心血管系疾患の一次予防に対する「地中海様式」の食事について
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT of parallel group design. | |
| Participants | Postmenopausal women recruited from a health clinic in Iran. Inclusion criteria: women had at least primary education, were postmenopausal (no menstruation for at least 12 months) and CVD free (by self report). 76 women randomised, 38 in the intervention group (mean age (SD) 51.4 years (4.9)), and 38 to the control group (mean age 51.6 years (5.7)). | |
| Interventions | Dietary education to increase consumption of fruits and vegetables and whole grains, to eat fish twice a week and limit saturated fat and salt. The intervention comprised 5 educational sessions (2 face‐to‐face and 3 lecture discussion classes with slide demonstrations) in the first month, a further face‐to‐face session at month 3 and telephone calls each month to remind women to remain on the diet. Information was also provided about CVD and the menopause as well as diet. The intervention period was 6 months, with follow‐up at 6 months. The comparison group received no intervention. | |
| Outcomes | Total cholesterol, LDL‐cholesterol, HDL‐cholesterol, triglycerides, SBP and DBP. | |
| Notes | Differential loss to follow‐up in the control group of greater than 20% so sensitivity analyses were performed to examine the effect of excluding this study on the overall effect estimates for lipid levels and blood pressure. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | High risk | Differential loss to follow‐up of 7.9% in the intervention group compared with 23.7% in the control group. Participants in the intervention group did not attend education sessions, reasons were not given for losses to follow‐up in the control group. |
| Selective reporting (reporting bias) | Low risk | Report all outcomes as stated. |
| Other bias | Unclear risk | Insufficient information to judge. |
| Methods | RCT of parallel group design. | |
| Participants | Healthy postmenopausal female volunteers aged 44‐71 years recruited by press campaign from Palermo (Southern Italy). Inclusion criteria: postmenopausal for at least 2 years, no history of bilateral ovariectomy, no HRT within the previous year, no history of cancer, no adherence to a vegetarian or macrobiotic diet, no treatment for diabetes, thyroid disease or chronic bowel disease. 230 fulfilled these eligibility criteria and 115 women were enrolled in the study based on serum testosterone levels equal to or greater than the median population level (0.14 μg/mL). 58 women were randomised to the intervention group, 55 women to the control group. | |
| Interventions | MEDIET project ‐ the intervention group were invited to a weekly cooking course and to a social dinner with chefs addressing the principles of the traditional Mediterranean diet. The proposed recipes were based on a traditional Sicilian diet including whole cereals, legumes, seeds, fish, fruits, vegetables, olive oil and red wine. Women were asked to avoid refined carbohydrates, salt and additional animal fat. The intervention ran for 6 months from January to June 2000, then from 3 months from October to December 2000. Women were instructed to consume the same foods on a daily basis at home. The comparison group followed their usual diet. The follow‐up period was at 6 and 12 months. | |
| Outcomes | Plasma cholesterol. | |
| Notes | The primary publication (Castagnetta 2002) stated that the comparison group was advised to increase the consumption of fruits and vegetables as recommended by the WHO. However, other reports of the study stated that women in the control group followed their usual diets (Carruba 2006, secondary reference for this study). No data were provided on cholesterol levels in the paper but simply a statement that they had reduced. We have contacted the authors several times to request the data to include in our analyses but, unfortunately, to date this has not been forthcoming. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Block randomisation stratified for baseline parameters. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Unclear risk | No ITT analysis, < 20% loss to follow‐up in both groups but no reasons provided. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge. |
| Other bias | Unclear risk | Insufficient information to judge. |
| Methods | RCT of parallel group design. | |
| Participants | Healthy non‐obese women aged 25‐65 years recruited from adverts in community newsletters, health fairs, flyers and employee newsletters in Michigan, US. Women completed 7‐day food diaries. Eligibility criteria: fat intake was at least 23% of calories with no more than 48% from MUFA and fruit and vegetable intake was < 5.5 servings per day. This was to reflect a typical American intake. Women had to have good general health, be current non‐smokers and be in the normal to overweight range (BMI 18‐30). Exclusion criteria: chronic diseases such as diabetes, autoimmune disease, hypertension, being on medically prescribed diets, taking dietary supplements > 150% RDA, pregnant or lactating and being treated with therapies or supplements that could obscure the results. 69 women were randomised, mean age 44 years (range 25‐59) and mean BMI 24 (19‐30). | |
