Liječenje stresne inkontinencije urina u žena pomoću postavljanja omče na srednji dio mokraćne cijevi
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT of TVT‐O vs TOT–ARIS | |
| Participants | 341 women from the west of Scotland, UK, Urogynaecology tertiary referral centre Inclusion criteria: women with USI or MUI (but with SUI as the predominant troublesome symptom). Women with previous incontinence surgery were included. All women had failed or declined pelvic floor muscle training Exclusion criteria: predominant OAB symptoms; or had specific co‐morbidities such as known neurological conditions (e.g. multiple sclerosis); diabetes; ≥ stage 2 POP‐Q or concomitant surgery, or both There were no significant differences in participant characteristics between the 2 groups Mean age (years): Group A: 51.5; Group B: 52.1 Mean BMI kg/m²: Group A: 28.1; Group B: 28.9 MUI: Group A: 40/170; Group B: 43/171 Previous incontinence surgery: Group A: 28/170; Group B: 18/171 | |
| Interventions | Group A: TVT‐O (n = 170) Group B: TOT (n = 171) | |
| Outcomes | Primary outcome: absence of USI on UDS Secondary outcome measures:
| |
| Notes | Loss to follow up at 1 year: Group A: 18/170, Group B: 24/171 Loss to follow up at 3 years: Group A: 44/170, Group B: 59/171 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A single‐blinded, prospective, randomized study … Women were assigned to either procedure by random allocation (computer generated)" |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation was concealed using opaque sealed envelopes, which were opened by the nursing staff on the morning of the operation" |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: “a single‐blinded, prospective, randomized study… Women were informed about the type of operation if they wished, for ethical considerations, but they were instructed not to disclose this information to the clinician at follow‐up” |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: “Post‐operative assessment at 6 months was performed by an independent clinician who was blinded to the type of surgery … “ |
| Incomplete outcome data (attrition bias) | Low risk | Quote: “No woman assigned to an arm asked to change her operation or to withdraw from the study prior to the operation. Withdrawals, unattendants and untraceables were accounted for without significant inter group differences” |
| Methods | RCT of Gynecare TVT vs Gynecare TVT‐O; Gynecare, Ethicon | |
| Participants | Trial conducted by Austrian Urogynecology Working Group in 25 gynaecology units in Austria and Germany 554 women Inclusion criteria: women with USI (positive cough stress test at bladder filling of 300 ml); no concomitant prolapse surgery or hysterectomy Exclusion criteria: DO or a predominant complaint of OAB; concomitant prolapse surgery; other major concomitant surgery (e.g. hysterectomy); previous incontinence surgery other than colporrhaphy; residual urine ≥100 ml; neurologic disease; allergy to local anaesthetic agents; and coagulation disorders or other contraindications for surgery Age (years): Group A: 59.7 ± 11.3; Group B: 58.6 ± 10.7 BMI kg/m²: Group A: 27.7 ± 5.3; Group B: 28.5 ± 4.9 Parity: Group A: 2.2 ± 1.2; Group B: 2.2 ± 1.3 | |
| Interventions | Group A: TVT: (n = 285; 38 of whom were lost to follow‐up) Group B: TVT‐O: (n = 269; 36 of whom were lost to follow‐up) | |
| Outcomes | Participants were evaluated at 3 months, with a further evaluation scheduled at 5 years
| |
| Notes | QoL: Short‐Form Health Survey (SF‐12), EuroQol‐5D (EQ‐5D) condition‐specific QoL was assessed with the German language version of the KHQ, the Incontinence Outcome Questionnaire (IOQ), and PGI‐S and PGI‐I Cystoscopy was performed with all retropubic placements but not routinely with transobturator insertions The number of women in each group seen at 5‐year follow‐up was not available, so the data reported could not be used for meta‐analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomized according to a computer generated |
| Allocation concealment (selection bias) | Low risk | Quote: "computer generated random list allocating trial identification number and treatment group" |
| Blinding of participants and personnel (performance bias) | High risk | Patients, surgeons, and physicians performing |
| Blinding of outcome assessment (detection bias) | High risk | Patients, surgeons, and physicians performing |
| Incomplete outcome data (attrition bias) | Low risk | Accounted for and no differentials in the groups in terms of loss to follow‐up |
| Methods | RCT of TVT vs TVT‐O | |
| Participants | 30 women with SUI in Kuwait Maternity Hospital Inclusion criteria: SUI with or without a prolapse; USI with or without urethral hypermobility; MUI without urodynamic DO; absence of a contractile urinary bladder or obstruction Exclusion criteria: acute cystitis; predominant urge incontinence; urodynamic DO; maximum flow (Qmax) less than 15 ml/s and/or PVR urine of more than 20% of the volume voided; genital prolapse of stage 4 or 5 Menopausal: Group A: 3/15; Group B: 4/15 | |
| Interventions | Group A: TVT (n = 15) Group B: TVT‐O (n = 15) | |
| Outcomes |
| |
| Notes | No participants lost to follow‐up at 6 and 12 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women were randomised using numbered, opaque, sealed envelopes containing computer‐generated random allocations in a ratio of 1:1 in balanced blocks of 10. |
| Allocation concealment (selection bias) | Low risk | Women were randomised using numbered, opaque, sealed envelopes containing computer‐generated random allocations in a ratio of 1:1 in balanced blocks of 10. |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Low risk | Quote: “All accounted for” |
| Methods | RCT comparing TVT with SPARC | |
| Participants | 84 women presenting with SUI, or SUI with MUI if cystometrogram showed normal capacity, compliance and no uninhibited contractions. Women with previous failed anti‐incontinence surgeries or bulking agents treatments were also eligible for the study. Both groups were similar in terms of age, severity of symptoms, 1‐h pad test and preoperative IIQ (of Shumaker) | |
| Interventions | Group A: SPARC (n = 41) Group B: TVT (n = 43) | |
| Outcomes | Primary endpoint: objective cure defined as 1‐h pad test of 2g | |
| Notes | Follow‐up assessment of cure at 1 year was unavailable in 1 woman (Group B) who died from a myocardial infarct | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were blinded to the procedure and had envelope randomization immediately prior to the start of the surgery" |
| Allocation concealment (selection bias) | Low risk | Adequate |
| Blinding of participants and personnel (performance bias) | Low risk | Both groups and outcome assessors were said to have been blinded but how this was achieved was not clear. Quote: "Patients were blinded to the procedure and had envelope randomization immediately prior to the start of the surgery" |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors blinded, quote: "dedicated UDS nurse (BS), who was blinded to the procedure" |
| Incomplete outcome data (attrition bias) | Low risk | Addressed |
| Methods | RCT of TOT (Obtape) versus distal urethral polypropylene sling (DUPS) versus TVT | |
| Participants | 190 women Inclusion criteria: women with SUI with or without POP or pelvic surgery; previous failed anti‐incontinence surgeries or bulking agent treatments permitted; women with MUI were not excluded as long as their cystometrogram showed normal capacity; compliance and no uninhibited contractions Exclusion criteria: obstruction; unstable bladder function, or neurogenic bladder; UTI | |
| Interventions | Group A: Obtape (n = 78) Group B: DUPS (n = 32) Group C: TVT (n = 80) 1 participant in the Obtape group had a urethral diverticulum, which was repaired, but the Obtape procedure was cancelled, leaving 77 patients in the Obtape group for the final analysis | |
| Outcomes | Primary outcome: objective cure defined by 1‐h pad test of ≤ 2 g Secondary outcome: subjective cure rates determined by the ICIQ‐SF Postoperatively, all women were re‐evaluated by history and physical examination at 1, 6, and 12 months. At the 12‐month visit, participants completed the ICIQ‐SF, and underwent the 1‐h pad test conducted by the dedicated UDS nurse who was blinded to the procedure | |
| Notes | Mentor's Obtape is a non woven monofilament thermally bonded micropore (50 µm) polypropylene mesh which was withdrawn by its manufacturers in 2006. There have been many reports of tape erosions and some cases of ischiorectal abscess and necrotizing fasciitis DUPS is not a minimally invasive sling, but a woven polypropylene mesh (by Ethicon, New Jersey). Absorbable sutures are used to fix the sling into position until adhesions form and adhere it naturally to the retropubic space. As it was not a minimally invasive sling there was no need to compare DUPS in the review The DUPS procedure was discontinued because of a higher postoperative retention rate combined with several complaints of suprapubic abdominal discomfort on straining | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomization was performed by an envelope method immediately before the start of surgery." |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding of participants and personnel (performance bias) | Low risk | The patients were blinded to the procedure |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors blinded, but how this was achieved was not explained |
| Incomplete outcome data (attrition bias) | Unclear risk | Unclear |
| Methods | A prospective RCT of TVT‐O vs TVT | |
| Participants | 264 women with SUI in Lithuania hospital setting. The degree of incontinence was 2–3 according to the Ingelman‐Sundberg scale Inclusion criteria: women with SUI Exclusion criteria: urogenitale prolapse greater than stage 2; urinary retention; OAB and psychiatric problems Post menopausal: Group A: 47/150; Group B: 48/114 Mean BMI kg/m² (SD): Group A: 28.2 (3.8); Group B: 27.9 (4.0) Previous incontinence surgery: Group A: 18/150; Group B: 16/114 POP‐Q stage 2: Group A: 29/150; Group B: 22/114 | |
| Interventions | Group A: TVT‐O (n = 150) Group B: TVT (n = 114) | |
| Outcomes |
| |
| Notes | Urodynamics assessment was not performed in all participants Cystoscopy and cough test were routinely performed only in the TVT group No patients were lost to follow‐up | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Low risk | No participants lost to follow‐up |
| Methods | RCT of TVT‐O versus TVT | |
| Participants | 240 women with different degrees of SUI Inclusion criteria: symptomatic SUI grades 1 and 2a (McGuire classification) Exclusion criteria: women with ISD; OAB; associated prolapses; neurovegetative disorders and recurrent SUI or under rehabilitative/medical therapies Diagnosis based on ambulatory UDS Average age of 54 years | |
| Interventions | Group A: TVT‐O (n = 120) | |
| Outcomes | Primary outcome: cure rate of SUI evaluated with the postoperative ambulatory urodynamic tests 1 year after surgery
A positive pad weight result was defined as > 2g of leakage | |
| Notes | The participants were classified according to the SUI system on the basis of urodynamics studies (McGuire classification), performed at 250 ml bladder volume. SUI was classified into 3 grades considering the severity of symptoms referred (SUI1 = loss of urine during excessive strains, SUI2 = during minor strains, SUI3 = at rest) and the urodynamic evaluation (McGuire classification: SUI1 = abdominal leak‐point pressure (ALPP) > 90 cm water, SUI2 = ALPP of 60‐90 cm water, SUI 3 = intrinsic sphincter deficiency and ALPP < 60 cm water) Loss to follow‐up: 32 women were lost to follow‐up due to work commitments, Group A:12/120 TVT, Group B: 20/120 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A stratified randomisation was carried out. Presented two identical closed envelopes to patients, one containing the paper “TVT” and the other “TVT‐O”. After choosing and opening of the envelope, further stratification was performed with a sampling chart. Four groups were formed on the basis of which operation they were going to receive." |
| Allocation concealment (selection bias) | Low risk | Quote: "Presented two identical closed envelopes to patients, one containing the paper “TVT” and the other “TVT‐O” |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Data was analysed by a surgeon who was not involved in the surgical intervention" |
| Incomplete outcome data (attrition bias) | High risk | Disproportionately higher numbers lost to follow‐up in TVT‐O group |
| Methods | RCT of TVT vs Monarc TOT | |
| Participants | Setting: 3 USA tertiary academic medical centres Inclusion criteria: 170 women aged over 21 years with USI with or without concurrent POP Exlusion criteria: DO; previous incontinence surgery; PVR > 100 ml; desiring future childbearing; history of hidradenitis suppurativa, inguinal lymphadenopathy, or an inguinal or vulvar mass; history of a bleeding diathesis or ongoing anticoagulation therapy; current genitourinary fistula or urethral diverticulum Mean age in years (SD): Group A: 52 (11); Group B: 53 (12) Mean BMI kg/m² (SD): Group A: 30 (7); Group B: 29 (6) Postmenopausal: Group A: 53/88; Group B: 58/82 Previous continence surgery: Group A: 5/88; Group B: 10/82 MUI: Group A: 76/88; Group B: 66/82 VLPP: < 60 cm/H2O: Group A: 14/88; Group B: 16/82 | |
| Interventions | Group A: TVT (n = 88) Group B: TOT (n = 82) | |
| Outcomes | Primary outcome: presence or absence of 'abnormal bladder function', a composite outcome defined as the presence of any the following: incontinence symptoms ‐ any type (ISI > 0), a positive cough‐stress test, re‐treatment for SUI or postoperative urinary retention assessed 1‐year after surgery Secondary outcomes: assessed by use of SF12, PISQ‐12, bladder diary at 12 and 24 months:
| |
| Notes | Intraoperative cystoscopy performed in both groups Concomitant surgery performed in Group A: 48/88; Group B: 45/82 Loss to follow‐up: Group A: 3/88; Group B: 7/82 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "were randomised using computer generated random allocation" |
| Allocation concealment (selection bias) | Low risk | Quote: "group assignment were concealed in consecutively numbered sealed opaque envelopes" |
| Blinding of participants and personnel (performance bias) | Unclear risk | Quote: "blinding of surgeon and participants was not possible ..." |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "all post op assessments were performed by research nurses who were blinded to treatment given" |
| Incomplete outcome data (attrition bias) | Low risk | All accounted for |
| Methods | RCT of TOT (Monarc) versus TVT Random allocation of participants but method of sequence generation and allocation concealment not described | |
| Participants | 140 women diagnosed with USI Participants in both groups had similar background characteristics including age, BMI, parity, HRT use, menopausal status, previous incontinence surgery, prolapse etc Inclusion criteria: participants had either failed conservative management for symptomatic stress incontinence or required prophylactic incontinence surgery during prolapse repair for occult stress incontinence (no preoperative subjective complaint of urinary stress leakage but found to have USI) Exclusion criteria: significant voiding dysfunction (maximum urine flow rate < 10th percentile according to Liverpool nomogram and PVR volume > 50 ml); known allergy to polypropylene; immunosuppressant therapy and a past history of neurological disease; urogenital malignancy; fistula or pelvic radiotherapy | |
| Interventions | Group A: TOT (n = 58) | |
| Outcomes | Outcomes included Immediate‐ and short‐term complications, cure rates and patient satisfaction Primary outcome: reduction in incidence of bladder injury Secondary outcomes:
Improvement of a particular symptom denoted at least 50% reduction in frequency of occurrence in 3‐day bladder diary when compared to preoperative state Measures used for assessment included:
| |
| Notes | 23 women from the TVT group and 21 from TOT group were lost to follow‐up. Thus, at follow‐up complete data set available for 82 women in TVT group and 58 in the TOT group. There were no differences between the group unavailable for analysis when compared to those finally analysed No mention of intraoperative cystoscopy in either group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were blinded and randomly allocated in a balanced way (blocks of 20) Randomisation was stratified according to a history of previous incontinence surgery |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding of participants and personnel (performance bias) | Unclear risk | Participants were blinded. How this was achieved was not explained |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Low risk | No differential loss to follow‐up or differential attrition |
| Methods | RCT of TVT‐O versus TOT (Monarc) | |
| Participants | 120 women with SUI (31) and MUI (89) Inclusion criteria: women with SUI, or MUI, with SUI as the predominant symptom Exclusion criteria: MUI with predominant UUI Performed under local anaesthesia Mean age years (SD): 52.6 (6.8) | |
| Interventions | Group A: TVT‐O (n = 60) Group B: TOT (n = 60) | |
| Outcomes |
| |
| Notes | Follow‐up 3 months All women attended for follow‐up | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Before the beginning of the study, the computer‐generated list of 120 random numbers (from one to 120) was made for two groups (60 random numbers for each group, optimum allocation ratio 1)" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "the consecutive study numbers were given after admission, and based on this admission number, either inside‐out or outside‐in procedure was selected later in the OR according to a computer‐ generated list of random number" |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Low risk | All data/information accounted for at follow‐up |
| Methods | RCT of TVT versus Monarc TOT | |
| Participants | 118 women Inclusion criteria: women with SUI and POP‐Q ≥ stage 2 Mean age 57.43 years All women had cystocoele repair and levator myorraphy 73 women were post menopausal | |
| Interventions | Group A: TVT Group B: TOT (exact numbers in each group not reported) | |
| Outcomes | Cure rates: TVT (98.3%), TOT (97.1%) as exact number of women in each group was not given there were no data that could be extracted Intraoperative and postoperative complications | |
| Notes | Numbers in each group unreported. It was, thus, impossible to abstract results | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women randomised into 2 groups (computer generated randomisation list) |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT comparing TVT, TOT and TVT‐O | |
| Participants | 187 women Inclusion criteria: women with urodynamically proven SUI in the urology department of a Chinese hospital | |
| Interventions | Group A: TVT (n = 77) Group B: TOT (n = 45) Group C: TVT‐O (n = 65) | |
| Outcomes |
| |
| Notes | No quality of life measures undertaken Cystoscopy performed in TVT group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT of TVT vs TVT‐O Recruitment Feb 2009‐Feb 2010 | |
| Participants | 205 women with SUI Inclusion criteria: women with urodynamically proven SUI with or without prolapse Exclusion criteria: DO; MUI All women had similar background characteristics | |
| Interventions | A: TVT (n = 102) B: TVT‐O (n = 103) | |
| Outcomes | Follow‐up 12‐24 months
| |
| Notes | Needs translation for further information Article written in Chinese and translated to English for interpretation and extraction | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Stated: ‘randomly allocated ’ |
| Allocation concealment (selection bias) | Unclear risk | Stated: ‘randomized’ |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT of Monarc system and TOT system | |
| Participants | 93 women having urodynamic evaluation | |
| Interventions | Group A: Monarc TOT (n = 48) Group B: TOT (n = 45) | |
| Outcomes | Outcomes assessed 12 months postoperatively
| |
| Notes | Monarc is outside‐to‐in TOT with open edge polypropylene mesh that contains an absorbable tensioning suture threaded into the length of the mesh. The tension free obturator tape (TOT) system used here is the same outside‐in type, but has a closed edge polypropylene mesh without absorbable tensioning suture | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "93 female patients were prospectively, randomly assigned to the study" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT OF TVT vs TOT | |
| Participants | 41 women Inclusion criteria: women with SUI; able to complete a questionnaire Exclusion criteria: prior spine surgery; back pain; scoliosis; traumatic spine injury; neurological disease; or hip or knee surgery | |
| Interventions | 41 women, number in each group was not given | |
| Outcomes | Postoperative pain was assessed using a 10‐point visual analogue scale (VAS) at fixed time‐points: 30 minutes, 3hr and 24hr after surgery Length of procedure (minutes) | |
| Notes | We were not able to use the data provided, as the number in each group was not specified | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "were randomized to receive" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT of TOT versus TVT | |
| Participants | Women with SUI Age in years (SD): Group A: 52.02 (0.88); Group B: 52.27 (7.34) | |
| Interventions | Group A: TOT (n = 40) Group B: TVT (n = 40) | |
| Outcomes | A validated stress and urge incontinence questionnaire 24‐h pad test 6‐month follow‐up of ICIQ Operative time Mean hospital stay | |
| Notes | Intraoperative cystoscopy not mentioned in either group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “In this randomised clinical trial, eighty female patients with SUI were randomly allocated to “ |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT comparing TOR and RTR of sling procedures for SUI using the I‐STOP device | |
| Participants | Multicentre (3 gynaecology and 2 urology departments in France) 88 women Inclusion criteria: women > 18 years with SUI, proven by clinical and urodynamic examinations, or MUI Exclusion criteria: women with previous history of radio‐ or chemotherapy; on anticoagulant or antipsychotic treatment; or pregnant Mean age: Group A: 58.8 years; Group B: 53.4 years | |
| Interventions | Group A: RPR (n = 42) Group B: TOR (n = 46) The I‐STOP device (CL Medical, Lyon, France) was used for both the RPR and the TOR procedures | |
| Outcomes |
| |
| Notes | Loss to follow‐up at 4 years: Group A: 8/42; Group B: 9/46 Length of follow‐up ranged from 48 months to 61 months (RPR) and 48 months to 63 months (TOR) The mean follow‐up was 10 months, with 37 women having 6 months of follow‐up and 51 women having at least 12 months of follow‐up Cystoscopy was performed for both procedures | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | " ... Prospective randomised Multicentre study .... using a predetermined computer generated randomisation code ..." |
| Allocation concealment (selection bias) | Low risk | Surgeon informed of allocated procedures by an uninvolved third‐party immediately before the operation |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) | Unclear risk | Unclear |
| Incomplete outcome data (attrition bias) | Unclear risk | Unclear |
| Methods | QRCT of TVT‐O vs modified TVT‐O | |
| Participants | 175 women Inclusion criteria: women aged 25‐85 years with USI; positive stress test with at least a maximum cystometric capacity of 300 ml Exclusion criteria: DO or detrusor acontractility; neurogenic bladder; or POP stage 3 or above Mean age years (SD): Group A: 60.0 (11.7); Group B: 57.2 (2.7) BMI kg/m² (SD): Group A: 26.4 (4.8) Group B: 26.8 (5.3) Previous surgery for SUI: Group A: 4/87; B Group: 4/88 Previous surgery for POP: Group A: 4/87; Group B: 2/88 | |
| Interventions | Group A: TVT‐O (n = 87) Group B: modified TVT‐O (n = 88) | |
| Outcomes | At 1 ‐year follow‐up:
At 3‐year follow‐up:
| |
| Notes | The modified TVT‐O was shortened to a total tape length of 12 cm and had a reduction in the depth of lateral dissection, the obturator membrane was not perforated with the scissors or the guide Follow‐up assessments carried out at 1, 6, 12 months, and 3 years Lost to follow‐up:
| |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "The randomisation process was performed with five sequential patients undergoing one approach before alternating surgical modality" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Low risk | Patients were blinded to the type of surgery they underwent |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "no patients withdrew from the study prior to their operation". 2 participants were completely lost to follow‐up after the 1‐month visit and 2 more after the 6‐month visit. One patient died before the 6‐month visit; the cause of death was unrelated to the surgery |
| Methods | RCT comparing TVT with TOT | |
| Participants | 61 women Inclusion criteria: USI Exclusion criteria: predominant urge incontinence; urodynamic detrusor instability; or prolapse Mean age (years; SD): Group A: 54.7 (11.9); Group B: 53.6 (12.5) Mean BMI kg/m² (SD): Group A: 24 (3.2); Group B: 25.2 (4.3) Postmenopausal status: Group A: 18/30; Group B: 16/31 Previous continence surgery: Group A: 4/30; Group B: 1/31 Previous prolapse surgery: Group A: 4/30; Group B: 1/31 ISD: Group A: 4/30; Group B: 3/31 | |
| Interventions | Group: A: TOT (n = 30) Group: B: TVT (n = 31) | |
| Outcomes |
| |
| Notes | The full article was retracted at the request of authors because appropriate ethics committee approval was not received prior to starting study. Nevertheless, participants did give written consent to be included in the trial and consented for the procedures. No methodological flaws were identified: the review authors therefore decided to include the data TOT: Uratape mentor‐porges Cystoscopy performed following TVT procedure | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women were randomised using numbered, opaque sealed envelopes containing computer‐generated random allocations in a ratio of 1:1 in balanced blocks of 10. Envelopes were opened in the operating room by a nurse just before starting the procedure |
| Allocation concealment (selection bias) | Low risk | Adequate |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors were blinded |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT of TVT and TVT‐O | |
| Participants | Multicentred RCT, 14 centres in France (university hospitals and 3 general hospitals) 149 women with SUI Inclusion criteria: age >18 years; isolated or mixed USI; indication for surgical treatment of USI; positive cough stress test Exclusion criteria: concomitant POP surgery; concomitant hysterectomy; previous incontinence surgery; pregnancy; anticoagulant therapy; higher than stage 1 urogenital prolapse (POP‐Q ICS) All women had similar background characteristics Mean age (years; SD): Group A: 54.6 (10.9); Group B: 52.8 (9.8) Mean BMI kg/m² (SD): Group A: 26.3 (4.5); Group B: 26.3 (5.7) Postmenopausal: Group A: 43/75; Group B: 40/74 POP‐Q stage 1: Group A: 245/75; Group B: 24/74 | |
| Interventions | Group A: TVT (n = 75) Group B: TVT‐O (n = 74) | |
| Outcomes | Outcomes assessed at 2, 6, 12 and 24 months
| |
| Notes | Cystoscopy performed in both groups Loss to follow‐up: at 12 months: Group A: 6/75; Group B: 5/74 Loss to follow‐up at 24 months: Group A: 8/75; Group B: 9/74 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The patients were randomized using sealed opaque envelopes, following computer‐generated random allocations" |
| Allocation concealment (selection bias) | Low risk | Quote: "The patients were randomized using sealed opaque envelopes, following computer‐generated random allocations, with a ratio of 1:1 in balanced blocks of four. The envelopes were opened just before each participant's surgical procedure" |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "blinding of surgeons and participants not possible" |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Low risk | Data complete |
| Methods | RCT of TOT vs TVT | |
| Participants | 70 women with SUI | |
| Interventions | Group A: TOT (n = 31) Group B: TVT (n = 32) | |
| Outcomes |
| |
| Notes | Mean follow up in months (SD): A: 28 (12.3) and B: 26 (13.6) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "were randomly distributed to two groups" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT comparing Gynecare TVT R and Aris TOTR outside‐in | |
| Participants | 40 women Inclusion criteria: women with urodynamically proven SUI Exclusion criteria: women who reported urgency incontinence as predominant complaint; had pelvic or vaginal surgery within the preceding 6 months; had associated urethral and/or bladder pathology or active UTI; neuropathic bladder; POP > stage 2 (Baden Walker classification) Mean age (years; SD): Group A:47 (5); Group B: 45 (7) Concomitant POP stage 1‐2: Group A: 10; Group B: 13 Mean BMI kg/m² (SD): Group A: 34 (5); Group B: 32(5) | |
| Interventions | Preliminary results: Group A: TVT: (n = 19) Group B: TOT: (n = 21) At 24 months: Group A: TVT: (n = 45) Group B: TOT: (n = 42) | |
| Outcomes | Follow‐up at 3, 6, 12 and 24 months
| |
| Notes | Intraoperative cystoscopy carried out only in the TVT group to exclude bladder or urethral injury Concomittant surgery was performed in 9 participants; 5 participants underwent abdominal hysterectomy, 4 participants underwent anterior colporrhaphy Lost to follow‐up at 12 months: Group A: 0/19; Group B: 0/21 Lost to follow‐up at 24 months: Group A: 9/45; Group B: 7/42 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patient’s randomisation is accomplished through closed envelopes. A randomly selected envelope is dispatched to a running nurse with the patient’s name and ID hand typed on the envelope" |
| Allocation concealment (selection bias) | Low risk | Quote: “randomisation is accomplished through closed envelopes. A randomly selected envelope is dispatched to a running nurse with the patient’s name and ID hand typed on the envelope” |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: “Follow up was carried out by a nurse blinded to the procedure” |
| Incomplete outcome data (attrition bias) | Low risk | All outcomes included |
| Methods | RCT of adjustable TOT vs TOT | |
| Participants | 96 women with SUI, with a mean age of 53 + 9.9 years | |
| Interventions | Group A: adjustable TOT (n = 48) Group B: TOT: (n = 48) | |
| Outcomes |
| |
| Notes | The advantage of the adjustable tape is that it can be adjusted postoperatively to address over‐ or under‐correction | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomized into 2 equal groups" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | QRCT comparing TVT and TOT | |
| Participants | 110 women Inclusion criteria: women with SUI, all had preoperative stress test Exclusion criteria: previous surgery for SUI; mixed incontinence; renal disease; metabolic disorders; or POP Mean age was 51 years | |
| Interventions | Group A: TOT (n = 56) Group B: TVT (n = 54) | |
| Outcomes |
| |
| Notes | No mention of intraoperative cystoscopy Followed‐up at 15 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐RCT |
| Allocation concealment (selection bias) | High risk | Inadequate |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT comparing TOT and TVT | |
| Participants | Multicentre RCT – 21 centres across the UK 192 women Inclusion criteria: women >21 years of age; USI or MUI for which SUI was the predominant symptom; must have failed with conservative measures Exclusion criteria: women with neurological disease; previous surgery for USI (those with previous prolapse surgery were not excluded); urodynamic DO or low compliance; POP extending beyond the hymen | |
| Interventions | Group A: Monarc TOT (n = 100) Group B: Gynaecare TVT (n = 92) | |
| Outcomes | Follow‐up at 4 weeks, 6 months and 12 months
| |
| Notes | The trial was a non‐inferiority design. Outcome measures calculated by intention‐to‐treat Assessed via ICIQ‐FLUTS long form, ICIQ LUTSqol; KHQ questionnaires and 4‐day urinary diary Sexual function assessed by ICIQ‐LUTSqol question, ‘does your urinary problem affect your sex life?’ Cystoscopy: not mentioned whether routinely performed in either group Lost to follow‐up: Group A: 5/100; Group B: 7/92 (and 1 excluded as she did not have the operation) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomisation list was stratified by study sites, using |
| Allocation concealment (selection bias) | Low risk | Quote: "The study co‐ordinator placed a treatment into consecutively |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "Patients and ward staff were blinded to the intervention group by ensuring that dressings were applied both suprapubically and to the obturator areas" |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Low risk | Patients and their data accounted for |
| Methods | RCT of TVT vs TVT‐O | |
| Participants | 110 women with SUI | |
| Interventions | Group A: TVT (n = 60) Group B: TVT‐O (n = 50) | |
| Outcomes | Subjective cure: | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "in a prospective randomized trial ... women were randomized between TVT and TVT‐O for treatment" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT of inside‐out TOT vs outside‐in TOT | |
| Participants | 250 women Inclusion criteria: women with SUI in a university teaching hospital in Cairo, Egypt | |
| Interventions | Group A: inside‐out TOT (n = 125) Group B: outside‐in TOT (n = 125) | |
| Outcomes | Primary outcomes:
Secondary outcomes:
| |
| Notes | Lost to follow‐up: Group A: 23/125; Group B: 28/125 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "A prospective single‐blinded randomised trial" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT of TVT‐O and TOT (Monarc) | |
| Participants | 191 women Inclusion criteria: women with SUI, USI and MUI. Those with MUI failed anti‐cholinergic medical treatment before surgical treatment Mean age (years; SD): Group A: 49.2 (8.9); Group B: 49.5 (10.3) SUI: Group A: 74/93 (80%); Group B: 74 /98 (76%) Postmenopausal: Group A: 33/93; Group B: 34/98 Previous incontinence surgery: Group A: 8/93; Group B: 9/98 Previous POP surgery: Group A: 19/93; Group B: 15/98 Urethral hypermobility: Group A: 80/93; Group B: 90/98 POP ≥ grade 1: Group A: 25/93; Group B: 24/98 ISD: Group A: 5/93; Group B: 1/98 DO: Group A: 5/93; Group B: 7/98 | |
| Interventions | Group A: TVT‐O (n = 93) Group B: Monarc TOT (n = 98) | |
| Outcomes |
| |
