Técnicas perineales durante el período expulsivo del trabajo de parto para reducir el traumatismo perineal
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en espera de evaluación
Referencias adicionales
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT. Procedure: computer‐generated block randomisation (1:1:1 within balanced blocks). Unit of randomisation: women in midwifery care were recruited antenatally but randomised in active labour when vaginal delivery appeared likely. | |
| Participants | 1211 women were included. Inclusion criteria: patients in midwifery care, 18 years or older, healthy, expecting a vaginal birth, no medical complications, a singleton vertex presentation at term. Exclusion criteria: those who did not meet the inclusion criteria. | |
| Interventions | Experimental interventions: Compresses versus hands off and massage versus hands off. 1) Warm compresses were held continuously to the mother’s perineum and external genitalia by the midwife’s gloved hand during and between pushes, regardless of mother’s position. 2) Perineal massage with lubricant was gentle, slow massage, with 2 fingers of the midwife’s gloved hand moving from side to side just inside the patient’s vagina. Mild, downward pressure (toward the rectum) was applied with steady, lateral strokes, which lasted 1 second in each direction. This motion precluded rapid strokes or sustained pressure. A sterile, water‐soluble lubricant was used to reduce friction with massage. Massage was continued during and between pushes, regardless of maternal position and the amount of downward pressure was dictated by the woman’s response. Comparison: 3) No touch the woman’s perineum until crowning of the infant’s head. | |
| Outcomes | Primary outcome was intact perineum (defined as no tissue separation at any site). Secondary outcomes: episiotomy, degree of trauma (1st, 2nd, 3rd, 4th), location of trauma (vaginal, labial, periurethral, clitoral, cervical), trauma sutured and from the postpartum visit: presence of anatomic abnormalities, faulty healing of childbirth lacerations, and continued perineal pain. Reported as postpartum perineal problems. | |
| Notes | Contact with the author did not supply us with further information of secondary outcome such as breastfeeding, maternal satisfaction with birth, stress incontinence or dyspareunia. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated, ratio 1:1:1 within balanced blocks. |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, sealed, opaque envelopes were prepared by the data manager and study administrator and stored in metal box in a restricted area at the hospitals labour unit. The clinical midwife selected the lowest numbered envelope once vaginal birth appeared likely. The envelope contained a card with the study group allocation. When the envelope was drawn, the midwife signed the study register and noted date and time. |
| Blinding (performance bias and detection bias) | High risk | It was not possible to blind the intervention for the participant or the clinician. The outcome assessment was done by the midwife that performed the delivery, and thus not blinded, but to counter this potential bias, a random 25% of the study births had a 2nd midwife observer present (additional information by contact with the author). |
| Incomplete outcome data (attrition bias) | Low risk | There were no loss to follow‐up for primary outcome after randomisation. Some (88 + 79 + 79) lost to follow‐up for data from the postpartum visit. There was no exclusion after randomisation. The analysis was intention to treat. |
| Selective reporting (reporting bias) | Unclear risk | There is no description of what healthy and no medical problems means. A suggestion in the article: concealment of the allocated perineal strategy from the clinical midwife was not possible ‐ therefore a potential for reporting bias in data collection immediate after birth was a possibility. |
| Other bias | Low risk | Very low episiotomy rate at baseline, under 1%. They also have a high baseline of intact perineum compared to most others. |
| Methods | RCT. | |
| Participants | 106 women were included. Inclusion criteria: no previous vaginal births; age ≧ 15 years, gestational age 37‐ 41 6/7weeks, live single cephalic fetus with no abnormality detected, uterine height no more than 36 cm, cervical dilatation of 5 cm or less, no perineal preparation during pregnancy, no infection in the perineum, agree to use the lateral left size position during delivery. Exclusion criteria: use of oxytocin, obstetrical conditions during labor and delivery which required intervention as episiotomy, forceps and caesarean. Nulliparous women. | |
| Interventions | Experimental intervention: petroleum jelly was applied to the entire area of the perineum with 2 fingers, using a sweeping motion. The clitoris, labia majora, labia minora, vestibule, fourchet and perineal body were covered with 30 ml of the lubricant without any stretching or massage of the complete cervical dilatation until the beginning of the cephalic delivery. It was done time after time from the complete cervical dilatation until the beginning of the cephalic delivery. Control/comparison intervention: routine care, did not receive the jelly. | |