| Interventions | The intervention was a Greek Mediterranean exchange list diet with exchange goals determined by dieticians at baseline and focused on increasing fruit and vegetable intake and variety and increasing MUFA intake while maintaining the baseline energy intake and total fat intake. The fruit and vegetable goal was 7‐9 servings/day depending on baseline calorie intake and maintaining baseline energy intake was achieved by substituting fruit and vegetables for other carbohydrates. Variety was achieved using exchange lists. The fat intake goal was PUFA:SFA:MUFA ratio of 1:2:5. This was achieved by reducing usual fat intakes by half using low‐fat food and then adding in olive oil or other high MUFA to the diet to keep energy and total fat intake at baseline levels. Participants were given 3 L of extra‐virgin olive oil at baseline and at 3 months. 7‐day food records were taken at baseline, 3 months and 6 months. Counselling by the dieticians occurred weekly by telephone for the first 3 months and twice weekly thereafter. Face‐to‐face counselling occurred at baseline and 3 months. The intervention period was 6 months. Women were counselled on home eating patterns, restaurant eating, eating at work and special occasions. The comparison group followed their usual diets. They did not receive counselling, but were given the National Cancer Institutes Action guide to healthy eating and written materials on nutritional deficiencies if below 67% RDA. Follow‐up was at 6 months after the end of the intervention period. | |
| Outcomes | Total cholesterol, LDL‐cholesterol, HDL‐cholesterol and triacylglycerol. | |
| Notes | Differential loss to follow‐up in the intervention group of > 20% so sensitivity analyses were performed to examine the effect of excluding this study on the overall effect estimates for lipid levels. Body weight increased by 0.24 kg in the control group and decreased by 1.21 kg in the intervention group after the 6‐month intervention period. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not stated. Subjects stratified by race and menopausal status prior to randomisation using a block design of 6. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | High risk | Differential loss to follow‐up of 23% in the intervention group compared with 3% in the control group. No reasons for loss to follow‐up reported. |
| Selective reporting (reporting bias) | Low risk | Report all outcomes as stated. |
| Other bias | Unclear risk | Insufficient information to judge. |
| Methods | RCT of parallel group design. | |
| Participants | Participants were overweight or obese with untreated hypertension (SBP 130‐159 mmHg, DBP 85‐99 mmHg based on 4 screening visits) recruited from physician referrals, community screenings, mass media advertising in North Carolina, US. 144 participants randomised (46 to DASH alone, 49 to control), mean age was 52 years and 32.6% were men. | |
| Interventions | The DASH diet:
Participants in the intervention group received counselling on the DASH diet and provided feedback on their adherence in weekly group sessions. The goal of the sessions was to assist participants in learning how to buy and prepare appropriate foods, enhance their motivation to choose to eat these foods and to overcome any obstacles. A nutritionalist made the recommendations and small group sessions were held weekly (30‐45 minutes each) at the research centre. Immediately after randomisation and before the counselling sessions participants entered a 2‐week controlled isocalorific feeding period to improve compliance with the DASH diet. The comparison group were asked to maintain their usual dietary and exercise habits. Follow‐up was at 4 months after the intervention period. | |
| Outcomes | Total, HDL‐cholesterol, LDL‐cholesterol, triglycerides, SBP, DBP. | |
| Notes | 2 intervention groups ‐ DASH alone and DASH plus weight management. The review looked at only at the DASH alone arm. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised in groups of 2‐5 participants using a computer program. |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes used so allocation was concealed. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Participants were provided their treatment group assignments in sealed envelopes, which suggests they were unblinded. However, blinding of participants and personnel for behavioural interventions is difficult and often not possible so we have not judged this as at high risk of bias. |
| Blinding of outcome assessment (detection bias) | Low risk | Staff members performing the assessments were unaware of group assignment. |
| Incomplete outcome data (attrition bias) | Low risk | Only 1 participant lost to follow‐up and ITT analysis used. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported. |
| Other bias | Unclear risk | Insufficient information to judge. |
| Methods | RCT of parallel group design. | |
| Participants | Men and women were recruited from June 2001 to January 2004 among those attending the outpatient department of the Division of Metabolic Diseases at the Second University of Naples, Naples, Italy. 180 adults (99 men and 81 women), mean age 44.3 years (intervention diet) and 43.5 years (control diet) with metabolic syndrome were enrolled in the study. Inclusion criteria: ≥ 3 of the following: (1) abdominal adiposity (defined as waist circumference 102 cm (men) or 88 cm (women)); (2) low levels of serum HDL‐cholesterol (40 mg/dL (men) or 50 mg/dL (women)); (3) hypertriglyceridaemia (triglycerides level of ≥ 150 mg/dL); (4) elevated blood pressure (≥ 130/85 mmHg); and (5) impaired glucose homeostasis (fasting plasma glucose concentration ≥ 110 mg/dL). Exclusion criteria: CVD, psychiatric problems, a history of alcohol abuse (alcohol consumption 500 g/week in the last year), if they smoked, or if they took any medication. | |
