Hystéroscopie dans le traitement de l'hypofertilité liée à des anomalies majeures suspectées de la cavité utérine
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Parallel‐group, randomised, controlled, single‐centre trial Power calculation not reported Approved by the hospital's ethics committee No source of funding or conflict of interest reported | |
| Participants | Country: Italy Setting: AGUNCO Obstetrics and Gynecology Centre, Rome Population: women referred to the centre from January 1998 until April 2005 for fertility problems were examined for inclusion in the study. All women underwent routine examinations including the study of ovarian function (FSH, luteinising hormone, estradiol and progesterone concentrations); prolactin, free triiodothyronine, free thyroxine and thyroid‐stimulating hormone concentrations; post‐coital test; TVUS; hysterosalpingography; and analysis of the partner’s semen. The TVUS was performed in order to diagnose the presence of uterine fibroids. After these examinations all patients who were found to be affected by uterine fibroids excluding all other causes of infertility were asked to participate in the study. Type of subfertility: all women had been suffering from infertility for at least 1 year (range: 1 to 5 years); no further clarification on primary versus secondary subfertility Mean age: the mean age in the patients with submucous fibroids alone was 31.4 ± 2.5 years; the mean age in the patients with mixed submucous‐intramural fibroids was 32.2 ± 2.5 years N recruited = 193 women N participants = 181 women N participants with submucous fibroids only = 52 women N participants with mixed submucous‐intramural fibroids = 42 women Inclusion criteria: age ≤ 35 years; infertility for at least 1 year; presence of one knot and/or fibroid of diameter ≤ 40 mm and absence of other causes of infertility at the performed examinations Exclusion criteria: presence of 2 or more knots and/or fibroids of diameter > 40 mm; body weight > 20% of normal weight; and use of medication containing oestrogens, progestins or androgens within 8 weeks prior to the study Duration of the study: 86 months; the study was conducted from January 1998 until April 2005 | |
| Interventions | Two interventions were compared:
Patients were examined by TVUS 3 months after surgery for control. Patients who did not undergo surgery were asked to immediately start having regular fertility‐oriented intercourse (intercourse during the 6‐day fertile interval ending on the day of ovulation). Patients who underwent surgery were suggested to abstain from having sexual intercourse for 3 months and then to start having regular fertility‐oriented intercourse. Patients were monitored for up to 12 months after study commencement. | |
| Outcomes | A clinical pregnancy was defined by the visualisation of an embryo with cardiac activity at 6 to 7 weeks of pregnancy Miscarriage was classified as clinical loss of an intrauterine pregnancy between the 7th and 12th weeks of gestation | |
| Notes | The authors state that the differences in pregnancy rates between the comparison groups are statistically significant for the patients with submucous fibroids (P < 0.05), which is in contrast with the calculation of the results in RevMan. The definition of knot is unclear: it could not be clarified since we failed to contact the study authors. It is not clear whether a hysteroscopy was done in all women to confirm the exact position of the ultrasonically detected fibroids. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Subsequently, women of each group were randomized into two subgroups, according to a randomisation table" Comment: low risk of selection bias related to random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Method not stated: no further clarification obtained from the study authors Comment: unclear risk of selection bias related to allocation concealment |
| Blinding of participants and personnel (performance bias) | Unclear risk | Method not stated: no further clarification obtained from the study authors Comment: unclear risk of performance bias |
| Blinding of outcome assessment (detection bias) | Unclear risk | Method not stated: no further clarification obtained from the study authors Comment: unclear risk of detection bias |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "One hundred and ninety‐three patients were diagnosed as affected by uterine fibroid excluding all other causes of infertility and met the requirements of the inclusion and exclusion criteria. Of these, 181 decided to participate in the study. Among the 181 patients, 52 had submucosal fibroids (SM group) while 45 had intramural fibroids (IM group), 11 had subserosal fibroids (SS group), 42 had a mix of submucosal–intramural (SM‐IM group) and 31 patients had a mix of intramural–subserosal fibroids (IM‐SS group)". Quote: "Out of 181 women, 68 become pregnant" Comment: low risk for attrition bias |
| Selective reporting (reporting bias) | High risk | The published report fails to include results for the live birth rate, which is the primary outcome of interest that would be expected to have been reported for a trial on fertility treatment conducted over a 7‐year period. |
| Other bias | Unclear risk | The mean ages and duration of infertility in the intervention and control group of women with submucous fibroids are not reported. No further clarification by the authors was obtained. It is unclear whether there might have been imbalance in the baseline characteristics between the comparison groups. Failure to do a hysteroscopy in all women to confirm the position of the ultrasonically detected fibroids could have caused information bias. |
