Relajación para la depresión
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en curso
Referencias adicionales
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Was allocation sequence adequately generated: No | |
| Participants | Primary or Secondary depression: Primary | |
| Interventions | RELAXATION PSYCHOLOGICAL THERAPY ANTIDEPRESSANTS | |
| Outcomes | 1) Depression: Beck Depression Inventory (Beck et al, 1961, 1979) (self rated) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
| Methods | Was allocation sequence adequately generated: Unclear | |
| Participants | Primary or Secondary depression: Primary | |
| Interventions | RELAXATION PSYCHOLOGICAL THERAPY | |
| Outcomes | 1) Depression: Beck Depression Inventory (BDI) (Beck et al, 1961) (self rated) | |
| Notes | Data were not presented separately for each group so could not be pooled. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Was allocation sequence adequately generated: Unclear | |
| Participants | Primary or Secondary depression: Primary (post‐natal) | |
| Interventions | RELAXATION MASSAGE THERAPY | |
| Outcomes | 1) Depressed mood: Profile of Mood States (McNair et al, 1971) (self rated) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Was allocation sequence adequately generated: Unclear | |
| Participants | Primary or Secondary depression: Primary (in pregnant women) | |
| Interventions | RELAXATION MASSAGE THERAPY NO TREATMENT CONTROL | |
| Outcomes | 1) Depression: Center for Epidemiologic Studies‐Depression (Radloff, 1977) (self rated) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Was allocation sequence adequately generated: Unclear | |
| Participants | Primary or Secondary depression: Primary | |
| Interventions | RELAXATION PSYCHOLOGICAL THERAPY 1 PSYCHOLOGICAL THERAPY 2 WAIT‐LIST CONTROL | |
| Outcomes | 1) Depression: Reynolds Adolescent Depression Scale (RADS) (Reynolds, 1987) (self rated) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
| Methods | Was allocation sequence adequately generated: No | |
| Participants | Primary or Secondary depression: Primary | |
| Interventions | RELAXATION PSYCHOLOGICAL THERAPY WAITLIST CONTROL | |
| Outcomes | 1) Depression: German version of Beck Depression Inventory (self report) (BDI; Hautzinger et al., 1994) | |
| Notes | Cross‐over study: data extracted from pre‐crossover only. Study also had assessments at 20 weeks, 8 months and 3 years. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
| Methods | Was allocation sequence adequately generated: Unclear | |
| Participants | Primary or Secondary depression: Primary | |
| Interventions | RELAXATION EXERCISE NO TREATMENT CONTROL | |
| Outcomes | 1) Depression: Beck Depression Inventory (Beck et al, 1961) (self rated) | |
| Notes | Means were estimated from Figure 1. SDs were imputed from results of post hoc paired comparison t‐tests. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Was allocation sequence adequately generated: Unclear | |
| Participants | Primary or Secondary depression: Primary | |
| Interventions | RELAXATION ANTIDEPRESSANTS PSYCHOLOGICAL THERAPY 1 PSYCHOLOGICAL THERAPY 2 | |
| Outcomes | 1) Depression: Depression Adjective Check List (Lubin, 1965) (self rated) | |
| Notes | No SDs present for post and follow‐up scores, therefore pre‐intervention SDs used. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Was allocation sequence adequately generated: Yes | |
| Participants | Primary or Secondary depression: Primary | |
| Interventions | RELAXATION PSYCHOLOGICAL THERAPY ANTIDEPRESSANTS | |
| Outcomes | 1) Depression: Beck Depression Inventory (self rated) | |
| Notes | Used "response" defined as 50% reduction on clinician rated scale, and "recovery" defined as <=9 on self‐rated scale (BDI) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
| Methods | Was allocation sequence adequately generated: Unclear | |
| Participants | Primary or Secondary depression: Primary | |
| Interventions | RELAXATION PSYCHOLOGICAL THERAPY PSYCHOLOGICAL THERAPY | |
| Outcomes | 1) Depression: Zung Self‐Rated Depression Scale (self rated) (Zung, 1965) | |
| Notes | Reported as study 2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Was allocation sequence adequately generated: Unclear | |
| Participants | Primary or Secondary depression: Primary | |
| Interventions | RELAXATION PSYCHOLOGICAL THERAPY PSYCHOLOGICAL THERAPY | |
| Outcomes | 1) Depression: Beck Depression Inventory (BDI) (self rated) (Beck et al, 1961) | |
| Notes | Reported as study 3. Study also included a wait‐list arm which did not have random assignment. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Was allocation sequence adequately generated: Unclear | |
| Participants | Primary or Secondary depression: Primary | |
| Interventions | RELAXATION PSYCHOLOGICAL THERAPY WAITLIST CONTROL | |
| Outcomes | 1) Depression:RADS (Reynolds, 1986) (self report) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Was allocation sequence adequately generated: Unclear | |
| Participants | Primary or Secondary depression: Primary | |