| Interventions | Intervention diet: 90 participants were given detailed advice about the usefulness of a Mediterranean‐style diet. Through a series of monthly small‐group sessions, participants received education in reducing dietary calories (if needed), personal goal‐setting and self monitoring using food diaries. Behavioural and psychological counselling was also offered. Dietary advice was tailored to each participant on the basis of 3‐day food records. The recommended composition of the dietary regimen was carbohydrates, 50‐60%; proteins, 15‐20%; total fat, < 30%; saturated fat, < 10%; and cholesterol consumption, < 300 mg/day. Participants were advised to consume at least 250‐300 g of fruits, 125‐150 g of vegetables, 25‐50 g of walnuts, 400 g of whole grains (legumes, rice, maize and wheat) daily and to increase their consumption of olive oil. Participants were in the programme for 24 months and had monthly sessions with the nutritionist for the first year and twice monthly sessions for the second year. Compliance with the programme was assessed by attendance at the meetings and completion of diet diaries. Control diet: 90 participants were given general oral and written information about healthy food choices at baseline and at subsequent visits. The general recommendation for macro‐nutrient composition of the diet was similar to that for the intervention group (carbohydrates, 50‐60%; proteins, 15‐20% and total fat, 30%). Participants had bimonthly sessions with study personnel. Participants in both groups also received guidance on increasing their level of physical activity, mainly by walking for a minimum of 30 minutes/day but also by swimming or playing aerobic ball games. Trial was conducted from June 2001 to January 2004. Follow‐up period was 2 years. | |
| Outcomes | Total cholesterol, HDL‐cholesterol, triglycerides, SBP, SBP. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number sequence. |
| Allocation concealment (selection bias) | Low risk | Stored in sealed study folders and held in a central, secured location until informed consent obtained. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Staff members involved in the intervention had to be aware of the group assignment; thus, the study was only partly blinded. Blinding of participants and personnel for behavioural interventions is difficult and often not possible, so we have not judged this as at high risk of bias. |
| Blinding of outcome assessment (detection bias) | Low risk | Laboratory staff did not know to which group the participants were assigned. |
| Incomplete outcome data (attrition bias) | Low risk | ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported. |
| Other bias | Unclear risk | Insufficient information to judge. |
| Methods | RCT cross‐over design (analysed as a parallel group, 12‐week intervention, 12‐week follow‐up). | |
| Participants | Hypercholesterolaemic men, 35‐64 years of age were screened from the clients of the occupational health service of 5 industrial plants and government offices in Turku in southwestern Finland. 120 men were enrolled. Inclusion criteria: a fasting serum cholesterol concentration 232‐309 mg/dL (6.0‐8.0 mmol/L) and fasting serum triglyceride concentration no higher than 266 mg/dL (3.0 mmol/L). Exclusion criteria: BMI > 32 kg/m2; coronary artery disease; cerebrovascular disease; claudication and pharmacologically treated hypertension, hyperlipidaemia, or diabetes. | |
| Interventions | Men included in the study entered first a 4‐ to 6‐week open placebo run‐in period, at the end of which they were randomly allocated to the intervention (60 men, mean age 48.0 years) or control group (60 men, mean age 48.4 years). The intervention (a weight stable, modified, Mediterranean‐type diet) consisted of no more than 10% energy from SFAa and transunsaturated fatty acids; cholesterol intake no more than 250 mg/day; omega‐3 fatty acid intake of plant origin (linolenic acid) and marine origin of at least 4 g/day and the ratio of omega‐6/omega‐3 PUFAs < 4; and increased intakes of fruits, vegetables and soluble fibre. Men were advised to use leaner meat products, low‐fat cheese, skimmed milk, fat‐free sour milk and low‐fat yogurt. Fish was recommended as a main meal once or twice a week. Rapeseed margarine was recommended as a replacement for butter, a mixture of butter and vegetable oils, and sunflower margarine. Rapeseed margarine and oil, oat bran (20 g/day), and frozen berries (blueberry, lingonberry or blackcurrant at 50 g/day) were supplied free to study subjects. The diet was supervised by a nutritionist in 1 individual session and in 2 group counselling sessions at the beginning of the treatment and in 5 subsequent monthly group brush‐up sessions during the dietary treatment. The control group participants (habitual diet group) were advised to continue eating their usual diet during the study period. The trial was conducted between August 1997 and June 1998. | |
| Outcomes | Total cholesterol, HDL‐cholesterol, LDL‐cholesterol, triglycerides. | |
| Notes | Data were only used for the first 12 weeks of the trial (before the second randomisation and subsequent cross‐over). Follow‐up data (mean and SD) for each of the outcomes was missing. Authors were contacted 3 times for follow‐up data for all outcomes but with no success. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Dietary treatment was performed single‐blind. Blinding of participants and personnel for behavioural interventions is difficult and often not possible so we have not judged this as at high risk of bias. |
| Blinding of outcome assessment (detection bias) | Low risk | All measurements and analyses were done blinded to the treatment allocation of the subject. |
| Incomplete outcome data (attrition bias) | High risk | No reason given for attrition. |
| Selective reporting (reporting bias) | Unclear risk | Blood pressure not reported. |
| Other bias | Unclear risk | Insufficient information to judge. |
| Methods | RCT of parallel group design. | |
| Participants | From October 2007 to October 2008, 90 eligible community‐dwelling adults (26 men and 64 women, aged 20‐50 years) were recruited from primary care centres. They were considered healthy on the basis of a physical examination and routine biochemical and haematological laboratory determinations. Exclusion criteria: intake of antioxidant supplements; intake of acetosalicylic acid or any other drug with established antioxidative properties; high levels of physical activity (3000 kcal/week in leisure‐time physical activity); obesity (BMI 30 kg/m2); hypercholesterolaemia (total cholesterol 8.0 mM or dyslipidaemia therapy); diabetes (glucose 126 mg/dL or diabetes treatment); hypertension (SBP ≥ 140 mmHg) or (DBP ≥ 90 mmHg), or both or antihypertensive treatment; multiple allergies; coeliac or other intestinal diseases; any condition that could limit the mobility of the subject, making study visits impossible; life‐threatening illnesses or other diseases or conditions that could worsen adherence to the measurements or treatments; vegetarianism or a need for other special diets; and alcoholism or other drug addiction. | |
