Maternal position in the second stage of labour for women with epidural anaesthesia
Abstract
Background
Epidural analgesia in labour prolongs the second stage and increases instrumental delivery. It has been suggested that a more upright maternal position during all or part of the second stage may counteract these adverse effects. This is an update of a Cochrane Review published in 2017.
Objectives
To assess the effects of different birthing positions (upright or recumbent) during the second stage of labour, on maternal and fetal outcomes for women with epidural analgesia.
Search methods
We searched Cochrane Pregnancy and Childbirth’s Trials Register, ClinicalTrials.gov, the WHO International Clinical Trials Registry Platform (ICTRP) (5 June 2018), and the reference lists of retrieved studies.
Selection criteria
All randomised or quasi‐randomised trials including pregnant women (primigravidae or multigravidae) in the second stage of induced or spontaneous labour receiving epidural analgesia of any kind. Cluster‐randomised controlled trials would have been eligible for inclusion but we found none. Studies published in abstract form only were also eligible.
We assumed the experimental intervention to be maternal use of any upright position during the second stage of labour, compared with the control condition of remaining in any recumbent position.
Data collection and analysis
Two review authors independently assessed trials for inclusion, assessed risks of bias, and extracted data. We contacted study authors to obtain missing data. We assessed the quality of the evidence using the GRADE approach.
We carried out a planned sensitivity analysis of the three studies with low risks of bias for allocation concealment and incomplete outcome data reporting, and further excluded one study with a co‐intervention (this was not prespecified).
Main results
We include eight randomised controlled trials, involving 4464 women, comparing upright positions versus recumbent positions in this update. Five were conducted in the UK, one in France and two in Spain.
The largest UK trial accounted for three‐quarters of all review participants, and we judged it to have low risk of bias. We assessed two other trials as being at low risk of selection and attrition bias. We rated four studies at unclear or high risk of bias for both selection and attrition bias and one study as high risk of bias due to a co‐intervention. The trials varied in their comparators, with five studies comparing different positions (upright and recumbent), two comparing ambulation with (recumbent) non‐ambulation, and one study comparing postural changes guided by a physiotherapist to a recumbent position.
Overall, there may be little or no difference between upright and recumbent positions for our combined primary outcome of operative birth (caesarean or instrumental vaginal): average risk ratio (RR) 0.86, 95% confidence interval (CI) 0.70 to 1.07; 8 trials, 4316 women; I2 = 78%; low‐quality evidence. It is uncertain whether the upright position has any impact on caesarean section (RR 0.94, 95% CI 0.61 to 1.46; 8 trials, 4316 women; I2 = 47%; very low‐quality evidence), instrumental vaginal birth (RR 0.90, 95% CI 0.72 to 1.12; 8 trials, 4316 women; I2 = 69%) and the duration of the second stage of labour (mean difference (MD) 6.00 minutes, 95% CI −37.46 to 49.46; 3 trials, 456 women; I2 = 96%), because we rated the quality of the evidence as very low for these outcomes. Maternal position in the second stage of labour probably makes little or no difference to postpartum haemorrhage (PPH), (PPH requiring blood transfusion): RR 1.20, 95% CI 0.83 to 1.72; 1 trial, 3093 women; moderate‐quality evidence. Maternal satisfaction with the overall childbirth experience was slightly lower in the upright group: RR 0.95, 95% CI 0.92 to 0.99; 1 trial, 2373 women. Fewer babies were born with low cord pH in the upright group: RR 0.43, 95% CI 0.20 to 0.90; 2 trials, 3159 infants; moderate‐quality evidence.
The results were less clear for other maternal or fetal outcomes, including trauma to the birth canal requiring suturing (average RR 1.00, 95% CI 0.89 to 1.13; 3 trials, 3266 women; I2 = 46%; low‐quality evidence), abnormal fetal heart patterns requiring intervention (RR 1.69, 95% CI 0.32 to 8.84; 1 trial, 107 women; very low‐quality evidence), or admission to neonatal intensive care unit (RR 0.54, 95% CI 0.02 to 12.73; 1 trial, 66 infants; very low‐quality evidence). However, the CIs around some of these estimates were wide, and we cannot rule out clinically important effects.
In our sensitivity analysis of studies at low risk of bias, upright positions increase the chance of women having an operative birth: RR 1.11, 95% CI 1.03 to 1.20; 3 trials, 3609 women; high‐quality evidence. In absolute terms, this equates to 63 more operative births per 1000 women (from 17 more to 115 more). This increase appears to be due to the increase in caesarean section in the upright group (RR 1.29; 95% CI 1.05 to 1.57; 3 trials, 3609 women; high‐quality evidence), which equates to 25 more caesarean sections per 1000 women (from 4 more to 49 more). In the sensitivity analysis there was no clear impact on instrumental vaginal births: RR 1.08, 95% CI 0.91 to 1.30; 3 trials, 3609 women; low‐quality evidence.
Authors' conclusions
There may be little or no difference in operative birth between women who adopt recumbent or supine positions during the second stage of labour with an epidural analgesia. However, the studies are heterogeneous, probably related to differing study designs and interventions, differing adherence to the allocated intervention and possible selection and attrition bias. Sensitivity analysis of studies at low risk of bias indicated that recumbent positions may reduce the need for operative birth and caesarean section, without increasing instrumental delivery. Mothers may be more satisfied with their experience of childbirth by adopting a recumbent position. The studies in this review looked at left or right lateral and semi‐recumbent positions. Recumbent positions such as flat on the back or lithotomy are not generally used due to the possibility of aorto‐caval compression, although we acknowledge that these recumbent positions were not the focus of trials included in this review.
PICO
Plain language summary
Maternal position in the second stage of labour for women with epidural anaesthesia
What is the issue?
Late labour, sometimes called the second stage, is made up of a latent or passive phase where the mother is fully dilated and the baby’s head descends without the mother pushing, and an active phase when the mother has an urge to push and the baby is born.
We wanted to find out whether different birthing positions (upright or lying down) during the second stage of labour could change birth outcomes both for women who have used an epidural for pain relief and for their babies. Outcomes included caesarean section, instrumental birth, excessive bleeding or stitches following tears to the vagina during the birth. For babies, we looked at whether they coped well with labour or needed admission to a special care baby unit. We also wanted to determine women's views on the experience of childbirth and their satisfaction with the labour. This is an update of a review first published in 2013.
Why is this important?
An epidural is the most effective method for pain relief in labour. It is popular, even though it may increase the length of the labour and the use of forceps and vacuum (ventouse) to assist the birth. Such instrumental births can cause later prolapse, urine leakage, or painful sexual intercourse. In recent years low‐dose techniques, also known as 'walking' or 'mobile' epidurals, have become popular. The low doses allow women to be more mobile during their labour and make it easier to assume an upright position. It has been suggested that such an upright position can make birth easier.
What evidence did we find?
We searched for evidence from randomised controlled trials in June 2018. This updated review now includes eight studies involving 4464 women and their babies. One of the new studies was very well conducted and accounted for three‐quarters of all women in the review. Five trials were conducted in the UK, one in France and two in Spain. They compared various upright positions with lying‐down (recumbent) positions.
Overall, there may be little or no difference between upright and lying‐down positions for caesarean section or instrumental vaginal (operative) births (8 trials, 4316 women; low‐quality evidence). The studies showed considerable variations in findings. However, when we looked only at the high‐quality studies we found a clear harm from upright positions (3 trials, 3609 women). There was evidence of an increased risk of operative birth (instrumental or caesarean birth combined) and an increase in caesarean births.
There was no difference in the number of women who had tears requiring stitches (3 trials, 3266 women; low‐quality evidence) or suffering excessive bleeding (1 trial; 3093 women; moderate‐quality evidence). It is uncertain whether the upright position has any impact on instrumental vaginal birth or the length of the second stage of labour, because we found the quality of the evidence to be very low for these outcomes.
Mothers were slightly more satisfied with lying‐down positions (1 trial, 2373 women). Although more babies had high acid levels in the cord at birth with lying‐down positions (2 trials, 3159 infants; moderate‐quality evidence), there was no other evidence of baby harm. Suitable lying‐down positions were on the left or right side, but not flat on their back nor with the legs raised in stirrups.
What does this mean?
The overall evidence did not show a clear difference in operative births for women with an epidural during the second stage of labour. Differences in how well the studies were designed and conducted and differing positions adopted may account for this. However, the high‐quality evidence showed better outcomes for women moving between lying‐down on the side positions that avoided lying flat on the back. These positions result in more normal births, a better experience and no harm to mother or baby when compared with an upright position.
