Dacriocistorrinostomía endonasal versus externa para la obstrucción del conducto nasolagrimal
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en espera de evaluación
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomised controlled trial; simple parallel group design with participants individually randomised to one of two intervention groups | |
| Participants | Country: Finland 64 eyes (63 participants) Age: range 23 to 89 years | |
| Interventions | Intervention 1: endonasal laser‐assisted dacryocystorhinostomy | |
| Outcomes | Patent lacrimal passage on irrigation at one year | |
| Notes | Operations performed between January and December 1994, manuscript received May 1997. Study supported in part by a grant from the Turku University Foundation, Turku, Finland. The authors did not have any proprietary interest in any of the equipment mentioned in the article. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description of sequence generation is provided in the trial report. |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment is provided in the trial report. |
| Blinding (performance bias and detection bias) | Unclear risk | No description of masking either the participants or outcome assessors is provided in the trial report. |
| Incomplete outcome data (attrition bias) | Low risk | At 12 months follow‐up all participants in both groups were assessed for success. Complication rates were also determined for the whole study group. Therefore there was no incomplete data. |
| Methods | Randomised controlled trial; simple parallel group design with participants individually randomised to one of two intervention groups | |
| Participants | Country: India 40 eyes (40 participants) Age: 16‐68 Mean age: not specified | |
| Interventions | Intervention 1: endonasal mechanical dacryocystorhinostomy using punch forceps | |
| Outcomes | Patent lacrimal drainage system on sac syringing at the end of 6 months | |
| Notes | Date of submission: December 2010 (date of study not available from article). No competing interests declared by authors. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'They were randomised into two groups' with no further description. |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment is provided in the trial report. |
| Blinding (performance bias and detection bias) | Unclear risk | Masking of surgeons not possible. No description of masking either the participants or outcome assessors is provided in the trial report. |
| Incomplete outcome data (attrition bias) | Low risk | At 6 months there were no participants lost to follow‐up. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Even though the authors describe their surgery as endonasal, the technique described in the full‐text of the trial is that of transcanalicular rather than endonasal DCR. | |
| Prospective study comparing outcomes of external DCR, mechanical endonasal DCR and transcanalicular DCR using multidiode laser. Study excluded as it was non‐randomised, the procedure being chosen according to participant preference. | |
| The endoscopic procedure involved a transcanalicular approach with the diode laser probe instead of an endonasal one. | |
| The same group conducted the two studies: Hartikainen 1998 and Hartikainen 1998b. The external DCR group in these two studies appear to be the same. We were unsuccessful in our attempts to contact the authors to clarify this matter. | |
| This trial uses a lacrimal microendoscope with a trephine to remove fibrous obstruction along the lacrimal sac and nasolacrimal sac. It does not create an alternative drainage pathway using an endonasal technique which is what our review evaluates. | |
