Irradiación parcial de la mama versus radioterapia en toda la mama para el cáncer de mama temprano
Información
- DOI:
- https://doi.org/10.1002/14651858.CD007077.pub4Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 30 agosto 2021see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Cáncer de mama
- Copyright:
-
- Copyright © 2021 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
ML, BH and DF wrote the protocol.
BH extracted data, created 'Risk of bias' tables and 'Characteristics of included studies' table, analysed the data, wrote the results section and discussion, and responded to editorial and peer review (in consultation with ML).
ML checked the analyses, risk of bias tables, collaborated with writing the results, discussion and conclusion sections.
AS checked the extracted data and ran the search strategy.
Sources of support
Internal sources
-
Nil, Australia
Nil
External sources
-
Princess Alexandra Cancer Collaborative Group, Australia
Financial support for research assistant
-
This project is funded by the National Institute for Health Research (NIHR) Cochrane Incentive Award 2020 (NIHR 133261). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care, UK, UK
Financial support to update the review
Declarations of interest
ML: none.
BH: none.
Acknowledgements
We thank the Princess Alexandra Hospital Cancer Collaborative Group.
We acknowledge the input from Adrienne See and David Francis for their help with our search strategy and running searches.
We thank Erin Fergus for help in resolving disagreements with respect to assessment of risk of bias.
We are grateful for peer review input from:
-
Clinical Associate Professor Kirsty Stuart, Department of Radiation Oncology, Crown Princess Mary Cancer Centre, Westmead, NSW; Westmead Breast Cancer Institute, Westmead, NSW; Western Clinical School, The University of Sydney, NSW Australia.
-
Rebecca Seago‐Coyle Consumer editor of the Cochrane Breast Cancer Group.
-
Sara Whiting, National Breast Cancer Coalition (NBCC), USA.
-
A statistical reviewer who wishes to name anonymous (Australia).
Version history
| Published | Title | Stage | Authors | Version |
| 2021 Aug 30 | Partial breast irradiation versus whole breast radiotherapy for early breast cancer | Review | Brigid E Hickey, Margot Lehman | |
| 2016 Jul 18 | Partial breast irradiation for early breast cancer | Review | Brigid E Hickey, Margot Lehman, Daniel P Francis, Adrienne M See | |
| 2014 Jun 18 | Partial breast irradiation for early breast cancer | Review | Margot Lehman, Brigid E Hickey, Daniel P Francis, Adrienne M See | |
| 2008 Apr 23 | Partial breast irradiation for early breast cancer | Protocol | Margot Lehman, Brigid E Hickey, Daniel P Francis | |
Differences between protocol and review
We amended our inclusion criteria to ensure only studies using contemporary radiation techniques were eligible. Two studies that were included in the original 2008 publication were excluded (Dodwell 2005; Ribeiro 1993) from the 2016 (Hickey 2016) and 2021 updates. This was because the surgery and techniques used to define volume of breast treated and the technology used in these two studies do not reflect current radiotherapy (RT) practice.
