Administración de suplementos de vitamina D para embarazadas
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en espera de evaluación
Referencias de los estudios en curso
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomised single‐blinded controlled trial with 2 arms: vitamin D plus calcium and placebo. | |
| Participants | 54 pregnant women at risk for pre‐eclampsia, primigravida, aged 18 to 35 years old carrying singleton pregnancy at their third trimester attending maternity clinics affiliated to Kashan University of Medical Sciences, Kashan, Islamic Republic of Iran (latitude: 33.9889° N, 51.4772° E). Exclusion criteria: maternal severe pre‐eclampsia, IUFD, placenta abortion, preterm delivery and GDM. | |
| Interventions | Participants were randomly allocated to 1 of 2 groups: group 1 (n = 27): women received 500 mg of carbonate calcium plus 200 IU of vitamin D (cholecalciferol‐D3) daily for 9 weeks; group 2 (n = 27): women received placebo. The intervention lasted 9 weeks overall, starting at 25 weeks of pregnancy until week 34. Participants were asked not to alter their routine PA or usual diets and not to consume any supplement other than the one provided to them by the investigators. Health worker cadre: the trial was carried out in maternity clinics affiliated to Kashan University of Medical Sciences, Kashan, Islamic Republic of Iran and the investigators provided the supplements to the participants. | |
| Outcomes | Maternal: body weight and height, BMI, fasting plasma glucose levels, serum total cholesterol, triglycerol concentrations, serum HDL‐cholesterol, serum LDL‐cholesterol levels, dietary intakes, total HDL: cholesterol ratio, gestational diabetes, severe pre‐eclampsia, preterm delivery. Laboratory method used for assessment of vitamin D concentrations: serum 25‐hydroxyvitamin D concentrations were measured using a commercial ELISA kit (Immuno Diagnostic Systems). The inter‐ and intra‐assay coefficient of variation for serum 25(OH)D assays ranged from 5% to 7.5%. | |
| Notes |
Source of funding: study was funded by research grant from the Vice‐Chancellor for research, KUMS, and Iran. Dates of the study and location: April 2011 to February 2012, Iran. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): none declared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Trial reported randomisation performed by the use of computer‐generated random numbers. |
| Allocation concealment (selection bias) | Low risk | Trial reported that the appearance of the placebo capsules, such as colour, shape, size, and packaging, was identical to the vitamin D3 capsules. |
| Blinding of participants and personnel (performance bias) | High risk | The trial reported that it was single‐blinded. Participants were blinded to the interventions so it is assumed that the research staff were not blinded. |
| Blinding of outcome assessment (detection bias) | High risk | Trial is reported as single‐blinded and the methods for concealment of the intervention were described for participants. Therefore, it is assumed that it was not blinded to research staff. |
| Incomplete outcome data (attrition bias) | Low risk | Lost to follow‐up of 3 women in the vitamin D group due to preterm delivery (n = 1), IUFD (n = 1), and placental abruption (n = 1). 3 women in the placebo group were also excluded for the following reasons: gestational diabetes (n = 1), preterm delivery (n = 1), and severe pre‐eclampsia (n = 1). |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled clinical trial with 2 arms: vitamin D and placebo, during March 2012 to September 2012. | |
| Participants | 48 healthy pregnant women, primigravida, aged 18–40 years old at 25 weeks of gestation and a singleton pregnancy attending maternity clinics affiliated with Kashan University of Medical Sciences, Kashan, Islamic Republic of Iran. Women with pre‐eclampsia, hypertension, GDM, IUFD, or those with a history of rheumatoid arthritis, hepatic or renal failure, metabolic bone disease and malabsorption, or thyroid, parathyroid, or adrenal diseases were excluded from the analysis. Also, smokers and those taking medications including nonsteroidal antiinflammatory drugs and aspirin were excluded. | |
| Interventions | Participants were randomly assigned to receive 1 of 2 groups: group 1 (n = 24) received 400 IU vitamin D (cholecalciferol‐D3) supplements daily; and group 2 (n = 24) received placebo for 9 weeks. Additionally, all participants also consumed 400 mcg (0.4 mg) folic acid daily from the beginning of pregnancy and 60 mg elemental iron (as ferrous sulphate) daily from the second trimester. Health worker cadre: the trial was carried out in maternity clinics affiliated to Kashan University of Medical Sciences, Kashan, Islamic Republic of Iran and the investigators provided the supplements to the participants. A trained midwife at the maternity clinic performed anthropometric measurements at study baseline and at 6 weeks after the intervention. | |
| Outcomes | Maternal: weight, height, BMI, systolic blood pressure and diastolic blood pressure, serum calcium concentrations, serum 25‐hydroxyvitamin D [25(OH)D], serum hs‐C‐reactive protein, fasting plasma glucose, serum cholesterol, LDL‐cholesterol, HDL‐cholesterol concentrations, serum insulin, quantitative Insulin sensitivity check index (QUICKI) score, plasma total antioxidant capacity, plasma total glutathione, GDM, preterm delivery, IUFD, placental abruption, severe pre‐eclampsia. Laboratory method used for assessment of vitamin D concentrations: serum 25‐hydroxyvitamin D concentrations were measured using a commercial ELISA kit (Immuno Diagnostic Systems). | |
| Notes |
Source of funding: study was funded by research grant from the Vice‐chancellor for Research, Kashan University of Medical Sciences, Kashan, Iran. Dates of the study and location: March 2012 to September 2012, Kashan, Iran. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): there are no conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random assignment was performed by the use of computer‐generated random numbers. |
| Allocation concealment (selection bias) | Low risk | A trained midwife at the maternity clinic performed the randomised allocation sequence and assigned participants to the groups. Placebo pills contained microcrystalline cellulose and were packed in identical tablets and coded by the producer to guarantee blinding. |
| Blinding of participants and personnel (performance bias) | Low risk | Participants and investigators were blind to the interventions. |
| Blinding of outcome assessment (detection bias) | Low risk | Measurements of laboratory were performed in a blinded fashion, in duplicate, in pairs (before/after intervention) at the same time, in the same analytical run, and in random order to reduce systematic error and inter assay variability. |
| Incomplete outcome data (attrition bias) | Low risk | 3 in each group were lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
| Methods | Randomised controlled trial. | |
| Participants | 78 pregnant women between 14 to 18 weeks' gestation at risk, defined as: dark skinned, veiled; with vitamin D deficiency that has not commenced treatment prior to recruitment. Exclusion criteria: women taking barbiturates or anticonvulsants (decreased vitamin D absorption) and severe renal failure. | |
| Interventions | Participants were individually randomised to 1 of 2 groups: group 1 (n = 38): 2000 IU of cholecalciferol orally daily commencing between 14 and 18 weeks' gestation (if still deficient at 28 weeks the dose was doubled to 4000 IU orally daily until birth); group 2 (n = 40): no treatment during pregnancy. The mother received 300,000 IU cholecalciferol orally immediately and the baby 150,000 IU cholecalciferol orally immediately after birth. Health worker cadre: in order to facilitate compliance, encouragement was given from midwifery/medical staff at each 2–4 weekly antenatal visit with additional intervening telephone calls to women with poor compliance. Pill counts were not performed. | |
| Outcomes | Maternal: vitamin D level. Infant: vitamin D level. Laboratory method used for assessment of vitamin D concentrations: serum 25‐OH vit D concentrations were determined by direct competitive chemiluminescence immunoassay for quantitative determination of total serum 25‐OH vit D (LIAISON®) Diasorin 25‐OH vitamin D assay (Stillwater, MN,USA). | |
| Notes |
Source of funding: J.E. Benson was a recipient of the Luke Proposch Perinatal Research Scholarship from the Australian and New Zealand College of Obstetrics and Gynaecology Research Foundation enabling her to undertake this research. Study was funded by research grant. Dates of the study and location: between 2008 and 2009, Melbourne, Australia. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): the authors have no conflict of interest to disclose. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly allocated (envelopes in a tamper proof box, ratio 1:1). |
| Allocation concealment (selection bias) | Low risk | Envelopes in a tamper‐proof box, ratio 1:1. |
| Blinding of participants and personnel (performance bias) | High risk | The trial reported that it was single‐blinded. It is assumed that it was not blinded to participants as one of the groups did not receive any supplementation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Single‐blinded study but authors did not specify if staff performing assessments were blinded. |
| Incomplete outcome data (attrition bias) | High risk | 57.9% intervention and 57.5% control data reported. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
| Methods | Randomised, parallel assignment, double‐blind trial. | |
| Participants | 115 pregnant females from 12 to 20 weeks of gestation who agreed to participate in the study with presence of at least 20 natural teeth in mouth excluding third molars. For controls: non pregnant, healthy females matched with pregnant women with respect to age and education. Exclusion criteria: pregnant females with high vitamin D levels, women with metabolic diseases such as diabetes (type 1 or 2), presence of acute dental or periodontal disease, presence of systemic disease and/or medication affecting the periodontium; receipt of systemic antibiotic treatment or dental prophylaxis in the previous 3 months and those who do not provide informed consent. | |
| Interventions | Participants were individually randomised to 1 of 2 groups: group 1 (n = 36): vitamin D3 4000 mg per day (given as 1 tablespoon syrup per day); and group 2 n = (49): placebo (given as 1 table spoon syrup per day,) for approximately 6 months. Health worker cadre: CHWs were responsible for the delivery of supplementation to the study participants. The CHWs were assigned to visit study participants, on a fortnightly basis. The first supplementation was provided by the physician at the time of recruitment; later on, the CHWs continued to replenish the supply fortnightly. | |
| Outcomes | Maternal: Periodontal Probing Depth, Interleukin 6 (IL‐6), IL‐2, IL‐4, IL‐10, TNF, IFN‐ɣ and IL‐17 levels. Laboratory method used for assessment of vitamin D concentrations: vitamin D levels were analysed on DiaSorin‐LIASON Inc, kit. | |
| Notes |
Source of funding: the study was supported with a research grant from Pakistan Initiative for Mothers and Newborns (PAIMAN). Dates of the study and location: launched in 2004, Jhelum, Pakistan. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): none declared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The study participants were randomised in blocks. |
| Allocation concealment (selection bias) | Low risk | Allocation codes for vitamin D and placebo were kept in a sealed envelope in a locked cabinet at the Aga Khan University until the completion of the study. |
| Blinding of participants and personnel (performance bias) | Low risk | The investigators, study staff, and the participants were blinded about the group allocation. |
| Blinding of outcome assessment (detection bias) | Low risk | Allocation codes for vitamin D and placebo were kept in a sealed envelope in a locked cabinet at the Aga Khan University until the completion of the study. |
| Incomplete outcome data (attrition bias) | High risk | Only recorded birthweight from 63/85 (74.1%) participants. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
| Methods | Randomised double‐blind controlled trial; 2‐arm design with individual randomisation. | |
| Participants | 126 Asian pregnant women 28 to 32 weeks of gestation attending the antenatal clinic at St George's Hospital, London, UK (latitude: 51°30'N, north of Tropic of Cancer). All pregnant women were first‐generation immigrants mostly from India, Pakistan, Bangladesh, Sri Lanka, Mauritius and east Africa. Exclusion and elimination criteria: preterm deliveries, congenital malformations and maternal illnesses likely to affect fetal growth (such as diabetes) although these data are not presented. | |
| Interventions | Participants were randomly allocated to 1 of 2 groups: group 1 (n = 59) received daily 1000 IU vitamin D (ergocalciferol‐D2) daily until term (estimated total dose: 56,000 to 84,000 IU); and group 2 (n = 67) received a placebo until term. Start of supplementation: 28 to 32 weeks gestation. Length of the intervention/follow‐up: 8 to 12 weeks from supplementation to term. Health worker cadre: St George's Hospital Medical School, London, UK. Medical doctors that were part of the team conducted the measurements and provided the supplements. | |
| Outcomes | Maternal: maternal weight gain, dietary vitamin D intake, 25‐hydroxyvitamin D (25‐OHD) concentrations in cord blood and at term. Plasma calcium (adjusted for albumin concentration), inorganic phosphate, bilirubin, albumin concentrations and total alkaline phosphatase activity, alanine transaminase and ʏ‐glutamyl transferase activities, vitamin D binding globulin concentration, compliance. Infant: weight, crown‐heel length, crown‐rump length, rump‐heel length, occipitofrontal head circumference, forearm length, lower leg length, triceps and subscapular skinfold thickness, fontanelle area, plasma cholecalciferol at day 3 and day 6. weight, length and head circumference at 3, 6, 9 and 12 months. Laboratory method used for assessment of vitamin D concentrations: Serum 25‐hydroxyvitamin D was measured by competitive protein binding assay after chromatographic purification of lipid extracts of serum. | |
| Notes |
Source of funding: the pathological research fund, St George's Hospital Medical School, and the South‐west Thames Regional Health Authority. This study was funded by a combination of a research grant and non governmental organisations. Dates of the study and location: autumn and winter 1977, the whole of 1978 and spring and summer 1979, London, UK. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): none declared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Trial reported random allocation to the groups, although the method of sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | The trial reported that it was double‐blinded but the method of concealment was not described. |
| Blinding of participants and personnel (performance bias) | Low risk | The trial reported that it was double‐blinded. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial reported that it was double‐blinded but they did not specify if those performing the assessments were blinded. |
| Incomplete outcome data (attrition bias) | High risk | Unclear number of randomised participants. Preterm deliveries, congenital malformations, and maternal illnesses likely to affect fetal growth (such as diabetes) were eliminated from the trial. There is not complete documentation of the exclusions. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The study appears to be free of other sources of bias. There were no significant baseline differences between the groups in maternal age, parity, height, vegetarian: non‐vegetarian ratio or the distribution of the various countries of origin. |
| Methods | Randomised trial; 2‐arm design with individual randomisation. | |
| Participants | 40 pregnant women attending their compulsory visit during the third month of pregnancy at the Obstetrical Unit of the Hopital Edouard Herriot, Lyon, France (latitude: 45° 45' 0" N north of Tropic of Cancer). Inclusion criterion: singleton pregnancy at term and uneventful vaginal deliveries. Pre‐gestational BMI and skin pigmentation not reported. | |
| Interventions | Participants were randomly assigned to 1 of 2 groups at the time of the compulsory visit: group 1 (n = 20): women received daily 1000 IU vitamin D (cholecalciferol‐D3) (estimated total dose: 55,000 IU) and group 2 (n = 20): women received no supplement, during the last trimester of pregnancy for 12 weeks from start of supplementation to term. Health worker cadre: compliance was verified by a weekly visit by a midwife. | |
| Outcomes | Maternal: serum (during last trimester of pregnancy) and cord blood immunoreactive PTH, 25‐hydroxyvitamin D (25‐OHD), 1‐alfa,25‐dihydroxyvitamin D (1,25(OH)2D), total calcium, ionised calcium, magnesium, inorganic phosphate. Infant: immunoreactive PTH, 25‐hydroxyvitamin D (25‐OHD), 1‐alfa,25‐dihydroxyvitamin D (1,25(OH)2D), total calcium, ionised calcium, magnesium, inorganic phosphate at 4 days of age. Laboratory method used for assessment of vitamin D concentrations: Serum 25‐hydroxyvitamin D and 1,25‐dihydroxyvitamin D levels were measured by radioligand assays with slight modifications. With sample volumes of 0.75 mL to 1.5 mL, the inter assay variation coefficient for the 2 assays were 8% and 10%, respectively. | |
| Notes |
Source of funding: Shriners of North America, the France‐Quebec Exchange Program, and INSERM Grant 121023. This study was funded by a combination of research grant and non governmental organisations. Dates of the study and location: not reported dates, Lyon, France. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): none declared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Trial reported as randomised but the method of sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | The method of concealment was not described. |
| Blinding of participants and personnel (performance bias) | High risk | The trial reported that women were assigned, by a blind randomisation process, to 1 of 2 groups at the compulsory visit in the third month of pregnancy. It is assumed that it was not blinded to participants as one of the groups did not receive any supplementation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | There is insufficient information to permit judgement. |
| Incomplete outcome data (attrition bias) | High risk | 1 participant from the control group (5%) and 5 (25%) from the vitamin D supplemented group were lost. Laboratory methods reported for 25 to 30 participants (depending on the outcome) out of 40 originally randomised. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
| Methods | Randomised, placebo‐controlled trial; 2‐arm design with individual randomisation. | |
| Participants | 84 pregnant adolescents (13 to 19 years of age) primigravidae (pregnant for the first time) with singleton pregnancies and 23 to 29 weeks of gestation attending prenatal care at the Maternidade Escola, Universidade Federal do Rio de Janeiro, Brazil (latitude: 22.9083° S, 43.1964° W) from September 2009 to June 2011 and intending to exclusively or predominantly breast feed. Women with chronic health problems, pregnancy complications, smokers, users of nutritional supplements besides iron plus folate supplements provided during standard prenatal care, and mothers who decided not to breast feed were excluded from the study. | |
| Interventions | Participants were randomly assigned to: 1 of 2 groups: group 1 (n = 43) received a commercially available supplement (Rexall Sundown®) containing 600 mg calcium (as calcium carbonate) plus 200 IU vitamin D (cholecalciferol‐D3) daily and group 2 (n = 41) received placebo (capsules of microcrystalline cellulose and corn starch; Quintessencia) daily. The protocol allowed pregnant women to continue with their iron and folate supplements, as part of their standard prenatal care. The use and composition of these supplements was not provided. Health worker cadre: capsules of calcium plus vitamin D or placebo were provided monthly to participants by a member of the research team during prenatal visits. Compliance was controlled by counting the remaining capsules at each visit and by telephone reminders. Calcium and vitamin D dietary intake was assessed by at least 3 24‐hour dietary recall questionnaires applied by a trained nutritionist. Standing height and body weight were measured by using a stadiometer (Seca) and a calibrated electronic scale (Filizola), respectively. The same operator performed all scanning and calibration. | |
| Outcomes | Maternal: 1 measurement at 5 and 20 weeks postpartum, serum 25(OH)D, PTH, insulin‐like growth factor (IGF‐I), lumbar spine PA, bone mineral content, serum prolactin and oestradiol. Laboratory method used for assessment of vitamin D concentrations: serum 25‐hydroxyvitamin D, intact PTH, and IGF‐I were analysed by using a chemiluminescent enzyme‐labelled immunometric assay. | |
| Notes |
Source of funding: Conselho Nacional de Desenvolvimento Cientıfico e Tecnologico [grant 471872/2008‐3 (to CMD) and a doctoral fellowship (to MELD)] and the Fundacao Carlos Chagas Filho de Amparo a` Pesquisa do Estado do Rio de Janeiro (grant E‐26/102.759/2008; to CMD), Brazil. This study was funded by a combination of Government programmes and non‐governmental organisations (NGOs). Dates of the study and location: September 2009 to June 2011, Rio de Janeiro, Brazil. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): none of the authors had a conflict of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random assignment was done by a member of the research team in a 1:1 ratio within permuted blocks of size 10. |
| Allocation concealment (selection bias) | Unclear risk | The trial did not report the method of concealment. |
| Blinding of participants and personnel (performance bias) | High risk | The trial reported that it was single‐blinded, only participants were blinded to the assigned groups. It is assumed that the assessment team was not blinded. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgment. |
| Incomplete outcome data (attrition bias) | High risk | Out of 43 women in the intervention group, 13 did not complete the study. Out of 41 women in the placebo group, 14 did not complete the study. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | The study appears to be free of other sources of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled multi‐arm parallel study. | |
| Participants | 260 pregnant women 26 to 30 weeks' gestation, with a singleton pregnancy attending community based primary care maternity clinic in Auckland, New Zealand (latitude 36°S) from April 2010 to July 2011 and then their infants, from birth to age 6 months. Women already taking vitamin D supplementation 200 IU per day, a history of renal stones or hypercalcaemia, or any serious pregnancy complication at enrolment were excluded from the study. | |
| Interventions | Participants were randomly assigned to 1 of 3 mother/infant groups: group 1 (n = 87) women received placebo from 26 to 30 weeks of pregnancy until parturition and their infants also received placebo from 0‐6 months of age; group 2 (n = 87) women received 1000 IU vitamin D (cholecalciferol‐D3) from 26 to 30 weeks of pregnancy until parturition and their infants received 400 IU vitamin D from 0 to 6 moths of age; group 3 (n = 86) women received 2000 IU vitamin D (cholecalciferol‐D3) from 26 to 30 weeks of pregnancy until parturition and their infants received 800 IU from birth to 6 months of age. Data from groups 2 and 3 were combined for our analysis. Health worker cadre: the study was conducted by the research team but it is not reported who provided the supplements or measured the outcomes. | |
| Outcomes | Maternal: serum 25(OH)D concentration. Infant: serum 25(OH)D concentration. Laboratory method used for assessment of vitamin D concentrations: serum 25‐hydroxyvitamin D concentration was measured using isotope‐dilution liquid chromatography–tandem mass spectrometry in a Vitamin D External Quality Assurance Scheme–certified laboratory. | |
| Notes |
Source of funding: Health Research Council of New Zealand, grant number 09/215R. Dr Mitchell is supported by Cure Kids. Study medicine was prepared by the Ddrops Company (Woodbridge, Ontario, Canada). This study was funded by a combination of government programmes and non‐governmental organisations (NGOs). Dates of the study and location: April 2010 to July 2011, Auckland, New Zealand. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): the authors have indicated they have no potential conflicts of interest to disclose. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Trial reported computer‐generated randomisation list. |
| Allocation concealment (selection bias) | Low risk | The allocation sequence was concealed from research staff involved in recruitment. Trial reported randomly allocated treatment to each participant and labelled identical study medicine bottles such that study staff and participants were unaware of the treatment status. |
| Blinding of participants and personnel (performance bias) | Low risk | The study statistician randomly allocated a treatment to each participant and labelled identical study medicine bottles such that study staff and participants were unaware of the treatment status. |
| Blinding of outcome assessment (detection bias) | Low risk | The study staff and participants were unaware of the treatment status. |
| Incomplete outcome data (attrition bias) | Low risk | Reported compliance did not differ between groups. In the placebo group, 6 did not complete the study; in the lower dose vitamin D group, 6 did not complete the study. In the higher vitamin D dose group, 6 did not complete the study. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial. | |
| Participants | 1200 pregnant women living in the UK, aged 18 years old and older, with a singleton pregnancy with less than 17 weeks' gestation at first assessment (based on last menstrual period and dating scan), aiming to give birth at local maternity hospital, and with serum 25‐hydroxyvitamin D is 25 to 100 nmol/L at nuchal fold/dating scan (10 to 17 weeks' gestation). | |