Authors' conclusions
Summary of findings
| Upright position compared to recumbent position for the second stage of labour for women with epidural anaesthesia | ||||||
| Patient or population: women in the second stage of labour with epidural anaesthesia | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with recumbent position | Risk with upright position | |||||
| Maternal outcomes | ||||||
| Operative birth (caesarean or instrumental vaginal) | Study population | RR 0.86 | 4316 | ⊕⊕⊝⊝ | ‐ | |
| 554 per 1000 | 476 per 1000 | |||||
| Duration of second stage labour (minutes) (from time of randomisation to birth) | The mean duration of second stage labour across control groups ranged from 52.06 minutes to 124.3 minutes | MD 6.00 minutes higher (37.46 lower to 49.46 higher) | ‐ | 456 | ⊕⊝⊝⊝ | ‐ |
| Caesarean section | Study population | RR 0.94 | 4316 | ⊕⊝⊝⊝ | ‐ | |
| 86 per 1000 | 81 per 1000 | |||||
| Instrumental vaginal birth | Study population | RR 0.90 | 4316 | ⊕⊝⊝⊝ | ‐ | |
| 468 per 1000 | 421 per 1000 | |||||
| Trauma to birth canal requiring suturing | Study population | RR 1.00 | 3266 | ⊕⊕⊝⊝ | ‐ | |
| 840 per 1000 | 832 per 1000 | |||||
| Blood loss (greater than 500 mL) (trial authors defined it as PPH requiring blood transfusion) | Study population | RR 1.20 | 3093 | ⊕⊕⊕⊝ | ‐ | |
| 34 per 1000 | 41 per 1000 | |||||
| Infant outcomes | ||||||
| Abnormal fetal heart rate patterns, requiring intervention | Study population | RR 1.69 | 107 | ⊕⊝⊝⊝ | ‐ | |
| 41 per 1000 | 69 per 1000 | |||||
| Low cord pH | Study population | RR 0.43 | 3159 | ⊕⊕⊕⊝ | ‐ | |
| 16 per 1000 | 7 per 1000 | |||||
| Admission to neonatal intensive care unit | Study population | RR 0.54 | 66 | ⊕⊝⊝⊝ | ‐ | |
| 24 per 1000 | 13 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aLimitations in study (no blinding possible in any of the studies, with some studies at high risk for incomplete data, selective reporting and other bias) (‐1). | ||||||
| Upright position compared to recumbent position (sensitivity analyses ‐ studies at low risk of bias only) for the second stage of labour for women with epidural anaesthesia | ||||||
| Patient or population: women in the second stage of labour with epidural anaesthesia | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with recumbent position (sensitivity analyses ‐ studies at low risk of bias only) | Risk with upright position | |||||
| Operative birth (caesarean or instrumental vaginal) | Study population | RR 1.11 | 3609 | ⊕⊕⊕⊕ | ‐ | |
| 573 per 1000 | 636 per 1000 | |||||
| Caesarean section | Study population | RR 1.29 | 3609 | ⊕⊕⊕⊕ | ‐ | |
| 86 per 1000 | 111 per 1000 | |||||
| Instrumental vaginal birth | Study population | RR 1.08 | 3609 | ⊕⊕⊝⊝ | ‐ | |
| 487 per 1000 | 526 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aLimitations in study design (no blinding possible in any of the studies, unclear allocation concealment) – but most of the pooled effect comes from one study with low risk of bias for all domains apart from blinding – impossible to blind and so not downgraded for lack blinding as this is an objective measure. | ||||||
Background
Description of the condition
Epidural analgesia is commonly used as a form of pain relief in labour. Traditionally epidurals used boluses of relatively high concentrations of local anaesthesia injected into the epidural space close to the nerves that transmit pain; this also results in temporary loss of motor function in the lower limbs so that women are unable to mobilise. Newer epidural techniques have evolved through the use of lower concentrations of local anaesthesia with the addition of opiates or the use of a combined spinal‐epidural (COMET 2001), resulting in effective analgesia with less dense motor blockade. Systematic reviews of randomised controlled trials (RCTs) have found that epidural is more effective for pain relief than other non‐epidural methods (Anim‐Somuah 2018; Jones 2012). However, epidurals traditionally result in a longer second stage of labour and more instrumental deliveries (Anim‐Somuah 2005), although studies from 2005 onwards suggest that with the newer epidural dosing techniques this effect is no longer evident (Anim‐Somuah 2018). This matters because prolonged second stage of labour may increase the risk of fetal respiratory acidosis and postpartum haemorrhage (Watson 1994). Instrumental deliveries are associated with prolapse, urinary incontinence, and dyspareunia (painful intercourse) (Liebling 2004; MacLennan 2000). A survey during 2005 and 2006 showed that 22% of all births in UK National Health Service (NHS) hospitals involved an epidural (Richardson 2007); this rate has remained stable, with 25% of women using an epidural for labour in 2013 (Wong 2015); in other countries, for example, Canada and France, epidural rates may be even higher. This is why strategies to shorten the second stage of labour and reduce instrumental deliveries in this setting are important.
There are several proposed mechanisms for the association between epidurals and increased instrumental deliveries. Epidurals increase the risk of malposition of the fetal head, in particular the fetal occiput‐posterior position, a key factor in instrumental delivery and prolonged labour (Lieberman 2005; Martino 2007). Secondly, epidurals may interfere with the release of oxytocin as the pelvic floor stretches in the late second stage of labour (Goodfellow 1983; Rahm 2002). Finally, epidurals may inhibit the mother's bearing‐down reflex at the same time.
Description of the intervention
With the advancement of low‐dose epidural techniques, also known as 'walking' or 'mobile' epidurals, women with an epidural are now being provided with the opportunity to remain mobile during their labour, and to adopt some upright positions such as standing and ambulation which may not be possible for women with a traditional epidural (COMET 2001). It was estimated in 2009 that only 10% of obstetrics units in the UK were still using 'conventional' or traditional epidural doses (Prabhu 2009). The use of ambulation during labour has been associated with more efficient uterine action, labours of a shorter duration, and aiding the descent of the fetal head through encouraging the effects of gravity (COMET 2001; Flynn 1978). The use of low‐dose epidurals is also thought to aid the maternal efforts required to give birth through the preservation of motor function (COMET 2001). The increased number of vaginal births seen with this form of analgesia is thought to be due to the ability of the women to adopt an upright position during labour (COMET 2001).
How the intervention might work
One suggestion to reduce adverse outcomes in labour with an epidural is the use of alternative maternal birth positions. Although it has become more common in the West to give birth in the supine position, this position may result in a higher number of instrumental deliveries and episiotomies (De Jonge 2004). In women without an epidural, a number of observational studies have suggested that birthing in an upright position results in shorter labours, lower incidence of instrumental deliveries and episiotomies, and is a more comfortable birth position (Bodner‐Adler 2003; Méndez‐Bauer 1975). Some small RCTs (e.g. Chen 1987) and two systematic reviews (De Jonge 2004; Gupta 2017) have confirmed this. It has been proposed that these benefits are due to a higher resting intrauterine pressure which contributes to the downward birth force and the bearing‐down forces (Chen 1987), as well as contractions of a greater intensity (Méndez‐Bauer 1975).
Another possible way to facilitate normal birth may be to adopt more recumbent positions that take the body weight off the sacrum and allow the pelvic outlet to expand, and has also been postulated to have a positive impact on blood flow in the region. Although it would be possible to classify positions into 'weight on' and 'weight off' the sacrum, and examine trials that compared such positions, we have not done this in our review.
Why it is important to do this review
Although a Cochrane Review (Gupta 2017) has assessed the use of upright positions in the second stage of labour, it excluded women with epidurals, and the findings therefore cannot be generalised. The benefits noted in women without an epidural may potentially offset some of the effect an epidural may have on prolongation of labour, and highlights the importance of carrying out this systematic review. Our review tests the effect of upright versus recumbent positions in women with all types of epidural. We recognise that some upright or vertical positions, such as ambulation, standing and squatting, as well as some recumbent positions, such as knee chest, may be difficult for women with a traditional epidural to maintain. However, other vertical positions, for example, sitting supported, are possible even with a traditional epidural, so we have included traditional epidurals as a subgroup in the analysis. We have also included a planned subgroup analysis of trials conducted in women with a mobile epidural.
This is an update of a Cochrane Review first published in 2013 (Kemp 2013), and is consequent upon the publication of further clinical trials on this question.
Objectives
To assess the effects of different birthing positions (upright and recumbent) during the second stage of labour, on important maternal and fetal outcomes for women with epidural analgesia.
Methods
Criteria for considering studies for this review
Types of studies
All randomised or quasi‐randomised trials. Cluster‐randomised controlled trials would have been eligible for inclusion in this review, but we found none. Studies published in abstract form only were eligible for inclusion. Where we needed further information, we planned to contact the authors of relevant studies.
Types of participants
All pregnant women (primigravidae and multigravidae) in the second stage of induced or spontaneous labour receiving epidural analgesia. We included women with any type of epidural. We included women recruited and randomised in any stage of labour. We only included singleton pregnancies at 36 weeks gestation onwards.
Types of interventions
We assumed the experimental type of intervention to be the maternal use of any upright position during the second stage of labour, compared with the control intervention of the use of any recumbent position. We included trials in which the intervention (upright or recumbent) was confined to the second stage of labour, and also where it was performed in the first stage of labour but also continued into the second stage.
The second stage of labour can be divided into two distinct phases: the latent phase (also known as the passive phase), and the active phase. We defined the latent phase as the period of time from full dilatation until the head has descended to the pelvic floor, with the mother experiencing no desire to push. We defined the active phase as the period from the head descending to the pelvic floor until the birth of the baby, with the mother having a strong desire to push (O'Driscoll 2003).
We classified studies as either a comparison of an upright versus a recumbent position in the latent phase of the second stage of labour, or as a comparison of an upright versus a recumbent position in the active phase of the second stage of labour. We considered studies eligible for inclusion if the intention was that participants spent at least 30% of time in the relevant phase of second‐stage labour in the allocated position. Finally, studies that compared an upright position in both phases of the second stage with a recumbent position in both phases of the second stage formed a third group. There are three potential time phases in which the effects of different positions can be studied: namely the latent phase, the active phase, and both.
We initially categorised the birthing positions as upright (the main axis of the body was more than 45 ° from the horizontal) or recumbent (the main axis of the body was less than 45 ° from the horizontal).
Upright positions included:
-
sitting (on a bed);
-
sitting (on a tilting bed more than 45 ° from the horizontal);
-
squatting (unaided or using squatting bars);
-
squatting (aided with a birth cushion);
-
semi‐recumbent (i.e. classified as an upright position if the main axis of the body (chest and abdomen) was 45 ° or more from the horizontal);
-
kneeling (upright, leaning on the head of the bed, or supported by a partner);
-
walking (only for comparison of positions in the latent phase).
Recumbent positions included:
-
lithotomy position;
-
lateral position (left or right);
-
Trendelenburg's position (head lower than pelvis);
-
knee‐elbow (all fours) position; this is considered recumbent because the axis of the trunk is horizontal;
-
semi‐recumbent (i.e. classed as a recumbent position if the main axis of the body (chest and abdomen) was less than 45 ° from the horizontal).
A number of other names have been used for birthing positions, including:
-
Fowler;
-
tug‐of‐war;
-
throne.