We reported time‐to‐event data where possible for cancer‐related outcomes. We reported local relapse‐free survival (LR‐FS) rather than local relapse (LR), distant metastasis‐free survival (DM‐FS) rather than distant metastases (DM), we reported locoregional relapse‐free survival (L‐R R‐FS) rather than locoregional control (LRC) as a secondary endpoint. We added the words 'elsewhere primary' to the name of the endpoint 'new primary in ipsilateral breast' because this term is used in the relevant literature, in order to add clarity for the reader.
We initially indicated that we would convert doses to their biological equivalent (BED), but have in fact used equivalent dose in 2 Gy fractions (EQD2). This allows numerical addition of separate components of a treatment and is more readily understood by clinical radiation oncologists because it results in numbers that can be directly related to clinical experience.
We added APBI as well as PBI: modern RT techniques that reduce the treated volume allow the use of high dose per fraction to the smaller treated volume. The ongoing studies tend to use APBI, which reflects modern RT practice, making the review results more applicable.
We added blinding to assessment of risk of bias, because the lack of blinding for the primary outcome of cosmesis would be a significant cause of bias. We added an additional database (i.e. Embase) and trial registry (World Health Organization International Clinical Trials Registry Platform) to our search strategy, and also handsearched other resources. This ensured that our searches were as comprehensive as possible, and complied with Cochrane search requirements.
We included studies with women with ductal carcinoma in situ for reporting of toxicity endpoints (RAPID). ELIOT used regional nodal irradiation for those women with four or more involved nodes (5% of the cohort), we excluded ELIOT from the analysis of L‐RR‐FS.
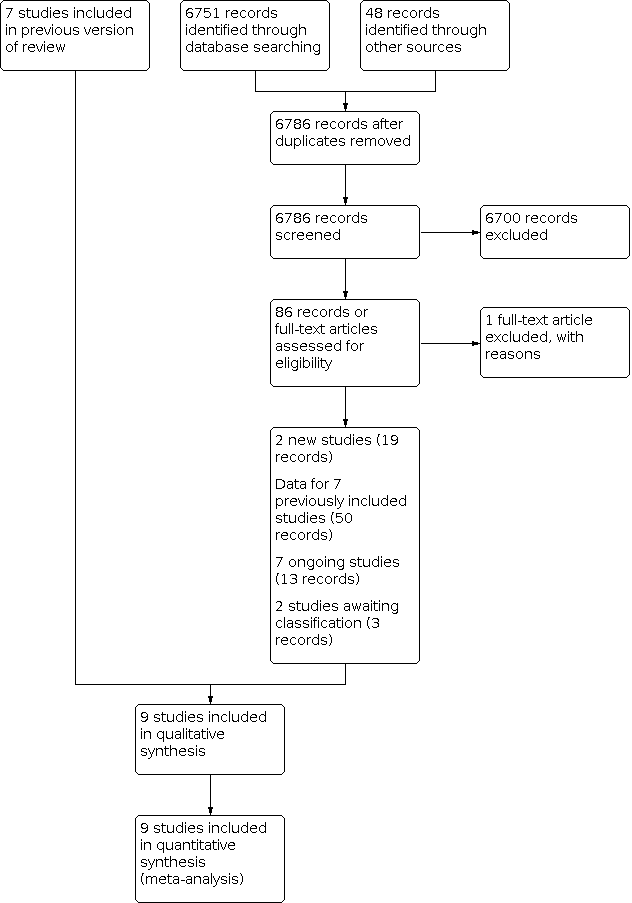
We pooled the studies in a quantitative meta‐analysis, but excluded the older studies, which used surgical, RT and systemic management practices which do not reflect current practice. We had planned sensitivity analysis based on excluding studies that used outmoded RT and surgical techniques, but as we decided to exclude them from our analysis, we did not do so. These studies were included in the previous iteration of this review, but were removed for the 2016 update.
We corrected the list and table of excluded studies so we are now compliant with MECIR guidelines, so that this list only includes studies that might reasonably be expected to be included, but which we deemed ineligible.
Current Contents were not searched separately. The conference abstracts from the International Journal of Radiation Oncology Biology Physics: proceedings of American Society for Radiation Oncology (ASTRO) and American Society of Clinical Oncology (ASCO) are now available via the Embase search.
We performed a sensitivity analysis by excluding the study at high risk of 'other bias' (TARGIT); this was a post‐hoc decision.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Female; Humans;
PICO

