Liječenje stresne inkontinencije urina u žena pomoću postavljanja omče na srednji dio mokraćne cijevi
Abstract
Background
Urinary incontinence is a very common and debilitating problem affecting about 50% of women at some point in their lives. Stress urinary incontinence (SUI) is a contributory or predominant cause in 30% to 80% of these women. Mid‐urethral sling (MUS) operations are a recognised minimally invasive surgical treatment for SUI. MUS involves the passage of a small strip of tape through either the retropubic or obturator space, with entry or exit points at the lower abdomen or groin, respectively. This review does not include single incision slings.
Objectives
To assess the clinical effects of mid‐urethral sling (MUS) operations for the treatment of stress urinary incontinence (SUI), urodynamic stress incontinence (USI) or mixed urinary incontinence (MUI) in women.
Search methods
We searched the Cochrane Incontinence Group Specialised Register, which contains trials identified from CENTRAL, MEDLINE, MEDLINE in process, ClinicalTrials.gov and handsearching of journals and conference proceedings (searched 26 June 2014), Embase and Embase Classic (January 1947 to Week 25 2014), WHO ICTRP (searched on 30 June 2014) and the reference lists of relevant articles.
Selection criteria
Randomised or quasi‐randomised controlled trials amongst women with SUI, USI or MUI, in which both trial arms involve a MUS operation.
Data collection and analysis
Two review authors independently assessed the methodological quality of potentially eligible studies and extracted data from the included trials.
Main results
We included 81 trials that evaluated 12,113 women. We assessed the quality of evidence for outcomes using the GRADE assessment tool; the quality of most outcomes was moderate, mainly due to risk of bias or imprecision.
Fifty‐five trials with data contributed by 8652 women compared the use of the transobturator route (TOR) and retropubic route (RPR). There is moderate quality evidence that in the short term (up to one year) the rate of subjective cure of TOR and RPR are similar (RR 0.98, 95% CI 0.96 to 1.00; 36 trials, 5514 women; moderate quality evidence) ranging from 62% to 98% in the TOR group, and from 71% to 97% in the RPR group. Short‐term objective cure was similar in the TOR and RPR groups (RR 0.98, 95% CI 0.96 to 1.00; 40 trials, 6145 women). Fewer trials reported medium‐term (one to five years) and longer‐term (over five years) data, but subjective cure was similar between the groups (RR 0.97, 95% CI 0.87 to 1.09; 5 trials, 683 women; low quality evidence; and RR 0.95, 95% CI 0.80 to 1.12; 4 trials, 714 women; moderate quality evidence, respectively). In the long term, subjective cure rates ranged from 43% to 92% in the TOR group, and from 51% to 88% in the RPR group.
MUS procedures performed using the RPR had higher morbidity when compared to TOR, though the overall rate of adverse events remained low. The rate of bladder perforation was lower after TOR (0.6% versus 4.5%; RR 0.13, 95% CI 0.08 to 0.20; 40 trials, 6372 women; moderate quality evidence). Major vascular/visceral injury, mean operating time, operative blood loss and length of hospital stay were lower with TOR.
Postoperative voiding dysfunction was less frequent following TOR (RR 0.53, 95% CI 0.43 to 0.65; 37 trials, 6200 women; moderate quality evidence). Overall rates of groin pain were higher in the TOR group (6.4% versus 1.3%; RR 4.12, 95% CI 2.71 to 6.27; 18 trials, 3221 women; moderate quality evidence) whereas suprapubic pain was lower in the TOR group (0.8% versus 2.9%; RR 0.29, 95% CI 0.11 to 0.78); both being of short duration. The overall rate of vaginal tape erosion/exposure/extrusion was low in both groups: 24/1000 instances with TOR compared with 21/1000 for RPR (RR 1.13, 95% CI 0.78 to 1.65; 31 trials, 4743 women; moderate quality evidence). There were only limited data to inform the need for repeat incontinence surgery in the long term, but it was more likely in the TOR group than in the RPR group (RR 8.79, 95% CI 3.36 to 23.00; 4 trials, 695 women; low quality evidence).
A retropubic bottom‐to‐top route was more effective than top‐to‐bottom route for subjective cure (RR 1.10, 95% CI 1.01 to 1.19; 3 trials, 477 women; moderate quality evidence). It incurred significantly less voiding dysfunction, and led to fewer bladder perforations and vaginal tape erosions.
Short‐and medium‐term subjective cure rates between transobturator tapes passed using a medial‐to‐lateral as opposed to a lateral‐to‐medial approach were similar (RR 1.00, 95% CI 0.96 to 1.06; 6 trials, 759 women; moderate quality evidence, and RR 1.06, 95% CI 0.91 to 1.23; 2 trials, 235 women; moderate quality evidence). There was moderate quality evidence that voiding dysfunction was more frequent in the medial‐to‐lateral group (RR 1.74, 95% CI 1.06 to 2.88; 8 trials, 1121 women; moderate quality evidence), but vaginal perforation was less frequent in the medial‐to‐lateral route (RR 0.25, 95% CI 0.12 to 0.53; 3 trials, 541 women). Due to the very low quality of the evidence, it is unclear whether the lower rates of vaginal epithelial perforation affected vaginal tape erosion (RR 0.42, 95% CI 0.16 to 1.09; 7 trials, 1087 women; very low quality evidence).
Authors' conclusions
Mid‐urethral sling operations have been the most extensively researched surgical treatment for stress urinary incontinence (SUI) in women and have a good safety profile. Irrespective of the routes traversed, they are highly effective in the short and medium term, and accruing evidence demonstrates their effectiveness in the long term. This review illustrates their positive impact on improving the quality of life of women with SUI. With the exception of groin pain, fewer adverse events occur with employment of a transobturator approach. When comparing transobturator techniques of a medial‐to‐lateral versus a lateral‐to‐medial insertion, there is no evidence to support the use of one approach over the other. However, a bottom‐to‐top route was more effective than top‐to‐bottom route for retropubic tapes.
A salient point illustrated throughout this review is the need for reporting of longer‐term outcome data from the numerous existing trials. This would substantially increase the evidence base and provide clarification regarding uncertainties about long‐term effectiveness and adverse event profile.
PICO
Laički sažetak
Liječenje stresne inkontinencije mokraće u žena pomoću postavljanja omče na srednji dio mokraćne cijevi
Dosadašnje spoznaje
Stresna inkontinencija mokraće (neželjeno curenje mokraće pri naporu i naprezanju, kihanju, kašlju ili smijehu) je najčešći oblik inkontinencije u žena i utječe na kvalitetu života. Uz te tegobe mogu se javiti i poteškoće sa spolnim odnosima, uslijed istjecanja mokraće. Svaka treća žena starija od 18 godina može doživjeti stresnu inkontinenciju mokraće tijekom života.
Kirurški zahvati za liječenje ove poteškoće su postali jednostavniji, ali postoje mnogi različiti pristupi. Najčešće se primjenjuje postavljanje omče na srednji dio mokraćne cijevi. Primjenjuje se u žena koje se po prvi put kirurški liječe od ove poteškoće, ali i u onih u kojih su prethodni zahvati bili neuspješni. Kod ovog zahvata se postavlja traka ispod mokraćne cijevi kojom istječe mokraća iz mjehura. Pri kašlju postavljena traka steže mokraćnu cijev i sprječava istjecanje mokraće.
Dva su pristupa kirurškog zahvata, umetanje trake iza stidne kosti kroz trbušnu stijenku (tzv. retropubični pristup) ili kroz prepone (tzv. transopturatorni pristup).
Istraživačko pitanje
Pregledali smo rezultate istraživanja ova dva pristupa postavljanja omče na srednji dio mokraćne cijevi. Također su ispitani rezultati postavljanja omče i vrste materijala od kojih je izrađena omča. Svrha ovog Cochrane sustavnog pregleda je ispitivanje učinkovitosti operacije u liječenju stresne inkontinencije mokraće i ustanovljavanje komplikacija koje proizlaze.
Glavni rezultati ovog Cochrane sustavnog pregleda
Pregledali smo medicinsku literaturu objavljenu do lipnja 2014. godine. Nađeno je 81 istraživanje koje je ukupno uključilo 12.113 žena. Ta istraživanja su pokazala da je više od 80% žena sa stresnom inkontinencijom mokraće izliječeno ili je stanje značajno poboljšano nezavisno od kirurškog pristupa, u trajanju do 5 godina nakon zahvata. To je bilo nezavisno od vrste omče koja je primijenjena i pristupa. Studije su koristile različite upitnike o kvaliteti života te se ovi rezultati nisu mogli objediniti. Unatoč toga je nađeno da je operacija dovela do poboljšanja i da nema razlike između pristupa kirurškog zahvata. Samo je u nekoliko istraživanja nađen podatak o učinkovitosti 5 godina nakon operacije, Dokazi koji su trenutno dostupni pokazuju da postoji pozitivan učinak ispitivane intervencije.
Nuspojave
Postavljanje trake iza stidne kosti je bilo povezano s većim rizikom ozljede mjehura i nemogućnost potpunog pražnjenja mjehura nakon zahvata. Kod ovog pristupa je bilo manje bolova u preponama u razdoblju kratko nakon operacije. Postoji određeni dokaz da ovaj pristup ima niži rizik za ponavljanim operacijama u dugoročnom praćenju u usporedbi s pristupom kroz prepone. Dokaz srednje kvalitete se odnosi na nizak rizik komplikacija postavljanja omče, primjerice u 2% slučajeva je omča probila stijenku rodnice. Poteškoće pri spolnom odnosu, uključujući bol su bile male, a istjecanje mokraće pri spolnom odnosu je smanjeno nakon operacije.
Ograničenja sustavnog pregleda
Većina rezultata se temelji na dokazima umjerene kvalitete. U većine istraživanja korištene metode nisu dovoljno jasno opisane, te su uzrokom određene nesigurnosti. Za sada postoji ograničeni broj randomiziranih kliničkih istraživanja (koja omogućuju pouzdane rezultate) u kojima je ishod praćen 5 godina nakon zahvata. Dokaz učinkovitosti i uspješnosti operacije je pouzdaniji za razdoblje neposredno nakon operacije u odnosu na dulji period. Potrebno je prikazati rezultate dugoročnog praćenje ishoda ovog zahvata.
Authors' conclusions
Summary of findings
| Transobturator (TOR) compared to retropubic (RPR) route for stress urinary incontinence in women | ||||||
| Patient or population: women with stress urinary incontinence | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Retropubic (RPR) route | Transobturator (TOR) | |||||
| Subjective cure (Short term < 1 year) | Study population | RR 0.98 | 5514 | ⊕⊕⊕⊝ | ||
| 844 per 1000 | 827 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 833 per 1000 | 816 per 1000 | |||||
| Subjective cure (medium term, 1 to 5 years) | Study population | RR 0.97 | 683 | ⊕⊕⊝⊝ | ||
| 881 per 1000 | 854 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 869 per 1000 | 843 per 1000 | |||||
| Subjective cure (long term, > 5 years) | Study population | RR 0.95 | 714 | ⊕⊕⊕⊝ | ||
| 707 per 1000 | 671 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 843 per 1000 | 801 per 1000 | |||||
| Bladder or urethral perforation | Study population | RR 0.13 | 6372 | ⊕⊕⊕⊝ | ||
| 49 per 1000 | 6 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 25 per 1000 | 3 per 1000 | |||||
| Voiding dysfunction (short and medium term, up to 5 years) | Study population | RR 0.53 | 6217 | ⊕⊕⊕⊝ | ||
| 72 per 1000 | 38 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 55 per 1000 | 29 per 1000 | |||||
| De novo urgency or urgency incontinence (short term, up to 12 months) | Study population | RR 0.98 | 4923 | ⊕⊕⊕⊝ | ||
| 82 per 1000 | 80 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 83 per 1000 | 81 per 1000 | |||||
| Groin pain | Study population | RR 4.62 | 3226 | ⊕⊕⊕⊝ | ||
| 14 per 1000 | 66 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 45 per 1000 | 208 per 1000 | |||||
| Suprapubic pain | Study population | RR 0.29 | 1105 | ⊕⊕⊕⊝ | ||
| 29 per 1000 | 8 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 18 per 1000 | 5 per 1000 | |||||
| Vaginal tape erosion (short and medium term, up to 5 years) | Study population | RR 1.13 | 4743 | ⊕⊕⊕⊝ | ||
| 20 per 1000 | 22 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 21 per 1000 | 24 per 1000 | |||||
| Repeat incontinence surgery (short term, within 12 months) | Study population | RR 1.64 | 1402 | ⊕⊕⊕⊝ | ||
| 19 per 1000 | 31 per 1000 | |||||
| mean control group across studies | ||||||
| 24 per 1000 | 39 per 1000 | |||||
| Repeat incontinence surgery (long term, > 5 years) | Study population | RR 8.79 | 695 | ⊕⊕⊝⊝ | ||
| 11 per 1000 | 100 per 1000 | |||||
| Mean control group across studies | ||||||
| 67 per 1000 | 589 per 1000 | |||||
| Cost effectiveness of intervention | An economic analysis was performed in only one RCT. This showed that over a 12‐month follow‐up period there was cost saving with TOR of CAD 1133 per patient (95% CI ‐2793 to 442), despite no difference in health outcome between the groups (adjusted to 2007 Canadian prices). The average cost of TOR was 17% less than that of RPR. | ‐ | (1 RCT) | |||
| Quality of life | 16 different validated questionnaires were used by different studies to assess QoL. This outcome was reported in 11 RCTs, but reported in different ways which precluded meta‐analysis. In all but one of the RCTs where QoL was assessed there was improvement in the QoL in women after the intervention, irrespective of which route was used, with no significant difference in scores between groups. Where assessment of sexual function was performed, there was an equal amount of improvement in sexual function following surgical treatment, irrespective of the route employed | ‐ | (11 RCTs) | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval RCT: randomised controlled trial RPR: retropubic route RR: risk ratio TOR: transobturator route | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Random sequence generation was unclear in 13 studies and at high risk of bias in 2 studies, and allocation concealment was unclear in 20 studies and at high risk in 2/37 studies 2Allocation concealment was unclear in 2/5 trials and sequence generation was unclear in 1/5 trials, so we decided to downgrade by 1 level 3There was potential substantial heterogeneity with an I² value of 67%, so we downgraded the quality rating by 1 level 4There was potential substantial heterogeneity among studies with an I² value of 65%, which lead us to downgrade by 1 level 5As allocation concealment was unclear in 18/40 trials and at high risk in 3/40, and sequence generation was unclear in 14/40 trials and at high risk in 3/40, we decided to downgrade by 1 level 6As allocation concealment was unclear in 16/37 trials and at high risk in 2/37, and sequence generation was unclear in 11/37 trials and at high risk in 2/37, we decided to downgrade by 1 level 7Random sequence generation was unclear in 10/31 studies and at high risk of bias in 2/31, and allocation concealment was unclear in 15/31 studies and at high risk in 2/31, so we downgraded by 1 level 8Random sequence generation was unclear in 4/18 studies and at high risk in 2/18, and allocation concealment was unclear in 9/18 studies and at high risk in 2/18, so we downgraded the quality of the evidence by 1 level 9Random sequence generation was at high risk in 1/4 studies, while allocation concealment was unclear in 2/4 and at high risk in 1/4, so we downgraded by 1 level 10Allocation concealment was unclear in 12/31 trials and at high risk in 1/31, while sequence generation was unclear in 6/31 trials and at high risk in 1/31, so we decided to downgrade by 1 level 11The wide confidence interval was judged to include a threshold for appreciable harm considered to be > 25% increase in RR, in this case there was much more than a 25% increase in RR for harm, so we downgraded the level by 1 12There was potential substantial heterogeneity with an I² value of 46%, so we downgraded the quality rating by 1 level 13Due to the low number of studies reporting data for this outcome, and the low number of events and wide CI around the estimate of the effect, we downgraded the quality of evidence by 1 level due to imprecision | ||||||
| Retropubic bottom‐to‐top approach compared to retropubic top‐to‐bottom approach for stress urinary incontinence in women | ||||||
| Patient or population: women with stress urinary incontinence | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| retropubic top‐to‐bottom approach | Retropubic bottom‐to‐top approach | |||||
| Subjective cure (short term, ≤ 1 year) | Study population | RR 1.10 | 492 | ⊕⊕⊕⊝ | ||
| 770 per 1000 | 847 per 1000 | |||||
| Mean control group across studies | ||||||
| 890 per 1000 | 979 per 1000 | |||||
| Subjective cure (medium term, 1 to 5 years) | No studies reported this outcome | ‐ | (0 studies) | |||
| Subjective cure long term: > 5 years | No studies reported this outcome | ‐ | (0 studies) | |||
| Bladder or urethral perforation | Study population | RR 0.55 | 631 | ⊕⊕⊕⊝ | ||
| 85 per 1000 | 47 per 1000 | |||||
| Mean control group across studies | ||||||
| 115 per 1000 | 63 per 1000 | |||||
| Voiding dysfunction | Study population | RR 0.40 | 631 | ⊕⊕⊕⊝ | ||
| 60 per 1000 | 24 per 1000 | |||||
| Mean control group across studies | ||||||
| 49 per 1000 | 20 per 1000 | |||||
| De novo urgency or urgency incontinence | Study population | RR 0.84 | 547 | ⊕⊕⊝⊝ | ||
| 123 per 1000 | 103 per 1000 | |||||
| Mean control group across studies | ||||||
| 187 per 1000 | 157 per 1000 | |||||
| Vaginal tape erosion | Study population | RR 0.27 | 569 | ⊕⊕⊕⊝ | ||
| 35 per 1000 | 9 per 1000 | |||||
| Mean control group across studies | ||||||
| 69 per 1000 | 19 per 1000 | |||||
| Repeat incontinence surgery short term | No studies reported this outcome | ‐ | (0 studies) | |||
| Repeat incontinence surgery long term | No studies reported this outcome | ‐ | (0 studies) | |||
| Cost effectiveness of intervention | No studies reported this outcome | ‐ | (0 studies) | |||
| Quality of life (IIQ scores) | The mean quality of life (IIQ scores) in the control group was 49.9 | The mean quality of life (IIQ scores) in the intervention group was 4.6 lower (14.17 lower to 4.97 higher) | ‐ | 84 | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). IIQ: Incontinence Impact questionnaire RCT: randomised controlled trial RR risk ratio; | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Sequence generation and allocation concealment was unclear in 2/3 trials, so we downgraded by 1 level 2Sequence generation and allocation concealment was unclear in 3/5 trials, so we downgraded by 1 level 3Sequence generation was unclear in 2/4 studies and allocation concealment unclear in 3/4 studies, so we downgraded by 1 level 4The wide confidence interval was judged to include a threshold for appreciable harm considered to be > 25% increase in RR, in this case there was much more than a 25% increase in RR for harm, so we downgraded the level by 1 5Sequence generation unclear in 3/4 studies and allocation concealment unclear in 2/4 studies, so we downgraded by 1 level | ||||||
| Obturator medial‐to‐lateral approach compared to obturator lateral‐to‐medial approach for stress urinary incontinence in women | ||||||
| Patient or population: women with stress urinary incontinence | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Obturator lateral‐to‐medial approach | Obturator medial‐to‐lateral approach | |||||
| Subjective cure (short term ≤ 1 year) | Study population | RR 1.00 | 759 | ⊕⊕⊝⊝ | ||
| 877 per 1000 | 877 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 880 per 1000 | 880 per 1000 | |||||
| Subjective cure (medium term, 1 to 5 years) | Study population | RR 1.06 | 235 | ⊕⊕⊝⊝ | ||
| 711 per 1000 | 753 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 736 per 1000 | 780 per 1000 | |||||
| Subjective cure | No studies reported this outcome | ‐ | (0 studies) | |||
| Bladder or urethral perforation | Study population | RR 0.38 | 794 | ⊕⊕⊕⊝ | ||
| 11 per 1000 | 4 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 6 per 1000 | 2 per 1000 | |||||
| Voiding dysfunction (short and medium term, up to 5 years) | Study population | RR 1.74 | 1121 | ⊕⊕⊕⊝ | ||
| 40 per 1000 | 70 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 55 per 1000 | 96 per 1000 | |||||
| De novo urgency or urgency incontinence (short term, up to 12 months) | Study population | RR 1.01 | 357 | ⊕⊕⊝⊝ | ||
| 63 per 1000 | 63 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 64 per 1000 | 65 per 1000 | |||||
| Groin pain | Study population | RR 1.15 | 837 | ⊕⊝⊝⊝ | ||
| 80 per 1000 | 92 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 74 per 1000 | 85 per 1000 | |||||
| Vaginal tape erosion (short and medium term, up to 5 years) | Study population | RR 0.42 | 1087 | ⊕⊝⊝⊝ | ||
| 24 per 1000 | 10 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 17 per 1000 | 7 per 1000 | |||||
| Repeat incontinence surgery (short term, up to 12 months) | Study population | RR 0.64 | 532 | ⊕⊕⊝⊝ | ||
| 71 per 1000 | 45 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 58 per 1000 | 37 per 1000 | |||||
| Repeat incontinence surgery | No studies reported this outcome | ‐ | (0 studies) | |||
| Cost effectiveness of intervention | No studies reported this outcome | ‐ | (0 studies) | |||
| Quality of life | The mean quality of life in the control group was 0 | The mean quality of life in the intervention group was 16.54 higher (4.84 higher to 28.24 higher) | ‐ | 46 | ⊕⊝⊝⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). RCT: randomised controlled trial RR: risk ratio; | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Random sequence generation was unclear in 4/6 studies, allocation concealment was unclear in5/6 and at high risk in 1/6 studies, so we downgraded the quality of evidence due to risk of bias by 2 levels 2Random sequence generation was unclear in all both studies, allocation concealment was unclear in 1 and high risk of bias in the other study, so we downgraded by 2 levels 3Sequence generation was unclear in 2 studies and allocation concealment was unclear in 3 studies, so we downgraded the quality rating by 1 level 4Sequence generation was unclear in 3 studies and at high risk in 1 study, while allocation concealment was unclear in 4 studies and at high risk in 1 study, so we downgraded by 1 level 5Sequence generation was unclear in 2/3 studies and at high risk in 1/3, allocation concealment was unclear in 2/3 studies and high in 1/3, so we downgraded by 2 levels 6Random sequence generation was unclear in 2/5 and high in 1/5 studies, while allocation concealment was unclear in 2/5 and high in 2/5 studies, so we downgraded the quality of evidence due to high risk of bias by 2 levels 7The wide confidence interval was judged to include a threshold for appreciable harm considered to be > 25% increase in RR, in this case there was > 65% increase in RR for harm, so we downgraded by 1 level 8Sequence generation was unclear in 3/7 studies and at high risk in 1/7. Allocation concealment was unclear in 5/7 studies and at high risk in 1/7. We downgraded the quality rating by 2 levels 9Sequence generation and allocation concealment were unclear in 1/2 studies, so we downgraded by 1 level 10Sequence generation and allocation concealment were unclear, so we downgraded by 1 level 11As there was only 1 study with very few events and CIs around estimates of effect included appreciable benefit and appreciable harm, we downgraded by 2 levels | ||||||
| Monofilament compared to multifilament tapes for stress urinary incontinence in women | ||||||
| Patient or population: women with stress urinary incontinence | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| multifilament tapes | Monofilament | |||||
| Subjective cure (short term ≤ 1 year) | Study population | RR 1.07 | 505 | ⊕⊕⊕⊝ | ||
| 784 per 1000 | 839 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 810 per 1000 | 867 per 1000 | |||||
| Subjective cure (medium term: 1 to 5 years) | No studies reported this outcome | ‐ | (0 studies) | |||
| Subjective cure (long term: > 5 years) | No studies reported this outcome | ‐ | (0 studies) | |||
| Bladder or urethral perforation | Study population | RR 0.76 | 496 | ⊕⊕⊕⊝ | ||
| 37 per 1000 | 28 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 32 per 1000 | 25 per 1000 | |||||
| Voiding dysfunction | Study population | RR 2.20 | 400 | ⊕⊕⊝⊝ | ||
| 41 per 1000 | 89 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 65 per 1000 | 143 per 1000 | |||||
| De novo urgency or urgency incontinence | Study population | RR 1.09 | 496 | ⊕⊕⊝⊝ | ||
| 102 per 1000 | 111 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 107 per 1000 | 117 per 1000 | |||||
| Vaginal tape erosion | Study population | RR 0.43 | 396 | ⊕⊕⊕⊕ | ||
| 62 per 1000 | 26 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 43 per 1000 | 18 per 1000 | |||||
| Repeat incontinence surgery (short term ≤ 1 year) | No studies reported this outcome | ‐ | (0 studies) | |||
| Repeat incontinence surgery (long term > 5 years) | No studies reported this outcome | ‐ | (0 studies) | |||
| Cost effectiveness of intervention | No studies reported this outcome | ‐ | (0 studies) | |||
| Quality of life scores ICIQ | The mean quality of life scores ICIQ in the control group was 2.1 | The mean quality of life scores ICIQ in the intervention group was 0.6 lower (0.76 lower to 0.44 lower) | ‐ | 96 | ⊕⊕⊕⊕ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ICIQ: International Consultation on Incontinence questionnaire RCT: randomised controlled trial RR: risk ratio | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Random sequence generation and allocation concealment unclear in 2/4 studies, so we downgraded by 1 level 2Random sequence generation and allocation concealment unclear in 2/3 studies, so downgraded by 1 level 3The wide confidence interval was judged to include a threshold for appreciable harm considered to be > 25% increase in RR, in this case there was much more than a 25% increase in RR for harm, so we downgraded by 1 level 4Sequence generation and allocation concealment were unclear in 2/4 studies, so we downgraded the quality rating by 1 level 5The wide confidence interval was judged to include a threshold for appreciable harm considered to be > 25% increase in RR, in this case there was > 65% increase in RR for harm, so we downgraded by 1 level | ||||||
Background
Urinary incontinence is a very common condition in women. It is associated with significant physical morbidity, sexual dysfunction, loss of independence and a reduction in psychological well being, with consequent decreased participation in social and domestic activities (Wetle 1995; Thom 1998; Van Oyen 2002; Salonia 2004; Botlero 2010). Overall the prevalence of urinary incontinence in adult women has been estimated to be between 10% and 40%, and is considered severe in about 3% to 17%, with annual incidence ranging from 2% to 11% (Hunskaar 2002; Milsom 2009). The prevalence of stress urinary incontinence (SUI) in women is between 12% to 46% (Irwin 2006; Botlero 2008; Coyne 2009). This is a potentially debilitating social problem with significant cost implications to the individuals and the healthcare service. The estimated annual cost to the healthcare system in the UK exceeds GBP 700 million and in the USA it is over USD 20 billion (Fantl 1996; Hu 2004; Turner 2004). There is also significant cost borne by women on an individual basis, with estimates of more than GBP 178 million annually (Turner 2004; Papanicolaou 2005).
Continence is achieved through interplay of the normal anatomical and physiological properties of the bladder, urethra, urethral sphincter and pelvic floor, with the nervous system co‐ordinating these organs. The urethra and its sphincter act as a closure mechanism during bladder filling to contain urine within the bladder, thereby allowing storage of urine until a convenient time and place to void is reached. The pelvic floor provides support to the bladder and urethra, and allows normal abdominal pressure transmission to the proximal urethra, which is essential in the maintenance of continence. Crucial to the healthy functioning of the bladder, urethra, sphincter and pelvic floor is co‐ordination between them, which is facilitated by an intact nervous system.
There are many theories hypothesizing the pathophysiology of stress urinary incontinence. Historically Goran Enhorning was first to measure simultaneous bladder and urethral pressures. He suggested that during the cough impulse, pressure is transmission from the abdomen to the urethra with a concurrent reduction in urethral closure pressure that results in SUI (Enhorning 1961). McGuire’s modified classification of SUI emphasizes the principle of intrinsic sphincter deficiency (ISD) as a cause of SUI. This is said to occur due to poor urethral closure function resulting from defective urethral mucosal coaptation. These two theories informed procedures such as the Burch Colposuspension and Marshall Marchetti Krantz operations. De Lancey’s 'hammock' theory suggested that abdominal pressure transmission to the bladder neck and urethra leads to the proximal urethra being compressed against the pubo‐vesical fascia and anterior vaginal wall, thus maintaining continence (DeLancey 1994).
Recent findings on the pathophysiology of urinary incontinence have demonstrated that mid‐urethral support, provided by the pubo‐urethral ligaments, also plays an important role in maintaining continence when the intra‐abdominal pressure rises. This has led to the 'integrated theory' for the maintenance of continence in female SUI (Petros 1990; Petros 1993). This theory, in turn, is the basis for the current use of minimally invasive mid‐urethral tapes in the treatment of SUI.
When performing mid‐urethral tape surgery there are different types of synthetic materials used. Synthetic meshes are divided into four groups:
-
type 1 are macroporous, monofilament;
-
type 2 are microporous;
-
type 3 are macroporous, multifilament;
-
type 4 are submicronic, coated biomaterials with pore sizes of less than 1 μm.
Type 1 mesh has the highest biocompatibility with the least propensity for infection. Differences in their efficacy and complications are likely to be due to several factors including the different knits and weaves of the various tape materials, their biomechanical properties and histological biocompatibility. Pore size affects the inflammatory response and resultant connective tissue formation within and into the mesh, and the rearrangement of materials such as collagen within the mesh structure. Macroporous meshes (pore size in excess of 75 μm) easily allow macrophages, leukocytes, fibroblasts, blood vessels and collagen to transverse the pores: thus macroporous meshes promote tissue host ingrowth with resultant biocompatibility and low risk of infection (Amid 1997). Monofilament tapes are widely available and now predominate in current clinical practice.
In contrast, microporous meshes (pore size greater than 10 μm) allow bacteria to pass through and replicate, but exclude macrophages. Multifilament tapes have smaller pore sizes, and are thus microporous. This perhaps explains why tape erosion was more common in the multifilament tapes, though statistical significance was not reached.
Description of the condition
Incontinence occurs when this normal relationship between the lower urinary tract components is disrupted, as a result of nerve damage or direct mechanical disruption to the pelvic organs. Advancing age, higher parity, vaginal delivery, obesity and post menopausal status are all associated with an increased risk of urinary incontinence (Wilson 1996).
There are different forms of urinary incontinence of which SUI is the most common type, accounting for at least 50% of cases of urinary incontinence in women (Hannestad 2000). SUI is the involuntary loss of urine that occurs with physical exertion (e.g. sporting activities), or on sneezing or coughing (Haylen 2010). Urodynamic stress incontinence (USI) is the involuntary leakage of urine observed during filling cystometry, it is associated with increased intra‐abdominal pressure, in the absence of a detrusor contraction (Haylen 2010). Two mechanisms for stress incontinence are recognized: hyper‐mobility or significant displacement of the urethra and bladder neck during exertion, and intrinsic urethral sphincter deficiency (Blaivas 1988). These mechanisms may co‐exist in women (O'Donnell 1994). Few clinical trials have distinguished between the two conditions, probably because there is currently no standardised and validated test available for this (Blaivas 1988; McGuire 1993). We considered women whose incontinence could be due to either mechanism together in this review.
The diagnosis of urodynamic stress incontinence implies that urodynamic investigation has been done to confirm stress incontinence; it may also identify the presence of detrusor overactivity, in mixed urinary incontinence. Standard clinical assessment includes history taking, physical examination, frequency/volume charts and urine analysis. Some authors described women with the symptom of stress urinary incontinence only (diagnosis made on clinical evaluation without urodynamics). Women with stress urinary incontinence and those with urodynamic stress incontinence have been included in this review.
Urgency urinary incontinence (UUI) is a sudden, compelling desire to pass urine, which is difficult to defer (urgency), accompanied by the involuntary loss of urine. Detrusor overactivity (DO) is a diagnosis that denotes involuntary detrusor contractions observed during the filling phase of a urodynamic assessment. It may be spontaneous or provoked and can be qualified according to cause ‐ neurogenic or idiopathic (Haylen 2010). We included women with UUI and the formal urodynamic diagnosis of DO in the review only if they had co‐existing stress incontinence (so called mixed urinary incontinence (MUI)).
Women with MUI who were included in this review had symptoms of SUI plus either urgency or UUI, or urodynamic stress incontinence (USI) plus DO (urodynamic diagnosis).
Description of the intervention
Management of SUI includes conservative, mechanical, pharmacological and surgical interventions.
-
Conservative management centres on lifestyle modifications, physical methods including pelvic floor muscle training, electrical stimulation, biofeedback and the use of weighted cones.
-
Mechanical devices that prevent or reduce urinary leakage are available, and include metal plugs or patches and urethral or vaginal inserts.
-
Drug therapies, such as oestrogens and alpha adrenergic agents, have been used in the past. Recently, inhibitors of serotonin and norepinephrine reuptake have been proposed as new drug therapy for SUI, used alone or in combination with other conservative management (Ghoniem 2005).
A trial of such conservative treatments should be undertaken before resorting to surgery. The following interventions are the subject of separate Cochrane reviews.
-
Lifestyle interventions for the treatment of urinary incontinence in adults (Imamura 2010).
-
Bladder training for urinary incontinence in adults (Wallace 2004).
-
Comparisons of approaches to pelvic floor muscle training for urinary incontinence in women (Hay‐Smith 2011).
-
Feedback or biofeedback to augment pelvic floor muscle training for urinary incontinence in women (Herderschee 2011).
-
Pelvic floor muscle training added to another active treatment versus the same active treatment alone for urinary incontinence in women (Ayeleke 2013).
-
Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women (Dumoulin 2014).
-
Combined conservative interventions for urge, stress or mixed incontinence in adults (French 2010).
-
Weighted vaginal cones for urinary incontinence (Herbison 2013).
-
Mechanical devices for urinary incontinence in women (Lipp 2011).
-
Oestrogen therapy for urinary incontinence in post‐menopausal women (Cody 2012).
-
Adrenergic drugs for urinary incontinence in adults (Alhasso 2005).
-
Serotonin and noradrenaline reuptake inhibitors (SNRI) for stress urinary incontinence in adults (Mariappan 2005).
-
Acupuncture for stress urinary incontinence in adults (Wang 2013).
Surgical procedures to remedy SUI generally aim to lift and support the urethro‐vesical junction, but in the last decade the emphasis has been on suburethral support at the mid‐urethral level. Owing to disagreement on the precise mechanism by which continence is achieved, the choice of surgical procedure is influenced by co‐existent problems, surgeon's preference and the physical features of the person affected.
Numerous surgical methods for SUI have been described and evaluated in Cochrane reviews. Traditionally, they fall into seven categories:
-
suburethral slings (including traditional suburethral slings and minimally invasive sling operations; Rehman 2011);
-
open abdominal retropubic suspension (e.g. colposuspension (Burch/modified Burch), Marshall‐Marchetti‐Krantz (MMK); Lapitan 2012);
-
laparoscopic retropubic suspension (Dean 2006);
-
anterior vaginal repair (anterior colporrhaphy; Glazener 2001);
-
needle suspensions (Glazener 2004);
-
urethral injections (Kirchin 2012); and
-
artificial sphincters.
Suburethral slings have become the favourite primary continence surgery in current clinical practice. Several developments in type and technique have resulted in the separation of the original sling review, Bezerra 2005, into three different reviews focusing on:
-
traditional suburethral slings (Rehman 2011)
-
minimally invasive slings such as TVT and TOT (Ogah 2009), and
-
single incision slings, also known as mini‐slings (Nambiar 2014).
The materials that have been used for slings may be biological or synthetic. The first of these reviews concentrates on traditional (biological) suburethral sling operations (Rehman 2011). A traditional suburethral sling operation requires a combined abdominal and vaginal approach. Strips of material are tunnelled under the proximal urethra. They are attached either to the rectus muscle or the iliopectineal ligaments, resulting in a tightening of the sling and increased bladder support every time the woman strains to prevent leaking. They are applied under open surgery and are fixed with sutures.
This current review is an update of the second of these reviews, focusing on minimally invasive suburethral sling operations using artifical (synthetic) non‐absorbable sling materials (Ogah 2009). The techniques of these procedures are described below. This review does not include single incision slings.
The third of these reviews is a new, recently published review that compares a new type of sling, the single incision sling, which is also known as the mini‐sling (Nambiar 2014). The technique differs from that of the original synthetic slings in that a single incision is made within the vagina using a significantly shorter tape and there are no tape exit incisions.
How the intervention might work
The current review focuses on mid‐urethral sling operations. These involve the insertion of a tape covered by a plastic sheath around the mid‐urethra without suture fixation, performed in some centres under local anaesthesia (Ulmsten 1995a; Ulmsten 1996; Smith 2002). The aim is to restore or enhance the patient's urethral support during a sudden movement, such as a cough or sneeze, which would prevent the involuntary loss of urine. Ultrasound studies suggest that the mechanism of action is the intermittent or dynamic obstruction of the urethra by the tape when increased abdominal pressure occurs (such as when coughing or sneezing; Dietz 2004).
There are two main types of surgical approaches.
-
Retropubic: This procedure involves the insertion of two needles passed through the retropubic space blindly from the vagina to abdomen or from the abdomen to the vagina. Cystoscopy is recommended to detect any perforation of the bladder or urethra (Ulmsten 1995a; Ulmsten 1995b).
-
Transobturator; This is another type of minimally invasive synthetic suburethral sling operation in which the tape is inserted in a horizontal plane underneath the middle of the urethra between the two obturator foramina. The ends of the tape are tunnelled percutaneously with a tunneller (curved needle), again without suture fixation. As the retropubic space is not breached, it is argued that cystoscopy is not required (Delorme 2001; Delorme 2003; Delorme 2004). Shortly after the development of this technique a similar operation was described in which a tape is passed percutaneously through the obturator foramina, using an inside‐to‐outside technique, i.e. medio‐lateral (de Leval 2003; de Leval 2005).
We included only mid‐urethral sling operations, with synthetic tape materials applied through minimally invasive surgeries, either through the retropubic space or the transobturator route in this review. However, a number of modifications of transobturator surgery using the same route have been described and we have included these too.
In this update, in contrast to the original review in which trials of minimally invasive slings were compared to traditional slings, open colposuspension, or laparoscopic colposuspension, these comparator techniques have not been included, as these are now covered by other Cochrane reviews (Dean 2006; Rehman 2011; Lapitan 2012).
A concern of using synthetic material is the potential risk of complications caused by infection and tissue reaction to the tapes. Some aspects of the material that may vary include pore size, mono‐ or multifilament design, and biocompatibility. We included all types of mesh used in different minimally invasive slings in this review, and assessed possible differences between the risk of complications.
Why it is important to do this review
There is a plethora of minimally invasive synthetic tapes available and used worldwide for treatment of SUI. The reported effectiveness and safety of these procedures have made them very popular, but in the past there has been controversy about which of these procedures is best, as the introduction of many of these procedures and tapes was market driven and was not accompanied by rigorous prospective randomised controlled trials of effectiveness. Now more randomised controlled trials that assess their effectiveness have been published, but many trials are too small to draw definitive conclusions, hence the need for the first review.
Our initial review, Ogah 2009, showed evidence of efficacy in the short‐term, as many trials only reported a 12‐month follow‐up. A significant advantage of a Cochrane review is not only the rigorous database search and methodology, but most importantly the ability to update the review and meta‐analysis as new evidence becomes available. This meta‐analysis of the trials available is necessary to help make judgements on medium‐ and longer‐term efficacy, since we now have 18 years‐worth of data since the initial report of the retropubic mid‐urethral tape, and it is over 11 years since the first randomised trials of the tension‐free vaginal tape and transobturator tapes were published. It is also necessary to provide evidence on medium‐ and longer‐term safety of the devices both suspected and expected, and the unexpected adverse events in the long‐term. This review update aims to clarify the uncertainty surrounding the use mid‐urethral slings in terms of surgical approach, route of insertion and the type of tape used.
This current update analyses only the effects of mid‐urethral slings, and excludes both single incision slings and other surgical procedures e.g. traditional slings and colposuspension. The options of no treatment, conservative treatment and pharmacological treatment are also excluded, as this will be addressed in a future Cochrane review.
Objectives
To assess the clinical effects of mid‐urethral sling (MUS) operations for the treatment of stress urinary incontinence (SUI), urodynamic stress incontinence (USI) or mixed urinary incontinence (MUI) in women.
Methods
Criteria for considering studies for this review
Types of studies
Randomised or quasi‐randomised controlled trials amongst women with USI (urodynamic diagnosis), or symptoms of SUI or MUI (clinical diagnosis), in which both trial arms involve a mid‐urethral sling operation.
Types of participants
Adult women with SUI due to hyper‐mobility and intrinsic sphincter deficiency, or both, diagnosed clinically or with urodynamics, and women with MUI in which stress incontinence was the predominant symptom. Classification of diagnoses were accepted as defined by the trialists.
Types of interventions
Both trial arms of a study must involve mid‐urethral sling operations to treat SUI or MUI.
We made the following comparisons.
-
Transobturator route (TOR) versus retropubic route (RPR).
-
Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach.
-
Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach.
-
One method of mid‐urethral tape insertion versus another method, same route.
-
One type of tape material versus another
Comparisons with other types of surgery (i.e. traditional slings, single incision slings and colposuspension) for urinary incontinence are covered in other recent Cochrane reviews. The options of no treatment, conservative treatment and pharmacological treatment have also been removed as these will be addressed in a future Cochrane review.
Types of outcome measures
Primary outcomes
We selected the outcome measures used in this review on the basis of their relevance to the clinical cure or improvement of incontinence. We regarded the principal measures of effectiveness as being:
1. Women's observations
-
the proportion of women cured (continent or dry) following surgery;
-
the proportion of women whose incontinence is improved;
-
cure and improvement measured in the short term (less than one year); medium term (one to five years); and long term (more than five years).
Secondary outcomes
2. Women's observations
-
Urgency symptoms or urgency incontinence.
3. Quantification of symptoms
-
Pad changes (from self‐reported number of pads used).
-
Incontinence episodes (from self‐completed bladder chart).
-
Pad tests of quantified leakage (mean volume or weight of urine loss).
4. Clinician's observations
-
Objective cure rates in the short term (less than one year); medium term (one to five years); and long term (more than five years).
-
De novo detrusor overactivity (urodynamic diagnosis).
5. Surgical outcome measures
-
Duration of operation.
-
Length of inpatient stay.
-
Time to return to normal activity level.
-
Operative blood loss.
6. Adverse events
-
Major vascular or visceral injury.
-
Bladder, urethral or bowel perforation.
-
Nerve damage.
-
Perioperative surgical complications (e.g. infection, bacteriuria, haemorrhage with or without major vessel lesion).
-
Voiding dysfunction or difficulty after three months (with or without urodynamic confirmation) or need for long‐term catheterisation.
-
Infection related to use of synthetic mesh.
-
Tape erosion or extrusion or exposure into the vagina.
-
Tape erosion or extrusion or exposure into the bladder or urethra.
7. Need for further treatment
-
Physiotherapy treatment.
-
Drug treatment for urinary incontinence or symptoms.
-
Pelvic organ prolapse (e.g. cystocoele, rectocoele, enterocoele).
-
Repeat incontinence surgery.
-
Later prolapse surgery.
8. Quality of life
Quality of life assessed by means of:
-
general health status measures (e.g. Short Form 36 (Ware 1993));
-
condition‐specific instruments designed to assess incontinence, e.g. the Bristol Female Lower Urinary Tract Symptoms questionnaire (BFLUTS; Jackson 1996);
-
condition‐specific sexual function assessment e.g. via Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire (PISQ‐12;Rogers 2003);
-
psychological measures.
9. Economic measures
-
Costs of interventions.
-
Cost‐effectiveness of interventions.
-
Resource implications.
10. Other outcomes
-
Non‐prespecified outcomes judged to be important when performing the review.
Search methods for identification of studies
Unless otherwise stated we did not impose language or other restrictions on any of the searches which are described below.
Electronic searches
This review drew on the search strategy developed for the Cochrane Incontinence Group. We identified relevant trials from the Cochrane Incontinence Group Specialised Trials Register. For more details of the search methods used to build the Specialised Register please see the Group's module in The Cochrane Library. The Register contains trials identified from the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, and MEDLINE in process, ClinicalTrials.gov and handsearching of journals and conference proceedings. Most of the trials in the Cochrane Incontinence Group Specialised Register are also contained in CENTRAL. The date of the last search was 26 June 2014.
The terms used to search the Incontinence Group Specialised Register are given in Appendix 1.
Additionally the following electronic databases were searched, details of the searches and the terms used are given in Appendix 1.
-
Embase and Embase Classic (January 1947 to Week 25 2014; searched on 26 June 2014; limited to those years not searched via the CENTRAL search of Embase, i.e. 1 January 2010 to Week 25 2014 inclusive).
-
WHO ICTRP (searched on 30 June 2014)
Details of the searches performed for the previous version of this review can be found in Appendix 2.
Searching other resources
We searched the reference lists of relevant articles.
Data collection and analysis
Selection of studies
Randomised and quasi‐randomised trials were identified using the above search strategy. We excluded studies from the review if they were not randomised or quasi‐randomised controlled trials for incontinent women, or if they made comparisons other than those pre‐specified. Excluded studies are listed in the Characteristics of excluded studies table along with reasons for their exclusion. We evaluated all potentially eligible studies for appropriateness for inclusion without prior consideration of the results. We retrieved reports of potentially eligible trials in full.
Data extraction and management
We extracted data independently using a standard form containing pre‐specified outcomes. Where data may have been collected but not reported, we sought clarification from the trialists. We processed included trial data as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved differences of opinion relating to study inclusion, methodological quality or data extraction by discussion among the reviewers, and when necessary, referred them to a third party for arbitration.
Assessment of risk of bias in included studies
Miss Abigail Ford and Mr Joseph Ogah (review authors) extracted data and independently assessed the included trials for methodological quality and validity using the 'Risk of bias' assessment tool (Higgins 2011). We assessed the risk of bias in the results of the included trials by examining the following features: selection bias, which results from insecure random allocation of treatments; performance bias that occurs when knowledge of the procedure actually performed might have affected the participant or care provider; attrition bias caused by incomplete reporting of outcome data, or from dropouts or losses to follow‐up, particularly if there is a differential dropout rate between groups; and biased ascertainment (detection bias) of outcome where knowledge of the allocation might have influenced the measurement of outcome. These were assessed under the headings below:
-
sequence generation;
-
allocation sequence concealment;
-
blinding of participants and personnel;
-
blinding of outcome assessment;
-
incomplete outcome data.
These were presented in the 'Risk of bias' tables, graphs and summary figures.
The GRADE (Grades of Recommendation, Assessment, Development and Evaluation) system was used to assess and grade the quality of evidence for each individual outcome (Guyatt 2011a; Guyatt 2011b; Guyatt 2013a; Guyatt 2013b).
Measures of treatment effect
The review was conducted using the standard Cochrane software Review Manager 'Revman' version 5.2 (Reference Manager 2012). For categorical outcomes we related the numbers reporting an outcome to the numbers at risk in each group to derive a summary risk ratio (RR). For continuous variables we used means and standard deviations to derive a mean difference (MD) if the outcomes were measured in the same way between trials. Any continuous data that were the product of a number of different scales (for example, scales used to assess symptoms such as pain or quality of life) we summarised as the standardised mean difference (SMD) using a fixed‐effect model. A fixed‐effect model was used for calculation of all summary estimates and 95% confidence intervals (CIs) except when there was significant heterogeneity. When appropriate, we undertook meta‐analysis.
We undertook a narrative review of eligible trials where statistical synthesis of data from more than one study was not possible, or considered inappropriate.
Unit of analysis issues
We did not perform analysis of trials with non‐standard designs, such as cross‐over trials and cluster‐randomised trials, as there were no such trials. We analysed trials with multiple treatment groups by treating each pair of arms as a separate comparison, as appropriate.
Dealing with missing data
We defined 'intention‐to‐treat analysis' as meaning that all participants were analysed in their randomised groups whether or not they received the allocated intervention. We included data as they were reported for each outcome and did not impute missing values, but used the data as presented by the trialists. Where intraoperative outcomes were reported, we used the number of patients undergoing the described procedure as the denominator. Follow‐up outcomes were reported with the exclusion of patients lost to follow‐up. We would have performed sensitivity analyses had there been differential dropout from the randomised groups, or another reason to suspect systematic bias from missing data.
Assessment of heterogeneity
We used a fixed‐effect approach for the analysis unless there was evidence of heterogeneity across trials. Differences between trials were investigated when apparent either through visual inspection of the results, or when statistically significant heterogeneity was demonstrated by using the Chi² test at the 10% probability level or assessment of the I² statistic (Higgins 2003).
Assessment of reporting biases
We examined publication bias by means of a funnel plot where there were 10 or more trials contributing to a meta‐analysis.
Data synthesis
We used fixed‐effect model analysis for the meta‐analyses, except when significant heterogeneity was suspected, when we used a random‐effects model.
Subgroup analysis and investigation of heterogeneity
Heterogeneity
Where there was no obvious reason for heterogeneity to exist (after consideration of populations, interventions, outcomes and settings of the individual trials), or it persisted despite the removal of trials that were clearly different from the others, we used a random‐effects model.
Subgroup analysis
Clinical factors such as symptoms of SUI, USI, MUI, diagnosis of intrinsic urethral sphincter deficiency or urethral hypermobility, obesity, previous incontinence surgery, presence or absence of prolapse, anaesthesia used, or experience of the surgeon and other concomitant surgical intervention, might all influence the outcomes of surgery and consideration of subgroup analysis was taken into account.
Sensitivity analysis
We performed sensitivity analysis to explore the robustness of the results in some outcomes. We planned to carry out sensitivity analysis for the primary outcomes by restricting our analysis to trials assessed as having a low risk of bias for the of domain attrition bias; if more than 30% of participants had been lost to follow‐up, these trials would have been excluded from sensitivity analyses. This was not necessary.
Summary of findings
We employed the GRADE approach to interpret findings (Guyatt 2011a; Guyatt 2011b; Guyatt 2013a; Guyatt 2013b; Langendam 2013), and the GRADE profiler (GRADEpro) was used to import data from RevMan 5.2 to create 'Summary of findings’ tables. These tables provide outcome‐specific information concerning the overall quality of evidence from trials included in a comparison, the magnitude of effect of the interventions examined, and the sum of the available data on the outcomes we considered.
We included the following outcomes in the 'Summary of findings’ tables.
-
Subjective cure: medium term (one to five years).
-
Subjective cure: long term (more than 5 years).
-
Bladder or urethral perforation.
-
Voiding dysfunction: short term and medium term (up to five years).
-
De novo urgency or urgency incontinence: short term (less than one year).
-
Vaginal tape erosion: short term and medium term (up to five years).
-
Repeat continence surgery: short term (less than one year).
-
Repeat continence surgery: long term (more than five years).
-
Groin pain: short term (less than one year).
-
Quality of life.
-
Economic analysis.
We assessed the overall quality of evidence for these outcomes and downgraded the evidence level from high quality by one level for serious, or by two levels for very serious study limitations (risk of bias), indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
Results
Description of studies
Results of the search
We screened the 841 records identified by the literature searches and obtained a total of 290 full‐text articles for further assessment. Altogether 217 reports concerning 81 randomised trials met the inclusion criteria. A further two trials were ongoing.
We excluded 551 records on the basis of either the title or abstract alone, and 71 reports relating to 62 studies after retrieval of the full text publication. Exclusion was either because they were not randomised trials, they did not include a mid‐urethral sling operation, or because the women included in the trial were not urinary incontinent. A full description of these trials can be found in the Characteristics of excluded studies section of this review. The flow of literature through the assessment process is shown in Figure 1.

