Terapia del espejo para mejorar la motricidad después de un accidente cerebrovascular
Información
- DOI:
- https://doi.org/10.1002/14651858.CD008449.pub3Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 11 julio 2018see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Accidentes cerebrovasculares
- Copyright:
-
- Copyright © 2018 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
Holm Thieme (HT), Christian Dohle (CD), and Nadine Morkisch (NM) were involved in all stages of the review and contributed to the conception and design of the review.
Bernhard Borgetto (BB) contributed to the conception and design of the review and was involved in interpreting the results.
Jan Mehrholz (JM) was involved in methodological planning and conducting the review, statistical analysis of outcome data, and interpreting the results. Johann Behrens (JB) and Marcus Pohl (MP) were involved in extracting data, assessing the methodological quality of selected studies, and interpreting the results.
All authors approved the protocol and the final review.
Sources of support
Internal sources
-
Erste Europäische Schule für Physiotherapie, Ergotherapie und Logopädie, Klinik Bavaria Kreischa, Germany.
-
Klinik Bavaria Kreischa, Germany.
-
SRH Hochschule Gera, Germany.
-
Martin‐Luther‐Universität Halle‐Wittenberg, Germany.
-
Median Klinik Berlin‐Kladow, Germany.
External sources
-
BMBF, Germany.
The research is funded by the Bundesministerium für Bildung und Forschung (01KG1025).
-
BMBF, Germany.
This research is funded by the Bundesminiterium für Bildung und Forschung (01KG1514).
Declarations of interest
Holm Thieme (HT) is an author of an included study on the effect of mirror therapy after stroke. He was not involved in checking this trial for eligibility, extracting data or assessing the methodological quality of this study. He has received and will receive honorarium for presentations and seminars on mirror therapy.
Christian Dohle (CD) is author of two included studies on the effect of mirror therapy after stroke. He was not involved in checking these trials for eligibility, extracting data or assessing the methodological quality of the studies. He has received and will receive honorarium for presentations and seminars on mirror therapy.
Christian Dohle (CD) and Nadine Morkisch (NM) are authors of corresponding therapy manuals (Bieniok 2011; Morkisch 2015).
Jan Mehrholz: None known
Marcus Pohl: Marcus Pohl (MP) is an author of an included study on the effect of mirror therapy after stroke. He was not involved in checking this trial for eligibility, extracting data or assessing the methodological quality of this study.
Johann Behrens: Johann Begrens (JB) is an author of an included study on the effect of mirror therapy after stroke. He was not involved in checking this trial for eligibility, extracting data or assessing the methodological quality of this study.
Bernhard Borgetto: None known
Acknowledgements
We thank Brenda Thomas and Josh Cheyne for their help with developing and running the search strategies, and Hazel Fraser for providing us with relevant trials from the Cochrane Stroke Group Trials Register and giving us helpful support. We also thank Gaby Voigt for providing us with many helpful studies and Luara Ferreira dos Santos for performing literature searches. We thank all authors and investigators who provided us with additional information and data on their studies. Finally, we owe thanks to the reviewers of this review who provided several helpful suggestions, especially Odie Geiger as Consumer Reviewer.
Version history
| Published | Title | Stage | Authors | Version |
| 2018 Jul 11 | Mirror therapy for improving motor function after stroke | Review | Holm Thieme, Nadine Morkisch, Jan Mehrholz, Marcus Pohl, Johann Behrens, Bernhard Borgetto, Christian Dohle | |
| 2012 Mar 14 | Mirror therapy for improving motor function after stroke | Review | Holm Thieme, Jan Mehrholz, Marcus Pohl, Johann Behrens, Christian Dohle | |
| 2010 Apr 14 | Mirror therapy for improving motor function after stroke | Protocol | Holm Thieme, Jan Mehrholz, Marcus Pohl, Christian Dohle | |
Differences between protocol and review
We added the outcome 'motor impairment' for this update and separated outcome measures for motor function and motor impairment.
We undertook a new subgroup analysis: subacute versus chronic stage after stroke: the cut‐off point between both subgroups was six months after stroke onset.
We added a further database for searching ongoing studies: International Clinical Trials Registry Platform (ICTRP).
We had previously planned to perform a subgroup analysis comparing studies that included participants with different severities of motor impairment. Based on the baseline data for motor function, we were not able to clearly differentiate studies based on this criterion. Most studies included participants with mixed severities of motor impairments. Due to these problems of differentiation, we decided not to do this subgroup analysis.
Two studies only included people after stroke with a diagnosis of CRPS‐type I, which might have influenced the effects of the intervention (Cacchio 2009a; Cacchio 2009b). We therefore performed a post hoc sensitivity analysis by removing these studies; this was not planned in the protocol.
