Hystéroscopie dans le traitement de l'hypofertilité liée à des anomalies majeures suspectées de la cavité utérine
Appendices
Appendix 1. CENTRAL search strategy
#1MeSH descriptor Hysteroscopy explode all trees (328)
#2hysteroscopic near polypectom* (11)
#3hysteroscopic near polyp removal* (11)
#4hysteroscopic near synechiolys* (1)
#5hysteroscopic near synechiotomy (1)
#6hysteroscopic near adhesiolys* (5)
#7hysteroscopic near metroplast* (17)
#8hysteroscopic near septoplast* (5)
#9hysteroscopic near sept* resection* (10)
#10MeSH descriptor Infertility explode tree 2 (1,430)
#11endometri* near polyp* (118)
#12leiomyom* (588)
#13fibromyom* (28)
#14fibroid* (462)
#15fibroma* (56)
#16myoma* (370)
#17synechia* (196)
#18intrauterine OR uterine near adhesion* (2,918)
#19Asherman* near syndrome* (9)
#20intrauterine OR uterine near sept* (2,915)
#21intrauterine OR uterine disease* (4,621)
#22uterine neoplasm* (2,610)
#23intrauterine OR uterine near congenital abnormalit* (2,890)
#24intrauterine OR uterine near malformation* (2,900)
#25septate near uterus (23)
#26in vitro near fertil* (2,822)
#27ICSI (1,206)
#28IVF (2,740)
#29intracytoplasm* sperm in* (1,047)
#30IUI (456)
#31(uterine OR intrauterine) OR artificial near insemination* (10,282)
#32assisted reproduct* near technique* (363)
#33ART (73,076)
#34embryo transfer (1,918)
#35zygote intrafallopian transfer (40)
#36(#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #6 OR #8 OR #9) (342)
#37(#11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35) (85,110)
#38(#10 AND #36 AND #37) (37)
Search 'Trials' (29)
29 records
Database: Cochrane Central Register of Controlled Trials : Issue 9 of 12, September 2014
Most recent update: 13 October 2014.
Appendix 2. Cochrane Menstrual Disorders and Subfertility Group Specialised Register search strategy
Keywords CONTAINS "hysteroscopic "or "hysteroscopy"or "hysteroscope"or "endoscopy" or Title CONTAINS "hysteroscopic "or "hysteroscopy"or "hysteroscope"or "endoscopy"
AND
Keywords CONTAINS "subfertility"or "subfertility‐Female"or "infertility" or "IVF" or "ICSI" or "IUI"or "in vitro fertilisation" or "in vitro fertilization" or "Intrauterine Insemination" or "artificial insemination" or "assisted conception" or "assisted reproduction techniques" or " embryo transfer" or "zygote intrafallopian transfer" or "myoma" or "myomas" or "myomectomy" or "septate uterus"or "polypectomy" or"polyp removal" or "polyps"or "adhesiolysis"or "adhesion" or"adhesions" or"synechiotomy" or"Leiomyoma" or"leiomyomata" or"fibroids" or"Asherman's Syndrome"or "uterine septa"or "uterine septum" or"uterine disease"or "uterine leiomyomas" or"uterine malformation" or"Uterine Neoplasms"or "uterine polyps"
180 records
Database: Cochrane MDSG Specialised Register
Most recent update: 8 September 2014.
