Intervenciones con música para mejorar los resultados psicológicos y físicos en pacientes con cáncer
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en espera de evaluación
Referencias de los estudios en curso
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT Cross‐over trial | |
| Participants | Adults with documented cancer‐related pain Type of cancer: breast (n = 7, 46.5%), multiple myeloma (n = 4, 26.5%), rectal (n = 1, 6.75%), prostate (n = 1, 6.75%), sarcoma (n = 1, 6.75%), lymphoma (n = 1, 6.75%) Total N randomized: 15 Total N analyzed: 15 Mean age: 55.6 years Sex: 12 (80%) females, 3 (20%) males Ethnicity: 15 (100%) white Setting: patients' home Country: USA | |
| Interventions | 2 study groups
Music provided: the researcher asked a registered music therapist to select relaxing music in 7 categories including classical, jazz, folk, rock, country and western, easy listening and new age. Participants were asked to select from these music options. Number of sessions: 3 Length of sessions: 45 min Categorized as music medicine trial | |
| Outcomes | Mood (Visual Analogue Scale, VAS), pain (VAS): change scores | |
| Notes | Because of significant pre‐test differences, JB used data provided in Beck's dissertation to compute change scores | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Using a coin flip for a random start, assignment was alternated between the 2 groups which differed on the order of the intervention" |
| Allocation concealment (selection bias) | Low risk | Cross‐over trial; all participants received both conditions |
| Blinding of participants and personnel (performance bias) | Unclear risk | It is unclear whether personnel were blinded |
| Blinding of outcome assessment (detection bias) | Low risk | The study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | High risk | 6 dropouts (28.6%) because of hospitalisation (n = 1), deterioration (n = 2), inadequate baseline (n = 2), or withdrawal during baseline (n = 1) |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Women undergoing mastectomy Type of cancer: breast cancer Total N randomized: 30 N randomized to music group: 15 N randomized to control group: 15 N analyzed in music group: 15 N analyzed in control group: 15 Mean age: 56.63 years Sex: 30 (100%) females, 0 (0%) males Ethnicity: 24 (80%) white, 6 (20%) black Setting: inpatient Country: USA | |
| Interventions | 2 study groups
(Note: iPod case concealed the function status of the iPod to ensure blinding of medical personnel) Music selections provided: 4 h of continuous non‐repeating music in genre selected by the participant from the following genres: classical, easy listening, inspirational or new age Number of sessions: 1 Length of sessions: duration of mastectomy (music was begun after the participant received midazolam preoperatively) Categorized as music medicine | |
| Outcomes | Anxiety (Spielberger State‐Trait Anxiety Inventory ‐ State Anxiety form, STAI‐S), pain (VAS): post‐test scores Heart rate (HR), mean arterial pressure (MAP): change scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "[T]he participants were assigned by the investigator to experimental or control groups by selecting numbers from an envelope which contained papers numbered 1 to 30 (odd numbers were assigned to the experimental group and even numbers to the control group)" (p. 53). |
| Allocation concealment (selection bias) | Low risk | Not reported. We assumed that the participants were present when the lot was drawn therefore assuring allocation concealment. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Personnel were blinded. Quote: "the iPOD was placed in a carrying case which concealed the function of the player; participants were not blinded." We decided to assign 'unclear risk' because it is unlikely that the participants' knowledge of group allocation influenced their physiological responses (objective outcome measures). However, this knowledge may have influenced their reporting on subjective outcomes. |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors were blinded for HR and MAP (iPod function was concealed from medical personnel who obtained the HR and MAP data). |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No report of conflict of interest |
| Methods | RCT Cross‐over trial | |
| Participants | Adults receiving cancer treatment Type of cancer: breast (n = 6, 19.4%), head and neck (n = 3, 9.7%), gastrointestinal (n = 3, 9.7%), gynecological (n = 3, 9.7%), hematologic (n = 7, 22.6%), lung (n = 4, 12.9%), other (n = 5, 16%) Total N randomized: 39 with 5 patients lost prior to initiation of treatment Total N analyzed: 31 Age: 53.8 years Sex: 21 (67.7%) females, 10 (32.3%) males Ethnicity: 23 (74.2%) black, 1 (3.2%) Asian, 6 (19.4%) white, 1 (3.2%) other Setting: inpatient and outpatient Country: USA | |
| Interventions | 2 study conditions:
Number of sessions: 2 of each condition Length of sessions: 30‐45 min Categorized as music therapy | |
| Outcomes | Anxiety (VAS), mood (VAS), relaxation (VAS), pain (NRS): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Using a list of random numbers, participants were randomized to one of two treatment sequences consisting of two MT sessions followed by two MM sessions or vice versa" (p.1262) |
| Allocation concealment (selection bias) | Low risk | "The use of sequentially numbered, opaque, sealed envelopes ensured allocation concealment" (p.1262). |
| Blinding of participants and personnel (performance bias) | Low risk | Study participants were blinded: "We minimized expectation effects of participants throughout the study by referring to both treatment conditions as music sessions rather than referring to one intervention as music therapy" (p1263). The music therapist could not be blinded. |
| Blinding of outcome assessment (detection bias) | Low risk | No objective outcomes were included in this study. |
| Blinding of outcome assessment (detection bias) | Low risk | Self report measures were used for subjective outcomes but participants were blinded to the study hypotheses. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition rate: 13% (p.1264) |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | Study was funded by Drexel University's College of Medicine |
| Methods | Controlled clinical trial (CCT) (randomization method unclear) 2‐arm parallel group design | |
| Participants | Children with cancer who had previously undergone more than 2 painful, invasive procedures (e.g. osteomedullar biopsy, lumbar puncture) and who were scheduled to undergo a painful medical procedure Type of cancer: acute lympathic leukemia (n = 18, 47% of music group, n = 25, 65% of control group), non‐Hodgkin's lymphoma (n = 12, 32% of music group, n = 8, 20% of control group), neuroblastoma (n = 4, 11% of music group, n = 4, 10% of control group), osteosarcoma (n = 2, 5% of music group, n = 2, 5% of control group), medulloblastoma (n = 2, 5% of music group, 0% of control group) Total N randomized: unclear N analyzed in music group: 20 N analyzed in control group: 19 Mean age: 6.72 years Sex: 15 (38%) females, 24 (72%) males Ethnicity: 39 (100%) white (Italian) Setting: inpatient Country: Italy | |
| Interventions | 2 study groups:
Music selections provided: during the initial music listening phase, the following music was used: lullabies (e.g. Brahms); children's songs (Walt Disney); folk songs (Italian/non‐Italian), ethnic songs (Albania, Romania, Latin America), pop (Italian /non‐Italian), classical music (e.g. Bach), other music (Celtic music, Simon and Garfunkel, etc.). This phase was followed by active music making with the child using small percussion instruments and vocal and body percussion. Number of sessions: 1 Length of sessions: 15 min for phase 1 (music listening); length of active music making is not specified Categorized as music therapy | |
| Outcomes | Anxiety (STAI‐S): post‐test scores Induction compliance (not used in this review) | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Low risk | Music therapist and participants could not be blinded as this trial used an interactive music therapy intervention |
| Blinding of outcome assessment (detection bias) | Low risk | The study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Unclear risk | It is unclear whether number of participants analyzed equals the number of participants recruited |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
| Methods | CCT 2‐arm parallel group design | |
| Participants | Women with breast cancer waiting for adjuvant chemotherapy Type of cancer: breast (n = 60, 100%) Total N randomized: 60 N randomized to music group: 30 N randomized to control group: 30 N analyzed in music group: 30 N analyzed in control group: 30 Mean age: 50.95 years Sex: 60 (100%) females Ethnicity: 60 (100%) white (Italian) Setting: inpatient Country: Italy | |
| Interventions | 2 study groups:
Music selections provided: participants were asked to select from new age music, nature music, film soundtracks, Celtic melodies, or classical music Number of sessions: 1 Length of sessions: 15 min Categorized as music medicine | |
| Outcomes | Anxiety (STAI‐S): post‐test scores | |
| Notes | The principal investigator provided us with standard deviations as these were not given in the study report | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternate assignment using order of admission (personal communication with principal investigator) |
| Allocation concealment (selection bias) | High risk | Alternate assignment prohibited allocation concealment |
| Blinding of participants and personnel (performance bias) | Unclear risk | It is unclear whether personnel were blinded; participants were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | The study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adult patients with cancer Diagnosis: ovarian (n = 1, 13%), breast (n = 7, 87%) Total N randomized: 8 N randomized to music group: 4 N randomized to control group: 4 N analyzed in music group: 4 N analyzed in control group: 4 Mean age: 48 (SD 6.56) years Sex: 8 (100%) females Ethnicity: no information provided Setting: outpatient Country: USA | |
| Interventions | 2 study groups:
Music selections provided: Quote from study report (p. 55): "The Bonny Method of Guided Imagery and Music is an in depth music psychotherapy that utilizes specially sequenced Western Art music to elicit imagery and emotional expression." Number of sessions: 10 Length of sessions: 90‐120 min Categorized as music therapy | |
| Outcomes | Mood (Profile of Mood States, POMS): could not be included because constant of 100 was not used in total score computation by the authors Quality of Life (QoL‐Cancer Scale): change scores were computed by JB to allow for computation of pooled effect size (SMD) with other studies that reported change scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated number list (personal communication with principal investigator) |
| Allocation concealment (selection bias) | Low risk | Statisticalprogram Aleator (personal communication with principal investigator) |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding of participants and music therapist was not possible given the interactive nature of the music therapy sessions |
| Blinding of outcome assessment (detection bias) | Low risk | The study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | No subject loss |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | Study was supported by Trustees of the Paul Jenkins fund |
| Methods | CCT 2‐arm parallel group design | |
| Participants | Adults with acute leukemia Diagnosis: acute leukemia, high‐grade non‐Hodgkin's lymphoma Total N randomized: 49 N randomized to music group: 25 N randomized to control group: 24 N analyzed in music group: 15 N analyzed in control group: 15 Mean age: 54 years Sex: 30 (61%) females, 19 (39%) males Ethnicity: not provided Setting: inpatient Country: USA | |
| Interventions | 2 study groups:
Music selections provided: classical music and new age music based on patient preference was used Number of sessions: 8 Length of sessions: 45 min Categorized as music therapy | |
| Outcomes | Anxiety (STAI‐S): 4‐weeks postintervention scores Fatigue (The Functional Assessment of Chronic Illness Therapy—Fatigue scale, FACIT‐F): 4‐week post‐intervention scores Positive and negative affect (Affect and Negative Affect Schedule, PANAS): 4 week post‐intervention scores (not used in this review) | |
| Notes | Post‐test scores were not reported in this study report. Values were obtained from the principal investigator. However, she could only provide us with the 4‐week post‐intervention scores. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding of participants and music therapist was not possible given the interactive nature of the music therapy sessions |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | High risk | Attrition rate is 38.8%. There were 10 withdrawals in the experimental group, 9 in the control group for the following reasons: too sick to complete the measures or carry out the intervention (n = 6), voluntary withdrawal (n = 4), transfer to ICU (n = 4), death (n = 3), did not complete follow‐up questionnaires (n = 2). |
| Selective reporting (reporting bias) | High risk | Only feasibility data were reported. No post‐test or follow‐up scores were reported. Follow‐up scores (4 weeks post‐intervention) were received from the author. |
| Other bias | Low risk | Supported by a grant from the National Center for Complementary and Alternative Medicine 5F32AT001144‐02, and Bardett‐Kenkel award from the Walter Cancer Institute |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adolescents and young adults with cancer during stem‐cell transplantation (SCT) Diagnosis: no further diagnosis details reported Total N randomized: 12 N randomized to music group: 7 N randomized to control group: 5 N analyzed in music group: 7 N analyzed in control group: 2 Mean age: 17.5 years Sex: 5 (42%) females, 7 (58%) males (at the onset of the trial) Ethnicity: 8 (66%) white, other information not provided Setting: inpatient Country: USA | |
| Interventions | 2 study groups:
Music selections provided: music videos of 10 songs from 5 music styles including pop, rock, rap, country, and rhythm and blues Number of sessions: 6 Length of sessions: 60 min Categorized as music therapy | |
| Outcomes | Distress (McCorkle Symptom Distress Scale): post‐test scores QoL (Index of Well‐Being): post‐test scores Spiritual beliefs (Reed Spiritual Perspective Scale): change scores Hope (Herth Hope index): not included in this review Mood (Mental Health Scale of the Child Health Questionnaire), pain (Child Health Questionnaire): cannot be included because of high attrition | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated number list (personal communication with principal investigator) |
| Allocation concealment (selection bias) | Unclear risk | Central randomizations was used, but author is unsure how information was transferred to field investigators (personal communication with principal investigator) |
| Blinding of participants and personnel (performance bias) | Low risk | Music therapist could not be blinded because of the interactive nature of the music therapy sessions; participants were blinded to the purpose of the study (personal communication with principal investigator) |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | 2 participants (16.6%) were dropped from the study when they became very ill and were transferred to the intensive care unit; 1 of these 2 participants eventually died. 1 participant withdrew from the study after learning randomizations status |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | Supported by American Cancer society IRG‐84‐002‐19 |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adults who met the eligibility criteria for diagnosis of cancer receiving chemotherapy treatment Type of cancer: metastatic cancer (n = 45, 86.6%), non‐metastatic cancer (n = 7, 13.4%) Total N randomized: 52 Total N analyzed: 52 N randomized to music group: 26 N randomized to control group: 26 N analyzed in music group: 26 N analyzed in control group: 26 Mean age: 64.5 years Sex: 43 (82.7%) females, 9 (17.3%) males Ethnicity: not reported Setting: inpatient Country: Italy | |
| Interventions | 2 study groups:
Music selections provided: participant was asked to select 5 or 6 musical pieces from a playlist that included music from a wide variety of styles Number of sessions: 3 Length of sessions: 30 min Categorized as music medicine | |
| Outcomes | SBP, DBP: change score HR, oxygen saturation: post‐test scores Mood (VAS): post‐test scores Glycemia: not included in this review Pain (VAS): not included in this review. Baseline levels indicated that participants were barely experiencing pain. | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "For the randomisation sequence generation for allocation of the participants, a computer‐generated list of random numbers was used. For the randomisation type, participants were randomly assigned following simple randomisation procedures (computerized random numbers) to 1 of 2 groups" (p. 304). |
| Allocation concealment (selection bias) | Low risk | "As for the allocation concealment mechanism, the allocation sequence was concealed from the researcher enrolling and assessing participants in sequentially numbered, opaque, sealed, and stapled envelopes. Envelopes were opened only after the enrolled participants completed all baseline assessments, and it was time to allocate the intervention" (p. 304). |
| Blinding of participants and personnel (performance bias) | Low risk | Live music was used; therefore blinding was not possible |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Flow chart (p. 305) indicates 0% dropouts |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "The authors have disclosed that they have no significant relationships with, or financial interest in, any commercial companies pertaining to this article" (p. 301) |
| Methods | CCT 2‐arm parallel group design | |
| Participants | Adults with cancer receiving chemotherapy or radiation therapy Diagnosis: lung cancer (n = 25, 14%), gastric carcinoma (n = 45, 25%), intestinal carcinoma (n = 28, 15%), breast cancer (n = 84, 46%) Total N randomized: unclear N randomized to music group: unclear N randomized to control group: unclear N analyzed in music group: 128 N analyzed control group: 54 Mean age: 51 years Sex: 107 (59%) females, 75 (41%) males Ethnicity: 182 (100%) Chinese Setting: inpatient Country: China | |
| Interventions | 2 study groups:
Music selections provided: Chinese classical music Number of sessions: 30 Length of sessions: 30 min Categorized as music medicine | |
| Outcomes | Depression (Zung Self Rating Depression Scale): post‐test scores Anxiety (Zung Self Rating Anxiety Scale): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not provided in the translation of the study report |
| Allocation concealment (selection bias) | Unclear risk | Not provided in the translation of the study report |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Unclear risk | It is unclear whether number of participants analyzed equals the number of participants randomized |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adults with hematologic malignancy admitted for high dose therapy with autologous stem cell transplantation Diagnosis: Hodgkin's (n = 8, 12%), non‐Hodgkin's lymphoma (n = 31, 45%), myeloma/amyloidosis (n = 30, 43%) Total N randomized: 69 Total N analyzed: 60 N randomized to music group: 36 N randomized to control group:33 N analyzed in music group: 34 N analyzed in control group: 26 Mean age: 52 years Sex: 37 (54%) females, 32 (46%) males Ethnicity: not provided Setting: inpatient Country: USA | |
| Interventions | 2 study groups:
Music selections provided: each music therapy session was individualized according to the needs of the participant Number of sessions: the treatment group received a median of 5 sessions during a median of 10 days Length of sessions: 20‐30 min Categorized as music therapy | |
| Outcomes | Depression (POMS): post‐test scores (after 1 session) Anxiety (POMS): change scores (after 1 session) Mood (POMS total score): change scores (after 1 session) Fatigue (POMS): post‐test scores (after 1 session) | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "[R]andomized by telephone using the MSKCC clinical research database" (p. 2724) and "randomly permuted blocks with the following strata: whole body/whole lymphatic irradiation (yes/no); diagnosis (lymphoma, Hodgkin disease, myeloma/amyloidosis); and center (MSKCC/ICC)." (p. 2724). |
| Allocation concealment (selection bias) | Low risk | Quote: "[T]he use of telephone registration and randomisation ensured concealment of treatment allocation" |
| Blinding of participants and personnel (performance bias) | Low risk | Music therapist and participants could not be blinded given the interactive nature of the music therapy session |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Attrition rate = 9 (13%) Withdrew before learning allocation (n = 7); discharged before post‐test (n = 2) |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | Supported in part, by the Memorial Sloan‐Kettering Cancer Center Translational/Integrative Medicine Research Fund |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adults who are ready to receive adjuvant chemotherapy after mastectomy Diagnosis: breast cancer Total N randomized: unclear N randomized to music group: unclear N randomized to control group: unclear N analyzed in music group: 42 N analyzed in control group: 44 Mean age: not provided Sex: 86 (100%) females Ethnicity: 86 (100%) Chinese Setting: inpatient Country: China | |
| Interventions | 2 study groups:
Music selections provided: music selection was based on the patient's psychological status (excited or inhibited), but no further details are provided Number of sessions: 36 Length of sessions: 60 min Categorized as music medicine | |
| Outcomes | CD3, CD4, CD8, CD4/CD8, NK cell activity: post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Translation sheet: "Table of random numbers" |
| Allocation concealment (selection bias) | High risk | No allocation concealment was used |
| Blinding of participants and personnel (performance bias) | High risk | Personnel and participants were not blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Information regarding blinding of outcome assessors is not provided in the translation of the report |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address subjective outcomes |
| Incomplete outcome data (attrition bias) | Unclear risk | It is unclear whether number of participants analyzed equals the number of participants recruited |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
| Methods | CCT 2‐arm parallel group design | |
| Participants | Adult oncology patients Type of cancer: head and neck (n = 67, 33.5%), gynecological (n = 23, 11.5%), breast (n = 38, 19%), digestive tract (n = 37, 18.5%), lung (n = 12, 6%), prostate (n = 18, 9%) (Numbers do not add up to total N of 200 but are reported as such in the published article) Total N randomized: 200 Total N analyzed: 200 N randomized to music group: 100 N randomized to control group: 100 N analyzed in music group: 100 N analyzed in control group: 100 Mean age: 55.4 years Sex: 79 (39.5%) females, 121 (60.5%) males Ethnicity: not provided Setting: outpatient Country: Taiwan | |
| Interventions | 2 study groups:
Music selections provided: slow‐paced, soft, melodic music at low volume with consistent tempo and dynamics and an average 60‐80 beats per minute. Subjects chose their own music tracks from a selection of songs in Mandarin, Mandarin pop, traditional Taiwanese songs, Western music (country and western), and classical music (e.g. chamber music with string instruments). Number of sessions: 1 Length of sessions: 15 min Categorized as music medicine trial | |
