تاثیر بستن قرارداد در بهبود استفاده از خدمات سلامت بالینی و پیامدهای سلامت در کشورهای با سطح درآمد پائین و متوسط
Información
- DOI:
- https://doi.org/10.1002/14651858.CD008133.pub2Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 03 abril 2018see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Práctica y organización sanitaria efectivas
- Copyright:
-
- Copyright © 2018 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
WO, KW, CJU, HC, and DC drafted the protocol and screened abstracts, titles, and full texts for eligibility. YB analysed the data. WO and TK drafted the manuscript, and KW, JU, HU, and DC commented on various drafts of the manuscript. All review authors approved the final version of the manuscript.
Sources of support
Internal sources
-
The respective employment organisations of the review authors supported their involvement in the review, Other.
External sources
-
Alliance for Health Policy and Systems Research, Other.
Declarations of interest
Willem A Odendaal: none known.
Kim Ward: none known.
Jesse Uneke: none known.
Henry Uro‐Chukwu: none known.
Dereck Chitama: none known.
Yusentha Balakrishna: none known.
Tamara Kredo: none known.
Acknowledgements
This review was made possible through various individuals and institutions, and we gratefully acknowledge their contributions.
-
Mylene Lagarde and Natasha Palmer for their work on the original review.
-
Cochrane Effective Practice and Organisation of Care (EPOC): Luke Vale, who patiently guided novice review authors through their first review; Elizabeth Paulsen, for reviewing the manuscript; Marit Johansen, for efficiency in developing the search strategies and running the searches; and Simon Lewin, for helping us navigate EPOC guidelines.
-
The Alliance for Health Policy and Systems Research for providing financial support to conduct the review.
-
David Clingingsmith, a co‐author of Bloom 2006, for sharing information about this study and reporting the data.
-
Gabriel Rada, co‐founder and president of the Epistemonikos Foundation, for providing abstract translations.
-
Solange Durao, Cochrane South Africa at the South African Medical Research Council, for providing abstract translations.
-
Ria Laubscher, at the South African Medical Research Council, for kind assistance in understanding the data.
-
Hlengiwe Moloi at the South African Medical Research Council, for assistance with Grey literature searches.
-
Peer reviewers, whose comments enabled us to improve the manuscript.
-
Dolores P. Matthews for copy‐editing the review.
-
Willem Odendaal and Kim Ward were supported by a fellowship offered by Cochrane South Africa at the South African Medical Research Council, funded by the Effective Health Care Research Consortium. This Consortium is funded by UK aid from the UK Government for the benefit of developing countries (Grant: 5242). The views expressed in this publication do not necessarily reflect UK government policy.
-
Willem Odendaal and Tamara Kredo are employed and funded by the South African Medical Research Council.
-
The Norwegian Satellite of the EPOC Group receives funding from the Norwegian Agency for Development Cooperation (Norad), via the Norwegian Institute of Public Health, to support review authors in the production of their reviews.
Version history
| Published | Title | Stage | Authors | Version |
| 2018 Apr 03 | Contracting out to improve the use of clinical health services and health outcomes in low‐ and middle‐income countries | Review | Willem A Odendaal, Kim Ward, Jesse Uneke, Henry Uro‐Chukwu, Dereck Chitama, Yusentha Balakrishna, Tamara Kredo | |
| 2009 Oct 07 | The impact of contracting out on health outcomes and use of health services in low and middle‐income countries | Review | Mylene Lagarde, Natasha Palmer | |
Differences between protocol and review
We made the following two changes: First, based on our reading of the literature and advice from the contact editor, we amended the measures of effects and study design criteria for this update as follows.
-
Measures of effects change: We expanded the outcome measures to include measures of cost‐effectiveness, health system performance, and health service delivery.
-
Study design change: We added studies with a repeated measurement design (RM). We amended one criterion for CBA studies based on revised EPOC study design criteria (EPOC 2017a), which specify that such studies have to include two sites in the control and intervention arms, respectively.