Appendix 3. MEDLINE search strategy (PubMed)
("Hysteroscopy"[Mesh] OR Uterine Endoscop*[All Fields] OR Uteroscop*[All Fields] OR Hysteroscopic Surg*[All Fields] OR (hysteroscopic[All Fields] AND (polypectom*[All Fields] OR polyp removal*[All Fields] OR myomectom*[All Fields] OR synechiolysis[All Fields] OR synechiotomy[All Fields] OR adhesiolysis[All Fields] OR metroplast*[All Fields] OR septoplast*[All Fields] OR septum resection*[All Fields]))) AND (Subfertility[tiab] OR "Infertility, Female"[Mesh] OR (female[tiab] AND (Infertility[tiab] OR Sterility[tiab]))) AND ((("Endometrium"[Mesh] OR Endometri*[All Fields]) AND (polyp[All Fields] OR polyps[All Fields])) OR "Leiomyoma"[Mesh] OR Leiomyoma[All Fields] OR Leiomyomas[All Fields] OR Fibromyoma[All Fields] OR Fibromyomas[All Fields] OR Fibroid[All Fields] OR Fibroids[All Fields] OR fibromas[All Fields] OR Myoma[All Fields] OR Myomas[All Fields] OR ((Synechiae[All Fields] AND ((Intrauterine[All Fields] OR uterine[All Fields]) AND adhesion*)) OR "Asherman Syndrome"[All Fields] OR "Asherman's Syndrome"[All Fields] OR "Ashermans Syndrome"[All Fields] OR ((septa[All Fields] OR septum[All Fields]) AND (uterine[All Fields] OR intrauterine[All Fields])) OR "Uterine Diseases"[Mesh] OR "Uterine Neoplasms"[Mesh] OR ((uterine[All Fields] OR intrauterine[All Fields]) AND "Congenital Abnormalities"[Mesh]) OR "Fertilization in Vitro"[Mesh] OR (Fertilization[All Fields] AND "in Vitro"[All Fields]) OR IVF[All Fields] OR ICSI[All Fields] OR "Reproductive Techniques"[Mesh] OR "Embryo Transfer"[Mesh] OR "Zygote Intrafallopian Transfer"[Mesh] OR "Insemination, Artificial"[Mesh] OR ((intrauterine OR artificial) AND insemination[All Fields]))) AND (randomized controlled trial[pt] OR controlled clinical trial[pt] OR randomized[tiab] OR placebo[tiab] OR drug therapy[sh] OR randomly[tiab] OR trial[tiab] OR groups[tiab]) NOT (animals[mh] NOT humans[mh])
89 records
Database: MEDLINE using PubMed
Most recent update: 12 October 2014.
Appendix 4. EMBASE search strategy (Embase.com)
#1. 'hysteroscopy'/exp (7,918)
#2. hysteroscopy (8,686)
#3. 'endoscopy' (184,646)
#4. 'endoscopy'/exp (416,527)
#5. 'infertility'/exp (92,710)
#6. 'subfertility' (4,551)
#7. 'infertility' (99,272)
#8. 'infertility therapy'/exp (79,750)
#9. ivf OR 'icsi' (34,185)
#10. artificial AND insemination (14,748)
#11. assisted AND conception (3,939)
#12. 'uterus myoma'/exp (10,149)
#13. 'leiomyoma'/exp (14,378)
#14. myoma OR myomectomy (15,999)
#15. septate AND uterus (666)
#16. 'polypectomy' (8,683)
#17. 'adhesiolysis' (1,803)
#18. 'polyp' (48,672)
#19. uterine AND septa (223)
#20. 'uterine septum' (351)
#21. synechiotomy (9)
#22. 'leiomyoma' (17,645)
#23. 'uterine malformation' (229)
#24. 'uterine anomaly' (265)
#25. 'fibroid' (3,694)
#26. OR (1‐4) (457,395)
#27. OR (5‐7) (118,016)
#28. OR (8‐25) (183,344)
#29. AND (26‐28) (3,184)
#30. #29 AND ([cochrane review]/lim OR [systematic review]/lim OR [controlled clinical trial]/lim OR [randomized controlled trial]/lim OR [meta analysis]/lim) (253)
253 records
Database: EMBASE using Embase.com
Most recent update: 7 October 2014.
