Position in the second stage of labour for women with epidural anaesthesia
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT in a consultant maternity unit in Hertfordshire, UK Participants were recruited between August 1999‐December 2000 | |
| Participants | Primiparous (n = 295) and multiparous (n = 113) women (total 408) in either induced or spontaneous labour with a working low dose, CSE in the first stage of labour, and a Modified Bromage score of ≥ 3 | |
| Interventions | The ambulant group were encouraged to walk around for at least 15 min in every hour, up to the point of active voluntary pushing, i.e. including the passive second stage of labour The non‐ambulant group received 'usual care'. This meant remaining non‐ambulant except for toilet purposes for the majority of the labour Among primigravidae the mean time in minutes spent ambulating (SD) was 46 (51) in the ambulant group and 18 (33) in the non‐ambulant. Among multigravidae the mean time in minutes spent ambulating (SD) was 37 in the ambulant group and 11 in the non‐ambulant. Note standard deviations were not reported for multigravidae. Use of oxytocin in the second stage was not reported. | |
| Outcomes | Maternal outcomes
Baby outcomes
| |
| Notes | Trial took place in consultant maternity unit in Hertfordshire, UK ‐ funding source unknown | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computer‐generated random number sequence was used |
| Allocation concealment (selection bias) | Unclear risk | Randomisation was achieved by the use of sequentially‐numbered sealed envelopes. Opacity not reported |
| Blinding of participants and personnel (performance bias) | High risk | Not mentioned ‐ assumed unblinded |
| Blinding of outcome assessment (detection bias) | High risk | Not mentioned ‐ assumed unblinded |
| Incomplete outcome data (attrition bias) | Low risk | No losses to follow‐up recorded and only short‐term outcomes reported |
| Selective reporting (reporting bias) | Unclear risk | Neither the trial, nor the protocol was registered |
| Other bias | Unclear risk | The trial protocol was not registered |
| Methods | A pragmatic prospective RCT, in a consultant‐led maternity unit in the East Midlands, UK. Recruitment from June 1993‐May 1994. | |
| Participants | 107 nulliparous women using traditional epidural analgesia, set up in the first stage of labour, maintained by bolus doses of local anaesthetic, and reaching the second stage without contraindication to spontaneous birth. In most cases the epidural was continued into the second stage of labour, a passive hour was allowed followed by encouraged pushing by the midwife. Entry criteria: nulliparity, uncomplicated pregnancy, no history of uterine surgery, live single cephalic fetus with no abnormality detected, once women in labour at 36 weeks' gestation or greater, with effective epidural analgesia, eligibility was confirmed Exclusion criteria: breech position, severe pregnancy‐induced hypertension, pre‐eclampsia or eclampsia, severe intrauterine growth retardation, known intrauterine fetal death, presence of uterine scar. The proportions of participants in spontaneous or induced labour were not reported. Use of oxytocin in the second stage was not reported. | |
| Interventions | 58 were allocated to the supported upright sitting position (normal practice in the unit). 6 of these used the lateral position. 49 were allocated to use the left or right facing lateral position whichever was most comfortable. 12 of these used the sitting position. | |