| Interventions | Participants were randomly assigned to 1 of 2 groups: group 1 (n = 565): received 1000 IU cholecalciferol orally daily and group 2 (n = 569): received placebo, starting from 14 weeks' gestation until delivery. Health worker cadre: the medication was blister packed in a single box for each woman for the duration of pregnancy. Study medication (active/placebo) was supplied to the local pharmacy pre‐randomised by the manufacturer (1:1, unstratified by centre) and sequentially numbered for storage and dispensing. Code break envelopes were supplied to the lead pharmacist, but were not available to the investigative team. Emergency code break access was available through the local principal investigator and on call pharmacist. A single pack for each participant was issued sequentially (containing all pills for duration of the study). Each pack was individually prescribed for each participant. The trials pharmacist allocated a pack to that prescription, documenting both the pack number and the MAVIDOS participant ID; these were checked again by the research nurse on collection, and documented in the participant’s notes; the medication pack came with a tear‐off adhesive label, which was placed in the participant’s notes as an added safeguard against errors in pack allocation. The research nurse collected the medication pack for all participants attending to the clinic that day and issued to the participants directly. | |
| Outcomes | Infant: whole body bone mineral content of the neonate adjusted for gestational age and age at neonatal DXA scan, whole body bone area, bone mineral density, and size corrected bone mineral density (BMC adjusted for BA, length and weight), body composition adjusted for gestational age and age at DXA scan. Laboratory method used for assessment of vitamin D concentrations: A blood sample was taken and plasma was stored at ‐80°C for measurement of 25(OH)‐vitamin D, vitamin D binding protein (DBP), calcium, bone specific alkaline phosphatase and albumin centrally (MRC Human Nutrition Research, Cambridge, UK) at the end of the study. | |
| Notes |
Source of funding: Arthritis Research UK, Medical Research Council, Bupa Foundation, and National Institute for Health Research. Study was funded by a combination of research grants, government programmes, non‐governmental organizations (NGOs). Dates of the study and location: October 2008 to February 2014, Southampton, Sheffield, Oxford, the UK. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): CC reports personal fees, consultancy, lecture fees, and honoraria from Alliance for Better Bone Health, Amgen, Eli Lilly, GlaxoSmithKline, Medtronic, Merck, Novartis, Pfizer, Roche, Servier, and Takeda, outside the submitted work. NCH reports personal fees, consultancy, lecture fees, and honoraria from Alliance for Better Bone Health, AMGen, MSD, Eli Lilly, Servier, Shire, Consilient Healthcare, and Internis Pharma, outside the submitted work. NJB reports remuneration from Internis Pharmaceuticals, outside the submitted work. ATP reports grants from the Arthritis Research Council, during the conduct of the study. NKA has received honoraria, held advisory board positions (which involved receipt of fees), and received consortium research grants from Merck, grants from Roche, Bioiberica, and Novartis, personal fees from Smith & Nephew, Nicox, Flexion, Bioventus, and Freshfields, outside the submitted work. KMG reports reimbursement for speaking at Nestle Nutrition Institute conferences, and grants from Abbott Nutrition and Nestec, outside the submitted work. KMG also has a patent pending for phenotype prediction, a patent pending for predictive use of CpG methylation, and a patent pending for maternal nutrition composition, not directly related to this work. HMI reports grants from the Medical Research Council (MRC), Arthritis Research UK, and European Union’s Seventh Framework Programme, during the conduct of the study; and while not directly receiving funding from other bodies, members of her team have received funding from the following companies from other work: Danone, Nestec, and Abbott Nutrition. RE reports grants and personal fees from Amgen and Alexion; grants from the Department of Health, AstraZeneca, ARUK/MRC Centre for Excellence in Musculoskeletal Ageing Research, National Institute for Health Research, MRC/AZ Mechanisms of Diseases Call, and the MRC; grants, personal fees, and non‐financial support from Immunodiagnostic Systems; grants and membership of a clinical and scientific committee from the National Osteoporosis Society; grants, personal fees, and advisory board membership from Roche; personal fees from Otsuka, Novartis, Merck, Bayer, Johnson & Johnson, Fonterra Brands, Janssen Research, Ono Pharma, Alere (Unipath), Chronos, Teijin Pharma Limited, D‐STAR, and GSK Nutrition; personal fees and advisory board membership from Eli Lilly, and CL Biosystems; and advisory board membership from the European Calcifi ed Tissue Society, IOF CSA, and the American Society for Bone and Mineral Research, outside the submitted work. MKJ reports personal fees from Stirling Anglia, Consilient Health, and Internis, outside the submitted work. All other authors declare no competing interests. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence in randomly permuted blocks of 10. |
| Allocation concealment (selection bias) | Low risk | The treatments were blister packed in a single box for each woman for the duration of pregnancy and supplied to the local pharmacy pre‐randomised by the manufacturer (1:1, unstratified by centre) and sequentially numbered for storage and dispensing. The lead pharmacist was the only one with access to the code break envelopes. |
| Blinding of participants and personnel (performance bias) | Low risk | Double‐blinded, matched pills, only lead pharmacist knew about pills. |
| Blinding of outcome assessment (detection bias) | Low risk | All assessments were double‐blinded. |
| Incomplete outcome data (attrition bias) | Low risk | 94% of sample had vitD assessment at term. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | High risk | Participants were allowed to continue taking their own multivitamin with 400 IU/d of vitamin D but this was not recorded. |
| Methods | Randomised controlled trial. | |
| Participants | 50 pregnant women with similar socioeconomic conditions in India. | |
| Interventions | Participants were randomised into 2 groups: group 1 (n = 25) received orally 2 pharmacological doses of vitamin D˜ (60,000 IU each) in 6th and 7th month of pregnancy; group 2 (n = 25) did not receive any vitamin supplement and served as controls. Health worker cadre: not specified. | |
| Outcomes | Infant: mean birthweight, placental weight and DNA content, total protein and RNA, protein/DNA and RNA/DNA ratios. Laboratory method used for assessment of vitamin D concentrations: not applicable. | |
| Notes |
Source of funding: unknown/unreported. Dates of the study and location: not reported dates, India. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Authors only mentioned that women were randomly selected for trial initially. |
| Allocation concealment (selection bias) | Unclear risk | The trial did not report the method of concealment. It is assumed that no method was used as one of the groups did not receive any supplementation. |
| Blinding of participants and personnel (performance bias) | High risk | The trial did not report if it was blinded. It is assumed that it was not blinded to participants as one of the groups did not receive any supplementation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | There is insufficient information to permit judgement. |
| Incomplete outcome data (attrition bias) | Unclear risk | The number lost to follow‐up was not reported in results. |
| Selective reporting (reporting bias) | Unclear risk | The total number of participants that completed the study was not specified in results. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
| Methods | Clinical controlled trial with 3 arms. | |
| Participants | 88 pregnant women with a predisposition to pregnancy‐induced hypertension, at 20 to 24 weeks' gestation, a BMI index of lower than 24, and an arterial pressure of < 11.3 kPa attending an outpatient clinic and labour ward of the First Afilliated Hospital of Xi’an Medical University, Xi’an, China. | |
| Interventions | Participants were divided into 3 groups: group 1 (n = 29) received a daily dose of a tablet containing 600 mg of calcium and 200 IU of vitamin D (Caltrate‐D) daily from 20 to 24 weeks until deliver; group 2 (n = 29) received 1200 mg of calcium and 400 IU vitamin D (Caltrate‐D) daily from 20 to 24 weeks until deliver; group 3 (n = 30) received no intervention from 20 to 24 weeks until delivery. Health worker cadre: not specified. | |
| Outcomes | Maternal: blood pressure, ionised calcium and platelet intracellular calcium, incidence rates of pregnancy‐induced hypertension. Laboratory method used for assessment of vitamin D concentrations: not applicable. | |
| Notes |
Source of funding: unknown/unreported. Dates of the study and location: August 1996 to December 1998, China. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): none declared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | The trial did not report if participants were randomly allocated to the treatment groups. It is unclear if it was random or not. |
| Allocation concealment (selection bias) | Unclear risk | The trial did not report the method of concealment. It is assumed that it was not conceal as one of the groups did not receive any supplementation |
| Blinding of participants and personnel (performance bias) | High risk | The trial did not report if it was blinded. It is assumed that it was not blinded to participants as one of the groups did not receive any supplementation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial did not mention if the study was single or double blinded. |
| Incomplete outcome data (attrition bias) | High risk | Loss to follow‐up not reported. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to make a judgement. |
| Other bias | High risk | The report is very short, with most details of the methods not available. |
| Methods | Randomised controlled trial; 3‐arm design with individual randomisation. | |
| Participants | 77 white pregnant women 18 to 36 years of age in the last trimester of pregnancy living in Northwest of France (latitude: 49° 26' 0" N north of Tropic of Cancer). Pre‐gestational BMI not reported. | |
| Interventions | Participants were randomly assigned to 1 of 3 groups: group 1 (n = 21) women received daily 1000 IU of vitamin D (ergocalciferol‐D2) for the last 3 months of pregnancy (estimated total dose throughout pregnancy: 90,000 IU); group 2 (n = 27) women received a single dose of 200,000 IU (5 mg) vitamin D at the 7th month of pregnancy; group 3 (n = 29) women received no supplement and served as controls. Length of the intervention/follow‐up: 12 weeks from start of supplementation to term. Health worker cadre: the study was conducted by the research team at the maternity of Balvedere, Rouen, France but the roles are not described. It is unclear who provided the supplements and measured the outcomes. | |
| Outcomes | Maternal: 24‐hour urinary calcium excretion after 6 weeks supplementation, calcium, 25‐hydroxyvitamin D (25‐OHD) and1‐alfa,25‐dihydroxyvitamin D (1,25(OH)2D) metabolites of vitamin D from serum and cord during labour and delivery. Infant: serum calcium levels at days 2 and 6 of life, birthweight. Laboratory method used for assessment of vitamin D concentrations: for 25‐hydroxyvitamin D and 1,25‐dihydroxyvitamin D determinations the following techniques were used: extraction with chloroform‐methanol‐water according to Preece, double step purification, first on a Sephadex LH 20 column with chloroform hexan 45 to 55 vol/vol as solvent, then on a high‐pressure liquid pression system according to Shepard. Plasma metabolites were measured by competitive assay using rat protein for 25 OHD and chicken intestine cytosol for 1,25 (OH)2 D according to Jongen. Assay sensitivity for 1,25 (OH)2 D was 5 pmol/tube and for 25 OHD was 25 pmol/tube. | |
| Notes |
Source of funding: unknown/unreported. Dates of the study and location: January 1979 to December 1982, France. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): none declared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was conducted by random numbers table. |
| Allocation concealment (selection bias) | Unclear risk | The trial did not report the method of concealment. It is assumed that it was not conceal as one of the groups did not receive any supplementation. |
| Blinding of participants and personnel (performance bias) | High risk | The trial did not report if it was blinded. It is assumed that it was not blinded to participants as one of the groups did not receive any supplementation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial did not report if it was blinded. |
| Incomplete outcome data (attrition bias) | High risk | It is unclear if there was attrition, but given the uneven number of participants reported, it is likely that there were losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | High risk | Groups are reported with notorious different sample sizes. It is unclear whether the numbers reflect the participants who finished the trial (unclear and uneven losses to follow‐up); a non randomised process; or a selection bias in which randomised participants did not receive the intervention. |
| Methods | Randomised controlled trial; 2‐arm design with randomisation at individual level. | |
| Participants | 400 pregnant women 20 to 35 years of age, attending the antenatal clinic of Medical College Hospital in Rohtak, India (latitude: 76° 34' 0' north of Tropic of Cancer). Pre‐gestational BMI and skin pigmentation not reported. | |
| Interventions | Participants were allocated to 1 of 2 groups: group 1 (n = 200) received a daily supplement containing 1200 IU vitamin D and 375 mg calcium (estimated total dose from week 20 to 24 of gestation to term:134,400‐168,000 IU); group 2 (n = 200) received no supplement from 20 to 24 weeks of pregnancy until delivery and served as controls. Length of the intervention/follow‐up: 20 to 24 weeks from start of supplementation to term. Health worker cadre: not specified. | |
| Outcomes | Maternal: pre‐eclampsia (defined as blood pressure of 140 mmHg or higher systolic and/or 90 mmHg diastolic along with proteinuria higher than 300 mg/24 hours); systolic and diastolic blood pressure at 24, 28, 32 and 36 weeks of gestation. Serum calcium and creatinine. Laboratory method used for assessment of vitamin D concentrations: not applicable. | |
| Notes | Biochemical analyses were made for those who developed pre‐eclampsia (n = 12) and also in a group of women with no pre‐eclampsia (n = 25) and a control group of non pregnant women. The results of the stratified analysis are not reported in this review.
Source of funding: unknown/unreported. Dates of the study and location: not reported dates, India. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): none declared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial reported that participants were randomly allocated to the intervention groups but they did not report the method of sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | The trial did not report the method of concealment. It is assumed that they did not conceal the allocation as one of the groups did not receive any supplementation. |
| Blinding of participants and personnel (performance bias) | High risk | The trial did not report if the study was blinded. It is assumed that it was not blinded to participants as one of the groups did not receive any supplementation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial did not report if the research staff was blinded. |
| Incomplete outcome data (attrition bias) | High risk | Only data on biochemical were reported for those who developed pre‐eclampsia and some of those with no pre‐eclampsia and a group of non pregnant controls. |
| Selective reporting (reporting bias) | High risk | Outcomes reported for some subgroups only. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
| Methods | Randomised clinical trial; 2‐arm design with individual randomisation. | |
| Participants | 200 pregnant women, aged 22 to 35 years old, attending the antenatal clinic of the Medical College Hospital, Rohtak, India (latitude: 76° 34' 0' north of Tropic of Cancer). Inclusion criterion: uncomplicated single pregnancy. Exclusion criteria: pre‐eclampsia, antepartum haemorrhage, premature delivery. Pre‐gestational BMI and skin pigmentation not reported. | |
| Interventions | Participants were allocated to 1 of the following groups: group 1 (n = 100) women received 2 doses of 600,000 IU (each dose at 7th and 8th month of pregnancy (estimated total dose: 1,200,000 IU); group 2 (n = 100) women received no intervention and served as controls. Length of the intervention/follow‐up: 12 weeks from start of supplementation to term. Health worker cadre: not specified. | |
| Outcomes | Maternal: venous and cord serum calcium, serum proteins, inorganic phosphate, alkaline phosphatase, weight. Radiological examination on women with abnormal biochemistry or osteomalacia symptomatology. Side effects: back age, leg‐pains, general weakness, cramps. Infant: birthweight, LBW, crown‐heel length, head circumference, mid‐arm circumference within 24 hours after birth. Skinfold thickness (triceps and infrascapular). Laboratory method used for assessment of vitamin D concentrations: not applicable. | |
| Notes |
Source of funding: unknown/unreported. Dates of the study and location: not reported dates, India. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): none declared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial reported that participants were randomly allocated to the intervention groups but they did not report the method of sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | The trial did not report the method of concealment. It is assumed that they did not conceal the allocation as one of the groups did not receive any supplementation. |
| Blinding of participants and personnel (performance bias) | High risk | The trial did not report if the study was blinded. It is assumed that it was not blinded to participants as one of the groups did not receive any supplementation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial did not report if the research staff was blinded. |
| Incomplete outcome data (attrition bias) | Unclear risk | Losses to follow‐up are not documented although exclusions included pregnancy complications. Results tables mention that each arm was comprised of 100 women, a number that corresponds to that described for the treatment allocation. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
| Methods | Randomised control trial. | |
| Participants | 72 pregnant women with physiological pregnancy aged 18 to 35 years with low alimentary consumption of calcium (< 600 mg/day) who attended to Moscow State University of medicine and dentistry, department of obstetrics and gynaecology. (Latitude: 55.7500° N, 37.6167° E). | |
| Interventions | Participants were randomly assigned to 1 of 2 groups: group 1 (n = 43) received 1250 mg of calcium carbonate and 200 IU of vitamin D (cholecalciferol‐D3) from the second pregnancy trimester until term, in 2 takes a day; group 2 (n = 29) did not receive any treatment and served as controls. Health worker cadre: not specified. | |
| Outcomes | Maternal: resistance of uterine arteries, resistance of umbilical arteries, uterine‐placental circulation. Infant: fetal‐placental circulation, intrauterine growth retardation, assessed by dopplerometry. Laboratory method used for assessment of vitamin D concentrations: not applicable. | |
| Notes |
Source of funding: unknown/unreported. Dates of the study and location: not reported dates, Moscow, Russia. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): none declared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial reported that participants were randomly allocated to the intervention groups but they did not report the method of sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | The trial did not report the method of concealment. It is assumed that they did not conceal the allocation as one of the groups did not receive any supplementation. |
| Blinding of participants and personnel (performance bias) | High risk | The trial did not report if the study was blinded. It is assumed that it was not blinded to participants as one of the groups did not receive any supplementation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial did not report if research staff was blinded. |
| Incomplete outcome data (attrition bias) | Unclear risk | There is insufficient information to permit judgement. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
| Methods | Triple‐blind randomised controlled clinical trial. | |
| Participants | 126 pregnant women, aged 18 to 39 years with gestational age of 25 to 30 weeks referring to Tabriz health centres, Iran in 2013 to 2014. | |
| Interventions | Participants were allocated to 3 groups using a randomised block design with block sizes of 3 and 6 with the allocation ratio 1:1:1: group 1 (n = 40) Calcium‐vitamin D group (300 mg carbonate calcium plus 1000 units of vitamin D supplements; group 2 (n = 42) vitamin D group (1000 units of vitamin D supplements; and group 3 (n = 42) received placebo. To hide the allocation, each participant received 2 small envelopes, each with enough medicine for 3 weeks, inside a large matte‐coloured envelope of the same shape that were serially numbered. Each participant received 1 pill every day for 42 days. All pills were of the same shape, size, and weight. Health worker cadre: not specified. | |
| Outcomes | Maternal: gestational age, mode of delivery based on gestational age. food consumption, in terms of calcium and vitamin D content, pre‐pregnancy BMI, BMI during pregnancy Infant: weight, height, and head circumference, birthweight, height, head circumference. Laboratory method used for assessment of vitamin D concentrations: not specified. | |
| Notes |
Source of funding: this study was funded by a research grant of Tabriz University of Medical Sciences (Project number: 388). Dates of the study and location: July 2013 to April 2014, Iran. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): no conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were allocated to 3 groups using a randomised block design with block sizes of 3 and 6 with the allocation ratio 1:1:1. |
| Allocation concealment (selection bias) | Unclear risk | To hide the allocation, each participant received 2 small envelopes, each with enough medicine for 3 weeks, inside a large matte‐coloured envelope of the same shape that were serially numbered. Each participant received 1 pill every day for 42 days. Pills were of the same shape, size, and weight. However, authors did not mention how this was concealed from study staff. |
| Blinding of participants and personnel (performance bias) | Low risk | Participants were blinded to the study treatments. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial reported that it was double‐blinded but they did not specify if those performing the assessments were blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Losses to follow‐up were documented. No missing data and no participant was eliminated from the analysis. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
| Methods | Double‐blind randomised controlled trial. | |
| Participants | 140 nulliparous pregnant women who had been referred to “Shahid Beheshti” hospital in Isfahan, Iran. Pregnant women at less than 16 weeks' gestation from outpatient clinics at “Shahid Beheshti” hospital were eligible if they did not have any sign of vitamin D deficiency, did not using aspirin and had no diagnosis of chronic hypertension, gestational diabetes, renal disease or systemic lupus erythematous. | |
| Interventions | Subjects were randomly divided into 2 groups: Group 1 (n = 70) received supplementation with 600 IU daily of vitamin D at 16 weeks' gestation until labour; Group 2 (n = 70) received daily supplementation free of vitamin D and followed until labour (placebo group). Women were unaware of the treatment allocation. Health worker cadre: women were followed up monthly by a doctor who was blinded to the study groups. | |
| Outcomes | Maternal: age and gestational age at delivery, pre‐eclampsia Infant: birthweight Laboratory method used for assessment of vitamin D concentrations: not applicable. | |
| Notes |
Source of funding: this study was funded by a research grant. Financial support was provided by the Isfahan University of Medical Sciences (Grant 392004); Isfahan, Iran. Dates of the study and location: May 2012 to January 2012, Iran. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): none declared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Using random‐maker software “Random Allocation”, participants were randomly divided into 2 groups: intervention and placebo. |
| Allocation concealment (selection bias) | Unclear risk | Women were unaware of the treatment allocation but no other information was provided. |
| Blinding of participants and personnel (performance bias) | Low risk | Research staff was unaware of the treatment allocation. |
| Blinding of outcome assessment (detection bias) | Low risk | Follow‐up visits was done by blinded study personnel. |
| Incomplete outcome data (attrition bias) | Low risk | 2 participants for the intervention group were missing, but it was explained in the results section that they did not want to continue in the study. Total of 138 participants (68 cases and 70 controls) were analysed and described |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
| Methods | Randomised placebo‐controlled trial (AViDD‐2 trial) | |
| Participants | 160 pregnant women aged 18 < 35 years old, attending to the International Centre for Diarrhoeal Disease Research, Dhaka, Bangladesh (latitude: 23.7000° N, 90.3750° E, north of the Tropic of Cancer). Inclusion criteria: women with residence in Dhaka, with plans to have the delivery performed at the Shimantik maternity centre, and to stay in Dhaka throughout the pregnancy and 1 month past the delivery, with gestational age of 26th to 29th (inclusive), estimated based on the first day of the last menstrual period. Exclusion criteria: use of any dietary supplement containing more than 400 IU/day (10 mcg/day) of vitamin D within the month prior to enrolment, or refusal to stop taking supplemental vitamin D at any dose after enrolment, current use of anti‐convulsant or anti‐mycobacterial (tuberculosis) medications, severe anaemia (haemoglobin concentration < 70 g/L), complicated medical or obstetric history: cardiovascular disease, uterine haemorrhage, placenta praevia, threatened abortion, hypertension, pre‐eclampsia, preterm labour, or multiple gestation), prior history of delivery of an infant with a major congenital anomaly, birth asphyxia, or perinatal death (stillbirth or death within first week of life). | |
