Educación del paciente en el tratamiento de la cardiopatía coronaria
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en espera de evaluación
Referencias de los estudios en curso
Referencias adicionales
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT | |
| Participants | N Randomised: 636 (Intervention (Rx) and control group N not reported) Trial Recruitment period: N/A When Randomised: Not Reported (N/R) Recruitment from: Review of outpatient cardiology clinics in four hospitals in Southern Eastern Michigan. CV Diagnosis (% of Patients (pts)): Post (Myocardial infarction) MI: 45% Angina: 57% Post CABG: 32% Post PTCA: 25% These groups are not mutually exclusive. Mean Age: 69.6 yrs (60‐93) Percentage male: 59% Inclusion criteria: >60 yrs; diagnosed cardiac disease (arrhythmia, angina, MI, valvular disease); treated daily by at least one heart medication; seen by a physician at least once every six months. Exclusion criteria: "If physicians felt that they wouldn't be able to benefit fully for the program due to medical reasons (e.g. terminal illness, memory loss, significant hearing loss)" | |
| Interventions | Description / Content: Take PRIDE Teaching Modalities: Videotape, guidebook, group teaching. Who taught by: Health educator Dose: Duration 4 weeks No of sessions 4 Length of session 2 hours Involvement of Family: N/R Time of start after event: six months to 20 yrs after initial diagnosis Follow up further reinforcement N/R Theoretical basis for intervention Yes Problem Identification, Researching one's routine, Identifying a management goal, Developing a plan to reach it, Expressing one's reactions and Establishing rewards for making progress. | |
| Outcomes | HRQofL‐ Sickness Impact Profile Withdrawal from Rx & control group | |
| Follow up | 6, 12 and 18 months | |
| Control | Usual care consisted of: "Seeing their physicians at the intervals specified by the particular physician and receiving any information or communications that would be provided as part of routine care in that setting." | |
| Country | USA | |
| Notes | Patients with arrhythmias and CCF also included. The following paper produced from the results of the same trial were used to inform the data collected: Clark 1992 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Use of random number table" |
| Allocation concealment (selection bias) | Low risk | "As the numbers were generated, each was placed in a sealed envelope. They were stored in a locked drawer in my office. As participants completed their baseline interview I was given their names and opened the next envelope in the numerical sequence." Correspondence with author J. Dodge. |
| Blinding (performance bias and detection bias) | Low risk | "Data collectors and data analysts were blinded. The health educators who delivered the intervention obviously knew who had been randomized to the intervention, but had no involvement with the collection of quantitative evaluation data at baseline or follow‐up." Correspondence with author J. Dodge. |
| Incomplete outcome data (attrition bias) | Unclear risk | 455 out of 636 had complete data at 18/12. "No appreciable difference in dropout rates between the intervention and control groups were found." Similarity of demographic details of those loss to follow up not discussed. |
| Selective reporting (reporting bias) | Low risk | All outcomes listed in the methods are reported in the results. |
| Groups balanced at baseline | Low risk | "There were no baseline differences between the experimental and control groups". |
| Intention to treat analysis | High risk | "Data analyses reported....participants who attended at least one of the four sessions." |
| Comparative care? | Low risk | Other than the stated intervention both groups appeared to have been treated similarly. |
| Methods | RCT | |
| Participants | N Randomised: 571 (n Rx 309; n control 262) ‐ 55:45 allocation ratio Trial Recruitment period: Not Reported When Randomised on agreeing to participate in study. Median of 13 yrs since initial cardiac diagnosis (Range 6 months ‐ 20 years) Recruitment from: Physician practices affiliated with six medical centers in Southeastern Michigan. CV Diagnosis (% of pts): Post MI 39% Angina 45% Post CABG 26% Post PTCA 29% These groups are not mutually exclusive. Mean Age: 71.9 yrs (Range 60‐93) Percentage male: 0% Inclusion criteria: >60; Female; Cardiac disease treated daily with at least one medication; Cardiac disease can be arrhythmia, angina, MI or valvular disease Exclusion criteria: "If physicians felt they could not benefit fully from the program due to medical reason (e.g. terminal illness or significant hearing loss)" | |
| Interventions | Description / Content: Specific information related to heart disease in women signs and symptoms of heart disease, effective communication with clinicians. Teaching Modalities: Classroom group sessions (Groups 6‐8 women). Workbook for use at home on the intervening days. Handouts summarising classroom sessions, daily self‐monitoring logs. Weekly telephone call during program period. Who taught by: Trained health educators and peer leaders (selected graduates from the program that received extra training) Dose: Duration 4 weeks No of sessions weekly (4) Length of session 2‐2.5hrs Involvement of Family: N/R Time of start after event N/A Follow up further reinforcement letter 3 months after program and a telephone call 6 months after Theoretical basis for intervention Yes ‐ PRIDE Problem Identification, Researching one's routine, Identifying a management goal, Developing a plan to reach it, Expressing one's reactions and Establishing rewards for making progress. | |
| Outcomes | Total Mortality HRQofL ‐ Sickness Impact Profile Adverse Events (Withdrawal from Rx group) Hospitalisations (number of admissions, number of inpatient days, hospital inpatient charges) (Wheeler 2003) Cost‐effectiveness (Wheeler 2003) | |
| Follow up | 12 months and 24 months (economic data (Wheeler 2003)). | |
| Control | Usual care was determined by individual responsible physicians who were not aware of group allocation. | |
| Country | USA | |
| Notes | The following paper produced from the results of the same trial were used to inform the data collected: Wheeler 2003 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...women were assigned, by use of random number tables (Clark 2000)" |
| Allocation concealment (selection bias) | Unclear risk | Not Reported |
| Blinding (performance bias and detection bias) | Low risk | "Interviewers were blind to women's participation in the program. (Clark 2000)" |
| Incomplete outcome data (attrition bias) | Low risk | Table detailing withdrawals |
| Selective reporting (reporting bias) | Low risk | Outcomes in methods reported in results |
| Groups balanced at baseline | High risk | Demographically similar but statistically significant differences in baseline disease symptoms and weight. |
| Intention to treat analysis | Low risk | Data was analysed in two different phases, one "an analysis of all women randomized" the other "all program women who attended one or more program sessions (Clark 2000)" |
| Comparative care? | Low risk | "In an effort to assure similar care to both the program and the control groups, no feedback about individual participants was provided to medical or nursing staff. The clinical staff had no knowledge of which patients had agreed to participate in research (Clark 2000)." |
| Methods | RCT ‐ 3 groups | |
| Participants | N Randomised: 575 (n Rx Self Directed: 201; n Rx Group Format: 190; n control: 184) Trial Recruitment period: N/A ‐ list compiled from physicians patient rota. When Randomised: After collecting baseline data. Recruitment from: Five hospital sites in Southeastern Michigan. CV Diagnosis (% of pts): Post MI 42% Angina 38% Post CABG ‐ N/R Post PTCA ‐ N/R These groups are not mutually exclusive. Mean Age: 72.8 Percentage male: 0% Inclusion criteria: >60 years; diagnosed cardiac condition (arrhythmia, angina, MI, congestive heart failure, valvular disease); treated by daily heart medication; seen by a physician in the last year; living within 1 hr drive of the study site. Exclusion criteria: If not able to fully participate because of medical reasons. | |
| Interventions | Description / Content: Content of the materials used in both groups was identical. Both 6 units. Teaching Modalities ‐ Self Directed: Single orientation session then: Dose: Duration program at home in six weeks The self directed group also have an instructional video tape that gives examples of group discussions. Teaching Modalities ‐ Group: 6‐8 women. Dose: Duration 6 sessions No of sessions weekly Length of session 2‐2.5 hrs Both groups received weekly telephone calls from a heath educator during the study period. Who taught by: Trained health educators and peer leaders Involvement of Family: N/R Time of start after event N/A Follow up further reinforcement. 3 monthly ‐ both groups receive news letter 6 months ‐ Group attend a reunion. Self directed participants receive an in depth telephone call. Theoretical basis for intervention: Yes, described in separate paper. | |
| Outcomes | Total Mortality HRQofL ‐ Sickness Impact Profile (SIP) Withdrawal from treatment | |