| Interventions | Participants were assigned to 1 of 2 interventions or a control group as follows: 1. Traditional Mediterranean diet with virgin olive oil (30 participants); 2. Traditional Mediterranean diet with washed virgin olive oil (30 participants). The dietician gave personalised advice during a 30‐minute session to each participant following the traditional Mediterranean diets, with recommendations on the desired frequency of intake of specific foods. Participants were instructed to use olive oil for cooking and dressing; increase consumption of fruit, vegetables and fish; consume white meat instead of red or processed meat; prepare homemade sauce with tomato, garlic, onion, aromatic herbs and olive oil to dress vegetables, pasta, rice, and other dishes; and, for alcohol drinkers, moderate consumption of red wine. 3. Control group (30 subjects): participants were advised by a dietician to maintain their habitual lifestyle. Intervention period and follow‐up was 3 months. | |
| Outcomes | Total cholesterol, HDL‐cholesterol, LDL‐cholesterol, triglycerides, SBP, DBP. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated random number sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | Only 1 participant dropped out of the trial. |
| Selective reporting (reporting bias) | Unclear risk | Not stated. |
| Other bias | Unclear risk | Not stated. |
| Methods | RCT of parallel group design. | |
| Participants | The Polyp Prevention Trial ‐ a multicentre trial (8 US clinical centres) to examine the effect of diet on recurrence of adenomatous polyps in the large bowel. Participants were at high risk with ≥ 1 colorectal adenomas removed within 6 months before recruitment. Referrals were from endoscopists and recruitment took place between 1991 and 1994. 2079 participants were randomised, 64.5% men, mean age 61 years. | |
| Interventions | Intensive counselling to follow a low‐fat (< 20% calories), high‐fibre (18 g/1000 cal) diet and to increase fruit and vegetable consumption to 3.5 servings/1000 cal. Nutritional education and behavioural modification techniques used by a registered dietician. In the first year, counselling sessions were weekly for the first 6 weeks, biweekly for the next 6 weeks and monthly thereafter. In year 2, counselling sessions were in groups every 2 months and participants were also contacted by telephone at least once a month. In years 3 and 4, counselling sessions were held quarterly in groups. More than 50 hours of counselling sessions over 4 years. Comparison group were given a standard brochure on healthy eating. Follow‐up at 4 years. | |
| Outcomes | Plasma cholesterol in mmoles/litre | |
| Notes | Plasma cholesterol only measured in a subgroup of participants, n = 370 and n = 374 for the intervention and control groups, respectively. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | ITT analysis used and loses to follow‐up reported. |
| Selective reporting (reporting bias) | Low risk | All outcomes stated are reported. |
| Other bias | Unclear risk | Insufficient information to judge. |
| Methods | RCT of parallel group design (2 x 2 factorial design). | |
| Participants | 219 older men with long‐standing hypercholesterolaemia were recruited from the Diet and Omega‐3 Intervention trial on atherosclerosis (DOIT) study, Norway. Mean age 69.7 years for both genotypes. | |
| Interventions | Men were randomised into 3 intervention groups or the control group as follows:
Diet counselling was given individually by a clinical nutritionist based on a food frequency questionnaire. The food frequency questionnaire was also answered by the participants at the end of the main study (36 months). Energy content and nutrient composition was of the diet were calculated from the questionnaires at baseline and 36 months. Dietary advice was given during 30‐45 minutes at time of randomisation, and for 30 minutes after 3 months. Participants were supported with a margarine rich in PUFA and vegetable oils free of cost. Advice was given to increase intake of vegetables, fruit and fish, and decrease consumption of meat and target energy percents at 27‐30% fat, 15‐18% protein and 50‐55% carbohydrate. To fulfil these goals participants were recommended to use rapeseed or olive oil for cooking; use leafy vegetables daily; include fruits, berries and nuts in the diet; eat fish 3 times per week; use wholemeal bread, skimmed milk and reduced‐fat cheese. 2 capsules were taken twice daily corresponding to 2.4 g VLC n‐3 capsules or 2.4 g corn oil (placebo capsules). Follow‐up period was 6 months. | |
| Outcomes | Triglycerides. | |
| Notes | Only data from the usual care and placebo capsules (control group) (n = 51) and dietary advice ('Mediterranean type' diet) and placebo capsules (n = 47). (The focus of the study was to investigate the effect of long‐term diet and VLC n‐3 fatty acids intervention on plasma coagulation factor VII (FVII), choline‐containing phospholipids and triglycerides, especially relating to the R353Q polymorphism of the FVII gene). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient reporting of attrition/exclusions. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge. |
| Other bias | Unclear risk | Insufficient information to judge. |
| Methods | RCT of parallel group design. | |