| Interventions | RELAXATION LIGHT TREATMENT | |
| Outcomes | 1) Depression: Children's depression rating scale (CDRS‐R) (Poznanski et al, 1984) (clinician rated) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Was allocation sequence adequately generated: Unclear | |
| Participants | Primary or Secondary depression: Primary | |
| Interventions | RELAXATION PSYCHOLOGICAL THERAPY MINIMAL CONTACT | |
| Outcomes | 1) Depression: BDI (Beck et al, 1961) (self rated) | |
| Notes | There was also another treatment arm where each of the three treatment conditions (relaxation, psychological therapy, minimal contact) concurrently took an antidepressant, rather than placebo | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Was allocation sequence adequately generated: Unclear | |
| Participants | Primary or Secondary depression: Primary | |
| Interventions | RELAXATION PSYCHOLOGICAL THERAPY | |
| Outcomes | 1) Depression: Mood and Feelings Questionnaire (MFQ) (Angold et al, 1987) (self report) | |
| Notes | SE for MFQ estimated from Figure1. SDs imputed from SEs. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Depression symptoms not measured on a validated, reliable depression symptom scale | |
| Non randomised study | |
| Relaxation intervention was part of a CBT package | |
| Participants not selected for diagnosed depression or high depression symptom score | |
| Participants not selected for diagnosed depression or high depression symptom score | |
| Participants not selected for diagnosed depression or high depression symptom score | |
| Participants not selected for diagnosed depression or high depression symptom score | |
| Inadequate relaxation intervention | |
| Participants not selected for diagnosed depression or high depression symptom score | |
| Participants not selected for diagnosed depression or high depression symptom score | |
| Participants had comorbid anxiety. | |
| Participants not selected for diagnosed depression or high depression symptom score | |
| Non randomised study | |
| Relaxation intervention based on yoga and meditation | |
| Inadequate relaxation intervention | |
| Relaxation intervention was based on yoga and participants not selected for diagnosed depression or high depression symptom score | |
| Participants not selected for diagnosed depression or high depression symptom score | |
| Participants not selected for diagnosed depression or high depression symptom score | |
| Participants not selected for diagnosed depression or high depression symptom score | |
| Relaxation intervention arm was dropped from the trial | |
| Participants not selected for diagnosed depression or high depression symptom score | |
| Participants not selected for diagnosed depression or high depression symptom score | |
| Relaxation included as part of a broader intervention (counselling). | |
| Participants not selected for diagnosed depression or high depression symptom score | |
| Participants not selected for diagnosed depression or high depression symptom score | |
| Participants not selected for diagnosed depression or high depression symptom score | |
| Non randomised study | |
| Participants not selected for diagnosed depression or high depression symptom score | |
| Relaxation intervention based on hypnosis. | |
| Participants not selected for diagnosed depression or high depression symptom score | |
| Depression not measured as an outcome | |
| Data on relaxation group not presented |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Pilot study of the short‐term effects of a multi‐sensory environment (MSE) on elderly patients suffering from depression |
| Methods | |
| Participants | Primary or Secondary depression: Primary |
| Interventions | RELAXATION MULTI‐SENSORY ENVIRONMENT (MSE) |
| Outcomes | Hospital Anxiety and Depression Scale (HADS) |
| Starting date | 1 September 2003 |
| Contact information | Sarah Baillon |
| Notes |
| Trial name or title | The DEMO trial: A randomized, parallel‐group, observer‐blinded clinical trial of aerobic versus non‐aerobic versus relaxation training for patients with light to moderate depression |
| Methods | |
| Participants | Primary or Secondary depression: Primary |
| Interventions | RELAXATION EXERCISE EXERCISE |
| Outcomes | 1) Depression: Hamilton Depression Scale‐17 (clinician rated), Beck Depression Inventory II (self rated), Montgomery‐Asberg Depression Rating Scale (self‐rated) |
| Starting date | February 2005 |
| Contact information | Jesper Krogh |
| Notes |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Depression scores ‐ self rated post intervention Show forest plot | 5 | 136 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.59 [‐0.94, ‐0.24] |
| Analysis 1.1  Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 1 Depression scores ‐ self rated post intervention. | ||||
| 2 Depression scores ‐ self rated follow‐up (short‐term) Show forest plot | 2 | 48 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.74 [‐1.34, ‐0.15] |
| Analysis 1.2  Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 2 Depression scores ‐ self rated follow‐up (short‐term). | ||||
