Irradiación parcial de la mama versus radioterapia en toda la mama para el cáncer de mama temprano
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en espera de evaluación
Referencias de los estudios en curso
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Study characteristics | ||
| Methods | Phase III RCT Single‐centred, tertiary institution Accrual dates: November 2000 to December 2007 Country: Italy Median follow‐up: 68 months | |
| Participants | Inclusion criteria: women aged 48–75 years with early breast cancer, maximum tumour diameter 2.5 cm, "suitable for breast conservation." All women with positive sentinel node biopsy had axillary dissection Sample size: 1305 Age: mean not reported Gender: 100% women | |
| Interventions | Experimental arm: intraoperative electron therapy to deliver 21 Gy at the 90% isodose delivered at the time of surgery after tumour excision using 6–9 MeV Control arm: postoperative EBRT (50 Gy/25 fractions + 10 Gy/5 fraction boost using electrons) | |
| Outcomes | LR‐FS (which included both LR and new ipsilateral breast primaries): Assessed by: clinicians. Quote: "Patients were followed up with a clinical examination every 3 months, an ultrasound mammary scan every 6 months, and a mammogram every year; examinations of the lung, liver, and bone were modulated according to a personalised assessment of risk" Time points assessed: median follow‐up 68 months Time points reported: 68 months Cosmesis: not assessed OS: defined as "time from diagnosis to last follow‐up or time of death" Assessed by: clinicians Time points assessed: median follow‐up 68 months Time points reported: 68 months Toxicity Assessed by: clinicians, late toxicity assessed using LENT‐SOMA Time points assessed: unclear, likely to have been > 6 months Time points reported: unclear C‐SS Assessed by: clinicians Time points assessed: 68 months Time points reported: 68 months DM‐FS: defined as "any recurrence to distant organs" Assessed by: clinicians. Quote: "Patients were followed up with a clinical examination every 3 months, an ultrasound mammary scan every 6 months, and a mammogram every year; examinations of the lung, liver, and bone were modulated according to a personalised assessment of risk" Time points assessed: median follow‐up 68 months Time points reported: median follow‐up 68 months R‐FS: defined as "any recurrence in the ipsilateral axillary, supra‐clavicular or internal mammary nodes" Assessed by: clinicians. Quote: "Patients were followed up with a clinical examination every 3 months, an ultrasound mammary scan every 6 months, and a mammogram every year; examinations of the lung, liver, and bone were modulated according to a personalised assessment of risk" Time points assessed: median follow‐up 68 months Time points reported: not reported L‐RR‐FS Assessed by: clinicians. Quote: "Patients were followed up with a clinical examination every 3 months, an ultrasound mammary scan every 6 months, and a mammogram every year; examinations of the lung, liver, and bone were modulated according to a personalised assessment of risk" Time points assessed: not reported Time points reported: not reported Mastectomy rate: not assessed Compliance Assessed by: number of women receiving allocated RT reported in each study arm Time points assessed: 68 months Time points reported: 68 months Costs: not assessed Quality of life: assessed but not reported. Quote: "Data … were poorly collected, so deemed inadequate for analysis" Consumer preference: not assessed | |
| Notes | Target volume: 4–12 MeV to 90% isodose 10–30 mm around sutured surgical breach Note: women with ≥ 4 involved nodes were treated with RNI (50 Gy/25 fractions). Adjuvant therapies were administered according to the European Institute of Oncology policy at the time Funding sources: Italian Association for Cancer Research, Jacqueline Seroussi Memorial Foundation for Cancer Research, Umberto Veronisi Foundation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "At the data centre, allocation was done by telephone with a computer‐generated list using a randomly permuted block design, stratified by tumour size (<1.0 cm vs 1.0‐1.4 cm vs ≥1.5 cm)," page 1270, paragraph 3. This method represented an adequate randomisation method; low risk of bias. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Immediately before the intervention, the surgeon contacted the data centre by telephone to receive the allocation group. At the data centre, allocation was done by telephone," page 1270, paragraph 3. Details of how this was done were not reported; unclear risk of bias. |
| Blinding of participants and personnel (performance bias): objective outcomes | Low risk | Quote: "Study coordinators, clinicians who verified eligibility criteria after pathological assessment of the surgical specimen, clinicians who followed up patients, investigators who did the statistical analyses, and the patients themselves were aware of the assignment," page 1270, paragraph 3. Low risk of bias LR‐FS: low risk of bias. OS: low risk of bias. New primary: low risk of bias. Subsequent mastectomy: not assessed. Compliance: low risk of bias. Costs: not assessed. |
| Blinding of participants and personnel (performance bias): subjective outcomes | High risk | Quote: "Study coordinators … clinicians who followed up patients … and the patients themselves were aware of the assignment," page 1270, paragraph 3. We judged this domain at high risk of bias. Cosmesis: not assessed. Toxicity: high risk of bias. C‐SS: high risk of bias. DM‐FS: high risk of bias. L‐RR‐FS: high risk of bias. Quality of life: high risk of bias (assessed, but not reported in view of poor data quality). |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "We defined local recurrence as the reappearance of the carcinoma at the site of the surgical intervention. We defined second ipsilateral breast tumours as any new carcinoma appearing in other quadrants of the same breast. IBTR was defined as the sum of local recurrence plus second ipsilateral tumours. A regional nodal failure included any recurrence in the ipsilateral axillary, supraclavicular, or internal mammary nodal regions. Distant metastases were defined as any recurrence to distant organs. Overall survival was defined as the time from diagnosis to last follow‐up or time of death." Quote: "Patients were followed up with a clinical examination every 3 months, an ultrasound mammary scan every 6 months, and a mammogram every year; examinations of the lung, liver, and bone were modulated according to a personalised assessment of risk." Quote: "investigators who did the statistical analyses," page 1270, paragraph 3. Although the outcome assessors for objective outcomes were not blinded, the clear prespecified definitions of what constituted outcomes and the prespecified follow‐up protocol reduced the risk of bias for this domain. LR‐FS: low risk of bias. OS: low risk of bias. New primary: low risk of bias. Subsequent mastectomy: not assessed. Compliance: low risk of bias. Costs: not assessed. |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "Study coordinators, clinicians who verified eligibility criteria after pathological assessment of the surgical specimen, clinicians who followed up patients, investigators who did the statistical analyses, and the patients themselves were aware of the assignment," page 1270, paragraph 3. Quote: "Side‐effects were scored using the Late Effect of Normal Tissue‐ Subjective Objective Management Analytic criteria." Assessment of subjective outcomes was not blinded; high risk of bias. Cosmesis: not assessed. Toxicity: high risk of bias. C‐SS: high risk of bias. DM‐FS: high risk of bias. L‐RR‐FS: high risk of bias. Quality of life: high risk of bias (assessed, but not reported in view of poor data quality). |
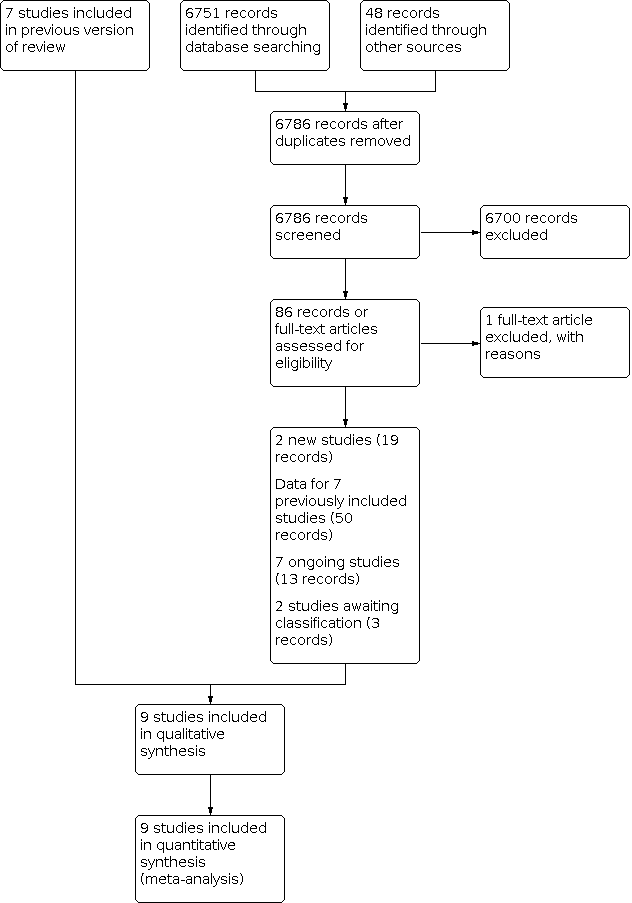
| Incomplete outcome data (attrition bias) | Low risk | No exclusions were reported and there was no postrandomisation attrition (see Figure 1); low risk of bias. LR‐FS: 651 reported/651 randomised PBI arm and 654 reported/654 randomised WBRT arm. Cosmesis: not assessed; low risk of bias. OS: 651/651 PBI arm and 654/654 WBRT arm; low risk of bias. Toxicity: evaluated in 464/651 PBI arm and 412/654 WBRT arm; low risk of bias. C‐SS: 651/651 PBI arm and 654/654 WBRT arm; low risk of bias. DM‐FS: 651/651 PBI arm and 654/654 WBRT arm; low risk of bias. R‐FS: not reported. L‐RR‐FS: 651/651 PBI arm and 654/654 WBRT arm; low risk of bias. Mastectomy rate: not assessed. Compliance: low risk of bias. Costs: not assessed. Quality of life: assessed, but not reported. Consumer preference: not assessed. |
| Selective reporting (reporting bias) | Unclear risk | Outcomes specified in paper:
Outcomes reported:
No access to study protocol; unclear risk of bias. |
| Other bias | Low risk | No other sources of bias identified. |
| Study characteristics | ||
| Methods | Phase III non‐inferiority RCT Open‐label trial Accrual dates: April 2000–July 2009 Countries: Germany, Austria, Czech Republic, Hungary, Poland, Spain and Switzerland Median follow‐up: 79.2 months | |
| Participants | Inclusion criteria: women aged > 40 years with Stage 0, I or II breast cancer (including DCIS), sentinel node biopsy optional; clear margin (≥ 2 mm in invasive disease, 5 mm in DCIS), unifocal or unicentric disease only ECOG performance status 0–2 Exclusion criteria: lymph or vascular invasion, lesions < 3 cm in diameter, pN0/pNmi, DCIS alone, multifocal tumours, extensive intraductal component, Paget's disease, synchronous or previous breast cancer, other malignant disease, pregnancy or lactation | |
| Interventions | Experimental arm (655 participants): APBI using interstitial brachytherapy HDR 32 Gy/8 fractions or 30.3 Gy/7 fractions PDR 50 Gy at 0.6‐0.8 Gy/fractions given hourly Control arm (673 participants): external beam WBRT 50.0–50.4 Gy/1.8–2.0 Gy fractions (5–28) plus 10 Gy/5 fraction boost | |
| Outcomes | LR‐FS Assessed by: defined as "tumour recurrence in the treated breast" evaluated via mammography 6 monthly to 24 months, then annually to 10 years Time point measured: 3 monthly for 2 years, 6 monthly for years 3–5, then annually Time points reported: 5 years Cosmesis Assessed by: 4‐point scale (Harris 1979), participant‐reported outcomes and physician assessed Time point measured, 3 monthly for 2 years, 6 monthly for years 3–5, then annually Time points reported: median 79 months OS Assessed by: from date of surgery, by investigators Time point measured: 3 monthly for 2 years, 6 monthly for years 3–5, then annually Time points reported: median follow‐up 76.2 months Toxicity Assessed by: patient and physician reported, breast pain and arm lymphoedema measured by CTCAE version 3.0, EORTC/RTOG Late Radiation Morbidity Scoring Scheme, fat necrosis measured using Lövey scoring system assessed by physicians (Lövey 2007). Time point measured, 3 monthly for 2 years, 6 monthly for years 3–5, then annually Time points reported:
New ipsilateral breast primary Assessed by: from date of surgery, by investigators Time point measured: 3 monthly for 2 years, 6 monthly years 3–5, then annually Time points reported: median follow‐up 76.2 months C‐SS Assessed by: investigators Time point measured: 3 monthly for 2 years, 6 monthly for years 3–5, then annually Time points reported: median follow‐up 76.2 months DM‐FS Assessed by: from date of surgery, by investigators Time point measured: 3 monthly for 2 years, 6 monthly for years 3–5, then annually Time points reported: median follow‐up 76.2 months R‐FS Assessed by: from date of surgery, by investigators Time point measured: 3 monthly for 2 years, 6 monthly for years 3–5, then annually Time points reported: median follow‐up 76.2 months L‐RR‐FS (which included both LR and new ipsilateral breast primaries): Assessed by: investigators Time point measured: 3 monthly for 2 years, 6 monthly for years 3–5, then annually Time points reported: median follow‐up 76.2 months Mastectomy rate Assessed by: investigators Time point measured: 3 monthly for 2 years, 6 monthly for years 3–5, then annually Time points reported: median follow‐up 76.2 months Compliance Assessed by: number receiving allocated RT reported in each study arm Time points assessed: median 76.2 months Time points reported: median 76.2 months Costs: not assessed Quality of life Assessed by: patient‐reported outcomes using EORTC QLQ‐C30 and QLQ‐BR23 Time points assessed: before RT, immediately after RT at 3, 6, 9, 12, 24, 36, 48, 60, 72, 96 and 120 months Time points reported: before RT, immediately after RT at 3 and 60 months Consumer preference: not assessed | |
| Notes | Target volume: tumour bed plus 20‐ to 30‐mm radial margin Funding source: German Cancer Aid | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomisation was stratified by study centre, menopausal status, and tumour type (e.g., invasive carcinoma vs DCIS), with a block size of ten, according to an automated dynamic algorithm," page 3, randomisation and masking, paragraph 1. Low risk of bias. |
| Allocation concealment (selection bias) | Low risk | Quote: "Patients were randomised centrally at the Department of Medical Informatics, Biometry and Epidemiology, University Erlangen‐Nuremberg, Germany, via an online interface," page 3, randomisation and masking, paragraph 1. Process described as concealed and remote; low risk of bias. |
| Blinding of participants and personnel (performance bias): objective outcomes | Low risk | Quote: "Neither patients nor investigators were masked to treatment allocation," page 3, randomisation and masking, paragraph 1. Although participants and personnel were not blinded, it is unlikely to have introduced bias; low risk of bias. LR‐FS: low risk of bias. OS: low risk of bias. New primary: low risk of bias. Subsequent mastectomy: low risk of bias. Compliance: low risk of bias. Costs: low risk of bias. |