| Outcomes | Anxiety (STAI): change scores HR, RR, SBP, DBP, oxygen saturation: change scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "The 200 patients were randomly assigned by simple random sampling (every other patient) into two groups" (p. 437) |
| Allocation concealment (selection bias) | High risk | Alternate assignment prohibited allocation concealment |
| Blinding of participants and personnel (performance bias) | High risk | Participants were blinded to the study hypothesis. Personnel were not blinded. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | "A total of 209 patients who met the inclusion criteria were enrolled. Nine of these patients withdrew at the early stage for reasons of severe clinical condition or personal reasons, and 200 patients were retained for analysis" (p. 437). Attrition rate: 4.4%. |
| Selective reporting (reporting bias) | Unclear risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adults with cancer undergoing radiation therapy Diagnosis: prostate (n = 8, 13%), breast (n = 13, 21%), lung (n = 8, 13%), head and neck (n = 14, 22%), gastrointestinal (n = 9, 14%), gynecological (n = 5, 8%), other (n = 6, 10%). Total N randomized: 63 N randomized to music group: 35 N randomized to control group: 28 Total N analyzed: 59 N analyzed in music group: 18‐28 (depending on outcome) N analyzed in control group: 14‐21 (depending on outcome) Mean age: 57.59 years Sex: 24 (38%) females, 39 (62%) males Ethnicity: 54 (86%) white, 7 (11%) black, 2 (3%) other Setting: not stated in study report Country: USA | |
| Interventions | 2 study groups:
Music selections provided: a personalized tape was created for each patient to use at any time during the course of therapy. Number of sessions: 2‐4 times per week for approximately 4‐5 weeks Length of sessions: unknown Categorized as music therapy | |
| Outcomes | Depression (Hospital Anxiety and Depression Scale, HADS): post‐test scores Fatigue (POMS): post‐test scores Pain (Numeric Rating Scale, NRS): change scores Distress (NRS): change scores | |
| Notes | No standard deviations were reported for post‐test scores in the publication. Standard deviations were obtained from the author. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomised using a minimization procedure in which the first subject is assigned to a group with a coin toss. Subsequent subjects were assigned based upon covariate (tumor site, gender and pain) and assignment of previous subjects using a computer program." (p. 251) |
| Allocation concealment (selection bias) | Low risk | Minimization procedure as described above |
| Blinding of participants and personnel (performance bias) | Low risk | The music therapist and participants could not be blinded |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Attrition rate: 8%. Participants did not meet inclusion criteria (n = 4) or did not return for radiation therapy treatment (n = 1) |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adult oncology patients Type of cancer: leukemia (n = 7, 41.2%), unspecified or other (n = 10, 58.8%) Total N randomized: 34 Total N analyzed: 17 N randomized to music group: 21 N randomized to control group: 13 N analyzed in music group: 10 N analyzed in control group: 7 Mean age: 59.8 years Sex: 9 (52.9%) females, 8 (47.1%) males Ethnicity: not reported Setting: inpatient Country: USA | |
| Interventions | 2 study groups:
Music selections provided: not reported Number of sessions: 3 Length of sessions: 15‐30 min Categorized as music therapy | |
| Outcomes | Spiritual well‐being (Functional Assessment of Chronic Illness Therapy‐Spiritual Well Being Scale, FACIT‐Sp.): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “...and after they signed the consent form, they were randomly assigned to a controlled condition or an experimental music therapy condition via a computer program” (p. 241). |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Low risk | Music therapist and participants could not be blinded. |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) | High risk | Ten participants were lost in music therapy group, seven in the control group. Attrition rate: 50%. |
| Selective reporting (reporting bias) | Unclear risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Patients with cancer undergoing bone marrow biopsy Diagnosis: hematological malignancy Total N randomized: 63 N randomized to music group: 29 N randomized to control group: 30 N analyzed in music group: 29 N analyzed in control group: 30 Mean age: 50.9 years Sex: not provided Ethnicity: 46 (78%) white, 13 (22%) black Setting: outpatient Country: USA | |
| Interventions | 2 study groups:
Music selections provided: participants selected from 8 music CDs with various types of relaxing music (classical, harp, general instrumental, nature sounds, country, gospel and jazz) Number of sessions: 1 Length of sessions: 20‐60 min Categorized as music medicine | |
| Outcomes | Anxiety (STAI‐S): post‐test scores Pain (VAS): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated number list (personal communication with principal investigator) |
| Allocation concealment (selection bias) | Low risk | Researcher was blind to randomized blocks (personal communication with principal investigator) |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Attrition rate: 6.3%. Data for 4 participants were incomplete |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No report of conflict of interest |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Children with neoplasms needing chemotherapy Diagnosis: acute lymphocytic leukemia (n = 9, 27%), osteosarcoma (n = 5, 15%), Burkitt's lymphoma (n = 2, 6%), acute myeloid leukemia (n = 2, 6%), synovial sarcoma (n = 2, 6%), Hodgkin's (n = 2, 6%), tumor in the trunk (n = 2, 6%), Wilm's tumor (n = 2, 6%), Ewings sarcoma (n = 1, 3%), brain tumor (n = 1, 3%), lymphoblastic lymphoma (n = 1, 3%), primitive neuroectodermal tumor (n = 1, 3%). Total N randomized: 33 Total N analyzed: 30 N randomized to music group: 17 N randomized to control group: 16 N analyzed in music group:15 N analyzed in control group:15 Mean age: 10.6 years Sex: 15 (50%) females, 15 (50%) males Ethnicity: not provided Setting: inpatient Country: Spain | |
| Interventions | 2 study groups:
Music selections provided: cultural and ethnic characteristics were considered in selecting songs and instruments. Number of sessions: 1 Length of sessions: 45 min Categorized as music therapy | |
| Outcomes | Mood (Patient Opinion Likert Scale, OPEL): post‐test scores Immunoglobulin A (IgA) levels: change scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Translation sheet: "Computer‐generated number list" |
| Allocation concealment (selection bias) | Low risk | Translation sheet: "Statistical program Aleator" |
| Blinding of participants and personnel (performance bias) | Low risk | The music therapist and the participants could not be blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Staff responsible for analysing IgA were likely unaware of the participants' group assignment |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective data |
| Incomplete outcome data (attrition bias) | Low risk | There were 3 dropouts (9%) (1 in control group) |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
| Methods | CCT 2‐arm parallel group design | |
| Participants | Adults with cancer receiving chemotherapy Diagnosis: no details reported Total N randomized: unclear N randomized to music group: unclear N randomized to control group: unclear N analyzed in music group: 25 N analyzed in control group: 25 Mean age: 55 years Sex: 26 (52%) females, 24 (48%) males Ethnicity: not provided Setting: outpatient Country: USA | |
| Interventions | 2 study groups:
Music selections provided: patient‐preferred music with guitar accompaniment Number of sessions: 1 Length of sessions: 20 min Categorized as music therapy | |
| Outcomes | Anxiety (VAS): post‐test scores Fatigue (VAS): post‐test scores Systolic blood pressure (SBP): post‐test scores Diastolic blood pressure (DBP): post‐test scores Heart rate: post‐test scores Fear (VAS), worry (VAS), level of comfort (VAS), level of relaxation (VAS): not used in this review | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Low risk | The music therapist and the participants were not blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Unclear risk | It is unclear whether number of participants analyzed equals the number of participants randomized |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No funding was received |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adult cancer patients recovering from a blood and marrow transplant Type of cancer: acute myelogenous leukemia (n = 3, 8.0%), acute lymphoblastic leukemia (n = 2, 5.9%), chronic lymphocytic leukemia (n = 3, 8.0%), non‐Hodgkin's lymphoma (n = 5, 14.7%), myelodysplastic syndromes (n = 2, 5.9%), multiple myeloma (n = 7, 20.6%), leukemia (not specified) (n = 6, 17.6%), lymphoma (not specified) (n = 1, 2.9%), other (n = 3, 8.0%) Total N randomized: 34 Total N analyzed: 32 N randomized to music group: 14 N randomized to control group: 20 N analyzed in music group: 12 N analyzed in control group: 20 Mean age: 53.5 Sex: 17 (55.9%) female, 15 (44.1%) male Ethnicity: Asian (n = 1, 2.9%), Latino (n = 3, 8%), white (n = 23, 67.6%), other (n = 5, 14.7%) Setting: inpatient Country: USA | |
| Interventions | 2 study groups:
Music selections provided: patient's preferred music Number of sessions: 1 Length of sessions: 30 min Categorized as music therapy | |
| Outcomes | Positive and negative affect (PANAS), pain (NRS): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomly assigned via a computer program to either the experimental group (n = 12) or wait‐list control group (n = 20)" (p. 176). |
| Allocation concealment (selection bias) | High risk | No allocation concealment used (personal communication with chief investigator) |
| Blinding of participants and personnel (performance bias) | Low risk | Music therapist and participants could not be blinded |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | "2 participants did not complete measures" (p. 177). Attrition rate:6% |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adults in bone marrow transplant unit Type of cancer: acute myelogenous leukemia (n = 2, 18.2%), acute lymphoblastic leukemia (n= 2, 18.2%), chronic lymphocytic leukemia (n = 2, 18.2%), Hodgkin's disease (n = 1, 9.1%), multiple myeloma (n = 1, 9.1%), non‐Hodgkin's lymphoma (n = 2, 18.2%), and lymphoma (n = 1, 9.1%) Total N randomized: 13 Total N analyzed: 11 N randomized to music group: 8 N randomized to control group: 5 N analyzed in music group: 7 N analyzed in control group: 4 Mean age: 49.69 Sex: n = 3 (27.3%) female, n = 8 (72.7%) male Ethnicity: white: n = 10 (90.9%), other: n = 1 (9.1%) Setting: inpatient Country: USA | |
| Interventions | 2 study groups:
Music selections provided: patient‐preferred live music Number of sessions: 3‐5 Length of sessions: 30‐45 min Categorized as music therapy | |
| Outcomes | Fatigue (Multidimensional Fatigue Inventory, MFI): change scores | |
| Notes | Means and standard errors are reported in the journal article. Standard deviations were obtained from the primary author. Because of large baseline differences between the groups, JB computed change scores and associated SDs. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The participants were randomly assigned via a computer program to either the experimental (n = 7) or wait‐list control (n = 4) groups " (p.436). |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Low risk | Music therapist and participants could not be blinded |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self‐report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Flowchart reported that 13 participants consented and randomized; 11 analyzed (p. 435). Attrition rate: 16%. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
| Methods | CCT cross‐over trial | |
| Participants | Adult patients with cancer undergoing chemotherapy Diagnosis: breast cancer (n = 10, 50%), non‐small cell lung cancer (n = 5, 25%), lymphoma (n = 2, 10%), sarcoma (n = 1, 5%), colon cancer (n = 1, 5%), tongue cancer (n = 1, 5%). Total N randomized: 20 Total N analyzed: 10 Mean age: 55.6 years Sex: 16 (80%) females, 4 (20%) males Ethnicity: 9 (45%) white, 1 (5%) black, 1 (5%) Latino, 9 (45%) Asian Setting: outpatient Country: USA | |
| Interventions | 2 study groups:
Music selections provided: new age music Number of sessions: 3 BMGIM sessions and 3 imagery‐only sessions Length of sessions: 60‐90 min Categorized as music therapy | |
| Outcomes | Heart rate: post‐test scores Nausea and emesis (no standard deviations (SD) reported): not included in this review | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Low risk | Cross‐over trial; all patients received both sessions. |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding of participants and music therapist was not possible given the interactive nature of the music therapy sessions |
| Blinding of outcome assessment (detection bias) | High risk | Outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | High risk | Attrition rate: 50% 1 patient was excluded from the analysis because she only completed 4 sessions. Principal investigator mentions other reasons for withdrawal but does not provide specific numbers |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Women with metastatic breast cancer Diagnosis: metastatic breast cancer (stage IV) Total N randomized: 70 N randomized to music group: 35 N randomized to control group: 35 N analyzed in music group: 20 N analyzed in control group: 22 Mean age: 51.5 years Sex: 70 (100%) females, 0 males Ethnicity: 58 (83%) white, 7 (10%) black, 1 (2%) Latino Setting: outpatient Country: USA | |
| Interventions | 2 study groups:
Music provided: live music based on participant's preferences and needs Number of sessions: 3 Length of sessions: 45 min Categorized as music therapy | |
| Outcomes | Depression (HADS): post‐test scores Anxiety (HADS): post‐test scores Physical well‐being (the Functional Assessment of Cancer Therapy‐General, FACT‐G Physical Wellbeing Subscale): post‐test scores QoL (FACT‐G): post‐test scores Spirituality (Functional Assessment of Chronic Illness Therapy‐Spiritual Well‐being Scale, FACIT‐Sp): change scores | |
| Notes | The 3 music sessions were spread over 15 weeks. Music therapy treatment is usually offered on a weekly or biweekly basis with this population. The author reported that it was not feasible to have patients come to the clinic each week and that because of this spread, the intervention was highly diluted. Therefore, the data of this study are not included in the meta‐analysis of this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Computer‐generated random numbers determined the assignment of numbered folders to control or experimental conditions" (p. 117). |
| Allocation concealment (selection bias) | Low risk | Quote: "the participants opened the sealed envelope to reveal group assignment to either the experimental/music therapy intervention or control/usual care condition" (p. 117) |
| Blinding of participants and personnel (performance bias) | Low risk | The music therapist and the participants could not be blinded |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | High risk | Attrition rate: n = 28 or 40%. Music therapy group participants cancelled; before initiation of the study (too busy, n = 5); from baseline to first follow‐up (too busy, n = 2; no interest, n = 2; moved, n = 1; health limits, n = 1; lost, n = 1); and from first to second follow‐up (health limits, n = 1; died, n = 1; lost, n = 1). Control group participants cancelled before the initiation of the study (too busy, n = 2; died, n = 2); from baseline to first follow‐up (not interested, n = 1; moved, n = 1; died, n = 2); and from first to second follow‐up (died, n = 2; lost, n = 3) |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | High risk | The 3 music sessions were spread over 15 weeks. Music therapy treatment is usually offered on a weekly or biweekly basis with this population. The author reported that it was not feasible to have patients come to the clinic each week. No report of conflict of interest |
| Methods | RCT 4‐arm parallel group design | |
| Participants | Adults with cancer undergoing chemotherapy Diagnosis: breast (n = 13, 32.5%), colon (n = 12, 30%), ovarian (n = 7, 17.5%), lung (n = 7, 17.5%), prostate (n = 1, 2.5%) Total N randomized: 40 N randomized to music‐only group: 10 N randomized to problem‐focused visualization group: 10 (not included in this review) N randomized to emotion‐focused visualization group: 10 (not included in this review) N randomized to control group: 10 N analyzed in music group: 10 N analyzed in control group: 10 N analyzed in problem‐focused visualization: 10 (not included in this review) N analyzed in emotion‐focused visualization: 10 (not included in this review) Mean age: 52 years Sex: 33 (83%) females, 7 (17%) males Ethnicity: 32 (80%) white, 4 (10%) black, 4 (10%) Latino Setting: outpatient Country: USA | |
| Interventions | 2 study groups:
Music selections provided: new age music, namely Health Journeys: Cancer Image Path Number of sessions: 1 Length of sessions: 30 min Categorized as music medicine | |
| Outcomes | Anxiety (STAI‐S): change scores Anxiety (Beck Anxiety Inventory, BAI): not used in this review Coping (Coping Orientations to Problems Experienced, COPE): not used in this review Heart rate, SBP, DBP: change scores White blood cell count (WBC), red blood cell count (RBC), absolute neutrophil count (ANC): not used in this review; only measured at intake and at 6 weeks follow‐up while only 1 music session was used | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A table of random numbers was used to assign each participant number to a condition" (personal communication with principal investigator) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Personnel and participants were not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Outcome assessors for WBC, RBC, and ANC were blinded. Outcome assessor for HR, SBP, and DBP was not blinded (personal communication with principal investigator). |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | No subject loss in music group or control group |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | — |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adults with terminal cancer Diagnosis: cancer of lung (n = 27, 33.75%), colon (n = 7, 8.75%), kidney (n = 3, 3.75%), nasopharynx (n = 1, 1.25%), prostate (n = 1, 1.25%), liver (n = 2, 2.5%), esophogeal (n = 3, 3.75%), breast (n = 5, 6.25%), pancreas (n = 5, 6.25%), brain (n = 5, 3.75%), oral cavity (n = 1, 1.25%), ovary (n = 2, 2.5%), stomach (n = 2, 2.5%), endometrium (n = 1, 1.25%), sinus (n = 1, 1.25%), larynx (n = 1, 1.25%), leukemia (n = 2, 2.5%), melanoma (n = 2, 2.5%), multiple myeloma (n = 3, 3.75%), lymphoma (n = 1, 1.25%), head, neck and face (n = 1, 1.25%) and unspecified cancer (n = 3, 3.75%) Total N randomized: unclear N randomized to music group: unclear N randomized to control group: unclear N analyzed in music group: 40 N analyzed in control group: 40 Mean age: 65.5 years Sex: 40 (50%) females, 40 (50%) males Ethnicity: 60 (75%) white, 20 (25%) black Setting: home hospice care Country: USA | |
| Interventions | 2 study groups:
Music provided: music therapy interventions were selected based on the participant's in‐the‐moment needs Number of sessions: 2 to 13. Sessions were offered weekly or bi‐weekly until the patient died. Length of sessions: unknown Categorized as music therapy | |
| Outcomes | QoL (Hospice QoL Index‐Revised): change scores were computed by JB to allow for computation of pooled effect size (SMD) with other studies that reported change scores Physical status (Palliative Performance Scale): post‐test scores Length of life (in days) | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: " A computer generated number list was used for randomisation" (personal communication with principal investigator) |
| Allocation concealment (selection bias) | Low risk | Quote: "Researcher and assistant did not know what treatment patient was assigned to until after consent was completed" (personal communication with principal investigator) |
| Blinding of participants and personnel (performance bias) | Low risk | The music therapists and participants could not be blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors were not blinded, but it is unlikely that the report of length of life (in days) would have been biased |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Unclear risk | Quote: "When participants were lost due to death before they had completed 2 sessions, additional participants were recruited until a complete data set of 80 participants was obtained" (personal communication with principal investigator) |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No report of conflict of interest |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adult cancer patients with pain Diagnosis of sample included in final analysis (n = 126): cancer of head or neck (n = 51, 41%), gastrointestinal (n = 25, 20%), hematological (n = 16, 13%), genitourinary (n = 15, 12%), lung (n = 7, 6%), bone (n = 1, 1%), other (n = 11, 9%) Total N randomized: 129 N randomized to music group: 65 N randomized to control group: 64 N analyzed in music group: 62 N analyzed in control group: 64 Mean age: 54 years Sex: 38 (30%) females, 88 (70%) males Ethnicity: 129 (100%) Taiwanese Setting: inpatient Country: Taiwan | |
| Interventions | 2 study groups:
Music provided: music was sedative (60‐80 beats) without lyrics, with a sustained melody quality, and controlled volume and pitch. Participants were asked to select from 4 audiotapes: 2 with Taiwanese music (Taiwanese folk songs and Buddhist music) and 2 with American music (harp music and piano music). Number of sessions:1 Length of sessions: 30 min Categorized as music medicine | |
| Outcomes | Pain (VAS): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A computerized minimization program was used to randomise and conceal the allocation until after assignment and to stratify the groups on hospital unit" (p.2) |
| Allocation concealment (selection bias) | Low risk | Quote: "A computerized minimization program was used to randomise and conceal the allocation until after assignment and to stratify the groups on hospital unit" (p.2 |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Attrition rate: 2.4%. Inability to focus on the music (n = 1), did not complete music protocol because of interruptions (n = 2). |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No report of conflict of interest |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adults with primary liver cancer Type of cancer: liver (n = 102, 100%) Total N randomized: 102 N randomized to music group: 50 N randomized to control group: 52 N analyzed in music group: 50 N analyzed in control group: 52 Mean age: 56.7 Sex: not reported Ethnicity: 100% Chinese Setting: inpatient Country: China | |
| Interventions | 2 study groups:
Music selections provided: This study used the Gaotian‐Music relaxation series, which is recorded by the Center of Music Therapy and published by the people's Liberation Army Health Audio Video Publishing House. The participants could choose any music they liked from the following 4 CDs: The Sea Reverie, Mountain Language, The Stream Chant, Grassland Meditation Number of sessions: 1 Length of sessions: for duration of surgery Categorized as music medicine | |
| Outcomes | HR, RR, SBP, DBP: post‐test scores Anxiety (STAI): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Translation sheet: Table of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Translation sheet: not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective data |
| Incomplete outcome data (attrition bias) | Low risk | No subject loss |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
