Propofol versus tiopental sódico para el tratamiento del estado epiléptico resistente
Resumen
Antecedentes
Esta revisión es una actualización de una revisión publicada anteriormente en la Base de Datos Cochrane de Revisiones Sistemáticas (Cochrane Database of Systematic Reviews), (número 6, 2015).
La falta de respuesta a los fármacos antiepilépticos en pacientes con actividad convulsiva no controlada, como el estado epiléptico resistente (EER), ha llevado al uso de fármacos anestésicos. El coma se induce con fármacos anestésicos para lograr el control completo de la actividad convulsiva. El tiopental sódico y el propofol se utilizan con frecuencia para esta finalidad. Ambos agentes se han mostrado eficaces. Sin embargo, no existe evidencia significativa sobre cuál de estos dos fármacos es mejor en cuanto a los resultados clínicos.
Objetivos
Comparar la eficacia, los efectos adversos y los resultados a corto y largo plazo del estado epiléptico refractario (EER) tratado con uno de los dos agentes anestésicos, el tiopental sódico o el propofol.
Métodos de búsqueda
Se realizaron búsquedas en el registro especializado del Grupo Cochrane de Epilepsia (Cochrane Epilepsy Group) (16 de agosto de 2016), en el Registro Cochrane Central de Ensayos Controlados (CENTRAL) a través del Registro Cochrane de Estudios en Línea (Cochrane Register of Studies Online, CRSO, 16 de agosto de 2016), en MEDLINE (Ovid, 1946 a 16 de agosto de 2016), en ClinicalTrials.gov (16 de agosto de 2016) y en la South Asian Database of Controlled Clinical Trials (16 de agosto de 2016). Anteriormente se buscó en IndMED, pero no estaba accesible en el momento de la última actualización.
Criterios de selección
Todos los ensayos controlados aleatorizados (ECA) o cuasialeatorizados (independientemente del cegamiento) que evalúan el control de la EER mediante el uso de tiopental sódico o propofol en pacientes de cualquier edad y sexo.
Obtención y análisis de los datos
Dos autores de la revisión revisaron los resultados de la búsqueda y revisaron los resúmenes de los ensayos relevantes y elegibles antes de recuperar las publicaciones de texto completo.
Resultados principales
Un estudio con un total de 24 participantes estaba disponible para la revisión. Este estudio fue un pequeño ensayo multicéntrico, de cegamiento simple, en el que se estudiaron adultos con EER que recibían propofol o tiopental sódico para el control de la actividad convulsiva. Este estudio se terminó antes de tiempo debido a problemas de reclutamiento. Para el resultado primario de control total de las convulsiones después del primer curso del fármaco en estudio, hubo 6/14 pacientes versus 2/7 pacientes en los grupos de propofol y tiopental sódico, respectivamente (riesgos relativos (RR) 1,50, intervalo de confianza (IC) del 95%: 0,40 a 5,61, evidencia de baja calidad). Se observó mortalidad en 3/14 pacientes versus 1/7 pacientes en los grupos de propofol y tiopental sódico, respectivamente (RR 1,50; IC del 95%: 0,19 a 11,93, evidencia de baja calidad). El tercer resultado primario de la duración de la estancia en la UCI no fue informado. En cuanto a los resultados secundarios de los eventos adversos, se observó una infección en 7/14 pacientes versus 5/7 pacientes en los grupos de propofol y sodio tiopental, respectivamente (RR 0,70; IC del 95%: 0,35 a 1,41). Se observó hipotensión durante la administración de los fármacos en estudio y que requería el uso de vasopresores en 7/14 pacientes versus 4/7 pacientes en los grupos de propofol y tiopental sódico, respectivamente (RR 0,87; IC del 95%: 0,38 a 2,00). La otra complicación grave que se observó fue el síndrome de infusión de propofol no mortal en un paciente. Los pacientes que recibían tiopental sódico requerían más días de ventilación mecánica en comparación con los pacientes que recibían propofol: (mediana (rango) 17 días (cinco a 70 días) con tiopental sódico versus cuatro días (dos a 28 días) con propofol). A los tres meses, no había evidencia de que hubiera una diferencia entre los fármacos con respecto a las medidas de resultado, como el control de la actividad convulsiva y el resultado funcional.
