Aspiración quística ovárica antes del tratamiento de fecundación in vitro para la subfertilidad
Información
- DOI:
- https://doi.org/10.1002/14651858.CD005999.pub2Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 12 diciembre 2014see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Ginecología y fertilidad
- Copyright:
-
- Copyright © 2017 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
JC, AB and RH jointly developed the protocol.
For the full review, RM, JC and AB conducted a preliminary literature search and reviewed the available literature. RM, JC and AB were responsible for screening the studies. RM collected the data. RM, JM and RH assessed the quality of the studies. Disagreements were resolved by a meeting of review authors and by consulting an external author. JM developed the summary of findings table, supplied methodological advice and fully edited the draft review.
RM, JM and RH wrote the review. All authors were involved in the review of the final manuscript. RH was the final consultant for the review.
Sources of support
Internal sources
-
None, Other.
External sources
-
None, Other.
Declarations of interest
RM and JM have no conflicts of interest to disclose. RH is a shareholder in Western IVF and is a member of the medical advisory boards of the pharmaceutical companies Merck‐Serono and MSD, which supply drugs used in IVF cycles.
Acknowledgements
We wish to acknowledge the peer reviewers and the staff at the Menstrual Disorders and Subfertlity Group (MDSG), in particular Helen Nagels and Marion Showell for their contribution to the review.
We acknowledge the contributions of Jason Chin and Angela Beard to the early development of this full review.
Version history
| Published | Title | Stage | Authors | Version |
| 2014 Dec 12 | Ovarian cyst aspiration prior to in vitro fertilization treatment for subfertility | Review | Rose McDonnell, Jane Marjoribanks, Roger J Hart | |
| 2006 Apr 19 | Ovarian cyst aspiration prior to in vitro fertilization treatment for subfertility. | Protocol | Samar Hassan, Roger J Hart, Hanan Al Kadri, Haya M Al‐Fozan | |
Differences between protocol and review
Adverse events, including infection, bleeding, injury to surrounding structures, need for further surgery including oophorectomy, anaesthetic complications, and costs of both the procedure itself and any subsequent complications, have been added as a primary outcome.
Cancellation rate per cycle has been added as a secondary outcome between publication of the review protocol and the review. We planned to report this outcome in "Other data" rather than in a forest plot. However, as the relevant study only included one cycle, we were able to report this as "per woman" data.
An additional author has been added between the publication of the review protocol and the review, and two authors moved to 'Acknowledgements'.
We have revised the methods section of the review to reflect current Cochrane standards for conducting and reporting reviews.
The effect estimate used in the final review was the Mantel‐Haenszel OR with 95% CI. In the protocol it was documented that the Peto OR would be used, and this was altered to the Mantel‐Haenszel OR prior to final publication.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- *Pregnancy Rate;
- Embryo Transfer;
- Fertilization in Vitro [*methods];
- Infertility, Female [*therapy];
- Oocyte Retrieval;
- Ovarian Cysts [*therapy];
- Ovarian Follicle;
- Ovulation Induction [methods];
- Randomized Controlled Trials as Topic;
- Suction [adverse effects, *methods];
- Ultrasonography, Interventional;
Medical Subject Headings Check Words
Adult; Female; Humans; Pregnancy;
PICO
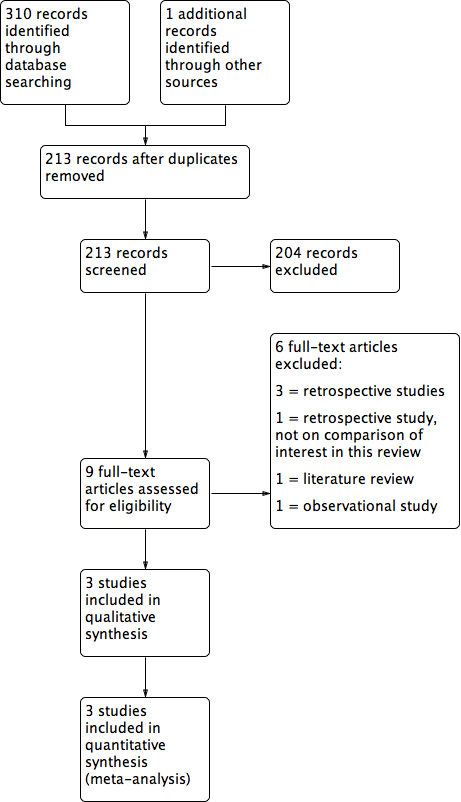
Study flow diagram.
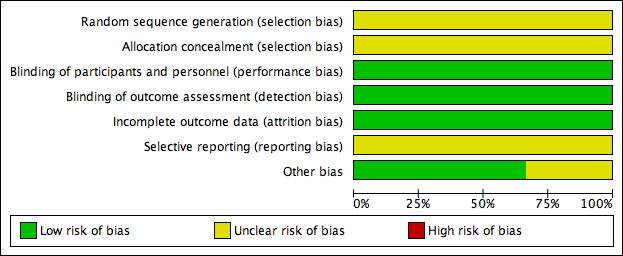
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: 1 Cyst aspiration versus conservative management, outcome: 1.1 NEW Clinical Pregnancy Rate.