| Methods | RCT 3‐arm parallel group design | |
| Participants | Adults with cancer having noxious medical procedures such as tissue biopsy or port placement or removal Diagnosis of sample that was included in final analysis (n = 58): breast cancer (n = 17, 29%), lymphoma (n = 17, 29%), leukemia (n = 9, 16%), colorectal cancer (n = 3, 5%), other (n = 12, 21%). Total N randomized: 60 N randomized to music group: 24 N randomized to audiobook group: 15 N randomized to control group: 21 N analyzed in music group: 24 N analyzed in audiobook group: 14 (not included in this review) N analyzed in control group: 20 Mean age: 53.28 years Sex: 40 (69%) females, 18 (31%) males Ethnicity: 60 (100%) white Setting: inpatient Country: USA | |
| Interventions | 2 study groups:
Music selections provided: participants selected preferred music from a variety of music styles offered by the researcher and listened to music through headphones Number of sessions: 1 Length of sessions: duration of procedure Categorized as music medicine | |
| Outcomes | Anxiety (STAI‐S): post‐test scores Pain (NRS): post‐test scores Sense of control: not included in this review | |
| Notes | Author's comment: "Patients may not want to be distracted or inattentive during the medical procedure as they may have felt the need to monitor what was happening. Some patients specifically commented that the music or book tape made it impossible for them to hear or focus on the surgeon" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated number list (personal communication with principal investigator) |
| Allocation concealment (selection bias) | Low risk | Opaque sealed envelopes (personal communication with principal investigator) |
| Blinding of participants and personnel (performance bias) | High risk | Personnel and participants were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Attrition rate: n = 2 (3%). 1 participant was excluded because he was randomized to the audiobook group but requested music; 1 from the control group was excluded because the surgeon requested that music be played. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | This work was funded by a 2001 grant from the Univeristy of Iowa, Central Investment Fund for Research Enhancement |
| Methods | CCT 2‐arm parallel group design | |
| Participants | Adults with gastric cancer awaiting surgery Diagnosis: stage II and III gastric cancer Total N randomized: unclear N randomized to music group: unclear N randomized to control group: unclear N analyzed in music group: 30 N analyzed in control group: 30 Mean age: 68.5 years Sex: 23 (38%) females, 37 (62%) males Ethnicity: 60 (100%) Chinese Setting: inpatient Country: China | |
| Interventions | 2 study groups:
Music selections provided: Chinese classical music (6 different compositions) (no further detailed provided) Number of sessions: 2 sessions/day for 4 days pre‐operatively, totaling 8 sessions Length of sessions: 20‐30 min Categorized as music medicine | |
| Outcomes | Anxiety (Zung State Anxiety Scale, SAS): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not provided in translation of study report |
| Allocation concealment (selection bias) | Unclear risk | Not provided in translation of study report |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not provided in translation of study report |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Unclear risk | It is unclear whether number of participants analyzed equals the number of participants recruited |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adult patients with breast cancer after radical mastectomy Type of cancer: breast (n = 120, 100%) Total N randomized: 120 N randomized to music group: 60 N randomized to control group: 60 N analyzed in music group: 60 at 1st post‐test; 54 at 3rd post‐test N analyzed in control group: 60 at 1st post‐test; 51 at 3rd post‐test Mean age: 42 years Sex: 120 (100%) female Ethnicity: not reported Setting: inpatient Country: China | |
| Interventions | 2 study groups:
Music selections provided: patients selected their preferred music and controlled the music volume Number of sessions: twice daily Length of sessions: 30 min Categorized as music medicine trial | |
| Outcomes | Anxiety (STAI): post‐test score Pain (Short‐Form of McGill Pain Questionnaire ‐ Chinese version): post‐test score Depression (Zung Self rating Depression Scale): change score (computed by JB) Length of hospital stay (days) | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The randomisation procedure was performed with 120 random numbers produced by a computer program and all patients were randomly allocated to two groups: an experimental group (n = 60) and a control group (n = 60)" (p. 1178). |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel were not blinded. "Because of the specificity of the study, no blinding was used" (p. 1147) |
| Blinding of outcome assessment (detection bias) | High risk | "Because of the specificity of the study, no blinding was used" (p. 1147) |
| Blinding of outcome assessment (detection bias) | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | "None of the participants in the experimental and control groups was lost at the first post‐test. Fifty‐four participants remained in the experimental group (six participants lost) and 51 participants remained in the control group (nine participants lost) at the second and third post‐tests, respectively. A total of 15 patients (12.5%) were lost to follow‐up" (p. 1150). |
| Selective reporting (reporting bias) | Low risk | The reporting of outcomes was divided over three publications but there is no indications that some outcomes may have not been reported |
| Other bias | Low risk | No conflict of interest reported |
| Methods | RCT 3‐arm parallel group design | |
| Participants | Advanced tumor node metastasis cancer patients Type of cancer: tumor node metastasis Total N randomized: 160 N randomized to Chinese Medicine (CM) 5‐element music group: 66 N randomized to Western music group: 63 (not included in this review) N randomized to control group: 31 N analyzed in Chinese Medicine (CM) 5‐element music group: 57 N analyzed in Western music group: 58 (not included in this review) N analyzed in control group: 31 Mean age: 63.1 years Sex: 83 (51.9%) female, 77 (48.1%) male Ethnicity: not reported although likely that the majority of the participants were Chinese Setting: inpatient Country: China | |
| Interventions | 3 study groups:
Music selections provided: participants in the CM 5‐element music group were offered CM 5‐element music composed by Prof Shi Feng Number of sessions: 1 session/day for 5 days/week for a total duration of 3 weeks Length of sessions: 30 min Categorized as music medicine | |
| Outcomes | Quality of life (Hospice Quality of Life Index‐Revised (HQLI‐R)) and physical functioning (KPS): change scores | |
| Notes | Change scores were computed by JB because of significant baseline differences between the groups | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "SAS 9.2 statistical software was used to generate random sequence numbers based on the 2:2:1 ratio" (p. 737) |
| Allocation concealment (selection bias) | Low risk | "The random allocation scheme was put into a brown envelope. When a patient accorded with the inclusion criteria, implementers opened the envelope to obtain the subject's random allocation" (p. 737). "The randomized scheme was sealed in an opaque envelope" (p. 737‐738). |
| Blinding of participants and personnel (performance bias) | High risk | "A single‐blind design was adopted in the trial, that is, the subject remained blinded, while the researcher knew the intervention program" (p. 738). However, participants knew whether they were listening to music or not thus participants in the control group were not blinded. |
| Blinding of outcome assessment (detection bias) | Low risk | No objective measures were included |
| Blinding of outcome assessment (detection bias) | High risk | "A single‐blind design was adopted in the trial, that is, the subject remained blinded, while the researcher knew the intervention program" (p. 738).However, participants knew whether they were listening to music or not thus participants in the control group were not blinded. |
| Incomplete outcome data (attrition bias) | Low risk | "Fourteen patients dropped out of the study. 7 patients dropped out because of aggravation to the disease condition. 7 patients withdrew voluntarily during the study" (p. 738). Attrition rate: 8.75% |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | Study was supported by the project of the Chinese geriatric oncology society of the "eleventh‐5 year: plan of ministry of civil affairs" (no 2008‐47‐2‐45). |
| Methods | RCT 3‐arm parallel group design | |
| Participants | Adult cancer patients receiving chemotherapy Type of cancer: lung (n = 14, 14.3%), breast (n = 40, 40.8%), other (n = 44, 44.9%) Total N randomized: 123 N randomized to music group: not reported N randomized to the verbal relaxation group: not reported N randomized to control group:not reported N analyzed in music group: 34 N analyzed in the verbal relaxation group: 30 (not used in this review) N analyzed in control group: 34 Mean age: 53 years Sex: 65 (66.3%) female, 33 (33.7%) male Ethnicity: not reported Setting: outpatient Country: Taiwan | |
| Interventions | 3 study groups:
Music selections provided: during the preparation period, participants listened to Songs of the Pacific ('Ambient Moods‐Whale Song') including the sound of sea waves, seabirds and whales. During the deep relaxation period, a meditation‐relaxation with taped recorded verbal instructions guides the patient. In the deep relaxation period, light music,Forest Piano with sounds of nature, such as wind, birds and piano were played. In the music listening period, Violin Rain and Aroma Lavender were played. Number of sessions: 1 Length of sessions: 60 min Categorized as music medicine. Although the authors write that the intervention used GIM, a music therapy intervention, the explanations provided indicate that participants listened through a pre‐recorded tape with verbal instructions rather than the intervention being implemented by a trained music therapist. | |
| Outcomes | Anxiety (C‐STAI): post‐test scores Skin temperature and behavioural state: no means and SDs reported, therefore not included in this review | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "To maintain good balance, a permuted block randomisation was used to randomise patients who met the inclusion criteria into experimental, comparison or control group. A random number sequence is generated. Each possible permuted block is assigned a number. Using each number in the random number sequence in turn selected the next block, determining the next participant allocations. The six block design contained equal proportions in each group with randomisation to remove sequence bias" (p. 991). |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | "Head phones were then applied for the intervention and comparison groups" (p. 992). Appears that personnel may have been blinded but this was not clearly reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | High risk | "Equipment malfunction occurring in 12 subjects resulted in incomplete data. Thirteen subjects withdrew during the study owing to complaints of music preference or personal needs (e.g. toileting). Ninety‐eight subjects provided data for analysis" (pp. 992‐993). Attrition rate: 20.3% |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
| Methods | RCT 3‐arm parallel group design | |
| Participants | Adults diagnosed with breast cancer Type of cancer: breast cancer Total N randomized: 99 N randomized to Nevasic audio group: 34 N randomized to music group: 32 N randomized to control group: 33 N analyzed in Nevasic audio group: 34 (not used in this review) N analyzed in music group: 32 N analyzed in control group: 33 Mean age: 49.6 years Sex: n = 99 (100%) females Ethnicity: not reported Setting: inpatient Country: Iran | |
| Interventions | 3 study groups:
Music selections provided: pre‐selected music via CD player with headphones Number of sessions: Participant daily self administered music listening Length of sessions: not reported Categorized as music medicine | |
| Outcomes | Mood (EORTC), QoL (EORTC ‐ Global Health Status), fatigue (EORTC), nausea (EORTC), pain (EORTC), physical functioning (EORTC): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The participants were randomly assigned to one of the three treatment groups using a list (generated by nQuery Advisor program), done by a statistician who was independent of this study” (p. 283). |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) | Low risk | No objective measures were included |
| Blinding of outcome assessment (detection bias) | High risk | Self‐report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | High risk | Intention to treat analysis was used. However, by day 5, there was loss to follow‐up for 30 participants representing an attrition rate of 30%. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Unclear risk | "The authors declare no conflicts of interest." "This work was supported in part by funding from the Cancer Experiences Collaborative (CECo), a Research Collaborative funded by the National Cancer Research Institute in the UK; and Mashhad University of Medical Sciences in Iran. We are grateful to DAVAL Ltd, UK for providing us with Nevasic CDs and CD players free of charge for the purposes of this study" (p. 290). |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Children with cancer undergoing lumbar puncture (LP) Diagnosis: leukemia Total N randomized: 40 N randomized to music group: 20 N randomized to control group:20 N analyzed in music group: 20 N analyzed in control group: 20 Mean age: 9.1 years Sex: 15 (38%) females, 25 (62%) males Ethnicity: 40 (100%) Vietnamese Setting: inpatient Country: Vietnam | |
| Interventions | 2 study groups:
Music selections provided: traditional Vietnamese songs and children's songs Number of sessions: 1 Length of sessions: music started 10 min before LP and continued for the length of the procedure. Duration of the procedure was on average 23 min Categorized as music medicine | |
| Outcomes | Anxiety (STAI‐S): post‐test scores Pain (NRS): post‐test scores Heart rate, respiratory rate, oxygen saturation level, SBP and DBP: post‐test scores | |
| Notes | Measurements for these outcomes were also obtained during the procedure and are reported in the study report | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was carried out using opaque envelopes, half of which contained a paper that said 'music' and half a paper that said 'no music' (p. 147) |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization was carried out using opaque envelopes, half of which contained a paper that said "music" and half a paper that said "no music." (p. 147) |
| Blinding of participants and personnel (performance bias) | Low risk | Personnel were blinded. Quote: "The researcher and the physician did not know to which group the patient belonged" (p. 148). Participants were not blinded since they knew whether they were listening to music or not. However, it is unlikely that this influenced their physiological responses. |
| Blinding of outcome assessment (detection bias) | Low risk | Blinding was used for objective outcomes. Quote: "The researcher and the physician did not know to which group the patient belonged. Heart rate (HR), blood pressure (BP), and oxygen saturation (SpO2) were recorded, and the respiratory rate (RR) was measured manually by the researcher" (p. 148). |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | The flowchart indicates no subject loss |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | The authors declared no conflicts of interest with respect to the authorship or publication of this article. The authors received no financial support for the research or authorship of this article. |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adult cancer patients during initial radiotherapy treatment Type of cancer: prostate (n = 42, 42%), cervix (n = 10, 10%), endometrium (n = 9, 9%), breast (n = 7, 7%), lung (n = 5, 5%), other (n = 27, 27%) Total N randomized: 100 N randomized to music group: 50 N randomized to control group: 50 N analyzed in music group: 48 N analyzed in control group: 49 Mean age: 52.5 years Sex: 41 (41%) female, 59 (59%) male Ethnicity: not reported Setting: outpatient Country: Australia | |
| Interventions | 2 study groups:
Music selections provided: participants were asked to bring their own preferred music to the first radiotherapy session Number of sessions: 1 Length of sessions: duration of the radiotherapy treatment Categorized as music medicine | |
| Outcomes | Anxiety (STAI): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "After obtaining informed consent from participants at radiotherapy planning stage, 100 participants were randomized into control (standard radiotherapy; no music) or intervention (standard radiotherapy plus self selected music) arms balanced by gender using a computer‐generated minimisation technique" (p. 474). |
| Allocation concealment (selection bias) | Low risk | Use of computer‐generated minimization technique |
| Blinding of participants and personnel (performance bias) | High risk | "The triangulation mixed method convergence model design comprised a single centre, non‐blinded parallel group, randomized controlled trial" (p. 474). |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | "One control group and two music group participants withdrew prior to initial radiotherapy" (p. 474). Attrition rate = 3% |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "Conflict of interest: The authors have no financial disclosures" (p. 473). |
| Methods | RCT 3‐arm parallel group design | |
| Participants | Female cancer patients Type of cancer: breast cancer Total N randomized: 207 N randomized to live music group: 69 N randomized to recorded music group: 70 N randomized to control group: 68 N analyzed in live music group: 68 N analyzed in recorded music group: 68 N analyzed in control group: 65 Mean age: 59.4 years Sex: 207 (100%) females Ethnicity: 150 (74.6%) white, 46 (22.9%) black, 3 (1.5%) Asian, 2 (1%) Latino Setting: inpatient Country: USA | |
| Interventions | 3 study groups:
Music selections provided: patient‐preferred music Number of sessions: 1 Length of sessions: 5 min Catogorized as: music therapy | |
| Outcomes | Anesthesia requirements: the amount of propofol needed to reach sedation of Bispectral Index (BIS) score of 70 Anxiety (Global Anxiety‐VAS): change scores Recovery time: recorded as the interval between surgery end time and the time when the patient had met discharge criteria according to hospital policy and procedure, determined by the recovery nurse. Patient satisfaction: measured with a 5‐item questionnaire administered to participants orally by a staff member before discharge, with use of a Likert scale. The questions were constructed from points on the Consumer Assessment of Health Providers and Systems (CAHPS) Surgical Care Survey. | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomly assigned at a 1:1:1 ratio to a control or one of two experimental groups with use of an online randomisation module, which ensured adequate concealment" (p. 3163). |
| Allocation concealment (selection bias) | Low risk | "Participants were randomly assigned at a 1:1:1 ratio to a control or one of two experimental groups with use of an online randomisation module, which ensured adequate concealment" (p. 3163). "A permuted block randomisation scheme was used with random block sizes to prevent personnel from guessing the next assignment" (p. 3163). |
| Blinding of participants and personnel (performance bias) | Low risk | Music therapist and participants could not be blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Intention‐to‐treat analysis was used for all analyses. 137 patients were randomized to the live music or the SC group; 133 completed all measurements. This represents a dropout rate of 3%. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "Supported by Grant No. J0251, from The Kulas Foundation. Assistance with REDCap was provided through Clinical and Translational Science Collaborative Grant No. UL1TR 000439 at Case Western Reserve University. The Kulas Foundation had no role in the design or conduct of the study; the collection, management, analysis, or interpretation of the data; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication." |
| Methods | CCT 2‐arm parallel group design | |
| Participants | Adult breast cancer patients after surgery Type of cancer: breast Total N randomized: 29 N randomized to music group: 15 N randomized to control group: 14 N analyzed in music group: 15 N analyzed in control group: 14 Mean age: 58 years Sex: 29 (100%) female Ethnicity: Brazilians (n = 29, 100%) Setting: inpatient Country: Brazil | |
| Interventions | 2 study groups:
Music selections provided: recording of The Four Seasons by Vivaldi Number of sessions: 2 Length of sessions: 20‐40 min Categorized as music medicine trial | |
| Outcomes | Anxiety (STAI), temperature, blood pressure, heart rate, respiratory rate: only means are reported. Since no SDs are reported, we were not able to include this study in the meta‐analysis. | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | [translation] Patients whose hospital records ending with even numbers were grouped in the experimental group. |
| Allocation concealment (selection bias) | High risk | Allocation concealment was not possible because of systematic method of group allocation. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) | High risk | No blinding was used. |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not include subjective outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | There were no withdrawals. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting. |
| Other bias | Low risk | No conflict of interest reported. |
| Methods | CCT 3‐arm parallel group design | |
| Participants | Adult cancer patients who have undergone hematopoietic stem cell transplant Type of cancer: leukemia (n = 57, 63.3%), lymphoma (n = 13, 14.4%), other (n = 20, 22.2%) Total N randomized: 90 N randomized to music therapy group: 29 N randomized to unstructured music group: 30 (not used in this review) N randomized to control group: 31 N analyzed in music therapy group: 29 N analyzed in unstructured music group: 30 (not used in this review) N analyzed in control group: 31 Mean age: 44.3 years Sex: 47 (52%) female, 43 (48%) male Ethnicity: 59 (65.5%) white, 7 (7.8%) African‐American, 11 (12.2%) Latino, 4 (4.4%) Asian, 9 (10%) other Setting: outpatient or inpatient in transition to outpatient setting. Country: USA | |
| Interventions | 3 study groups:
Music selections provided: patient‐preferred music selected from a researcher provided database Number of sessions: 4 Length of sessions: 50 min Categorized as music therapy trial | |
| Outcomes | Mood (POMS‐Short Form): change score (computed by JB) Quality of Life (FACIT‐G and FACIT‐BMT): change scores Cancer‐related symptoms (MD Anderson Symptom Inventory): not included in meta‐analysis | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomly assigned to one of three groups: (1) ISO‐principle music therapy (MT) group, (2) unstructured music (UM) group, and (3) usual care (UC) control group" (p. 2). |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding of music therapist and participants was not possible. |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not include objective outcomes. |
| Blinding of outcome assessment (detection bias) | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) | High risk | At the 1 week follow‐up, there was 8.4% attrition. At the 4 week follow‐up, there was 27% attrition (additional data received from Dr. Lorenzo) |