| Notes | No concomitant urogynaecological surgery performed Follow‐up occurred at 12 months and at 2 ‐4 years Loss to follow‐up at 12 months: Group A: 15/39; Group B: 14/36. Loss to follow‐up at 4 years: Group A: 18/93; Group B: 12/98 Cystoscopy was performed only when bloody urine was encountered Analysis of cure used the numbers that completed follow‐up as denominator | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Women with an indication for surgical treatment of SUI were at random assigned to either TVT‐O or Monarc..."(from abstract Vervest HAM 2005) |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT comparing TVT and TVT‐O: POLTOS study | |
| Participants | Multicentre RCT in Poland 35 women Inclusion criteria: women with urodynamically proven (bladder filled to a minimum of 300 ml) SUI; no prior incontinence surgery Exclusion criteria: women with UTI; BMI > 33 kg/m²; previous hysterectomy; neurological incontinence; POP; PVR > 150 ml; OAB and MUI Age: 40‐80 years | |
| Interventions | Group A: TVT (n = 19) Group B: TVT‐O (n = 16) | |
| Outcomes |
| |
| Notes | Follow‐up at 6 months Cystoscopy was performed in both groups Lost to follow‐up: Group A: 4/19; Group B: 0/16 (3 participants with bladder perforation had the tape removed and were excluded) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “The randomisation was done through a web page secured with a 128‐bit code” |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: “every patient had extra skin incisions for masking the type of procedure (“sham operation”). Each patient had 4 skin incisions in localization typical for needle introduced in TVT and TVT‐O procedure” |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | Information not clear |
| Methods | RCT of trans‐obturator tension‐free vaginal tape (TVT‐O) versus TVT‐O with modified Ingelman‐Sundberg (IS) procedure | |
| Participants | 96 women Inclusion criteria: women with MUI after poor response to medical treatment DO at baseline: Group A: 19/43; Group B: 15/49 Post menopausal: Group A: 32/43; Group B: 27/49 | |
| Interventions | Group A: TVT‐O (n = 47) Group B: TVT‐O plus IS: (n = 49) | |
| Outcomes |
Follow‐up QOL scores: Both IIQ‐7 and UDI‐6 demonstrated a significant decrease at the 3‐months follow‐up in the TVT‐O plus IS group. Scores remained relatively stable after 3 months of follow‐up and until the end of the study. | |
| Notes | The IS bladder denervation procedure is designed to disrupt most of the innervations from the inferior hypogastric plexus to the bladder to treat refractory urgency or urge incontinence (the vaginal epithelium and perivesical fascia were dissected off the trigone. The plane of dissection was just within the serosal layer of the bladder. Lateral and posterior sharp dissection was performed to obtain more extensive division in the area of the terminal branches of the pelvic nerve). Follow‐up was at 12‐months, but urodynamic profile was repeated at the 3‐month follow‐up Loss to follow‐up: Group A: 2/47; Group B: 1/49 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “After an objective evaluation, 96 eligible patients were randomised” |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT of TVT vs TVT‐O | |
| Participants | 120 women Inclusion criteria: women with urodynamically proven SUI and urethral hypermobility Exclusion criteria: not defined | |
| Interventions | A: TVT (n = 60) B: TVT‐O (n = 60) | |
| Outcomes |
| |
| Notes | TVT group underwent cystoscopy | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Stated: "randomised" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT comparing TVT and TVT‐O | |
| Participants | 167 women Inclusion criteria: women with urodynamically proven SUI Exclusion criteria: urogenital prolapse > stage 1 (POP‐Q); DO; symptoms of OAB; urinary retention; previous anti‐incontinence surgery including anterior colporrhaphy and neurological bladder Mean age (years; SD): Group A: 49.31 (5.00); Group B: 49.08 (4.93) Postmenopausal: Group A: 16/83; Group B: 14/84 Mean BMI kg/m² (SD): Group A: 25.99 (1.27); Group B: 26.18 (1.88) | |
| Interventions | Group A: TVT (n = 83) Group B: TVT‐O (n = 84) | |
| Outcomes |
| |
| Notes | Cystoscopy only performed in TVT group Lost to follow‐up: Group A: 2/83; Group B: 1/84 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "predetermined computer‐generated randomisation code" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "two independent physicians blinded to the different procedures" |
| Incomplete outcome data (attrition bias) | Low risk | All data included |
| Methods | RCT of TVT vs TOT | |
| Participants | 20 women Inclusion criteria: women with SUI confirmed on urodynamics Mean age (years; SD): Group A: 55.8 (13.7); Group B: 60.2 (12.2) | |
| Interventions | Group A: TVT (n = 10) Group B: TOT (n = 10) | |
| Outcomes |
| |
| Notes | None lost to follow‐up Follow‐up assessment at 12 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT comparing the IRIS (Innovative Replacement of Incontinence Surgery) tape with TVT and SPARC procedure | |
| Participants | 96 women with SUI were randomised | |
| Interventions | Group A: TVT (n = 32) Group B: SPARC (n = 30) All 3 groups had comparable background characteristics | |
| Outcomes |
| |
| Notes | Follow‐up was for 1 year | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "In this controlled, prospective, randomised study ...." |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT comparing Monarc TOT with SPARC retropubic tape | |
| Participants | 130 women Inclusion criteria: women with SUI with similar background characteristics Preoperative assessment included the use of voiding diaries, stress and pad tests, and urodynamics Mean age (years; SD): Group A: 45.7 (9.8); Group B: 45.4 (12.4) | |
| Interventions | Group A: Monarc (TOR; n = 65) Group B: SPARC (RPR; n = 65) | |
| Outcomes |
| |
| Notes | Follow‐up at 3 months. Cystoscopy only in the TVT group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "43 women withUI were randomly assigned..." |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT of TVT vs TVT‐O | |
| Participants | 300 women Inclusion criteria: women with SUI after failed conservative treatment. All confirmed on a positive stress test (cough provocation). Women with symptoms of MUI were included if SUI was the predominant symptom Exclusion criteria: DO; previous incontinence, POP surgery, or pelvic radiotherapy; POP‐Q ≥ stage 2; PVR > 100 ml; preoperative use of anticholinergics; need for concomitant surgery Cough provocation test, multichannel UDS, urethral pressure profilometry and uroflometry were done preoperatively and at 12‐month follow‐up | |
| Interventions | Group A: TVTTM (n = 149) Group B: TVT –OTM (n = 151) | |
| Outcomes |
| |
| Notes | All women with TVT had intraoperative cystoscopy but this was not performed in those with TVT‐O Loss to follow‐up: Group A: 8/141; Group B: 4/147 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "women were prospectively, randomly assigned to the study. We used the method of block randomisation with a random‐number generator" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "The current randomised, non‐blinded study" |
| Blinding of outcome assessment (detection bias) | Low risk | All participants were evaluated at follow‐up by 3 urogynaecologists, blinded to the different procedures |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "In the TVT group, 141/149 patients returned for a 1‐year follow‐up (dropout rate of 5.3%), and in the TVT‐O group, 147/151 patients were present for the 1‐year follow‐up (dropout rate of 2.6%)" |
| Methods | RCT comparing TVT and TVT‐O | |
| Participants | Multicenter study from 7 Finnish hospitals (4 university hospitals and 3 central hospitals) Inclusion criteria: history of SUI; indication for surgical treatment of stress incontinence; positive cough‐stress test; detrusor instability score (DIS) ≤ 7 | |
| Interventions | Group A: TVT‐O (n = 131) | |
| Outcomes |
| |
| Notes | Cystoscopy with 70° optic was performed twice during the TVT and once during the TVT‐O to detect possible bladder injury Follow‐up was for 5 years:
| |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The investigator called an independent randomisation centre to enter the patient participant in the allocated group. Participant were randomized using computer‐generated random allocations in a ratio of 1:1 in balanced blocks of 4. |
| Allocation concealment (selection bias) | Low risk | The investigator called an independent randomisation centre to enter the patient participant in the allocated group. Participant were randomized using computer‐generated random allocations in a ratio of 1:1 in balanced blocks of 4. |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | The 3‐year postoperative evaluation was performed by an independent physician or by the operating surgeon together with a study nurse |
| Incomplete outcome data (attrition bias) | Low risk | All data accounted for |
| Methods | RCT of retropubic versus transobturator tension‐free incontinence cystocoele treatment (TICT) procedures | |
| Participants | 449 women with USI | |
| Interventions | Group A: r‐TICT (n = 229; retropubic) Group B: t‐TICT (n = 220; transobturator) | |
| Outcomes |
| |
| Notes | TICT, a retropubic technique developed using a polypropylene T‐shaped mesh made up by a central body (positioned under both urethra and bladder) and 2 wings that cross the Retzius (retropubic TICT or r‐TICT) and the transobturator foramen (transobturator TICT or t‐TICT). The advantage of T‐shaped mesh is to give a good support both on the mid‐urethral complex (with tapes) and on the whole anterior compartment (with body of mesh). The target consists of treating the functional (incontinence) and the anatomical defect (cystocoele) Average follow‐up was 45 months. Loss to follow‐up: Group A: 14/229; Group B: 12/220 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “women with urodynamic stress incontinence were randomly allocated to 2 treatment groups” |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT of TVT versus TVT‐O | |
| Participants | 120 women Inclusion criteria: women with USI Exclusion criteria: predominant urge incontinence or POP Women had similar characteristics with regard to age, parity, incontinence symptoms and menopausal status | |
| Interventions | Group A: TVT (n = 60) Group B: TVT‐O (n = 60) | |
| Outcomes |
Follow‐up was for 12 months | |
| Notes | Cystoscopy was performed only in the TVT group Mean follow‐up 13 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Patients were alternately assigned to the TVT or TVT‐O group" (Randomisation was by alternation method) |
| Allocation concealment (selection bias) | High risk | Not concealed |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | QRCT comparing the efficacy and safety of TVT‐O and TOT (TOT, Dow Medics, Korea) | |
| Participants | 100 women Inclusion criteria: women with USI Exclusion criteria: predominant urge incontinence or POP Preoperative work‐up included a medical history, physical examination, urinalysis, urodynamic evaluation, and I‐QOL questionnaire | |
| Interventions | Group A: TVT‐O (n = 50) Group B: TOT (n = 50) | |
| Outcomes | Surgical outcomes were evaluated by the cough‐stress test and symptom questionnaire and scored as cured, improved, or failed. Participants were considered ‘cured’ of SUI if they had a negative cough‐stress test result and there were no reports of urine leakage during stress. Participants were considered ‘improved’ if they did not leak on the cough‐stress test but may have had occasional urine leakage during stress; this occasional leakage did not influence their daily activities or require further treatment. Participants who did not meet these criteria were considered to have ‘failed’ treatment | |
| Notes | Surgical outcomes in the 2 groups were compared about 1 year after surgery. TOT, Dow Medics, Korea = woven monofilament polypropylene mesh | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | 100 women with SUI were alternately assigned |
| Allocation concealment (selection bias) | High risk | Quasi‐randomised study with no mention of allocation concealment |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT comparing TVT and TVT‐O | |
| Participants | 89 women Inclusion criteria: women with confirmed SUI without DO Exclusion criteria: DO; other gynaecological disease requiring hysterectomy; other gynaecologic operation; failed surgical treatment for incontinence Mean age (years): Group A: 53; Group B 52 Post menopausal: Group A: 22/46; Group B: 26/43 | |
| Interventions | Group A: TVT (n = 46) Group B: TVT‐O (n = 43) | |
| Outcomes | Participants assessed by means of voiding diaries, pad test, negative cough‐stress test at UDS, unvalidated symptom questionnaire
Subjective cure and failure determined by direct questions using an unvalidated questionnaire Follow‐up 12 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "... All patients were randomly assigned to an operation from the outpatient department ..." |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Low risk | No differential loss to follow‐up or differential attrition |
| Methods | RCT comparing Monarc TOT and TVT‐O | |
| Participants | 120 women were randomised Exclusion criteria: preoperative maximum urethral closure pressure < 20 cm water; urodynamic findings of DO; previous operation of the anterior vaginal wall or prolapse > stage 1 according to the ICS classification | |
| Interventions | Group A: TVT‐O (n = 61) Group B: Monarc TOT (n = 53) | |
| Outcomes |
| |
| Notes | Both groups had perioperative cystoscopy. Follow‐up was 12 months. 6 lost to follow‐up leaving a total of 114 women | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients were randomly allocated on an alternative fashion to one or another operation." |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded |
| Incomplete outcome data (attrition bias) | Low risk | No differential loss to follow‐up or differential attrition |
| Methods | RCT comparing TVT with IVS and SPARC | |
| Participants | 195 women Inclusion criteria: women with USI were randomly allocated to suburethral slingoplasty with either TVT, IVS or SPARC. Exclusion criteria: women with a past history of urogenital malignancy, fistula or pelvic radiotherapy At 6‐12 weeks follow‐up, 4, 5 and 4 women from the TVT, IVS and SPARC groups, respectively, were excluded from statistical analysis because of incomplete or missing hospital charts | |
| Interventions | Group A: TVT (n = 61) Group B: IVS (n = 60) Group C: SPARC (n = 61) | |
| Outcomes |
| |
| Notes | Group A: 4 patients; Group B: 5 patients; and Group C: 4 patients were excluded from the analysis due to incomplete or missing data. Those with missing records, those lost to follow‐up and those who failed to have postoperative UDS were assumed to be failures in the assessment of objective cure. Occult cases were excluded from subjective cure rates Follow‐up initially for 12 weeks and results reported, a follow‐on study reviewed the incidence of erosion and tape infections | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...195 consenting patients with urodynamic stress incontinence (USI) were randomly allocated in a balanced way (three groups of 65 patients each)..." |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: " ... and the patients were blinded to the type of slings being implanted ..." No description of how this was achieved. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | Unclear |
| Methods | RCT comparing TVT with SPARC sling | |
| Participants | 301 women Inclusion criteria: women presenting with SUI whether or not they had had previous incontinence or other pelvic surgery, or both Exclusion criteria: < 18 years old; pregnant; had a major voiding dysfunction specified as an abnormal flow (i.e. maximum urinary flow rate < 10 ml/s) or residual urinary volume of > 150 ml 254 women had UDS and USI diagnosed MUI: 47 women | |
| Interventions | Group A: TVT (n = 147) | |
| Outcomes | Primary outcome: bladder perforation Secondary outcomes:
The subjective assessments of cure were the participants' reported use of protection, their perceptions of the severity of their SUI symptoms and a scale of improvement (1 to 100). The objective definition of cure was the observed absence of urinary leakage when the participant coughed while supine and with a comfortably full bladder Follow‐up was 6 weeks | |
| Notes | The women and the outcome assessors were blinded, but no clear description was provided for how this was achieved | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were stratified based on previous UI surgery (yes, no) and the experience of the surgeon (consultant, registrar) and allocated to either TVT or SPARC using computer‐generated random numbers. The biostatistician generated the random allocations, which were sealed in opaque, sequentially numbered envelopes. The surgeons recruited participants and accessed the allocations by a telephone call to a third party. Varying block sizes of 4, 6 and 8 were used within each stratum to preclude prediction of allocation by the surgeons |
| Allocation concealment (selection bias) | Low risk | Concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "The analyst was unaware of the treatment allocation, but it was obviously not possible to ensure that the surgeons were unaware of treatment, although the patients were unable to detect, from their incisions, which sling they had received" |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The analyst was unaware of the treatment allocation, but it was obviously not possible to ensure that the surgeons were unaware of treatment, although the patients were unable to detect, from their incisions, which sling they had received" |
| Incomplete outcome data (attrition bias) | Low risk | No differential loss to follow‐up or differential attrition |
| Methods | RCT comparing TVT‐O and TVT | |
| Participants | 102 women with SUI with or without POP Preoperative urodynamics carried out | |
| Interventions | Group A: TVT‐O (n = 48) | |
| Outcomes |
| |
| Notes | Follow‐up 6 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A prospectively randomised and comparative study....." |
| Allocation concealment (selection bias) | Low risk | Quote:"...technique was randomly drawn using blinded envelopes containing the same no of ..." |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT of TVT vs TOT | |
| Participants | 32 women with SUI | |
| Interventions | A: TOT (n = 17) B: TVT (n = 15) | |
| Outcomes | Subjective cure Bladder Injury Major vascular injury: De novo UUI Mean operative time | |
| Notes | I‐QoL questionnaire was used | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients were randomised for TOT and TVT operations" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT of TVT compared with IVS | |
| Participants | 190 women randomised with 11 lost to follow‐up, thus 179 available for analysis at 2‐year follow‐up. The 2 groups were no different in terms of age, parity, BMI, previous hysterectomy, or presence of OAB symptoms Exclusion criteria: previous anti‐incontinence surgery; vaginal prolapse requiring treatment; coexisting pelvic pathology; known bleeding diathesis or current anticoagulant therapy; DO; and urethral hypomobility (Q‐tip <20° from the horizontal with straining) | |
| Interventions | Group A: TVT (n = 92) | |
| Outcomes | Primary outcome: success rate Secondary outcome measure: complication rate The outcome of surgical treatment was estimated both subjectively and objectively. Objective cure was defined as no leakage of urine while performing the cough provocation test, with at least 300 ml of saline in the bladder and as a pad weight gain < 1g during the 1‐h test. Test‐retest reliability of the cough test and 1‐hr pad test have been previously demonstrated. Subjective cure was defined as no urine loss during 'stress' and failure as any reported leakage of urine during exertion | |
| Notes | IVS = multifilament threads with smaller pores with insertion similar to TVT | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...a prospective randomised multicenter trial ... were randomly assigned to treatments according to a centralized computer‐generated random list.... Researchers randomly assigned participants by a telephone system to 1 of the treatment groups" |
| Allocation concealment (selection bias) | Low risk | Concealed |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT of TVT versus TVT‐O | |
| Participants | Inclusion criteria: women with urodynamic SUI and urethral hypermobility Exclusion criteria: previous anti‐incontinence surgery; vaginal prolapse requiring treatment; coexisting pelvic pathology; known bleeding diathesis or current anticoagulant therapy; DO and urethral hypomobility (Q‐tip <20° from the horizontal with straining) | |
| Interventions | 206 women randomised, but 25 lost to follow‐up Group B: TVT‐O (n = 117) | |
| Outcomes | Primary outcome: success rate Secondary outcome: complication rate Outcome of surgical treatment was estimated both subjectively and objectively. Objective cure was defined as no leakage of urine whilst performing the cough provocation test. Subjective cure was defined as no urine loss during ‘stress’, and failure as any reported leakage of urine during exertion ICIQ‐SF, Women Irritative Prostate Symptoms Score (W‐IPSS), PGI‐S and PGI‐I questionnaires were used to evaluate the impact of incontinence and voiding dysfunction on QoL, and to measure the participant’s perception of incontinence severity and improvement | |
| Notes | Median follow‐up time was 6 months 6 women from Group A and 7 from Group B were lost to follow‐up without outcome data; reasons for loss to follow‐up not explored Cystoscopy was performed in all cases of TVT and 50% of cases of TVT‐O | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women with SUI and urethral hypermobility were randomised to treatments according to a centralised computer‐generated random list. Researchers randomised participants by a telephone system to one of the treatment groups |
| Allocation concealment (selection bias) | Low risk | Concealed |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Low risk | No differential loss to follow‐up or differential attrition |
| Methods | RCT of classic TVT tape by Gynecare compared with LIFT by Cousin Biotech, with the distinctive feature of a suburethral pad (assumed to be inserted as classic TVT) | |
| Participants | 254 women with SUI | |
| Interventions | Group A: TVT (n = 123) Group B: LIFT (n = 125) | |
| Outcomes |
| |
| Notes | Follow‐up 12 months LIFT is a woven monofilament polypropylene tape that can be passed through the transobturator and also the retropubic routes The study seemed to compare the 2 tapes (TVT and LIFT), which have similar characteristics and were both passed through the retropubic routes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "..an open, prospective, randomised, multicentric study". How sequence generation was achieved not mentioned |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | QRCT of TVT vs TOT | |
| Participants | Inclusion criteria: women > 18 years; with SUI or MUI if SUI is the predominant symptom; women with ISD Exclusion criteria: predominant urge incontinence; UTI; malignancy; pregnancy; POP stage 3 or 4 Mean age (years; SD): Group A: 39.5 (1.95); Group B: 50.2 (1.89) Post menopausal status: Group A 8/18; Group B: 6/18 | |
| Interventions | Group A: TVT (n = 18) Group B: TOT (n = 18) | |
| Outcomes |
| |
| Notes | Cystoscopy performed only in the TVT group I‐QOL questionnaire assessed at 12 month F/U: significant improvement in I‐QOL total scores in both groups from the pre‐operative baseline scores. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Allocation of participants by alternation (quasi randomised) |
| Allocation concealment (selection bias) | High risk | Allocation not concealed |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT of TVT (Gynecare) vs TOT ('outside‐in' Monarc) | |
| Participants | 100 women Inclusion criteria: women with SUI or MUI with a predominant stress component, after failed conservative treatment Exclusion criteria: urge incontinence; previous mini invasive operation for SUI and the need for another concomitant surgical procedure SUI diagnosed with a positive cough test Urodynamic testing was only done in 5 patients (10%) Pure SUI: Group A: 38/50; Group B: 30/50 Preoperative characteristics similar between groups | |
| Interventions | Group A: TOT (n = 50) Group B: TVT (n = 50) | |
| Outcomes |
Follow‐up at 3, 14 and 46 months Cough stress test was performed. Subjective cure and patient satisfaction recorded with aid of UISS and Detrusor Instability Score questionnaires with a specific question about satisfaction | |
| Notes | Cystoscopy only performed in the TVT group Number available for follow‐up assessments: 14 months: Group A: 43/50; Group B: 43/50 At 46 months: Group A: 46/50; Group B: 47/50 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "This prospective randomized study included ... 100 patients were randomized either to the TVT or to the TOT" |
| Allocation concealment (selection bias) | Low risk | Quote: "randomization was performed with sealed and numbered envelopes" |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Low risk | No evidence suggestive of attrition bias |
| Methods | RCT of Vypro mesh (Ethicon, USA) vs Ultrapro mesh (Ethicon) vs Prolene light mesh (condensed monofilament non‐absorbable polypropylene) | |
| Participants | 144 women with SUI in Turkey Inclusion criteria: previous incontinence surgery or hysterectomy; SUI or USI; positive stress test Exclusion criteria: urodynamically MUI and DO; ≥ 100 ml PVR; contraindication to anaesthesia; POP; pregnancy; neurogenic bladder; bladder outlet obstructions; urinary fistula; or active urinary or vaginal infection Mean age (years; SD): Group A: 50.06 (9.2); Group B: 50.9 (8.8); Group C: 48.1 (7.9) Mean BMI kg/m² (SD): Group A: 27.8 (3.4); Group B: 27.9 (4.1); Group C: 27.7 (2.9) Post menopausal: Group A: 10/48; Group B: 11/48; Group C: 8/48 Previous incontinence surgery: Group A: 4/48; Group B: 5/48; Group C:4/48 | |
| Interventions | Group A: Vypro mesh: (n = 48; multifilament) Group B: Ultrapro mesh: (n = 48; monofilament + biological combined mesh) Group C: Prolene light mesh: (n = 48; monofilament) | |
| Outcomes | Primary outcome: urinary continence rates at 4‐year follow‐up Secondary outcomes assessed at 4‐year follow‐up:
| |
| Notes | Follow‐up at 6, 12, 24 and 48 months Loss to follow‐up Group A: 2/48; Group B: 0/48; Group C: 1/48 QoL and incontinence was evaluated with the ICIQ‐SF | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “The patients and the mesh materials were randomised 1:1:1 to each group in blocks of three via a centralized computerized system to ensure a good balance of participant characteristics in each group." |
| Allocation concealment (selection bias) | Low risk | Quote: “via a centralized computerized system to ensure a good balance of participant characteristics in each group” |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT of TVT‐O and TVT | |
| Participants | 45 women Inclusion criteria: women with SUI with and without ISD Exclusion criteria: women with stage 2 or more POP, women with ISD Mean age of 53.9 years Participants had preoperative UDS diagnosis | |
| Interventions | Group A: TVT (n = 17) | |
| Outcomes |
| |
| Notes | Follow‐up 12 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...women with SUI were randomly assigned ..." |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT of TOT + mesh repair of POP vs TVT + mesh repair of POP | |
| Participants | Inclusion criteria: 15 women with cystocoele and SUI with urethral hypermobility Exclusion criteria: BMI > 30 kg/m²; previous incontinence surgery and detrusor instability and/or intrinsic sphincter dysfunction | |
| Interventions | Group A: TOT + mesh repair of POP Group B: TVT + mesh repair of POP | |
| Outcomes | Trial terminated due to poor recruitment, no results published | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Stated: "randomised" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT of synthetic UretexTO® vs biological PelviLaceTO® outside‐inside TOT | |
| Participants | Inclusion criteria: women with SUI and USI; SUI with urethro‐vesical junction hypermobility without ISD Exclusion criteria: POP > stage 1; previous urogynaecological or anti‐incontinence surgery; concurrent diseases such as psychiatric disease, diabetes, peripheral vascular disease; history of pelvic radiation; urge and mixed incontinence; DO; urgency or neurologic bladder; maximum urethral closure pressure < 20 cm H2O and VLPP < 60 cm H2O (indicators of intrinsic sphincter deficiency); maximum flow ≤ 12 ml/s; and PVR volume ≥ 100 ml Mean age (years; SD): Group A: 60.7 (7.1); Group B: 59.4 (8.4) Mean BMI kg/m² (SD): Group A: 25.4 (1.8); Group B: 24.9 (1.8) Menopausal: Group A: 26/34; Group B: 30/36 (participants in menopause were subjected to at least 1 month of local hormone replacement therapy both before and after the surgery) QoL and sexual impact measured via: KHQ and PISQ‐12 | |
| Interventions | Group A: synthetic UretexTO® (n = 34) Group B: biological PelviLaceTO® (n‐36) | |
| Outcomes |
| |
| Notes | Group A: synthetic (UretexTO®; Bard, Covington, GA) is self‐anchoring transobturator suburethral sling (1.2 cm wide and 45 cm long) made of the same monofilament polypropylene fibres used in many modern tension‐free sling devices (for example TVT, TVT‐O, TOT Monarc, TOT ARIS etc). Polypropylene is a very biocompatible material that has been used for many years in the construction of medical‐grade synthetic meshes. The important difference is how the polypropylene fibres are knitted to form a cohesive macroporous mesh Group B: biological material (PelviLaceTO®; Bard, Covington, GA) is a tension‐free and self‐anchoring transobturator suburethral sling (1.5 cm wide and 40 cm long). It consists of a porcine dermal collagen implant that is intended to provide a matrix for the incorporation of new tissue, cells and blood vessels, thanks to a natural porosity and artificial V‐shaped holes along the arms. Its collagen matrix consists of 3 amino acid chains arranged in a triple helix that has been cross‐linked with hexamethylenediisocyanate to improve durability making the collagen non‐resorbable by the collagenase (enzymes produced by inflammatory cells and fibroblasts that increase during surgery). It is also described as an acellular and deproteinised material so it should not cause an immune response Follow‐up evaluation was carried out after 6 weeks, 6 months, 1, and 2 years 2‐year follow‐up: Group A: 16.6 (3.0); Group B: 17.2 (3.0) Loss to follow‐up: Group A: 1/34; Group B: 0/36 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “Randomization was done using sealed opaque envelopes containing computer‐generated random allocations in a ratio of 2:2 in balanced blocks of 4” |
| Allocation concealment (selection bias) | Low risk | Quote: “Randomization was done using sealed opaque envelopes containing computer‐generated random allocations in a ratio of 2:2 in balanced blocks of 4” |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: “Follow‐up evaluation was carried out after 6 weeks, 6 months, 1, and 2 years (and/or earlier if problems were experienced) for all patients by two independent physicians” |
| Incomplete outcome data (attrition bias) | Low risk | Quote: “All patients in both arms completed the follow‐up (2 years)” |
| Methods | Pseudo RCT of TVT‐O vs TOT (Monarc) | |
| Participants | 74 women Inclusion criteria: women with SUI including those with MUI Exclusion criteria: neurogenic bladder; POP; suspected ISD; or a past history of radical pelvic surgery Mean age (years): Group A: 54.4 (10.13); Group B: 55.1 (10.63) Mean BMI kg/m²: Group A: 28.9 (0.53); Group B: 25.9 (0.48) Urgency/UUI: Group A: 25/39; Group B: 22/35 | |
| Interventions | Group A: TVT‐O (n = 39) Group B: TOT Monarc (n = 35) | |
| Outcomes | Cure was defined as the absence of any episodes of involuntary urine leakage during stressful activities and a stress test. Improvement was defined as a significant reduction in urine leakage, such that it did not require further treatment
| |
| Notes | Cystoscopy was performed in all women | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “were included in this randomised, prospective, observational study” |
| Allocation concealment (selection bias) | High risk | Quote: "The procedure was performed by a single surgeon, and patients underwent one of the two techniques in accordance with the scheduling order (MONARC and TVT‐O), in alternation" |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Low risk | All accounted for |
| Methods | RCT TVT‐O vs Monarc TOT | |
| Participants | Inclusion criteria: women having a primary continence procedure without other surgery; diagnosis of USI; completed course of physiotherapy; completed family Exclusion criteria: previous continence or prolapse surgery; neurological disease; pregnancy; UTI or vaginal infection; DO; voiding problem; anticoagulant use | |
| Interventions | Group A: TVT‐O Group B: TOT | |
| Outcomes | Primary outcomes: objective and subjective cure of USI Secondary outcomes:
| |
| Notes | Note: trial started recruitment 2006 but no evidence of current status i.e. completed or recruitment stopped or abandoned. No data published | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "patient allocation by random numbers with blocking" |
| Allocation concealment (selection bias) | Low risk | Quote: "patient allocation by random numbers with blocking" |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information. |
| Methods | RCT of TVT versus TOT | |
| Participants | 145 women Inclusion criteria: women with stress or MUI (stress component clinically predominant) associated with urethral hypermobility (ICS definitions) Exclusion criteria: previous anti‐incontinence surgery and POP > stage 1, according to the Half‐Way system and POP‐Q system classification, in any vaginal compartment With the exception of DO, which was significantly more common in the TOT group, no significant intergroup differences emerged with regard to surgical histories, SUI grade, frequency of mixed incontinence, preoperative voiding or storage symptoms and preoperative urodynamic parameters VLPP determined at a bladder volume of 200 mL and participants performed several Valsalva manoeuvers with a gradual increase in abdominal pressure. Participants stratified by VLPP > 60 cm H2O or VLPP ≤ 60 cm H2O VLPP ≤ 60 cm H2O (ISD): Group A: 25/70; Group B: 25/75 Mean age (years; SD): Group A: 61.8 (10.7); Group B: 60.6 (10) Postmenopausal: Group A: 61/70; Group B: 64/75 SUI: Group A: 42/70; Group B: 41/75 MUI: Group A: 28/70; Group B: 34/75 DO: Group A: 4/70; Group B: 14/75 | |
| Interventions | Group A: TVT (n = 70) Group B: TOT (n = 75) | |
| Outcomes | Primary outcomes:
Secondary outcomes:
All participants completed 2 validated questionnaires on QoL, the UDI‐6 and the IIQ‐7 before surgery, at 3, 6, 12 months postoperatively and then annually Patient satisfaction outcome was measured via a VAS scale Objective cure (dry) Objective cure and improved (dry + wet but improved) Subjective cure (dry) Subjective cure and improved(dry + wet but improved) Bladder injury Vaginal perforation Major vascular injury Voiding Dysfunction Tape erosion Long‐term follow‐up (> 6 years, mean 99 ± 19 months): 83 participants (45 TOT; 38 TVT) underwent a telephone interview in October 2012. | |
| Notes | TVTTM (Gynecare; Ethicon, Somerville, NJ, USA) TOTTM was a fusion‐welded, non woven, non knitted polypropylene tape (Obtapej; Mentor‐Porges, Le Plessis‐Robinson, France) All participants underwent a preoperative urodynamic assessment and intraoperative cystoscopy Follow‐up was at 3, 6, and 12 months postoperatively, and then annually Lower urinary tract dysfunctions and continence status were measured at each follow‐up visit by a blinded assessor The overall median follow‐up was 35 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "prospectively randomized by a predetermined computer‐generated randomization code, to the retropubic approach (TVT) or the transobturator route (TOT)" |
| Allocation concealment (selection bias) | Low risk | Quote: " Randomization was done using sealed, opaque, numbered envelopes, which contained the randomized allocation" |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors were blinded |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "No patient was lost during follow‐up" |
| Methods | RCT comparing TVT and IVS | |
| Participants | 100 women Inclusion criteria: women with USI without concomitant pelvic pathology requiring surgery, some had had anti‐incontinence surgery previously Exclusion criteria: ISD | |
| Interventions | Group A: TVT (n = 50) Group B: IVS (n = 50) | |
| Outcomes |
Participants were considered totally cured when free of all SUI symptoms, and cough tests in supine and standing positions were negative. The operation was noted as a failure if the participant still reported urine leakage during increases in intra‐abdominal pressure, the cough test with a comfortably full bladder was positive, and the woman had to change her pads because of being wet during the day In the improvement group the cough test was negative but participants still experienced stress urinary leakage (much less frequent than previously) and the pads were occasionally wet Postoperative UDS was not performed | |
| Notes | Median follow‐up of 13.5 months (range 4 to 18 months) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear |
| Allocation concealment (selection bias) | Unclear risk | Simple randomisation was used from pseudo‐random numbers (pseudo‐random number means that the participants were operated on by the TVT or the IVS method in a ratio of 1:1). Generated by computer in order to allocate participant to the monofilament or the multifilament group. Investigator KR was not involved in surgical procedure but was responsible for proper randomisation. |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded |
| Incomplete outcome data (attrition bias) | Unclear risk | Unclear |
| Methods | RCT of retropubic IVS‐02 vs transobturator IVS‐04, multifilament type 3 tape | |
| Participants | Inclusion criteria: women with SUI with a positive cough provocation test Exclusion criteria: presence of uterine myoma; ovarian cyst; or advanced uterine or vaginal prolapse (POP‐Q scale > grade 1) Mean age (years; SD): Group A: 55.56 (10.19); Group B: 55.75 (11.29) Postmenopausal: Group A: 119/269; Group B: 125/268 VLPP: leak pressure during Valsalva manoeuvre was measured. VLPP was determined at 180 ml of bladder filling. ISD was defined as VLPP of ≤ 60 cm H2O ISD: Group A: 45/269; Group B: 40/268 | |
| Interventions | Group A: retropubic (IVS‐02; n = 269) Group B: transobturator (IVS‐04; n = 268) | |
| Outcomes |
| |
| Notes | The follow‐up visits were at 1, 4, 6, 12, and 18 months Cystoscopy only performed in the retropubic group Loss to follow‐up: Group A: 68/269; Group B: 71/268 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “Simple randomisation was used from pseudorandom numbers generated by a computer to allocate patients into the IVS‐02 group or the IVS‐04 group” |
| Allocation concealment (selection bias) | Unclear risk | Investigators Jankiewicz and Futyma were not involved in the surgical procedures, but they were responsible for the randomisation process |
| Blinding of participants and personnel (performance bias) | Unclear risk | Quote: "the surgeon was aware of the procedure being used” |
| Blinding of outcome assessment (detection bias) | Unclear risk | Quote:"Only investigators Jankiewicz and Futyma were involved in the follow‐up process, and they were blinded with regard to the treatment procedure used" |
| Incomplete outcome data (attrition bias) | Low risk | All outcome data accounted for and the equivalent no of women were lost to follow‐up in the 2 groups |
| Methods | RCT of standard TOT vs TOT with 2‐point tape fixation sutures to prevent tape displacement | |
| Participants | 463 women Inclusion criteria: women with urodynamically proven SUI, Including women with ISD Exclusion criteria: OAB, MUI Mean age (years; SD): Group A: 55.8 (11.3); Group B: 54.8 (9.8) Mean BMI kg/m² (SD): Group A: 28.9 (6.7); Group B: 28.2 (3.8) ISD: Group A: 41/232; Group B: 42/231 | |
| Interventions | Group A: TOT (n = 232) Group B: TOT with fixation (n = 231) | |
| Outcomes |
| |
| Notes | Both tapes were monofilament Lost to follow‐up: Group A: 19/232; Group B: 26/231 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomly allocated to 2 groups" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT: multi‐centre randomised equivalence trial conducted in the USA | |
| Participants | 597 women Inclusion criteria: age >21 years; predominant SUI for >3 months (urgency UI allowed); positive urinary stress test; bladder volume >300 ml Exclusion criteria: not defined Baseline characteristics similar between groups Mean age (years; SD): Group A: 52.7 (10.5); Group B: 53.1 (11.5) Previous incontinence surgery: Group A: 38/297; Group B: 41/298 Previous prolapse surgery: Group A: 13/297; Group B: 10/298 Postmenopausal: Group A: 209/297; Group B: 206/298 BMI kg/m²: Group A: 30.6; Group B: 30 HRT: Group A: 81/297; Group B: 90/298 Concomitant pelvic surgery: Group A: 73/298; Group B: 78/299 | |
| Interventions | Group A: retropubic sling (TVT; n = 298) Group B: transobturator tapes (TVT‐O, and TOT Monarc; n = 299) (Group C (?): TVT‐O (inside‐out) ‐ separate data not provided) (Group D (?): TOT (Monarch, outside‐in) ‐ separate data not provided) | |
| Outcomes | Composite primary outcomes:
Secondary outcomes:
| |
| Notes | TOMUS trial NCT00325039 Per protocol Lost to follow‐up: Group A: 18/298; Group B: 14/299 PISQ measures dyspareunia, coital incontinence and fear of coital incontinence | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Permuted block randomisation schedule with stratification by centre |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | Quote: "patients who were lost to follow‐up were considered to have had treatment failure and when patients who were lost to follow‐up were excluded” |
| Methods | RCT TVT versus TOT | |
| Participants | Inclusion criteria: SUI with urethral hypermobility; age 40‐85 years; urethro‐cystocoele of grade 0‐2 Exclusion criteria: previous prolapse or IU surgery; anterior or posterior vaginal wall repair with mesh No difference recorded between the 2 groups for age, parity, or incontinence severity | |
| Interventions | Group A: TOT (n = 65) Group B: TVT (n = 66) | |
| Outcomes | Gynaecological examination, full urodynamic evaluation, voiding diary and KHQ were performed pre‐ and postoperatively | |
| Notes | 12‐month follow‐up | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "A randomised study". No description of how randomisation was achieved or if allocation was concealed |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT TVT vs TOT | |
| Participants | 199 women from tertiary care hospital and 2 academic community hospitals in Calgary, Canada Inclusion criteria: elected surgical management of SUI following positive cough stress test Exclusion criteria: previous incontinence surgery; requirement for any concurrent surgery; OAB (urinary frequency and urgency with or without urgency incontinence); >100 ml PVR; intended to have more children; Alzheimer’s or Parkinson’s disease; progressive neurological disease such as multiple sclerosis; immunocompromised Mean age (years; SD) Group A: 51.8 (10.4); Group B: 50.1 (8.3) Mean BMI kg/m² (SD): Group A: 28.1 (5.4); Group B: 27.8 (5.7) Postmenopausal: Group A: 46/105; Group B: 37/94 | |
| Interventions | Group A: TVT (n = 105) Group B: TOT (n = 94) | |
| Outcomes | Measured at 12 months
| |
| Notes | The outside‐in Obtryx Halo mid‐urethral sling system was used for transobturator tape procedures, and the Advantage retropubic mid‐urethral sling system was used for TVT procedure. Intraoperative cystoscopy was carried out for all participants Loss to follow‐up at 12 months: Group A: 9/105; Group B: 8/94 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. Quote: “The randomization list was generated by the study statistician (using ralloc procedure in Stata [StataCorp LP” |
| Allocation concealment (selection bias) | Low risk | The randomisation list was generated by the study statistician (using ralloc procedure in Stata (StataCorp LP, College Station, TX)) using permuted block randomisation with block sizes varying from 2 to 8 and stratification by surgeon. Neither the surgical team nor the participant knew the next treatment allocation. Randomisation was carried out a few days before surgery to ensure that the appropriate surgical device was available in the operating room |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | Quote: “Data were collected by an independent research nurse” Outcome measurement was not carried out blindly, but was conducted by a research nurse who was independent of clinical care |
| Incomplete outcome data (attrition bias) | Low risk | All data accounted for |
| Methods | RCT of TOT vs TVT | |
| Participants | 76 women with SUI, all had urodynamics | |
| Interventions | Group A: TOT (n = 37) Group B: TVT (n = 39) | |
| Outcomes |
| |
| Notes | No usable data provided | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "were included in this randomized controlled study .... Patients were randomly grouped" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT of TVT vs TOT (Monarc) vs TVT‐O | |
| Participants | 2 public teaching hospitals in Switzerland Inclusion criteria: women with urodynamically confirmed SUI, or MUI with predominant SUI Exclusion criteria: missing urodynamic assessment; previous sling procedure; predominant OAB; a PVR > 100 ml Mean age (years; SD): Group A: 57.8 (13.0); Group B: 56.6 (10.3); Group C: 59.3 (12.1) Mean BMI kg/m² (SD): Group A: 26.4 (3.7) Group B: 27.8 (4.6); Group C: 27.6 (4.8) | |
| Interventions | Group A: TVT (n = 80) Group B: TOT outside‐in approach (Monarc; n = 40) Group C: TVT‐O inside‐out approach (Gynecare; n = 40) | |
| Outcomes |
| |
| Notes | Preoperatively, conservative measures for SUI were recommended, such as use of local estrogens, pelvic floor re‐education, or incontinence pessaries. A symptomatic cystocele stage 2 or higher according to the POP‐Q system was corrected first. Participants with concomitant sling insertion to repair prolapse were included Cystoscopy was mandatory for every procedure Lost to follow‐up: Group A: 15; Group B: 6; Group C: 3 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Predetermined computer generated block randomisation in blocks of 8 to promote group balance |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Low risk | All participants accounted for |
| Methods | RCT of retropubic (TVT™ ) versus transobturator (Monarc™)) sling in the treatment of women with USI and ISD | |
| Participants | 163 women Inclusion criteria: women with SUI who had unsuccessful conservative therapy and, on UDS, had a diagnosis of USI and ISD ISD was defined as either a maximum urethral closure pressure (measured both with the bladder empty and at capacity) of <20 cm H2O and/or a pressure rise from baseline required to cause incontinence (Valsalva or cough leak point pressure) of ≤60 cm H2O Exclusion criteria: presence of pelvic infection; a persistent PVR volume > 100 ml; malignancy; fistula; or congenital or neurogenic bladder disorder Mean age (years; SD): Group A: 60 (11.5); Group B: 60 (10.9) Post menopausal: Group A: 66/82; Group B: 68/82 Previous incontinence surgery: Group A: 6/82; Group B: 11/82 Concomitant surgery: Group A: 29/82; Group B: 26/82 | |
| Interventions | Group A: TVT (n = 81) Group B: Monarc sling (n = 82) | |
| Outcomes |
| |
| Notes | Follow‐up was at 6 weeks and 6 months, then yearly for 3 years Loss to follow‐up: Group A: 5/82; Group B: 4/82 At 3‐year follow‐up: Group A: 72 followed‐up with 70 completing questionnaires, and 48 completing examination Group B: 75 followed‐up with 60 completing questionnaires, and 40 completing examination The number available for follow up or number lost to follow up at 5yrs was not made clear (authors have been contacted and response is awaited) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "... A prospective, randomised controlled trial was conducted using computer generated random allocation." |
| Allocation concealment (selection bias) | Unclear risk | No description of how allocation was concealed |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | The number of participants who withdrew or were lost to follow‐up (dropouts) was higher in the TVT group |
| Methods | RCT of retropubic Safyre VS adjustable sling system and Safyre T adjustable transobturator sling system | |
| Participants | 30 women Inclusion criteria: women with SUI Exclusion criteria: use of drugs (adrenergic, anticholinergic or serotonergic); hormone therapy within the previous 6 months; prior pelvic radiotherapy or current chemotherapy or hormone therapy; POP > stage 2; MUI | |
| Interventions | Group A: Safyre VS retropubic tape (n = 10) Group B: Safyre T transobturator tape (n = 20) | |
| Outcomes |
| |
| Notes | Follow‐up was at 1, 6 and 12 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomised into 2 groups |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Low risk | Data for all participants accounted for |
| Methods | RCT: TVT (AdvantageR) vs TOT (ObtryxR) | |
| Participants | 54 women with urodynamic SUI SUI: n = 10; MUI: n = 35 Median age in years (range): 54 (31‐76) BMI kg/m²: Group A: 27.8 (4.6); Group B: 27.4 (4.04) Concomittant POP surgery: Group A: 5/27; Group B: 2/27 | |
| Interventions | Group A: TVT (n = 27) Group B: TOT (n = 27) | |
| Outcomes | 12‐month follow‐up assessed:
2 year follow‐up assessed:
| |
| Notes | Concomitant POP surgery was performed in 7 women (6 cystocele, 1 rectocoele) No mention of intraoperative cystoscopy | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT of TVT vs TVT‐O | |
| Participants | 127 women recruited from 2 hospitals in the UK Inclusion criteria: women with USI Exclusion criteria: previous continence surgery; OAB symptoms; DO; POP‐Q > stage 1; presence of voiding dysfunction (defined as maximum flow rate < 15 ml/s or PVR volume ≥ 100 ml) Women in both groups had similar background characteristics, degree of severity of symptoms and QoL scores Mean age (years; SD): Group A: 52.4 (11.8); Group B: 50.9 (11.4) Median BMI kg/m² (range): Group A: 27 (21‐37); Group B: 29 (21‐50) Postmenopausal: Group A: 24/66; Group B: 19/61 | |
| Interventions | Group A: TVT (n = 66) Group B: TVT‐O (n = 61) | |
| Outcomes |
| |
| Notes | Intraoperative cystoscopy with a 70° cystoscope performed in all cases Loss to follow‐up at 12 months: Group A: 25/66; Group B: 32/61 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was done by a computer generated list randomised in blocks to ensure balanced allocation |
| Allocation concealment (selection bias) | Low risk | Randomization was done by a computer generated list randomised in blocks to ensure balanced allocation. Block size was randomised between 4 and 10. Numbered opaque envelopes were opened immediately before surgery |
| Blinding of participants and personnel (performance bias) | High risk | Participants and assessors were not blinded to the treatment received |
| Blinding of outcome assessment (detection bias) | High risk | Participants and assessors were not blinded to the treatment received |
| Incomplete outcome data (attrition bias) | High risk | High numbers lost to follow‐up; disproportionately higher in TVT‐O group |
| Methods | RCT comparing TVT‐O and a modified version of TVT‐O | |
| Participants | 72 women Inclusion criteria: urodynamically proved SUI; age > 30 years; and previously failed pelvic floor muscle training Exclusion criteria: previous surgery for SUI; isolated OAB; POP ≥ stage 2; neurological disease Mean age (years; SD): Group A: 51 (9.5); Group B: 55 (6.8) Mean BMI kg/m² (SD): Group A: 27.5 (4.9); Group B: 28.9 (3.7) | |
| Interventions | Group A: TVT‐O (n = 48) Group B: modified TVT‐O (n = 24) | |
| Outcomes |
| |
| Notes | For the modified TVT‐O: “Briefly, in contrast with the traditional technique, the paraurethral dissection was minimal and carried only up to the pubic ramus, without perforating the obturator membrane with the scissors The aim of this reduced dissection was to create a passage of very limited size to introduce the guide only up to the bone, without perforating the membrane. Thus, as opposed to the original procedure, the obturator membrane was perforated only by the helical passer” Lost to follow‐up: Group A: 2/48; Group B: 1/24 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “Patients were randomised using a randomisation list generated by computer” |
| Allocation concealment (selection bias) | Low risk | Quote: "The allocation sequence was concealed from the researchers (CF and AF) who enrolled, assessed, and assigned the participants to the interventions in sequentially numbered, opaque, sealed, and stapled envelopes. The envelopes were opened on the morning of the procedure for the surgeon to perform the allocated procedure" |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: “Patients were blinded to the procedure until the end of the study” |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Low risk | All data accounted for |
| Methods | RCT comparing TVT with SPARC | |
| Participants | 62 women Inclusion criteria: women with USI with or without POP Exclusion criteria: those with POP > ICS stage 2 and those with previous anti‐incontinence surgery Mean age was 51 years and median parity of 3. The 2 groups were similar in terms of age, parity and menopausal status | |
| Interventions | Group A: SPARC (n = 31) | |
| Outcomes | Objective cure: defined as pad weight ≤1g Improved: participants whose loss decreased to < half of the preoperative value were considered to have improved | |
| Notes | All women had routine suprapubic ultrasonography for detecting unrecognised subcutaneous or retropubic haematoma on the day immediately after the operation, and 7/8 of those with retropubic haematoma of >5 cm diameter were discharged uneventfully from the hospital within 7 days of the operation. Ultrasonography performed at the 1 month follow‐up visit revealed complete resolution of the haematoma for every participant Follow‐up at 2 years Women and their outcome assessors were blinded, but the exact method used to achieve this was unclear | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | By using a predetermined computer‐generated randomisation code, those subjects who acquiesced and satisfied the inclusion criteria were assigned randomly by the authors (except LHT) to the SPARC or TVT procedure at the outpatient clinic |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "The patients were blinded to the procedure, but the principle based on the integral theory was briefly explained to them" |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded |
| Incomplete outcome data (attrition bias) | Low risk | No differential loss to follow‐up or differential attrition |
| Methods | RCT of PELVILACE TO (biological TOT material) vs synthetic TOT material (ALIGN TO urethral support system) | |
| Participants | 100 women Inclusion criteria: women >18 years with SUI, MUI or USI in whom conservative treatment had failed. Women with or without POP were included Exclusion criteria: women with ISD Pre‐ and postoperative assessments included evaluation of urinalysis and urine culture POP evaluation using POP‐Q system, 1‐hr pad test, 4‐day bladder diary, stress test, Q‐tip test, and QoL assessment using the KHQ, UDI‐6, and the IIQ‐7. This was repeated at the 12‐month follow‐up. Postoperative urodynamics was performed in all patients accepting the procedure Mean age (years; SD): Group A: 55.0 (12.3); Group B: 52.9 (10.6) Mean BMI kg/m² (SD): Group A: 31.8 (6.6); Group B: 31.3 (4.8) Postmenopausal: Group A: 29 (56.9%); Group B: 30 (58.8%) Previous incontinence surgery: Group A: 2 (4%); Group B: 2 (4%) Concomitant POP surgery: Group A: 28/50; Group B: 28/50 | |
| Interventions | Group A: biological PELVILACE TO (n = 50) Group B: synthetic TOT ALIGN ®TO (n = 50) | |
| Outcomes | Primary outcome: patient‐reported improvement in urinary incontinence (either completely dry or improvement in symptoms of SUI; reported as 'cure,' 'better than before,' 'no change at all,' and 'worse than before.')
| |
| Notes | Biological tape was PELVILACE® TO system; Bard, Covington, GA, USA and the synthetic tape was ALIGN ®TO urethral support system; Bard TOT operation. The PELVILACE® TO system consists of a PELVICOL® self‐anchoring, natural tissue sling implant and an introducer system. This system contains a self‐anchoring, 1.5 cm wide, and 40 cm long suburethral sling of porcine dermal collagen. The ALIGN® TO urethral support system is a suburethral sling device made of type 1 monofilament polypropylene mesh designed for the treatment of SUI through the TOR Postmenopausal patients received local estrogen treatment for 1 month before and after the operation Concomitant POP was performed in a cohort of women | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: " In this prospective randomized study ... Randomization was carried out using computer‐generated random allocations prepared by an investigator with no clinical involvement in the trial" |
| Allocation concealment (selection bias) | Low risk | Quote: "computer‐generated random allocations prepared by an investigator with no clinical involvement in the trial" |
| Blinding of participants and personnel (performance bias) | Unclear risk | Quote: "The patients were blinded to the sling material used." |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Follow‐up was performed ... by the same physician who was blinded to the type of sling used" |
| Incomplete outcome data (attrition bias) | Low risk | All accounted for |
| Methods | RCT comparing RPR and TOT | |
| Participants | Dutch multicentre diagnostic cohort study with an embedded RCT 587 women with SUI; 123 randomised to surgery Inclusion criteria: women with urodynamically‐proven SUI, or MUI with SUI as predominant symptom following failed conservative treatment Exclusion criteria: prior incontinence surgery; POP > stage 2 POP‐Q; post PVR of >150 ml (by USS or characterisation) MUI: Group A: 18/33; Group B: 61/90 | |
| Interventions | Group A: RPR (n = 33) Group B: TOT (n = 90) | |
| Outcomes | Outcome results for TOT and RPR not reported as separate figures; we contacted the authors who supplied separate figures
| |
| Notes | QoL questionnaires: UDI | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A web‐based application was used for block randomisation and computer‐generated random number list prepared by a database designer" |
| Allocation concealment (selection bias) | Low risk | Quote: "Patient data were entered into a password‐protected web‐ based database" |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "Participants and health professionals were not blinded to the allocated arm and the urodynamic results" |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Data input of subjective outcome measurements was per‐formed by researchers who were blinded to the treat‐ment allocation" |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT of TOT (Monarc) and SPARC suburethral sling procedures | |
| Participants | 60 women with an average age of 50 years (SD 10.71 ) Exclusion criteria: women suffering from preoperative voiding dysfunction, which was defined as either: free Q max of ≤ 12ml/s in repeated free uroflow studies combined with Pdet Q max of ≥20cm H2O, PVR urine ≥ 100 ml, and participants with a pad increase of at least 10cm H2O, compared to the baseline abdominal pressure in a pressure‐flow study. Women who had previous anti‐incontinence surgery and/or with pelvic prolapse > stage 2 of the ICS grading system were also excluded. | |
| Interventions | Group A: Monarc (n = 31) Group B: SPARC (n = 29) | |
| Outcomes | Assessed via 1‐hr pad test, multichannel urodynamic assessment, complications and postoperative voiding function. Transabdominal USS to detect subcutaneous, retropubic or obturator haematoma | |
| Notes | The women were blinded to the procedure performed Intraoperative cystoscopy was performed in both groups | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "By using a predetermined computer‐generated randomisation code ... were assigned randomly by the senior author ..." |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | Quote: " ... The patients were blinded to the procedure ..." How this was achieved was not explained |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "an independent continence advisor and one of the authors both of whom were blinded to the procedures performed carried out the follow‐up examinations and post operative outcome assessments" |
| Incomplete outcome data (attrition bias) | Low risk | No differential loss to follow‐up or differential attrition |
| Methods | RCT of TVT vs TVT‐O Single‐blinded | |
| Participants | 69 women Inclusion criteria: severe female SUI with or without prolapse (< POP‐Q stage 3) Exclusion criteria: pregnancy; previous surgery for urinary incontinence Mean BMI kg/m² (SD): Group A: 25 (3); Group B: 25 (3) Mean age (years; SD): Group A: 52 (11); Group B: 52 (11) | |
| Interventions | Group A: TVT (n = 35) Group B: TVT‐O (n = 34) | |
| Outcomes |
| |
| Notes | Concomittant surgery: some women also had transvaginal hysterectomy and prolapse repair Follow‐up: mean 14.5 months Cystoscopy performed in TVT group only Article written in Chinese and translated to English for interpretation and data extraction | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation schedule |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | Single‐blinded (no information about who was blinded) |
| Blinding of outcome assessment (detection bias) | Unclear risk | Single‐blinded (no information about who was blinded) |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "All patients were evaluable" |
| Methods | RCT of TVT vs inside‐out TVT‐O 55 were participants in a previous study (ref 8, Zhu 2007: 23870; 27325) – already included | |
| Participants | 300 women Inclusion criteria: demonstrable severe SUI, or mild to moderate SUI that failed to respond to conservative treatment. All women had urodynamically confirmed USI (no detrusor contraction on leakage) Exclusion criteria: ;ISD MUI; pregnancy; UTI; UUI; PVR volume > 100 ml; neurological disease; urogenital malignancy, fistula, or pelvic radiotherapy Menopausal: Group A: 87/154; Group B: 88/146 Previous prolapse surgery: Previous incontinence surgery: Group A: 5; Group B: 5 | |
| Interventions | Group A: TVT (n = 154) Group B: TVT‐O (n = 146) | |
| Outcomes |
| |
| Notes | Signed informed consent, approved by Ethics committee Mean follow‐up: (months; SD): Group A: 19.6 (11.9); Group B: 20.5 (10.7; twice in first year, then yearly) Loss to follow‐up: Group A: 6; Group B: 8, + 1 withdrawn (operation postponed) Cystoscopy only performed in the TVT group Concomitant prolapse and other surgery | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The 315 women were allocated to the TVT or the TVT‐O group by an SAS randomisation schedule (SAS Institute Inc, Cary, NC, USA) |
| Allocation concealment (selection bias) | Unclear risk | Stated: ‘randomly allocated’, no further information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors blind: ‘independent gynaecologist’ |
| Incomplete outcome data (attrition bias) | Low risk | No differential dropout (Group A: 6; Group B: 9) |
| Methods | RCT comparing TVT and TOT‐outside/in | |
| Participants | 140 women Inclusion criteria: women with urodynamically proven SUI Exclusion criteria: OAB syndrome dry or wet Age (years; SD): Group A: 60 (10.8); Group B: 58 (11.6) Previous incontinence surgery: Group A: 5; Group B: 3 BMI kg/m² (SD): Group A: 24 (2.4); Group B: 24.6 (2.6) Concomitant POP: Group A: 30/70; Group B: 22/70 | |
| Interventions | Group A: TVT (n = 70) Group B: TOT (n = 70) | |
| Outcomes |
| |
| Notes | Cystoscopy only performed when bladder perforation suspected in TOT group. All TVT participants cystoscoped post procedure Concomitant surgery: All participants with POP had this repaired at the time of tape insertion Lost to follow‐up: Group A: 0 women; Group B: 0 women | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “Our study was a single blind randomised trial and the patients were randomly allocated to ...” |
| Allocation concealment (selection bias) | Unclear risk | Quote: “Our study was a single blind randomised trial and the patients were randomly allocated to ...” |
| Blinding of participants and personnel (performance bias) | High risk | Quote: “The patients were not blinded to the operative procedure” |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: “post op assessment was performed by FMW who did not take part in the operation , YFS who performed the surgery was not involved in follow up” |
| Incomplete outcome data (attrition bias) | Low risk | No participants withdrew. None were lost to follow‐up |
| Methods | RCT comparing TVT, TVT‐O and TVT‐Secur | |
| Participants | Total of 102 women included in this Chinese trial Inclusion criteria: women with urodynamically proven SUI. If MUI, then SUI was the predominant symptom Exclusion criteria: women with previous surgical procedures for SUI Mean age (years; SD): Group A: 56.6 (9.6); Group B: 56.0 (9.1) Mean BMI kg/m² (SD): Group A: 25.3 (2.0); Group B: 27.3 (1.9) | |
| Interventions | Group A: TVT (n = 32) Group B: TVT‐O (n = 36) Group C: TVT‐ Secur (data not included in this review) | |
| Outcomes |
| |
| Notes | Power test calculation performed Women with SUI were put on anticholinergic treatment prior to surgery QoL assessment was performed using the ICI‐Q‐SF pre‐operatively; no data for post‐operative scores Cystoscopy routinely performed in TVT. Cystoscopy only performed if bladder injury was suspected in the TVT‐O group Follow‐up 1, 3, 6 and 12 months All women completed the trial (no loss to follow‐up) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "computer generated randomisation" |
| Allocation concealment (selection bias) | Low risk | Quote: “allocation was concealed using opaque sealed envelopes” |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Low risk | All participants completed follow‐up. All outcomes reported |
| Methods | RCT comparing TVT‐O with a modified version of TVT‐O using a self‐tailored mesh | |
| Participants | 156 women in a Chinese hospital Inclusion criteria: women with SUI aged > 18 years Exclusion criteria: women with urgency; persistent urinary retention (PVR > 50 ml); dysuria; other urologic diseases and psychiatric disorders Mean age (years; SD): Group A: 61.4 (5.4); Group B: 62.6 (3.2) | |
| Interventions | Group A: TVT‐O (n = 76) Group B: modified TVT‐O (n = 80) | |
| Outcomes |
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “stratified randomisation” |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) | Unclear risk | No information |
| Methods | RCT comparing TVT and TVT‐O | |
| Participants | 72 women Inclusion criteria: women affected by SUI with no contraindications to vaginal surgery Excluded criteria: women with urogenital prolapse > stage 1; DO; symptoms of OAB; intrinsic urethral sphincter deficiency; urinary retention; previous anti‐incontinence surgery; neurologic bladder; and psychiatric disease Age (years; SD): Group A: 52.8 (11.8); Group B: 53.4 (10.7) BMI kg/m²: Group A: 25.7 (2.9); Group B: 26.5 (2.7) Menopausal: Group A: 6/35; Group B: 8/37 POP stage 1 and 2: Group A: 34/35; Group B: 35/37 | |
| Interventions | Group A: TVT (n = 35) Group B: TVT‐O (n = 37) | |
| Outcomes |
| |
| Notes | Intraoperative cystoscopy only performed in the TVT group 12 participants did not return for 5‐year follow‐up: 3 participants were lost (2 in the TVT group and 1 in the TVT‐O group), and 9 withdrew (4 in the TVT group and 5 in the TVT‐O group) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: " .. were randomly allocated to undergo a TVT or TVTO procedure by using a predetermined computer‐generated randomisation code" |
| Allocation concealment (selection bias) | Low risk | Allocation concealed |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) | Low risk | " ... outcome assessors at 5 years follow up blinded |
| Incomplete outcome data (attrition bias) | Low risk | No differential loss to follow‐up or differential attrition |
Abbreviations
BFLUTS: Bristol lower urinary tract symptoms questionnaires
BMI: body‐mass index
DO: detrusor overactivity
DUP: distal urethral polypropylene sling
EQOL‐5D: Euro Quality of life ‐5 Dimension
g: gram
hr: hour
HRT: hormone replacement therapy
ICIQ: International Consultation on Incontinence questionnaire
ICIQ‐FLUTS: International Consultation on Incontinence questionnaire ‐ female lower urinary tract symptoms
ICIQ‐ LUTSquol: International Consultation on Incontinence questionnaire ‐ lower urinary tract quality of life questionnaire
ICIQ‐SF: International Consultation on Incontinence questionnaire short form
ICIQ‐SF15: International Consultation on Incontinence questionnaire short form 15
IIQ: Incontinence Impact questionnaire
ICS: International Continence Society
I‐QoL: Incontinence Quality of Life questionnaire
ISD: intrinsic sphincter deficiency
IVS: intravaginal slingoplasty
KHQ: King's Health questionnaireMUI: mixed urinary incontinence
MUCP: Maximum urethral closure pressure
MUI: mixed urinary incontinence
OAB: overactive bladder
PGI‐I: Patient Global Impression of Improvment
PGI‐S: Patient Global Impression of Severity