| Methods | Parallel‐group, randomised, controlled, single‐centre trial A power analysis was performed. To detect an expected difference in pregnancy rate between the intervention and control group of 15% at a level of 0.05 with a power of 80%, a sample size of 200 women (i.e. 100 women per group) was required. From 2800 women attending the centre, 452 women fulfilling the inclusion criteria were selected; 215 women were randomised (107 women in the intervention group and 108 women in the control group). Data on outcomes of 204 women were available for analysis (101 in the intervention group and 103 in the control group). This study had therefore adequate statistical power to detect a difference between the comparison groups if really present. Approved by the hospital's ethics committee No source of funding or conflict of interest reported | |
| Participants | Country: Spain Setting: infertility unit of an university tertiary hospital in the Spanish capital Madrid Population: women with unexplained, male or female factor infertility for at least 24 months bound to undergo intrauterine insemination with a sonographic diagnosis of endometrial polyps Unexplained infertility was diagnosed in patients with normal ovulatory cycles, semen analysis, HSG and postcoital testing. Male factor infertility was diagnosed if 2 semen analyses obtained at least 1 month apart were subnormal according to the WHO criteria. Female factor infertility was diagnosed in patients with ovulatory dysfunction, cervical factor or endometriosis. Type of subfertility: primary subfertility (correspondence with the study authors) Mean age: treatment group = 30.8 years (26.7 to 34.9), control group = 30.9 years (26.5 to 35.3) N recruited = 452 women N randomised = 215 women Inclusion criteria: women with at least 24 months of subfertility with a sonographic diagnosis of endometrial polyps bound to undergo intrauterine insemination for unexplained, male or female factor infertility Duration of the study: 50 months; the study was conducted from January 2000 to February 2004 | |
| Interventions | One surgeon (the first author of the study TP‐M) performed all hysteroscopic procedures by intention in an outpatient office setting under local anaesthesia Two interventions were compared:
Duration: women were scheduled to receive 4 cycles of IUI with subcutaneous injection of recombinant FSH 50 IU daily from the third day, and the first IUI was planned for 3 cycles after hysteroscopy in both groups. 4 IUI cycles were attempted before finishing the trial. | |
| Outcomes | Primary: Quote: "We studied the crude pregnancy rate in both groups" Comment: clinical pregnancy; crude pregnancy was defined by the study authors as follows: "the presence of a gestational sac on ultrasound" (correspondence with the study authors) | |
| Notes | 1. Quote: "Patients underwent a complete infertility evaluation that included TVUS in the early proliferative phase, basal body temperature recording to assess ovulation, postcoital test (PCT), HSG, semen analysis and, in some patients, diagnostic laparoscopy" Comment: according to correspondence with the first author, the aim of the laparoscopy was exclusively diagnostic in the evaluation of cases of unexplained infertility of unknown origin. If tubal pathology was detected by laparoscopy, the patient was excluded from randomisation. The numbers of women undergoing a laparoscopy were balanced between the 2 comparison groups. 2. In this study IUI was performed for various indications: male factor (21%), cervical factor (11%), endometriosis (11%), or unexplained subfertility (49%) and ovulation disorder (33%). Anovulation is reported in the methods section as an exclusion criterion. The study authors defined ovulation disorder as follows: Quote: "A combination of irregular menstrual cycles with multicystic ovaries on TVUS and basal gonadotrophin measurements within the normal range" (correspondence with the first study author). Comment: In everyday clinical practice ovulation disorder is not an indication for IUI by itself. 3. Data on the number or the localisation of the polyps could not be retrieved since the first author no longer works in the university hospital. 4. Data on the size of the polyps in the control group could not be obtained for similar reasons as footnote 3. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomised to one of the two groups with use of an opaque envelope technique, with assignment determined by a computerized random number table" Quote: "Subjects were randomised into one of two groups in a 1:1 ratio using a restricted randomisation" Comment: probably done, but using simple randomisation, with an equal allocation ratio, by referring to a table of random numbers generated by a computer |
| Allocation concealment (selection bias) | Low risk | Quote: "Patients were randomised to one of the two groups with use of an opaque envelope technique, with assignment determined by a computerized random number table". Comment: sequentially numbered, opaque, sealed envelopes were used according to correspondence with the first author; probably done |
| Blinding of participants and personnel (performance bias) | Unclear risk | Method not stated: no further clarification obtained from the study authors Comment: unclear risk of performance bias |
| Blinding of outcome assessment (detection bias) | Unclear risk | Method not stated: no further clarification obtained from the study authors Comment: unclear risk of detection bias |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "11 patients were lost from the study, 6 in the study group (3 lost to follow‐up, 2 pathologic reports of submucosal myoma and 1 in whom the polyp was not confirmed) and 5 in the control group (1 lost to follow‐up, 2 in whom the polyp was not confirmed and 2 pathologic reports of myoma)" Comment: missing outcome data are balanced in numbers across the comparison groups, with similar reasons for missing data across groups |