| Participants | Participants were adults with mild to moderate hypercholesterolaemia with serum cholesterol levels above 5.2 mmol/L, not current or previous (within 3 months) users of lipid‐lowering medication and with no serious illness. Participants were recruited from dietetic clinics, hospital physicians and general practitioners in London and the South East, UK. 117 participants were randomised, mean age 53.5 years, 43.5% men. | |
| Interventions | The intervention (Mediterranean diet) was delivered in 8 sessions during the 12‐week intervention period using a combination of individual and group sessions with a dietician and psychologist. Dietary advice was to increase intake of fruit and vegetables, and oily fish and to reduce fat to 30% of energy with substitution of predominantly monosaturated fat for saturated fat. All participants received individualised advice to implement dietary changes based on their lifestyle and food preferences and group support in maintaining changes. Intervention participants were also given free spreading fats and oils high in monosaturated fats. The comparison group was a wait‐list control. Participants were told it was necessary to wait for treatment but that they would be seen at 6‐week intervals. They were not given any specific dietary advice but were not discouraged from making changes and some participants did so. 12 weeks' follow‐up. | |
| Outcomes | Total cholesterol, LDL‐cholesterol, HDL‐cholesterol, triglycerides. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Low risk | Opaque sealed envelopes. |
| Blinding of participants and personnel (performance bias) | Unclear risk | No details provided but the control group was a wait‐list control. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Outcome assessment done by a member of the research team who was blinded (in most cases). |
| Incomplete outcome data (attrition bias) | Low risk | No ITT but details of attrition provided and reasons. |
| Selective reporting (reporting bias) | Low risk | All of the outcomes stated were reported. |
| Other bias | Unclear risk | Insufficient information to judge. |
| Methods | RCT of parallel group design. | |
| Participants | 48,835 postmenopausal women aged 50‐79 years were recruited and enrolled between 1993 and 1998 at 40 clinical centres across the US. Eligibility criteria: being postmenopausal and consuming at baseline a diet with fat intake of 32% or more of total calories, as assessed by a food frequency questionnaire. Exclusion criteria: history of breast cancer or colorectal cancer, any cancer within the previous 10 years except non‐melanoma skin cancer, medical conditions with a predicted survival of less than 3 years, adherence or retention concerns, current dietary intake of less than 32% of energy from fat, and type 1 diabetes mellitus. | |
| Interventions | Women were randomly assigned to a usual‐diet comparison group (n = 29,294, 60.0%) or an intervention group with a 20% low‐fat dietary pattern with increased vegetables, fruits and grains (n = 19,541, 40.0%). The intervention was designed to promote dietary change with the goals of reducing intake of total fat to 20% of energy intake (in kilocalories) by increasing intake of vegetables and fruits to at least 5 servings daily and of grains to at least 6 servings daily. The intervention did not include total energy reduction or weight loss goals. Although not a separate focus of the intervention, it was presumed that by reducing total fat intake to 20% kcal, intake of saturated fat would also be reduced (7% energy intake). The intensive behavioural modification programme involved 18 group sessions in the first year and quarterly maintenance sessions thereafter, led by specially trained and certified nutritionists. Participants self monitored total fat‐gram intake and also servings of vegetables, fruits and grains. Women in the comparison group received a copy of the Dietary Guidelines for Americans as well as other health‐related materials, but had no contact with the nutrition interventionists. Mean follow‐up time for the WHI DMT was 8.1 years. | |
| Outcomes | CVD mortality, myocardial infarction and stroke (at 8.1 years); total cholesterol, HDL‐cholesterol and LDL‐cholesterol (at year 3); triglycerides (at year 3); SBP and DBP (at years 1 and 3); type 2 diabetes (at 8.1 years). | |
| Notes | Blood measures (total, HDL‐cholesterol, LDL‐cholesterol and triglycerides) were performed on a 5.8% subsample at year 3. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a randomised permuted block algorithm. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) | Low risk | Carried out by physician adjudicators not involved in trial. |
| Incomplete outcome data (attrition bias) | Low risk | ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Unclear risk | Insufficient information to judge. |
BMI: body mass index; CVD: cardiovascular disease; DASH: ; DBP: diastolic blood pressure; HDL: high‐density lipoprotein; HRT: hormone replacement therapy; ITT: intention to treat; LDL: low‐density lipoprotein; MUFA: monounsaturated fatty acid; PUFA: polyunsaturated fatty acid; RCT: randomised controlled trial; RDA: recommended daily allowance; SBP: systolic blood pressure; SD: standard deviation; SFA: saturated fatty acid; VLC: very‐long‐chain; WHO: World Health Organization.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Not an RCT ‐ control group were a separate population. | |
| PREDIMED study. Low‐fat diet arm had face‐to‐face nutritional advice as well as leaflets, therefore, not a minimal control. | |
| Substudy of PREDIMED. Control group received face‐to‐face nutritional advice, therefore, not a minimal control, and there were no relevant outcomes. | |
| Not all subjects were randomised. | |
| Not an RCT. | |
| Medi‐RIVAGE study. Control group was given dietary advice to eat fruit and vegetables, therefore, not a minimal control. |
RCT: randomised controlled trial.