| Blinding of participants and personnel (performance bias): subjective outcomes | High risk | Quote: "Neither patients nor investigators were masked to treatment allocation," page 3, randomisation and masking, paragraph 1. High risk of bias for evaluation of toxicity, and cosmesis. Cosmesis: high risk of bias. Toxicity: high risk of bias. C‐SS: high risk of bias. DM‐FS: high risk of bias. L‐RR‐FS: high risk of bias. Quality of life: high risk of bias. |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Follow up mammography was scheduled at 6, 12, 18 and 24 months after radiation therapy," page 3, paragraph 8. Although outcome assessors were not blinded, we considered the prespecified follow‐up protocol meant this domain was at low risk of bias. LR‐FS: low risk of bias. OS: low risk of bias. New primary: low risk of bias. Subsequent mastectomy: low risk of bias. Compliance: low risk of bias. Costs: low risk of bias. |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "Clinical examination included documentation of late side‐effects with Common Terminology Criteria for Adverse Events and with the Radiation Therapy Oncology Group (RTOG)/European Organisation for Research and Treatment of Cancer (EORTC) Late Radiation Morbidity Scoring Schema 14," page 3. Quote: "Patients and investigators were not masked to treatment allocation" (Polgar 2017, page 216); high risk of bias for this reason. Quote: "The clinicians were not masked to group allocation at the time of toxicity and cosmetic outcome assessment" (Polgar 2017, page 261): despite the prespecified follow‐up schema and the use of a Grading system for documenting late effects, we considered this domain at high risk of bias. Cosmesis: high risk of bias. Toxicity: high risk of bias. C‐SS: high risk of bias. DM‐FS: high risk of bias. L‐RR‐FS: high risk of bias. Quality of life: high risk of bias. |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "after randomisation, 98 patients … administrative error," page 4, paragraph 1. Postrandomisation exclusions are detailed by arm, with reasons; low risk of bias. LR‐FS: 633 analysed of 655 randomised APBI/PBI and 551 analysed of 673 randomised; low risk of bias. Cosmesis: 1111/1184 evaluable participants analysed at 12 months, 1037/1184 evaluable participants analysed at three years, 1007/1184 evaluable participants analysed at five years; low risk of bias. OS: 633 analysed of 655 randomised APBI/PBI and 551 analysed of 673 randomised; low risk of bias. Toxicity 1. acute toxicity data: 630/655 APBI/PBI participants randomised and 552/673 WBRT participants randomised; low risk of bias. 2. late effects data for 545/655 APBI/PBI participants and 462/673 WBRT participants was analysed at five years for later RT toxicity; low risk of bias. Second primary: 633 analysed of 655 randomised APBI/PBI and 551 analysed of 673 randomised; low risk of bias. C‐SS: 633 analysed of 655 randomised APBI/PBI and 551 analysed of 673 randomised; low risk of bias. DM‐FS: 633 analysed of 655 randomised APBI/PBI and 551 analysed of 673 randomised; low risk of bias. R‐FS: 633 analysed of 655 randomised APBI/PBI and 551 analysed of 673 randomised; low risk of bias. L‐RR‐FS: 633 analysed of 655 randomised APBI/PBI and 551 analysed of 673 randomised; low risk of bias. Mastectomy rate: 633 analysed of 655 randomised APBI/PBI and 551 analysed of 673 randomised; low risk of bias. Compliance: 633 analysed of 655 randomised APBI/PBI and 551 analysed of 673 randomised; low risk of bias. Costs: not assessed. Quality of life At baseline: 334/663 (analysed) PBI women and 314/551 analysed WBRT women were eligible for assessment. After RT: 276/633 PBI arm and 267/551 WBRT arm. At 3/12: 403/633 PBI arm and 272/551 WBRT arm. At 5 years: 321/633 PBI arm and 232/551 WBRT arm; low risk of bias. |
| Selective reporting (reporting bias) | Low risk | Quote: "Detailed analyses of early and late side‐effects, quality of life, and cosmetic results are not presented here," page 4, paragraph 1. Although detailed reporting of acute and late adverse effects and quality of life were not in this publication, the authors made it clear there will be further publications; low risk of bias. We had access to the study protocol. |
| Other bias | Low risk | No other bias; low risk of bias. |
| Study characteristics | ||
| Methods | Randomised, non‐inferiority, phase III multicentre trial, ratio 1:1:1 Outpatient, multicentre, national, 30 sites Study dates: 2007–2010 Country: UK Median follow‐up: 72.2 months | |
| Participants | Inclusion criteria: women aged > 50 years, with invasive breast cancer pT1‐2pN0, who had BCS with negative margins (≥ 2 mm) who had < 1% annual risk of LR Exclusion criteria: > 3 positive nodes, distant metastases, previous malignancy, had mastectomy, previous RT, neoadjuvant chemotherapy or chemoradiation Amendments to inclusion criteria during study accrual: participants with Grade III tumours or tumours > 2 cm, or both, became eligible; participants with LVI and 1–3 positive nodes became eligible Sample size: 2018 enrolled, 2 did not allow their data to be collected Sex ratio: 100% women | |
| Interventions | Experimental arm (669 women): 40Gy/15 fractions EBRT PBI daily on days 1–5 for 3 weeks Control arm 1 (674 women): WBRT 40 Gy/15 fractions daily on days 1–5 for 3 weeks Control arm 2 (673 women): WBRT 40 Gy/15 fractions daily on days 1–5 for 3 weeks + integrated boost to while breast 36 Gy/15 fractions | |
| Outcomes | LR‐FS: defined as the presence of any ipsilateral any invasive or non‐invasive cancer in breast parenchyma, or overlying skin assessed at each centre Assessed by: investigators and mammography Time points assessed: annually years 1–5, then every 3 years via national screening programme Time points reported: median 72.2 months Cosmesis: assessed by clinicians, patients and photographically, clinician assessment using validated 4‐point scale Assessed by: photos assessed by 3 investigators masked to treatment allocation, but not year of study follow‐up, using a previously described and validated method Time points assessed: photos scored at 2 and 5 years Time points reported: at 2 and 5 years OS Assessed by: investigators Time points assessed: median follow‐up 72 months Time points reported: median follow‐up 72.2 months Toxicity Assessed by: clinicians, patients and photographically Time points assessed: at 5 years Time points reported: at 5 years C‐SS Assessed by: investigators Time points assessed: at median follow‐up 72 months Time points reported: at median follow‐up 72 months DM‐FS: time to distant relapse Assessed by: investigators Time points assessed: at median follow‐up 72 months Time points reported: at median follow‐up 72 months R‐FS: defined as any local, regional or distant relapse; contralateral breast cancer; or death due to breast cancer Assessed by: investigators Time points assessed: at median follow‐up 72 months Time points reported: at median follow‐up 72 months L‐RR‐FS Assessed by: investigators Time points assessed: at median follow‐up 72 months Time points reported: at median follow‐up 72 months Mastectomy rate: not reported Compliance Assessed by: number receiving allocated RT reported in each study arm Time points assessed: median 72 months Time points reported: median 72 months Costs: not reported in this publication Quality of life Assessed using QLQ‐C30 (Aaronson 1998) and BR23 (Sprangers 1996), HADS, EuroQol EQ‐5D‐3L participants‐reported outcomes. Time points assessed: at baseline, 6 months, 1, 2 and 5 years Time points reported: reported at 2 and 5 years Consumer preference: not reported | |
| Notes | NCT00814567 CSDR0000629765, ICR‐IMPORT‐LOW, ICR‐CTSU/2006/10001, ISCTN12852634, EU‐20896 Funding sources: Institute of Cancer Research Conflicts of interests: authors declared they had no conflicts of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "computer‐generated random permuted blocks … were used to assign patients to groups," Coles 2018, page 1. Low risk of bias. |
| Allocation concealment (selection bias) | Low risk | Quote: "To randomly assign a patient, research staff at the centers telephoned ICR‐CTSU to obtain the treatment allocation and trial ID number," Coles 2018, page 3. Low risk of bias. |
| Blinding of participants and personnel (performance bias): objective outcomes | Low risk | Quote: "Treatment allocation was not masked from patients, clinicians or those analysing data," Coles 2018 page 3. Low risk of bias. LR‐FS: low risk of bias. OS: low risk of bias. New primary: not reported. Subsequent mastectomy: not reported. Compliance: low risk of bias. Costs: not reported. |
| Blinding of participants and personnel (performance bias): subjective outcomes | High risk | Quote: "Treatment allocation was not masked from patients, clinicians or those analysing data," Coles 2018 page 3. Lack of blinding; high risk of bias. Quote: "by three observers (CC, AK, and JRY) using a previously described and validated consensus method. These observers were masked to treatment allocation but not to year of follow‐up," Coles 2018, page 1052. Cosmesis: low risk of bias. Toxicity: high risk of bias. C‐SS: high risk of bias. DM‐FS: high risk of bias. L‐RR‐FS: not reported in a usable form. Quality of life: not reported in this publication. |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Treatment allocation was not masked from patients, clinicians or those analysing data," Coles 2018 page 3. Quote: "These observers were masked to treatment allocation …" Coles 2018, page 5. Low risk of bias. Quote: "The mammography schedule was followed according to local practice and was typically done annually for the first five years, then every three years as part of the national screening programme," Coles 2018, page 3. LR‐FS: low risk of bias. OS: low risk of bias. New primary: not reported. Mastectomy rate: not reported. Compliance: low risk of bias. Costs: not reported in this publication. Consumer preference: not reported. |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "Treatment allocation was not masked from patients, clinicians or those analysing data," Coles 2018 page 3. Lack of blinding; high risk of bias. Cosmesis: photographs assessed by observers masked to treatment arm; low risk of bias. Toxicity: clinicians were not masked to study arm; high risk of bias. C‐SS: clinicians were not masked to study arm; high risk of bias. DM‐FS: participants and clinicians were not masked to study arm; high risk of bias as knowledge of study arm could have influenced timing of investigations. L‐RR‐FS: not reported in a usable form. Quality of life: participants and clinicians were not masked to study arm; high risk of bias. |
| Incomplete outcome data (attrition bias) | Low risk | LR‐FS: 699/699 PBI analysed, 674/674 WBRT analysed: low risk of bias. Cosmesis: clinician‐assessed breast appearance 421/699 PBI analysed, 411/674 WBRT analysed (but late effects were assessed in a subgroup of participants) (see Table 11): low risk of bias. OS: assessed in 674/675 PBI analysed, 699/699 WBRT analysed: low risk of bias. Toxicity: assessed in 674/675 PBI analysed and 699/699 WBRT analysed: low risk of bias C‐SS: assessed in 674/675 PBI analysed and 699/699 WBRT analysed: low risk of bias DM‐FS: assessed in 674/675 PBI analysed and 699/699 WBRT analysed: low risk of bias R‐FS: not reported in usable form L‐RR‐FS: not reported in usable form Mastectomy rate: not reported Compliance: assessed in 674/675 PBI analysed and 699/699 WBRT analysed: low risk of bias Costs: not reported in this publication Consumer preference: not reported |
| Selective reporting (reporting bias) | Unclear risk | Costs not reported in this publication. |
| Other bias | Low risk | No other sources of bias identified. |
| Study characteristics | ||
| Methods | RCT Single cancer centre Accrual dates: March 2005 to June 2013 Country: Italy Median follow‐up: 10.7 years | |
| Participants | Inclusion criteria: women aged > 40 years, wide local excision or quadrantectomy for invasive breast cancer, negative margins, tumour size ≤ 25 mm Sample size: 520 women | |
| Interventions | Experimental arm: PBI/APBI (using IMRT) Control arm: WBRT (conventional RT) | |
| Outcomes | LR‐FS: defined as breast cancer in same quadrant Assessed by: clinical examination and annual mammography Time points assessed: reviewed monthly for 3 months, 4 monthly for 2 years, then 6 monthly Time points reported: median 5 and 10.7 years Cosmesis Assessed using Harvard Cosmetic Score Time points assessed: reviewed monthly for 3 months, 4 monthly for 2 years, then 6 monthly Time points reported: median 5 and 10.7 years OS Assessed by: death any cause Time points assessed: reviewed monthly for 3 months, 4 monthly for 2 years, then 6 monthly Time points reported: median 5 and 10.7 years Toxicity 1. acute toxicity using RTOG/EORTC toxicity scoring criteria 2. late toxicity assessed using RTOG/EORTC toxicity scoring criteria and LENT‐SOMA Time points assessed: reviewed monthly for 3 months, 4 monthly for 2 years, then 6 monthly Time points reported: median 5 and 10.7 years New ipsilateral breast primary assessed: any new breast cancer ipsilateral breast in different quadrant of ipsilateral breast Time points assessed: reviewed monthly for 3 months, 4 monthly for 2 years, then 6 monthly Time points reported: median 5 and 10.7 years C‐SS Assessed by: not stated Time points assessed: reviewed monthly for 3 months, 4 monthly for 2 years, then 6 monthly Time points reported: median 5 and 10.7 years DM‐FS Assessed by: any recurrence to distant organs Time points assessed: reviewed monthly for 3 months, 4 monthly for 2 years, then 6 monthly Time points reported: median 5 and 10.7 years R‐FS: not assessed L‐RR‐FS Assessed: any recurrence in the ipsilateral axillary, supraclavicular or internal mammary chain nodal regions Time points assessed: reviewed monthly for 3 months, 4 monthly for 2 years, then 6 monthly Time points reported: median 5 and 10.7 years Mastectomy rate: not assessed Compliance: number receiving allocated RT reported in each study arm Assessed by: not stated Time points assessed: reviewed monthly for 3 months, 4 monthly for 2 years, then 6 monthly Time points reported: median 5 years Costs: not assessed Quality of life Assessed using QLQ‐C30 (Aaronson 1998) and QLQ‐BR23 (Sprangers 1996)(PROs) Time points assessed: at baseline after RT completion and 2 years Time points reported: at baseline after RT completion and 2 years Consumer preference: not assessed | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomly assigned to receive either WBI or APBI using IMRT in a 1:1 ratio. Allocation was performed with a computer‐generated sequence using a randomly permuted block design, without any stratification of main prognostic factors," page 453, paragraph 1. Low risk of bias. |
| Allocation concealment (selection bias) | Low risk | Quote: "The random sequence was kept by an external centre (local Oncological Centre for Departmental Reference, CORD). The clinicians were required to query it every time an eligible patient had provided written informed consent to determine the allocation arm," page 453, paragraph 1. Low risk of bias. |
| Blinding of participants and personnel (performance bias): objective outcomes | Low risk | Quote: "Clinicians, investigators and the patients themselves were aware of the arm assignment," page 453, paragraph 1. Blinding would have been difficult in view of the 2 very obviously different treatments; low risk of bias. LR‐FS: low risk of bias. OS: low risk of bias. New primary: low risk of bias. Subsequent mastectomy: low risk of bias. Compliance: low risk of bias. Costs: not assessed. |
| Blinding of participants and personnel (performance bias): subjective outcomes | High risk | Quote: "Clinicians, investigators and the patients themselves were aware of the arm assignment," page 453, paragraph 1. Blinding would have been difficult in view of the 2 very obviously different treatments; high risk of bias. Cosmesis: high risk of bias. Toxicity: high risk of bias. C‐SS: high risk of bias. DM‐FS: high risk of bias. L‐RR‐FS: high risk of bias. Quality of life: high risk of bias. |
| Blinding of outcome assessment (detection bias) | Low risk | Clinicians and investigators were not blinded to treatment arm, but the prespecified mammographic follow‐up would have reduced the risk of bias related to the primary outcome. LR‐FS: low risk of bias. OS: low risk of bias. New primary: low risk of bias. Subsequent mastectomy: not assessed Compliance: low risk of bias. Costs: not assessed. |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "mammography was annually programmed," page 454, paragraph 13. Clinicians and investigators were not blinded to treatment arm, which makes assessment of subjective outcomes at high risk of bias. Cosmesis: high risk of bias. C‐SS: high risk of bias. DM‐FS: high risk of bias. L‐RR‐FS: high risk of bias. Quality of life: high risk of bias. |