| Follow up | 12 and 18 months | |
| Control | "see their physician on the routine schedule and receive any information that would normally be provided as part of regular care in the practice." | |
| Country | USA | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...complied using,...book of random numbers." |
| Allocation concealment (selection bias) | Low risk | "Sealed opaque and sequentially numbered envelopes." |
| Blinding (performance bias and detection bias) | Low risk | "Those assessing outcomes were blinded to the group allocation unless the participant happened to reference program participation during the follow‐up telephone interviews or at the physical assessment visit." Correspondence with author, J. Dodge. |
| Incomplete outcome data (attrition bias) | Low risk | Clear description of withdrawals from trial given. |
| Selective reporting (reporting bias) | Low risk | Sickness Impact Profile numerical scores were not individually reported as no significant difference was found. These were subsequently made available through correspondence with the author, J Dodge. |
| Groups balanced at baseline | Low risk | Described in table one. "no significant differences among study conditions....." |
| Intention to treat analysis | Low risk | "Analyses were carried out using the women as they were randomized to each of the three study conditions" |
| Comparative care? | Low risk | "In an effort to ensure similar care to all participants, no feedback about individual study participants was provided to health care personnel at the study sites." |
| Methods | RCT | |
| Participants | N Randomised: 688 (n Rx 342 n control 346) Trial recruitment period: Data collected between 1990 and 1993. When randomised: Not reported Recruitment from: 18 General Practices in Greater Belfast CV Diagnosis (% of pts): Angina 100% Mean age: Rx 62.7 Control 63.6 Percentage male: 59% Inclusion criteria: ≥6 month history of angina diagnosed by classical history. Exclusion criteria: No other severe illness | |
| Interventions | "Personal health education intervention” Description / Content: "Patients in the intervention group were given practical relevant advice regarding cardiovascular risk factors. They were reviewed at four monthly intervals and given appropriate health education (Cupples 1994).” "Visited by a health visitor, whose brief was discuss ways of living more easily with their disease and ways in which risks of further events might be reduced (O'Neill 1996)." "The education involved giving information which was tailored to the individuals' coronary risk factors and the use of medication (Cupples 1996).” Teaching modalities: Individual one to one visits Who taught by: health visitor Dose: Duration 2 years No of sessions 6 visits (every 4 months for 2 years) Length of session Not Reported Involvement of Family: No Time of start after event N/A Follow up further reinforcement: Not following 2 year intervention Theoretical basis for intervention none stated | |
| Outcomes | Total Mortality Cardiovascular related mortality Hospitalisations recorded as part of cost analysis (not independently reported) (O'Neill 1996) HRQofL (Nottingham Health Profile Questionnaire) (Cupples 1996) Adverse Events (Withdrawal from Rx group) Cost Analysis (O'Neill 1996) | |
| Follow up | Patients reviewed at 2 years (Cupples 1994; O'Neill 1996) and 5 years (Cupples 1999) | |
| Control | Usual care consisted of: Had the same screening interview as the intervention group but once randomised to control had no further intervention. | |
| Country | Northern Ireland, UK. | |
| Notes | The following papers produced from the results of the same trial were used to inform the data collected: Cupples 1996; Cupples 1999; O'Neill 1996 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "generated by a computer program using permuted blocks (Cupples 1996)." |
| Allocation concealment (selection bias) | Low risk | "The health visitor opened an opaque, sealed, and numbered envelope containing the allocation (Cupples 1994)." |
| Blinding (performance bias and detection bias) | Low risk | "After 2 years both groups were reviewed by a research worker who had not previously been involved with the subjects (Cupples 1994)." At five year follow‐up: "nurse (performing interview) was blind to trial group allocation (Cupples 1999)." |
| Incomplete outcome data (attrition bias) | Low risk | Detailed report of drop outs and losses to follow up reported. Cupples 1994 Yes Cupples 1996 No O'Neill 1996 No Cupples 1999 No |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes listed in methods were reported in methods. |
| Groups balanced at baseline | Low risk | "No significant differences were found between the two groups at baseline (Cupples 1994)." |
| Intention to treat analysis | Low risk | "We also analysed the data in an intention to treat basis, with baseline or adjusted values being substituted for missing data, but this did not alter the conclusions (Cupples 1999)." |
| Comparative care? | Low risk | Both groups received same usual care and only difference between groups was the educational intervention. |
| Methods | RCT | |
| Participants | N Randomised: 46,606 (n Rx ‐ 33,267 n Control ‐ 13,339) Trail Recruitment period: All Florida Medicare beneficiaries enrolled in Medicaid as of March 2006 who met eligibility criteria. When Randomised "When eligible beneficiaries are identified." Recruitment from: Medicare database CV Diagnosis (% of pts): 69% Coronary Artery Disease (Not further defined) 10% in combination with heart failure 19% in combination with diabetes 12% with all three diagnoses Mean Age: 68.4 yrs Percentage male: 34% Inclusion criteria: Enrolled in Medicare and receiving Medicard benefits; have congestive cardiac failure, diabetes or coronary artery disease. Exclusion criteria: Psychiatric inpatient therapy of more than 14 consecutive days in the prior 12 months; long term nursing home residence | |
| Interventions | Description / Content: The education component: "Nurse case managers provided education to patients on the recognition of signs and symptoms of their disease; how to monitor vital signs; the cause of diseases; how to better adhere to diet, exercise, and medication regimes; and strategies to cope with chronic illness. When providing education to patients, nurses use pre‐designed scripts. Geared towards educating patients on how to attain clinical goals." Teaching Modalities: "The intervention is primarily telephonic, but also had an in‐person component." Who taught by: Individually assigned "nurse care manager" Dose: Duration ‐ 18 months No of sessions ‐ patients has 1.1 contacts per active month, on average. Length of session‐ N/R Involvement of Family: ‐ N/R Time of start after event ‐ N/A Follow up further reinforcement ‐ Intervention continued until end of follow up period Theoretical basis for intervention ‐ N/R | |
| Outcomes | Hospitalisations ‐ Emergency and inpatient use HRQofL [Survey of selected 613 enrollees only and claims based quality of care measures] Cost Analysis | |
| Follow up | 6 months, 1 yr and 18 months | |
| Control | Usual care consisted of: Not Reported | |
| Country | USA | |
| Notes | Analysed 1st and second 6 month periods, first year and 18 months. Population based study that only a relatively small proportion of those assigned to the intervention group actually actively continued to participate in. Therefore treatment effect may be difficult to statistically demonstrate. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | Divided patients in to mediated ‐ those that fully engaged with the intervention and instructional ‐ those that were less that fully engaged but did not opt out. Breakdown of mediated patients demonstrated in a table. |
| Selective reporting (reporting bias) | Low risk | Primary outcomes stated in methods were reported in the results. |
| Groups balanced at baseline | Low risk | Detailed table (Table 4) of pre‐enrollment characteristics showed no statistically significant differences seen. Authors reported that there was a difference in that the treatment group utilised health services 5% more in 2 year run up period to the trial (not statistically significant) |
| Intention to treat analysis | Low risk | "intention of treat study design." |
| Comparative care? | High risk | Education only part of the intervention: "intervention components include patient assessment, care planning, routine nurse monitoring, patient self‐monitoring, education, care co‐ordination, and service arrangement." Physicians were alerted to "important changes in patients' health." |
| Methods | RCT | |
| Participants | N Randomised: 288 (n Rx: 156 n control: 132) Trail Recruitment period: Sept 2001 to Sept 2005 When Randomised: After hospitalisation of at least 2 days Recruitment from: 413 patients in Haukeland University Hospital, Bergen, Norway CV Diagnosis (% of pts): Post Myocardial Infarction 100% Mean age: 60 Percentage male: 81% Inclusion criteria: All patients with confirmed Acute MyocardiaI Infarction (AMI) and admitted to the hospital Exclusion criteria: Severe co‐existing chronic disabling disease; Nursing home resident; unable to receive telephone calls; unable to fill in questionnaires; if expected to have CABG in that admission; In the first year of the study >80 yr olds were excluded, after the first year they were included. | |