| 3 Depression scores ‐ self rated follow‐up (long‐term) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.3  Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 3 Depression scores ‐ self rated follow‐up (long‐term). | ||||
| 4 Depression scores ‐ clinician rated post intervention Show forest plot | 2 | 52 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.35 [‐3.06, 0.37] |
| Analysis 1.4  Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 4 Depression scores ‐ clinician rated post intervention. | ||||
| 5 Depression scores ‐ clinician rated follow‐up (short‐term) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.5  Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 5 Depression scores ‐ clinician rated follow‐up (short‐term). | ||||
| 6 Non response/remission ‐ self rated post intervention Show forest plot | 2 | 52 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.28 [0.14, 0.54] |
| Analysis 1.6  Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 6 Non response/remission ‐ self rated post intervention. | ||||
| 7 Non response/remission ‐ self rated follow‐up (short‐term) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.7  Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 7 Non response/remission ‐ self rated follow‐up (short‐term). | ||||
| 8 Non response/remission ‐ clinician rated post intervention Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.8  Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 8 Non response/remission ‐ clinician rated post intervention. | ||||
| 9 Dropouts during intervention Show forest plot | 4 | 122 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.08, 6.73] |
| Analysis 1.9  Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 9 Dropouts during intervention. | ||||
| 10 Dropouts during follow‐up (short‐term) Show forest plot | 2 | 54 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.19, 5.29] |
| Analysis 1.10  Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 10 Dropouts during follow‐up (short‐term). | ||||
| 11 Dropouts during follow‐up (long‐term) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.11  Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 11 Dropouts during follow‐up (long‐term). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Depression scores ‐ self rated post intervention Show forest plot | 9 | 286 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.38 [0.14, 0.62] |
| Analysis 2.1  Comparison 2 Relaxation versus psychological treatment, Outcome 1 Depression scores ‐ self rated post intervention. | ||||
| 2 Depression scores ‐ self rated follow‐up (short‐term) Show forest plot | 6 | 192 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.36 [0.07, 0.65] |
| Analysis 2.2  Comparison 2 Relaxation versus psychological treatment, Outcome 2 Depression scores ‐ self rated follow‐up (short‐term). | ||||
| 3 Depression scores ‐ self rated follow‐up (long‐term) Show forest plot | 2 | 62 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.11 [‐0.39, 0.61] |
| Analysis 2.3  Comparison 2 Relaxation versus psychological treatment, Outcome 3 Depression scores ‐ self rated follow‐up (long‐term). | ||||
| 4 Depression scores ‐ clinician rated post intervention Show forest plot | 3 | 72 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.29 [‐0.18, 0.75] |
| Analysis 2.4  Comparison 2 Relaxation versus psychological treatment, Outcome 4 Depression scores ‐ clinician rated post intervention. | ||||
| 5 Depression scores ‐ clinician rated follow‐up (short‐term) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.5  Comparison 2 Relaxation versus psychological treatment, Outcome 5 Depression scores ‐ clinician rated follow‐up (short‐term). | ||||
| 6 Non response/remission ‐ self rated post intervention Show forest plot | 5 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.71 [1.25, 2.34] |
| Analysis 2.6  Comparison 2 Relaxation versus psychological treatment, Outcome 6 Non response/remission ‐ self rated post intervention. | ||||
| 7 Non response/remission ‐ self rated follow‐up (short‐term) Show forest plot | 3 | 89 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.88 [1.05, 3.34] |
| Analysis 2.7  Comparison 2 Relaxation versus psychological treatment, Outcome 7 Non response/remission ‐ self rated follow‐up (short‐term). | ||||
| 8 Non response/remission ‐ clinician rated post intervention Show forest plot | 3 | 104 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.96 [1.20, 3.22] |
| Analysis 2.8  Comparison 2 Relaxation versus psychological treatment, Outcome 8 Non response/remission ‐ clinician rated post intervention. | ||||
| 9 Non response/remission ‐ clinician rated follow‐up (short‐term) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.9  Comparison 2 Relaxation versus psychological treatment, Outcome 9 Non response/remission ‐ clinician rated follow‐up (short‐term). | ||||
| 10 Dropouts during intervention Show forest plot | 8 | 289 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.59 [0.83, 3.05] |