| Incomplete outcome data (attrition bias) | Low risk | No exclusions or attrition reported; low risk of bias. LR‐FS: 260/260 PBI arm and 260/260 in WBRT arm analysed: low risk of bias. Cosmesis: 246/260 in PBI arm and 260 WBRT arm analysed: low risk of bias. OS: 260/260 PBI arm and 260/260 in WBRT arm analysed: low risk of bias. Toxicity 1. acute 246/260 in PBI arm and 260 WBRT arm assessed: low risk of bias. 2. late 246/260 in PBI arm and 260 WBRT arm assessed: low risk of bias. New ipsilateral breast primary: 260/260 PBI arm and 260/260 in WBRT arm analysed: low risk of bias. C‐SS: 260/260 PBI arm and 260/260 in WBRT arm analysed: low risk of bias. DM‐FS: 260/260 PBI arm and 260/260 in WBRT arm analysed: low risk of bias. Quality of life: 105/260 APBI/PBI participants and 100/260 WBRT participants fully completed all the questionnaires: low risk of bias. |
| Selective reporting (reporting bias) | Unclear risk | We did not review the protocol; unclear risk of bias. |
| Other bias | Low risk | No other sources of bias. |
| Study characteristics | ||
| Methods | Phase III RCT Multicentred (154 centres) Accrual dates: March 2005 to April 2013 Country: the UK, Canada, Ireland and Israel Median follow‐up: 10.2 years | |
| Participants | Inclusion criteria: women aged > 18 years with histologically confirmed DCIS or invasive adenocarcinoma of the breast (T0‐2N0‐1M0), negative histological margins, must have had BCS Exclusion criteria: tumour > 3 cm, > 3 involved nodes Sample size: 4216 participants enrolled Sex ratio: 100% women Median age: 54 years (range 47–64 years) | |
| Interventions | Experimental arm (2107 women): PBI 34 Gy in 10 fractions brachytherapy or 38.5 Gy/10 fractions over 5 days (note: 518/ 2109 had DCIS) Control arm (2109 women): WBRT (50 Gy in 25 fractions at 1.8–2 Gy per fraction, optional boost to 60–66 Gy) (513/2109 had DCIS) Brachytherapy: 34 Gy/10 fractions MammoSite: 34 Gy/10 fractions 3D‐CRT: 38.5 Gy/10 fractions | |
| Outcomes | LR‐FS: in‐breast tumour recurrence (IBTR) included both DCIS and invasive recurrence in the ipsilateral breast (we counted only invasive recurrences) Assessed by: annual mammograms Time points assessed: physical examination or telephone follow‐up every 6 months years 1–5, then every 12 months or at the occurrence of a protocol event. Median follow‐up 10.2 years Time points reported: 10.2 years Cosmesis Assessed by: radiation oncologist or surgeon, attempts made to ensure assessment completed by single person, photos. Participant reported using Breast Cancer Treatment Outcome Scale (Stanton 2001). Digital images assessed by a panel of physicians Time points assessed: at baseline, 4 weeks after RT completed; 6, 12, 24 and 36 months, photos taken at 12 and 36 months (primary endpoint is cosmetic outcome at 3 years). Time points reported: not reported OS: deaths due to all causes Assessed by: not stated, assume by treating clinican Time points assessed: physical examination or telephone follow‐up every 6 months years 1–5, then every 12 months or at the occurrence of a protocol event. Median follow‐up 10.2 years Time points reported: 10.2 years Toxicity Assessed by: physician using CTCAE Version 4.0 Time points assessed: acute toxicity assessed at 1 month post‐RT, late toxicity assessed at 6 and 12 months after RT completed, then annually New ipsilateral primary 'elsewhere primary' Defined as: tumour recurrence in the remainder of the ipsilateral breast, biopsy confirmation required Assessed: biopsy confirmation required Time points assessed: physical examination or telephone follow‐up every 6 months years 1–5, then every 12 months or at the occurrence of a protocol event Time points reported: median follow‐up 10.2 years C‐SS Autopsy reports should be secured where possible, and copy of death certificate with cause of death Assessed by: not stated Time points assessed: physical examination or telephone follow‐up every 6 months years 1–5, then every 12 months or at the occurrence of a protocol event. Median follow‐up 10.2 years. Time points reported: not reported DM‐FS: defined as the time from randomisation to first diagnosis of distant disease Assessed by: not stated, assume by treating clinican Time points assessed: physical examination or telephone follow‐up every 6 months years 1–5, then every 12 months or at the occurrence of a protocol event. Median follow‐up 10.2 years Time points reported: 10.2 years R‐FS: defined as the time from randomisation to first diagnosis of local, regional or distant recurrence, second primary or death Assessed by: not stated, assume by treating clinican Time points assessed: physical examination or telephone follow‐up every 6 months years 1–5, then every 12 months or at the occurrence of a protocol event. Median follow‐up 10.2 years Time points reported: 10.2 years L‐RR‐FS Defined as: tumour in ipsilateral internal mammary, axillary nodes or ipsilateral axilla, biopsy confirmation required Assessed by: not stated, assume by treating clinican Time points assessed: physical examination or telephone follow‐up every 6 months years 1–5, then every 12 months or at the occurrence of a protocol event. Median follow‐up 10.2 years. Time points reported: not reported Mastectomy rate Assessed by: not assessed Time points assessed: not assessed Time points reported: not assessed Compliance Assessed by: percentage of participants who received RT according to protocol Time points assessed: physical examination or telephone follow‐up every 6 months years 1–5, then every 12 months or at the occurrence of a protocol event Time points reported: median follow‐up 10.2 years Costs Assessed by: not assessed Time points assessed: not assessed Time points reported: not assessed Quality of life Assessed by: SF‐36 vitality scale (Saris‐Baglama 2010) Time points assessed: 4 weeks after RT completed, 6, 12, 24 and 36 months Time points reported: not reported Consumer preference: not assessed | |
| Notes | NCT00103181 NSABP B‐39/RTOG 0413, SWOG‐NSABP‐B‐39 Collaborators: Southwest Oncology Group, NCI, RTOG, National Surgical Adjuvant Breast and Bowel Project For brachytherapy and 3D‐CRT: cavity plus 15 mm = CTV + 10 mm = PTV MammoSite: PTV = 10 mm expansion on balloon minus balloon volume | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomly assigned." Abstract. |
| Allocation concealment (selection bias) | Low risk | Quote: "randomly assigned using a biased‐coin‐based minimisation algorithm," abstract, 2019, page 2155. Quote: "Randomisation was done centrally by the statistical and data management centre …" "Online patient data entry was done via the NSABP server, which provided treatment assignment to the investigator for enrolment," 2019, page 2157, paragraph 2. |
| Blinding of participants and personnel (performance bias): objective outcomes | Low risk | Quote: "Patients, investigators, and statisticians could not be masked to treatment allocation," abstract, 2019, page 2155. LR‐FS: low risk of bias. OS: low risk of bias. Ipsilateral second primary: low risk of bias. Mastectomy rate: low risk of bias. Compliance: low risk of bias. Costs: not assessed. |
| Blinding of participants and personnel (performance bias): subjective outcomes | High risk | Quote: "Patients, investigators, and statisticians could not be masked to treatment allocation," abstract, 2019, page 2155. Cosmesis: low risk of bias. Toxicity: high risk of bias. C‐SS: low risk of bias. DM‐FS: high risk of bias. R‐FS: high risk of bias. L‐RR‐FS: high risk of bias. Quality of life: high risk of bias. Consumer preference: not assessed. |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Patients, investigators, and statisticians could not be masked to treatment allocation," abstract, 2019, page 2155. LR‐FS: evaluated using annual mammography and histological confirmation required; low risk of bias. OS: low risk of bias. Ipsilateral second primary: histological confirmation required, low risk of bias. Mastectomy rate: not assessed. Compliance: low risk of bias. Costs: not assessed. |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "Patients, investigators, and statisticians could not be masked to treatment allocation," abstract, 2019, page 2155. Cosmesis: quote: "Radiation Oncologist or Surgeon, attempts made to ensure assessment completed by single person, photos. Patient reported using Breast Cancer Treatment Outcome Scale (BCTOS) (Stanton 2001) … Digital images assessed by a panel of physicians" because outcome assessors were not masked to treatment arm; high risk of bias. Toxicity: high risk of bias. C‐SS: because of the requirement for "Autopsy reports should be secured where possible, and copy of death certificate with cause of death;" low risk of bias. DM‐FS: biopsy or radiological confirmation were required; low risk of bias. R‐FS: biopsy or radiological confirmation were required; low risk of bias. L‐RR‐FS: biopsy or radiological confirmation were required; low risk of bias Quality of life: high risk of bias. Consumer preference: not assessed. |
| Incomplete outcome data (attrition bias) | Low risk | 4216 women enrolled (included both DCSI and invasive disease). 2109 WBRT: 70 women withdrew consent or were LTFU, so 2039/2109 WBRT participants were available for survival analysis. 2107 APBI: 14 women withdrew consent or were LTFU, so 2093/2017 APBI participants were available for survival analysis. LR‐FS: 2089/2107 APBI arm and 2036/2109 WBRT arm were available for analysis; low risk of bias. Cosmesis: assessed in 482 participants who indicated they intended to have chemotherapy and 482 participants who intended not to have chemotherapy, i.e. 964/3216 participants in substudy, not reported, so deemed at unclear risk of bias. OS: 2039/2109 WBRT participants were available for survival analysis, 2093/2107 APBI participants were available for survival analysis; low risk of bias. Toxicity: 2020/2109 WBRT participants were available for survival analysis, 2089/2107 APBI participants were available for survival analysis; low risk of bias. Ipsilateral second primary: 2089/2107 APBI participants and 2036/2109 WBRT participants were available for analysis; low risk of bias. C‐SS: 2089/2107 APBI participants and 2036/2109 WBRT participants were available for analysis; low risk of bias. DM‐FS: 2089/2107 APBI participants and 2036/2109 WBRT participants were available for analysis; low risk of bias. R‐FS: 2089/2107 APBI participants and 2036/2109 WBRT participants were available for analysis; low risk of bias. L‐RR‐FS: 2089/2107 APBI participants and 2036/2109 WBRT participants were available for analysis; low risk of bias. Mastectomy rate: not assessed. Compliance: low risk of bias. Costs: not assessed. Quality of life: 964/3216 participants in substudy not reported; unclear risk of bias. Consumer preference: not assessed. |
| Selective reporting (reporting bias) | Low risk | We had access to the study protocol. Some outcomes prespecified in the protocol (cosmesis and quality of life) were not reported, it is reasonable to expect they will be the subject of future publications; low risk of bias. |
| Other bias | Low risk | No other sources of bias identified. |
| Study characteristics | ||
| Methods | RCT Single‐centre Accrual dates: July 1998 to May 2004 Country: Hungary Median follow‐up: 10.2 years | |
| Participants | 258 women with invasive breast cancer Inclusion criteria: wide excision with negative margins, unifocal tumour, tumour size < 20 mm, clinically or pathologically N0, or single microscopic nodal metastasis (> 0.2 mm and < 2.0 mm), i.e. pT1N0‐1miM0, Grade I or II Exclusion criteria: bilateral breast cancer, prior unilateral or contralateral breast cancer, concomitant or previous other malignancies, invasive lobular cancer, pure ductal or lobular cancer in situ. After 2001, women aged < 40 years excluded Mean age: 58–59 years (given for each arm) | |
| Interventions | Experimental arm: PBI; 88/128 women had 7 × 5.2 Gy HDR multicatheter brachytherapy and 40/128 women unsuitable for HDR had 50 Gy/25 fractions electron beam RT to partial breast Control arm: 50 Gy/25 fractions WBRT (130 women) Surgery: wide excision (resection of tumour with ≥ 1 cm macroscopic free margin). Cavity marked with titanium clips Central pathology review performed Systemic therapy given according to institutional protocol Baseline mammography was performed at 6 months after RT then annually. Women were followed up every 3 months in the first year, then every 6 months | |
| Outcomes | LR‐FS (confirmed histologically): Assessed by: investigators and mammograms Time points assessed: 6 months after RT then annually Time points reported: 5 and 10 years Cosmesis Assessed: treating clinicians and independently bt the main investigator Table 1 Assessed by: Harvard Cosmetic Score, see Table 1 Time points assessed: 6 monthly for 3 years, then annually Time points reported: median 124 months' follow‐up OS Assessed by: death any cause Time points assessed: 6 monthly for 3 years, then annually Time points reported: 5 and 10 years Toxicity Assessed: by clinicians using CTCAE for acute and EORTC/RTOG and LENT‐SOMA for late toxicity Time points assessed: 6 monthly for 3 years, then annually Time points reported: at four years Elsewhere breast primary Assessed by: clinicians and mammograms (defined as ipsilateral breast recurrence ≥ 2 cm away from surgical clips marking tumour bed) Time points assessed: 6 months after RT then annually Time points reported: 5 and 10 years C‐SS Assessed by: deaths due to breast cancer Time points assessed: 6 monthly for 3 years, then annually Time points reported: 5 and 10 years DM‐FS Assessed by: investigators Time points assessed: 6 monthly to 3 years, then annually Time points reported: 5 years and 10 years R‐FS Assessed by: investigators Time points assessed: 6 monthly to 3 years, then annually Time points reported: 5 years and 10 years L‐RR‐FS Assessed by: investigators Time points assessed: 6 monthly to 3 years, then annually Time points reported: 5 years and 10 years Mastectomy rate Assessed by: investigators Time points assessed: 6 monthly for 3 years, then annually Time points reported:10.3 years Compliance: defined as the number of women who commence treatment with PBI/APBI or conventional EBRT and complete the treatment course Assessed by: investigators Time points assessed: at completion of RT Time points reported: at completion of RT Costs: not assessed Quality of life: not assessed Consumer preference: not assessed | |
| Notes | Early stopping of 258 women enrolled because another multicentred trial commenced. LR defined as any detection of cancer in the treated breast, confirmed histologically. An "elsewhere breast failure" defined as ipsilateral (LR) ≥ 2 cm from the clips. All other LR classified as true recurrence or marginal miss. Harvard Cosmetic Score, scored by treating radiation oncologist and chief investigator at analysis date (June–August 2006). In case of discrepancy, worst score used for analysis. Event‐free intervals defined as time between date of surgery and date of event or last follow‐up. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "were randomised," Polgár 2007, page 694, paragraph 3. Quote: "randomly allocated to treatment options by a sealed envelope system in blocks of 10." Randomisation was done by the main investigator (CP). Polgár 2007, page 695, paragraph 2. The trial was likely to have been randomised. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "randomly allocated to treatment options by a sealed envelope system in blocks of 10," Polgár 2007, page 695, paragraph 2. Allocation concealment appeared to have been done, although the description was incomplete, which contributed to the judgement of unclear bias risk. |