| Interventions | Description / Content: " structured intervention encompassing telephone follow up and an open telephone line" "to provide patients with information, education and support on the basis of individual needs. To provide patients with information about what are common questions after AMI and encourage elaboration on the issues if desired. One issue was addressed in each call." (Detailed list of topics covered itemised in paper) Teaching Modalities: Telephone follow up Who taught by: "nurses with interests and experience in counselling and providing information to patients with ischaemic heart disease." Dose: Duration 6 months (could stop earlier if requested) but encouraged to have at least the first 5 months intervention No of sessions weekly first 4 weeks, then weeks 6,8,12 and 24. 8 sessions in total Length of session as long as required (mean telephone call 6.88 mins (SD 3.89)) Involvement of Family: [telephone] "Lines were open to patients and relatives/relations" Time of start after event: On discharge following the event Follow up further reinforcement: none Theoretical basis for intervention: "intervention was developed on the basis of the Lazarus and Folkmans theory on stress, appraisal and copy, principles about patient education, findings from previous research and according to guideline recommendations." | |
| Outcomes | HRQofL (SF36) Rehospitalisation Mortality | |
| Follow up | 6 and 18 months | |
| Control | Usual care consisted of: "Managed in accordance with current clinical practice. One visit to a physician at the outpatient clinic 6‐8 weeks after discharge, and subsequent visits to the patient's general practitioner." | |
| Country | Norway | |
| Notes | The following paper produced from the results of the same trial were used to inform the data collected: Hanssen 2009 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A simple randomization procedure using a computer‐generated list of random numbers" |
| Allocation concealment (selection bias) | Low risk | "..group allocation in sealed opaque envelopes prepared by the researcher." |
| Blinding (performance bias and detection bias) | Unclear risk | Not clear from as to whether researchers were blinded to group allocations. |
| Incomplete outcome data (attrition bias) | Low risk | CONSORT diagram of trial flow reported with details of drop out and loss to follow up |
| Selective reporting (reporting bias) | Low risk | Outcomes in methods reported in results. |
| Groups balanced at baseline | Low risk | "No statistically differences were found" in baseline characteristics |
| Intention to treat analysis | Low risk | Although intention to treat analysis not explicitly stated, the groups were analysed according to original random allocation. |
| Comparative care? | High risk | Intervention included both education and counselling ‐ psychological based intervention. "Providing emotional support and alternative coping strategies". Which was not received by control group |
| Methods | RCT | |
| Participants | N Randomised: 203 (n Rx: 101 & n control 102) Trial Recruitment period: August 2003 to 2004 When Randomised: Not stated Recruitment from: All N=502 elective CABG admitted to a single hospital CV Diagnosis (% of pts): Post CABG 100% Mean Age: 62 Percentage male: 89.5% Inclusion criteria: All elective CABG patients 18‐80 yrs Exclusion criteria: More than 3 hrs driving distance | |
| Interventions | "A psychoeducative intervention" Description / Content: Structured information and psychological support for the topics of angina symptoms, medications, sexuality, anxiety, and depression. Material developed for the study. Teaching Modalities: Home based, 2 x 1‐hr home visits at 2 & 4 post CABG. Who taught by: "Masters prepared critical care nurse with 12 years experience" Dose: Duration 4 weeks No of sessions 2 (at 2 and 4 weeks) Length of session 1 hr Involvement of Family: Not stated Time of start after event: Post CABG 2 and 4 weeks Follow up further reinforcement: No Theoretical basis for intervention: None stated | |
| Outcomes | HRQofL ‐ SF‐36 and Seattle Angina Questoinnaire (SAQ) | |
| Follow up | 6‐months post CABG | |
| Control | Usual care consisted of: "Patients in the intervention group and the control group received standard discharge care that involved a non‐standardised short talk with the nurse/doctor." | |
| Country | Norway | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Statistician made the randomisation codes by using a computer program." |
| Allocation concealment (selection bias) | Low risk | "a secretary created sealed opaque envelopes containing individual codes with sequential numbers." |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | Clear table demonstrating patients excluded and the attrition. All accounted for at the end of the trial. Minimal incomplete data from responses in each group in both questionnaires e.g. "number of respondents for each subscale and each measurement point ranged between 74 and 92 for each group" |
| Selective reporting (reporting bias) | Low risk | All stated outcomes SAQ and SF‐36 at 6 months reported |
| Groups balanced at baseline | Low risk | Baseline characteristics "did not differ significantly between groups". |
| Intention to treat analysis | Low risk | ITT not explicitly stated. Reported patient flow chart suggests that groups analysed according to original random allocation. |
| Comparative care? | Low risk | "Patients in the intervention group and the control group received standard discharge care that involved a non‐standardised short talk with the nurse/doctor." |
| Methods | RCT | |
| Participants | N Randomised: 87 (n Rx 46; n control 41) Recruitment period: Recruited Feb 1993 and Dec 1995. When Randomised: not reported Recruitment from: 151 consecutive referrals to cardiology outpatients of 1 hospital. CV Diagnosis (% of pts): Post PTCA 100% Average (SD) Age: 53 (7) Percentage male: 75% Inclusion criteria: "at least one coronary stenosis suitable for PTCA and at least one additional clinically insignificant coronary artherosclerotic lesion that could be evaluated by quantitative computerized angiography Hofman‐Bang 1999"; employed; able to perform bike test Exclusion criteria: Abscence of other disease that would prevent completion of programme; age >65; unemployed | |
| Interventions | Description / Content: 4 week residential stay, which was focused on health education and the achievement of behaviour change. During the first year of follow‐up, a maintenance programme included regular contacts with a nurse...The second year did not contain any active intervention. Teaching Modalities: 4 weeks residential stay (group of 5‐8) Seminars/Lectures/Discussion /Skills (e.g. food preparation/ relaxation). Then 11 month structured maintenance programme. Nurse led. Who taught by: Individualisation of material by trained nurse ("personal coach (Lisspers 1999)") Dose: Duration ‐12 months No of sessions ‐ Not reported Length of session ‐ 4 weeks then not reported Involvement of Family: Not reported Time of start after event Not reported Follow up further reinforcement yes for 1 year ("regular follow‐up contacts between the patient and his/her personal coach for verbal feedback, problem‐solving, and replanning discussions when needed (Lisspers 1999)"). Theoretical basis for intervention stated no | |
| Outcomes | Total Mortality, Total CV Events, non fatal MI Total Revascularisations (both CABG and PTCA) Hospitalisations HRQofL: Angina Pectoris Quality of Life Questionnaire (AP‐QLQ) | |
| Follow up | 12, 24, 30 and 60 months | |
| Control | Usual care consisted of: PTCA, one outpatient visit. Then referral to family physician. | |
| Country | Sweden | |
| Notes | In direct communication with the author he would describe the program as a "behaviour change program" primarily and he viewed patient education as "secondary and supportive to behavior change procedures." The following papers produced from the results of the same trial were used to inform the data collected: Hofman‐Bang 1999; Lisspers 2005 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not Reported. |
| Allocation concealment (selection bias) | Unclear risk | Not Reported |
| Blinding (performance bias and detection bias) | High risk | Not reported in the paper but from direct communication with the author it was confirmed that those analysing the results were not blinded to the group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | "Two patients in the intervention and four in the control group were excluded soon after randomization at their own request leaving 87 subjects as the final patient population Hofman‐Bang 1999." |
| Selective reporting (reporting bias) | Low risk | All stated rehabilitation and secondary prevention endpoints in methods documented in results. |
| Groups balanced at baseline | Low risk | Patient characteristics table and statistical comparison included. Apart from beta‐blocker usage, groups not different. |
| Intention to treat analysis | Low risk | Intention to treat (ITT) not stated in the test but calculations stated in the results appear to be analysed according to original allocation worked out on an ITT basis. |
