Isoniazida para la prevención de la tuberculosis en niños con infección por VIH
Información
- DOI:
- https://doi.org/10.1002/14651858.CD006418.pub3Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 29 agosto 2017see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Enfermedades infecciosas
- Clasificada:
-
- Actualizada
All studies incorporated from most recent search
All eligible published studies found in the last search (17 Feb, 2017) were includedEvaluada: 12 April 2019
- Actualizada
- Copyright:
-
- Copyright © 2017 The Authors. Cochrane Database of Systematic Reviews published by John Wiley & Sons, Ltd. on behalf of The Cochrane Collaboration.
- This is an open access article under the terms of the Creative Commons Attribution‐Non‐Commercial Licence, which permits use, distribution and reproduction in any medium, provided the original work is properly cited and is not used for commercial purposes.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
-
DG was the lead author for the first version of the review.
-
DG and HZ conducted the search and scrutinized identified studies for eligibility.
-
DG and TY assessed the methodological quality of included studies.
-
All authors critically reviewed the manuscript before submission (initial review).
-
MZ was the lead author of the review update.
-
MZ and TY screened the search results and assessed potential studies for eligibility.
-
MZ and a research assistant assessed the methodological quality of included studies.
-
DG, MC, and HZ critically reviewed the manuscript for content (review update). All authors approved the final version of the review.
Sources of support
Internal sources
-
Liverpool School of Tropical Medicine, UK.
External sources
-
HIV/AIDS mentoring programme, South African Cochrane Centre, South Africa.
-
Cochrane Child Health Field Bursary, Canada.
-
Department for International Development, UK. Research Programme Grant, UK.
Grant: 5242
Declarations of interest
MZ: MZ is supported by the Effective Health Care Research Consortium funded by UK aid from the UK Government for the benefit of developing countries (Grant: 5242). The views expressed in this publication do not necessarily reflect UK government policy.
DG: Author of an included study
TY: TY is supported by the Effective Health Care Research Consortium funded by UK aid from the UK Government for the benefit of developing countries (Grant: 5242). The views expressed in this publication do not necessarily reflect UK government policy.
MC: Author of an included study
HZ: Author of an included study
To avoid potential bias, authors who were investigators on included studies did not do data extraction and methodological quality assessment of included studies.
Acknowledgements
We thank Paul Garner, Co‐ordinating Editor of the Cochrane Infectious Diseases Group (CIDG), for his guidance. We thank Olatunji Adetokunboh (OA) who assisted with data extraction and assessment of risk of bias.
Moleen Zunza and Taryn Young are partly supported by the Effective Health Care Research Consortium. This Consortium and the CIDG editorial base are funded by UK aid from the UK Government for the benefit of developing countries (Grant: 5242). The views expressed in this publication do not necessarily reflect UK government policy.
Version history
| Published | Title | Stage | Authors | Version |
| 2017 Aug 29 | Isoniazid for preventing tuberculosis in HIV‐infected children | Review | Moleen Zunza, Diane M Gray, Taryn Young, Mark Cotton, Heather J Zar | |
| 2009 Jan 21 | Impact of tuberculosis preventive therapy on tuberculosis and mortality in HIV‐infected children | Review | Diane M Gray, Taryn Young, Mark Cotton, Heather Zar | |
| 2007 Jan 24 | The impact of tuberculosis preventive therapy on tuberculosis and mortality in HIV‐infected children | Protocol | Di Gray, Heather Zar, Mark Cotton | |
Differences between protocol and review
This is an update of the 2009 version Gray 2009b of this review. Gray 2009b included one completed and two ongoing RCTs. The latter two RCTs are complete and now included in the update. An updated search identified no other studies. The methods now include the latest Cochrane risk of bias assessment tool, GRADE and Summary of findings tables. Findings are stratified into HIV positive children on ART and not on ART. Moleen Zunza joined the author team.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- AIDS-Related Opportunistic Infections [mortality, *prevention & control];
- Anti-HIV Agents [therapeutic use];
- Antitubercular Agents [adverse effects, *therapeutic use];
- HIV Infections [drug therapy, *mortality];
- Incidence;
- Isoniazid [adverse effects, *therapeutic use];
- Randomized Controlled Trials as Topic;
- Trimethoprim, Sulfamethoxazole Drug Combination [adverse effects, therapeutic use];
- Tuberculosis, Multidrug-Resistant [epidemiology];
- Tuberculosis, Pulmonary [drug therapy, *mortality, *prevention & control];
Medical Subject Headings Check Words
Child; Humans;
PICO

Study flow diagram.
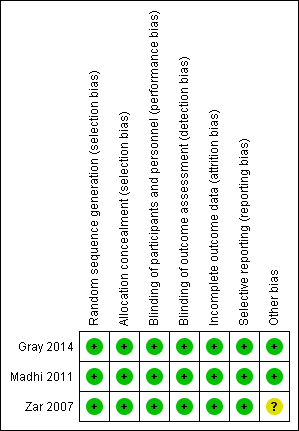
'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included study.

'Risk of bias' graph: review authors' judgements about each 'Risk of bias' item presented as percentages across all included studies.

Forest plot of comparison: 1 Isoniazid prophylaxis versus placebo, outcome: 1.1 Active TB, HIV‐positive children on ART.

Forest plot of comparison: 1 Isoniazid prophylaxis versus placebo, outcome: 1.2 Death, HIV‐positive children on ART.

Comparison 1 Isoniazid prophylaxis versus placebo for HIV‐positive children on antiretroviral therapy (ART), Outcome 1 Active TB.

Comparison 1 Isoniazid prophylaxis versus placebo for HIV‐positive children on antiretroviral therapy (ART), Outcome 2 Death.
| Isoniazid prophylaxis compared to placebo for HIV‐positive children not on antiretroviral therapy (ART) | ||||||
| Patient or population: HIV‐positive children not taking ART | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comment | |
| Assumed risk | Corresponding risk | |||||
| Placebo | Isoniazid prophylaxis | |||||
| Active TB | 10 per 100 | 3 per 100 (1 to 9) | HR 0.31 (95% CI 0.11 to 0.87) | 240 (1 trial) | ⊕⊕⊝⊝ due to serious indirectness and imprecision | Isoniazid prophylaxis may reduce active TB |
| Death | 17 per 100 | 8 per 100 (8 per 17) | HR 0.46 (95% CI 0.22 to 0.95) | 240 (1 trial) | ⊕⊕⊝⊝ due to serious indirectness and imprecision | Isoniazid prophylaxis may reduce death |
| The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1No serious risk of bias: this trial was at low risk of selection bias, and adequately blinded study participants and personnel. However, the study was stopped early on the recommendation of the data safety monitoring board after only 277 of the planned 432 were enrolled. Not downgraded. | ||||||
| Isoniazid prophylaxis compared to placebo for HIV‐positive children on antiretroviral therapy (ART) | ||||||
| Patient or population: HIV‐positive children on ART | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Placebo | Isoniazid prophylaxis | |||||
| Active TB | 13 per 100 | 9 per 100 | RR 0.76 | 737 | ⊕⊝⊝⊝ due to serious indirectness and imprecision | We don't know if Isoniazid prophylaxis reduce active TB |
| Death | 4 per 100 | 6 per 100 | RR 1.45 (0.78 to 2.72) | 737 | ⊕⊝⊝⊝ due to serious indirectness and imprecision | We don't know if Isoniazid prophylaxis reduce death |
| The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1No serious risk of bias: trials were at low risk of selection bias. Both studies adequately blinded study participants and personnel. | ||||||
| Number of children with adverse events | Number of adverse events | |||||||
| Children not on ART | Children on ART | Children on ART | Children on ART | |||||
| Isoniazid prophylaxis group N = 91 | Placebo group N = 91 | Isoniazid prophylaxis group N = 41 | Placebo group N = 40 | Isoniazid prophylaxis group N = 273 | Placebo group N = 274 | Isoniazid prophylaxis group N= 85 | Placebo group N = 82 | |
| Clinical adverse events | ||||||||
| Peripheral neuropathy | Not reported | Not reported | Not reported | Not reported | 3 | 2 | Not reported | Not reported |
| Other clinical adverse events | Not reported | Not reported | Not reported | Not reported | 14 | 23 | 1 | 1 |
| Laboratory adverse events | ||||||||
| Haematological (neutropenia, thrombocytopenia, anaemia) | 5 | 6 | 0 | 0 | 10 | 9 | Not reported | Not reported |
| Liver enzyme abnormalities | 0 | 2 | 0 | 0 | 12 | 12 | 3 | 1 |
| Other laboratory adverse events | Not reported | Not reported | 0 | 0 | Not reported | Not reported | Not reported | Not reported |
| Abbreviations: ART: antiretroviral therapy; N: number of participants. | ||||||||
| Outcome | Assumed risk | Source | Clinically important relative reduction | Sample size required1,2 |
| Active TB | 46/366 (13%) | 25% | 2990 | |
| Death | 15/366 (4%) | 50% | 2282 | |
| 1We based all calculations on: 2‐sided tests, with a ratio of 1:1, power of 0.8, and confidence level of 0.05. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Active TB Show forest plot | 3 | 737 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.50, 1.14] |
| 2 Death Show forest plot | 3 | 737 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [0.78, 2.72] |

