تاثیر بستن قرارداد در بهبود استفاده از خدمات سلامت بالینی و پیامدهای سلامت در کشورهای با سطح درآمد پائین و متوسط
Referencias
منابع مطالعات واردشده در این مرور
منابع مطالعات خارجشده از این مرور
منابع مطالعات در انتظار ارزیابی
منابع اضافی
منابع دیگر نسخههای منتشرشده این مرور
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Cluster‐randomised trial; 4 districts each were randomised to intervention and control arms | |
| Participants | The study was conducted in rural districts in Cambodia, and served a population of about 1.26 million people ‐ adults and children (11% of Cambodia's population). | |
| Interventions | NGPs were contracted to provide all preventive, promotional, and basic curative healthcare services mandated for a district by the Ministry of Health. These NGPs were contracted to deliver specific services and corresponding targets at health facilities. The programme was implemented over 4 years ‐ between 1999 and 2003. | |
| Outcomes | We reported the following outcomes (all measured over a 12 month period): immunisation of children 12 to 24 months old, high‐dose vitamin A to children 6 to 59 months old, antenatal visits, birth deliveries by trained professionals, female use of contraceptives, use of district public healthcare facilities when sick, mortality in the past year of children younger than 1 year, incidence of diarrhoea in children younger than 5 years, government healthcare expenditures Health information: accuracy of facility registers Availability of selected essential medicines: availability of child vaccines at facilities over the previous 3 months Health financing: individual healthcare expenditures (ITT; important benefit) (measured over a 12 month period) | |
| Notes | Contextual factors
| |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | This is not described in the paper. |
| Allocation concealment (selection bias) | Unclear risk | This is not described in the paper. |
| Baseline outcome measurements | Low risk | The numbers reported in baseline measures appear to be similar across intervention and control arms; however no details of statistical differences are provided. |
| Baseline participant characteristics | High risk | Characteristics are not reported in text or tables. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Blinding is not described, and it is unlikely that it was done. It is unclear whether this would affect the performance of participants or personnel. |
| Blinding of outcome assessment (detection bias) | Unclear risk | It is unclear whether the assessors ‐ those who conducted baseline and post‐intervention surveys ‐ were blinded to whether participants belonged to intervention or control arms. |
| Incomplete outcome data (attrition bias) | Unclear risk | This is not described in the paper. |
| Protection against contamination | Low risk | Allocation to intervention and control arms was done at the district level, and it unlikely that the control group received the intervention. |
| Selective reporting (reporting bias) | Unclear risk | The study protocol could not be accessed. |
| Other bias | Unclear risk | Review authors did not identify other risks of bias. |
| Methods | Controlled before‐after study | |
| Participants | The study was conducted in rural districts in Guatemala, and served a population of about 4.2 million people ‐ a third of the country’s population. | |
| Interventions | NGPs were contracted to provide all preventive, promotional, and basic curative healthcare services mandated for a district by the Ministry of Health. Services were provided by mobile medical teams comprising a physician or a nurse and a health assistant. These teams conducted visits to communities at least monthly. NGPs were contracted to deliver specific services and corresponding targets at health facilities. The intervention was implemented over ten years, from 1997 to 2007. | |
| Outcomes | We reported the following outcomes: immunisation of children 12 to 24 months old, antenatal visits, and female use of contraceptives over a 12 month period. | |
| Notes | Contextual factors
| |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Risk of selection bias was high because the intervention communities were selected in a non‐random manner. |
| Allocation concealment (selection bias) | High risk | Selection and allocation of the intervention communities were performed ad‐hoc; therefore this study can be assumed to have high risk of selection bias due to lack of allocation concealment. |
| Baseline outcome measurements | Low risk | The numbers reported in baseline measures appear to be similar across intervention and control arms; however no details of statistical differences are provided. |
| Baseline participant characteristics | Low risk | Baseline characteristics and differences between intervention and control arms are well balanced except for a statistical difference in age among children aged 2 to 24 months. We rated this study as having low risk of potential bias. |
| Blinding of participants and personnel (performance bias) | Unclear risk | It is unlikely that this was done. It is unclear whether this would affect the performance of participants or personnel. |
| Blinding of outcome assessment (detection bias) | Low risk | Data used to assess intervention effects were extracted from routine surveys that were independent of the intervention itself. |
| Incomplete outcome data (attrition bias) | Unclear risk | Attrition is not reported; therefore we assessed this to show unclear risk of attrition bias. |
| Protection against contamination | High risk | The intervention was delivered at village level, and we cannot exclude the potential that people may have received the intervention when visiting neighbouring villages. |
| Selective reporting (reporting bias) | Unclear risk | The study protocol could not be accessed. |
| Other bias | High risk | Data show changes in the context in which the intervention was delivered from the start of evaluation to completion. At the time of the post‐intervention survey, the intervention had been implemented for about 8 years, and trial authors reported that estimates of effects correspond with an improved version of the intervention. |
ITT, intention‐to‐treat.