| Comparative care? | High risk | As well as education: intervention group received stress management, exercise, smoking habits and dietary advice. |
| Methods | RCT | |
| Participants | N Randomised: 182 (intervention ("rehabilitation": n=60; n control I ("counselling programme" n= 61 control II ("usual care"): 61) Trial Recruitment period: Feb 1981 to May 1984 When Randomised: 30‐60 days post MI Recruitment from: 1308 patients with suspected MI CV Diagnosis (% of pts): Post MI 100% Age: Mean Age Control: 51, Intervention: 51 Percentage male: 100% Inclusion criteria: MI < 65 yrs Exclusion criteria: Contraindicaton to exercise: recent stroke, disability lower limbs, uncontrolled heart failure, severe rhythm disturbances, SBP > 250 mmHg, severe angina pectoris, severe hypotension, chest pain or low HR on exercise. | |
| Interventions | Description/Content: Education/counselling: Recommendations on cardiovascular risk factors and exercise‐ control CVS risk factors. Teaching Modalities: One group session Plus individual session with Cardiologist ‐ full medical and personal adjusted recommendations Who taught by: (the group session) Cardiologist, psychiatrist, nutritionist & physiotherapist Dose: Duration Not reported No of sessions one Length of session Not reported Involvement of Family: " spouse/partner encouraged to attend" Time of start after event Not reported Follow up further reinforcement ‐ no Theoretical basis for intervention stated‐ no | |
| Outcomes | Total Mortality Cardiovascualar mortality Other cardiovascular events Total Revascularisations (CABG) | |
| Follow up | 12 & 24 months | |
| Control | Usual care consisted of: "Referral to private practitioner and/or cardiologist" | |
| Country | France | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | Reasons for exclusions pre‐randomisation given. "Exclusion of women and men above the age of 65 alone contributed to almost 60% of all reasons for non‐eligibility...the reasons for non‐inclusion in the other patients were either inability to perform the exercise test or major ECG abnormalities." "No patient was lost to follow‐up" but number actually completing interventions not reported. Results for all those randomised, reported for non‐fatal events and mortality outcomes. |
| Selective reporting (reporting bias) | Low risk | All outcomes listed in methods reported in results. |
| Groups balanced at baseline | Low risk | "No statistically significant differences were observed among the treatment groups for any of the tested variable." |
| Intention to treat analysis | Low risk | "The analysis followed the intention‐to‐treat principle; patients were counted in the groups in which they were allocated" |
| Comparative care? | Low risk | Intervention and control group received identical care other than the intervention stated. |
| Methods | RCT | |
| Participants | N Randomised: 18,402 n Rx 9,427, n control 8,975 Trial Recruitment period: April 2002 and June 2005 When Randomised Recruitment from: "Eligible‐fee for service Medicare patients...who volunteers to participate" CV Diagnosis (% of pts): 61% CHD, 48% congestive heart failure Age Not Reported Percentage male: 45% Inclusion and Exclusion criteria: "Each program was allowed to define within broad boundaries its own target population and exclusion criteria, and designed its intervention accordingly." 10/15 sites required a hospital admission within the previous year, 4/15 sites excluded <65 yrs old & 14/15 excluded "terminal illness and conditions that affected their ability to learn self management" | |
| Interventions | Description / Content:"Nurses provided patient education and monitoring." The Interventions varied and are described in detail in Brown 2008. "All but 1 of the programs educated patients to improve adherence to medication, diet, exercise, and self‐care regimens, mostly through the nurses conveying factual information." Teaching Modalities: Who taught by: Care co‐ordinator. Licensed or registered nurses (4 programs required a BSc level qualification in nursing studies) Dose: Duration: on average 30 months eligibility (range 18‐31 months) No of sessions: 11 programs: 1‐2.5 times / month: 3 programs 4‐8 times / month. Other programs did not record contact frequency. Length of session: Not Reported Involvement of Family: Not Reported Time of start after event Not Reported Follow up further reinforcement: N/A Theoretical basis for intervention: Not Reported | |
| Outcomes | Hospitalisations HRQofL Cost Analysis ‐ monthly Medicare expenditure | |
| Follow up | At least 1 year. Mean F/U 51 months. | |
| Control | Not reported. | |
| Country | USA | |
| Notes | The following paper produced from the results of the same trial were used to inform the data collected: Brown 2008 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly generated concealed 4‐digit "strings". |
| Allocation concealment (selection bias) | Low risk | Randomised assignment was returned via the trial Web site. |
| Blinding (performance bias and detection bias) | High risk | "Because of the nature of the intervention, no individuals were blinded to which group participants were randomized."Peikes 2009 |
| Incomplete outcome data (attrition bias) | Unclear risk | "Observations are weighted by the number of months in the follow‐up period that the same member meets eligibility requirements."Peikes 2009. A full breakdown of periods that patients were eligible is not given. |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in the methods are reported in the results. |
| Groups balanced at baseline | Low risk | "Across all of the 15 programs and the baseline characteristics the treatment and control groups differed significantly on only 11 of the 255 comparisons at the p<0.05 level, less than the expected number of statistical significant differences that would be observed by chance."Peikes 2009 |
| Intention to treat analysis | Low risk | "Effects were calculated using .... an intention to treat design."Peikes 2009 |
| Comparative care? | High risk | "7 of the programs used behaviour change models. 14 programs attempted to improve communication between patients and physicians."Peikes 2009 Education was not the only intervention that the treatment groups received. |
| Methods | RCT | |
| Participants | N Randomised: 100 (n Rx = 50 & n control = 50) Trial Recruitment period: NR (total study period: March 2004 ‐ January 2006) When Randomised NR Recruitment from: Ambulatory patients of the Moscow polyclinic Nr112 (n=100) with stable angina of 1‐3 functional class, aged between 47‐65 CV Diagnosis (% of pts): Post MI = 52% in Rx; 48% in control Angina = all Post CABG = 14% in Rx; 8% in control Post PTCA = 18% Rx; 14% in control (transluminal balloon angioplasty) Age: Mean 59.9 (SD 0.4) Percentage male: 60% in Rx; 58% in control Inclusion criteria: Diagnosis of CHD, stable angina, age <65 Exclusion criteria: acute coronary syndromes and acute cerebrovascular disorders in 6 months before selection; patients with severe somatic disorders (life‐threatening arrhythmia, heart failure (3‐4 functional class), kidney or liver failure; decompensated diabetes, severe bronchial asthma), psychiatric disorders and alcoholic, narcotic and prescription drug addictions. | |
| Interventions | Description / Content: A course at the "Health school for CHD patients"; Structured programme of 6 sessions (90 min each, twice a week), during which 1 or 2 risk factors were discussed. Evaluation of knowledge about the disease and risk factors after the course. Teaching Modalities: NR Who taught by: NR Dose: twice a week Duration: 3 weeks No of sessions: 6 sessions Length of session: 90 min Involvement of Family: NR Time of start after event Follow up further reinforcement NR Theoretical basis for intervention: Organisation of Health Schools for CHD patients in practical health‐care setting. Organisational‐methodical letter. Appendix 2. M 2003 | |
| Outcomes | HRQofL: SF‐36 | |
| Follow up | 6 and 12 months post randomisation | |
| Control | Usual care (for all patients) consisted of 3 visits during a 12 months follow‐up. 1st visit ‐ evaluating inclusion criteria, giving informed consent, randomisation, evaluation of knowledge about the disorder and risk factors; clinical examination; blood test for lipids and glucose; psychological survey. 2 and 3rd visits ‐ 6 and 12 months after the start of the study; consisted of clinical examination (blood test for lipids and glucose), evaluation of knowledge and psychological survey. | |
| Country | Russia | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Likely, description of the results in text indicates missing data but no breakdown given. |
| Selective reporting (reporting bias) | Low risk | All outcomes are accounted for in the results in either table, graphical or text format. |
| Groups balanced at baseline | Low risk | Groups at baseline were comparable. |
| Intention to treat analysis | Unclear risk | Not reported |
| Comparative care? | Low risk | Control group received standard care only. |
| Methods | RCT | |