Appendix 5. CINAHL search strategy (EBSCOHOST)
S1 TX hysteroscopy (391)
S2 TX uterine endoscop* (4)
S3 TX uteroscop* (1,001) Smart Text searching
S4 MH hysteroscopy (331)
S5 TX hysteroscopic polypectom* (4)
S6 TX hysteroscopic polyp removal* (13,517) Smart Text searching
S7 TX hysteroscopic myomectom* (16)
S8 TX hysteroscopic adhesiolys* (2)
S9 TX hysteroscopic synechiolys* (1,246) Smart Text searching
S10 TX hysteroscopic synechiotomy (1,246) Smart Text searching
S11 TX hysteroscopic metroplast* (7)
S12 TX hysteroscopic septoplast* (1)
S13 TX hysteroscopic septum resection (1)
S14 TX hysteroscopic sept* resection (3)
S15 TX subfertility (281)
S16 MHinfertility (3,706)
S17 TX sterility (361)
S18 MHfemale (776,980)
S19 TX endometri* polyp* (78)
S20 TX leiomyoma* (1,219)
S21 TX fibromyoma* (5)
S22 TX fibroid* (560)
S23 TX fibroma* (394)
S24 TX myoma* (169)
S25 TX synechia* (79)
S26 TX intrauterine adhesion* (11)
S27 TX uterine adhesion* (20)
S28 TX Asherman* syndrome (9)
S29 TX uterine sept* (18)
S30 TX intrauterine sept* (10)
S31 TX septate uterus (23)
S32 MHuterine diseases (432)
S33 MH uterine neoplasm* (1,005)
S34 ""uterine congenital abnormalit*"" (19,260) Smart Text searching
S35 TX uterine congenital abnormalities (42,155) Smart Text searching
S36 TX uterine malformation* (29)
S37 MH Fertilization in vitro(1834)
S38 TX in vitro fertilisation (216)
S39 TX IVF (800)
S40 MHReproduction Techniques (1,945)
S41 TX ICSI (155)
S42 MHembryo transfer(350)
S43 MH Gamete Intrafallopian Transfer (55)
S44 MH Insemination, Artificial (301)
S45 TX intrauterine insemination (97)
S46 TX IUI (50)
S47 MH Clinical Trials"# OR #MH "Randomized Controlled Trials# (502,384) SmartText Searching
S48 PT clinical trial* (51,468)
S49 PT Randomized Controlled Trials (181,244)
S50 MH Randomized Controlled Trials (20,360)
S51 TXrandomised controlled trial (6,360)
S52 PT randomised controlled trial* (118,899) SmartText Searching
S53 MH Random Assignment (31,296)
S54 TX Randomi*ation (3,619)
S55 MH Single‐Blind Studies (6,144)
S56 MH Double‐Blind Studies (20,422)
S57 MH Triple‐Blind Studies (65)
S58 TX treble blind* (34,072) Smart Text searching
S59 MH Placebos (7,082)
S60 MH Prospective Studies (162,939)
S61 OR/S47‐60 (631,229)
S62 OR/S1‐14 (13,795)
S63 OR/S15‐17 (4,227)
S64 S18 AND S63 (2,550)
S65 0R/S19‐46 (46,874)
S66 S61 and S62 and S64 and S65 (21)
21 records
Database: CINAHL using EBSCOHOST
Most recent update: 11 October 2014.
Appendix 6. Web of Science search strategy (WoS Core Collection)
TS=((((Hysteroscopy OR Uterine Endoscop* OR Uteroscop* OR Hysteroscopic Surg* OR (hysteroscopic AND (polypectom* OR myomectom* OR synechiolysis OR adhesiolysis OR metroplast* OR septoplast* OR septum resection*))) AND (female AND (Subfertility OR Infertility OR Sterility)) AND ((Endometri* AND (polyp OR polyps)) OR Leiomyoma* OR Fibromyoma* OR Fibroid* OR fibromas OR Myoma* OR Synechiae OR ((Intrauterine OR uterine) AND adhesion*) OR (Asherman* AND Syndrome*) OR ((septa OR septum) AND (uterine OR intrauterine)) OR uterine diseases OR uterine neoplasms OR ((uterine OR intrauterine) AND (congenital abnormalities)) OR (Fertilization SAME "in Vitro") OR IVF OR ICSI OR reproductive techniques OR embryo transfer Or zygote intrafallopian transfer OR ((intrauterine OR artificial) AND insemination))))) (70)
70 records
Database: Web of Science Core Collection Indexes=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH Timespan=All years
Most recent update: 11 October 2014.