| Selective reporting (reporting bias) | High risk | Although the published report includes results on all the outcomes specified in the methods section, it nevertheless fails to include results for the live birth rate, which is the primary outcome of interest that would be expected to have been reported for a trial on fertility treatment conducted over a 4‐year period. Data on the outcomes live birth and miscarriage were not available since most the majority of randomised women were referred by gynaecologists from outside the tertiary university hospital and were referred back when pregnant for further follow‐up by the referring gynaecologist. No clarification could be obtained for the lack of data on hysteroscopic complications. |
| Other bias | Low risk | No evidence for imbalance in the baseline characteristics |
FSH: follicle‐stimulating hormone
HSG: hysterosalpingography
IU: international units
IUI: intrauterine insemination
TVUS: transvaginal ultrasound
WHO: World Health Organization
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing intrauterine balloon stenting versus no stenting following hysteroscopic treatment for septate uterus. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial studying the efficacy of hyaluronic acid gel in preventing the development of intrauterine adhesions following hysteroscopic adhesiolysis. Mixed population of women with intrauterine adhesions, presenting with subfertility or other gynaecological complaints. Primary outcome: adhesion scores. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing hysteroscopy prior to a subsequent IVF attempt versus immediate IVF without prior hysteroscopy conducted in patients with 2 or more failed IVF cycles with unsuspected or no uterine cavity abnormalities. Main outcomes: biochemical pregnancy, clinical pregnancy and delivery rates. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial in subfertile women comparing the application of amnion graft, either fresh or dried to an intrauterine balloon versus the application of an intrauterine balloon without amnion graft as an adjunctive procedure after the hysteroscopic lysis of severe intrauterine adhesions, diagnosed at office hysteroscopy in women with infertility with or without menstrual disorders as the primary symptom. Outcomes assessed were improvement in adhesion grade, improvement in menstruation, increased uterine length at sounding, complications and reproductive outcome. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing two different surgical techniques for metroplasty: operative hysteroscopy using the resectoscope with a unipolar knife versus the Versapoint device. Mixed population of women with septate uterus and a history of recurrent miscarriage or primary subfertility. Outcomes assessed were operative parameters, complications, need for a second intervention and reproductive outcome parameters. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing extended sectioning by resectoscopy versus sequential cold knife excision for treating a complete utero‐cervicovaginal septum in a mixed population of women suffering from infertility or pregnancy loss. Main outcome measures: operating time, perioperative bleeding, complications, reproductive outcome, and patient and husband satisfaction. | |
| Study on the effectiveness of hysteroscopic metroplasty for small septate uterus in women with repeated IVF implantation failure. Although denoted by the authors as the first prospective randomised controlled study on this subject, the trial did not use a valid random sequence generation. Quote: "These patients, once informed about the situation, were randomly allocated, depending on their personal decision ...". | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing the application of hyaluronan derivative gel (Hyalobarrier® gel) after hysteroscopic surgery versus surgical treatment alone in women aged 18 to 65 years, suffering from other gynaecological conditions than subfertility. Primary outcome: adhesion score at second look hysteroscopy. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised comparison between office hysteroscopy prior to a subsequent IVF attempt or immediate IVF without prior office hysteroscopy conducted in patients with 2 or more failed IVF cycles with unsuspected or no uterine cavity abnormalities. Outcome measures: number of oocytes retrieved, fertilisation rate, number of embryos transferred, first trimester miscarriage and clinical pregnancy rates. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing the use of Intercoat® absorbable adhesion barrier gel versus no adhesion barrier after hysteroscopic synechiolysis in a mixed population of women suffering from infertility or other gynaecological conditions. Primary outcome: incidence of de novo intrauterine adhesions, adhesion scores, patency of the internal uterine ostium. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing diagnostic hysteroscopy with directed biopsy and/or hysteroscopic treatment of unsuspected uterine cavity abnormalities versus no hysteroscopy in women with primary infertility treated with ICSI. Primary outcome: clinical pregnancy. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing hysteroscopy versus no hysteroscopy in women with recurrent implantation failure with IVF.Status: completed. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial aimed at assessing the role of using the office hysteroscopy as a routine investigation in improving ICSI pregnancy rates in two groups of infertile women with no abnormality detected on transvaginal ultrasonographic examination | |
| Not addressing the PICO research question of this Cochrane review. | |
| Observational non‐randomised study on the effectiveness of hysteroscopy in women with repeated implantation failure. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing hysteroscopic surgery for the removal of polyps, fibroids or septa followed by the application of auto‐cross linked hyaluronic acid gel versus hysteroscopic surgery without the adhesion barrier in a mixed population of women with subfertility and other gynaecological symptoms associated with endometrial polyps, submucous fibroids or septa. Main outcomes: rates of adhesion formation and adhesion scores. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing transcervical resection by hysteroscopy of endometrial polyps suspected on TVUS and SIS versus observation for 6 months. The study population included premenopausal women with bleeding problems associated with endometrial polyps. The aim of the trial was to study the clinical effectiveness of transcervical resection of endometrial polyps for the outcome periodic blood loss. Women wishing to become pregnant were excluded from the trial. Primary outcome: periodic blood loss measured by the Pictorial Blood Assessment Chart. | |