| Outcomes | Maternal outcomes
Baby outcomes
| |
| Notes | Funding was from the HSA Hospital Trust/ SDH Scholarship Fund/ Southern Derbyshire Acute Hospitals NHS Trust. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | Opaque envelopes stapled to patient notes. Numbering and sealing not reported |
| Blinding of participants and personnel (performance bias) | High risk | Not mentioned ‐ assumed unblinded |
| Blinding of outcome assessment (detection bias) | High risk | Not mentioned ‐ assumed unblinded |
| Incomplete outcome data (attrition bias) | Low risk | The main outcomes were reported for all 107 women randomised |
| Selective reporting (reporting bias) | Unclear risk | Trial protocol not registered |
| Other bias | Unclear risk | Trial protocol not registered |
| Methods | RCT, conducted in a university teaching hospital in London, UK The period of recruitment was not recorded | |
| Participants | Entry criteria: primigravidae, singleton fetus in vertex presentation, 37 weeks or greater, continuous spinal catheter sited during the first stage and in situ, achieved full dilatation, motor function adequate for mobilisation Exclusion criteria: inadequate motor function, received pethidine 4 h before full dilatation Analgesia was maintained by intermittent bolus injections. A 1‐h passive phase was allowed in the second stage 66 (upright = 25, recumbent = 41). 13 (7 recumbent, 6 upright) had induced labour. 8 (4 in each group) were given oxytocin in the second stage | |
| Interventions | 25 women allocated to the upright group were asked to spend as much as possible of the passive phase of the second stage standing or walking. Of these 22 (88%) were upright for more than 30 min 41 women allocated to the recumbent group were asked to be in bed or a chair during the passive phase. Of these 27 (65%) spent more than 30 min in bed, 8 (20%) sat in a chair for more than 30 min and 6 (15%) were walking or standing | |
| Outcomes | Maternal outcomes
Baby outcomes
| |
| Notes | Authors employed at Maternal and Fetal Research Unit, St. Thomas’s Hospital and Queen Charlotte’s and Chelsea Hospital, London, UK. It is not clear how the study was funded | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers. A copy [of the randomisation sequence] was kept safe to ensure no violation of randomisation |
| Allocation concealment (selection bias) | Unclear risk | Sealed brown envelopes. Opacity and numbering not reported |
| Blinding of participants and personnel (performance bias) | High risk | Not mentioned ‐ assumed unblinded |
| Blinding of outcome assessment (detection bias) | High risk | Not mentioned ‐ assumed unblinded |
| Incomplete outcome data (attrition bias) | Unclear risk | There is a discrepancy in the number of participants reported. The total randomised is stated to be 70, with 7 post‐randomisation withdrawals (i.e. 63 remaining). But the number reported in the remainder of the paper is 66 |
| Selective reporting (reporting bias) | Unclear risk | Trial protocol not registered |
| Other bias | Unclear risk | Trial protocol not registered |
| Methods | A randomised prospective study, in a regional maternity hospital in France The randomisation ratio was 2:1 ambulatory: recumbent Recruitment from February 1999‐April 2001 | |