Conclusiones de los autores
Desde la última versión de esta revisión, no se han encontrado nuevos estudios.
Falta evidencia sólida, aleatorizada y controlada que aclare la eficacia del propofol y el tiopental sódico comparados entre sí en el tratamiento de la ERM. Se requieren ensayos controlados aleatorizados amplios sobre esta grave enfermedad.
PICO
Resumen en términos sencillos
Propofol versus tiopental sódico para el tratamiento del estado epiléptico resistente (EER)
Pregunta de la revisión: En esta revisión, se evaluó la evidencia del uso de estos fármacos anestésicos para controlar la actividad convulsiva en pacientes con ERS.
Antecedentes: Las convulsiones persistentes (que duran 30 minutos o más) son una emergencia médica importante asociada a una morbilidad y mortalidad significativas. En algunos casos, estas convulsiones no logran responder a la farmacoterapia de primera y segunda línea, y pueden ocurrir hasta en el 31% de los pacientes que sufren una crisis convulsiva persistente o actividades convulsivas. La actividad convulsiva persistente puede convertirse en resistente a los fármacos antiepilépticos. Los anestésicos como el tiopental sódico y el propofol se administran con frecuencia para el control de las crisis convulsivas en tales situaciones. Ambos agentes tienen sus propios efectos secundarios y complicaciones.
Características de los estudios: La evidencia está actualizada hasta agosto de 2016. Sólo se pudo identificar un ensayo, que se terminó antes de tiempo debido a problemas de reclutamiento. En este estudio se reclutaron sólo 24 participantes de los 150 requeridos. Este estudio fue un pequeño ensayo multicéntrico, de cegamiento simple, en el que se estudiaron adultos con EER que recibían propofol o tiopental sódico para el control de la actividad convulsiva.
Resultados clave: No había ninguna diferencia entre los dos fármacos en cuanto a su capacidad para controlar la actividad convulsiva. La única diferencia observada fue la necesidad de ventilación mecánica prolongada para los pacientes del grupo del tiopental sódico. Esto podría deberse a la prolongada presencia del fármaco en el cuerpo debido a su lenta eliminación.
Calidad de la evidencia: Se consideró que la calidad de la evidencia de los resultados primarios de control total de las convulsiones y la mortalidad intrahospitalaria era baja. Existe la necesidad clara de un ensayo controlado aleatorizado amplio para estudiar la eficacia de los agentes anestésicos en el tratamiento de la EER.
Authors' conclusions
Summary of findings
| Propofol compared to Thiopental sodium for the treatment of refractory status epilepticus | ||||||
| Patient or population: patients with the treatment of refractory status epilepticus | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Thiopental sodium | Propofol | |||||
| Total control of seizures | Study population | RR 1.5 | 21 | ⊕⊕⊝⊝ | ||
| 286 per 1000 | 429 per 1000 | |||||
| In‐hospital mortality | Study population | RR 1.5 | 21 | ⊕⊕⊝⊝ | ||
| 143 per 1000 | 214 per 1000 | |||||
| Length of intensive care unit (ICU) stay | Not reported | Not reported | NA | NA | NA | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Single blinded study: we downgraded one level for risk of bias | ||||||
Background
This review is an update of a previously published review in the Cochrane Database of Systematic Reviews (Issue 6, 2015).
Although there is no universally accepted definition of status epilepticus (SE), it has been defined as a condition in which there is either continuous seizure activity for more than 30 minutes, or two or more seizure activities in a sequence without return of full consciousness between the episodes (Prasad 2005; Working Group 1993).
There is no consensus on the duration of seizure activity that may be required to define SE. SE may be broadly classified into two types, convulsive and non‐convulsive. The common aetiologies for SE are stroke, traumatic brain injury, brain tumours, central nervous system infection, metabolic or toxic encephalopathies, and electrolyte disorders. SE is a major medical emergency associated with significant morbidity and mortality (16% to 23%) (Rossetti 2007).