| Outcomes | Perineal conditions: frequency, intact perineum or trauma, degree of trauma (1st, 2nd ) and location (posterior or anterior or both). Newborn outcomes: Apgar score. Expulsive period length: the time between full cervical dilatation to fetal delivery. | |
| Notes | We contacted the author and were provided with more information on why the inclusion took so long time, on details on the application of the jelly on the perineum and of the routine care in the hospital. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation was computer‐generated random numbers |
| Allocation concealment (selection bias) | Low risk | The nurse‐midwifes were informed about which group (control or experimental) the woman was allocated by the researcher when the woman was in the expulsive period. |
| Blinding (performance bias and detection bias) | High risk | |
| Incomplete outcome data (attrition bias) | Low risk | 106 were assessed for eligibility at stage 1, 3 excluded because of exclusion criteria (2) and lack of consent (1). After randomisation:15 excluded from the intervention and 12 from the control group because of episiotomy. |
| Selective reporting (reporting bias) | Low risk | |
| Other bias | Low risk | Very few women followed the eligibility criteria: 106 of > 600 primiparas. |
| Methods | RCT. Randomly generated numbers with participants being stratified into 6 subgroups by age and ethnicity. Unit of randomisation: nulliparous women in the late second stage of labour. Pregnant women were asked at the antenatal clinics or in the labour ward if they were not in labour. | |
| Participants | 717 women were included. Inclusion criteria: nulliparous women, at least 36 weeks' pregnant, singleton pregnancy with a cephalic presentation; anticipated a normal birth, who had not performed perineal massage antenatally and were older than 16 years. Exclusion criteria: women not fulfilling the inclusion criteria and those women who experienced intrauterine fetal death. The 6 strata were: Asian younger than 25, non‐Asian younger than 25, Asian 25 to 34 years old, non‐Asian 24 to 34 years old, Asian older than 34 and non‐Asian older than 34. | |
| Interventions | Experimental intervention: 1) warm packs/pads on the perineum as the baby's had began to distend the perineum and the woman was aware of a stretching sensation. A sterile pad was soaked in a metal jug with boiled tap water (between 45 and 59 degrees C) then wrung out and gently placed on the perineum during contractions. The pad was re‐soaked to maintain warmth between contractions. The water in the jug was replaced every 15 min until delivery. Comparison: standard group which did not have warm pack applied to their perineum in second stage. | |
| Outcomes | Primary outcome was suturing after birth (defined as perineal trauma greater than first‐degree tear, any tear that was bleeding and any tear that did not fall into anatomical apposition). Secondary outcomes: degree of trauma divided into minor or no trauma (intact, 1st degree, vaginal/labial tear), major trauma (2nd, 3rd, 4th degree and episiotomy), episiotomy and severe perineal trauma including 3rd and 4th degree tears. Other secondary outcome: pain when giving birth, and perineal pain on day 1 and 2, at 6 weeks and 3 months and urinary incontinence, sexual intercourse and breastfeeding. | |
| Notes | We contacted the author and asked for additional information according to more detailed data on the perineal trauma and for this reviews secondary outcomes but such data were not available. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation by the National Health and Medical Research Clinical Trials Centre using randomly generated numbers. The article does not state if this was computer generated, but it is perfectly possible to randomly generate numbers without a computer. |
| Allocation concealment (selection bias) | Low risk | Randomisation by the National Health and Medical Research Clinical Trials Centre using randomly generated numbers. Sealed, opaque envelopes at the National Health and Medical Research Clinical Trials Centre kept at the neonatal intensive care unit to ensure remote allocation concealment, with randomisation occurring as close as possible to second stage of labour. |
| Blinding (performance bias and detection bias) | High risk | It was not possible to blind the intervention for the participant or the clinician. An independent, senior midwife, blinded to the allocation group, was asked to give an independent assessment of the degree of perineal trauma after birth and whether or not suturing was required. Midwives were instructed not to let the other midwives know the allocation. For this purpose the equipment for the intervention was set up for every woman in the trial regardless of allocated group. |
| Incomplete outcome data (attrition bias) | Low risk | No loss of outcome data for the primary outcome. However, some loss of data for pain scores. No participants were excluded after randomisation, but in both groups a number of women did not receive the care they were allocated to due to surgical intervention. A couple refused the allocated treatment. 1 gave birth too fast, 1 delivered in water and 1 received the intervention treatment while allocated to standard care. The analysis was intention to treat. |