| Participants | Entry criteria: 36‐42 weeks pregnant, a singleton pregnancy, cephalic presentation, uncomplicated pregnancies Exclusion criteria: pre‐eclampsia, previous caesarean section All participants had a low‐dose "ambulatory" epidural using intermittent bolus doses (0.1% ropivacaine and 0.6 micro grams/mL sufentanil) titrated against pain relief Women in spontaneous (86 ambulatory, 45 non‐ambulatory) and induced labour were included Use of oxytocin in the second stage was not reported 221 participants were included. 144 were allocated to the upright position and 77 to recumbent | |
| Interventions | Women allocated to the ambulatory group were allowed to walk if they had acceptable analgesia, systolic BP > 100 mmHg, and were able to stand on 1 leg. The number who walked and the time spent walking were not reported Women allocated to the non‐ambulatory group were not allowed to sit or walk. They were only allowed to lie supine, semi supine or in a lateral position on the bed. The number who complied, and the time spent in each position were not reported | |
| Outcomes | Maternal outcomes
Baby outcomes
| |
| Notes | This study was conducted at the Department of Anesthesiology and Intensive Care, Beauvais Central Hospital, France.The Departments of Anesthesiology and Obstetrics and Gynecology funded this study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly divided into 2 groups. Randomised in 2:1 ratio (upright: recumbent) |
| Allocation concealment (selection bias) | Unclear risk | Not recorded |
| Blinding of participants and personnel (performance bias) | High risk | Not mentioned ‐ assumed unblinded |
| Blinding of outcome assessment (detection bias) | High risk | Not mentioned ‐ assumed unblinded |
| Incomplete outcome data (attrition bias) | Unclear risk | No data reported for 6 post‐randomisation exclusions (3 per group) |
| Selective reporting (reporting bias) | Unclear risk | Trial protocol not registered |
| Other bias | Unclear risk | Trial protocol not registered |
| Methods | RCT Single centre. University Teaching Hospital, UK | |
| Participants | Nulliparous women at term. Single fetus. Epidural sited and analgesia established The type of epidural, and whether it was a 'walking' epidural was not reported Numbers of spontaneous and induced labours not reported Use of oxytocin in the second stage not reported Random allocated using computer randomisation 39 women allocated to sitting. 38 allocated to lateral position | |
| Interventions | Sitting for 1 h passive second stage of labour Lateral position for 1 h passive second stage of labour | |
| Outcomes |
| |
| Notes | 120 women consented. 43 dropped out after consent Not stated how study was funded (abstract only) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer randomisation |
| Allocation concealment (selection bias) | Unclear risk | Not recorded |
| Blinding of participants and personnel (performance bias) | High risk | Not mentioned ‐ assumed unblinded |
| Blinding of outcome assessment (detection bias) | High risk | Not mentioned ‐ assumed unblinded |
| Incomplete outcome data (attrition bias) | High risk | 43 participants dropped out after consent. Unclear if this was post randomisation |
| Selective reporting (reporting bias) | High risk | Secondary outcomes of maternal acceptability, CTG abnormality and neonatal outcomes not reported. Trial protocol not registered |
| Other bias | Unclear risk | Intended sample size 300. Study stopped after 77 recruited |
BP: blood pressure
CSE: combined spinal epidural
CTG: cardiotocograph
RCT: randomised controlled trial
SD: standard deviation
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Trial compared positions in labour for women without epidural | |