| Not addressing the research questions described in the protocol. Randomised trial comparing the efficacy of intrauterine balloon and intrauterine contraceptive device in the prevention of adhesion reformation following hysteroscopic adhesiolysis. | |
| Comparative non‐randomised study on the value of hysteroscopy prior to IVF/ICSI. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial in women aged 18 to 75 years comparing operative hysteroscopy using the monopolar resectoscope versus hysteroscopic bipolar electrode excision for the treatment of endometrial polyps. Outcomes: operating times, difficulty of the operation, surgeon satisfaction with the procedure, complications, postoperative pain and patient satisfaction. | |
| Quasi‐randomised trial comparing early second look office hysteroscopic adhesiolysis after hysteroscopic adhesiolysis and IUD insertion versus no early second look operative hysteroscopy in subfertile women with intrauterine adhesions. The method of sequence generation is based on alternation: women were allocated to the intervention or control groups based on their study entry. Main outcomes: pregnancy and live birth rate. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial studying the effectiveness of an anti‐adhesion barrier gel in women treated by operative hysteroscopy for retained products of conception. Status:completed. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial in a mixed study population of women with a history of pregnancy wastage or infertility and an associated complete uterine septum comparing metroplasty with complete section of the cervical septum versus metroplasty with preservation of the cervical septum. Outcome measures: operating time, distending media deficit, total distending media used, intraoperative bleeding, complications and reproductive outcome. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial conducted in patients with 2 or more failed IVF cycles with unsuspected or no uterine cavity abnormalities comparing office hysteroscopy prior to a subsequent IVF attempt or immediate IVF without prior hysteroscopy. Outcomes: number of oocytes retrieved, fertilisation rate, number of embryos transferred and clinical pregnancy rates. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial conducted to determine the incidence of unsuspected uterine cavity abnormalities detected by office hysteroscopy in patients before ICSI treatment compared to ICSI without prior hysteroscopy. Main outcomes were the incidence of unsuspected uterine abnormalities and implantation and clinical pregnancy rates. | |
| Published report describing a parallel‐group randomised trial comparing hysteroscopic myomectomy versus diagnostic hysteroscopy and biopsy in women with otherwise unexplained primary infertility and submucous fibroids. Primary outcome: clinical pregnancy rates. Quote from Fertility and Sterility searched on 16 January 2012: "This article has been retracted at the request of the editor as it duplicates parts of a paper that had already appeared in Hum. Reprod., 20 (2005) 1632–1635, DOI:10.1093/humrep/deh822". | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised comparing hysteroscopic lysis of intrauterine adhesions with or without adjunctive therapy (cyclical hormone replacement therapy alone or intrauterine device alone or both co‐treatments combined) after hysteroscopic metroplasty in a mixed population of women with subfertility and/or recurrent miscarriage. Main outcomes: incidence of de novo adhesion formation and ongoing pregnancy rate. | |
| Clinical controlled trial on the effectiveness of hysteroscopy prior to IVF; no random sequence generation. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing the hysteroscopic removal of polyps or fibroids by conventional hysteroscopy using a resectoscope versus hysteroscopic morcellation in a mixed population of women suffering from infertility or other gynaecological conditions. Outcome measures: mean number of insertions into the uterine cavity and mean operating time. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised comparing metroplasty using the resectoscope versus micro scissors for treating uterine septum in women with repeated miscarriage. Outcome measures: mean operating time, mean amount of distension medium used and complications. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing 2 different surgical techniques for metroplasty: resectoscopy with monopolar knife versus small‐diameter hysteroscopy fitted with a 5 Fr reusable bipolar electrode.Outcomes measures included pregnancy, miscarriage and live birth rates. |
ICSI: intracytoplasmic sperm injection
IUD: intrauterine device
IVF: in vitro fertilisation
PICO: Participants, Interventions, Comparisons and Outcomes
SIS: saline infusion sonography
TVUS: transvaginal ultrasound
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Randomised controlled multi‐centre equivalence trial |
| Participants | Abnormal uterine bleeding associated with a benign polyp. Inclusion criteria: 1. Abnormal uterine bleeding requiring diagnostic micro‐hysteroscopy Exclusion criteria: 1. Hysteroscopic features suggesting malignant lesion |