| Participants | N Randomised: 104 (n Rx: 53; n control: 51) Trail Recruitment period: 10 months When Randomised: Recruitment from: 46 Outpatient facilities throughout SW Virginia) or through news paper adverts (number of patients screened prior to randomization not reported) CV Diagnosis (% of pts): "diagnosed coronary heart disease, congestive heart failure or both" Breakdown not reported. Mean age: 62 Percentage male: 75% Inclusion criteria: Diagnosis of CHD or CHF or both Approval of either primary care physician or cardiologist Needs access to the Internet Exclusion criteria: None reported | |
| Interventions | Description / Content: Log in on to the site at least once a week for 30 mins, communicating with a case manager through a secure form of e‐mail, completing education modules assigned by the case manager, and entering data into progress graphs. They had the opportunity to use an on‐line discussion group. There were material incentives for active participation. Also dietary input Teaching Modalities:"interactive, multiple choice, self tests followed by feedback.” Who taught by:"Case Managers” and dieticians Dose: Duration: 6 months No of sessions: one/week Length of session: at least 30 mins Involvement of Family: Not stated Time of start after event: Not relevant Follow up further reinforcement: No Theoretical basis for intervention: None stated | |
| Outcomes | Total CV Events (fatal / none fatal MI and other fatal / nonfatal CV event Total Revascularisations (PTCA) Hospitalisations HRQofL ‐ Dartmouth COOP Qof L Cost Analysis | |
| Follow up | 6 months post randomisation | |
| Control | Usual care (details not explicitly stated) | |
| Country | USA | |
| Notes | n.b. included heart failure not just CHD patients; percentage with just heart failure not clear; the breakdown table shows "multiple diagnoses". Included a proportion of patients who had previously received cardiac rehabilitation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomly assigned to SI or UC on the basis of a computer‐generated random number.” ”study population was stratified on the basis of minority status, participation in cardiac rehabilitation, and acute status (time since event)” |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | High risk | Case managers collected number of outcomes (height, weight, blood pressure) at follow up and were not blind to intervention or control. |
| Incomplete outcome data (attrition bias) | Low risk | "Of the 104 subjects randomized to the study, 6‐month follow‐up data was obtained on 100. Four subjects were lost to follow up evaluation." Details of drop outs /loss to follow up reported. |
| Selective reporting (reporting bias) | High risk | Dartmouth COOP Quality of life taken at entry and exit. Results reported on entry but not at exit. |
| Groups balanced at baseline | Low risk | Table of demographics and baseline outcome values presented and baseline statistical analysis did not demonstrate any differences. |
| Intention to treat analysis | Low risk | Although not explicitly stated, there groups appear to have been analysed according to initial random allocation. |
| Comparative care? | Unclear risk | Not clear whether intervention group received same usual care as control arm. |
| Methods | RCT | |
| Participants | N Randomised: 207 (n Rx 104 & n control 103) Trail Recruitment period: Not reported When Randomised: Not reported Recruitment from: 427 consecutive patients from 2 participating hospitals CV Diagnosis (% of pts): Post MI n=84 (40.5%) MI &/or Post CABG n=46 (22%) (just CABG 46 MI & CABG MI &/or Post PTCA‐ n=77 (37%) just PCI 77 MI with PCI Age: 59 (SD 7) Percentage male: 74% Inclusion criteria: Recent CAD; MI &/or PTCA &/or CABG Exclusion criteria: Planned CABG; senility; psychiatric medication; expected poor prognosis within a year; deficient in Swedish; participation in other studies. | |
| Interventions | Description / Content: Problem based learning rehabilitation "real life situations or scenarios were presented to the group...consisted of pictures, press cuttings, or short texts about exercise, food, drugs, smoking and cholesterol." Planned curriculum programme explicitly stated. Teaching Modalities: Groups of 6‐8 people. Who taught by: " Tutor ‐ member of rehabilitation team, trained to take the role of the facilitator" Dose: (weekly for the first month, every other week for the next month and the spread over the year) Duration: 1 year No of sessions: 13 group sessions Length of session 1.5hrs Involvement of Family: Not Stated Time of start after event: Not Stated Follow up further reinforcement Theoretical basis for intervention: Yes, Schmidt seven step model of problem solving. | |
| Outcomes | HRQofL ‐ Ladder of Life, Self‐Rated Health, SF‐36, Cardiac Health Profile Withdrawal from intervention group | |
| Follow up | 12‐months post‐randomisation | |
| Control | Usual care consisted of: "Standard treatment from the rehabilitation team....The standard treatment included visits to a nurse and physician during the study period. All patients were also offered the possibility of taking part in physical exercise groups, smoking cessation groups and individual counselling by a dietician." | |
| Country | Sweden | |
| Notes | High attendance rate to the educational sessions. Mean 9.4 (median 11) out of 13 sessions. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Not reported in the study itself but from communication with the author it was confirmed that sealed envelopes were randomly organised by a person outside of the research team |
| Allocation concealment (selection bias) | Low risk | Not reported in the study. However, from communication with the author a sealed envelope method was utilised. |
| Blinding (performance bias and detection bias) | High risk | Not reported in the study. Confirmed by communication with author. |
| Incomplete outcome data (attrition bias) | Low risk | QUORUM trial flow diagram reported with exclusions and attrition documented and reasons given. |
| Selective reporting (reporting bias) | Low risk | All stated outcomes in methods are reported in results at pre and post tests. Although the self rated health score was not reported in detail. |
| Groups balanced at baseline | Low risk | Table of baseline characteristics showed no statistically differences. |
| Intention to treat analysis | Low risk | Confirmed by communication with the author. "For all analyses intention to treat was used." |
| Comparative care? | Low risk | "both groups were offered standard treatment by the rehabilitation team..." |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Identifed from Lie 2009. Review not a RCT | |
| Systematic Review: 21 references identified and reviewed as being of potential interest to this review | |
| Education not primary aim of intervention. (Risk Factor intervention clinic) | |
| Performance bias, intervention included exercise as well as education. | |
| Education not primary aim of intervention. (Psychological Counselling) | |
| "quasi‐experimental" investigating patient satisfaction with teaching. | |
| Performance bias: education only part of the intervention. | |
| Education not primary aim of intervention: symptom management intervention (pain management / incremental physical exercise.) | |
| Performance bias: education only part of the intervention. | |
| Identified from Clark 2007. Not RCT. | |
| A review of a meta‐analysis Dusseldorp 1999 | |
| Systematic Review: 2 references identified and reviewed as being of potential interest to this review | |
| Identified from Clark 2005. Education not primary aim of intervention (Exercise based intervention). | |
| Not education: exercise intervention. | |
| Not a RCT. | |
| Performance bias, intervention included exercise as well as education. Not a RCT compared with historical controls. | |
| Performance bias, intervention included exercise as well as education. | |
| Education not primary aim of intervention. Psychological ‐ "Rational Emotive behavioural therapy". | |
| Education not primary aim of intervention (nurse intervention clinic). | |
| Education not primary aim of intervention (nurse intervention clinic). | |
| Review of implementation of Acute Coronary Syndrome patient pathway. Not an intervention. | |
| No relevant outcomes ‐ self care questionnaires. | |
| Identified from Eshah 2009. Not RCT: Prospective pre‐test / post‐test design. | |
| No specified follow‐up period. | |
| Systematic Review: 45 references identified and reviewed as being of potential interest to this review | |
| Systematic Review: 35 references identified and reviewed as being of potential interest to this review | |
| Systematic Review: 3 references identified and reviewed as being of potential interest to this review | |
| Education not primary aim of intervention ‐ multidisciplinary interventional clinic. | |
| Entrance into study after cardiac rehabilitation. | |
| Identifed from Hanssen 2007. Review not an RCT | |
| Education not primary aim of intervention. Nurse led intervention. | |
| Education not primary aim of intervention ‐ a nurse led intervention clinic. | |
| Duplicate of Mullen 1992; Systematic Review: 0 references identified (all pre1990) | |
| Commentary on a meta‐analysis: Dusseldorp 1999 | |
| Systematic Review: 12 references identified and reviewed as being of potential interest to this review | |