NGP, non‐governmental health service provider.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Ineligible study design: ITS study without pre‐intervention assessment data | |
| Ineligible study design: no control group or assessments at points before and after the intervention | |
| Ineligible study design: ITS study without pre‐intervention assessment data | |
| Ineligible study design: a description of different contracting out models without reported assessment of intervention effects | |
| Ineligible study design: a description of a contracting out model without a design to assess intervention effects | |
| Ineligible study design: a description of contracting out models without a design to assess intervention effects | |
| Ineligible intervention: supply services ‐ not clinical health services ‐ were contracted out. | |
| Ineligible study design: a report on best practices for contracting out without reported assessment of intervention effects | |
| Ineligible study outcomes: patient satisfaction with contracted out services reported | |
| Ineligible study design: a retrospective longitudinal study design that is purely descriptive and provides no evidence of a cause (contracting out intervention) and effect (improved outcomes) relationship | |
| Ineligible topic: about privatisation ‐ not contracting out | |
| Ineligible intervention: about deploying skilled birth attendants ‐ not contracting out health services | |
| Ineligible comparison: comparison of a contracting out model vs a model in which the central government contracted the local government | |
| Ineligible study design: a description of a contracting out model without a design for assessment of intervention effects | |
| Ineligible comparison: both groups given the same intervention | |
| Ineligible comparison: comparison of the contracting out model vs a model in which the central government contracted the local government | |
| Ineligible study design: a retrospective study design that is purely descriptive and provides no evidence of a cause and effect relationship | |
| Ineligible study design | |
| Ineligible study design: a literature review | |
| Ineligible study design: a CBA study with only 1 intervention site in the initial design | |
| Ineligible study design: a description of a contracting out model without a design for assessment of intervention effects | |
| Ineligible study design: a description of a contracting out model without a design for assessment of intervention effects | |
| Ineligible study design: a case study, involving only 1 site | |
| Ineligible participants: not an LMIC | |
| Ineligible intervention: about medical equipment maintenance ‐ not clinical healthcare services | |
| Ineligible study design: an evaluation study to identify which aspects of the contracting process and the context in which it takes place are important in influencing whether contracting with the private sector is a desirable means of service provision | |
| Ineligible study design: a description of a contracting out model without a design for assessment of intervention effects | |
| Ineligible intervention: no formal contract between the government and the non‐governmental service provider | |
| Ineligible study design: a description of contracting out models without a design for assessment of intervention effects | |
| Ineligible study design: a description of contracting out models without a design for assessment of intervention effects | |
| Ineligible intervention: clinical health services managed in part by a non‐governmental service provider | |
| Ineligible study design: a description of contracting out models without a design for assessment of intervention effects | |
| Ineligible intervention: clinical health services managed in part by non‐governmental service provider | |
| A case study of outsourced primary healthcare services in Sindh, Pakistan: Is this real reform? | |
| Ineligible participants: not an LMIC | |
| Ineligible study design: CBA study with only 1 intervention site | |
| Ineligible study design: a description of contracting out models without a design for assessment of intervention effects | |
| Ineligible intervention: National TB programme partnered with NGOs and private medical practitioners, but services were not contracted out. |
CBA: controlled before‐after.