PRISMA study flow diagram
We analysed trials with multiple treatment groups by treating each pair of arms as a separate comparison, as appropriate. There were six trials in this review that supplied data and for which this method was employed, thus leading to 87 comparisons. There were no trials with non‐standard designs, such as cross‐over trials and cluster‐randomised trials.
Included studies
Further characteristics of the trials are reported in the Characteristics of included studies table.
Comparisons and interventions
1. Transobturator (TOR) versus retropubic route (RPR)
This comparison of mid‐urethral sling operations was based on the routes that the tapes traverse, i.e. transobturator route (TOR) versus retropubic route (RPR). There were 55 trials that investigated this (Aigmuller 2014; Alkady 2009; Andonian 2007; Aniuliene 2009; Araco 2008; Barber 2008; Barry 2008; Cervigni 2006; Chen 2010; Chen 2012; Choe 2013; Darabi Mahboub 2012; David‐Montefiore 2006; Deffieux 2010; de Tayrac 2004; Diab 2012; El‐Hefnawy 2010; Enzelsberger 2005; Freeman 2011; Hammoud 2011; Jakimiuk 2012; Kamel 2009; Karateke 2009; Kilic 2007; Kim 2005; Krofta 2010; Laurikainen 2007; Leanza 2009; Lee 2007; Liapis 2006; Mansoor 2003; Mehdiyev 2010; Meschia 2007; Nerli 2009; Nyyssonen 2014; Oliveira 2006; Palomba 2008; Porena 2007; Rechberger 2009; Richter 2010; Riva 2006; Ross 2009; Salem 2014; Scheiner 2012; Schierlitz 2008; Tanuri 2010; Tarcan 2011; Teo 2011; van Leijsen 2013; Wang 2006; Wang 2008; Wang 2009; Wang 2010; Wang 2011; Zullo 2007).
2. Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach
Trials in this group compared the retropubic bottom‐to‐top approach (e.g. tension‐free vaginal tape (TVTTM); tape inserted from the vagina through the retropubic space and exiting onto the abdominal skin in the suprapubic region) with a retropubic top‐to‐bottom approach (e.g. suprapubic urethral support sling (SPARCTM); tape inserted from the abdomen in the suprapubic region through the retropubic space and exiting in the vagina). There were five such trials (Andonian 2005; Kim 2004; Lim 2005; Lord 2006; Tseng 2005).
3. Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach
Ten trials reported on this comparison which compared tapes traversing the obturator route: obturator lateral‐to‐medial approach, (e.g. TOTTM tape inserted in the thigh crease and through the obturator route exiting in the vagina) with obturator medial‐to‐lateral approach (e.g. TVT‐OTM tape inserted in the vagina and through the obturator route exiting in the thigh crease; Abdel‐Fattah 2010; But 2008; Chen 2010; Hassan 2013; Houwert 2009; Lee 2008; Liapis 2008; Park 2012; Peattie 2006; Scheiner 2012).
4. One method of mid‐urethral tape insertion versus another method, same route
Ten trials compared different methods of carrying out operations using the same route (Cho 2010; de Leval 2011; Elbadry 2014; Juang 2007; Naumann 2006; Paparella 2010; Rechberger 2011; Tommaselli 2012; Ugurlucan 2013; Zhang 2011).
The trials compared the following operations.
Transobturator lateral to medial
-
Monarc® TOT versus TOT® (Cho 2010).
-
TOT versus adjustable TOT (Elbadry 2014).
-
TOT versus TOT with two‐point fixation sutures (Rechberger 2011).
-
Synthetic TOT versus biological TOT (Paparella 2010; Ugurlucan 2013).
Transobturator medial to lateral
-
TVT‐O versus modified TVT‐O (shorter tape and less lateral dissection; de Leval 2011).
-
TVT‐O versus TVT‐O plus Ingleman‐Sundberg bladder denervation procedure (Juang 2007).
-
TVT‐O versus modified TVT‐O (reduced dissection; Tommaselli 2012).
-
TVT‐O versus modified TVT‐O (self‐tailored mesh; Zhang 2011).
Retropubic
-
TVT versus modified TVT, bottom‐to‐top (suburethral pad; Naumann 2006).
5. One type of tape material versus another
A final group compared different mid‐urethral sling operations based on the properties of the tape material. All used synthetic non‐absorbable mesh for the tape material, but differed in the structure of the material, i.e. monofilament tapes versus multifilament tapes. There were four such trials (Lim 2005; Meschia 2006; Okulu 2013; Rechberger 2003), which made the following comparisons.
-
Monofilament (TVT SPARC) verus multifilament (IVS; Lim 2005).
-
Monofilament (TVT) versus multifilament (IVS; Meschia 2006).
-
Synthetic monofilament (prolene light mesh) versus a combined synthetic mesh coated with a biological film (Ultrapro mesh) versus a multifilament mesh (Vypro; Okulu 2013).
-
Monofilament (TVT) versus multifilament (IVS; Rechberger 2003).
Publication type and sample characteristics
1. Retropubic route versus transobturator route
The sample sizes ranged from 20 to 597; with a median of 131.
Twelve of the 55 trials were reported only as abstracts (Cervigni 2006; Choe 2013; Darabi Mahboub 2012; Diab 2012; Hammoud 2011; Kamel 2009; Leanza 2009; Mansoor 2003; Oliveira 2006; Riva 2006; Salem 2014; Tarcan 2011).
Inclusion and exclusion criteria were not clearly stated in eight trials (Cervigni 2006; Chen 2010; Darabi Mahboub 2012; Kamel 2009; Mansoor 2003; Mehdiyev 2010; Oliveira 2006; Tarcan 2011).
All trials had women either presenting with SUI or had USI confirmed. In addition other characteristics included:
-
23 trials included women with MUI (Alkady 2009; Aigmuller 2014; Andonian 2007; Barber 2008; Barry 2008; Cervigni 2006; David‐Montefiore 2006; Deffieux 2010; El‐Hefnawy 2010; Freeman 2011; Kim 2005; Krofta 2010; Laurikainen 2007; Lee 2007; Nerli 2009; Nyyssonen 2014; Porena 2007; Richter 2010; Riva 2006; Scheiner 2012; Tarcan 2011; van Leijsen 2013; Wang 2011).
-
ten trials included women with previous incontinence surgery (Andonian 2007; Aniuliene 2009; Barber 2008; Barry 2008; David‐Montefiore 2006; de Tayrac 2004; Kim 2005; Lee 2007; Richter 2010; Wang 2010).
-
28 trials included women with pelvic organ prolapse (POP; Alkady 2009; Andonian 2007; Aniuliene 2009; Barber 2008; Barry 2008; Cervigni 2006; Chen 2012; David‐Montefiore 2006; El‐Hefnawy 2010; Freeman 2011; Krofta 2010; Laurikainen 2007; Mansoor 2003; Meschia 2007; Nerli 2009; Porena 2007; Rechberger 2009; Richter 2010; Riva 2006; Scheiner 2012; Schierlitz 2008; Tanuri 2010; Tarcan 2011; van Leijsen 2013; Wang 2006; Wang 2008; Wang 2009; Wang 2010).
-
in 13 trials women had concomitant pelvic or prolapse surgery (Andonian 2007; Barber 2008; Barry 2008; Cervigni 2006; David‐Montefiore 2006; Richter 2010; Riva 2006; Scheiner 2012; Schierlitz 2008; Tarcan 2011; Wang 2008; Wang 2009; Wang 2010).
Follow‐up for women ranged from one month to five years with a median follow‐up of 12 months.
2. Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach
Five trials investigated a retropubic bottom‐to‐top approach versus a retropubic top‐to‐bottom approach (Andonian 2005; Kim 2004; Lim 2005; Lord 2006; Tseng 2005). One of the five trials was reported only as an abstract (Kim 2004), and this was the only study without clear inclusion and exclusion criteria.
The sample sizes ranged from 62 to 304; the average sample size, 'n' (standard deviation), for retropubic in‐out was 62 (49) and for retropubic out‐in was 64 (53).
All trials had women either presenting with SUI or had USI confirmed. All trials except Tseng 2005 included women with MUI. Andonian 2005 and Lord 2006 included women with previous incontinence surgery.
All the trials included women with POP and had concomitant pelvic or POP surgery performed.
Follow‐up for women ranged from 1.5 months to 2 years with a median of 12 months.
3. Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach
Nine trials compared the obturator medial‐to‐lateral approach with the obturator lateral‐to‐medial approach (Abdel‐Fattah 2010; But 2008; Chen 2010; Hassan 2013; Houwert 2009; Lee 2008; Liapis 2008; Park 2012; Scheiner 2012). With the exception of Hassan 2013, which was reported only as an abstract, the other eight trials were reported as full articles. Peattie 2006 appears in a trials registry but its status is unclear; we have contacted the authors and are awaiting a response.
The sample sizes ranged from 74 to 341 with a median size of 110.
Inclusion and exclusion criteria were not clearly stated in two trials (But 2008; Hassan 2013).
All trials had women either presenting with SUI or had USI confirmed.
Five trials included women with MUI (Abdel‐Fattah 2010; But 2008; Lee 2008; Park 2012; Scheiner 2012), and two trials included women who had undergone previous incontinence surgery (Abdel‐Fattah 2010; Scheiner 2012). Scheiner 2012 included women with POP and women with concomitant pelvic or POP surgery.
Follow‐up ranged from three months to three years with a median follow up of 12 months.
4. One method of mid‐urethral tape insertion versus another method, same route
Ten trials investigated one method of mid‐urethral tape versus another method, using the same route (Cho 2010; de Leval 2011; Elbadry 2014; Juang 2007; Naumann 2006; Paparella 2010; Rechberger 2011; Tommaselli 2012; Ugurlucan 2013; Zhang 2011). Three of these trials were reported only as abstract publications (Cho 2010; Elbadry 2014; Naumann 2006). The sample sizes ranged from 72 to 463 with a median of 156.
All the trials included women with SUI or USI. Rechberger 2011 reported women with ISD. Inclusion and exclusion criteria were not clearly defined in four of the ten trials (Cho 2010; Elbadry 2014; Juang 2007; Naumann 2006). Juang 2007, Tommaselli 2012 and Ugurlucan 2013 included women with MUI, whilst de Leval 2011 and Ugurlucan 2013 included women who had undergone previous incontinence surgery. Women with prolapse were included in de Leval 2011 and Ugurlucan 2013, but concomitant POP surgery was performed only in Ugurlucan 2013.
Follow‐up ranged from three months to three years.
5. One type of tape material versus another
Four trials investigated the use of monofilament tape versus multifilament tape (Lim 2005; Meschia 2006; Okulu 2013; Rechberger 2003). All four trials were reported as full article publications.
The sample sizes ranged from 70 to 182 with a median value of 144.
The trials had women either presenting with SUI or had USI confirmed: all had clear inclusion and exclusion criteria. Three trials included women with POP (Lim 2005; Meschia 2006; Rechberger 2003). Two trials included women with MUI (Lim 2005; Meschia 2006). Three trials included women with previous incontinence surgery (Lim 2005; Okulu 2013; Rechberger 2003), whereas only Lim 2005 included women who had concomitant pelvic or POP surgery.
Follow‐up for women ranged from three months to three years.
Outcomes
The trials reported their outcomes in a variety of different ways. The primary outcome, subjective cure of urinary incontinence (UI), was defined as follows:
-
no subjective report of UI (Aniuliene 2009; Barber 2008; But 2008; Cho 2010; Darabi Mahboub 2012; de Leval 2011; de Tayrac 2004; Deffieux 2010; El‐Hefnawy 2010; Freeman 2011; Hassan 2013; Houwert 2009; Jakimiuk 2012; Kim 2004; Laurikainen 2007; Leanza 2009; Liapis 2006; Lim 2005; Lord 2006; Mansoor 2003; Naumann 2006; Nerli 2009; Okulu 2013; Paparella 2010; Porena 2007; Richter 2010; Riva 2006; Scheiner 2012; Schierlitz 2008; Tanuri 2010; Tarcan 2011; Ugurlucan 2013; van Leijsen 2013; Wang 2010; Wang 2011; Zhang 2011);
-
no subjective report of UI and negative stress test (Lee 2007; Meschia 2006; Meschia 2007; Park 2012; Rechberger 2003; Rechberger 2009; Wang 2008);
-
no or improved subjective report of UI (Abdel‐Fattah 2010; Aigmuller 2014; Barry 2008; Karateke 2009; Ross 2009; Teo 2011; Zullo 2007).
Secondary outcome objective cure was defined by the trialists as follows:
-
absence of USI on urodynamics (UDS) (Abdel‐Fattah 2010; Araco 2008; Barry 2008; Cervigni 2006; Enzelsberger 2005; Kamel 2009; Karateke 2009; Kilic 2007; Kim 2005; Krofta 2010; Lim 2005; Riva 2006; Schierlitz 2008; Zullo 2007);
-
absence of SUI and negative stress test (Alkady 2009; Paparella 2010; Porena 2007);
-
one‐hour pad test less than 2 g (Andonian 2005; Andonian 2007; But 2008; Ross 2009; Tseng 2005);
-
24‐hour pad test less than 5 g (Darabi Mahboub 2012; Okulu 2013; Teo 2011);
-
negative stress test (Aigmuller 2014; Aniuliene 2009; Barber 2008; Chen 2010; David‐Montefiore 2006; de Leval 2011; de Tayrac 2004; Deffieux 2010; El‐Hefnawy 2010; Juang 2007; Kim 2004; Kim 2005; Laurikainen 2007; Lord 2006; Meschia 2007; Nerli 2009; Tarcan 2011; van Leijsen 2013; Wang 2009; Wang 2011);
-
multiple objective measures used (El‐Hefnawy 2010; Juang 2007; Kamel 2009; Kim 2005; Krofta 2010; Liapis 2006; Liapis 2008; Mansoor 2003; Meschia 2006; Naumann 2006; Nyyssonen 2014; Oliveira 2006; Rechberger 2011; Richter 2010; Scheiner 2012; Tanuri 2010; Tommaselli 2012; Wang 2006; Wang 2008; Wang 2010).
Excluded studies
We excluded 62 studies after retrieval of the full text publication because they were not randomised trials, did not include a mid‐urethral sling operation, the participants did not have urinary incontinence, or the participants were randomised to an intervention other than a mid‐urethral sling (such as no treatment, pelvic floor muscle training, drugs, or a different class of surgery). The details of the reasons for exclusion are given in the Characteristics of excluded studies table.
Ongoing trials
There are two ongoing trials: Cavkaytar 2013 and Sung 2013.
Cavkaytar 2013 is a randomised controlled trial (RCT) comparing RPR and TOR for the treatment of SUI in women with no intrinsic sphincter deficiency. This study is currently recruiting and includes women with SUI and excludes women with MUI or detrusor overactivity (DO), previous incontinence surgery, and women with a body mass index greater than 35. Fifty women have been randomly assigned into each arm for evaluation.
Sung 2013 is an RCT comparing mid‐urethral sling operations and behavioural or pelvic floor therapy in combination versus suburethral sling operations alone for women with MUI. The ESTEEM trial includes women over 18 years of age who have had urodynamic investigation within the last 18 months, and excludes women with prolapse, previous incontinence surgery, and women currently on antimuscarinic medication. This trial is currently recruiting participants.
Studies awaiting classification
There are no studies awaiting classification.
New trials included in this update
We have included 48 new trials in this update (Abdel‐Fattah 2010; Aigmuller 2014; Alkady 2009; Andonian 2007; Aniuliene 2009; Chen 2010; Chen 2012; Cho 2010; Choe 2013; Darabi Mahboub 2012; de Leval 2011; Diab 2012; Elbadry 2014; El‐Hefnawy 2010; Freeman 2011; Hassan 2013; Hammoud 2011; Jakimiuk 2012; Juang 2007; Kamel 2009; Karateke 2009; Kilic 2007; Krofta 2010; Leanza 2009; Mehdiyev 2010; Naumann 2006; Nerli 2009; Nyyssonen 2014; Okulu 2013; Palomba 2008; Paparella 2010; Park 2012; Peattie 2006; Rechberger 2011; Richter 2010; Ross 2009; Salem 2014; Scheiner 2012; Tanuri 2010; Tarcan 2011; Teo 2011; Tommaselli 2012; Ugurlucan 2013; van Leijsen 2013; Wang 2008; Wang 2010; Wang 2011; Zhang 2011).
Previously included trials with new outcome data
We have included new data from 11 trials previously included in this review, including the report of medium‐ or long‐term outcomes (Barber 2008; But 2008; David‐Montefiore 2006; Deffieux 2010; Houwert 2009; Laurikainen 2007; Porena 2007; Rechberger 2009; Schierlitz 2008; Wang 2009; Zullo 2007).
Previously included trials with no new outcome data
Twenty‐two trials included in the earlier version of this review have not published new outcome data (Andonian 2005; Araco 2008; Barry 2008; Cervigni 2006; de Tayrac 2004; Enzelsberger 2005; Kim 2004; Kim 2005; Lee 2007; Lee 2008; Liapis 2006; Liapis 2008; Lim 2005; Lord 2006; Mansoor 2003; Meschia 2006; Meschia 2007; Oliveira 2006; Rechberger 2003; Riva 2006; Tseng 2005; Wang 2006).
Risk of bias in included studies
Details of the criteria used to assess the risk of bias and the ratings for each study are reported in the 'Risk of bias' tables that accompany the Characteristics of included studies. Further information on the risk of bias in included trials is shown in Figure 2 the 'Risk of bias' graph and Figure 3 the ‘Risk of bias' summary.

Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgments about each risk of bias item for each included study.
The risk of bias in the trials included was variable, though overall only few trials were judged to be at high risk of bias. In over 50% of trials the random sequence generation was judged to be adequate, for example with the use of a computer‐generated list or a table of random numbers. Approximately 30% of trials confirmed that secure concealment of the randomisation process was used, for example allocation by a remote person or the use of sealed envelopes.
Blinding of participants was unclear in the majority of trials. This is an obvious limitation with trials comparing surgical interventions, though one trial described the use of a 'sham' procedure (Jakimiuk 2012). Blinding of patients and the post‐operative reviewer was not reported in most trials. Loss to follow‐up in most trials was minimal, and in approximately 50% of included trials the risk of attrition bias was judged to be low.
We judged that 39 trials had adequate random sequence generation (Abdel‐Fattah 2010; Aigmuller 2014; Alkady 2009; Andonian 2005; Araco 2008; Barber 2008; But 2008; Cervigni 2006; Chen 2012; David‐Montefiore 2006; Deffieux 2010; de Tayrac 2004; Freeman 2011; Jakimiuk 2012; Karateke 2009; Krofta 2010; Laurikainen 2007; Lord 2006; Mansoor 2003; Meschia 2006; Meschia 2007; Nyyssonen 2014; Okulu 2013; Paparella 2010; Porena 2007; Richter 2010; Ross 2009; Scheiner 2012; Schierlitz 2008; Teo 2011; Tommaselli 2012; Tseng 2005; Ugurlucan 2013; van Leijsen 2013; Wang 2006; Wang 2008; Wang 2009; Wang 2011; Zullo 2007).
We judged that adequate allocation concealment occurred in 26 trials (Abdel‐Fattah 2010; Aigmuller 2014; Alkady 2009; Andonian 2005; Araco 2008; Barber 2008; David‐Montefiore 2006; Deffieux 2010; de Tayrac 2004; El‐Hefnawy 2010; Freeman 2011; Laurikainen 2007; Lord 2006; Mansoor 2003; Meschia 2006; Meschia 2007; Nyyssonen 2014; Okulu 2013; Paparella 2010; Porena 2007; Ross 2009; Teo 2011; Tommaselli 2012; van Leijsen 2013; Wang 2011; Zullo 2007).
We judged that 24 trials had an adequate randomisation process and secure concealment of the randomisation process (Aigmuller 2014; Alkady 2009; Andonian 2005; Araco 2008; Barber 2008; David‐Montefiore 2006; Deffieux 2010; de Tayrac 2004; Freeman 2011; Laurikainen 2007; Lord 2006; Mansoor 2003; Meschia 2006; Meschia 2007; Nyyssonen 2014; Okulu 2013; Paparella 2010; Porena 2007; Ross 2009; Teo 2011; Tommaselli 2012; van Leijsen 2013; Wang 2011; Zullo 2007).
We judged that 22 trials adequately blinded outcome assessors (Abdel‐Fattah 2010; Andonian 2005; Andonian 2007; Araco 2008; Barber 2008; de Tayrac 2004; El‐Hefnawy 2010; Karateke 2009; Krofta 2010; Liapis 2006; Liapis 2008; Lord 2006; Paparella 2010; Porena 2007; Rechberger 2003; Tseng 2005; Ugurlucan 2013; van Leijsen 2013; Wang 2006; Wang 2009; Wang 2010; Zullo 2007).
We judged 36 trials to be at a low risk of attrition bias (Abdel‐Fattah 2010; Aigmuller 2014; Alkady 2009; Andonian 2005; Aniuliene 2009; Barber 2008; Barry 2008; But 2008; Deffieux 2010; de Leval 2011; El‐Hefnawy 2010; Freeman 2011; Karateke 2009; Krofta 2010; Laurikainen 2007; Liapis 2006; Liapis 2008; Lord 2006; Meschia 2007; Nyyssonen 2014; Paparella 2010; Park 2012; Porena 2007; Rechberger 2009; Ross 2009; Scheiner 2012; Tanuri 2010; Tommaselli 2012; Tseng 2005; Ugurlucan 2013; Wang 2006; Wang 2008; Wang 2009; Wang 2010; Wang 2011; Zullo 2007).
Effects of interventions
See: Summary of findings for the main comparison Transobturator (TOR) compared to retropubic (RPR) route for stress urinary incontinence in women; Summary of findings 2 Retropubic bottom‐to‐top approach compared to retropubic top‐to‐bottom approach for stress urinary incontinence in women; Summary of findings 3 Obturator medial‐to‐lateral approach compared to obturator lateral‐to‐medial approach for stress urinary incontinence in women; Summary of findings 4 Monofilament compared to multifilament tapes for stress urinary incontinence in women
Comparison 1. Transobturator versus retropubic route
Fifty‐five trials addressed this comparison (Aigmuller 2014; Alkady 2009; Andonian 2007; Aniuliene 2009; Araco 2008; Barber 2008; Barry 2008; Cervigni 2006; Chen 2010; Chen 2012; Choe 2013; Darabi Mahboub 2012; David‐Montefiore 2006; de Tayrac 2004; Deffieux 2010; Diab 2012; El‐Hefnawy 2010; Enzelsberger 2005; Freeman 2011; Hammoud 2011; Jakimiuk 2012; Kamel 2009; Karateke 2009; Kilic 2007; Kim 2005; Krofta 2010; Laurikainen 2007; Leanza 2009; Lee 2007; Liapis 2006; Mansoor 2003; Mehdiyev 2010; Meschia 2007; Nerli 2009; Nyyssonen 2014; Oliveira 2006; Palomba 2008; Porena 2007; Rechberger 2009; Richter 2010; Riva 2006; Ross 2009; Salem 2014; Scheiner 2012; Schierlitz 2008; Tanuri 2010; Tarcan 2011; Teo 2011; van Leijsen 2013; Wang 2006; Wang 2008; Wang 2009; Wang 2010; Wang 2011; Zullo 2007).
1.1 Women's observations
Subjective cure within 12 months was reported in 36 trials with a total of 5514 participants. Assessment of cure was self‐reported by participants and by responses to symptom‐based questionnaires. The combined results from the 36 trials showed no statistically significant difference in the subjective cure rates between the two routes (RR 0.98, 95% CI 0.96 to 1.00; Analysis 1.1). The short‐term subjective cure ranged from 62% to 98% for TOR and from 71% to 97% for RPR.
The mean subjective cure rate across both groups was 83.3% and, using this as the assumed control subjective cure rate in the RPR group, for every 1000 women there were 17 fewer cured in the TOR group (95% CI from 0 fewer to 33 fewer per 1000). This was not statistically significant and is also unlikely to be considered to be a clinically significant difference. The funnel plot inspection shows no strong evidence of publication bias Figure 4.
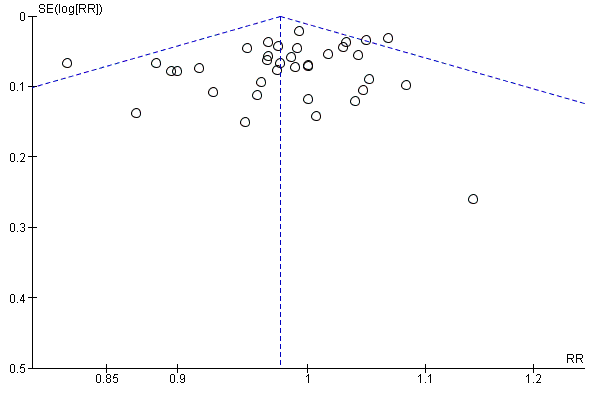
Funnel plot of comparison: 1 Transobturator (TOR) versus retropubic (RPR) route, outcome: 1.1 Subjective cure (short term, ≤ 1 year)
There was also no statistically significant difference between the two groups in terms of symptomatic improvement and cure rate (RR 0.98, 95% CI 0.96 to 1.00; Analysis 1.2).
Medium‐term outcomes
Only seven trials provided information after the first year (Deffieux 2010; Laurikainen 2007; Nyyssonen 2014; Porena 2007; Schierlitz 2008; Tarcan 2011; Zullo 2007). Five trials (683 participants) contributed medium‐term data between one and five years after surgery, which showed no significant difference in subjective cure between the two groups (RR 0.97, 95% CI 0.87 to 1.09; Analysis 1.3). Subjective cure rates ranged from 82% to 91% in the TOR group and from 77% to 98% in the RPR group.
The average medium‐term subjective cure rate across both groups was 86.9% and, using this as the assumed control cure rate in the RPR group, for every 1000 women there were 26 fewer women cured in the TOR group (95% CI from 26 per 1000 more to 70 per 1000 fewer).
Long‐term outcomes
Four trials (714 women) reported long‐term results for subjective cure after five years (Laurikainen 2007; Porena 2007; Richter 2010; Zullo 2007); the difference between the groups was not statistically significant (RR 0.95, 95% CI 0.80 to 1.12; Analysis 1.4). Subjective cure rates range from 43% to 92% in the TOR group and from 51% to 88% in the RPR group.
The average long‐term subjective cure rate across both groups was 84.3% and, using this as the assumed control cure rate in the RPR group, for every 1000 women there were 42 fewer women cured in the TOR group (95% CI from 110 per 1000 less to 34 per 1000 more).
Two trials with 340 women reported long‐term data for subjective cure and improvement and the difference between the groups was not statistically significant (RR 0.92, 95% CI 0.67 to 1.28; Analysis 1.5); due to significant heterogeneity we also performed a random‐effects analysis that produced similar results and, as there were only two trials, the fixed‐effect analysis was maintained.
1.2 Quantification of symptoms
Only two trials provided data about pad test weights (Tanuri 2010 used a non standardised modified/simplified pad test and Wang 2006 used the standard one‐hour pad test). The information provided was not suitable for meta‐analysis, but each reported a significant reduction in pad weight postoperatively in each group without a significant difference between the groups.
1.3 Clinician's observations
Objective cure was assessed by 40 trials with 6145 participants in the short term using a variety of measures such as urodynamic assessment, negative cough‐stress test, one‐hour pad test of 2 g or less, one‐hour pad test of 1 g or less, and 24‐hour pad test of 5g or less. The cure rate with the obturator route was 85.7% versus 87.2% for the RPR (RR 0.98, 95% CI 0.96 to 1.00, Analysis 1.6). The confidence interval was narrow and this statistically non significant difference between the groups (2%) is unlikely to represent a clinically significant difference in outcome between the two methods in the short term.
The small difference in the objective cure and improvement rate in the short term was not statistically ‐ nor was it likely to be clinically ‐ significant (RR 0.98, 95% CI 0.96 to 1.01; 10 studies, 1478 women; Analysis 1.7). The same holds true for the medium‐term objective cure rates (RR 1.00, 95% CI 0.95 to 1.06; 5 studies, 596 women; Analysis 1.8), and long‐term cure rates (RR 0.97, 95% CI 0.90 to 1.06; 3 studies, 400 women; Analysis 1.9).
1.4 Surgical outcome measures
Duration of operation was significantly shorter, by an average of approximately seven minutes, with the TOR compared with the RPR (MD ‐7.54 minutes, 95% CI ‐9.31 to ‐5.77). There was statistically significant heterogeneity, but all the trials reported a shorter operating time with the TOR. This may be attributable to most surgeons routinely performing a cystoscopy following a RPR procedure, but not necessarily doing this after a TOR procedure.
To investigate this theory, we performed a sensitivity analysis to assess the difference in operative time between the RPR and TOR approach in trials where cystoscopy was performed in both comparison groups as defined by the trialists. In eight trials where cystoscopy was performed in both TOR and RPR groups we still found a shorter operating time with the TOR in comparison to the RPR (MD ‐6.50 95% CI ‐7.57 to ‐5.44) although high heterogeneity persisted. Using a random‐effects method on the full analysis of 31 trials still showed the duration of operation to be statistically significantly shorter with TOR approach (MD ‐7.54 minutes, 95% CI ‐9.31 to ‐5.77; Analysis 1.10).
Intraoperative blood loss was small (mean loss ranged from 15 ml to 125 ml), but was significantly less with the TOR approach (MD ‐6.49 ml, 95% CI ‐12.33 to ‐0.65; Analysis 1.11). There was significant heterogeneity that was accounted for by three small trials (Nerli 2009; Wang 2008; Zullo 2007). In view of the small blood volumes involved, this is unlikely to be a clinically significant finding.
Length of stay was also significantly shorter by an average of 0.17 days with the TOR compared with the retropubic route (MD ‐0.17, 95% CI ‐0.25 to ‐0.10; Analysis 1.12). A high level of between‐study heterogeneity (I² 94%) was present with the length of stay, thus a random‐effects model was used, which then showed no significant difference (MD ‐0.25, 95% CI ‐0.59 to 0.09; Analysis 1.12).
The mean time the women took to return to normal activity ranged from under two weeks to just over five weeks, with no statistically significant difference between the two surgical approaches (MD ‐0.05, 95% CI ‐0.15 to 0.06; Analysis 1.13). This confirms the minimally invasive nature of both operations, compared with a more normal recovery period of three months after major abdominal surgery.
1.5 Adverse events
In trials where overall perioperative complication rates were reported there were no statistically significant differences in the rate of perioperative complications between the TOR and RPR groups (RR 0.91, 95% CI 0.73 to 1.14; Analysis 1.14).
In trials where specific complications were recorded there were significant differences in the rate of each individual complication sustained.
Major vascular/visceral injury
Major vascular injury such as retropubic haematoma or major visceral injury, for example bowel perforation, was reported by 28 trials with 4676 women. This occurred significantly less often with TOR than with RPR (RR 0.33, 95% CI 0.19 to 0.55; Analysis 1.15).
Bladder/urethral perforation
Forty trials assessed rate of bladder perforation. The rate was significantly lower in the TOR group than the RPR group (RR 0.13, 95% CI 0.08 to 0.20; Analysis 1.16). The average bladder perforation rate across both groups was 2.54% and, using this as the assumed control bladder perforation rate in the RPR group, there were 22 fewer perforations per 1000 in the TOR group (95% CI from 20 to 23 per 1000 fewer). There was some degree of asymmetry in the funnel plot, which raised the possibility of some publication bias Figure 5.

