| QUALITY CRITERION: question | Study | Response | Comments |
| STRUCTURE: Statement of decision problem/objective |
| Is there a clear statement of the decision problem? | NICE 2011 | Yes | Clinical effectiveness and cost effectiveness of ranibizumab monotherapy and ranibizumab in combination with laser photocoagulation compared with laser photocoagulation alone. |
| Mitchell 2012 | Yes |
| Is the objective of the evaluation and model specified and consistent with the stated decision problem? | NICE 2011 | Yes | See above. |
| Mitchell 2012 | Yes |
| Is the primary decision‐maker specified? | NICE 2011 | Yes | Not reported, but models submitted to NICE should take the perspective of the health service provider. |
| Mitchell 2012 | Yes | UK healthcare payer perspective. |
| STRUCTURE: Statement of scope/perspective |
| Is the perspective of the model stated clearly? | NICE 2011 | Yes | Ranibizumab manufacturer’s submission to NICE including an effectiveness review of two RCTs (RESTORE and DRCRnet), costs of treatment and visits and of some of its complications, as well as costs of low vision. Bevacizumab was not included in the submission but was considered a comparator by the Appraisal Committee. |
| Mitchell 2012 | Yes | Manufacturer’s sponsored study on cost‐effectiveness of ranibizumab adopting similar model boundaries as NICE 2011. Bevacizumab not mentioned as a potential comparator. |
| Are the model inputs consistent with the stated perspective? | NICE 2011 | Yes | See above. |
| Mitchell 2012 | Yes | See above. |
| Has the scope of the model been stated and justified? | NICE 2011 | Yes | See above. |
| Mitchell 2012 | Yes | See above. |
| Are the outcomes of the model consistent with the perspective, scope and overall objective of the model? | NICE 2011 | Yes | Utility‐based health‐related quality‐of‐life associated to visual acuity data from RCTs and costs of disease and treatment. |
| Mitchell 2012 | Yes |
| STRUCTURE: Rationale for structure |
| Is the structure of the model consistent with a coherent theory of the health condition under evaluation? | NICE 2011 | Yes | Health states and transition probabilities based on changes of best corrected visual acuity changes, although treatment of better‐seeing vs. worse eye or both eyes is a problem. |
| Mitchell 2012 | Yes |
| Are the sources of data used to develop the structure of the model specified? | NICE 2011 | Yes | EQ‐5D data from RESTORE related to visual acuity, NHS reference cost of treatment and visits. Cost of low vision from a published cost study. |
| Mitchell 2012 | Yes | Same as above, plus Wisconsin study (WESDR) data for natural disease history. |
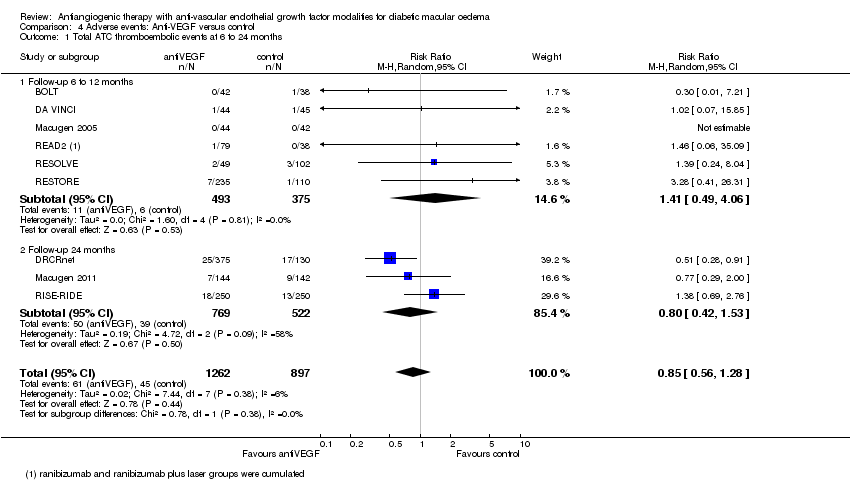
| Are the causal relationships described by the model structure justified appropriately? | NICE 2011 | Unclear | Treatment effect and adverse events are based on RCTs, but costs, and not utility decrement, related to adverse events considered. Although adverse events associated with the treatments were low, unclear if they impact on cost‐effectiveness. |
| Mitchell 2012 | No | Adverse events assumed to have negligible impact on cost‐effectiveness, but no demonstration given. |
| STRUCTURE: Structural assumptions |
| Are the structural assumptions transparent and justified? | NICE 2011 | No | See Table 12. We accept the criticism of the Appraisal committee, including the fact that treatment in better‐seeing, worse‐seeing eye or both eyes s not considered. |
| Mitchell 2012 | No | Same as for NICE 2011. |
| Are the structural assumptions reasonable given the overall objective, perspective and scope of the model? | NICE 2011 | No | See above. |
| Mitchell 2012 | No |
| STRUCTURE: Strategies/comparators |
| Is there a clear definition of the options under evaluation? | NICE 2011 | Yes | The manufacturer considered bevacizumab as a potential comparator but concluded that significant methodological and clinical differences between studies precluded a valid analysis. |
| Mitchell 2012 | No | Options under evaluation not discussed. |
| Have all feasible and practical options been evaluated? | NICE 2011 | No | See above. Bevacizumab is used off‐label for treatment of DMO in several countries. |
| Mitchell 2012 | No | See above. |
| Is there justification for the exclusion of feasible options? | NICE 2011 | No | See above. |
| Mitchell 2012 | No | See above. |
| STRUCTURE: Model type |
| Is the chosen model type appropriate given the decision problem and specified causal relationships within the model? | NICE 2011 | Yes | Appropriate given what reported above. |
| Mitchell 2012 | Yes |
| STRUCTURE: Time horizon |
| Is the time horizon of the model sufficient to reflect all important differences between options? | NICE 2011 | Yes | 15‐year horizon. |
| Mitchell 2012 | Yes |