| Blinding of participants and personnel (performance bias): objective outcomes | Low risk | Participants: not mentioned, unlikely to have been done. Quote: "Blinding of physicians performing treatments and follow‐up of patients was not possible for technical reasons," Polgár 2007, page 695, paragraph 2. Physicians: not done. Quote: "Blinding of physicians performing treatments and follow‐up of patients was not possible for technical reasons," Polgár 2007, page 695, paragraph 2. We judged this domain at low risk of bias. LR‐FS: low risk of bias. OS: low risk of bias. Elsewhere primary: low risk of bias. Subsequent mastectomy: low risk of bias. Compliance: low risk of bias. Costs: not assessed. |
| Blinding of participants and personnel (performance bias): subjective outcomes | High risk | Participants: not mentioned, unlikely to have been done. Quote: "Blinding of physicians performing treatments and follow‐up of patients was not possible for technical reasons," Polgár 2007, page 695, paragraph 2. Physicians: not done. Quote: "Blinding of physicians performing treatments and follow‐up of patients was not possible for technical reasons," Polgár 2007, page 695, paragraph 2. We judged this domain at high risk of bias. Cosmesis: high risk of bias. Toxicity: high risk of bias. C‐SS: high risk of bias. DM‐FS: high risk of bias. R‐FS: high risk of bias. L‐RR‐FS: high risk of bias. Quality of life: high risk of bias. Consumer preference: not assessed. |
| Blinding of outcome assessment (detection bias) | Low risk | Participants: not mentioned, unlikely to have been done. Quote: "Blinding of physicians performing treatments and follow‐up of patients was not possible for technical reasons," Polgár 2007, page 695, paragraph 2. Physicians: not done, but in view of prespecified follow‐up protocol, with regular mammography, unlikely to have introduced bias. Quote: "Patients were seen every three months in the first two years after RT and every six months thereafter. Baseline mammography was performed six months after completion of RT and yearly thereafter," Polgár 2007, page 697, paragraph 6. Quote: "Blinding of physicians performing treatments and follow‐up of patients was not possible for technical reasons," Polgár 2007, page 695, paragraph 2. Quote: "Local recurrence … proved by histological confirmation in every case," Polgár 2007, page 697, paragraph 6. Assessors: not done. Unlikely to be a source of bias in view of the prespecified schedule for follow‐up visits and investigations. LR required biopsy confirmation, which would reduce the risk of bias in evaluation of this outcome. LR‐FS: low risk of bias. OS: low risk of bias. Elsewhere primary: low risk of bias. Subsequent mastectomy: low risk of bias. Compliance: low risk of bias. Costs: not assessed. |
| Blinding of outcome assessment (detection bias) | High risk | Participants: not mentioned, unlikely to have introduced bias. Physicians: not mentioned, may be a source of bias. Assessors: not mentioned, unlikely to have been done, this is potentially a source of bias. Quote: "Cosmetic outcome scored independently by treating radiation oncologist and the main investigator…in the case of discrepancy, the worse cosmetic score was used for analysis," Polgár 2007, page 697, paragraph 5. Cosmesis: high risk of bias. Toxicity: high risk of bias. C‐SS: high risk of bias. DM‐FS: high risk of bias. R‐FS: high risk of bias. L‐RR‐FS: high risk of bias. Quality of life: high risk of bias. Consumer preference: not assessed. |
| Incomplete outcome data (attrition bias) | Low risk | Exclusions: none. Attrition: 0 in PBI arm, 2 in WBRT arm (declined follow‐up at 18 and 22 months postoperatively) LR‐FS: 128/128 PBI participants and 130/130 WBRT participants analysed. Cosmesis: 125/125 PBI participants and 116/93 WBRT participants analysed. OS: 128/128 PBI participants and 130/130 WBRT participants analysed. Toxicity 1. acute: not reported 2. late: 127/128 PBI participants and 129/130 WBRT participants analysed. C‐SS: 128/128 PBI participants and 130/130 WBRT participants analysed. DM‐FS: 128/128 PBI participants and 130/130 WBRT participants analysed. R‐FS: 128/128 PBI participants and 130/130 WBRT participants analysed. L‐RR‐FS: 128/128 PBI participants and 130/130 WBRT participants analysed. Mastectomy rate: 128/128 PBI participants and 130/130 WBRT participants analysed. Compliance: 128/128 PBI participants and 130/130 WBRT participants analysed. |
| Selective reporting (reporting bias) | Unclear risk | Outcomes in methods section
Outcomes reported in paper
Outcomes in methods and protocol: protocol not reviewed. |
| Other bias | Low risk | Trial stopped early (the trial enrolled 258 women of a planned sample size of 570 participants) because of a competing trial, GEC‐ESTRO, started recruiting. |
| Study characteristics | ||
| Methods | Phase III RCT 33 centres Accrual dates: 2006–2011 Country: Canada, Australia, New Zealand Median follow‐up: 8.6 years (range 7.3–9.9 years) | |
| Participants | Inclusion criteria: aged ≥ 40 years with new diagnosis of DCIS or with microscopically clear margins after BCS of non‐invasive or invasive disease (or no residual disease on re‐excision) Exclusion criteria: tumour size > 3 cm, axillary nodal involvement including micrometastasis (> 0.2 mm or positive cells only identified on IHC as determined by sentinel node biopsy; axillary node dissection; or clinical examination for DCIS only Sample size: 2135 enrolled Median age: 61 years (range 54–68 years) Gender: 1005 women | |
| Interventions | Experimental arm: APBI (1070 participants) (3D‐CRT: 38.5 Gy in 10 fractions, bd over 5‐8 days. 6–8 hour gap between doses required) Control arm: WBRT (1065 participants) (42.5 Gy in 16 fractions daily over 22 days). Women with large breast size: 50 Gy in 25 fractions over 25 days. Boost 10 Gy in 4 or 5 fractions over 4–7 days was permitted for those women deemed at moderate to high risk of LR as per local cancer centre guidelines | |
| Outcomes | LR‐FS: which included both LR and new ipsilateral breast primaries, defined as recurrent invasive or in situ cancer in the ipsilateral breast including the axillary tail. IBTR defined as true or marginal recurrence if recurred within 2 cm of the tumour bed Assessed by: annual mammogram and physical examination and adjudicated by 2 physicians unaware of treatment allocation Time points assessed: 2 weeks; 3, 6 and 12 months, then annually Time points reported: median 8.6 years Cosmesis Assessed: using the EORTC Cosmetic Rating system (a 4‐point scale) Assessed by: trained nurses, participants and physicians Time points assessed: baseline before RT; 2 weeks; 3, 6 and 12 months; then annually. Time points reported: 5 years OS Assessed by: investigators: death any cause and adjudicated by 2 physicians unaware of treatment allocation Time points assessed: 2 weeks; 3, 6 and 12 months; then annually Time points reported: not reported in this publication Toxicity Assessed: by investigators, using NCI version 3.0 Time points assessed: baseline before RT; 2 weeks; 3, 12, 36 and 60 months Time points reported: 36 months C‐SS Assessed by: investigators Time points assessed: 2 weeks; 3, 6 and 12 months; then annually Time points reported: not reported in this publication DM‐FS: not assessed R‐FS: time from random assignment to documented recurrence in ipsilateral breast, regional lymph nodes or distant sites, contralateral breast cancer, second cancer or death and adjudicated by 2 physicians unaware of treatment allocation Assessed by: investigators Time points assessed: 2 weeks; 3, 12, 36 and 60 months Time points reported: not reported in this publication L‐RR‐FS: not assessed Mastectomy rate: Assessed by: investigators Time points assessed: 2 weeks; 3, 12, 36, 60 months and 10.2 years Time points reported: 10.2 years Compliance: number receiving allocated RT reported in each study arm Assessed by: not stated Time points assessed: at median follow‐up 36 months Time points reported: at median follow‐up 36 months Costs: not assessed Quality of life Assessed by: not stated Time points assessed: baseline before RT; 2 weeks; 3, 6 and 12 months, then annually Time points reported: not reported in this publication Consumer preference: not assessed | |
| Notes | QA: extensive QA processes (credentialing, real‐time and post‐hoc plan review) NCT00282035 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "were randomly assigned using a telephone‐based central minimization procedure." This was deemed an adequate method of sequence generation; low risk of bias. |
| Allocation concealment (selection bias) | Low risk | The sequence generation was described as "telephone‐based central minimisation procedure," randomisation appears to have been remote and concealed; low risk of bias. |
| Blinding of participants and personnel (performance bias): objective outcomes | Low risk | Quote: "For technical reasons, blinding of participants and personnel was not possible, this is likely to have introduced bias." LR‐FS: low risk of bias. OS: low risk of bias. New primary: not assessed. Compliance: low risk of bias. Costs: not reported in this publication; low risk of bias. |
| Blinding of participants and personnel (performance bias): subjective outcomes | Low risk | Quote: "For technical reasons, blinding of participants and personnel was not possible, this is likely to have introduced bias." Cosmesis: high risk of bias. Toxicity: high risk of bias. R‐FS: high risk of bias. L‐RR‐FS: not assessed. Quality of life: not reported in this publication, high risk of bias. |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Bilateral mammograms were performed annually." We judged this domain at low risk of bias, because the mammography interval was prespecified and this ensured the primary objective outcome (IBTR) was at low risk of bias and adjudicated by 2 physicians unaware of treatment allocation. LR‐FS: low risk of bias. OS: low risk of bias. Compliance: low risk of bias. |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "… addition to nurse and patient assessments, cosmesis was assessed by two panels of three radiation oncologists using the digital photographs. The physicians had breast cancer expertise and were trained to use the EORTC Cosmetic Rating System. After demonstrating good agreement in the ability to identify adverse cosmesis (0.71; Appendix, online only), each panel reviewed half of the available 3‐year post‐RT photographs. The panels, blinded to treatment allocation, provided one consensus global cosmetic score for each patient (Appendix, online only)," Olivotto 2013, page 4014. It was not stated whether the trained nurses evaluating the cosmetic outcome were blinded to treatment arm; however, the physician reviewers were blinded to treatment arm; low risk of bias. Quote: "All events (recurrence, second cancer and deaths) were adjudicated by two physicians unaware of treatment allocation." Cosmesis: low risk of bias (for physician and nurse determinations, high risk of bias for patient‐reported outcomes). Toxicity: high risk of bias. DM‐FS: high risk of bias. R‐FS: high risk of bias. L‐RR‐FS: not assessed. Quality of life: not reported in this publication, high risk of bias. |
| Incomplete outcome data (attrition bias) | Low risk | 1070 participants were assigned to APBI, 6 withdrew before treatment, 4 did not receive RT, 16 were treated with WBRT, 14 LTFU and 9 withdrew during follow‐up period. 1065 participants were assigned to WBRT: 16 withdrew before treatment, 2 did not receive RT. 20 LTFU and 35 withdrew during follow‐up period. Cosmesis 1. Nurse‐assessed 2055 analysed of 2135 randomised at baseline. 1108 analysed of 2135 randomised at 3 years. 335 analysed of 2135 randomised at 5 years. 2. Participant reported 2055 analysed of 2135 randomised at baseline. 1100 analysed of 2135 randomised at 3 years. 328 analysed of 2135 randomised at 5 years. 3. Physician‐assessed 766 analysed of 2135 randomised at 3 years. Toxicity: acute and late toxicity outcomes reported on 2135/2135 randomised participants; low risk of bias. |
| Selective reporting (reporting bias) | Unclear risk | Because this was an interim report, we judged this domain at unclear risk of bias. |
| Other bias | Low risk | No other sources of bias noted. |
| Study characteristics | ||
| Methods | Phase III RCT (relative non‐inferiority) Single centre Accrual dates: started accrual 2004 Country: Spain Median follow‐up: 60 months | |
| Participants | 102 women with invasive ductal carcinoma breast Inclusion criteria: aged ≥ 60 years; unifocal tumour; primary tumour size 30 mm (pT2); cN0, pN0 axillary status; and histological Grade ≤ II Exclusion criteria: bilateral breast carcinoma; prior unilateral or contralateral breast cancer; concomitant or other previous malignancies; pure ductal or lobular carcinoma in situ (pTis); invasive lobular carcinoma; presence of an extensive intraductal component; excision with microscopically positive or close (3 mm) surgical margins; multicentric disease; node‐positive disease; concomitant or neoadjuvant chemotherapy; and postsurgical haematoma > 2 cm, or seroma fluid that required multiple aspirations | |
| Interventions | Experimental arm: PBI/APBI delivered by 3D‐CRT at 48 Gy/24 fractions ± 10 Gy boost (depending on risk factors for LR) (51 women) Control arm: conventional WBRT at 48 Gy/24 fractions ± 10 Gy boost (51 women) | |
| Outcomes | LR‐FS (which included both LR and new ipsilateral breast primaries): Assessed by: treating radiation oncologist, defined as "any histologically confirmed cancer in the treated breast," baseline mammogram at 6 months, then annually Time points assessed: weekly for 6 weeks; then at 1, 3, 6 and 12 months; then annually Time points reported: median follow‐up 60 months Cosmesis Assessed using Harvard Cosmetic Score (4‐point scale) Assessed by: treating radiation oncologist and participants Time points assessed: weekly for 6 weeks; then at 1, 3, 6 and 12 months; then annually; participants with > 1 year's follow‐up self‐assessed cosmetic outcome Time points reported: median follow‐up 60 months OS: not reported Toxicity: assessed: 1. acute RTOG CTC 2. late RTOG CTC and skin elasticity measured using a dedicated device Time points assessed: weekly for 6 weeks; then at 1, 3, 6 and 12 months; then annually Time points reported: 60 months C‐SS: not reported DM‐FS: not reported R‐FS Assessed by: treating radiation oncologist Time points assessed: weekly for 6 weeks; then at 1, 3, 6 and 12 months; then annually Time points reported: median 60 months' follow‐up L‐RR‐FS Assessed by: treating radiation oncologist Time points assessed: weekly for 6 weeks; then at 1, 3, 6 and 12 months; then annually Time points reported: median 60 months' follow‐up Mastectomy rate: not reported Compliance: number receiving allocated RT reported in each study arm Time points reported: at median 60 months' follow‐up Costs: not reported Quality of life: not reported Consumer preference: not reported | |
| Notes | QA: not mentioned. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was performed by a computer‐generated, randomized list," page 1052, paragraph 5. Adequate method of sequence generation; low risk of bias. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment was not clearly described; unclear risk of bias. |
| Blinding of participants and personnel (performance bias): objective outcomes | Low risk | Blinding of participants and personnel not mentioned, and probably not done, as it would have seen difficult in view of the technical aspects of the 2 intervention arms; low risk of bias. Quote: "Baseline mammography was performed at six months after completion of RT and then annually," (Rodríguez 2013, page 1053). LR‐FS: low risk of bias OS: not assessed New primary: not assessed Compliance: low risk of bias Costs: not assessed |