| Selective reporting (reporting bias) | High risk | "...blood samples were drown but results will be reported in future manuscript." (p. 3). |
| Other bias | Low risk | "This research was funded in part by a grant from The Maurice Amado Foundation, by Cancer Center Support Grant CA016672 from the National Institutes of Health, and by a cancer prevention fellowship for Chelsea Ratcliff supported by the National Cancer Institute Grant R25T CA057730, Shine Chang, Ph.D., Principal Investigator" (p. 8). |
| Methods | CCT 3‐arm parallel group design | |
| Participants | Children with cancer Diagnosis: no further details provided Total N randomized: 83 N randomized to active music engagement group: 27 N randomized to music listening group: 28 (not included in this review) N randomized to control group: 28 N analyzed in active music engagement group: 27 N analyzed in music listening group: 28 (not included in this review) N analyzed in audiobook control group: 28 Mean age: not reported Sex: not reported Ethnicity: not reported Setting: inpatient Country: USA | |
| Interventions | 2 study groups:
Music selections provided: children's songs Number of sessions: 1 Length of sessions: 30 min Categorized as music therapy | |
| Outcomes | Positive affect (behavioral form): post‐test scores Active engagement (behavioral form): post‐test scores Initiation (behavioral form): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "[P]articipants were not allocated to the research conditions at random, but were sequentially assigned to one of three study conditions" (Erratum published online). |
| Allocation concealment (selection bias) | High risk | Quote: "Participants were sequentially assigned one of three study conditions. Assignment was done in the same manner at each hospital to maintain an equal number of participants in each condition across all sites." |
| Blinding of participants and personnel (performance bias) | Low risk | The music therapist could not be blinded given the interactive nature of the music therapy session. It is unclear whether the children were blinded to the purpose of the study. |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) | High risk | No data records were kept on number of subjects approached, consented and withdrawn (personal communication with principal investigator) |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "This research study was sponsored through a National Academy of Recording Arts and Sciences (NARAS) grant awarded to the American Music Therapy Association (AMTA). This study received additional support through an institutional post‐doctoral fellowship, CA 117865‐O1A1. |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adolescents and young adults undergoing hematopoietic stem cell transplant Type of cancer: leukemia ( n = 53, 46.4%), lymphoma ( n = 28, 25.0 %), solid tumor ( n = 32, 28.6%) Total N randomized: 113 N randomized to music group: 59 N randomized to control group: 54 N analyzed in music group: 40 N analyzed in control group: 40 Mean age: 17.3 years Sex: 42.5% female, 57.5% male Ethnicity: 12 (10.6%) African‐American, 66 (58.4%); white, 23 (20.4%); mixed ethnicity, 7 (6.2%); other, 5 (4.4%); Setting: inpatient Country: USA | |
| Interventions | 2 study groups:
Music selections provided: participants created their own songs with the music therapist Number of sessions: 6 Length of sessions: not reported Categorized as music therapy | |
| Outcomes | Illness‐related distress (McCorkle Symptom Distress Scale), coping (Jalowiec Coping Scale‐Revised), spiritual perspective (Reed Spiritual Perspective Scale); social integration (Perceived Social Support), family environment (Family Adaptability/Cohesion Scale), hope‐derived meaning (Herth Hope Index), self transcendence (Reed Self Transcendence Scale), and resilience (Haase Resilience in Illness Scale): effect sizes | |
| Notes | Effect sizes were reported in the publication. No means or SDs were reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomised to the TMV or low‐dose, control group using 24 strata (8 sites individually stratified by 3 age groups: 11‐14, 15‐ 18, and 19‐24 years)" (p. 911). |
| Allocation concealment (selection bias) | Low risk | "We used central randomisation by a third party. So after a participant completed the baseline measures, the computer triggered randomisation. The project manager is then notified electronically (e‐mail generation) about the participant's group assignment" (personal communication with investigator). |
| Blinding of participants and personnel (performance bias) | Low risk | Music therapist and participants could not be blinded |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | High risk | "An intent‐to‐treat analysis was performed in which all available questionnaire data at T2 and T3 were used, and participants were analysed according to their assigned group regardless of their degree of adherence to the protocols for the intervention and low‐dose control groups" (p. 913‐914). Dropout rate was 28% at T2 and 41% at T3. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | "This work as funded by the National Institute of Nursing Research (R01NR008583) and the National Cancer Institute (U10CA098543 and U10CA095861)" (p 916) |
| Methods | CCT 2‐arm parallel group design | |
| Participants | Adult breast cancer patients receiving chemotherapy Type of cancer: localized tumor (n = 50, 80.6%), metastatic tumor (n = 12, 19.4%) Total N randomized: 62 Total N analyzed: 62 N randomized to music group: 31 N randomized to control group: 31 N analyzed in music group: 31 N analyzed in control group: 31 Mean age: 54.2 years Sex: 62 (100%) female Ethnicity: not reported Setting: outpatient Country: Italy | |
| Interventions | 2 study groups:
Music selections provided: active singing using vocal holding techniques Number of sessions: 1 Length of sessions: 150 min Categorized as music therapy | |
| Outcomes | Depression, anxiety, anger, stress, need for help: only means were reported (no standard deviations). Therefore the results could not be included in the meta‐analysis. | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "The patients gave informed consent to participate and were quasi‐randomly assigned to the experimental and control arms of the study" (p. 439). "On Mondays and Wednesdays of each week, the first consecutive eligible patients of the day who gave their informed consent to participate in the study were placed in the same room for chemotherapy infusion and took part in the experimental group. On Tuesdays and Thursdays the same procedure was followed and these patients were assigned to the control groups. 31 patients were allocated to the experimental group and 31 to the control group" (p. 439). |
| Allocation concealment (selection bias) | High risk | Alternate assignment prohibited allocation concealment |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding of music therapist and participants was not possible |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | No evidence of selective reporting |
| Other bias | Low risk | "The authors declare that there is no conflict of interest" (p 443) |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adult patients recovering from a bone marrow transplant Type of cancer: leukemia (n = 12, 66.7%), multiple melanoma (n = 5, 27.8%), unknown (n = 1, 5.6%) Total N randomized: 18 N randomized to music group: 8 N randomized to control group: 10 N analyzed in music group: 8 N analyzed in control group:10 Mean age: 53.6 years Sex: 100% female Ethnicity: 2 (11.1%) African‐American, 1 (5.6%) Asian‐American, 14 (77.8%) white, 1 (5.6%) Latino Setting: inpatient Country: USA | |
| Interventions | 2 study groups:
Music selections provided: music therapist played patient‐preferred live music with guitar and voice Number of sessions: 1 Length of sessions: 45 min Categorized as music therapy | |
| Outcomes | Fatigue (The Brief Fatigue Inventory): change scores | |
| Notes | This manuscript included 2 studies. Only the second study is used in this review as the first study was not an RCT or CCT | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "After obtaining consent to participate in the study, the researchers consulted a randomized list to ascertain each participant’s condition in the study" (p. 68). |
| Allocation concealment (selection bias) | High risk | Not reported |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding of music therapist and participants was not possible. |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) | High risk | Self‐report measures were used for subjective outcomes. |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | No evidence of selective reporting. |
| Other bias | Low risk | No conflict of interests reported |
| Methods | CCT 2‐arm parallel group design | |
| Participants | Adults with cancer with pain Diagnosis: no further details available in translation of study report Total N randomized: 100 N randomized to music group: 50 N randomized to control group: 50 N analyzed in music group: 50 N analyzed in control group: 50 Mean age: not reported Sex: not reported Ethnicity: 100 (100%) white Setting: unclear if inpatient or outpatient (treatment provided in hospital) Country: Iran | |
| Interventions | 2 study groups:
Music selections provided: 3 types of music (no further detail provided in translation of study report) Number of sessions: 3 Length of sessions: 30 min Categorized as music medicine | |
| Outcomes | Pain (VAS): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternate assignment. Quote: "The first patient included in one group and second person to another group" (personal communication with principal investigator) |
| Allocation concealment (selection bias) | High risk | Alternation method |
| Blinding of participants and personnel (performance bias) | High risk | Personnel and participants were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Unclear risk | No dropouts reported. However, it is unlikely that no attrition occurred in a study with this sample size. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Unclear risk | Funding information and conflict of interest statement are not provided in the translation of the study report |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adults with cancer receiving radiation therapy Diagnosis: prostate (n = 24, 55%), lung (n = 6, 14%), head or neck (n = 4, 9%), colorectal (n = 4, 9%), squamous cell skin (n = 2, 5%), stomach (n = 1, 2%), melanoma (n = 1, 2%) Total N randomized: 44 N randomized to music group: 20 N randomized to control group:24 N analyzed in music group: 19 N analyzed in control group: 23 Mean age: 62.8 years Sex: 42 (100%) males Ethnicity: 31 (74%) white, 5 (12%) black, 5 (12%) Latino, and 1 (2%) other Setting: outpatient Country: USA | |
| Interventions | 2 study groups:
Music selections provided: participants were asked to select from rock and roll, big band, country and western, classical, easy listening, Spanish, or religious music Number of sessions: daily for duration of treatment Length of sessions: 30 min Categorized as music medicine | |
| Outcomes | Anxiety (STAI‐S): post‐test scores after 1 week of music interventions | |
| Notes | Post‐test scores for week 3 and week 5 are also reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A biostatistician prepared a randomisation list using a computer. Only one member of the research team had access to this list of case numbers and randomisation assignments, which was maintained in a locked filing cabinet" (p. 856). |
| Allocation concealment (selection bias) | Low risk | Central randomization. Quote: "At the time the patient agreed to participate in the study and the consent form was signed, the research associate called the registrar to obtain the patient's assigned case number and randomisation group." |
| Blinding of participants and personnel (performance bias) | Unclear risk | Participants were not blinded. It is unclear whether the personnel were blinded. |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Attrition rate: 5% Quote:"Two patients, one from each group, were excluded from final analysis because of incomplete data". |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting. |
| Other bias | Low risk | This study was supported, in part, by a grant from Sigma Theta Tau, Delta Beta Chapter, of the College of Nursing at the University of South Florida. |
| Methods | CCT 2‐arm parallel group design | |
| Participants | Women at the completion of treatment for breast cancer Type of cancer: breast (n = 20, 100%) Total N randomized: 20 Total N analyzed: 20 N randomized to music group: 10 N randomized to control group: 10 N analyzed in music group: 10 N analyzed in control group: 10 Mean age: 48.35 years Sex: n = 20 (100%) females Ethnicity: n = 9 (45%) Latino, n = 6 (30%) white, n = 5 (25%) African‐American/Caribbean black Setting: outpatient Country: USA | |
| Interventions | 2 treatment conditions:
Music selections provided: contemporary sedative music was paired with standard spoken relaxation directives Number of sessions: 4 Length of sessions: 20‐30 min Categorized as music therapy trial | |
| Outcomes | Depression [Center for Epidimiologic Diseases ‐ Depression Scale (CES‐D)]: post‐test scores Mood (POMS ‐ Short Form): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Low risk | Participants and personnel could not be blinded |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not include objective measures |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of conflict of interest |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adults with cancer receiving chemotherapy Diagnosis: no further details provided Total N randomized: unclear N randomized to music group: unclear N randomized to control group: unclear N analyzed in music group: 9 N analyzed in control group: 10 Mean age: 49 years Sex: 13 (27%) females, 26 (73%) males Ethnicity: not provided Setting: unclear if inpatient or outpatient Country: USA | |
| Interventions | 2 study groups:
Music selections provided: a music tape was created by the researcher. If the participants disliked the music, they could listen to a tape of their own. Number of sessions: participants listened to tape during chemotherapy treatments and at home. Participants were encouraged to listen to the tape each day. Length of sessions: 30‐40 min Categorized as music medicine | |
| Outcomes | Anxiety (STAI‐S): post‐test scores QoL (Functional Living Index): post‐test scores Level of control: not included in this review | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random assignment of subjects to condition involved choosing pieces of paper from a box. Half of the pieces had 'one' written on them, and half a 'two'. In this way, subjects had an equal chance being assigned to either group". |
| Allocation concealment (selection bias) | Low risk | Not reported but we assume that lots were drawn in the presence of the subjects. |
| Blinding of participants and personnel (performance bias) | High risk | Personnel and participants were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Unclear risk | It is unclear whether number of participants analyzed equals the number of participants recruited |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | — |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adults with skin cancer Type of cancer: skin (100%) Total N randomized: 100 Total N analyzed: 100 N randomized to music group: 50 N randomized to control group: 50 N analyzed in music group: 50 N analyzed in control group: 50 Mean age: 64.3 years Sex: 33 (33%) female, 67 (67%) male Ethnicity: not reported Setting: inpatient Country: USA | |
| Interventions | 2 study groups:
Music selections provided: patients chose a musical genre, artist, or track, which was entered into internet radio (Pandora Media, Inc., Oakland, CA), which creates a mix of music according to the listener's preferences Number of sessions: 1 Length of sessions: 15‐60 min Categorized as music medicine trial | |
| Outcomes | Anxiety (STAI): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Using a randomisation table (a table of random numbers), eligible subjects were randomly assigned into one of two groups: a control group with no music or a treatment group that listened to the music of their choice during surgery" (p. 299). |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participant was not possible. Personnel was not blinded. "This study was designed as an open‐labelled randomized controlled trial" (p. 299). |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes. |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No conflict of interest reported |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adult cancer patients with pain Diagnosis: cancer of the lung, liver, gastrointestinal, lymphoma Total N randomized: 136 Total N analyzed: 136 N randomized to music group: unclear N randomized to control group: unclear N analyzed in music group: 65 N analyzed in control group: 71 Mean age: 52.5 years Sex: 76 (56%) females, 60 (44%) males Ethnicity: 136 (100%) Chinese (Han) Setting: inpatient Country: China | |
| Interventions | 2 study groups:
Music selections provided: no details on the music reported Number of sessions: 1 Length of sessions: 30 min Categorized as music medicine | |
| Outcomes | Depression (Center for Epidemiologic Studies Depression Scale, CES‐D): post‐test scores Anxiety (STAI‐S): post‐test scores Pain (NRS): post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Translation quote: "Simple randomizations" |
| Allocation concealment (selection bias) | High risk | Not used |
| Blinding of participants and personnel (performance bias) | High risk | Personnel and participants were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Unclear risk | It is unclear whether number of participants analyzed equals the number of participants recruited |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting. |
| Other bias | Unclear risk | Funding information and conflict of interest statement are not provided in the translation of the study report |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adults after surgery for lung cancer Type of cancer: lung (n = 60, 100%) Total N randomized: 60 Total N analyzed: 60 N randomized to music group: 30 N randomized to control group: 30 N analyzed in music group: 30 N analyzed in control group: 30 Mean age: 53.65 Sex: 25 (41%) females, 35 (58%) males Ethnicity: not reported Setting: inpatient Country: China | |
| Interventions | 2 study groups:
Music selections provided: Western classical music and Chinese music Number of Sessions: 5 pre‐surgery music‐assisted relaxation and 4 postsurgery in ICU Length of Sessions: pre‐surgery 15 min, postsurgery 1 h Categorized as music therapy | |
| Outcomes | Pain Self Rating Anxiety Scale (SAS) and visual analogue scale (VAS): pre‐test, post‐SBP, DBP, heart rate (HR), pulse oxygen saturation (SpO2), respiratory rate, SAS score, VAS score, drug dose, and total consumption of sufentanil at 4, 8, 12, 16, 20, and 24 h were recorded postoperatively | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Consecutive patients were recruited and randomly assigned to the MT group and control (C) group by using a random‐numbers table and sealed sequential envelopes prepared by an independent statistician" (p. 668). |
| Allocation concealment (selection bias) | Low risk | "Consecutive patients were recruited and randomly assigned to the MT group and control (C) group by using a random‐numbers table and sealed sequential envelopes prepared by an independent statistician" (p. 668). |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | For objective outcomes, the following is reported: "All postoperative measurements were evaluated and confirmed by two independent observers. Observations were compared between them, and differences were solved by discussion." (p. 669). Therefore rating of low risk for objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | There were no withdrawals |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Unclear risk | "The study was funded by grant no. 2012FJ2004 from the Department of Science and Technology of Hunan Province, China". "No competing financial interests exist" (p. 672) |
| Methods | CCT (randomization method unclear) 2‐arm parallel group design | |
| Participants | Adults with cancer receiving chemotherapy Diagnosis: no further details available in the translation of the study report Total N randomized: 260 Total N analyzed: 260 N randomized to music group: 124 N randomized to control group: 136 N analyzed in music group: 124 N analyzed in control group: 136 Mean age: not reported Sex: not reported Ethnicity: 260 (100%) Chinese Setting: not reported Country: China | |
| Interventions | 2 study groups:
Music selections provided: no details provided Number of sessions: 2 times per day for 20 days Length of sessions: 60 min Categorized as music medicine | |
| Outcomes | Physical functioning (Karnofsky Performance Scale): post‐test scores QoL (QoL Questionnaire for Chinese cancer patients): change scores were computed by JB to allow for computation of pooled effect size (SMD) with other studies that reported change scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Personnel and participants were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Unclear risk | It is unclear whether number of participants analyzed equals the number of participants recruited |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Unclear risk | Funding information and conflict of interest statement are not provided in the translation of the study report |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adult Type of cancer: appendix (n = 1, 3%), bladder (n = 1, 3%), breast (n = 2, 7%), colon/rectal (n = 5, 19%), liposarcoma (n = 1, 3%), melanoma (n = 1, 3%), ovarian (n = 2, 7%), pancreatic (n = 1, 3%), papillary (n = 1, 3%), tumor (reported as such in article, no further detail is provided) (n = 2, 7%), uterine (n = 3, 11%), other (n = 6, 23%) Total N randomized: 26 Total N analyzed: 22 N randomized to music group: 13 N randomized to control group: 13 N analyzed in music group: 11 N analyzed in control group: 11 Mean age: 57.59 Sex: 22 ( 84 % ) females, 4 ( 15 %) males Ethnicity: 2 (7%) Latino, 21 (80%) white, 3 (11%) other Setting: inpatient Country: USA | |
| Interventions | 2 study groups:
Music selections provided: patient‐preferred live music Number of sessions:1 Length of sessions: 20‐30 min Categorized as music therapy | |
| Outcomes | 6 mood states measured by the Quick Mood Scale (QMS), namely wide awake/drowsy, relaxed/anxious, cheerful/depressed, friendly/aggressive, clearheaded/confused, well‐coordinated/clumsy. Only the relaxed/anxious and cheerful/depressed states are included in this review: post‐test scores | |
| Notes | Means and standard errors are reported in the journal article. Standard deviations were obtained from the primary author. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “We used a computer program on randomizer.org to create a series of 0 and 1. A 0 meant a participant was in the control group” (personal communication with chief investigator). |
| Allocation concealment (selection bias) | High risk | No allocation concealment used (personal communication with chief investigator). |
| Blinding of participants and personnel (performance bias) | Low risk | Music therapist and participants could not be blinded. |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not include objective outcomes. |
| Blinding of outcome assessment (detection bias) | High risk | Self‐report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Out of 26 participants, 4 were lost: “Four participants were not included in data analyses as two participants fell asleep,one participant had a visit from the doctor, and one participant did not complete the form correctly" (p. 59). Attrition rate: 8.5%. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting. |
| Other bias | Low risk | No conflict of interest reported. |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adults with cancer undergoing radiation therapy Diagnosis: cancer of the lung, esophogus, gastric, liver, breast, ovary, uterine, renal, bladder, ureter Total N randomized: 95 Total N analyzed: 95 N randomized to music group: 49 N randomized to control group: 46 N analyzed in music group: 49 N analyzed in control group: 46 Mean age: 53.87 years Sex: 43 (45%) females, 52 (55%) males Ethnicity: 95 (100%) Chinese (Han) Setting: outpatient Country: China | |
| Interventions | 2 study groups:
Music selections provided: sacred music (Buddhism and Christianity), Chinese classical music, Western classical music, or yoga music Number of sessions: 1 Length of sessions: 30 min Categorized as music medicine | |
| Outcomes | Anxiety (Zung State Anxiety Scale): post‐test scores Anxiety (Hamilton Anxiety Scale, HAMA): not included in this review HR, RR, SBP, DBP: post‐test scores | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Drawing of lots |
| Allocation concealment (selection bias) | High risk | Not used |
| Blinding of participants and personnel (performance bias) | High risk | Personnel and participants were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Unclear risk | It is unclear whether number of participants analyzed equals the number of participants recruited |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Unclear risk | Funding information and conflict of interest statement are not provided in the translation of the study report |
| Methods | RCT 2‐arm parallel group design | |
| Participants | Adults with breast cancer (n = 170, 100%) Total N randomized: 170 Total N analyzed: 170 N randomized to music group: 85 N randomized to control group: 85 N analyzed in music group: 85 N analyzed in control group: 85 Mean age: 47.01 years Sex: n = 170 (100%) females Ethnicity: not reported Setting: Inpatient Country: PR China | |
| Interventions | 2 study groups:
Music selections provided: Chinese relaxation music, classical folk music, religious music Number of sessions: Not reported Length of sessions: 30 min Categorized as music medicine | |
| Outcomes | Depression (Zung Self rating Depression Scale, ZSDS) Anxiety (State Anxiety Inventory, SAI) | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The patients were randomly allocated to two groups using 170 random numbers produced by computer software" (p. 55). |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not include objective outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | There were no withdrawals |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting. |
| Other bias | Low risk | "We thank the Dreyfus Health Foundation, New York for funding this study" (p 59). |
ANC: absolute neutrophil count;BIS: Bispectral Index; BMGIM: Bonny Method of Guided Imagery and Music CCT: controlled clinical trial; CM: Chinese medicine; DBP: diastolic blood pressure; EORTC: European Organization for Research and Treatment on Cancer; FACIT‐BMT/G/Sp: Functional Assessment of Chronic Illness Therapy‐Bone Marrow Transplant/General/Spiritual; GIM: guided imagery and music; HADS: Hospital Anxiety and Depression Scale; HAMA: Hamilton Anxiety Scale;HR: heart rate;ICU: intensive care unit; KPS: Karnofsky Performance Scale; LP: lumbar puncture; MAP: mean arterial pressure; MM: music medicine; MT: music therapy; NRS: numeric rating scale; PI: principal investigator; POMS: Profile of Mood States; QoL: quality of life; RBC: red blood cell; RCT: randomized controlled trial; RR: respiration rate; SAS: State Anxiety Scale; SBP: systolic blood pressure; SC: standard care;SCT: stem‐cell transplantation; SD: standard deviation; STAI‐S: Spielberger State‐Trait Anxiety Inventory ‐ State Anxiety form; TMV: therapeutic music video; VAS: visual analogue scale; WBC: white blood cell.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Not RCT/CCT | |
| Study with cancer survivors ‐ not population of interest | |
| Not RCT/CCT | |
| Not population of interest | |
| Not RCT/CCT | |
| Not RCT/CCT | |
| Not RCT/CCT | |
| Standard care control group was allowed to listen to music (authors state that otherwise they would not have been able to obtain ethics approval), and 4 out of 6 pediatric patients did. If all patients had opted to listen to music, we could have included this study in the music therapy versus music medicine comparison. | |
| Not RCT or CCT | |
| Not RCT or CCT | |
| Not RCT or CCT | |
| Sample included participants with malignant as well as benign tumours | |
| Not RCT/CCT | |
| Not RCT/CCT | |
| Not RCT/CCT; summary article of the Nguyen 2010 study | |
| Severe confounding issues with study design: the music group received 2 sessions whereas the control group only received 1. In addition, only post‐test data were obtained in this small scaled study; therefore we could not ascertain baseline equivalence between groups. | |
| No music intervention | |
| Not RCT/CCT | |
| Used non‐standardized measurement tools. The authors used a standardized scale (HADS) to measure anxiety and depression but reported a total score for the scale whereas this scale's scoring guidelines explicitly state that only subscale total scores (one for anxiety and one for depression) should be used. | |
| Study included cancer patients and their caregivers. Statistics are reported per treatment arm for patients and caregivers combined. Separate statistics are reported for cancer patients in the experimental group but not for those in the control group. | |
| Insufficient data reporting; attempts to contact authors unsuccessful | |
| Not RCT/CCT | |
| Not RCT/CCT | |
| Not RCT or CCT | |
| Insufficient data reporting; attempts to contact authors unsuccessful | |
| Unacceptable methodological quality: there were important pain‐related differences between the 2 groups at pre‐test. For example, there was unequal distribution of different procedures with the music group, which had significantly more biopsy procedures than the control group. Because biopsy procedures are more painful than other procedures included in the study, the author flagged this as a serious confounding variable. In addition, the amount of time that the patient listened to music was not controlled. The author stated that some patients only listened for 30 seconds prior to procedure. | |
| Not RCT/CCT | |
| Not RCT/CCT | |
| Not RCT/CCT | |
| Not intervention of interest | |
| Not RCT/CCT | |
| Not RCT/CCT | |
| Insufficient data reporting; study report includes graphic representation of results but does not include means and standard deviations | |
| This is poster abstract. Multiple attempts to contact author to get additional data unsuccessful | |
| Article cannot be located. We requested the article through our interlibrary loan departments and through our Cochrane Review Group. These attempts were unsuccessful. We then googled the investigator and e‐mailed her to request the research report. We sent 3 email requests over a period of 8 months but received no response. | |
| Not RCT/CCT | |
| Not RCT/CCT | |
| Not RCT/CCT | |
| Not RCT/CCT | |
| Not RCT/CCT | |
| Not RCT/CCT | |
| Not RCT/CCT | |
| Not RCT/CCT | |
| Thesis cannot be located; attempts to contact author unsuccessful | |
| Not RCT/CCT | |
| Not population of interest | |
| Unacceptable methodological quality; control group exposed to background music | |
| Not RCT/CCT | |
| Not RCT or CCT | |
| Not RCT/CCT | |
| Not RCT/CCT | |
| Not RCT/CCT | |
| Not RCT/CCT | |
| Not RCT/CCT | |
| Not RCT/CCT (personal communication with principal investigator) | |
| Not RCT/CCT | |
| Not RCT/CCT |
CCT: controlled clinical trial; HADS: Hospital Anxiety and Depression Scale; RCT: randomized controlled trial.
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | RCT |
| Participants | Adults newly diagnosed with malignant lymphoma and planned first line chemotherapy treatment |
| Interventions | Patient‐preferred live music during chemotherapy session compared with patient‐preferred taped music during chemotherapy compared with usual care during chemotherapy only |
| Outcomes | Mental health (anxiety and distress), nausea, serum catecholamines, and QoL |
| Notes | Results are not yet published (personal communication with investigator) |
| Methods | RCT |
| Participants | Adult cancer patients with chronic pain |
| Interventions | Music entrainment compared to preferred recorded music |
| Outcomes | Pain, vital signs, medication usage, quality of life and medication side effects |
| Notes | Study has been completed but findings are not yet available |
| Methods | RCT |
| Participants | Adult patients with multiple myeloma or lymphoma (Hodgkin's or non‐Hodgkin's) who are undergoing ASCT |
| Interventions | Music therapy versus standard care |
| Outcomes | Primary outcomes: nausea and pain Secondary outcomes: mood disturbance, quality of life, use of morphine‐equivalent dose of narcotic medications |
| Notes | Study has been completed but findings are not yet available (personal communication with co‐investigator) |
| Methods | RCT |
| Participants | Patients who are undergoing chemotherapy for newly diagnosed solid tumors |
| Interventions | Mindfulness relaxation compared with relaxing music and standard symptom management education |
| Outcomes | Conditioned and nonconditioned nausea and vomiting, mental health (anxiety, depression, and distress), QoL (cancer‐related symptoms, fatigue, sleep, and pain), and immune function |
| Notes | Study has been completed but findings are still not available (personal communication with PI) |
| Methods | RCT |
| Participants | Newly diagnosed patients with breast cancer, and newly diagnosed patients with head and neck cancer |
| Interventions | Music therapy compared with no intervention control |
| Outcomes | Mental health (anxiety and distress) |
| Notes | Article is in press. Authors cannot provide results at this time because of embargo (Personal communication with authors) |
| Methods | RCT |
| Participants | Adult patients undergoing hematopoietic stem cell transplantation |
| Interventions | Apply live music in group format compared with standard treatment |
| Outcomes | Mental health (distress) |
| Notes | We have been unsuccessful in locating the principal investigator to obtain trial results |
| Methods | RCT mixed methods |
| Participants | Adult patients with cancer |
| Interventions | Guided Original Lyrics and Music (GOLM) songwriting |
| Outcomes | Mood, distress levels, QoL, and satisfaction with hospital stay |
| Notes | Study has been completed but has not yet been published. We attempted multiple times to obtain the full text dissertation from the investigator but have not received this from the investigator. |
ASCT: autologous stem cell transplant; PI: principal investigator; QoL: quality of life; RCT: randomized controlled trial.
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Effects of clinical music improvisation on resiliency in adults undergoing infusion therapy |
| Methods | RCT |
| Participants | Adults diagnosed with breast cancer, lung cancer, or gastrointestinal cancer |
| Interventions | Instrumental improvisational music therapy compared with vocal improvisational music therapy compared with standard care |
| Outcomes | Mental health (resilience, anxiety, stress, and depression), pain |
| Starting date | June 2011 |
| Contact information | |
| Notes | Anticipated completion date: June 2018 |
| Trial name or title | Guided imagery and music for the reduction of side effects of chemotherapy in teenagers |
| Methods | RCT |
| Participants | Teenagers receiving chemotherapy for cancer treatment |
| Interventions | Guided imagery and music, chemotherapy, and standard care compared with chemotherapy and standard care |
| Outcomes | Acute nausea, distress regarding nausea, amount of nausea reducing medicine consumed, chemotherapy side effects, acute vomiting, pain, days to absolute neutrophil count recovery, duration of fatigue, distress regarding fatigue, food intake, weight, sense of coherence, and satisfaction with music intervention |
| Starting date | 2014 |
| Contact information | |
| Notes | 2017 |
| Trial name or title | The effect and meaning of designed music narratives on anticipatory, acute, and delayed side effect of chemotherapy in children (7‐12 years) with cancer: a randomized controlled multisite study |
| Methods | RCT |
| Participants | Children (7‐12 years old) with cancer who are receiving chemotherapy |
| Interventions | 4 music narratives for children each comprising an introductory relaxation exercise, a resource‐oriented narrative including guided imagery suggestions and relaxing nature scenarios plus specially composed music |
| Outcomes | Duration (min) and intensity of acute nausea, frequency of vomiting, fatigue, pain, food intake, weight |
| Starting date | 2014 |
| Contact information | |
| Notes | Anticipated completion date: 2018 |
RCT: randomized controlled trial.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Anxiety (STAI) Show forest plot | 13 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.1 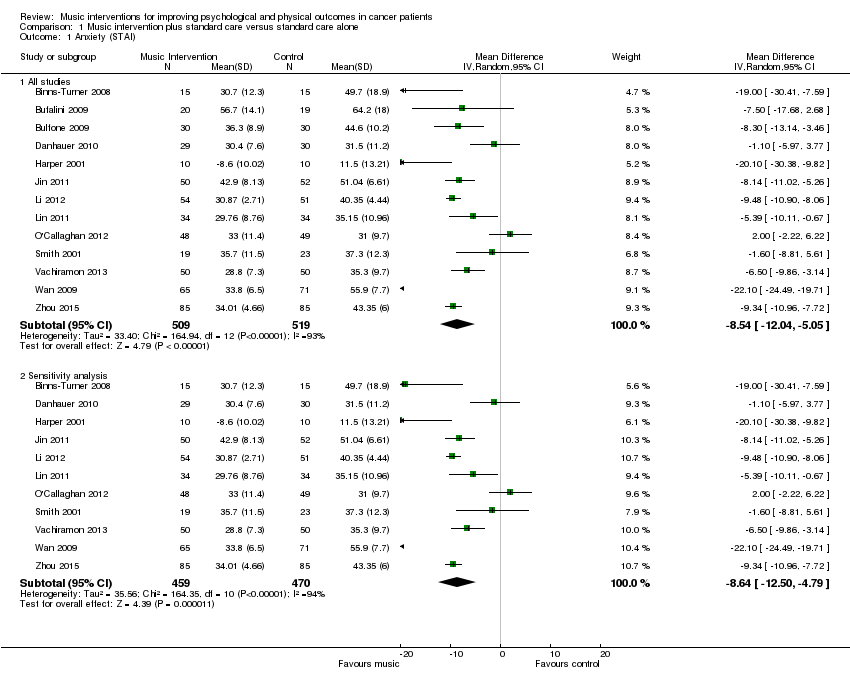 Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 1 Anxiety (STAI). | ||||
| 1.1 All studies | 13 | 1028 | Mean Difference (IV, Random, 95% CI) | ‐8.54 [‐12.04, ‐5.05] |
| 1.2 Sensitivity analysis | 11 | 929 | Mean Difference (IV, Random, 95% CI) | ‐8.64 [‐12.50, ‐4.79] |
| 2 Anxiety (non‐STAI (full version) measures) Show forest plot | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.2 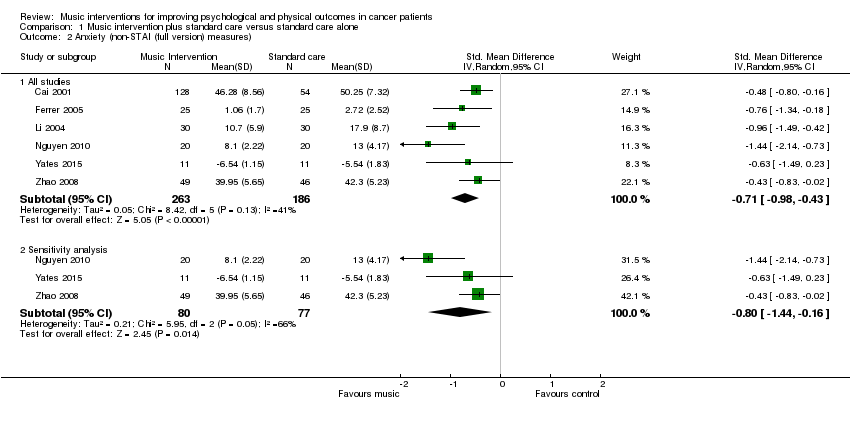 Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 2 Anxiety (non‐STAI (full version) measures). | ||||
| 2.1 All studies | 6 | 449 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐0.98, ‐0.43] |
| 2.2 Sensitivity analysis | 3 | 157 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐1.44, ‐0.16] |
| 3 Anxiety (intervention subgroup) Show forest plot | 18 | 1457 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.94 [‐1.34, ‐0.55] |
| Analysis 1.3  Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 3 Anxiety (intervention subgroup). | ||||
| 3.1 Music therapy studies | 3 | 111 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.62 [‐1.01, ‐0.24] |
| 3.2 Music medicine studies | 15 | 1346 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.00 [‐1.45, ‐0.55] |
| 4 Anxiety (music preference) Show forest plot | 13 | 1142 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.88 [‐1.28, ‐0.47] |
| Analysis 1.4  Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 4 Anxiety (music preference). | ||||
| 4.1 Patient‐preferred music | 10 | 860 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.86 [‐1.38, ‐0.34] |
| 4.2 Researcher‐selected music | 3 | 282 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.89 [‐1.43, ‐0.35] |
| 5 Anxiety (music‐guided relaxation) Show forest plot | 14 | 1306 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.98 [‐1.44, ‐0.51] |
| Analysis 1.5  Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 5 Anxiety (music‐guided relaxation). | ||||
| 5.1 Music‐guided relaxation studies | 4 | 476 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.61 [‐2.56, ‐0.65] |
| 5.2 Listening to music only | 10 | 830 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐1.16, ‐0.26] |
| 6 Depression Show forest plot | 7 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.6 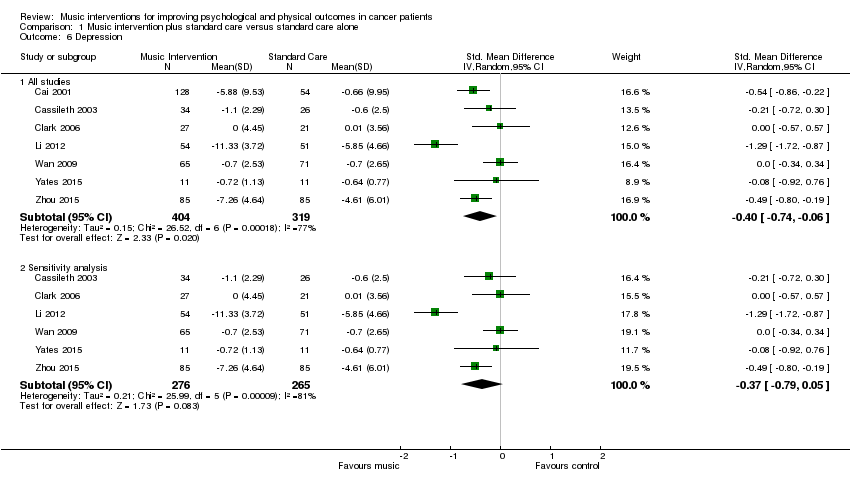 Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 6 Depression. | ||||
| 6.1 All studies | 7 | 723 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.74, ‐0.06] |
| 6.2 Sensitivity analysis | 6 | 541 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.79, 0.05] |
| 7 Depression (intervention subgroup) Show forest plot | 7 | 723 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.74, ‐0.06] |
| Analysis 1.7 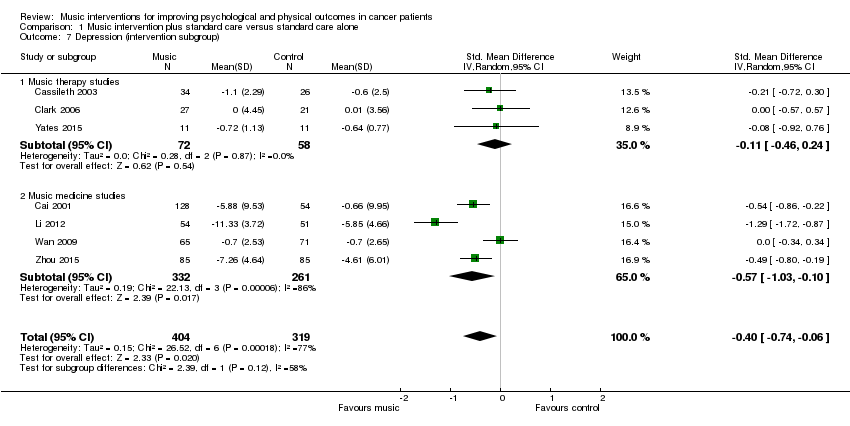 Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 7 Depression (intervention subgroup). | ||||
| 7.1 Music therapy studies | 3 | 130 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.46, 0.24] |
| 7.2 Music medicine studies | 4 | 593 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.57 [‐1.03, ‐0.10] |
| 8 Depression (music preference) Show forest plot | 4 | 505 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.04, ‐0.16] |
| Analysis 1.8 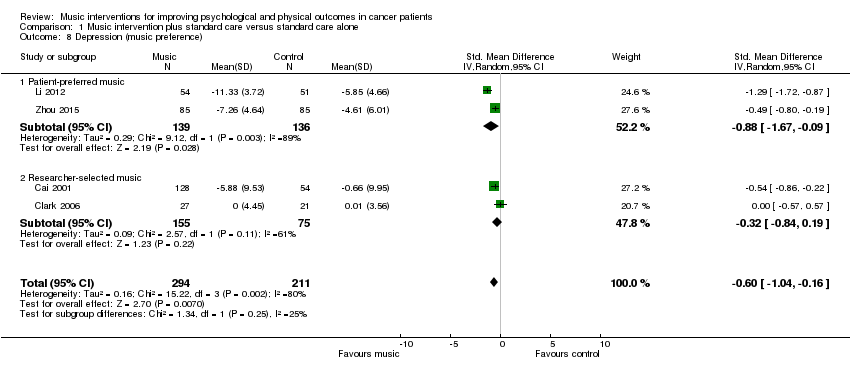 Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 8 Depression (music preference). | ||||
| 8.1 Patient‐preferred music | 2 | 275 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.88 [‐1.67, ‐0.09] |
| 8.2 Researcher‐selected music | 2 | 230 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.84, 0.19] |
| 9 Mood Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.9  Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 9 Mood. | ||||
| 9.1 All studies | 5 | 236 | Std. Mean Difference (IV, Random, 95% CI) | 0.47 [‐0.02, 0.97] |
| 9.2 Sensitivity analysis | 4 | 192 | Std. Mean Difference (IV, Random, 95% CI) | 0.57 [‐0.03, 1.18] |
| 10 Mood (intervention subgroup) Show forest plot | 5 | 236 | Std. Mean Difference (IV, Random, 95% CI) | 0.47 [‐0.02, 0.97] |
| Analysis 1.10 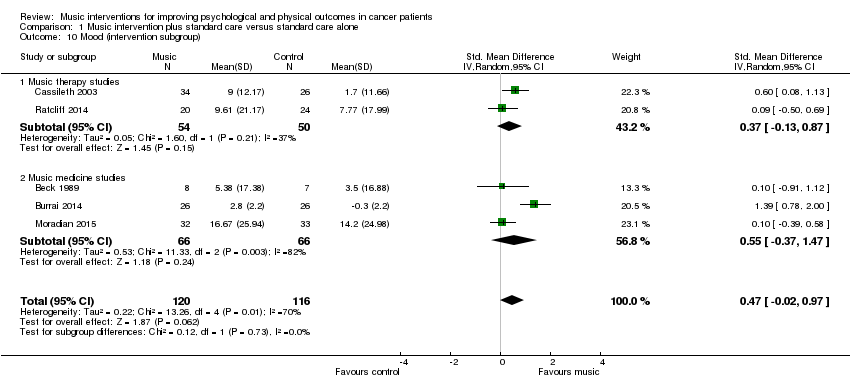 Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 10 Mood (intervention subgroup). | ||||
| 10.1 Music therapy studies | 2 | 104 | Std. Mean Difference (IV, Random, 95% CI) | 0.37 [‐0.13, 0.87] |
| 10.2 Music medicine studies | 3 | 132 | Std. Mean Difference (IV, Random, 95% CI) | 0.55 [‐0.37, 1.47] |
| 11 Pain Show forest plot | 7 | 528 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.91 [‐1.46, ‐0.36] |
| Analysis 1.11 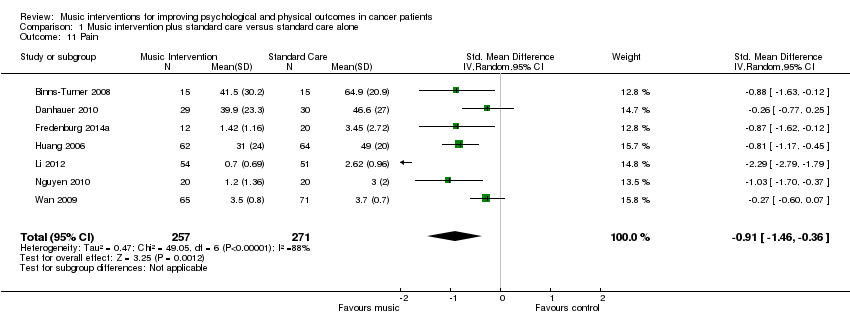 Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 11 Pain. | ||||
| 12 Pain (music preference) Show forest plot | 6 | 496 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.92 [‐1.53, ‐0.30] |
| Analysis 1.12 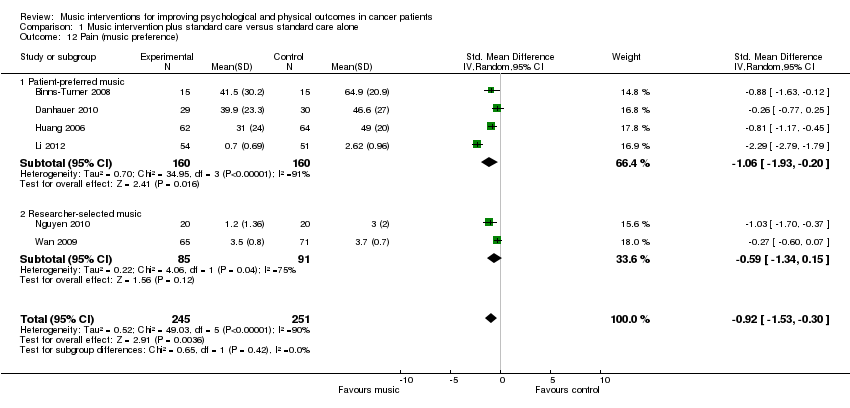 Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 12 Pain (music preference). | ||||
| 12.1 Patient‐preferred music | 4 | 320 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.06 [‐1.93, ‐0.20] |
| 12.2 Researcher‐selected music | 2 | 176 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.59 [‐1.34, 0.15] |
| 13 Fatigue Show forest plot | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.13 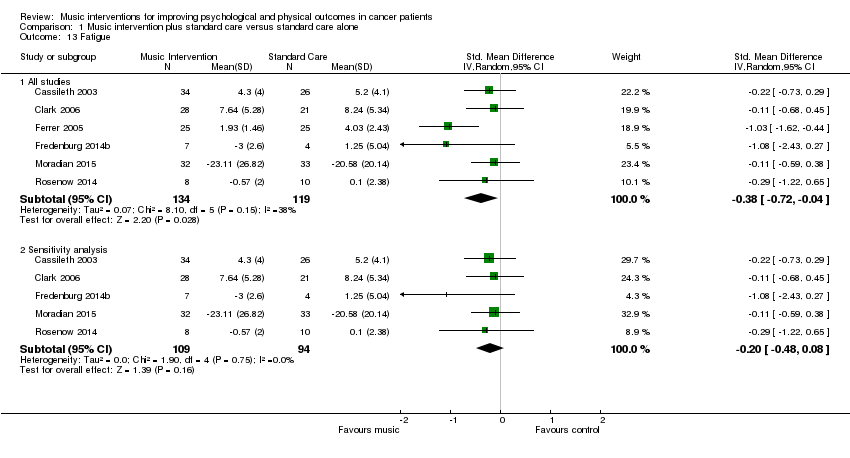 Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 13 Fatigue. | ||||
| 13.1 All studies | 6 | 253 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.72, ‐0.04] |
| 13.2 Sensitivity analysis | 5 | 203 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.48, 0.08] |
| 14 Physical functioning Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.14 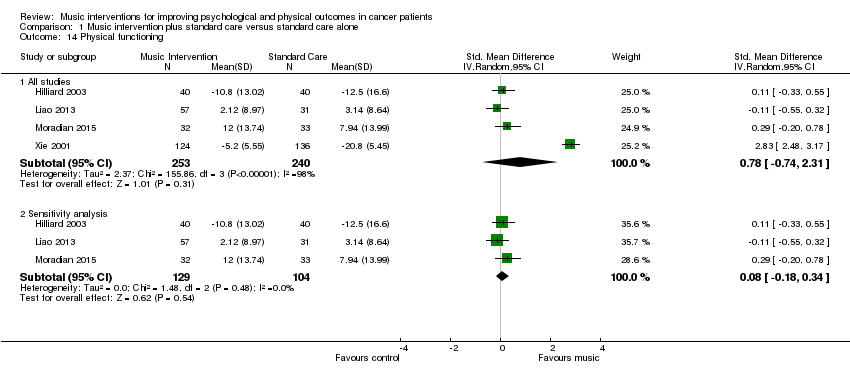 Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 14 Physical functioning. | ||||
| 14.1 All studies | 4 | 493 | Std. Mean Difference (IV, Random, 95% CI) | 0.78 [‐0.74, 2.31] |
| 14.2 Sensitivity analysis | 3 | 233 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.18, 0.34] |
| 15 Heart rate Show forest plot | 8 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.15  Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 15 Heart rate. | ||||
| 15.1 All studies | 8 | 589 | Mean Difference (IV, Random, 95% CI) | ‐3.32 [‐6.21, ‐0.44] |
| 15.2 Sensitivity analysis | 6 | 339 | Mean Difference (IV, Random, 95% CI) | ‐4.63 [‐8.18, ‐1.09] |
| 16 Heart rate (music preference) Show forest plot | 7 | 539 | Mean Difference (IV, Random, 95% CI) | ‐3.77 [‐6.97, ‐0.58] |
| Analysis 1.16  Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 16 Heart rate (music preference). | ||||
| 16.1 Patient‐preferred music | 5 | 479 | Mean Difference (IV, Random, 95% CI) | ‐3.13 [‐6.54, 0.27] |
| 16.2 Researcher‐selected music | 2 | 60 | Mean Difference (IV, Random, 95% CI) | ‐7.94 [‐15.10, ‐0.78] |
| 17 Respiratory rate Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.17 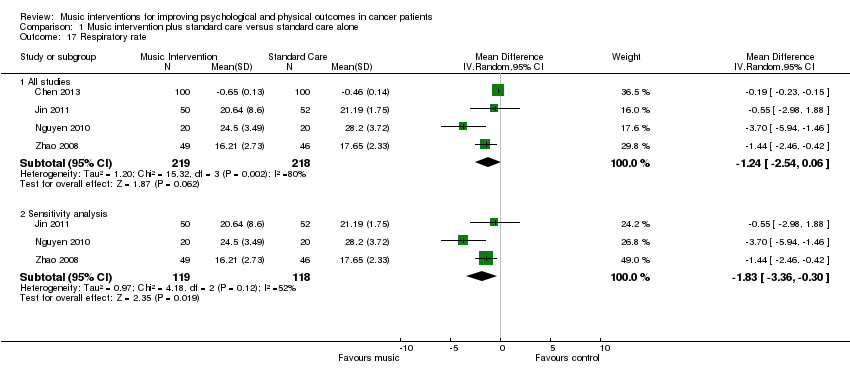 Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 17 Respiratory rate. | ||||
| 17.1 All studies | 4 | 437 | Mean Difference (IV, Random, 95% CI) | ‐1.24 [‐2.54, 0.06] |
| 17.2 Sensitivity analysis | 3 | 237 | Mean Difference (IV, Random, 95% CI) | ‐1.83 [‐3.36, ‐0.30] |
| 18 Systolic blood pressure Show forest plot | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.18 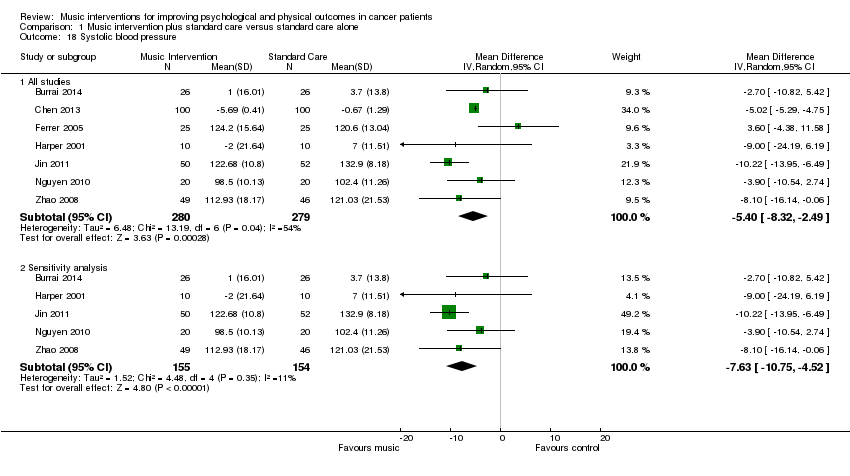 Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 18 Systolic blood pressure. | ||||
| 18.1 All studies | 7 | 559 | Mean Difference (IV, Random, 95% CI) | ‐5.40 [‐8.32, ‐2.49] |
| 18.2 Sensitivity analysis | 5 | 309 | Mean Difference (IV, Random, 95% CI) | ‐7.63 [‐10.75, ‐4.52] |
| 19 Systolic blood pressure (music preference) Show forest plot | 6 | 509 | Mean Difference (IV, Random, 95% CI) | ‐6.29 [‐8.86, ‐3.72] |
| Analysis 1.19  Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 19 Systolic blood pressure (music preference). | ||||
| 19.1 Patient‐preferred music | 4 | 449 | Mean Difference (IV, Random, 95% CI) | ‐6.65 [‐10.07, ‐3.23] |
| 19.2 Researcher‐selected music | 2 | 60 | Mean Difference (IV, Random, 95% CI) | ‐4.72 [‐10.80, 1.37] |
| 20 Diastolic blood pressure Show forest plot | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.20  Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 20 Diastolic blood pressure. | ||||
| 20.1 All studies | 7 | 559 | Mean Difference (IV, Random, 95% CI) | ‐2.35 [‐5.88, 1.18] |
| 20.2 Sensitivity analysis | 5 | 309 | Mean Difference (IV, Random, 95% CI) | ‐4.94 [‐7.78, ‐2.09] |
| 21 Diastolic blood pressure (music preference) Show forest plot | 6 | 509 | Mean Difference (IV, Random, 95% CI) | ‐3.74 [‐7.53, 0.05] |
| Analysis 1.21  Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 21 Diastolic blood pressure (music preference). | ||||
| 21.1 Patient‐preferred music | 4 | 449 | Mean Difference (IV, Random, 95% CI) | ‐4.10 [‐8.78, 0.59] |
| 21.2 Researcher‐selected music | 2 | 60 | Mean Difference (IV, Random, 95% CI) | ‐2.01 [‐6.26, 2.25] |
| 22 Oxygen Saturation Show forest plot | 3 | 292 | Mean Difference (IV, Random, 95% CI) | 0.50 [‐0.18, 1.18] |
| Analysis 1.22  Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 22 Oxygen Saturation. | ||||
| 23 Quality of Life Show forest plot | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.23 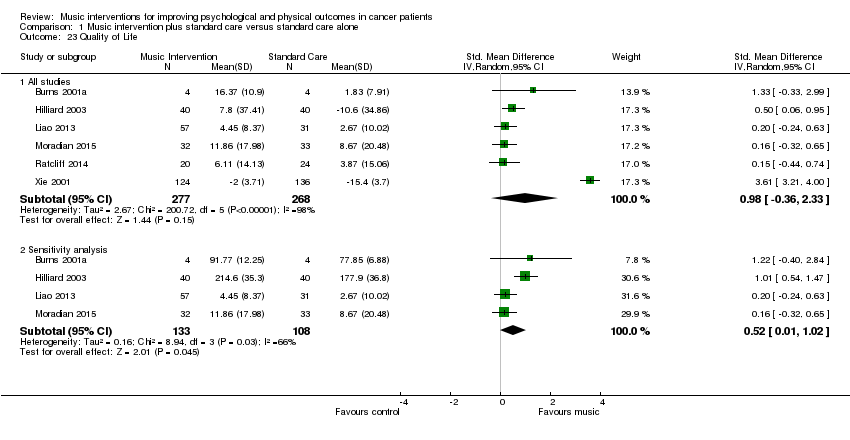 Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 23 Quality of Life. | ||||
| 23.1 All studies | 6 | 545 | Std. Mean Difference (IV, Random, 95% CI) | 0.98 [‐0.36, 2.33] |
| 23.2 Sensitivity analysis | 4 | 241 | Std. Mean Difference (IV, Random, 95% CI) | 0.52 [0.01, 1.02] |
| 24 Quality of life (intervention subgroup) Show forest plot | 5 | 568 | Std. Mean Difference (IV, Random, 95% CI) | 0.99 [‐0.34, 2.31] |
| Analysis 1.24 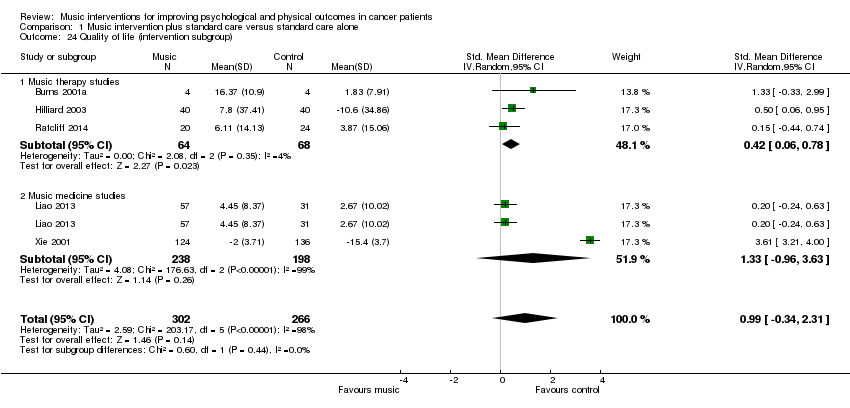 Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 24 Quality of life (intervention subgroup). | ||||
| 24.1 Music therapy studies | 3 | 132 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [0.06, 0.78] |
| 24.2 Music medicine studies | 2 | 436 | Std. Mean Difference (IV, Random, 95% CI) | 1.33 [‐0.96, 3.63] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Anxiety Show forest plot | 2 | 166 | Mean Difference (IV, Fixed, 95% CI) | ‐3.67 [‐11.68, 4.35] |
| Analysis 2.1  Comparison 2 Music therapy plus standard care versus music medicine plus standard care, Outcome 1 Anxiety. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Distress Show forest plot | 2 | Mean Difference (Random, 95% CI) | ‐0.07 [‐0.39, 0.26] | |
| Analysis 3.1  Comparison 3 Music interventions plus standard care versus standard care plus placebo control, Outcome 1 Distress. | ||||
| 2 Spiritual well‐being Show forest plot | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.31 [‐0.11, 0.73] | |
| Analysis 3.2  Comparison 3 Music interventions plus standard care versus standard care plus placebo control, Outcome 2 Spiritual well‐being. | ||||