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: 1 Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), outcome: 1.1 Local recurrence‐free survival.

Forest plot of comparison: 1 Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), outcome: 1.3 Overall survival.

Forest plot of comparison: 1 Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), outcome: 1.8 Cause‐specific survival.

Forest plot of comparison: 1 Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), outcome: 1.9 Distant metastasis‐free survival.

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 1: Local recurrence‐free survival

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 2: Cosmesis (participant‐reported)

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 3: Cosmesis, physician/nurse‐reported

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 4: Overall survival

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 5: Acute radiotherapy (RT) skin toxicity

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 6: Late RT skin toxicity

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 7: Telangiectasia (late RT toxicity)

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 8: Fat necrosis

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 9: Subcutaneous fibrosis (late RT toxicity)

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 10: Breast pain (late RT toxicity)

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 11: New primary tumours in ipsilateral breast, 'elsewhere primary'

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 12: Cause‐specific survival

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 13: Distant metastasis‐free survival

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 14: Relapse‐free survival

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 15: Locoregional recurrence‐free survival

Comparison 1: Partial breast irradiation (PBI)/accelerated partial breast irradiation (APBI) versus whole breast radiotherapy (WBRT), Outcome 16: Subsequent mastectomy
| PBI/APBI compared to WBRT for early breast cancer | ||||||
| Patient or population: health problem or population Setting: Academic, tertiary and community practice Intervention: PBI/APBI Comparison: WBRT | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with WBRT | Risk with PBI/APBI | |||||
| Local recurrence‐free survival ‐ total (LR‐FS) | Low | HR 1.21 | 13168 | ⊕⊕⊕⊝ | ||
| 985 per 1000 | 982 per 1000 | |||||
| Cosmesis, physician/nurse‐reported | 138 per 1000 | 201 per 1000 | OR 1.57 | 3652 | ⊕⊕⊕⊝ | |
| Overall survival | Low | HR 0.99 | 13175 | ⊕⊕⊕⊕ | ||
| 949 per 1000 | 949 per 1000 | |||||
| Subcutaneous fibrosis (late RT toxicity) | 43 per 1000 | 184 per 1000 | OR 5.07 | 3011 | ⊕⊕⊕⊝ | |
| Cause‐specific survival (C‐SS) | Low | HR 1.06 | 9865 | ⊕⊕⊕⊝ | ||
| 983 per 1000 | 982 per 1000 | |||||
| Distant metastasis‐free survival (DM‐FS) | Low | HR 0.95 | 11033 | ⊕⊕⊕⊝ | ||
| 971 per 1000 | 972 per 1000 | |||||
| Subsequent mastectomy | 97 per 1000 | 95 per 1000 | OR 0.98 | 3740 | ⊕⊕⊕⊕ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| See interactive version of this table: https://gdt.gradepro.org/presentations/#/isof/isof_question_revman_web_416473753410884319. | ||||||
| a. There was considerable clinical heterogeneity with respect to radiotherapy dose, technique and use of quality assurance procedures. However, the techniques employed delivered a dose that was the same or higher in the APBI/PBI arm than the WBRT arm, which should mean the local recurrence‐free survival is better or at least the same. | ||||||
| Cosmetic score |
|---|
| Excellent |
| Good |
| Fair |
| Poor |
| RTOG CTC | Grade I | Grade II | Grade III | Grade IV |
|---|---|---|---|---|
| Acute skin | Follicular, faint or dull erythema/epilation/dry desquamation/decreased sweating | Tender or bright erythema, patchy moist desquamation/moderate oedema | Confluent, moist desquamation other than skin folds, pitting oedema | Ulceration, haemorrhage, necrosis |