Refractory status epilepticus (RSE) is defined as SE that fails to respond to first‐ and second‐line therapy, and it is observed in 9% to 31% of patients with SE (Mayer 2002; Treiman 1998). To be categorised as RSE, some authors have suggested a time frame (Mayer 2002), whereas others have not (Holtkamp 2007; Rossetti 2005). The first line of treatment for SE includes benzodiazepines; the second line includes antiepileptic drugs such as phenytoin, phenobarbital, or valproic acid. The assistance of an anaesthetist is required for managing RSE, where coma may be induced with anaesthetic agents in order to achieve complete control of seizures. The use of anaesthetic agents such as thiopental sodium and propofol for managing RSE is common in many centres (Parviainen 2002; Van Gestel 2005). Thiopental sodium belongs to the barbiturates group of drugs unrelated to propofol, which is a phenolic compound. Both agents have been found to be effective in controlling seizures in RSE (Parviainen 2002; Van Gestel 2005). There is substantial lack of evidence as to which of the two drugs, thiopental sodium or propofol, is better in terms of clinical outcome of patients with RSE.
Description of the condition
RSE develops when patients become resistant to antiepileptic drugs with the passage of time. In hospital‐based treatment, it develops in 31% to 44% of patients with SE (Mayer 2002). Significant morbidity and mortality are associated with RSE. Failure to respond to antiepileptic drugs has led to the use of anaesthetic agents to control seizures. The popular anaesthetic agents are barbiturates, propofol, and isoflurane.
Description of the intervention
Anaesthetic agents have been used for the treatment of RSE. Barbiturates and propofol have been commonly used in this regard. However, most of the published literature is anecdotal. There is no consensus as to which of the two agents is better in terms of clinical outcome.
How the intervention might work
Thiopental sodium, a barbiturate, is a γ‐aminobutyric acid‐A (GABAA) agonist with possible actions on calcium channels (Rogowski 2004). Barbiturates have a prolonged duration of action, mainly due to their accumulation in the body. They are also known to produce hypotension during use. In contrast, propofol is gaining popularity because of its shorter duration of action and little tendency to accumulate in the body. Similar to barbiturates, propofol also produces hypotension, and reduces intracranial pressure and brain metabolic requirements (Marik 2004). Prolonged use of propofol as an infusion has been shown to result in potentially fatal cardiovascular collapse associated with lactic acidosis, hypertriglyceridaemia, and rhabdomyolysis, the so‐called "propofol infusion syndrome" (Zarovnaya 2007). Both agents are also N‐methyl‐D‐aspartate (NMDA) antagonists in vitro (Zhan 2001).
Why it is important to do this review
The current literature provides enough evidence to suggest that both thiopental sodium and propofol are effective in the treatment of RSE (Parviainen 2002; Van Gestel 2005). As both agents are associated with inherent side effects and complications, the choice of the agent is usually left at the discretion of the attending anaesthetist. There is a lack of evidence to suggest the superiority of one drug over the other. The aim of this Cochrane Review is to establish which of the two commonly used anaesthetic agents, thiopental sodium or propofol, is better suited for the treatment of RSE.
Objectives
To compare the efficacy, adverse effects, and short‐ and long‐term outcomes of refractory status epilepticus (RSE) treated with one of the two anaesthetic agents, thiopental sodium or propofol.
Methods
Criteria for considering studies for this review
Types of studies
We included all relevant RCTs or quasi‐RCTs, regardless of blinding. Diagnosis of RSE was based on any given standard definition specified in the articles and treatment consisting either of propofol or thiopental sodium. We excluded studies that did not define RSE, prior treatment with any other intravenous anaesthetic before treatment with thiopental sodium or propofol, and use of intermittent boluses of thiopental sodium or propofol for treating RSE.
Types of participants
We included individuals of any age and gender diagnosed with RSE of any aetiology.
Types of interventions
Patients receiving either thiopental sodium or propofol for the treatment of RSE, in addition to standard antiepileptic drugs used in status epilepticus (SE).
Types of outcome measures
Primary outcomes
-
Total control of seizures (after the first course of study drug).