PISQ‐12: pelvic organ prolapse/urinary incontinence sexual questionnaire
POP: pelvic organ prolapse
POP‐Q: pelvic organ prolapse quantification
POP‐Q ICS: pelvic organ prolapse quantification International Continence Society
PVR: post void residual
RCT: randomized controlled trial
RPR: retropubic route
QoL: quality of life
QRCT: quasi‐randomised trial
SEAPI‐QMM: Stress related leak, Empyting ability, Anatomy, Protection, Inhibition‐Quality of life, Mobility and Mental status incontinence classification system
SD: standard deviation
SIS: Single incision sling
SPARC: suprapubic arc (procedure)
SUI: stress urinary incontinence
TOR: transobturator
TOT: transobturator tape
TOT‐ARIS: transobturator tape‐ARIS
TVT: tension‐free vaginal tape
TVT‐O: transobturator tension‐free vaginal tape
UDI: Urinary Distress Impact questionnaire
UDI‐6: Urinary Distress Impact questionnaire short form
UDS: urodynamics study
UI: urinary incontinence
UISS: urinary incontinence severity score
USI: urodynamic stress incontinence
USS: ultrasound
UTI: urinary tract infection
UUI: urgency urinary incontinence
VAS: visual analogue scale
VLPP: Valsalval leak point pressure
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Not an RCT | |
| Sling apparently equivalent to TVT, but too little information provided to determine equivalence | |
| Not an RCT | |
| Sexual function analysis of 2 retrospective studies (not RCTs) | |
| Retrospective study, not an RCT | |
| RCT of bupivacaine and saline versus saline only for hydrodissection during TVT | |
| Not an RCT | |
| Not randomized | |
| Prospective comparative study with participants assigned not randomized. | |
| Was prospective, but not stated that randomized | |
| All women had TVT. Intervention groups were division vs no division of tape | |
| Traditional slings. No minimally invasive sling | |
| No minimally invasive sling | |
| An ultrasound study comparing tape position between RPR and TOR | |
| Trial stopped due to difficulty recruiting. Planned to recruit 30 participants to each arm but actually randomized less than 15 participants in total | |
| Non randomized prospective study | |
| Imaging study: aim of the study was to determine the mobility of the slings from ultrasound imaging of slings inserted in the parent trial (SUSPEND trial, Lim 2005) | |
| Not an RCT | |
| All had TVT | |
| Not an RCT | |
| Monarc vs mini single incision sling | |
| No minimally invasive sling | |
| Qualitative analysis on nonresponders of single incision sling RCT | |
| RCT of antibiotic use preoperatively for TVT and TOT (surgeons discretion for what tape was used) | |
| RCT of antibiotic vs. placebo for MUS surgery | |
| Not an RCT | |
| Not an RCT | |
| A prospective cohort study not an RCT | |
| Retrospective review of medical records | |
| Not an RCT | |
| RCT ‐ does not meet the inclusion criteria. Not MUS vs MUS. Tradition Sling vs TVT. This trial compares three techniques for performing sling surgery: TVT, porcine xenograft (Pelvicol) sling and the short autologous fascial sling technique 'Sling on a string'. | |
| A prospective cohort study not an RCT | |
| Prolapse trial not urinary incontinence | |
| RCT with randomisation based on the type of anaesthesia used for one minimally invasive sling procedure (TVT) | |
| RCT of TVT‐O vs TVT‐O plus 6 months postoperative estrodiol therapy. Both groups had TVT‐O performed | |
| RCT of Burch colposuspension versus traditional sling ‐ SISTEr Trial. Not MUS vs MUS | |
| Statistical modelling and not a trial in itself. No minimally invasive sling | |
| 1 tape used (TVT) and only occult urinary incontinence investigated | |
| No minimally invasive sling arm in the trial | |
| Prospective study of SPARC vs Monarc TOT but no evidence of randomisation | |
| Randomisation based on immediate or deferred cutting and readjustment of tape | |
| Same tape TOT randomized to either high‐tension or tension‐free | |
| Cohort study, not an RCT | |
| Investigated occult incontinence | |
| Not an RCT and no minimally invasive sling | |
| Not an RCT, retrospective study | |
| Non randomized longitudinal study | |
| No minimally invasive sling | |
| Not an RCT and only 1 arm, IVS | |
| Improvised instrument used | |
| A review article, not an RCT | |
| RCT of colposuspension or TVT with concomitant anterior repair (1 tape) | |
| Same tape TVT: randomized to either immediate TVT or TVT after 21 days of preoperative estrogen treatment | |
| Investigated occult urinary incontinence | |
| All women received TVT. Compared types of anaesthesia | |
| RCT of women with occult stress urinary incontinence undergoing POP surgery with and without concomitant MUS insertion | |
| Statistical modelling and not a trial in itself | |
| Non randomised inferiority study | |
| A comparative study but not an RCT | |
| RCT of single incision sling and TOT | |
| RCT of pelvic floor muscle training on comfort. | |
| All had TVT. Women were randomly allocated to receive TVT plus postoperative vaginal oestrogen therapy (ET group) or TVT without adjunctive medical treatment (no ET group) |
Abbreviations
IVS: intravaginal slingoplasty
MUS: mid‐urethral sling
POP: pelvic organ prolapse
RCT: randomized controlled trial
RPR: retropubic route
SIS: Single incision sling
TOR: transobturator route
TOT: transobturator tape
TVT: tension‐free vaginal tape
TVT‐O: tension‐free vaginal tape ‐ Obturator
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Prospective randomised study comparing TVT and TOT in female SUI with no ISD |
| Methods | RCT |
| Participants | Inclusion criteria: women aged 18‐70 years; with USI; with or without POP Exclusion criteria: previous incontinence surgery; UI or OAB; mixed incontinence; ISD; BMI > 35 |
| Interventions | Participants underwent either TVT or TOT procedures |
| Outcomes | Primary outcome: postoperative UDI‐6 and IIQ‐7 score <10 and negative cough test will be defined as 'cured' Secondary outcomes:
|
| Starting date | June 2013 |
| Contact information | |
| Notes | NCT01903590, expected completion date June 2014 |
| Trial name or title | Effects of surgical treatment enhanced with exercise for mixed urinary incontinence (ESTEEM) |
| Methods | |
| Participants | Women > 21 years Inclusion criteria:
Exclusion criteria:
|
| Interventions | Group A: mid‐urethral sling combined with peri‐ and postoperative behavioral/pelvic floor therapy Group B: mid‐urethral sling |
| Outcomes | |
| Starting date | October 2013, expected completion date October 2016 |
| Contact information | |
| Notes | NCT01959347 |
Abbreviations
BMI: body‐mass index
BPTx: behavioural/pelvic floor therapy
ESTEEM: Effects of surgical treatment enhanced with exercise for mixed urinary incontinence trial
IE; incontinence event
IIQ‐7: Incontinence Impact questionnaire
ISD: intrinsic sphincter deficiency
MUI: mixed urinary incontinence
OAB: overactive bladder
POP: pelvic organ prolapse
POP‐Q: pelvic organ prolapse quantification
PVF: post void residual
SUI: stress urinary incontinence
TOT: transobturator tape
TVT: tension‐free vaginal tape
UDI: Urinary Distress Impact questionnaire
UDI‐6: Urinary Distress Impact questionnaire short form
UI: urinary incontinence
USI: urodynamic stress incontinence
UUI: urgency urinary incontinence
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Subjective cure (short term, ≤ 1 year) Show forest plot | 36 | 5514 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.96, 1.00] |
| Analysis 1.1  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 1 Subjective cure (short term, ≤ 1 year). | ||||
| 2 Subjective cure and improvement (short term, ≤ 1 year) Show forest plot | 10 | 1651 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.96, 1.00] |
| Analysis 1.2 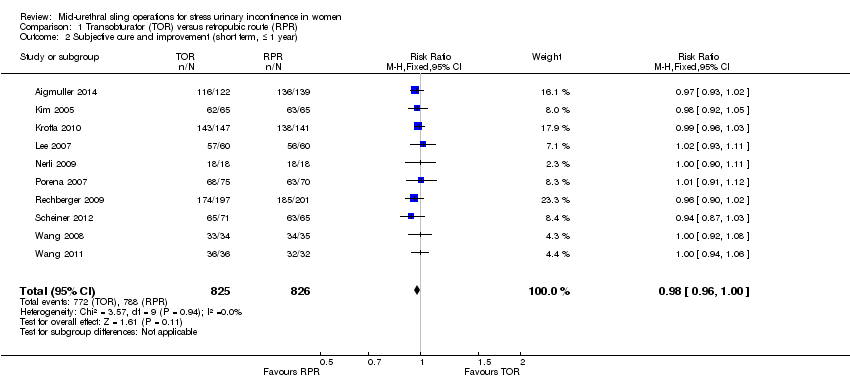 Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 2 Subjective cure and improvement (short term, ≤ 1 year). | ||||
| 3 Subjective cure (medium term, 1 to 5 years) Show forest plot | 5 | 683 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.87, 1.09] |
| Analysis 1.3  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 3 Subjective cure (medium term, 1 to 5 years). | ||||
| 4 Subjective cure (long term, > 5 years) Show forest plot | 4 | 714 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.80, 1.12] |
| Analysis 1.4  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 4 Subjective cure (long term, > 5 years). | ||||
| 5 Subjective cure and improvement (long term, > 5 years) Show forest plot | 2 | 340 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.67, 1.28] |
| Analysis 1.5  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 5 Subjective cure and improvement (long term, > 5 years). | ||||
| 6 Objective cure (short term, ≤ 1 year) Show forest plot | 40 | 6145 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.96, 1.00] |
| Analysis 1.6  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 6 Objective cure (short term, ≤ 1 year). | ||||
| 7 Objective cure and improvement (short term, ≤ 1 year) Show forest plot | 10 | 1478 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.96, 1.01] |
| Analysis 1.7  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 7 Objective cure and improvement (short term, ≤ 1 year). | ||||
| 8 Objective cure (medium term, 1 to 5 years) Show forest plot | 5 | 596 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.95, 1.06] |
| Analysis 1.8  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 8 Objective cure (medium term, 1 to 5 years). | ||||
| 9 Objective cure (long term, > 5 years) Show forest plot | 3 | 400 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.90, 1.06] |
| Analysis 1.9  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 9 Objective cure (long term, > 5 years). | ||||
| 10 Operative time (minutes) Show forest plot | 31 | 4713 | Mean Difference (IV, Random, 95% CI) | ‐7.54 [‐9.31, ‐5.77] |
| Analysis 1.10  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 10 Operative time (minutes). | ||||
| 11 Operative blood loss (ml) Show forest plot | 14 | 1869 | Mean Difference (IV, Random, 95% CI) | ‐6.49 [‐12.33, ‐0.65] |
| Analysis 1.11  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 11 Operative blood loss (ml). | ||||
| 12 Length of hospital stay (days) Show forest plot | 17 | 2170 | Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.59, 0.09] |
| Analysis 1.12  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 12 Length of hospital stay (days). | ||||
| 13 Time to return to normal activity level (weeks) Show forest plot | 4 | 626 | Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.15, 0.06] |
| Analysis 1.13  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 13 Time to return to normal activity level (weeks). | ||||
| 14 Perioperative complications Show forest plot | 15 | 2205 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.73, 1.14] |
| Analysis 1.14 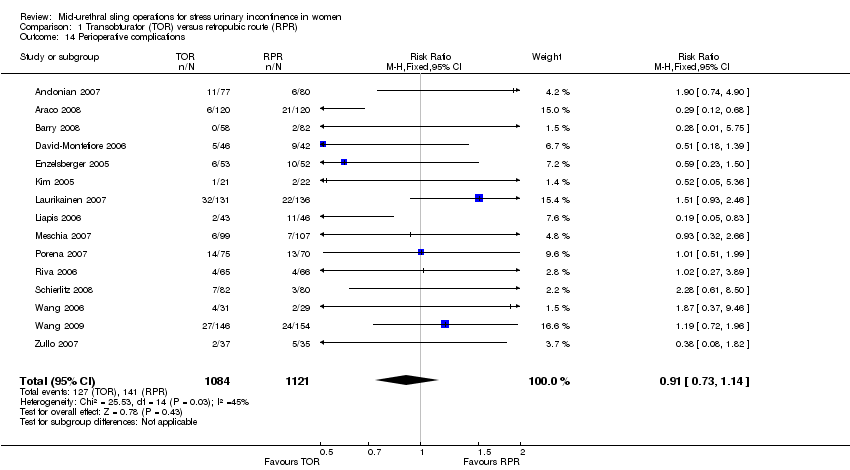 Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 14 Perioperative complications. | ||||
| 15 Major vascular or visceral injury Show forest plot | 28 | 4676 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.19, 0.55] |
| Analysis 1.15  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 15 Major vascular or visceral injury. | ||||
| 16 Bladder or urethral perforation Show forest plot | 40 | 6372 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.08, 0.20] |
| Analysis 1.16  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 16 Bladder or urethral perforation. | ||||
| 17 Voiding dysfunction Show forest plot | 37 | 6200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.43, 0.65] |
| Analysis 1.17  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 17 Voiding dysfunction. | ||||
| 18 De novo urgency or urgency incontinence (short term, ≤ 1 year) Show forest plot | 31 | 4923 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.82, 1.17] |
| Analysis 1.18  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 18 De novo urgency or urgency incontinence (short term, ≤ 1 year). | ||||
| 19 De novo urgency or urgency incontinence (medium term, 1 to 5 years) Show forest plot | 4 | 481 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.55, 1.73] |
| Analysis 1.19  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 19 De novo urgency or urgency incontinence (medium term, 1 to 5 years). | ||||
| 20 De novo urgency or urgency incontinence (long term, > 5 years) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.20  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 20 De novo urgency or urgency incontinence (long term, > 5 years). | ||||
| 21 Detrusor overactivity Show forest plot | 4 | 566 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.58, 1.73] |
| Analysis 1.21 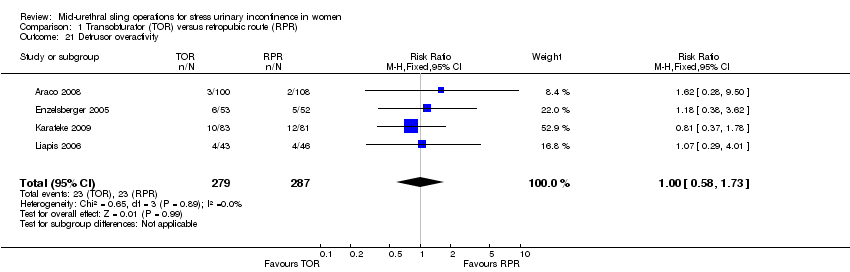 Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 21 Detrusor overactivity. | ||||
| 22 Vaginal tape erosion Show forest plot | 31 | 4743 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.78, 1.65] |
| Analysis 1.22  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 22 Vaginal tape erosion. | ||||
| 23 Bladder/urethral erosion Show forest plot | 4 | 374 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.01, 8.13] |
| Analysis 1.23  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 23 Bladder/urethral erosion. | ||||
| 24 Groin pain Show forest plot | 18 | 3221 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.12 [2.71, 6.27] |
| Analysis 1.24  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 24 Groin pain. | ||||
| 25 Suprapubic pain Show forest plot | 4 | 1105 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.11, 0.78] |
| Analysis 1.25  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 25 Suprapubic pain. | ||||
| 26 Repeat incontinence surgery (short term, ≤ 1 year) Show forest plot | 9 | 1402 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [0.85, 3.16] |
| Analysis 1.26  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 26 Repeat incontinence surgery (short term, ≤ 1 year). | ||||
| 27 Repeat incontinence surgery (medium term , 1 to 5 years) Show forest plot | 2 | 355 | Risk Ratio (M‐H, Fixed, 95% CI) | 21.89 [4.36, 109.77] |
| Analysis 1.27  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 27 Repeat incontinence surgery (medium term , 1 to 5 years). | ||||
| 28 Repeat incontinence surgery (long term > 5 years) Show forest plot | 4 | 695 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.79 [3.36, 23.00] |
| Analysis 1.28  Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 28 Repeat incontinence surgery (long term > 5 years). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Subjective cure (short term, ≤ 1 year) Show forest plot | 3 | 477 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [1.01, 1.19] |
| Analysis 2.1  Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 1 Subjective cure (short term, ≤ 1 year). | ||||
| 2 Objective cure (short term, ≤ 1 year) Show forest plot | 5 | 622 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.97, 1.17] |
| Analysis 2.2 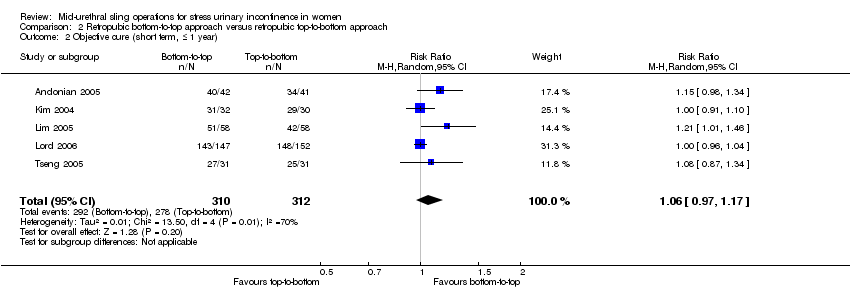 Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 2 Objective cure (short term, ≤ 1 year). | ||||
| 3 Operative time (minutes) Show forest plot | 2 | 124 | Mean Difference (IV, Fixed, 95% CI) | ‐2.15 [‐4.68, 0.38] |
| Analysis 2.3 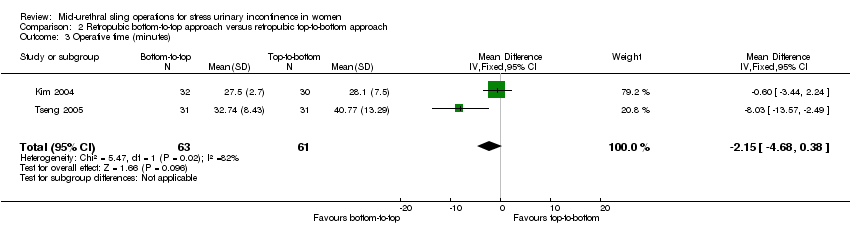 Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 3 Operative time (minutes). | ||||
| 4 Length of hospital stay (days) Show forest plot | 2 | 124 | Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.37, 0.30] |
| Analysis 2.4  Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 4 Length of hospital stay (days). | ||||
| 5 Perioperative complications Show forest plot | 4 | 507 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.53, 1.84] |
| Analysis 2.5  Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 5 Perioperative complications. | ||||
| 6 Bladder or urethral perforation Show forest plot | 5 | 631 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.31, 0.98] |
| Analysis 2.6  Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 6 Bladder or urethral perforation. | ||||
| 7 Voiding dysfunction Show forest plot | 5 | 631 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.18, 0.90] |
| Analysis 2.7  Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 7 Voiding dysfunction. | ||||
| 8 De novo urgency or urgency incontinence Show forest plot | 4 | 541 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.52, 1.34] |
| Analysis 2.8  Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 8 De novo urgency or urgency incontinence. | ||||
| 9 Detrusor overactivity Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.9  Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 9 Detrusor overactivity. | ||||
| 10 Vaginal tape erosion Show forest plot | 4 | 563 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.08, 0.95] |
| Analysis 2.10  Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 10 Vaginal tape erosion. | ||||
| 11 QoL specific Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.11  Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 11 QoL specific. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Subjective cure (short term, ≤ 1 year) Show forest plot | 6 | 759 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.96, 1.06] |
| Analysis 3.1  Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 1 Subjective cure (short term, ≤ 1 year). | ||||
| 2 Subjective cure and improvement (short term, ≤ 1 year) Show forest plot | 5 | 732 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.97, 1.08] |
| Analysis 3.2  Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 2 Subjective cure and improvement (short term, ≤ 1 year). | ||||
| 3 Subjective cure (medium term, 1 to 5 years) Show forest plot | 2 | 235 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.91, 1.23] |
| Analysis 3.3  Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 3 Subjective cure (medium term, 1 to 5 years). | ||||
| 4 Subjective cure and improvement (medium term, 1 to 5 years) Show forest plot | 2 | 399 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.90, 1.11] |
| Analysis 3.4  Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 4 Subjective cure and improvement (medium term, 1 to 5 years). | ||||
| 5 Objective cure (short term, ≤ 1 year) Show forest plot | 6 | 745 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.95, 1.04] |
| Analysis 3.5  Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 5 Objective cure (short term, ≤ 1 year). | ||||
| 6 Objective cure and improvement (short term, ≤ 1 year) Show forest plot | 2 | 214 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.95, 1.07] |
| Analysis 3.6  Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 6 Objective cure and improvement (short term, ≤ 1 year). | ||||
| 7 Operative time (minutes) Show forest plot | 4 | 481 | Mean Difference (IV, Random, 95% CI) | 0.52 [‐1.09, 2.13] |
| Analysis 3.7 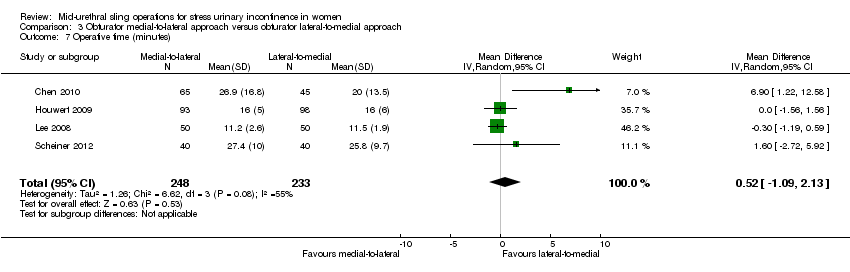 Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 7 Operative time (minutes). | ||||
| 8 Operative blood loss (ml) Show forest plot | 3 | 255 | Mean Difference (IV, Fixed, 95% CI) | 1.11 [‐6.01, 8.22] |
| Analysis 3.8  Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 8 Operative blood loss (ml). | ||||
| 9 Length of hospital stay (days) Show forest plot | 2 | 190 | Mean Difference (IV, Random, 95% CI) | ‐0.77 [‐2.54, 0.99] |
| Analysis 3.9  Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 9 Length of hospital stay (days). | ||||
| 10 Time to return to normal activity level Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.10  Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 10 Time to return to normal activity level. | ||||
| 11 Perioperative complications Show forest plot | 2 | 214 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.23, 7.51] |
| Analysis 3.11 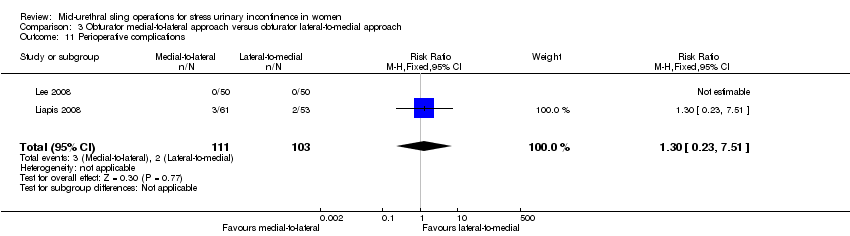 Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 11 Perioperative complications. | ||||
| 12 Major vascular or visceral injury Show forest plot | 4 | 622 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.23, 2.19] |
| Analysis 3.12 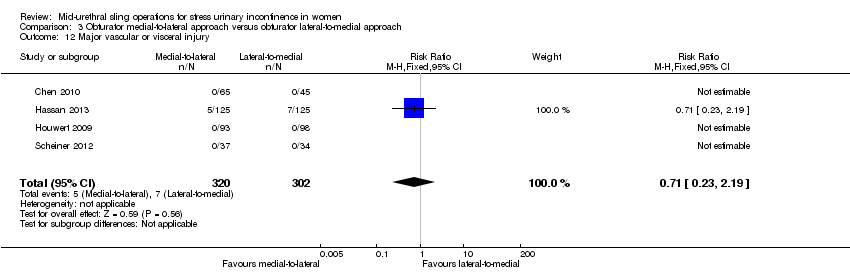 Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 12 Major vascular or visceral injury. | ||||
| 13 Vaginal perforation/injury Show forest plot | 3 | 541 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.12, 0.53] |
| Analysis 3.13 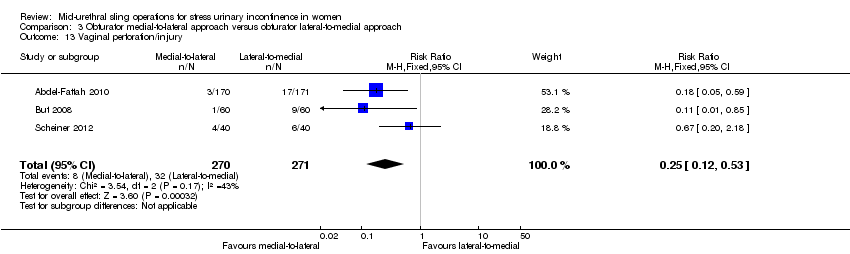 Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 13 Vaginal perforation/injury. | ||||
| 14 Bladder or urethral perforation Show forest plot | 6 | 794 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.07, 1.92] |
| Analysis 3.14 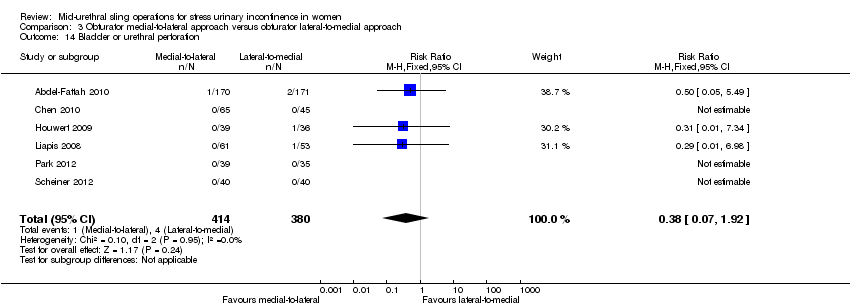 Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 14 Bladder or urethral perforation. | ||||
| 15 Voiding dysfunction Show forest plot | 8 | 1121 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.74 [1.06, 2.88] |
| Analysis 3.15 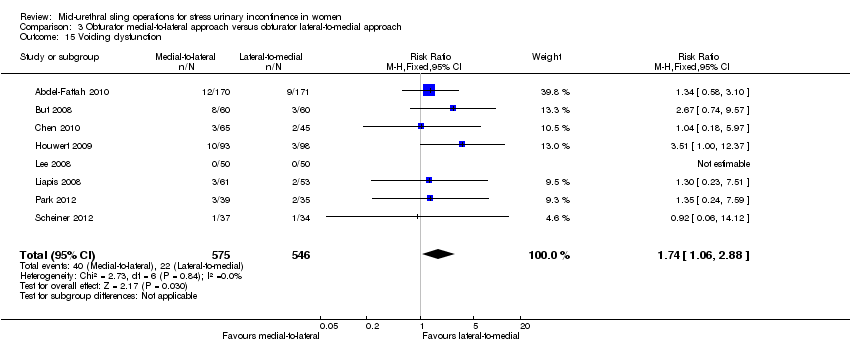 Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 15 Voiding dysfunction. | ||||
| 16 De novo urgency or urgency incontinence Show forest plot | 3 | 357 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.46, 2.20] |
| Analysis 3.16  Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 16 De novo urgency or urgency incontinence. | ||||
| 17 Detrusor overactivity Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.17  Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 17 Detrusor overactivity. | ||||
| 18 Vaginal tape erosion Show forest plot | 7 | 1087 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.16, 1.09] |
| Analysis 3.18  Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 18 Vaginal tape erosion. | ||||
| 19 Groin/thigh pain Show forest plot | 6 | 837 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.75, 1.76] |
| Analysis 3.19  Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 19 Groin/thigh pain. | ||||
| 20 Repeat incontinence surgery Show forest plot | 2 | 532 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.32, 1.30] |
| Analysis 3.20  Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 20 Repeat incontinence surgery. | ||||
| 21 QoL specific Show forest plot | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | 16.54 [4.84, 28.24] |
| Analysis 3.21  Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 21 QoL specific. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Subjective cure (short term, up to 1 year) Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.1  Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 1 Subjective cure (short term, up to 1 year). | ||||
| 1.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.90, 1.11] |
| 1.2 Modified TVT (suburethral pad) versus TVT | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.91, 1.10] |
| 1.3 Self‐tailored TVT‐O vs TVT‐O | 1 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.93, 1.11] |
| 1.4 Monarc®TOT open edge + tension suture vs TOT® | 1 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.87, 1.24] |
| 1.5 AdjustableTOT vs TOT® | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.87, 1.28] |
| 1.6 Synthetic vs biological | 2 | 169 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.86, 1.22] |
| 2 Subjective cure and improvement (short term, up to 1 year) Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.2  Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 2 Subjective cure and improvement (short term, up to 1 year). | ||||
| 2.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.97, 1.09] |
| 2.2 TOT + 2‐point tape fixation vs TOT | 1 | 418 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [1.00, 1.14] |
| 2.3 TVT versus modified TVT (suburethral pad) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.98, 1.08] |
| 3 Subjective cure (medium term, 1 to 5 years) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.3  Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 3 Subjective cure (medium term, 1 to 5 years). | ||||
| 3.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 153 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.86, 1.12] |
| 4 Objective cure (medium term, 1 to 5 years) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.4 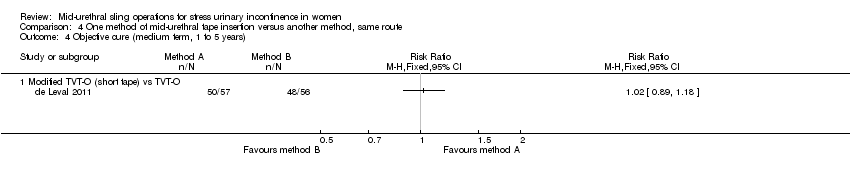 Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 4 Objective cure (medium term, 1 to 5 years). | ||||
| 4.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Objective cure (short term, ≤ 1 year) Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.5  Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 5 Objective cure (short term, ≤ 1 year). | ||||
| 5.1 Modified TVT‐O (less dissection) vs TVT‐O | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.91, 1.15] |
| 5.2 Synthetic vs biological | 2 | 136 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.94, 1.14] |
| 5.3 TVT‐O + IS vs TVT‐O | 1 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [1.02, 2.06] |
| 5.4 TOT + 2‐point tape fixation vs TOT | 1 | 418 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [1.01, 1.13] |
| 6 Operative time (minutes) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.6  Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 6 Operative time (minutes). | ||||
| 6.1 TVT‐O + IS vs TVT‐O | 1 | 96 | Mean Difference (IV, Fixed, 95% CI) | 12.0 [8.91, 15.09] |
| 6.2 Self‐tailored TVT‐O vs TVT‐O | 1 | 156 | Mean Difference (IV, Fixed, 95% CI) | ‐25.0 [‐26.73, ‐23.27] |
| 7 Operative blood loss (ml) Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.7 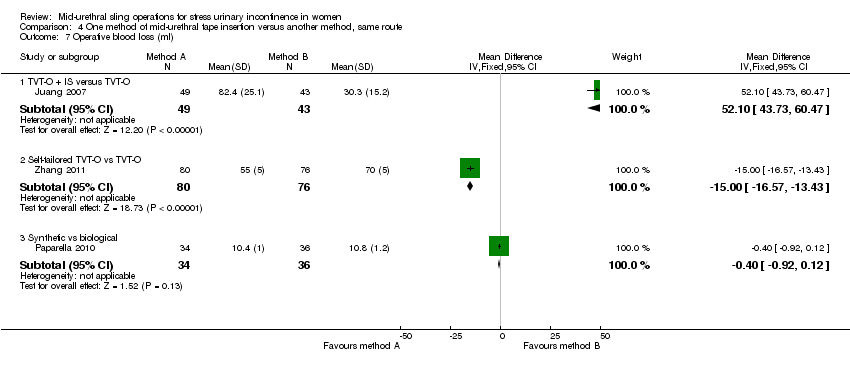 Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 7 Operative blood loss (ml). | ||||
| 7.1 TVT‐O + IS versus TVT‐O | 1 | 92 | Mean Difference (IV, Fixed, 95% CI) | 52.10 [43.73, 60.47] |
| 7.2 Self‐tailored TVT‐O vs TVT‐O | 1 | 156 | Mean Difference (IV, Fixed, 95% CI) | ‐13.00 [‐16.57, ‐13.43] |
| 7.3 Synthetic vs biological | 1 | 70 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐0.92, 0.12] |
| 8 Length of hospital stay (days) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.8 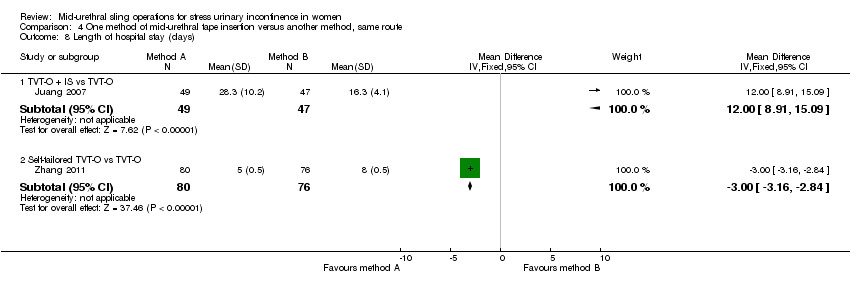 Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 8 Length of hospital stay (days). | ||||
| 8.1 TVT‐O + IS vs TVT‐O | 1 | 96 | Mean Difference (IV, Fixed, 95% CI) | 12.0 [8.91, 15.09] |
| 8.2 Self‐tailored TVT‐O vs TVT‐O | 1 | 156 | Mean Difference (IV, Fixed, 95% CI) | ‐3.0 [‐3.16, ‐2.84] |
| 9 Perioperative complications Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.9  Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 9 Perioperative complications. | ||||
| 9.1 Synthetic vs biological | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Major vascular or visceral injury Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.10  Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 10 Major vascular or visceral injury. | ||||
| 10.1 TVT‐O + IS vs TVT‐O | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.17, 3.04] |
| 10.2 Synthetic vs biological | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.3 AdjustableTOT vs TOT® | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Bladder/urethral perforation Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.11  Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 11 Bladder/urethral perforation. | ||||
| 11.1 TVT‐O + IS vs TVT‐O | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 TOT + 2‐point tape fixation vs TOT | 1 | 463 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.17, 3.33] |
| 11.3 TVT versus modified TVT (suburethral pad) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.05, 5.36] |
| 11.4 AdjustableTOT vs TOT® | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Voiding dysfunction Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.12  Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 12 Voiding dysfunction. | ||||
| 12.1 Modified TVT‐O (less dissection) vs TVT‐O | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.13, 30.61] |
| 12.2 TVT versus modified TVT (suburethral pad) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.21 [0.70, 7.00] |
| 12.3 Self‐tailored TVT‐O vs TVT‐O | 1 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.06, 14.92] |
| 12.4 Monarc®TOT open edge + tension suture vs TOT® | 1 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.04, 4.99] |
| 12.5 Synthetic vs biological | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.25, 101.58] |
| 13 De novo urgency or urgency incontinence Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.13  Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 13 De novo urgency or urgency incontinence. | ||||
| 13.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.51, 2.94] |
| 14 Vaginal tape erosion Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.14  Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 14 Vaginal tape erosion. | ||||
| 14.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.88] |
| 14.2 TVT versus modified TVT (suburethral pad) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.30 [0.61, 8.68] |
| 14.3 TVT‐O + IS vs TVT‐O | 1 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.06, 14.55] |
| 14.4 Monarc®TOT open edge + tension suture vs TOT® | 1 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.01, 2.53] |
| 14.5 Synthetic vs biological | 2 | 169 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 71.92] |
| 15 Bladder/urethral erosion Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.15  Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 15 Bladder/urethral erosion. | ||||
| 15.1 TVT versus modified TVT (suburethral pad) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.06, 15.56] |
| 16 Groin pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.16 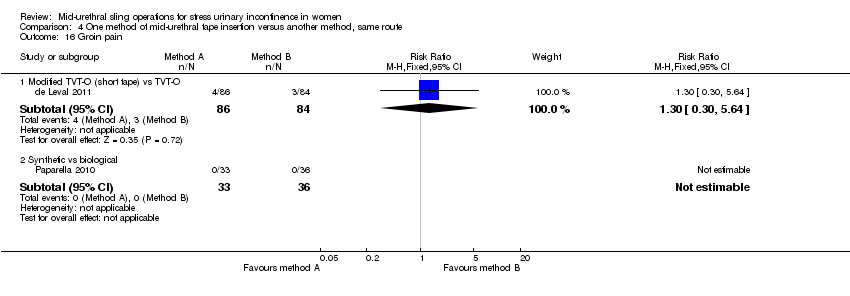 Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 16 Groin pain. | ||||
| 16.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.30, 5.64] |
| 16.2 Synthetic vs biological | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Subjective cure (short term, ≤ 1 year) Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.1 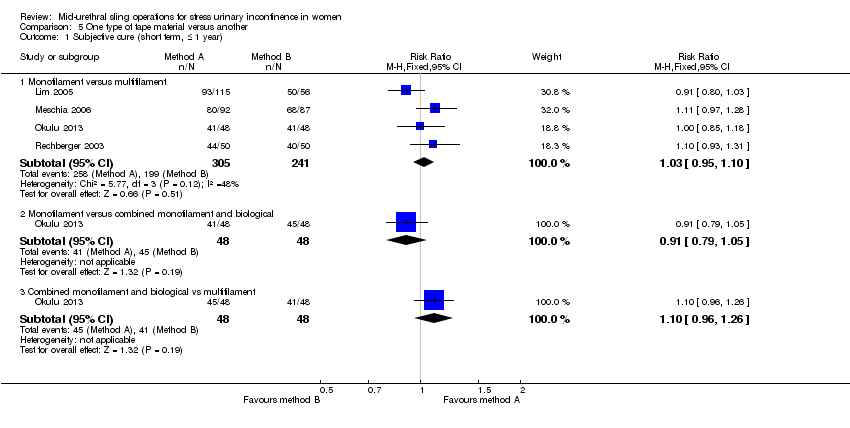 Comparison 5 One type of tape material versus another, Outcome 1 Subjective cure (short term, ≤ 1 year). | ||||
| 1.1 Monofilament versus multifilament | 4 | 546 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.95, 1.10] |
| 1.2 Monofilament versus combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.79, 1.05] |
| 1.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.96, 1.26] |
| 2 Subjective cure (medium term, 1 to 5 years) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.2  Comparison 5 One type of tape material versus another, Outcome 2 Subjective cure (medium term, 1 to 5 years). | ||||
| 2.1 Monofilament vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.85, 1.23] |
| 2.2 Monofilament vs combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.78, 1.06] |
| 2.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.96, 1.32] |
| 3 Objective cure (short term, ≤ 1 year) Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.3 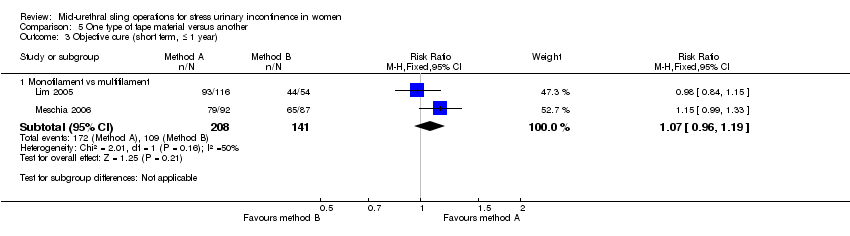 Comparison 5 One type of tape material versus another, Outcome 3 Objective cure (short term, ≤ 1 year). | ||||
| 3.1 Monofilament vs multifilament | 2 | 349 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.96, 1.19] |
| 4 Operative time (minutes) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.4  Comparison 5 One type of tape material versus another, Outcome 4 Operative time (minutes). | ||||
| 4.1 Monofilament vs multifilament | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Length of hospital stay (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.5 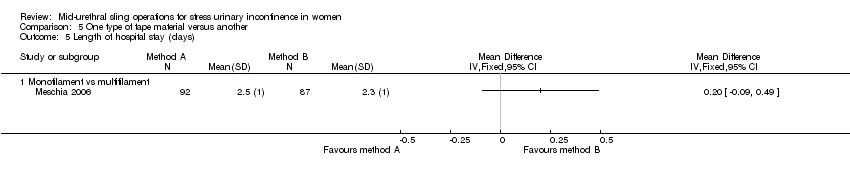 Comparison 5 One type of tape material versus another, Outcome 5 Length of hospital stay (days). | ||||
| 5.1 Monofilament vs multifilament | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Perioperative complications Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.6 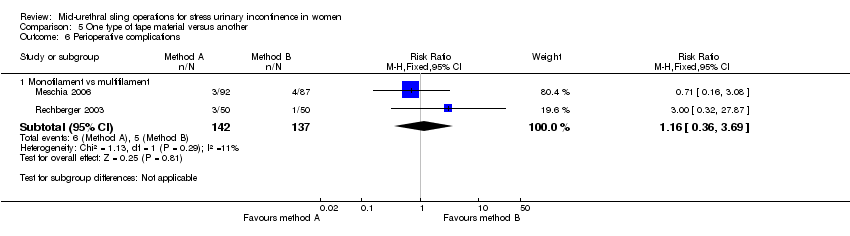 Comparison 5 One type of tape material versus another, Outcome 6 Perioperative complications. | ||||
| 6.1 Monofilament vs multifilament | 2 | 279 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.36, 3.69] |
| 7 Major vascular or visceral injury Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.7 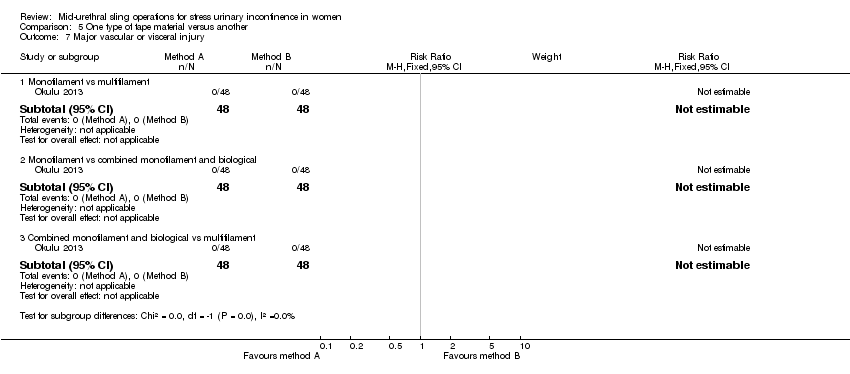 Comparison 5 One type of tape material versus another, Outcome 7 Major vascular or visceral injury. | ||||
| 7.1 Monofilament vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Monofilament vs combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Bladder or urethral perforation Show forest plot | 4 | 749 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.49, 2.70] |
| Analysis 5.8  Comparison 5 One type of tape material versus another, Outcome 8 Bladder or urethral perforation. | ||||
| 8.1 Monofilament vs multifilament | 4 | 557 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.49, 2.70] |
| 8.2 Monofilament vs combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Voiding dysfunction Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.9  Comparison 5 One type of tape material versus another, Outcome 9 Voiding dysfunction. | ||||
| 9.1 Monofilament vs multifilament | 3 | 461 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.10 [0.96, 4.59] |
| 10 De novo urgency or urgency incontinence Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.10  Comparison 5 One type of tape material versus another, Outcome 10 De novo urgency or urgency incontinence. | ||||
| 10.1 Monofilament vs multifilament | 4 | 545 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.68, 1.82] |
| 10.2 Monofilament vs combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.38, 10.41] |
| 10.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.4 [0.08, 1.96] |
| 11 Detrusor overactivity Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.11  Comparison 5 One type of tape material versus another, Outcome 11 Detrusor overactivity. | ||||
| 11.1 Monofilament vs multifilament | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Vaginal tape erosion Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 5.12  Comparison 5 One type of tape material versus another, Outcome 12 Vaginal tape erosion. | ||||
| 12.1 Monofilament vs multifilament | 3 | 445 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.09, 6.84] |
| 12.2 Monofilament vs combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 3.0 [0.32, 27.83] |
| 12.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.04, 3.09] |
| 13 QoL specific (ICIQ) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.13  Comparison 5 One type of tape material versus another, Outcome 13 QoL specific (ICIQ). | ||||
| 13.1 Monofilament vs multifilament | 1 | 96 | Mean Difference (IV, Fixed, 95% CI) | ‐0.60 [‐0.76, ‐0.44] |
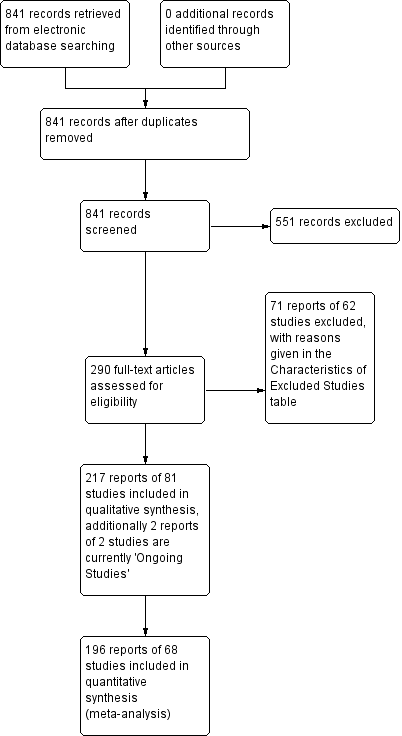
PRISMA study flow diagram

Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgments about each risk of bias item for each included study.

Funnel plot of comparison: 1 Transobturator (TOR) versus retropubic (RPR) route, outcome: 1.1 Subjective cure (short term, ≤ 1 year)
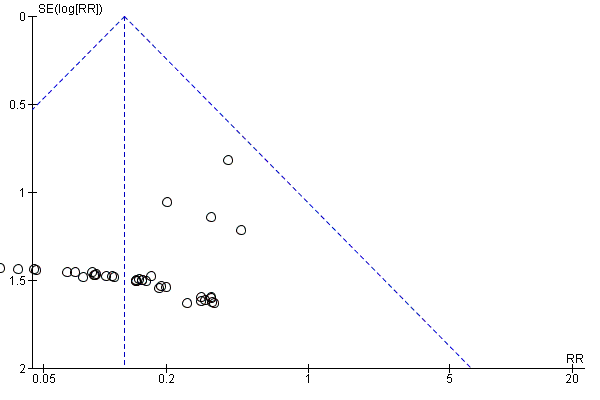
Funnel plot of comparison: 1 Transobturator (TOR) versus retropubic (RPR) route, outcome: 1.16 Bladder or urethral perforation
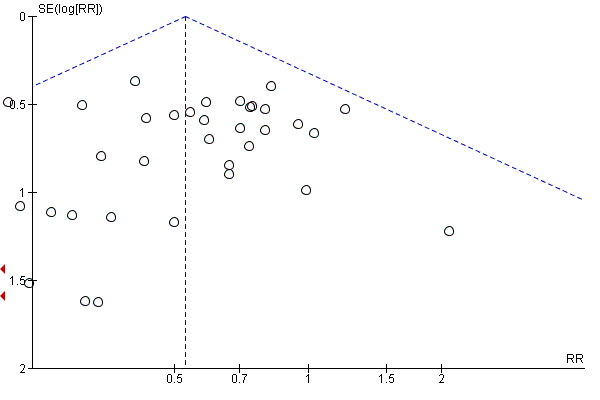
Funnel plot of comparison: 1 Transobturator (TOR) versus retropubic (RPR) route, outcome: 1.17 Voiding dysfunction