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | RCT of parallel group design |
| Participants | 219 participants with metabolic syndrome (NCEP‐ATPIII criteria). |
| Interventions | 4 intervention groups: to follow a Mediterranean diet, a low GI Mediterranean diet, low GI diet and a generic diet (comparison group). Follow‐up after the 12‐week intervention period. |
| Outcomes | Lipid levels, blood pressure |
| Notes | Conference abstract. Contacted authors for further details of the trial and outcome data. Authors are currently trying to publish a paper and are unwilling at present to share their data with us. |
GI: glycaemic index; NCEP‐ATPIII: National Cholesterol Education Program‐ Adult Treatment Panel III; RCT: randomised controlled trial.
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Cardiovascular risk REduction Study: Supported by an Integrated Dietary Approach |
| Methods | Randomised parallel design single‐centre controlled trial |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions | This is a controlled dietary intervention trial comparing a cardioprotective diet (decreased salt and saturated fatty acid intake, and increased whole grain cereals, fruit and vegetables and oily fish intake) with a control diet (average UK diet) for 3 months. |
| Outcomes | Primary outcome measures:
Secondary outcome measures:
|
| Starting date | 16 July 2010 |
| Contact information | Prof Thomas Sanders Nutritional Science Division London SE1 9NH UK +44 (0)20 7848 4273 +44 (0)20 7848 4171 |
| Notes | Ongoing trial (ISRCTN92382106) that has been classified as 'completed' on www.controlled‐trials.com Trial website: www.medscinet.net/CRESSIDA/ Study duration: July 2010 to December 2012 |
NICE: national Institute for Health and Clinical Excellence.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total cholesterol (mmol/L), change from baseline Show forest plot | 8 | 4151 | Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.26, ‐0.06] |
| Analysis 1.1 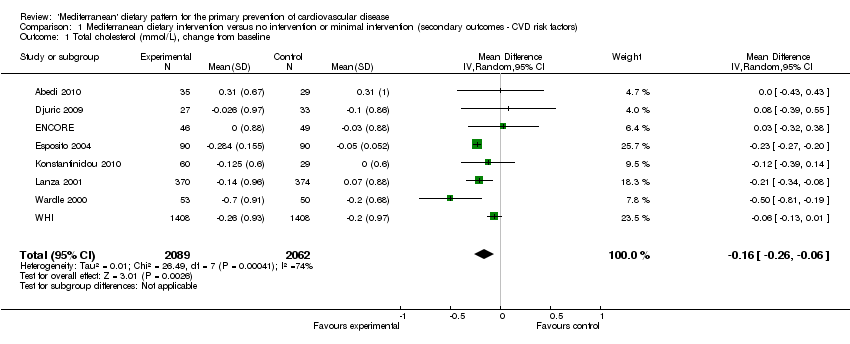 Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 1 Total cholesterol (mmol/L), change from baseline. | ||||
| 2 Total cholesterol (mmol/L), change from baseline, subgroup analysis Show forest plot | 8 | 3815 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.23, ‐0.17] |
| Analysis 1.2  Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 2 Total cholesterol (mmol/L), change from baseline, subgroup analysis. | ||||
| 2.1 Interventions described as Mediterranean diet (or comprise both increased fruit and vegetables and monounsaturated fatty acids) | 4 | 436 | Mean Difference (IV, Fixed, 95% CI) | ‐0.23 [‐0.27, ‐0.20] |
| 2.2 Interventions with 2 components but not described as Mediterranean diet or comprising both increased fruit and vegetables and monounsaturated fatty acids | 4 | 3379 | Mean Difference (IV, Fixed, 95% CI) | ‐0.06 [‐0.13, 0.01] |
| 3 LDL‐cholesterol (mmol/L), change from baseline Show forest plot | 6 | 3227 | Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐0.13, ‐0.01] |
| Analysis 1.3  Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 3 LDL‐cholesterol (mmol/L), change from baseline. | ||||
| 4 LDL‐cholesterol (mmol/L), change from baseline, subgroup analysis Show forest plot | 6 | 3227 | Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.17, 0.03] |
| Analysis 1.4 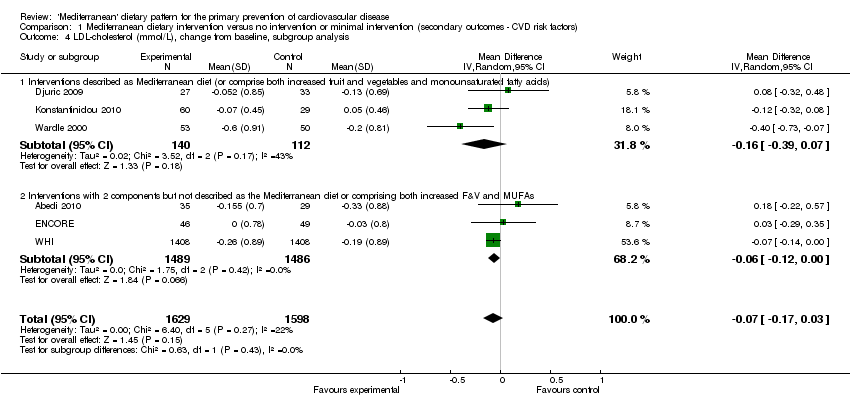 Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 4 LDL‐cholesterol (mmol/L), change from baseline, subgroup analysis. | ||||
| 4.1 Interventions described as Mediterranean diet (or comprise both increased fruit and vegetables and monounsaturated fatty acids) | 3 | 252 | Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.39, 0.07] |
| 4.2 Interventions with 2 components but not described as the Mediterranean diet or comprising both increased F&V and MUFAs | 3 | 2975 | Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.12, 0.00] |
| 5 HDL‐cholesterol (mmol/L), change from baseline Show forest plot | 7 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.5 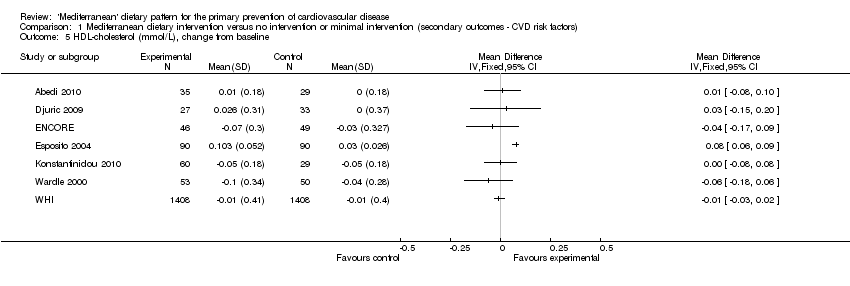 Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 5 HDL‐cholesterol (mmol/L), change from baseline. | ||||
| 6 Triglycerides (mmol/L), change from baseline Show forest plot | 6 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.6  Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 6 Triglycerides (mmol/L), change from baseline. | ||||
| 7 Systolic blood pressure (mmHg), change from baseline Show forest plot | 5 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.7 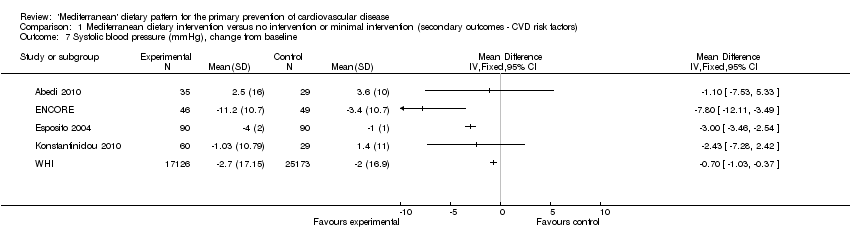 Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 7 Systolic blood pressure (mmHg), change from baseline. | ||||
| 8 Diastolic blood pressure (mmHg), change from baseline Show forest plot | 5 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.8  Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 8 Diastolic blood pressure (mmHg), change from baseline. | ||||

Study flow diagram.
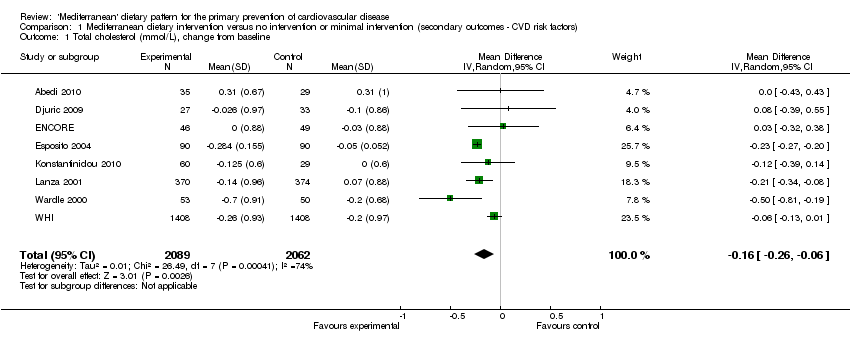
Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 1 Total cholesterol (mmol/L), change from baseline.