| Late skin toxicity | Slight atrophy, pigmentation change, some hair loss | Patchy atrophy, moderate telangiectasia, total hair loss | Marked atrophy, gross telangiectasia | Ulceration |
| Late subcutaneous fibrosis | Slight induration, loss of subcutaneous fat | Moderate fibrosis (asymptomatic) < 10% linear field contraction | Severe induration, loss of subcutaneous tissue, linear contraction > 10% | Ulceration |
| CTCAE: Common Terminology Criteria for Adverse Events; EORTC: European Organisation for Research and Treatment of Cancer; RTOG CTC: Radiation Therapy Oncology Group Common Toxicity Criteria. | ||||
| Toxicity | Grade 1 | Grade 2 | Grade 3 | Grade 4 |
|---|---|---|---|---|
| Induration (subcutaneous fibrosis) | Increased density on palpation | Moderate increase in density, not interfering with ADL; marked increase in density and firmness on palpation with or without minimal retraction | Dysfunction interfering with ADL; very marked density, retraction or fixation | — |
| Telangiectasia | Few | Moderate | Many and confluent | — |
| Pain | Pain mild, not interfering with function | Moderate pain; pain or analgesics interfering with function, but not with ADL | Severe pain; pain or analgesics interfering with ADL | Disability |
| ADL: activities of daily living; NCI CTC: National Cancer Institute Common Toxicity Criteria. | ||||
| Adverse effect | Grade I | Grade II | Grade III | Grade IV | Grade V |
|---|---|---|---|---|---|
| Pain | Mild, not interfering with function | Moderate/analgesics, interferes with function, but not ADL | Severe or interferes with ADL, or both | — | — |
| Telangiectasia | Few | Moderate | Many or confluent, or both | — | — |
| Acute skin toxicity | Faint erythema or dry desquamation | Moderate‐to‐brisk erythema, patchy moist desquamation | Moist desquamation not limited to creases or skin folds, bleeding subsequent to minor trauma or abrasion | Skin necrosis or full dermal thickness ulceration | Death |
| Induration/fibrosis | Increased density on palpation | Moderate functional impairment, not interfering with ADL, increased density and firmness on palpation with or without minor retraction | Interferes with ADL, very marked increased density, retraction or fixation | — | — |
| ADL: activities of daily living; CTCAE: Common Terminology Criteria for Adverse Events; EORTC: European Organisation for Research and Treatment of Cancer; RTOG: Radiation Therapy Oncology Group. | |||||
| Adverse effect | Grade I | Grade II | Grade III | Grade IV | Grade V |
|---|---|---|---|---|---|
| Subcutaneous fibrosis | — | Mild induration, can move skin parallel to the plane (sliding) and perpendicular to the plane (pinching up) | Moderate induration, can slide, cannot pinch up skin | Severe induration cannot slide or pinch skin | Death |
| Telangiectasia | < 10 % of body surface area | ≥ 10% of body surface area, psychosocial impact | — | — | — |
| Pain | mild | Moderate, not limiting instrumental ADL | Severe, limiting self‐care ADL | — | — |
| ADL: activities of daily living; CTCAE: Common Terminology Criteria for Adverse Events; EORTC: European Organisation for Research and Treatment of Cancer; RTOG: Radiation Therapy Oncology Group. | |||||
| Grade | Findings |
|---|---|
| 0 | No fat necrosis |
| 1 | Asymptomatic fat necrosis (only radiological or cytological findings, or both) |
| 2 | Symptomatic fat necrosis not requiring medication (palpable mass with or without mild pain) |
| 3 | Symptomatic fat necrosis requiring medication (palpable mass with significant pain) |
| 4 | Symptomatic fat necrosis requiring surgical intervention |
| Study | Age | Stage | Margins | Tumour size | Nodal status | Surgery |
|---|---|---|---|---|---|---|
| After 2000, < 40 years excluded | Unifocal tumour, pT1N0‐1miM0, Grade I or II | Negative | < 2.0 cm (< 2 mm: 1/258, ≥ 2 mm: 246/258 or had no tumour at ink: 11/258) | — | WLE | |