Second, a new review author team was established for the update of the previous version of this review (Lagarde 2009). The new review author team consists of Willem A Odendaal, Kim Ward, Jesse Uneke, Henry Uro‐Chukwu, Dereck Chitama, Yusentha Balakrishna, and Tamara Kredo.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- *Developing Countries;
- *Health Services Accessibility [economics, statistics & numerical data];
- *Health Services Needs and Demand [economics, statistics & numerical data];
- *Outsourced Services [economics, statistics & numerical data];
- *Process Assessment, Health Care;
- Cambodia;
- Contraceptive Agents, Female [administration & dosage];
- Controlled Before‐After Studies;
- Diarrhea [epidemiology];
- Guatemala;
- Health Expenditures;
- Immunization [economics];
- Infant Mortality;
- Prenatal Care [statistics & numerical data];
- Randomized Controlled Trials as Topic;
Medical Subject Headings Check Words
Humans; Infant;
PICO
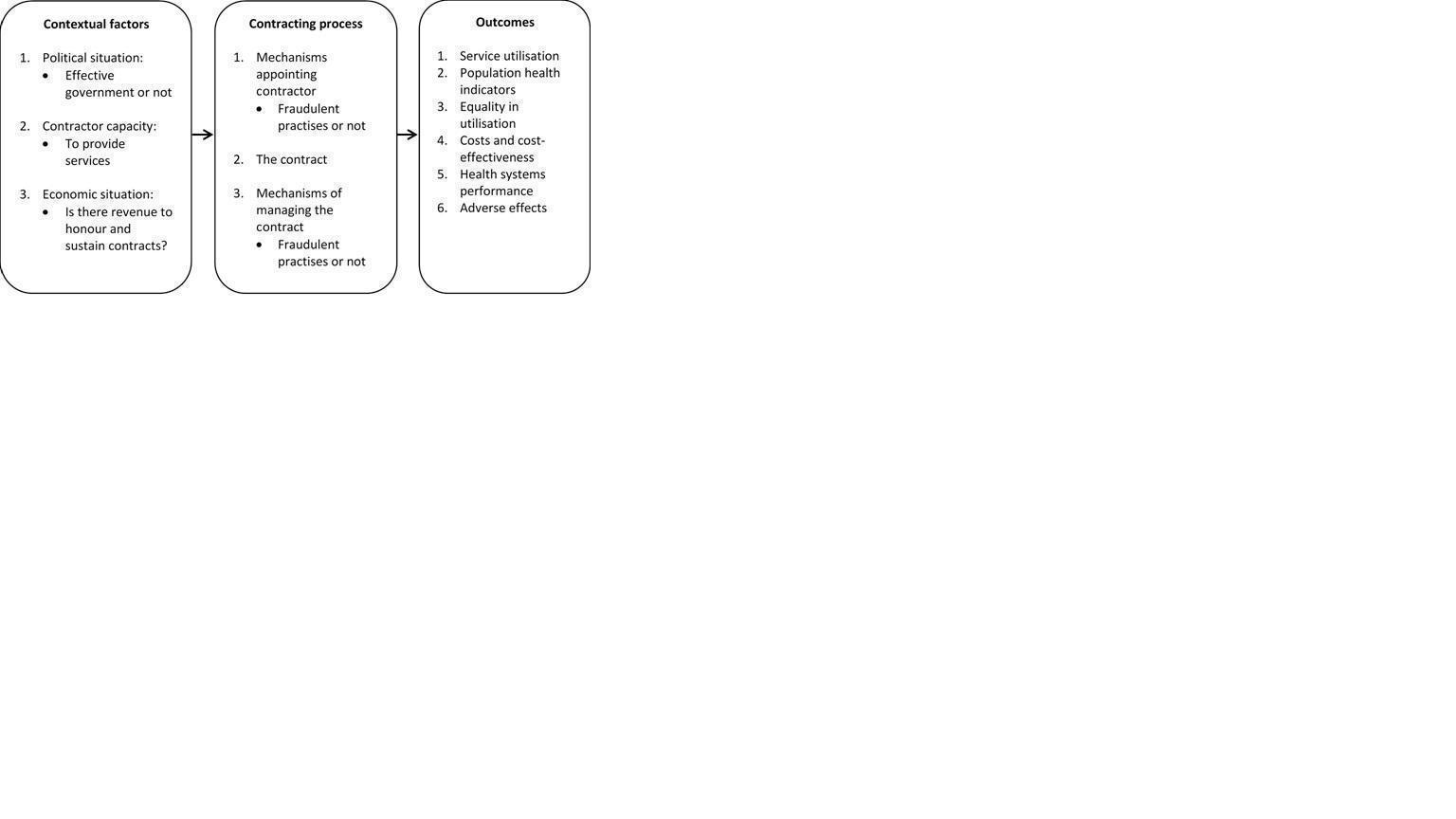
How the intervention might work.

Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
| Contracting out compared with not contracting out for providing clinical healthcare services | |||||
| Population: people who use governmental clinical health services that are contracted out to non‐governmental providers Intervention: provision of any clinical health service on behalf of the government by for‐profit and/or not‐for‐profit, non‐governmental providers Comparison: contracting out vs no contracting out | |||||
| Outcomes | Net effecta | No. of studies | Certainty of the evidence | Results in words | Comments |
| Utilisation of health services | |||||
| Immunisation of children 12 to 24 months old (over a 12 month period) | Fully immunised Net effect = ‐39.4%, intervention effect P = 0.46, clustered SE = 9.0%; see Table 1 for the CI Measles Net effect = 46.5%, SE = 28.5%, 95% CI ‐9.4% to 102.4% DPT Net effect = ‐1.4%, SE = 22.9%, 95% CI ‐46.3% to 43.5% Polio Net effect = ‐7.6%, SE = 24.1%, 95% CI ‐54.8% to 39.6% | 2c,d | ⊕⊕⊕⊖ Moderatee | Contracting out probably makes little or no difference in immunisation uptake of children 12 to 24 months old over the previous 12 months. | |
| Antenatal visits (over the previous 12 months) | > 2 antenatal care visits Net effect = ‐12.2 %, intervention effect P = 0.35, clustered SE = 10.0%; see Table 1 for the CI ≥ 3 antenatal care visits Net effect = 27.4%, SE = 22.2%, 95% CI ‐16.1% to 70.9% | 2c,d | ⊕⊕⊕⊖ Moderatee | Contracting out probably makes little or no difference in the number of women who had > 2 antenatal care visits over the previous 12 months. | |
| Female use of contraceptives (over a 12 month period) | Net effect = ‐11.5%, intervention effect P = 0.78, clustered SE = 3.0%; see Table 1 for the CI Net effect = 1.9%, SE = 6.9%, 95% CI ‐11.6% to 15.4% | 2c,d | ⊕⊕⊕⊖ Moderatee | Contracting out probably makes little or no difference in female use of contraceptives over the previous 12 months. | |
| Health outcomes | |||||
| Mortality in the past year of children younger than 1 year (over a 12 month period) | Net effect = ‐4.3%, intervention effect P = 0.36, clustered SE = 3.0%; see Table 1 for the CI | 1c | ⊕⊕⊖⊖ Lowe,f | Contracting out may make little or no difference in the mortality of children younger than 1 year over a 12 month period. | Trial authors conclude that the sample size was too small to detect typical mortality. |
| Incidence of diarrhoea in children younger than 5 years (over a 12 month period) | Net effect = ‐16.2%, intervention effect P = 0.07, clustered SE = 19.0%; see Table 1 for the CI | 1c | ⊕⊕⊖⊖ Lowe,f | Contracting out may make little or no difference in the incidence of childhood diarrhoea over a 12 month period. | |
| Equity in utilisation of clinical health services | |||||
| Not reported in the included studies | |||||
| Economic outcomes | |||||
| Individual healthcare expenditures (over a 12 month period) | Net effect = $ ‐19.25 (2003 USD), intervention effect P = 0.01, clustered SE = $ 5.21; see Table 1 for the CI | 1c | ⊕⊕⊕⊖ Moderatee | Contracting out probably reduces individual out‐of‐pocket spending on curative care over a 12 month period. | The reduction in individuals’ healthcare expenditure is in line with the reported decrease in people visiting private healthcare providers. |
| Adverse effects | |||||
| Not reported in the included studies. | |||||
| a Calculated as the difference between the change in the intervention group and the change in the control group: Net effect = (INTpost – INTpre) – (CONTpost – CONTpre). bGRADE Working Group grades of evidence: * Substantially different = a large enough difference that it might affect a decision. cBloom 2006 (cluster‐randomised trial). dCristia 2015 (CBA). e Downgraded by 1 for serious risk of bias. Study 1 (Bloom 2006) is at high risk of bias as baseline participant characteristics are not reported, and Study 2 (Cristia 2015) is at high risk of other bias because estimates of effects correspond with a strengthened model of the intervention compared with the initial model. f Downgraded by one for serious imprecision. The study reported treatment of the treated (ToT) estimates. Actual numbers for numerator and denominator were not provided. | |||||
| DPT: diphtheria‐pertussis‐tetanus | |||||
| Outcome | Intervention effect (CI) |
| Immunisation of children 12 to 24 months old over a 12 month period | 7.6% (‐10.0% to 25.2%) |
| High‐dose vitamin A to children 6 to 59 months old over a 12 month period | 20.3% (6.6% to 34.0%) |
| Antenatal visits in the previous 12 months | 13.8% (‐5.8% to 33.4%) |
| Birth deliveries by trained professionals over a 12 month period | ‐5.5% (‐11.4% to 0.4%) |
| Female use of contraceptives in the previous 12 months | ‐1.5% ( ‐7.4% to 4.4%) |
| Use of district public healthcare facilities when sick in the previous 12 months | 16.6% (6.8% to 26.4%) |
| Mortality in the past year of children younger than 1 year over a 12 month period | ‐4.3% (‐10.2% to 1.6%) |
| Incidence of diarrhoea in children younger than 5 years over a 12 month period | ‐25.2% (‐62.4% to 12.0%) |
| Individual healthcare expenditures over a 12 month period | $ ‐25.89 (2003 USD) ($ ‐35.93 to $ ‐15.855) |
| Health information: accuracy of facility registers | 12.7% (‐57.9% to 83.3%) |
| Availability of selected essential medicines: availability of child vaccines at facilities in the previous 3 months | 14.6% (‐20.7% to 49.9%) |
| Publication | Setting | Contracting model | Key messages | Study design |
| Afghanistan, 2003‐2006/7 (post‐Taliban conflict) | Three models: 1. Province‐wide lump sum contracts; performance bonuses; an independent group monitored performance; a high degree of NGP autonomy; limited capacity building of NGP; government managed contracts 2. Monthly reimbursements made; monitoring through an international non‐profit organisation; no performance bonuses 3. 80% of Year 1 budget paid in advance; donor‐monitored NGP performance; no performance bonuses | 1. Contracting out has been associated with substantial increases in use of curative care, in particular that of poor and female patients. 2. No conclusive evidence shows that any 1 model is more effective than another. 3. Linking equity goals to performance bonuses may reduce the inequity of service utilisation between the poor and the non‐poor. 4. Using service characteristics and geographical distances as planning parameters does not guarantee better resource allocation. 5. The impact of contracting out on the quality of services needs to be researched. | Contracting out was implemented as routine care. | |
| India, 2000‐2010 | 1. The government contracted private obstetricians who own hospitals to enable poor women in rural areas to deliver at these facilities. 2. Hospitals had to meet criteria related to size and emergency services. 3. Obstetricians received a fixed reimbursement per 100 deliveries. 4. The reimbursement amount had a build‐in disincentive for caesarean deliveries. | 1. Institutional deliveries increased by 50%. 2. Quality of care and provider attrition need to be researched. Mohanan 2014 3. Investigators contested the success of the programme: Studies claiming programme success did not (i) address the impact of self‐selection of institutional delivery, or (ii) address inaccurate reporting from hospitals. 4. Investigators found no important changes in the probability of institutional delivery. | Contracting out was implemented as routine care. | |
| Bangladesh, 1999‐2004 | 1. The government contracted with an NGP or with local government to deliver basic PHC. 2. Competitive bidding for NGP contracts 3. NGPs, but not the local government, were allowed to recruit staff and set salaries and working conditions. 4. NGPs, but not the local government, procured products directly from suppliers. 5. Both NGPs and the local government were reimbursed for documented expenditures. | 1. Improvement in PHC was seen in both models, but the overall quality of care was better in the NGP facilities. 2. NGP facilities provided more PHC services per capita spending. 3. Investing in PHC facilities and contracting with NGPs may improve urban health services. | Contracting out was implemented as routine care. | |
| India, 1‐year project, 2007‐2008 | 1. The government partnered with NGPs to improve TB case finding through including it in routine HIV prevention services. 2. 48% of NGPs had formal contracts. 3. The model was translated into national policy through a public sector‐funded TB‐HIV partnership scheme with NGPs. 4. No other details were reported. | 1. TB services can be effectively integrated into HIV prevention services and can be delivered through public‐private partnerships (PPPs). | The PPP was implemented as routine care. | |
| India, 2008‐2012 | 1. PPP to attract and retain skilled health workers 2. Management functions in facilities were contracted to NGPs through a memorandum of understanding. 3. No other details were reported. | 1. Improved service delivery, building maintenance, and staff availability 2. NGPs’ flexible approach in staff recruitment and creating a supportive working environment reduced staff attrition. 3. Being isolated from government‐supported functions limited access to training programmes. 4. Contracting out must happen in the context of broader government support to address isolation from government support. | The PPP was implemented as routine care. | |
| India, 2004‐2007 | 1. At the public‐private facility, the government provided free treatment and the private hospital provided the premises, infrastructure, and human resources. 2. No other details were reported. | 1. The fully public and PPP facilities had notably better health outcomes compared with the fully private facility. 2. The fully public facility reported fewer treatment failures compared with PPP and private facilities. 3. Larger studies are required. | The PPP was implemented as routine care. | |
| Pakistan, 2005‐2011 | 1. The government outsourced administration of PHC to a semi‐autonomous government entity. 2. No other details were reported. | 1. Healthcare services were better managed in contracted out facilities than in fully governmental facilities. 2. Contracting may be effective in rebuilding PHC in low‐ and middle‐income countries. | Contracting out was implemented as routine care. | |
| Guinea Bissau, 2012‐2013 | 1. The government entered a PPP with an NGP to manage a national TB reference centre. 2. Government provided the drugs and electricity, and paid staff. 3. The NGP topped up salaries and provided services. | 1. Since the contracting period, mortality and treatment failure were notably lower compared with during the pre‐contracting period. 2. Direct costs to patients were reduced. 3. PPP may, in the short term, increase adherence to the hospitalisation phase of intensive treatment. | The PPP was implemented as routine care. | |
| Pakistan, 2003‐2008 | 1. HIV prevention services were contracted out to NGPs through competitive bidding. 2. These were performance‐based contracts according to predefined targets. 3. Contracts were managed by the government. | 1. Contracting out is inherently a political process affected by the wider policy context. 2. Rapid roll‐out in unprepared contexts can be confounded by governments’ capacity to manage it. 3. Governments should be careful that contracting out does not distance NGPs from their historical attributes. 4. Governments’ political willingness and technical capacity are key components of successful programmes. | Contracting out was implemented as routine care. | |
| HIV: human immunodeficiency virus. NGP: non‐governmental provider. PHC: primary health care. PPP: public‐private partnership TB: tuberculosis | ||||