ITS: interrupted time series.
LMIC: low‐ and middle‐income country.
NGO: non‐governmental organisation.
TB: tuberculosis.
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Controlled before‐after study |
| Participants | Municipalities in Sao Paulo, Brazil |
| Interventions | Municipalities implemented the Family Health Program, a community‐based programme to deliver primary healthcare services, and contracted out these services to precertified non‐profit, non‐governmental organisations. |
| Outcomes | Infant and child mortality, hospitalisation for preventable diseases |
| Notes |
| Methods | Controlled before‐after study. |
| Participants | Rural communities in Pakistan. |
| Interventions | A MOU was signed between the government and the Punjab Rural Support programme (PRSP) which gave the PRSP administrative and financial control over the management of all BHUs in the Rahim Yar Khan district. The MOU provided the PRSP with the autonomy to implement organizational and management changes regarding the BHU infrastructure, staff, budget and procurement of medicines. |
| Outcomes | Seeking care for unknown general illness and childhood diarrhoea. |
| Notes |
BHU: basic health unit.
MOU: memorandum of understanding.
PRSP: Punjab Rural Support Programme.
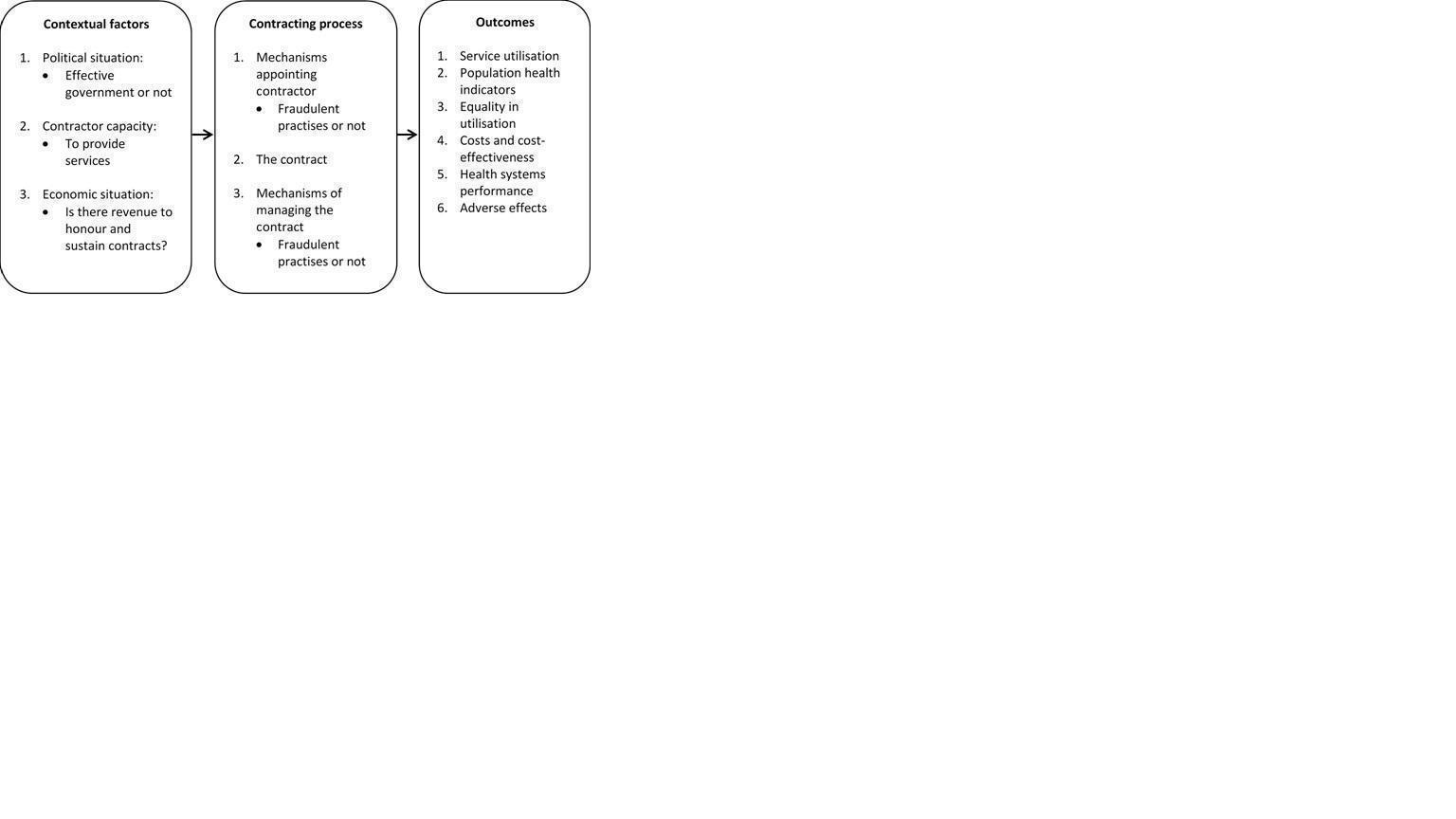
How the intervention might work.

Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
| Contracting out compared with not contracting out for providing clinical healthcare services | |||||
| Population: people who use governmental clinical health services that are contracted out to non‐governmental providers Intervention: provision of any clinical health service on behalf of the government by for‐profit and/or not‐for‐profit, non‐governmental providers Comparison: contracting out vs no contracting out | |||||
| Outcomes | Net effecta | No. of studies | Certainty of the evidence | Results in words | Comments |
| Utilisation of health services | |||||
| Immunisation of children 12 to 24 months old (over a 12 month period) | Fully immunised Net effect = ‐39.4%, intervention effect P = 0.46, clustered SE = 9.0%; see Table 1 for the CI Measles Net effect = 46.5%, SE = 28.5%, 95% CI ‐9.4% to 102.4% DPT Net effect = ‐1.4%, SE = 22.9%, 95% CI ‐46.3% to 43.5% Polio Net effect = ‐7.6%, SE = 24.1%, 95% CI ‐54.8% to 39.6% | 2c,d | ⊕⊕⊕⊖ Moderatee | Contracting out probably makes little or no difference in immunisation uptake of children 12 to 24 months old over the previous 12 months. | |
| Antenatal visits (over the previous 12 months) | > 2 antenatal care visits Net effect = ‐12.2 %, intervention effect P = 0.35, clustered SE = 10.0%; see Table 1 for the CI ≥ 3 antenatal care visits Net effect = 27.4%, SE = 22.2%, 95% CI ‐16.1% to 70.9% | 2c,d | ⊕⊕⊕⊖ Moderatee | Contracting out probably makes little or no difference in the number of women who had > 2 antenatal care visits over the previous 12 months. | |
| Female use of contraceptives (over a 12 month period) | Net effect = ‐11.5%, intervention effect P = 0.78, clustered SE = 3.0%; see Table 1 for the CI Net effect = 1.9%, SE = 6.9%, 95% CI ‐11.6% to 15.4% | 2c,d | ⊕⊕⊕⊖ Moderatee | Contracting out probably makes little or no difference in female use of contraceptives over the previous 12 months. | |
| Health outcomes | |||||
| Mortality in the past year of children younger than 1 year (over a 12 month period) | Net effect = ‐4.3%, intervention effect P = 0.36, clustered SE = 3.0%; see Table 1 for the CI | 1c | ⊕⊕⊖⊖ Lowe,f | Contracting out may make little or no difference in the mortality of children younger than 1 year over a 12 month period. | Trial authors conclude that the sample size was too small to detect typical mortality. |
| Incidence of diarrhoea in children younger than 5 years (over a 12 month period) | Net effect = ‐16.2%, intervention effect P = 0.07, clustered SE = 19.0%; see Table 1 for the CI | 1c | ⊕⊕⊖⊖ Lowe,f | Contracting out may make little or no difference in the incidence of childhood diarrhoea over a 12 month period. | |
| Equity in utilisation of clinical health services | |||||
| Not reported in the included studies | |||||
| Economic outcomes | |||||
| Individual healthcare expenditures (over a 12 month period) | Net effect = $ ‐19.25 (2003 USD), intervention effect P = 0.01, clustered SE = $ 5.21; see Table 1 for the CI | 1c | ⊕⊕⊕⊖ Moderatee | Contracting out probably reduces individual out‐of‐pocket spending on curative care over a 12 month period. | The reduction in individuals’ healthcare expenditure is in line with the reported decrease in people visiting private healthcare providers. |
| Adverse effects | |||||
| Not reported in the included studies. | |||||
| a Calculated as the difference between the change in the intervention group and the change in the control group: Net effect = (INTpost – INTpre) – (CONTpost – CONTpre). bGRADE Working Group grades of evidence: * Substantially different = a large enough difference that it might affect a decision. cBloom 2006 (cluster‐randomised trial). dCristia 2015 (CBA). e Downgraded by 1 for serious risk of bias. Study 1 (Bloom 2006) is at high risk of bias as baseline participant characteristics are not reported, and Study 2 (Cristia 2015) is at high risk of other bias because estimates of effects correspond with a strengthened model of the intervention compared with the initial model. f Downgraded by one for serious imprecision. The study reported treatment of the treated (ToT) estimates. Actual numbers for numerator and denominator were not provided. | |||||