| Analysis 2.10  Comparison 2 Relaxation versus psychological treatment, Outcome 10 Dropouts during intervention. | ||||
| 11 Dropouts during follow‐up (short‐term) Show forest plot | 5 | 135 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.54 [0.43, 5.51] |
| Analysis 2.11  Comparison 2 Relaxation versus psychological treatment, Outcome 11 Dropouts during follow‐up (short‐term). | ||||
| 12 Dropouts during follow‐up (long‐term) Show forest plot | 2 | 73 | Risk Ratio (M‐H, Random, 95% CI) | 2.72 [0.03, 251.39] |
| Analysis 2.12  Comparison 2 Relaxation versus psychological treatment, Outcome 12 Dropouts during follow‐up (long‐term). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Depression scores ‐ self rated post intervention Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.1  Comparison 3 Relaxation versus lifestyle and complementary treatments, Outcome 1 Depression scores ‐ self rated post intervention. | ||||
| 2 Dropouts during intervention Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.2  Comparison 3 Relaxation versus lifestyle and complementary treatments, Outcome 2 Dropouts during intervention. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Depression scores ‐ self rated post intervention Show forest plot | 2 | 115 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.59 [‐2.07, 0.89] |
| Analysis 4.1  Comparison 4 Relaxation versus medication, Outcome 1 Depression scores ‐ self rated post intervention. | ||||
| 2 Depression scores ‐ self rated follow‐up (short‐term) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.2  Comparison 4 Relaxation versus medication, Outcome 2 Depression scores ‐ self rated follow‐up (short‐term). | ||||
| 3 Depression scores ‐ clinician rated post intervention Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.3  Comparison 4 Relaxation versus medication, Outcome 3 Depression scores ‐ clinician rated post intervention. | ||||
| 4 Non response/remission ‐ self rated post intervention Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.4  Comparison 4 Relaxation versus medication, Outcome 4 Non response/remission ‐ self rated post intervention. | ||||
| 5 Dropouts during intervention Show forest plot | 2 | 127 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.39, 1.31] |
| Analysis 4.5  Comparison 4 Relaxation versus medication, Outcome 5 Dropouts during intervention. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Depression scores ‐ self rated post intervention (SMD) Show forest plot | 2 | 40 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.56, ‐0.24] |
| Analysis 5.1  Comparison 5 Relaxation + medication versus medication alone, Outcome 1 Depression scores ‐ self rated post intervention (SMD). | ||||
| 2 Depression scores ‐ self rated post intervention (WMD) Show forest plot | 2 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐8.03 [‐13.32, ‐2.74] |
| Analysis 5.2  Comparison 5 Relaxation + medication versus medication alone, Outcome 2 Depression scores ‐ self rated post intervention (WMD). | ||||
| 3 Depression scores ‐ self rated follow‐up (long‐term, SMD) Show forest plot | 1 | 20 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.90, 0.86] |
| Analysis 5.3  Comparison 5 Relaxation + medication versus medication alone, Outcome 3 Depression scores ‐ self rated follow‐up (long‐term, SMD). | ||||
| 4 Depression scores ‐ self rated follow‐up (long‐term, WMD) Show forest plot | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐9.18, 8.78] |
| Analysis 5.4  Comparison 5 Relaxation + medication versus medication alone, Outcome 4 Depression scores ‐ self rated follow‐up (long‐term, WMD). | ||||
| 5 Depression scores ‐ clinician rated post intervention (SMD) Show forest plot | 1 | 20 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐1.08, 0.68] |
| Analysis 5.5  Comparison 5 Relaxation + medication versus medication alone, Outcome 5 Depression scores ‐ clinician rated post intervention (SMD). | ||||
| 6 Depression scores ‐ clinician rated post intervention (WMD) Show forest plot | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐1.20 [‐6.23, 3.83] |
| Analysis 5.6  Comparison 5 Relaxation + medication versus medication alone, Outcome 6 Depression scores ‐ clinician rated post intervention (WMD). | ||||
| 7 Non response/remission ‐ self rated post intervention Show forest plot | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.05 [0.00, 0.72] |
| Analysis 5.7  Comparison 5 Relaxation + medication versus medication alone, Outcome 7 Non response/remission ‐ self rated post intervention. | ||||
| 8 Non response/remission ‐ clinician rated post intervention Show forest plot | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.78, 1.63] |
| Analysis 5.8  Comparison 5 Relaxation + medication versus medication alone, Outcome 8 Non response/remission ‐ clinician rated post intervention. | ||||
| 9 Dropouts during intervention Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.9  Comparison 5 Relaxation + medication versus medication alone, Outcome 9 Dropouts during intervention. | ||||

Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 1 Depression scores ‐ self rated post intervention.

Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 2 Depression scores ‐ self rated follow‐up (short‐term).

Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 3 Depression scores ‐ self rated follow‐up (long‐term).

Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 4 Depression scores ‐ clinician rated post intervention.

Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 5 Depression scores ‐ clinician rated follow‐up (short‐term).

Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 6 Non response/remission ‐ self rated post intervention.
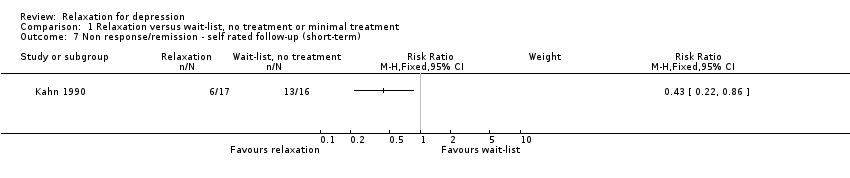
Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 7 Non response/remission ‐ self rated follow‐up (short‐term).
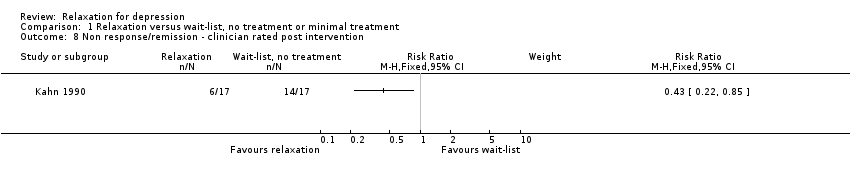
Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 8 Non response/remission ‐ clinician rated post intervention.

Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 9 Dropouts during intervention.
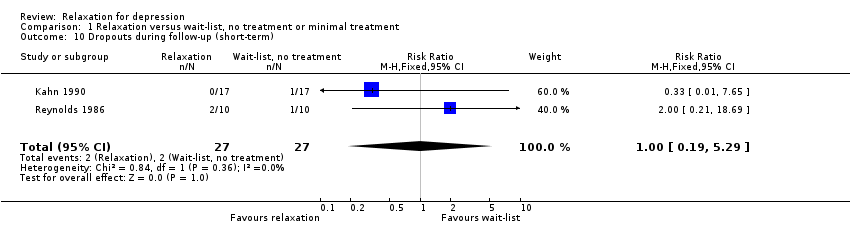
Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 10 Dropouts during follow‐up (short‐term).

Comparison 1 Relaxation versus wait‐list, no treatment or minimal treatment, Outcome 11 Dropouts during follow‐up (long‐term).

Comparison 2 Relaxation versus psychological treatment, Outcome 1 Depression scores ‐ self rated post intervention.

Comparison 2 Relaxation versus psychological treatment, Outcome 2 Depression scores ‐ self rated follow‐up (short‐term).
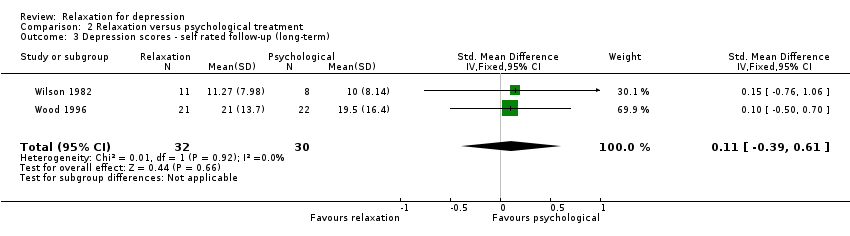
Comparison 2 Relaxation versus psychological treatment, Outcome 3 Depression scores ‐ self rated follow‐up (long‐term).

Comparison 2 Relaxation versus psychological treatment, Outcome 4 Depression scores ‐ clinician rated post intervention.

Comparison 2 Relaxation versus psychological treatment, Outcome 5 Depression scores ‐ clinician rated follow‐up (short‐term).
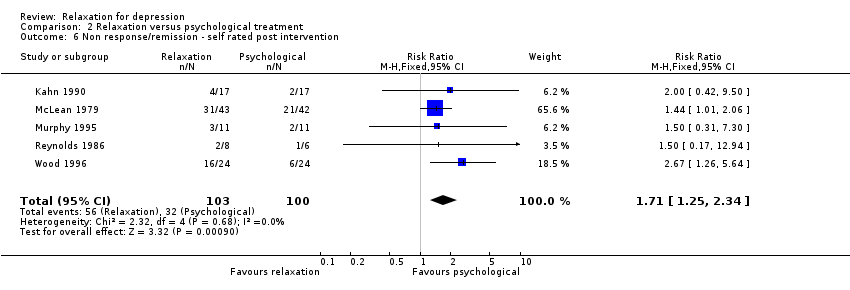
Comparison 2 Relaxation versus psychological treatment, Outcome 6 Non response/remission ‐ self rated post intervention.