| Blinding of participants and personnel (performance bias): subjective outcomes | Unclear risk | Binding of participants and personnel not mentioned, and probably not done, as it would have seen difficult in view of the technical aspects of the 2 intervention arms; unclear risk of bias. Cosmesis: unclear risk of bias Toxicity: unclear risk of bias C‐SS: unclear risk of bias R‐FS: unclear risk of bias L‐RR‐FS: unclear risk of bias Quality of life: not assessed Consumer preference: not assessed |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Baseline mammography was performed 6 months after the completion of radiation therapy and yearly thereafter. Abdominal ultrasonography, chest radiography, and blood tests were performed at least annually. Local recurrence was defined as any histologically confirmed cancer tissue in the treated breast," page 1053, paragraph 2. Because the mammography intervals were prespecified and LR required histological confirmation, the lack of blinding on the part of the outcome assessors was not judged at high risk of bias. LR‐FS: low risk of bias. OS: not assessed. New primary: not assessed. Compliance: low risk of bias. |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "Cosmetic results were evaluated according to the Harvard criteria at baseline and at each follow‐up visit by the treating radiation oncologist," page 1053, paragraph 5. All participants who had a minimum of 1 year' follow‐up were asked to rate cosmetic results on a 10‐point scale, as follows: excellent (10–9), good (8–6), fair (5–4), or poor (3–1). Acute, late RT toxicity and cosmesis were evaluated by the treating physician (not blinded, so at risk of bias). However, participants (who were not masked to treatment group) also rated the cosmetic outcome; high risk of bias. Cosmesis: high risk of bias. Toxicity: high risk of bias. R‐FS: high risk of bias. L‐RR‐FS: high risk of bias. Quality of life: not assessed. Consumer preference: not assessed. |
| Incomplete outcome data (attrition bias) | Low risk | LR‐FS: 51 analysed of 51 randomised PBI arm and 51 analysed of 51 randomised WBRT arm; low risk of bias. Cosmesis: 51 analysed of 51 randomised PBI arm and 51 analysed of 51 randomised WBRT arm; low risk of bias. Toxicity 1. acute: 51 analysed of 51 randomised PBI arm and 51 analysed of 51 randomised WBRT arm; low risk of bias. 2. late: 51 analysed of 51 randomised PBI arm and 51 analysed of 51 randomised WBRT arm; low risk of bias. R‐FS: 51 analysed of 51 randomised PBI arm and 51 analysed of 51 randomised WBRT arm; low risk of bias. L‐RR‐FS: 51 analysed of 51 randomised PBI arm and 51 analysed of 51 randomised WBRT arm; low risk of bias. Compliance: 51 analysed of 51 randomised PBI arm and 51 analysed of 51 randomised WBRT arm; low risk of bias. |
| Selective reporting (reporting bias) | Unclear risk | Interim report; unclear risk of bias. |
| Other bias | Unclear risk | Interim report; unclear risk of bias. |
| Study characteristics | ||
| Methods | Multicentre international randomised non‐inferiority Phase III trial Accrual: March 2000 – data lock 2 May 2010 Country: 10 countries (across Europe, the UK, the US and Australia) Median follow‐up: 8.6 years | |
| Participants | 2298 women aged ≥ 45 years, with T1 and small T2N0‐1M0 invasive breast cancer, suitable for BCS, available for 10 years' follow‐up | |
| Interventions | Experimental arm (1140 participants): 1 fraction of RT given intraoperatively (using Intrabeam); 50 kV 20 Gy/fraction at 2 mm beyond surface of 1.5–5.0 cm spherical applicator placed in excision cavity Control arm (1158 participants): standard postoperative RT (40–56 Gy ± 10–16 Gy boost) | |
| Outcomes | LR‐FS (which included both invasive LR and new ipsilateral breast primaries) Assessed by: monitored as per individual centre's policy, pathological confirmation mandatory. Mammogram ipsilateral breast annually, contralateral breast 3 yearly, clinic visit and examinations 6 monthly for 5 years, then annually Time points assessed: clinic visit and examinations 6 monthly for 5 years, then annually Time points reported: median follow‐up 5 years and 8.6 years Cosmesis Assessed by: photos assessed by clinicians and nurses (masked to treatment allocation) Time points assessed: 2 and 5 years Time points reported: median 29 months OS Assessed by: death any cause Time points assessed: clinic visit and examinations 6 monthly for 5 years, then annually Time points reported: median follow‐up 5 years and 8.6 years Toxicity Assessed: using RTOG, LENT‐SOMA and CTCAE Time points assessed: clinic visit and examinations 6 monthly for 5 years, then annually Time points reported: late toxicity reported at 6 months New primary: site of recurrence in breast recorded Time points assessed: clinic visit and examinations 6 monthly for 5 years, then annually Time points reported: not reported in this publication C‐SS Assessed by: investigator masked to study arm Time points assessed: clinic visit and examinations 6 monthly for 5 years, then annually Time points reported: median follow‐up 8.6 years DM‐FS Assessed by: investigators Time points assessed: clinic visit and examinations 6 monthly for 5 years, then annually Time points reported: median follow‐up 8.6 years R‐FS Assessed by: investigators Time points assessed: clinic visit and examinations 6 monthly for 5 years, then annually Time points reported: median follow‐up 29 months L‐RR‐FS Assessed by: investigators Time points assessed: clinic visit and examinations 6 monthly for 5 years, then annually Time points reported: median follow‐up 29 months Mastectomy rate Assessed by: investigators Time points assessed: clinic visit and examinations 6 monthly for 5 years, then annually Time points reported: median follow‐up 8.6 years Compliance Assessed by: investigators, number receiving allocated RT reported in each study arm Time points assessed: number receiving allocated RT reported in each study arm Time points reported: median follow‐up 29 months Costs: not reported in this publication Quality of life Assessed by: QLQ‐C30, QLQ‐BR23 and Body image scale Time points assessed: at baseline, three, six, nine months then annually Time points reported: 12 months Consumer preference: not reported in this publication Time points assessed: 6 weeks, 2–3 months (for those women not having chemotherapy) and 8–9 months for women having chemotherapy) | |
| Notes | Intrabeam uses low kilovolt x‐rays to deliver 20 Gy at the surface of the tumour bed, attenuating to 5–7 Gy at 1 cm. QA: training and auditing by member of International Standards Organisation (ISO) required before centre could join. NCT00983684, ISCTN 34086741, ISRCTN 34086741, REC No. 99/0307, UKCRN. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomisation schedules were generated centrally by computer (securely kept in trial centres in Perth for Australian centres and London, UK, for all other centres)," page 94, paragraph 1. |
| Allocation concealment (selection bias) | Low risk | Quote: "Patients were randomly assigned in a 1:1 ratio … with blocks stratified by centre," abstract, page 1, paragraph 2. Quote: "The randomisation schedules were generated centrally by computer (securely kept in trial centres in Perth for Australian centres, and London, UK for all other centres). Requests for randomisation were via telephone or fax to the trials office (Perth or London), where a trained member of staff checked patient eligibility. Treatment was allocated from a pre‐printed randomisation schedule available to authorised staff only. Written confirmation of randomisation was sent by fax to the site," methods, page 94, paragraph 1. Likely to have had adequate allocation concealment; low risk of bias. |
| Blinding of participants and personnel (performance bias): objective outcomes | Low risk | Participants: "Neither patients nor investigators or their teams were masked to treatment assignment," abstract, page 1, paragraph 2. Physicians: "Neither patients nor investigators or their teams were masked to treatment assignment," abstract, page 1, paragraph 2. Quote: "Individual centres were unblinded to treatment given in their own centres, but they were not given access to these data for other sites," methods, page 1, paragraph 3. Quote: "Patient assessments were scheduled at entry." Because of the nature of the intervention, it was not possible to blind the women participating or the personnel involved in their care, this is not likely to have resulted in bias. Because the patient assessments were scheduled at trial entry with pre‐specified times for follow‐up visits this is likely to have reduced the risk of bias from the lack of blinding of personnel. LR‐FS: low risk of bias. OS: low risk of bias. New elsewhere primary: low risk of bias. Subsequent mastectomy: low risk of bias. Compliance: low risk of bias. Costs: low risk of bias. |
| Blinding of participants and personnel (performance bias): subjective outcomes | High risk | Participants: "Neither patients nor investigators or their teams were masked to treatment assignment," abstract, page 1, paragraph 2. Physicians: "Neither patients nor investigators or their teams were masked to treatment assignment," abstract, page 1, paragraph 2. Quote: "Individual centres were unblinded to treatment given in their own centres, but they were not given access to these data for other sites," methods, page 4, paragraph 3. Quote: "Patient assessments were scheduled at entry." Because of the nature of the intervention, it was not possible to blind the women participating or the personnel involved in their care, this is not likely to have resulted in bias. Because the participant assessments were scheduled at trial entry with prespecified times for follow‐up visits this is likely to have reduced the risk of bias from the lack of blinding of personnel. Cosmesis: high risk of bias. Toxicity: high risk of bias. C‐SS: high risk of bias. DM‐FS: high risk of bias. L‐RR‐FS: high risk of bias. Quality of life: high risk of bias. Consumer preference: high risk of bias. |
| Blinding of outcome assessment (detection bias) | Low risk | Participants: not relevant. Physicians: not relevant. Assessors: "Patient's assessments were scheduled at entry, 3 months and 6 months," page 94, paragraph 4. This means the risk of lead time bias was reduced. Quote: "We recommend that mammography of the ipsilateral breast occurs annually and of the contralateral breast at least every three years," TARGIT protocol, 7.1 page 25. Quote: "Confidential unblinded reports for the DMC, and blinded reports for the ISO were produced by the trial statistician. Unblinded analyses were done according to a prespecified statistical analysis plan," methods, page 4, paragraph 3. If there were prespecified time intervals for mammography, this would have reduced the risk of bias for detection of the primary endpoint: local relapse. LR‐FS: low risk of bias. OS: low risk of bias. New primary: low risk of bias. Subsequent mastectomy: low risk of bias. Compliance: low risk of bias. Costs: low risk of bias. |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "The secondary outcome measure of local toxicity, or morbidity was assessed from data recorded on the complications form which contained a pre‐specified checklist," page 94, paragraph 3. It was not stated who assessed the subjective outcomes, however, we know: "Neither patients nor investigators or their teams were masked to treatment assignment," abstract, page 1, paragraph 2. The blinding of outcome assessors was not reported, this does mean that there was risk of bias with assessment of toxicity; however, the use of a prespecified form would help to reduce bias because the data would be collected for all women. Quote: "digital photographs … were assessed, blinded to treatment arm" (Keshtgar et al. Journal of Clinical Oncology 2010;28(15 Suppl):Abstract 570) Quote: "An independent senior clinician, masked to randomisation, reviewed the available data and ascertained the cause of death in all cases" (Erratum: radiotherapy for breast cancer, the TARGIT‐A trial (The Lancet (2014) 383(9930) (1716). Lancet 2015;385(9976):1396). Cosmesis: low risk of bias. Toxicity: high risk of bias. C‐SS: low risk of bias. DM‐FS: high risk of bias. L‐RR‐FS: high risk of bias. Quality of life: high risk of bias. Consumer preference: high risk of bias. |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "All randomised patients were included in the intention‐to‐treat analysis," Abstract, page 1, paragraph 2 LR‐FS: 1140 analysed of 1140 randomised PBI arm and 1158 analysed of 1158 randomised WBRT arm Cosmesis: analysed in 55 in PBI arm and 50 in WBRT arm OS: 1140 analysed of 1140 randomised PBI arm and 1158 analysed of 1158 randomised WBRT arm Toxicity: C‐SS: 1140 analysed of 1140 randomised PBI arm and 1158 analysed of 1158 randomised WBRT arm DM‐FS: 1140 analysed of 1140 randomised PBI arm and 1158 analysed of 1158 randomised WBRT arm L‐RR‐FS: 1140 analysed of 1140 randomised PBI arm and 1158 analysed of 1158 randomised WBRT arm Salvage mastectomy: 1140 analysed of 1140 randomised PBI arm and 1158 analysed of 1158 randomised WBRT arm Quality of life: not reported Consumer preference: not assessed |
| Selective reporting (reporting bias) | Low risk | Outcomes specified in the protocol
Outcomes specified in methods
Outcomes reported in paper
Quote: "no changes were made to trial outcomes after commencement of the trial." Low risk of bias. |
| Other bias | Low risk | No other risk of bias identified. |
3D‐CRT: 3‐dimensional conformal radiotherapy; APBI: accelerated partial breast irradiation; BCS: breast‐conserving surgery; bd: twice a day; C‐SS: cause‐specific survival; CTCAE: Common Terminology Criteria for Adverse Events; DCIS: ductal carcinoma in situ; DM‐FS: distant metastasis‐free survival; DMC: data monitoring committee; EBRT: external beam radiotherapy; ECOG: Eastern Cooperative Oncology Group; EORTC: European Organisation for Research and Treatment of Cancer; EORTC QLQ‐C30: European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire; EORTC QLQ‐BR23: European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire – Breast Specific Module; EQ‐5D‐3L: 3‐level version of European Quality of Life Five Dimension; Gy: Gray; HADS: Hospital Anxiety and Depression Scale; HDR: high‐dose rate; IBRT: ipsilateral breast tumour recurrence; IHC: immunohistochemistry; IMRT: intensity‐modulated radiotherapy; L‐RR‐FS: locoregional recurrence‐free survival; LENT‐SOMA: late effects in normal tissues – subjective objective, management and analytic; LR: local recurrence; LR‐FS: local recurrence‐free survival; LTFU: lost to follow‐up; LVI: lymphovascular invasion; M: metastases; MeV: mega electron volts; N: lymph node; NCI: National Cancer Institute; OS: overall survival; PBI: partial breast irradiation; PDR: pulsed‐dose rate; QA: quality assurance; RCT: randomised controlled trial; RNI: regional nodal irradiation; RT: radiotherapy; RTOG: Radiation Therapy Oncology Group; RTOG CTC: Radiation Therapy Oncology Group Common Toxicity Criteria; WBRT: whole breast radiotherapy.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| RCT, but used surgical, systemic management and RT techniques that were not consistent with contemporary practice. | |
| PBI used in both study arms. | |
| PBI used in both study arms. | |
| PBI used in both study arms. | |
| RCT, but used surgical, systemic management and RT techniques that were not consistent with contemporary practice. | |
| WBRT used in both study arms. | |
| Feasibility study and not an RCT. |
PBI: partial breast irradiation; RCT: randomised controlled trial; RT: radiotherapy; WBRT: whole breast radiotherapy.