| Interventions | Participants were randomly assigned to 1 of 2 groups: group 1 (n = 80): women received vitamin D (cholecalciferol‐D3) 35,000 IU per week, started at 26 to 29 weeks' gestation, until delivery; group 2 (n = 80): women received placebo control administered weekly from 26 to 29 weeks' gestation until delivery. Health worker cadre: supplement doses were measured in disposable plastic syringes and orally administered by study personnel. | |
| Outcomes | Maternal: serum 25‐hydroxyvitamin D concentration, serum calcium concentration, urine Ca:Cr ratio. Infant: immune function, infant growth, postnatal vitamin D status, serum calcium. Laboratory method used for assessment of vitamin D concentrations: Serum 25‐hydroxyvitamin D was quantified by high‐performance liquid chromatography tandem mass spectroscopy (LCMS/MS) in the Department of Pathology and Laboratory Medicine at the Hospital for Sick Children. | |
| Notes |
Source of funding: this study was funded by a Non‐governmental organization (NGO). The Thrasher Research Fund, Salt Lake City, USA. Dates of the study and location: August 2010 to January 2011, Dhaka, Bangladesh. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): the authors declare that they have no competing interests. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Trial reported computer‐generated randomisation list for the randomisation procedures. |
| Allocation concealment (selection bias) | Low risk | The allocation sequence was prepared by International Centre for Diarrhoeal Disease Research, Dhaka, Bangladesh personnel not otherwise involved in the study, and was concealed from investigators. |
| Blinding of participants and personnel (performance bias) | Low risk | Trial reported that participants were blinded to allocation. |
| Blinding of outcome assessment (detection bias) | Low risk | Trial reported that research staff (including lab personnel) were blinded to allocation. |
| Incomplete outcome data (attrition bias) | Low risk | Of the 160 participants recruited and randomly assigned to intervention or placebo, 13 were lost to follow‐up prior to delivery (6 in the placebo group and 7 in the vitamin D group), all because of having left the Dhaka area. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial (MDIG trial). | |
| Participants | 1300 generally‐healthy pregnant women between 17 and 24 weeks of gestation. | |
| Interventions | Participants were randomly assigned at enrolment to 1 of 5 groups: group 1 (n = 260) received placebo throughout the prenatal period and for 26 weeks postpartum; group 2 (n = 260) received 4200 IU per week prenatally and no supplementation postpartum; group 3 (n = 260) received 16,800 IU per week prenatally and no supplementation postpartum; group 4 (n = 260) received 28,000 IU per week prenatally and no supplementation postpartum; and group 5 (n = 260) received 28,000 IU per week prenatally and during the postpartum for 26 weeks. Data from groups 2‐5 were combined into the intervention group for this analysis. All participants received calcium (500 mg per day), iron (66 mg per day), and folic acid (350 mcg per day) throughout the intervention phase. Health worker cadre: trial personnel contacted participants weekly from enrolment until 26 weeks postpartum, and infants were further assessed at 9 months and 12 months of age. Visits were conducted in the home or at a clinic and included the use of standardized questionnaires, point‐of‐care tests, anthropometric measurements, and specimen collection. | |
| Outcomes | Maternal: maternal serum 25‐hydroxyvitamin D and calcium concentration, urinary calcium excretion, and maternal PTH concentrations. Infant: length‐for‐age, birth outcomes, morbidity and serum 25‐hydroxyvitamin D and calcium concentrations. Laboratory method used for assessment of vitamin D concentrations: point‐of‐care tests. | |
| Notes |
Source of funding: this study was funded by the Bill & Melinda Gates Foundation. Dates of the study and location: March 2014 to September 2015, Dhaka, Bangladesh. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): no potential conflict of interest was reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was conducted by computer‐generated, simple randomisation scheme created independently by the trial statistician. |
| Allocation concealment (selection bias) | Low risk | Concealment of trial‐group assignments was ensured with the use of pre‐labelled and sequentially numbered but otherwise identical supplement vials. |
| Blinding of participants and personnel (performance bias) | Low risk | The trial reported that a master list linking participants to supplementation groups was not accessible to trial personnel until final group assignments were revealed. |
| Blinding of outcome assessment (detection bias) | Low risk | The trial reported that a master list linking participants to supplementation groups was not accessible to trial personnel until final group assignments were revealed. |
| Incomplete outcome data (attrition bias) | Low risk | Among 1164 infants assessed at 1 year of age (89.5% of 1300 pregnancies), < 5% of participants withdrew or were excluded after randomisation until birth. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | There is no any evidence of other bias. |
| Methods | Randomised, double‐blind trial | |
| Participants | 50 pregnant women, in their third trimester, who were scheduled to deliver at Mahdieh Hospital in Tehran. | |
| Interventions | Participants were randomly allocated to 1 of 2 groups: Group 1 (n = 25) received oral vitamin D3 100,000 IU monthly, 3 times; Group 2 (n = 25) control (placebo); until term. Health worker cadre: not specified. | |
| Outcomes | Maternal: the final maternal 25(OH) serum concentrations at delivery, cord 25(OH) vitamin D concentration serum 25(OH), maternal serum iPTH and cord blood iPTH concentration mean PTH concentration Infant: serum vitamin D lower than30 ng/mL in newborn infants Laboratory method used for assessment of vitamin D concentrations: Serum 25 (OH) D concentrations were measured by EIA using the 25(OH) Vit D kit (Immune diagnostic system Ltd, Bolden, UK). | |
| Notes |
Source of funding: this study was funded by a research grant from the Research Institute of Endocrine Sciences, Shahid Beheshti University of Medical Sciences. Dates of the study and location: 2009 to 2010, Tehran, Iran. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): no conflict of interest declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomly allocated to the treatment or placebo but methods describing this process were not reported. |
| Allocation concealment (selection bias) | Unclear risk | The trial reported that it was double‐blinded, but no methods of describing the process were reported. |
| Blinding of participants and personnel (performance bias) | Low risk | The trial reported that it was double‐blinded, but no methods of describing the process were reported. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial reported that it was double‐blinded but they did not specify if those performing the assessments were blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Data reported for all 50 participants. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
| Methods | Randomised controlled trial with 2 arms, with randomisation at the individual level from years 2010 to 2012. | |
| Participants | 180 primigravidae women with singleton pregnancy at 14 to 20 weeks in the Department of Obstetrics and Gynaecology in Safdarjung Hospital, New Delhi, India (28°38′08″ N, 77°13′28″ E north of Tropic of Cancer). | |
| Interventions | Participants were randomly assigned to 1 of 2 groups: group 1 (n = 60) did not receive any supplementation of vitamin D; group 2 (n = 120) received vitamin D (cholecalciferol‐D3) supplementation in dosages depending upon the level of serum 25(OH)‐D levels estimated at entry into the study. Participants from this second group with sufficient levels of vitamin D (serum 25(OH)‐D levels > 50 nmol/L), received only 1 dose of 60,000 IU vitamin D (cholecalciferol‐D3) at 20 weeks; participants with insufficient levels of vitamin D (serum 25(OH)‐D levels 25–50 nmol/L) received 2 doses of 120,000 IU vitamin D (cholecalciferol‐D3) at 20 weeks and 24 weeks; and participants with deficient levels of vitamin D status (serum 25(OH)‐D levels < 25 nmol/L) received 4 doses of 120,000 IU vitamin D cholecalciferol‐D3) at 20, 24, 28 and 32 weeks. Independently of the dose, all participants in group 2 were grouped and compared to group 1 for this analysis. Health worker cadre: unclear what the roles of the researchers and other workers in the health worker cadre. | |
| Outcomes | Maternal: preterm labour, pre‐eclampsia, gestational diabetes, serum 25(OH)‐D concentration, serum calcium, phosphorus and serum ALP levels. Laboratory method used for assessment of vitamin D concentrations: serum 25‐hydroxyvitamin D was quantified by sandwich ELISA. | |
| Notes |
Source of funding: self‐funded. Dates of the study and location: 2010 to 2012, India. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): all the authors have nothing to disclose | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was performed using computer‐generated random number tables. |
| Allocation concealment (selection bias) | High risk | As participants were assigned to either no intervention or intervention and the intervention dosage depended on the vitamin D status, there was a selection bias based on status of vitamin D at baseline. |
| Blinding of participants and personnel (performance bias) | High risk | The trial did not report if the study was blinded. It is assumed that it was not blinded to participants as one of the groups did not receive any supplementation and the other groups received different doses of vitamin D at different times. |
| Blinding of outcome assessment (detection bias) | Unclear risk | At the time of delivery, both the groups underwent clinical evaluations and complete anthropometric assessment of the neonate, but it was not reported if staff was blinded to the intervention groups. |
| Incomplete outcome data (attrition bias) | High risk | The level of attrition was different in groups 1 and 2: 3/60 (5%) participants in group 1 and 12/120 (10%) participants in group 2 were lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The study appears to be free of other evident sources of bias. |
| Methods | Prospective, double‐blind, placebo‐controlled trial. | |
| Participants | 60 primigravida pregnant women, aged 18–40 years old, who were at risk for pre‐eclampsia, and lived approximately 20 km or less from the clinic and hospital. Women ‘at‐risk’ for pre‐eclampsia were recognised by laboratory tests including free β‐human chorionic gonadotrophin, inhibin a dimeric, unconjugated oestriol and maternal serum α‐foetoprotein, and haemodynamic assessment of uterine artery Doppler wave form at 16 to 20 weeks of gestation. | |
| Interventions | Participants were randomly allocated into 2 groups: Group 1 (n = 30) received 50,000 IU vitamin D3 every 2 weeks plus 1000 mg day 1 calcium supplements (as calcium carbonate); Group 2 (n = 30) received placebos at the same times; from 20 to 32 weeks of gestation. Health worker cadre: an investigator with no clinical involvement in the present study packed cholecalciferol, calcium supplements and placebos into numbered bottles based on the random list. Anthropometric measurements of pregnant women at maternity clinic were measured by a trained midwife at baseline and then after 12 weeks of intervention. | |
| Outcomes | Maternal: serum 25(OH)D concentrations, fasting plasma glucose, serum insulin concentrations, homeostasis model assessment (HOMA)‐B, inQUICKI score, serum HDL‐cholesterol, plasma GSH concentrations, systolic blood pressure, diastolic blood pressure, lipid profiles and inflammatory markers, pre‐eclampsia. Infant: LBW (< 2500 g), newborn’s birth size (newborn’s weight, length and head circumference) and prevalence of preterm delivery (< 37 weeks). Laboratory method used for assessment of vitamin D concentrations: Serum 25‐hydroxyvitamin D concentrations was determined using a commercial enzyme‐linked immunosorbent assay (ELISA) kit (IDS, Boldon, UK) with inter‐ and intra‐assay coefficients of variation (CVs) of 4.5–7.0%, respectively. | |
| Notes |
Source of funding: the study was supported by a research grant from Kashan University of Medical Sciences. Dates of the study and location: September 2014 to February 2015, Kashan, Iran. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): the authors declare that there are no conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Parallel, balanced randomisation (1:1). |
| Allocation concealment (selection bias) | Low risk | Randomisation and allocation were concealed from both researchers and participants until the statistical analysis was completed. |
| Blinding of participants and personnel (performance bias) | Low risk | Only the person responsible for the distribution of drugs knew how the women were allocated to the treatment groups. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial reported that it was double‐blinded but they did not specify if those performing the assessments were blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Data were reported for all participants. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
| Methods | Double‐blind randomised and controlled clinical trial. | |
| Participants | 80 women aged 18 to 35 years were examined from November 2013 to March 2015 at the Shabihkhani Maternity Hospital in Kashan, Iran. | |
| Interventions | Participants were randomised into 2 groups: Group 1 (n = 40) received a pill of vitamin D3 400 IU/day and Group 2 (n = 40) received a placebo tablet that was similar to vitamin D3, with no active ingredient as a placebo. Both groups received standard treatment with vaginal progesterone (Behvarzan, Iran) at a dose of 400 mg per day. The serum levels of vitamin D3 were evaluated in the tenth and twentieth weeks to prevent any possible poisoning. If so, the patient was excluded from the study. Health worker cadre: all participants in the study received antenatal care and were given folic acid and ferrous sulphate at least 1 month prior to pregnancy, under the supervision of a gynaecologist. They were checked by monitoring serum β‐hCG level levels and abdominal ultrasound until the confirmation of pregnancy, after which the mothers were divided into 2 groups of intervention and control using permuted block randomisation with twenty blocks of size 4. Only the person responsible for the distribution of drugs knew how the women were allocated to the treatment groups. | |
| Outcomes | Maternal: the serum level of vitamin D3, serum level of IL‐23, serum levels of vitamin D3 and IL‐23, spontaneous abortions. Laboratory method used for assessment of vitamin D concentrations: not specified. | |
| Notes |
Source of funding: this study was funded by a research grant of the Kashan University of Medical Sciences. Dates of the study and location: November 2013 to March 2015, Kashan, Iran. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): the authors declare that there is no conflict of interests regarding the publication of this paper. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were divided into 2 groups of intervention and control using permuted block randomisation with 20 blocks of size 4. |
| Allocation concealment (selection bias) | Low risk | Only the person responsible for the distribution of drugs knew how the women were allocated to the treatment groups. |
| Blinding of participants and personnel (performance bias) | Low risk | Only the person responsible for the distribution of drugs knew how the women were allocated to the treatment groups. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial reported that it was double blinded but they did not specify if those performing the assessments were blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Data were reported for all participants. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
| Methods | Randomised controlled clinical trial. | |
| Participants | 142 women who were referred to the obstetrical clinic in Besat Hospital of Sanandaj City, Kurdistan Province, Iran, who were receiving prenatal care and had a history of pre‐eclampsia in previous pregnancies. | |
| Interventions | The participants were randomly placed into 2 groups: Group 1 (n = 70) received 50,000 IU pearl vitamin D3 once every 2 weeks; and Group 2 (n = 72) received placebo. Vitamin D or placebo was given until the 36th week of pregnancy. Health worker cadre: not specified. | |
| Outcomes | Maternal: level of vitamin D, pre‐eclampsia. Laboratory method used for assessment of vitamin D concentrations: level of vitamin D was determined through Liebermann–Burchard method. | |
| Notes |
Source of funding: unknown/unreported. Dates of the study: not reported dates, Iran. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): the authors announce that there are no conflicts of interest between different individuals and organisations involved in the study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 140 pockets of drug and placebo were randomly (by using table of random numbers). |
| Allocation concealment (selection bias) | Unclear risk | 140 pockets of drug and placebo were randomly offered and both study staff and participants did not know about administration of the treatments. |
| Blinding of participants and personnel (performance bias) | Low risk | Both study staff and participants did not know about administration of the treatments. |
| Blinding of outcome assessment (detection bias) | Low risk | Both study staff and participants did not know about administration of the treatments. |
| Incomplete outcome data (attrition bias) | Low risk | Data reported for all participants. |
| Selective reporting (reporting bias) | Unclear risk | Although participant's level of 25‐hydroxy vitamin D was used to determine study eligibility, serum levels of vitamin D were not reported. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
| Methods | Randomised double‐blind placebo‐controlled trial. | |
| Participants | 90 pregnant women with at least 1 risk factor for gestational diabetes including BMI (BMI; kg/m2) more than 25, history of macrosomic neonate, positive family history for diabetes and gestational diabetes, history of gestational diabetes in previous pregnancies, and glycosuria. | |
| Interventions | Participants were randomised into 1 of 2 groups: group 1 (n = 46) received 5000 units of vitamin D weekly; and group 2 (n = 44) received placebo. Both groups were treated until the 26th week of pregnancy. Then the glucose challenge test (GCT) and the glucose tolerance test (GTT) were performed to evaluate GDM. Health worker cadre: not specified. | |
| Outcomes | Maternal: vitamin D levels and GCT, incidence of diabetes. Laboratory method used for assessment of vitamin D concentrations: vitamin D level was determined in a laboratory by the Liebermann–Burchard method, in which the patient should fast for 12 hours and not have a fatty dinner. | |
| Notes |
Source of funding: no funding. Dates of the study and location: 2013, Iran. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): the authors have no conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women were included and randomly divided into 2 groups using permuted block randomisation of size 2. |
| Allocation concealment (selection bias) | Low risk | Blinding was carried out in which drugs and placebos were prepared to be completely similar in appearance and taste and put in numbered pockets based on a randomisation. |
| Blinding of participants and personnel (performance bias) | Low risk | Both study staff and participants did not know about administration of the treatments. |
| Blinding of outcome assessment (detection bias) | Low risk | Both study staff and participants did not know about administration of the treatments. |
| Incomplete outcome data (attrition bias) | Low risk | Data reported for all participants. |
| Selective reporting (reporting bias) | Unclear risk | Apgar score was taken but is not in results. |
| Other bias | High risk | Intervention described in abstract does not match intervention described in methods. In abstract: participants in the intervention group took 5000 units of vitamin D daily. In methods: participants in the intervention group took 5000 units of vitamin D weekly. |
| Methods | Randomised controlled trial | |
| Participants | 100 healthy, pregnant women, primigravida with a singleton pregnancy, gestational age: 12‐16 weeks in Sawangi, Meghe, Wardha. | |
| Interventions | Participants were randomised into 2 groups: Group 1 (n = 50): received 2000 IU of vitamin D3 per day from 12‐16 weeks of gestation of pregnancy; and Group 2 (n = 50) received no supplementation and served as controls. 25‐hydroxyvitamin D [25(OH)D]in maternal blood was measured by chemiluminescence immunoassay, at recruitment and at the time of delivery and a serum 25(OH)D level lower than30 nmol/L was defined as deficiency. Health worker cadre: not specified. | |
| Outcomes | Maternal: deficiency of vitamin D, mean gestational age, preterm birth. Laboratory method used for assessment of vitamin D concentrations: Mean serum 25(OH)D levels were measured by Roche diagnostic ELECSYS (Electrochemiluminescence immunoassay) 2010 Cobase E 411 Analyser Immunoassay System Germany. | |
| Notes |
Source of funding: no funding sources reported. Dates of the study and location: October 2012 to September 2014, India. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): none declared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial reported that participants were randomly allocated to the treatment or no supplementation but methods describing this process were not reported. |
| Allocation concealment (selection bias) | Unclear risk | The trial did not report this; however, since one group did not receive any supplementation, it is assumed that the intervention was not concealed to participants. |
| Blinding of participants and personnel (performance bias) | High risk | The trial did not report this; however, it is assumed that participants were not blinded as one group did not receive any supplementation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial did not report if study staff was blinded. |
| Incomplete outcome data (attrition bias) | High risk | It is assumed that each group had 50 participants as stated in the abstract but the trial did not report final number of participants that completed the trial or the sample size in any of the tables. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The study appears to be free of other evident sources of bias. |
| Methods | Randomised controlled study with 3 arms. | |
| Participants | 990 nulliparous women attending antenatal outpatient clinics of Isfahan Health Centers (32.6333° N, 51.6500° E north of Tropic of Cancer) between April 1998 and March 2001, with singleton pregnancies, first prenatal visit before 20 weeks of gestation, systolic/diastolic blood pressure lower than 130/80 mmHg, and no proteinuria detectable by a dipstick. Women with history of cardiovascular, renal or endocrinologic problems, medical or obstetric complications and those with known hazardous condition (multifetal gestation, hydatidiform mole) were excluded. | |
| Interventions | Participants were randomly assigned to 1 of 3 groups: Group 1 (n = 330) received 75 mg aspirin each day from 20th week of gestation until delivery; Group 2 (n = 330) received a tablet containing 500 mg calcium carbonate + 200 IU vitamin D (cholecalciferol‐D3) daily from 20th week of gestation until delivery; and group 3 received no intervention (n = 330). All cases received standard prenatal care. Health worker cadre: the women were examined by trained staff every 4 weeks through the 28 weeks of gestation, and every 2 weeks through the 36th week and weekly thereafter. Blood pressure was measured by a certified examiner. | |
| Outcomes | Maternal: blood pressure, bodyweight, BMI, maternal height, urine protein measurements, maternal weight gain, duration of gestation. Infant: neonatal weight at birth, the presence of respiratory distress syndrome, sepsis, jaundice and intrauterine growth retardation, fetal or neonatal death. Laboratory method used for assessment of vitamin D concentrations: not applicable. | |
| Notes |
Source of funding: this study was funded by a research grant of the Research Deputy of Isfahan University of Medical Sciences grant (No: 76085). Dates of the study and location: April 1998 to March 2001, Iran. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): none declared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised by table of random numbers. |
| Allocation concealment (selection bias) | Unclear risk | The trial did not report the methods for allocation concealment. It is unclear whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment. It is assumed that it was not conceal as one group did not receive any treatment. |
| Blinding of participants and personnel (performance bias) | High risk | The trial did not mention if it was blinded. It is assumed that it was not blinded to participants as one group did not receive any treatment. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial did not mention if it was blinded to those conducting the assessments. |
| Incomplete outcome data (attrition bias) | Low risk | No attrition reported. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The study appears to be free of other evident sources of bias. |
| Methods | Single‐arm study, not blinded. | |
| Participants | 210 pregnant women referring to obstetric clinic of Shahid Beheshti and Alzahra hospital in Esfahan city in 2012. Inclusion criteria: patient satisfaction; normal BMI; gestational age below 16 weeks; no history of diabetes mellitus type 2 or GDM; no family history of diabetes mellitus type 1 in first degree relatives. Exclusion criteria: patient dissatisfaction; incorrect consumption of vitamin D supplementation; follow‐up discontinuation. | |
| Interventions | Participants will be individually randomised to 1 of 2 groups: Group 1 (n = 70) received vitamin D supplementation with dose of 50,000 unit every 2 weeks for 10 weeks; Group 2 received a placebo. Pregnant women with levels of above 25 nmol/L were selected as the normal healthy control group and were the ones who received placebo. Health worker cadre: not specified. | |
| Outcomes | Maternal: gestational blood sugar level, serum vitamin D level. Laboratory method used for assessment of vitamin D concentrations: not specified. | |
| Notes |