| This was not a randomised trial. Translation from the French indicates that the ambulatory group was selected by having no contraindications to ambulation and gave consent. The non‐ambulatory group was made up of women who were "chosen at random" from women receiving epidural analgesia. | |
| This trial compared upright versus recumbent in the first stage of labour, "The time at which full cervical dilatation was diagnosed was recorded and all mothers returned to bed". | |
| The trial compared two recumbent positions, supine and lateral. | |
| Trial compared modified Sims position with Sims or Semi‐fowler positions. None of these options were upright positions so did not satisfy this review's inclusion criteria. | |
| Trial compared positions in labour for women without epidural. |
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | RCT |
| Participants | 150 women at full dilatation |
| Interventions | Intervention group: delay pushing and change position (hands and knees, sitting lateral, kneeling and supine). Delivered in lithotomy Comparison group: delay pushing, rest in horizontal position without postural changes |
| Outcomes | Mode of delivery Perineal trauma Duration of second stage |
| Notes | Awaiting clarification of intervention from study authors. May be eligible for inclusion |
| Methods | RCT |
| Participants | 199 women randomised Nulliparous and multiparous women (gestational age > 36 or < 42 weeks), single fetus in cephalic presentation, spontaneous or induced labour, and effective epidural anaesthesia with a standardised continuous‐infusion technique |
| Interventions | Intervention group (103 participants): alternative model of birth (study group) AMB consisted of 2 consecutive interventions during the second stage of labour. Firstly, women move to different positions while delaying the onset of pushing during the passive phase and, secondly, women were placed in the modified lateral Gasquet position during the active pushing phase. Comparison group (96 participants): In the traditional model of birth (TMB), women were encouraged to perform pushing efforts with each contraction, as soon as they were found to be completely dilated. They had no postural changes, and delivery was in the lithotomy position. |
| Outcomes | Primary outcomes were rates of AVD (defined by the use of forceps, vacuum, spatulas, or fundal pressure, also known as Kristeller maneuver) and PT, defined as trauma requiring suturing (episiotomy, tear, or both). Secondary outcomes were length of the second stage (duration from full dilatation to delivery), duration of pushing efforts (from starting active pushing to delivery), umbilical arterial cord blood pH, Apgar scores, birthweight, and FH station at full dilatation (classified by FH unengaged and FH engaged or below inlet). |
| Notes | Awaiting clarification of intervention from authors. May be eligible for inclusion |
AMB: alternative model of birth
AVD: assisted vaginal delivery
FH: fetal head
PT: perineal trauma
TMB: traditional model of birth
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | A study of position during the late stages of labour in women with an epidural ‐ BUMPES: a randomised controlled trial. |
| Methods | RCT Anticipated start date: 01/04/2010 Anticipated end date: 30/04/2015 Entry criteria: women who are: nulliparous, single cephalic presentation, ≥ 37 weeks' gestation, intend spontaneous vaginal birth, in second stage of labour, with an effective mobile epidural in situ Exclusion criteria: unable to understand written and spoken English language |