Funnel plot of comparison: 1 Transobturator (TOR) versus retropubic (RPR) route, outcome: 1.16 Bladder or urethral perforation
Postoperative voiding dysfunction (POVD)
Rates of postoperative voiding dysfunction (POVD) was assessed in 37 trials with 6200 participants. This showed significantly lower rates in the TOR group than in the RPR group (RR 0.53 95% CI 0.43 to 0.65; Analysis 1.17). The average POVD rate across both groups was 5.53% and, using this as the assumed control rate in the RPR group, there were 26 fewer POVD per 1000 in the TOR group (95% CI from 19 to 32 per 1000 fewer). The funnel plot showed symmetry on visual inspection, which suggests a low likelihood of publication bias Figure 6.

Funnel plot of comparison: 1 Transobturator (TOR) versus retropubic (RPR) route, outcome: 1.17 Voiding dysfunction
Urgency and urgency urinary incontinence (UUI)
The 31 trials (4923 women) that reported de novo urgency and urgency urinary incontinence (UUI) showed no statistically significant difference between the two groups (RR 0.98, 95% CI 0.82 to 1.17; Analysis 1.18). In the short term the average rate of de novo urgency/UUI across both groups was 8.35% and, using this as the assumed control rate in the RPR group, there were two fewer cases per 1000 in the TOR group (95% CI from 15 per 1000 fewer to 14 per 1000 more).
Equally, in the medium term the rate of de novo urgency and UUI was not significantly different (RR 0.98, 95% CI 0.55 to 1.73, Analysis 1.19). Laurikainen 2007 reported long‐term data for de novo urgency and UUI for 253 women; this showed no difference between the groups (RR 0.81, 95% CI 0.18 to 3.53; 253 women; Analysis 1.20).
Four trials with 853 women with DO showed a rate of 8% in both groups (RR 1.00, 95% CI 0.58 to 1.73; Analysis 1.21).
In one trial of women with MUI (Laurikainen 2007), 84% who had pre‐existing moderate or severe urinary frequency and urgency symptoms were cured of these symptoms post operatively at the five‐year follow‐up.
Vaginal tape erosion
Vaginal tape erosion was assessed in 31 trials with 4743 participants. No significant difference was demonstrated between the groups (RR 1.13, 95% CI 0.78 to 1.65; Analysis 1.22). The average rate of vaginal tape erosion across both groups was 2.09%, and, using this as the assumed control rate in the RPR group, there were three more cases per 1000 in the TOR group (95% CI from 5 per 1000 fewer to 14 per 1000 more). The funnel plot showed symmetry on visual inspection suggesting low likelihood of publication bias Figure 7. In the one trial that reported long‐term tape erosion (Laurikainen 2007), no tape erosion was reported in either group. Bladder or urethral tape erosion was assessed in four trials with 374 participants. No significant difference was demonstrated between the groups (RR 0.34, 95% CI 0.01 to 8.13; Analysis 1.23).
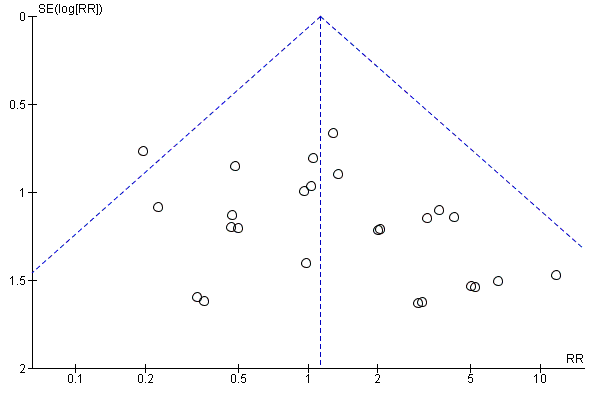
Funnel plot of comparison: 1 Transobturator (TOR) versus retropubic (RPR) route, outcome: 1.22 Vaginal tape erosion
Pain
There was a significantly higher occurrence of groin pain in women who underwent a TOR procedure than in women who underwent a RPR procedure (RR 4.12, 95% CI 2.71 to 6.27; Analysis 1.24). The average rate of groin pain across both groups was 4.51% and, using this as the assumed control rate in the RPR group, there were 163 more cases per 1000 in the TOR group (95% CI from 94 to 266 per 1000 more). Conversely, suprapubic pain was found to be significantly lower in women who underwent a TOR procedure than a RPR procedure (RR 0.29, 95% CI 0.11 to 0.78; Analysis 1.25). Both groin and suprapubic pain occurrence were short‐lasting, with most resolving within the first six months. The duration of pain ranged from two to 52 weeks, with a median duration of eight weeks. The funnel plot for groin pain showed symmetry on visual inspection, suggesting low likelihood of publication bias Figure 8.