| Performance bias: Intervention multifactorial involves exercise and psychological therapy. | |
| Performance bias: Intervention multifactorial involves exercise and psychological therapy. | |
| Performance bias: Intervention multifactorial involves exercise and psychological therapy. | |
| Performance bias: Intervention multifactorial involves exercise and psychological therapy. | |
| Identified from Beranova 2007. Not relevant outcomes. | |
| Systematic Review: 8 references identified and reviewed as being of potential interest to this review | |
| Education not primary aim of intervention‐ Performance bias | |
| Education not primary aim of intervention: Exercise intervention | |
| Intervention cognitive behavioural therapy compared with standard cardiac rehabilitation (including education). | |
| Education not primary aim of intervention: Individualised psychological intervention. | |
| Individualised educational intervention in CABG patients: Study designed to investigate the time of delivery of education ‐ both groups received the same intervention | |
| Systematic Review: 7 references identified and reviewed as being of potential interest to this review | |
| Not relevant outcomes (patients recruited between 1977 and 79). | |
| Not education, exercise is the primary focus post CABG. | |
| Commentary: paper excluded education not primary intervention. | |
| Follow‐up period only 3 months post discharge from CABG. | |
| Commentary on meta‐analysis Clark, A.M., et al., Meta‐analysis: Secondary prevention programs for patients with coronary artery. Annals of Internal Medicine, 2005. 143(9): p. 659‐672+I87. | |
| Identified from Clark 2007. Education not primary aim of intervention | |
| Education not primary aim of intervention ‐ Performance bias. | |
| Education not primary aim of intervention ‐ Performance bias. | |
| Not RCT "experimental design" | |
| Editorial referring to Shuldham 2002, Pre‐CABG education. No relevant outcomes investigated. | |
| Systematic Review: 0 references identified | |
| Identified from Clark 2009. No relevant outcomes. | |
| Identifed from Beranova 2007. Outcomes; Effectiveness of education package in promoting learning only. | |
| Not education, psycho‐social intervention, post MI. | |
| Education not primary aim of intervention. Nurse led clinic. | |
| Identified from Eshah 2009. Education not primary aim of intervention (diet and stress management and social support). | |
| Education not primary aim of intervention: computer support group ‐ comparison of moderated and unmoderated access. | |
| Education not primary aim of intervention | |
| Systematic Review: 0 references identified | |
| Education not primary aim of intervention: Psychological intervention ‐ cognitive behavioural therapy. | |
| Education not primary aim of intervention‐Psychological intervention | |
| Identified from Fredericks 2009. Education not primary aim of intervention. Symptom management program using audiotapes. | |
| No relevant outcomes | |
| Duplicate of Dolan 1992; Systematic Review: 0 references identified (all pre1990) | |
| Education not primary aim of intervention: secondary prevention clinic. | |
| Education not primary aim of intervention: secondary prevention clinic. | |
| Systematic Review: 11 references identified and reviewed as being of potential interest to this review | |
| Identified from Clark 2007. Education not primary aim of intervention (exercise and low fat diet) | |
| Education not primary aim of intervention: psychological intervention | |
| Education not primary aim of intervention: case management ‐ not relevant outcomes (only risk factor modification). | |
| Education not primary aim of intervention: psychological intervention. | |
| Identified from Clark 2007. Education not primary aim of intervention | |
| Education not primary aim of intervention: lifestyle regime | |
| Education not primary aim of intervention: nurse managed cholesterol control program. | |
| No relevant outcomes | |
| Education not primary aim of intervention | |
| Non‐standard RCT design with non‐randomised control group. | |
| Not RCT. "True experimental post‐test only, control group design, including the process of randomisation." | |
| Commentary on a Systematic Review, subsequently reviewed and demonstrated: 9 references identified and reviewed as being of potential interest to this review | |
| Education not primary aim of intervention, combined with psychological counselling and no relevant outcomes. | |
| Systematic Review: 0 references identified | |
| pre‐CABG education. No relevant outcomes investigated. | |
| Follow‐up only 100 days. | |
| Identified from Hanssen 2007. Review not an RCT | |
| Identified from Hanssen 2007. Review not an RCT | |
| Education not primary aim of intervention, telephone nurse management. | |
| Cost analysis of Khunti 2007; Education not primary aim of intervention | |
| Education not primary aim of intervention: Program is a risk factor targeted prompting of treatment. | |
| No relevant outcomes. | |
| Not RCT ‐" quasi‐experimental pre‐test / post test control group design." | |
| Identified from Eshah 2009. Not RCT: Retrospective Study | |
| Dietary intervention, Education not primary aim of intervention. | |
| Systematic Review: 0 references identified. | |
| No relevant outcomes. | |
| Education not primary aim of intervention‐Performance bias | |
| Identified from Neubeck 2009. No relevant outcome measures |
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Unable to gain access to paper. |
| Methods | RCT |
| Participants | Post CABG patients. n=88 |
| Interventions | Weekly, individualized, telephone, educational intervention. |
| Outcomes | Difficult to ascertain from abstract alone |
| Notes | Abstract only |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Randomised controlled trial of secondary prevention program for myocardial infarction patients ('ProActive Heart') |
| Methods | RCT |
| Participants | Post MI patients recruited from Brisbane Hospitals. |
| Interventions | 6 month telephone delivered secondary prevention program |
| Outcomes | SF‐36, Cost‐effective analysis |
| Starting date | December 2007 |
| Contact information | |
| Notes |
| Trial name or title | Randomised Trial of Cardiac Rehabilitation Program Delivered Remotely through the Internet |
| Methods | RCT |
| Participants | Men and Women > 18. Diagnosed Ischaemic Heart Disease. Aim to recruit 74 patients from consecutive inpatient admissions with acute coronary syndrome or revascularisation procedure. |
| Interventions | 4 month interactive Internet based CR program. Input from nurse, dietitian and exercise specialist. |
| Outcomes | Healthcare utilisation at 16 months |
| Starting date | |
| Contact information | Dr S.C. Lear. [email protected] |
| Notes | clinicaltrials.gov identifier NCT00683813 |
| Trial name or title | A Psychoeducation Trial for People with Chronic Stable Angina |
| Methods | RCT |
| Participants | CHD for at least 6 months |
| Interventions | Supportive and educational self‐management program (Chronic Angina Self‐Management Program (CASMP). |
| Outcomes | HRQofL (SF‐36 and SAQ) |
| Starting date | 9/2003 |
| Contact information | Dr MH McGillion, University of Toronto, Toronto, Ontario, Canada M5T 1P8 |
| Notes | clinicaltrails.gov identifier NCT00350922 |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total mortality at the end of the follow up period Show forest plot | 6 | 2330 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.55, 1.13] |
| Analysis 1.1  Comparison 1 Total Mortality, Outcome 1 Total mortality at the end of the follow up period. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Myocardial Infarction at the end of the follow up period Show forest plot | 2 | 209 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.26, 1.48] |
| Analysis 2.1  Comparison 2 Cardiovascular Events, Outcome 1 Myocardial Infarction at the end of the follow up period. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Patients requiring Coronary Artery Bypass Grafting (CABG) at end of follow‐up period Show forest plot | 2 | 209 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.19, 1.71] |
| Analysis 3.1  Comparison 3 Revascularisations, Outcome 1 Patients requiring Coronary Artery Bypass Grafting (CABG) at end of follow‐up period. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Cardiac Hospitalisations at end of follow up period Show forest plot | 4 | 12905 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.65, 1.07] |
| Analysis 4.1  Comparison 4 Hospitalisations, Outcome 1 Cardiac Hospitalisations at end of follow up period. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 All cause withdrawal / drop‐out at follow‐up Show forest plot | 8 | 2862 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.83, 1.27] |
| Analysis 5.1  Comparison 5 All cause withdrawal / drop‐out at follow‐up, Outcome 1 All cause withdrawal / drop‐out at follow‐up. | ||||

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
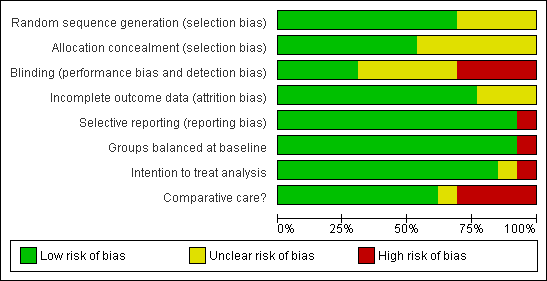
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Comparison 1 Total Mortality, Outcome 1 Total mortality at the end of the follow up period.

Comparison 2 Cardiovascular Events, Outcome 1 Myocardial Infarction at the end of the follow up period.

Comparison 3 Revascularisations, Outcome 1 Patients requiring Coronary Artery Bypass Grafting (CABG) at end of follow‐up period.

Comparison 4 Hospitalisations, Outcome 1 Cardiac Hospitalisations at end of follow up period.
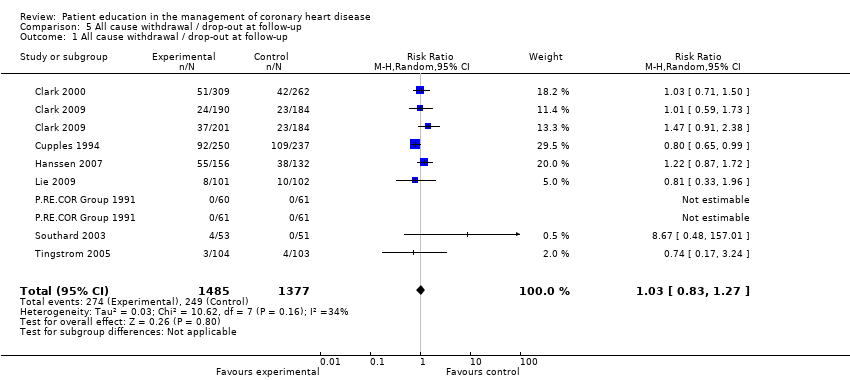
Comparison 5 All cause withdrawal / drop‐out at follow‐up, Outcome 1 All cause withdrawal / drop‐out at follow‐up.
| Description of Intervention | Theoretical Basis | Tailored | Duration | One to One | Group | Face to Face | Telephone | Internet | Notes | |
| Clark 1997 | *PRIDE | Y | Y | Once a week for 4 weeks | Y | Y | Taught by health educator. Videotape and workbook aids. | |||
| Clark 2000 | *PRIDE | Y | Y | Once a week for 4 weeks | Y | Y | Taught by health educator. Videotape and workbook aids. | |||
| Clark 2009 | *PRIDE | Y | Y | Once a week for 6 weeks | Y | Y | Y | 3 groups (self‐directed and group intervention and a control) | ||
| Cupples 1994 | Practical tailored advice on cardiovascular risk factors and appropriate health education. | N/S | Y | 3 times a year for 2 years | Y | Y | Delivered at home by health visitor | |||
| Esposito 2008 | Predesigned scripts to provide education on various aspects of care, geared to personalised clinical goals. | N/S | Y | Average 1.1 contacts a month for 18 months | Y | Y | Y | Nurse case manager, primarily by telephone but also face to face. | ||
| Hanssen 2007 | Individualised education from a menu of topics to be covered. | Y | Y | 6 months (8 sessions in total) | Y | Y | Structured element and an on‐call element | |||
| Lie 2009 | A psychoeducative intervention. Structured information and psychological support. | N/S | N/S | 2 visits (1 hour each) | Y | Y | Critical care nurse, home based. | |||
| Lisspers 1999 | Health education and achievement of behavioural change. | N/S | Y | 4 week residential then 11 month one to one individual sessions | Y | Y | Y | Trained nurses (personal coaches). Seminars, lectures, discussion and skills sessions. | ||
| P.RE.Cor Group 1991 | Education and counselling on management of cardiovascular risk factors and exercise. | N/s | Y | 1 group session, 1 individual session with cardiologist | Y | Y | Y | Multi‐disciplinary input to group. Cardiologist tailors therapy. | ||
| Piekes 2009 | Variable ‐ nurse provision of patient education. | N/s | N/S | 1‐2.5 times a month for an average of 30 months | Y | Y | 15 different programs, majority telephone, one‐to‐one | |||
| Pogosova 2008 | Structured program addressing different risk factors in each session. | Y | N/S | 6 Sessions (twice a week, 90 mins) | Y | Y | ||||
| Southard 2003 | Modular internet sessions, Interactive multiple choice and self tests followed by feedback. | N/S | N/S | Once a week for 6 months (at least 30 mins) | Y | Y | Y | Communication with case manager and on‐line discussion group. | ||
| Tingstrom 2005 | Problem based rehabilitation to teach a planned curriculum | Y | N/S | 13 sessions over 1 year | Y | Y | Trained Facilitator | |||
| PRIDE = Problem Identification, Researching one's routine, Identifying a management goal, Developing a plan to reach it, Expressing one's reactions and Establishing rewards for making progress. Y = Yes N/S = Not Stated | ||||||||||
| Study | Number Randomised | Number Lost at Follow‐up* | Notes | |
| Clark 2000 | Intervention | 309 | 51 | 36 withdrew, 14 died, 1 data missing |
| Control | 262 | 42 | 33 withdrew, 8 died, 1 data missing | |
| Clark 2009 | Intervention | 201 | 37 | Self‐directed program 33 withdrew, 4 died |
| Intervention | 190 | 24 | Group format 19 withdrew, 5 died | |
| Control | 184 | 23 | 15 withdrew, 8 died | |
| Cupples 1994 | Intervention | 250 | 92 | 45 defaulted, 47 died 21 defaulted at 2 yrs |
| Control | 237 | 109 | 44 defaulted, 65 died 25 defaulted at 2 yrs | |
| Hanssen 2007 | Intervention | 156 | 55 | 40 withdrew, 7 died, 8 missing data |
| Control | 132 | 38 | 21 withdrew, 7 died, 10 missing data | |
| Lie 2009 | Intervention | 101 | 8 | 6 withdrew, 2 medical exclusions |
| Control | 102 | 10 | 5 withdrew, 5 medical exclusions | |
| P.RE.COR 1991 | Intervention | 60 | 0 | Comprehensive cardiac rehabilitation |
| Intervention | 61 | 0 | Counseling program without exercise | |
| Control | 61 | 0 | ||
| Southard 2003 | Intervention | 53 | 4 | Reasons for drop out stated; Relocation, dietary intervention instead, psychiatric diagnosis, loss of interest |
| Control | 51 | 0 | ||
| Tingstrom 2005 | Intervention | 104 | 3 | Out of the 7 lost to follow‐up 2 died and 5 did not attend |
| Control | 103 | 4 | ||
| Combined Results | Intervention | 1485 | 274 | 18.5% |
| Control | 1132 | 226 | 20.0% | |
| * All causes of drop out from follow up included (including mortality) | ||||
| Seattle Angina Questionnaire | |||||
| Lie 2009 (6 months) | Absolute mean (SD) outcome values at follow‐up | Comparison | |||
| Rx | p‐value | Control | p‐value | ||
| Physical Limitation | 86.4(15.6) | p<0.001 | 83.2(18.7) | p<0.001 | Rx=Control |
| Angina Frequency | 91.7(16.6) | p<0.001 | 90.8(18.9) | p<0.001 | Rx=Control |
| Treatment Satisfaction | 89.2(15.4) | NS | 88.0(16.1) | NS | Rx=Control |
| Disease Perception | 77.8(20.2) | p<0.001 | 73.9(24.2) | p<0.001 | Rx=Control |
| AP‐QLQ (Angina Pectoris ‐ Quality of Life Questionnaire) | ||||
| Lisspers 1999 (24 Months) | Mean (SD) score at follow‐up | Between group p‐value | Comparison | |
| Rx | Control | |||
| QLQ (Total) | 4.7(0.8) | 4.3(1.0) | NS | Rx=Control |
| Somatic symptoms | 4.8(1.0) | 4.3(1.1) | NS | Rx=Control |
| Physical Activity | 4.8(1.0) | 4.1(1.2) | NS | Rx=Control |
| Emotional Distress | 4.8(0.8) | 4.6(1.1) | NS | Rx=Control |
| Life Satisfaction | 4.2(1.0) | 3.9(1.2) | NS | Rx=Control |
| Figures quoted represent an absolute score on a self‐rating scale. | ||||
| SF‐36* (Short Form 36 item survey) | |||
| Between group difference in mean change from baseline (95% CI) at follow‐up | Between group p‐value | Comparison | |
| Hanssen 2007 (6 months) | |||
| Overall Physical | ‐2.33 (‐4.54,‐0.12) | 0.039 | Rx=Control |
| Physical Functioning | ‐1.16 (‐3.28,0.95) | 0.28 | Rx=Control |
| Role Physical | ‐1.84 (‐5.32,1.64) | 0.299 | Rx=Control |
| Bodily Pain | ‐1.74 (‐4.54,1.05) | 0.22 | Rx=Control |
| General Health | ‐0.36 (‐2.64,1.91) | 0.752 | Rx=Control |
| Overall Mental | 1.07 (‐1.71,3.86) | 0.447 | Rx=Control |
| Vitality | ‐0.07 (‐2.23,2.10) | 0.951 | Rx=Control |
| Social Functioning | 0.36 (‐2.96,3.67) | 0.832 | Rx=Control |
| Role Emotional | 0.78 (‐3.29,4.84) | 0.706 | Rx=Control |
| Mental Health | 0.4 (‐1.81,2.60) | 0.723 | Rx=Control |
| Hanssen 2007 (18 months) | |||
| Overall Physical | ‐1.44 (‐3.89,1.02) | 0.25 | Rx=Control |
| Physical Functioning | ‐0.79 (‐3.06,1.48) | 0.491 | Rx=Control |
| Role physical | ‐0.94 (‐4.76,2.88) | 0.627 | Rx=Control |
| Bodily Pain | ‐0.77 (‐4.00,2.47) | 0.641 | Rx=Control |
| General Health | 0.25 (‐2.15,2.64) | 0.838 | Rx=Control |
| Overall Mental | 1.65 (‐1.35,4.65) | 0.28 | Rx=Control |
| Vitality | 0.58 (‐1.95,3.12) | 0.65 | Rx=Control |
| Social Functioning | 0.55 (‐3.95,2.85) | 0.751 | Rx=Control |
| Role Emotional | 2.59 (‐1.58,6.77) | 0.221 | Rx=Control |
| Mental Health | 0.31 (‐2.11,2.73) | 0.8 | Rx=Control |
| * Negative baseline‐follow‐up difference favours intervention and positive favours control. | |||
| SF‐36* (Short Form 36 item survey) | ||||
| Tingstrom 2005 (12 months) | Mean change from baseline (SD) | Between group p‐value+ | Comparison | |
| Rx | Control | |||
| Physical Functioning | 3.6 (17.6) | 4.4 (15.1) | 0.749 | Rx=Control |
| Role Physical | 38.2 (46.9) | 33.8 (42.4) | 0.504 | Rx=Control |
| Bodily Pain | 5.69 (31.1) | 6.18 (29.1) | 0.911 | Rx=Control |
| General Health | 1.4 (15.9) | 1.8 (16.3) | 0.862 | Rx=Control |
| Vitality | 5.3 (22.7) | 4.9 (21.8) | 0.921 | Rx=Control |
| Social Functioning | 9.7 (24) | 9.1 (25.3) | 0.869 | Rx=Control |
| Role Emotional | 15.8 (48.1) | 16.5 (41.1) | 0.913 | Rx=Control |
| Mental Health | 2.9 (16.6) | 4.2 (17.8) | 0.566 | Rx=Control |
| *Positive values indicate improvement in HRQofL from baseline +p‐values are calculated on the difference between groups at pre‐test and on the mean change (post test minus pre‐test). | ||||
| SF‐36 (Short Form 36 item survey) | |||
| Pogosova 2008 (12 months) | Mean change from baseline p‐value | Comparison | |
| Control | Rx | ||
| Overall Physical | p>0.05 | p≤0.05 | Favours Rx |
| Physical Functioning | p>0.05 | p≤0.05 | Favours Rx |
| Bodily Pain | p>0.05 | p≤0.05 | Favours Rx |
| Overall Mental | p>0.05 | p≤0.05 | Favours Rx |
| Vitality | p>0.05 | p≤0.05 | Favours Rx |
| Social Functioning | p>0.05 | p≤0.05 | Favours Rx |
| Mental Health | p>0.05 | p≤0.05 | Favours Rx |
| There were no significant changes demonstrated in the control group but no statistical comparison of the mean change between the groups was reported. | |||
| SF‐36 (Short Form 36 item survey) | |||||
| Lie 2009 (6 months) | Absolute mean (SD) outcome values at follow‐up | Comparison | |||
| Rx | p‐value | Control | p‐value | ||
| Overall Physical | 47.4 (9.6) | p<0.001 | 47 (10) | p<0.001 | Rx=Control |
| Physical Functioning | 82.2 (19.2) | p<0.001 | 82.3 (19.8) | p<0.001 | Rx=Control |
| Role Physical | 64 (41.2) | p<0.001 | 57.2 (43.3) | p<0.001 | Rx=Control |