| Selective reporting (reporting bias) | Low risk | |
| Other bias | Low risk | Took a long time to include enough participants, from 1997 to 2004. Recruitment stopped at 717, only 599 women actually received the allocated treatment. 95 less than required by the power calculation. In the flow chart it is stated that 1047 were assessed for eligibility while only 717 were randomised. The main reason for not randomising was that midwives were too busy. It is difficult to know if this introduced bias. It was difficult to differentiate between intact perineum and trauma. The classification of the degree of perineal trauma makes it difficult to compare to other studies. |
| Methods | RCT. Prosedyre: electronically produced randomised tables. Unit of randomisation: pregnant nulliparous women in labour. | |
| Participants | 70 women were included. A hospital birth centre, in Etapecerica de Serra, Brazil. Low‐risk pregnancies receive antenatal care in the basic healthcare units. The birth centre has an average of 403 deliveries a month (71% vaginal birth), and nurse‐midwives attend 100% of the births. Inclusion criteria: primiparous expectant mothers aged 15 to 35, full‐term pregnancies and vertex presentation. On admission: uterine height more than 36 cm, cervical dilatation 8 cm or less, intact membranes. Additional limitations were that labour did not exceed 12 hours after hospitalisation, no use of oxytocin during the first or second stage of labour, no perineal preparation during pregnancy or no episiotomy. Exclusion criteria: women were excluded if there was dystocia requiring any other procedure than those described in the detailed description of the 2 methods compared. Women were excluded if they chose to deliver in the lithotomy position, if they had a caesarean section, if there were any abnormalities during labour related to fetal distress. | |
| Interventions | Experimental intervention: hands off: during the expulsive period, the nurse‐midwife’s conduct is exclusively expectant, only observing the successive movements of restitution, external rotation, delivery of the shoulders and the remainder of the body. During delivery, the nurse‐midwife should support the baby's head with one hand and the baby's torso with the other hand. If external rotation of the head or delivery of the shoulders does not occur spontaneously within 15 seconds of the delivery of the head, or if the newborn appear hypoxic, the professional must manually rotate the head by grasping it and applying gentle downward tracking. Once the anterior shoulder is delivered, gentle upward traction is used to deliver the posterior shoulder. After the shoulders have been delivered, the newborn's neck is held with one hand, while the other hand follows along the infant's back, and the legs or feel are grasped as they are delivered. Comparison: hands on: when the infant's head is crowning, the nurse‐midwife places the index, middle ring and little fingers of the left hand close together on the infant's occiput, with the palm turned toward the anterior region of the perineum. In this manner, expulsion is controlled, by maintaining the flexion of the head, protecting the anterior region of the perineum and bilaterally supporting the ischio‐cavernous and bulbo‐ cavernous muscles, the urethral introitus, and the labia majora and minora. Simultaneously, the right hand is flattened out and placed on the posterior perineum, with the index finger and the thumb, forming a "U" shape, exerting pressure on the posterior region of the perineum during the crowning process. The nurse‐midwife leaves no area without protection, particularly the region of the fourchette. During the delivery of the shoulders and the remainder of the body, the right hand is kept in place, protecting the posterior region of the perineum, while the left hand supports the infant's head, allowing external rotation and the delivery of the shoulders spontaneously. If this does not occur, the professional continues with posterior perineal pressure, and with the left hand, pulls gently downward to deliver the anterior shoulder. Once the anterior shoulder is delivered, gentle traction is applied upward to ease delivery of the posterior shoulder. After both shoulders have been delivered, the practitioner removes the right hand from the posterior perineum and supports the infant's neck with one hand, while supporting the remainder of the body with the other hand. In both techniques, the women are allowed to push spontaneously during labour, without being directed in bearing down efforts, responding to involuntary contractions of the abdominal muscles. | |
| Outcomes | 1) Perineal conditions (frequency, degree (intact perineum, 1st, 2nd, 3rd and 4th), and location of perineal laceration) 2) newborn outcomes, Apgar score, length of second stage. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Electronically produced randomised table. It is not clear when randomisation took place (those with episiotomy excluded?). |