We delayed classifying these until after we had identified the trials. We planned to classify them from the Methods section without knowledge of the trial results, again using the dividing line of the body at 45 ° from the horizontal.
Some trials may compare positions with varying degrees of uprightness, which fall the same side of the 45 ° dividing line. For example, a study might compare the horizontal position (0 °) with semi‐recumbent (40 °). So long as the two groups clearly differed in degree of verticality, we planned to classify them as 'more vertical' and 'less vertical'.
We found no studies reporting 'Fowler', 'tug of war' or 'throne' positions and no 'more vertical/less vertical' studies.
Types of outcome measures
Primary outcomes
Maternal outcomes
-
Operative birth (defined as caesarean section or vaginal instrumental delivery)
-
Duration of second‐stage labour. Since the assessment of the onset of second‐stage labour is susceptible to bias, we reported and analysed the randomisation‐to‐birth interval, where available.
Secondary outcomes
Maternal outcomes
-
Caesarean section
-
Instrumental vaginal birth (forceps or ventouse (vacuum))
-
Trauma to birth canal, requiring suturing
-
Blood loss (greater than 500 mL, or as defined by trial authors)
-
Prolonged second stage, defined as pushing for more than 60 minutes (or as defined by trial authors)
-
Maternal experience and satisfaction with labour
Baby outcomes
-
Abnormal fetal heart rate patterns, requiring intervention
-
Apgar score of less than seven at five minutes (or as defined by trial authors)
-
Low cord pH less than 7.1 (or as defined by trial authors)
-
Admission to neonatal intensive care unit
-
Need for ventilation
-
Perinatal death
Search methods for identification of studies
The following Methods section of this review is based on a standard template used by Cochrane Pregnancy and Childbirth.
Electronic searches
For this update, we searched Cochrane Pregnancy and Childbirth’s Trials Register by contacting their Information Specialist (5 June 2018).
The Register is a database containing over 25,000 reports of controlled trials in the field of pregnancy and childbirth. It represents over 30 years of searching. For full current search methods used to populate Pregnancy and Childbirth’s Trials Register including the detailed search strategies for CENTRAL, MEDLINE, Embase and CINAHL; the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service, please follow this link
Briefly, Cochrane Pregnancy and Childbirth’s Trials Register is maintained by their Information Specialist and contains trials identified from:
-
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
-
weekly searches of MEDLINE (Ovid);
-
weekly searches of Embase (Ovid);
-
monthly searches of CINAHL (EBSCO);
-
handsearches of 30 journals and the proceedings of major conferences;
-
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Two people screen the search results and review the full text of all relevant trial reports identified through the searching activities described above. Based on the intervention described, each trial report is assigned a number that corresponds to a specific Pregnancy and Childbirth review topic (or topics), and is then added to the Register. The Information Specialist searches the Register for each review using this topic number rather than keywords. This results in a more specific search set that has been fully accounted for in the relevant review sections (Included studies; Excluded studies).
In addition, we searched ClinicalTrials.gov and the WHO International Clinical Trials Registry Platform (ICTRP) for unpublished, planned and ongoing trial reports (5 June 2018), using the search methods detailed in Appendix 1.
Searching other resources
We searched the reference lists of retrieved studies. We did not apply any language or date restrictions.
Data collection and analysis
For methods used in the previous version of this review, see Kibuka 2017.
The following Methods section of this review is based on a standard template used by Cochrane Pregnancy and Childbirth.
Selection of studies
Two review authors independently assessed for inclusion all studies identified as a result of the search strategy. We resolved any disagreement through discussion or, if required, we consulted a third person.
Data extraction and management
We designed a form to extract data. For eligible studies, two review authors extracted the data using the agreed form. We resolved discrepancies through discussion or, if required, we consulted a third person. We entered data into Review Manager 5 (RevMan 5) software (RevMan 2014) and checked them for accuracy.
When information about any of the above was unclear, we planned to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Two review authors independently assessed risks of bias for each study, using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a), resolving any disagreement by discussion or by involving a third person.
(1) Random sequence generation (checking for possible selection bias)
We describe for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
-
low risk of bias (any truly random process, e.g. random‐number table; computer random‐number generator);
-
high risk of bias (any non‐random process, e.g. odd or even date of birth, hospital or clinic record number);
-
unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We describe for each included study the method used to conceal allocation to interventions prior to assignment and assessed whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
-
low risk of bias (e.g. telephone or central randomisation, consecutively‐numbered sealed opaque envelopes);
-
high risk of bias (open random allocation, unsealed or non‐opaque envelopes, alternation, date of birth);
-
unclear risk of bias.
(3.1) Blinding of participants and personnel (checking for possible performance bias)
We describe for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that studies were at low risk of bias if they were blinded, or if we judged that the lack of blinding was unlikely to affect results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods as:
-
low, high or unclear risk of bias for participants;
-
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
We describe for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed methods used to blind outcome assessment as:
-
low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We describe for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported, and the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or could be supplied by the trial authors, we planned to re‐include missing data in the analyses that we undertook.
We assessed methods as:
-
low risk of bias (e.g. no missing outcome data, missing outcome data balanced across groups);
-
high risk of bias (e.g. numbers or reasons for missing data unbalanced across groups, ‘as treated’ analysis done with substantial departure of intervention received from that assigned at randomisation);
-
unclear risk of bias.
(5) Selective reporting (checking for reporting bias)
We describe for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
-
low risk of bias (where it was clear that the study had been prospectively registered, all of the study’s prespecified outcomes and all expected outcomes of interest to the review had been reported);
-
high risk of bias (where the study was registered but not all the study’s prespecified outcomes had been reported; one or more reported primary outcomes were not prespecified; outcomes of interest were reported incompletely and so could not be used; study failed to include results of a key outcome that would have been expected to have been reported);
-
unclear risk of bias.
(6) Other bias (checking for bias due to problems not covered by (1) to (5) above)
We described for each included study any important concerns we had about other possible sources of bias.
(7) Overall risk of bias
We made explicit judgements about whether studies were at high risk of bias, according to the criteria given in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). With reference to (1) to (6) above, we planned to assess the likely magnitude and direction of the bias and whether we considered it was likely to impact on the findings. We explored the impact of the level of bias through undertaking sensitivity analyses ‐ see Sensitivity analysis.
Assessment of the quality of the evidence using the GRADE approach
For this update we assessed the quality of the evidence using the GRADE approach, as outlined in the GRADE handbook, in order to assess the quality of the body of evidence relating to the following outcomes for the main comparison: upright position versus recumbent position.
Maternal outcomes
-
Operative birth (defined as caesarean section or vaginal instrumental delivery)
-
Duration of second‐stage labour
-
Caesarean section
-
Instrumental vaginal birth (forceps or ventouse (vacuum))
-
Trauma to birth canal, requiring suturing
-
Blood loss (greater than 500 mL, or as defined by trial authors)
Infant outcomes
-
Abnormal fetal heart rate patterns, requiring intervention
-
Low cord pH less than 7.1 (or as defined by trial authors)
-
Admission to neonatal intensive care unit
We also assessed the quality of the evidence using the GRADE approach for the following outcomes for the sensitivity analyses of studies at low risk of bias.
-
Operative birth
-
Caesarean section
-
Instrumental vaginal birth
'Summary of findings' tables
We used the GRADEpro Guideline Development Tool to import data from RevMan 5 (RevMan 2014) in order to create ’Summary of findings’ tables. We produced a summary of the intervention effect and a measure of quality for each of the above outcomes using the GRADE approach. The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence for each outcome. The evidence can be downgraded from 'high quality' by one level for serious (or by two levels for very serious) limitations, depending on assessments for risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
Measures of treatment effect
Dichotomous data
For dichotomous data, we present results as a summary risk ratio (RR) with a 95% confidence interval (CI).
Continuous data
We used the mean difference (MD) if outcomes were measured in the same way between trials. In future updates, we will use the standardised mean difference to combine trials that measured the same outcome, but use different methods.
Unit of analysis issues
Cluster‐randomised trials
In future updates, we will include cluster‐randomised trials in the analyses along with individually‐randomised trials. We will adjust their sample sizes or standard errors appropriately, using the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Section 16.3.4 or 16.3.6 respectively), using an estimate of the intracluster correlation co‐efficient (ICC) derived from the trial if possible, from a similar trial or from a study of a similar population (Higgins 2011b). If we use ICCs from other sources, we will report this and will conduct sensitivity analyses to investigate the effect of variation in the ICC. If we identify both cluster‐randomised trials and individually‐randomised trials, we plan to synthesise the relevant information. We will consider it reasonable to combine the results from both if there is little heterogeneity between the study designs and if we consider the interaction between the effect of intervention and the choice of randomisation unit to be unlikely.
We will also acknowledge heterogeneity in the randomisation unit and perform a sensitivity analysis to investigate the effects of the randomisation unit.
Cross‐over trials
It is not appropriate to include cross‐over design trials in this review.
Other unit of analysis issues
Multiple pregnancies
We include only women with singleton pregnancies in this review. In future updates, we will exclude trials of women with multiple pregnancies.
Trials with more than one treatment arm
If we had identified a trial with more than one treatment arm, we would have followed the most appropriate method for dealing with multiple groups, as described in section 16.5 of the Handbook (Higgins 2011b): combined groups to create a single pair‐wise comparison; or selected one pair of interventions and excluded the others; or split the ‘shared’ group into two or more groups with smaller sample size, and include two or more (reasonably independent) comparisons.
Dealing with missing data
For included studies, we noted levels of attrition. In future updates, if more eligible studies are included, we will explore the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using sensitivity analysis.
For all outcomes, we carried out analyses, as far as possible, on an intention‐to‐treat basis, i.e. we attempted to include all participants randomised to each group in the analyses. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta‐analysis using the Tau2, I2 (Higgins 2003) and Chi2 statistics. We regarded heterogeneity as substantial if I2 was greater than 30% and either Tau2 was greater than zero, or there was a low P value (less than 0.10) in the Chi2 test for heterogeneity. If we identified substantial heterogeneity (above 30%), we explored it by prespecified subgroup analysis (Deeks 2011).