Forest plot of comparison: 1 Cyst aspiration versus conservative management, outcome: 1.2 Number of Follicles Recruited.

Comparison 1 Cyst aspiration versus conservative management, Outcome 1 Clinical Pregnancy Rate.

Comparison 1 Cyst aspiration versus conservative management, Outcome 2 Number of Follicles Recruited.
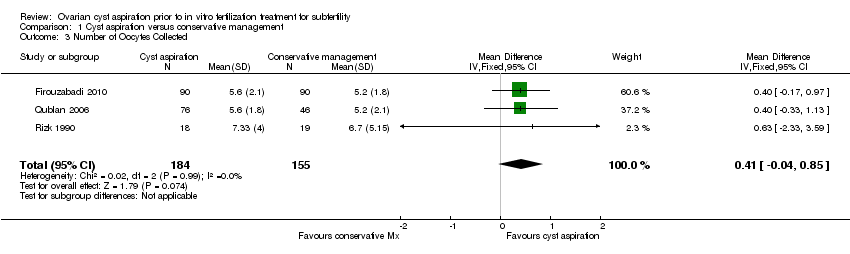
Comparison 1 Cyst aspiration versus conservative management, Outcome 3 Number of Oocytes Collected.
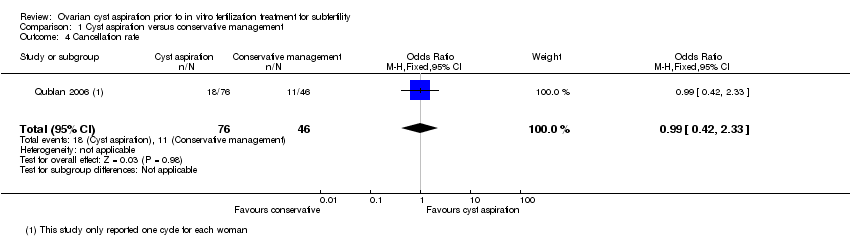
Comparison 1 Cyst aspiration versus conservative management, Outcome 4 Cancellation rate.
| Cyst aspiration versus conservative management for subfertility | ||||||
| Population: women with subfertility | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Conservative management | Cyst aspiration | |||||
| Live birth rate | This primary review outcome was not reported in any of the included studies | Not estimable | ||||
| Adverse events rate | This primary review outcome was not reported in any of the included studies | Not estimable | ||||
| Clinical pregnancy rate | 62 per 1,000 | 72 per 1,000 (21 to 220) | OR 1.19 (0.33 to 4.29) | 159 | ⊕⊝⊝⊝ | |
| Number of follicles recruited | The mean number of follicles recruited in the cyst aspiration groups was | 159 | ⊕⊝⊝⊝ | |||
| Number of oocytes collected | The mean number of oocytes collected in the cyst aspiration groups was | 339 | ⊕⊕⊝⊝ | |||
| Cancellation rate per cycle | 239 per 1,000 | 237 per 1,000 (117 to 423) | OR 0.99 (0.42 to 2.33) | 122 | ⊝⊝⊝⊝ | Each woman had only one cycle |
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level for serious risk of bias; none of the studies adequately described their methods of randomization and allocation concealment | ||||||
| Treatment group | Control | P | |
| Randomised | 90 | 90 | |
| Cycles cancelled prior to egg collection | 2 | 13 | |
| Completed | 88 | 77 | |
| Live birth rate | Not available | Not available | |
| Clinical pregnancy rate | 10.6% | 14.3% | > 0.05 |
| Number of follicles recruited | Not available | Not available | |
| Number of oocytes collected | 5.6±2.1 | 5.2±1.8 | > 0.05 |
| Treatment group | Control | ||
| Randomised | 76 | 46 | |
| Cycle cancelled (poor response) | 17 | 12 | |
| Completed | 59 | 34 | |
| Live birth rate | Not available | Not available | |
| Clinical pregnancy rate | 10.2% | 8.8% | > 0.05 |
| Number of follicles recruited | 5.4 ± 3.1 | 5 ± 2.9 | > 0.05 |
| Number of oocytes collected | 5.6 ± 1.8 | 5.2 ± 2.1 | > 0.05 |
| Treatment group | Control | P | |
| Randomised | 18 | 19 | |
| Discontinued | 0 | 0 | |
| Completed | 18 | 19 | |
| Live birth rate | Not available | Not available | |
| Clinical pregnancy rate | 1 out of 18 (5.56%) | 1 out of 19 (5.26%) | > 0.05 |
| Number of follicles recruited | 10.9 ± 5.33 | 8.9 ± 5.05 | > 0.05 |
| Number of oocytes collected | 7.33 ± 4.0 | 6.7 ± 5.15 | > 0.05 |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical Pregnancy Rate Show forest plot | 2 | 159 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.33, 4.29] |
| 2 Number of Follicles Recruited Show forest plot | 2 | 159 | Mean Difference (IV, Fixed, 95% CI) | 0.55 [‐0.48, 1.59] |
| 3 Number of Oocytes Collected Show forest plot | 3 | 339 | Mean Difference (IV, Fixed, 95% CI) | 0.41 [‐0.04, 0.85] |
| 4 Cancellation rate Show forest plot | 1 | 122 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.42, 2.33] |