| Allocation concealment (selection bias) | Unclear risk | Electronically produced randomised table. The researchers supervised both allocation to groups and delivery technique. Insufficient information about concealment. It is not clear when randomisation took place. Not intention to treat for 16 women who were included at first. |
| Blinding (performance bias and detection bias) | High risk | Nurse‐midwives attended the births and filled out the data collection forms after each birth. |
| Incomplete outcome data (attrition bias) | Unclear risk | 16 women were excluded after first meeting the inclusion criteria and presumably having been included first, women receiving an episiotomy, women who chose to give birth in an lithotomy position, possibly also some women receiving oxytocin after randomisation and some with fetal distress. The analysis was not intention to treat as women with an episiotomy were not included in the analysis. Presumably randomisation took place before that. |
| Selective reporting (reporting bias) | Unclear risk | There is no report on the 16 women excluded after inclusion? Why were they excluded. Which group did they belong to? Are the results of this study generalis able after so many exclusion criteria? Extreme selection. |
| Other bias | Low risk | |
| Methods | RCT. Unit of randomisation: women in the beginning of the second stage of labour at full cervical dilatation. | |
| Participants | 1575 women were included. Inclusion criteria: eligible for the study were primigravida, women with singleton pregnancy, fetus in cephalic presentation, admitted for labour, rupture of the membranes or induction after 37 weeks. Women were asked for consent on admission in labour. Exclusion criteria: instrumental deliveries, emergency caesarean deliveries, parous women and preterm deliveries that had been erroneously included. | |
| Interventions | Experimental intervention: modified Ritgen's manoeuvre: lifting the fetal chin interiorly, using the fingers of one hand placed between anus and coccyx, and thereby extending the fetal neck, whereas the other hand should be place on the fetal occiput to control the pace of expulsion of the fetal head. The maneuver was used during a uterine contraction. Control/comparison intervention: the standard practice at delivery was using one hand to apply pressure against the perineum, and the other hand on the fetal occiput to control the expulsion of the fetal head. Standard practice was also to perform a lateral episiotomy only on indication. | |
| Outcomes | The rate of third‐to fourth‐degree perineal ruptures including external anal sphincter. | |
| Notes | We contacted the author and asked for additional information according to more data on the perineal trauma (intact perineum, perineal trauma not requiring suturing, perineal trauma requiring suturing, 1st‐ and 2nd‐degree tear) but these data were not registered in the study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The allocated randomisation was registered in an existing clinical data base, containing information of all deliveries at the 2 units. |
| Allocation concealment (selection bias) | Low risk | The allocated randomisation was registered in an existing clinical data base, containing information of all deliveries at the 2 units. Randomisation was done at the beginning of the second stage of labour (at full cervical dilatation) at each unit by a phone call from the delivering midwife to the other department, where randomisation lists with number of allocation were kept. |
| Blinding (performance bias and detection bias) | High risk | Blinding of the clinician and the patient is not discussed in the article. The diagnosis and initial grading of perineal ruptures were primarily made by the delivering midwives. If the midwife suspected involvement of the anal sphincter, or if she was in doubt, she called the obstetrician on duty. |
| Incomplete outcome data (attrition bias) | Low risk | There is a flowchart in the article that describes any loss to follow‐up. The flow chart describes the excluded participants: failure in the randomisation itself is also described in detail. After randomisation: 71 women were excluded from the intervention group (7 because of caesarean delivery, 64 instrumental delivery) 81 women were excluded from the control group after randomisation (3 because of caesarean delivery, 78 instrumental delivery). For the remaining 1423 women, the results were analysed according to intention to treat. |
| Selective reporting (reporting bias) | Low risk | |
| Other bias | Low risk | |
| Methods | Quasi‐randomised study. Women were randomised according to date of delivery (even or odd day). Unit of randomisation: pregnant women entering the second stage of delivery. | |
| Participants | 1161 women were included. Inclusion criteria: all women with an uncomplicated pregnancy and cephalic presentation, normal first and second stages of labour, gestational age > 37 weeks. Exclusion criteria: women with multiple pregnancy, non‐cephalic presentation, caesarean section, forceps, vacuum, planned birth in water, visible perineal scar, language difficulties, gestation < 37 weeks. | |
