at baseline. In addition, there was similar postoperative care |
| Methods | Study design: RCT Methods of randomisation: not reported Settings: Helsinki University Central Hospital, Finland Study period: 1982 "through" 1984 | |
| Participants | 25 adults with closed olecranon fractures Mean age: 49.8 years (range 17‐85 years) Sex: 8 men and 17 women Side of fracture: 12 right sided and 13 left sided Mechanism of injury: no details Fracture population: no details aside from inclusion criteria Inclusion criteria: participants > 16 years of age with closed olecranon fractures; transverse or oblique fractures in 2 or 3 parts without additional fragmentation Exclusion criteria: participants with mental illness or chronic alcoholism All participants were included in the final analysis | |
| Interventions | 1. Intervention group: biodegradable wire and screw tension band wiring (n = 15). A special biodegradable wire made of self reinforced poly‐L‐lactide acid (SR‐PLLA) was developed. The length of the wire was 50 cm and the diameter, 0.5 or 0.9 ram. This wire was used together with self reinforced polyglycolide acid (SR‐PGA) screws or SR‐PLLA plugs 2. Control group: standard tension band wiring (n = 10). 2 K wires and metal cerclage wire Postoperatively, participants wore a splint for 4 weeks, and slight elbow movements (75°‐95°) were allowed. Stitches were removed after 2 weeks All metallic implants were removed 1 year after the primary operation | |
| Outcomes | Mean follow‐up: 19.7 months (range 6‐24 months)
| |
| Notes | The trial also included 9 participants with patella fractures | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomised to 2 groups ‐ no further details |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether the allocation was concealed |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was practical for surgeons. There was no mention of blinding for the participants |
| Blinding of outcome assessment (detection bias) | High risk | There was no report of measures taken to blind outcome assessment |
| Incomplete outcome data (attrition bias) | Low risk | All participants were included in the final analysis, all participants completed the follow‐up |
| Selective reporting (reporting bias) | Unclear risk | None noted. No access to trial protocol |
| Other bias | Unclear risk | It is unclear whether both groups were similar at baseline |
| Methods | Study design: quasi‐RCT Method of randomisation: participants were divided to intervention groups according to whether they were admitted on even or odds days Setting: Gentofte Hospital, University of Copenhagen, Denmark Study period: 1982 "through" 1984 | |
| Participants | 46 participants with displaced olecranon fractures requiring surgical fixation Median age: 60 years (men); 67 years (women) (range 16‐87 years) Sex: 14 men and 32 women Side: not stated Mechanism of injury: no details Fracture population: 26 transverse, 5 oblique, 15 comminuted Inclusion criteria: olecranon fracture Exclusion criteria: no details All participants were included in the final analysis | |
| Interventions | 1. Intervention group: modified tension band wiring using Netz pins (n = 21): Netz pins are non‐sliding pins made of stainless steel, diameter 2.0 mm, available from 60‐120 mm in length; they have a lancet‐shaped point and a hole of 1.1 mm at the base for introduction of the cerclage wire 2. Control group: standard tension band wiring (n = 25) To prevent the cerclage wire from sliding off, the K‐wires at the tip were bent 180º Postoperative care: not stated | |
| Outcomes | Follow‐up: until fracture healing and elbow range of motion was considered stationary, median 13 weeks (range 4‐54 weeks)
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Participants were divided to intervention groups according to whether they were admitted on even or odds days |
| Allocation concealment (selection bias) | High risk | Allocation was very unlikely to be concealed in a quasi‐RCT |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was practical for surgeons. There was no mention of blinding for the participants |
| Blinding of outcome assessment (detection bias) | High risk | There was no report of measures taken to blind outcome assessment |
| Incomplete outcome data (attrition bias) | Unclear risk | All participants were included in the analysis but variable timing of follow‐up based on assessment of fracture healing and achievement of maximum range of motion. No criteria for these given |
| Selective reporting (reporting bias) | Unclear risk | No access to trial protocol |