Funnel plot of comparison: 1 Transobturator (TOR) versus retropubic (RPR) route, outcome: 1.24 Groin pain
1.6 Need for further treatment
Nine trials (1402 women) reported the number of women who required repeat incontinence surgery in the short term (up to one year). The difference between the TOR and RPR groups was not statistically significant (RR 1.64, 95% CI 0.85 to 3.16; Analysis 1.26). The average rate of repeat incontinence surgery in the short term across both groups was 2.43% and, using this as the assumed control rate in the RPR group, there were 12 more cases per 1000 in the TOR group (95% CI from 3 per 1000 fewer to 41 per 1000 more).
More women required repeat incontinence surgeries in the TOR group in the medium term (RR 21.89, 95% CI 4.36 to 109.77; two studies, 355 women; Analysis 1.27).
In the long term, three trials with data from 487 women, found that more women required repeat incontinence surgery in the TOR group (RR 8.79, 95% CI 3.36 to 23.00; Analysis 1.28). The average rate of repeat incontinence surgery in the long term across both groups was 5.34% and, using this as the assumed control rate in the RPR group, there were 231 more cases per 1000 in the TOR group (95% CI from 45 to 767/1000 more).
1.7 Quality of life
Thirty‐three of the 55 trials in this comparison assessed quality of life (QoL; Aigmuller 2014; Andonian 2007; Barber 2008; Barry 2008; Chen 2012; Darabi Mahboub 2012; David‐Montefiore 2006; Deffieux 2010; de Tayrac 2004; El‐Hefnawy 2010; Freeman 2011; Jakimiuk 2012; Karateke 2009; Kim 2005; Krofta 2010; Laurikainen 2007; Leanza 2009; Mansoor 2003; Meschia 2007; Nerli 2009; Porena 2007; Richter 2010; Riva 2006; Ross 2009; Scheiner 2012; Schierlitz 2008; Tanuri 2010; Tarcan 2011; Teo 2011; Wang 2008; Wang 2010; Wang 2011; Zullo 2007); however only 11 of these trials reported QoL scores (Andonian 2007; Barber 2008; Barry 2008; David‐Montefiore 2006; de Tayrac 2004; Laurikainen 2007; Meschia 2007; Porena 2007; Riva 2006; Schierlitz 2008; Wang 2008).
A wide variety of measures were used by different trials to assess this outcome, including:
Condition‐specific measures
-
Incontinence Impact Questionnaire (IIQ‐7).
-
Urogenital Distress Inventory (UDI‐6).
-
International Consultation on Incontinence Questionnaire (ICIQ).
-
Urinary Incontinence Quality of Life Scale (I‐QOL).
-
Kings Health Questionnaire (KHQ).
-
Bristol Female Lower Urinary Tract Symptoms questionnaire (BFLUTS).
-
Women Irritative Prostate Symptoms Score (W‐IPSS).
-
Urinary Incontinence Severity Score (UISS).
-
Detrusor Instability Score (DIS).
-
A Visual Analogue Scale (VAS).
-
CONTILIFE.
Generic measures
-
EuroQoL 5‐Dimensional Classification Component Scores (EuroQoL‐5D).
-
Short‐Form Health‐Related QoL (SF‐36).
-
Patient Global Impression of Severity (PGI‐S).
-
Patient Global Impression of Improvement (PGI‐I).
The data on quality of life outcomes were reported in different ways, which precluded meta‐analysis. In general, with the exception of Araco 2008, all trials found that women's QoL improved significantly post‐operatively within each group, but no statistically significant differences were found between the randomised groups. Only the Araco 2008 trial found the I‐QOL scores to be statistically significantly higher postoperatively after the retropubic approach.
Sexual function quality of life measures
Sexual function was addressed in 10 trials (Barber 2008; Barry 2008; Deffieux 2010; de Tayrac 2004; Freeman 2011; Krofta 2010; Richter 2010; Ross 2009; Scheiner 2012; Schierlitz 2008), which used a variety of measures including validated questionnaires and direct questioning. Questionnaires employed were:
-
Prolapse/Incontinence Symptoms Questionairre (PISQ‐12);
-
Bristol Female Lower Urinary Tract Symptoms questionnaire (BFLUTS);
-
International Consultation on Incontinence Questionnaire Lower Urinary Tract Symptoms quality of life questionnaire (ICIQ‐LUTSqol); and
-
Visual Analogue Scale (VAS).
In all the trials there was significant improvement in sexual function from baseline scores during the follow‐up period that spanned six to 24 months. There were no significant differences between the two groups. At 24‐month follow‐up, rates of superficial and deep dyspareunia were low, with no difference between the groups.
1.8 Economic measures
Economic analysis from an RCT comparing TOR and RPR showed that over a 12‐month follow‐up period there was a cost saving with TOR of CAD (Canadian Dollars) 1135 per patient despite no difference in health outcome between the groups (Ross 2009). The average cost of TOR was 17% less than that of RPR. Despite no significant difference there was a probability greater than 80% of TOR being more cost effective than RPR (Lier 2011).
Comparison 2. Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach
Five small trials, with 636 women in total, addressed this comparison (Andonian 2005; Kim 2004; Lim 2005; Lord 2006; Tseng 2005).
2.1 Women's observations
Three trials (477 women) investigated subjective cure defined as self‐reported absence of urinary leakage on stress (Kim 2004; Lim 2005; Lord 2006). In the 12 months following surgery, women were significantly more often dry with the bottom‐to‐top approach (TVTTM) compared to the top‐to‐bottom approach (SPARCTM; 87.34% versus 79.58%; RR 1.10, 95% CI 1.01 to 1.19; Analysis 2.1).
2.2 Quantification of symptoms
No data were reported for this outcome.
2.3 Clinician's observation
Five trials assessed objective cure using a variety of measures (Andonian 2005; Kim 2004; Lim 2005; Lord 2006; Tseng 2005): one‐hour pad test of 2g or less, negative stress test on urodynamics (UDS), the observed absence of urinary leakage when the patient coughed while supine and with a comfortably full bladder, and one‐hour pad test of 1g or less, respectively. In a total of 622 participants, the objective cure rate was similar between the two groups (94.19% versus 89.10%; RR 1.06, 95% CI 0.97 to 1.17; Analysis 2.2).
2.4 Surgical outcome measures
Two small trials, Kim 2004 and Tseng 2005, reported that there were no statistically significant differences in duration of operation (Analysis 2.3) or length of hospital stay (Analysis 2.4).
2.5 Adverse events
No statistically significant difference was seen in overall perioperative complications, but the confidence interval was wide (RR 0.98, 95% CI 0.53 to 1.84; Analysis 2.5).
Significantly fewer women experienced certain complications with the bottom‐to‐top approach (TVTTM), which included:
-
bladder perforation (RR 0.55, 95% CI 0.31 to 0.98; 5 trials; Analysis 2.6);
-
voiding dysfunction after the bottom‐to‐top approach (TVTTM; RR 0.40, 95% CI 0.18 to 0.90; 5 trials; Analysis 2.7);
-
vaginal tape erosions (RR 0.27, 95% CI 0.08 to 0.95; 4 trials; Analysis 2.10).
There were no statistically significant differences between the two groups with respect to:
-
postoperative de novo urgency symptoms and UUI (RR 0.84, 95% CI 0.52 to 1.34; 4 trials; Analysis 2.8); or
-
DO (1 trial; Analysis 2.9).
However, the confidence intervals were wide for each of these five outcomes, which reflects the small number of trials.
2.6 Need for further treatment
No data were reported on the need for further treatment.
2.7 Quality of life
Only one of the five trials, Andonian 2005, assessed the QoL of women using the Incontinence Impact Questionnaire (IIQ; Shumaker 1994), where a score of less than 50 represents a good QoL, 50 to 70 represents moderate QoL, and over 70 indicates a poor QoL. In this study the mean IIQ scores were similar in the groups preoperatively and improved postoperatively, but there was no significant difference between the groups after operation. At one year follow‐up, there was no statistically significant difference in the mean IIQ scores (mean difference of ‐4.6; 95% CI: ‐7.5 to 16.7).
2.8 Economic measures
No economic data were reported for this comparison.
Comparison 3. Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach
Ten trials reported this comparison (Abdel‐Fattah 2010; But 2008; Chen 2010; Hassan 2013; Houwert 2009; Lee 2008; Liapis 2008; Park 2012; Peattie 2006; Scheiner 2012).
3.1 Women's observations
Six trials investigated short‐term subjective cure rate and five of these assessed subjective cure and improvement in the short term (within 12 months of surgery). There were no statistically significant differences in either subjective cure rates (RR 1.0, 95% CI 0.96 to 1.06; Analysis 3.1) or subjective cure and improvement rates (RR 1.02, 95% CI 0.97 to 1.08 Analysis 3.2), and the confidence intervals for each were quite narrow. Two trials reported no statistically significant difference in subjective cure in the medium term (RR 1.06, 95% CI 0.91 to 1.23; Analysis 3.3) and a further two trials reported no significant difference in subjective cure and improvement in the medium term (RR 1.00, 95% CI 0.90 to 1.11; Analysis 3.4). There are no published trials with long‐term data.
3.2 Quantification of symptoms
No data were reported for this comparison.
3.3 Clinician's observation
Six trials assessed objective cure (short term, ≤ 1 year); there was no statistically significant difference between the two groups (RR 0.99, 95% CI 0.95 to 1.04; Analysis 3.5), and the confidence interval was narrow. There was also no statistically significant difference in the objective cure or improvement rate between the two groups (RR 1.00, 95% CI 0.95 to 1.07; Analysis 3.6).
3.4 Surgical outcome measures
There were no statistically significant differences between the two groups in terms of:
-
duration of operation, (in minutes, MD 0.52, 95% CI ‐1.09 to 2.13; 4 studies, 481 women; Analysis 3.7);
-
operative blood loss (in ml, MD 1.11, 95% CI ‐6.01 to 8.22; 3 studies, 255 women; Analysis 3.8);
-
length of hospital stay (in days, MD ‐0.77, 95% CI ‐2.54 to 0.99; 2 studies, 190 women; Analysis 3.9);
-
time to return to normal activity (in weeks, MD ‐0.60, 95% CI ‐1.80 to 0.60; 1 study, 100 women; Analysis 3.10).
3.5 Adverse events
Vaginal perforation was significantly less likely to occur with the medial‐to‐lateral approach (RR 0.25, 95% CI 0.12 to 0.53; I² of 43%; Analysis 3.13). The average rate of vaginal wall perforation across both groups was 7.39% and, using this as the assumed control rate in the lateral‐to‐medial group, there were 55 fewer cases per 1000 in the medial‐to‐lateral group (95% CI from 35 per 1000 fewer to 65 per 1000 more).
Voiding dysfunction occurred significantly more in the medial‐to‐lateral compared to the lateral‐to‐medial group (RR 1.74, 95% CI 1.06 to 2.88; I² of 0%; 8 studies, 1121 women; Analysis 3.15). The average rate of POVD across both groups was 5.53% and, using this as the assumed control rate in the lateral‐to‐medial group, there were 41 more cases per 1000 in the medial‐to‐lateral group (95% CI from 3 to 104 per 1000 more).
There were no statistically significant differences between the two groups in terms of:
-
overall perioperative complication rate (RR 1.30, 95% CI 0.23 to 7.51; 2 studies, 214 women; Analysis 3.11);
-
major vascular/visceral injury (RR 0.71, 95% CI 0.23 to 2.19; 4 studies, 622 women; Analysis 3.12);
-
bladder perforation (RR 0.38, 95% CI 0.07 to 1.92; 6 studies, 794 women; Analysis 3.14);
-
de novo urgency symptoms and UUI rates (RR 1.01, 95% CI 0.46 to 2.20; 3 studies, 357 women; Analysis 3.16);
-
detrusor overactivity (RR 0.87, 95% CI 0.27 to 2.84; 1 study, 114 women; Analysis 3.17);
-
vaginal tape erosions (RR 0.42, 95% CI 0.16 to 1.09; 7 studies, 1087 women; Analysis 3.18);
-
groin/thigh pain (9.2% versus 8%; RR 1.15, 95% CI 0.75 to 1.76; 6 studies, 837 women; Analysis 3.19).
3.6 Need for further treatment
Two large trials showed no significant difference in the rates of repeat incontinence surgery in the medium term (4.6% versus 7.1%; RR 0.64, 95% CI 0.32 to 1.30; Analysis 3.20).
3.7 Quality of life
Quality of life was assessed in five of the ten trials using validated QoL questionnaires. All of these trials reported QoL scores.
Condition‐specific QoL scores
-
Houwert 2009 used the short forms of the IIQ‐7 and UDI‐6. Within each group there was significant improvement postoperatively compared to scores obtained preoperatively, but no significant postoperative differences between the two groups (MD 16.54, 95% CI 4.84 to 28.24; 1 study, 42 women).
-
But 2008 assessed QoL with IIQ and UDI questionnaires and VAS scores, but reported no results.
-
Lee 2008 used a validated Korean version of the Incontinence QoL questionnaire (I‐QoL) and showed improvements within the groups, but with no significant differences between the groups after surgery.
-
Scheiner 2012 used the KHQ and found no significantly difference between the groups at baseline and postoperatively, but with improvement following surgery compared to baseline scores in all domains.
-
Abdel‐Fattah 2010 used the KHQ, Birmingham Bowel and Urinary Symptoms Questionnaire (BBUSQ‐22), PISQ‐12, PGI‐I and the short form of the ICIQ (ICIQ‐SF) to assess QoL. Overall there was statistically significant improvement in total scores, as well as in each of the nine domains of the KHQ. This remained the case when comparing baseline score in each group postoperatively; there was no significant difference in the QoL scores between the two routes.
Sexual function
Sexual function was addressed in three trials that used a variety of measures including validated questionnaires and direct questioning (Abdel‐Fattah 2010; Houwert 2009; Park 2012). Questionnaires included: the PISQ‐12, and BFLUTS (Abdel‐Fattah 2010). There was significant improvement in PISQ‐12 scores following surgery (improved sexual function compared to baseline), but no significant difference between the two groups at follow‐up. Rates of dyspareunia following surgery were extremely low, with evidence of resolution by 24 months.
3.8 Economic measures
No economic data were reported for this comparison.
Comparison 4. One method of mid‐urethral tape insertion versus another method, same route
Ten trials compared different methods of carrying out TOR and RPR operations using the same route (Cho 2010; de Leval 2011; Elbadry 2014; Juang 2007; Naumann 2006; Paparella 2010; Rechberger 2011; Tommaselli 2012; Ugurlucan 2013; Zhang 2011). The following operations were compared.
Transobturator lateral‐to‐medial
-
Monarc® TOT versus TOT® (Cho 2010).
-
TOT versus adjustable TOT (Elbadry 2014).
-
TOT versus TOT with two‐point fixation sutures (Rechberger 2011).
-
Synthetic TOT versus biological TOT (Paparella 2010; Ugurlucan 2013).
Transobturator medial‐to‐lateral
-
TVT‐O versus modified TVT‐O (shorter tape and less lateral dissection; de Leval 2011).
-
TVT‐O versus TVT‐O plus Ingleman‐Sundberg bladder denervation procedure (Juang 2007).
-
TVT‐O versus modified TVT‐O (reduced dissection; Tommaselli 2012).
-
TVT‐O versus modified TVT‐O (self‐tailored mesh; Zhang 2011).
Retropubic
-
TVT versus modified TVT, bottom‐to‐top (suburethral pad; Naumann 2006).
Each comparison group included only a small single trial, which precluded any meaningful statistical analysis of the outcomes measured, except for the synthetic versus biological TOT comparison, for which there were two small trials (Analysis 4.1; Analysis 4.2; Analysis 4.3; Analysis 4.5; Analysis 4.4; Analysis 4.6; Analysis 4.7; Analysis 4.8; Analysis 4.10; Analysis 4.11; Analysis 4.12; Analysis 4.13; Analysis 4.14; Analysis 4.15; Analysis 4.16). Naumann 2006 reported no usable data.
For all outcomes measured in each trial, there were no statistically significant differences reported, with the exception of Juang 2007, where significant differences were found in favour of TVT‐O plus Ingleman‐Sundberg bladder denervation procedure for objective cure, operative time and intraoperative blood loss. Objecture cure in the short term for synthetic versus biological TOT showed no significant difference (RR 1.03, 95% CI 0.94 to 1.14; 2 trials; Analysis 4.5.2)
Sexual function was assessed by Paparella 2010 and Tommaselli 2012 using the PISQ‐12. The PISQ‐12 scores decreased after the procedure in both groups, indicating improved sexual function after surgery. No significant differences were observed between groups after the procedures.
Comparison 5. One type of tape material versus another
Four trials compared different mid‐urethral sling operations based on their tape properties, e.g. monofilament tapes versus multifilament tapes (Lim 2005; Meschia 2006; Okulu 2013; Rechberger 2003). The interventions compared were:
-
monofilament (TVT SPARC) verus multifilament (IVS; Lim 2005);
-
monofilament (TVT) versus multifilament (IVS; Meschia 2006);
-
synthetic monofilament (prolene light mesh) versus combined synthetic and biological (Ultrapro mesh) versus multifilament mesh (Vypro; Okulu 2013);
-
monofilament (TVT) versus multifilament (IVS; Rechberger 2003).
5.1 Women's observations
In the short and medium term there was no statistically significant difference between monofilament and multifilament tapes in terms of their subjective cure rates; neither was there a significant difference found where the combined synthetic and biological tapes were compared to monofilament tapes (RR 1.03, 95% CI 0.95 to 1.10; RR 0.91, 95% CI 0.79 to 1.05; RR 1.10, 95% CI 0.96 to 1.26; Analysis 5.1: RR 1.03, 95% CI 0.85 to 1.23; RR 0.91, 95% CI 0.78 to 1.06; RR 1.13, 95% CI 0.96 to 1.32; Analysis 5.2).
5.2 Quantification of symptoms
No data were reported for this comparison.
5.3 Clinician's observation
The objective cure rate for monofilament tape and multifilament tapes show no significant difference between the groups (RR 1.07, 95% CI 0.96 to 1.19; Analysis 5.3).
5.4 Surgical outcome measures
There were no statistically significant differences in the duration of operation or length of hospital stay reported (RR 0.00, 95% CI ‐1.49 to 1.49; Analysis 5.4: RR 0.20, 95% CI ‐0.09 to 0.49; Analysis 5.5).
5.5 Adverse events
There were few perioperative complications with no statistically significant difference between the groups (RR 1.16, 95% CI 0.36 to 3.69; Analysis 5.6). No major vascular/visceral injury was reported in any of the trials (Analysis 5.7). Bladder perforation occurred in 4.49% of monofilament and 3.67% of multifilament tape procedures (RR 1.15, 95% CI 0.49 to 2.70; Analysis 5.8).
There were no statistically significant differences between the groups for:
-
POVD (RR 2.10, 95% CI 0.96 to 4.59; Analysis 5.9);
-
de novo urgency symptoms and UUI (RR 1.11, 95% CI 0.68 to 1.82; Analysis 5.10);
-
DO (RR 0.70, 95% CI 0.12 to 4.06; Analysis 5.11).
In three trials, vaginal tape erosions were more common in the multifilament group, but this did not reach statistical significance (RR 0.79, 95% CI 0.09 to 6.84; Analysis 5.12).
5.6 Need for further treatment
No data were reported regarding the need for further treatment in this comparison.
5.7 Quality of life
Only the Okulu 2013 study assessed QoL and showed improvement from baseline scores, with no significant difference between the comparison groups. At 48 months mean postoperative ICI‐Q QoL scores were significantly better in the monofilament group than in the multifilament group (MD ‐0.06, 95% CI ‐0.76 to ‐0.44; 1 study, 96 women; Analysis 5.13).
5.8 Economic measures
No economic data were reported for this comparison.
We have included extracted data of all the included studies in Table 1
| Study | Outcome data |
| Abdel‐Fattah 2010 | Group A: TVT‐O (n = 170) Group B: TOT (n = 171) Loss to follow up at 1yr: A: 18/170, B: 24/171 Loss to follow up at 3yrs: A: 44/170, B: 59/171 Objective cure: A: 114/121, B: 96/109 Subjective success: A: 121/149, B: 111/143 Bladder/urethral perforation: A: 1/170, B: 2/171 Voiding dysfunction: A: 12/170, B: 9/171 Tape erosion: A: 3/153, B: 5/149 Groin pain: A: 27/150, B: 19/147 Repeat continence surgery: A: 7/170, B: 15/171 QoL assessed via: King’s Health Questionnaire (KHQ) [10], Birmingham Bowel Urinary Symptom (BBUSQ‐22) [11] and Pelvic Organ Prolapse/Incontinence Sexual Function Questionnaire (PISQ‐12). In addition Patient Global Impression of Improvement (PGI‐I) [13] and International Consultation on Incontinence Questionnaire‐ Short form (ICIQ‐SF) [14] questionnaires. QOL scores were much improve following surgery with no significant inter group (A vs B) differences. Sexual dysfunction: PISQ‐12 employed. 199 patients completed this assessment and in most domains a significant improvement in postoperative PISQ‐12 scores was found with no significant difference demonstrated between the two groups. Intermediate (3 yr) Subjective success (very much & much improved) on PGI‐I: A: 93/126, B: 81/112 |
| Aigmuller 2014 | Group A: TVT: (n = 285; 38 of whom were lost to follow‐up) Group B: TVT‐O: (n = 269; 36 of whom were lost to follow‐up) Participants were evaluated at 3 months, with a further evaluation scheduled at 5 years
At 5‐year review:
|
| Alkady 2009 | Group A: TVT (n = 15) Group B: TVT‐O (n = 15)
|
| Andonian 2005 | Group A: SPARC Group B: TVT
|
| Andonian 2007 | Group A: Obtape (n = 78) Group B: DUPS (n = 32) ‐ suspended Group C: TVT (n = 80)
|
| Aniuliene 2009 | Group A: TVT‐O (n = 150) Group B: TVT (n = 114)
|
| Araco 2008 | Group A: TVT‐O (n = 120)
|
| Barber 2008 | Group A: TVT (n = 88) Group B: TOT (n = 82)
|
| Barry 2008 | Group A: TOT (n = 58)
|
| But 2008 | Group A: TVT‐O (n = 60) Group B: TOT (n = 60)
|
| Cervigni 2006 | Numbers in each group unreported. It was, thus, impossible to abstract results |
| Chen 2010 | Group A: TVT (n = 77) Group B: TOT (n = 45) Group C: TVT‐O (n = 65)
|
| Chen 2012 | A: TVT (n = 102) B: TVT‐O (n = 103)
|
| Cho 2010 | Group A: Monarc TOT (n = 48) Group B: TOT (n = 45)
|
| Choe 2013 | We were not able to use the data provided, as the number in each group was not specified |
| Darabi Mahboub 2012 | Group A: TOT (n = 40) Group B: TVT (n = 40) Operative time (minutes (SD): A: 64.50 (9.04), B: 64.00 (9.48) Mean hospital stay (days): A: 2.56 (0.51), B: 2.52 (0.47) |
| David‐Montefiore 2006 | Group A: RPR (n = 42) Group B: TOR (n = 46)
|
| de Leval 2011 | Group A: TVT‐O (n = 87) Group B: modified TVT‐O (n = 88)
At 3‐year follow‐up:
|
| de Tayrac 2004 | Group: A: TOT (n = 30) Group: B: TVT (n = 31)
|
| Deffieux 2010 | Group A: TVT (n = 75) Group B: TVT‐O (n = 74)
|
| Diab 2012 | Group A: TOT (n = 31) Group B: TVT (n = 32)
All the preoperative parameters were comparable in both groups. The mean operative time was significantly longer and bladder injury was significantly higher in the TVT group. There were no significant difference in cure rates, voiding dysfunction, de novo urgency and reoperation rate. The postoperative groin/thigh pain was higher in the TOT group. |
| El‐Hefnway 2010 | Preliminary results: Group A: TVT: (n = 19) Group B: TOT: (n = 21) At 24 months: Group A: TVT: (n = 45) Group B: TOT: (n = 42)
|
| Elbadry 2014 | Group A: adjustable TOT (n = 48) Group B: TOT: (n = 48)
|
| Enzelsberger 2005 | Group A: TOT (n = 56) Group B: TVT (n = 54)
|
| Freeman 2011 | Group A: Monarc TOT (n = 100) Group B: Gynaecare TVT (n = 92)
|
| Hammoud 2011 | Group A: TVT (n = 60) Group B: TVT‐O (n = 50) Subjective cure: A: 56/60, B: 48/50 |
| Hassan 2013 | Group A: inside‐out TOT (n = 125) Group B: outside‐in TOT (n = 125)
|
| Houwert 2009 | Group A: TVT‐O (n = 93) Group B: Monarc TOT (n = 98)
|
| Jakimiuk 2012 | Group A: TVT (n = 19) Group B: TVT‐O (n = 16)
|
| Juang 2007 | Group A: TVT‐O (n = 47) Group B: TVT‐O plus IS: (n = 49)
|
| Kamel 2009 | A: TVT (n = 60) B: TVT‐O (n = 60)
|
| Karateke 2009 | Group A: TVT (n = 83) Group B: TVT‐O (n = 84)
|
| Kilic 2007 | Group A: TVT (n = 10) Group B: TOT (n = 10)
|
| Kim 2004 | Group A: TVT (n = 32) Group B: SPARC (n = 30)
|
| Kim 2005 | Group A: Monarc (n = 65) Group B: SPARC (n = 65)
|
| Krofta 2010 | Group A: TVTTM (n = 149) Group B: TVT –OTM (n = 151)
|
| Laurikainen 2007 | Group A: TVT‐O (n = 131)
QoL: The scores of the condition specific quality of life questionnaires were significantly lower at the 3 and 5 year follow up compared with pre‐operative scores. This improvements were statistically significant, but with no difference between the groups. 84% of women with pre‐operative moderate and severe frequency and urgency symptoms were cured of these symptoms at the 5 year follow up. |
| Leanza 2009 | Group A: r‐TICT (n = 229; retropubic) Group B: t‐TICT (n = 220; transobturator) Subjective cure: A: 190/215, B: 178/208 |
| Lee 2007 | Group A: TVT (n = 60) Group B: TVT‐O (n = 60)
|
| Lee 2008 | Group A: TVT‐O (n = 50) Group B: TOT (n = 50)
|
| Liapis 2006 | Group A: TVT (n = 46) Group B: TVT‐O (n = 43)
|
| Liapis 2008 | Group A: TVT‐O (n = 61) Group B: Monarc TOT (n = 53)
|
| Lim 2005 | Group A: TVT (n = 61) Group B: IVS (n = 60) Group C: SPARC (n = 61)
|
| Lord 2006 | Group A: TVT (n = 147)
|
| Mansoor 2003 | Group A: TVT‐O (n = 48)
|
| Mehdiyev 2010 | A: TOT (n = 17) B: TVT (n = 15)
|
| Meschia 2006 | Group A: TVT (n = 92)
|
| Meschia 2007 | Group A: TVT‐O (n = 117) Group B: TVT (n = 114)
|
| Naumann 2006 | Group A: TVT (n = 123) Group B: LIFT (n = 125)
|
| Nerli 2009 | Group A: TVT (n = 18) Group B: TOT (n = 18)
|
| Nyyssonen 2014 | Group A: TOT (n = 50) Group B: TVT (n = 50)
|
| Okulu 2013 | Group A: Vypro mesh: (n = 48; multifilament) Group B: Ultrapro mesh: (n = 48; monofilament + biological combined mesh) Group C: Prolene light mesh: (n = 48; monofilament)
|
| Oliveira 2006 | Group A: TVT (n = 17)
|
| Palomba 2008 | Trial terminated. |
| Paparella 2010 | Group A: synthetic UretexTO® (n = 34) Group B: biological PelviLaceTO® (n‐36)
|
| Park 2012 | Group A: TVT‐O (n = 39) Group B: TOT Monarc (n = 35)
|
| Peattie 2006 | No published data. |
| Porena 2007 | Group A: TVT (n = 70) Group B: TOT (n = 75)
|
| Rechberger 2003 | Group A: TVT (n = 50) Group B: IVS (n = 50)
|
| Rechberger 2009 | Group A: retropubic (IVS‐02; n = 269) Group B: transobturator (IVS‐04; n = 268)
|
| Rechberger 2011 | Group A: TOT (n = 232) Group B: TOT with fixation (n = 231)
|
| Richter 2010 | Group A: retropubic sling (TVT; n = 298) Group B: transobturator tapes (TVT‐O, and TOT Monarc; n = 299) (Group C (?): TVT‐O (inside‐out) ‐ separate data not provided) (Group D (?): TOT (Monarch, outside‐in) ‐ separate data not provided) Objective cure at 1 year: A: 232/280 (80.8%), B: 233/285 (77.7%) Subjective cure at 1 year: A: 181/280 (62.2%), B: 163/285 (55.8%) Secondary outcomes:
PISQ‐12 (Prolapse / urinary incontinence sexual questionnaire): Analysis of results for group A and group B combined showed significant improvement in sexual function in both groups with a mean PISQ‐12 score increase from 32.8+/‐7.1 at baseline to 37.3+/‐ 6 at 24 months. These changes are >0.6 SD units, which reflects “medium” improvement in the PISQ‐12 score after surgery. Compared with women with successful surgery, women who experienced surgical failure, regardless of assigned type of surgery, reported worse adjusted sexual function scores at all postoperative time points. Improvement in PISQ‐12 scores was consistent with change in the 3 specific items from the sexual function measure of interest: (1) the experience of pain during sexual activity, (2) UI during sexual activity, and (3) fear of incontinence during sexual activities. Pain with intercourse was reported by 153 of 406 of sexually active women (38%) at baseline and decreased to 27% at 12 months after surgery (P.003). Self‐reported UI and the fear of incontinence occurring during sexual activity also significantly improved by 12 months after surgery, regardless of sling route. To specifically investigate the association of synthetic mesh slings on dyspareunia, we repeated the analysis on the 247 women who underwent MUS only (no concurrent procedures) and who completed baseline and 12‐month assessments. In this subset of women, dyspareunia decreased from 57% at baseline to 43% at 12 months after surgery (P .03). 5‐year data provided, but without numbers in each group, so could not be used for meta‐analysis |
| Riva 2006 | Group A: TOT (n = 65) Group B: TVT (n = 66) |
| Ross 2009 | Group A: TVT (n = 105) Group B: TOT (n = 94)
|
| Salem 2014 | Group A: TOT (n = 37) Group B: TVT (n = 39) No significant difference was noticed between the two groups as regard the mean operative time, perioperative complications, intraoperative blood loss, hospital stay, and time to return to normal activities. The mean of abdominal leak point pressure and urethral closure pressure showed marked and maintained improvement for 5 years later in group I whereas in group II, they showed marked and maintained improvement for only one year then shows significant decline in comparison with group I. As regard the mean of objective SEAPI score shows marked decrease (improvement) in both groups and this was maintained for the five years in group I but in group II, it increased after one year later. No usable data provided. |
| Scheiner 2012 | Group A: TVT (n = 80) Group B: TOT outside‐in approach (Monarc; n = 40) Group C: TVT‐O inside‐out approach (Gynecare; n = 40)
|
| Schierlitz 2008 | Group A: TVT (n = 81) Group B: Monarc sling (n = 82)
|
| Tanuri 2010 | Group A: Safyre VS retropubic tape (n = 10) Group B: Safyre T transobturator tape (n = 20)
|
| Tarcan 2011 | Group A: TVT (n = 27) Group B: TOT (n = 27) 12‐month follow‐up assessed:
2 year follow‐up assessed:
|
| Teo 2011 | Group A: TVT (n = 66) Group B: TVT‐O (n = 61)
|
| Tommaselli 2012 | Group A: TVT‐O (n = 48) Group B: modified TVT‐O (n = 24)
|
| Tseng 2005 | Group A: SPARC (n = 31)
|
| Ugurlucan 2013 | Group A: biological PELVILACE TO (n = 50) Group B: synthetic TOT ALIGN ®TO (n = 50)
|
| van Leijsen 2013 | Group A: RPR (n = 33) Group B: TOT (n = 90)
|
| Wang 2006 | Group A: Monarc (n = 31) Group B: SPARC (n = 29)
|
| Wang 2008 | Group A: TVT (n = 35) Group B: TVT‐O (n = 34)
|
| Wang 2009 | Group A: TVT (n = 154) Group B: TVT‐O (n = 146)
|
| Wang 2010 | Group A: TVT (n = 70) Group B: TOT (n = 70)
|
| Wang 2011 | Group A: TVT (n = 32) Group B: TVT‐O (n = 36)
|
| Zhang 2011 | Group A: TVT‐O (n = 76) Group B: modified TVT‐O (n = 80)
|
| Zullo 2007 | Group A: TVT (n = 35) Group B: TVT‐O (n = 37)
|
Abbreviations
BFLUTS: Bristol lower urinary tract symptoms questionnaires
BMI: body‐mass index
DO: detrusor overactivity
DUP: distal urethral polypropylene sling
EQOL‐5D: Euro Quality of life ‐5 Dimension
hr: hour/s
HRT: hormone replacement therapy
ICIQ: International Consultation on Incontinence questionnaire
ICIQ‐FLUTS: International Consultation on Incontinence questionnaire ‐ female lower urinary tract symptoms
ICIQ‐ LUTSquol: International Consultation on Incontinence questionnaire ‐ lower urinary tract quality of life questionnaire
ICIQ‐SF: International Consultation on Incontinence questionnaire short form
ICIQ‐SF15: International Consultation on Incontinence questionnaire short form 15
IIQ: Incontinence Impact questionnaire
ICS: International Continence Society
I‐QoL: Incontinence Quality of Life questionnaire
ISD: intrinsic sphincter deficiency
IVS: intravaginal slingoplasty
KHQ: King's Health questionnaireMUI: mixed urinary incontinence
MUCP: Maximum urethral closure pressure
MUI: mixed urinary incontinence
OAB: overactive bladder
PGI‐I: Patient Global Impression of Improvment
PGI‐S: Patient Global Impression of Severity
PISQ‐12: pelvic organ prolapse/urinary incontinence sexual questionnaire
POP: pelvic organ prolapse
POP‐Q: pelvic organ prolapse quantification
POP‐Q ICS: pelvic organ prolapse quantification International Continence Society
PVR: post void residual
RCT: randomized controlled trial
RPR: retropubic route
QoL: quality of life
QRCT: quasi‐randomised trial
SEAPI‐QMM: Stress related leak, Empyting ability, Anatomy, Protection, Inhibition‐Quality of life, Mobility and Mental status incontinence classification system
SD: standard deviation
SIS: Single incision sling
SPARC: suprapubic arc (procedure)
SUI: stress urinary incontinence
TOR: transobturator
TOT: transobturator tape
TOT‐ARIS: transobturator tape‐ARIS
TVT: tension‐free vaginal tape
TVT‐O: transobturator tension‐free vaginal tape
UDI: Urinary Distress Impact questionnaire
UDI‐6: Urinary Distress Impact questionnaire short form
UDS: urodynamics study
UI: urinary incontinence
UISS: urinary incontinence severity score
USI: urodynamic stress incontinence
USS: ultrasound
UTI: urinary tract infection
UUI: urgency urinary incontinence
VAS: visual analogue scale
VLPP: Valsalval leak point pressure
Discussion
Summary of main results
1. Transobturator (TOR) versus retropubic route (RPR)
Comparison of the transobturator (TOR) versus retropubic route (RPR) was addressed by 55 trials that included 8652 women. Thirty‐six of these trials (5514 women) contributed data to the primary outcome of subjective cure, which showed that in the short term there was no difference between TOR and RPR. Only six of these 53 trials reported medium‐ or long‐term data, again with relatively small numbers of women showing no significant difference in symptomatic cure. These small numbers limit the judgements that can be made about cure rates in the longer term for both the efficacy of individual tapes, or for comparison of the route of tape insertion. There was potential for at least 22 of these trials to have published either medium‐ or longer‐term outcomes, given their dates of publication. Similarly, objective cure rates showed no significant difference between the two routes.
Evidence from 40 trials (6372 women) showed a 30 fold percentage increase in the rate of bladder perforation with the RPR approach compared to the TOR approach. In practice, for this reason, some clinicians favour the TOR for patients at higher risk of bladder/urethral perforation, for example, those who have had previous pelvic or incontinence surgery. Similarly, 37 trials (6217 women) that assessed postoperative voiding dysfunction (POVD) showed this adverse outcome to be significantly less frequent when the TOR was employed. However, the reported sequale for both of these outcomes is usually of short duration.
Thirty‐one trials (4743 women) that assessed vaginal tape erosion showed no significant difference when either route was used. More women experienced groin pain in the TOR group than in the RPR group. This groin pain was usually of short duration and resolved within eight weeks in most cases. The occurrence of suprapubic pain following an RPR procedure was poorly reported. This was more common in the RPR group; however, when data was provided, only a minority of women suffered this symptom and for a short period of time.
Overall mid‐urethral slings are a highly effective treatment for stress urinary incontinence (SUI). In the short term there is equivalence in the efficacy between the two routes, and this persists into the medium and longer term, though the data for this is somewhat limited by small numbers. There is some evidence that suggests women are more likely to require repeat incontinence surgery in the longer term with the TOR, but this requires cautious interpretation, as there are extremely small numbers. There is an equal improvement in the overall quality of life of women for both routes. Sexual function improved in both groups as a result of the surgery, most probably from reduction in coital incontinence, with no significant difference in sexual function between the two groups. The only economic analysis performed in one trial showed favoured TOR.
2. Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach
Five trials with 636 women compared the retropubic bottom‐to‐top with the retropubic top‐to‐bottom approach. These showed that passage of the tape through the retropubic route in a bottom‐to‐top path (e.g. TVTTM) was more effective than passage in a top‐to‐bottom path (e.g. SPARCTM), and resulted in fewer intra and postoperative adverse events.
3. Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach
Ten trials with 1199 women compared the obturator medial‐to‐lateral approach with the obturator lateral‐to‐medial approach. Evidence from the ten trials, two of which reported medium‐term data, showed no difference between the two approaches with respect to most outcomes measured. The only exceptions were voiding dysfunction, where higher rates were reported in the medial‐to‐lateral group, and vaginal perforation, which had higher rates in the lateral‐to‐medial group. Despite this, there was no resultant increase in the rate of tape erosion. It is, therefore, not unreasonable to exercise operator preference when deciding which of these two approaches to adopt. Noteably each route improved quality of life and sexual function postoperatively.
4. One method of mid‐urethral tape insertion versus another method, same route
Ten trials with 1569 women compared one method of mid‐urethral tape insertion with another using using the same route. Despite several design or procedural modifications to tapes traversing the same route, there was no difference in the efficacy, surgical outcomes or occurrence of adverse events.
5. One type of tape material versus another
Four trials with 505 women compared monofilament tapes with multifilament tapes. There was no statistical difference in physician‐observed cure rates or patient‐reported cure between the groups. There was no significant difference in the rate of vaginal tape erosion.
Overall completeness and applicability of evidence
Many of the trials contributing to this review did provide evidence regarding the primary outcome, which was to determine the effectiveness of mid‐urethral sling operations in the treatment of urinary incontinence. They confirm that mid‐urethral sling operations for SUI are an effective surgical treatment available in current practice. A major limitation was the variable quality of many of the trials.
We did not attempt to analyse the data by subgroups according to the clinical characteristics of the women, such as symptoms of SUI, urodynamic stress incontinence, diagnosis of intrinsic urethral sphincter deficiency or urethral hypermobility, obesity, previous incontinence surgery, presence or absence of prolapse, anaesthesia used, or experience of the surgeon. In fact the majority of trials did not describe these characteristics of the women.
Economic implications both for the women personally and the cost to the health service were poorly investigated by many trials. Similarly, quality of life was poorly reported using a variety of instruments that precluded meta‐analysis, although these outcomes are of utmost importance to women and decision makers.
Complications
Major complications such as nerve, bowel or major vascular injuries, pelvic haematoma, necrotizing fasciitis, ischiorectal abscess and death are uncommon and unlikely to be picked up by small randomised controlled trials (RCTs). There is potential to determine a more accurate incidence from large national registries and voluntary reporting registries or databases for reporting complications, such as the United States Food and Drug Administration's (FDA) manufacturer and user facility device experience (MAUDE). One must bear in mind, though, the limitations of this method. Several of these registries have reported their findings (Collinet 2008; Dyrkorn 2010; Kuuva 2002; Koops 2005; Tamussino 2001; Tamussino 2007; Tincello 2011).
Retropubic tapes
From the above list of registries, for tension‐free vaginal tape the number of procedures reported ranged from 809 to 4281, and there were found to be low rates of major complications.
-
Bladder perforation occurred in 2.7% to 3.9% of cases.
-
Reoperation rates relating to tape insertion or postoperative voiding dysfunction (POVD) ranged from 1.6% to 2.4%.
-
Urinary retention rate was 1.6%.
-
Pelvic haematoma occurred in 0.7% to 1.9% of women.
-
Infection rate was 0.7%.
-
Vaginal tape erosion/extrusion rate was 1.5%.
-
Groin pain occurred in 0.4% of women.
These rates are largely of the same order as those reported in the trials included in this review. There were also a few cases of major visceral injuries such as bowel and urethral injuries.
Transobturator tapes
Registries of transobturator tapes reported much lower rates of complications.
-
Bladder perforation occurred in 0.4% of cases.
-
Reoperation rates relating to tape insertion ranged from 0.8% to 2.2%.
-
Urinary retention rate was 0.5%.
-
Pelvic haematoma occurred in 0.5% of women.
-
Infection rate was 0.6%.
-
Vaginal tape erosion/extrusion rate was 0.4%.
-
Groin pain occurred in 1.6% of women.
The FDA received 1876 reports of complications associated with the use of slings for SUI in the period between 1 January 2008 to 30 September 2011. The most common complications reported were pain, vaginal tape erosion (exposure, extrusion or protrusion), infection, urinary problems, recurrent incontinence, pain during sexual intercourse (dyspareunia), bleeding, organ perforation, neuro‐muscular problems and vaginal scarring. Many of these complications required further medical intervention, and sometimes required surgical treatment or hospitalisation, or both. With the exception of tape erosion, the above complications were also found to occur following non‐mesh surgical repairs for SUI. It should be borne in mind that this sort of reporting system is a passive surveillance system limited by the inclusion of the potential submission of incomplete or inaccurate data, under‐reporting of events, lack of denominator data (number of tapes), and the lack of report timeliness.
It should be noted that the latest FDA white paper and safety communications on meshes released in 2011 ‐ unlike the previous 2008 release (FDA 2008) ‐ relates to ongoing concern with mesh used to treat pelvic organ prolapse (POP) and not the small strip of mesh/tape/sling used to treat SUI (FDA 2011a; FDA 2011b). In fact the FDA states that the safety and effectiveness of mid‐urethral slings is well established in clinical trials with 1‐year follow‐up (FDA 2013).
Equally, because of the increasing numbers of adverse events and patient concerns reported, in 2012 the Medicines and Healthcare Products and Regulatory Agency (MHRA) in Europe published a commissioned report on the most frequently reported adverse events associated with different meshes/tapes/slings (MHRA 2012). The report showed that for the treatment of SUI the rate of vaginal tape erosion was low, at between 1.1% to 2.5%. Even in a selected cohort of women presenting primarily with adverse events of mesh, those with mid‐urethral sling were significantly less likely to present with mesh erosions than those who had mesh for POP repair. Presentation of mesh erosion following SUI treatment is less severe, and less likely to require surgical treatment under general anaesthesia than erosion following mesh insertion for POP repair. This relates to complication classification severity grade 4 (Abbott 2014; Strasberg 2009).
In their 2014 report, the MHRA concluded that from the review of the information available, there appeared to be no evidence that vaginal mesh implants for SUI are unsafe, nor was there evidence to justify MHRA taking enforcement action to take them off the market, or remove them from use. The report concluded that the overall benefit outweighed the relatively low rate of complications (MHRA 2014).
Although the number of adverse events was generally low and they were rarely serious, it is recognised that the ability of RCTs to identify rarer adverse effects is poor. With the increasing popularity of MUS procedures the occurrence of complications in the short term is well established, but in general these are easily treated or resolve spontaneously. However, because few trialists have carried out long‐term follow‐up, there is very little information about whether there is a hidden cache of serious adverse effects that might be set against the benefits of curing incontinence.
Longer‐term outcomes after MUS
Observational studies of MUS show data confirming effectiveness in the long term with some data that cover 15 to 17 years (Aigmueller 2011; Athanasiou 2014; Heinonen 2013; Nilsson 2013; Serati 2012; Serati 2013; Svenningsen 2013a; Svenningsen 2013b). These trials of MUS, like similar observational studies for open colposuspension, show a decline in effectiveness that is time‐dependent, and also reveal high rates of de novo urgency symptoms (15%) and voiding difficulties (23%). It is difficult to elucidate the reasons for these long‐term symptoms, but they could be age related, or due to new pathology, or a true consequence of the surgery. Nevertheless, they emphasise the need for longer‐term data from RCTs to help counsel women appropriately.
With regard to long‐term data from RCTs, there is a paucity of trials that reported longer‐term outcomes and most long‐term data reported for both open colposuspension and MUS are for five to six years. If evidence from RCTs mirrors that from observational studies, we will not only require the many RCTs that have been published for MUS to report their longer‐term data, but will in fact need to follow these women up for at least 10 to 15 years. This would allow us to discover whether there is a time‐dependent decline in effectiveness, and enable us to elucidate the development in the long term of new adverse effects.
Comparisons with other methods of continence surgery
'Gold standard' surgical treatment for stress urinary incontinence (SUI)
Open abdominal retropubic colposuspension used to be considered the gold standard treatment for SUI. It is noteworthy that there are no randomised controlled trials of open colposuspension versus no treatment. Two small trials that compared open colposuspension with conservative treatment were unreliable because of very small numbers of participant and a high risk of bias (Lapitan 2012). Equaliy the evidence for MUS versus no treatment or conservative treatment is limited and we will be addressing this in a future Cochrane review.
Our initial review showed the effectiveness of MUS in the short term and, as time has moved on, it was hoped that with reports of long‐term data it would become clear whether long‐term efficacy of MUS could be compared with that of open retropubic colposuspension. A Cochrane review of open retropubic colposuspension identified 15 RCTs that compared the mid‐urethral sling operations (12 RPR and three TOR) with colposuspension (Lapitan 2012). This review concluded that there was no significant difference in incontinence rates between the two procedures for all time periods assessed. Both procedures led to improvement in the quality of life of women. While some complications, such as bladder perforation, were reported more with MUS, the numbers were small. Other complications such as POVD, which were reported to be higher with MUS, were influenced by a large trial that reported no risk of voiding difficulties at all after colposuspension, but consistent data from TVT trials showed no significant difference in the risk of voiding dysfunction between MUS and colposuspension. MUS had a shorter operating time, length of hospital stay and cost. Only one RCT that compared MUS with open colposuspension has reported results for a five‐year follow‐up, and it failed to detect significant difference between the success rates of MUS and colposuspension. It also showed that the effect on cure of incontinence and improvement in quality of life was maintained for both procedures at five years (Ward 2008).
Observational data for open colposuspension with follow‐up of 10 to 20 years show high rates of effectiveness in the long term (Alcalay 1995; Kjolhede 2005; Brubaker 2012). This long‐term cure is shown to be time‐dependent with cure rates plateauing at about 69% at 10 to 12 years. In addition some reports show continence rates of only 44% at 14 years, with high rates of voiding difficulties (of 36%) at 14‐year follow‐up.
Mid‐urethral sling operations versus traditional slings
Historically, traditional suburethral sling procedures were used for women who had recurrent stress incontinence (after a previous failed continence operation). However, the review did not report the results separately for women with new or recurrent incontinence (Rehman 2011). These procedures were designed to restore normal urethrovesical junction support by mechanical compression or kinking of the proximal urethra.
Minimally invasive synthetic suburethral slings appeared to be as effective as traditional suburethral slings in short‐term incontinence rates (RR 0.97; 95% CI 0.78 to 1.20), although the confidence interval is compatible with minimally invasive slings being 20% better or 12% worse. The operating time and length of stay were also significantly shorter with minimally invasive synthetic suburethral sling operations, and women had fewer perioperative complications and less detrusor overactivity.
Mid‐urethral sling operations versus open retropubic colposuspension
Although 14 RCTs were found that compared TVT operations with colposuspension (Lapitan 2012), data from five of them showed no clear differences in the short‐ or medium‐term chance of incontinence compared with open colposuspension. While there were more complications after the sling operations, the numbers were small.
Mid‐urethral sling operations versus laparoscopic colposuspension
Another Cochrane review identified eight trials that compared mid‐urethral sling operations to laparoscopic colposuspension (Dean 2006). Overall, the review showed that the subjective cure rates were similar for both of these minimal access techniques in the short term, while operation times were shorter for the slings. Long‐term data are lacking, however.
Mid‐urethral sling operations versus single incision slings
Single‐incision slings compared with retropubic mid‐urethral slings
Women were twice as likely to be incontinent after a single‐incision sling as after a retropubic TVT (RR 2.08, 95% CI 1.04 to 4.14; Nambiar 2014), although the surgery took less time to perform. However, this finding mostly related to one type of single‐incision sling (TVT‐Secur), which has now been withdrawn from the market due to this lack of efficacy.
Single‐incision slings compared with transobturator mid‐urethral slings
Women were also twice as likely to be incontinent after a single‐incision sling procedure as after a transobturator sling procedure (RR 1.91, 95% CI 1.53 to 2.39; Nambiar 2014). In addition, they were more likely to need a further operation for complications or repeat surgery for their incontinence. However, the risks of postoperative pain and long‐term pain were slightly higher with transobturator slings.
Mid‐urethral sling operations versus anterior repair
To date, no trials have been identified that compared the original operation for SUI, anterior repair (with urethral buttressing sutures, or Kelly sutures) directly to mid‐urethral slings (Glazener 2001). However, in the current climate of concern about adverse effects from the use of synthetic mesh or tape materials, perhaps it is time to reassess the value of this operation, not least because of its additional role in the management of prolapse.
Quality of the evidence
We judged the quality of evidence using the GRADE classification as moderate for the majority of outcomes. The remaining outcomes assessed were low level evidence. The main reason for the decrease in the quality of evidence for many outcomes was a high risk of bias where allocation concealment or random sequence generation were deemed uncertain. Imprecision of effects estimates also contributed to the variable quality of evidence in some outcomes.
In the main comparison between TOR and RPR, the quality of evidence for most outcomes was moderate. The downgrade from high quality to moderate quality evidence was mainly because of a small proportion of trials in which there was a high risk of bias from either study design or implementation, which then reduced our confidence in the estimates of effects.
Potential biases in the review process
GRADE‐specific outcomes were selected at the time of the original review. These have been modified for this update. There is potential for introduction of bias, as ideally these GRADE‐specific outcomes should have been selected at the time of the protocol, and there would have been consistency between the outcomes selected in the original review and in the update.
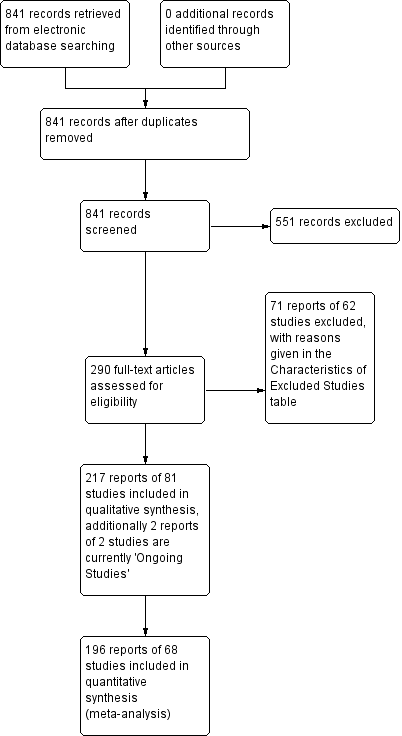
PRISMA study flow diagram

Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgments about each risk of bias item for each included study.

Funnel plot of comparison: 1 Transobturator (TOR) versus retropubic (RPR) route, outcome: 1.1 Subjective cure (short term, ≤ 1 year)
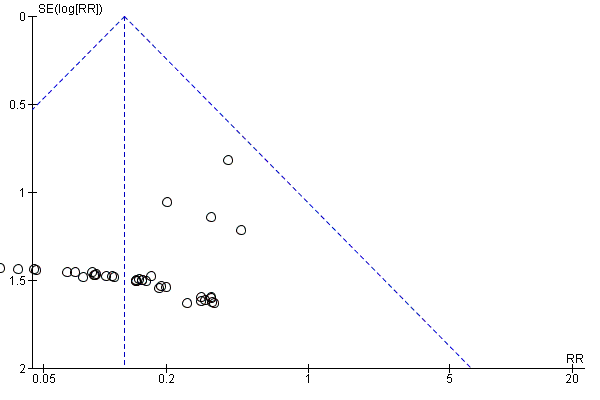
Funnel plot of comparison: 1 Transobturator (TOR) versus retropubic (RPR) route, outcome: 1.16 Bladder or urethral perforation
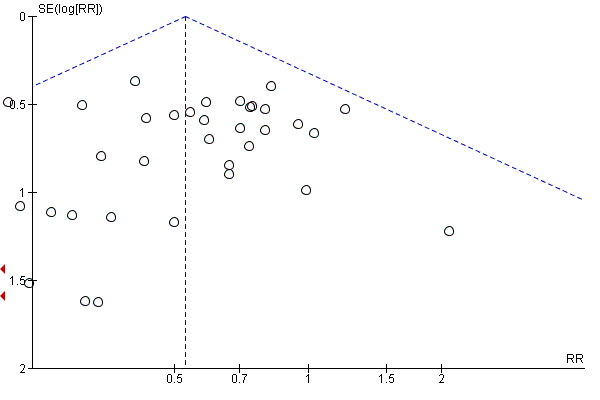
Funnel plot of comparison: 1 Transobturator (TOR) versus retropubic (RPR) route, outcome: 1.17 Voiding dysfunction

Funnel plot of comparison: 1 Transobturator (TOR) versus retropubic (RPR) route, outcome: 1.22 Vaginal tape erosion

Funnel plot of comparison: 1 Transobturator (TOR) versus retropubic (RPR) route, outcome: 1.24 Groin pain

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 1 Subjective cure (short term, ≤ 1 year).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 2 Subjective cure and improvement (short term, ≤ 1 year).
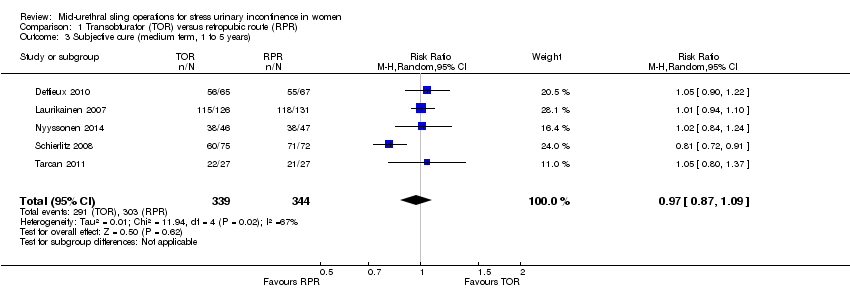
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 3 Subjective cure (medium term, 1 to 5 years).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 4 Subjective cure (long term, > 5 years).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 5 Subjective cure and improvement (long term, > 5 years).
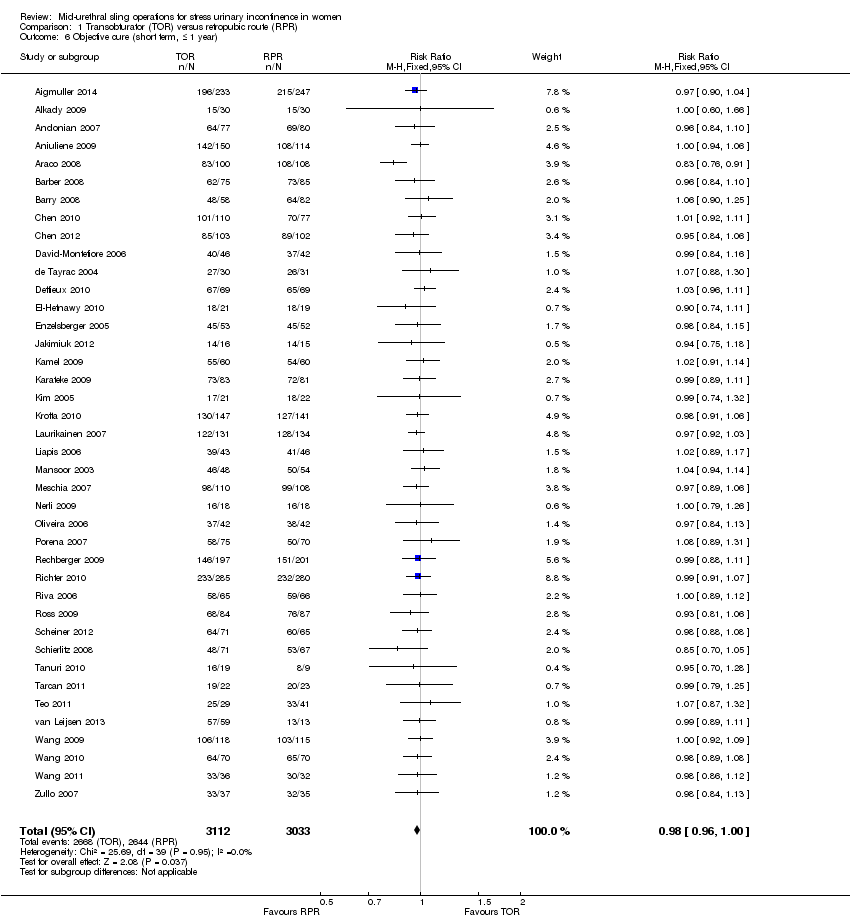
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 6 Objective cure (short term, ≤ 1 year).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 7 Objective cure and improvement (short term, ≤ 1 year).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 8 Objective cure (medium term, 1 to 5 years).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 9 Objective cure (long term, > 5 years).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 10 Operative time (minutes).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 11 Operative blood loss (ml).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 12 Length of hospital stay (days).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 13 Time to return to normal activity level (weeks).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 14 Perioperative complications.

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 15 Major vascular or visceral injury.

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 16 Bladder or urethral perforation.

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 17 Voiding dysfunction.

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 18 De novo urgency or urgency incontinence (short term, ≤ 1 year).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 19 De novo urgency or urgency incontinence (medium term, 1 to 5 years).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 20 De novo urgency or urgency incontinence (long term, > 5 years).

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 21 Detrusor overactivity.

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 22 Vaginal tape erosion.

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 23 Bladder/urethral erosion.
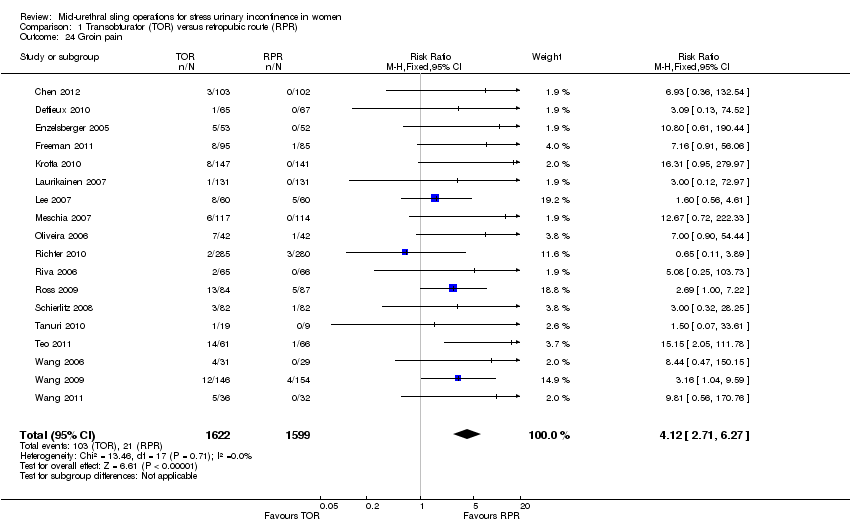
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 24 Groin pain.
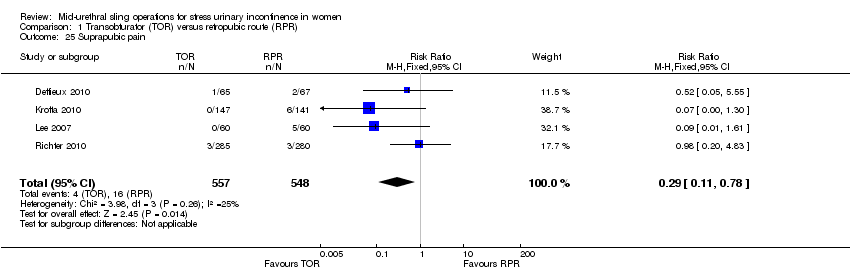
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 25 Suprapubic pain.

Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 26 Repeat incontinence surgery (short term, ≤ 1 year).
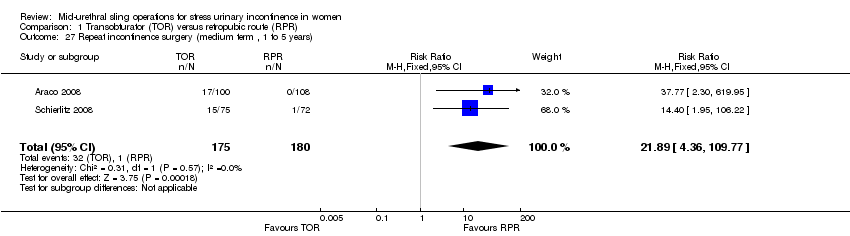
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 27 Repeat incontinence surgery (medium term , 1 to 5 years).
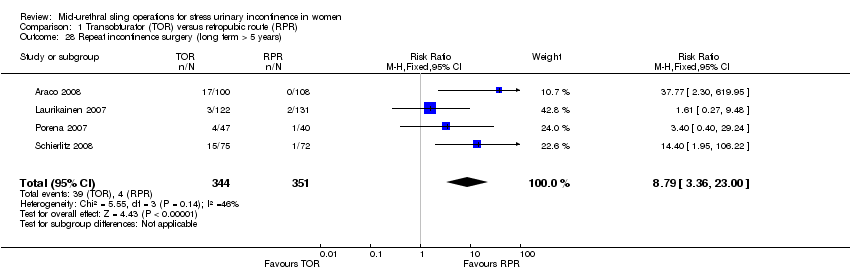
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 28 Repeat incontinence surgery (long term > 5 years).

Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 1 Subjective cure (short term, ≤ 1 year).

Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 2 Objective cure (short term, ≤ 1 year).

Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 3 Operative time (minutes).
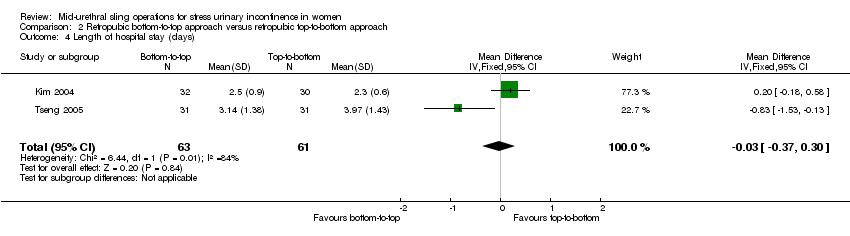
Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 4 Length of hospital stay (days).
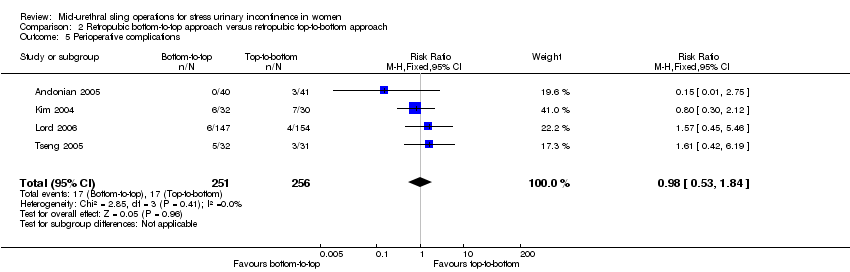
Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 5 Perioperative complications.

Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 6 Bladder or urethral perforation.

Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 7 Voiding dysfunction.

Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 8 De novo urgency or urgency incontinence.
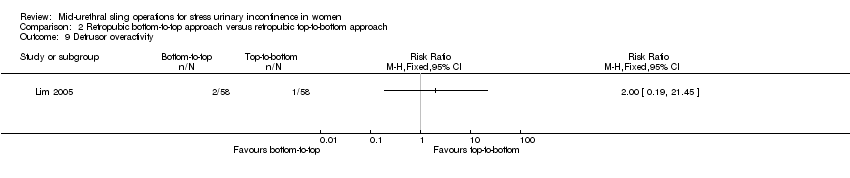
Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 9 Detrusor overactivity.

Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 10 Vaginal tape erosion.

Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 11 QoL specific.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 1 Subjective cure (short term, ≤ 1 year).

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 2 Subjective cure and improvement (short term, ≤ 1 year).
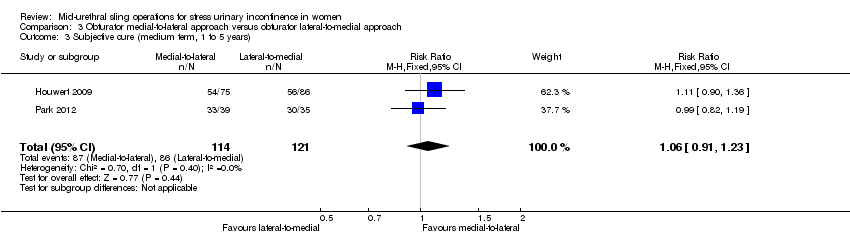
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 3 Subjective cure (medium term, 1 to 5 years).
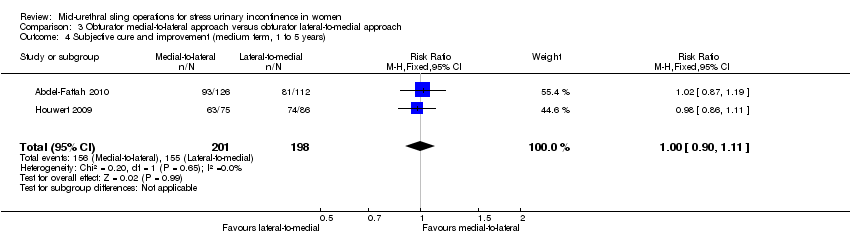
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 4 Subjective cure and improvement (medium term, 1 to 5 years).

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 5 Objective cure (short term, ≤ 1 year).

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 6 Objective cure and improvement (short term, ≤ 1 year).

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 7 Operative time (minutes).

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 8 Operative blood loss (ml).

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 9 Length of hospital stay (days).

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 10 Time to return to normal activity level.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 11 Perioperative complications.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 12 Major vascular or visceral injury.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 13 Vaginal perforation/injury.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 14 Bladder or urethral perforation.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 15 Voiding dysfunction.
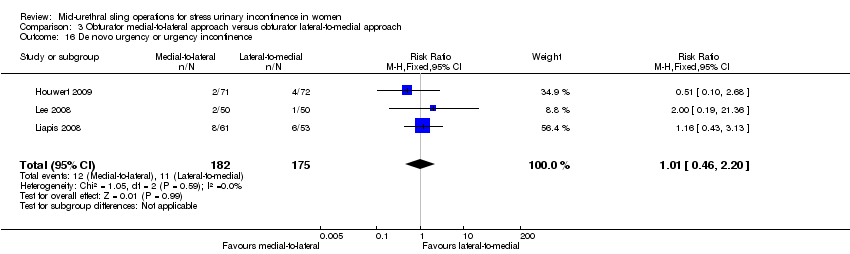
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 16 De novo urgency or urgency incontinence.
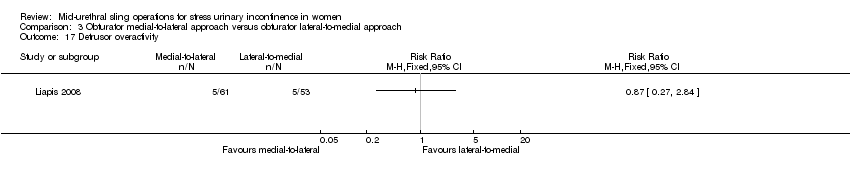
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 17 Detrusor overactivity.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 18 Vaginal tape erosion.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 19 Groin/thigh pain.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 20 Repeat incontinence surgery.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 21 QoL specific.

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 1 Subjective cure (short term, up to 1 year).

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 2 Subjective cure and improvement (short term, up to 1 year).
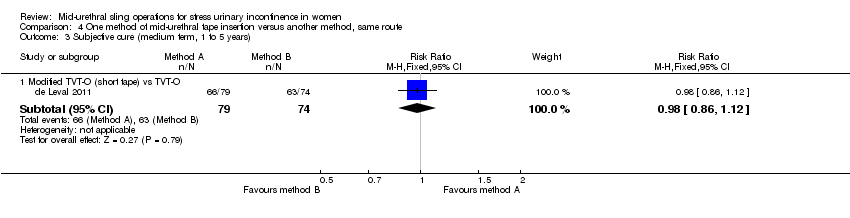
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 3 Subjective cure (medium term, 1 to 5 years).

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 4 Objective cure (medium term, 1 to 5 years).

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 5 Objective cure (short term, ≤ 1 year).
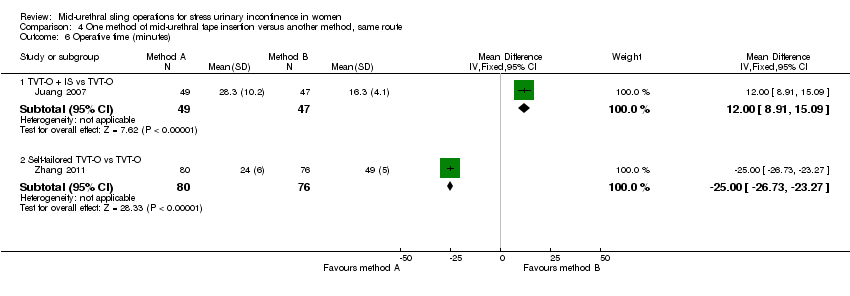
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 6 Operative time (minutes).