| DPT: diphtheria‐pertussis‐tetanus | |||||
| Outcome | Intervention effect (CI) |
| Immunisation of children 12 to 24 months old over a 12 month period | 7.6% (‐10.0% to 25.2%) |
| High‐dose vitamin A to children 6 to 59 months old over a 12 month period | 20.3% (6.6% to 34.0%) |
| Antenatal visits in the previous 12 months | 13.8% (‐5.8% to 33.4%) |
| Birth deliveries by trained professionals over a 12 month period | ‐5.5% (‐11.4% to 0.4%) |
| Female use of contraceptives in the previous 12 months | ‐1.5% ( ‐7.4% to 4.4%) |
| Use of district public healthcare facilities when sick in the previous 12 months | 16.6% (6.8% to 26.4%) |
| Mortality in the past year of children younger than 1 year over a 12 month period | ‐4.3% (‐10.2% to 1.6%) |
| Incidence of diarrhoea in children younger than 5 years over a 12 month period | ‐25.2% (‐62.4% to 12.0%) |
| Individual healthcare expenditures over a 12 month period | $ ‐25.89 (2003 USD) ($ ‐35.93 to $ ‐15.855) |
| Health information: accuracy of facility registers | 12.7% (‐57.9% to 83.3%) |
| Availability of selected essential medicines: availability of child vaccines at facilities in the previous 3 months | 14.6% (‐20.7% to 49.9%) |
| Publication | Setting | Contracting model | Key messages | Study design |
| Afghanistan, 2003‐2006/7 (post‐Taliban conflict) | Three models: 1. Province‐wide lump sum contracts; performance bonuses; an independent group monitored performance; a high degree of NGP autonomy; limited capacity building of NGP; government managed contracts 2. Monthly reimbursements made; monitoring through an international non‐profit organisation; no performance bonuses 3. 80% of Year 1 budget paid in advance; donor‐monitored NGP performance; no performance bonuses | 1. Contracting out has been associated with substantial increases in use of curative care, in particular that of poor and female patients. 2. No conclusive evidence shows that any 1 model is more effective than another. 3. Linking equity goals to performance bonuses may reduce the inequity of service utilisation between the poor and the non‐poor. 4. Using service characteristics and geographical distances as planning parameters does not guarantee better resource allocation. 5. The impact of contracting out on the quality of services needs to be researched. | Contracting out was implemented as routine care. | |
| India, 2000‐2010 | 1. The government contracted private obstetricians who own hospitals to enable poor women in rural areas to deliver at these facilities. 2. Hospitals had to meet criteria related to size and emergency services. 3. Obstetricians received a fixed reimbursement per 100 deliveries. 4. The reimbursement amount had a build‐in disincentive for caesarean deliveries. | 1. Institutional deliveries increased by 50%. 2. Quality of care and provider attrition need to be researched. Mohanan 2014 3. Investigators contested the success of the programme: Studies claiming programme success did not (i) address the impact of self‐selection of institutional delivery, or (ii) address inaccurate reporting from hospitals. 4. Investigators found no important changes in the probability of institutional delivery. | Contracting out was implemented as routine care. | |