Assessment of reporting biases
In future updates, if there are 10 or more studies in the meta‐analysis we will investigate reporting biases (such as publication bias) using funnel plots. We will assess funnel plot asymmetry visually. If asymmetry is suggested by a visual assessment, we will perform exploratory analyses to investigate it (Sterne 2011).
Data synthesis
We carried out statistical analysis using RevMan 5 software (RevMan 2014). Since all analyses included trials comparing different upright and recumbent positions, we used the random‐effects model throughout. We treated the random‐effects summary as the average of the range of possible treatment effects and we have discussed the clinical implications of treatment effects differing between trials. If the average treatment effect was not clinically meaningful we did not combine trials.
For random‐effects analyses, we have presented the results as the average treatment effect with its 95% CI, and the estimates of Tau2 and I2.
Subgroup analysis and investigation of heterogeneity
If we identified substantial heterogeneity, we investigated it using subgroup analyses and sensitivity analyses.
We planned to carry out the following subgroup analyses.
-
Time of epidural: sited in the first stage of labour or sited in the second stage of labour.
-
Type of epidural: traditional versus 'mobile' or 'walking'. We classified low‐dose combined spinal epidurals and low‐dose infusion epidurals as 'walking'.
-
Nulliparous versus multiparous women.
-
Oxytocin used/not used in the second stage.
Due to insufficient data we were only able to carry out subgroup analysis 2. Type of epidural.
We used the following outcomes in subgroup analyses.
-
Operative birth. Caesarean section or instrumental vaginal birth.
-
Duration of second‐stage labour. Since the assessment of the onset of second stage is susceptible to bias, we have reported and analysed the randomisation‐to‐birth interval, where available.
-
Caesarean section.
-
Instrumental vaginal birth.
We assessed subgroup differences by interaction tests available within RevMan 5 (RevMan 2014). We report the results of subgroup analyses quoting the Chi2 statistic and P value, and the interaction test I2 statistic value.
Sensitivity analysis
We carried out sensitivity analyses to explore the effect of trial quality. This involved an analysis limited to trials at low risk of bias. We restricted analysis to those trials with 'adequate' 'Risk of bias' judgements by excluding studies with high or unclear risk of bias for both allocation concealment and incomplete outcome data. We also planned to exclude studies from this low‐risk‐of‐bias analysis where the outcome assessor was not blinded, with the exception of the outcomes perinatal death, mode of birth and duration of second stage (randomisation to birth). None of the included studies blinded outcome assessment so we did not conduct this analysis. In future updates, if there are adequate data, we will perform this analysis.
Results
Description of studies
Results of the search
See: Figure 1.

Study flow diagram.
For this 2018 update, we retrieved 202 citations and screened out 195 (not a trial or outside the scope of this review). We also re‐assessed two trials that were awaiting further classification, two that were ongoing in the previous version of the review and one found by searching reference lists of retrieved studies. This yielded 15 full trial reports to assess in total.
We included three new trials (11 reports), and excluded two (four reports). This review now includes eight trials (Boyle 2001; BUMPES 2017; Downe 2004; Golara 2002; Karraz 2003; Simarro 2017; Theron 2011 (abstract only); Walker 2012), having excluded eight trials in total (Amiri 2012; Asselineau 1996; Collis 1999; Danilenko‐Dixon 1996; Hofmeyr 2018, Martin 2011; Thies‐Lagergren 2011; Zaibunnisa 2015).
Included studies
Four studies (Boyle 2001; Golara 2002; Simarro 2017; Theron 2011) did not report their funding source. One study (BUMPES 2017) was funded by the National Institute for Health Research (NIHR) through its Health Technology Assessment (HTA) programme (project No. 08.22.02), one study (Downe 2004) by Southern Derbyshire Acute Hospitals NHS Trust, one study (Karraz 2003) by the Department of Anaesthesiology and Obstetrics & Gynaecology in Beauvais Central Hospital, and one study (Walker 2012) by the Health Research Fund of the Carlos III Health institute of the Spanish Ministry of Health (Pi 05/1235), with additional financial aid from the European University of Madrid. Authors of the BUMPES 2017, Simarro 2017 and Walker 2012 trials included a declaration of conflicts of interest; this is not reported by the rest of the studies. Boyle 2001 recruited between 1999 and 2000, BUMPES 2017 between 2010 and 2014, Downe 2004 between 1993 and 1994, Karraz 2003 between 1999 and 2001, Simarro 2017 between 2010 and 2011, and Golara 2002 did not report the recruitment period although this must have been before 1996 when their results were first reported in abstract. Theron 2011 and Walker 2012 did not report trial recruitment dates.
We have included eight studies, involving 4464 women, in the review, see Characteristics of included studies.
Methods
All eight studies were randomised controlled trials using individual randomisation.
Participants
Boyle 2001 and Karraz 2003 included both nulliparous and multiparous women in induced or spontaneous labour with an effective low‐dose mobile epidural. Golara 2002 and BUMPES 2017 also compared women with mobile epidurals, but only included nulliparous women.
Downe 2004 included primiparous women with an effective traditional epidural. Theron 2011 also only included nulliparous women, but did not specify whether the epidural was mobile or traditional. Simarro 2017 and Walker 2012 included both nulliparous and multiparous women but again did not clearly specify the type of epidural.
All trials only included women with singleton pregnancies at term (37 weeks or above gestation), or above 36 weeks' gestation (Downe 2004; Karraz 2003; Walker 2012).
Settings
All trials took place in hospital settings in the UK (Boyle 2001; BUMPES 2017; Downe 2004; Golara 2002; Theron 2011), France (Karraz 2003) or Spain (Simarro 2017; Walker 2012).
Interventions and comparisons
All the included studies had two intervention groups that could be classified into an upright or recumbent position, using the criteria in the Methods section.
Downe 2004 compared "lateral (left‐ or right‐facing positions)" and "sitting positions (supported upright sitting position)". Golara 2002 compared "recumbent (as much time as possible in bed or a chair)" and "upright (as much time as possible during the passive phase either standing or walking)" and after one hour, their chosen pushing position was allowed. Boyle 2001 compared ambulant (walking around for at least 15 minutes every hour, up to the point of active voluntary pushing) and non‐ambulant (usual care, where the women were non‐ambulant for most of the labour). Karraz 2003 compared "ambulatory (walking, sitting in a chair, reclining in semi‐supine position)" with "non‐ambulatory (not allowed to sit or walk, had to remain in the supine, semi‐supine or lateral position)". Theron 2011 compared a "sitting position" with a "lateral position" during the passive second stage of labour, usually one hour. BUMPES 2017 compared an "upright" position, which would maintain the pelvis in as vertical a plane as possible (and could include walking, standing, sitting, supported kneeling or any other upright position) to "lying down" to maintain the pelvis in a horizontal plane (left or right lateral and up to 30 º inclination of the bed). Simarro 2017 compared the intervention of "postural changes" for between five and 30 minutes under the guidance of an attending physiotherapist (including sitting, kneeling, hands‐and‐knees, lateral decubitus and supine) to the "control" of a traditional supine position. Walker 2012 studied an "alternative model of birth" which consisted of two consecutive interventions in the second stage; firstly to move to different positions (including sitting, kneeling, hands‐and‐knees or lateral decubitus) and secondly delayed onset of pushing in the modified lateral Gasquet (decubitus) position. The comparator was a "traditional model of birth" with birth in the lithotomy position and a flexed trunk, with active pushing encouraged from diagnosis of full dilatation, i.e. no passive second stage.
Five studies (BUMPES 2017; Downe 2004; Golara 2002; Theron 2011; Walker 2012) specifically restricted the period of randomisation to the second stage of labour. One study (Boyle 2001) explicitly, and one (Karraz 2003) implicitly, also included the first stage of labour within the period of randomisation. However, since both studies included the passive second stage within the period of randomisation, we have included them in this review. We recognise that there will be some overlap between these studies and the Cochrane Review Maternal positions and mobility in the first stage of labour (Lawrence 2013). One study (Simarro 2017) did not specify the period of randomisation.
All the studies had their own entry and exclusion criteria, which can be seen in the Characteristics of included studies tables.
Outcomes
All studies reported operative deliveries including instrumental delivery and caesarean section. BUMPES 2017 and Downe 2004 were the only studies to report instrumental deliveries for fetal distress. Trauma to the birth canal requiring suturing was reported by three trials (BUMPES 2017; Downe 2004; Golara 2002). BUMPES 2017 is the only trial to report a postpartum haemorrhage (PPH), which was defined as a PPH requiring blood transfusion within the trial. Maternal experience and satisfaction of labour was reported in one study (BUMPES 2017).
The duration of second stage of labour was reported by Downe 2004, Simarro 2017 and Walker 2012. Golara 2002 also reported duration of second stage of labour but only the median and range, and BUMPES 2017 only reported it as a geometric mean. We contacted the two trial authors to see if the raw data or means and standard deviations were available, but we could not obtain them so we could not include the data in the review. Karraz 2003 randomised women in the first stage of labour and reported the duration of labour as the time between epidural insertion and birth, so duration included the first stage of labour; we excluded the study from the analysis of duration of second stage of labour.
BUMPES 2017 and Golara 2002 reported low cord pH, and only Golara 2002 reported admission to neonatal intensive care unit. BUMPES 2017 reported admission to a "higher level of care" and included admission to the neonatal unit and transitional care combined; we therefore could not include it in the meta‐analysis. Low Apgar scores were variably defined and reported.
Excluded studies
We excluded one study because it was not a randomised controlled trial (Asselineau 1996). We excluded Collis 1999 because it compared upright versus recumbent position in the first stage of labour only (when cervical full dilation was identified, the women returned to their beds). We excluded Danilenko‐Dixon 1996 because it did not compare an upright position with a lateral position (it compared two recumbent positions (supine and lateral)). We excluded Amiri 2012, Thies‐Lagergren 2011 and Zaibunnisa 2015 because they included participants without epidural, Hofmeyr 2018 included too few participants with an epidural to allow subgroup analysis, and Martin 2011 compared modified Sims position (lateral position) with Sims (lateral position) or semi‐Fowler positions (semi‐recumbent position).