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 7 Operative blood loss (ml).
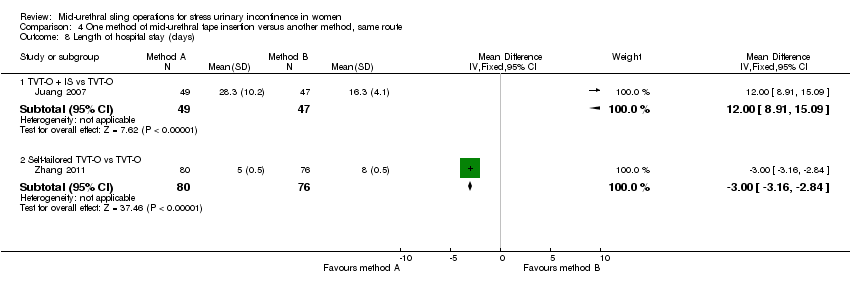
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 8 Length of hospital stay (days).

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 9 Perioperative complications.

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 10 Major vascular or visceral injury.

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 11 Bladder/urethral perforation.

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 12 Voiding dysfunction.

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 13 De novo urgency or urgency incontinence.
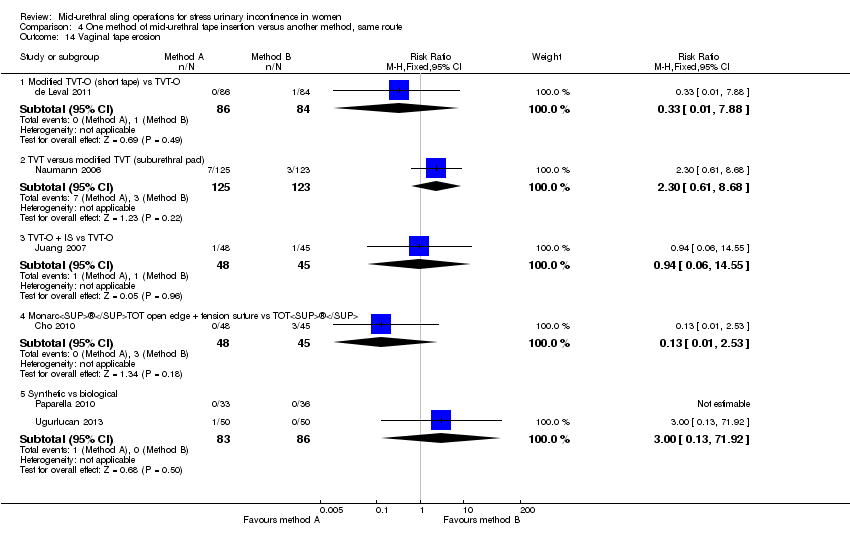
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 14 Vaginal tape erosion.

Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 15 Bladder/urethral erosion.
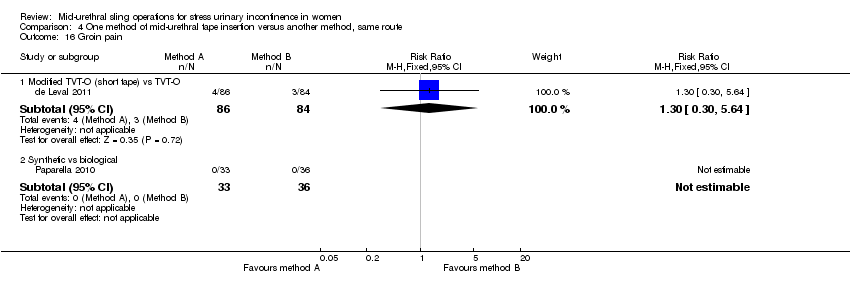
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 16 Groin pain.

Comparison 5 One type of tape material versus another, Outcome 1 Subjective cure (short term, ≤ 1 year).
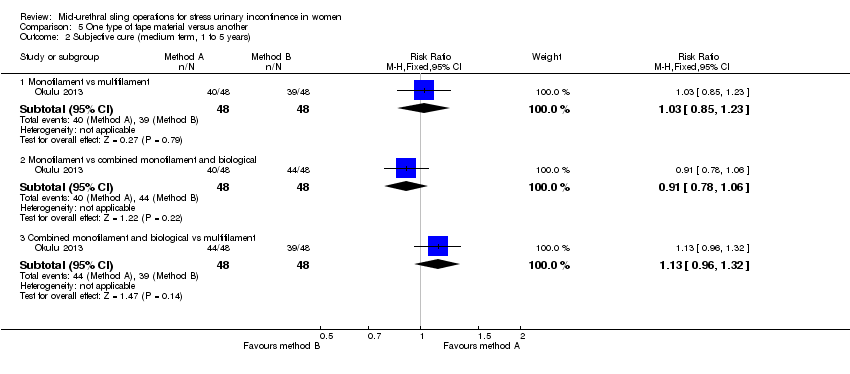
Comparison 5 One type of tape material versus another, Outcome 2 Subjective cure (medium term, 1 to 5 years).
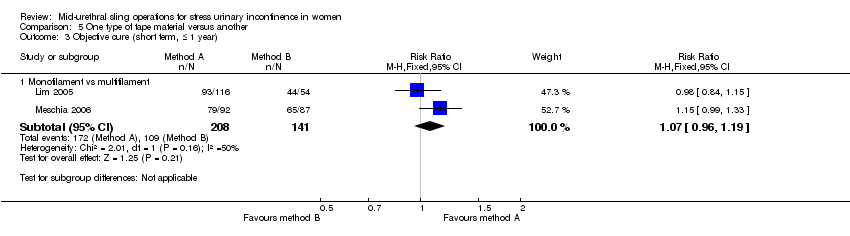
Comparison 5 One type of tape material versus another, Outcome 3 Objective cure (short term, ≤ 1 year).

Comparison 5 One type of tape material versus another, Outcome 4 Operative time (minutes).

Comparison 5 One type of tape material versus another, Outcome 5 Length of hospital stay (days).

Comparison 5 One type of tape material versus another, Outcome 6 Perioperative complications.

Comparison 5 One type of tape material versus another, Outcome 7 Major vascular or visceral injury.

Comparison 5 One type of tape material versus another, Outcome 8 Bladder or urethral perforation.
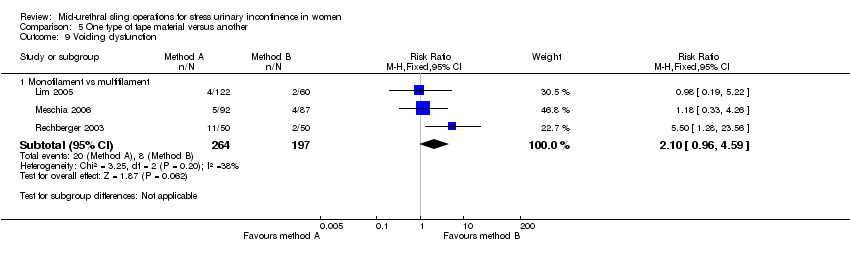
Comparison 5 One type of tape material versus another, Outcome 9 Voiding dysfunction.

Comparison 5 One type of tape material versus another, Outcome 10 De novo urgency or urgency incontinence.

Comparison 5 One type of tape material versus another, Outcome 11 Detrusor overactivity.
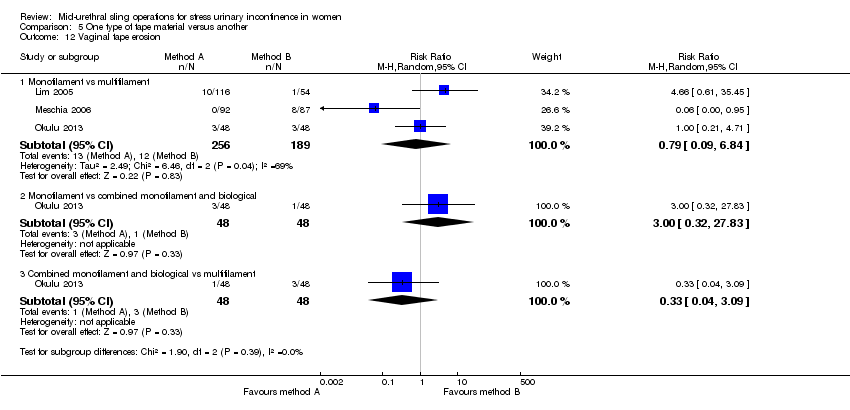
Comparison 5 One type of tape material versus another, Outcome 12 Vaginal tape erosion.