| Bodily Pain | 77.2 (22.3) | p<0.001 | 78.5 (25.2) | p<0.001 | Rx=Control |
| General Health | 69.9 (23.3) | NS | 65.7 (27.2) | NS | Rx=Control |
| Overall Mental | 52.1 (10.7) | p<0.05 | 50.5 (10.8) | NS | Favours Rx |
| Vitality | 61.9 (23.9) | p<0.001 | 60.5 (21.6) | p<0.001 | Rx=Control |
| Social Functioning | 86.3 (21.4) | p<0.001 | 84.3 (21.9) | p<0.001 | Rx=Control |
| Role Emotional | 73.3 (38.2) | p<0.01 | 67.4 (41.6) | p<0.01 | Rx=Control |
| Mental Health | 81.9 (17.3) | p<0.001 | 78.5 (21) | p<0.01 | Rx=Control |
| Nottingham Health Profile+ | ||||
| Cupples 1994 (24 months) | Mean change from baseline (SD) at follow‐up | Comparison | ||
| Rx | Control | Between group p‐value | ||
| Emotional Reaction | ‐0.79 (19.52) | ‐1.91 (21.31) | 0.52 | Rx=Control |
| Energy | ‐3.88 (33.97) | ‐6.52 (35.87) | 0.33 | Rx=Control |
| Physical Mobility | ‐1.49 (16.17) | ‐6.19 (18.12) | 0.003 | Rx>Control |
| Pain | ‐1.23 (20.5) | ‐2.7 (23.46) | 0.92 | Rx=Control |
| Sleep | ‐1.67 (26.22) | ‐0.1 (24.95) | 0.38 | Rx=Control |
| Social Isolation | 1.42 (16.96) | ‐3.01 (21.27) | 0.08 | Rx=Control |
| + Higher scores reflect poorer quality of life | ||||
| Nottingham Health Profile+ | |||
| Cupples 1994 (60 months) | Mean difference (95% CI) between groups in change from baseline at follow‐up | Between group p‐value | Comparison |
| Emotional Reaction | ‐2.1 (‐7.5,3.3) | NS | Rx=Control |
| Energy |
‐4.7 (‐13.2,3.7) | NS | Rx=Control |
| Physical Mobility |
‐1.3 (‐6.3,3.6) | <0.05 | Rx>Control |
| Pain | ‐3.4 (‐9.2,2.3) | <0.05 | Rx>Control |
| Sleep |
‐2.4 (‐9.3,4.5) | NS | Rx=Control |
| Social Isolation | 0.0 (‐4.3,4.3) | NS | Rx=Control |
| + Higher scores reflect poorer quality of life The value quoted is the mean difference (CI) between groups from baseline to follow‐up p‐value related to t‐tests (two tailed) | |||
| Sickness Impact Profile+++ | ||||
| Absolute mean outcome values at follow‐up++ | Comparison | |||
| Rx | Control | Between group p‐value | ||
| Clark 1997 (12 months) | ||||
| Total Score | 7.26 | 8.09 | NS | Rx=Control |
| Psychosocial Dimension | 5.52 | 7.05 | ≤0.05 | Rx>Control |
| Physical Dimension | 5.89 | 6.00 | NS | Rx=Control |
| Clark 1997 (18 months) | ||||
| Total Score | 7.93 | 7.41 | NS | Rx=Control |
| Psychosocial Dimension | 6.05 | 6.23 | NS | Rx=Control |
| Physical Dimension | 6.40 | 5.25 | NS | Rx=Control |
| ++ for mean scores at follow‐up (adjusted for baseline scores) +++lower score higher HRQofL | ||||
| Sickness Impact Profile | ||||
| Clark 2000 (12 months) | Absolute means at follow‐up++ | Comparison | ||
| Rx | Control | Between group p‐value | ||
| Psychosocial Dimension | 5.15 | 5.91 | 0.144 | Rx=Control |
| Physical Dimension | 7.09 | 7.66 | 0.05 | Rx>Control |
| Means were adjusted to take account of baseline values. | ||||
| Sickness Impact Profile | |||||
| Absolute means (SD) at follow‐up | Comparison | ||||
| Rx group | Rx self directed | Control | Between group p‐value | ||
| Clark 2009 (12 months) | |||||
| Total Score | 8.13 (8.63) | 9.79 (10.17) | 9.49 (9.46) | NS | Rx=Control |
| Psychosocial Dimension | 5.84 (8.02) | 7.31 (10.74) | 6.75 (9.39) | NS | Rx=Control |
| Physical Dimension | 8.07 (9.63) | 9.46 (10.11) | 9.85 (10.79) | NS | Rx=Control |
| Clark 2009 (18 months) | |||||
| Total Score | 8.44 (9.13) | 8.98 (10.29) | 9.64 (9.45) | NS | Rx=Control |
| Psychosocial Dimension | 5.74 (9.68) | 6.16 (8.20) | 7.17 (10.40) | NS | Rx=Control |
| Physical Dimension | 8.27 (10.02) | 8.98 (9.33) | 9.65 (10.19) | NS | Rx=Control |
| n.b. the analysis of this data was reported in the paper but the individual results were not. These have been obtained by direct contract with the author. | |||||
| Patients' Assessment of their Quality of Life on a five‐point scale | ||||||
| Cupples 1994 (24 months) | Initial scores (% of patients) | Follow‐up Scores (% of patients) | Between group p‐value | Comparison | ||
| Rx | Control | Rx | Control | p<0.03 | Rx>Control | |
| Poor | 6.3 | 5.3 | 6.9 | 8.3 | ||
| Fair | 27.8 | 23.3 | 18.9 | 21.7 | ||
| Average | 35 | 39 | 33.1 | 33.7 | ||
| Good | 22.7 | 22.7 | 29.3 | 25.3 | ||
| Very Good | 8.2 | 9.7 | 11.7 | 11 | ||
| n.b. for Table 13 the between group p value represents the overall "comparison of change in individuals' assessment for intervention and control groups" the significant difference being in favour of the intervention group. For all tables summarising HRQofL Data (Tables 2‐13) Rx: Intervention NS: No significant difference demonstrated Rx=Control: no significant difference (p>0.05) in HRQof L between the intervention and the control groups at follow‐up. Rx>Control: significant difference (p≤0.05) in HRQofL in favour of the intervention group at follow‐up. Control>Rx: significant difference (p≤0.05) in HRQofL in favour of the control group at follow‐up. Favours Rx: Available evidence favours the intervention group but direct statistical comparison between intervention and control groups was not reported. Favours Control: Available evidence favours the control group but direct statistical comparison between intervention and control groups was not reported. | ||||||
| Variable | Clark 2000 | Cupples 1994 | Esposito 2008 | Southard 2003 | Peikes 2009 | |||
| Follow‐up | 24 months | 24 months | 6 months | 7‐12 months | 12 months | 18 months | 6 months | 25 months |
| Year of Costs | 2000 | NR | 2005‐6 | NR | 2002‐2005 | |||
| Currency | US$ | GBP£ | US$ | US$ | US$ | |||
| Mean cost of cardiac rehabilitation program per patient | ||||||||
| Total Costs | $187 | £49.72 | $162 | $453 | $196 | |||
| Costs Considered | Personnel, Instructional Materials, Telephone Supplies, Ongoing Staff Training | Direct Costs by Health Visitors (Staff Time), Travel Costs. | Average monthly fee paid to the program per member | Nurse Salary Overheads Subscription Costs | Average monthly fee paid to the program per member | |||
| Comments | Participating site overheads were not measured, a "conservatively high" estimate of these was taken to double the cost of the Rx to $374. | Costs of the health visitor also included time spent recording data collection for the study. | Cost varied between the included 15 studies. Negotiated locally with center of Medicare and Medicaid Services. (Range $50‐$444) | |||||
| Mean total healthcare costs per patient | ||||||||
| Total Cost (Intervention) | ˜$3300 (calc) | £1801 | $1627 | $2356 | $2288 | $1793 | $635 | $1283 * |
| Total Cost (Control) | ˜$6500 | £1812 | $1632 | $2464 | $2372 | $1818 | $2053 | $1314 * |
| Between Group Difference | ˜$1800* | £9.60 | $5 | $107 | $84 | $25 | $1418 | $144 (80% CI 99 to 188) |
| p value | NR | NS | 0.895 | 0.077 | 0.132 | 0.365 | NR | <0.001 |
| Cost Saving per pt (when cost of intervention taken into account§) | ˜$1610 or ˜$1420 if estimated overheads are included. | £40 | ‐$157 | ‐$55 | ‐$78 | ‐$137 | $965 | ‐$52 |
| Additional Healthcare Costs Considered | Number of Admissions (Heart Related), Number of inpatient days, In patient cost. Emergency Dept costs | Prescription of drugs, visits to the GP, Visits to hospital as inpatients and outpatients, all tests investigations and treatments carried out | Medicare Medical Claims | Cardiovascular related emergency room visits and hospitalisations | ||||
| Comments | Expenditure was calculated from differences in % utilisation of hospital services. i.e. Hospital charges for participants were on average 49% lower and the average annual expenditure was $6500. * There was a calculated saving of a hospital charge of $3200, the ratio of payments to charges was 0.56 therefore $1800 actual saving. | There was a difference in the drug usage at baseline which is not accounted for in these figures although this would make minimal impact to the results. The intervention group were more costly for drugs, procedures and service use. | Claims quoted are per member per month. | *Expenditure/pt/month enrolled
Overall costs were increased by 11% when the care coordination fees were taken into account. | ||||
| Summary Difference Between Groups | Favours Rx | Rx=Control | Rx=Control (for all time periods studied) | Favours Rx | Favours Control | |||
| § = Negative mean difference indicates a net cost of the intervention group NR = Not Recorded NS = Not Significant | ||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total mortality at the end of the follow up period Show forest plot | 6 | 2330 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.55, 1.13] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Myocardial Infarction at the end of the follow up period Show forest plot | 2 | 209 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.26, 1.48] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Patients requiring Coronary Artery Bypass Grafting (CABG) at end of follow‐up period Show forest plot | 2 | 209 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.19, 1.71] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Cardiac Hospitalisations at end of follow up period Show forest plot | 4 | 12905 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.65, 1.07] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 All cause withdrawal / drop‐out at follow‐up Show forest plot | 8 | 2862 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.83, 1.27] |