| Participants | Target number: 3000 |
| Interventions | 'Upright position' versus 'lying‐down' position throughout the second stage of labour |
| Outcomes | Primary outcome measures: incidence of spontaneous vaginal birth Secondary outcome measures: mode of birth, outcomes from randomisation until birth, immediate post‐birth outcomes, postnatal period for both mother and infant, 1‐year outcomes for both mother and infant |
| Starting date | April 2010 |
| Contact information | Professor Peter Brocklehurst, Director and Professor of Perinatal Epidemiology National Perinatal Epidemiology Unit Telephone: +44 (0)1865 289700 |
| Notes |
| Trial name or title | GAP Trial ‐ Gentle Assisted Pushing A multicentre randomised controlled trial of gentle assisted pushing in the upright posture (GAP) or upright posture alone compared with routine practice to reduce prolonged second stage of labour (the Gentle Assisted Pushing study): study protocol |
| Methods | Randomised, controlled, unblinded, clinical trial with 3 parallel arms across 4 hospital sites in South Africa |
| Participants | Inclusion: nulliparous women ≥ 18 years old; gestational age > 35 weeks; singleton pregnancy; vaginal delivery anticipated; cephalic fetal presentation; fetal heartbeat detected Exclusion: no chronic medical conditions, including heart disease, epilepsy, hypertension, diabetes mellitus and renal disease; no obstetric complications, including hypertensive disorders of pregnancy, cephalo‐pelvic disproportion, antepartum haemorrhage, intrauterine growth restriction, fetal distress, intra‐amniotic infection |
| Interventions | Intervention 1: gentle assisted pushing. The woman will be assisted to assume an upright kneeling or squatting posture on the bed. The trained birth attendant will kneel behind her on the bed or stand behind her with the woman positioned at right angles to the length of the bed and back close to the side of the bed. The trained birth attendant will wrap her arms around the woman passing below her axillae, and place both open palms, overlapping, on the fundus of her uterus. Steady pressure in the long axis of the uterus will be applied only during contractions. The duration of pressure will be limited to 30 seconds, with a minimum of 30 seconds rest before the next pressure. Intervention 2: upright crouching or kneeling position for second stage Control: recumbent/supine posture only |
| Outcomes | The primary outcome is defined as mean time (minutes) from randomisation to delivery. Secondary outcomes include the following Delivery outcomes:
Neonatal outcomes:
Mothers will also be asked to grade their discomfort experienced during the second stage of labour All adverse events |
| Starting date | March 2015 |
| Contact information | Correspondence to [email protected]. |
| Notes | Likely to finish June 2017 |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Operative birth (caesarean or instrumental vaginal) Show forest plot | 5 | 874 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.76, 1.25] |
| Analysis 1.1  Comparison 1 Upright position versus recumbent position, Outcome 1 Operative birth (caesarean or instrumental vaginal). | ||||
| 1.1 "Mobile" epidurals | 3 | 690 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.61, 1.26] |
| 1.2 Traditional epidurals or type not specified | 2 | 184 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.62, 2.12] |