| Interventions | Experimental intervention: the midwife keeps her hands poised, ready to put light pressure on the infants head to avoid rapid expulsion. However, in contrast to the hands‐on method, the midwife does not touch the perineum with her right hand at any time during delivery. Delivery of the shoulders is supported with both of the midwife’s hands. Control/comparison intervention: hands on method: the left hand of the midwife puts pressure on the infants head in the belief that flexion will be increased. The right hand is placed against the perineum to support this structure and to use lateral flexion to facilitate delivery of the shoulders. | |
| Outcomes | Maternal outcomes: perineal tear,1st , 2nd 3rd degree, vaginal, labial, episiotomy (median or lateral). Neonatal outcomes: infant birthweight, length, head diameter, infant shoulders, Apgar score (1 min < 7, 5 min < 7) and cord pH < 7.1). (All perineal trauma were confirmed by an experienced obstetrician‐gynaecologist.) | |
| Notes | We tried to contact the author and asked for supplementing information but did not succeed. We would like to know what the authors meant by "visible perineal scar" and for information of "perineal trauma requiring suturing", whether they had calculated the mean and the standard deviation of the length of second stage and how they defined the length of the second stage. We also asked for more details on the differences between the groups for the characteristics in table 1 and how the authors defined "normal in the first and the second stage. In addition, were the women with augmented labour, continuous fetal monitoring and prolonged labour excluded from the study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomised according to the date of delivery. On even days and odd days. Noon as a break point of randomisation. Women entering the second stage of labour before noon and delivering after noon were treated according to the randomisation policy of the previous day. Quasi‐randomisation. |
| Allocation concealment (selection bias) | High risk | Randomised according to the date of delivery. On even days and odd days. Noon as a break point of randomisation. Women entering the second stage of labour before noon and delivering after noon were treated according to the randomisation policy of the previous day. There was no concealment. |
| Blinding (performance bias and detection bias) | High risk | It was not blinded for the participant: for the clinician blinding was not possible. For the outcome assessor it is unclear whether it was blinded. All perineal tears were confirmed by an experienced obstetrician. |
| Incomplete outcome data (attrition bias) | Low risk | Data were missing from 85 women (40 + 45) = 5, 6% of the total number of deliveries. Due to incomplete study forms. Describe any exclusion of participants after randomisation: the analyses were performed according to group assignment irrespective of the form of perineal care delivered, i.e. Intention to treat. |
| Selective reporting (reporting bias) | Unclear risk | It is not possible to extract from the article if the primiparas was divided equally between groups. It is unclear if there are significant differences between the groups for the characteristics in table 1 (characteristics of the clinical population). |
| Other bias | Low risk | |
| Methods | RCT. Block randomisation, with blocks of 4 to 8, stratified by centre. Unit of randomisation: pregnant women at the end of the second stage when the midwife considered a vaginal birth imminent. | |
| Participants | 5471 women were included. Recruitment and randomisation happened at 2 hospitals, both National Health Service hospitals in England (not private but for the general public funded by the state). Both hospitals had approximately 5500 births a year. Inclusion criteria: women with a singleton pregnancy with cephalic presentation, anticipating a normal birth giving consent antenatally. Exclusion criteria: women planning to have a water birth, women who had an elective episiotomy prescribed, women planning adoption. Women were excluded on admission if they gave birth before 37 weeks' gestation. | |
| Interventions | Experimental intervention: hands poised method in which the midwife keeps her hands poised, prepared to put light pressure on the baby’s head in case of rapid expulsion, but not to touch the head or perineum otherwise and to allow spontaneous delivery of the shoulders. Control/comparison intervention: hands on method in which the midwife’s hands are used to put pressure on the baby’s head in the belief that flexion will be increased, and to support (guard) the perineum, and to use lateral flexion to facilitate the delivery of the shoulders. | |