Comparison 5 One type of tape material versus another, Outcome 13 QoL specific (ICIQ).
| Transobturator (TOR) compared to retropubic (RPR) route for stress urinary incontinence in women | ||||||
| Patient or population: women with stress urinary incontinence | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Retropubic (RPR) route | Transobturator (TOR) | |||||
| Subjective cure (Short term < 1 year) | Study population | RR 0.98 | 5514 | ⊕⊕⊕⊝ | ||
| 844 per 1000 | 827 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 833 per 1000 | 816 per 1000 | |||||
| Subjective cure (medium term, 1 to 5 years) | Study population | RR 0.97 | 683 | ⊕⊕⊝⊝ | ||
| 881 per 1000 | 854 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 869 per 1000 | 843 per 1000 | |||||
| Subjective cure (long term, > 5 years) | Study population | RR 0.95 | 714 | ⊕⊕⊕⊝ | ||
| 707 per 1000 | 671 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 843 per 1000 | 801 per 1000 | |||||
| Bladder or urethral perforation | Study population | RR 0.13 | 6372 | ⊕⊕⊕⊝ | ||
| 49 per 1000 | 6 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 25 per 1000 | 3 per 1000 | |||||
| Voiding dysfunction (short and medium term, up to 5 years) | Study population | RR 0.53 | 6217 | ⊕⊕⊕⊝ | ||
| 72 per 1000 | 38 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 55 per 1000 | 29 per 1000 | |||||
| De novo urgency or urgency incontinence (short term, up to 12 months) | Study population | RR 0.98 | 4923 | ⊕⊕⊕⊝ | ||
| 82 per 1000 | 80 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 83 per 1000 | 81 per 1000 | |||||
| Groin pain | Study population | RR 4.62 | 3226 | ⊕⊕⊕⊝ | ||
| 14 per 1000 | 66 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 45 per 1000 | 208 per 1000 | |||||
| Suprapubic pain | Study population | RR 0.29 | 1105 | ⊕⊕⊕⊝ | ||
| 29 per 1000 | 8 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 18 per 1000 | 5 per 1000 | |||||
| Vaginal tape erosion (short and medium term, up to 5 years) | Study population | RR 1.13 | 4743 | ⊕⊕⊕⊝ | ||
| 20 per 1000 | 22 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 21 per 1000 | 24 per 1000 | |||||
| Repeat incontinence surgery (short term, within 12 months) | Study population | RR 1.64 | 1402 | ⊕⊕⊕⊝ | ||
| 19 per 1000 | 31 per 1000 | |||||
| mean control group across studies | ||||||
| 24 per 1000 | 39 per 1000 | |||||
| Repeat incontinence surgery (long term, > 5 years) | Study population | RR 8.79 | 695 | ⊕⊕⊝⊝ | ||
| 11 per 1000 | 100 per 1000 | |||||
| Mean control group across studies | ||||||
| 67 per 1000 | 589 per 1000 | |||||
| Cost effectiveness of intervention | An economic analysis was performed in only one RCT. This showed that over a 12‐month follow‐up period there was cost saving with TOR of CAD 1133 per patient (95% CI ‐2793 to 442), despite no difference in health outcome between the groups (adjusted to 2007 Canadian prices). The average cost of TOR was 17% less than that of RPR. | ‐ | (1 RCT) | |||
| Quality of life | 16 different validated questionnaires were used by different studies to assess QoL. This outcome was reported in 11 RCTs, but reported in different ways which precluded meta‐analysis. In all but one of the RCTs where QoL was assessed there was improvement in the QoL in women after the intervention, irrespective of which route was used, with no significant difference in scores between groups. Where assessment of sexual function was performed, there was an equal amount of improvement in sexual function following surgical treatment, irrespective of the route employed | ‐ | (11 RCTs) | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval RCT: randomised controlled trial RPR: retropubic route RR: risk ratio TOR: transobturator route | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Random sequence generation was unclear in 13 studies and at high risk of bias in 2 studies, and allocation concealment was unclear in 20 studies and at high risk in 2/37 studies 2Allocation concealment was unclear in 2/5 trials and sequence generation was unclear in 1/5 trials, so we decided to downgrade by 1 level 3There was potential substantial heterogeneity with an I² value of 67%, so we downgraded the quality rating by 1 level 4There was potential substantial heterogeneity among studies with an I² value of 65%, which lead us to downgrade by 1 level 5As allocation concealment was unclear in 18/40 trials and at high risk in 3/40, and sequence generation was unclear in 14/40 trials and at high risk in 3/40, we decided to downgrade by 1 level 6As allocation concealment was unclear in 16/37 trials and at high risk in 2/37, and sequence generation was unclear in 11/37 trials and at high risk in 2/37, we decided to downgrade by 1 level 7Random sequence generation was unclear in 10/31 studies and at high risk of bias in 2/31, and allocation concealment was unclear in 15/31 studies and at high risk in 2/31, so we downgraded by 1 level 8Random sequence generation was unclear in 4/18 studies and at high risk in 2/18, and allocation concealment was unclear in 9/18 studies and at high risk in 2/18, so we downgraded the quality of the evidence by 1 level 9Random sequence generation was at high risk in 1/4 studies, while allocation concealment was unclear in 2/4 and at high risk in 1/4, so we downgraded by 1 level 10Allocation concealment was unclear in 12/31 trials and at high risk in 1/31, while sequence generation was unclear in 6/31 trials and at high risk in 1/31, so we decided to downgrade by 1 level 11The wide confidence interval was judged to include a threshold for appreciable harm considered to be > 25% increase in RR, in this case there was much more than a 25% increase in RR for harm, so we downgraded the level by 1 12There was potential substantial heterogeneity with an I² value of 46%, so we downgraded the quality rating by 1 level 13Due to the low number of studies reporting data for this outcome, and the low number of events and wide CI around the estimate of the effect, we downgraded the quality of evidence by 1 level due to imprecision | ||||||
| Retropubic bottom‐to‐top approach compared to retropubic top‐to‐bottom approach for stress urinary incontinence in women | ||||||
| Patient or population: women with stress urinary incontinence | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| retropubic top‐to‐bottom approach | Retropubic bottom‐to‐top approach | |||||
| Subjective cure (short term, ≤ 1 year) | Study population | RR 1.10 | 492 | ⊕⊕⊕⊝ | ||
| 770 per 1000 | 847 per 1000 | |||||
| Mean control group across studies | ||||||
| 890 per 1000 | 979 per 1000 | |||||
| Subjective cure (medium term, 1 to 5 years) | No studies reported this outcome | ‐ | (0 studies) | |||
| Subjective cure long term: > 5 years | No studies reported this outcome | ‐ | (0 studies) | |||
| Bladder or urethral perforation | Study population | RR 0.55 | 631 | ⊕⊕⊕⊝ | ||
| 85 per 1000 | 47 per 1000 | |||||
| Mean control group across studies | ||||||
| 115 per 1000 | 63 per 1000 | |||||
| Voiding dysfunction | Study population | RR 0.40 | 631 | ⊕⊕⊕⊝ | ||
| 60 per 1000 | 24 per 1000 | |||||
| Mean control group across studies | ||||||
| 49 per 1000 | 20 per 1000 | |||||
| De novo urgency or urgency incontinence | Study population | RR 0.84 | 547 | ⊕⊕⊝⊝ | ||
| 123 per 1000 | 103 per 1000 | |||||
| Mean control group across studies | ||||||
| 187 per 1000 | 157 per 1000 | |||||
| Vaginal tape erosion | Study population | RR 0.27 | 569 | ⊕⊕⊕⊝ | ||
| 35 per 1000 | 9 per 1000 | |||||
| Mean control group across studies | ||||||
| 69 per 1000 | 19 per 1000 | |||||
| Repeat incontinence surgery short term | No studies reported this outcome | ‐ | (0 studies) | |||
| Repeat incontinence surgery long term | No studies reported this outcome | ‐ | (0 studies) | |||
| Cost effectiveness of intervention | No studies reported this outcome | ‐ | (0 studies) | |||
| Quality of life (IIQ scores) | The mean quality of life (IIQ scores) in the control group was 49.9 | The mean quality of life (IIQ scores) in the intervention group was 4.6 lower (14.17 lower to 4.97 higher) | ‐ | 84 | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). IIQ: Incontinence Impact questionnaire RCT: randomised controlled trial RR risk ratio; | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Sequence generation and allocation concealment was unclear in 2/3 trials, so we downgraded by 1 level 2Sequence generation and allocation concealment was unclear in 3/5 trials, so we downgraded by 1 level 3Sequence generation was unclear in 2/4 studies and allocation concealment unclear in 3/4 studies, so we downgraded by 1 level 4The wide confidence interval was judged to include a threshold for appreciable harm considered to be > 25% increase in RR, in this case there was much more than a 25% increase in RR for harm, so we downgraded the level by 1 5Sequence generation unclear in 3/4 studies and allocation concealment unclear in 2/4 studies, so we downgraded by 1 level | ||||||
| Obturator medial‐to‐lateral approach compared to obturator lateral‐to‐medial approach for stress urinary incontinence in women | ||||||
| Patient or population: women with stress urinary incontinence | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Obturator lateral‐to‐medial approach | Obturator medial‐to‐lateral approach | |||||
| Subjective cure (short term ≤ 1 year) | Study population | RR 1.00 | 759 | ⊕⊕⊝⊝ | ||
| 877 per 1000 | 877 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 880 per 1000 | 880 per 1000 | |||||
| Subjective cure (medium term, 1 to 5 years) | Study population | RR 1.06 | 235 | ⊕⊕⊝⊝ | ||
| 711 per 1000 | 753 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 736 per 1000 | 780 per 1000 | |||||
| Subjective cure | No studies reported this outcome | ‐ | (0 studies) | |||
| Bladder or urethral perforation | Study population | RR 0.38 | 794 | ⊕⊕⊕⊝ | ||
| 11 per 1000 | 4 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 6 per 1000 | 2 per 1000 | |||||
| Voiding dysfunction (short and medium term, up to 5 years) | Study population | RR 1.74 | 1121 | ⊕⊕⊕⊝ | ||
| 40 per 1000 | 70 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 55 per 1000 | 96 per 1000 | |||||
| De novo urgency or urgency incontinence (short term, up to 12 months) | Study population | RR 1.01 | 357 | ⊕⊕⊝⊝ | ||
| 63 per 1000 | 63 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 64 per 1000 | 65 per 1000 | |||||
| Groin pain | Study population | RR 1.15 | 837 | ⊕⊝⊝⊝ | ||
| 80 per 1000 | 92 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 74 per 1000 | 85 per 1000 | |||||
| Vaginal tape erosion (short and medium term, up to 5 years) | Study population | RR 0.42 | 1087 | ⊕⊝⊝⊝ | ||
| 24 per 1000 | 10 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 17 per 1000 | 7 per 1000 | |||||
| Repeat incontinence surgery (short term, up to 12 months) | Study population | RR 0.64 | 532 | ⊕⊕⊝⊝ | ||
| 71 per 1000 | 45 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 58 per 1000 | 37 per 1000 | |||||
| Repeat incontinence surgery | No studies reported this outcome | ‐ | (0 studies) | |||
| Cost effectiveness of intervention | No studies reported this outcome | ‐ | (0 studies) | |||
| Quality of life | The mean quality of life in the control group was 0 | The mean quality of life in the intervention group was 16.54 higher (4.84 higher to 28.24 higher) | ‐ | 46 | ⊕⊝⊝⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). RCT: randomised controlled trial RR: risk ratio; | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Random sequence generation was unclear in 4/6 studies, allocation concealment was unclear in5/6 and at high risk in 1/6 studies, so we downgraded the quality of evidence due to risk of bias by 2 levels 2Random sequence generation was unclear in all both studies, allocation concealment was unclear in 1 and high risk of bias in the other study, so we downgraded by 2 levels 3Sequence generation was unclear in 2 studies and allocation concealment was unclear in 3 studies, so we downgraded the quality rating by 1 level 4Sequence generation was unclear in 3 studies and at high risk in 1 study, while allocation concealment was unclear in 4 studies and at high risk in 1 study, so we downgraded by 1 level 5Sequence generation was unclear in 2/3 studies and at high risk in 1/3, allocation concealment was unclear in 2/3 studies and high in 1/3, so we downgraded by 2 levels 6Random sequence generation was unclear in 2/5 and high in 1/5 studies, while allocation concealment was unclear in 2/5 and high in 2/5 studies, so we downgraded the quality of evidence due to high risk of bias by 2 levels 7The wide confidence interval was judged to include a threshold for appreciable harm considered to be > 25% increase in RR, in this case there was > 65% increase in RR for harm, so we downgraded by 1 level 8Sequence generation was unclear in 3/7 studies and at high risk in 1/7. Allocation concealment was unclear in 5/7 studies and at high risk in 1/7. We downgraded the quality rating by 2 levels 9Sequence generation and allocation concealment were unclear in 1/2 studies, so we downgraded by 1 level 10Sequence generation and allocation concealment were unclear, so we downgraded by 1 level 11As there was only 1 study with very few events and CIs around estimates of effect included appreciable benefit and appreciable harm, we downgraded by 2 levels | ||||||
| Monofilament compared to multifilament tapes for stress urinary incontinence in women | ||||||
| Patient or population: women with stress urinary incontinence | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| multifilament tapes | Monofilament | |||||
| Subjective cure (short term ≤ 1 year) | Study population | RR 1.07 | 505 | ⊕⊕⊕⊝ | ||
| 784 per 1000 | 839 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 810 per 1000 | 867 per 1000 | |||||
| Subjective cure (medium term: 1 to 5 years) | No studies reported this outcome | ‐ | (0 studies) | |||
| Subjective cure (long term: > 5 years) | No studies reported this outcome | ‐ | (0 studies) | |||
| Bladder or urethral perforation | Study population | RR 0.76 | 496 | ⊕⊕⊕⊝ | ||
| 37 per 1000 | 28 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 32 per 1000 | 25 per 1000 | |||||
| Voiding dysfunction | Study population | RR 2.20 | 400 | ⊕⊕⊝⊝ | ||
| 41 per 1000 | 89 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 65 per 1000 | 143 per 1000 | |||||
| De novo urgency or urgency incontinence | Study population | RR 1.09 | 496 | ⊕⊕⊝⊝ | ||
| 102 per 1000 | 111 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 107 per 1000 | 117 per 1000 | |||||
| Vaginal tape erosion | Study population | RR 0.43 | 396 | ⊕⊕⊕⊕ | ||
| 62 per 1000 | 26 per 1000 | |||||
| Mean control group risk across studies | ||||||
| 43 per 1000 | 18 per 1000 | |||||
| Repeat incontinence surgery (short term ≤ 1 year) | No studies reported this outcome | ‐ | (0 studies) | |||
| Repeat incontinence surgery (long term > 5 years) | No studies reported this outcome | ‐ | (0 studies) | |||
| Cost effectiveness of intervention | No studies reported this outcome | ‐ | (0 studies) | |||
| Quality of life scores ICIQ | The mean quality of life scores ICIQ in the control group was 2.1 | The mean quality of life scores ICIQ in the intervention group was 0.6 lower (0.76 lower to 0.44 lower) | ‐ | 96 | ⊕⊕⊕⊕ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ICIQ: International Consultation on Incontinence questionnaire RCT: randomised controlled trial RR: risk ratio | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Random sequence generation and allocation concealment unclear in 2/4 studies, so we downgraded by 1 level 2Random sequence generation and allocation concealment unclear in 2/3 studies, so downgraded by 1 level 3The wide confidence interval was judged to include a threshold for appreciable harm considered to be > 25% increase in RR, in this case there was much more than a 25% increase in RR for harm, so we downgraded by 1 level 4Sequence generation and allocation concealment were unclear in 2/4 studies, so we downgraded the quality rating by 1 level 5The wide confidence interval was judged to include a threshold for appreciable harm considered to be > 25% increase in RR, in this case there was > 65% increase in RR for harm, so we downgraded by 1 level | ||||||
| Study | Outcome data |
| Abdel‐Fattah 2010 | Group A: TVT‐O (n = 170) Group B: TOT (n = 171) Loss to follow up at 1yr: A: 18/170, B: 24/171 Loss to follow up at 3yrs: A: 44/170, B: 59/171 Objective cure: A: 114/121, B: 96/109 Subjective success: A: 121/149, B: 111/143 Bladder/urethral perforation: A: 1/170, B: 2/171 Voiding dysfunction: A: 12/170, B: 9/171 Tape erosion: A: 3/153, B: 5/149 Groin pain: A: 27/150, B: 19/147 Repeat continence surgery: A: 7/170, B: 15/171 QoL assessed via: King’s Health Questionnaire (KHQ) [10], Birmingham Bowel Urinary Symptom (BBUSQ‐22) [11] and Pelvic Organ Prolapse/Incontinence Sexual Function Questionnaire (PISQ‐12). In addition Patient Global Impression of Improvement (PGI‐I) [13] and International Consultation on Incontinence Questionnaire‐ Short form (ICIQ‐SF) [14] questionnaires. QOL scores were much improve following surgery with no significant inter group (A vs B) differences. Sexual dysfunction: PISQ‐12 employed. 199 patients completed this assessment and in most domains a significant improvement in postoperative PISQ‐12 scores was found with no significant difference demonstrated between the two groups. Intermediate (3 yr) Subjective success (very much & much improved) on PGI‐I: A: 93/126, B: 81/112 |
| Aigmuller 2014 | Group A: TVT: (n = 285; 38 of whom were lost to follow‐up) Group B: TVT‐O: (n = 269; 36 of whom were lost to follow‐up) Participants were evaluated at 3 months, with a further evaluation scheduled at 5 years
At 5‐year review:
|
| Alkady 2009 | Group A: TVT (n = 15) Group B: TVT‐O (n = 15)
|
| Andonian 2005 | Group A: SPARC Group B: TVT
|
| Andonian 2007 | Group A: Obtape (n = 78) Group B: DUPS (n = 32) ‐ suspended Group C: TVT (n = 80)
|
| Aniuliene 2009 | Group A: TVT‐O (n = 150) Group B: TVT (n = 114)
|
| Araco 2008 | Group A: TVT‐O (n = 120)
|
| Barber 2008 | Group A: TVT (n = 88) Group B: TOT (n = 82)
|
| Barry 2008 | Group A: TOT (n = 58)
|
| But 2008 | Group A: TVT‐O (n = 60) Group B: TOT (n = 60)
|
| Cervigni 2006 | Numbers in each group unreported. It was, thus, impossible to abstract results |
| Chen 2010 | Group A: TVT (n = 77) Group B: TOT (n = 45) Group C: TVT‐O (n = 65)
|
| Chen 2012 | A: TVT (n = 102) B: TVT‐O (n = 103)
|
| Cho 2010 | Group A: Monarc TOT (n = 48) Group B: TOT (n = 45)
|
| Choe 2013 | We were not able to use the data provided, as the number in each group was not specified |
| Darabi Mahboub 2012 | Group A: TOT (n = 40) Group B: TVT (n = 40) Operative time (minutes (SD): A: 64.50 (9.04), B: 64.00 (9.48) Mean hospital stay (days): A: 2.56 (0.51), B: 2.52 (0.47) |
| David‐Montefiore 2006 | Group A: RPR (n = 42) Group B: TOR (n = 46)
|
| de Leval 2011 | Group A: TVT‐O (n = 87) Group B: modified TVT‐O (n = 88)
At 3‐year follow‐up:
|
| de Tayrac 2004 | Group: A: TOT (n = 30) Group: B: TVT (n = 31)
|
| Deffieux 2010 | Group A: TVT (n = 75) Group B: TVT‐O (n = 74)
|
| Diab 2012 | Group A: TOT (n = 31) Group B: TVT (n = 32)
All the preoperative parameters were comparable in both groups. The mean operative time was significantly longer and bladder injury was significantly higher in the TVT group. There were no significant difference in cure rates, voiding dysfunction, de novo urgency and reoperation rate. The postoperative groin/thigh pain was higher in the TOT group. |
| El‐Hefnway 2010 | Preliminary results: Group A: TVT: (n = 19) Group B: TOT: (n = 21) At 24 months: Group A: TVT: (n = 45) Group B: TOT: (n = 42)
|
| Elbadry 2014 | Group A: adjustable TOT (n = 48) Group B: TOT: (n = 48)
|
| Enzelsberger 2005 | Group A: TOT (n = 56) Group B: TVT (n = 54)
|
| Freeman 2011 | Group A: Monarc TOT (n = 100) Group B: Gynaecare TVT (n = 92)
|
| Hammoud 2011 | Group A: TVT (n = 60) Group B: TVT‐O (n = 50) Subjective cure: A: 56/60, B: 48/50 |
| Hassan 2013 | Group A: inside‐out TOT (n = 125) Group B: outside‐in TOT (n = 125)
|
| Houwert 2009 | Group A: TVT‐O (n = 93) Group B: Monarc TOT (n = 98)
|
| Jakimiuk 2012 | Group A: TVT (n = 19) Group B: TVT‐O (n = 16)
|
| Juang 2007 | Group A: TVT‐O (n = 47) Group B: TVT‐O plus IS: (n = 49)
|
| Kamel 2009 | A: TVT (n = 60) B: TVT‐O (n = 60)
|
| Karateke 2009 | Group A: TVT (n = 83) Group B: TVT‐O (n = 84)
|
| Kilic 2007 | Group A: TVT (n = 10) Group B: TOT (n = 10)
|
| Kim 2004 | Group A: TVT (n = 32) Group B: SPARC (n = 30)
|
| Kim 2005 | Group A: Monarc (n = 65) Group B: SPARC (n = 65)
|
| Krofta 2010 | Group A: TVTTM (n = 149) Group B: TVT –OTM (n = 151)
|
| Laurikainen 2007 | Group A: TVT‐O (n = 131)
QoL: The scores of the condition specific quality of life questionnaires were significantly lower at the 3 and 5 year follow up compared with pre‐operative scores. This improvements were statistically significant, but with no difference between the groups. 84% of women with pre‐operative moderate and severe frequency and urgency symptoms were cured of these symptoms at the 5 year follow up. |
| Leanza 2009 | Group A: r‐TICT (n = 229; retropubic) Group B: t‐TICT (n = 220; transobturator) Subjective cure: A: 190/215, B: 178/208 |
| Lee 2007 | Group A: TVT (n = 60) Group B: TVT‐O (n = 60)
|
| Lee 2008 | Group A: TVT‐O (n = 50) Group B: TOT (n = 50)
|
| Liapis 2006 | Group A: TVT (n = 46) Group B: TVT‐O (n = 43)
|
| Liapis 2008 | Group A: TVT‐O (n = 61) Group B: Monarc TOT (n = 53)
|
| Lim 2005 | Group A: TVT (n = 61) Group B: IVS (n = 60) Group C: SPARC (n = 61)
|
| Lord 2006 | Group A: TVT (n = 147)
|
| Mansoor 2003 | Group A: TVT‐O (n = 48)
|
| Mehdiyev 2010 | A: TOT (n = 17) B: TVT (n = 15)
|
| Meschia 2006 | Group A: TVT (n = 92)
|
| Meschia 2007 | Group A: TVT‐O (n = 117) Group B: TVT (n = 114)
|
| Naumann 2006 | Group A: TVT (n = 123) Group B: LIFT (n = 125)
|
| Nerli 2009 | Group A: TVT (n = 18) Group B: TOT (n = 18)
|
| Nyyssonen 2014 | Group A: TOT (n = 50) Group B: TVT (n = 50)
|
| Okulu 2013 | Group A: Vypro mesh: (n = 48; multifilament) Group B: Ultrapro mesh: (n = 48; monofilament + biological combined mesh) Group C: Prolene light mesh: (n = 48; monofilament)
|
| Oliveira 2006 | Group A: TVT (n = 17)
|
| Palomba 2008 | Trial terminated. |
| Paparella 2010 | Group A: synthetic UretexTO® (n = 34) Group B: biological PelviLaceTO® (n‐36)
|
| Park 2012 | Group A: TVT‐O (n = 39) Group B: TOT Monarc (n = 35)
|
| Peattie 2006 | No published data. |
| Porena 2007 | Group A: TVT (n = 70) Group B: TOT (n = 75)
|
| Rechberger 2003 | Group A: TVT (n = 50) Group B: IVS (n = 50)
|
| Rechberger 2009 | Group A: retropubic (IVS‐02; n = 269) Group B: transobturator (IVS‐04; n = 268)
|
| Rechberger 2011 | Group A: TOT (n = 232) Group B: TOT with fixation (n = 231)
|
| Richter 2010 | Group A: retropubic sling (TVT; n = 298) Group B: transobturator tapes (TVT‐O, and TOT Monarc; n = 299) (Group C (?): TVT‐O (inside‐out) ‐ separate data not provided) (Group D (?): TOT (Monarch, outside‐in) ‐ separate data not provided) Objective cure at 1 year: A: 232/280 (80.8%), B: 233/285 (77.7%) Subjective cure at 1 year: A: 181/280 (62.2%), B: 163/285 (55.8%) Secondary outcomes:
PISQ‐12 (Prolapse / urinary incontinence sexual questionnaire): Analysis of results for group A and group B combined showed significant improvement in sexual function in both groups with a mean PISQ‐12 score increase from 32.8+/‐7.1 at baseline to 37.3+/‐ 6 at 24 months. These changes are >0.6 SD units, which reflects “medium” improvement in the PISQ‐12 score after surgery. Compared with women with successful surgery, women who experienced surgical failure, regardless of assigned type of surgery, reported worse adjusted sexual function scores at all postoperative time points. Improvement in PISQ‐12 scores was consistent with change in the 3 specific items from the sexual function measure of interest: (1) the experience of pain during sexual activity, (2) UI during sexual activity, and (3) fear of incontinence during sexual activities. Pain with intercourse was reported by 153 of 406 of sexually active women (38%) at baseline and decreased to 27% at 12 months after surgery (P.003). Self‐reported UI and the fear of incontinence occurring during sexual activity also significantly improved by 12 months after surgery, regardless of sling route. To specifically investigate the association of synthetic mesh slings on dyspareunia, we repeated the analysis on the 247 women who underwent MUS only (no concurrent procedures) and who completed baseline and 12‐month assessments. In this subset of women, dyspareunia decreased from 57% at baseline to 43% at 12 months after surgery (P .03). 5‐year data provided, but without numbers in each group, so could not be used for meta‐analysis |
| Riva 2006 | Group A: TOT (n = 65) Group B: TVT (n = 66) |
| Ross 2009 | Group A: TVT (n = 105) Group B: TOT (n = 94)
|
| Salem 2014 | Group A: TOT (n = 37) Group B: TVT (n = 39) No significant difference was noticed between the two groups as regard the mean operative time, perioperative complications, intraoperative blood loss, hospital stay, and time to return to normal activities. The mean of abdominal leak point pressure and urethral closure pressure showed marked and maintained improvement for 5 years later in group I whereas in group II, they showed marked and maintained improvement for only one year then shows significant decline in comparison with group I. As regard the mean of objective SEAPI score shows marked decrease (improvement) in both groups and this was maintained for the five years in group I but in group II, it increased after one year later. No usable data provided. |
| Scheiner 2012 | Group A: TVT (n = 80) Group B: TOT outside‐in approach (Monarc; n = 40) Group C: TVT‐O inside‐out approach (Gynecare; n = 40)
|
| Schierlitz 2008 | Group A: TVT (n = 81) Group B: Monarc sling (n = 82)
|
| Tanuri 2010 | Group A: Safyre VS retropubic tape (n = 10) Group B: Safyre T transobturator tape (n = 20)
|
| Tarcan 2011 | Group A: TVT (n = 27) Group B: TOT (n = 27) 12‐month follow‐up assessed:
2 year follow‐up assessed:
|
| Teo 2011 | Group A: TVT (n = 66) Group B: TVT‐O (n = 61)
|
| Tommaselli 2012 | Group A: TVT‐O (n = 48) Group B: modified TVT‐O (n = 24)
|
| Tseng 2005 | Group A: SPARC (n = 31)
|
| Ugurlucan 2013 | Group A: biological PELVILACE TO (n = 50) Group B: synthetic TOT ALIGN ®TO (n = 50)
|
| van Leijsen 2013 | Group A: RPR (n = 33) Group B: TOT (n = 90)
|
| Wang 2006 | Group A: Monarc (n = 31) Group B: SPARC (n = 29)
|
| Wang 2008 | Group A: TVT (n = 35) Group B: TVT‐O (n = 34)
|
| Wang 2009 | Group A: TVT (n = 154) Group B: TVT‐O (n = 146)
|
| Wang 2010 | Group A: TVT (n = 70) Group B: TOT (n = 70)
|
| Wang 2011 | Group A: TVT (n = 32) Group B: TVT‐O (n = 36)
|
| Zhang 2011 | Group A: TVT‐O (n = 76) Group B: modified TVT‐O (n = 80)
|
| Zullo 2007 | Group A: TVT (n = 35) Group B: TVT‐O (n = 37)
|
| Abbreviations BFLUTS: Bristol lower urinary tract symptoms questionnaires BMI: body‐mass index DO: detrusor overactivity DUP: distal urethral polypropylene sling EQOL‐5D: Euro Quality of life ‐5 Dimension hr: hour/s HRT: hormone replacement therapy ICIQ: International Consultation on Incontinence questionnaire ICIQ‐FLUTS: International Consultation on Incontinence questionnaire ‐ female lower urinary tract symptoms ICIQ‐ LUTSquol: International Consultation on Incontinence questionnaire ‐ lower urinary tract quality of life questionnaire ICIQ‐SF: International Consultation on Incontinence questionnaire short form ICIQ‐SF15: International Consultation on Incontinence questionnaire short form 15 IIQ: Incontinence Impact questionnaire ICS: International Continence Society I‐QoL: Incontinence Quality of Life questionnaire ISD: intrinsic sphincter deficiency IVS: intravaginal slingoplasty KHQ: King's Health questionnaireMUI: mixed urinary incontinence MUCP: Maximum urethral closure pressure MUI: mixed urinary incontinence OAB: overactive bladder PGI‐I: Patient Global Impression of Improvment PGI‐S: Patient Global Impression of Severity PISQ‐12: pelvic organ prolapse/urinary incontinence sexual questionnaire POP: pelvic organ prolapse POP‐Q: pelvic organ prolapse quantification POP‐Q ICS: pelvic organ prolapse quantification International Continence Society PVR: post void residual RCT: randomized controlled trial RPR: retropubic route QoL: quality of life QRCT: quasi‐randomised trial SEAPI‐QMM: Stress related leak, Empyting ability, Anatomy, Protection, Inhibition‐Quality of life, Mobility and Mental status incontinence classification system SD: standard deviation SIS: Single incision sling SPARC: suprapubic arc (procedure) SUI: stress urinary incontinence TOR: transobturator TOT: transobturator tape TOT‐ARIS: transobturator tape‐ARIS TVT: tension‐free vaginal tape TVT‐O: transobturator tension‐free vaginal tape UDI: Urinary Distress Impact questionnaire UDI‐6: Urinary Distress Impact questionnaire short form UDS: urodynamics study UI: urinary incontinence UISS: urinary incontinence severity score USI: urodynamic stress incontinence USS: ultrasound UTI: urinary tract infection UUI: urgency urinary incontinence VAS: visual analogue scale VLPP: Valsalval leak point pressure | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Subjective cure (short term, ≤ 1 year) Show forest plot | 36 | 5514 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.96, 1.00] |
| 2 Subjective cure and improvement (short term, ≤ 1 year) Show forest plot | 10 | 1651 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.96, 1.00] |
| 3 Subjective cure (medium term, 1 to 5 years) Show forest plot | 5 | 683 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.87, 1.09] |
| 4 Subjective cure (long term, > 5 years) Show forest plot | 4 | 714 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.80, 1.12] |
| 5 Subjective cure and improvement (long term, > 5 years) Show forest plot | 2 | 340 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.67, 1.28] |
| 6 Objective cure (short term, ≤ 1 year) Show forest plot | 40 | 6145 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.96, 1.00] |
| 7 Objective cure and improvement (short term, ≤ 1 year) Show forest plot | 10 | 1478 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.96, 1.01] |
| 8 Objective cure (medium term, 1 to 5 years) Show forest plot | 5 | 596 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.95, 1.06] |
| 9 Objective cure (long term, > 5 years) Show forest plot | 3 | 400 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.90, 1.06] |
| 10 Operative time (minutes) Show forest plot | 31 | 4713 | Mean Difference (IV, Random, 95% CI) | ‐7.54 [‐9.31, ‐5.77] |
| 11 Operative blood loss (ml) Show forest plot | 14 | 1869 | Mean Difference (IV, Random, 95% CI) | ‐6.49 [‐12.33, ‐0.65] |
| 12 Length of hospital stay (days) Show forest plot | 17 | 2170 | Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.59, 0.09] |
| 13 Time to return to normal activity level (weeks) Show forest plot | 4 | 626 | Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.15, 0.06] |
| 14 Perioperative complications Show forest plot | 15 | 2205 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.73, 1.14] |
| 15 Major vascular or visceral injury Show forest plot | 28 | 4676 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.19, 0.55] |
| 16 Bladder or urethral perforation Show forest plot | 40 | 6372 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.08, 0.20] |
| 17 Voiding dysfunction Show forest plot | 37 | 6200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.43, 0.65] |
| 18 De novo urgency or urgency incontinence (short term, ≤ 1 year) Show forest plot | 31 | 4923 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.82, 1.17] |
| 19 De novo urgency or urgency incontinence (medium term, 1 to 5 years) Show forest plot | 4 | 481 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.55, 1.73] |
| 20 De novo urgency or urgency incontinence (long term, > 5 years) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 21 Detrusor overactivity Show forest plot | 4 | 566 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.58, 1.73] |
| 22 Vaginal tape erosion Show forest plot | 31 | 4743 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.78, 1.65] |
| 23 Bladder/urethral erosion Show forest plot | 4 | 374 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.01, 8.13] |
| 24 Groin pain Show forest plot | 18 | 3221 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.12 [2.71, 6.27] |
| 25 Suprapubic pain Show forest plot | 4 | 1105 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.11, 0.78] |
| 26 Repeat incontinence surgery (short term, ≤ 1 year) Show forest plot | 9 | 1402 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [0.85, 3.16] |
| 27 Repeat incontinence surgery (medium term , 1 to 5 years) Show forest plot | 2 | 355 | Risk Ratio (M‐H, Fixed, 95% CI) | 21.89 [4.36, 109.77] |
| 28 Repeat incontinence surgery (long term > 5 years) Show forest plot | 4 | 695 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.79 [3.36, 23.00] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Subjective cure (short term, ≤ 1 year) Show forest plot | 3 | 477 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [1.01, 1.19] |
| 2 Objective cure (short term, ≤ 1 year) Show forest plot | 5 | 622 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.97, 1.17] |
| 3 Operative time (minutes) Show forest plot | 2 | 124 | Mean Difference (IV, Fixed, 95% CI) | ‐2.15 [‐4.68, 0.38] |
| 4 Length of hospital stay (days) Show forest plot | 2 | 124 | Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.37, 0.30] |
| 5 Perioperative complications Show forest plot | 4 | 507 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.53, 1.84] |
| 6 Bladder or urethral perforation Show forest plot | 5 | 631 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.31, 0.98] |
| 7 Voiding dysfunction Show forest plot | 5 | 631 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.18, 0.90] |
| 8 De novo urgency or urgency incontinence Show forest plot | 4 | 541 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.52, 1.34] |
| 9 Detrusor overactivity Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10 Vaginal tape erosion Show forest plot | 4 | 563 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.08, 0.95] |
| 11 QoL specific Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Subjective cure (short term, ≤ 1 year) Show forest plot | 6 | 759 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.96, 1.06] |
| 2 Subjective cure and improvement (short term, ≤ 1 year) Show forest plot | 5 | 732 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.97, 1.08] |
| 3 Subjective cure (medium term, 1 to 5 years) Show forest plot | 2 | 235 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.91, 1.23] |
| 4 Subjective cure and improvement (medium term, 1 to 5 years) Show forest plot | 2 | 399 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.90, 1.11] |
| 5 Objective cure (short term, ≤ 1 year) Show forest plot | 6 | 745 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.95, 1.04] |
| 6 Objective cure and improvement (short term, ≤ 1 year) Show forest plot | 2 | 214 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.95, 1.07] |
| 7 Operative time (minutes) Show forest plot | 4 | 481 | Mean Difference (IV, Random, 95% CI) | 0.52 [‐1.09, 2.13] |
| 8 Operative blood loss (ml) Show forest plot | 3 | 255 | Mean Difference (IV, Fixed, 95% CI) | 1.11 [‐6.01, 8.22] |
| 9 Length of hospital stay (days) Show forest plot | 2 | 190 | Mean Difference (IV, Random, 95% CI) | ‐0.77 [‐2.54, 0.99] |
| 10 Time to return to normal activity level Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11 Perioperative complications Show forest plot | 2 | 214 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.23, 7.51] |
| 12 Major vascular or visceral injury Show forest plot | 4 | 622 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.23, 2.19] |
| 13 Vaginal perforation/injury Show forest plot | 3 | 541 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.12, 0.53] |
| 14 Bladder or urethral perforation Show forest plot | 6 | 794 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.07, 1.92] |
| 15 Voiding dysfunction Show forest plot | 8 | 1121 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.74 [1.06, 2.88] |
| 16 De novo urgency or urgency incontinence Show forest plot | 3 | 357 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.46, 2.20] |
| 17 Detrusor overactivity Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 18 Vaginal tape erosion Show forest plot | 7 | 1087 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.16, 1.09] |
| 19 Groin/thigh pain Show forest plot | 6 | 837 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.75, 1.76] |
| 20 Repeat incontinence surgery Show forest plot | 2 | 532 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.32, 1.30] |
| 21 QoL specific Show forest plot | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | 16.54 [4.84, 28.24] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Subjective cure (short term, up to 1 year) Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.90, 1.11] |
| 1.2 Modified TVT (suburethral pad) versus TVT | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.91, 1.10] |
| 1.3 Self‐tailored TVT‐O vs TVT‐O | 1 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.93, 1.11] |
| 1.4 Monarc®TOT open edge + tension suture vs TOT® | 1 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.87, 1.24] |
| 1.5 AdjustableTOT vs TOT® | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.87, 1.28] |
| 1.6 Synthetic vs biological | 2 | 169 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.86, 1.22] |
| 2 Subjective cure and improvement (short term, up to 1 year) Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.97, 1.09] |
| 2.2 TOT + 2‐point tape fixation vs TOT | 1 | 418 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [1.00, 1.14] |
| 2.3 TVT versus modified TVT (suburethral pad) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.98, 1.08] |
| 3 Subjective cure (medium term, 1 to 5 years) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 153 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.86, 1.12] |
| 4 Objective cure (medium term, 1 to 5 years) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Objective cure (short term, ≤ 1 year) Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 Modified TVT‐O (less dissection) vs TVT‐O | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.91, 1.15] |
| 5.2 Synthetic vs biological | 2 | 136 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.94, 1.14] |
| 5.3 TVT‐O + IS vs TVT‐O | 1 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [1.02, 2.06] |
| 5.4 TOT + 2‐point tape fixation vs TOT | 1 | 418 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [1.01, 1.13] |
| 6 Operative time (minutes) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 TVT‐O + IS vs TVT‐O | 1 | 96 | Mean Difference (IV, Fixed, 95% CI) | 12.0 [8.91, 15.09] |
| 6.2 Self‐tailored TVT‐O vs TVT‐O | 1 | 156 | Mean Difference (IV, Fixed, 95% CI) | ‐25.0 [‐26.73, ‐23.27] |
| 7 Operative blood loss (ml) Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 TVT‐O + IS versus TVT‐O | 1 | 92 | Mean Difference (IV, Fixed, 95% CI) | 52.10 [43.73, 60.47] |
| 7.2 Self‐tailored TVT‐O vs TVT‐O | 1 | 156 | Mean Difference (IV, Fixed, 95% CI) | ‐13.00 [‐16.57, ‐13.43] |
| 7.3 Synthetic vs biological | 1 | 70 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐0.92, 0.12] |
| 8 Length of hospital stay (days) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 TVT‐O + IS vs TVT‐O | 1 | 96 | Mean Difference (IV, Fixed, 95% CI) | 12.0 [8.91, 15.09] |
| 8.2 Self‐tailored TVT‐O vs TVT‐O | 1 | 156 | Mean Difference (IV, Fixed, 95% CI) | ‐3.0 [‐3.16, ‐2.84] |
| 9 Perioperative complications Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 Synthetic vs biological | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Major vascular or visceral injury Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 TVT‐O + IS vs TVT‐O | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.17, 3.04] |
| 10.2 Synthetic vs biological | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.3 AdjustableTOT vs TOT® | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Bladder/urethral perforation Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 11.1 TVT‐O + IS vs TVT‐O | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 TOT + 2‐point tape fixation vs TOT | 1 | 463 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.17, 3.33] |
| 11.3 TVT versus modified TVT (suburethral pad) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.05, 5.36] |
| 11.4 AdjustableTOT vs TOT® | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Voiding dysfunction Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 12.1 Modified TVT‐O (less dissection) vs TVT‐O | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.13, 30.61] |
| 12.2 TVT versus modified TVT (suburethral pad) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.21 [0.70, 7.00] |
| 12.3 Self‐tailored TVT‐O vs TVT‐O | 1 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.06, 14.92] |
| 12.4 Monarc®TOT open edge + tension suture vs TOT® | 1 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.04, 4.99] |
| 12.5 Synthetic vs biological | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.25, 101.58] |
| 13 De novo urgency or urgency incontinence Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 13.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.51, 2.94] |
| 14 Vaginal tape erosion Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 14.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.88] |
| 14.2 TVT versus modified TVT (suburethral pad) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.30 [0.61, 8.68] |
| 14.3 TVT‐O + IS vs TVT‐O | 1 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.06, 14.55] |
| 14.4 Monarc®TOT open edge + tension suture vs TOT® | 1 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.01, 2.53] |
| 14.5 Synthetic vs biological | 2 | 169 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 71.92] |
| 15 Bladder/urethral erosion Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 15.1 TVT versus modified TVT (suburethral pad) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.06, 15.56] |
| 16 Groin pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 16.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.30, 5.64] |
| 16.2 Synthetic vs biological | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Subjective cure (short term, ≤ 1 year) Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Monofilament versus multifilament | 4 | 546 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.95, 1.10] |
| 1.2 Monofilament versus combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.79, 1.05] |
| 1.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.96, 1.26] |
| 2 Subjective cure (medium term, 1 to 5 years) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Monofilament vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.85, 1.23] |
| 2.2 Monofilament vs combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.78, 1.06] |
| 2.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.96, 1.32] |
| 3 Objective cure (short term, ≤ 1 year) Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Monofilament vs multifilament | 2 | 349 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.96, 1.19] |
| 4 Operative time (minutes) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Monofilament vs multifilament | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Length of hospital stay (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 Monofilament vs multifilament | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Perioperative complications Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Monofilament vs multifilament | 2 | 279 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.36, 3.69] |
| 7 Major vascular or visceral injury Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 Monofilament vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Monofilament vs combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Bladder or urethral perforation Show forest plot | 4 | 749 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.49, 2.70] |
| 8.1 Monofilament vs multifilament | 4 | 557 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.49, 2.70] |
| 8.2 Monofilament vs combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Voiding dysfunction Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 Monofilament vs multifilament | 3 | 461 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.10 [0.96, 4.59] |
| 10 De novo urgency or urgency incontinence Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 Monofilament vs multifilament | 4 | 545 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.68, 1.82] |
| 10.2 Monofilament vs combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.38, 10.41] |
| 10.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.4 [0.08, 1.96] |
| 11 Detrusor overactivity Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 11.1 Monofilament vs multifilament | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Vaginal tape erosion Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 12.1 Monofilament vs multifilament | 3 | 445 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.09, 6.84] |
| 12.2 Monofilament vs combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 3.0 [0.32, 27.83] |
| 12.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.04, 3.09] |
| 13 QoL specific (ICIQ) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 13.1 Monofilament vs multifilament | 1 | 96 | Mean Difference (IV, Fixed, 95% CI) | ‐0.60 [‐0.76, ‐0.44] |