Appendix 7. Items of data extraction
1. Source
-
Study ID
-
Report ID
-
Review author ID
-
Citation and contact details
2. Eligibility
-
Confirm eligibility for review
-
Reason for exclusion
3. Trial characteristics
1.Study design
-
Random sequence generation
-
Patient recruitment
-
Patient in‐ and exclusion criteria
-
Allocation concealment
-
Blinding of participants and personnel
-
Blinding of outcome assessors
-
Completeness of outcome data
-
Selective outcome reporting
-
Other potential sources of bias
2. Follow‐up
-
Duration of follow‐up
-
Type of follow‐up
3. Size of study
-
Number of women recruited
-
Number of women randomised
-
Number of women excluded
-
Number of women withdrawn and lost to follow‐up
-
Number of women analysed
4. Study setting
-
Single‐centre or multicentre
-
Location
-
Timing and duration
5. Diagnostic criteria
-
Screening by TVS
-
Screening by HSG
-
Screening by TVS and HSG
-
Screening by other ultrasound diagnostic procedures, e.g. SIS or GIS
-
Screening by hysteroscopy
-
Diagnosis confirmed by hysteroscopy and biopsy
4. Characteristics of the study participants
-
Baseline characteristics
-
Age
-
Primary or secondary subfertility
-
Duration of subfertility
-
Diagnostic work‐up: baseline FSH, semen analysis, diagnosis of tubal pathology, confirmatory test of ovulation
-
Other contributory causes to subfertility than uterine factor
-
Previous treatments ‐ IVF, IUI or other treatments
2. Treatment characteristics
-
IUI natural cycle
-
IUI controlled ovarian stimulation with anti‐oestrogens or gonadotropins
-
IVF protocol and number of embryos transferred
-
ICSI protocol and number of embryos transferred
-
detailed description of the hysteroscopic procedure
5. Interventions
-
Total number of intervention groups
-
Absence of other interventions in the treatment and control group
For each intervention and comparison group of interest:
-
Specific intervention
-
Intervention details
-
Timing of the intervention
6. Outcomes
-
Outcomes and time points collected
-
Outcomes and time points reported
Definition and unit of measurement for each of the following outcomes:
Primary outcome:
-
Live birth delivery rate
-
Hysteroscopy complication rate
Secondary outcome:
-
Ongoing pregnancy rate
-
Clinical pregnancy with fetal heart beat
-
Clinical pregnancy rate
-
Miscarriage rate
For each outcome of interest:
-
Sample size
-
Missing participants
-
Summary data for each intervention group in 2 x 2 table
-
Estimate of effect with 95% CI
-
Subgroup analyses
7. Miscellaneous
-
Funding source
-
Key conclusions of the study authors
-
Miscellaneous comments from the study authors
-
References to other relevant studies
-
Correspondence required
-
Miscellaneous comments by the review authors

PRISMA study flow diagram.
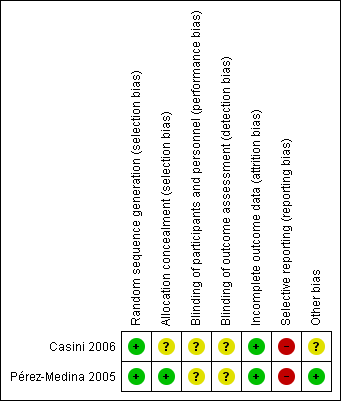
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Forest plot of comparison: 1 Hysteroscopic myomectomy vs regular fertility‐oriented intercourse in women with unexplained subfertility and submucous fibroids.Outcome: 1.1 Clinical pregnancy per woman randomised.