We only included studies with a minimum amount of 50% mirror therapy in the experimental intervention.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Adult; Aged; Humans; Middle Aged;
PICO
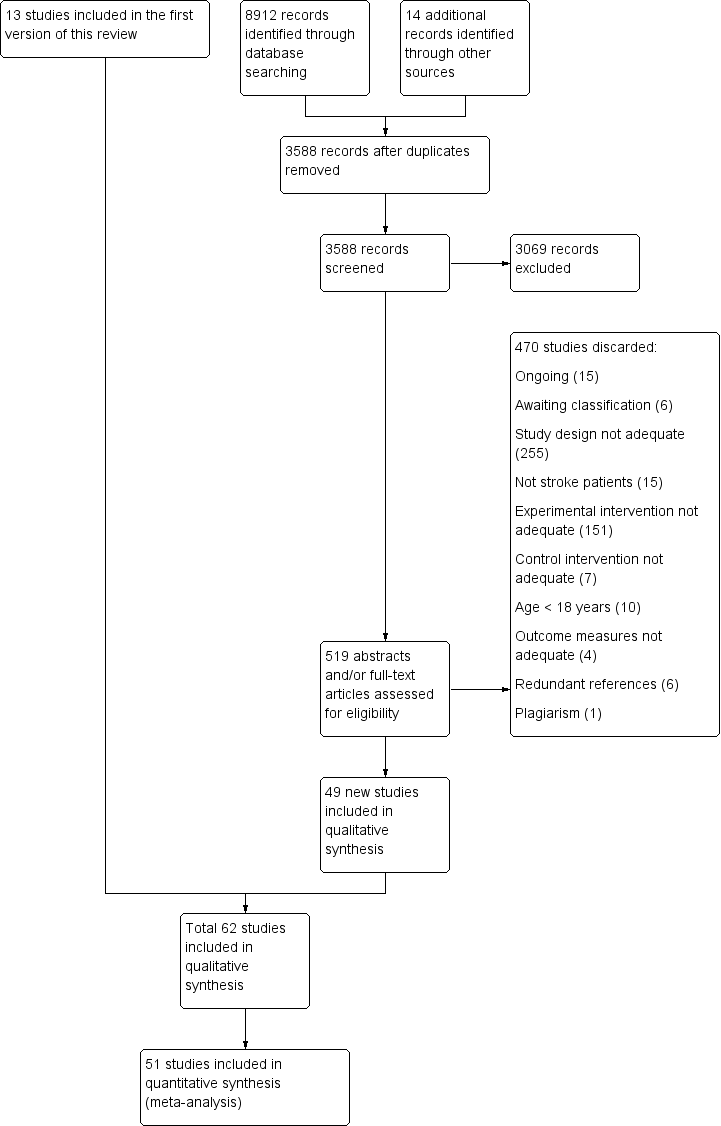
Study flow diagram of updated search and selection process

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
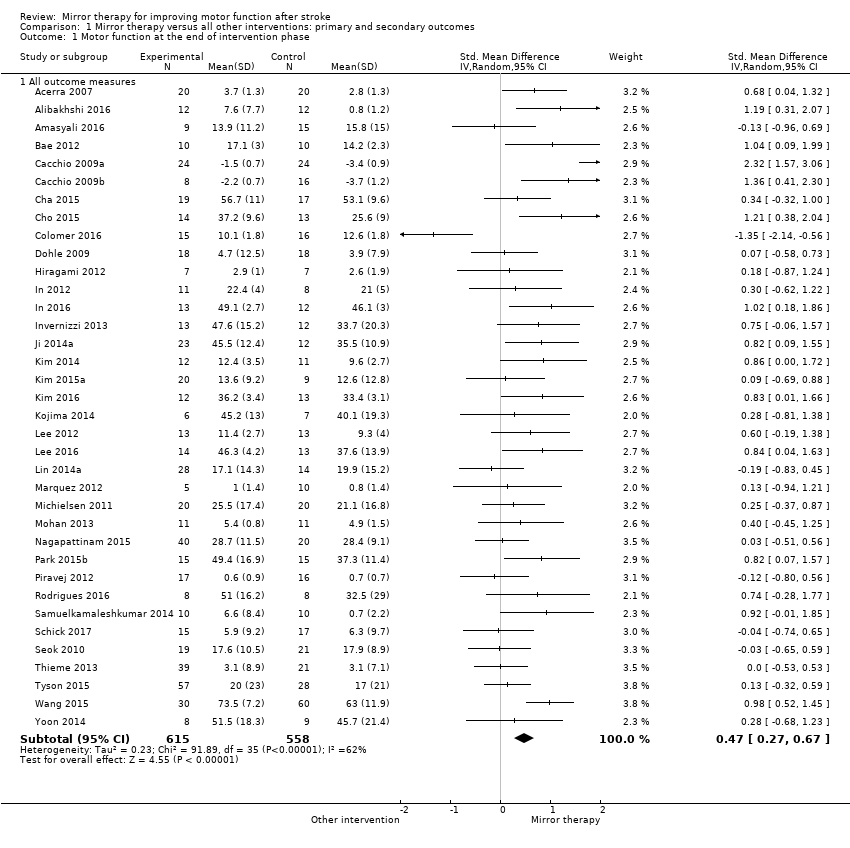
Comparison 1 Mirror therapy versus all other interventions: primary and secondary outcomes, Outcome 1 Motor function at the end of intervention phase.
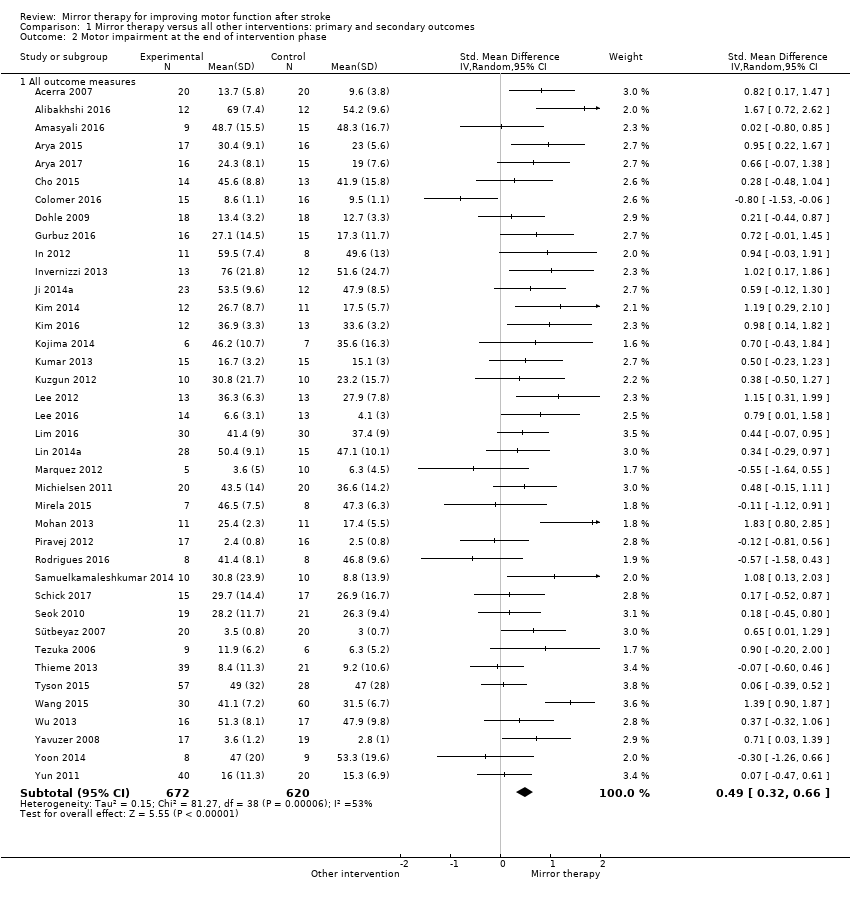
Comparison 1 Mirror therapy versus all other interventions: primary and secondary outcomes, Outcome 2 Motor impairment at the end of intervention phase.

Comparison 1 Mirror therapy versus all other interventions: primary and secondary outcomes, Outcome 3 Fugl‐Meyer Assessment upper extremity at the end of intervention phase.

Comparison 1 Mirror therapy versus all other interventions: primary and secondary outcomes, Outcome 4 Activities of daily living at the end of intervention phase.

Comparison 1 Mirror therapy versus all other interventions: primary and secondary outcomes, Outcome 5 Pain at the end of intervention phase.

Comparison 1 Mirror therapy versus all other interventions: primary and secondary outcomes, Outcome 6 Visuospatial neglect at the end of intervention.
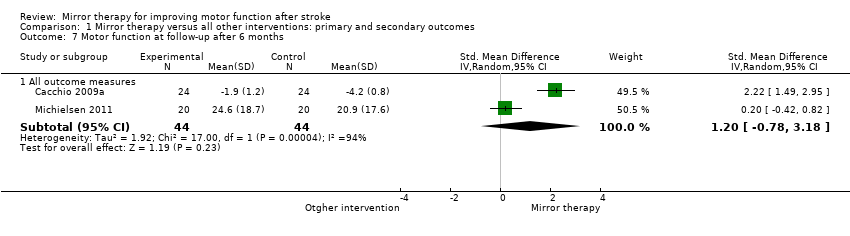
Comparison 1 Mirror therapy versus all other interventions: primary and secondary outcomes, Outcome 7 Motor function at follow‐up after 6 months.
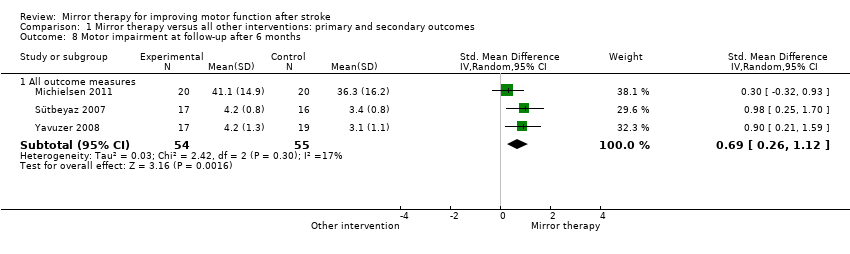
Comparison 1 Mirror therapy versus all other interventions: primary and secondary outcomes, Outcome 8 Motor impairment at follow‐up after 6 months.

Comparison 1 Mirror therapy versus all other interventions: primary and secondary outcomes, Outcome 9 Dropouts at the end of intervention phase.

Comparison 2 Subgroup analysis: upper versus lower extremity, Outcome 1 Motor function at the end of intervention.

Comparison 3 Subgroup analysis: sham intervention (covered mirror) versus other intervention (unrestricted view), Outcome 1 Motor function at the end of intervention phase.

Comparison 4 Subgroup analysis: subacute versus chronic stage after stroke, Outcome 1 Motor function at the end of intervention phase.
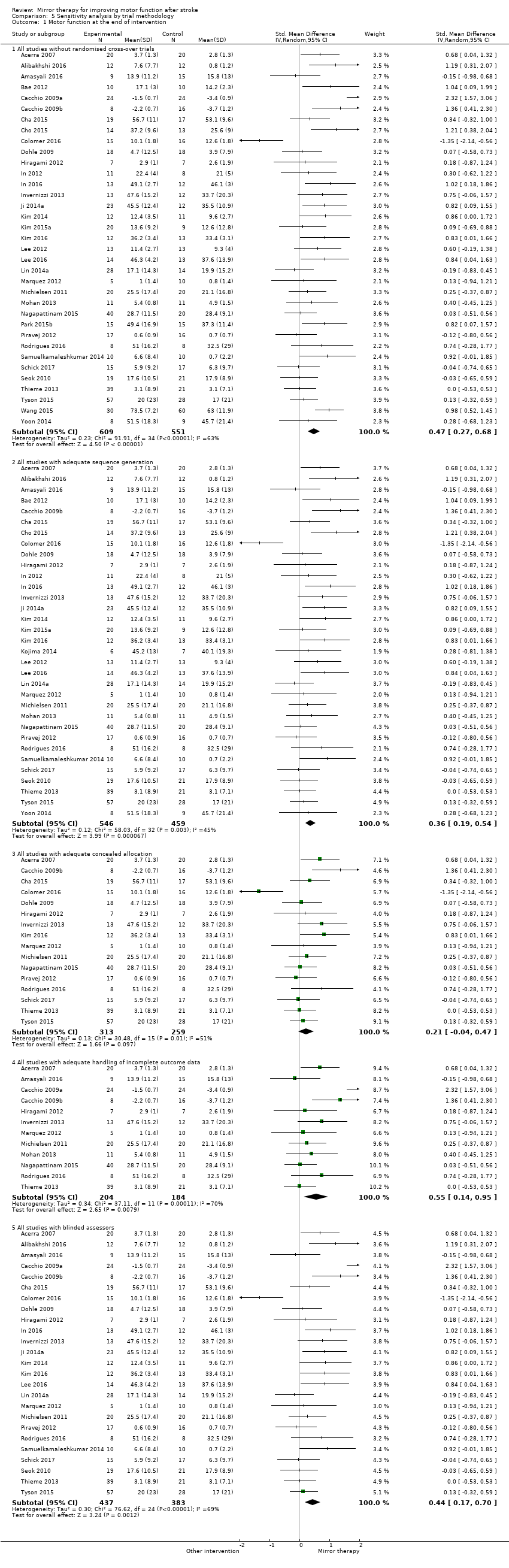
Comparison 5 Sensitivity analysis by trial methodology, Outcome 1 Motor function at the end of intervention.

Comparison 5 Sensitivity analysis by trial methodology, Outcome 2 Motor impairment at the end of intervention.