-
In‐hospital mortality.
-
Length of intensive care unit (ICU) stay.
Secondary outcomes
-
Adverse events, such as infection, hypotension, and propofol infusion syndrome.
-
Duration of mechanical ventilatory support.
-
Duration of hospital stay.
-
Cognitive deficits.
-
Long‐term outcomes, such as dependence for daily activities (walking, eating, bathing, dressing, and toileting).
Search methods for identification of studies
Searches were run for the original review in May 2011. Subsequent searches were run in June 2011, March 2014, and March 2015. For the latest update we searched the following databases.
-
Cochrane Epilepsy Group Specialized Register (16 August 2016) using the search strategy outlined in Appendix 1.
-
Cochrane Central Register of Controlled Trials (CENTRAL) via the Cochrane Register of Studies Online (CRSO, 16 August 2016) using the search strategy outlined in Appendix 2.
-
MEDLINE (Ovid, 1946 to 16 August 2016) using the search strategy outlined in Appendix 3.
-
ClinicalTrials.gov (16 August 2016) using the search strategy outlined in Appendix 4.
-
South Asian Database of Controlled Clinical Trials (16 August 2016) using the search strategy outlined in Appendix 5.
Previously we searched IndMED (26 March 2015) using the search terms: 'Propofol AND (thiopental OR thiopentone) AND (epilepsy OR epileptic)', but this was not accessible at the time of the latest update.
We did not apply any language restrictions.
Data collection and analysis
Selection of studies
Using the results of the above searches, we screened all titles and abstracts for eligibility. Two review authors (HP and MK) independently performed this screening. We obtained and assessed the full articles of all eligible RCTs for relevance based on the pre‐planned checklist. Each author documented the reason for each trial that was excluded. We resolved any disagreement by discussion and decided on the inclusion or exclusion of the study. We compiled a list of all eligible trials. We recorded the selection process in sufficient detail to complete a PRISMA flow diagram' (Moher 2009).
Data extraction and management
Two review authors (HP and MK) planned to independently extract the data and assess the trial quality. We resolved any disagreement through consultation and discussion. In case of additional information being required, HP was chosen to contact the first author of the relevant trial. Data extracted from the included trial, Rossetti 2011, were total control of seizures, mortality, adverse events, long‐term outcome, and the duration of mechanical ventilation.
Assessment of risk of bias in included studies
Two review authors assessed the methodological quality of the eligible trials independently (HP and MK). We resolved any disagreement by discussion. We performed the assessment as suggested in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We judged the quality of the study on the basis of the following.
-
Random sequence generation.
-
Allocation concealment.
-
Blinding and outcome assessment.
-
Incomplete outcome data.
-
Selective reporting.
-
Any other bias.
We included a 'Risk of bias' table as part of the 'Characteristics of included studies' and a 'Risk of bias' summary figure (Figure 1), which details all of the judgements made for all included studies in the review.
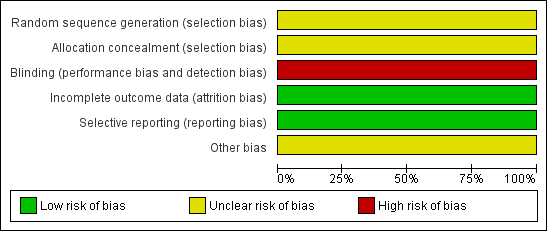
'Risk of bias' graph: review authors' judgements about each 'Risk of bias' item presented as percentages across all included studies.
Measures of treatment effect
We planned to record the number (percentage) of participants experiencing each categorical outcome, such as total control of seizures, mortality, adverse events, and long‐term outcomes. We planned to record the mean (standard deviation (SD))/median (range) for continuous outcomes, such as duration of mechanical ventilation, per randomised group. We carried out all primary analyses by 'intention‐to‐treat'. We used risk ratios (RRs) to measure the treatment effect for proportions (dichotomous outcomes) among the various outcomes. We planned to convert continuous data to mean differences (MDs) using the inverse variance method and calculate an overall MD. We planned to use a fixed‐effect model when we found no evidence of significant heterogeneity between studies, and a random‐effects or fixed‐effect model when heterogeneity was likely.