| This study used a transcanalicular approach using a fifth generation lacrimal endoscope with a microdrill, instead of an endonasal technique. | |
| Alternate allocation used, therefore this study does not qualify as a randomised controlled trial. | |
| The full‐text article revealed that the study was not a randomised trial. |
DCR: dacryocystorhinostomy
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Participants randomly divided into 3 treatment groups; details of randomisation process not available |
| Participants | 182 cases (202 eyes) |
| Interventions | External dacryocystorhinostomy Endonasal endoscopic dacryocystorhinostomy Nd:YAG laser dacryoplasty |
| Outcomes | Criteria for success not defined in abstract |
| Notes | Only Chinese version of article available. Chinese translator asked by CEV Information Specialist to contact study authors on June 4th 2015 for additional information about study (methods of randomisation etc). No response from study authors. |
| Methods | Participants randomly divided into 2 treatment groups. Translation of methods section in full‐text Chinese article is as follows 'The sample is a collection of cases of people with chronic dacryocystitis from November 2010 to January 2011 within the author’s hospital ‐ Songjiang District Central Hospital. There are 2 males and 35 females, aged from 25 to 63 years of age (average 44.03±7.13)'. Unable to ascertain method of randomisation from this description. |
| Participants | 37 cases (37 eyes) with chronic dacryocystitis |
| Interventions | External dacryocystorhinostomy Endonasal endoscopic dacryocystorhinostomy combined with intubation of lacrimal ducts |
| Outcomes | Criteria of 'success' not defined in abstract |
| Notes | Study authors emailed by Chinese translator on 12 Oct 2015 ‐ no response from study authors to date |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Anatomic success Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.1 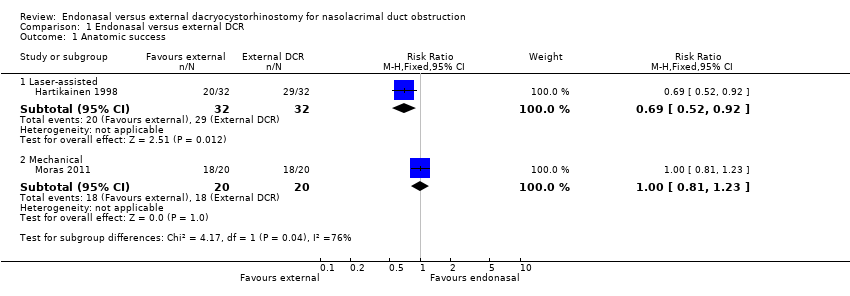 Comparison 1 Endonasal versus external DCR, Outcome 1 Anatomic success. | ||||
| 1.1 Laser‐assisted | 1 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.52, 0.92] |
| 1.2 Mechanical | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.81, 1.23] |
| 2 Subjective success Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.2 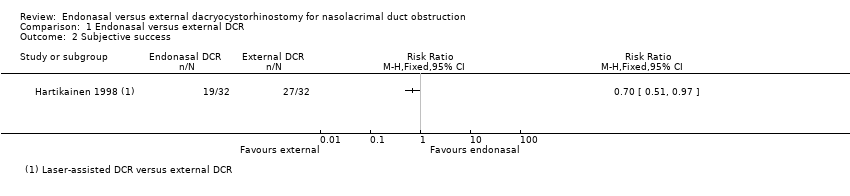 Comparison 1 Endonasal versus external DCR, Outcome 2 Subjective success. | ||||
| 3 Intraoperative bleeding Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.3  Comparison 1 Endonasal versus external DCR, Outcome 3 Intraoperative bleeding. | ||||
| 3.1 Laser‐assisted | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Mechanical | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Postoperative bleeding Show forest plot | 2 | 104 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.04, 3.10] |
| Analysis 1.4  Comparison 1 Endonasal versus external DCR, Outcome 4 Postoperative bleeding. | ||||
| 4.1 Laser‐assisted | 1 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.89] |
| 4.2 Mechanical | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.72] |
| 5 Wound infection/gaping Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.5 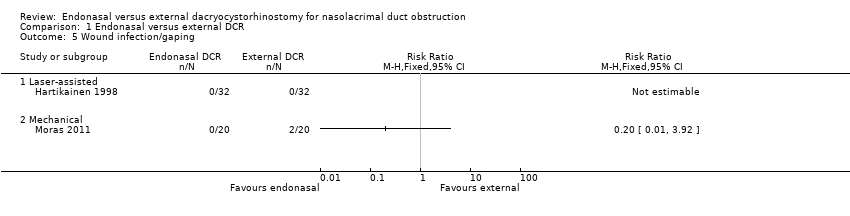 Comparison 1 Endonasal versus external DCR, Outcome 5 Wound infection/gaping. | ||||
| 5.1 Laser‐assisted | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Mechanical | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

Study flow diagram.
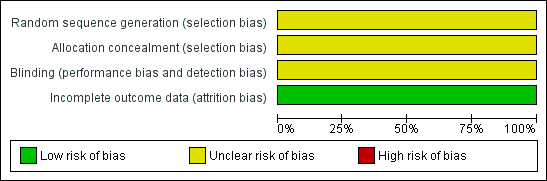
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
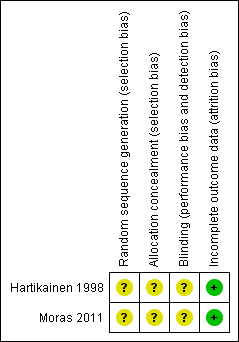
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Endonasal versus external DCR, Outcome 1 Anatomic success.

Comparison 1 Endonasal versus external DCR, Outcome 2 Subjective success.

Comparison 1 Endonasal versus external DCR, Outcome 3 Intraoperative bleeding.
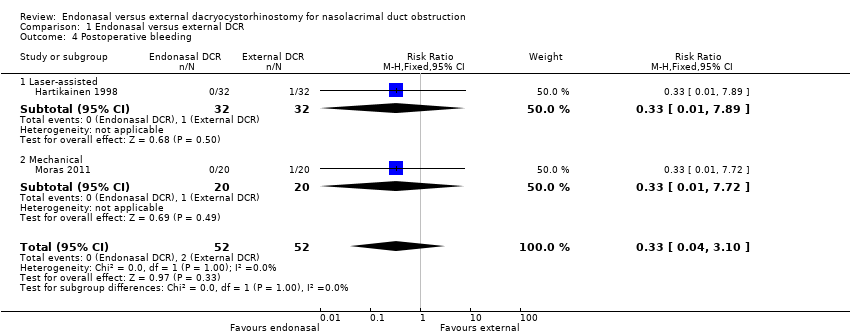
Comparison 1 Endonasal versus external DCR, Outcome 4 Postoperative bleeding.

Comparison 1 Endonasal versus external DCR, Outcome 5 Wound infection/gaping.
| Endonasal dacryocystorhinostomy (DCR) compared with external DCR for nasolacrimal duct obstruction | ||||||
| Patient or population: People with nasolacrimal duct obstruction Settings: Hospital Intervention: Endonasal DCR Comparison: External DCR | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of Participants | Certainty of the evidence | Comments | |
| Assumed risk1 | Corresponding risk | |||||
| External DCR | Endonasal DCR | |||||
| Anatomic success (i.e. patent lacrimal passage after a period of at least six months after operation) | 900 per 1000 | Laser‐assisted endonasal DCR | ⊕⊝⊝⊝ | |||
| 621 per 1000 (468 to 828) | RR 0.69 (0.52 to 0.92) | 64 (1) | ||||
| Mechanical endonasal DCR | ||||||
| 900 per 1000 (729 to 1000) | RR 1.00 (0.81 to 1.23) | 40 | ||||
| Subjective success (i.e. resolution of symptoms of watering following surgery) | 840 per 1000 | Laser‐assisted endonasal DCR5 | ⊕⊕⊝⊝ | |||
| 588 per 1000 (428 to 815) | RR 0.70 (0.51 to 0.97) | 64 (1) | ||||
| Intraoperative bleeding | 170 per 1000 | Laser‐assisted endonasal DCR | ⊕⊝⊝⊝ | No cases of intraoperative bleeding reported in trial of laser‐assisted endonasal DCR | ||
| Not estimable | Not estimable | 64 (1) | ||||
| Mechanical endonasal DCR | ||||||
| 170 per 1000 (85 to 337) | RR 1.00 (0.50 to 1.98) | 40 (1) | ||||
| Postoperative bleeding | 40 per 1000 | 13 per 1000 (2 to 124) | RR 0.33 (0.04 to 3.10) | 104 (2) | ⊕⊝⊝⊝ | |
| Wound infection/gaping | 40 per 1000 | Laser‐assisted endonasal DCR | ⊕⊝⊝⊝ | No cases of wound infection/gaping reported in trial of laser‐assisted endonasal DCR | ||
| Not estimable | Not estimable | 64 (1) | ||||
| Mechanical endonasal DCR | ||||||
| 8 per 1000 (0 to 157) | RR 0.20 (0.01 to 3.92) | 40 (1) | ||||
| CI: confidence interval; DCR: dacryocystorhinostomy; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1The assumed control risk was estimated from the control group in the included studies. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Anatomic success Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Laser‐assisted | 1 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.52, 0.92] |
| 1.2 Mechanical | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.81, 1.23] |
| 2 Subjective success Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Intraoperative bleeding Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Laser‐assisted | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Mechanical | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Postoperative bleeding Show forest plot | 2 | 104 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.04, 3.10] |
| 4.1 Laser‐assisted | 1 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.89] |
| 4.2 Mechanical | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.72] |
| 5 Wound infection/gaping Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 Laser‐assisted | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Mechanical | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