| Bangladesh, 1999‐2004 | 1. The government contracted with an NGP or with local government to deliver basic PHC. 2. Competitive bidding for NGP contracts 3. NGPs, but not the local government, were allowed to recruit staff and set salaries and working conditions. 4. NGPs, but not the local government, procured products directly from suppliers. 5. Both NGPs and the local government were reimbursed for documented expenditures. | 1. Improvement in PHC was seen in both models, but the overall quality of care was better in the NGP facilities. 2. NGP facilities provided more PHC services per capita spending. 3. Investing in PHC facilities and contracting with NGPs may improve urban health services. | Contracting out was implemented as routine care. | |
| India, 1‐year project, 2007‐2008 | 1. The government partnered with NGPs to improve TB case finding through including it in routine HIV prevention services. 2. 48% of NGPs had formal contracts. 3. The model was translated into national policy through a public sector‐funded TB‐HIV partnership scheme with NGPs. 4. No other details were reported. | 1. TB services can be effectively integrated into HIV prevention services and can be delivered through public‐private partnerships (PPPs). | The PPP was implemented as routine care. | |
| India, 2008‐2012 | 1. PPP to attract and retain skilled health workers 2. Management functions in facilities were contracted to NGPs through a memorandum of understanding. 3. No other details were reported. | 1. Improved service delivery, building maintenance, and staff availability 2. NGPs’ flexible approach in staff recruitment and creating a supportive working environment reduced staff attrition. 3. Being isolated from government‐supported functions limited access to training programmes. 4. Contracting out must happen in the context of broader government support to address isolation from government support. | The PPP was implemented as routine care. | |
| India, 2004‐2007 | 1. At the public‐private facility, the government provided free treatment and the private hospital provided the premises, infrastructure, and human resources. 2. No other details were reported. | 1. The fully public and PPP facilities had notably better health outcomes compared with the fully private facility. 2. The fully public facility reported fewer treatment failures compared with PPP and private facilities. 3. Larger studies are required. | The PPP was implemented as routine care. | |
| Pakistan, 2005‐2011 | 1. The government outsourced administration of PHC to a semi‐autonomous government entity. 2. No other details were reported. | 1. Healthcare services were better managed in contracted out facilities than in fully governmental facilities. 2. Contracting may be effective in rebuilding PHC in low‐ and middle‐income countries. | Contracting out was implemented as routine care. | |
| Guinea Bissau, 2012‐2013 | 1. The government entered a PPP with an NGP to manage a national TB reference centre. 2. Government provided the drugs and electricity, and paid staff. 3. The NGP topped up salaries and provided services. | 1. Since the contracting period, mortality and treatment failure were notably lower compared with during the pre‐contracting period. 2. Direct costs to patients were reduced. 3. PPP may, in the short term, increase adherence to the hospitalisation phase of intensive treatment. | The PPP was implemented as routine care. | |
| Pakistan, 2003‐2008 | 1. HIV prevention services were contracted out to NGPs through competitive bidding. 2. These were performance‐based contracts according to predefined targets. 3. Contracts were managed by the government. | 1. Contracting out is inherently a political process affected by the wider policy context. 2. Rapid roll‐out in unprepared contexts can be confounded by governments’ capacity to manage it. 3. Governments should be careful that contracting out does not distance NGPs from their historical attributes. 4. Governments’ political willingness and technical capacity are key components of successful programmes. | Contracting out was implemented as routine care. | |
| HIV: human immunodeficiency virus. NGP: non‐governmental provider. PHC: primary health care. PPP: public‐private partnership TB: tuberculosis | ||||