Comparison 2 Relaxation versus psychological treatment, Outcome 7 Non response/remission ‐ self rated follow‐up (short‐term).

Comparison 2 Relaxation versus psychological treatment, Outcome 8 Non response/remission ‐ clinician rated post intervention.
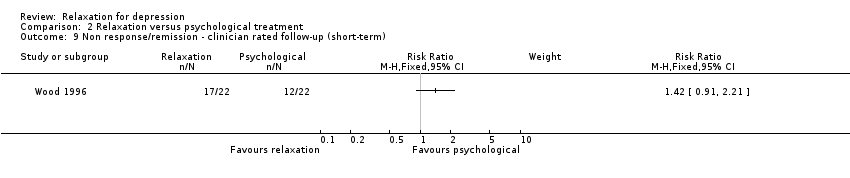
Comparison 2 Relaxation versus psychological treatment, Outcome 9 Non response/remission ‐ clinician rated follow‐up (short‐term).
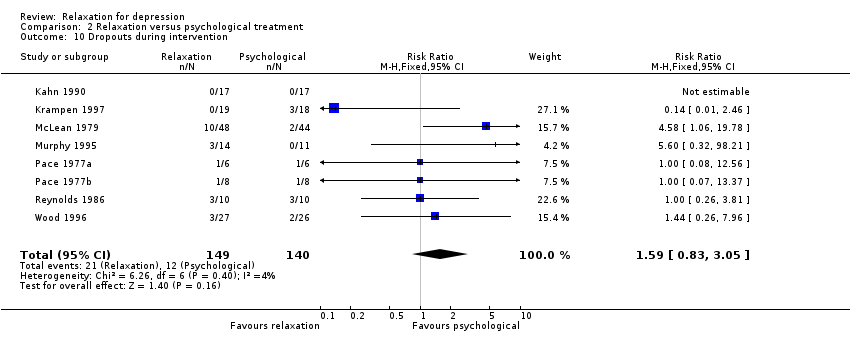
Comparison 2 Relaxation versus psychological treatment, Outcome 10 Dropouts during intervention.

Comparison 2 Relaxation versus psychological treatment, Outcome 11 Dropouts during follow‐up (short‐term).
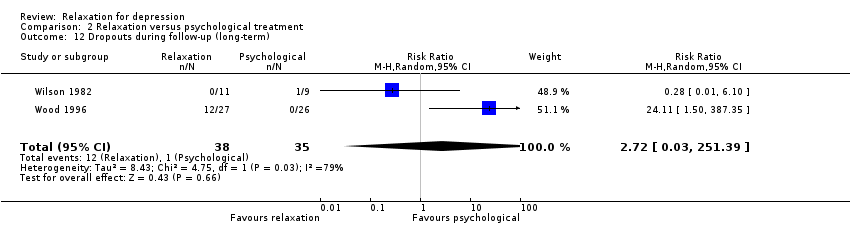
Comparison 2 Relaxation versus psychological treatment, Outcome 12 Dropouts during follow‐up (long‐term).
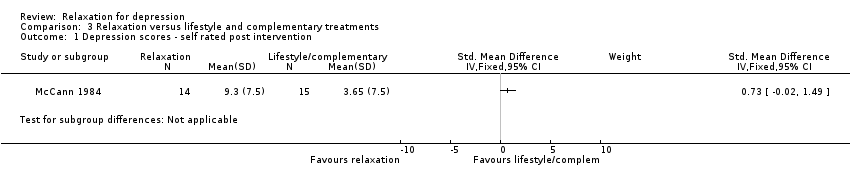
Comparison 3 Relaxation versus lifestyle and complementary treatments, Outcome 1 Depression scores ‐ self rated post intervention.

Comparison 3 Relaxation versus lifestyle and complementary treatments, Outcome 2 Dropouts during intervention.
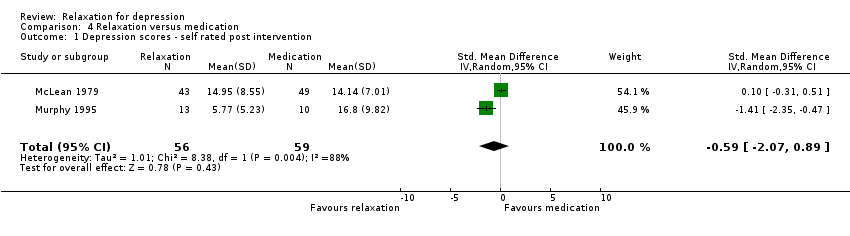
Comparison 4 Relaxation versus medication, Outcome 1 Depression scores ‐ self rated post intervention.