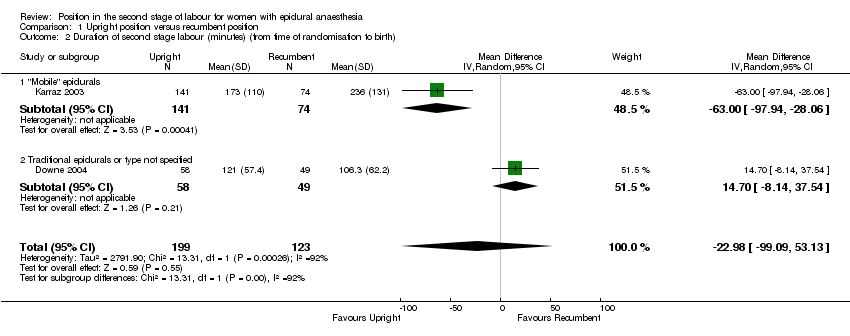
| 2 Duration of second stage labour (minutes) (from time of randomisation to birth) Show forest plot | 2 | 322 | Mean Difference (IV, Random, 95% CI) | ‐22.98 [‐99.09, 53.13] |
| Analysis 1.2  Comparison 1 Upright position versus recumbent position, Outcome 2 Duration of second stage labour (minutes) (from time of randomisation to birth). | ||||
| 2.1 "Mobile" epidurals | 1 | 215 | Mean Difference (IV, Random, 95% CI) | ‐63.0 [‐97.94, ‐28.06] |
| 2.2 Traditional epidurals or type not specified | 1 | 107 | Mean Difference (IV, Random, 95% CI) | 14.70 [‐8.14, 37.54] |
| 3 Caesarean section Show forest plot | 5 | 874 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.38, 1.69] |
| Analysis 1.3 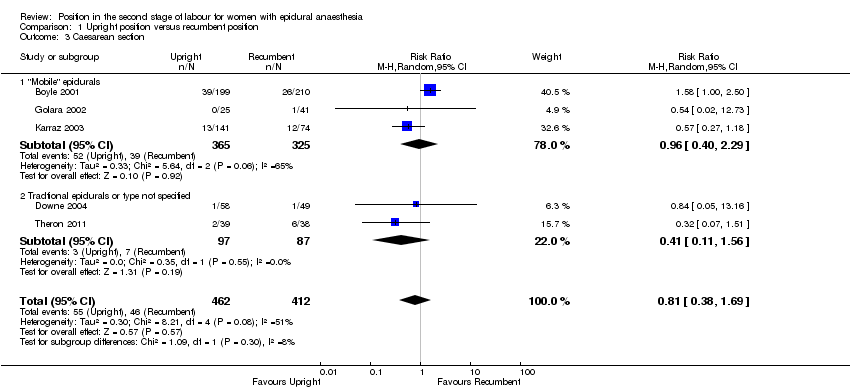 Comparison 1 Upright position versus recumbent position, Outcome 3 Caesarean section. | ||||
| 3.1 "Mobile" epidurals | 3 | 690 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.40, 2.29] |
| 3.2 Tradtional epidurals or type not specified | 2 | 184 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.11, 1.56] |
| 4 Instrumental vaginal birth Show forest plot | 5 | 874 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.81, 1.28] |
| Analysis 1.4 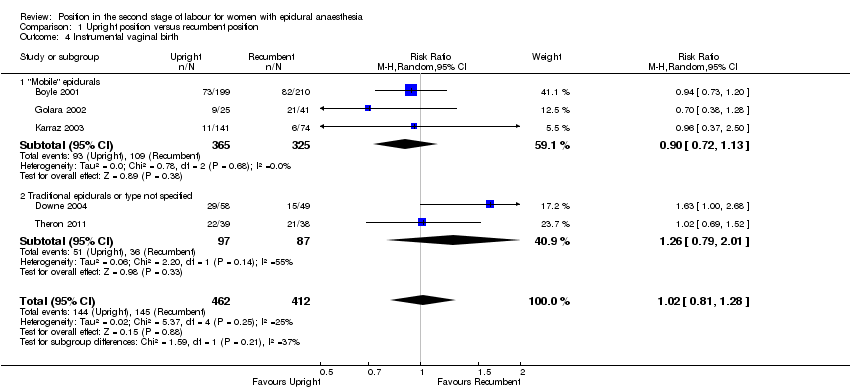 Comparison 1 Upright position versus recumbent position, Outcome 4 Instrumental vaginal birth. | ||||
| 4.1 "Mobile" epidurals | 3 | 690 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.72, 1.13] |
| 4.2 Traditional epidurals or type not specified | 2 | 184 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [0.79, 2.01] |
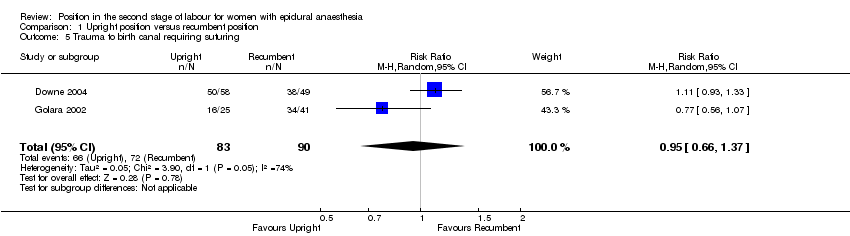
| 5 Trauma to birth canal requiring suturing Show forest plot | 2 | 173 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.66, 1.37] |
| Analysis 1.5 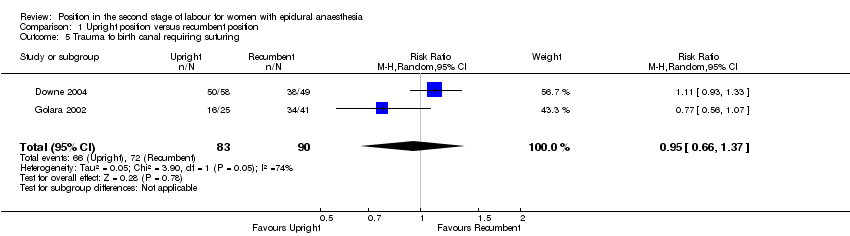 Comparison 1 Upright position versus recumbent position, Outcome 5 Trauma to birth canal requiring suturing. | ||||
| 6 Abnormal fetal heart rate patterns, requiring intervention Show forest plot | 1 | 107 | Risk Ratio (M‐H, Random, 95% CI) | 1.69 [0.32, 8.84] |
| Analysis 1.6  Comparison 1 Upright position versus recumbent position, Outcome 6 Abnormal fetal heart rate patterns, requiring intervention. | ||||
| 7 Low cord pH Show forest plot | 1 | 66 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.18, 2.10] |
| Analysis 1.7 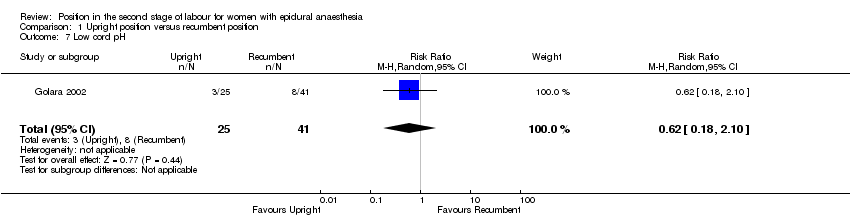 Comparison 1 Upright position versus recumbent position, Outcome 7 Low cord pH. | ||||
| 8 Admission to neonatal intensive care unit Show forest plot | 1 | 66 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.02, 12.73] |
| Analysis 1.8  Comparison 1 Upright position versus recumbent position, Outcome 8 Admission to neonatal intensive care unit. | ||||

Study flow diagram

Risk of bias summary: review authors' judgements about each risk of bias item for each included study

Comparison 1 Upright position versus recumbent position, Outcome 1 Operative birth (caesarean or instrumental vaginal).
Comparison 1 Upright position versus recumbent position, Outcome 2 Duration of second stage labour (minutes) (from time of randomisation to birth).

Comparison 1 Upright position versus recumbent position, Outcome 3 Caesarean section.

Comparison 1 Upright position versus recumbent position, Outcome 4 Instrumental vaginal birth.
Comparison 1 Upright position versus recumbent position, Outcome 5 Trauma to birth canal requiring suturing.

