Drenaje retroperitoneal versus ningún drenaje después de la linfadenectomía pélvica para la prevención de formación de linfoquistes en pacientes con neoplasias ginecológicas
Información
- DOI:
- https://doi.org/10.1002/14651858.CD007387.pub4Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 29 junio 2017see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Cáncer ginecológico, neurooncología y otros cánceres
- Copyright:
-
- Copyright © 2019 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
Kittipat Charoenkwan: took the lead in writing the review, selected trials for inclusion, extracted data, and performed statistical analysis and interpretation of data.
Chumnan Kietpeerakool: selected trials for inclusion, extracted data, performed statistical analysis and interpretation of data, and commented on drafts of the review.
Sources of support
Internal sources
-
Department of Obstetrics and Gynaecology, Faculty of Medicine, Chiang Mai University, Thailand.
-
Department of Obstetric and Gynaecology, Faculty of Medicine, Khon Kaen University, Thailand.
External sources
-
None, Other.
Declarations of interest
Kittipat Charoenkwan is a coauthor of the article 'A prospective randomised study comparing retroperitoneal drainage with no drainage and no peritonization following radical hysterectomy and pelvic lymphadenectomy for invasive cervical cancer', published in the Journal of Obstetrics and Gynaecology Research 2002;28(3):149‐53.
Chumnan Kierpeerakool: None known
Acknowledgements
We thank Jo Morrison for clinical and editorial advice, Clare Jess, Gail Quinn, and Tracey Louise Harrison for their contributions to the editorial process, and Joanne Platt and Jane Hayes for their assistance in designing the search strategies and literature search.
The National Institute for Health Research (NIHR) is the largest single funder of the Cochrane Gynaecological Cancer Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health.
Version history
| Published | Title | Stage | Authors | Version |
| 2017 Jun 29 | Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy for the prevention of lymphocyst formation in women with gynaecological malignancies | Review | Kittipat Charoenkwan, Chumnan Kietpeerakool | |
| 2014 Jun 04 | Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy for the prevention of lymphocyst formation in patients with gynaecological malignancies | Review | Kittipat Charoenkwan, Chumnan Kietpeerakool | |
| 2010 Jan 20 | Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy for the prevention of lymphocyst formation in patients with gynaecological malignancies | Review | Kittipat Charoenkwan, Chumnan Kietpeerakool | |
| 2008 Oct 08 | Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy for the prevention of lymphocyst formation in patients with gynaecological malignancies | Protocol | Kittipat Charoenkwan, Chumnan Kietpeerakool | |
Differences between protocol and review
Searching other resources
In this update review, we added sources for ongoing trials, including the WHO International Clinical Trials Registry Platform (WHO ICTRP) (www.who.int/ictrp/en/) and ClinicalTrials.gov (www.clinicaltrials.gov), and sources of unpublished studies and grey literature including GreyNet.org (www.greynet.org), the Ohio College Library Center (OCLC) WorldCat dissertations and theses (www.oclc.org/support/services/firstsearch/documentation/dbdetails/details/WorldCatDissertations.en.html) and index to theses (ProQuest Dissertations & Theses: UK & Ireland). We also added the lists of conferences used for searching abstracts and proceedings.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Female; Humans;
PICO

Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.

PRISMA flow diagram.

Comparison 1 Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy, Outcome 1 Short‐term lymphocyst formation: both asymptomatic and symptomatic within 4 weeks after surgery.
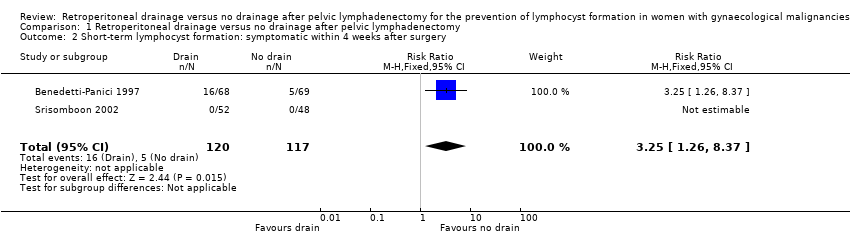
Comparison 1 Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy, Outcome 2 Short‐term lymphocyst formation: symptomatic within 4 weeks after surgery.

Comparison 1 Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy, Outcome 3 Short‐term lymphocyst formation: both asymptomatic and symptomatic at 8 weeks after surgery.
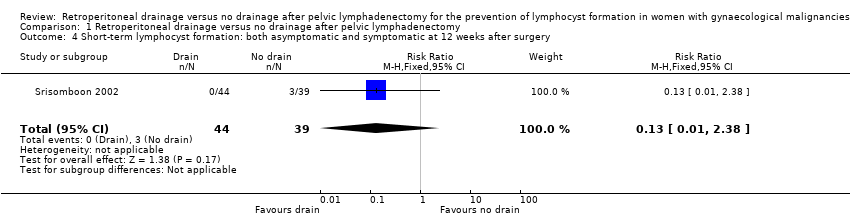
Comparison 1 Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy, Outcome 4 Short‐term lymphocyst formation: both asymptomatic and symptomatic at 12 weeks after surgery.