For more details, see Characteristics of excluded studies tables.
Risk of bias in included studies
Overall we considered three studies to be at low risk of bias (Boyle 2001; BUMPES 2017; Downe 2004), with four other studies assessed as being at high risk of bias for allocation concealment and incomplete outcome data (Golara 2002; Karraz 2003; Simarro 2017; Theron 2011) and one study (Walker 2012) at high risk due to the co‐intervention of varying the timing of active pushing (See summaries of risk of bias Figure 2; Figure 3).

Risk of bias summary: review authors' judgements about each risk of bias item for each included study

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
Six trials reported either using "computer‐generated random numbers" (low risk of bias) (Boyle 2001; BUMPES 2017; Downe 2004; Golara 2002; Theron 2011; Walker 2012) and one said that participants were "randomly divided into two groups" (Karraz 2003) (unclear risk of bias). One trial (Simarro 2017) did not report the method of randomisation, which was conducted two days a week (unclear risk of bias).
For allocation concealment BUMPES 2017 used a web‐based, central randomisation with allocation concealment facilitated by random permuted blocks so that staff could not predict the next allocation (low risk of bias). In one study (Walker 2012) participant allocation was prepared by a researcher with no clinical involvement in the trial (low risk of bias). Three trials used envelopes that were either opaque (Downe 2004) or sealed brown (Golara 2002) or sealed (Boyle 2001), but if the numbering, sealed status, or opacity of the envelopes was not reported in all cases, we judged the risk of bias to be 'unclear'. Three trials did not report the allocation sequence concealment (Karraz 2003; Simarro 2017; Theron 2011), and we also rated them as 'unclear'.
Blinding
None of the studies masked the participants or the assessor to the treatment allocation. We assessed all of the studies as high risk of bias, as some of the outcomes may have been influenced by this lack of blinding.
Incomplete outcome data
Three studies (Boyle 2001; Downe 2004; Walker 2012) reported results for all participants randomised (low risk of bias). One study (BUMPES 2017) excluded 4.4% of women (143/3236) from analysis of the primary outcome but the study includes reasons for exclusions that are balanced across groups (low risk of bias). We rated the other studies as having 'unclear' (Karraz 2003; Simarro 2017) or 'high' (Golara 2002; Theron 2011) risks of bias for post‐randomisation exclusions. Golara 2002 had unbalanced groups (41 versus 25) that were not accounted for and there were discrepancies in the numbers reported. Theron 2011 reported 43 participants who dropped out after consent, but did not clarify if this was also post‐randomisation.
Selective reporting
One study (BUMPES 2017) prospectively registered its protocol and reported all expected outcomes (low risk of bias). We rated Theron 2011 as being at high risk of reporting bias because it did not report its planned secondary outcomes of maternal acceptability, cardiotocograph abnormality and neonatal outcomes, and had not registered the trial protocol. Similarly, we rated Walker 2012 as high risk, as outcomes differ slightly between the conference proceedings and the full publication and some of the neonatal outcomes are not fully reported for each group. The protocol was not registered and the primary outcome of perineal trauma (defined as trauma requiring suturing) is not reported clearly, but separately for episiotomy and tears without reporting the number of women requiring suturing for either or both. The other five trials had also not registered trial protocols (Boyle 2001; Downe 2004; Golara 2002; Karraz 2003; Simarro 2017) and we rated these as unclear risk of bias.
Other potential sources of bias
BUMPES 2017 was the only study to independently register its sample size, primary endpoint and other aspects of the analysis plan, and we judged it to be at low risk of other bias. We considered two studies to be at high risk of other bias due to sample size issues: Theron 2011 reported a sample size of 77 that was much lower than the intended sample size of 300, and Golara 2002 also reported that their sample size of 66 was lower than the target size of 300. One study (Walker 2012) we rated at high risk due to co‐intervention as the traditional (control) group started pushing as soon as second stage was diagnosed whereas the experimental group, as well as undergoing postural changes, were instructed to delay pushing for up to 120 minutes unless they felt an urge to push. We rated the four other included studies as being at an unclear risk of other bias.
Effects of interventions
See: Summary of findings for the main comparison Upright position compared to recumbent position for the second stage of labour for women with epidural anaesthesia; Summary of findings 2 Upright position compared to recumbent position (sensitivity analyses ‐ studies at low risk of bias only) for the second stage of labour for women with epidural anaesthesia
Comparison: upright position versus recumbent position
Primary outcomes
We identified data for 15 of our prespecified outcomes. We were able to perform six meta‐analyses. Since all analyses included trials comparing different upright and recumbent positions, we have used the random‐effects model throughout. We conducted sensitivity analyses to test the robustness of the analyses, by excluding studies with high or unclear risk of bias both for allocation concealment and for incomplete outcome data. Where possible we carried out analyses according to subgroups by type of epidural: traditional versus 'mobile' or 'walking'. We classified low‐dose combined spinal epidurals and low‐dose infusion epidurals as 'mobile' or 'walking'.
Operative birth (defined as caesarean section or vaginal instrumental birth)
Overall, upright positions may make little or no difference on the rates of operative birth when compared to recumbent positions (caesarean or instrumental vaginal): average risk ratio (RR) 0.86, 95% confidence interval (CI) 0.70 to 1.07; 8 trials, 4316 women; Tau2 = 0.06, I² = 78%; low‐quality evidence; Analysis 1.1. There was no evidence of a subgroup difference between mobile and traditional epidurals according to the subgroup interaction test (test for subgroup differences: Chi2 = 1.32, df = 1 (P = 0.25), I2 = 24.3%), although it should be noted that there were opposite directions of effect for each subgroup: favouring the recumbent position for the mobile group, and favouring the upright position for the traditional group.
We also performed the planned sensitivity analysis by excluding four studies with high or unclear risk of bias for both allocation concealment and incomplete outcome data (Golara 2002; Karraz 2003; Simarro 2017; Theron 2011). We also excluded Walker 2012, as this study was complicated by a co‐intervention of difference in timing of the active second stage. When we restricted analysis to studies at low risk of bias, upright positions appear to increase the chance of women having an operative birth: average RR 1.11, 95% CI 1.03 to 1.20; 3 trials, 3609 women; Tau2 = 0.00; I2 = 12%; high‐quality; Analysis 2.1. Additionally, there was a notable increase in operative birth rate in the upright group in the subgroup of high‐quality studies using mobile epidurals: average RR 1.10, 95% CI 1.04 to 1.16; 2 trials; 3502 women; Tau² = 0.00, I² = 0%.
Duration of second stage of labour
We identified no clear difference and inconsistent results for duration of the second stage of labour, measured as the randomisation‐to‐birth interval in minutes: mean difference (MD) 6.00 minutes; 95% CI −37.46 to 49.46; 3 trials, 456 women; Tau2 = 1404.42, I2 = 96%; very low‐quality evidence; Analysis 1.2. Note the high degree of heterogeneity between the three trials included in the analysis of duration of second stage of labour. There were no data available for analysis of the studies that used mobile epidurals. Karraz 2003, which randomised in the first stage of labour, reports results for duration of labour (defined as time between epidural insertion and delivery) rather than duration of second stage, and has therefore been excluded from this analysis. We contacted the authors of several studies (BUMPES 2017; Downe 2004; Golara 2002; Walker 2012) requesting raw data or means and standard deviations for the labour duration but we could not obtain them and therefore could not include the data in the review.
Secondary outcomes
Maternal outcomes
Caesarean section
It is uncertain whether there is any difference between upright and recumbent position in caesarean section, because the quality of the evidence was very low: average RR 0.94, 95% CI 0.61 to 1.46; 8 trials, 4316 women; Tau2 = 0.13, I2 = 47%; Analysis 1.3. There was evidence of a subgroup difference between mobile and traditional epidurals according to the subgroup interaction test (test for subgroup differences: Chi2 = 3.26, df = 1 (P = 0.07), I2 = 69.4%). There appear to be opposite directions of effect for each subgroup, again favouring the recumbent position for the mobile group and favouring the upright position for the traditional group.
However, planned sensitivity analysis of the three studies at low risk of bias demonstrated an increase in caesarean section rates in the upright group: average RR 1.29, 95% CI 1.05 to 1.57; 3 trials, 3609 women; Tau2 = 0.00, I2 = 0%; high‐quality evidence Analysis 2.2.
Instrumental birth (forceps or ventouse (vacuum))
It is uncertain whether there is any difference between upright and recumbent position in instrumental birth, because the quality of the evidence was very low: average RR 0.90, 95% CI 0.72 to 1.12; 8 trials, 4316 women; Tau2 = 0.06, I2 = 69%; Analysis 1.4. There was no evidence of a subgroup difference between mobile and traditional epidurals according to the subgroup interaction test (test for subgroup differences: Chi2 = 0.79, df = 1 (P = 0.38), I2 = 0%), although it should be noted that there were opposite directions of effect for each subgroup, favouring the recumbent position for the mobile group and favouring the upright position for the traditional group.
Planned sensitivity analysis of the three studies at low risk of bias also showed that position may make little or no difference in instrumental birth based on position in the second stage of labour: average RR 1.08, 95% CI 0.91 to 1.30; 3 trials, 3609 women; Tau2 = 0.01, I2 = 49%; low‐quality evidence; Analysis 2.3.
Trauma to birth canal, requiring suturing
Positions may make little or no difference on trauma to birth canal requiring suturing: average RR 1.00, 95% CI 0.89 to 1.13; 3 trials, 3266 women; Tau2 = 0.01, I2 = 46%; low‐quality evidence; Analysis 1.5.