| Are the time horizon of the model, the duration of treatment and the duration of treatment effect described and justified? | NICE 2011 | No | The model’s assumption that the relative benefit achieved during the treatment phase lasts indefinitely is unrealistic. |
| Mitchell 2012 | No |
| STRUCTURE: Disease states/pathways |
| Do the disease states (state transition model) or the pathways (decision tree model) reflect the underlying biological process of the disease in question and the impact of interventions? | NICE 2011 | Yes | Course of visual acuity change after treatment for diabetic macular oedema. |
| Mitchell 2012 | Yes |
| STRUCTURE: Cycle length |
| Is the cycle length defined and justified in terms of the natural history of disease? | NICE 2011 | Yes | 3‐monthly cycles. |
| Mitchell 2012 | Yes |
| DATA: Data identification |
| Are the data identification methods transparent and appropriate given the objectives of the model? | NICE 2011 | Unclear | A discussion of the choices of the sources is given but a systematic search is not mentioned. |
| Mitchell 2012 | No | No discussion of the choices of the sources. |
| Where choices have been made between data sources, are these justified appropriately? | NICE 2011 | Yes | RESTORE and DRCRnet data used. The choice of excluding RESOLVE and READ2 is discussed. |
| Mitchell 2012 | No | No discussion of the choices of the sources. |
| Has particular attention been paid to identifying data for the important parameters in the model? | NICE 2011 | Yes | Model revised following ERG comments considered all relevant parameters. |
| Mitchell 2012 | Yes | We believe all the important parameters have been considered. |
| Has the quality of the data been assessed appropriately? | NICE 2011 | Yes | Unclear, but NICE comment, quoted above, uses standard quality assessments methods, and assessments correspond to our review. |
| Mitchell 2012 | No | No discussion of data quality. |
| Where expert opinion has been used, are the methods described and justified? | NICE 2011 | NA | |
| Mitchell 2012 | NA | |
| DATA: Data modelling |
| Is the data modelling methodology based on justifiable statistical and epidemiological techniques? | NICE 2011 | Yes | Markov model using RCT data. |
| Mitchell 2012 | Yes |
| DATA: Data modelling ‐ Baseline data |
| Is the choice of baseline data described and justified? | NICE 2011 | Yes | See above: data from two RCTs. |
| Mitchell 2012 | Yes |
| Are transition probabilities calculated appropriately? | NICE 2011 | Yes | Extraction of transition probabilities were revised and agreed with NICE, see Table 12. |
| Mitchell 2012 | Unclear | Insufficient details. |
| Has a half‐cycle correction been applied to both cost and outcome? | NICE 2011 | Unclear | Not specified. |
| Mitchell 2012 | Yes | |
| If not, has this omission been justified? | NICE 2011 | NA | |
| Mitchell 2012 | NA | |
| DATA: Data modelling ‐ Treatment effect |
| If relative treatment effects have been derived from trial data, have they been synthesised using appropriate techniques? | NICE 2011 | NA | Effects from individual studies. |
| Mitchell 2012 | NA |
| Have the methods and assumptions used to extrapolate short‐term results to final outcomes been documented and justified? | NICE 2011 | Yes | Explanation given: no change in treatment effect during year 2, according to DRCRnet, and from year 2 to 15. Mortality data from UK‐based literature (2.45 RR for diabetics with DMO). |
| Mitchell 2012 | Yes | Same as NICE 2011, plus decline of visual acuity after year 2 modelled according to Wisconsin study (WESDR), the Diabetes Control and Complications Trial and UK Prospective Diabetes Study. |
| Have alternative assumptions been explored through sensitivity analysis? | NICE 2011 | Yes | The manufacturer presented a series of deterministic sensitivity analyses in which parameters were varied across plausible ranges, including: number of ranibizumab injections during year 3 and 4; retreatment need and treatment of both eyes in 35% of patients. |
| Mitchell 2012 | No | Sensitivity analyses on number of injections performed. Sensitivity analysis regarding treatment need after 2 years and treatment in better vs. worse seeing eye or both eyes not presented. |
| Have assumptions regarding the continuing effect of treatment once treatment is complete been documented and justified? Have alternative assumptions been explored through sensitivity analysis? | NICE 2011 | No | See previous comments and Table 12. |
| Mitchell 2012 | No | See previous comments and Table 12. |
| DATA: Data modelling ‐ Costs |
| Are the costs incorporated into the model justified? | NICE 2011 | Yes | All sources of costs considered, UK setting. Cost of adverse events not considered but suggested to be minimal due to the very low rate. |
| Mitchell 2012 | Yes |
| Has the source for all costs been described? | NICE 2011 | Yes | See Table 12. |
| Mitchell 2012 | Yes | See Table 10. |