Characteristics of studies awaiting classification [ordered by study ID]
| Methods | Phase II RCT |
| Participants | Postmenopausal women with node negative, hormone receptor‐positive breast cancer, < 3 cm |
| Interventions | APBI arm: 30 Gy in 5 fractions VMAT, daily IGRT Control arm: either 40.5 Gy in 15 fractions or 48 Gy in 15 fractions VMAT, daily IGRT. |
| Outcomes | Toxicity assessed using CTCAE version 4.0 Cosmesis assessed using Harvard Cosmetic Score Local control, D‐FS, OS, quality of life |
| Notes | Accrual dates: study terminated early |
| Methods | RCT |
| Participants | Women aged ≥ 35 years, unifocal tumour, invasive ductal carcinoma, tumour size ≤ 4 cm, cN0, pN0‐1, any grade histology |
| Interventions | Experimental arm: 34 Gy/ 10 fractions given twice daily Control arm: 40 Gy/16 fractions plus or minus boost (10–16 Gy in 5–8 fractions) |
| Outcomes | Primary outcome: ipsilateral breast tumour recurrence Secondary outcomes: toxicity (acute and late), cosmesis, D‐FS, OS |
| Notes |
APBI: accelerated partial breast irradiation; CTCAE: Common Toxicity Criteria for Adverse Events; Gy: Gray; IGRT: image‐guided radiotherapy; OS: overall survival; RCT: randomised controlled trial; VMAT: volume modulated arc therapy.
Characteristics of ongoing studies [ordered by study ID]
| Study name | Breast cancer with low risk of LR: partial and accelerated radiation with three‐dimensional conformal radiotherapy (3DCRT) vs. standard radiotherapy after conserving surgery (Phase III study) |
| Methods | Multicentre Phase III controlled randomised, unblinded study of non‐inferiority |
| Participants | Women aged ≥ 49 years, ECOG 0–2, undergoing conservative breast surgery for invasive breast cancer, pT1‐2 (< 3 cm in diameter), pN0‐N1 M0, unifocal, resection margins histologically negative (2 mm) at first intervention or after subsequent widening |
| Interventions | Experimental arm: 38.5 Gy total in 10 fractions (3.85 Gy per fraction) bd with an interval of ≥ 6 hours between the 2 fractions, for 5 consecutive working days of the sole cavity Control arm: 50.0 Gy in 25 fractions (2 Gy per fraction), once a day for 5 days in the week RT of the entire breast |
| Outcomes | Primary: survival free of local ipsilateral recurrence as prime event Secondary: global survival, L‐RR‐FS, distant recurrence‐free, acute and late toxicity (RTOG) and cosmetic result |
| Starting date | |
| Contact information | Data Center Office Clinical Trials Office, Integrated Department of Oncology and Hematology Polyclinic Hospital, University of Modena and Reggio Emilia R D'Amico, G Jovic, R Vicini Tel: 059 4223865 Email: [email protected] |
| Notes | Study currently accruing participants. Target volume: GTV + 15 mm = CTV + 5 mm = PTV |
| Study name | Partial breast versus whole breast irradiation in elderly women operated on for early breast cancer |
| Methods | RCT |
| Participants | Inclusion criteria: women aged ≥ 60 years; operated for unilateral, unifocal early breast cancer pT1, pN0, M0, Grade I or II, positive ER or PgR (or both), HER2 negative Exclusion criteria: lobular carcinoma |
| Interventions | Experimental arm: 40 Gy/15 fractions PBI Control arm: 40 Gy/15 fractions WBI |
| Outcomes | Primary outcomes: Grade II or III fibrosis Secondary outcomes: late toxicity, recurrence, survival |
| Starting date | 2009 |
| Contact information | Birgitte Offersen, Danish Breast Cancer Cooperative Group |
| Notes | DGCG PBI protocol, CIRRO 03610 |
| Study name | A Phase 3 trial of accelerated whole breast irradiation with hypofractionation plus sequential boost for early stage breast cancer |
| Methods | RCT |
| Participants | |
| Interventions | Hypofractionated WBI with concurrent boost
WBI with sequential boost
|
| Outcomes | Local recurrence; OS |
| Starting date | 2011 |
| Contact information | Kwan Ho Cho, Radiation Oncologist, National Cancer Center, Korea |
| Notes |
| Study name | A phase II randomized clinical trial of accelerated partial breast irradiation compared with whole breast irradiation with IMRT in early breast cancer |
| Methods | RCT Allocation: randomised Intervention model: parallel assignment Masking: none (open label) |
| Participants | Inclusion criteria: life expectation: > 5 years; enrolment date: ≤ 12 weeks after breast‐conserving surgery or ≤ 8 weeks after adjuvant chemotherapy; histologically confirmed diagnosis of invasive ductal carcinoma (Grade I–II), or mucinous carcinoma, or papillary carcinoma, or tubular carcinoma, or medullary carcinoma: primary tumour ≤ 3.0 cm in maximum diameter and pN0; or histologically confirmed DCIS: primary tumour ≤ 2.5 cm in maximum diameter, low‐medium grade; unifocal tumour (confirmed by diagnostic MRI); no lymphovascular invasion; ER positive (defined as medium‐strongly nuclear staining in > 1% of the cancer cells); negative radial resection margins of ≥ 2 mm; surgical clips placed in the tumour bed; written informed consent Exclusion criteria: Stage II–III; multifocal tumours; histologically confirmed diagnosis of invasive ductal carcinoma (Grade III), invasive micropapillary carcinoma, carcinoma of lobular in situ, invasive lobular carcinoma; Paget's disease of the nipple; underwent oncoplastic surgery of ipsilateral breast; underwent neoadjuvant chemotherapy or hormonal therapy; previous or simultaneous contralateral breast cancer; undergone ipsilateral chest wall RT; active collagen vascular disease |
| Interventions | Experimental arm: APBI: radiation to the breast tumour bed to a total dose of 40 Gy/10 fractions/2 weeks, using IMRT technique Control arm: WBI: radiation to the WB to a total dose of 43.5 Gy/15 fractions/3 weeks, using IMRT technique |
| Outcomes | Primary outcome
Secondary outcomes
|
| Starting date | 19 July 2017 |
| Contact information | Shu lian Wang, Chinese Academy of Medical Sciences; [email protected] |
| Notes |
| Study name | Phase III randomized study of adjuvant whole breast versus partial breast irradiation using once daily or twice daily fractionation scheme in women with Stage I or II breast cancer |
| Methods | RCT |
| Participants | Women aged ≥ 40 years with histologically confirmed adenocarcinoma breast, ≤ 3 cm, unifocal, margin negative, axillary staging (sentinel node biopsy, if negative no further required, if positive, axillary dissection required, if no SNB, AD required, with removal of ≥ 6 nodes. Clearly defined cavity which occupies no > 30% of entire breast volume. Exclusion criteria: no multifocal disease in > 1 quadrant, separated by 4 cm, node‐positive, Paget's DCIS or invasive disease, collagen disorders |
| Interventions | Experimental arm: 3D‐CRT 38.5 Gy/10 fractions or 38.5 Gy/5 fractions Control arm: 3D‐CRT 50 Gy/25 fractions + 10 Gy/5 fraction boost for high‐grade tumour or age < 50 years |
| Outcomes | Primary outcome
Secondary outcome
|
| Starting date | 2013 |
| Contact information | Rimoun Boutrus, Cairo, Egypt |
| Notes |
| Study name | Medico economic study, randomized, comparing intraoperative radiotherapy with Intrabeam® on surgical resection bed versus conventional surgery + EBRT in postmenopausal patients operated by conservative surgery for low risk breast cancer |
| Methods | RCT |
| Participants | Women aged > 55 years Inclusion criteria: histologically confirmed invasive ductal breast cancer; menopausal women aged ≥ 55 years; clinical and ultrasound size ≤ 20 mm, N0; biopsy with all following criteria: SBR I or II, HER2 (0, +, ++ with fluorescence in situ hybridisation or silver in situ hybridisation required), positive ERs, no embolus; no personal history of breast cancer or BRCA gene mutation; social insurance; signed consent Exclusion criteria: bifocal or bilateral breast cancer; presence of invasive ductal carcinoma with diffuse microcalcifications on mammography; invasive lobular carcinoma; presence of lymph node involvement; history of malignant disease if life expectancy without recurrence at 10 years < 90%; adults under guardianship; history of chest RT (Hodgkin's) |
| Interventions | PBI using RIOP‐Intrabeam 2 0Gy/single fraction WBRT 50 Gy/25 fractions + 10 Gy/5 fraction boost |
| Outcomes | Primary
Secondary outcomes
|
| Starting date | 2012 |
| Contact information | Le Blanc M, Institut Cancerologie de l'Ouest, Saint‐Herblain, France |
| Notes | ICO‐2012‐03 |
| Study name | Standard or hypofractionated radiotherapy versus accelerated partial breast irradiation (PBI/APBI) for breast cancer (SHARE) phase III multicentric trial comparing accelerated partial breast irradiation (PBI/APBI) versus standard or hypofractionated whole breast irradiation in low risk of local recurrence of breast cancer |
| Methods | Multicentre RCT |
| Participants | Inclusion criteria: women aged ≥ 50 years; menopausal status confirmed; pathology confirmation of invasive carcinoma (all types); complete tumour removal and conservative surgery; pathological tumour size of invasive carcinoma ≤ 2 cm (including the in situ component) pT1; all histopathological grades; clear lateral margins for the invasive and in situ disease (> 2 mm); pN0 or pN(i+); no metastasis; RT should be started > 4 weeks and < 12 weeks after last surgery; surgical clips (4 or 5 clips in the tumour bed); no prior breast or mediastinal RT; ECOG 0–1; information to the participant and signed informed consent Exclusion criteria: multifocal invasive ductal carcinoma defined as the presence of ≥ 2 distinct tumours that are separated by normal tissue or when the distance between the 2 lesions does not permit conservative surgery; bilateral breast cancer; no or < 4 surgical clips in the tumour bed; nodal involvement: pN1 (including micrometastasis, mi+), pN2, pN3; metastatic disease; internal mammary node involvement or supraclavicular lymph node involvement; indication of chemotherapy or trastuzumab; involved or close lateral margins for the invasive with or without in situ components (< 2 mm) AND impossibility to re‐operate or impossible to perform another conservative surgery; women with known BRCA1 or BRCA2 mutations; previous mammoplasty; previous homolateral breast or mediastinal irradiation, or both; previous invasive cancer (except basocellular epithelioma or in situ carcinoma of the cervix); no geographical, social or psychological reasons that would prevent study follow‐up |
| Interventions | Experimental arm: APBI; 3D‐CRT; 40 Gy/10 fractions. Tumour bed 40 Gy in 10 fractions, 2 fractions of 4 Gy per day in 5–7 days. PBI/APBI using 3D‐CRT technique, in 5 days, 40 Gy to the tumour bed Control arm: standard or hypofractionated RT |
| Outcomes | Primary
Secondary
|
| Starting date | October 2010 |
| Contact information | Jerome Lemonnier, PhD; Tel: +33 1 7193 6702; Email: j‐[email protected] |
| Notes |
3D‐CRT: 3‐dimensional conformal radiotherapy; APBI: accelerated partial breast irradiation; BCS: breast‐conserving surgery; bd: twice a day; CTV: clinical target volume; DCIS: ductal carcinoma in situ; ECOG: Eastern Cooperative Oncology Group; ER: oestrogen receptor; GTV: gross tumour volume; Gy: Gray; IGRT: image‐guided radiotherapy; IMRT: intensity‐modulated radiotherapy; M: metastases; MRI: magnetic resonance imaging; N: lymph node; PBI: partial breast irradiation; PgR: progesterone receptor; PTV: planning target volume; RCT: randomised controlled trial; RT: radiotherapy; RTOG: Radiation Therapy Oncology Group; SN: sentinel node biopsy; WB: whole breast; T: tumour; WBI: whole breast irradiation; WBRT: whole breast radiotherapy.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Local recurrence‐free survival Show forest plot | 8 | 13168 | (Exp[(O‐E) / V], Fixed, 95% CI) | 1.21 [1.03, 1.42] |
| Analysis 1.1  Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 1: Local recurrence‐free survival | ||||
| 1.1.1 5 years' follow‐up | 5 | 8265 | (Exp[(O‐E) / V], Fixed, 95% CI) | 1.20 [0.99, 1.45] |
| 1.1.2 10 years' follow‐up | 3 | 4903 | (Exp[(O‐E) / V], Fixed, 95% CI) | 1.22 [0.92, 1.64] |
| 1.2 Cosmesis (participant‐reported) Show forest plot | 2 | 2775 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.08 [1.68, 2.57] |
| Analysis 1.2  Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 2: Cosmesis (participant‐reported) | ||||
| 1.3 Cosmesis, physician/nurse‐reported Show forest plot | 6 | 3652 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.57 [1.31, 1.87] |
| Analysis 1.3  Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 3: Cosmesis, physician/nurse‐reported | ||||
| 1.4 Overall survival Show forest plot | 8 | 13175 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 0.99 [0.88, 1.12] |
| Analysis 1.4  Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 4: Overall survival | ||||
| 1.5 Acute radiotherapy (RT) skin toxicity Show forest plot | 4 | 3925 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.66, 0.88] |
| Analysis 1.5  Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 5: Acute radiotherapy (RT) skin toxicity | ||||
| 1.6 Late RT skin toxicity Show forest plot | 3 | 3465 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.27 [1.63, 3.15] |
| Analysis 1.6  Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 6: Late RT skin toxicity | ||||
| 1.7 Telangiectasia (late RT toxicity) Show forest plot | 2 | 3010 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.40 [3.34, 5.80] |
| Analysis 1.7  Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 7: Telangiectasia (late RT toxicity) | ||||
| 1.8 Fat necrosis Show forest plot | 4 | 3565 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.76 [1.74, 4.38] |
| Analysis 1.8  Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 8: Fat necrosis | ||||
| 1.9 Subcutaneous fibrosis (late RT toxicity) Show forest plot | 2 | 3011 | Odds Ratio (M‐H, Fixed, 95% CI) | 5.07 [3.81, 6.74] |
| Analysis 1.9  Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 9: Subcutaneous fibrosis (late RT toxicity) | ||||
| 1.10 Breast pain (late RT toxicity) Show forest plot | 2 | 3012 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.81 [1.15, 2.86] |
| Analysis 1.10  Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 10: Breast pain (late RT toxicity) | ||||
| 1.11 New primary tumours in ipsilateral breast, 'elsewhere primary' Show forest plot | 4 | 5144 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.82 [1.55, 5.12] |
| Analysis 1.11  Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 11: New primary tumours in ipsilateral breast, 'elsewhere primary' | ||||
| 1.12 Cause‐specific survival Show forest plot | 7 | 9865 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 1.06 [0.83, 1.36] |
| Analysis 1.12  Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 12: Cause‐specific survival | ||||
| 1.13 Distant metastasis‐free survival Show forest plot | 7 | 11033 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 0.95 [0.80, 1.13] |
| Analysis 1.13  Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 13: Distant metastasis‐free survival | ||||
| 1.14 Relapse‐free survival Show forest plot | 6 | 11756 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 1.25 [1.05, 1.48] |
| Analysis 1.14  Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 14: Relapse‐free survival | ||||
| 1.15 Locoregional recurrence‐free survival Show forest plot | 5 | 6718 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 1.36 [1.06, 1.74] |
| Analysis 1.15  Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 15: Locoregional recurrence‐free survival | ||||
| 1.16 Subsequent mastectomy Show forest plot | 3 | 3740 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.78, 1.23] |
| Analysis 1.16  Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 16: Subsequent mastectomy | ||||