Funnel plot of comparison: 1 Transobturator (TOR) versus retropubic (RPR) route, outcome: 1.22 Vaginal tape erosion

Funnel plot of comparison: 1 Transobturator (TOR) versus retropubic (RPR) route, outcome: 1.24 Groin pain

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 1 Subjective cure (short term, ≤ 1 year).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 2 Subjective cure and improvement (short term, ≤ 1 year).
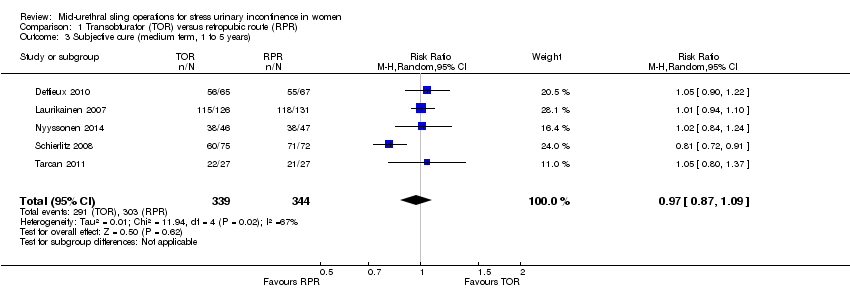
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 3 Subjective cure (medium term, 1 to 5 years).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 4 Subjective cure (long term, > 5 years).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 5 Subjective cure and improvement (long term, > 5 years).
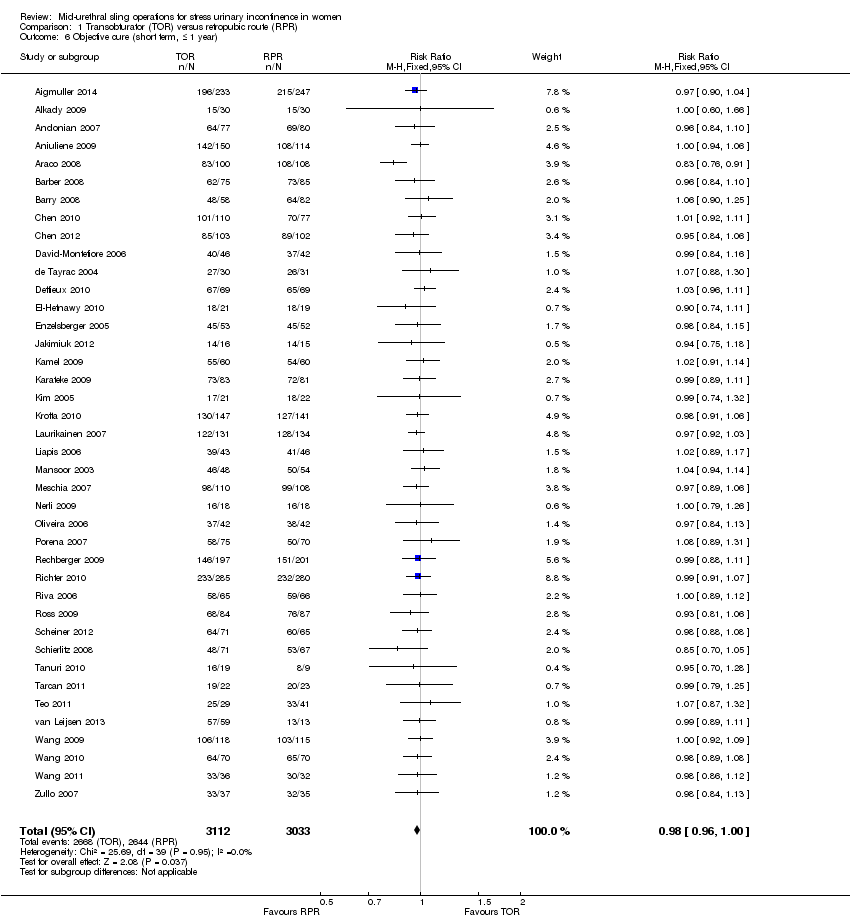
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 6 Objective cure (short term, ≤ 1 year).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 7 Objective cure and improvement (short term, ≤ 1 year).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 8 Objective cure (medium term, 1 to 5 years).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 9 Objective cure (long term, > 5 years).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 10 Operative time (minutes).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 11 Operative blood loss (ml).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 12 Length of hospital stay (days).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 13 Time to return to normal activity level (weeks).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 14 Perioperative complications.

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 15 Major vascular or visceral injury.

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 16 Bladder or urethral perforation.

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 17 Voiding dysfunction.

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 18 De novo urgency or urgency incontinence (short term, ≤ 1 year).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 19 De novo urgency or urgency incontinence (medium term, 1 to 5 years).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 20 De novo urgency or urgency incontinence (long term, > 5 years).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 21 Detrusor overactivity.

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 22 Vaginal tape erosion.

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 23 Bladder/urethral erosion.
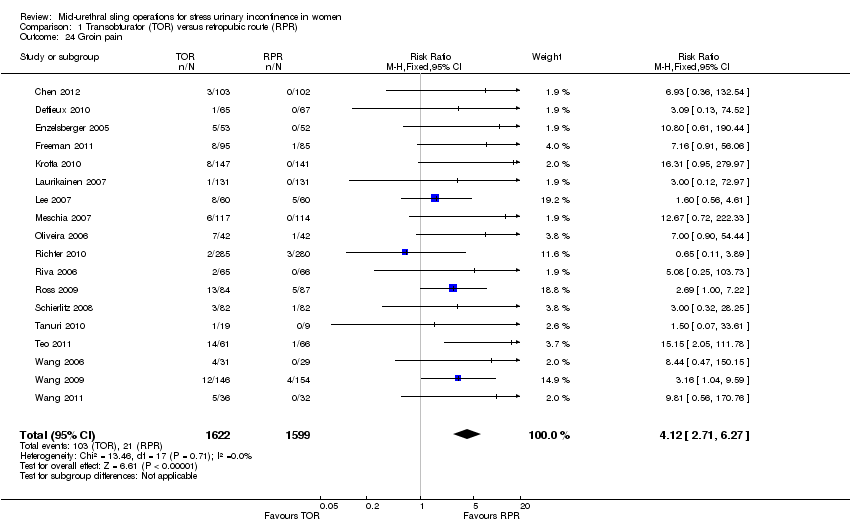
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 24 Groin pain.
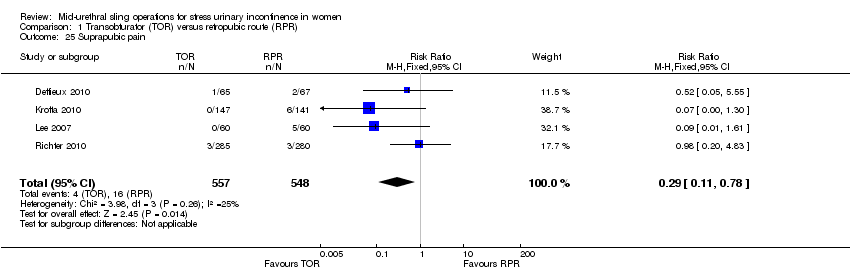
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 25 Suprapubic pain.

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 26 Repeat incontinence surgery (short term, ≤ 1 year).
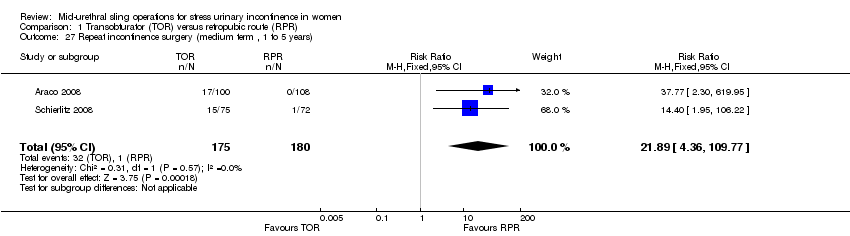
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 27 Repeat incontinence surgery (medium term , 1 to 5 years).
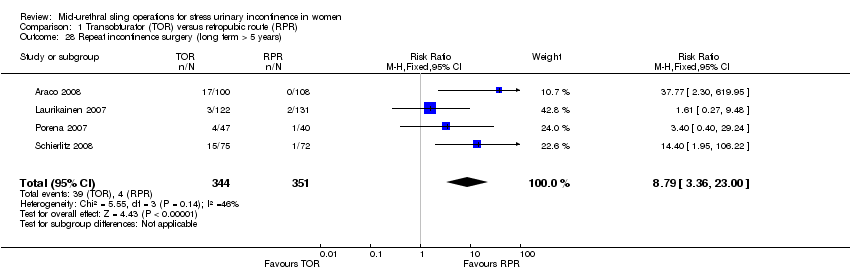
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 28 Repeat incontinence surgery (long term > 5 years).

Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 1 Subjective cure (short term, ≤ 1 year).

Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 2 Objective cure (short term, ≤ 1 year).

Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 3 Operative time (minutes).
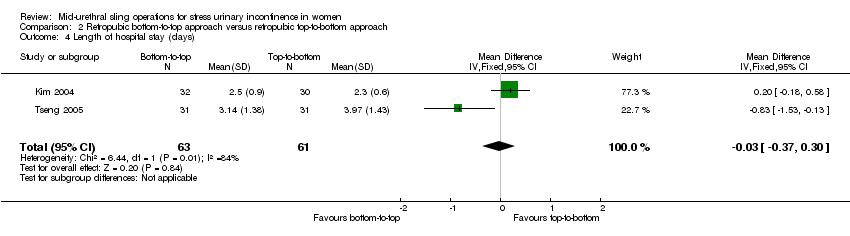
Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 4 Length of hospital stay (days).
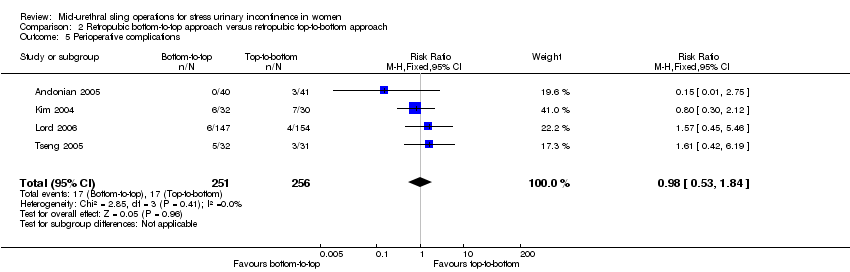
Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 5 Perioperative complications.

Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 6 Bladder or urethral perforation.

Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 7 Voiding dysfunction.

Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 8 De novo urgency or urgency incontinence.
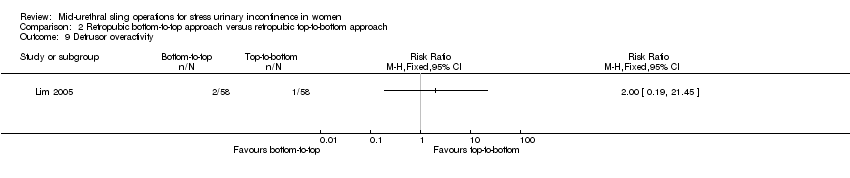
Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 9 Detrusor overactivity.

Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 10 Vaginal tape erosion.

Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 11 QoL specific.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 1 Subjective cure (short term, ≤ 1 year).

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 2 Subjective cure and improvement (short term, ≤ 1 year).
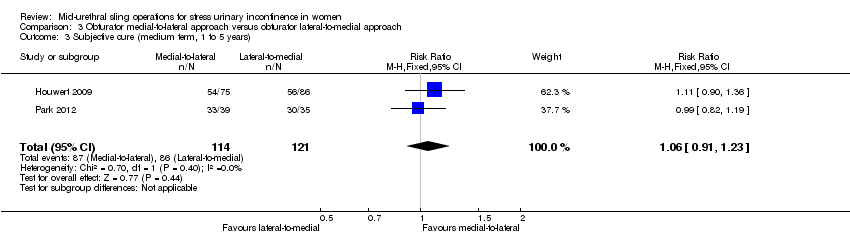
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 3 Subjective cure (medium term, 1 to 5 years).
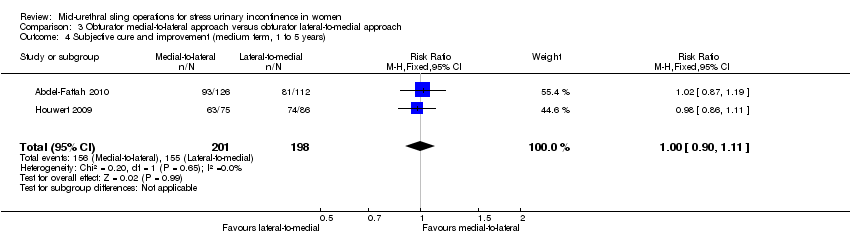
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 4 Subjective cure and improvement (medium term, 1 to 5 years).

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 5 Objective cure (short term, ≤ 1 year).

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 6 Objective cure and improvement (short term, ≤ 1 year).

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 7 Operative time (minutes).

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 8 Operative blood loss (ml).

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 9 Length of hospital stay (days).

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 10 Time to return to normal activity level.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 11 Perioperative complications.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 12 Major vascular or visceral injury.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 13 Vaginal perforation/injury.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 14 Bladder or urethral perforation.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 15 Voiding dysfunction.
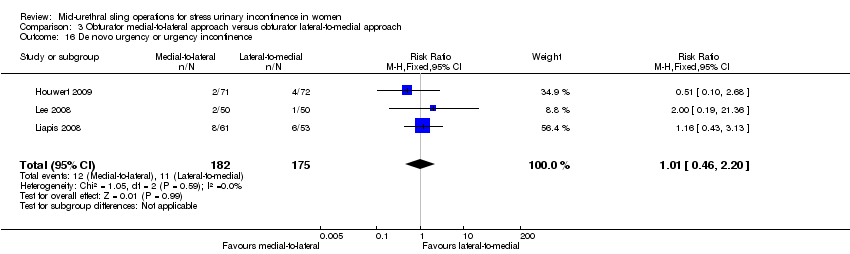
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 16 De novo urgency or urgency incontinence.
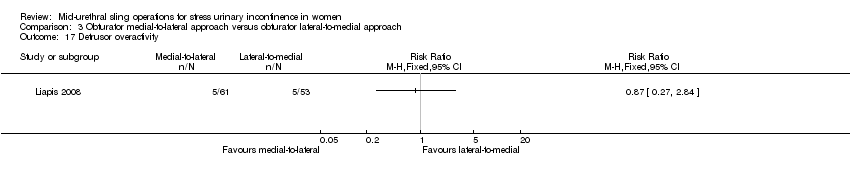
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 17 Detrusor overactivity.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 18 Vaginal tape erosion.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 19 Groin/thigh pain.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 20 Repeat incontinence surgery.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 21 QoL specific.

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 1 Subjective cure (short term, up to 1 year).

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 2 Subjective cure and improvement (short term, up to 1 year).
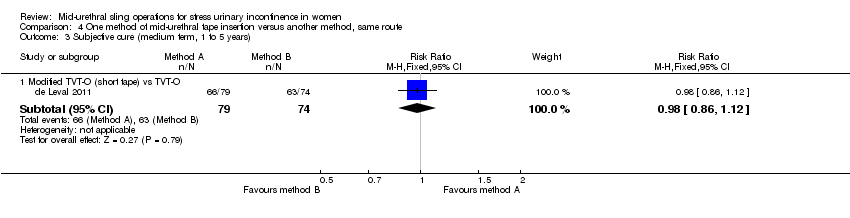
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 3 Subjective cure (medium term, 1 to 5 years).

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 4 Objective cure (medium term, 1 to 5 years).

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 5 Objective cure (short term, ≤ 1 year).
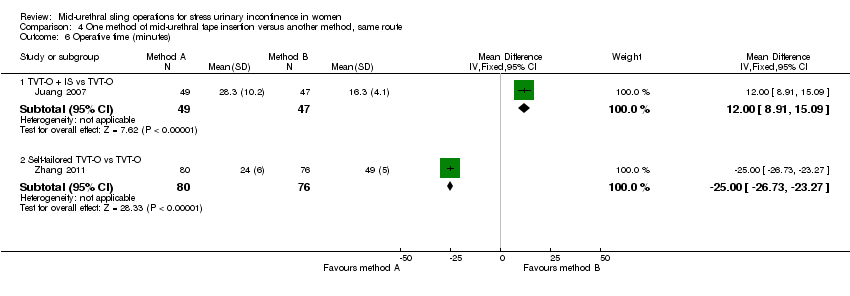
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 6 Operative time (minutes).