Source of funding: this study was funded by a non‐governmental organization, Sponsor: Isfahan University of Medical Sciences. Dates of the study and location: January 2013 to January 2014, Iran. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): there are no conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised by table of random numbers. |
| Allocation concealment (selection bias) | Low risk | Researcher, the distributors of the drug and the women, did not know which group was taken the vitamin D or placebo. |
| Blinding of participants and personnel (performance bias) | Low risk | Researcher, the distributors of the drug and the women, did not know which group was taken the vitamin D or placebo. |
| Blinding of outcome assessment (detection bias) | Low risk | Researcher, the distributors of the drug and the women, did not know which group was taken the vitamin D or placebo. |
| Incomplete outcome data (attrition bias) | Low risk | All data reported. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The study appears to be free of other evident sources of bias. |
| Methods | Randomised clinical trial. | |
| Participants | 169 pregnant women, both nulliparous and multiparous, aged 18 years or older, no history of mental illness and internal diseases such as hyper/hypothyroidism, no addiction to any kind of narcotic drugs or alcohol, not divorced or widowed, no pregnancy complications such as pre‐eclampsia, gestational diabetes, ruptured membranes and suspicion of preterm birth, no previous caesarean sections, with a live fetus singleton pregnancy, and gestational age of 26 to 28 weeks based on ultrasound results. who were under prenatal care in Hafez teaching hospital in Shiraz, Iran. | |
| Interventions | Participants were assigned to 2 groups through block randomisation design: Group 1 (n = 78) received 2000 IU of vitamin D3 per day; and Group 2 (n = 75) received placebo. Both groups received their assigned treatments from 26 to 28 weeks of gestation until childbirth. Maternal serum 25‐hydroxyvitamin D concentrations were measured at baseline and childbirth. Besides, depression scores were evaluated 4 times: at 26 to 28 and 38 to 40 weeks of gestation, and finally at 4 and 8 weeks after birth. Participants were allowed to use prescribed supplementation outside this study’s protocol. Usually, pregnant women in Iran are prescribed iron and folic acid, which may be consumed as part of the multivitamin supplementation with 200–400 IU of vitamin D. They reported that 55 participants in the intervention and 69 in the control used other supplements but they did not provide the composition of the supplements. Health worker cadre: at first, a research team member who was responsible for data collection visited the prenatal care clinic of the hospital daily and based on the inclusion criteria, invited the mothers to participate in the study. The consumption of pills were assessed in later prenatal care visits and over the phone. | |
| Outcomes | Maternal: baseline 25‐hydroxy vitamin D concentrations and at childbirth, depression score. Infant: vitamin D concentrations, anthropometric measurements of their infants at birth, 4th and 8th weeks of birth. Laboratory method used for assessment of vitamin D concentrations: Serum 25‐hydroxyvitamin D was measured with the Chemiluminescence immunoassay (CLIA) method. | |
| Notes |
Source of funding: the study was financially supported by a research grant from the Research Vice‐chancellor of Shiraz University of Medical Sciences. Dates of the study and location: November 2014 to October 2015, Iran. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): the authors declare that they have no competing interests. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised using a block randomisation design. |
| Allocation concealment (selection bias) | Unclear risk | The trial reported that it was a single‐blinded study, but it is not clear who was blinded and they did not report the allocation concealment. It is assumed that participants were blinded as the control group also received 2 pills, similar to the intervention group. |
| Blinding of participants and personnel (performance bias) | Unclear risk | The trial reported that it was a single‐blinded study. However, data collection related to depression was done by a trained midwife outside the research team, who was blinded to group allocations but the rest of the assessments were not clear if they were performed by a blinded staff. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial did not report if study staff conducting the assessments were blinded. |
| Incomplete outcome data (attrition bias) | Unclear risk | 143 women began study and 136 finished. Serum vit D checked for 130 women, but does not specify how many women were in each group. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The study appears to be free of other evident sources of bias. |
| Methods | Randomised controlled trial; 4 x 3 block design with randomisation at individual level. | |
| Participants | 180 pregnant women (45 Indian Asians, 45 Middle Eastern, 45 Black and 45 Caucasian) women at 27 weeks' gestation attending the routine antenatal clinic at St Mary’s Hospital, London, the UK (latitude: 51°30'N north of tropic of Cancer). Exclusion criteria: pre‐existing sarcoidosis, osteomalacia, renal dysfunction and tuberculosis. Pre‐gestational BMI and skin pigmentation (in addition to ethnicity) not reported. The study took place between April 2007 and November 2007. As well, a follow‐up trial of the infants of these trial participants. All of the offspring of the 180 mothers recruited in this trial were eligible and were invited to participate in a follow‐up study when their children were 3 years of age. | |
| Interventions | Participants were randomised in blocks of 15 within each of the 4 ethnic groups to 3 groups; Group 1 (n = 60) received a daily dose of vitamin D (ergocalciferol D2) at 800 IU; Group 2 (n = 60) received a one dose of 200,000 IU of calciferol; Group 3 (n = 60) received no treatment and served as controls. All groups received the intervention for 13 weeks, from start of supplementation to term. Data from groups 1 and 2 were collapsed for this analysis. Health worker cadre: each woman collected her tablets directly from the hospital pharmacy department or her local pharmacy. | |
| Outcomes | Maternal: maternal and cord 25‐hydroxyvitamin D levels at delivery, maternal PTH and corrected calcium levels at delivery, adverse events. Infant: small‐for‐gestational age was defined as birthweight less than the 10th percentile after adjustments for gestation at delivery, infant sex, maternal ethnicity, parity, height and weight. Wheezing episode in the first 3 years of life, measured at 36 to 48 months, use of inhaled bronchodilators in the last 12 months, doctor‐diagnosed rhinitis, any wheezing episode in the preceding 12 months, doctor‐diagnosed asthma, doctor‐diagnosed eczema, doctor‐diagnosed food allergy, positive skin prick test responses, 25‐hydroxyvitamin D levels, bronchodilator responsiveness, exhaled nitric oxide level (in parts per billion), nasal secretions for inflammatory mediators, pulmonary airflow resistance and reactance at a range of frequencies using impulse oscillometry, total number of all wheezing episodes since birth and total number of upper and lower respiratory tract infections since birth, at 36 to 48 months. Laboratory method used for assessment of vitamin D concentrations: not specified. | |
| Notes | Women who did not speak English were only included if a health advocate was able to interpret and a leaflet was provided in their language;
Source of funding: this study was funded by a research grant from the Institute of Obstetrics and Gynaecology Trust, Wolfson and Weston Research Centre for Family Health, Imperial College, Du Cane Road, Hammersmith Hospital, London W12 0NN, UK. Dates of the study and location: April 2007 to November 2007, London, UK. Declarations of interest among primary researchers (or state where this information is not reported by the trial authors): none declared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number lists were drawn up by an independent researcher, with randomisation in blocks of 15. |
| Allocation concealment (selection bias) | Low risk | The research staff allocating participants used the next available number on entry to the trial, and each woman collected her tablets directly from the hospital pharmacy department or her local pharmacy. |
| Blinding of participants and personnel (performance bias) | High risk | Study personnel and participants were not blinded to treatment assignment. |
| Blinding of outcome assessment (detection bias) | High risk | Study personnel was not blinded to treatment assignment. |
| Incomplete outcome data (attrition bias) | Low risk | Only 1 loss to follow‐up on group 3. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | Women were randomised within each ethnic group. It is not clear if the ethnicity can be clearly established as it was self reported. Women who did not speak English were included only if a health advocate was able to interpret and a leaflet was provided in their language (English, Arabic, Bengali and Farsi) although the ability to read was not clearly established. |
β‐hCG: beta human chorionic gonadotropin
BMI: body mass index
CHW: community health workers
ELISA: enzyme‐linked immunosorbent assay
GDM: gestational diabetes mellitus
GSH: glutathione
HDL: high‐density lipoprotein
IGF‐I: insulin‐like growth factor
IU: international units
IUFD: intrauterine fetal death
LBW: low birthweight
LDL: low‐density lipoprotein
mcg: microgram
PA: physical activity
PTH: parathyroid hormone
25 (OH)D: 25‐hydroxycholecalciferol
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| 49 healthy, well‐nourished mothers delivering in January 1984 in the maternity wards and outpatient clinic of the Department of Paediatrics of the University Central Hospital of Tampere, Finland (latitude 61°N) and exclusively breastfeeding their infants, were divided in succession into 3 groups: group 1 (n = 17): mothers were given 2000 IU vitamin D3 a day, infants not supplemented; group 2 (n = 16): mothers were given 1000 IU vitamin D3 a day, infants not supplemented; group 3 (n = 16): mothers were not supplemented, and their breast fed infants were given 400 IU of vitamin D2 a day. This is not a randomised trial and the intervention includes mothers at postpartum and their infants. | |
| 54 pregnant women aged 18 to 40 years diagnosed with GDM by a 100‐g oral glucose‐tolerance test at 24 to 28 weeks' gestation attending maternity clinics affiliated with Kashan University of Medical Sciences, Kashan, Islamic Republic of Iran. Participants were randomly assigned to 1 of 2 groups: group 1 (n = 27), women received capsules containing 50,000 IU vitamin D (cholecalciferol‐D3) (D‐Vitin 50000; Zahravi Pharm Co) 2 times during the study (at baseline and at day 21 of the intervention): group 2 (n = 27), women received 2 placebos (Barij Essence Co) at the same times. All pregnant women in the study had a diagnosis of gestational diabetes. The type of participant is outside the scope of this review. | |
| 56 pregnant women 18 to 40 years of age with gestational diabetes and 24 to 28 weeks' gestation attending prenatal care at maternity clinics affiliated to Kashan University of Medical Sciences, Kashan, Iran were randomly assigned to 1 of 2 groups: group 1 (n = 28) received 1000 mg calcium per day and a 50,000 U vitamin D (cholecalciferol‐D3) pearl twice during the study (at study baseline and on day 21 of the intervention); group 2 (n = 28) received 2 placebos at the same times. Participants were pregnant women with diagnosis of gestational diabetes. The type of participant is outside the scope of this review. | |
| 46 women at risk for pre‐eclampsia at 27 weeks' gestation with positive roll‐over test were randomly assigned to receive either the multi mineral‐vitamin D supplements (n = 23) or the placebo (n = 23) for 9 weeks. Study was conducted in Kashan, Iran, during November 2013 to May 2014. Multi mineral‐vitamin D supplements were containing 800 mg calcium, 200 mg magnesium, 8 mg zinc, and 400 IU vitamin D3. Fasting blood samples were taken at baseline and after 9‐week intervention to measure related factors. Newborn's outcomes were determined. This type of intervention is outside the scope of this review. | |
| 120 African American or Caucasian primigravidae women 19 to 40 years of age in their first trimester of pregnancy in Children’s Hospital & Research Center Oakland, California, USA were included in this study. Women who were smokers, had a pre‐pregnancy BMI higher than 30, had a medical condition that affected bone or taking a medication that affected bone were excluded. Participants were randomly assigned to 1 of 3 groups: group 1: 1000 mg of calcium; group 2: 2000 IU vitamin D; group 3: placebo. The intervention started at week 16 of pregnancy until delivery. The type of intervention is outside the scope of this review. | |
| 90 pregnant women,with least 1 of the risk factors for PE were randomly divided into 3 groups according to randomised selection: Group A received 1 ferrous sulphate tablet (Rooz daru©, Iran) + 1 Claci‐care multimineral‐vitamin D tablet [(VitanePharma©, Germany) contained 800 mg Ca, 200 mg Mg, 8 mg Zn and 400 IU vitamin D3)]per day; Group B received 1 ferrous sulphate tablet (Rooz daru©, Iran,) + 250 mg vitamin C and 55 mg vitamin E, and control group only received Ferrous sulphate daily. This type of intervention is outside the scope of this review. | |
| 28 pregnant women were enrolled at a maternal health clinic in inner‐city Dhaka, Bangladesh Aged 18 to 34 years; at 27 to 30 weeks of pregnancy. Participants were randomly assigned to 1 of 2 groups: group 1 (N = 14) were assigned to receive a single dose of vitamin D3 70,000 IU (1.75 mg, where 1 mg = 40,000 IU) on day 0 followed by vitamin D3 35,000 IU (0.875 mg) per week starting on day 7 and continuing until delivery); Group 2 (N = 14), were assigned to receive vitamin D3 14,000 IU (0.350 mg) per week starting on day 0 and continuing until delivery. All participants received vitamin D supplementation in different regimens. The type of intervention is outside the scope of this review. | |
| 150 consecutive pregnant women pregnant women during their second trimester from 6 villages of a poor socio‐economic region in district Barabanki (latitude 26.8 ºN), Uttar Pradesh, north India. The participants were initially randomised to receive either no dose or 1 dose of 60,000 IU cholecalciferol under observation in the 5th gestational month. This is not a randomised trial and the comparisons are outside the scope of this review. | |
| 299 pregnant women with 12 and 24 weeks of gestation of lower‐middle and middle socio‐economic groups attending the antenatal clinic in Queen Mary Hospital, Chhatrapati Sahuji Maharaj, India, were randomly assigned to 1 of 2 groups, group 1: received 1500 mcg cholecalciferol at induction into the study, or group 2 3000 mcg cholecalciferol at induction as well as at 28 weeks of gestation. All were prescribed 1 g of elemental calcium daily as calcium carbonate without vitamin D. This type of intervention is outside the scope of our review. | |
| 623 women were recruited at 24 weeks of pregnancy. Women were randomised 1:1 to a daily dose of 2400 IU vitamin D3 supplementation or matching placebo tablets (Camette A/S) from pregnancy week 24 to 1 week postpartum. In addition, all women were instructed to continue supplementation of 400 IU of vitamin D3 during pregnancy as recommended by the Danish National Board of Health; thus, the study is a dose comparison of 2800 IU/day vs 400 IU/day of vitamin D3 supplementation. Both groups received vitamin D. This type of intervention is outside the scope of our review. | |
| 230 infants and mothers giving birth in 2 maternity units of the institution, who intended to continue exclusive breast‐feeding until the first 6 months and come to the hospital of birth for immunisation, were eligible, from September 2012 and June 2014 at the King George Medical University, and Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow (latitude 26°N). After maternal blood sample was collected for serum 25(OH)D 2 to 4 days after delivery, mother–infant pairs were randomly assigned at birth to 1 of 3 treatment regimens described below, to be followed for 9 months. Intervention was postpartum. | |
| 1139 pregnant women were assigned to 1 of 2 wards: group 1 (n = 506) Caucasian pregnant women assigned to 1 ward of the Simpson Memorial Maternity Pavilion, Edinburgh, UK during the 9 months from September to May, were given a daily dietary supplement of 400 IU of vitamin D2 from about the 12th week of pregnancy until delivery; group 2 women (n = 633) were assigned to another ward over the same period and were given a placebo containing no vitamin D. This is not a randomised trial. | |
| 174 healthy postpartum women who had delivered babies at term in Poland, were randomised to 1 of 2 groups: group 1 (n = 70) received 1200 IU/day vitamin D (cholecalciferol‐D3 as 800 IU/day alone + 400 IU/day from a multiple micronutrient supplements; group 2 (n = 67) received 400 IU/day vitamin D (cholecalciferol‐D3 as placebo + 400 IU/day from multiple micronutrient supplements) during 6 months of lactation. Participants from both groups received vitamin D supplements. The participants were postpartum women. The type of participant and the type of interventions are outside the scope of this review. | |
| 200 consecutive pregnant women attending antenatal clinic of at Queen Mary Hospital in CSMMU (former KGMC) were enrolled into the study after taking informed consent and randomly allocated to 1 of 3 groups: (1) Intervention group 1 vitamin D 1,20,000IU in 3 doses each 8 weeks apart + calcium carbonate containing 500 mg elemental calcium with 250 IU vitamin D twice a day, daily throughout pregnancy; (2) Intervention group 2 vitamin D 60,000IU in 3 doses each 8 weeks apart + calcium carbonate containing 500 mg elemental calcium with 250 IU vitamin D twice a day, daily throughout pregnancy; (3) Comparator agent group 3 calcium carbonate containing 500 mg elemental calcium with 250 IU vitamin D twice a day, daily throughout pregnancy. This is a registry for an ongoing study (open to recruitment). The type of intervention is outside the scope of this review. | |
| 192 Arab women between 12–16 weeks of gestation after their last menstrual period or by ultrasound assessment who had a singleton pregnancy; and planned to receive prenatal and delivery care in primary healthcare clinics affiliated with Tawam Hospital, Al Ain, United Arab Emirates. All participants received vitamin D supplementation in different regimens. The type of intervention is outside the scope of this review. | |
| 77 mother‐child couples were divided into 3 groups, according to whether women were not receiving vitamin D (29 couples) during the last 3 months of pregnancy ending in winter or taking 1000 units of vitamin D in the form of uvesterol (21 pairs) or a single dose of 200,000 units of vitamin D at 7 months (27 pairs). This type of intervention, with no placebo group, is outside the scope of this review. | |
| 45 pregnant women with confirmed multiple sclerosis who attended an outpatient clinic in Isfahan University of Medical Sciences, Iran aged 20 to 40 years with low serum 25‐hydroxyvitamin D (25(OH)D) levels were randomly allocated to 2 groups in an open‐label randomised, controlled clinical Phase I/II pilot study. 1 group received 50,000 IU/week vitamin D3 (n = 21) or routine care (n = 22) from 12 to 16 weeks of gestation till delivery. This type of participant is outside the scope of this review. | |
| 88 women were recruited at different gestational age, the incidence of vitamin D deficiency about 66%. A single daily dose ranging from 1000 IU to 2000 IU according to the level of deficiency were given to the patient for 6 weeks. In our study 34.1% of women had a level below 10 ng/mL This type of intervention, with no placebo group, is outside the scope of this review. | |
| 160 pregnant women (24 to 26 weeks of gestation) who attended an obstetric clinic in Qazvin, Iran, from December 2011 to March 2012 were randomised, and included in 2 arms. Women in the control group received a multivitamin containing 400 IU vitamin D3 plus 200 mg elemental calcium each day until delivery. Women in the intervention group received a weekly dose of 50,000 IU oral vitamin D3 for 8 weeks (from 26 to 28 weeks of pregnancy) as well as the drug regimen (multivitamin and elemental calcium) given to the control group. Both groups received vitamin D and calcium. This type of intervention is outside the scope of our review. | |
| 200 pregnant women who attended the Department of Obstetrics & Gynaecology unit 3, Dow University and Civil Hospital Karachi, Pakistan aged between 18 and 40 years were randomised, and included in 2 arms. Participants were allocated to 1 of 2 groups: group 1 (n = 100) received along with ferrous sulphate, 4000 IU of vitamin D3; group 2 (n = 100) received routine antenatal care (ferrous sulphate and calcium). Both groups received above medications from 20 weeks of pregnancy until delivery. This type of intervention is outside the scope of our review. | |
| 876 singleton pregnant women with blood pressure lower than 140/90 mmHg at 20 weeks’ gestation, and no evidence of proteinuria, who were attending the obstetric clinic of Kumamoto University Hospital, Japan were divided into 2 groups: group 1 (n = 666) women received conventional antenatal care; group 2 (n = 210 women) were managed under a protocol for the prediction of pre‐eclampsia with an angiotensin sensitivity test and prevention of the condition by calcium supplementation. This is not a randomised trial and the type of intervention is outside the scope of this review. | |
| 60 participants with GDM were divided into 2 groups of either 1000 IU vitamin D3 and 1000 mg EPO or placebo for 6 weeks. At the beginning and end of the study, fasting blood samples were obtained from the participants to measure related variables. The type of participant is outside the scope of this review. | |
| 140 GDM patients. Participants were randomly divided into 4 groups to receive: (1) 1000 mg omega‐3 fatty acids containing 360 mg eicosapentaenoic acid and 240 mg docosahexaenoic acid (DHA) twice a day + vitamin D placebo (n = 35); (2) 50,000 IU vitamin D every 2 weeks + omega‐3 fatty acids placebo (n = 35); (3) 50,000 IU vitamin D every 2 weeks + 1000 mg omega‐3 fatty acids twice a day (n = 35), and (4) vitamin D placebo + omega‐3 fatty acids placebo (n = 35) for 6 weeks. The type of participant is outside the scope of this review. | |
| 243 pregnant patients attending the antenatal clinic, between 18 to 40 years old and with gestational age between 12 to 16 weeks were randomised into 4 groups in a ratio of 1:1:1:1. Group 1 active control group received 600 units of vitamin D per day, group 2: 1000 units/day, group 3: 2000 units/day and group 4: 4000 units per day. This type of intervention is outside the scope of our review. | |
| 60 women in Arak, Iran, with GDM were divided into 2 groups to receive Ca + vitamin D supplements or placebo. Individuals in the Ca + vitamin D group (n 30) received 1000 mg Ca/day and 2 pearls containing 1250 μg (50 000 IU) of cholecalciferol (vitamin D3) during the intervention (one at study baseline and another at day 21 of the intervention); those in the placebo group (n 30) received 2 placebos of vitamin D at the mentioned times and placebos of Ca every day for 6 weeks. The type of participant is outside the scope of this review. | |
| 60 pregnant women Arak, Iran at risk for pre‐eclampsia according to abnormal uterine artery Doppler waveform were randomly divided into 2 groups to receive 50,000 IU vitamin D supplements (n = 30) or receive placebo (n = 30) every 2 weeks from 20 to 32 weeks of gestation. All pregnant women were also taking 400 μg/day folic acid from the start of pregnancy, 60 mg/day ferrous sulphate from the second trimester, and a multivitamin mineral capsule (containing 400 IU vitamin D) from the second half of pregnancy. The type of participant is outside the scope of this review. | |
| 111 couples were recruited for a 6‐week intervention prior to oocyte retrieval consisted of a daily drink, containing 2 g of DHA plus EPA and 10 mcg of vitamin D, and olive oil and olive oil spreads, all in unmarked containers. The control group received a placebo drink and sun flower oil and spreads, again in unmarked containers. 55 couples were randomised to the treatment group and 56 to placebo. Following IVF, embryos were cultured in an Embryoscope and validated morphokinetic markers of embryo quality were recorded; day 3 and 5 KIDScores (Known Implantation Data Score) were calculated for individual embryos. This type of intervention is outside the scope of our review. | |
| 144 pregnant women aged older than 18 years of age, with no more than 18 weeks' gestation, in good general health, with low‐risk pregnancy and not consuming > 10 mcg/day vitamin D from supplements were randomised in a 3‐arm, parallel, double‐blind, placebo‐controlled dose‐response intervention study with vitamin D. Group 1 received 10 mcg (400 IU) vitamin D3 once daily taken from baseline visit (approximately 15 weeks' gestation) until endpoint (delivery). Group 2 received 20 mcg (800 IU) vitamin D3 once daily from baseline visit (approximately 15 weeks' gestation) until endpoint (delivery). Group 3 (placebo) received a placebo capsule containing 0 mcg (0 IU) of vitamin D3 taken from baseline visit (approximately 15 weeks' gestation) until endpoint (delivery). The primary outcome was serum 25‐hydroxyvitamin D in pregnant women and cord blood. Women were permitted to continue with self‐administration of antenatal supplements containing ≤ 10 μg vitamin D per day. This type of intervention is outside the scope of our review. | |
| Participants were randomly assigned to 1 of 2 groups: group 1: vitamin D capsule 50,000 U weekly for 8 weeks from 28 gestational age and multivitamin tablet include 400 IU vitamin D daily till termination; group 2: multivitamin tab include 400 IU vitamin D daily till termination. This type of intervention is outside the scope of our review. | |
| 103 pregnant GDM women were eligible to participate, using a permuted block randomisation method stratified according to their baseline 1‐hour OGTT results, all participants in their second trimester were randomly assigned to consume 2 servings (100 g per serving) of either plain yogurt (PY) drink (‘PY’ without any vitamin D3 supplement, from Mengniu Dairy, Hohhot, China) or VDY drink (‘PY’ supplemented with 500 IU vitamin D3, from Mengniu Dairy, Hohhot, China), with 1 serving at breakfast and the other 1 at dinner, on a daily basis for a period of 16 weeks. The type of participant is outside the scope of this review. | |
| This trial was registered in 1986 on the Oxford Database of Perinatal Trials and reports the recruitment and follow‐up completed in 1979. The registration form reports a randomised controlled trial to assess the efficacy of calcium and vitamin D supplementation versus placebo in the prevention of maternal and fetal hypocalcaemia. The reports indicates that the sample size was 55 Asian women with morbidity and laboratory results as primary outcomes but no further information is available. | |
| 226 healthy pregnant women from Greater Vancouver, British Columbia, Canada, from 13 to 24 weeks of gestation were randomly allocated to 10, 25, or 50 mg vitamin D/d from 13 to 24 weeks of gestation until 8 weeks postpartum, with no infant supplementation. Mother and infant blood was collected at 8 weeks postpartum (n = 76, n = 76, and n = 74, respectively). The overall study retention rate from beginning to end was 76% (n = 172). This type of intervention, with no placebo group, is outside the scope of this review. | |
| 45 Hindu pregnant women were randomly assigned to 1 of 2 groups: group 1 (n = 25) received tablets containing 1200 IU vitamin D and 375 mg calcium daily throughout the 3rd trimester; group 2 (n = 20) received oral single dose of 600,000 IU vitamin D2 once during 7th month and 8th month (total 2 doses). This group was compared with group 3 (n = 75) who had not received vitamin D supplements during pregnancy. The results were also compared with data from 25 non pregnant, non‐lactating healthy women. The randomised study compares 2 doses of vitamin D supplementation. The type of study, type of participants and types of interventions are outside the scope of this review. | |
| Pregnant women, aged 18 years or more, with less than 20 weeks’ gestation at recruitment. Participants will be randomly assigned to 1 of 2 groups: group 1: received high‐dose vitamin D supplementation (5000 IU/day); group 2: standard dose pregnancy vitamin supplementation (400 IU vitamin D daily), administered as an oral capsule, from the time of the first antenatal clinic visit (around 12 weeks’ gestation) until delivery. This type of intervention is outside the scope of this review. | |
| 500 women with gestational age 12 to 16 weeks and serum 25 hydroxy vitamin D (25 (OH) D ) less than 30 ng/mL randomly categorized in 2 groups: group A received 400 IU vitamin D daily and group B 50,000 IU vitamin D every 2 weeks orally until delivery. Maternal and neonatal outcomes were assessed in 2 groups. This intervention had no placebo group. | |
| Women between 20 to 45 years old with gestational diabetes at their recent pregnancy, from the list of GDM Diabetes Research Center of Yazd University, and without thyroid disease, kidney disease, bone disease, PCO, liver disease and not using anti‐epilepsy drugs, glucocorticoids, and statins. Exclusion criteria: risk of any illness that requires medication and lack of any willingness to co‐operate, were randomly assigned to 1 of 2 groups: group 1: intramuscular injection of vitamin D with 300,000 IU dose; group 2: control: not receive any intervention. The type of participant is outside the scope of this review. | |
| 91 pregnant women aged 16 to 42 years were admitted to Kocaeli Maternity and Children Hospital between April 2011 and April 2012. The participants were randomly divided into 3 groups: 600 IU/d (control group; n = 31); 1,200 IU/d (n = 31), and 2,000 IU/d (n = 32) of vitamin D. All groups received vitamin D supplements. This type of comparison is outside the scope of our review. | |
| 315 pregnant women aged 15 to 45 years with less than 16 weeks of gestation in a hospital in Pakistan. Pregnant women with pre‐existing type 1 or type II diabetes, pre‐existing hypertension, multiple fetuses,babies (twins, triplets) or with a diagnosis of pregnancy with a fetal anomaly in scan will be excluded. Participants were randomly assigned to 1 of 3 groups: groups 1 received a dose of 400 IU/day till the time of delivery; group 2 received 2000 IU/day till the time of delivery; group 3 received 4000 IU/day till the time of delivery. This type of intervention is outside the scope of this review. | |
| 76 Thai lactating mothers and their breast‐fed infants were studied with maternal 25 hydroxyvitamin D 25 (OH) D levels of 10‐30 ng/mL determined using Liquid Chromatography Mass Spectrometry Tandem (LC‐MS/MS). 1 group received vitamin D3 1800 IU/day supplementation for 6 weeks, and members of the other group were given a placebo. 25 (OH) D level of colostrum and 6‐week serum from breast‐fed milk were measured by High Performance Liquid Chromatography (HPLC). The data from the 2 groups were analysed and compared. The type of participant is outside the scope of this review. | |
| 20 women with 25 (OH) D < 20 ng/mL & Hb = 8‐10 g/dL were randomised into groups using a computerised program (8 patients in iron alone group and 12 pregnant mothers in iron + vitamin D group). Recruited pregnant mothers received group iron + vitamin D: tablets containing fixed dose combination of vitamin D (1000 IU) + ferrous ascorbate (100 mg of elemental iron) + folic acid (1 mg) + vit B12 (7.5 mcg) (1 tablet/day) for 12 weeks. Group iron alone: tablets containing fixed dose combination of ferrous ascorbate (100 mg of elemental iron) + folic acid (1.1 mg) (1 tablet/day) for 12 weeks. This type of intervention is outside the scope of this review. | |
| 60 pregnant women at risk for pre‐eclampsia, experiencing their first pregnancy, aged between 20 and 32 years, between 18 and 20 weeks' gestation, and pregnant with a single fetus were eligible. Each pregnant woman selected for the study showed the following abnormalities on uterine artery Doppler, qualifying them as high‐risk: average resistance index (RI) > 0.67, pulsatility index (PI) > 1.65, and incisura at early diastole phase. Pregnant women were randomised into 2 groups to take either cholecalciferol supplements (n = 30) or placebo (n = 30). This study was retracted due to having data very similar to another paper. | |
| 120 women with GDM were randomly divided into 4 groups to receive: 1) 1000 mg omega‐3 fatty acids containing 180 mg eicosapentaenoicacid (EPA) and 120 mg docosahexaenoic acid (DHA) twice a day + vitamin D placebo (n = 30); 2) 50,000 IU vitamin D every 2 weeks + omega‐3 fatty acids placebo (n = 30); 3) 50,000 IU vitamin D every 2 weeks + 1000 mg omega‐3 fatty acids twice a day (n = 30) and 4) vitamin D placebo + omega‐3 fatty acids placebo (n = 30) for 6 weeks. The type of participant is outside the scope of this review. | |
| 1600 and 900 first trimester pregnant women, aged 18 to 40 years, with gestational age < 14 weeks, with singleton pregnancy in Masjed‐Soleiman, Khuzestan province,Iran were randomised by levels of vitamin D in serum to: Moderate deficiency
Severe deficiency
Pregnant women with normal vitamin D status were the controls. All women were allowed to consumed multivitamins containing no more than 400 IU per day of vitamin D3. This type of intervention is outside the scope of this review. | |
| 51 healthy pregnant women from the beginning of their second trimester of pregnancy during the autumn and winter of 2009 in recruited from 2 primary care clinics in Yazd (31°53’50”N/54°22’04”E), Iran. Participants were distributed in 3 groups according to their serum 25(OH)D at the beginning of the second trimester of pregnancy. Participants with low concentrations (25(OH)D levels < 20 ng/mL) (n = 17) were treated with 200,000 IU (50,000 IU/week for 4 weeks) of vitamin D (as (cholecalciferol‐D3), followed by supplementation with 50,000 IU/month vitamin D (cholecalciferol‐D3). The other 34 participants were randomly assigned to 1 of 2 groups: group 1 received 50,000 IU/month vitamin D (cholecalciferol‐D3); group 2 received 100,000 IU/month vitamin D (50,000 IU every 2 weeks) of vitamin D (cholecalciferol‐D3) supplementation. All participants received vitamin D supplements. The type of study design and the type of intervention are outside the scope of this review. | |
| 602 women with singleton pregnancy who were diagnosed of pre‐eclampsia in Cangzhou Central Hospital participated in the present trial and were divided into 2 groups using stratified permuted‐block randomisation method with diastolic blood pressure as a factor: (1) nifedipine + VD group (n = 298), given 1 capsule containing nifedipine (10 mg per capsule) and VD (200 IU per capsule) every 15 min orally, up to 4 doses, until blood pressure was equal to or below 150/100 mmHg; (2) nifedipine + placebo group (n = 304), given 1 capsule containing nifedipine (10 mg per capsule) plus glucose (20 mg per capsule) as placebo every 15 minutes orally, up to 4 doses, until blood pressure was equal to or below 150/100 mmHg. The type of participant is outside the scope of this review. | |
| Women with gestational diabetes, defined by the WHO criteria: fasting glucose ≥ 7.0 mmol/L or; oral glucose tolerance test: 75 g glucose, 2‐hour glucose ≥ 7.8 mmol/L recognised during pregnancy with a written informed consent, aged between 18 to 42 years. Participants will be randomly assigned to 1 of 2 groups: group 1: cholecalciferol 15,000 IU once a week during pregnancy; group 2: placebo. Per communication with the author, this study was not completed due to low recruitment. | |
| 120 women with gestational age less than 12 weeks without gestational diabetes, history of PCO, BMI less than 30 kg/m2 before pregnancy, no vitamin D supplementation in the past 6 months were randomised into 2 groups: supplementation with 50,000 IU of vitamin D monthly (2000 IU daily) or 50,000 IU every 2 weeks (4000 IU daily). Maternal and neonatal outcomes were assessed in 2 groups. This intervention had no placebo group. | |
| Pregnant women less than 20 weeks' gestation and over 18 years of age with no use of medications known to affect vitamin D metabolism, diagnosis of type 1 diabetes, history of thyroid, renal, or liver disease, problems with digestion or absorption participated in the study at USDA Western Human Nutrition Research Center and clinicians at UC Davis Medical Center. They were distributed into 2 groups, receiving: either 400 IU or 2000 IU of vitamin D per day for the duration of their pregnancy. Both groups received vitamin D supplements. This type of intervention is outside the scope of our review. | |
| 2300 HIV‐infected pregnant women receiving triple‐drug ART under Option B+ in Dar es Salaam Tanzania. HIV‐infected pregnant women of 12 to 27 weeks' gestation were randomised to either: 1) 3000 IU vitamin D3 taken daily from randomisation in pregnancy until trial discharge at 12 months postpartum; or 2) a matching placebo regimen. Maternal participants are followed‐up at monthly clinic visits during pregnancy, at delivery, and then with their children at monthly postpartum clinic visits. The type of participant is outside the scope of this review. | |
| 229 women 18 to 35 years old, who were confirmed to be vitamin D deficient (vitamin D < 75 nmol/L), were randomised into the intervention, and control groups and after 15 weeks consumption of the supplement (2000 IU/day oral vitamin D) and placebo. The study was conducted among reproductive women in a high‐risk population for vitamin D deficiency. The participants of the study were not pregnant women. The type of participant is outside the scope of this review. | |
| 16 pregnant women at 24 to 28 weeks' gestation were enrolled. The control group (N = 8) received a prenatal vitamin containing 400 IU vitamin D daily, plus a placebo capsule. The experimental group (N = 8) received the same prenatal vitamin with an additional capsule containing 3400 IU vitamin D, for a total of 3800 IU daily. This study had no placebo group, therefore, this type of intervention is outside the scope of this review. | |
| 96 women with GDM at weeks 12 to 32 of gestation, age > 16 years, singleton pregnancy were randomly assigned to either the intervention (n = 48) or control group (n = 48). Patients were referred from primary health centres affiliated with Zanjan University of Medical Sciences, as well as private obstetric clinics throughout the city. The type of participant is outside the scope of this review. | |
| 235 South Asian women, aged 23 to 68 years, living in Auckland, New Zealand were recruited for the study and those who were insulin resistant ‐ homeostasis model assessment 1 (HOMA1) > 1.93 and had serum 25‐hydroxyvitamin D concentration < 50 nmol/L were randomly assigned to 1 of 2 groups: group 1 (n = 42) received 100 μg (4000 IU) vitamin D(3); group 2 (n = 39) received a placebo daily for 6 months. The study participants were non‐pregnant women. The type of participant is outside the scope of this review. | |
| 494 apparently healthy pregnant women (16 to 45 years of age) with 12 to 16 weeks' gestation of singletons attending prenatal care in Medical University of South Carolina, Charleston, United States were randomised into 1 of 3 groups stratified by race: group 1 received 400 IU vitamin D (cholecalciferol‐D3)/day; group 2 received 2000 IU vitamin D (cholecalciferol‐D3)/day; and group 3 received 4000 IU vitamin D (cholecalciferol‐D3)/day until delivery. All women received daily multiple micronutrients supplements. All women received vitamin D supplementation at different doses. The type of intervention is outside the scope of this review. | |
| This is an analysis of data from 2 randomised controlled trials by the same research group (Wagner 2006a; Wagner 2010a). In Wagner 2006a, women were randomised to 400, 2000, or 4000 IU vitamin D (cholecalciferol‐D3)/day, stratified by race. In Wagner 2010a, participants were randomised to 2000 or 4000 IU vitamin D (cholecalciferol‐D3)/day. | |
| 258 women, exclusively breastfeeding (n = 201) and formula‐feeding (n = 57) women participating in a prospective, randomised controlled trial of vitamin D supplementation were compared at baseline 1 month postpartum (V1), at 4 months (V4), and 7 months postpartum (V7) on the basis of vitamin D status (measured by total circulating 25(OH)D concentration) and BMI. The type of intervention is outside the scope of this review. | |
| 881 pregnant women with either a personal history of asthma or allergies or a similar history in the spouse or partner, between 18 and 40 years of age and at an estimated gestational age between 10 and 18 weeks, were recruited at a scheduled obstetrical prenatal visit at 3 clinical centres: Boston Medical Center (Boston, MA), Washington University at Saint Louis (St. Louis, MO), and Kaiser Permanente Southern California Region (San Diego, CA). Participants were randomised to either vitamin D (cholecalciferol, 4000 IU/day; equivalent to 100 μg/day) or placebo. All pregnant mother participants received prenatal vitamins containing 400 IU (10 μg/day) of cholecalciferol; thus, the vitamin D arm received a total of 4400 IU/day (110 μg/day) and the placebo arm received 400 IU/day (10 μg/day). Both groups received vitamin D supplements. This type of intervention is outside the scope of our review. | |
| 179 pregnant women 18 years of age or older, with singleton pregnancy, with plasma 25‐hydroxivitamin D (25OHD) concentrations lower than 32 ng/mL, less than 20 weeks of gestation were randomly assigned to 1 of 2 groups: group 1 (n = 89) received 5000 IU/d of vitamin D (cholecalciferol‐D3) until delivery; group 2 (n = 90) received 400 IU/d of vitamin D (cholecalciferol‐D3) until delivery. Outcomes included glycaemia and glucose tolerance, gestational diabetes at 26‐28 weeks of gestation; neonatal 25OHD, maternal hypertension, mode of delivery, prematurity, birthweight, crown‐heel length, occipitofrontal head circumference. All participants received vitamin D supplements at different doses. The type of intervention is outside the scope of this review. | |
| 76 pregnant women without a prior diagnosis of glucose intolerance in the first trimester were asked to participate in a 75‐g OGTT at 24‐28 weeks of gestation. Diagnosis of GDM was based on the International Association of Diabetes and Pregnancy Study Groups criteria. Patients were recruited from Al‐Zahra Hospital, the academic outpatient centre of the Tabriz University of Medical Sciences, Tabriz, Iran. Participants in the vitamin D group received oral capsules containing 50,000 IU vitamin D 3 (D‐Vitin50000; Zahravi Pharm Co., Iran), once every 2 weeks for 2 months, for a total of 4 capsules. Those in the placebo group received placebos composed of paraffin oil (Dana Pharm Co., Iran) using the same schedule, for a total of 4 placebos. The type of participant is outside the scope of this review. | |
| 133 pregnant women with GDM during weeks 24 to 28 of pregnancy. The patients were randomly divided into 4 groups. The control group (n = 20) received a placebo (sucrose; 1 granule/day), the low‐dosage group (n = 38) received the daily recommended intake of 200 IU vitamin D (calciferol) daily, the medium‐dosage group (n = 38) received 50,000 IU monthly (2000 IU daily for 25 days) and the high‐dosage group (n = 37) received 50,000 IU every 2 weeks (4000 IU daily for 12.5 days). The general characteristics and dietary intakes of the patients with GDM were similar between each group. High‐dose vitamin D supplementation (50,000 IU every 2 weeks) significantly improved insulin resistance in pregnant women with GDM. The type of participant is outside the scope of this review. |
BMI: body mass index
Ca: calcium
DHA: docosahexaenoic
DRI: dietary references intakes
EPA: eicosapentaenoic acid
FPG: fasting plasma glucose
GDM: gestational diabetes mellitus
Hb: haemoglobin
IU: international units
IVF: in vitro fertilisation
mcg: microgram
OGTT: oral glucose tolerance test
PCO: polycystic ovary syndrome
PTH: parathyroid hormone
25OHD: 25‐hydroxycholecalciferol
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Randomised, double‐blind, placebo‐controlled study. |
| Participants | 67 pregnant women with vitamin D (25(OH)D) level lower than 25 ng/mL, English or Spanish literacy, age 18 years and gestational age less than 20 weeks. |
| Interventions | Women were randomised to: group 1 (n = 36) received 50,000 IU vitamin D3 or group 2 (n = 31) received placebo, once a week for 8 weeks in addition to a prenatal vitamin with 400 IU vitamin D3. |
| Outcomes | After 8 weeks of treatment, VD levels were 48.1 19.6 ng/mL and 21.1 5.9 ng/mL (P <.0001) with 84.4% and 3.9% achieving VD sufficiency (> 30 ng/mL) in the TG and PG, respectively (P <.0001). At delivery, VD levels were 28.8 9.8 ng/mL and 20.58.9 ng/mL in the TG and PG, respectively (P < 0.0027). |
| Notes | Mount Sinai, West Hospital, New York, NY, USA |
| Methods | Randomised controlled trial |
| Participants | 150 pregnant women in 2nd trimester from 6 villages of North India |
| Interventions | All women were educated regarding sunshine exposure & were given 1 g calcium carbonate daily. They were randomised to 3 groups no vitamin D, 60,000 IU vitamin D and 2,40,000 IU vitamin D supplementation. |
| Outcomes | Maternal: serum 25 OH D levels at baseline and post delivery |
| Notes | This is an abstract. No information on registry or funding source. |
IU: international units
PG: placebo group
TG: treatment group
VD: vitamin D
25OHD: 25‐hydroxycholecalciferol
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Southampton PRegnancy Intervention for the Next Generation (SPRING): protocol for a randomised controlled trial |
| Methods | Randomised controlled trial that uses a 2‐by‐2 factorial design |
| Participants | 600 women, with less than 17 weeks' gestation at recruitment based on LMP, aged over 18 years, with a singleton pregnancy and aiming to give birth at local maternity (Princess Anne) hospital |
| Interventions | Healthy conversation skills support plus vitamin D supplementation (1000 IU cholecalciferol) (n = 150); healthy conversation skills support plus placebo (n = 150); usual care plus vitamin D supplementation (n = 150); usual care plus placebo (n = 150) |
| Outcomes | This trial is evaluating 2 approaches to improving maternal diet: a behaviour change intervention and vitamin D supplementation. The factorial design of this trial has the advantage of enabling each intervention be tested separately as well as allowing exploration of the synergistic effect of both interventions on women’s diets and vitamin D levels. |
| Starting date | Registered on 13 September 2013 |
| Contact information | Janis Baird: MRC Lifecourse Epidemiology Unit, University of Southampton,Southampton SO16 6YD, UK. [email protected] |
| Notes | Sponsor: Medical Research Council,NIHR Southampton Nutrition Biomedical Research Centre and Danone Nutricia Early Life Nutrition. |
| Trial name or title | DALI: vitamin D and lifestyle intervention for gestational diabetes mellitus (GDM) prevention. |
| Methods | Randomised controlled trial with a factorial design. |
| Participants | Pregnant women with gestational age at recruitment < 12 weeks, and more than 18 years of age. Inclusion criteria: pre‐pregnancy BMI (self‐reported weight, measured height) is >= 29 kg/m2), sufficiently fluent in major language of the country of recruitment, being able to be moderately physically active, giving written informed consent, agree to give birth in 1 of the participating hospitals. Exclusion criteria: pre‐existing diabetes, diagnosed with (gestational) diabetes mellitus before randomisation, defined as fasting glucose ≥ 5.1 mmol/L and/or 1‐hour glucose ≥ 10 mmol/L and/or 2‐hour glucose ≥ 8.5 mmol/L at baseline, not able to walk at least 100 metres safely, requirement for complex diets, advanced chronic conditions (e.g. valvular heart disease), significant psychiatric disease, unable to speak major language of the country of recruitment fluently, known abnormal calcium metabolism (hypo/hyperparathyroidism, nephrolithiasis, hypercalciuria) or hypercalciuria detected at screening (0.6 mmol/mmol creatinine in spot morning urine) and twin pregnancy. |
| Interventions | The design is that of 2 trials with a factorial design: PA, diet, PA & diet, control, vitamin D, PA & diet and placebo, vitamin D & PA & diet, placebo; to compare the impact of increased PA, enhanced nutrition and vitamin D supplementation either alone or in combination on maternal glucose tolerance, maternal weight gain and insulin sensitivity. The doses of vitamin D that will be tested in the dosing study are 500, 1000 and 1500 IU/day. One of these doses will be used in the trial. |
| Outcomes | Maternal: weight gain during pregnancy, fasting plasma glucose, HbA1c, fasting C peptide, leptin, triglycerides, free fatty acids, high density lipoprotein cholesterol (HDL‐C) and low density lipoprotein cholesterol (LDL‐C), adiponectin 2. 3 beta‐hydroxybutyrate, blood pressure, C‐reactive protein. Infant: neonatal growth, adiposity, adipo‐insular axis, glucose‐insulin axis, electrolyte concentrations, clinical outcomes and hypoxia exposure at birth, biparietal diameter, head circumference, abdominal circumference, femur length and determinants of fetal body composition variables (lean body mass and fat body mass, C‐peptide, glucose, leptin, triglycerides, 3‐ beta‐hydroxybutyric acid, pH and erythropoietin, jaundice, hypocalcaemia, hypomagnesaemia. |
| Starting date | 21/11/2011. |
| Contact information | Dr David Simmons Addenbrooke's Treatment Centre UK |
| Notes | Sponsor: European Union (EU) (Belgium) ‐ Seventh Framework Programme (FP7). |
| Trial name or title | A randomised double‐blinded interventional trial to determine the effect of 50,000 IU vitamin D supplementation monthly or twice monthly from 20 weeks' gestation. |
| Methods | Randomised double‐masked clinical trial with randomisation at the individual level. Method of sequence generation: serial tossing of a coin. Allocation will be not concealed. |
| Participants | Pregnant women seeking maternity care with midwifery services involved in the study. Exclusion criteria: antenatal vitamin D level is > 75 nmol/L when enrolling in study. |
| Interventions | Participants will be assigned to 1 of 2 groups: group 1: will receive 50,000 IU tablets twice monthly, 2 weeks apart; group 2: will receive 50,000 IU monthly and a placebo monthly, 2 weeks apart from 20 weeks' gestation until delivery of baby. The placebo tablet contains lactose monohydrate, acacia, calcium carbonate, castor oil, maize starch, povidone, sucrose, purified talc, hydrated silica, powdered cellulose, magnesium stearate, shellac, gelatin, beeswax white, titanium dioxide and prepared theobroma. |
| Outcomes | Infant: vitamin D levels taken from the cord blood samples at delivery. If emergencies at delivery prevent a cord blood sample being taken then a maternal venous blood sample will be taken for analysis. |
| Starting date | Status: not yet recruiting participants. |
| Contact information | Dr Annie Judkins Newtown Union Health Service Email: [email protected] |
| Notes | Sponsors: Royal New Zealand College of GP's, New Zealand and Wellington Medical Research Foundation, New Zealand. ACTR Number: ACTRN12610001044011. |
| Trial name or title | Vitamin D supplementation for prevention of placenta mediated pregnancy complications. |
| Methods | Randomised, controlled trial. |
| Participants | Pregnant women > 18 years of age, from 3 maternal healthcare units who agree to participate in the study. Exclusion criteria: < 18 years of age, hyperparathyroidism and sarcoidosis. |
| Interventions | Participants will be randomly assigned to 1 of 2 groups: group 1: will receive vitamin D, oral drops; group 2: will receive placebo. |
| Outcomes | Maternal: pre‐eclampsia, blood loss at delivery. Infant: blood flow in umbilical artery, growth restriction, and prematurity. |
| Starting date | 06/04/2011. |
| Contact information | N/A |
| Notes | Sponsor: Karolinska University Hospital. EudraCT Number: 2010‐019483‐37. |
| Trial name or title | Compare the effect of vitamin D and calcium plus vitamin D on pregnancy outcomes in pregnant women |
| Methods | Randomised single‐blind controlled clinical trial |
| Participants | 460 pregnant women between 20 to 40 ages, with gestational age less than 10 weeks of gestation; with no history of diabetes; HTN; a history of PCO syndrome; lack of family history of diabetes in first‐degree relatives; no family history of high blood pressure in first‐degree relatives; tend the sick; the vitamin D < 30 ng/L in women 10 to 16 weeks of pregnancy; BMI between 19 to 26; lack of vitamin D during the last 6 months; singleton pregnancy; gestational first to third who referred to women clinic of Shariati Hospital of Bandarabas, Iran from 2015‐2016 |
| Interventions | In intervention group is used vitamin D3 1000 unit oral daily since 16 weeks until the end of pregnancy. They also prescribed as routine prenatal care multivitamin that has 400 units vitamin D‐ca since 16 weeks of pregnancy. The control group is used multivitamin that has 400 unit vitamin D daily until the end of pregnancy |
| Outcomes | Vitamin D concentration in the serum, diabetes, pre‐eclampsia, preterm delivery |
| Starting date | Registration date: 2016‐12‐26, 1395/10/06 |
| Contact information | Najmehsadat Mosalanejad, email: [email protected] |
| Notes | Sponsor: Hormozgan University of Medical Sciences |
| Trial name or title | Effects of vitamin D supplement before and during and after pregnancy on complications, birthweight and bone mineral density during lactation. |
| Methods | Double‐blind, randomised, placebo‐controlled trial. |
| Participants | 400 apparently healthy women 30 to 35 years of age, all with concentrations of P‐25‐hydroxyvitamin D‐ lower than 50 nmol/L. All women included attempts to get pregnant. Visits take place at Clinic of Osteoporosis, Department of Endocrinology, at Aarhus University Hospital, Aarhus, Denmark. Women with infertility, an intake of 400 IU or more vitamin D/day, cancer, history of alcohol or drug abuse, calcium metabolic disturbances or spontaneous abortion within last 6 months will be excluded. |
| Interventions | Participants will be randomly assigned to 1 of 3 groups: group 1: will receive 35 mcg per day cholecalciferol; group 2: will receive 70 mcg per day cholecalciferol; group 3: will receive placebo. All women will receive 2 tablets daily from baseline until 16 weeks after delivery. Intervention with cholecalciferol or placebo starts before pregnancy is achieved and continues until 4 months after the women has given birth. |
| Outcomes | Primary: Infant: birthweight. Maternal: none. Secondary: Infant: weight, crown‐heel length and head circumference, and infections within 16 weeks after birth. Concentration of 25‐hydroxyvitamin D in umbilical cord and venous sample 16 weeks after birth. Maternal: postpartum effects of vitamin D supplement on maternal bone mineral density, concentration of 25‐hydroxyvitamin D in mothers milk, incidence of pre‐eclampsia and abortions. |
| Starting date | Date of start: 12/2009. Status: recruiting participants. Estimated study completion date: December 2011. |
| Contact information | Gitte Bloch Rasmussen, MD Department of Endocrinology, Aarhus University Hospital University of Aarhus Tel: +45 89 4976 81 Email: [email protected] |
| Notes | Sponsor: University of Aarhus, Denmark. |
BMI: body mass index
DRI: dietary references intakes
GDM: gestational diabetes mellitus
HTN: hypertension
IU: international units
LMP: last menstrual period
mcg: microgram
PA: physical activity
PCO: polycystic ovary
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pre‐eclampsia (ALL) Show forest plot | 4 | 499 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.30, 0.79] |
| Analysis 1.1  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 1 Pre‐eclampsia (ALL). | ||||
| 2 Gestational diabetes (ALL) Show forest plot | 4 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.97] |
| Analysis 1.2  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 2 Gestational diabetes (ALL). | ||||
| 3 Maternal adverse events Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.3  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 3 Maternal adverse events. | ||||
| 3.1 Severe postpartum haemorrhage | 1 | 1134 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.51, 0.91] |
| 3.2 Nephritic syndrome | 1 | 135 | Risk Ratio (M‐H, Random, 95% CI) | 0.17 [0.01, 4.06] |
| 3.3 Hypercalcaemia | 1 | 1134 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Preterm birth (less than 37 weeks' gestation) (ALL) Show forest plot | 7 | 1640 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.34, 1.30] |
| Analysis 1.4  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 4 Preterm birth (less than 37 weeks' gestation) (ALL). | ||||
| 5 Low birthweight (less than 2500 g) (ALL) Show forest plot | 5 | 697 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.35, 0.87] |
| Analysis 1.5  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 5 Low birthweight (less than 2500 g) (ALL). | ||||
| 6 Pre‐eclampsia (by start of supplementation) Show forest plot | 4 | 499 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.30, 0.79] |
| Analysis 1.6  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 6 Pre‐eclampsia (by start of supplementation). | ||||
| 6.1 Less than 20 weeks of pregnancy | 1 | 138 | Risk Ratio (M‐H, Random, 95% CI) | 0.29 [0.06, 1.37] |
| 6.2 20 weeks of pregnancy or more | 2 | 219 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.21, 1.24] |
| 6.3 Unknown/unreported/mixed | 1 | 142 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.98] |
| 7 Pre‐eclampsia (by pre‐gestational BMI) Show forest plot | 4 | 499 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.30, 0.79] |
| Analysis 1.7  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 7 Pre‐eclampsia (by pre‐gestational BMI). | ||||
| 7.1 Underweight (lower than 18.5) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Normal weight (18.5 to 24.9) | 1 | 165 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.21, 1.33] |
| 7.3 Overweight (25 or higher) | 1 | 54 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.84] |
| 7.4 Unknown/unreported/mixed | 2 | 280 | Risk Ratio (M‐H, Random, 95% CI) | 0.47 [0.26, 0.86] |
| 8 Pre‐eclampsia (by supplementation scheme/regimen) Show forest plot | 4 | 499 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.30, 0.79] |
| Analysis 1.8  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 8 Pre‐eclampsia (by supplementation scheme/regimen). | ||||
| 8.1 Single dose | 1 | 165 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.21, 1.33] |
| 8.2 Daily | 2 | 192 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.08, 1.20] |
| 8.3 Weekly/monthly | 1 | 142 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.98] |
| 9 Pre‐eclampsia (by skin pigmentation based on Fitzpatrick skin tone chart) Show forest plot | 4 | 499 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.30, 0.79] |
| Analysis 1.9  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 9 Pre‐eclampsia (by skin pigmentation based on Fitzpatrick skin tone chart). | ||||
| 9.1 Three or less | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 Four or more | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.3 Unknown/unreported/mixed | 4 | 499 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.30, 0.79] |
| 10 Pre‐eclampsia (by latitude) Show forest plot | 4 | 499 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.30, 0.79] |
| Analysis 1.10  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 10 Pre‐eclampsia (by latitude). | ||||
| 10.1 Between Tropics of Cancer and Capricorn | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10.2 North of the Tropic of Cancer or South of the Tropic of Capricorn | 4 | 499 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.30, 0.79] |
| 10.3 Unknown/unreported | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Pre‐eclampsia (by season at the start of pregnancy) Show forest plot | 4 | 499 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.30, 0.79] |
| Analysis 1.11  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 11 Pre‐eclampsia (by season at the start of pregnancy). | ||||
| 11.1 Summer | 1 | 54 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.84] |
| 11.2 Fall | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.3 Winter | 1 | 138 | Risk Ratio (M‐H, Random, 95% CI) | 0.29 [0.06, 1.37] |
| 11.4 Mixed/unknown | 2 | 307 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.31, 0.88] |
| 12 Gestational diabetes (by start of supplementation) Show forest plot | 4 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.97] |
| Analysis 1.12  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 12 Gestational diabetes (by start of supplementation). | ||||
| 12.1 Less than 20 weeks of pregnancy | 1 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.34, 2.28] |
| 12.2 20 weeks of pregnancy or more | 2 | 219 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.05, 3.45] |
| 12.3 Unknown/unreported/mixed | 1 | 87 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.13, 0.82] |
| 13 Gestational diabetes (by pre‐gestational BMI) Show forest plot | 4 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.97] |
| Analysis 1.13  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 13 Gestational diabetes (by pre‐gestational BMI). | ||||
| 13.1 Underweight (lower than 18.5) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.2 Normal weight (18.5 to 24.9) | 2 | 305 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.33, 2.05] |
| 13.3 Overweight (25 or higher) | 2 | 141 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.13, 0.79] |
| 13.4 Unknown/unreported/mixed | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Gestational diabetes (by supplementation scheme/regimen) Show forest plot | 4 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.97] |
| Analysis 1.14  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 14 Gestational diabetes (by supplementation scheme/regimen). | ||||
| 14.1 Single dose | 1 | 165 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.03, 8.28] |
| 14.2 Daily | 2 | 141 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.13, 0.79] |
| 14.3 Weekly/monthly | 1 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.34, 2.28] |
| 15 Gestational diabetes (by skin pigmentation based on Fitzpatrick skin tone chart) Show forest plot | 4 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.97] |
| Analysis 1.15  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 15 Gestational diabetes (by skin pigmentation based on Fitzpatrick skin tone chart). | ||||
| 15.1 Three or less | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 Four or more | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.3 Unknown/unreported/mixed | 4 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.97] |
| 16 Gestational diabetes (by latitude) Show forest plot | 4 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.97] |
| Analysis 1.16  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 16 Gestational diabetes (by latitude). | ||||
| 16.1 Between Tropics of Cancer and Capricorn | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16.2 North of the Tropic of Cancer or South of the Tropic of Capricorn | 4 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.97] |
| 16.3 Unknown/unreported | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Gestational diabetes (by season at the start of supplementation) Show forest plot | 4 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.97] |
| Analysis 1.17  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 17 Gestational diabetes (by season at the start of supplementation). | ||||
| 17.1 Summer | 1 | 54 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.84] |
| 17.2 Fall | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.3 Winter | 1 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.34, 2.28] |
| 17.4 Mixed/unknown | 2 | 252 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.14, 0.82] |
| 18 Preterm birth (less than 37 weeks' gestation) (by start of supplementation) Show forest plot | 7 | 1640 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.34, 1.30] |
| Analysis 1.18  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 18 Preterm birth (less than 37 weeks' gestation) (by start of supplementation). | ||||
| 18.1 Less than 20 weeks of pregnancy | 3 | 1149 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.26, 2.04] |
| 18.2 20 weeks of pregnancy or more | 4 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.13, 1.87] |
| 18.3 Unknown/unreported/mixed | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Preterm birth (less than 37 weeks' gestation) (by pre‐gestational BMI) Show forest plot | 7 | 1640 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.34, 1.30] |
| Analysis 1.19  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 19 Preterm birth (less than 37 weeks' gestation) (by pre‐gestational BMI). | ||||
| 19.1 Underweight (lower than 18.5) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 19.2 Normal weight (18.5 to 24.9) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 19.3 Overweight (25 or higher) | 2 | 138 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.15, 2.46] |
| 19.4 Unknown/unreported/mixed | 5 | 1502 | Risk Ratio (M‐H, Random, 95% CI) | 0.64 [0.27, 1.54] |
| 20 Preterm birth (less than 37 weeks' gestation) (by supplementation scheme/regimen) Show forest plot | 7 | 1640 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.34, 1.30] |
| Analysis 1.20  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 20 Preterm birth (less than 37 weeks' gestation) (by supplementation scheme/regimen). | ||||
| 20.1 Single dose | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 20.2 Daily | 6 | 1495 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.23, 1.58] |
| 20.3 Weekly/monthly | 1 | 145 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.32, 1.54] |
| 21 Preterm birth (less than 37 weeks' gestation) (by skin pigmentation based on Fitzpatrick skin tone chart) Show forest plot | 9 | 1943 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.30, 0.91] |
| Analysis 1.21  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 21 Preterm birth (less than 37 weeks' gestation) (by skin pigmentation based on Fitzpatrick skin tone chart). | ||||
| 21.1 Three or less | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 21.2 Four or more | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 21.3 Unknown/unreported/mixed | 9 | 1943 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.30, 0.91] |
| 22 Preterm birth (less than 37 weeks' gestation) (by latitude) Show forest plot | 7 | 1640 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.34, 1.30] |
| Analysis 1.22  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 22 Preterm birth (less than 37 weeks' gestation) (by latitude). | ||||
| 22.1 Between Tropics of Cancer and Capricorn | 2 | 358 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.05, 1.34] |
| 22.2 North of the Tropic of Cancer or South of the Tropic of Capricorn | 5 | 1282 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.59, 1.66] |
| 22.3 Unknown/unreported | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23 Preterm birth (less than 37 weeks' gestation) (by season at the start of supplementation) Show forest plot | 7 | 1640 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.34, 1.30] |
| Analysis 1.23  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 23 Preterm birth (less than 37 weeks' gestation) (by season at the start of supplementation). | ||||
| 23.1 Summer | 2 | 199 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.34, 1.53] |
| 23.2 Winter | 1 | 34 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23.3 Mixed/unknown | 4 | 1407 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.19, 1.66] |
| 24 Low birthweight (less than 2500 g) (by start of supplementation) Show forest plot | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.24, 0.65] |
| Analysis 1.24  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 24 Low birthweight (less than 2500 g) (by start of supplementation). | ||||
| 24.1 Less than 20 weeks of pregnancy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 24.2 20 weeks of pregnancy or more | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.24, 0.65] |
| 24.3 Unknown/unreported/mixed | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25 Low birthweight (less than 2500 g) (by pre‐gestational BMI) Show forest plot | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.24, 0.65] |
| Analysis 1.25  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 25 Low birthweight (less than 2500 g) (by pre‐gestational BMI). | ||||
| 25.1 Underweight (lower than 18.5) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25.2 Normal weight (18.5 to 24.9) | 1 | 165 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.19, 0.98] |
| 25.3 Overweight (25 or higher) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25.4 Unknown/unreported/mixed | 2 | 326 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.14, 0.88] |
| 26 Low birthweight (less than 2500 g) (by supplementation scheme/regimen) Show forest plot | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.24, 0.65] |
| Analysis 1.26  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 26 Low birthweight (less than 2500 g) (by supplementation scheme/regimen). | ||||
| 26.1 Single dose | 2 | 365 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.16, 0.65] |
| 26.2 Daily | 1 | 126 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.23, 1.21] |
| 26.3 Weekly/monthly | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27 Low birthweight (less than 2500 g) (by skin pigmentation based on Fitzpatrick skin to Show forest plot | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.24, 0.65] |
| Analysis 1.27  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 27 Low birthweight (less than 2500 g) (by skin pigmentation based on Fitzpatrick skin to. | ||||
| 27.1 Three or less | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27.2 Four or more | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27.3 Unknown/unreported/mixed | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.24, 0.65] |
| 28 Low birthweight (less than 2500 g) (by latitude) Show forest plot | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.24, 0.65] |
| Analysis 1.28  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 28 Low birthweight (less than 2500 g) (by latitude). | ||||
| 28.1 Between Tropics of Cancer and Capricorn | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 28.2 North of the Tropic of Cancer or South of the Tropic of Capricorn | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.24, 0.65] |
| 28.3 Unknown/unreported | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29 Low birthweight (less than 2500 g) (by season at the start of pregnancy) Show forest plot | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.24, 0.65] |
| Analysis 1.29  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 29 Low birthweight (less than 2500 g) (by season at the start of pregnancy). | ||||
| 29.1 Summer | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29.2 Fall | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29.3 Winter | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29.4 Mixed/unknown | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.24, 0.65] |
| 30 Caesarean section Show forest plot | 10 | 1104 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.80, 1.21] |
| Analysis 1.30  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 30 Caesarean section. | ||||
| 31 Gestational hypertension Show forest plot | 2 | 1130 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.41, 1.49] |
| Analysis 1.31  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 31 Gestational hypertension. | ||||
| 32 Maternal death (death while pregnant or within 42 days of termination of pregnancy) (ALL) Show forest plot | 1 | 180 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 1.32  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 32 Maternal death (death while pregnant or within 42 days of termination of pregnancy) (ALL). | ||||
| 33 Maternal vitamin D concentration at term (25‐hydroxyvitamin D) (nmol/L) (ALL) Show forest plot | 14 | 2470 | Mean Difference (IV, Random, 95% CI) | 35.66 [24.19, 47.13] |
| Analysis 1.33  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 33 Maternal vitamin D concentration at term (25‐hydroxyvitamin D) (nmol/L) (ALL). | ||||
| 34 Birth length (cm) Show forest plot | 8 | 931 | Mean Difference (IV, Random, 95% CI) | 0.57 [0.19, 0.95] |
| Analysis 1.34  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 34 Birth length (cm). | ||||
| 35 Head circumference at birth (cm) Show forest plot | 8 | 1841 | Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.21, 0.44] |
| Analysis 1.35  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 35 Head circumference at birth (cm). | ||||
| 36 Birthweight (g) Show forest plot | 17 | 2828 | Mean Difference (IV, Random, 95% CI) | 80.30 [‐14.40, 175.00] |
| Analysis 1.36  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 36 Birthweight (g). | ||||
| 37 Stillbirth Show forest plot | 3 | 584 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.06, 1.98] |
| Analysis 1.37  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 37 Stillbirth. | ||||
| 38 Neonatal death Show forest plot | 2 | 326 | Risk Ratio (M‐H, Random, 95% CI) | 0.27 [0.04, 1.67] |
| Analysis 1.38  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 38 Neonatal death. | ||||
| 39 Apgar score less than seven at five minutes Show forest plot | 1 | 165 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.11, 2.53] |
| Analysis 1.39  Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 39 Apgar score less than seven at five minutes. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pre‐eclampsia (ALL) Show forest plot | 4 | 1174 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.32, 0.78] |
| Analysis 2.1  Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 1 Pre‐eclampsia (ALL). | ||||
| 2 Gestational diabetes (ALL) Show forest plot | 1 | 54 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.84] |
| Analysis 2.2  Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 2 Gestational diabetes (ALL). | ||||
| 3 Preterm birth (less than 37 weeks' gestation) (ALL) Show forest plot | 5 | 942 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [1.01, 2.28] |
| Analysis 2.3  Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 3 Preterm birth (less than 37 weeks' gestation) (ALL). | ||||
| 4 Low birthweight (less than 2500 g) (ALL) Show forest plot | 2 | 110 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.10, 4.55] |
| Analysis 2.4  Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 4 Low birthweight (less than 2500 g) (ALL). | ||||
| 5 Caesarean section Show forest plot | 2 | 146 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.87, 1.54] |
| Analysis 2.5  Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 5 Caesarean section. | ||||
| 6 Gestational hypertension Show forest plot | 1 | 59 | Risk Ratio (M‐H, Random, 95% CI) | 0.26 [0.06, 1.12] |
| Analysis 2.6  Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 6 Gestational hypertension. | ||||
| 7 Maternal vitamin D concentration at term (25‐hydroxyvitamin D) (nmol/L) (ALL) Show forest plot | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 12.5 [3.80, 21.20] |
| Analysis 2.7  Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 7 Maternal vitamin D concentration at term (25‐hydroxyvitamin D) (nmol/L) (ALL). | ||||
| 8 Birth length (cm) Show forest plot | 3 | 194 | Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.67, 0.52] |
| Analysis 2.8  Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 8 Birth length (cm). | ||||
| 9 Head circumference at birth (cm) Show forest plot | 3 | 198 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.39, 0.33] |
| Analysis 2.9  Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 9 Head circumference at birth (cm). | ||||
| 10 Birthweight (g) Show forest plot | 3 | 194 | Mean Difference (IV, Random, 95% CI) | 42.39 [‐86.96, 171.74] |
| Analysis 2.10  Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 10 Birthweight (g). | ||||
| 11 Neonatal death Show forest plot | 1 | 660 | Risk Ratio (M‐H, Random, 95% CI) | 0.2 [0.01, 4.15] |
| Analysis 2.11  Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 11 Neonatal death. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Gestational diabetes (ALL) Show forest plot | 1 | 1298 | Risk Ratio (M‐H, Random, 95% CI) | 0.42 [0.10, 1.73] |
| Analysis 3.1  Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 1 Gestational diabetes (ALL). | ||||
| 2 Maternal adverse events Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 3.2  Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 2 Maternal adverse events. | ||||
| 2.1 Hypercalcaemia | 1 | 1298 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Hypercalciuria | 1 | 1298 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.02, 3.97] |
| 3 Preterm birth (less than 37 weeks' gestation) (ALL) Show forest plot | 1 | 1298 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.68, 1.59] |
| Analysis 3.3  Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 3 Preterm birth (less than 37 weeks' gestation) (ALL). | ||||
| 4 Low birthweight (less than 2500 g) (ALL) Show forest plot | 1 | 1298 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.82, 1.51] |
| Analysis 3.4  Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 4 Low birthweight (less than 2500 g) (ALL). | ||||
| 5 Caesarean section Show forest plot | 1 | 1298 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.95, 1.27] |
| Analysis 3.5  Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 5 Caesarean section. | ||||
| 6 Gestational hypertension Show forest plot | 1 | 1298 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.31, 2.79] |
| Analysis 3.6  Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 6 Gestational hypertension. | ||||
| 7 Maternal death (death while pregnant or within 42 days of termination of pregnancy) Show forest plot | 1 | 1300 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.02, 3.98] |
| Analysis 3.7  Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 7 Maternal death (death while pregnant or within 42 days of termination of pregnancy). | ||||
| 8 Maternal vitamin D concentration at term (25‐hydroxyvitamin D) (nmol/L) (ALL) Show forest plot | 1 | 635 | Mean Difference (IV, Random, 95% CI) | 75.17 [71.97, 78.37] |
| Analysis 3.8  Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 8 Maternal vitamin D concentration at term (25‐hydroxyvitamin D) (nmol/L) (ALL). | ||||
| 9 Birth length (cm) Show forest plot | 1 | 1297 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.28, 0.28] |
| Analysis 3.9  Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 9 Birth length (cm). | ||||
| 10 Head circumference at birth (cm) Show forest plot | 1 | 1297 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.17, 0.17] |
| Analysis 3.10  Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 10 Head circumference at birth (cm). | ||||
| 11 Birthweight (g) Show forest plot | 1 | 1297 | Mean Difference (IV, Random, 95% CI) | ‐7.0 [‐55.95, 41.95] |
| Analysis 3.11  Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 11 Birthweight (g). | ||||
| 12 Stillbirth Show forest plot | 1 | 1300 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.29, 1.46] |
| Analysis 3.12  Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 12 Stillbirth. | ||||
| 13 Neonatal death Show forest plot | 1 | 1298 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.22, 2.14] |
| Analysis 3.13  Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 13 Neonatal death. | ||||