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: 1 Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), outcome: 1.1 Local recurrence‐free survival.

Forest plot of comparison: 1 Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), outcome: 1.3 Overall survival.

Forest plot of comparison: 1 Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), outcome: 1.8 Cause‐specific survival.

Forest plot of comparison: 1 Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), outcome: 1.9 Distant metastasis‐free survival.

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 1: Local recurrence‐free survival

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 2: Cosmesis (participant‐reported)

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 3: Cosmesis, physician/nurse‐reported

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 4: Overall survival

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 5: Acute radiotherapy (RT) skin toxicity

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 6: Late RT skin toxicity

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 7: Telangiectasia (late RT toxicity)

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 8: Fat necrosis

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 9: Subcutaneous fibrosis (late RT toxicity)

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 10: Breast pain (late RT toxicity)

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 11: New primary tumours in ipsilateral breast, 'elsewhere primary'

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 12: Cause‐specific survival

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 13: Distant metastasis‐free survival

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 14: Relapse‐free survival

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 15: Locoregional recurrence‐free survival

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 16: Subsequent mastectomy
| PBI/APBI compared to WBRT for early breast cancer | ||||||
| Patient or population: health problem or population Setting: Academic, tertiary and community practice Intervention: PBI/APBI Comparison: WBRT | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with WBRT | Risk with PBI/APBI | |||||
| Local recurrence‐free survival ‐ total (LR‐FS) | Low | HR 1.21 | 13168 | ⊕⊕⊕⊝ | ||
| 985 per 1000 | 982 per 1000 | |||||
| Cosmesis, physician/nurse‐reported | 138 per 1000 | 201 per 1000 | OR 1.57 | 3652 | ⊕⊕⊕⊝ | |
| Overall survival | Low | HR 0.99 | 13175 | ⊕⊕⊕⊕ | ||
| 949 per 1000 | 949 per 1000 | |||||
| Subcutaneous fibrosis (late RT toxicity) | 43 per 1000 | 184 per 1000 | OR 5.07 | 3011 | ⊕⊕⊕⊝ | |
| Cause‐specific survival (C‐SS) | Low | HR 1.06 | 9865 | ⊕⊕⊕⊝ | ||
| 983 per 1000 | 982 per 1000 | |||||
| Distant metastasis‐free survival (DM‐FS) | Low | HR 0.95 | 11033 | ⊕⊕⊕⊝ | ||
| 971 per 1000 | 972 per 1000 | |||||
| Subsequent mastectomy | 97 per 1000 | 95 per 1000 | OR 0.98 | 3740 | ⊕⊕⊕⊕ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| See interactive version of this table: https://gdt.gradepro.org/presentations/#/isof/isof_question_revman_web_416473753410884319. | ||||||
| a. There was considerable clinical heterogeneity with respect to radiotherapy dose, technique and use of quality assurance procedures. However, the techniques employed delivered a dose that was the same or higher in the APBI/PBI arm than the WBRT arm, which should mean the local recurrence‐free survival is better or at least the same. | ||||||
| Cosmetic score |
|---|
| Excellent |
| Good |
| Fair |
| Poor |
| RTOG CTC | Grade I | Grade II | Grade III | Grade IV |
|---|---|---|---|---|
| Acute skin | Follicular, faint or dull erythema/epilation/dry desquamation/decreased sweating | Tender or bright erythema, patchy moist desquamation/moderate oedema | Confluent, moist desquamation other than skin folds, pitting oedema | Ulceration, haemorrhage, necrosis |
| Late skin toxicity | Slight atrophy, pigmentation change, some hair loss | Patchy atrophy, moderate telangiectasia, total hair loss | Marked atrophy, gross telangiectasia | Ulceration |
| Late subcutaneous fibrosis | Slight induration, loss of subcutaneous fat | Moderate fibrosis (asymptomatic) < 10% linear field contraction | Severe induration, loss of subcutaneous tissue, linear contraction > 10% | Ulceration |
| CTCAE: Common Terminology Criteria for Adverse Events; EORTC: European Organisation for Research and Treatment of Cancer; RTOG CTC: Radiation Therapy Oncology Group Common Toxicity Criteria. | ||||
| Toxicity | Grade 1 | Grade 2 | Grade 3 | Grade 4 |
|---|---|---|---|---|
| Induration (subcutaneous fibrosis) | Increased density on palpation | Moderate increase in density, not interfering with ADL; marked increase in density and firmness on palpation with or without minimal retraction | Dysfunction interfering with ADL; very marked density, retraction or fixation | — |
| Telangiectasia | Few | Moderate | Many and confluent | — |
| Pain | Pain mild, not interfering with function | Moderate pain; pain or analgesics interfering with function, but not with ADL | Severe pain; pain or analgesics interfering with ADL | Disability |
| ADL: activities of daily living; NCI CTC: National Cancer Institute Common Toxicity Criteria. | ||||
| Adverse effect | Grade I | Grade II | Grade III | Grade IV | Grade V |
|---|---|---|---|---|---|
| Pain | Mild, not interfering with function | Moderate/analgesics, interferes with function, but not ADL | Severe or interferes with ADL, or both | — | — |
| Telangiectasia | Few | Moderate | Many or confluent, or both | — | — |
| Acute skin toxicity | Faint erythema or dry desquamation | Moderate‐to‐brisk erythema, patchy moist desquamation | Moist desquamation not limited to creases or skin folds, bleeding subsequent to minor trauma or abrasion | Skin necrosis or full dermal thickness ulceration | Death |
| Induration/fibrosis | Increased density on palpation | Moderate functional impairment, not interfering with ADL, increased density and firmness on palpation with or without minor retraction | Interferes with ADL, very marked increased density, retraction or fixation | — | — |
| ADL: activities of daily living; CTCAE: Common Terminology Criteria for Adverse Events; EORTC: European Organisation for Research and Treatment of Cancer; RTOG: Radiation Therapy Oncology Group. | |||||
| Adverse effect | Grade I | Grade II | Grade III | Grade IV | Grade V |
|---|---|---|---|---|---|
| Subcutaneous fibrosis | — | Mild induration, can move skin parallel to the plane (sliding) and perpendicular to the plane (pinching up) | Moderate induration, can slide, cannot pinch up skin | Severe induration cannot slide or pinch skin | Death |
| Telangiectasia | < 10 % of body surface area | ≥ 10% of body surface area, psychosocial impact | — | — | — |
| Pain | mild | Moderate, not limiting instrumental ADL | Severe, limiting self‐care ADL | — | — |
| ADL: activities of daily living; CTCAE: Common Terminology Criteria for Adverse Events; EORTC: European Organisation for Research and Treatment of Cancer; RTOG: Radiation Therapy Oncology Group. | |||||
| Grade | Findings |
|---|---|
| 0 | No fat necrosis |
| 1 | Asymptomatic fat necrosis (only radiological or cytological findings, or both) |
| 2 | Symptomatic fat necrosis not requiring medication (palpable mass with or without mild pain) |
| 3 | Symptomatic fat necrosis requiring medication (palpable mass with significant pain) |
| 4 | Symptomatic fat necrosis requiring surgical intervention |
| Study | Age | Stage | Margins | Tumour size | Nodal status | Surgery |
|---|---|---|---|---|---|---|
| After 2000, < 40 years excluded | Unifocal tumour, pT1N0‐1miM0, Grade I or II | Negative | < 2.0 cm (< 2 mm: 1/258, ≥ 2 mm: 246/258 or had no tumour at ink: 11/258) | — | WLE | |
| 48–75 years | "Early breast cancer," "suitable for breast conservation" | Not described | ≤ 2.5 cm | AD if SNBx positive | BCS | |
| > 40 years | — | Negative, ≥ 5 mm | ≤ 2.5 cm | — | WLE or quadrantectomy | |
| ≥ 45 years | T1 and small T2N0‐1M0 invasive breast cancer, suitable for BCS, available for 10 years' follow‐up | ≥ 1 mm Re‐excision strongly advised for close or positive margins | — | — | BCS | |
| ≥ 40 years | DCISa or invasive breast cancer | Negative | ≤ 3 cm | Negative axillary nodal involvement including micrometastasis (> 0.2 mm or positive cells only identified on IHC as determined by sentinel node biopsy; axillary node dissection or clinical examination for DCIS only. | BCS | |
| ≥ 60 years | Invasive ductal carcinoma (pT1‐2cNO MO), unifocal tumour, Grade I or II | < 3 mm | ≤ 3 cm | — | — | |
| ≥ 50 years | Invasive breast cancer pT1‐2pN0 who have < 1% annual risk of local recurrence | ≥ 2 mm | ≤ 3 cm | 0–3 nodes positive | BCS | |
| > 40 years | Stage 0, I or II pN0/pNmi breast cancer (including DCIS) no vascular invasion, unifocal or unicentric disease only, no LVINote: 60/1184 (5%) participants had DCIS | ≥ 2 mm in invasive disease, 5 mm in DCIS | Lesions < 3 cm in diameter | Node negative, for DCIS alone: sentinel node biopsy optional | WLE or quadrantectomy, level I–II axillary dissection, removing ≥ 6 (preferably 10 lymph nodes) | |
| > 18 years | T0‐2N0‐1M0 DCIS or invasive breast cancer Note: 531/4216 (12%) participants had DCIS | Negative: "free of cancer, including DCSI" | Lesions < 3 cm | ≤ 3 involved nodes permitted | Lumpectomy | |
| AD: axillary dissection; BCS: breast‐conserving surgery; DCIS: ductal carcinoma in situ; IHC: immunohistochemistry; LVI: lymphovascular invasion; SNBx: sentinel node biopsy; WLE: wide local excision. | ||||||
| Study | RT quality assurance | RT technique | PIB/APBI target volume definition |
|---|---|---|---|
| Postimplant CT scans were performed | Interstitial brachytherapy (88/128) EBRT using photons (40/128) 2‐dimensional CT‐based | PTV: excision cavity delineated by the surgical clips + 2 cm isotropic margin. For interstitial therapy: if electrons were used, 6–15 MeV were used to treat the cavity with a 2 cm margin | |
| Not stated | Intraoperative electrons 6–9 MeV | CTV: quote: "decided according to the site and size of the tumour. The energy of the electron beams was selected according to the thickness of the gland measured by a graduated needle" | |
| Not stated | EBRT (IMRT) | CTV = +1 cm isotropic margin around surgical clips PTV = CTV +10 mm isotropic margina | |
| Nob | Intraoperative kV RT 3D‐CRT for WBRT | The target volume was the tumour cavityc | |
| Yesd | EBRT (3D‐CRT) APBI: 3–5 non‐coplanar fields | CTV = tumour bed on CT (surgical clips plus a 1‐cm margin inside breast PTV = CTV +1 cm isotropic margin | |
| Not stated | EBRT (3D‐CRT) | PTV was defined by contouring the same quadrant as the primary tumor sitee | |
| Yesf | Field‐in‐field IMRT | Tumour bed, surgical clipsg recommended | |
| Yesh | HDR or PDR multicatheter brachytherapy | PBI: tumour bedi +2 cm isotropic margin | |
| Quote: "Every institution's RT facilities were quality assessed and each case of APBI was centrally reviewed for RT quality." Benchmarking performed with "dummy run" | HDR brachytherapyj APBI EBRT: 3D‐CRTk (IMRT not permitted). WBRT: 3D‐CRT (IMRT not permitted) | No RNI permitted WBRT: entire ipsilateral breast APBI: CTV = cavity = PTV | |
| Study | RT quality assurance | RT technique | Target volume definition |
| 3D‐CRT: 3‐dimensional conformal radiotherapy; APBI: accelerated partial breast irradiation; CRT: conformal radiotherapy; CT: computer tomography; CTV: clinical target volume; EBRT: external beam radiotherapy; HDR: high‐dose rate; IMRT: intensity‐modulated radiotherapy; PDR: pulsed‐dose rate; PIB: partial breast irradiation; PTV: planning target volume; RNI: regional nodal irradiation; RT: radiotherapy; WBRT: whole breast radiotherapy. aThe surgeons were requested to place clips at the borders of the surgical bed, using a minimum of four clips. CTV was drawn on a planning CT (0.3 mm slices) with a uniform 1 cm margin around the surgical clips, then a 1 cm margin added to construct the PTV. | |||
| Score | Definition |
|---|---|
| Excellent | Perfect symmetry, no visible distortion or skin changes and no visible catheter entry/exit sequelae |
| Good | Slight skin distortion, retraction or oedema, any visible telangiectasia, any visible catheter entry/exit scar or mild hyperpigmentation |
| Fair | Moderate distortion of the nipple or breast symmetry, moderate hyperpigmentation, or prominent skin retraction, oedema or telangiectasia |
| Poor | Marked distortion, oedema, fibrosis or severe hyperpigmentation |
| Trial | PBI/APBI dose | Fraction size (Gy) | EQD2 PBI/APBI alpha/beta = 4 | Control dose | Fraction size (Gy) | EQD2 Control alpha/beta = 4 |
|---|---|---|---|---|---|---|
| 20 Gy at surface of the applicator (attenuated to 5–7 Gy at 1 cm) (APBI) | 80 at cavity surface 12.8 at 1 cm | 80 Gy at cavity surface 12.8 Gy at 1 cm | 40–56 Gy/20–28 fractions ± 10–16 Gy boost | 2 | 40–56 Gy ± 10–16 Gy | |
| 30 Gy/5 daily fractions EBRT IMRT. 100% of the PTV was covered by 95% of the prescribed dose | 6 | 50 Gy | 50 Gy/25 fractions + 10 Gy/5 fractions boost | 2 | 50 + 10 = 60 Gy | |
| 38.5 Gy/10 fractions twice daily (with 6‐hour gap) Dose‐evaluation volume (that part of PTV within the breast) received 95–107% of prescription dose | 3.85 | 49.4 Gy | 50 Gy/25 fractions or 42.5 Gy/16 fractions ± boost (10 Gy/4–5 fractions) based on criteria such as young age or close margins, prespecified by centre | 2 or 2.65 | 50 Gy or 47.1 Gy | |
| 37.5 Gy/10 fractions twice daily (with 6‐hour gap) (APBI). PTV covered by ≥ 95% of prescribed dose, with < 105% hot spot | 3.75 | 47.48 Gy | 48 Gy/24 fractions ± 10 Gy/5 fractions boost | 2 | 48 ± 10 = 48–58 Gy | |
| 7 × 5.2 Gy HDR (APBI) or 50 Gy/25 fractions (PBI) | 5.2 or 2 | 57.5 Gy or 50 Gy | 50 Gy/25 fractions (3D‐CRT was not used) | 2 | 50 Gy | |
| 30.3 Gy/7 fractions or 32 Gy/8 fractions HDR twice daily or 50 Gy at 0.6–0.8 Gy/hour pulses (1 pulse per hour, 24 hours per day) PDR | 7–8 | 41.64–42.67 Gy | 50.0–50.4 Gy to a reference point + 10 Gy/5 fractions boost. Electron dose was prescribed to the point of maximum dose on the beam axis (Dmax), ensuring the 85% isodose encompassed the tumour bed | 1.8–2.0 | 48.72–50 + 10 = 58.72–60 Gy | |
| 21 Gy/1 fraction at 90% using 6–9 MeV | 21 | 84 Gy | 50 Gy/25 fractions + 10 Gy/5 fractions boost (using electrons) | 2.0 | 50 + 10 Gy | |
| 40 Gy/15 fractions (EBRT) | 2.72 | 45.23 | 40 Gy/15 fractions 36 Gy/15 fractions + boost 40 Gy/15 fractions | 2.72 2.4 | 45.23 38.4 + 45.23 | |
| 3D‐CRT: 3‐dimensional conformal radiotherapy; APBI: accelerated partial breast irradiation; CT: computer tomography; EBRT: external beam radiotherapy; EQD2: equivalent dose in 2 Gy fractions; Gy: Gray; HDR: high‐dose‐rate; IMRT: intensity‐modulated radiotherapy; MeV: mega electron volt; PBI: partial breast irradiation; PDR: pulsed‐dose rate; PTV: planning target volume. | ||||||
| Study | Mammography | Radiotherapy toxicity | Patient‐reported outcomes (PRO) | Cosmesis |
|---|---|---|---|---|
| At 6 months, then annually | Acute: CTCAEa Late: EORTC/RTOGb and LENT‐SOMAc | Not assessed | Harvard Cosmetic Scored | |
| Annually | LENT‐SOMAc | Not assessed | Not assessed | |
| Annually | Acute and late: EORTC/RTOGb | EORTC QLQ‐C30e QLQ‐BR23 breast cancer modulef | Harvard Cosmetic Scored | |
| Annually | Acute: nil Late: EORTC/RTOG,b LENT‐SOMA,c CTCAEa | EORTC QLQ‐C30e QLQ‐BR23 breast cancer module Body‐image scale | Clinician and nurse assessed | |
| Annually | Acute and late: NCI version 3.0 | EORTC QLQ‐C30e QLQ‐BR23 breast cancer module Body‐image scale | EORTC/RTOG Rating Systemg | |
| Baseline 6 months after RT than annually | Late: EORTC/RTOGb | Not assessed | Harvard Cosmetic Scored | |
| Annually 1–5 years, 3 yearly to 10 years | Symptomatic rib fracture and lung fibrosis Ischaemic heart disease recorded at 1, 2, 5 and 10 years' follow‐up | EORTC QLQ‐C30e QLQ‐BR23 breast cancer module Body‐image scale protocol‐specific questionsh HADS scale EuroQol EQ‐5D‐3L health status questionnaire at baseline; 6 months; 1, 2 and 5 years | Patient‐ and clinician‐assessedi Photosj | |
| At 6, 12, 18, 24 months after radiotherapy then annually for 10 years | Fat necrosis measured using Lövey scoring systemk Physician scored late toxicity Acute radiotherapy toxicity: CTCAE version 3.0a LENT‐SOMAc Late RT toxicity: EORTC/RTOGb | Breast pain and arm lymphoedema measured by CTCAE version 3.0a EORTC QLQ‐C30e and QLQ‐BR23 at baseline and during follow‐up | Harvard Cosmetic Scored Physician‐ and patient‐reported Digital photosl | |
| Annually | Acute radiotherapy toxicity: CTCAE version 4.0 Late RT toxicity: CTCAE version 4.0 | Not assessed | Physician reported | |
| CTCAE: Common Terminology Criteria for Adverse Events; EORTC: European Organisation for Research and Treatment of Cancer; EORTC QLQ‐C30: European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire; EORTC QLQ‐BR23: European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire – Breast Specific Module; EORTC/RTOG: European Organisation for Research and Treatment of Cancer/Radiation Therapy Oncology Group; HADS: Hospital Anxiety and Depression Scale; LENT‐SOMA: late effects in normal tissues – subjective objective, management and analytic; RT: radiotherapy. aTrotti 2013. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Local recurrence‐free survival Show forest plot | 8 | 13168 | (Exp[(O‐E) / V], Fixed, 95% CI) | 1.21 [1.03, 1.42] |
| 1.1.1 5 years' follow‐up | 5 | 8265 | (Exp[(O‐E) / V], Fixed, 95% CI) | 1.20 [0.99, 1.45] |
| 1.1.2 10 years' follow‐up | 3 | 4903 | (Exp[(O‐E) / V], Fixed, 95% CI) | 1.22 [0.92, 1.64] |
| 1.2 Cosmesis (participant‐reported) Show forest plot | 2 | 2775 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.08 [1.68, 2.57] |
| 1.3 Cosmesis, physician/nurse‐reported Show forest plot | 6 | 3652 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.57 [1.31, 1.87] |
| 1.4 Overall survival Show forest plot | 8 | 13175 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 0.99 [0.88, 1.12] |
| 1.5 Acute radiotherapy (RT) skin toxicity Show forest plot | 4 | 3925 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.66, 0.88] |
| 1.6 Late RT skin toxicity Show forest plot | 3 | 3465 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.27 [1.63, 3.15] |
| 1.7 Telangiectasia (late RT toxicity) Show forest plot | 2 | 3010 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.40 [3.34, 5.80] |
| 1.8 Fat necrosis Show forest plot | 4 | 3565 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.76 [1.74, 4.38] |
| 1.9 Subcutaneous fibrosis (late RT toxicity) Show forest plot | 2 | 3011 | Odds Ratio (M‐H, Fixed, 95% CI) | 5.07 [3.81, 6.74] |
| 1.10 Breast pain (late RT toxicity) Show forest plot | 2 | 3012 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.81 [1.15, 2.86] |
| 1.11 New primary tumours in ipsilateral breast, 'elsewhere primary' Show forest plot | 4 | 5144 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.82 [1.55, 5.12] |
| 1.12 Cause‐specific survival Show forest plot | 7 | 9865 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 1.06 [0.83, 1.36] |
| 1.13 Distant metastasis‐free survival Show forest plot | 7 | 11033 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 0.95 [0.80, 1.13] |
| 1.14 Relapse‐free survival Show forest plot | 6 | 11756 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 1.25 [1.05, 1.48] |
| 1.15 Locoregional recurrence‐free survival Show forest plot | 5 | 6718 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 1.36 [1.06, 1.74] |
| 1.16 Subsequent mastectomy Show forest plot | 3 | 3740 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.78, 1.23] |