Comparison 6 Post hoc sensitivity analysis removing studies that only included participants with CRPS after stroke. Subgroup analysis: pain without complex regional pain syndrome (CRPS), Outcome 1 Pain at the end of intervention.
| Mirror therapy compared to all other interventions: primary and secondary outcomes for improving motor function after stroke | |||||
| Participants: people with paresis of the upper or lower limb, or both, caused by stroke Setting: inpatient and outpatient Intervention: mirror therapy Control: no treatment, placebo or sham therapy, or other treatments for improving motor function and motor impairment after stroke | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | № of participants | Quality of the evidence | Comment | |
| Assumed risk | Corresponding risk | ||||
| Control | Mirror therapy versus all other interventions | ||||
| Motor function at the end of intervention phase: all outcome measures | The mean motor function at the end of intervention phase ‐ all studies in the control groups was NA | The mean motor function at the end of intervention phase ‐ all studies in the intervention groups was 0.47 SDs higher (0.27 to 0.67 higher) | 1173 | ⊕⊕⊕⊝ | SMD 0.47, 95% CI 0.27 to 0.67; as a rule of thumb, 0.2 SD represents a small difference, 0.5 a moderate, and 0.8 a large difference |
| Motor impairment at the end of intervention phase: all outcome measures | The mean motor impairment at the end of intervention phase ‐ all studies in the control groups was NA | The mean motor impairment at the end of intervention phase ‐ all studies in the intervention groups was 0.49 SDs higher (0.32 to 0.66 higher) | 1292 | ⊕⊕⊕⊝ Moderatea | SMD 0.49, 95% CI 0.32 to 0.66; as a rule of thumb, 0.2 SD represents a small difference, 0.5 a moderate, and 0.8 a large difference |
| Fugl‐Meyer Assessment upper extremity at the end of intervention phase | The mean Fugl‐Meyer Assessment score at the end of intervention phase ‐ all studies in the control groups was NA | The mean Fugl‐Meyer Assessment score at the end of intervention phase ‐ all studies in the intervention groups was 4.32 pointshigher (2.46 to 6.19 higher) | 898 | ⊕⊕⊝⊝ | MD 4.32, 95% CI 2.46 to 6.19; the minimum important difference is approximately 5.25 |
| Activities of daily living at the end of intervention phase: all studies | The mean activities of daily living at the end of intervention phase ‐ all studies in the control groups was NA | The mean activities of daily living at the end of intervention phase ‐ all studies in the intervention groups was 0.48 SDs higher (0.29 to 0.67 higher) | 622 | ⊕⊕⊕⊝ | SMD 0.48, 95% CI 0.30 to 0.65; as a rule of thumb, 0.2 SD represents a small difference, 0.5 a moderate, and 0.8 a large difference |
| Pain at the end of intervention phase: all studies | The mean pain at the end of intervention phase ‐ all studies in the control groups was NA | The mean pain at the end of intervention phase ‐ all studies in the intervention groups was 0.89 SDs lower (1.67 to 0.11 lower) | 248 | ⊕⊕⊝⊝ | SMD −0.89, 95% CI −1.67 to −0.11; as a rule of thumb, 0.2 SD represents a small difference, 0.5 a moderate, and 0.8 a large difference |
| Pain at the end of intervention phase after excluding studies with CRPS | The mean pain at the end of intervention phase ‐ studies without CRPS in the control groups was NA | The mean pain at the end of intervention phase ‐ studies without CRPS in the intervention groups was 0.23 SDs lower (0.53 lower to 0.08 higher) | 176 (4 RCTs) | ⊕⊕⊕⊝ | SMD −0.23, 95% CI −0.53 to 0.08; as a rule of thumb, 0.2 SD represents a small difference, 0.5 a moderate, and 0.8 a large difference |
| Visuospatial neglect at the end of intervention: all studies | The mean visuospatial neglect at the end of intervention phase ‐ all studies in the control groups was NA | The mean visuospatial neglect at the end of intervention phase ‐ all studies in the intervention groups was 1.06SDs higher (0.10 lower to 2.23 higher) | 175 | ⊕⊕⊝⊝ | SMD 1.06, 95% CI −0.10 to 2.23; as a rule of thumb, 0.2 SD represents a small difference, 0.5 a moderate, and 0.8 a large difference |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| aDowngraded due to several ratings in one or more items with high or unknown risk of bias. | |||||
| Study ID | Mean age | Sex | Side of paresis | Time since stroke | Type of stroke | |||
| Years | Women | Men | Left | Right | Mean time | Ischaemic | Haemorrhagic | |
| 68 | 22 | 18 | 16 | 24 | 5.3 days | 40 | 0 | |
| 50.9 | 9 | 15 | 15 | 9 | n/r | n/r | n/r | |
| 58.2 | 4 | 5 | 8 | 1 | 4.8 years | n/r | n/r | |
| 58.8 | 11 | 13 | 8 | 16 | 5.3 months | 24 | 0 | |
| 45.6 | 8 | 25 | 7 | 26 | 12.9 months/12.3 months. | 17 | 16 | |
| 46.4 | 6 | 30 | 16 | 20 | 15.9 months | 17 | 9 | |
| 53.9 | 7 | 13 | 13 | 7 | 4.6 months | 9 | 11 | |
| n/r | n/r | n/r | n/r | n/r | n/r | n/r | n/r | |
| 58.4 | 26 | 22 | 34 | 14 | 5 months | 35 | 13 | |
| 62 | 13 | 11 | 15 | 9 | 15.7 months | 19 | 5 | |
| 58.7 | 17 | 19 | n/r | n/r | 1.8 months | n/r | n/r | |
| 59.3 | 12 | 15 | 14 | 13 | 13.2 months/15.5 months | 17 | 10 | |
| 53.5 | 5 | 26 | 24 | 7 | 551 days | 23 | 8 | |
| n/r | n/r | n/r | n/r | n/r | n/r | n/r | n/r | |
| 56.5 | 10 | 26 | 25 | 11 | 27 days | 48 | 0 | |
| n/r | 3 | 3 | n/r | n/r | n/r | n/r | n/r | |
| 60.9 | 14 | 17 | 14 | 17 | 44.3 days | 25 | 6 | |
| 67.5 | 6 | 8 | 6 | 8 | 47 days | 9 | 5 | |
| 63.9 | 8 | 11 | 9 | 10 | 14.1 months | 10 | 9 | |
| 55.9 | 10 | 15 | 13 | 12 | 13.1 days | 16 | 9 | |
| 66.6 | 9 | 17 | 13 | 13 | 23 days | 26 | 0 | |
| 52.6 | 13 | 22 | 14 | 21 | 8.9 months | 19 | 16 | |
| 64.1 | 24 | 43 | 35 | 32 | 32.3 days | 28 | 39 | |
| 55.8 | 9 | 14 | 13 | 10 | 34.5 days | 14 | 9 | |
| 57.7 | 9 | 20 | 20 | 9 | 404.4 days | 14 | 15 | |
| 49.1 | 9 | 16 | 16 | 9 | n/r | 8 | 17 | |
| 69.1 | 3 | 10 | 5 | 8 | 78.8 days | 10 | 3 | |
| 57.3 | 8 | 22 | n/r | n/r | n/r | n/r | n/r | |
| 61.4 | 10 | 10 | 10 | 10 | n/r | n/r | n/r | |
| 57.1 | 11 | 15 | 11 | 15 | 3.6 months | n/r | n/r | |
| 54.7 | 13 | 14 | 8 | 19 | 39.6 months | 8 | 20 | |
| 64.9 | 21 | 39 | 31 | 29 | 52 days | 19 | 41 | |
| 55 | 11 | 32 | 22 | 21 | 19.6 months | 20 | 28 | |
| n/r | n/r | n/r | n/r | n/r | n/r | n/r | n/r | |
| 68.7 | 8 | 7 | 9 | 6 | 24.3 days | 10 | 5 | |
| 57 | 20 | 20 | 28 | 12 | 4.6 years | 28 | 12 | |
| 57.5 | 8 | 7 | 5 | 10 | 53.2 days | 15 | 0 | |
| 63 | 10 | 12 | 6 | 16 | 6.4 days | 14 | 8 | |
| 53.5 | 4 | 4 | 4 | 4 | 4.5 months | n/r | n/r | |
| 44.9 | 20 | 40 | n/r | n/r | 4.2 months | 60 | 0 | |
| 63.4 | 20 | 28 | 37 | 11 | 2 days | 26 | 22 | |
| 56.3 | 13 | 17 | 14 | 16 | 20.9 months | 16 | 14 | |
| 60 | 15 | 15 | 17 | 13 | 8.2 months | 17 | 13 | |
| 56 | 19 | 21 | 25 | 15 | 7.2 months | 27 | 13 | |
| 58 | 9 | 21 | 3 | 27 | 5 months | 20 | 10 | |
| 56.3 | n/r | n/r | n/r | n/r | 83.9 days | n/r | n/r | |
| 57.5 | 6 | 10 | 11 | 5 | 34.8 months | 16 | 0 | |
| 73.4 | 10 | 6 | 8 | 8 | 9.5 months | 16 | 0 | |
| n/r | n/r | n/r | n/r | n/r | n/r | n/r | n/r | |
| 51.2 | 4 | 16 | 9 | 11 | 4.1weeks | 14 | 6 | |
| 63 | 13 | 19 | 15 | 17 | 50 days | 27 | 5 | |
| 51.4 | 22 | 18 | n/r | n/r | 4.0 months | n/r | n/r | |
| 63.4 | 17 | 23 | 27 | 13 | 3.7 months | 33 | 7 | |
| 63.7 | 9 | 6 | 6 | 9 | 32.7 days | n/r | n/r | |
| 67.2 | 25 | 35 | 37 | 23 | 45 days | 45 | 15 | |
| 64 | 34 | 60 | 56 | 38 | 29 days | 76 | 18 | |
| 64.9 | 40 | 50 | 39 | 51 | 63.7 days | 57 | 33 | |
| 54.2 | 10 | 23 | 18 | 15 | 20.6 months | 20 | 13 | |
| 63.3 | 17 | 19 | 21 | 19 | 5.5 months | 29 | 7 | |
| 57.8 | 10 | 16 | 15 | 11 | 22.7 days | 16 | 10 | |
| 63.3 | 21 | 39 | 31 | 29 | 25.8 days | 46 | 14 | |
| n/r | n/r | n/r | n/r | n/r | n/r | n/r | n/r | |
| n/r: not reported | ||||||||
| Study ID | Extremity | Mirror therapy variation | Control intervention | Type of movements | Minutes per session | Sessions per week | Total duration (weeks) | Total amount of therapy (minutes) | Setting |
| Upper extremity | Bilateral activities | Bilateral activities; covered mirror | Functional motor tasks (i.e. with objects); motor co‐ordination tasks; sensory discrimination tasks; grip strength; active range of motion | 20 to 30 | 7 | 2 | 280 ‐ 420 | Inpatient hospital | |
| Upper extremity | Bilateral activities | Bilateral activities without mirror | n/r | 30 | 5 | 3 | 450 | Inpatient hospital | |
| Upper extremity | Bilateral activities | Bilateral activities; transparent plastic between limbs | Proximal and distal movements | 15 (2 times a day) | 12 | 4 (1st period) | 720 | n/r | |
| Upper extremity | Activities of the unaffected limb | 1. EMG‐triggered electrostimulation; | Wrist, hand flexion, extension and forearm circumduction, and supination–pronation | 30 | 5 | 3 | 450 | Inpatient rehabilitation centre | |
| Upper extremity | Activities of the unaffected limb | Conventional therapy based on Brunnstrom and Bobath principles | Task‐based mirror therapy: finger dexterity, mass grasp/finger flexion, release/finger extension, wrist dorsiflexion, | 45 | 5 | 8 | 1800 | Inpatient hospital, home after discharge | |
| Lower extremity | Activities of the unaffected limb | Conventional motor therapy based on neurophysiological approaches | Activity‐based MT: ball‐rolling, rocker‐board and pedaling | 60 | n/r | 3 ‐ 4 (30 session) | 1800 | Inpatient rehabilitation centre | |
| Upper extremity | Bilateral activities | Activities of the non‐paretic arm, without mirror | Flexion/extension of the shoulder, radial/ulnar deviation and pro‐/supination of the forearm, flexion/extension of the fingers | 30 | 5 | 4 | 600 | Inpatient rehabilitation centre | |
| Upper and lower extremity | Activities of the unaffected limbs | Routine programme (physiotherapy and neuromuscular stimulation) | Range of motion of the healthy limbs | 30 | 5 | 4 | 600 | n/r | |
| Upper extremity | Activities of the unaffected limb | Activities of the unaffected limb; covered mirror | Flexion/extension of shoulder, elbow and wrist; prone/supination forearm | 30 1st 2 weeks; 60 last 2 weeks | 5 | 4 | 900 | Inpatient and outpatient rehabilitation centre | |
| Upper extremity | Activities of the unaffected limb | Activities of the unaffected limb; covered mirror (control group 1); imagination of movements of the affected limb (control group 2) | Flexion/extension of shoulder, elbow and wrist; prone/supination forearm | 30 | Daily | 4 | 840 | Inpatient and outpatient rehabilitation centre | |
| Lower extremity | Activities of the unaffected limb + rTMS | Activities of the unaffected limb; covered mirror + rTMS | Flexing and extending the hip, knee, and ankle at a self‐selected speed under supervision but without additional verbal feedback | 20 | 5 | 4 | 400 | n/r | |
| Upper extremity | Activities of the unaffected limb + tDCS /anode attached over primary motor cortex | Activities of the unaffected limb; covered mirror + tDCS | Pronation, supination, flexion, and extension of both wrists, flexion and extension of the fingers, and flexion and extension of the elbows (10 sets, 20 repetitions per motion and set, 2 min rest between sets) | 20 | 3 | 6 | 360 | n/r | |
| Upper extremity | Activities of the unaffected limb | Passive mobilisation of the affected limb | Flexion and extension of shoulder, pronation and supination of forearm, gross and fine motor movements of wrist, hand and fingers (also with objects) | 45 | 3 | 8 | 1080 | Outpatient rehabilitation centre | |
| Upper extremity | 10 Hz TMS applied by 8‐coil on the ipsilesional somatosensory cortex, followed by MT | TMS only | n/r | 30 | 3 | 4 | 360 | n/r | |
| Upper extremity | Bilateral activities | Bilateral activities; without mirror | Execution of arm, hand and finger postures | 30 | 5 | 6 | 900 | Inpatient rehabilitation centre | |
| Upper extremity | Bilateral and unilateral activities | Traditional occupational therapy | n/r | 30 | 5 | 6 | 900 | Home setting | |
| Upper extremity | Activities of the unaffected limb | Movements of the unaffected limb; covered mirror | Flexion and extension of wrist and finger | 20 | 5 | 4 | 400 | Inpatient rehabilitation centre | |
| Upper extremity | Bilateral activities | No additional therapy | Supination and eversion of the forearm, flexion and extension of the wrist and finger, grasp a block | 30 | 6 or 7 | 4 | 720 ‐ 840 | Inpatient Hospital | |
| Upper extremity | Bilateral activities; virtual mirror on a screen; arm projected by a camera | Bilateral activities; without mirror (screen was off) | 1st week: wrist flexion/ extension, forearm pro‐/supination, clenching and opening the hand, 2nd week gross motor tasks, 3rd and 4th week fine motor tasks; 3 sets of 10 repetitions, comfortable speed of movement, supervision of caregivers, using checklist | 30 | 5 | 4 | 600 | Inpatient rehabilitation centre | |
| Lower extremity | Uni‐ and bilateral activities; virtual mirror on the screen, leg projected by a camera | Uni‐ and bilateral activities; without mirror (screen was off) | 1st week: dorsiflexion and plantarflexion (lifting of the heel) of the unaffected ankle; adduction and abduction of forefoot and rear foot; and adduction and abduction of the hip (moving the knees inward and outward), 2nd week mimicked the movements (1st week) of the unaffected lower limb on the monitor with the affected lower limb, 3rd dorsiflexion, adduction and abduction of the unaffected ankle; plantar flexion, adduction and abduction of the ankle; and adduction and abduction of the hip; 4th week: complex movements and different tasks (remote control with up and down buttons); 3 sets of 10 repetitions, comfortable speed of movement, supervision of caregivers, using checklist | 30 | 5 | 5 | 600 | Inpatient rehabilitation centre | |
| Upper extremity | Movements of the unaffected limb | Movements of the unaffected limb; covered mirror | Flexion/extension of shoulder, elbow and wrist, pro‐ /supination of the forearm, self selected speed, no additional verbal feedback | 30 1st 2 weeks; 60 last 2 weeks | 5 | 4 | 900 | Inpatient rehabilitation centre | |
| Upper extremity | Experimental 1: MT: Movements of the unaffected limb + rTMS; Experimental 2: MT: Movements of the unaffected limb | Activities of the unaffected limb, covered mirror | Experimental 1: finger flexion and extension + 10Hz rTMS on lesioned hemisphere; | 15 | 5 | 6 | 450 | University hospital | |
| Lower extremity | Bilateral activities and activities of the unaffected limb | 4 control groups: (1) EMG triggered electrical muscle stimulation; (2) electrical muscle stimulation; (3) repetitive facilitation exercises; (4) passive and active‐assistive range of motion exercises | Dorsiflexion of the ankle joint, stepping over, and abduction/adduction of the hip joint) | 20 | 7 | 4 | 560 | Inpatient rehabilitation centre | |
| Upper extremity | Bilateral activities + FES | Bilateral activities + FES; covered mirror | Extension of wrist and fingers to lift of the hand from an FES switch, at the same time attempt to extend affected hand supported by electrical stimulation (20 Hz), pulse rate 300 μs, individual intensity for muscle contraction and complete extension | 30 | 5 | 4 | 600 | University hospital | |
| Upper extremity | Bilateral activities + FES | No additional therapy | 2 experimental groups: (1) EMG‐triggered FES (due to unaffected limb) of affected wrist extension + physiological and object‐related movements; (2) FES of affected wrist extension + physiological and object‐related movements | 30 | 5 | 4 | 600 | Inpatient rehabilitation centre | |
| Upper extremity | Activities of the unaffected limb | Conventional therapy | Arm bicycling, peg board exercise, skateboard‐supported exercises on a tabletop, donut on base putty kneading, double curved arch, bimanual placing cone, block stacking, graded pinch exercise, plastic cone stacking, shoulder curved arch | 30 | 5 | 4 | 300 | Outpatient hospital | |
| Upper extremity | Bilateral activities + EMTS | No additional therapy | Extension of wrist and fingers to reach EMG threshold on 50 ‐ 70% of maximum wrist extension, neuromuscular stimulation 10 seconds symmetrical biphasic pulses at 50 Hz, pulse width 200 μs, followed by 20 seconds of rest to assist full range of motion; bimanual wrist and finger extension during 'on' and 'off' period, difficulty of exercises dependent upon participants’ levels of functioning with regard to wrist and finger flexion and extension or thumb opposition | 20 (2 times a day) | 5 | 4 | 800 | Inpatient rehabilitation centre | |
| Lower extremity | Activities of the unaffected limb | No additional therapy | Flexion/ extension of the knee and ankle; self‐selected speed; under supervision | 2 times daily for 15 minutes | 5 | 2 | 300 | n/r | |
| Upper extremity | n/r | No additional therapy | Wrist extension | 4 times daily for 15 minutes | 5 | 4 | 1200 | n/r | |
| Upper extremity | Bilateral activities | No additional therapy | Lifting both arms, flexion/ extension of the elbow, pronation of the forearm, wrist extension, internal/ external rotation of the wrist, clenching and opening the fist, tapping on the table; self‐performed; supervision of a guardian | 2 times daily for 25 minutes | 5 | 4 | 1000 | Inpatient rehabilitation ward | |
| Lower extremity | Bilateral activities + NMES | Conventional therapy | Dorsiflexion movements of the ankle | n/r | 5 | 4 | n/r | Rehabilitation hospital | |
| Upper extremity | Bilateral activities | Bilateral activities, covered mirror | Task‐oriented MT: forearm pronation‐supination and wrist flexion/extension, finger flexion‐extension, counting numbers, tapping, and opposing; simple manipulating tasks (such as picking up coins and beans, flipping over cards); complicated tasks (plugging and unplugging pegboards, drawing simple figures, and colouring) | 20 | 5 | 4 | 400 | Inpatient rehabilitation ward | |
| Upper extremity | Experimental 1: MT: Bilateral activities; Experimental 2: MT and sensory electrical stimulation by a mesh‐glove | Task‐oriented training | Transitive movements (e.g. gross motor tasks, such as reaching out to put a cup on a shelf, or fine motor tasks, such as picking up marbles); intransitive movements (e.g. gross motor movements, such as pronation and supination, or fine motor movements, such as finger opposition) | 60 | 5 | 4 | 1200 | In‐ and outpatient setting | |