Comparison 1 Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy, Outcome 5 Long‐term lymphocyst formation: both asymptomatic and symptomatic at 12 months after surgery.
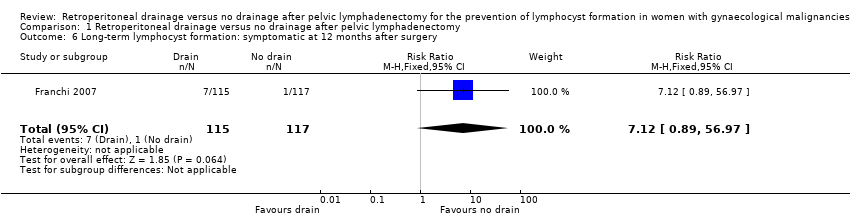
Comparison 1 Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy, Outcome 6 Long‐term lymphocyst formation: symptomatic at 12 months after surgery.
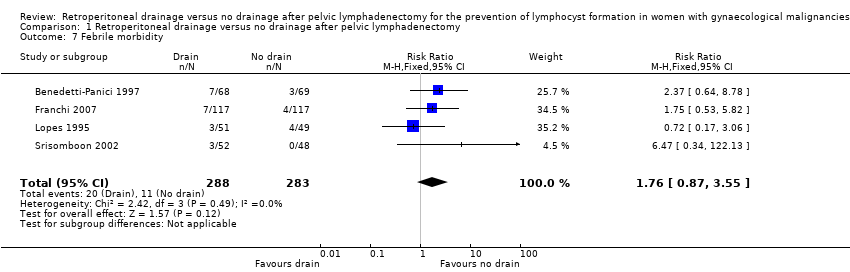
Comparison 1 Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy, Outcome 7 Febrile morbidity.

Comparison 1 Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy, Outcome 8 Pelvic infection.

Comparison 1 Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy, Outcome 9 Wound infection.

Comparison 1 Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy, Outcome 10 Wound dehiscence.

Comparison 1 Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy, Outcome 11 Fistula.

Comparison 1 Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy, Outcome 12 Bowel obstruction.

Comparison 1 Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy, Outcome 13 Leg oedema.

Comparison 1 Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy, Outcome 14 Deep venous thrombosis.

Comparison 1 Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy, Outcome 15 Symptomatic ascites.
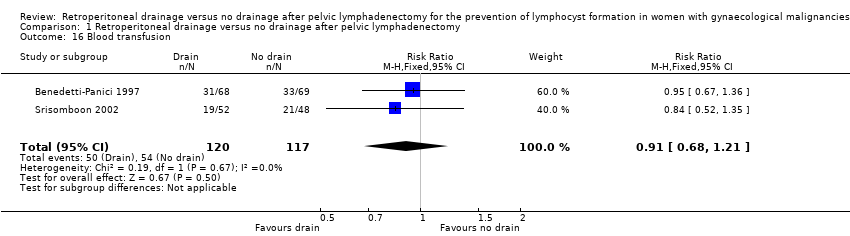
Comparison 1 Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy, Outcome 16 Blood transfusion.
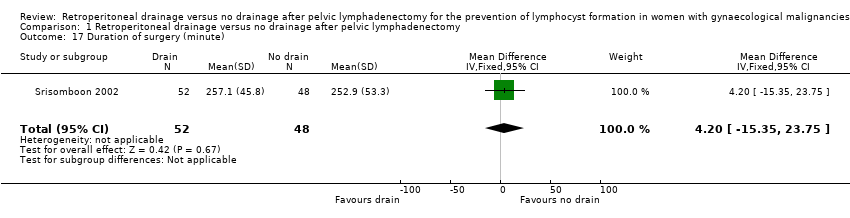
Comparison 1 Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy, Outcome 17 Duration of surgery (minute).
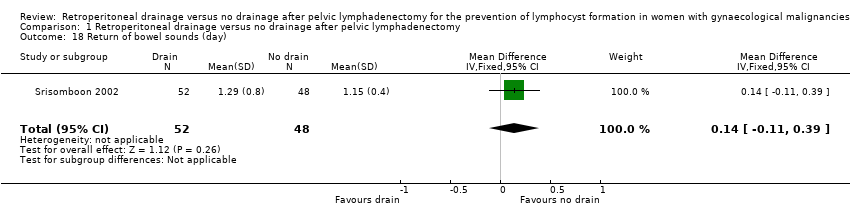
Comparison 1 Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy, Outcome 18 Return of bowel sounds (day).
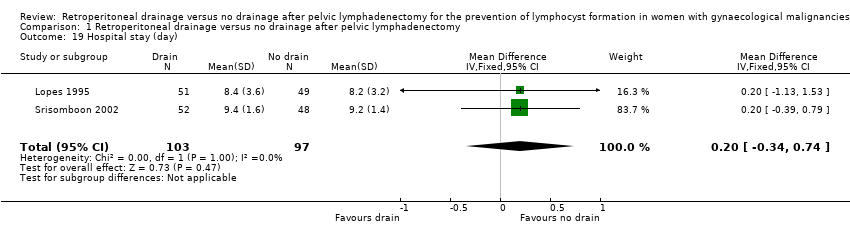
Comparison 1 Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy, Outcome 19 Hospital stay (day).
| Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy for gynaecological malignancies | ||||||
| Patient or population: Women with gynaecological malignancies | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy | |||||
| Short‐term lymphocyst formation: both asymptomatic and symptomatic within 4 weeks after surgery | Study population | RR 0.76 | 204 | ⊕⊕⊕ | ||
| 172 per 1000 | 131 per 1000 | |||||
| Medium‐risk population | ||||||
| 161 per 1000 | 122 per 1000 | |||||
| Short‐term lymphocyst formation: symptomatic within 4 weeks after surgery | Study population | RR 3.25 | 237 | ⊕⊕⊕⊕ | ||
| 43 per 1000 | 140 per 1000 | |||||
| Medium‐risk population | ||||||
| 36 per 1000 | 117 per 1000 | |||||
| Short‐term lymphocyst formation: both asymptomatic and symptomatic at 8 weeks after surgery | Study population | RR 0.72 | 180 | ⊕⊕⊕⊕ | ||
| 112 per 1000 | 81 per 1000 | |||||
| Medium‐risk population | ||||||
| 110 per 1000 | 79 per 1000 | |||||
| Long‐term lymphocyst formation: both asymptomatic and symptomatic at 12 months after surgery | Study population | RR 1.48 | 232 | ⊕⊕⊕⊕ | ||
| 171 per 1000 | 253 per 1000 | |||||
| Medium‐risk population | ||||||
| 171 per 1000 | 253 per 1000 | |||||
| Long‐term lymphocyst formation: symptomatic at 12 months after surgery | Study population | RR 7.12 | 232 | ⊕⊕⊕⊕ | ||
| 9 per 1000 | 64 per 1000 | |||||
| Medium‐risk population | ||||||
| 9 per 1000 | 64 per 1000 | |||||
| Febrile morbidity | Study population | RR 1.76 | 571 | ⊕⊕⊕⊕ | ||
| 39 per 1000 | 69 per 1000 | |||||
| Medium‐risk population | ||||||
| 39 per 1000 | 69 per 1000 | |||||
| Pelvic infection | Study population | RR 0.42 | 571 | ⊕⊕⊕ | ||
| 18 per 1000 | 8 per 1000 | |||||
| Medium‐risk population | ||||||
| 19 per 1000 | 8 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Wide confidence interval. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Short‐term lymphocyst formation: both asymptomatic and symptomatic within 4 weeks after surgery Show forest plot | 2 | 204 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.04, 13.35] |
| 2 Short‐term lymphocyst formation: symptomatic within 4 weeks after surgery Show forest plot | 2 | 237 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.25 [1.26, 8.37] |
| 3 Short‐term lymphocyst formation: both asymptomatic and symptomatic at 8 weeks after surgery Show forest plot | 2 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.30, 1.71] |
| 4 Short‐term lymphocyst formation: both asymptomatic and symptomatic at 12 weeks after surgery Show forest plot | 1 | 83 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.01, 2.38] |
| 5 Long‐term lymphocyst formation: both asymptomatic and symptomatic at 12 months after surgery Show forest plot | 1 | 232 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.48 [0.89, 2.45] |
| 6 Long‐term lymphocyst formation: symptomatic at 12 months after surgery Show forest plot | 1 | 232 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.12 [0.89, 56.97] |
| 7 Febrile morbidity Show forest plot | 4 | 571 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.76 [0.87, 3.55] |
| 8 Pelvic infection Show forest plot | 4 | 571 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.11, 1.62] |
| 9 Wound infection Show forest plot | 2 | 334 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.07, 1.18] |
| 10 Wound dehiscence Show forest plot | 2 | 237 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.14, 6.89] |
| 11 Fistula Show forest plot | 3 | 471 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.34, 4.57] |
| 12 Bowel obstruction Show forest plot | 2 | 334 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.12] |
| 13 Leg oedema Show forest plot | 1 | 137 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.71 [0.75, 9.77] |
| 14 Deep venous thrombosis Show forest plot | 2 | 371 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.02 [0.38, 10.84] |
| 15 Symptomatic ascites Show forest plot | 1 | 137 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.12, 3.92] |
| 16 Blood transfusion Show forest plot | 2 | 237 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.68, 1.21] |
| 17 Duration of surgery (minute) Show forest plot | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | 4.20 [‐15.35, 23.75] |
| 18 Return of bowel sounds (day) Show forest plot | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | 0.14 [‐0.11, 0.39] |
| 19 Hospital stay (day) Show forest plot | 2 | 200 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.34, 0.74] |