Unit of analysis issues
We planned to include only RCTs with parallel design in our review. The nature of the intervention here suggested that unit of analysis issues, such as those associated with cluster‐randomisation, were unlikely to arise. If we had included any cluster‐randomised studies we would have assessed the risk of bias following the suggestions in Section 16.3.2 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), and the approach to analysis suggested in the subsequent sections. We would have taken a similar approach to any cross‐over trials included.
Dealing with missing data
We contacted the first author of the relevant trial and collected the required information.
Assessment of heterogeneity
We planned to assess the clinical heterogeneity of included studies, defined as methodological diversity, such as distribution of patient characteristics (age, seizure type, and number of drugs taken at the time of randomisation) and trial factors (randomisation concealment, blinding, and loss to follow‐up). We planned to use the Q statistic to test the statistical heterogeneity between trials and the I2 statistic to assess the magnitude of heterogeneity (Higgins 2002).
Assessment of reporting biases
We planned to assess publication bias/small‐study effects in a qualitative manner, using a funnel plot. Due to limited data, we did not assess this bias.
Data synthesis
We quantitatively reviewed the included data and combined data by intervention, outcome and population using the Cochrane Collaboration's statistical software, Review Manager (RevMan 2014). We planned to assess statistical heterogeneity using the Chi2 test and consider P values of 0.05 or less as statistically significant. We planned to assess the level of inconsistency across the studies using the I2 statistic, where an I2 value greater than 50% indicates substantial heterogeneity. Had we found statistically significant heterogeneity that we could not readily explain, we would have assessed it using a random‐effects model.
Due to only one study meeting our inclusion criteria, we did not perform a meta‐analysis.
Subgroup analysis and investigation of heterogeneity
We planned to perform subgroup analyses for the following: age groups (children (< 14 years of age) and adults), gender, aetiology, and type of seizure (convulsive or non‐convulsive).
Due to limited data, we did not perform a subgroup analysis.
Sensitivity analysis
We planned to perform a sensitivity analysis to assess the influence of including studies judged to have low methodological quality and characteristics of the interventions; that is, the doses of propofol and thiopental used.
Due to limited data, we did not perform a sensitivity analysis.
Summary of findings
In this review update, we used the principles of the GRADE approach (Guyatt 2008) to assess the quality of the body of evidence associated with our primary outcomes (total control of seizures, in‐hospital mortality, length of ICU stay), and we constructed a Summary of Findings table (summary of findings Table for the main comparison) using the GRADE software. When using the GRADE approach, one appraises the quality of a body of evidence on the basis of the extent to which one can be confident that an estimate of effect or association reflects the item being assessed. Assessment of the quality of a body of evidence considers within‐study risk of bias (methodological quality), directness of the evidence, heterogeneity of the data, precision of effect estimates and risk of publication bias. For assessments of the overall quality of evidence for each outcome that included pooled data from RCTs only, we downgraded evidence from 'high quality' by one level for serious (and by two levels for very serious) study limitations (risk of bias), indirectness of evidence, serious inconsistency, imprecision of effect or potential publication bias.
Results
Description of studies
See: Characteristics of included studies.
Results of the search
Our searches yielded 48 references (13 from MEDLINE, 7 from CENTRAL, 2 from the Cochrane Epilepsy Group Specialized Register, 22 from the South Asian Database of Controlled Clinical Trials, and 4 from ClinicalTrials.gov). The search of IndMED yielded no references. After de‐duplication, 38 references remained. After further scrutiny, we identified only one study for inclusion in this review.
Figure 2 shows the results of our searches.

Study flow diagram.
Included studies
We included only one study in the review (Rossetti 2011). An overview of the study is given in Table 1. This study was supported in part by grants from the Swiss League against Epilepsy, AstraZeneca (Switzerland) and UCB (Switzerland).
| Study ID | Interventions | Screened (n) | Randomised (n) | Safety analysis (n) | ITT (n) | Finishing study (n) | [%] of randomised participants |
| I1 Propofol I2 Barbiturate (thiopental (n = 7) and pentobarbital (n = 3)) | I1 14 I2 10 | I1 14 I2 10 | I1 14 I2 10 | I1 14 I2 10 | I1 14 I2 9 | I1 100 I2 90 |
I1: intervention 1; I2: intervention 2; ITT: intention‐to‐treat; n: number.