| 48–75 years | "Early breast cancer," "suitable for breast conservation" | Not described | ≤ 2.5 cm | AD if SNBx positive | BCS | |
| > 40 years | — | Negative, ≥ 5 mm | ≤ 2.5 cm | — | WLE or quadrantectomy | |
| ≥ 45 years | T1 and small T2N0‐1M0 invasive breast cancer, suitable for BCS, available for 10 years' follow‐up | ≥ 1 mm Re‐excision strongly advised for close or positive margins | — | — | BCS | |
| ≥ 40 years | DCISa or invasive breast cancer | Negative | ≤ 3 cm | Negative axillary nodal involvement including micrometastasis (> 0.2 mm or positive cells only identified on IHC as determined by sentinel node biopsy; axillary node dissection or clinical examination for DCIS only. | BCS | |
| ≥ 60 years | Invasive ductal carcinoma (pT1‐2cNO MO), unifocal tumour, Grade I or II | < 3 mm | ≤ 3 cm | — | — | |
| ≥ 50 years | Invasive breast cancer pT1‐2pN0 who have < 1% annual risk of local recurrence | ≥ 2 mm | ≤ 3 cm | 0–3 nodes positive | BCS | |
| > 40 years | Stage 0, I or II pN0/pNmi breast cancer (including DCIS) no vascular invasion, unifocal or unicentric disease only, no LVINote: 60/1184 (5%) participants had DCIS | ≥ 2 mm in invasive disease, 5 mm in DCIS | Lesions < 3 cm in diameter | Node negative, for DCIS alone: sentinel node biopsy optional | WLE or quadrantectomy, level I–II axillary dissection, removing ≥ 6 (preferably 10 lymph nodes) | |
| > 18 years | T0‐2N0‐1M0 DCIS or invasive breast cancer Note: 531/4216 (12%) participants had DCIS | Negative: "free of cancer, including DCSI" | Lesions < 3 cm | ≤ 3 involved nodes permitted | Lumpectomy | |
| AD: axillary dissection; BCS: breast‐conserving surgery; DCIS: ductal carcinoma in situ; IHC: immunohistochemistry; LVI: lymphovascular invasion; SNBx: sentinel node biopsy; WLE: wide local excision. | ||||||
| Study | RT quality assurance | RT technique | PIB/APBI target volume definition |
|---|---|---|---|
| Postimplant CT scans were performed | Interstitial brachytherapy (88/128) EBRT using photons (40/128) 2‐dimensional CT‐based | PTV: excision cavity delineated by the surgical clips + 2 cm isotropic margin. For interstitial therapy: if electrons were used, 6–15 MeV were used to treat the cavity with a 2 cm margin | |
| Not stated | Intraoperative electrons 6–9 MeV | CTV: quote: "decided according to the site and size of the tumour. The energy of the electron beams was selected according to the thickness of the gland measured by a graduated needle" | |
| Not stated | EBRT (IMRT) | CTV = +1 cm isotropic margin around surgical clips PTV = CTV +10 mm isotropic margina | |
| Nob | Intraoperative kV RT 3D‐CRT for WBRT | The target volume was the tumour cavityc | |
| Yesd | EBRT (3D‐CRT) APBI: 3–5 non‐coplanar fields | CTV = tumour bed on CT (surgical clips plus a 1‐cm margin inside breast PTV = CTV +1 cm isotropic margin | |
| Not stated | EBRT (3D‐CRT) | PTV was defined by contouring the same quadrant as the primary tumor sitee | |
| Yesf | Field‐in‐field IMRT | Tumour bed, surgical clipsg recommended | |
| Yesh | HDR or PDR multicatheter brachytherapy | PBI: tumour bedi +2 cm isotropic margin | |
| Quote: "Every institution's RT facilities were quality assessed and each case of APBI was centrally reviewed for RT quality." Benchmarking performed with "dummy run" | HDR brachytherapyj APBI EBRT: 3D‐CRTk (IMRT not permitted). WBRT: 3D‐CRT (IMRT not permitted) | No RNI permitted WBRT: entire ipsilateral breast APBI: CTV = cavity = PTV | |
| Study | RT quality assurance | RT technique | Target volume definition |
| 3D‐CRT: 3‐dimensional conformal radiotherapy; APBI: accelerated partial breast irradiation; CRT: conformal radiotherapy; CT: computer tomography; CTV: clinical target volume; EBRT: external beam radiotherapy; HDR: high‐dose rate; IMRT: intensity‐modulated radiotherapy; PDR: pulsed‐dose rate; PIB: partial breast irradiation; PTV: planning target volume; RNI: regional nodal irradiation; RT: radiotherapy; WBRT: whole breast radiotherapy. aThe surgeons were requested to place clips at the borders of the surgical bed, using a minimum of four clips. CTV was drawn on a planning CT (0.3 mm slices) with a uniform 1 cm margin around the surgical clips, then a 1 cm margin added to construct the PTV. | |||
| Score | Definition |
|---|---|
| Excellent | Perfect symmetry, no visible distortion or skin changes and no visible catheter entry/exit sequelae |
| Good | Slight skin distortion, retraction or oedema, any visible telangiectasia, any visible catheter entry/exit scar or mild hyperpigmentation |
| Fair | Moderate distortion of the nipple or breast symmetry, moderate hyperpigmentation, or prominent skin retraction, oedema or telangiectasia |
| Poor | Marked distortion, oedema, fibrosis or severe hyperpigmentation |
| Trial | PBI/APBI dose | Fraction size (Gy) | EQD2 PBI/APBI alpha/beta = 4 | Control dose | Fraction size (Gy) | EQD2 Control alpha/beta = 4 |
|---|---|---|---|---|---|---|
| 20 Gy at surface of the applicator (attenuated to 5–7 Gy at 1 cm) (APBI) | 80 at cavity surface 12.8 at 1 cm | 80 Gy at cavity surface 12.8 Gy at 1 cm | 40–56 Gy/20–28 fractions ± 10–16 Gy boost | 2 | 40–56 Gy ± 10–16 Gy | |
| 30 Gy/5 daily fractions EBRT IMRT. 100% of the PTV was covered by 95% of the prescribed dose | 6 | 50 Gy | 50 Gy/25 fractions + 10 Gy/5 fractions boost | 2 | 50 + 10 = 60 Gy | |
| 38.5 Gy/10 fractions twice daily (with 6‐hour gap) Dose‐evaluation volume (that part of PTV within the breast) received 95–107% of prescription dose | 3.85 | 49.4 Gy | 50 Gy/25 fractions or 42.5 Gy/16 fractions ± boost (10 Gy/4–5 fractions) based on criteria such as young age or close margins, prespecified by centre | 2 or 2.65 | 50 Gy or 47.1 Gy | |
| 37.5 Gy/10 fractions twice daily (with 6‐hour gap) (APBI). PTV covered by ≥ 95% of prescribed dose, with < 105% hot spot | 3.75 | 47.48 Gy | 48 Gy/24 fractions ± 10 Gy/5 fractions boost | 2 | 48 ± 10 = 48–58 Gy | |
| 7 × 5.2 Gy HDR (APBI) or 50 Gy/25 fractions (PBI) | 5.2 or 2 | 57.5 Gy or 50 Gy | 50 Gy/25 fractions (3D‐CRT was not used) | 2 | 50 Gy | |
| 30.3 Gy/7 fractions or 32 Gy/8 fractions HDR twice daily or 50 Gy at 0.6–0.8 Gy/hour pulses (1 pulse per hour, 24 hours per day) PDR | 7–8 | 41.64–42.67 Gy | 50.0–50.4 Gy to a reference point + 10 Gy/5 fractions boost. Electron dose was prescribed to the point of maximum dose on the beam axis (Dmax), ensuring the 85% isodose encompassed the tumour bed | 1.8–2.0 | 48.72–50 + 10 = 58.72–60 Gy | |
| 21 Gy/1 fraction at 90% using 6–9 MeV | 21 | 84 Gy | 50 Gy/25 fractions + 10 Gy/5 fractions boost (using electrons) | 2.0 | 50 + 10 Gy | |
| 40 Gy/15 fractions (EBRT) | 2.72 | 45.23 | 40 Gy/15 fractions 36 Gy/15 fractions + boost 40 Gy/15 fractions | 2.72 2.4 | 45.23 38.4 + 45.23 | |
| 3D‐CRT: 3‐dimensional conformal radiotherapy; APBI: accelerated partial breast irradiation; CT: computer tomography; EBRT: external beam radiotherapy; EQD2: equivalent dose in 2 Gy fractions; Gy: Gray; HDR: high‐dose‐rate; IMRT: intensity‐modulated radiotherapy; MeV: mega electron volt; PBI: partial breast irradiation; PDR: pulsed‐dose rate; PTV: planning target volume. | ||||||
| Study | Mammography | Radiotherapy toxicity | Patient‐reported outcomes (PRO) | Cosmesis |
|---|---|---|---|---|
| At 6 months, then annually | Acute: CTCAEa Late: EORTC/RTOGb and LENT‐SOMAc | Not assessed | Harvard Cosmetic Scored | |
| Annually | LENT‐SOMAc | Not assessed | Not assessed | |
| Annually | Acute and late: EORTC/RTOGb | EORTC QLQ‐C30e QLQ‐BR23 breast cancer modulef | Harvard Cosmetic Scored | |
| Annually | Acute: nil Late: EORTC/RTOG,b LENT‐SOMA,c CTCAEa | EORTC QLQ‐C30e QLQ‐BR23 breast cancer module Body‐image scale | Clinician and nurse assessed | |
| Annually | Acute and late: NCI version 3.0 | EORTC QLQ‐C30e QLQ‐BR23 breast cancer module Body‐image scale | EORTC/RTOG Rating Systemg | |
| Baseline 6 months after RT than annually | Late: EORTC/RTOGb | Not assessed | Harvard Cosmetic Scored | |
| Annually 1–5 years, 3 yearly to 10 years | Symptomatic rib fracture and lung fibrosis Ischaemic heart disease recorded at 1, 2, 5 and 10 years' follow‐up | EORTC QLQ‐C30e QLQ‐BR23 breast cancer module Body‐image scale protocol‐specific questionsh HADS scale EuroQol EQ‐5D‐3L health status questionnaire at baseline; 6 months; 1, 2 and 5 years | Patient‐ and clinician‐assessedi Photosj | |
| At 6, 12, 18, 24 months after radiotherapy then annually for 10 years | Fat necrosis measured using Lövey scoring systemk Physician scored late toxicity Acute radiotherapy toxicity: CTCAE version 3.0a LENT‐SOMAc Late RT toxicity: EORTC/RTOGb | Breast pain and arm lymphoedema measured by CTCAE version 3.0a EORTC QLQ‐C30e and QLQ‐BR23 at baseline and during follow‐up | Harvard Cosmetic Scored Physician‐ and patient‐reported Digital photosl | |
| Annually | Acute radiotherapy toxicity: CTCAE version 4.0 Late RT toxicity: CTCAE version 4.0 | Not assessed | Physician reported | |
| CTCAE: Common Terminology Criteria for Adverse Events; EORTC: European Organisation for Research and Treatment of Cancer; EORTC QLQ‐C30: European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire; EORTC QLQ‐BR23: European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire – Breast Specific Module; EORTC/RTOG: European Organisation for Research and Treatment of Cancer/Radiation Therapy Oncology Group; HADS: Hospital Anxiety and Depression Scale; LENT‐SOMA: late effects in normal tissues – subjective objective, management and analytic; RT: radiotherapy. aTrotti 2013. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Local recurrence‐free survival Show forest plot | 8 | 13168 | (Exp[(O‐E) / V], Fixed, 95% CI) | 1.21 [1.03, 1.42] |
| 1.1.1 5 years' follow‐up | 5 | 8265 | (Exp[(O‐E) / V], Fixed, 95% CI) | 1.20 [0.99, 1.45] |
| 1.1.2 10 years' follow‐up | 3 | 4903 | (Exp[(O‐E) / V], Fixed, 95% CI) | 1.22 [0.92, 1.64] |
| 1.2 Cosmesis (participant‐reported) Show forest plot | 2 | 2775 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.08 [1.68, 2.57] |
| 1.3 Cosmesis, physician/nurse‐reported Show forest plot | 6 | 3652 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.57 [1.31, 1.87] |
| 1.4 Overall survival Show forest plot | 8 | 13175 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 0.99 [0.88, 1.12] |
| 1.5 Acute radiotherapy (RT) skin toxicity Show forest plot | 4 | 3925 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.66, 0.88] |
| 1.6 Late RT skin toxicity Show forest plot | 3 | 3465 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.27 [1.63, 3.15] |
| 1.7 Telangiectasia (late RT toxicity) Show forest plot | 2 | 3010 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.40 [3.34, 5.80] |
| 1.8 Fat necrosis Show forest plot | 4 | 3565 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.76 [1.74, 4.38] |
| 1.9 Subcutaneous fibrosis (late RT toxicity) Show forest plot | 2 | 3011 | Odds Ratio (M‐H, Fixed, 95% CI) | 5.07 [3.81, 6.74] |
| 1.10 Breast pain (late RT toxicity) Show forest plot | 2 | 3012 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.81 [1.15, 2.86] |
| 1.11 New primary tumours in ipsilateral breast, 'elsewhere primary' Show forest plot | 4 | 5144 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.82 [1.55, 5.12] |
| 1.12 Cause‐specific survival Show forest plot | 7 | 9865 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 1.06 [0.83, 1.36] |
| 1.13 Distant metastasis‐free survival Show forest plot | 7 | 11033 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 0.95 [0.80, 1.13] |
| 1.14 Relapse‐free survival Show forest plot | 6 | 11756 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 1.25 [1.05, 1.48] |
| 1.15 Locoregional recurrence‐free survival Show forest plot | 5 | 6718 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 1.36 [1.06, 1.74] |
| 1.16 Subsequent mastectomy Show forest plot | 3 | 3740 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.78, 1.23] |