| Upper extremity | n/r | n/r; transparent plastic between limbs | n/r | n/r | n/r | 4 | n/r | Home | |
| Lower extremity | Bilateral activities | 1: Bilateral activities, covered mirror; | Alternate dorsiflexion and plantarflexion in both ankles as best as possible, self‐paced speed | 15 | 5 | 3 | 225 | Inpatient rehabilitation unit | |
| Upper extremity | Bilateral activities | Bilateral activities | Exercises based on the Brunnstrom phases of motor recovery; functional tasks (i.e. with objects) | 60 | 1 (under supervision) + 5 (at home) | 6 | 2160 | Home | |
| Upper extremity | Bilateral activities | No additional therapy | Flexion and extension of shoulder, elbow, wrist and finger, prone‐supination of the forearm | 30 | 5 | 6 | 900 | Inpatient | |
| Lower extremity | Activities of the unaffected limb | Activities of the unaffected limb, non‐reflecting surface | Lying position: hip‐knee‐ankle flexion, with the hip and knee placed in flexion, moving the knee inward and outward, hip abduction with external rotation followed by hip adduction with internal rotation; sitting position: Hip‐knee‐ankle flexion, knee extension with ankle dorsiflexion, knee flexion beyond 90 °; each exercise 2 sets of 10 repetitions | 60 | 6 | 2 | 720 | Inpatient rehabilitation | |
| Upper extremity | Bilateral activities | Landscape images were shown to participants, they should try to describe the images, without movements | Finger and hand movements | 30 | 5 | 1 | 150 | n/r | |
| Upper extremity | Bilateral activities | functional electrical stimulation, covered mirror | Experimental 1: wrist and finger extension, grasping and releasing a bottle; Experimental 2: combined MT and functional electrical stimulation | 30 | 6 | 2 | 360 | Hospital | |
| Upper extremity | Bilateral activities, therapist supported if patients were not able to move paretic limb | Bilateral activities, covered mirror | Flexion and extension movements of wrist and fingers | 60 | 5 | 4 | 1200 | inpatient rehabilitation and home training after discharge | |
| Upper extremity | Activities of the unaffected limb | Activities of the unaffected limb; covered mirror | Pronation and supination of the forearm and the flexion and extension movements of the wrist and fingers; 5 sets each motion, 30 repetitions per set | 30 | 5 | 4 | 600 | Inpatient | |
| Upper extremity | Activities of the unaffected limb | Activities of the unaffected limb, non‐reflecting surface | Task‐oriented activities consisted with reaching, grasping, lifting and releasing objects | n/r | 5 | 6 | n/r | Rehabilitation unit | |
| Upper extremity | Not stated | Same tasks; covered mirror | Task‐oriented activities consisting of grasping and releasing objects | 30 | 5 | 2 | 300 | Inpatient rehabilitation centre | |
| Upper extremity | bilateral activities | Same tasks; covered mirror | Finger and wrist movements, grasping different objects | 30 | 5 | 4 | 600 | Nursing homes | |
| Upper extremity | Bilateral activities | Motor relearning programme | Hand‐opening, wrist flexion/ extension, forearm pronation/ supination, hand sliding on surface | n/r | 6 | 4 | n/r | Outpatient | |
| Upper extremity | Bilateral activities | Bilateral activities; covered mirror | Task‐orientend activities consisted with manipulating objects | 60 | 3 | 4 | 720 | Home | |
| Upper extremity | Bilateral activities (hypotone muscles); unilateral activities (hypertone muscles) | Bilateral activities; without mirror | Gross motor arm and hand movements; functional activities (i.e. with objects); fine motor activities (i.e. with objects) | 30 | Total number of sessions: 17 | 5 | 510 | Outpatient centre | |
| See Rothgangel 2004a | See Rothgangel 2004a | See Rothgangel 2004a | See Rothgangel 2004a | 30 | Total number of sessions: 37 | 5 | 1110 | Inpatient rehabilitation centre | |
| Lower extremity | MT + Electrical stimulation | Conventional therapy | n/r | 50 | 4 | 2 | 400 | n/r | |
| Upper extremity | Activities of the unaffected limb | No additional therapy | Wrist flexion, extension, radial and ulnar deviation, circumduction, fisting, releasing, abduction, and adduction of all fingers; activities such as squeezing a ball, stacking rings, flipping cards, placing pegs on a board | 2 times for 30 | 5 | 3 | 900 | Inpatient rehabilitation centre | |
| Upper extremity | Bilateral activities | Electromyographic‐triggered muscular electrical stimulation | Grasping movements in combination with electromyographic‐triggered muscular electrical stimulation | 30 | 5 | 3 | 450 | 3 inpatient rehabilitation centres | |
| Upper extremity | Activities of the unaffected limb | No therapy | 5 movements of wrist and fingers, each 6 minutes | 30 | 5 | 4 | 500 | Inpatient rehabilitation centre | |
| Lower extremity | Activities of the unaffected limb | Activities of the unaffected limb; covered mirror | Dorsiflexion movements of the ankle | 30 | 5 | 4 | 600 | Inpatient rehabilitation centre | |
| Upper extremity | Activities of the unaffected limb; affected limb passively moved by therapist | Activities of the unaffected limb; affected limb passively moved by therapist; without mirror | 13 kinds of movements, i.e. flexion/extension of wrist, pinching fingers, gripping ball | 10 to 15 | Daily | 4 (1st period) | 280 to 420 | Inpatient rehabilitation centre | |
| Upper extremity | Bilateral activities | Bilateral activities; covered mirror | 1st week: isolated movements of fingers, wrist, lower arm, elbow and shoulder in all degrees of freedom, up to 50 repetitions per series, up to 4 series; | 30 | 3 ‐ 5 | 4 ‐ 5 | 600 | Inpatient rehabilitation centre | |
| Upper extremity | Not stated; self‐performed, daily checking by therapist | Lower limb activities; without a mirror | n/r | 30 | 5 | 4 | 600 | 12 inpatient stroke services | |
| Upper extremity | n/r | 1: no additional therapy; | n/r | n/r | n/r | n/r | n/r | n/r | |
| Upper extremity | Bilateral activities | Usual occupational therapy | Transitive movements: fine motor tasks of squeezing sponges, placing pegs in holes, flipping a card, gross motor tasks (reaching out for touch); intransitive movements (repetitive wrist flexion/extension, finger opposition, forearm pro‐/supination) | 60 | 5 | 4 | 1200 | 4 hospitals | |
| Upper extremity | Bilateral activities | Bilateral activities; nonreflecting side of the mirror | Flexion/extension of wrist and fingers | 30 | 5 | 4 | 600 | Inpatient rehabilitation centre | |
| Upper extremity | Activities of the unaffected limb | 1: constraint induced movement therapy (6 hours/day) + palliative rehabilitation programme + self‐exercise; | Flexion/extension of the shoulder, elbow, wrist, finger, and pronation/supination of the forearm | 30 | 5 | 2 | 300 | Inpatient rehabilitation centre | |
| Upper extremity | Experimental 1: activities of the unaffected limb Experimental 2: activities of the unaffected limb and additionally neuromuscular electrical stimulation of the affected arm | Neuromuscular electrical stimulation of finger and wrist extensors of the affected arm | Flexion/extension of wrist and fingers | 30 | 5 | 3 | 450 | Inpatient rehabilitation centre | |
| n/r | n/r | n/r | n/r | 30 | Total: 20 ‐ 24 | 8 | 600 ‐ 720 | n/r | |
| EMG: electromyography | |||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Motor function at the end of intervention phase Show forest plot | 36 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 All outcome measures | 36 | 1173 | Std. Mean Difference (IV, Random, 95% CI) | 0.47 [0.27, 0.67] |
| 2 Motor impairment at the end of intervention phase Show forest plot | 39 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 All outcome measures | 39 | 1292 | Std. Mean Difference (IV, Random, 95% CI) | 0.49 [0.32, 0.66] |
| 3 Fugl‐Meyer Assessment upper extremity at the end of intervention phase Show forest plot | 28 | 898 | Mean Difference (IV, Random, 95% CI) | 4.32 [2.46, 6.19] |
| 4 Activities of daily living at the end of intervention phase Show forest plot | 19 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 All outcome measures | 19 | 622 | Std. Mean Difference (IV, Random, 95% CI) | 0.48 [0.30, 0.65] |
| 5 Pain at the end of intervention phase Show forest plot | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 All outcome measures | 6 | 248 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.89 [‐1.67, ‐0.11] |
| 6 Visuospatial neglect at the end of intervention Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 All outcome measures | 5 | 175 | Std. Mean Difference (IV, Random, 95% CI) | 1.06 [‐0.10, 2.23] |
| 7 Motor function at follow‐up after 6 months Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 All outcome measures | 2 | 88 | Std. Mean Difference (IV, Random, 95% CI) | 1.20 [‐0.78, 3.18] |
| 8 Motor impairment at follow‐up after 6 months Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 8.1 All outcome measures | 3 | 109 | Std. Mean Difference (IV, Random, 95% CI) | 0.69 [0.26, 1.12] |
| 9 Dropouts at the end of intervention phase Show forest plot | 42 | 1438 | Odds Ratio (M‐H, Random, 95% CI) | 1.14 [0.74, 1.76] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Motor function at the end of intervention Show forest plot | 36 | 1173 | Std. Mean Difference (IV, Random, 95% CI) | 0.47 [0.27, 0.67] |
| 1.1 Mirror therapy for the upper extremity | 31 | 1048 | Std. Mean Difference (IV, Random, 95% CI) | 0.46 [0.23, 0.69] |
| 1.2 Mirror therapy for the lower extremity | 5 | 125 | Std. Mean Difference (IV, Random, 95% CI) | 0.56 [0.19, 0.92] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Motor function at the end of intervention phase Show forest plot | 36 | 1199 | Std. Mean Difference (IV, Random, 95% CI) | 0.50 [0.29, 0.72] |
| 1.1 Studies that used a covered mirror in the control group | 16 | 506 | Std. Mean Difference (IV, Random, 95% CI) | 0.67 [0.36, 0.99] |
| 1.2 Studies that used unrestricted view in the control group | 14 | 474 | Std. Mean Difference (IV, Random, 95% CI) | 0.27 [‐0.05, 0.59] |
| 1.3 Studies that used no additional control intervention | 8 | 219 | Std. Mean Difference (IV, Random, 95% CI) | 0.57 [‐0.02, 1.15] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Motor function at the end of intervention phase Show forest plot | 32 | 994 | Std. Mean Difference (IV, Random, 95% CI) | 0.44 [0.22, 0.66] |
| 1.1 All studies including participants within 6 months after stroke | 18 | 596 | Std. Mean Difference (IV, Random, 95% CI) | 0.45 [0.18, 0.73] |
| 1.2 All studies including participants with more than 6 months after stroke | 14 | 398 | Std. Mean Difference (IV, Random, 95% CI) | 0.43 [0.06, 0.81] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Motor function at the end of intervention Show forest plot | 36 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 All studies without randomised cross‐over trials | 35 | 1160 | Std. Mean Difference (IV, Random, 95% CI) | 0.47 [0.27, 0.68] |
| 1.2 All studies with adequate sequence generation | 33 | 1005 | Std. Mean Difference (IV, Random, 95% CI) | 0.36 [0.19, 0.54] |
| 1.3 All studies with adequate concealed allocation | 16 | 572 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.04, 0.47] |
| 1.4 All studies with adequate handling of incomplete outcome data | 12 | 388 | Std. Mean Difference (IV, Random, 95% CI) | 0.55 [0.14, 0.95] |
| 1.5 All studies with blinded assessors | 25 | 820 | Std. Mean Difference (IV, Random, 95% CI) | 0.44 [0.17, 0.70] |
| 2 Motor impairment at the end of intervention Show forest plot | 36 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 All studies with adequate sequence generation | 36 | 1157 | Std. Mean Difference (IV, Random, 95% CI) | 0.46 [0.29, 0.63] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain at the end of intervention Show forest plot | 4 | 176 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.53, 0.08] |