Comparison 1 Upright position versus recumbent position, Outcome 6 Abnormal fetal heart rate patterns, requiring intervention.

Comparison 1 Upright position versus recumbent position, Outcome 7 Low cord pH.

Comparison 1 Upright position versus recumbent position, Outcome 8 Admission to neonatal intensive care unit.
| Upright position compared to recumbent position for the second stage of labour for women with epidural anaesthesia | ||||||
| Patient or population: women with epidural anaesthesia in the second stage of labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with recumbent position | Risk with upright position | |||||
| Operative birth (caesarean or instrumental vaginal) | Study population | RR 0.97 | 874 | ⊕⊕⊕⊝ | ||
| 464 per 1000 | 450 per 1000 | |||||
| Duration of second stage labour (minutes) (from time of randomisation to birth) | The mean duration of second stage labour was 22.98 minutes less for women in the upright position (99.09 minutes less to 53.13 minutes more) | 322 | ⊕⊝⊝⊝ | |||
| Trauma to birth canal requiring suturing | Study population | RR 0.95 | 173 | ⊕⊝⊝⊝ | ||
| 800 per 1000 | 760 per 1000 | |||||
| Blood loss (greater than 500 mL) (or as defined by trial authors) | Study population | ‐ | (0 studies) | ‐ | No trial reported this outcome | |
| see comment | see comment | |||||
| Abnormal fetal heart rate patterns, requiring intervention | Study population | RR 1.69 | 107 | ⊕⊝⊝⊝ | ||
| 41 per 1000 | 69 per 1000 | |||||
| Low cord pH less than 7.1 (or as defined by trial authors) | Study population | RR 0.61 | 66 | ⊕⊝⊝⊝ | ||
| 195 per 1000 | 119 per 1000 | |||||
| Admission to neonatal intensive care unit | Study population | RR 0.54 | 66 | ⊕⊝⊝⊝ | ||
| 24 per 1000 | 13 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1All studies had design limitations. One trial contributing 24.2% weight had serious design limitations (‐1). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Operative birth (caesarean or instrumental vaginal) Show forest plot | 5 | 874 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.76, 1.25] |
| 1.1 "Mobile" epidurals | 3 | 690 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.61, 1.26] |
| 1.2 Traditional epidurals or type not specified | 2 | 184 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.62, 2.12] |
| 2 Duration of second stage labour (minutes) (from time of randomisation to birth) Show forest plot | 2 | 322 | Mean Difference (IV, Random, 95% CI) | ‐22.98 [‐99.09, 53.13] |
| 2.1 "Mobile" epidurals | 1 | 215 | Mean Difference (IV, Random, 95% CI) | ‐63.0 [‐97.94, ‐28.06] |
| 2.2 Traditional epidurals or type not specified | 1 | 107 | Mean Difference (IV, Random, 95% CI) | 14.70 [‐8.14, 37.54] |
| 3 Caesarean section Show forest plot | 5 | 874 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.38, 1.69] |
| 3.1 "Mobile" epidurals | 3 | 690 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.40, 2.29] |
| 3.2 Tradtional epidurals or type not specified | 2 | 184 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.11, 1.56] |
| 4 Instrumental vaginal birth Show forest plot | 5 | 874 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.81, 1.28] |
| 4.1 "Mobile" epidurals | 3 | 690 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.72, 1.13] |
| 4.2 Traditional epidurals or type not specified | 2 | 184 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [0.79, 2.01] |
| 5 Trauma to birth canal requiring suturing Show forest plot | 2 | 173 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.66, 1.37] |
| 6 Abnormal fetal heart rate patterns, requiring intervention Show forest plot | 1 | 107 | Risk Ratio (M‐H, Random, 95% CI) | 1.69 [0.32, 8.84] |
| 7 Low cord pH Show forest plot | 1 | 66 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.18, 2.10] |
| 8 Admission to neonatal intensive care unit Show forest plot | 1 | 66 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.02, 12.73] |