| Interventions | Outpatient polypectomy will be performed immediately following diagnosis at outpatient hysteroscopy in most instances, although some participants may have their outpatient treatment scheduled to a later date, depending upon local circumstances, within the following 8 weeks, as not all clinics are able to offer immediate “see & treat” outpatient treatment. Polyp removal will be carried out under direct hysteroscopic vision using miniature mechanical or electrosurgical instruments, with or without the need for minor degrees of cervical dilatation and local anaesthesia (direct cervical infiltration or paracervical injection). Occasionally blind avulsion with small polypectomy forceps after hysteroscopic localisation may be required. Inpatient polypectomy will be performed within 8 weeks of the initial diagnosis at outpatient hysteroscopy. Inpatient polypectomy will be performed by traditional dilatation and endometrial curettage ('D&C'), blind avulsion with or without prior localising hysteroscopy or under direct vision using an operative hysteroscope. In most instances, wide dilation of the cervical canal will be required to accommodate the larger diameter inpatient instruments within the uterus. General or spinal anaesthesia facilitates major degrees of cervical dilatation and manipulation of these larger diameter instruments within the uterine cavity. |
| Outcomes | Primary outcome: The patient's own assessment of bleeding symptoms at 6 months, using a dichotomous outcome measure, will be used to establish if the treatment has been successful. Secondary outcome: The following secondary outcomes will be assessed by a booklet sent to the women at home containing questionnaires/questions at baseline, 6, 12 and 24 months post‐randomisation: |
| Notes | Status of the trial: completed. Query clarified by Dr Justin Clark on 08‐12‐2014: "Our paper is just undergoing revision and should be published in the BMJ early next year. Our full NIHR HTA report will be published shortly afterwards – publication being held until the BMJ paper is in. I am unaware of any similar trials in female infertility – only MH Emanuel septoplasty trial and Dick Schoot RPOC morcellation study". |
| Methods | Randomisation: randomised; blinding: not blinded; placebo: not used; assignment: parallel |
| Participants | Infertile patients aged 20 to 40 years who are candidates for IUI with normal hysterosalpingography Exclusion criterion: ovarian hyperstimulation syndrome in patients suffering complications during surgery and hysteroscopy |
| Interventions | Intervention group: hysteroscopy Control group: no hysteroscopy |
| Outcomes | Primary outcome: pregnancy, diagnosed by ultrasound at 2 months after intervention Secondary outcome: complications of hysteroscopy and treatment side effects of ovulation induction |
| Notes | Recruitment status: completed. The primary study author will be contacted. |
HRQL: health‐related quality of life
IUI: intrauterine insemination
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | The effect of hysteroscopy on successful pregnancy in IVF in the infertile women who are candidate for the first IVF cycle |
| Methods | Parallel‐group randomised controlled trial |
| Participants | Inclusion criteria: age less than 38 years; BMI > 35, did not undergo hysteroscopy in the two past months, absence of uterine and tubal pathology which is incurable by hysteroscopy, couples undergoing ART with their own gametes. |
| Interventions | Intervention 1: In the control group: no intervention will be done. Intervention 2: In the intervention group, hysteroscopy is performed within 14 days prior to in vitro fertilisation and If there is an abnormality in the uterine cavity, this will be correct at the same time. |
| Outcomes | Primary outcome: biochemical pregnancy. Timepoint: 2 weeks after IVF. Method of measurement: ßHCG. Secondary outcome:clinical pregnancy. Timepoint: 4 weeks after IVF. Method of measurement: vaginal sonography. |
| Starting date | 24 May 2014 |
| Contact information | Amene Abiri Infertility department, second floor, Shariati Hospital, Jalal al Ahmad avenue, Tehran 14114, Islamic Republic of Iran Telephone: 00982184902421 e‐mail: abiriir@ yahoo.com |
| Notes | Recruitment status: completed. |
| Trial name or title | Hysteroscopy before first trial ICSI |
| Methods | Parallel‐group randomised controlled trial |
| Participants | Primary infertility Inclusion criteria: No previous IVF/ICSI cycle Exclusion criteria: Antral follicle count (AFC) 4, Anti‐mullarian hormone (AMH) `0.7, detectable uterine pathology by ultrasound Age minimum: 20 years |
| Interventions | Not reported in the registered study protocol |
| Outcomes | Primary outcome: clinical pregnancy with cardiac pulsation Secondary outcome: abortion, implantation rate |
| Starting date | 01 June 2013 |
| Contact information | Elsayedamr Basma 30 Garden City Smouha, Alexandria, Egypt Telephone: 00201223106023 e‐mail: [email protected] |
| Notes |
| Trial name or title | SIGnificance of Routine Hysteroscopy Prior to a First 'in Vitro Fertilization' (IVF) Treatment Cycle ‐ inSIGHT ClinicalTrials.gov NCT01242852 |
| Methods | Multicentre, single‐blind, parallel‐group randomised controlled trial |
| Participants | Women with primary or secondary infertility due to undergo IVF treatment with normal transvaginal ultrasound in the follicular phase of the menstrual cycle |
| Interventions | Office hysteroscopy combined with a saline infusion sonography prior to a first IVF cycle compared to starting IVF without prior hysteroscopy |
| Outcomes | Primary: ongoing pregnancy Secondary: costs, implantation rate, miscarriage rate and patient tolerance |
| Starting date | Current status on 1 November 2012: recruiting |
| Contact information | F.J. Broekmans, M.D., PhD University Medical Center Utrecht, Utrecht the Netherlands 3584CX Telephone: +31 887551041 |
| Notes |
| Trial name or title | Does office hysteroscopy and endometrial snip improve IUI outcome?: a randomized controlled trial |
| Methods | Allocation: randomised; endpoint classification: efficacy study; intervention model: parallel assignment; masking: single‐blind (participant); primary purpose: treatment |
| Participants | Inclusion criteria: 18 to 38 years old, at least 1 patent tube, unexplained infertility or anovulation or mild to moderate male factor infertility, previous failed IUI |
| Interventions | Control group: office hysteroscopy Intervention group: office hysteroscopy and endometrial snip |
| Outcomes | Primary outcome: clinical pregnancy rate at 10 months Secondary outcome: ongoing pregnancy rate at 12 months |
| Starting date | Current status on 1 November 2012: recruiting since February 2012 |
| Contact information | Waleed El‐Khayat, MD Faculty of Medicine, Cairo University Telephone: 23655215 |
| Notes | Status: recruiting. |
| Trial name or title | Hysteroscopy before in vitro fertilization ‐ Does it improve the outcome? |
| Methods | Parallel group randomised trial |
| Participants | Inclusion Criteria: Women submitted to IVF or ISCI treatment, age > 18 years,able to read, speak and understand Danish, written consent. Age minimum: 18 years |
| Interventions | Office‐hysteroscopy with biopsy |
| Outcomes | pregnancy rates [Time Frame: individual outcome will be evaluated within 8 weeks after IVF treatment. Over all outcome will be evaluated after 3 years.] |
| Starting date | January 2013 |
| Contact information | Kristine Juul Hare, MD, PhD Hvidovre University Hospital, Danmark e‐mail: [email protected] |
| Notes | Recruiting. |
| Trial name or title | Safety study of use of hyaluronic acid gel to prevent intrauterine adhesions in hysteroscopic surgery |
| Methods | Single‐centre, parallel‐group, randomised, single‐blind controlled trial |
| Participants | Women 18 years of age or older, undergoing hysteroscopic treatment |
| Interventions | Application of hyaluronic acid gel (study group); the control intervention is not described |
| Outcomes | Patient satisfaction following gel application at 2 months |
| Starting date | Current status on 1 November 2012: not yet recruiting |
| Contact information | Ariel Revel, MD Hadassah Medical Organization Telephone: 97226777111 ext 76389 e‐mail: [email protected] |
| Notes |
| Trial name or title | Evaluation of diagnostic hysteroscopy findings in patients candidate for ART (IVF, ICSI) and its effect on pregnancy rate compared to control group |
| Methods | Randomisation: randomised; blinding: not blinded; placebo: not used; assignment: parallel; purpose: treatment |
| Participants | Inclusion criteria: hysterosalpingography normal during the past 12 months; normal vaginal ultrasound; age between 25 and 40 years; absence of abnormal uterine bleeding and no hysteroscopy performed in the last 6 months |
| Interventions | Control group: hysteroscopy is not done In the intervention group a hysteroscopy is performed; submucosal myoma or polyps 1 cm or larger cervical or uterine adhesions will be resolved |
| Outcomes | Primary outcomes: presence of pathology Secondary outcomes: pregnancy 14 days after embryo transfer |
| Starting date | Current status on 1 November 2012: recruiting since June 2012 |
| Contact information | Farnaz Sohrabvand Vali‐e‐Asr Reproductive Health & Research Center Telephone: 00982166939320 e‐mail: [email protected] |
| Notes |
| Trial name or title | Endometrial hysteroscopy and curettage prior to embryo transfer |
| Methods | Parallel group randomised study |
| Participants | Inclusion Criteria: informed consent, in‐vitro fertilisation candidate, normal blood coagulation. Age minimum: 18 years |
| Interventions | Hysteroscopy and curettage |
| Outcomes | Primary outcomes: Endometrial receptivity, implantation rate and pregnancy rate |
| Starting date | December 2005 |
| Contact information | Amir Weiss HaEmek Medicak Center and Technion, Israel Institute of Technology Telephone: 972‐4‐6494031 e‐mail: [email protected] |
| Notes | Status: recruiting. The first author will be contacted. |
ART: assisted reproductive technology
ßHCG: beta human chorionic gonadotropin
BMI: body mass index
ICSI: intracytoplasmic sperm injection
IUI: intrauterine insemination
IVF: in vitro fertilisation
OHSS: Ovarian hyperstimulation syndrome
TESE: Testicular sperm extraction
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical pregnancy Show forest plot | 1 | 94 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.44 [0.97, 6.17] |
| Analysis 1.1 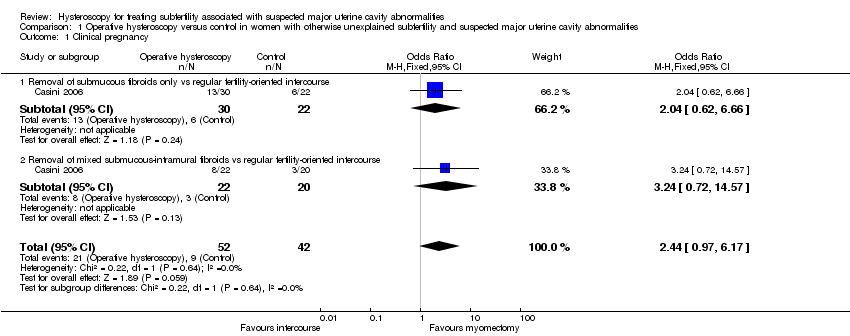 Comparison 1 Operative hysteroscopy versus control in women with otherwise unexplained subfertility and suspected major uterine cavity abnormalities, Outcome 1 Clinical pregnancy. | ||||
| 1.1 Removal of submucous fibroids only vs regular fertility‐oriented intercourse | 1 | 52 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.04 [0.62, 6.66] |
| 1.2 Removal of mixed submucous‐intramural fibroids vs regular fertility‐oriented intercourse | 1 | 42 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.24 [0.72, 14.57] |
| 2 Miscarriage Show forest plot | 1 | 30 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.12, 2.85] |
| Analysis 1.2  Comparison 1 Operative hysteroscopy versus control in women with otherwise unexplained subfertility and suspected major uterine cavity abnormalities, Outcome 2 Miscarriage. | ||||
| 2.1 Removal of submucous fibroids only vs regular fertility‐oriented intercourse | 1 | 19 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.09, 4.40] |
| 2.2 Removal of mixed submucous‐intramural fibroids vs regular fertility‐oriented intercourse | 1 | 11 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.03, 7.99] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical pregnancy Show forest plot | 1 | 204 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.41 [2.45, 7.96] |
| Analysis 2.1  Comparison 2 Operative hysteroscopy versus control in women undergoing MAR with suspected major uterine cavity abnormalities, Outcome 1 Clinical pregnancy. | ||||
| 1.1 Hysteroscopic polypectomy vs diagnostic hysteroscopy and biopsy only prior to IUI | 1 | 204 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.41 [2.45, 7.96] |

PRISMA study flow diagram.