The study conducted by Rossetti et al was a randomised, single‐blind, multicentre trial studying adults with RSE (Rossetti 2011). Patients received either propofol or barbiturates for control of seizures. Fourteen patients received propofol. In the barbiturates group, seven patients received thiopental sodium, and three patients received pentobarbital. The primary endpoint was the proportion of patients with RSE controlled after the first course of the study drug, and secondary endpoints included drug tolerability. The trial was terminated after three years with only 24 patients recruited of the 150 required. The trial was terminated before completion due to inadequate recruitment and the prolonged mechanical ventilation requirement identified in the barbiturate arm. Treatment‐related complications were comparable for both propofol and barbiturates.
Excluded studies
None.
Risk of bias in included studies
The study conducted by Rossetti et al was single‐blind (Rossetti 2011). The small sample size and lack of double‐blinding could have influenced the results.
Allocation
It is difficult to understand how allocation was done, as the authors have not commented on this in their paper. Personal communication with the authors failed to clarify this issue.
Blinding
This was a single‐blind study where only the patient was blinded, so there is a chance of performance bias and detection bias.
Incomplete outcome data
Attrition bias is unlikely, as there were no incomplete outcome data.
Selective reporting
Reporting bias is unlikely as the authors reported all the outcomes that they described in the methodology.
Other potential sources of bias
This study was supported in part by grants from the Swiss League against Epilepsy, AstraZeneca (Switzerland) and UCB (Switzerland).
Effects of interventions
Propofol versus thiopental sodium
Primary outcomes
Total control of seizures
There was no statistically significant difference between propofol and thiopental sodium in total control of seizures after the first course of the study drug; 6/14 patients versus 2/7 patients in the propofol and thiopental sodium groups, respectively (risk ratio (RR) 1.50, 95% confidence interval (CI) 0.40 to 5.61) (Analysis 1.1).
In‐hospital mortality
There was no statistically significant difference in mortality between propofol and thiopental sodium; 3/14 patients versus 1/7 patients in the propofol and thiopental sodium groups, respectively (RR 1.50, 95% CI 0.19 to 11.93). In the propofol group, deaths presumed to be in‐hospital were secondary to Creutzfeldt‐Jakob disease (day five), cardiac asystole (day six) and progressive brain tumour (day 11). In the thiopental sodium group, one patient died on day five, secondary to colic ischaemia. Deaths on days 21, 29, and 42 were due to paraneoplastic encephalitis, pneumonia, and sepsis, respectively, which are presumed to be out‐of‐hospital (Analysis 1.2).
Length of ICU stay
Data on this outcome were not reported.
Secondary outcomes
Adverse events
There was no statistically significant difference in adverse events between propofol and thiopental sodium (Table 2). Infection was seen in 7/14 patients versus 5/7 patients in the propofol and thiopental sodium groups, respectively (RR 0.70, 95% CI 0.35 to 1.41) (Analysis 1.3).
| Characteristic | |
| I1 I2 | Propofol Thiopental |
| Participants who died (n) Epilepsy‐related I1 Propofol I2 Thiopental | 0 0 |
| Participants who died (n) All causes I1 Propofol I2 Thiopental | 3 1 |
| Adverse events (n) I1 Propofol I2 Thiopental | 14 11 |
| Serious adverse events (n) I1 Propofol I2 Thiopental | 1 1 |
| Duration of ICU stay | Not reported |
| Duration of mechanical ventilation (median (range)) I1 Propofol I2 Thiopental | 17 days (5 to 70 days) 4 days (2 to 28 days) |
| Duration of hospitalisation | Not reported |
| Neurological deficits | Not reported |
| Cognitive deficits | Not reported |
| Haematological toxicity | Not reported |
| Liver toxicity | Not reported |
| Hypersensitivity or drug allergy | Not reported |
| Bronchopneumonia | Not reported |
| Other side effects | Not reported |
I1: intervention 1; I2: intervention 2; ICU: intensive care unit; n: number.