Study flow diagram for this update

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
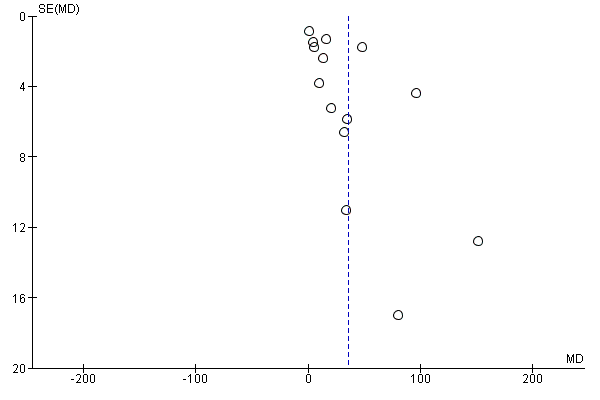
Funnel plot of comparison: 1 Vitamin D alone versus no treatment/placebo (no vitamins or minerals), outcome: 1.15 Maternal vitamin D concentration at term (25‐hydroxyvitamin D) (nmol/L) (ALL).
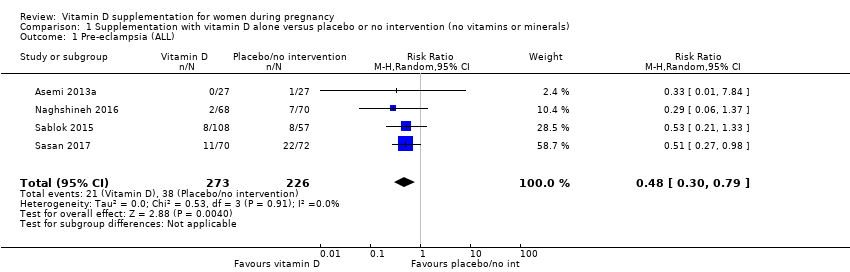
Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 1 Pre‐eclampsia (ALL).
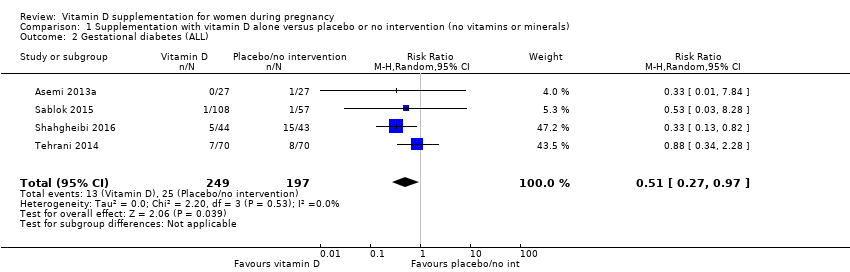
Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 2 Gestational diabetes (ALL).
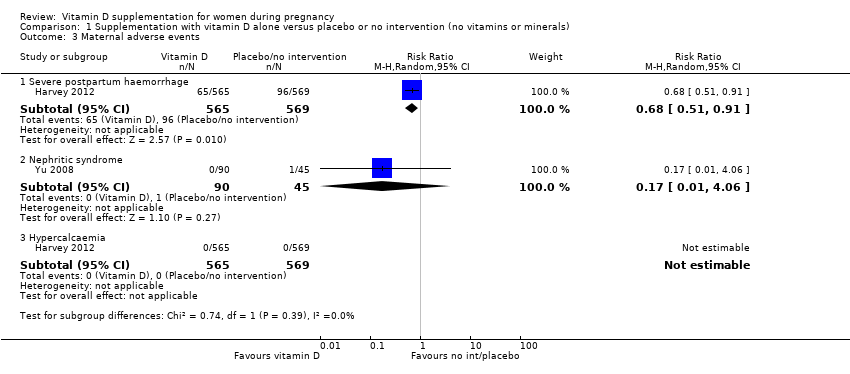
Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 3 Maternal adverse events.
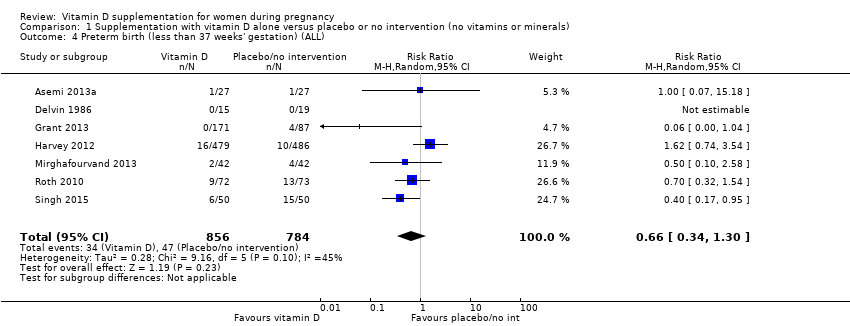
Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 4 Preterm birth (less than 37 weeks' gestation) (ALL).
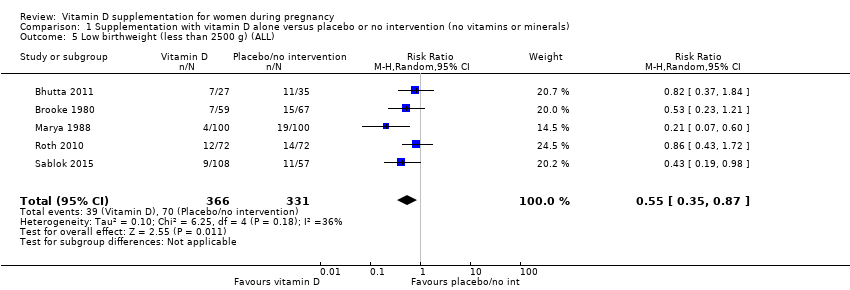
Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 5 Low birthweight (less than 2500 g) (ALL).
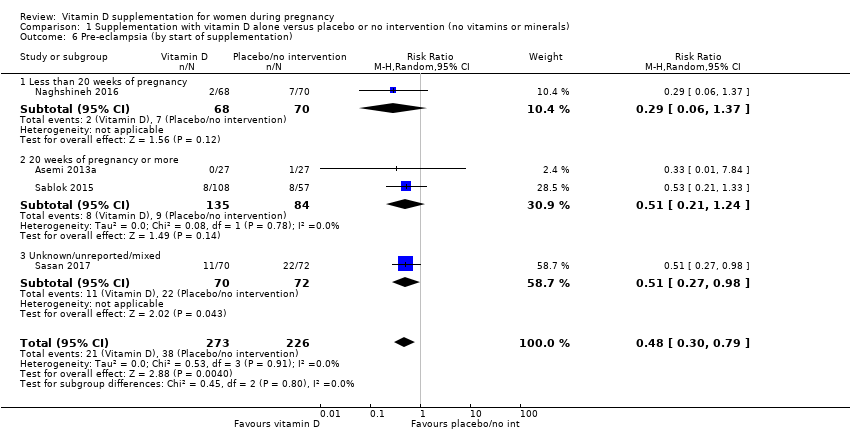
Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 6 Pre‐eclampsia (by start of supplementation).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 7 Pre‐eclampsia (by pre‐gestational BMI).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 8 Pre‐eclampsia (by supplementation scheme/regimen).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 9 Pre‐eclampsia (by skin pigmentation based on Fitzpatrick skin tone chart).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 10 Pre‐eclampsia (by latitude).
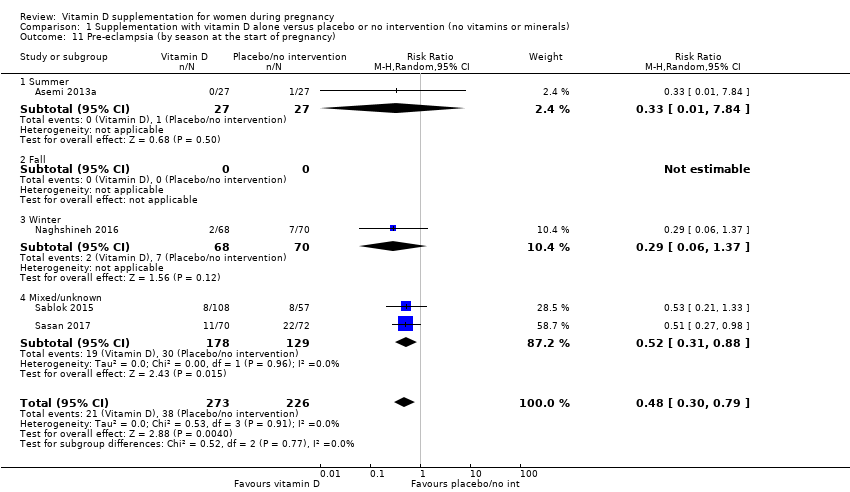
Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 11 Pre‐eclampsia (by season at the start of pregnancy).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 12 Gestational diabetes (by start of supplementation).
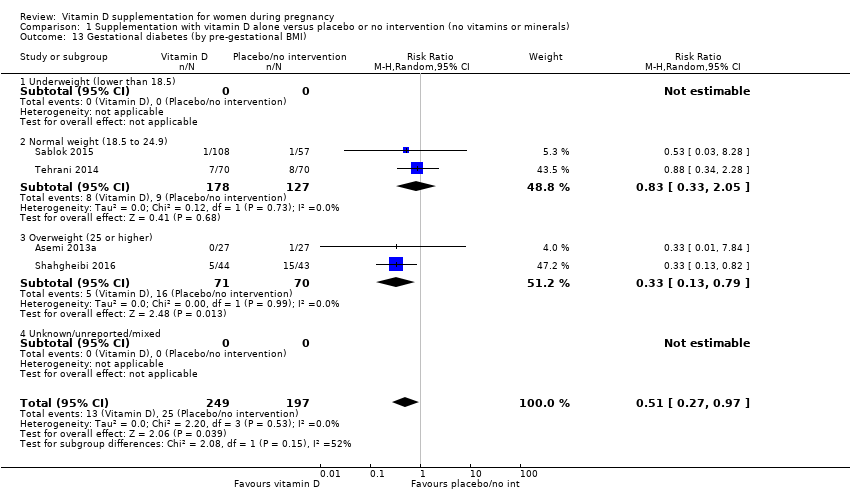
Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 13 Gestational diabetes (by pre‐gestational BMI).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 14 Gestational diabetes (by supplementation scheme/regimen).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 15 Gestational diabetes (by skin pigmentation based on Fitzpatrick skin tone chart).
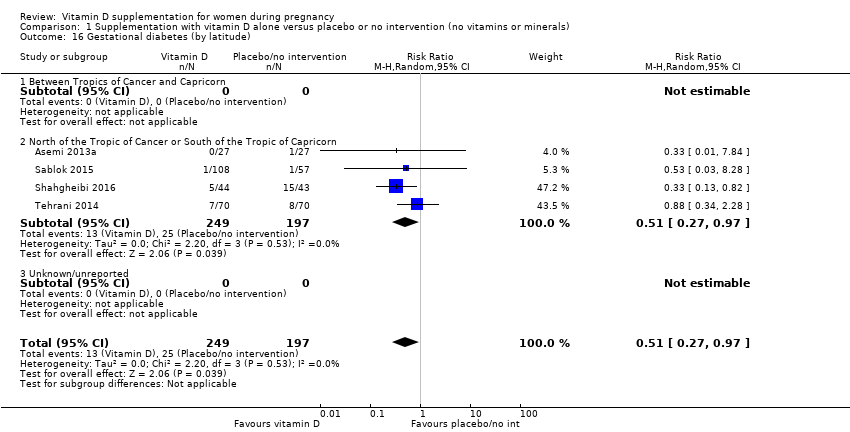
Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 16 Gestational diabetes (by latitude).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 17 Gestational diabetes (by season at the start of supplementation).
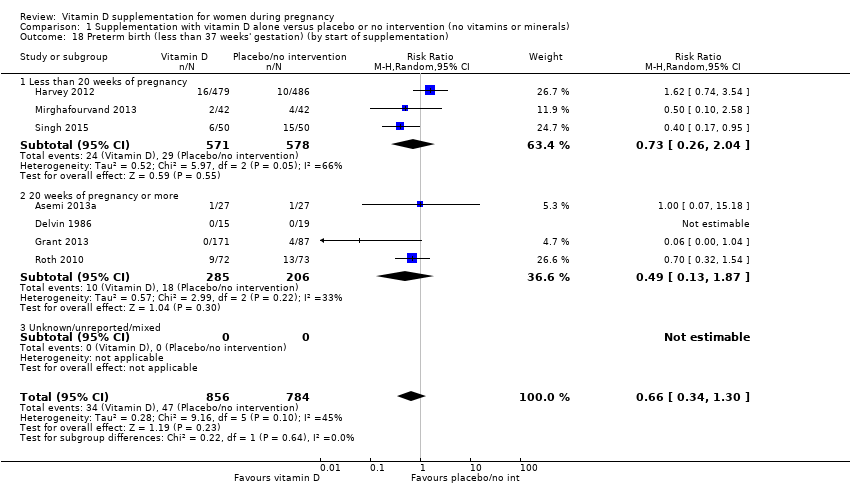
Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 18 Preterm birth (less than 37 weeks' gestation) (by start of supplementation).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 19 Preterm birth (less than 37 weeks' gestation) (by pre‐gestational BMI).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 20 Preterm birth (less than 37 weeks' gestation) (by supplementation scheme/regimen).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 21 Preterm birth (less than 37 weeks' gestation) (by skin pigmentation based on Fitzpatrick skin tone chart).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 22 Preterm birth (less than 37 weeks' gestation) (by latitude).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 23 Preterm birth (less than 37 weeks' gestation) (by season at the start of supplementation).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 24 Low birthweight (less than 2500 g) (by start of supplementation).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 25 Low birthweight (less than 2500 g) (by pre‐gestational BMI).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 26 Low birthweight (less than 2500 g) (by supplementation scheme/regimen).
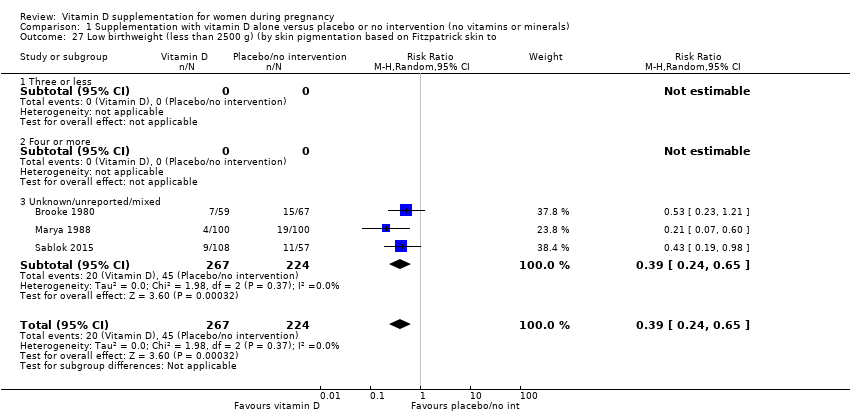
Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 27 Low birthweight (less than 2500 g) (by skin pigmentation based on Fitzpatrick skin to.
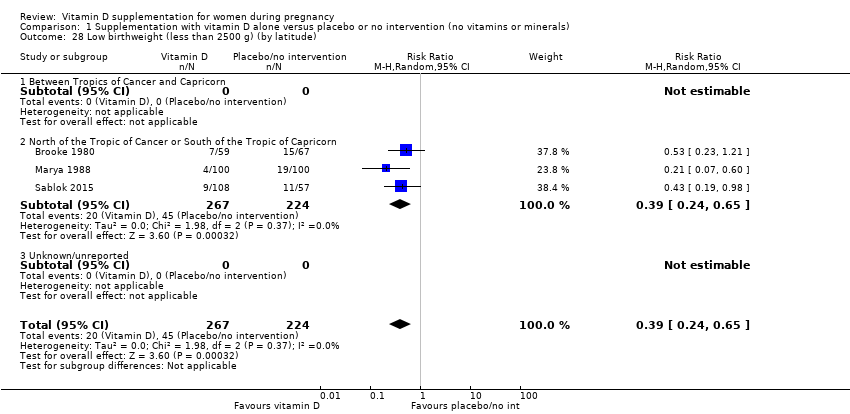
Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 28 Low birthweight (less than 2500 g) (by latitude).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 29 Low birthweight (less than 2500 g) (by season at the start of pregnancy).
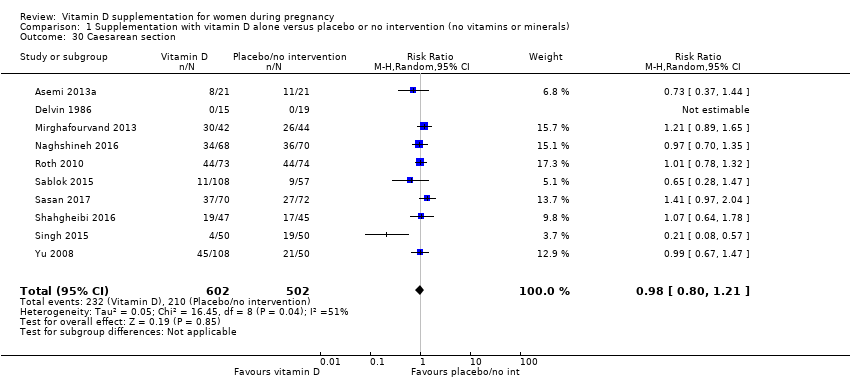
Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 30 Caesarean section.
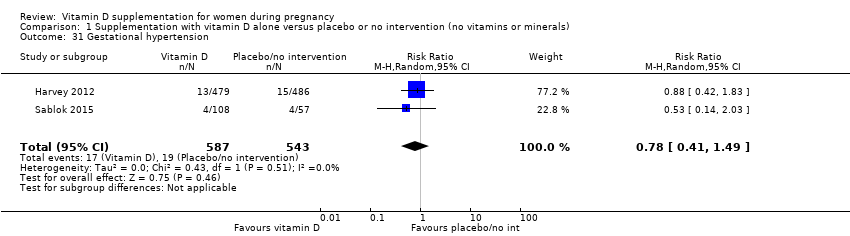
Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 31 Gestational hypertension.

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 32 Maternal death (death while pregnant or within 42 days of termination of pregnancy) (ALL).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 33 Maternal vitamin D concentration at term (25‐hydroxyvitamin D) (nmol/L) (ALL).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 34 Birth length (cm).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 35 Head circumference at birth (cm).
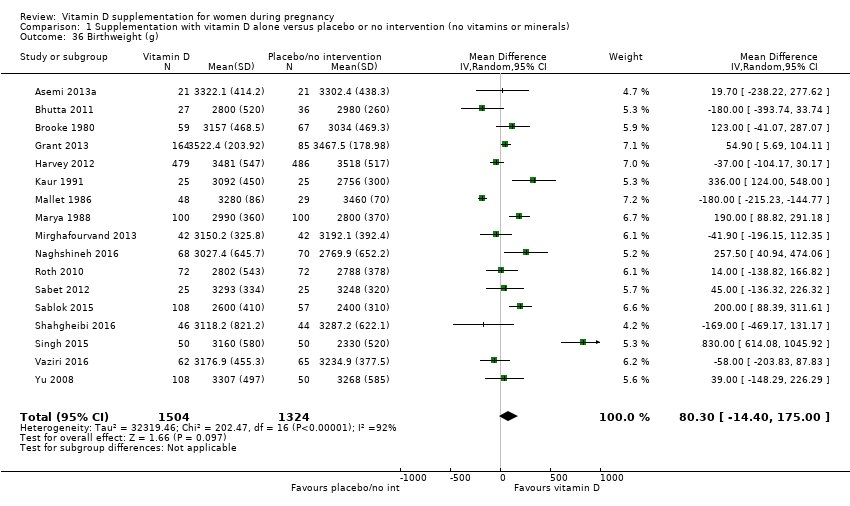
Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 36 Birthweight (g).

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 37 Stillbirth.
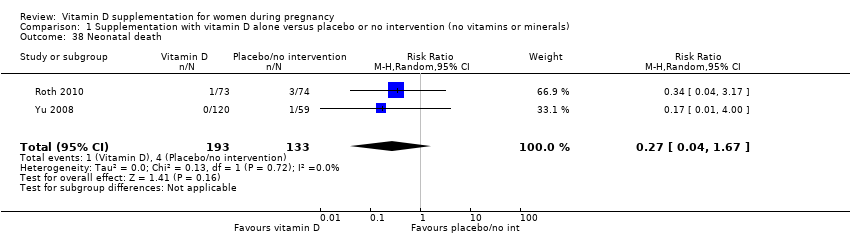
Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 38 Neonatal death.

Comparison 1 Supplementation with vitamin D alone versus placebo or no intervention (no vitamins or minerals), Outcome 39 Apgar score less than seven at five minutes.
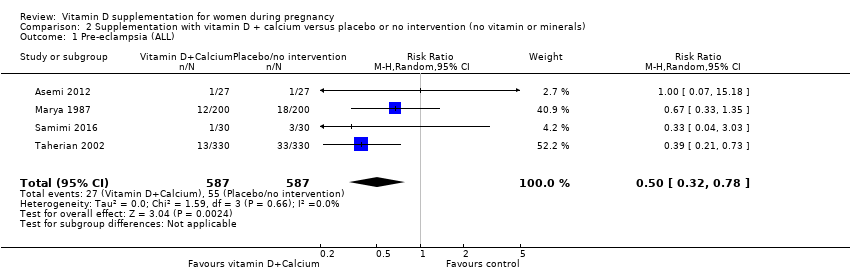
Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 1 Pre‐eclampsia (ALL).

Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 2 Gestational diabetes (ALL).
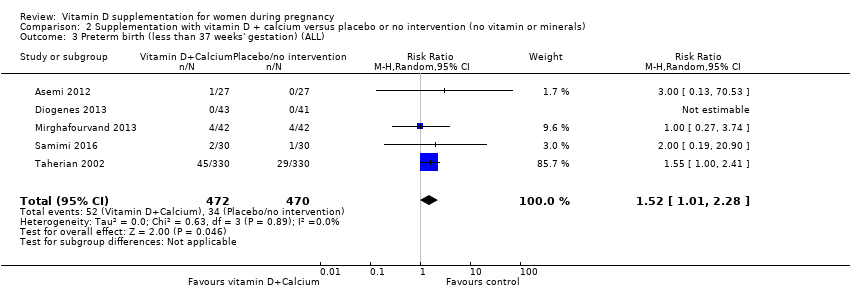
Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 3 Preterm birth (less than 37 weeks' gestation) (ALL).
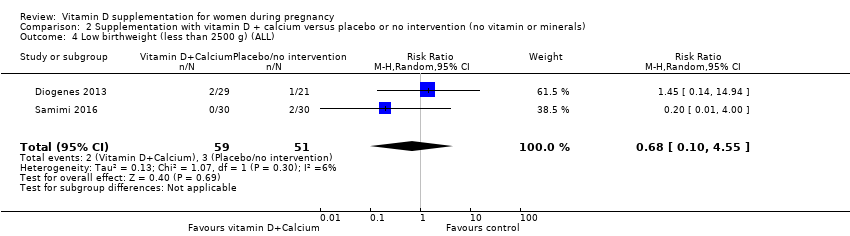
Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 4 Low birthweight (less than 2500 g) (ALL).

Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 5 Caesarean section.
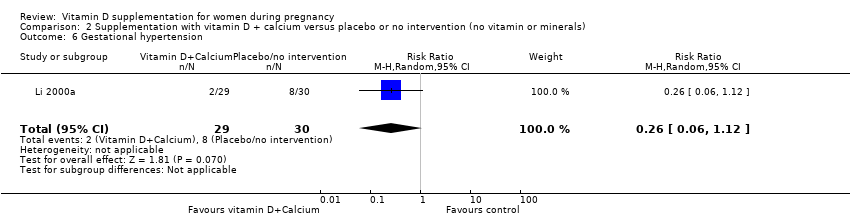
Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 6 Gestational hypertension.

Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 7 Maternal vitamin D concentration at term (25‐hydroxyvitamin D) (nmol/L) (ALL).

Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 8 Birth length (cm).

Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 9 Head circumference at birth (cm).
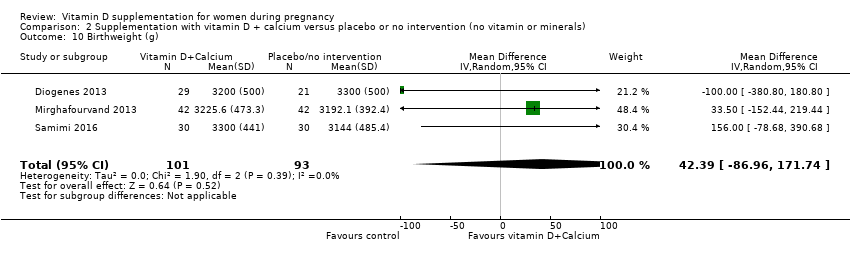
Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 10 Birthweight (g).

Comparison 2 Supplementation with vitamin D + calcium versus placebo or no intervention (no vitamin or minerals), Outcome 11 Neonatal death.
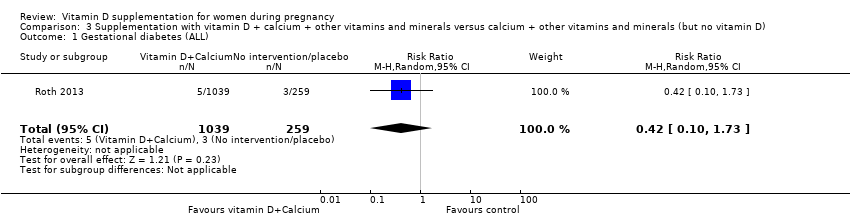
Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 1 Gestational diabetes (ALL).
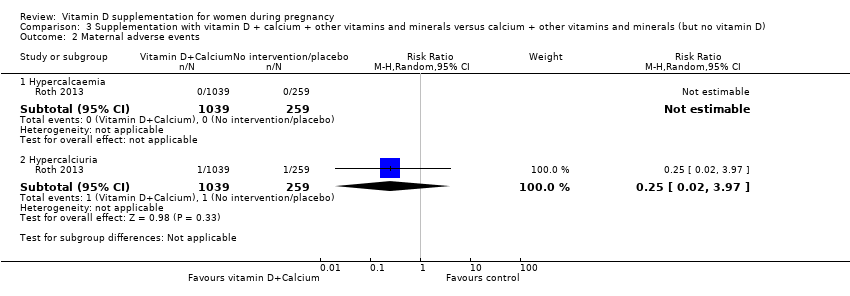
Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 2 Maternal adverse events.

Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 3 Preterm birth (less than 37 weeks' gestation) (ALL).

Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 4 Low birthweight (less than 2500 g) (ALL).
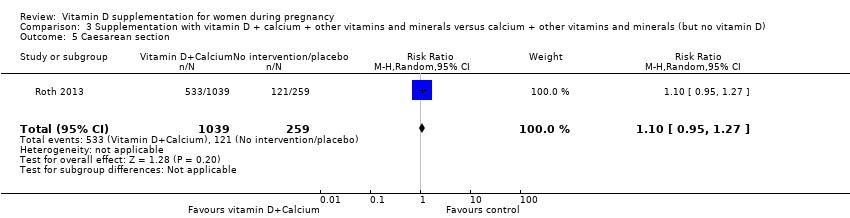
Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 5 Caesarean section.

Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 6 Gestational hypertension.

Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 7 Maternal death (death while pregnant or within 42 days of termination of pregnancy).

Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 8 Maternal vitamin D concentration at term (25‐hydroxyvitamin D) (nmol/L) (ALL).

Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 9 Birth length (cm).
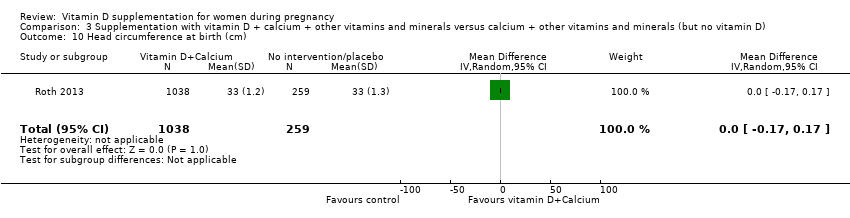
Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 10 Head circumference at birth (cm).
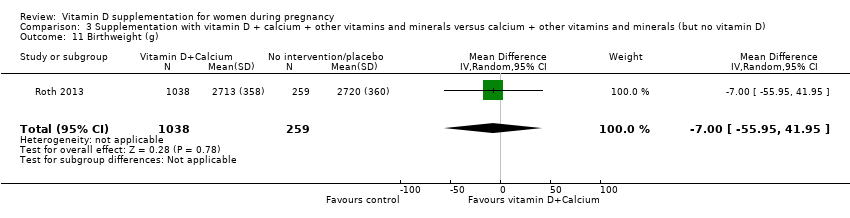
Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 11 Birthweight (g).

Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 12 Stillbirth.
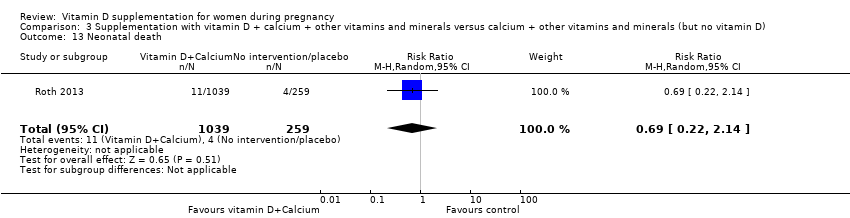
Comparison 3 Supplementation with vitamin D + calcium + other vitamins and minerals versus calcium + other vitamins and minerals (but no vitamin D), Outcome 13 Neonatal death.
| Vitamin D supplementation compared to placebo/control for pregnancy and neonatal health outcomes | ||||||
| Patient or population: pregnant women and their infants. | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with placebo/control | Risk with vitamin D supplementation | |||||
| Pre‐eclampsia | Study population | RR 0.48 (0.30, 0.79) | 499 | ⊕⊕⊕⊝ | Included trials: Asemi 2013a; Naghshineh 2016; Sablok 2015; Sasan 2017 | |
| 168 per 1000 | 79 per 1000 | |||||
| Gestational diabetes | Study population | RR 0.51 | 446 | ⊕⊕⊕⊝ | Included trials: Asemi 2013a; Sablok 2015; Shahgheibi 2016; Tehrani 2014 | |
| 127 per 1000 | 65 per 1000 | |||||
| Maternal adverse events: severe postpartum haemorrhage | Study population | RR 0.68 | 1134 | ⊕⊕⊝⊝ | Included trial: Harvey 2012 | |
| 158 per 1000 | 106 per 1000 | |||||
| Maternal adverse event: nephritic syndrome | Study population | RR 0.17 (0.01 to 4.06) | 135 (1 RCT) | ⊕⊝⊝⊝ | Included trial: Yu 2008 | |
| 22 per 1000 | 4 per 1000 (0 to 90) | |||||
| Maternal adverse event: hypercalcaemia | Study population | Not estimable | 1134 | ⊕⊕⊝⊝ | Included trial: Harvey 2012 | |
| 0 per 1000 | 0 per 1000 | |||||
| Preterm birth (less than 37 weeks' gestation) | Study population | RR 0.66 (0.34 to 1.30) | 1640 | ⊕⊕⊝⊝ | Included trials: Asemi 2013a; Delvin 1986; Grant 2013; Harvey 2012; Mirghafourvand 2013; Roth 2010; Singh 2015 | |
| 87 per 1000 | 57 per 1000 | |||||
| Low birthweight (less than 2500 g) | Study population | RR 0.55 | 697 | ⊕⊕⊕⊝ | Included trials: Brooke 1980; Bhutta 2011; Marya 1988; Roth 2010; Sablok 2015 | |
| 136 per 1000 | 75 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 We downgraded (1) level for serious limitations in study design due to one trial being assessed as high risk of bias for several domains and two trials having unclear allocation concealment. 2 We downgraded (1) level for serious limitations in study design due to one trial being assessed as high risk of bias for several domains. 3 We downgraded (2) levels for very serious limitations in study design due to one study being assessed as high risk of other bias because we do not know the impact of the participants who were allowed to continue taking their own multivitamin with 400 IU/d of vitamin D as this was not recorded. 4 We downgraded (1) level for serious limitations in study design due to one study being assessed as high risk of bias for performance and detection bias. 5 We downgraded (2) levels for very serious limitations in imprecision as only one small study, with a small number of events and wide 95% confidence intervals (CI) contributed data. 6 We downgraded (1) level for serious limitations in imprecision due to a single study with zero events contributing data. 7 We downgraded (1) level for serious limitations in study design due to two studies being at unclear risk of selection bias and one study being at high risk of other bias. 8 We downgraded (1) level for serious limitations in imprecision as the 95% confidence interval (CI) was wide and crossed the line of no effect. 9 We downgraded (1) level for serious limitations in study design due to two studies being at unclear risk of selection bias, one study being at high risk of bias for allocation concealment, and three studies being at high risk of attrition bias. | ||||||
| Vitamin D + calcium supplementation compared to placebo/control for pregnancy and neonatal health outcomes | |||||||
| Patient or population: pregnant women and their infants.. | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | ||
| Risk with placebo/control | Risk with vitamin D + calcium supplementation | ||||||
| Pre‐eclampsia | Study population | RR 0.50 | 1174 | ⊕⊕⊕⊝ | Included trials: Asemi 2012; Marya 1987; Samimi 2016; Taherian 2002 | ||
| 94 per 1000 | 47 per 1000 | ||||||
| Gestational diabetes | Study population | RR 0.33 | 54 | ⊕⊝⊝⊝ | Included trial: Asemi 2012 | ||
| 37 per 1000 | 12 per 1000 | ||||||
| Maternal adverse events | ‐ | ‐ | ‐ | ‐ | ‐ | No trials reported on this outcome | |
| Preterm birth (less than 37 weeks' gestation) | Study population | RR 1.52 | 942 | ⊕⊕⊝⊝ | Included trials: Asemi 2012; Diogenes 2013, Mirghafourvand 2013, Samimi 2016; Taherian 2002; | ||
| 72 per 1000 | 110 per 1000 | ||||||
| Low birthweight (less than 2500 g) | Study population | RR 0.68 | 110 | ⊕⊝⊝⊝ | Included trials: Diogenes 2013; Samimi 2016 | ||
| 59 per 1000 | 40 per 1000 | ||||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||||
| GRADE Working Group grades of evidence | |||||||
| 1 We downgraded (1) level for serious limitations in study design due to one study being at high risk of attrition and selection bias and three studies being at high risk of performance and detection bias. 2 We downgraded (1) level for serious limitations in study design due to one study being at high risk of performance and detection bias. 3 We downgraded (2) levels for very serious limitations in imprecision due to one small study, with a single event and wide 95% confidence intervals (CI) crossing the line of no effect contributing data. 4 We downgraded (1) level for serious limitations in study design due to three studies being at unclear risk of allocation concealment and three studies being at high risk of performance and detection bias. 5 We downgraded (1) level for serious limitations in imprecision due to wide 95% confidence intervals (CI). 6 We downgraded (1) level for serious limitations in study design due to one study being at unclear risk of allocation concealment and one study being at high risk of attrition bias. 7 We downgraded (2) levels for very serious limitations in imprecision due two small studies, with very few events and wide 95% confidence intervals (CI) crossing the line of no effect contributing data. | |||||||
| Vitamin D + calcium + other vitamins and minerals compared to calcium + other vitamins and minerals (but no vitamin D) for pregnancy and neonatal health outcomes | ||||||
| Patient or population: pregnant women and their infants.. | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with calcium + other vitamins and minerals (but no vitamin D) | Risk with vitamin D + calcium + other vitamins and minerals | |||||
| Pre‐eclampsia | Study population | ‐ | (0 trials) | ‐ | No trials reported on this outcome | |
| see comment | see comment | |||||
| Gestational diabetes | Study population | RR 0.42 | 1298 | ⊕⊝⊝⊝ | Included trial: Roth 2013 | |
| 12 per 1000 | 5 per 1000 | |||||
| Maternal adverse event: hypercalcaemia | Study population | ‐ | 1298 | ⊕⊝⊝⊝ | Included trial: Roth 2013 | |
| 23 per 1000 | 64 per 1000 | |||||
| Maternal adverse event: hypercalciuria | Study population | 0.25 (0.02 to 3.97) | 1298 | ⊕⊝⊝⊝ | Included trial: Roth 2013 | |
| 4 per 1000 | 1 per 1000 (0 to 15) | |||||
| Preterm birth (less than 37 weeks' gestation) | Study population | RR 1.04 | 1298 | ⊕⊕⊝⊝ | Included trial: Roth 2013 | |
| 93 per 1000 | 96 per 1000 | |||||
| Low birthweight (less than 2500 g) | Study population | RR 1.12 | 1298 | ⊕⊕⊝⊝ | Included trial: Roth 2013 | |
| 162 per 1000 | 182 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 We downgraded (2) levels for very serious limitations in imprecision with only one trial, with few events, and wide 95% confidence intervals (CI) crossing the line of no effect contributing data. 2 We downgraded (1) level for serious indirectness as there were multiple nutrient interventions in addition to vitamin D. 2 We downgraded (2) levels for very serious limitations in imprecision with only one trial, with zero events, and wide 95% confidence intervals (CI) crossing the line of no effect contributing data. 3 We downgraded (1) level for serious limitations in imprecision due to only one trial with wide 95% confidence intervals (CI) crossing the line of no effect contributing data. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pre‐eclampsia (ALL) Show forest plot | 4 | 499 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.30, 0.79] |
| 2 Gestational diabetes (ALL) Show forest plot | 4 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.97] |
| 3 Maternal adverse events Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 Severe postpartum haemorrhage | 1 | 1134 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.51, 0.91] |
| 3.2 Nephritic syndrome | 1 | 135 | Risk Ratio (M‐H, Random, 95% CI) | 0.17 [0.01, 4.06] |
| 3.3 Hypercalcaemia | 1 | 1134 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Preterm birth (less than 37 weeks' gestation) (ALL) Show forest plot | 7 | 1640 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.34, 1.30] |
| 5 Low birthweight (less than 2500 g) (ALL) Show forest plot | 5 | 697 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.35, 0.87] |
| 6 Pre‐eclampsia (by start of supplementation) Show forest plot | 4 | 499 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.30, 0.79] |
| 6.1 Less than 20 weeks of pregnancy | 1 | 138 | Risk Ratio (M‐H, Random, 95% CI) | 0.29 [0.06, 1.37] |
| 6.2 20 weeks of pregnancy or more | 2 | 219 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.21, 1.24] |
| 6.3 Unknown/unreported/mixed | 1 | 142 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.98] |
| 7 Pre‐eclampsia (by pre‐gestational BMI) Show forest plot | 4 | 499 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.30, 0.79] |
| 7.1 Underweight (lower than 18.5) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Normal weight (18.5 to 24.9) | 1 | 165 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.21, 1.33] |
| 7.3 Overweight (25 or higher) | 1 | 54 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.84] |
| 7.4 Unknown/unreported/mixed | 2 | 280 | Risk Ratio (M‐H, Random, 95% CI) | 0.47 [0.26, 0.86] |
| 8 Pre‐eclampsia (by supplementation scheme/regimen) Show forest plot | 4 | 499 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.30, 0.79] |
| 8.1 Single dose | 1 | 165 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.21, 1.33] |
| 8.2 Daily | 2 | 192 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.08, 1.20] |
| 8.3 Weekly/monthly | 1 | 142 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.98] |
| 9 Pre‐eclampsia (by skin pigmentation based on Fitzpatrick skin tone chart) Show forest plot | 4 | 499 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.30, 0.79] |
| 9.1 Three or less | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 Four or more | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.3 Unknown/unreported/mixed | 4 | 499 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.30, 0.79] |
| 10 Pre‐eclampsia (by latitude) Show forest plot | 4 | 499 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.30, 0.79] |
| 10.1 Between Tropics of Cancer and Capricorn | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10.2 North of the Tropic of Cancer or South of the Tropic of Capricorn | 4 | 499 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.30, 0.79] |
| 10.3 Unknown/unreported | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Pre‐eclampsia (by season at the start of pregnancy) Show forest plot | 4 | 499 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.30, 0.79] |
| 11.1 Summer | 1 | 54 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.84] |
| 11.2 Fall | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.3 Winter | 1 | 138 | Risk Ratio (M‐H, Random, 95% CI) | 0.29 [0.06, 1.37] |
| 11.4 Mixed/unknown | 2 | 307 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.31, 0.88] |
| 12 Gestational diabetes (by start of supplementation) Show forest plot | 4 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.97] |
| 12.1 Less than 20 weeks of pregnancy | 1 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.34, 2.28] |
| 12.2 20 weeks of pregnancy or more | 2 | 219 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.05, 3.45] |
| 12.3 Unknown/unreported/mixed | 1 | 87 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.13, 0.82] |
| 13 Gestational diabetes (by pre‐gestational BMI) Show forest plot | 4 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.97] |
| 13.1 Underweight (lower than 18.5) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.2 Normal weight (18.5 to 24.9) | 2 | 305 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.33, 2.05] |
| 13.3 Overweight (25 or higher) | 2 | 141 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.13, 0.79] |
| 13.4 Unknown/unreported/mixed | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Gestational diabetes (by supplementation scheme/regimen) Show forest plot | 4 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.97] |
| 14.1 Single dose | 1 | 165 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.03, 8.28] |
| 14.2 Daily | 2 | 141 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.13, 0.79] |
| 14.3 Weekly/monthly | 1 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.34, 2.28] |
| 15 Gestational diabetes (by skin pigmentation based on Fitzpatrick skin tone chart) Show forest plot | 4 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.97] |
| 15.1 Three or less | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 Four or more | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.3 Unknown/unreported/mixed | 4 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.97] |
| 16 Gestational diabetes (by latitude) Show forest plot | 4 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.97] |
| 16.1 Between Tropics of Cancer and Capricorn | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16.2 North of the Tropic of Cancer or South of the Tropic of Capricorn | 4 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.97] |
| 16.3 Unknown/unreported | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Gestational diabetes (by season at the start of supplementation) Show forest plot | 4 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.27, 0.97] |
| 17.1 Summer | 1 | 54 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.84] |
| 17.2 Fall | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.3 Winter | 1 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.34, 2.28] |
| 17.4 Mixed/unknown | 2 | 252 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.14, 0.82] |
| 18 Preterm birth (less than 37 weeks' gestation) (by start of supplementation) Show forest plot | 7 | 1640 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.34, 1.30] |
| 18.1 Less than 20 weeks of pregnancy | 3 | 1149 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.26, 2.04] |
| 18.2 20 weeks of pregnancy or more | 4 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.13, 1.87] |
| 18.3 Unknown/unreported/mixed | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Preterm birth (less than 37 weeks' gestation) (by pre‐gestational BMI) Show forest plot | 7 | 1640 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.34, 1.30] |
| 19.1 Underweight (lower than 18.5) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 19.2 Normal weight (18.5 to 24.9) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 19.3 Overweight (25 or higher) | 2 | 138 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.15, 2.46] |
| 19.4 Unknown/unreported/mixed | 5 | 1502 | Risk Ratio (M‐H, Random, 95% CI) | 0.64 [0.27, 1.54] |
| 20 Preterm birth (less than 37 weeks' gestation) (by supplementation scheme/regimen) Show forest plot | 7 | 1640 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.34, 1.30] |
| 20.1 Single dose | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 20.2 Daily | 6 | 1495 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.23, 1.58] |
| 20.3 Weekly/monthly | 1 | 145 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.32, 1.54] |
| 21 Preterm birth (less than 37 weeks' gestation) (by skin pigmentation based on Fitzpatrick skin tone chart) Show forest plot | 9 | 1943 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.30, 0.91] |
| 21.1 Three or less | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 21.2 Four or more | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 21.3 Unknown/unreported/mixed | 9 | 1943 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.30, 0.91] |
| 22 Preterm birth (less than 37 weeks' gestation) (by latitude) Show forest plot | 7 | 1640 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.34, 1.30] |
| 22.1 Between Tropics of Cancer and Capricorn | 2 | 358 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.05, 1.34] |
| 22.2 North of the Tropic of Cancer or South of the Tropic of Capricorn | 5 | 1282 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.59, 1.66] |
| 22.3 Unknown/unreported | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23 Preterm birth (less than 37 weeks' gestation) (by season at the start of supplementation) Show forest plot | 7 | 1640 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.34, 1.30] |
| 23.1 Summer | 2 | 199 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.34, 1.53] |
| 23.2 Winter | 1 | 34 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23.3 Mixed/unknown | 4 | 1407 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.19, 1.66] |
| 24 Low birthweight (less than 2500 g) (by start of supplementation) Show forest plot | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.24, 0.65] |
| 24.1 Less than 20 weeks of pregnancy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 24.2 20 weeks of pregnancy or more | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.24, 0.65] |
| 24.3 Unknown/unreported/mixed | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25 Low birthweight (less than 2500 g) (by pre‐gestational BMI) Show forest plot | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.24, 0.65] |
| 25.1 Underweight (lower than 18.5) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25.2 Normal weight (18.5 to 24.9) | 1 | 165 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.19, 0.98] |
| 25.3 Overweight (25 or higher) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25.4 Unknown/unreported/mixed | 2 | 326 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.14, 0.88] |
| 26 Low birthweight (less than 2500 g) (by supplementation scheme/regimen) Show forest plot | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.24, 0.65] |
| 26.1 Single dose | 2 | 365 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.16, 0.65] |
| 26.2 Daily | 1 | 126 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.23, 1.21] |
| 26.3 Weekly/monthly | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27 Low birthweight (less than 2500 g) (by skin pigmentation based on Fitzpatrick skin to Show forest plot | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.24, 0.65] |
| 27.1 Three or less | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27.2 Four or more | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27.3 Unknown/unreported/mixed | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.24, 0.65] |
| 28 Low birthweight (less than 2500 g) (by latitude) Show forest plot | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.24, 0.65] |
| 28.1 Between Tropics of Cancer and Capricorn | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 28.2 North of the Tropic of Cancer or South of the Tropic of Capricorn | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.24, 0.65] |
| 28.3 Unknown/unreported | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29 Low birthweight (less than 2500 g) (by season at the start of pregnancy) Show forest plot | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.24, 0.65] |
| 29.1 Summer | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29.2 Fall | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29.3 Winter | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29.4 Mixed/unknown | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.24, 0.65] |
| 30 Caesarean section Show forest plot | 10 | 1104 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.80, 1.21] |
| 31 Gestational hypertension Show forest plot | 2 | 1130 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.41, 1.49] |
| 32 Maternal death (death while pregnant or within 42 days of termination of pregnancy) (ALL) Show forest plot | 1 | 180 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33 Maternal vitamin D concentration at term (25‐hydroxyvitamin D) (nmol/L) (ALL) Show forest plot | 14 | 2470 | Mean Difference (IV, Random, 95% CI) | 35.66 [24.19, 47.13] |
| 34 Birth length (cm) Show forest plot | 8 | 931 | Mean Difference (IV, Random, 95% CI) | 0.57 [0.19, 0.95] |
| 35 Head circumference at birth (cm) Show forest plot | 8 | 1841 | Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.21, 0.44] |
| 36 Birthweight (g) Show forest plot | 17 | 2828 | Mean Difference (IV, Random, 95% CI) | 80.30 [‐14.40, 175.00] |
| 37 Stillbirth Show forest plot | 3 | 584 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.06, 1.98] |
| 38 Neonatal death Show forest plot | 2 | 326 | Risk Ratio (M‐H, Random, 95% CI) | 0.27 [0.04, 1.67] |
| 39 Apgar score less than seven at five minutes Show forest plot | 1 | 165 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.11, 2.53] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pre‐eclampsia (ALL) Show forest plot | 4 | 1174 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.32, 0.78] |
| 2 Gestational diabetes (ALL) Show forest plot | 1 | 54 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.84] |
| 3 Preterm birth (less than 37 weeks' gestation) (ALL) Show forest plot | 5 | 942 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [1.01, 2.28] |
| 4 Low birthweight (less than 2500 g) (ALL) Show forest plot | 2 | 110 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.10, 4.55] |
| 5 Caesarean section Show forest plot | 2 | 146 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.87, 1.54] |
| 6 Gestational hypertension Show forest plot | 1 | 59 | Risk Ratio (M‐H, Random, 95% CI) | 0.26 [0.06, 1.12] |
| 7 Maternal vitamin D concentration at term (25‐hydroxyvitamin D) (nmol/L) (ALL) Show forest plot | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 12.5 [3.80, 21.20] |
| 8 Birth length (cm) Show forest plot | 3 | 194 | Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.67, 0.52] |
| 9 Head circumference at birth (cm) Show forest plot | 3 | 198 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.39, 0.33] |
| 10 Birthweight (g) Show forest plot | 3 | 194 | Mean Difference (IV, Random, 95% CI) | 42.39 [‐86.96, 171.74] |
| 11 Neonatal death Show forest plot | 1 | 660 | Risk Ratio (M‐H, Random, 95% CI) | 0.2 [0.01, 4.15] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Gestational diabetes (ALL) Show forest plot | 1 | 1298 | Risk Ratio (M‐H, Random, 95% CI) | 0.42 [0.10, 1.73] |
| 2 Maternal adverse events Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 Hypercalcaemia | 1 | 1298 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Hypercalciuria | 1 | 1298 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.02, 3.97] |
| 3 Preterm birth (less than 37 weeks' gestation) (ALL) Show forest plot | 1 | 1298 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.68, 1.59] |
| 4 Low birthweight (less than 2500 g) (ALL) Show forest plot | 1 | 1298 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.82, 1.51] |
| 5 Caesarean section Show forest plot | 1 | 1298 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.95, 1.27] |
| 6 Gestational hypertension Show forest plot | 1 | 1298 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.31, 2.79] |
| 7 Maternal death (death while pregnant or within 42 days of termination of pregnancy) Show forest plot | 1 | 1300 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.02, 3.98] |
| 8 Maternal vitamin D concentration at term (25‐hydroxyvitamin D) (nmol/L) (ALL) Show forest plot | 1 | 635 | Mean Difference (IV, Random, 95% CI) | 75.17 [71.97, 78.37] |
| 9 Birth length (cm) Show forest plot | 1 | 1297 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.28, 0.28] |
| 10 Head circumference at birth (cm) Show forest plot | 1 | 1297 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.17, 0.17] |
| 11 Birthweight (g) Show forest plot | 1 | 1297 | Mean Difference (IV, Random, 95% CI) | ‐7.0 [‐55.95, 41.95] |
| 12 Stillbirth Show forest plot | 1 | 1300 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.29, 1.46] |
| 13 Neonatal death Show forest plot | 1 | 1298 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.22, 2.14] |