| Have discount rates been described and justified given the target decision‐maker? | NICE 2011 | Unclear | Cannot find it in the report. |
| Mitchell 2012 | Yes | 3.5% discount rate. |
| DATA: Data modelling ‐ Quality of life weights (utilities) |
| Are the utilities incorporated into the model appropriate? | NICE 2011 | No | Utility gain for treatment in the better‐seeing vs. worse‐seeing eye or in both eyes still a problem in the revised model. |
| Mitchell 2012 | No | Utility gain for treatment in the better‐seeing vs. worse‐seeing eye or in both eyes still not considered. |
| Is the source for the utility weights referenced? | NICE 2011 | Yes | EQ‐5D data from RESTORE were transformed to utility values using standard social tariffs and then related to BCVA in the treated eye using linear regression. Covariate adjustment used in revised submission. sensitivity analyses based on other sources available. |
| Mitchell 2012 | Yes | EQ‐5D data from RESTORE were transformed to utility values using standard social tariffs and then related to BCVA in the treated eye using linear regression. |
| Are the methods of derivation for the utility weights justified? | NICE 2011 | No | See above. |
| Mitchell 2012 | No | See above. |
| DATA: Data incorporation |
| Have all data incorporated into the model been described and referenced in sufficient detail? | NICE 2011 | Yes | |
| Mitchell 2012 | Yes | |
| Has the use of mutually inconsistent data been justified (i.e. are assumptions and choices appropriate)? | NICE 2011 | NA | Sources were specific to each type of data and no calibration was possible. |
| Mitchell 2012 | NA |
| Is the process of data incorporation transparent? | NICE 2011 | Yes | Use of data from RCT described. |
| Mitchell 2012 | Yes | Use of data from RCT and population‐based study described. |
| If data have been incorporated as distributions, has the choice of distribution for each parameter been described and justified? | NICE 2011 | NA | Individual data from RCTs used to estimate parameters. |
| Mitchell 2012 | NA |
| If data have been incorporated as distributions, is it clear that second order uncertainty is reflected? | NICE 2011 | NA | |
| Mitchell 2012 | NA | |
| DATA: Assessment of uncertainty |
| Have the four principal types of uncertainty been addressed? | NICE 2011 | No | See below |
| Mitchell 2012 | No |
| If not, has the omission of particular forms of uncertainty been justified? | NICE 2011 | No | |
| Mitchell 2012 | No | |
| DATA: Assessment of uncertainty: Methodological |
| Have methodological uncertainties been addressed by running alternative versions of the model with different methodological assumptions? | NICE 2011 | No | Single model structure as far as reported in NICE document |
| Mitchell 2012 | No | Single model structure. |
| DATA: Assessment of uncertainty: Structural |
| Is there evidence that structural uncertainties have been addressed via sensitivity analysis? | NICE 2011 | Yes | Sensitivity analyses presented. |
| Mitchell 2012 | Yes |
| DATA: Assessment of uncertainty: Heterogeneity |
| Has heterogeneity been dealt with by running the model separately for different subgroups? | NICE 2011 | Yes/Unclear | The manufacturer’s subgroup analysis suggesting that ranibizumab has a favourable cost‐effectiveness profile in people with a thicker retina (central foveal thickness greater than 400 micrometres), but The Appraisal Committee concluded that it could not consider this subgroup analysis sufficiently robust to support separate recommendations to the NHS because of small sample sizes. |
| Mitchell 2012 | No | No subgroup analyses reported. |
| DATA: Assessment of uncertainty: Parameter |
| Are the methods of assessment of parameter uncertainty appropriate? | NICE 2011 | Yes | One‐way sensitivity analyses of point estimates of parameters. |
| Mitchell 2012 | Yes |
| If data are incorporated as point estimates, are the ranges used for sensitivity analysis stated clearly and justified? | NICE 2011 | Yes | |
| Mitchell 2012 | Yes | |
| CONSISTENCY: Internal consistency |
| Is there evidence that the mathematical logic of the model has been tested thoroughly before use? | NICE 2011 | Unclear | Not reported. |
| Mitchell 2012 | Unclear | Not reported. |
| CONSISTENCY: External consistency |
| Are any counterintuitive results from the model explained and justified? | NICE 2011 | Unclear | No such results. |
| Mitchell 2012 | Unclear |
| If the model has been calibrated against independent data, have any differences been explained and justified? | NICE 2011 | NA | No such calibration. |
| Mitchell 2012 | NA |
| Have the results of the model been compared with those of previous models and any differences in results explained? | NICE 2011 | NA | No previous models. |
| Mitchell 2012 | No | No comparison with NICE 2011, published in July 2011 and available to manufacturer. |