| Outcomes | Primary outcome was perineal pain in the previous 24 hours reported by the mother 10 days after birth (formed the basis for the power calculation). Other outcomes recorded: perineal trauma, if trauma was sutured, perineal pain at around 2 days and 3 months after birth, dyspareunia at 3 months, urinary and bowel problems at 10 days and 3 months and breastfeeding at 10 days and 3 months. For the newborn the Apgar score, if applicable type of resuscitation given, admission with reason for the admission were recorded. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Details of the allocated group were given on coloured cards contained in sequentially numbered, opaque, sealed envelopes. Prepared at the National Perinatal Epidemiology Unit and kept in an agreed location on each labour ward. To enter a woman into the study the midwife opened the next consecutively numbered envelope. If an envelope was not opened, the reason for non‐use was recorded by the midwife who had drawn it. All envelopes, whether used or not were returned to the NPEU. Unopened but not used envelopes were not returned to the unit. |
| Allocation concealment (selection bias) | Low risk | Details of the allocated group were given on coloured cards contained in sequentially numbered, opaque, sealed envelopes, prepared at the National Perinatal Epidemiology Unit and kept in an agreed location on each labour ward. To enter a woman into the study the midwife opened the next consecutively numbered envelopes. If an envelope was not opened, the reason for non‐use was recorded by the midwife who had drawn it. All envelopes, whether used or not were returned to the NPEU. Unopened but not used envelopes were not returned to the unit. |
| Blinding (performance bias and detection bias) | High risk | Women were not told which group they ended up in but the information was given at the woman’s request, this was noted in the trial data form. About a third of the women were informed of their allocation. Outcome assessor: the main outcome was pain at 10 days after birth as reported by women through a questionnaire. Even though women may not have asked the midwife about allocation she may have felt or noticed what the midwife did with her hands. The other outcome such as degree of perineal trauma and condition of the newborn at birth was presumably recorded by the midwife who did the delivery and knew the allocation. |
| Incomplete outcome data (attrition bias) | Low risk | During the study period, 18,458 deliveries took place. There is a detailed flow chart that describes the excluded participants. The reasons for not being randomised were: Not recruited ante natally, planned instrumental delivery or Caesarean section, maternal refusal, non‐cephalic presentation, multiple pregnancy, planned birth in water, intrauterine death, episiotomy prescribed and other. However 5471 (29.6%) women were randomised into experimental group 2740 and controls 2731. There was no exclusion after randomisation. The analysis was intention to treat. |
| Selective reporting (reporting bias) | Low risk | The article is very open about all aspects of interest. |
| Other bias | Low risk | |
| Methods | RCT 1:1, prepared batches of 100. Stratification for nulliparous and multiparous women. Unit of randomisation: women in uncomplicated labour having progressed to either visible vertex, full dilatation or 8 cm or more if nulliparous and 5 cm or more if multiparous. | |
| Participants | 1340 women were included. From 3 hospitals in Australia with 7000 births per year (presumably the 3 together and not at each hospital). It took nearly 3 years to collect the data. From March 1995 to January 1998. Inclusion criteria: women who at 36 weeks of pregnancy had given written consent while expecting a normal vaginal birth of a single baby and who presented in uncomplicated labour having progressed to either visible vertex, full dilatation or 8 cm or more if nulliparous and 5 cm or more if multiparous. English speaking. Exclusion criteria: not specified specifically. | |
| Interventions | Experimental intervention: massage and stretching of the perineum with each contraction during the second stage of labour. The midwife inserted 2 fingers inside the vagina and using a sweeping motion, gently stretched the perineum with water soluble lubricating jelly, stopping if it was uncomfortable. Control/comparison intervention: the midwife’s usual technique but refraining from perineal massage. | |
| Outcomes | Main outcome was intact perineum. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Envelopes were sequentially numbered, prepared by a research assistant not involved in care of the women. It appears that each hospital had their own boxes for nulliparous and multiparous women. |
| Allocation concealment (selection bias) | Low risk | Envelopes were sequentially numbered, prepared by a research assistant not involved in care of the women. It appears that each hospital had their own boxes for nulliparous and multiparous women. To find out allocation the midwife had to ring to the emergency department were the duty midwife or clerk opened the next double packed, sealed envelope. |
| Blinding (performance bias and detection bias) | High risk | It was not possible to blind the intervention for the participant or the clinician. Data on outcome by an independent caregiver were available in 1053 (79%) of the cases. |
| Incomplete outcome data (attrition bias) | Low risk | 3050 eligible women were approached. However, in that period about 19,000 women gave birth at these 3 hospitals. It appears likely that quite a number of eligible women were not asked. Of the 2291 who consented only 1340 were randomised. The reasons for not randomising women were as follows: 217 caesarean section, 105 instrumental birth, 168 no reason, 112 women changed their mind, 121 rapid progress, 77 midwife forgot, 80 midwife too busy, 71 other reasons. There were no exclusions after randomisation. The analyses was performed according to intention to treat. |
| Selective reporting (reporting bias) | Low risk | |
| Other bias | Low risk | |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| This randomised controlled trial did not have perineal tear as an outcome and therefore not suitable for this review. Besides this is only a small abstract and too little methodological information. | |
| This study is presented as a short abstract and investigated the usefulness of perineal lubrication in decreasing the episiotomy rates in primiparous women. It is excluded from our review because there was insufficient information about methodological issues. | |
| This RCT was conducted to evaluate the effect of perineal preservation and heat application during second stage of labour. It is excluded from our review because of methodological weaknesses, especially in the procedure of randomisation and lack of reporting of outcome. | |
| This RCT was conducted to determine whether obstetric gel shortened the second stage of labour or exerted a protective effect on the perineum. It is not a perineal technique in the second stage of labour and therefore not suitable for this review. |
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Prospective, randomised double blind study. |
| Participants | 164 women undergoing vaginal deliveries between July 2008 and July 2009. Multiple gestations excluded. |
| Interventions | Liquid wax (jojoba oil) versus purified formula of almond and olive oil, enriched with vitamin B1, B6 E and fatty acids. |
| Outcomes | Perineal lacerations, number of sutures and length of suturing. |
| Notes | This randomised controlled trial was presented as a poster. |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 3rd or 4th degree tears Show forest plot | 3 | 6617 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.21, 2.56] |
| Analysis 1.1  Comparison 1 Hands off (or poised) versus hands on, Outcome 1 3rd or 4th degree tears. | ||||
| 2 Episiotomy Show forest plot | 2 | 6547 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.50, 0.96] |
| Analysis 1.2  Comparison 1 Hands off (or poised) versus hands on, Outcome 2 Episiotomy. | ||||
| 3 Intact perineum Show forest plot | 2 | 6547 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.95, 1.12] |
| Analysis 1.3  Comparison 1 Hands off (or poised) versus hands on, Outcome 3 Intact perineum. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 3rd or 4th degree tears Show forest plot | 2 | 1525 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.28, 0.84] |
| Analysis 2.1  Comparison 2 Warm compresses versus control (hands off or no warm compress), Outcome 1 3rd or 4th degree tears. | ||||
| 2 Episotomy Show forest plot | 2 | 1525 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.62, 1.39] |
| Analysis 2.2  Comparison 2 Warm compresses versus control (hands off or no warm compress), Outcome 2 Episotomy. | ||||
| 3 Intact perineum Show forest plot | 2 | 1525 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.86, 1.26] |
| Analysis 2.3  Comparison 2 Warm compresses versus control (hands off or no warm compress), Outcome 3 Intact perineum. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 3rd or 4th degree tears Show forest plot | 2 | 2147 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.29, 0.94] |
| Analysis 3.1  Comparison 3 Massage versus control (hands off or care as usual), Outcome 1 3rd or 4th degree tears. | ||||
| 2 Episiotomy Show forest plot | 2 | 2147 | Risk Ratio (M‐H, Random, 95% CI) | 1.42 [0.42, 4.87] |
| Analysis 3.2  Comparison 3 Massage versus control (hands off or care as usual), Outcome 2 Episiotomy. | ||||
| 3 Intact perineum Show forest plot | 2 | 2147 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.90, 1.20] |
| Analysis 3.3  Comparison 3 Massage versus control (hands off or care as usual), Outcome 3 Intact perineum. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 3rd degree tears Show forest plot | 1 | 1423 | Risk Ratio (M‐H, Random, 95% CI) | 1.42 [0.86, 2.36] |
| Analysis 4.1  Comparison 4 Ritgen's manoeuvre versus standard care, Outcome 1 3rd degree tears. | ||||
| 2 4th degree tears Show forest plot | 1 | 1423 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.18, 2.03] |
| Analysis 4.2  Comparison 4 Ritgen's manoeuvre versus standard care, Outcome 2 4th degree tears. | ||||
| 3 3rd or 4th degree tears Show forest plot | 1 | 1423 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.78, 1.96] |
| Analysis 4.3  Comparison 4 Ritgen's manoeuvre versus standard care, Outcome 3 3rd or 4th degree tears. | ||||
| 4 Episiotomy Show forest plot | 1 | 1423 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.63, 1.03] |
| Analysis 4.4  Comparison 4 Ritgen's manoeuvre versus standard care, Outcome 4 Episiotomy. | ||||
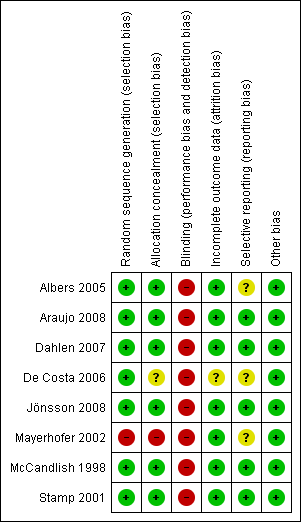
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.

Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.

Comparison 1 Hands off (or poised) versus hands on, Outcome 1 3rd or 4th degree tears.

Comparison 1 Hands off (or poised) versus hands on, Outcome 2 Episiotomy.

Comparison 1 Hands off (or poised) versus hands on, Outcome 3 Intact perineum.

Comparison 2 Warm compresses versus control (hands off or no warm compress), Outcome 1 3rd or 4th degree tears.

Comparison 2 Warm compresses versus control (hands off or no warm compress), Outcome 2 Episotomy.

Comparison 2 Warm compresses versus control (hands off or no warm compress), Outcome 3 Intact perineum.

Comparison 3 Massage versus control (hands off or care as usual), Outcome 1 3rd or 4th degree tears.
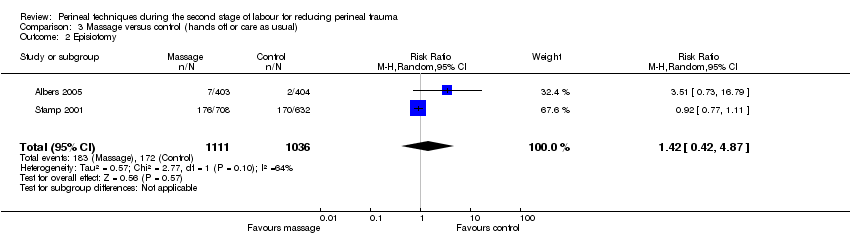
Comparison 3 Massage versus control (hands off or care as usual), Outcome 2 Episiotomy.

Comparison 3 Massage versus control (hands off or care as usual), Outcome 3 Intact perineum.

Comparison 4 Ritgen's manoeuvre versus standard care, Outcome 1 3rd degree tears.

Comparison 4 Ritgen's manoeuvre versus standard care, Outcome 2 4th degree tears.

Comparison 4 Ritgen's manoeuvre versus standard care, Outcome 3 3rd or 4th degree tears.

Comparison 4 Ritgen's manoeuvre versus standard care, Outcome 4 Episiotomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 3rd or 4th degree tears Show forest plot | 3 | 6617 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.21, 2.56] |
| 2 Episiotomy Show forest plot | 2 | 6547 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.50, 0.96] |
| 3 Intact perineum Show forest plot | 2 | 6547 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.95, 1.12] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 3rd or 4th degree tears Show forest plot | 2 | 1525 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.28, 0.84] |
| 2 Episotomy Show forest plot | 2 | 1525 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.62, 1.39] |
| 3 Intact perineum Show forest plot | 2 | 1525 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.86, 1.26] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 3rd or 4th degree tears Show forest plot | 2 | 2147 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.29, 0.94] |
| 2 Episiotomy Show forest plot | 2 | 2147 | Risk Ratio (M‐H, Random, 95% CI) | 1.42 [0.42, 4.87] |
| 3 Intact perineum Show forest plot | 2 | 2147 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.90, 1.20] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 3rd degree tears Show forest plot | 1 | 1423 | Risk Ratio (M‐H, Random, 95% CI) | 1.42 [0.86, 2.36] |
| 2 4th degree tears Show forest plot | 1 | 1423 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.18, 2.03] |
| 3 3rd or 4th degree tears Show forest plot | 1 | 1423 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.78, 1.96] |
| 4 Episiotomy Show forest plot | 1 | 1423 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.63, 1.03] |