Postpartum haemorrhage
This outcome was only reported in one study (BUMPES 2017), which they defined as PPH requiring blood transfusion. Position probably makes little or no difference in the number of women with a PPH: average RR 1.20, 95% CI 0.83 to 1.72; 1 trial, 3093 women; moderate‐quality evidence; Analysis 1.6.
Prolonged second stage
This outcome was only reported in one study (Walker 2012) and influenced by the co‐intervention of immediate pushing in the upright group compared to delay of up to 120 minutes in the recumbent group. Findings suggested that the time pushing may be slightly lower in the upright group (MD ‐16.37 minutes, 95% CI ‐24.55 to ‐8.19 minutes; 1 trial, 199 women; Analysis 1.7).
Maternal experience and satisfaction with labour
This outcome was only assessed in one trial (BUMPES 2017), and was measured using a self‐completed maternal satisfaction questionnaire. The questionnaire consisted of 11 domains/statements (questions). For each domain or statement, women were asked to indicate whether they agreed with the statement or not by choosing one of five categories: strongly agree, agree, neutral, disagree, strongly disagree. We dichotomised the data and combined counts for the 'strongly agree' and 'agree' domains, as presented in Analysis 1.8. The results for maternal satisfaction were similar between the upright and recumbent groups for most domains. However women in the upright groups were overall less likely to feel satisfied with childbirth: RR 0.95, 95% CI 0.92 to 0.99; 1 trial, 2373 women.
Baby outcomes
Abnormal fetal heart rate patterns, requiring intervention
It is uncertain whether position has any effect on abnormal fetal heart rate patterns, because the quality of the evidence was very low and the outcome was only reported in one trial (Downe 2004): RR 1.69, 95% CI 0.32 to 8.84; 1 trial, 107 women; very low‐quality evidence; Analysis 1.9.
Low cord pH less than 7.1 (or as defined by trial authors)
Fewer babies were found to have low cord pH in the upright group: RR 0.43, 95% CI 0.20 to 0.90; 2 trials, 3159 infants; moderate‐quality evidence; Analysis 1.12. The largest study (BUMPES 2017) defined low cord pH as umbilical artery pH less than 7.05 with a base deficit greater than or equal to 12 mmol/L; Golara 2002 defined low cord pH as less than 7.2.
Admission to neonatal intensive care unit and need for ventilation
It is uncertain whether position has any effect on admission to neonatal intensive care unit because the quality of the evidence was very low, and there was only one admission in the recumbent group: RR 0.54, 95% CI 0.02 to 12.73; 1 trial, 66 infants; very low‐quality evidence; Analysis 1.13. One study reported on the need for ventilation and found no difference between the two positions: RR 0.74, 95% CI 0.26 to 2.13; 1 trial, 3093 infants; Analysis 1.14.
Apgar score of less than seven at five minutes (or as defined by trial authors)
The rate of events of low Apgar scores were low in the two studies that reported these outcomes. Due to differing definitions meta‐analysis was not possible.
Perinatal death
There was only one stillbirth recorded at the one‐year follow‐up in the upright group; this was reported as one of the reasons for loss to follow‐up at one year in BUMPES 2017: RR 2.96, 95% CI 0.12 to 72.69; 1 trial, 3093 participants; Analysis 1.15.
Discussion
Summary of main results
The results for all eight studies together did not show a clear difference between upright and recumbent positions for our combined primary outcome of operative birth (caesarean or instrumental vaginal). This may be related to the heterogeneity of these studies and potentially reflects the differing interventions used as well as possible bias in allocation concealment, incomplete outcome data and co‐interventions. However, results were quite different for the sensitivity analysis of studies at low risk of bias (exclusion of those with unclear or high risk of bias for both allocation concealment and incomplete outcome data or a co‐intervention). In the sensitivity analysis an upright position for women with an epidural was associated with around a 10% increased risk of operative birth, which equates to an absolute effect of 63 more operative births for every 1000 women (but this number may be as low as 17 or as high as 115 operative births per 1000 women). Sensitivity analysis also suggests around a 30% higher caesarean section rate in the upright group, which equates to an absolute effect of 25 more caesarean sections for every 1000 women (from 4 more to 49 more), but with no clear effect on the rates of instrumental deliveries. There was also no clear difference in the duration of the second stage of labour based on position, but the quality of this evidence was very low. Blood loss was only reported in one study (BUMPES 2017), which they defined as a PPH requiring blood transfusion, and position probably makes little or no difference in the number of women with a PPH.
Results for maternal satisfaction were only reported in one study and were overall very similar between upright and recumbent groups, although women in the upright group were a little less satisfied with their birth experience than women in the recumbent group.
There is insufficient evidence for reliable conclusions on many outcomes for the baby, with meta‐analysis only possible for one outcome (low cord pH). However there is some evidence to suggest that babies born to mothers in an upright position were less likely to have a low cord pH at birth, but there were no differences demonstrated in neonatal unit admission or perinatal death.
Overall completeness and applicability of evidence
This review includes all known available evidence from randomised controlled trials which test the theory that maternal position in the second stage can help the process of birth. Many of the studies were relatively small and all but one (BUMPES 2017) had some methodological concerns; lack of registration, unclear randomisation concealment, or post‐randomisation exclusions, which means their results should be interpreted with caution. The studies also varied in their comparators, with some studies comparing different positions (upright and recumbent), some comparing ambulation with (recumbent) non‐ambulation, and one study (Simarro 2017) comparing postural changes guided by a physiotherapist to recumbent position. This may explain some of the heterogeneity observed between some of the trials. Most studies randomised women to the allocated intervention for the passive second stage, with one study (BUMPES 2017) continuing the same allocated position into the active second stage. One study reported that women could use their desired position for the active second stage, whilst the rest did not report whether women should continue in their allocated position or not for the active second stage. Furthermore, only four studies (Boyle 2001; BUMPES 2017; Downe 2004; Golara 2002) reported adherence to the allocated position.
There were concerns about the interpretation of the intervention in one study, as it appeared that there was a plan for women to change from upright to recumbent and vice versa with the planned interventions (Walker 2012); the active/alternative group were allowed upright positions in the passive second stage but active second stage was in a recumbent (lateral Gasquet/decubitus) position, whilst the traditional group were placed in lithotomy in the passive second stage but moved in the active second stage to flexion trunk position. There is no definition of the angle of this flexion, as to whether it was less than 45 º and therefore maintained the recumbent position. Furthermore the study included a co‐intervention that may have affected the results in that the intervention group delayed pushing for up to 120 minutes following diagnosis of the second stage, compared with immediate pushing in the traditional group. We therefore opted to exclude this study from the sensitivity analysis of trials at low risk of bias.
There was much heterogeneity of results for the primary outcome of instrumental birth, which may be accounted for by differences in study design, with differing positions recommended in the two intervention groups, and also unclear reporting on whether or not women complied with these allocated positions. A potential confounder is the position of the baby's head in the maternal pelvis at the onset of second stage, with malposition associated with a longer second stage and operative birth. Only one study (Downe 2004) reported this variable, with the fetal head in a lateral or posterior position in around 25% of participants with no significant difference found between the groups. This characteristic was found to be an important confounder, increasing the risk of instrumental birth 2.7‐fold. Failure to account for this confounder in the other studies may also play a part in the heterogeneity of the results.
In this review we have not considered studies which assess positions which free the pelvis to expand a little compared with those where the pelvis is fixed. Such a comparison would test if positions which let the pelvis expand and give more room for the baby to pass through might help. Sitting upright on a bed would be a 'pelvis fixed' position. The benefits of the upright position may then be negated if the woman rests on the sacrum and ischial tuberosities (Gardosi 1989), as this may rotate the sacrum forward and reduce the anterior‐posterior pelvic outlet dimensions (Borell 1957). There were insufficient data for this analysis but we will consider this comparison in the next update.
We grouped women by whether they had a traditional or mobile epidural, but in some cases the type of epidural used was not adequately reported and those that were unclear we classified in the traditional group. We reported results for all the studies together and planned a subgroup analysis for those where it was clear that they had a mobile epidural. Overall there was no clear difference in operative births when we grouped studies by the type of epidural used (traditional or mobile), but there was significant heterogeneity in the results, particularly in the traditional group. Limiting the analysis to studies at low risk of bias left only one study (Downe 2004) of 107 women in the traditional group.
We had planned to include studies where participants had singleton pregnancies at term, i.e. 37 weeks onwards. Three of the studies (Downe 2004; Karraz 2003; Walker 2012) included women at earlier gestational time points than that prespecified in our protocol. These studies recruited women from 36 weeks onwards. Outcomes were not available for term and preterm gestational ages separately, so we include data on women from 36 weeks onwards in the review rather than restricting to term participants only. This deviation is unlikely to have significantly altered the results, and the numbers of women between 36 and 37 weeks included in the review are likely to be small, with results applicable to women at term with an epidural.
We acknowledge that the results from this review have been influenced by the choice of statistical model. We chose random effects due to the heterogeneity in populations and interventions and, as a result, we assume that the 'true' result may differ between studies. The random‐effects model gives a more conservative estimate with wider confidence intervals. It also potentially gives more weight to smaller, less robust studies, so the overall conclusions of the updated meta‐analysis remain the same. However, sensitivity analyses excluding smaller studies at high risk of bias suggest a clear increase in operative births with upright positions. These results are largely driven by the most recent, large multicentre trial (BUMPES 2017). We are aware that a fixed‐effect model gives results which are very different and clearly favour the large trial (BUMPES 2017) and recumbent position for some outcomes.
Quality of the evidence
We assessed the quality of the evidence using the GRADE approach for the six prespecified GRADE maternal outcomes and three prespecified fetal outcomes for the comparison of upright position versus recumbent position (see summary of findings Table for the main comparison). We also assessed the quality of evidence using the GRADE approach for the sensitivity analysis of studies at low risk of bias for three outcomes. For the overall data we assessed the evidence for blood loss greater than 500 ml and low cord pH less than 7.1 as being of moderate quality; operative birth and trauma to birth canal requiring suturing as being of low quality; duration of second stage, caesarean section, instrumental birth, abnormal fetal heart rate patterns requiring intervention, and admission to neonatal intensive care unit as being of very low quality. For the sensitivity analyses of studies at low risk of bias we assessed the evidence for operative birth and caesarean section as being of high quality and for instrumental vaginal birth as low quality. We downgraded outcomes due to design limitations in studies contributing data, inconsistency, and imprecision of effect estimates.