Hypotension during administration of study drugs and requiring use of vasopressors was seen in 7/14 patients versus 4/7 patients in the propofol and thiopental sodium groups, respectively (RR 0.87, 95% CI 0.38 to 2.00) (Analysis 1.3).
The other severe complication noted was non‐fatal propofol infusion syndrome in one patient (RR 0.50, 95% CI 0.04 to 6.86) (Analysis 1.3).
Duration of mechanical ventilatory support
The number of days of mechanical ventilation was greater in the thiopental sodium group when compared with the propofol group (median (range): 17 days (5 to 70 days) with thiopental sodium versus four days (2 to 28 days) with propofol).
Duration of hospital stay
Data on this outcome were not reported.
Cognitive deficits
Data on this outcome were not reported.
Long‐term outcomes
There was no statistical difference in the functional outcome between propofol and thiopental sodium at three months; 5/14 patients versus 3/7 patients in the propofol and thiopental sodium groups, respectively (RR 0.83, 95% CI 0.28 to 2.52) (Analysis 1.5).
Discussion
Our search identified only one study that addressed the issue of treatment of refractory status epilepticus (RSE) using thiopental sodium and propofol in a randomised, single‐blind, multicentric trial (Rossetti 2011). The trial was terminated before completion due to inadequate recruitment. Twenty‐four patients were recruited in five centres; 14 received propofol and seven received thiopental sodium. The primary endpoint, that is, control of seizure with first course of drug treatment, was achieved in 43% in the propofol group and 22% in the barbiturate group (seven patients received thiopental sodium and three patients received pentobarbital). The overall mortality was 43% and 34% in the propofol and barbiturate groups, respectively. However, the authors fail to report the in‐hospital mortality. Patients returning to baseline condition at the three‐month follow‐up were similar in the two groups. No information was provided on the length of intensive care unit (ICU) and hospital stay of the patients. However, days of mechanical ventilation were significantly more in the thiopental group. This could be due to the long elimination half‐life of the drug when compared with propofol. The fact that the trial was prematurely stopped could have introduced bias. At the same time, the under‐sampling resulted in loss of power to detect a difference between the two treatment arms.
This study confirms that RSE is a serious clinical condition carrying high morbidity and mortality. The authors of the study agree that a larger multicentric study is needed with a larger sample size and adequate funding to obtain conclusive results. The authors also suggest that a third treatment arm using midazolam as the treatment drug may be included in the study, which may address the issue of tolerability of the drugs, propofol and thiopental.
Summary of main results
Both propofol and thiopental sodium are broadly comparable in terms of seizure control, mortality, rate of complications, adverse events and long‐term outcomes in patients with refractory status epilepticus (RSE). The 95% confidence interval was wide and allowed for up to a more than two‐fold difference between the two drugs. Patients receiving thiopental sodium required more days of mechanical ventilation when compared with patients receiving propofol.
Overall completeness and applicability of evidence
There is a lack of evidence as to the efficacy of propofol and thiopental sodium when compared with each other in the treatment of RSE. We are unable to detect a difference between the two drugs due to methodological issues. There is a need for a large randomised controlled trial (RCT) for this serious condition.
Quality of the evidence
This review included a single trial, which was terminated prior to completion due to inadequate recruitment of patients (Rossetti 2011). This trial was not double‐blinded, introducing a high risk of bias. We judged the quality of the limited evidence available for this review to be low (summary of findings Table for the main comparison).
Potential biases in the review process
We followed the strict criteria for study selection and used a data extraction form for included studies as suggested in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We do not feel that any form of bias could have been introduced by the review authors during the preparation of this Cochrane Review.
Agreements and disagreements with other studies or reviews
To date this is the only eligible study available which has been included in our review. In a systematic review published in 2002 (Claassen 2002), the authors compared the efficacy of midazolam, propofol, and pentobarbital for terminating seizures in RSE patients. Considering all possible limitations, the authors concluded that pentobarbital was more effective than any other strategy suggested for treatment of RSE.