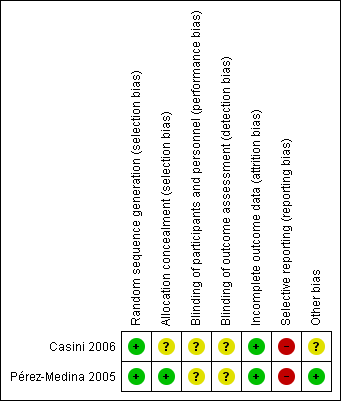
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Forest plot of comparison: 1 Hysteroscopic myomectomy vs regular fertility‐oriented intercourse in women with unexplained subfertility and submucous fibroids.Outcome: 1.1 Clinical pregnancy per woman randomised.
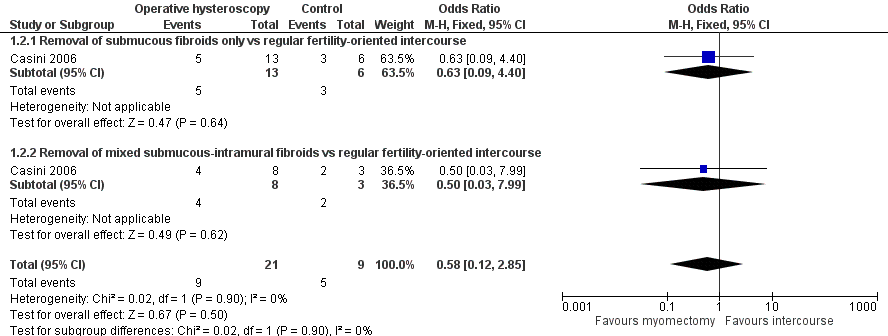
Forest plot of comparison: 1 Hysteroscopic myomectomy vs regular fertility‐oriented intercourse in women with unexplained subfertility and submucous fibroids. Outcome: 1.2 Miscarriage per clinical pregnancy.

Forest plot of comparison: 2 Hysteroscopic removal of polyps vs diagnostic hysteroscopy and biopsy only prior to IUI. Outcome: 2.1 Clinical pregnancy per woman randomised.

Comparison 1 Operative hysteroscopy versus control in women with otherwise unexplained subfertility and suspected major uterine cavity abnormalities, Outcome 1 Clinical pregnancy.

Comparison 1 Operative hysteroscopy versus control in women with otherwise unexplained subfertility and suspected major uterine cavity abnormalities, Outcome 2 Miscarriage.

Comparison 2 Operative hysteroscopy versus control in women undergoing MAR with suspected major uterine cavity abnormalities, Outcome 1 Clinical pregnancy.
| Operative hysteroscopy compared with control for unexplained subfertility associated with suspected major uterine cavity abnormalities | ||||||
| Patient or population: women with submucous fibroids and otherwise unexplained subfertility Settings: infertility centre in Rome, Italy Intervention: hysteroscopic removal of one submucous fibroid ≤ 40 mm Comparison: regular fertility‐oriented intercourse | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Myomectomy | |||||
| Live birth | No data were reported for this primary outcome. | |||||
| Hysteroscopy complications | No data were reported for this primary outcome. | |||||
| Clinical pregnancy ultrasound1 12 months | Medium‐risk population | OR 2.44 (0.97 to 6.17) | 94 | ⊕⊝⊝⊝ | ||
| 214 per 1000 | 399 per 1000 | |||||
| Miscarriage ultrasound5 12 months | Medium‐risk population | OR 0.58 (0.12 to 2.8) | 30 pregnancies in 94 women | ⊕⊝⊝⊝ | ||
| 556 per 1000 | 421 per 1000 | |||||
| *The basis for the assumed risk is the control group risk of the single included study (Casini 2006). The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 A clinical pregnancy was defined by the visualisation of an embryo with cardiac activity at six to seven weeks' gestational age. 2 Unclear allocation concealment. 3 Wide confidence intervals. 4 High risk of selective outcome reporting and unclear whether there is other bias caused by imbalance in the baseline characteristics. 5 Miscarriage was defined by the clinical loss of an intrauterine pregnancy between the 7th and 12th weeks of gestation. | ||||||
| Operative hysteroscopy compared with control for suspected major uterine cavity abnormalities prior to medically assisted reproduction | ||||||
| Patient or population: subfertile women with endometrial polyps diagnosed by ultrasonography prior to treatment with gonadotropin and intrauterine insemination Settings: infertility unit of a university tertiary hospital in the Spanish capital Madrid Intervention: hysteroscopic polypectomy using a 5.5 mm continuous flow office hysteroscope with a 1.5 mm scissors and forceps Comparison: diagnostic hysteroscopy using a 5.5 mm continuous flow office hysteroscope and polyp biopsy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Polypectomy | |||||
| Live birth | No data were reported for this primary outcome. | |||||
| Hysteroscopy complications | No data were reported for this primary outcome. | |||||
| Clinical pregnancy ultrasound1 4 IUI cycles | Low‐risk population2 | OR 4.41 (2.45 to 7.96) | 204 | ⊕⊕⊕⊝ | ||
| 250 per 1000 | 595 per 1000 | |||||
| Medium‐risk population3 | ||||||
| 366 per 1000 | 718 per 1000 | |||||
| High‐risk population4 | ||||||
| 528 per 1000 | 831 per 1000 | |||||
| Miscarriage | No data were reported for this secondary outcome. | |||||
| *The basis for the assumed risk in the low‐, medium‐ or high‐risk populations is the control group risk of three studies provided in the footnotes below. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Clinical pregnancy was defined by the presence of at least one gestational sac on ultrasound. 2 Based on the clinical pregnancy rate per woman after 4 cycles gonadotropins and IUI for male factor subfertility based on data from Bensdorp 2007. 3 Based on the clinical pregnancy rate per woman after 4 cycles gonadotropins and IUI for unexplained subfertility based on data from Veltman‐Verhulst 2012. 4 Based on the clinical pregnancy rate per woman after 4 cycles gonadotropins and IUI for female factor subfertility based on data from Spiessens 2003. 5 There was high risk for selective outcome reporting. | ||||||
| Polyp size | Clinical pregnancy1 | Clinical pregnancy rate (95% CI)2 |
| < 5 mm | 19/25 | 76% (from 72% to 80%) |
| 5 to 10 mm | 18/32 | 56% (from 53% to 59%) |
| 11 to 20 mm | 16/26 | 61% (from 58% to 65%) |
| > 20 mm | 11/18 | 61% (from 58% to 64%) |
| 1 Clinical pregnancy is defined by a pregnancy diagnosed by ultrasound visualisation of at least one gestational sac per woman randomised. 2 No significant difference was found for the clinical pregnancy rates between the 4 subgroups (P = 0.32). | ||
| Quality assessment Submucous fibroids and unexplained subfertility | ||||||
| No of studies | Design | Limitations | Inconsistency | Indirectness | Imprecision | Other considerations |
| Clinical pregnancy (follow‐up 1 year; ultrasound1) | ||||||
| 1 | RCT | Serious2 | No serious inconsistency | No serious indirectness | Serious3 | Reporting bias4 |
| Miscarriage (follow‐up 1 year; ultrasound5) | ||||||
| 1 | RCT | Serious2 | No serious inconsistency | No serious indirectness | Serious3 | Reporting bias4 |
| 1 A clinical pregnancy was defined by the visualisation of an embryo with cardiac activity at six to seven weeks' gestational age. 2 Unclear allocation concealment. 3 Wide confidence intervals. 4 High risk of selective outcome reporting and unclear whether there is other bias caused by imbalance in the baseline characteristics. 5 Miscarriage was defined by the clinical loss of an intrauterine pregnancy between the 7th and 12th weeks of gestation. | ||||||
| Quality assessment Endometrial polyps prior to gonadotropin and IUI treatment | ||||||
| No of studies | Design | Limitations | Inconsistency | Indirectness | Imprecision | Other considerations |
| Clinical pregnancy (follow‐up 4 IUI cycles; ultrasound1) | ||||||
| 1 | RCT | No serious limitations | No serious inconsistency | No serious indirectness | No serious imprecision | Selective outcome reporting2 |
| 1 Clinical pregnancy was defined by the presence of at least one gestational sac on ultrasound. 2 There was high risk for selective outcome reporting bias. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical pregnancy Show forest plot | 1 | 94 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.44 [0.97, 6.17] |
| 1.1 Removal of submucous fibroids only vs regular fertility‐oriented intercourse | 1 | 52 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.04 [0.62, 6.66] |
| 1.2 Removal of mixed submucous‐intramural fibroids vs regular fertility‐oriented intercourse | 1 | 42 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.24 [0.72, 14.57] |
| 2 Miscarriage Show forest plot | 1 | 30 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.12, 2.85] |
| 2.1 Removal of submucous fibroids only vs regular fertility‐oriented intercourse | 1 | 19 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.09, 4.40] |
| 2.2 Removal of mixed submucous‐intramural fibroids vs regular fertility‐oriented intercourse | 1 | 11 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.03, 7.99] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical pregnancy Show forest plot | 1 | 204 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.41 [2.45, 7.96] |
| 1.1 Hysteroscopic polypectomy vs diagnostic hysteroscopy and biopsy only prior to IUI | 1 | 204 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.41 [2.45, 7.96] |