Comparison 4 Relaxation versus medication, Outcome 2 Depression scores ‐ self rated follow‐up (short‐term).

Comparison 4 Relaxation versus medication, Outcome 3 Depression scores ‐ clinician rated post intervention.

Comparison 4 Relaxation versus medication, Outcome 4 Non response/remission ‐ self rated post intervention.

Comparison 4 Relaxation versus medication, Outcome 5 Dropouts during intervention.

Comparison 5 Relaxation + medication versus medication alone, Outcome 1 Depression scores ‐ self rated post intervention (SMD).
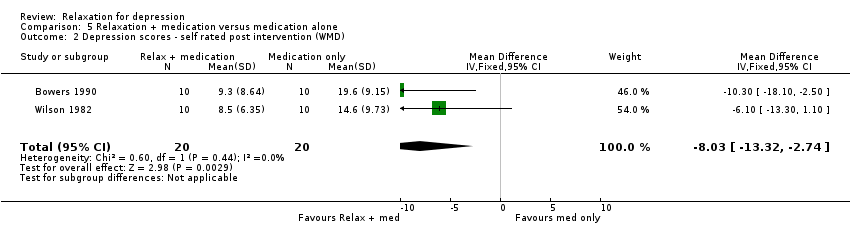
Comparison 5 Relaxation + medication versus medication alone, Outcome 2 Depression scores ‐ self rated post intervention (WMD).

Comparison 5 Relaxation + medication versus medication alone, Outcome 3 Depression scores ‐ self rated follow‐up (long‐term, SMD).
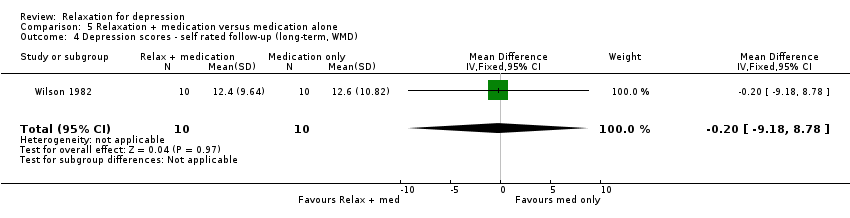
Comparison 5 Relaxation + medication versus medication alone, Outcome 4 Depression scores ‐ self rated follow‐up (long‐term, WMD).

Comparison 5 Relaxation + medication versus medication alone, Outcome 5 Depression scores ‐ clinician rated post intervention (SMD).
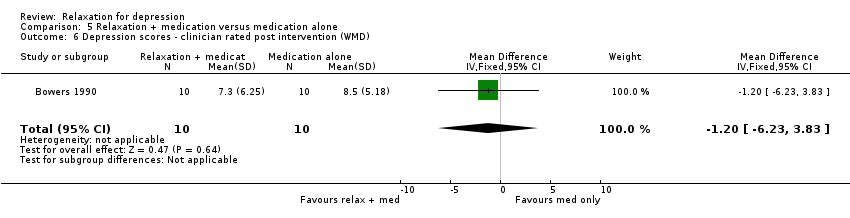
Comparison 5 Relaxation + medication versus medication alone, Outcome 6 Depression scores ‐ clinician rated post intervention (WMD).
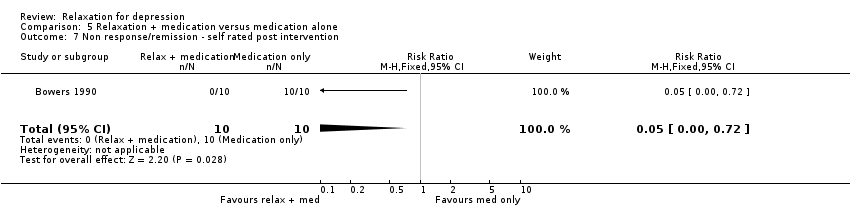
Comparison 5 Relaxation + medication versus medication alone, Outcome 7 Non response/remission ‐ self rated post intervention.
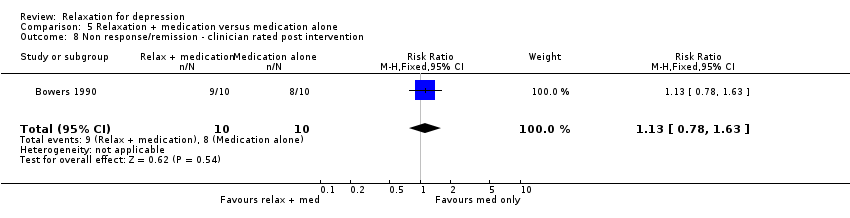
Comparison 5 Relaxation + medication versus medication alone, Outcome 8 Non response/remission ‐ clinician rated post intervention.

Comparison 5 Relaxation + medication versus medication alone, Outcome 9 Dropouts during intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Depression scores ‐ self rated post intervention Show forest plot | 5 | 136 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.59 [‐0.94, ‐0.24] |
| 2 Depression scores ‐ self rated follow‐up (short‐term) Show forest plot | 2 | 48 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.74 [‐1.34, ‐0.15] |
| 3 Depression scores ‐ self rated follow‐up (long‐term) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4 Depression scores ‐ clinician rated post intervention Show forest plot | 2 | 52 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.35 [‐3.06, 0.37] |
| 5 Depression scores ‐ clinician rated follow‐up (short‐term) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6 Non response/remission ‐ self rated post intervention Show forest plot | 2 | 52 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.28 [0.14, 0.54] |
| 7 Non response/remission ‐ self rated follow‐up (short‐term) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8 Non response/remission ‐ clinician rated post intervention Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9 Dropouts during intervention Show forest plot | 4 | 122 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.08, 6.73] |
| 10 Dropouts during follow‐up (short‐term) Show forest plot | 2 | 54 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.19, 5.29] |
| 11 Dropouts during follow‐up (long‐term) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Depression scores ‐ self rated post intervention Show forest plot | 9 | 286 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.38 [0.14, 0.62] |
| 2 Depression scores ‐ self rated follow‐up (short‐term) Show forest plot | 6 | 192 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.36 [0.07, 0.65] |
| 3 Depression scores ‐ self rated follow‐up (long‐term) Show forest plot | 2 | 62 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.11 [‐0.39, 0.61] |
| 4 Depression scores ‐ clinician rated post intervention Show forest plot | 3 | 72 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.29 [‐0.18, 0.75] |
| 5 Depression scores ‐ clinician rated follow‐up (short‐term) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6 Non response/remission ‐ self rated post intervention Show forest plot | 5 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.71 [1.25, 2.34] |
| 7 Non response/remission ‐ self rated follow‐up (short‐term) Show forest plot | 3 | 89 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.88 [1.05, 3.34] |
| 8 Non response/remission ‐ clinician rated post intervention Show forest plot | 3 | 104 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.96 [1.20, 3.22] |
| 9 Non response/remission ‐ clinician rated follow‐up (short‐term) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10 Dropouts during intervention Show forest plot | 8 | 289 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.59 [0.83, 3.05] |
| 11 Dropouts during follow‐up (short‐term) Show forest plot | 5 | 135 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.54 [0.43, 5.51] |
| 12 Dropouts during follow‐up (long‐term) Show forest plot | 2 | 73 | Risk Ratio (M‐H, Random, 95% CI) | 2.72 [0.03, 251.39] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Depression scores ‐ self rated post intervention Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2 Dropouts during intervention Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Depression scores ‐ self rated post intervention Show forest plot | 2 | 115 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.59 [‐2.07, 0.89] |
| 2 Depression scores ‐ self rated follow‐up (short‐term) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3 Depression scores ‐ clinician rated post intervention Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4 Non response/remission ‐ self rated post intervention Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5 Dropouts during intervention Show forest plot | 2 | 127 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.39, 1.31] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Depression scores ‐ self rated post intervention (SMD) Show forest plot | 2 | 40 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.56, ‐0.24] |
| 2 Depression scores ‐ self rated post intervention (WMD) Show forest plot | 2 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐8.03 [‐13.32, ‐2.74] |
| 3 Depression scores ‐ self rated follow‐up (long‐term, SMD) Show forest plot | 1 | 20 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.90, 0.86] |
| 4 Depression scores ‐ self rated follow‐up (long‐term, WMD) Show forest plot | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐9.18, 8.78] |
| 5 Depression scores ‐ clinician rated post intervention (SMD) Show forest plot | 1 | 20 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐1.08, 0.68] |
| 6 Depression scores ‐ clinician rated post intervention (WMD) Show forest plot | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐1.20 [‐6.23, 3.83] |
| 7 Non response/remission ‐ self rated post intervention Show forest plot | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.05 [0.00, 0.72] |
| 8 Non response/remission ‐ clinician rated post intervention Show forest plot | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.78, 1.63] |
| 9 Dropouts during intervention Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |