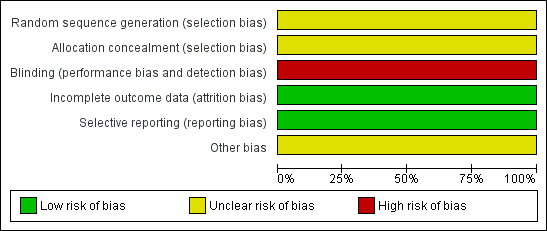
'Risk of bias' graph: review authors' judgements about each 'Risk of bias' item presented as percentages across all included studies.

Study flow diagram.

Comparison 1 Propofol versus thiopental sodium, Outcome 1 Total control of seizures.

Comparison 1 Propofol versus thiopental sodium, Outcome 2 In‐hospital mortality.

Comparison 1 Propofol versus thiopental sodium, Outcome 3 Adverse events.
| Study | Propofol group | Thiopentone sodium group |
| Rossetti 2011 | Median: 4 days | Median: 17 days |
| Rossetti 2011 | Range: 2 to 28 days | Range: 5 to 70 days |
Comparison 1 Propofol versus thiopental sodium, Outcome 4 Duration of mechanical ventilation.

Comparison 1 Propofol versus thiopental sodium, Outcome 5 Long‐term outcomes.
| Propofol compared to Thiopental sodium for the treatment of refractory status epilepticus | ||||||
| Patient or population: patients with the treatment of refractory status epilepticus | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Thiopental sodium | Propofol | |||||
| Total control of seizures | Study population | RR 1.5 | 21 | ⊕⊕⊝⊝ | ||
| 286 per 1000 | 429 per 1000 | |||||
| In‐hospital mortality | Study population | RR 1.5 | 21 | ⊕⊕⊝⊝ | ||
| 143 per 1000 | 214 per 1000 | |||||
| Length of intensive care unit (ICU) stay | Not reported | Not reported | NA | NA | NA | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Single blinded study: we downgraded one level for risk of bias | ||||||
| Study ID | Interventions | Screened (n) | Randomised (n) | Safety analysis (n) | ITT (n) | Finishing study (n) | [%] of randomised participants |
| I1 Propofol I2 Barbiturate (thiopental (n = 7) and pentobarbital (n = 3)) | I1 14 I2 10 | I1 14 I2 10 | I1 14 I2 10 | I1 14 I2 10 | I1 14 I2 9 | I1 100 I2 90 | |
| I1: intervention 1; I2: intervention 2; ITT: intention‐to‐treat; n: number. | |||||||
| Characteristic | |
| I1 I2 | Propofol Thiopental |
| Participants who died (n) Epilepsy‐related I1 Propofol I2 Thiopental | 0 0 |
| Participants who died (n) All causes I1 Propofol I2 Thiopental | 3 1 |
| Adverse events (n) I1 Propofol I2 Thiopental | 14 11 |
| Serious adverse events (n) I1 Propofol I2 Thiopental | 1 1 |
| Duration of ICU stay | Not reported |
| Duration of mechanical ventilation (median (range)) I1 Propofol I2 Thiopental | 17 days (5 to 70 days) 4 days (2 to 28 days) |
| Duration of hospitalisation | Not reported |
| Neurological deficits | Not reported |
| Cognitive deficits | Not reported |
| Haematological toxicity | Not reported |
| Liver toxicity | Not reported |
| Hypersensitivity or drug allergy | Not reported |
| Bronchopneumonia | Not reported |
| Other side effects | Not reported |
| I1: intervention 1; I2: intervention 2; ICU: intensive care unit; n: number. | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total control of seizures Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2 In‐hospital mortality Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Infection | 1 | 21 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.35, 1.41] |
| 3.2 Hypotension | 1 | 21 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.38, 2.00] |
| 3.3 Other serious complications | 1 | 21 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.04, 6.86] |
| 4 Duration of mechanical ventilation Show forest plot | Other data | No numeric data | ||
| 5 Long‐term outcomes Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |

