Resección del tabique en mujeres en edad reproductiva con un útero tabicado
Resumen
Antecedentes
Las mujeres con un útero tabicado tienen mayor riesgo de sufrir subfertilidad, abortos espontáneos recurrentes y partos prematuros. La restauración de la anatomía del útero por medio de la resección del tabique histeroscópico es una intervención establecida. Este tratamiento se ha evaluado principalmente en estudios de cohorte retrospectivos, que indicaron un efecto positivo sobre los resultados del embarazo. El mayor defecto de estos estudios es el diseño tipo antes/después, que siempre favorecerá la intervención probada.
Objetivos
Determinar si la resección histeroscópica del tabique en mujeres en edad fértil con un útero tabicado mejora las tasas de nacidos vivos, y evaluar la seguridad de este procedimiento.
Métodos de búsqueda
Se realizaron búsquedas en el Registro Especializado del Grupo Cochrane de Ginecología y Fertilidad (Cochrane Gynaecology and Fertility Group) (inicio hasta mayo 2016), en el Registro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials, CENTRAL CRSO) (inicio hasta mayo 2016), MEDLINE (1946 hasta mayo 2016), Embase (1974 hasta mayo 2016), PsycINFO (1806 hasta mayo 2016) y en la base de datos CINAHL (1982 hasta mayo 2016). También se realizaron búsquedas en los registros de ensayos para encontrar ensayos en curso y registrados, listas de referencias, The Cochrane Library, tesis y disertaciones no publicadas, resúmenes de congresos, OpenGrey, LILACS, PubMed y Google.
Criterios de selección
Se planificó incluir ensayos controlados aleatorizados que evaluaran el efecto sobre los resultados reproductivos y la seguridad, de la resección histeroscópica del tabique en mujeres en edad reproductiva con un útero tabicado.
Obtención y análisis de los datos
Si hubiera habido estudios para inclusión, dos autores de la revisión de forma independiente habrían seleccionado los estudios, evaluado el riesgo de sesgo del ensayo y extraído los datos. Los autores de la revisión habrían establecido contacto con autores de los estudios para obtener información adicional.
Resultados principales
Al igual que en la versión 2011 de esta revisión, no se identificaron ensayos controlados aleatorizados para su inclusión en esta actualización.
Conclusiones de los autores
La resección histeroscópica del tabique en mujeres en edad fértil con un útero tabicado se realiza en todo el mundo para mejorar los resultados de la reproducción. En la actualidad no hay evidencia que apoye el procedimiento quirúrgico en estas mujeres. Se necesitan urgentemente ensayos controlados aleatorizados. Actualmente se realizan dos ensayos.
PICO
Resumen en términos sencillos
Resección del tabique en mujeres en edad fértil con un útero tabicado
Pregunta de la revisión
Los autores Cochrane deseaban conocer si la resección histeroscópica del tabique (extirpación quirúrgica del tabique) mejora las posibilidades de un nacido vivo en las mujeres con un útero tabicado, y si estos efectos beneficiosos superan las posibles complicaciones del procedimiento.
Antecedentes
Un útero tabicado es una anomalía congénita del útero (matriz), en la que el útero está dividido en dos cavidades. Las mujeres con útero tabicado tienen riesgo de sufrir subfertilidad, abortos espontáneos recurrentes y partos prematuros. Se cree que la extirpación quirúrgica del tabique mejora estos resultados, pero se desconoce la efectividad de este procedimiento quirúrgico.
Características de los estudios
Se examinaron los estudios de investigación publicados hasta mayo 2016. Fueron elegibles para inclusión los ensayos controlados aleatorizados que evaluaron el efecto sobre los resultados reproductivos de la resección histeroscópica del tabique en mujeres en edad fértil con un útero tabicado. En estos ensayos, las mujeres serían asignadas al azar a resección del tabique o a tratamiento expectante (ninguna cirugía). No hubo estudios para inclusión, por lo que no es posible informar sobre las fuentes de financiación.
Resultados clave
Al igual que en la versión 2011 de esta revisión, no se identificaron ensayos controlados aleatorizados publicados para su inclusión en esta actualización.
Authors' conclusions
Background
Description of the condition
The uterus originates from the paramesonephric, or Müllerian ducts. In a septate uterus, the Müllerian ducts have not fused during the period of embryologic development. A septate uterus is defined as a uterus with a division of the uterine cavity (septum) without any restrictions to the length of the septum, according to the new ESHRE (European Society of Human Reproduction and Embryology)/ESGE (European Society for Gynaecological Endoscopy) classification system for female genital tract congenital anomalies. The external contour of the uterus should not have an indentation (Grimbizis 2013) (Figure 1). Septate uterus is the most common uterine anomaly, accounting for 35% of all identified uterine anomalies.

The ESHRE/ESGE classification system for female genital congenital anomalies (Grimbizis 2013).
A septate uterus is associated with reduced fertility (risk ratio (RR) 0.86, 95% confidence interval (CI) 0.77 to 0.96), increased miscarriage rates (RR 2.9, 95% CI 2.0 to 4.1), and increased preterm births (RR 2.1, 95% CI 1.5 to 3.1) (Chan 2011).
Description of the intervention
Traditionally, the uterine septum was resected by a laparotomic hysterotomy (Paradisi 2014), but since the introduction of hysteroscopic septum resection in 1970, the latter approach is considered first‐line therapy (Edström 1970). Possible complications of a hysteroscopic septum resection are bleeding, perforation of the uterus, postoperative intrauterine adhesions, and uterine rupture in subsequent pregnancies (Valle 2013). Even so, hysteroscopic septum resection is still common practice in many countries (Paradisi 2014). This procedure is assumed to be effective based on non‐randomised and mainly retrospective trials. These studies are at high risk of bias due to their mainly before/after design, with the same group of women serving as their own controls. Before‐after comparisons will always favour the intervention (Christiansen 2005; Mastenbroek 2006).
How the intervention might work
The pathophysiology behind poor reproductive outcomes in women with a septate uterus is unknown. Earlier studies asserted that the septum is avascular and mainly consists of fibrous tissue (Fayez 1986; March 1983). The main cause of impaired fertility in women with a septate uterus was considered to be a disturbed implantation. More recent studies suggest that the septum consists of normal endometrium and myometrium, and resembles the uterine wall (Candiani 1983; Sparac 2001; Zreik 1998). It is unclear whether restoring normal anatomy also restores normal function, and thereby improves fertility outcomes in women who wish to conceive.
Why it is important to do this review
Various studies (mainly retrospective) have assessed the efficacy of the hysteroscopic removal of the uterine septum and restoration of uterine anatomy. Observational studies report large improvements in likelihood of pregnancy in a before/after septum resection study design (88% miscarriages before and 5.9% after surgery) (Homer 2000). However, these results are prone to bias as the prognosis without the intervention is usually good. (Christiansen 2005). As a consequence, we currently do not know whether a septum resection increases the chances of a live birth and whether this outweighs the possible complications of the procedure.
Objectives
To determine whether hysteroscopic septum resection in women of reproductive age with a septate uterus improves live birth rates and to assess the safety of the procedure.
Methods
Criteria for considering studies for this review
Types of studies
Truly randomised controlled trials (RCTs) were eligible for inclusion. We excluded quasi‐ or pseudo‐RCTs, as they are associated with a high risk of bias (Vail 2003).
Types of participants
Women of reproductive age with a septate uterus, defined as a uterus with a division of the uterine cavity (septum), without any restrictions to the length of the septum. We excluded women diagnosed with a septate uterus, with abnormal bleeding and who might not necessarily wish to conceive.
Types of interventions
Hysteroscopic septum resection of the septate uterus versus expectant management.
Types of outcome measures
Primary outcomes
-
Effectiveness: live birth rate, defined as the birth of a live baby after 24 completed weeks of gestation
-
Safety: surgical complications following septum resection: uterine perforation, fluid overload, endometritis, and repeat surgery
Secondary outcomes
-
Ongoing pregnancy
-
Clinical pregnancy
-
Pregnancy complications; miscarriage, placental abruption, uterine rupture, preterm birth and mode of delivery (vaginal versus caesarean section), postoperative intrauterine adhesions, neonatal morbidity and mortality
Search methods for identification of studies
We searched for all relevant published and unpublished RCTs of hysteroscopic septum resection versus expectant management in women of reproductive age with a septate uterus using a defined search strategy, without language restriction. We searched relevant studies from inception up to 30 May 2016. We carried out all searches in consultation with the Cochrane Gynaecology and Fertility Group Information Specialist.
Electronic searches
We searched the following electronic databases.
-
Cochrane Gynaecology and Fertility Group (CGF) Specialised Register (from inception to 30 May 2016) (Appendix 1),
-
Cochrane Central Register of Studies (CRSO) (from inception May 2016) (Appendix 2)
-
MEDLINE,(from 1946 to 30 May 2016) (Appendix 3)
-
Embase,(from 1974 to 30 May 2016) (Appendix 4)
-
PsycINFO (from 1806 to 30 May 2016) (Appendix 5)
-
CINAHL from 1982 to 30 May 2016) (Appendix 6)
The MEDLINE search was combined with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials, described in Section 6.4.11 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
The Embase and PsycINFO searches were combined with trial filters developed by the Scottish Intercollegiate Guidelines Network (SIGN) (www.sign.ac.uk/mehodology/filters.html#random).
We used no language or date restriction in these searches.
In addition, we searched the following sources, all to 5 July 2016
-
Trial registers for ongoing and registered trials: ClinicalTrials.gov, which is a service of the US National Institutes of Health (clinicaltrials.gov/ct2/home) and the World Health Organization International Clinical Trials Registry Platform (WHO ICTRP) (www.who.int/trialsearch/Default.aspx)(Appendix 7; Appendix 8)
-
The Cochrane Library (www.cochrane.org/index.htm) for the Database of Abstracts of Reviews of Effects (DARE) (Appendix 9)
-
ProQuest Dissertations & Theses for unpublished dissertations and theses (Appendix 10)
-
OpenGrey for unpublished literature from Europe (http://www.opengrey.eu/) (Appendix 11)
-
LILACS database (regional.bvsalud.org/php/index.php?lang=en) (Appendix 12)
-
Google and PubMed for any recent trials that have not yet been indexed in MEDLINE (Appendix 13; Appendix 14)
Searching other resources
-
Reference lists from reviews and trials
-
Handsearching of appropriate journals (in liaison with the CGFG Information Specialist)
-
Conference abstracts on the Web of Science (www.wokinfo.com/)
Data collection and analysis
Selection of studies
Two review authors (JR and CK) screened titles and abstracts of all identified studies against the inclusion criteria. We retrieved all potentially relevant articles in full text. We attempted to obtain translations of non‐English language papers sufficient to judge their suitability for inclusion. A list of ongoing studies is provided in the Characteristics of ongoing studies. We communicated with the contact persons of these trials for missing information.
In future updates when eligible studies are available, two review authors will independently examine full‐text articles for compliance with the inclusion criteria and select studies that fulfil these criteria. Any difference of opinion regarding trials for inclusion will be resolved by consensus or by discussion with a third review author.
Data extraction and management
We planned that two review authors would independently extract the data from each study using a data extraction form that the review authors had designed and pilot tested. Should studies have had multiple publications, we would have used the main trial report as the reference and additional details supplemented from secondary papers. Review authors would have corresponded with study investigators in order to resolve any data queries, as required. Two review authors would have independently extracted the data. Any disagreements between the review authors would have been resolved by a third review author.
Assessment of risk of bias in included studies
We planned that two review authors (JR and CK) would independently assess the included studies for risk of bias using the Cochrane 'Risk of bias' assessment tool. Disagreements would have been resolved by discussion or by consulting a third review author (MG). We planned to assess selection (random sequence generation and allocation concealment); performance (blinding of participants and personnel); detection (blinding of outcome assessors); attrition (incomplete outcome data); reporting (selective reporting); and other potential biases such as differences in demographic characteristics between treatment groups at baseline. We planned to describe all judgements and present the conclusions in the 'Risk of bias' table.
(1) Random sequence generation
We planned to describe for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We would assess the method as:
-
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
-
unclear risk of bias.
(2) Allocation concealment
We planned to describe for each included study the method used to conceal allocation to interventions prior to assignment and would assess whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We would assess the methods as:
-
low risk of bias (e.g. web or telephone randomisation; consecutively numbered, sealed, opaque envelopes);
-
high risk of bias (open list of random allocation; unsealed or non‐opaque envelopes; alternation; date of birth);
-
unclear risk of bias.
(3.1) Blinding of participants and personnel
Lack of blinding is unlikely to introduce bias, so we planned to assess methods as at low risk of bias.
(3.2) Blinding of outcome assessment
We planned to describe the methods used for each included study, if any, to blind outcome assessors from knowledge of which intervention a participant received. We planned to assess blinding separately for different outcomes or classes of outcomes.
We planned to assess the methods used to blind outcome assessment as low, high, or unclear risk of bias.
(4) Incomplete outcome data
We planned to describe for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We planned to state whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total number of randomised participants), reasons for attrition or exclusion were reported, and whether missing data were balanced across groups or were related to outcomes.
We planned to assess methods as:
-
low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
-
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; 'as treated' analysis done with substantial departure of intervention received from that assigned at randomisation);
-
unclear risk of bias.
(5) Selective reporting
We planned to describe for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We planned to assess the methods as:
-
low risk of bias, where it is clear that all of the study’s prespecified outcomes and all expected outcomes of interest to the review have been reported, and the outcomes of interest have been prespecified in a prospectively registered protocol;
-
high risk of bias, where not all of the study’s prespecified outcomes were reported; one or more reported primary outcomes were not prespecified; outcomes of interest were reported incompletely and so cannot be used; the study failed to include results of a key outcome that would have been expected to have been reported;
-
unclear risk of bias.
(6) Other bias (checking for bias due to problems not covered by (1) to (5) above)
We planned to describe for each included study any important concerns we had about other possible sources of bias.
Measures of treatment effect
We planned to perform statistical analyses in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We would report only dichotomous outcomes, and for such outcomes use the numbers of events in the control and intervention groups of each study to calculate Mantel‐Haenszel odds ratios in a fixed‐effect model. We planned to present 95% confidence intervals for all outcomes and use Review Manager 5 software (RevMan 2014) for statistical analysis. We planned to translate primary outcomes to absolute risks for reporting purposes.
We planned to use a random‐effects model in the case of an I2 statistic above 50%.
Unit of analysis issues
The primary analysis would be per woman randomised. We would have counted multiple live births (for example twins or triplets) as one live birth event.
Dealing with missing data
We planned to analyse the data on an intention‐to‐treat basis. If important data were missing, we would attempt to obtain the missing data by contacting the original investigators. If this was not possible, we would impute the missing data with replacement values for the primary outcome in a sensitivity analysis.
Assessment of heterogeneity
We planned to consider whether the clinical and methodological characteristics of the included studies were sufficiently similar for meta‐analysis to provide a clinically meaningful summary. We would assess statistical heterogeneity using the I2 statistic. We would consider an I2 measurement greater than 50% as indicating substantial heterogeneity (Higgins 2011). If we detected substantial heterogeneity, we would explore possible explanations for it in sensitivity analyses.
Assessment of reporting biases
We planned to minimise the impact of reporting biases by ensuring a comprehensive search for eligible studies while being alert to duplication of data. If there were 10 or more studies in an analysis, we would use a funnel plot to explore the possibility of small‐study effects, since there is a tendency for estimates of the intervention effect to be more beneficial in smaller studies.
Data synthesis
If trials were sufficiently similar, we would combine the data using a fixed‐effect model.
Subgroup analysis and investigation of heterogeneity
We planned to perform a subgroup analysis by participant clinical characteristics (women with recurrent miscarriage, women with subfertility or other complaints). We anticipated heterogeneity between subgroups and planned to discuss possible reasons for it.
Sensitivity analysis
If data from more than four studies were available, we planned to perform sensitivity analyses. We would assess the influence of risk of bias on effect size by removing trials deemed to be at high risk of bias. Studies with high risk of bias would include those that did not use an intention‐to‐treat approach and those that had inadequate concealment of allocation. We would repeat analyses using a random‐effects model to explore whether different conclusions were reached. We would report sensitivity analyses for the primary outcomes only.
Overall quality of the body of evidence: Summary of findings table
We planned to prepare a 'Summary of findings' table using GRADEpro (GRADEpro GDT 2014) and Cochrane methods (Higgins 2011). We planned that this table would evaluate the overall quality of the body of evidence for the main review outcomes (live birth rate, ongoing pregnancy, adverse effects) for the main review comparison (septum resection versus expectant management). We planned to assess the quality of the evidence using GRADE criteria: risk of bias, consistency of effect, imprecision, indirectness, and publication bias. We planned that two review authors would independently make judgements about evidence quality (high, moderate, low, or very low), with disagreements resolved by discussion, and that judgements would be justified, documented, and incorporated into the reporting of results for each outcome.
We planned to extract study data, format our comparisons in data tables, and prepare a 'Summary of findings' table before writing the results and conclusions of our review.
Results
Description of studies
We found no RCTs assessing whether hysteroscopic septum resection influences reproductive outcomes in women of reproductive age with a septate uterus.
Results of the search
After removal of duplicates and we identified 78 articles (Figure 2).
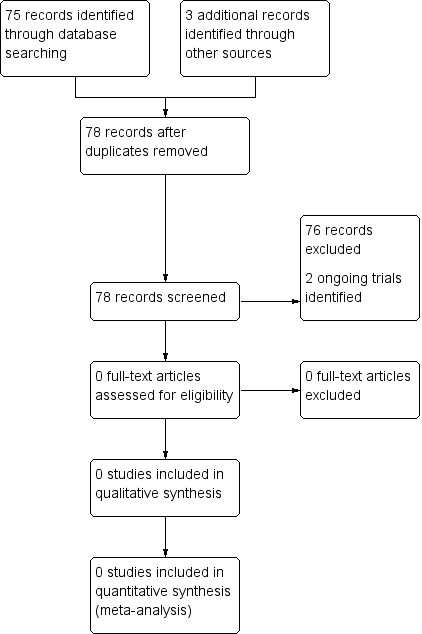
Study flow diagram.
Included studies
None.
Ongoing studies
We found two ongoing trials in our search of the WHO ICTRP: the TRUST study, NTR1676, and the Pilot randomised controlled trial of hysteroscopic septal resection (ISRCTN28960271). Results of neither trial have been published.
Excluded studies
Not applicable.
Risk of bias in included studies
Not applicable.
Effects of interventions
Not applicable.
Discussion
Summary of main results
Consistent with the first issue of the review in 2011, we did not find any RCTs comparing hysteroscopic septum resection with expectant management in women of reproductive age with a septate uterus in this update.
Potential biases in the review process
The search was systematic and thorough, therefore the risk of introducing bias was low.
Agreements and disagreements with other studies or reviews
Over the years, nine comparative studies have been published. These studies describe miscarriage, pregnancy, or live birth rate in women with a septate uterus who consented to hysteroscopic septum resection, compared with women who chose expectant management. Three of these studies showed a significantly higher pregnancy rate in women with a septate uterus who were treated with surgery (Gaucherand 1994; Pang 2011; Tonguc 2011), while six found no significant difference between the groups (Heinonen 1997; Kirk 1993; Lin 2009; Maneschi 1991; Sugiura‐Ogasawara 2013; Valli 2004).
In conclusion, there is no evidence that hysteroscopic septum resection improves reproductive outcome in women with a septate uterus and outweighs the possible complications of the procedure.

The ESHRE/ESGE classification system for female genital congenital anomalies (Grimbizis 2013).

Study flow diagram.