Potential biases in the review process
While there is the potential to introduce bias at all stages of this review process, we undertook various steps to minimise this. We adopted systematic methods as part of our criteria for selecting studies for inclusion and used a protocol aimed at minimising bias. Two review authors independently assessed eligibility of trials for inclusion in the review, and carried out data extraction. A third review author carried out data checks. Two people working independently assessed the included studies for risks of bias, and conducted GRADE assessments to minimise biases within the review process. We had prespecified our restriction of the main analysis to subgroups of studies on women with a mobile or traditional epidural and sensitivity analysis limited to trials at low risk of bias (based on an unclear or high risk of bias judgement for both allocation concealment and incomplete outcome data). However, we did not prespecify the exclusion of studies with co‐interventions from the sensitivity analysis of trials at low risk of bias.
Agreements and disagreements with other studies or reviews
The conclusions of this review have altered from the previous version (Kibuka 2017), due primarily to the addition of one further large trial at low risk of bias (BUMPES 2017). The sensitivity analysis of studies at low risk of bias clearly shows a reduction in operative births in the recumbent position. However, results from the main analysis of all the included studies in this review (high to low risk of bias) have again shown that position may make little or no difference to the rates of operative birth.
The results of this updated review both agree and disagree with another Cochrane Review comparing positions in second stage in women without epidural analgesia (Gupta 2017). We found similar results for admission to neonatal intensive care and for caesarean section. However, women without epidural analgesia in an upright position had fewer assisted deliveries, shorter durations for the second stage of labour and less abnormal fetal heart rates noted, but experienced more second‐degree tears than those in recumbent positions without epidural analgesia.

Study flow diagram.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
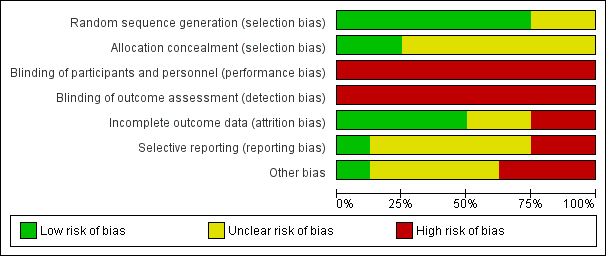
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Comparison 1 Upright position versus recumbent position, Outcome 1 Operative birth (caesarean or instrumental vaginal).
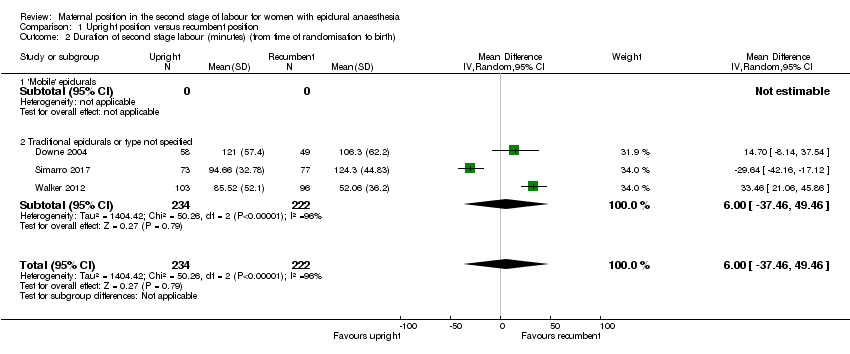
Comparison 1 Upright position versus recumbent position, Outcome 2 Duration of second stage labour (minutes) (from time of randomisation to birth).

Comparison 1 Upright position versus recumbent position, Outcome 3 Caesarean section.
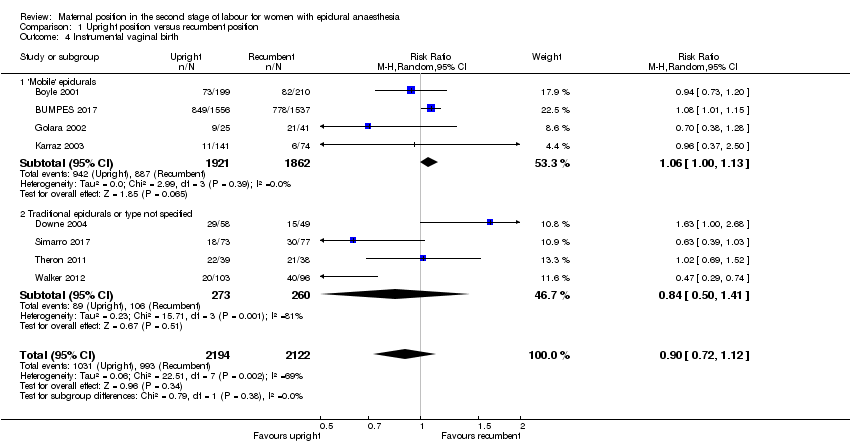
Comparison 1 Upright position versus recumbent position, Outcome 4 Instrumental vaginal birth.

Comparison 1 Upright position versus recumbent position, Outcome 5 Trauma to birth canal requiring suturing.
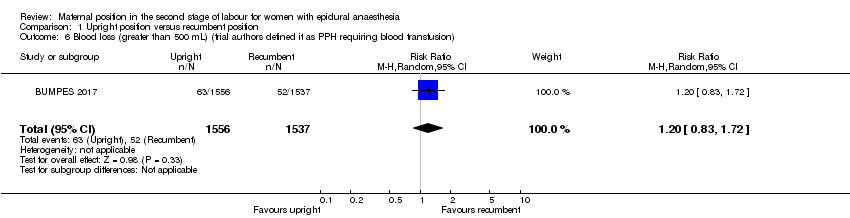
Comparison 1 Upright position versus recumbent position, Outcome 6 Blood loss (greater than 500 mL) (trial authors defined it as PPH requiring blood transfusion).

Comparison 1 Upright position versus recumbent position, Outcome 7 Prolonged second stage, defined as pushing for more than 60 minutes (trial authors report 'duration of pushing phase' in minutes.

Comparison 1 Upright position versus recumbent position, Outcome 8 Maternal experience and satisfaction of labour.

Comparison 1 Upright position versus recumbent position, Outcome 9 Abnormal fetal heart rate patterns, requiring intervention.

Comparison 1 Upright position versus recumbent position, Outcome 10 Apgar score less than seven at five minutes.
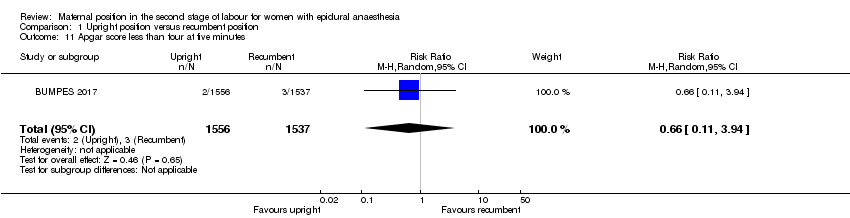
Comparison 1 Upright position versus recumbent position, Outcome 11 Apgar score less than four at five minutes.
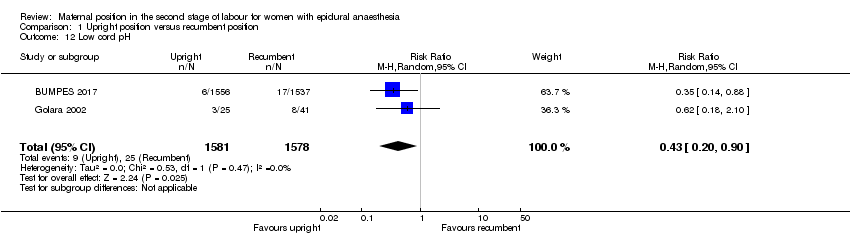
Comparison 1 Upright position versus recumbent position, Outcome 12 Low cord pH.

Comparison 1 Upright position versus recumbent position, Outcome 13 Admission to neonatal intensive care unit.

Comparison 1 Upright position versus recumbent position, Outcome 14 Need for ventilation (trial authors report 'intubation').
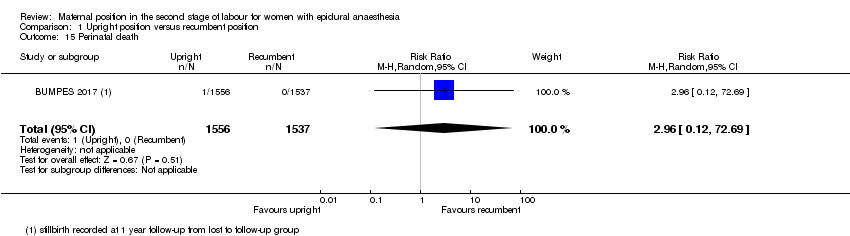
Comparison 1 Upright position versus recumbent position, Outcome 15 Perinatal death.
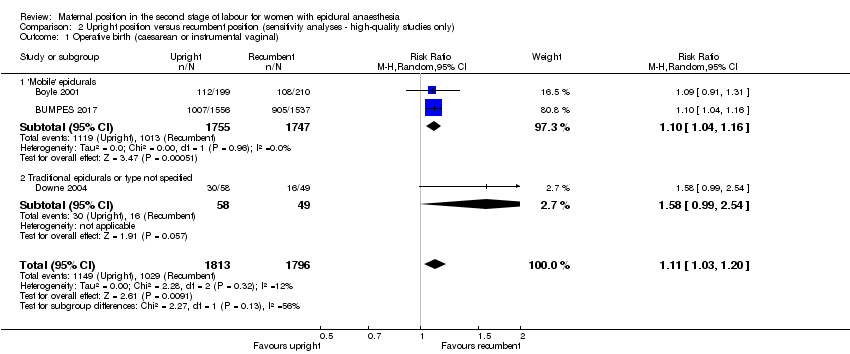
Comparison 2 Upright position versus recumbent position (sensitivity analyses ‐ high‐quality studies only), Outcome 1 Operative birth (caesarean or instrumental vaginal).