| Other bias | Unclear risk | Although the groups were balanced by fracture type, the comparability of other baseline characteristics was not established. No information on postoperative care |
| Methods | Study design: RCT Methods of randomisation: participants' fractures were classified according to the Mayo classification system, then randomly divided into 2 groups using an adaptive biased coin design to protect against prognostic imbalance between the groups. Randomisation was carried out by a research assistant once eligible participants admitted, the result was placed in a sealed envelope, both doctors and participants were blinded to the participant's group until the envelope was opened after signing the consent form Settings: 2 university hospitals, Beijing, China Study period: June 2007 to December 2010 | |
| Participants | 62 participants with closed olecranon fractures Mean age: 47 years (range 20‐70 years) Sex: 30 men, 32 women Mechanism of injury: fall 55%, road traffic accident 36%, sports injury 8% Fracture population: 50 Mayo type IIA, 12 Mayo type IIIA fractures (see footnote for explanation) Inclusion criteria: aged 20‐70 years, with transverse or slight oblique olecranon fractures that were fresh, closed and 2 mm above displacement Exclusion criteria: non‐traumatic fracture, serious comminuted fracture, other fractures or injuries that could affect elbow joint function or postoperative function exercise All participants were included in the analysis | |
| Interventions | 1. Intervention group: modified tension band wiring using cable pin system (n = 30) 2. Control group: standard tension band wiring (n = 32) Postoperatively, the elbow was secured in a sling flexed to 90° for 2 days, active flexion and gravity‐assisted extension were initiated afterwards | |
| Outcomes | Mean follow‐up: 21 months (range 12‐36)
| |
| Notes | The following description was largely copied from Liu 2012. Cable pin system Zimmer® (CPS): 2 x 4.0‐mm diameter, specially sharpened, partially threaded cancellous lag screws (pin length 35‐60 mm). The tail of the pin was connected to a stainless steel multi‐filament cable (diameter 1.3 mm, length 448 mm) and the other end of the cable was attached to a smooth shank end, which was used as a leader needle Operative technique: 2.5‐mm‐diameter drill bit was used to drill the holes, the first hole was drilled from the proximal end of the olecranon across the fracture site. The hole depth was measured and a pin of appropriate length was chosen. Next, the threaded portion of the pin was drilled across the fracture site through the hole until the tail was slightly countersunk into the bone. A second 2.5‐mm‐diameter hole was drilled parallel to the first, and the second pin was drilled across the fracture site in a similar manner to the first. The third drill hole was created perpendicular to the long axis of the ulna and posterior to the pins, at the same or slightly longer distance from the fracture site as the tip of the olecranon (usually 3‐4 cm distal to the fracture site). The 2 cables connecting the pins were crossed in a figure of 8 over the posterior surface of the olecranon. The leader needle of 1 cable was passed through the perpendicular drill hole (the third hole) in the ulna and pulled out. The free ends of the 2 cables were passed in opposite directions through a crimp, and the cables were adjusted by turning the button on the tensioning handle. When the appropriate tension was achieved, the arms of the tensioning handle were squeezed to secure the crimp | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly divided into 2 groups using an adaptive biased coin design |
| Allocation concealment (selection bias) | Low risk | Sealed envelope containing the randomisation were opened immediately after the consent form was signed |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was practical for surgeons. There was no mention of blinding for the participants |
| Blinding of outcome assessment (detection bias) | Low risk | An independent group of physicians (not involved in the initial fracture treatment and blinded to the fixation method) evaluated the clinical outcomes of all participants |
| Incomplete outcome data (attrition bias) | Low risk | All participants were included in the final analysis, all participants completed the follow‐up |
| Selective reporting (reporting bias) | Unclear risk | No access to trial protocol |
| Other bias | Low risk | Both groups were similar at baseline with no major differences in baseline characteristics. In addition, there was similar postoperative care |