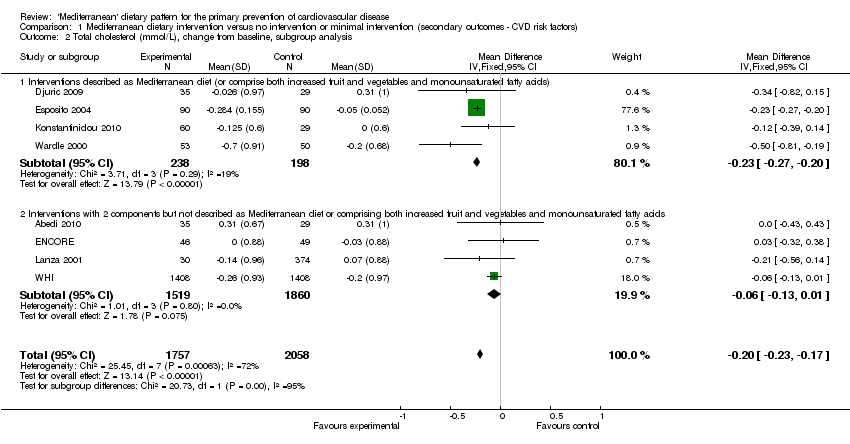
Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 2 Total cholesterol (mmol/L), change from baseline, subgroup analysis.

Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 3 LDL‐cholesterol (mmol/L), change from baseline.
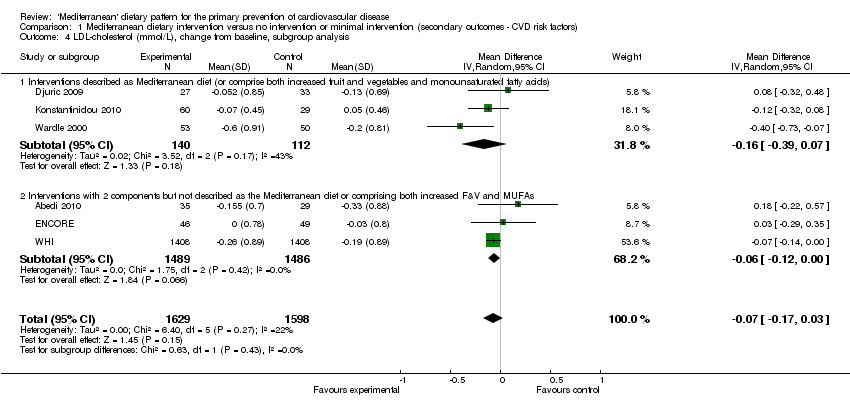
Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 4 LDL‐cholesterol (mmol/L), change from baseline, subgroup analysis.

Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 5 HDL‐cholesterol (mmol/L), change from baseline.

Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 6 Triglycerides (mmol/L), change from baseline.

Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 7 Systolic blood pressure (mmHg), change from baseline.

Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 8 Diastolic blood pressure (mmHg), change from baseline.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total cholesterol (mmol/L), change from baseline Show forest plot | 8 | 4151 | Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.26, ‐0.06] |
| 2 Total cholesterol (mmol/L), change from baseline, subgroup analysis Show forest plot | 8 | 3815 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.23, ‐0.17] |
| 2.1 Interventions described as Mediterranean diet (or comprise both increased fruit and vegetables and monounsaturated fatty acids) | 4 | 436 | Mean Difference (IV, Fixed, 95% CI) | ‐0.23 [‐0.27, ‐0.20] |
| 2.2 Interventions with 2 components but not described as Mediterranean diet or comprising both increased fruit and vegetables and monounsaturated fatty acids | 4 | 3379 | Mean Difference (IV, Fixed, 95% CI) | ‐0.06 [‐0.13, 0.01] |
| 3 LDL‐cholesterol (mmol/L), change from baseline Show forest plot | 6 | 3227 | Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐0.13, ‐0.01] |
| 4 LDL‐cholesterol (mmol/L), change from baseline, subgroup analysis Show forest plot | 6 | 3227 | Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.17, 0.03] |
| 4.1 Interventions described as Mediterranean diet (or comprise both increased fruit and vegetables and monounsaturated fatty acids) | 3 | 252 | Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.39, 0.07] |
| 4.2 Interventions with 2 components but not described as the Mediterranean diet or comprising both increased F&V and MUFAs | 3 | 2975 | Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.12, 0.00] |
| 5 HDL‐cholesterol (mmol/L), change from baseline Show forest plot | 7 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 Triglycerides (mmol/L), change from baseline Show forest plot | 6 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7 Systolic blood pressure (mmHg), change from baseline Show forest plot | 5 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8 Diastolic blood pressure (mmHg), change from baseline Show forest plot | 5 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |