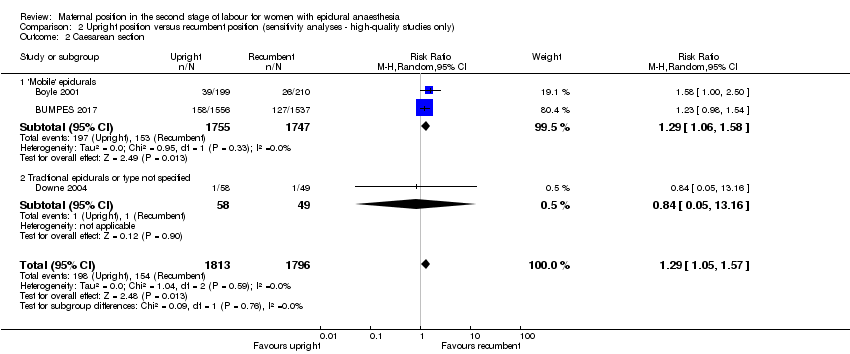
Comparison 2 Upright position versus recumbent position (sensitivity analyses ‐ high‐quality studies only), Outcome 2 Caesarean section.

Comparison 2 Upright position versus recumbent position (sensitivity analyses ‐ high‐quality studies only), Outcome 3 Instrumental vaginal birth.
| Upright position compared to recumbent position for the second stage of labour for women with epidural anaesthesia | ||||||
| Patient or population: women in the second stage of labour with epidural anaesthesia | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with recumbent position | Risk with upright position | |||||
| Maternal outcomes | ||||||
| Operative birth (caesarean or instrumental vaginal) | Study population | RR 0.86 | 4316 | ⊕⊕⊝⊝ | ‐ | |
| 554 per 1000 | 476 per 1000 | |||||
| Duration of second stage labour (minutes) (from time of randomisation to birth) | The mean duration of second stage labour across control groups ranged from 52.06 minutes to 124.3 minutes | MD 6.00 minutes higher (37.46 lower to 49.46 higher) | ‐ | 456 | ⊕⊝⊝⊝ | ‐ |
| Caesarean section | Study population | RR 0.94 | 4316 | ⊕⊝⊝⊝ | ‐ | |
| 86 per 1000 | 81 per 1000 | |||||
| Instrumental vaginal birth | Study population | RR 0.90 | 4316 | ⊕⊝⊝⊝ | ‐ | |
| 468 per 1000 | 421 per 1000 | |||||
| Trauma to birth canal requiring suturing | Study population | RR 1.00 | 3266 | ⊕⊕⊝⊝ | ‐ | |
| 840 per 1000 | 832 per 1000 | |||||
| Blood loss (greater than 500 mL) (trial authors defined it as PPH requiring blood transfusion) | Study population | RR 1.20 | 3093 | ⊕⊕⊕⊝ | ‐ | |
| 34 per 1000 | 41 per 1000 | |||||
| Infant outcomes | ||||||
| Abnormal fetal heart rate patterns, requiring intervention | Study population | RR 1.69 | 107 | ⊕⊝⊝⊝ | ‐ | |
| 41 per 1000 | 69 per 1000 | |||||
| Low cord pH | Study population | RR 0.43 | 3159 | ⊕⊕⊕⊝ | ‐ | |
| 16 per 1000 | 7 per 1000 | |||||
| Admission to neonatal intensive care unit | Study population | RR 0.54 | 66 | ⊕⊝⊝⊝ | ‐ | |
| 24 per 1000 | 13 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aLimitations in study (no blinding possible in any of the studies, with some studies at high risk for incomplete data, selective reporting and other bias) (‐1). | ||||||
| Upright position compared to recumbent position (sensitivity analyses ‐ studies at low risk of bias only) for the second stage of labour for women with epidural anaesthesia | ||||||
| Patient or population: women in the second stage of labour with epidural anaesthesia | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with recumbent position (sensitivity analyses ‐ studies at low risk of bias only) | Risk with upright position | |||||
| Operative birth (caesarean or instrumental vaginal) | Study population | RR 1.11 | 3609 | ⊕⊕⊕⊕ | ‐ | |
| 573 per 1000 | 636 per 1000 | |||||
| Caesarean section | Study population | RR 1.29 | 3609 | ⊕⊕⊕⊕ | ‐ | |
| 86 per 1000 | 111 per 1000 | |||||
| Instrumental vaginal birth | Study population | RR 1.08 | 3609 | ⊕⊕⊝⊝ | ‐ | |
| 487 per 1000 | 526 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aLimitations in study design (no blinding possible in any of the studies, unclear allocation concealment) – but most of the pooled effect comes from one study with low risk of bias for all domains apart from blinding – impossible to blind and so not downgraded for lack blinding as this is an objective measure. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Operative birth (caesarean or instrumental vaginal) Show forest plot | 8 | 4316 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.70, 1.07] |
| 1.1 'Mobile' epidurals | 4 | 3783 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.90, 1.20] |
| 1.2 Traditional epidurals or type not specified | 4 | 533 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.48, 1.25] |
| 2 Duration of second stage labour (minutes) (from time of randomisation to birth) Show forest plot | 3 | 456 | Mean Difference (IV, Random, 95% CI) | 6.00 [‐37.46, 49.46] |
| 2.1 'Mobile' epidurals | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Traditional epidurals or type not specified | 3 | 456 | Mean Difference (IV, Random, 95% CI) | 6.00 [‐37.46, 49.46] |
| 3 Caesarean section Show forest plot | 8 | 4316 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.61, 1.46] |
| 3.1 'Mobile' epidurals | 4 | 3783 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.78, 1.67] |
| 3.2 Tradtional epidurals or type not specified | 4 | 533 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.15, 1.16] |
| 4 Instrumental vaginal birth Show forest plot | 8 | 4316 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.72, 1.12] |
| 4.1 'Mobile' epidurals | 4 | 3783 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [1.00, 1.13] |
| 4.2 Traditional epidurals or type not specified | 4 | 533 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.50, 1.41] |
| 5 Trauma to birth canal requiring suturing Show forest plot | 3 | 3266 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.89, 1.13] |
| 6 Blood loss (greater than 500 mL) (trial authors defined it as PPH requiring blood transfusion) Show forest plot | 1 | 3093 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.83, 1.72] |
| 7 Prolonged second stage, defined as pushing for more than 60 minutes (trial authors report 'duration of pushing phase' in minutes Show forest plot | 1 | 199 | Mean Difference (IV, Random, 95% CI) | ‐16.37 [‐24.55, ‐8.19] |
| 8 Maternal experience and satisfaction of labour Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.1 Satisfaction with overall childbirth experience (strongly agree & agree) | 1 | 2373 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.92, 0.99] |
| 8.2 Involved in making decisions (strongly agree & agree) | 1 | 2373 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.96, 1.00] |
| 8.3 Treated with respect by all staff (strongly agree & agree) | 1 | 2373 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.98, 1.01] |
| 8.4 Expectations for labour & birth were met (strongly agree & agree) | 1 | 2373 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.93, 1.05] |
| 8.5 Felt safe at all times (strongly agree & agree) | 1 | 2373 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.97, 1.02] |
| 8.6 Good communication from staff (strongly agree & agree) | 1 | 2373 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.98, 1.02] |
| 8.7 Felt in control (strongly agree & agree) | 1 | 2373 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.95, 1.06] |
| 8.8 Able to move as much as wanted (strongly agree & agree) | 1 | 2373 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.86, 1.01] |
| 8.9 Satisfied with position before pushing (strongly agree & agree) | 1 | 2373 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.98, 1.05] |
| 8.10 Satisfied with position while pushing (strongly agree & agree) | 1 | 2373 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.98, 1.04] |
| 8.11 Satisfied with labour pain relief (strongly agree & agree) | 1 | 2373 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.97, 1.02] |
| 9 Abnormal fetal heart rate patterns, requiring intervention Show forest plot | 1 | 107 | Risk Ratio (M‐H, Random, 95% CI) | 1.69 [0.32, 8.84] |
| 10 Apgar score less than seven at five minutes Show forest plot | 1 | 199 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Apgar score less than four at five minutes Show forest plot | 1 | 3093 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.11, 3.94] |
| 12 Low cord pH Show forest plot | 2 | 3159 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.20, 0.90] |
| 13 Admission to neonatal intensive care unit Show forest plot | 1 | 66 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.02, 12.73] |
| 14 Need for ventilation (trial authors report 'intubation') Show forest plot | 1 | 3093 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.26, 2.13] |
| 15 Perinatal death Show forest plot | 1 | 3093 | Risk Ratio (M‐H, Random, 95% CI) | 2.96 [0.12, 72.69] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Operative birth (caesarean or instrumental vaginal) Show forest plot | 3 | 3609 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [1.03, 1.20] |
| 1.1 'Mobile' epidurals | 2 | 3502 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [1.04, 1.16] |
| 1.2 Traditional epidurals or type not specified | 1 | 107 | Risk Ratio (M‐H, Random, 95% CI) | 1.58 [0.99, 2.54] |
| 2 Caesarean section Show forest plot | 3 | 3609 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [1.05, 1.57] |
| 2.1 'Mobile' epidurals | 2 | 3502 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [1.06, 1.58] |
| 2.2 Tradtional epidurals or type not specified | 1 | 107 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.05, 13.16] |
| 3 Instrumental vaginal birth Show forest plot | 3 | 3609 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.91, 1.30] |
| 3.1 'Mobile' epidurals | 2 | 3502 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.98, 1.15] |
| 3.2 Traditional epidurals or type not specified | 1 | 107 | Risk Ratio (M‐H, Random, 95% CI) | 1.63 [1.00, 2.68] |