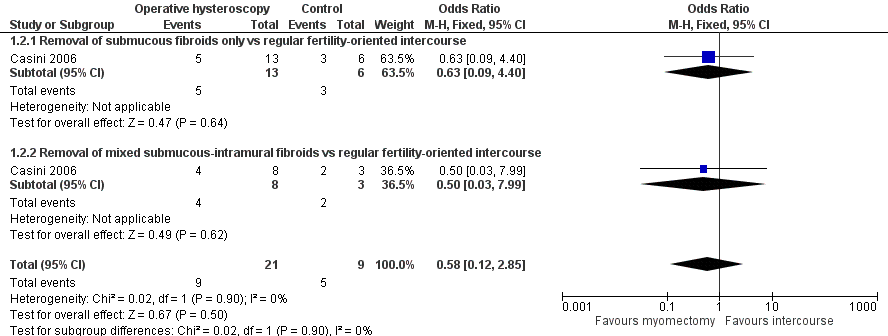
Forest plot of comparison: 1 Hysteroscopic myomectomy vs regular fertility‐oriented intercourse in women with unexplained subfertility and submucous fibroids. Outcome: 1.2 Miscarriage per clinical pregnancy.

Forest plot of comparison: 2 Hysteroscopic removal of polyps vs diagnostic hysteroscopy and biopsy only prior to IUI. Outcome: 2.1 Clinical pregnancy per woman randomised.

Comparison 1 Operative hysteroscopy versus control in women with otherwise unexplained subfertility and suspected major uterine cavity abnormalities, Outcome 1 Clinical pregnancy.

Comparison 1 Operative hysteroscopy versus control in women with otherwise unexplained subfertility and suspected major uterine cavity abnormalities, Outcome 2 Miscarriage.

Comparison 2 Operative hysteroscopy versus control in women undergoing MAR with suspected major uterine cavity abnormalities, Outcome 1 Clinical pregnancy.
| Operative hysteroscopy compared with control for unexplained subfertility associated with suspected major uterine cavity abnormalities | ||||||
| Patient or population: women with submucous fibroids and otherwise unexplained subfertility Settings: infertility centre in Rome, Italy Intervention: hysteroscopic removal of one submucous fibroid ≤ 40 mm Comparison: regular fertility‐oriented intercourse | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Myomectomy | |||||
| Live birth | No data were reported for this primary outcome. | |||||
| Hysteroscopy complications | No data were reported for this primary outcome. | |||||
| Clinical pregnancy ultrasound1 12 months | Medium‐risk population | OR 2.44 (0.97 to 6.17) | 94 | ⊕⊝⊝⊝ | ||
| 214 per 1000 | 399 per 1000 | |||||
| Miscarriage ultrasound5 12 months | Medium‐risk population | OR 0.58 (0.12 to 2.8) | 30 pregnancies in 94 women | ⊕⊝⊝⊝ | ||
| 556 per 1000 | 421 per 1000 | |||||
| *The basis for the assumed risk is the control group risk of the single included study (Casini 2006). The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 A clinical pregnancy was defined by the visualisation of an embryo with cardiac activity at six to seven weeks' gestational age. 2 Unclear allocation concealment. 3 Wide confidence intervals. 4 High risk of selective outcome reporting and unclear whether there is other bias caused by imbalance in the baseline characteristics. 5 Miscarriage was defined by the clinical loss of an intrauterine pregnancy between the 7th and 12th weeks of gestation. | ||||||
| Operative hysteroscopy compared with control for suspected major uterine cavity abnormalities prior to medically assisted reproduction | ||||||
| Patient or population: subfertile women with endometrial polyps diagnosed by ultrasonography prior to treatment with gonadotropin and intrauterine insemination Settings: infertility unit of a university tertiary hospital in the Spanish capital Madrid Intervention: hysteroscopic polypectomy using a 5.5 mm continuous flow office hysteroscope with a 1.5 mm scissors and forceps Comparison: diagnostic hysteroscopy using a 5.5 mm continuous flow office hysteroscope and polyp biopsy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Polypectomy | |||||
| Live birth | No data were reported for this primary outcome. | |||||
| Hysteroscopy complications | No data were reported for this primary outcome. | |||||
| Clinical pregnancy ultrasound1 4 IUI cycles | Low‐risk population2 | OR 4.41 (2.45 to 7.96) | 204 | ⊕⊕⊕⊝ | ||
| 250 per 1000 | 595 per 1000 | |||||
| Medium‐risk population3 | ||||||
| 366 per 1000 | 718 per 1000 | |||||
| High‐risk population4 | ||||||
| 528 per 1000 | 831 per 1000 | |||||
| Miscarriage | No data were reported for this secondary outcome. | |||||
| *The basis for the assumed risk in the low‐, medium‐ or high‐risk populations is the control group risk of three studies provided in the footnotes below. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Clinical pregnancy was defined by the presence of at least one gestational sac on ultrasound. 2 Based on the clinical pregnancy rate per woman after 4 cycles gonadotropins and IUI for male factor subfertility based on data from Bensdorp 2007. 3 Based on the clinical pregnancy rate per woman after 4 cycles gonadotropins and IUI for unexplained subfertility based on data from Veltman‐Verhulst 2012. 4 Based on the clinical pregnancy rate per woman after 4 cycles gonadotropins and IUI for female factor subfertility based on data from Spiessens 2003. 5 There was high risk for selective outcome reporting. | ||||||
| Polyp size | Clinical pregnancy1 | Clinical pregnancy rate (95% CI)2 |
| < 5 mm | 19/25 | 76% (from 72% to 80%) |
| 5 to 10 mm | 18/32 | 56% (from 53% to 59%) |
| 11 to 20 mm | 16/26 | 61% (from 58% to 65%) |
| > 20 mm | 11/18 | 61% (from 58% to 64%) |
| 1 Clinical pregnancy is defined by a pregnancy diagnosed by ultrasound visualisation of at least one gestational sac per woman randomised. 2 No significant difference was found for the clinical pregnancy rates between the 4 subgroups (P = 0.32). | ||
| Quality assessment Submucous fibroids and unexplained subfertility | ||||||
| No of studies | Design | Limitations | Inconsistency | Indirectness | Imprecision | Other considerations |
| Clinical pregnancy (follow‐up 1 year; ultrasound1) | ||||||
| 1 | RCT | Serious2 | No serious inconsistency | No serious indirectness | Serious3 | Reporting bias4 |
| Miscarriage (follow‐up 1 year; ultrasound5) | ||||||
| 1 | RCT | Serious2 | No serious inconsistency | No serious indirectness | Serious3 | Reporting bias4 |
| 1 A clinical pregnancy was defined by the visualisation of an embryo with cardiac activity at six to seven weeks' gestational age. 2 Unclear allocation concealment. 3 Wide confidence intervals. 4 High risk of selective outcome reporting and unclear whether there is other bias caused by imbalance in the baseline characteristics. 5 Miscarriage was defined by the clinical loss of an intrauterine pregnancy between the 7th and 12th weeks of gestation. | ||||||
| Quality assessment Endometrial polyps prior to gonadotropin and IUI treatment | ||||||
| No of studies | Design | Limitations | Inconsistency | Indirectness | Imprecision | Other considerations |
| Clinical pregnancy (follow‐up 4 IUI cycles; ultrasound1) | ||||||
| 1 | RCT | No serious limitations | No serious inconsistency | No serious indirectness | No serious imprecision | Selective outcome reporting2 |
| 1 Clinical pregnancy was defined by the presence of at least one gestational sac on ultrasound. 2 There was high risk for selective outcome reporting bias. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical pregnancy Show forest plot | 1 | 94 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.44 [0.97, 6.17] |
| 1.1 Removal of submucous fibroids only vs regular fertility‐oriented intercourse | 1 | 52 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.04 [0.62, 6.66] |
| 1.2 Removal of mixed submucous‐intramural fibroids vs regular fertility‐oriented intercourse | 1 | 42 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.24 [0.72, 14.57] |
| 2 Miscarriage Show forest plot | 1 | 30 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.12, 2.85] |
| 2.1 Removal of submucous fibroids only vs regular fertility‐oriented intercourse | 1 | 19 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.09, 4.40] |
| 2.2 Removal of mixed submucous‐intramural fibroids vs regular fertility‐oriented intercourse | 1 | 11 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.03, 7.99] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical pregnancy Show forest plot | 1 | 204 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.41 [2.45, 7.96] |
| 1.1 Hysteroscopic polypectomy vs diagnostic hysteroscopy and biopsy only prior to IUI | 1 | 204 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.41 [2.45, 7.96] |