Study flow diagram.
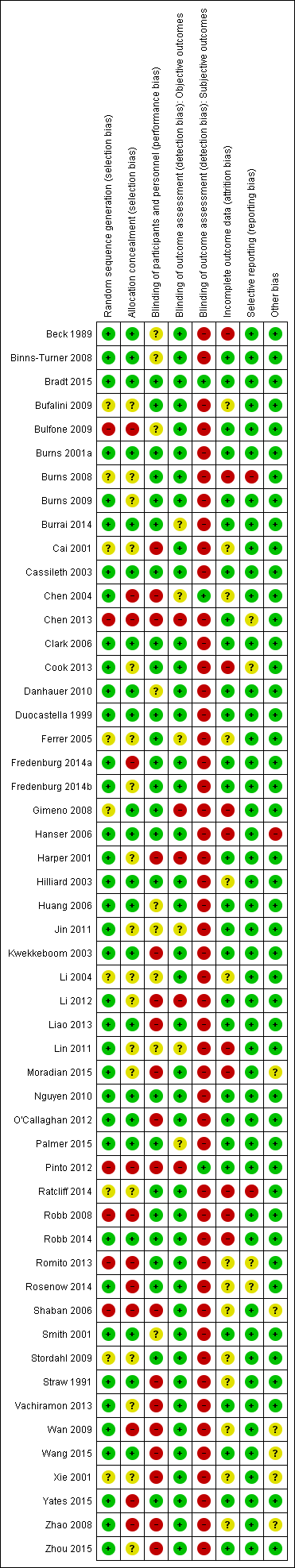
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
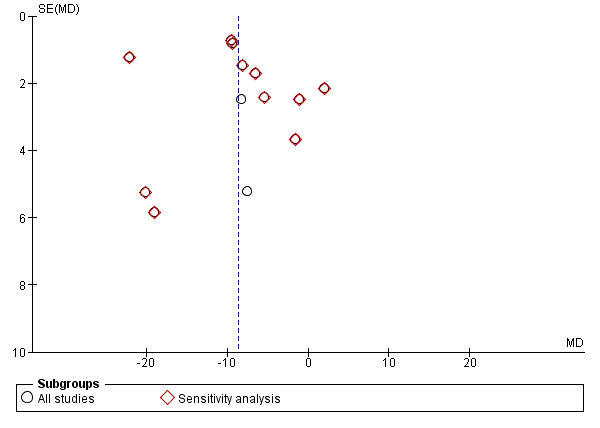
Funnel plot of comparison: 1 Music intervention plus standard care versus standard care alone, outcome: 1.1 Anxiety (STAI).