K wires: Kirschner wires; MEPS: Mayo Elbow Performance Score; n: number; OMC: olecranon memory connector; RCT: randomised controlled trial.
Mayo classification: type I fractures are undisplaced, type II are displaced and stable, and type III are displaced and unstable. Each is divided into subtype A (non‐comminuted) or B (comminuted).
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Study design: RCT Participants: older women with complex elbow fractures including distal humerus fractures. No isolated olecranon fractures Interventions: primary total elbow replacement versus open reduction and internal fixation | |
| Study design: historical cohort study | |
| Study design: RCT Participants: people with intra‐articular distal humeral fracture or a fracture‐dislocation of the elbow with proximal radial or ulnar (or both) fractures were included Interventions: single‐fraction radiotherapy postoperatively versus no radiotherapy for prevention of heterotopic ossification | |
| Study design: RCT Participants: children with displaced elbow fractures | |
| Study design: concurrent cohort study | |
| Study design: historical cohort study | |
| Study design: retrospective comparison | |
| Study design: case‐control study | |
| Study design: non‐controlled clinical trial | |
| Study design: historical cohort study | |
| Study design: historical cohort study | |
| Study design: non‐controlled clinical trial | |
| Study design: historical cohort study | |
| Study design: retrospective comparison | |
| Study design: non‐controlled clinical trial |
RCT: randomised controlled trial.
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Comparative study |
| Participants | 63 participants with olecranon fractures, 41 males and 22 females, mean age 49.6 years (range 15‐67) |
| Interventions | Plate fixation (n = 28) versus tension band wiring (n = 35) |
| Outcomes | Follow‐up: 6‐15 months for all participants PANG Gui‐gen criteria used as 'Excellent', 'Good', 'Fair' and 'Bad'. The breakdown results as reported in the English abstract did not add up |
| Notes | Article in Chinese with English abstract, it is unclear from the abstract whether this was a randomised or quasi‐randomised comparative trial. Attempts made to contact the corresponding author (xujie‐[email protected]; contacted December 2012, November 2013), without success |
n: number.
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | A prospective randomised trial of plate fixation versus tension band wire for olecranon fractures |
| Methods | Allocation: randomised Intervention model: parallel assignment Masking: single blind (outcomes assessor) |
| Participants | 67 participants with displaced olecranon fractures |
| Interventions | Plate fixation versus tension band wiring |
| Outcomes | Primary outcome measures
Secondary outcome measures
|
| Starting date | September 2010 |
| Contact information | Andrew D Duckworth, MSc, MRCSEd Royal Infirmary of Edinburgh Tel: 07769701875 |
| Notes | Follow‐up completed: September 2014 Number of participants and completed of follow‐up information from conversation with Mr Duckworth (17 September 2014) |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Good clinical outcome (little pain or loss of elbow motion: Helm criteria) 16‐86 weeks follow‐up Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.1  Comparison 1 Plate fixation versus tension band wiring, Outcome 1 Good clinical outcome (little pain or loss of elbow motion: Helm criteria) 16‐86 weeks follow‐up. | ||||
| 2 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.2  Comparison 1 Plate fixation versus tension band wiring, Outcome 2 Adverse events. | ||||
| 2.1 Metal prominence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Delayed or non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Heterotopic ossification | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Functional assessment (Modified Murphy Scoring System) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.1  Comparison 2 Intramedullary screw plus tension band wiring (TBW) versus tension band wiring, Outcome 1 Functional assessment (Modified Murphy Scoring System). | ||||
| 2 Murphy score (including function, pain, loss of movement, joint space): excellent or good result Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.2  Comparison 2 Intramedullary screw plus tension band wiring (TBW) versus tension band wiring, Outcome 2 Murphy score (including function, pain, loss of movement, joint space): excellent or good result. | ||||
| 3 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.3  Comparison 2 Intramedullary screw plus tension band wiring (TBW) versus tension band wiring, Outcome 3 Adverse events. | ||||
| 3.1 Hardware prominence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Loss in flexion > 20° Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.4  Comparison 2 Intramedullary screw plus tension band wiring (TBW) versus tension band wiring, Outcome 4 Loss in flexion > 20°. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Good clinical outcome: objective clinical improvement 6‐24 months follow‐up Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.1  Comparison 3 Biodegradable wire and screw versus metal wires tension band wiring, Outcome 1 Good clinical outcome: objective clinical improvement 6‐24 months follow‐up. | ||||
| 1.1 Subjective assessment: move elbow freely without pain, same use as other elbow | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Objective assessment: good functional movement and stable elbow | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Painless elbow joint Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.2  Comparison 3 Biodegradable wire and screw versus metal wires tension band wiring, Outcome 2 Painless elbow joint. | ||||
| 3 Normal range of movement Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.3  Comparison 3 Biodegradable wire and screw versus metal wires tension band wiring, Outcome 3 Normal range of movement. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Adverse events (4‐54 weeks follow‐up) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.1 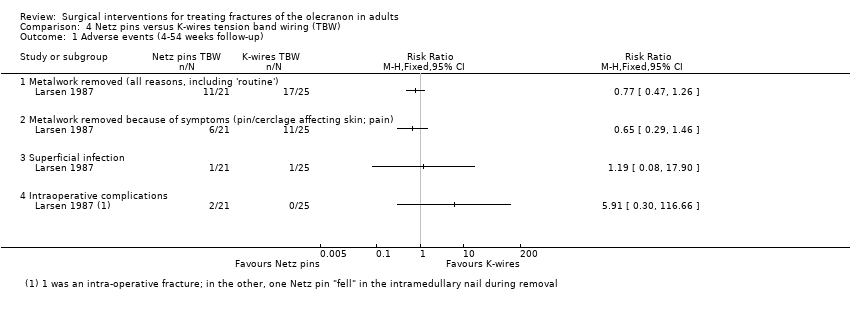 Comparison 4 Netz pins versus K‐wires tension band wiring (TBW), Outcome 1 Adverse events (4‐54 weeks follow‐up). | ||||
| 1.1 Metalwork removed (all reasons, including 'routine') | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Metalwork removed because of symptoms (pin/cerclage affecting skin; pain) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Superficial infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Intraoperative complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mayo Elbow Performance Score 12‐36 months follow‐up Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.1  Comparison 5 Cable pin system (CPS) versus tension band wiring (TBW), Outcome 1 Mayo Elbow Performance Score 12‐36 months follow‐up. | ||||
| 2 Postoperative complications Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.2 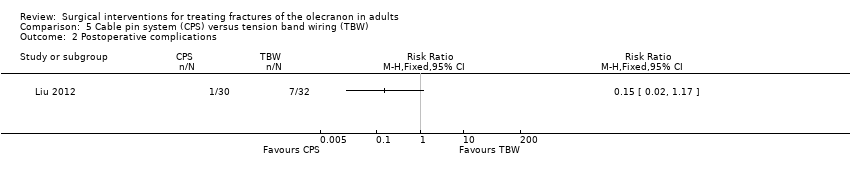 Comparison 5 Cable pin system (CPS) versus tension band wiring (TBW), Outcome 2 Postoperative complications. | ||||
| 3 Operation time and blood loss Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.3  Comparison 5 Cable pin system (CPS) versus tension band wiring (TBW), Outcome 3 Operation time and blood loss. | ||||
| 3.1 Operation time (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Intraoperative blood loss (mL) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Disabilities of the Arm, Shoulder and Hand Score (DASH) (0‐100: 100 = worst outcome) at 2‐5 years Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.1 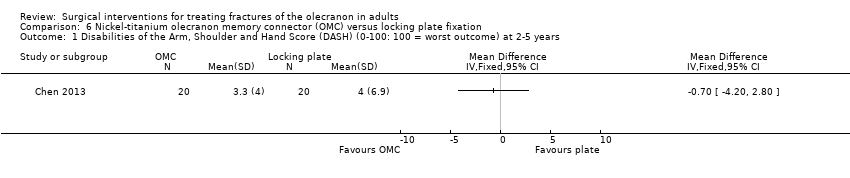 Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 1 Disabilities of the Arm, Shoulder and Hand Score (DASH) (0‐100: 100 = worst outcome) at 2‐5 years. | ||||
| 2 Mayo Elbow Performance Score (0‐100: 100 = best outcome) at 2‐5 years Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.2  Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 2 Mayo Elbow Performance Score (0‐100: 100 = best outcome) at 2‐5 years. | ||||
| 3 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.3 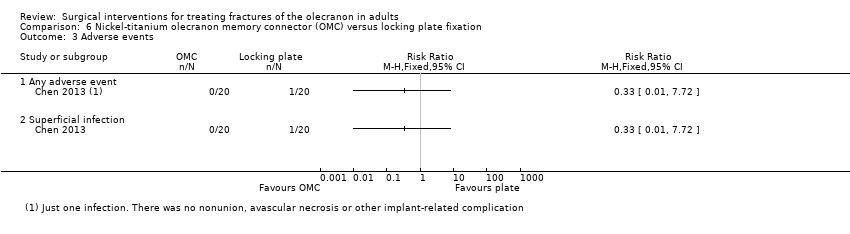 Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 3 Adverse events. | ||||
| 3.1 Any adverse event | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Superficial infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Range of elbow motion Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.4  Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 4 Range of elbow motion. | ||||
| 4.1 Flexion (°) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Extension (°) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Pronation (°) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Supination (°) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Participant dissatisfaction Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.5  Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 5 Participant dissatisfaction. | ||||

Flow diagram of search results.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Comparison 1 Plate fixation versus tension band wiring, Outcome 1 Good clinical outcome (little pain or loss of elbow motion: Helm criteria) 16‐86 weeks follow‐up.

Comparison 1 Plate fixation versus tension band wiring, Outcome 2 Adverse events.

Comparison 2 Intramedullary screw plus tension band wiring (TBW) versus tension band wiring, Outcome 1 Functional assessment (Modified Murphy Scoring System).

Comparison 2 Intramedullary screw plus tension band wiring (TBW) versus tension band wiring, Outcome 2 Murphy score (including function, pain, loss of movement, joint space): excellent or good result.

Comparison 2 Intramedullary screw plus tension band wiring (TBW) versus tension band wiring, Outcome 3 Adverse events.

Comparison 2 Intramedullary screw plus tension band wiring (TBW) versus tension band wiring, Outcome 4 Loss in flexion > 20°.

Comparison 3 Biodegradable wire and screw versus metal wires tension band wiring, Outcome 1 Good clinical outcome: objective clinical improvement 6‐24 months follow‐up.

Comparison 3 Biodegradable wire and screw versus metal wires tension band wiring, Outcome 2 Painless elbow joint.

Comparison 3 Biodegradable wire and screw versus metal wires tension band wiring, Outcome 3 Normal range of movement.
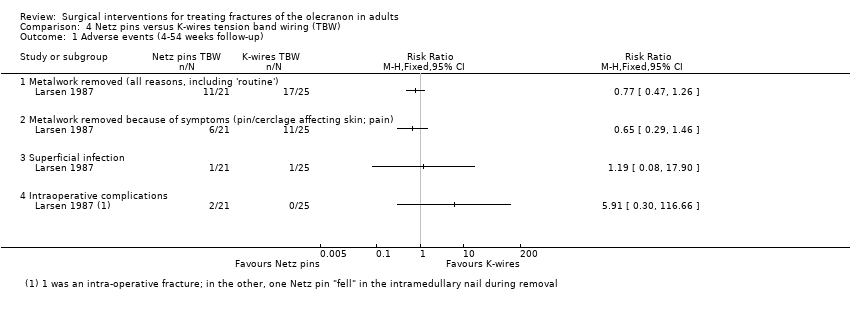
Comparison 4 Netz pins versus K‐wires tension band wiring (TBW), Outcome 1 Adverse events (4‐54 weeks follow‐up).

Comparison 5 Cable pin system (CPS) versus tension band wiring (TBW), Outcome 1 Mayo Elbow Performance Score 12‐36 months follow‐up.
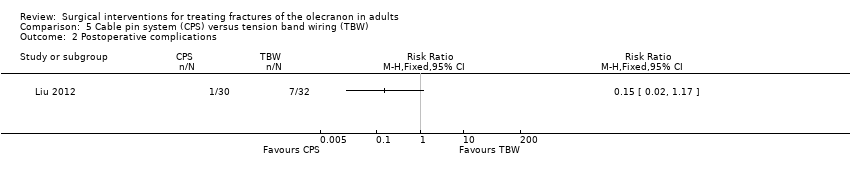
Comparison 5 Cable pin system (CPS) versus tension band wiring (TBW), Outcome 2 Postoperative complications.

Comparison 5 Cable pin system (CPS) versus tension band wiring (TBW), Outcome 3 Operation time and blood loss.
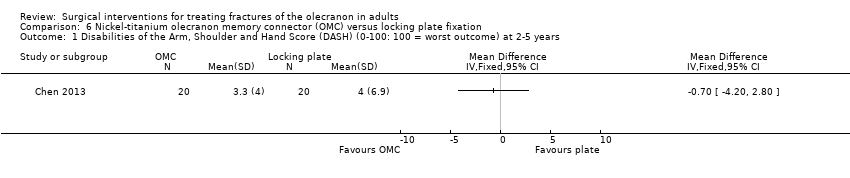
Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 1 Disabilities of the Arm, Shoulder and Hand Score (DASH) (0‐100: 100 = worst outcome) at 2‐5 years.

Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 2 Mayo Elbow Performance Score (0‐100: 100 = best outcome) at 2‐5 years.
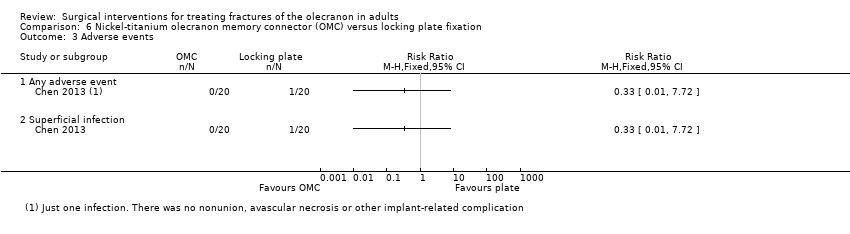
Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 3 Adverse events.

Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 4 Range of elbow motion.

Comparison 6 Nickel‐titanium olecranon memory connector (OMC) versus locking plate fixation, Outcome 5 Participant dissatisfaction.
| Plate fixation compared with tension band wiring for treating olecranon fractures in adults | ||||||
| Patient or population: adults with olecranon fractures Settings: hospital Intervention: plate fixation (using 1/3 tubular plates) Comparison: tension band wiring fixation | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk1 | Corresponding risk | |||||
| Tension band wiring | Plate fixation | |||||
| Functional assessment (e.g. via patient‐reported outcome measures of elbow function) | see Comments | see Comments | ‐ | ‐ | ‐ | Not reported. 1 ongoing trial (67 participants) testing this comparison will be reporting DASH (Disabilities of the Arm, Shoulder and Hand) scores at 1 year (NCT01391936) |
| Good clinical outcome (little pain or loss of elbow motion: Helm criteria) Follow‐up: mean 28.5 weeks, range 16‐86 weeks | Study population | RR 1.82 (1.10 to 3.01) | 41 participants | ⊕⊝⊝⊝ | Results were rated 'good' if there was no more than slight or occasional pain, loss of movement was less than 15° at the elbow and no revision surgery for operative failure | |
| 474 per 1000 | 863 per 1000 | |||||
| Pain | see Comments | see Comments | ‐ | 41 participants | ‐ | Separate pain data were not available; these should be in the 1 ongoing trial (67 participants) testing this comparison (NCT01391936) |
| Adverse events ‐ overall | see Comments | see Comments | ‐ | 41 participants | ‐ | Incomplete reporting and discrepancies in the reporting of infection meant that numbers of participants with ≥ 1 adverse events data could not be reported here |
| Adverse events ‐ symptomatic metal prominence Follow‐up: mean 28.5 weeks, range 16‐86 weeks | Study population | RR 0.11 (0.01 to 0.79) | 41 participants | ⊕⊝⊝⊝ | Metalwork prominence is a well‐known problem of tension band wiring. Symptoms were local discomfort or pain over the implant. There was no record of implant removal surgery in either group | |
| 421 per 1000 | 46 per 1000 | |||||
| Adverse events ‐ delayed or non‐union Follow‐up: 6 months | Study population | RR 0.17 [0.01 to 3.41] | 41 participants | ⊕⊝⊝⊝ | Surgical treated (debridement) infection preceded both cases in the tension band wiring group | |
| 106 per 1000 | 18 per 1000 | |||||
| Adverse events ‐ heterotopic ossification (bone formation) Follow‐up: mean 28.5 weeks, range 16‐86 weeks | Study population | RR 0.29 [0.01 to 6.72] | 41 participants | ⊕⊝⊝⊝ | The single participant with heterotopic ossification in the tension band wiring group developed ulnar neuropathy | |
| 53 per 1000 | 16 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1. The basis of the assumed risk is that for control group (tension band wiring) in the study population. 2. The evidence was downgraded 2 levels for limitations in design and implementation (including lack of blinding and spread of timing of outcome measurement) and 1 level for indirectness (the Herm criteria were not validated and could be considered surrogate to functional outcome). 3. The evidence was downgraded 2 levels for limitations in design and implementation (including lack of blinding and spread of timing of outcome measurement) and 1 level for imprecision. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Good clinical outcome (little pain or loss of elbow motion: Helm criteria) 16‐86 weeks follow‐up Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Metal prominence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Delayed or non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Heterotopic ossification | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Functional assessment (Modified Murphy Scoring System) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Murphy score (including function, pain, loss of movement, joint space): excellent or good result Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Hardware prominence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Loss in flexion > 20° Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Good clinical outcome: objective clinical improvement 6‐24 months follow‐up Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Subjective assessment: move elbow freely without pain, same use as other elbow | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Objective assessment: good functional movement and stable elbow | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Painless elbow joint Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Normal range of movement Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Adverse events (4‐54 weeks follow‐up) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Metalwork removed (all reasons, including 'routine') | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Metalwork removed because of symptoms (pin/cerclage affecting skin; pain) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Superficial infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Intraoperative complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mayo Elbow Performance Score 12‐36 months follow‐up Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Postoperative complications Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Operation time and blood loss Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Operation time (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Intraoperative blood loss (mL) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Disabilities of the Arm, Shoulder and Hand Score (DASH) (0‐100: 100 = worst outcome) at 2‐5 years Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Mayo Elbow Performance Score (0‐100: 100 = best outcome) at 2‐5 years Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Any adverse event | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Superficial infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Range of elbow motion Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Flexion (°) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Extension (°) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Pronation (°) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Supination (°) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Participant dissatisfaction Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |