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 7 Operative blood loss (ml).
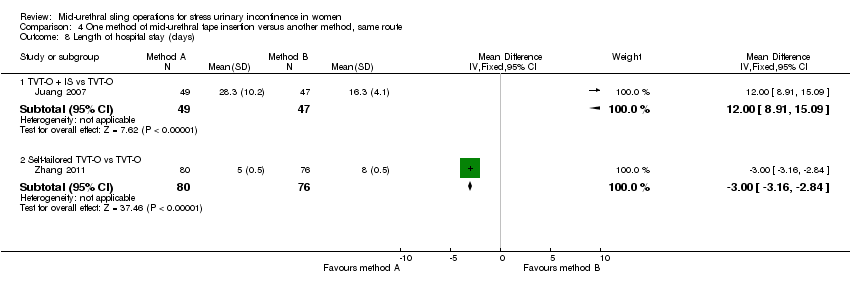
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 8 Length of hospital stay (days).

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 9 Perioperative complications.

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 10 Major vascular or visceral injury.

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 11 Bladder/urethral perforation.

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 12 Voiding dysfunction.

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 13 De novo urgency or urgency incontinence.
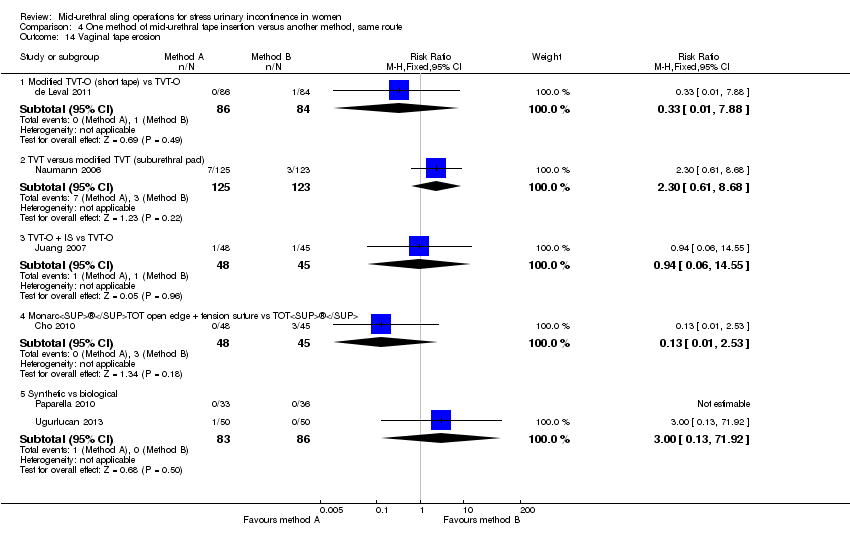
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 14 Vaginal tape erosion.

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 15 Bladder/urethral erosion.
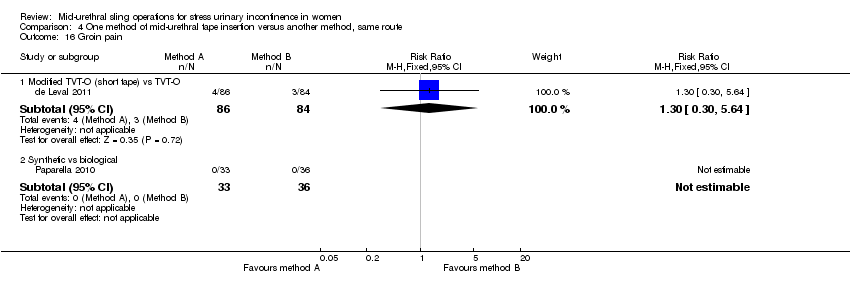
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 16 Groin pain.

Comparison 5 One type of tape material versus another, Outcome 1 Subjective cure (short term, ≤ 1 year).
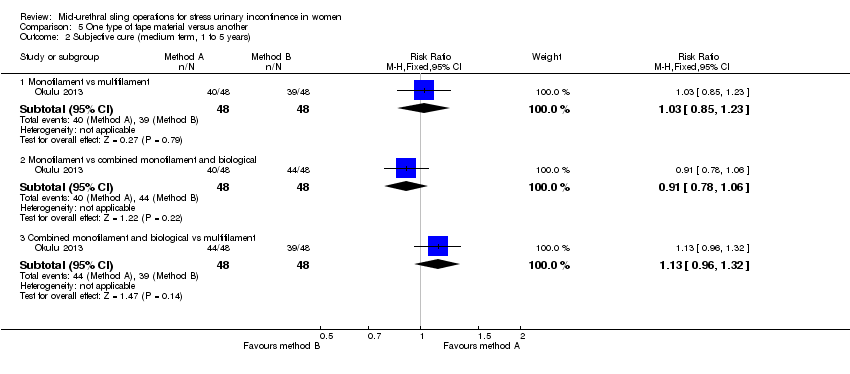
Comparison 5 One type of tape material versus another, Outcome 2 Subjective cure (medium term, 1 to 5 years).
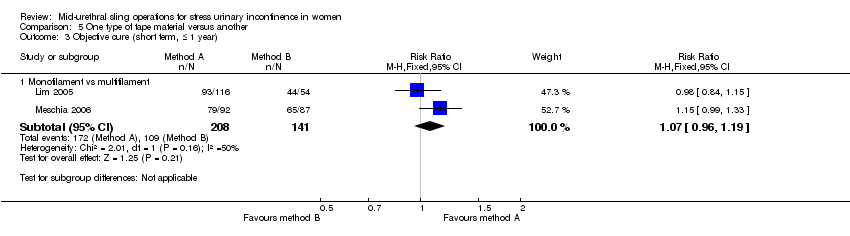
Comparison 5 One type of tape material versus another, Outcome 3 Objective cure (short term, ≤ 1 year).

Comparison 5 One type of tape material versus another, Outcome 4 Operative time (minutes).

Comparison 5 One type of tape material versus another, Outcome 5 Length of hospital stay (days).

Comparison 5 One type of tape material versus another, Outcome 6 Perioperative complications.

Comparison 5 One type of tape material versus another, Outcome 7 Major vascular or visceral injury.

Comparison 5 One type of tape material versus another, Outcome 8 Bladder or urethral perforation.
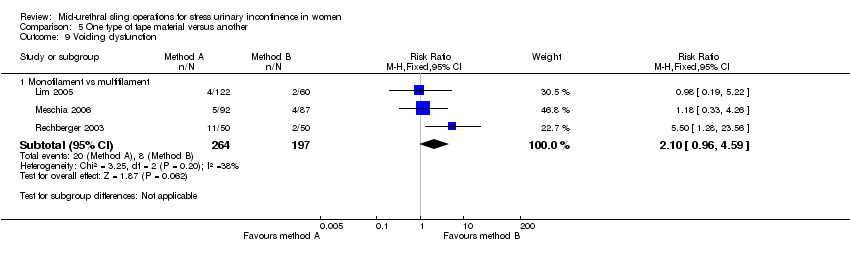
Comparison 5 One type of tape material versus another, Outcome 9 Voiding dysfunction.

Comparison 5 One type of tape material versus another, Outcome 10 De novo urgency or urgency incontinence.

Comparison 5 One type of tape material versus another, Outcome 11 Detrusor overactivity.
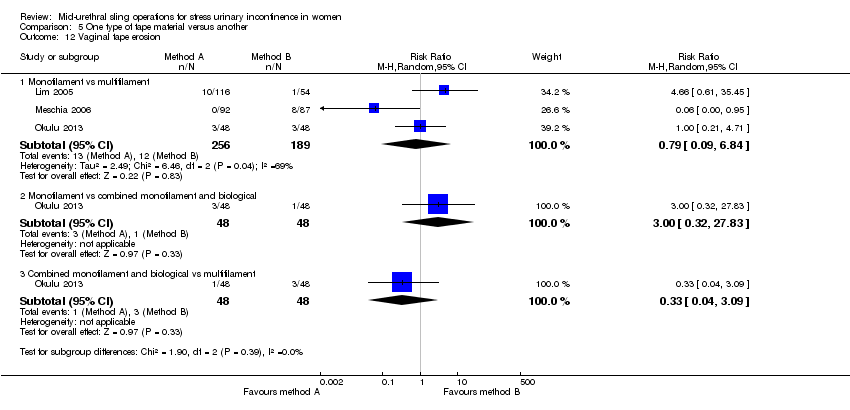
Comparison 5 One type of tape material versus another, Outcome 12 Vaginal tape erosion.

Comparison 5 One type of tape material versus another, Outcome 13 QoL specific (ICIQ).
| Transobturator (TOR) compared to retropubic (RPR) route for stress urinary incontinence in women | ||||||
| Patient or population: women with stress urinary incontinence | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Retropubic (RPR) route | Transobturator (TOR) | |||||
| Subjective cure (Short term < 1 year) | Study population | RR 0.98 | 5514 | ⊕⊕⊕⊝ | ||
| 844 per 1000 | 827 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 833 per 1000 | 816 per 1000 | |||||
| Subjective cure (medium term, 1 to 5 years) | Study population | RR 0.97 | 683 | ⊕⊕⊝⊝ | ||
| 881 per 1000 | 854 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 869 per 1000 | 843 per 1000 | |||||
| Subjective cure (long term, > 5 years) | Study population | RR 0.95 | 714 | ⊕⊕⊕⊝ | ||
| 707 per 1000 | 671 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 843 per 1000 | 801 per 1000 | |||||
| Bladder or urethral perforation | Study population | RR 0.13 | 6372 | ⊕⊕⊕⊝ | ||
| 49 per 1000 | 6 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 25 per 1000 | 3 per 1000 | |||||
| Voiding dysfunction (short and medium term, up to 5 years) | Study population | RR 0.53 | 6217 | ⊕⊕⊕⊝ | ||
| 72 per 1000 | 38 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 55 per 1000 | 29 per 1000 | |||||
| De novo urgency or urgency incontinence (short term, up to 12 months) | Study population | RR 0.98 | 4923 | ⊕⊕⊕⊝ | ||
| 82 per 1000 | 80 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 83 per 1000 | 81 per 1000 | |||||
| Groin pain | Study population | RR 4.62 | 3226 | ⊕⊕⊕⊝ | ||
| 14 per 1000 | 66 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 45 per 1000 | 208 per 1000 | |||||
| Suprapubic pain | Study population | RR 0.29 | 1105 | ⊕⊕⊕⊝ | ||
| 29 per 1000 | 8 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 18 per 1000 | 5 per 1000 | |||||
| Vaginal tape erosion (short and medium term, up to 5 years) | Study population | RR 1.13 | 4743 | ⊕⊕⊕⊝ | ||
| 20 per 1000 | 22 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 21 per 1000 | 24 per 1000 | |||||
| Repeat incontinence surgery (short term, within 12 months) | Study population | RR 1.64 | 1402 | ⊕⊕⊕⊝ | ||
| 19 per 1000 | 31 per 1000 | |||||
| mean control group across studies | ||||||
| 24 per 1000 | 39 per 1000 | |||||
| Repeat incontinence surgery (long term, > 5 years) | Study population | RR 8.79 | 695 | ⊕⊕⊝⊝ | ||
| 11 per 1000 | 100 per 1000 | |||||
| Mean control group across studies | ||||||
| 67 per 1000 | 589 per 1000 | |||||
| Cost effectiveness of intervention | An economic analysis was performed in only one RCT. This showed that over a 12‐month follow‐up period there was cost saving with TOR of CAD 1133 per patient (95% CI ‐2793 to 442), despite no difference in health outcome between the groups (adjusted to 2007 Canadian prices). The average cost of TOR was 17% less than that of RPR. | ‐ | (1 RCT) | |||
| Quality of life | 16 different validated questionnaires were used by different studies to assess QoL. This outcome was reported in 11 RCTs, but reported in different ways which precluded meta‐analysis. In all but one of the RCTs where QoL was assessed there was improvement in the QoL in women after the intervention, irrespective of which route was used, with no significant difference in scores between groups. Where assessment of sexual function was performed, there was an equal amount of improvement in sexual function following surgical treatment, irrespective of the route employed | ‐ | (11 RCTs) | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval RCT: randomised controlled trial RPR: retropubic route RR: risk ratio TOR: transobturator route | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Random sequence generation was unclear in 13 studies and at high risk of bias in 2 studies, and allocation concealment was unclear in 20 studies and at high risk in 2/37 studies 2Allocation concealment was unclear in 2/5 trials and sequence generation was unclear in 1/5 trials, so we decided to downgrade by 1 level 3There was potential substantial heterogeneity with an I² value of 67%, so we downgraded the quality rating by 1 level 4There was potential substantial heterogeneity among studies with an I² value of 65%, which lead us to downgrade by 1 level 5As allocation concealment was unclear in 18/40 trials and at high risk in 3/40, and sequence generation was unclear in 14/40 trials and at high risk in 3/40, we decided to downgrade by 1 level 6As allocation concealment was unclear in 16/37 trials and at high risk in 2/37, and sequence generation was unclear in 11/37 trials and at high risk in 2/37, we decided to downgrade by 1 level 7Random sequence generation was unclear in 10/31 studies and at high risk of bias in 2/31, and allocation concealment was unclear in 15/31 studies and at high risk in 2/31, so we downgraded by 1 level 8Random sequence generation was unclear in 4/18 studies and at high risk in 2/18, and allocation concealment was unclear in 9/18 studies and at high risk in 2/18, so we downgraded the quality of the evidence by 1 level 9Random sequence generation was at high risk in 1/4 studies, while allocation concealment was unclear in 2/4 and at high risk in 1/4, so we downgraded by 1 level 10Allocation concealment was unclear in 12/31 trials and at high risk in 1/31, while sequence generation was unclear in 6/31 trials and at high risk in 1/31, so we decided to downgrade by 1 level 11The wide confidence interval was judged to include a threshold for appreciable harm considered to be > 25% increase in RR, in this case there was much more than a 25% increase in RR for harm, so we downgraded the level by 1 12There was potential substantial heterogeneity with an I² value of 46%, so we downgraded the quality rating by 1 level 13Due to the low number of studies reporting data for this outcome, and the low number of events and wide CI around the estimate of the effect, we downgraded the quality of evidence by 1 level due to imprecision | ||||||
| Retropubic bottom‐to‐top approach compared to retropubic top‐to‐bottom approach for stress urinary incontinence in women | ||||||
| Patient or population: women with stress urinary incontinence | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| retropubic top‐to‐bottom approach | Retropubic bottom‐to‐top approach | |||||
| Subjective cure (short term, ≤ 1 year) | Study population | RR 1.10 | 492 | ⊕⊕⊕⊝ | ||
| 770 per 1000 | 847 per 1000 | |||||
| Mean control group across studies | ||||||
| 890 per 1000 | 979 per 1000 | |||||
| Subjective cure (medium term, 1 to 5 years) | No studies reported this outcome | ‐ | (0 studies) | |||
| Subjective cure long term: > 5 years | No studies reported this outcome | ‐ | (0 studies) | |||
| Bladder or urethral perforation | Study population | RR 0.55 | 631 | ⊕⊕⊕⊝ | ||
| 85 per 1000 | 47 per 1000 | |||||
| Mean control group across studies | ||||||
| 115 per 1000 | 63 per 1000 | |||||
| Voiding dysfunction | Study population | RR 0.40 | 631 | ⊕⊕⊕⊝ | ||
| 60 per 1000 | 24 per 1000 | |||||
| Mean control group across studies | ||||||
| 49 per 1000 | 20 per 1000 | |||||
| De novo urgency or urgency incontinence | Study population | RR 0.84 | 547 | ⊕⊕⊝⊝ | ||
| 123 per 1000 | 103 per 1000 | |||||
| Mean control group across studies | ||||||
| 187 per 1000 | 157 per 1000 | |||||
| Vaginal tape erosion | Study population | RR 0.27 | 569 | ⊕⊕⊕⊝ | ||
| 35 per 1000 | 9 per 1000 | |||||
| Mean control group across studies | ||||||
| 69 per 1000 | 19 per 1000 | |||||
| Repeat incontinence surgery short term | No studies reported this outcome | ‐ | (0 studies) | |||
| Repeat incontinence surgery long term | No studies reported this outcome | ‐ | (0 studies) | |||
| Cost effectiveness of intervention | No studies reported this outcome | ‐ | (0 studies) | |||
| Quality of life (IIQ scores) | The mean quality of life (IIQ scores) in the control group was 49.9 | The mean quality of life (IIQ scores) in the intervention group was 4.6 lower (14.17 lower to 4.97 higher) | ‐ | 84 | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). IIQ: Incontinence Impact questionnaire RCT: randomised controlled trial RR risk ratio; | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Sequence generation and allocation concealment was unclear in 2/3 trials, so we downgraded by 1 level 2Sequence generation and allocation concealment was unclear in 3/5 trials, so we downgraded by 1 level 3Sequence generation was unclear in 2/4 studies and allocation concealment unclear in 3/4 studies, so we downgraded by 1 level 4The wide confidence interval was judged to include a threshold for appreciable harm considered to be > 25% increase in RR, in this case there was much more than a 25% increase in RR for harm, so we downgraded the level by 1 5Sequence generation unclear in 3/4 studies and allocation concealment unclear in 2/4 studies, so we downgraded by 1 level | ||||||
| Obturator medial‐to‐lateral approach compared to obturator lateral‐to‐medial approach for stress urinary incontinence in women | ||||||
| Patient or population: women with stress urinary incontinence | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Obturator lateral‐to‐medial approach | Obturator medial‐to‐lateral approach | |||||
| Subjective cure (short term ≤ 1 year) | Study population | RR 1.00 | 759 | ⊕⊕⊝⊝ | ||
| 877 per 1000 | 877 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 880 per 1000 | 880 per 1000 | |||||
| Subjective cure (medium term, 1 to 5 years) | Study population | RR 1.06 | 235 | ⊕⊕⊝⊝ | ||
| 711 per 1000 | 753 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 736 per 1000 | 780 per 1000 | |||||
| Subjective cure | No studies reported this outcome | ‐ | (0 studies) | |||
| Bladder or urethral perforation | Study population | RR 0.38 | 794 | ⊕⊕⊕⊝ | ||
| 11 per 1000 | 4 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 6 per 1000 | 2 per 1000 | |||||
| Voiding dysfunction (short and medium term, up to 5 years) | Study population | RR 1.74 | 1121 | ⊕⊕⊕⊝ | ||
| 40 per 1000 | 70 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 55 per 1000 | 96 per 1000 | |||||
| De novo urgency or urgency incontinence (short term, up to 12 months) | Study population | RR 1.01 | 357 | ⊕⊕⊝⊝ | ||
| 63 per 1000 | 63 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 64 per 1000 | 65 per 1000 | |||||
| Groin pain | Study population | RR 1.15 | 837 | ⊕⊝⊝⊝ | ||
| 80 per 1000 | 92 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 74 per 1000 | 85 per 1000 | |||||
| Vaginal tape erosion (short and medium term, up to 5 years) | Study population | RR 0.42 | 1087 | ⊕⊝⊝⊝ | ||
| 24 per 1000 | 10 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 17 per 1000 | 7 per 1000 | |||||
| Repeat incontinence surgery (short term, up to 12 months) | Study population | RR 0.64 | 532 | ⊕⊕⊝⊝ | ||
| 71 per 1000 | 45 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 58 per 1000 | 37 per 1000 | |||||
| Repeat incontinence surgery | No studies reported this outcome | ‐ | (0 studies) | |||
| Cost effectiveness of intervention | No studies reported this outcome | ‐ | (0 studies) | |||
| Quality of life | The mean quality of life in the control group was 0 | The mean quality of life in the intervention group was 16.54 higher (4.84 higher to 28.24 higher) | ‐ | 46 | ⊕⊝⊝⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). RCT: randomised controlled trial RR: risk ratio; | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Random sequence generation was unclear in 4/6 studies, allocation concealment was unclear in5/6 and at high risk in 1/6 studies, so we downgraded the quality of evidence due to risk of bias by 2 levels 2Random sequence generation was unclear in all both studies, allocation concealment was unclear in 1 and high risk of bias in the other study, so we downgraded by 2 levels 3Sequence generation was unclear in 2 studies and allocation concealment was unclear in 3 studies, so we downgraded the quality rating by 1 level 4Sequence generation was unclear in 3 studies and at high risk in 1 study, while allocation concealment was unclear in 4 studies and at high risk in 1 study, so we downgraded by 1 level 5Sequence generation was unclear in 2/3 studies and at high risk in 1/3, allocation concealment was unclear in 2/3 studies and high in 1/3, so we downgraded by 2 levels 6Random sequence generation was unclear in 2/5 and high in 1/5 studies, while allocation concealment was unclear in 2/5 and high in 2/5 studies, so we downgraded the quality of evidence due to high risk of bias by 2 levels 7The wide confidence interval was judged to include a threshold for appreciable harm considered to be > 25% increase in RR, in this case there was > 65% increase in RR for harm, so we downgraded by 1 level 8Sequence generation was unclear in 3/7 studies and at high risk in 1/7. Allocation concealment was unclear in 5/7 studies and at high risk in 1/7. We downgraded the quality rating by 2 levels 9Sequence generation and allocation concealment were unclear in 1/2 studies, so we downgraded by 1 level 10Sequence generation and allocation concealment were unclear, so we downgraded by 1 level 11As there was only 1 study with very few events and CIs around estimates of effect included appreciable benefit and appreciable harm, we downgraded by 2 levels | ||||||
| Monofilament compared to multifilament tapes for stress urinary incontinence in women | ||||||
| Patient or population: women with stress urinary incontinence | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| multifilament tapes | Monofilament | |||||
| Subjective cure (short term ≤ 1 year) | Study population | RR 1.07 | 505 | ⊕⊕⊕⊝ | ||
| 784 per 1000 | 839 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 810 per 1000 | 867 per 1000 | |||||
| Subjective cure (medium term: 1 to 5 years) | No studies reported this outcome | ‐ | (0 studies) | |||
| Subjective cure (long term: > 5 years) | No studies reported this outcome | ‐ | (0 studies) | |||
| Bladder or urethral perforation | Study population | RR 0.76 | 496 | ⊕⊕⊕⊝ | ||
| 37 per 1000 | 28 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 32 per 1000 | 25 per 1000 | |||||
| Voiding dysfunction | Study population | RR 2.20 | 400 | ⊕⊕⊝⊝ | ||
| 41 per 1000 | 89 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 65 per 1000 | 143 per 1000 | |||||
| De novo urgency or urgency incontinence | Study population | RR 1.09 | 496 | ⊕⊕⊝⊝ | ||
| 102 per 1000 | 111 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 107 per 1000 | 117 per 1000 | |||||
| Vaginal tape erosion | Study population | RR 0.43 | 396 | ⊕⊕⊕⊕ | ||
| 62 per 1000 | 26 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 43 per 1000 | 18 per 1000 | |||||
| Repeat incontinence surgery (short term ≤ 1 year) | No studies reported this outcome | ‐ | (0 studies) | |||
| Repeat incontinence surgery (long term > 5 years) | No studies reported this outcome | ‐ | (0 studies) | |||
| Cost effectiveness of intervention | No studies reported this outcome | ‐ | (0 studies) | |||
| Quality of life scores ICIQ | The mean quality of life scores ICIQ in the control group was 2.1 | The mean quality of life scores ICIQ in the intervention group was 0.6 lower (0.76 lower to 0.44 lower) | ‐ | 96 | ⊕⊕⊕⊕ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ICIQ: International Consultation on Incontinence questionnaire RCT: randomised controlled trial RR: risk ratio | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Random sequence generation and allocation concealment unclear in 2/4 studies, so we downgraded by 1 level 2Random sequence generation and allocation concealment unclear in 2/3 studies, so downgraded by 1 level 3The wide confidence interval was judged to include a threshold for appreciable harm considered to be > 25% increase in RR, in this case there was much more than a 25% increase in RR for harm, so we downgraded by 1 level 4Sequence generation and allocation concealment were unclear in 2/4 studies, so we downgraded the quality rating by 1 level 5The wide confidence interval was judged to include a threshold for appreciable harm considered to be > 25% increase in RR, in this case there was > 65% increase in RR for harm, so we downgraded by 1 level | ||||||
| Study | Outcome data |
| Abdel‐Fattah 2010 | Group A: TVT‐O (n = 170) Group B: TOT (n = 171) Loss to follow up at 1yr: A: 18/170, B: 24/171 Loss to follow up at 3yrs: A: 44/170, B: 59/171 Objective cure: A: 114/121, B: 96/109 Subjective success: A: 121/149, B: 111/143 Bladder/urethral perforation: A: 1/170, B: 2/171 Voiding dysfunction: A: 12/170, B: 9/171 Tape erosion: A: 3/153, B: 5/149 Groin pain: A: 27/150, B: 19/147 Repeat continence surgery: A: 7/170, B: 15/171 QoL assessed via: King’s Health Questionnaire (KHQ) [10], Birmingham Bowel Urinary Symptom (BBUSQ‐22) [11] and Pelvic Organ Prolapse/Incontinence Sexual Function Questionnaire (PISQ‐12). In addition Patient Global Impression of Improvement (PGI‐I) [13] and International Consultation on Incontinence Questionnaire‐ Short form (ICIQ‐SF) [14] questionnaires. QOL scores were much improve following surgery with no significant inter group (A vs B) differences. Sexual dysfunction: PISQ‐12 employed. 199 patients completed this assessment and in most domains a significant improvement in postoperative PISQ‐12 scores was found with no significant difference demonstrated between the two groups. Intermediate (3 yr) Subjective success (very much & much improved) on PGI‐I: A: 93/126, B: 81/112 |
| Aigmuller 2014 | Group A: TVT: (n = 285; 38 of whom were lost to follow‐up) Group B: TVT‐O: (n = 269; 36 of whom were lost to follow‐up) Participants were evaluated at 3 months, with a further evaluation scheduled at 5 years
At 5‐year review:
|
| Alkady 2009 | Group A: TVT (n = 15) Group B: TVT‐O (n = 15)
|
| Andonian 2005 | Group A: SPARC Group B: TVT
|
| Andonian 2007 | Group A: Obtape (n = 78) Group B: DUPS (n = 32) ‐ suspended Group C: TVT (n = 80)
|
| Aniuliene 2009 | Group A: TVT‐O (n = 150) Group B: TVT (n = 114)
|
| Araco 2008 | Group A: TVT‐O (n = 120)
|
| Barber 2008 | Group A: TVT (n = 88) Group B: TOT (n = 82)
|
| Barry 2008 | Group A: TOT (n = 58)
|
| But 2008 | Group A: TVT‐O (n = 60) Group B: TOT (n = 60)
|
| Cervigni 2006 | Numbers in each group unreported. It was, thus, impossible to abstract results |
| Chen 2010 | Group A: TVT (n = 77) Group B: TOT (n = 45) Group C: TVT‐O (n = 65)
|
| Chen 2012 | A: TVT (n = 102) B: TVT‐O (n = 103)
|
| Cho 2010 | Group A: Monarc TOT (n = 48) Group B: TOT (n = 45)
|
| Choe 2013 | We were not able to use the data provided, as the number in each group was not specified |
| Darabi Mahboub 2012 | Group A: TOT (n = 40) Group B: TVT (n = 40) Operative time (minutes (SD): A: 64.50 (9.04), B: 64.00 (9.48) Mean hospital stay (days): A: 2.56 (0.51), B: 2.52 (0.47) |
| David‐Montefiore 2006 | Group A: RPR (n = 42) Group B: TOR (n = 46)
|
| de Leval 2011 | Group A: TVT‐O (n = 87) Group B: modified TVT‐O (n = 88)
At 3‐year follow‐up:
|
| de Tayrac 2004 | Group: A: TOT (n = 30) Group: B: TVT (n = 31)
|
| Deffieux 2010 | Group A: TVT (n = 75) Group B: TVT‐O (n = 74)
|
| Diab 2012 | Group A: TOT (n = 31) Group B: TVT (n = 32)
All the preoperative parameters were comparable in both groups. The mean operative time was significantly longer and bladder injury was significantly higher in the TVT group. There were no significant difference in cure rates, voiding dysfunction, de novo urgency and reoperation rate. The postoperative groin/thigh pain was higher in the TOT group. |
| El‐Hefnway 2010 | Preliminary results: Group A: TVT: (n = 19) Group B: TOT: (n = 21) At 24 months: Group A: TVT: (n = 45) Group B: TOT: (n = 42)
|
| Elbadry 2014 | Group A: adjustable TOT (n = 48) Group B: TOT: (n = 48)
|
| Enzelsberger 2005 | Group A: TOT (n = 56) Group B: TVT (n = 54)
|
| Freeman 2011 | Group A: Monarc TOT (n = 100) Group B: Gynaecare TVT (n = 92)
|
| Hammoud 2011 | Group A: TVT (n = 60) Group B: TVT‐O (n = 50) Subjective cure: A: 56/60, B: 48/50 |
| Hassan 2013 | Group A: inside‐out TOT (n = 125) Group B: outside‐in TOT (n = 125)
|
| Houwert 2009 | Group A: TVT‐O (n = 93) Group B: Monarc TOT (n = 98)
|
| Jakimiuk 2012 | Group A: TVT (n = 19) Group B: TVT‐O (n = 16)
|
| Juang 2007 | Group A: TVT‐O (n = 47) Group B: TVT‐O plus IS: (n = 49)
|
| Kamel 2009 | A: TVT (n = 60) B: TVT‐O (n = 60)
|
| Karateke 2009 | Group A: TVT (n = 83) Group B: TVT‐O (n = 84)
|
| Kilic 2007 | Group A: TVT (n = 10) Group B: TOT (n = 10)
|
| Kim 2004 | Group A: TVT (n = 32) Group B: SPARC (n = 30)
|
| Kim 2005 | Group A: Monarc (n = 65) Group B: SPARC (n = 65)
|
| Krofta 2010 | Group A: TVTTM (n = 149) Group B: TVT –OTM (n = 151)
|
| Laurikainen 2007 | Group A: TVT‐O (n = 131)
QoL: The scores of the condition specific quality of life questionnaires were significantly lower at the 3 and 5 year follow up compared with pre‐operative scores. This improvements were statistically significant, but with no difference between the groups. 84% of women with pre‐operative moderate and severe frequency and urgency symptoms were cured of these symptoms at the 5 year follow up. |
| Leanza 2009 | Group A: r‐TICT (n = 229; retropubic) Group B: t‐TICT (n = 220; transobturator) Subjective cure: A: 190/215, B: 178/208 |
| Lee 2007 | Group A: TVT (n = 60) Group B: TVT‐O (n = 60)
|
| Lee 2008 | Group A: TVT‐O (n = 50) Group B: TOT (n = 50)
|
| Liapis 2006 | Group A: TVT (n = 46) Group B: TVT‐O (n = 43)
|
| Liapis 2008 | Group A: TVT‐O (n = 61) Group B: Monarc TOT (n = 53)
|
| Lim 2005 | Group A: TVT (n = 61) Group B: IVS (n = 60) Group C: SPARC (n = 61)
|
| Lord 2006 | Group A: TVT (n = 147)
|
| Mansoor 2003 | Group A: TVT‐O (n = 48)
|
| Mehdiyev 2010 | A: TOT (n = 17) B: TVT (n = 15)
|
| Meschia 2006 | Group A: TVT (n = 92)
|
| Meschia 2007 | Group A: TVT‐O (n = 117) Group B: TVT (n = 114)
|
| Naumann 2006 | Group A: TVT (n = 123) Group B: LIFT (n = 125)
|
| Nerli 2009 | Group A: TVT (n = 18) Group B: TOT (n = 18)
|
| Nyyssonen 2014 | Group A: TOT (n = 50) Group B: TVT (n = 50)
|
| Okulu 2013 | Group A: Vypro mesh: (n = 48; multifilament) Group B: Ultrapro mesh: (n = 48; monofilament + biological combined mesh) Group C: Prolene light mesh: (n = 48; monofilament)
|
| Oliveira 2006 | Group A: TVT (n = 17)
|
| Palomba 2008 | Trial terminated. |
| Paparella 2010 | Group A: synthetic UretexTO® (n = 34) Group B: biological PelviLaceTO® (n‐36)
|
| Park 2012 | Group A: TVT‐O (n = 39) Group B: TOT Monarc (n = 35)
|
| Peattie 2006 | No published data. |
| Porena 2007 | Group A: TVT (n = 70) Group B: TOT (n = 75)
|
| Rechberger 2003 | Group A: TVT (n = 50) Group B: IVS (n = 50)
|
| Rechberger 2009 | Group A: retropubic (IVS‐02; n = 269) Group B: transobturator (IVS‐04; n = 268)
|
| Rechberger 2011 | Group A: TOT (n = 232) Group B: TOT with fixation (n = 231)
|
| Richter 2010 | Group A: retropubic sling (TVT; n = 298) Group B: transobturator tapes (TVT‐O, and TOT Monarc; n = 299) (Group C (?): TVT‐O (inside‐out) ‐ separate data not provided) (Group D (?): TOT (Monarch, outside‐in) ‐ separate data not provided) Objective cure at 1 year: A: 232/280 (80.8%), B: 233/285 (77.7%) Subjective cure at 1 year: A: 181/280 (62.2%), B: 163/285 (55.8%) Secondary outcomes:
PISQ‐12 (Prolapse / urinary incontinence sexual questionnaire): Analysis of results for group A and group B combined showed significant improvement in sexual function in both groups with a mean PISQ‐12 score increase from 32.8+/‐7.1 at baseline to 37.3+/‐ 6 at 24 months. These changes are >0.6 SD units, which reflects “medium” improvement in the PISQ‐12 score after surgery. Compared with women with successful surgery, women who experienced surgical failure, regardless of assigned type of surgery, reported worse adjusted sexual function scores at all postoperative time points. Improvement in PISQ‐12 scores was consistent with change in the 3 specific items from the sexual function measure of interest: (1) the experience of pain during sexual activity, (2) UI during sexual activity, and (3) fear of incontinence during sexual activities. Pain with intercourse was reported by 153 of 406 of sexually active women (38%) at baseline and decreased to 27% at 12 months after surgery (P.003). Self‐reported UI and the fear of incontinence occurring during sexual activity also significantly improved by 12 months after surgery, regardless of sling route. To specifically investigate the association of synthetic mesh slings on dyspareunia, we repeated the analysis on the 247 women who underwent MUS only (no concurrent procedures) and who completed baseline and 12‐month assessments. In this subset of women, dyspareunia decreased from 57% at baseline to 43% at 12 months after surgery (P .03). 5‐year data provided, but without numbers in each group, so could not be used for meta‐analysis |
| Riva 2006 | Group A: TOT (n = 65) Group B: TVT (n = 66) |
| Ross 2009 | Group A: TVT (n = 105) Group B: TOT (n = 94)
|
| Salem 2014 | Group A: TOT (n = 37) Group B: TVT (n = 39) No significant difference was noticed between the two groups as regard the mean operative time, perioperative complications, intraoperative blood loss, hospital stay, and time to return to normal activities. The mean of abdominal leak point pressure and urethral closure pressure showed marked and maintained improvement for 5 years later in group I whereas in group II, they showed marked and maintained improvement for only one year then shows significant decline in comparison with group I. As regard the mean of objective SEAPI score shows marked decrease (improvement) in both groups and this was maintained for the five years in group I but in group II, it increased after one year later. No usable data provided. |
| Scheiner 2012 | Group A: TVT (n = 80) Group B: TOT outside‐in approach (Monarc; n = 40) Group C: TVT‐O inside‐out approach (Gynecare; n = 40)
|
| Schierlitz 2008 | Group A: TVT (n = 81) Group B: Monarc sling (n = 82)
|
| Tanuri 2010 | Group A: Safyre VS retropubic tape (n = 10) Group B: Safyre T transobturator tape (n = 20)
|
| Tarcan 2011 | Group A: TVT (n = 27) Group B: TOT (n = 27) 12‐month follow‐up assessed:
2 year follow‐up assessed:
|
| Teo 2011 | Group A: TVT (n = 66) Group B: TVT‐O (n = 61)
|
| Tommaselli 2012 | Group A: TVT‐O (n = 48) Group B: modified TVT‐O (n = 24)
|
| Tseng 2005 | Group A: SPARC (n = 31)
|
| Ugurlucan 2013 | Group A: biological PELVILACE TO (n = 50) Group B: synthetic TOT ALIGN ®TO (n = 50)
|
| van Leijsen 2013 | Group A: RPR (n = 33) Group B: TOT (n = 90)
|
| Wang 2006 | Group A: Monarc (n = 31) Group B: SPARC (n = 29)
|
| Wang 2008 | Group A: TVT (n = 35) Group B: TVT‐O (n = 34)
|
| Wang 2009 | Group A: TVT (n = 154) Group B: TVT‐O (n = 146)
|
| Wang 2010 | Group A: TVT (n = 70) Group B: TOT (n = 70)
|
| Wang 2011 | Group A: TVT (n = 32) Group B: TVT‐O (n = 36)
|
| Zhang 2011 | Group A: TVT‐O (n = 76) Group B: modified TVT‐O (n = 80)
|
| Zullo 2007 | Group A: TVT (n = 35) Group B: TVT‐O (n = 37)
|
| Abbreviations BFLUTS: Bristol lower urinary tract symptoms questionnaires BMI: body‐mass index DO: detrusor overactivity DUP: distal urethral polypropylene sling EQOL‐5D: Euro Quality of life ‐5 Dimension hr: hour/s HRT: hormone replacement therapy ICIQ: International Consultation on Incontinence questionnaire ICIQ‐FLUTS: International Consultation on Incontinence questionnaire ‐ female lower urinary tract symptoms ICIQ‐ LUTSquol: International Consultation on Incontinence questionnaire ‐ lower urinary tract quality of life questionnaire ICIQ‐SF: International Consultation on Incontinence questionnaire short form ICIQ‐SF15: International Consultation on Incontinence questionnaire short form 15 IIQ: Incontinence Impact questionnaire ICS: International Continence Society I‐QoL: Incontinence Quality of Life questionnaire ISD: intrinsic sphincter deficiency IVS: intravaginal slingoplasty KHQ: King's Health questionnaireMUI: mixed urinary incontinence MUCP: Maximum urethral closure pressure MUI: mixed urinary incontinence OAB: overactive bladder PGI‐I: Patient Global Impression of Improvment PGI‐S: Patient Global Impression of Severity PISQ‐12: pelvic organ prolapse/urinary incontinence sexual questionnaire POP: pelvic organ prolapse POP‐Q: pelvic organ prolapse quantification POP‐Q ICS: pelvic organ prolapse quantification International Continence Society PVR: post void residual RCT: randomized controlled trial RPR: retropubic route QoL: quality of life QRCT: quasi‐randomised trial SEAPI‐QMM: Stress related leak, Empyting ability, Anatomy, Protection, Inhibition‐Quality of life, Mobility and Mental status incontinence classification system SD: standard deviation SIS: Single incision sling SPARC: suprapubic arc (procedure) SUI: stress urinary incontinence TOR: transobturator TOT: transobturator tape TOT‐ARIS: transobturator tape‐ARIS TVT: tension‐free vaginal tape TVT‐O: transobturator tension‐free vaginal tape UDI: Urinary Distress Impact questionnaire UDI‐6: Urinary Distress Impact questionnaire short form UDS: urodynamics study UI: urinary incontinence UISS: urinary incontinence severity score USI: urodynamic stress incontinence USS: ultrasound UTI: urinary tract infection UUI: urgency urinary incontinence VAS: visual analogue scale VLPP: Valsalval leak point pressure | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Subjective cure (short term, ≤ 1 year) Show forest plot | 36 | 5514 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.96, 1.00] |
| 2 Subjective cure and improvement (short term, ≤ 1 year) Show forest plot | 10 | 1651 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.96, 1.00] |
| 3 Subjective cure (medium term, 1 to 5 years) Show forest plot | 5 | 683 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.87, 1.09] |
| 4 Subjective cure (long term, > 5 years) Show forest plot | 4 | 714 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.80, 1.12] |
| 5 Subjective cure and improvement (long term, > 5 years) Show forest plot | 2 | 340 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.67, 1.28] |
| 6 Objective cure (short term, ≤ 1 year) Show forest plot | 40 | 6145 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.96, 1.00] |
| 7 Objective cure and improvement (short term, ≤ 1 year) Show forest plot | 10 | 1478 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.96, 1.01] |
| 8 Objective cure (medium term, 1 to 5 years) Show forest plot | 5 | 596 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.95, 1.06] |
| 9 Objective cure (long term, > 5 years) Show forest plot | 3 | 400 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.90, 1.06] |
| 10 Operative time (minutes) Show forest plot | 31 | 4713 | Mean Difference (IV, Random, 95% CI) | ‐7.54 [‐9.31, ‐5.77] |
| 11 Operative blood loss (ml) Show forest plot | 14 | 1869 | Mean Difference (IV, Random, 95% CI) | ‐6.49 [‐12.33, ‐0.65] |
| 12 Length of hospital stay (days) Show forest plot | 17 | 2170 | Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.59, 0.09] |
| 13 Time to return to normal activity level (weeks) Show forest plot | 4 | 626 | Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.15, 0.06] |
| 14 Perioperative complications Show forest plot | 15 | 2205 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.73, 1.14] |
| 15 Major vascular or visceral injury Show forest plot | 28 | 4676 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.19, 0.55] |
| 16 Bladder or urethral perforation Show forest plot | 40 | 6372 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.08, 0.20] |
| 17 Voiding dysfunction Show forest plot | 37 | 6200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.43, 0.65] |
| 18 De novo urgency or urgency incontinence (short term, ≤ 1 year) Show forest plot | 31 | 4923 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.82, 1.17] |
| 19 De novo urgency or urgency incontinence (medium term, 1 to 5 years) Show forest plot | 4 | 481 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.55, 1.73] |
| 20 De novo urgency or urgency incontinence (long term, > 5 years) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 21 Detrusor overactivity Show forest plot | 4 | 566 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.58, 1.73] |
| 22 Vaginal tape erosion Show forest plot | 31 | 4743 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.78, 1.65] |
| 23 Bladder/urethral erosion Show forest plot | 4 | 374 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.01, 8.13] |
| 24 Groin pain Show forest plot | 18 | 3221 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.12 [2.71, 6.27] |
| 25 Suprapubic pain Show forest plot | 4 | 1105 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.11, 0.78] |
| 26 Repeat incontinence surgery (short term, ≤ 1 year) Show forest plot | 9 | 1402 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [0.85, 3.16] |
| 27 Repeat incontinence surgery (medium term , 1 to 5 years) Show forest plot | 2 | 355 | Risk Ratio (M‐H, Fixed, 95% CI) | 21.89 [4.36, 109.77] |
| 28 Repeat incontinence surgery (long term > 5 years) Show forest plot | 4 | 695 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.79 [3.36, 23.00] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Subjective cure (short term, ≤ 1 year) Show forest plot | 3 | 477 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [1.01, 1.19] |
| 2 Objective cure (short term, ≤ 1 year) Show forest plot | 5 | 622 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.97, 1.17] |
| 3 Operative time (minutes) Show forest plot | 2 | 124 | Mean Difference (IV, Fixed, 95% CI) | ‐2.15 [‐4.68, 0.38] |
| 4 Length of hospital stay (days) Show forest plot | 2 | 124 | Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.37, 0.30] |
| 5 Perioperative complications Show forest plot | 4 | 507 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.53, 1.84] |
| 6 Bladder or urethral perforation Show forest plot | 5 | 631 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.31, 0.98] |
| 7 Voiding dysfunction Show forest plot | 5 | 631 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.18, 0.90] |
| 8 De novo urgency or urgency incontinence Show forest plot | 4 | 541 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.52, 1.34] |
| 9 Detrusor overactivity Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10 Vaginal tape erosion Show forest plot | 4 | 563 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.08, 0.95] |
| 11 QoL specific Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Subjective cure (short term, ≤ 1 year) Show forest plot | 6 | 759 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.96, 1.06] |
| 2 Subjective cure and improvement (short term, ≤ 1 year) Show forest plot | 5 | 732 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.97, 1.08] |
| 3 Subjective cure (medium term, 1 to 5 years) Show forest plot | 2 | 235 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.91, 1.23] |
| 4 Subjective cure and improvement (medium term, 1 to 5 years) Show forest plot | 2 | 399 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.90, 1.11] |
| 5 Objective cure (short term, ≤ 1 year) Show forest plot | 6 | 745 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.95, 1.04] |
| 6 Objective cure and improvement (short term, ≤ 1 year) Show forest plot | 2 | 214 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.95, 1.07] |
| 7 Operative time (minutes) Show forest plot | 4 | 481 | Mean Difference (IV, Random, 95% CI) | 0.52 [‐1.09, 2.13] |
| 8 Operative blood loss (ml) Show forest plot | 3 | 255 | Mean Difference (IV, Fixed, 95% CI) | 1.11 [‐6.01, 8.22] |
| 9 Length of hospital stay (days) Show forest plot | 2 | 190 | Mean Difference (IV, Random, 95% CI) | ‐0.77 [‐2.54, 0.99] |
| 10 Time to return to normal activity level Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11 Perioperative complications Show forest plot | 2 | 214 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.23, 7.51] |
| 12 Major vascular or visceral injury Show forest plot | 4 | 622 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.23, 2.19] |
| 13 Vaginal perforation/injury Show forest plot | 3 | 541 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.12, 0.53] |
| 14 Bladder or urethral perforation Show forest plot | 6 | 794 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.07, 1.92] |
| 15 Voiding dysfunction Show forest plot | 8 | 1121 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.74 [1.06, 2.88] |
| 16 De novo urgency or urgency incontinence Show forest plot | 3 | 357 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.46, 2.20] |
| 17 Detrusor overactivity Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 18 Vaginal tape erosion Show forest plot | 7 | 1087 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.16, 1.09] |
| 19 Groin/thigh pain Show forest plot | 6 | 837 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.75, 1.76] |
| 20 Repeat incontinence surgery Show forest plot | 2 | 532 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.32, 1.30] |
| 21 QoL specific Show forest plot | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | 16.54 [4.84, 28.24] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Subjective cure (short term, up to 1 year) Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.90, 1.11] |
| 1.2 Modified TVT (suburethral pad) versus TVT | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.91, 1.10] |
| 1.3 Self‐tailored TVT‐O vs TVT‐O | 1 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.93, 1.11] |
| 1.4 Monarc®TOT open edge + tension suture vs TOT® | 1 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.87, 1.24] |
| 1.5 AdjustableTOT vs TOT® | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.87, 1.28] |
| 1.6 Synthetic vs biological | 2 | 169 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.86, 1.22] |
| 2 Subjective cure and improvement (short term, up to 1 year) Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.97, 1.09] |
| 2.2 TOT + 2‐point tape fixation vs TOT | 1 | 418 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [1.00, 1.14] |
| 2.3 TVT versus modified TVT (suburethral pad) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.98, 1.08] |
| 3 Subjective cure (medium term, 1 to 5 years) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 153 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.86, 1.12] |
| 4 Objective cure (medium term, 1 to 5 years) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Objective cure (short term, ≤ 1 year) Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 Modified TVT‐O (less dissection) vs TVT‐O | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.91, 1.15] |
| 5.2 Synthetic vs biological | 2 | 136 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.94, 1.14] |
| 5.3 TVT‐O + IS vs TVT‐O | 1 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [1.02, 2.06] |
| 5.4 TOT + 2‐point tape fixation vs TOT | 1 | 418 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [1.01, 1.13] |
| 6 Operative time (minutes) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 TVT‐O + IS vs TVT‐O | 1 | 96 | Mean Difference (IV, Fixed, 95% CI) | 12.0 [8.91, 15.09] |
| 6.2 Self‐tailored TVT‐O vs TVT‐O | 1 | 156 | Mean Difference (IV, Fixed, 95% CI) | ‐25.0 [‐26.73, ‐23.27] |
| 7 Operative blood loss (ml) Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 TVT‐O + IS versus TVT‐O | 1 | 92 | Mean Difference (IV, Fixed, 95% CI) | 52.10 [43.73, 60.47] |
| 7.2 Self‐tailored TVT‐O vs TVT‐O | 1 | 156 | Mean Difference (IV, Fixed, 95% CI) | ‐13.00 [‐16.57, ‐13.43] |
| 7.3 Synthetic vs biological | 1 | 70 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐0.92, 0.12] |
| 8 Length of hospital stay (days) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 TVT‐O + IS vs TVT‐O | 1 | 96 | Mean Difference (IV, Fixed, 95% CI) | 12.0 [8.91, 15.09] |
| 8.2 Self‐tailored TVT‐O vs TVT‐O | 1 | 156 | Mean Difference (IV, Fixed, 95% CI) | ‐3.0 [‐3.16, ‐2.84] |
| 9 Perioperative complications Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 Synthetic vs biological | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Major vascular or visceral injury Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 TVT‐O + IS vs TVT‐O | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.17, 3.04] |
| 10.2 Synthetic vs biological | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.3 AdjustableTOT vs TOT® | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Bladder/urethral perforation Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 11.1 TVT‐O + IS vs TVT‐O | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 TOT + 2‐point tape fixation vs TOT | 1 | 463 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.17, 3.33] |
| 11.3 TVT versus modified TVT (suburethral pad) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.05, 5.36] |
| 11.4 AdjustableTOT vs TOT® | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Voiding dysfunction Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 12.1 Modified TVT‐O (less dissection) vs TVT‐O | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.13, 30.61] |
| 12.2 TVT versus modified TVT (suburethral pad) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.21 [0.70, 7.00] |
| 12.3 Self‐tailored TVT‐O vs TVT‐O | 1 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.06, 14.92] |
| 12.4 Monarc®TOT open edge + tension suture vs TOT® | 1 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.04, 4.99] |
| 12.5 Synthetic vs biological | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.25, 101.58] |
| 13 De novo urgency or urgency incontinence Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 13.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.51, 2.94] |
| 14 Vaginal tape erosion Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 14.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.88] |
| 14.2 TVT versus modified TVT (suburethral pad) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.30 [0.61, 8.68] |
| 14.3 TVT‐O + IS vs TVT‐O | 1 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.06, 14.55] |
| 14.4 Monarc®TOT open edge + tension suture vs TOT® | 1 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.01, 2.53] |
| 14.5 Synthetic vs biological | 2 | 169 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 71.92] |
| 15 Bladder/urethral erosion Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 15.1 TVT versus modified TVT (suburethral pad) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.06, 15.56] |
| 16 Groin pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 16.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.30, 5.64] |
| 16.2 Synthetic vs biological | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Subjective cure (short term, ≤ 1 year) Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Monofilament versus multifilament | 4 | 546 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.95, 1.10] |
| 1.2 Monofilament versus combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.79, 1.05] |
| 1.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.96, 1.26] |
| 2 Subjective cure (medium term, 1 to 5 years) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Monofilament vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.85, 1.23] |
| 2.2 Monofilament vs combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.78, 1.06] |
| 2.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.96, 1.32] |
| 3 Objective cure (short term, ≤ 1 year) Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Monofilament vs multifilament | 2 | 349 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.96, 1.19] |
| 4 Operative time (minutes) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Monofilament vs multifilament | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Length of hospital stay (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 Monofilament vs multifilament | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Perioperative complications Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Monofilament vs multifilament | 2 | 279 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.36, 3.69] |
| 7 Major vascular or visceral injury Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 Monofilament vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Monofilament vs combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Bladder or urethral perforation Show forest plot | 4 | 749 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.49, 2.70] |
| 8.1 Monofilament vs multifilament | 4 | 557 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.49, 2.70] |
| 8.2 Monofilament vs combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Voiding dysfunction Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 Monofilament vs multifilament | 3 | 461 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.10 [0.96, 4.59] |
| 10 De novo urgency or urgency incontinence Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 Monofilament vs multifilament | 4 | 545 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.68, 1.82] |
| 10.2 Monofilament vs combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.38, 10.41] |
| 10.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.4 [0.08, 1.96] |
| 11 Detrusor overactivity Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 11.1 Monofilament vs multifilament | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Vaginal tape erosion Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 12.1 Monofilament vs multifilament | 3 | 445 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.09, 6.84] |
| 12.2 Monofilament vs combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 3.0 [0.32, 27.83] |
| 12.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.04, 3.09] |
| 13 QoL specific (ICIQ) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 13.1 Monofilament vs multifilament | 1 | 96 | Mean Difference (IV, Fixed, 95% CI) | ‐0.60 [‐0.76, ‐0.44] |