Funnel plot of comparison: 1 Music intervention plus standard care versus standard care alone, outcome: 1.6 Depression.

Funnel plot of comparison: 1 Music intervention plus standard care versus standard care alone, outcome: 1.11 Pain.

Funnel plot of comparison: 1 Music intervention plus standard care versus standard care alone, outcome: 1.15 Heart rate.

Funnel plot of comparison: 1 Music intervention plus standard care versus standard care alone, outcome: 1.13 Fatigue.
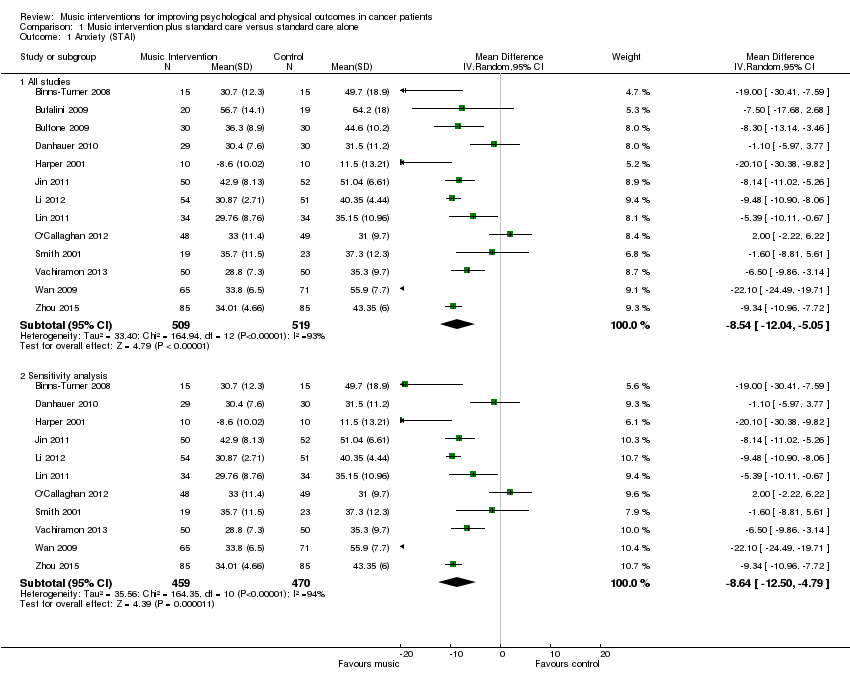
Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 1 Anxiety (STAI).
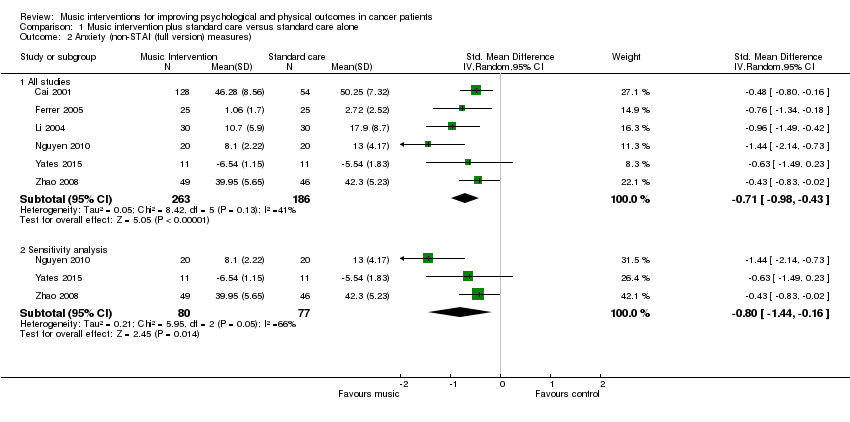
Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 2 Anxiety (non‐STAI (full version) measures).

Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 3 Anxiety (intervention subgroup).

Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 4 Anxiety (music preference).

Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 5 Anxiety (music‐guided relaxation).
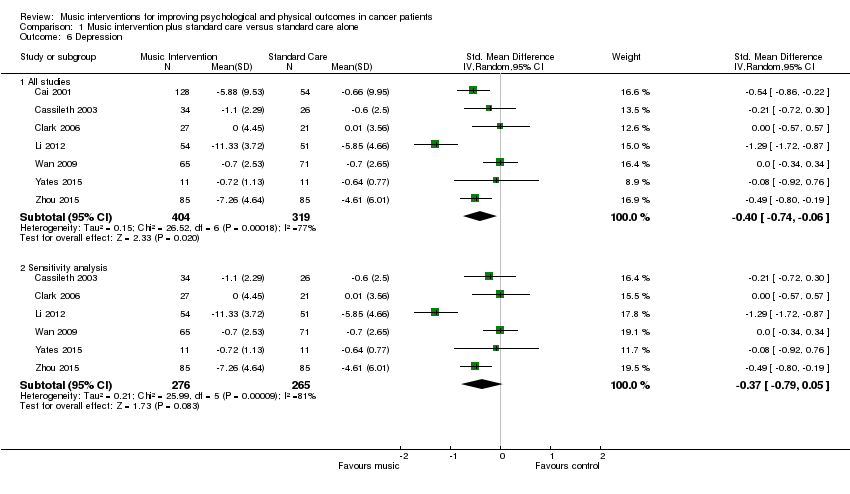
Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 6 Depression.

Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 7 Depression (intervention subgroup).

Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 8 Depression (music preference).

Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 9 Mood.

Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 10 Mood (intervention subgroup).

Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 11 Pain.

Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 12 Pain (music preference).

Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 13 Fatigue.

Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 14 Physical functioning.

Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 15 Heart rate.

Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 16 Heart rate (music preference).

Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 17 Respiratory rate.
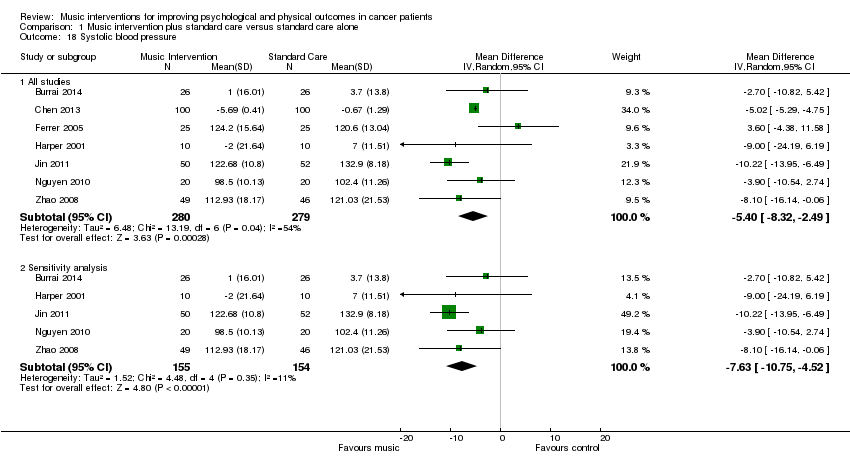
Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 18 Systolic blood pressure.
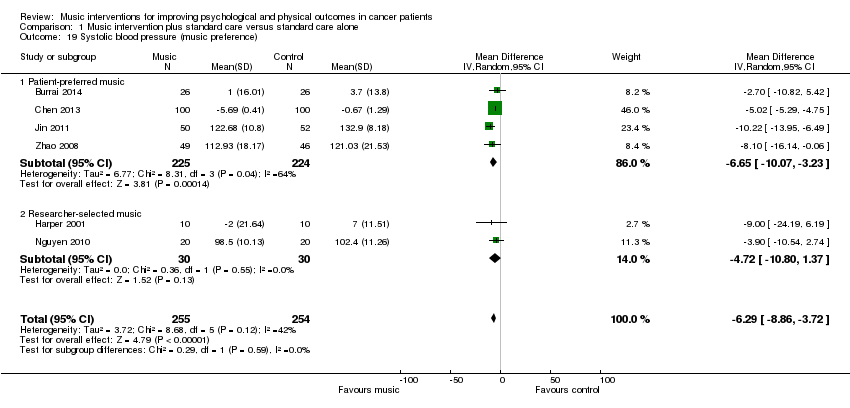
Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 19 Systolic blood pressure (music preference).

Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 20 Diastolic blood pressure.
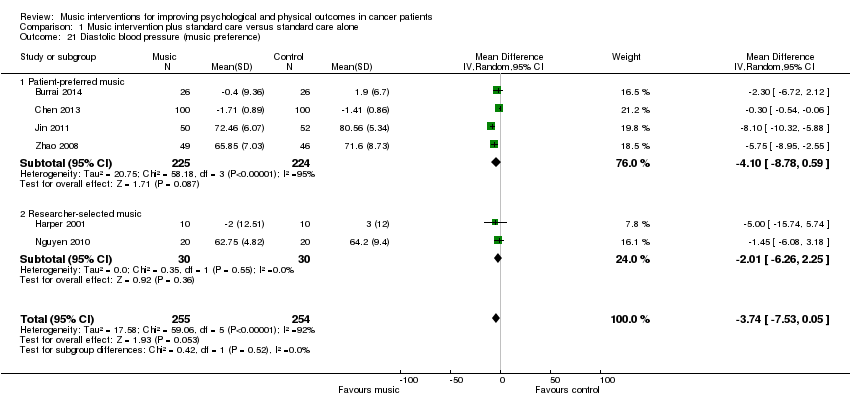
Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 21 Diastolic blood pressure (music preference).

Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 22 Oxygen Saturation.

Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 23 Quality of Life.

Comparison 1 Music intervention plus standard care versus standard care alone, Outcome 24 Quality of life (intervention subgroup).

Comparison 2 Music therapy plus standard care versus music medicine plus standard care, Outcome 1 Anxiety.
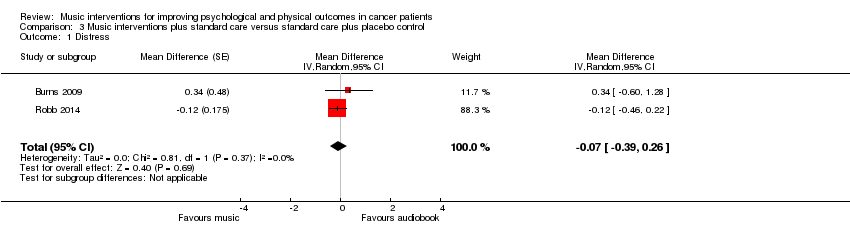
Comparison 3 Music interventions plus standard care versus standard care plus placebo control, Outcome 1 Distress.

Comparison 3 Music interventions plus standard care versus standard care plus placebo control, Outcome 2 Spiritual well‐being.
| Music interventions versus standard care for psychological and physical outcomes in cancer patients | ||||
| Patient or population: cancer patients | ||||
| Outcomes | Relative effect (95% CI) | No of participants | Quality of the evidence | Comments |
| Anxiety | The mean anxiety in the music intervention group was 8.54 units less (12.04 less to 5.05 less) than in the standard care group | 1028 | ⊕⊕⊝⊝ | — |
| Depression | The mean depression in the music intervention group was 0.40 standard deviations less (0.74 less to 0.06 less) than in the standard care group | 723 | ⊕⊝⊝⊝ | An SMD of 0.40 is considered a low to moderate effect size |
| Mood | The mean mood in the music intervention group was 0.47 standard deviations better (0.02 worse to 0.97 better) than in the standard care group | 236 | ⊕⊕⊝⊝ | An SMD of 0.47 is considered a moderate effect size |
| Pain | The mean pain in the intervention group was 0.91 standard deviations less (1.46 less to 0.36 less) than in the standard care group | 528 | ⊕⊕⊝⊝ | An SMD of 0.91 is considered a large effect size |
| Fatigue | The mean fatigue in the music intervention group was 0.38 standard deviations less (0.72 less to 0.04 less) than in the standard care group | 253 | ⊕⊕⊝⊝ | An SMD of 0.38 is considered a small to moderate effect size |
| Quality of life | The mean quality of life in the music intervention group was 0.98 standard deviations more (0.36 less to 2.33 more) than in the standard care group | 545 | ⊕⊕⊝⊝ | An SMD of 0.98 is considered a large effect size |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||
| GRADE Working Group grades of evidence | ||||
| a The majority of the trials were at high risk of bias. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Anxiety (STAI) Show forest plot | 13 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 All studies | 13 | 1028 | Mean Difference (IV, Random, 95% CI) | ‐8.54 [‐12.04, ‐5.05] |
| 1.2 Sensitivity analysis | 11 | 929 | Mean Difference (IV, Random, 95% CI) | ‐8.64 [‐12.50, ‐4.79] |
| 2 Anxiety (non‐STAI (full version) measures) Show forest plot | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 All studies | 6 | 449 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐0.98, ‐0.43] |
| 2.2 Sensitivity analysis | 3 | 157 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐1.44, ‐0.16] |
| 3 Anxiety (intervention subgroup) Show forest plot | 18 | 1457 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.94 [‐1.34, ‐0.55] |
| 3.1 Music therapy studies | 3 | 111 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.62 [‐1.01, ‐0.24] |
| 3.2 Music medicine studies | 15 | 1346 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.00 [‐1.45, ‐0.55] |
| 4 Anxiety (music preference) Show forest plot | 13 | 1142 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.88 [‐1.28, ‐0.47] |
| 4.1 Patient‐preferred music | 10 | 860 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.86 [‐1.38, ‐0.34] |
| 4.2 Researcher‐selected music | 3 | 282 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.89 [‐1.43, ‐0.35] |
| 5 Anxiety (music‐guided relaxation) Show forest plot | 14 | 1306 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.98 [‐1.44, ‐0.51] |
| 5.1 Music‐guided relaxation studies | 4 | 476 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.61 [‐2.56, ‐0.65] |
| 5.2 Listening to music only | 10 | 830 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐1.16, ‐0.26] |
| 6 Depression Show forest plot | 7 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 All studies | 7 | 723 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.74, ‐0.06] |
| 6.2 Sensitivity analysis | 6 | 541 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.79, 0.05] |
| 7 Depression (intervention subgroup) Show forest plot | 7 | 723 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.74, ‐0.06] |
| 7.1 Music therapy studies | 3 | 130 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.46, 0.24] |
| 7.2 Music medicine studies | 4 | 593 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.57 [‐1.03, ‐0.10] |
| 8 Depression (music preference) Show forest plot | 4 | 505 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.04, ‐0.16] |
| 8.1 Patient‐preferred music | 2 | 275 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.88 [‐1.67, ‐0.09] |
| 8.2 Researcher‐selected music | 2 | 230 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.84, 0.19] |
| 9 Mood Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 All studies | 5 | 236 | Std. Mean Difference (IV, Random, 95% CI) | 0.47 [‐0.02, 0.97] |
| 9.2 Sensitivity analysis | 4 | 192 | Std. Mean Difference (IV, Random, 95% CI) | 0.57 [‐0.03, 1.18] |
| 10 Mood (intervention subgroup) Show forest plot | 5 | 236 | Std. Mean Difference (IV, Random, 95% CI) | 0.47 [‐0.02, 0.97] |
| 10.1 Music therapy studies | 2 | 104 | Std. Mean Difference (IV, Random, 95% CI) | 0.37 [‐0.13, 0.87] |
| 10.2 Music medicine studies | 3 | 132 | Std. Mean Difference (IV, Random, 95% CI) | 0.55 [‐0.37, 1.47] |
| 11 Pain Show forest plot | 7 | 528 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.91 [‐1.46, ‐0.36] |
| 12 Pain (music preference) Show forest plot | 6 | 496 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.92 [‐1.53, ‐0.30] |
| 12.1 Patient‐preferred music | 4 | 320 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.06 [‐1.93, ‐0.20] |
| 12.2 Researcher‐selected music | 2 | 176 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.59 [‐1.34, 0.15] |
| 13 Fatigue Show forest plot | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 13.1 All studies | 6 | 253 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.72, ‐0.04] |
| 13.2 Sensitivity analysis | 5 | 203 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.48, 0.08] |
| 14 Physical functioning Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 14.1 All studies | 4 | 493 | Std. Mean Difference (IV, Random, 95% CI) | 0.78 [‐0.74, 2.31] |
| 14.2 Sensitivity analysis | 3 | 233 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.18, 0.34] |
| 15 Heart rate Show forest plot | 8 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 15.1 All studies | 8 | 589 | Mean Difference (IV, Random, 95% CI) | ‐3.32 [‐6.21, ‐0.44] |
| 15.2 Sensitivity analysis | 6 | 339 | Mean Difference (IV, Random, 95% CI) | ‐4.63 [‐8.18, ‐1.09] |
| 16 Heart rate (music preference) Show forest plot | 7 | 539 | Mean Difference (IV, Random, 95% CI) | ‐3.77 [‐6.97, ‐0.58] |
| 16.1 Patient‐preferred music | 5 | 479 | Mean Difference (IV, Random, 95% CI) | ‐3.13 [‐6.54, 0.27] |
| 16.2 Researcher‐selected music | 2 | 60 | Mean Difference (IV, Random, 95% CI) | ‐7.94 [‐15.10, ‐0.78] |
| 17 Respiratory rate Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 17.1 All studies | 4 | 437 | Mean Difference (IV, Random, 95% CI) | ‐1.24 [‐2.54, 0.06] |
| 17.2 Sensitivity analysis | 3 | 237 | Mean Difference (IV, Random, 95% CI) | ‐1.83 [‐3.36, ‐0.30] |
| 18 Systolic blood pressure Show forest plot | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 18.1 All studies | 7 | 559 | Mean Difference (IV, Random, 95% CI) | ‐5.40 [‐8.32, ‐2.49] |
| 18.2 Sensitivity analysis | 5 | 309 | Mean Difference (IV, Random, 95% CI) | ‐7.63 [‐10.75, ‐4.52] |
| 19 Systolic blood pressure (music preference) Show forest plot | 6 | 509 | Mean Difference (IV, Random, 95% CI) | ‐6.29 [‐8.86, ‐3.72] |
| 19.1 Patient‐preferred music | 4 | 449 | Mean Difference (IV, Random, 95% CI) | ‐6.65 [‐10.07, ‐3.23] |
| 19.2 Researcher‐selected music | 2 | 60 | Mean Difference (IV, Random, 95% CI) | ‐4.72 [‐10.80, 1.37] |
| 20 Diastolic blood pressure Show forest plot | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 20.1 All studies | 7 | 559 | Mean Difference (IV, Random, 95% CI) | ‐2.35 [‐5.88, 1.18] |
| 20.2 Sensitivity analysis | 5 | 309 | Mean Difference (IV, Random, 95% CI) | ‐4.94 [‐7.78, ‐2.09] |
| 21 Diastolic blood pressure (music preference) Show forest plot | 6 | 509 | Mean Difference (IV, Random, 95% CI) | ‐3.74 [‐7.53, 0.05] |
| 21.1 Patient‐preferred music | 4 | 449 | Mean Difference (IV, Random, 95% CI) | ‐4.10 [‐8.78, 0.59] |
| 21.2 Researcher‐selected music | 2 | 60 | Mean Difference (IV, Random, 95% CI) | ‐2.01 [‐6.26, 2.25] |
| 22 Oxygen Saturation Show forest plot | 3 | 292 | Mean Difference (IV, Random, 95% CI) | 0.50 [‐0.18, 1.18] |
| 23 Quality of Life Show forest plot | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 23.1 All studies | 6 | 545 | Std. Mean Difference (IV, Random, 95% CI) | 0.98 [‐0.36, 2.33] |
| 23.2 Sensitivity analysis | 4 | 241 | Std. Mean Difference (IV, Random, 95% CI) | 0.52 [0.01, 1.02] |
| 24 Quality of life (intervention subgroup) Show forest plot | 5 | 568 | Std. Mean Difference (IV, Random, 95% CI) | 0.99 [‐0.34, 2.31] |
| 24.1 Music therapy studies | 3 | 132 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [0.06, 0.78] |
| 24.2 Music medicine studies | 2 | 436 | Std. Mean Difference (IV, Random, 95% CI) | 1.33 [‐0.96, 3.63] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Anxiety Show forest plot | 2 | 166 | Mean Difference (IV, Fixed, 95% CI) | ‐3.67 [‐11.68, 4.35] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Distress Show forest plot | 2 | Mean Difference (Random, 95% CI) | ‐0.07 [‐0.39, 0.26] | |
| 2 Spiritual well‐being Show forest plot | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.31 [‐0.11, 0.73] | |

