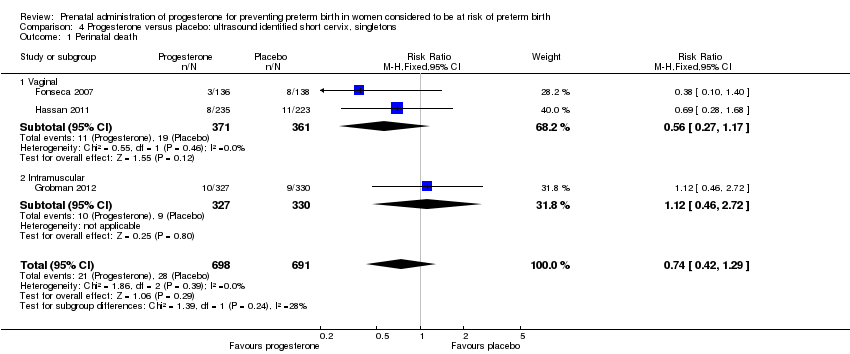
| 1 Perinatal death Show forest plot | 7 | 4136 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.45, 1.94] |
|
| 1.1 Intramuscular | 4 | 2228 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.30, 3.71] |
| 1.2 Vaginal | 3 | 1908 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.24, 2.41] |
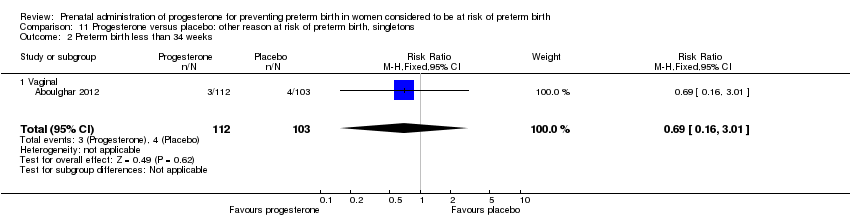
| 2 Preterm birth less than 34 weeks Show forest plot | 6 | 1758 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.74, 1.27] |
|
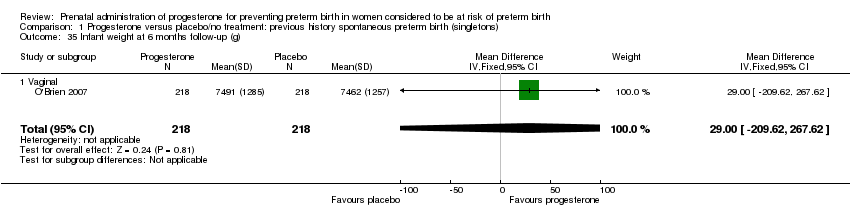
| 2.1 Vaginal | 5 | 1520 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.69, 1.23] |
| 2.2 Intramuscular | 1 | 238 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [0.73, 2.59] |
| 3 Preterm PROM Show forest plot | 3 | 995 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.74, 1.70] |
|
| 3.1 Intramuscular | 2 | 802 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.72, 1.71] |
| 3.2 Vaginal | 1 | 193 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.30, 5.74] |
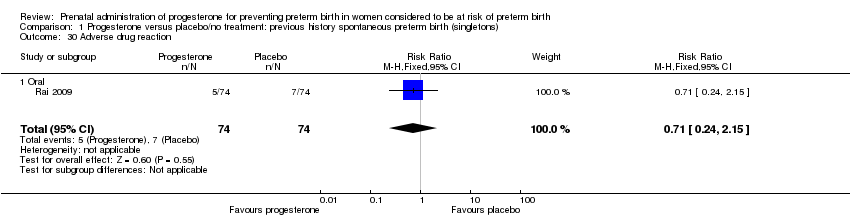
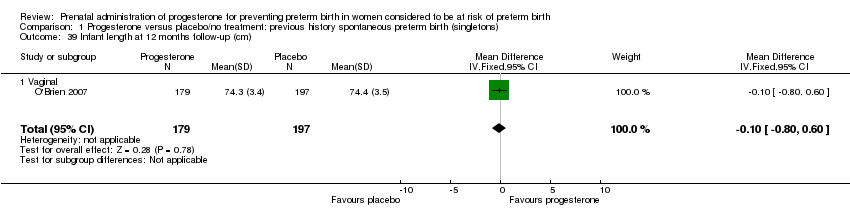
| 4 Adverse drug reaction Show forest plot | 2 | 1162 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.64, 1.19] |
|
| 4.1 Intramuscular | 1 | 668 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.54, 1.01] |
| 4.2 Vaginal | 1 | 494 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.89, 1.08] |
| 5 Caesarean section Show forest plot | 8 | 3136 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.91, 1.02] |
|
| 5.1 Intramuscular | 5 | 1773 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.94, 1.09] |
| 5.2 Vaginal | 3 | 1363 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.84, 0.98] |
| 6 Spontaneous birth Show forest plot | 2 | 1168 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.62, 2.38] |
|
| 6.1 Intramuscular | 1 | 668 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.75, 1.04] |
| 6.2 Vaginal | 1 | 500 | Risk Ratio (M‐H, Random, 95% CI) | 1.74 [1.21, 2.49] |
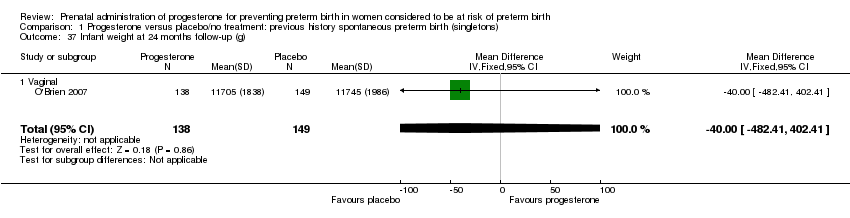
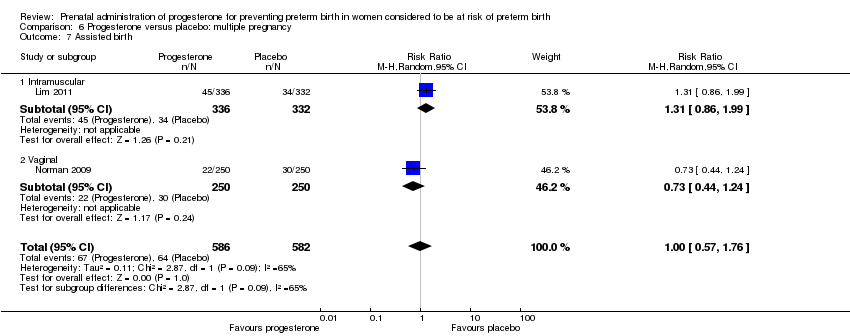
| 7 Assisted birth Show forest plot | 2 | 1168 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.57, 1.76] |
|
| 7.1 Intramuscular | 1 | 668 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [0.86, 1.99] |
| 7.2 Vaginal | 1 | 500 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.44, 1.24] |
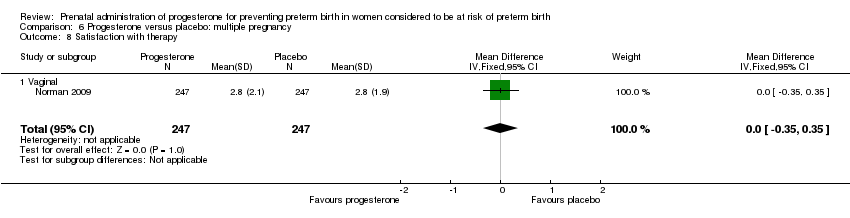
| 8 Satisfaction with therapy Show forest plot | 1 | 494 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.35, 0.35] |
|
| 8.1 Vaginal | 1 | 494 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.35, 0.35] |
| 9 Antenatal tocolysis Show forest plot | 7 | 2642 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.80, 1.10] |
|
| 9.1 Intramuscular | 5 | 1775 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.82, 1.17] |
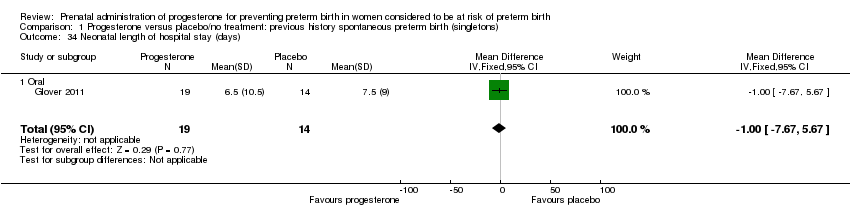
| 9.2 Vaginal | 2 | 867 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.55, 1.03] |
| 10 Antenatal corticosteroids Show forest plot | 2 | 847 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.77, 1.26] |
|
| 10.1 Intramuscular | 1 | 654 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.70, 1.17] |
| 10.2 Vaginal | 1 | 193 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.68 [0.81, 3.49] |
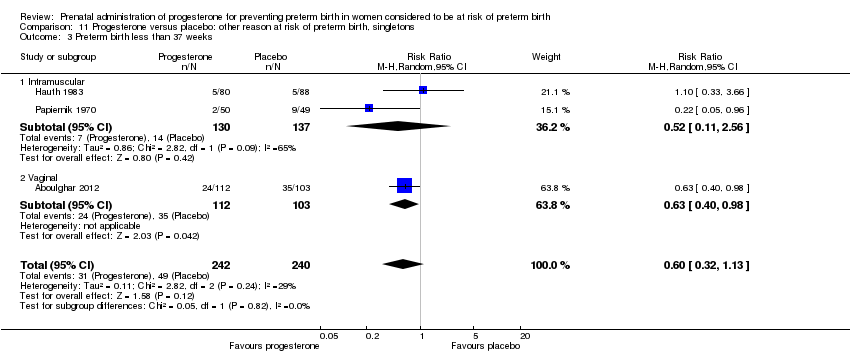
| 11 Preterm birth less than 37 weeks Show forest plot | 8 | 2674 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.95, 1.14] |
|
| 11.1 Intramuscular | 4 | 1638 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.96, 1.22] |
| 11.2 Vaginal | 4 | 1036 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.85, 1.13] |
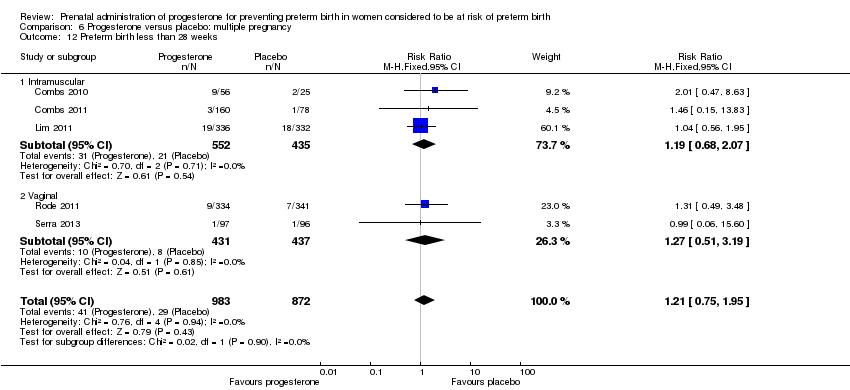
| 12 Preterm birth less than 28 weeks Show forest plot | 5 | 1855 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.75, 1.95] |
|
| 12.1 Intramuscular | 3 | 987 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.68, 2.07] |
| 12.2 Vaginal | 2 | 868 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.51, 3.19] |
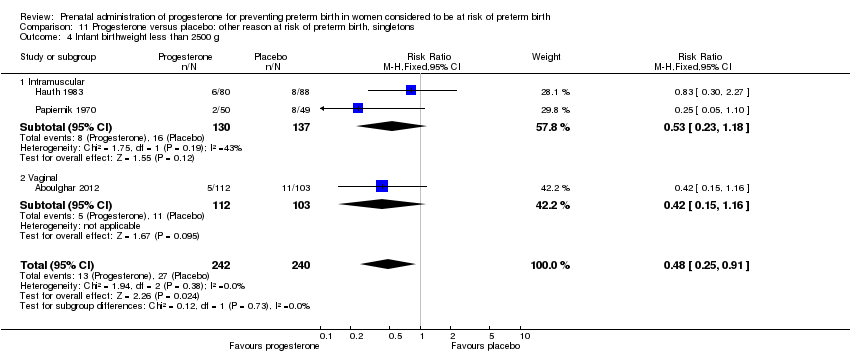
| 13 Infant birthweight less than 2500 g Show forest plot | 7 | 5404 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.88, 1.03] |
|
| 13.1 Intramuscular | 4 | 3502 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.91, 1.14] |
| 13.2 Vaginal | 3 | 1902 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.80, 0.94] |
| 14 Apgar score < 7 at 5 minutes Show forest plot | 4 | 3451 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.66, 1.21] |
|
| 14.1 Intramuscular | 2 | 1750 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.70, 1.38] |
| 14.2 Vaginal | 2 | 1701 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.28, 1.23] |
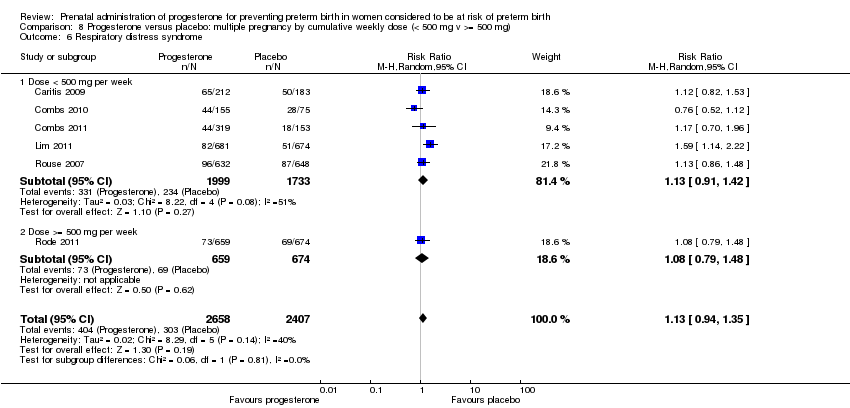
| 15 Respiratory distress syndrome Show forest plot | 6 | 5065 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.94, 1.35] |
|
| 15.1 Intramuscular | 5 | 3732 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.91, 1.42] |
| 15.2 Vaginal | 1 | 1333 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.79, 1.48] |
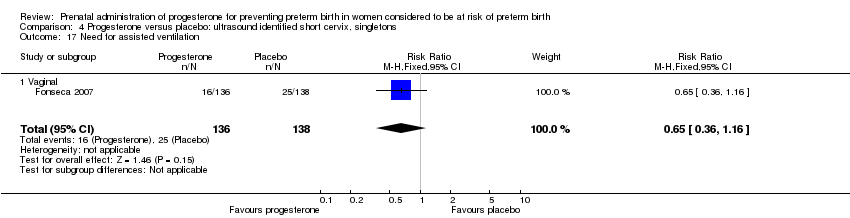
| 16 Use of assisted ventilation Show forest plot | 4 | 3392 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.78, 1.16] |
|
| 16.1 Intramuscular | 2 | 1675 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.80, 1.22] |
| 16.2 Vaginal | 2 | 1717 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.45, 1.36] |
| 17 Intraventricular haemorrhage ‐ grades III or IV Show forest plot | 4 | 2368 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.45, 1.92] |
|
| 17.1 Intramuscular | 4 | 2368 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.45, 1.92] |
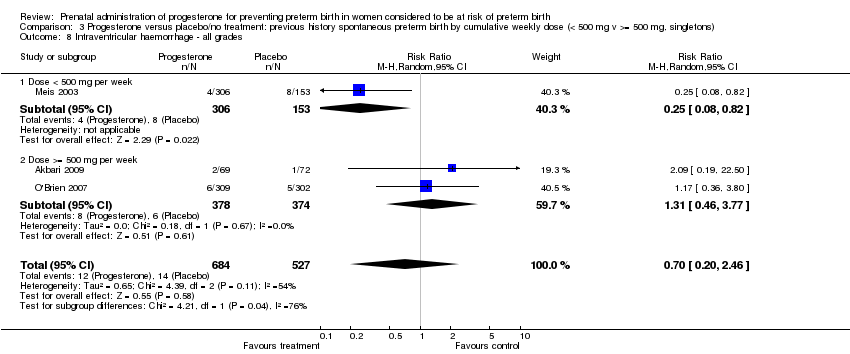
| 18 Intraventricular haemorrhage ‐ all grades Show forest plot | 2 | 2688 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.77 [0.75, 4.21] |
|
| 18.1 Intramuscular | 1 | 1355 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.98 [0.36, 10.77] |
| 18.2 Vaginal | 1 | 1333 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.70 [0.62, 4.66] |
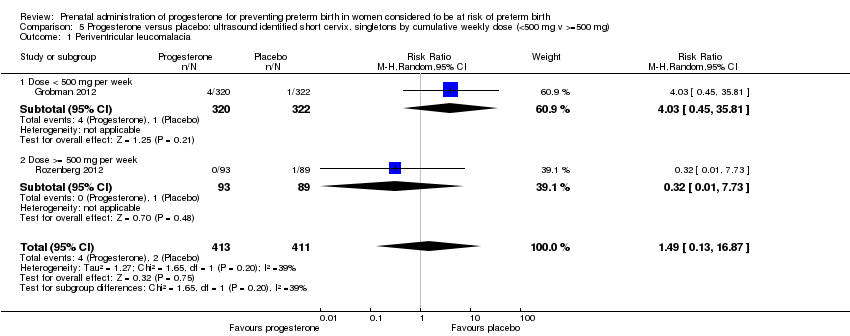
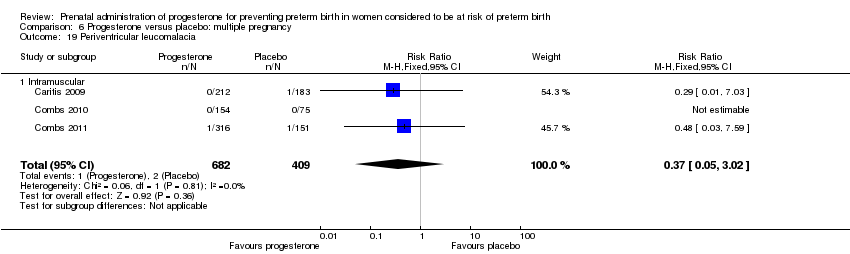
| 19 Periventricular leucomalacia Show forest plot | 3 | 1091 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.05, 3.02] |
|
| 19.1 Intramuscular | 3 | 1091 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.05, 3.02] |
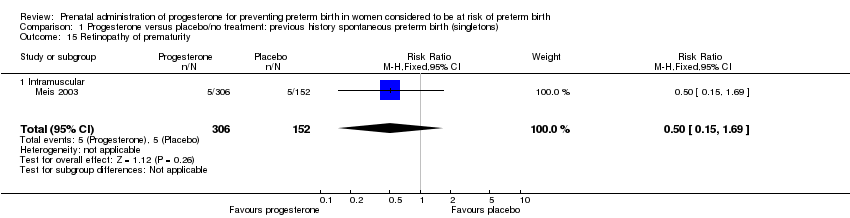
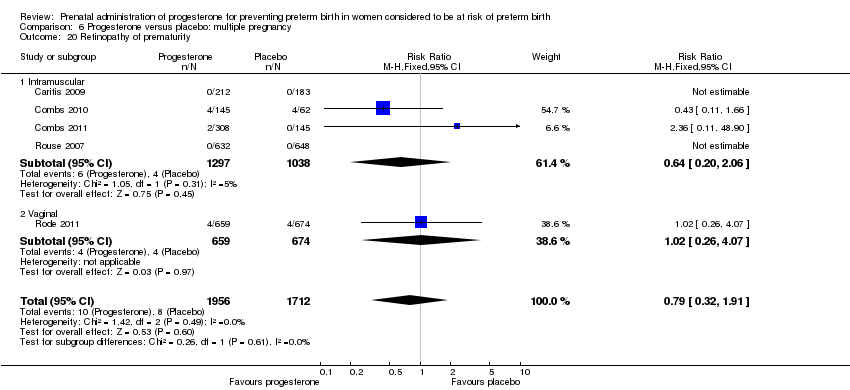
| 20 Retinopathy of prematurity Show forest plot | 5 | 3668 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.32, 1.91] |
|
| 20.1 Intramuscular | 4 | 2335 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.20, 2.06] |
| 20.2 Vaginal | 1 | 1333 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.26, 4.07] |
| 21 Chronic lung disease Show forest plot | 2 | 681 | Risk Ratio (M‐H, Random, 95% CI) | 1.91 [0.13, 27.80] |
|
| 21.1 Intramuscular | 2 | 681 | Risk Ratio (M‐H, Random, 95% CI) | 1.91 [0.13, 27.80] |
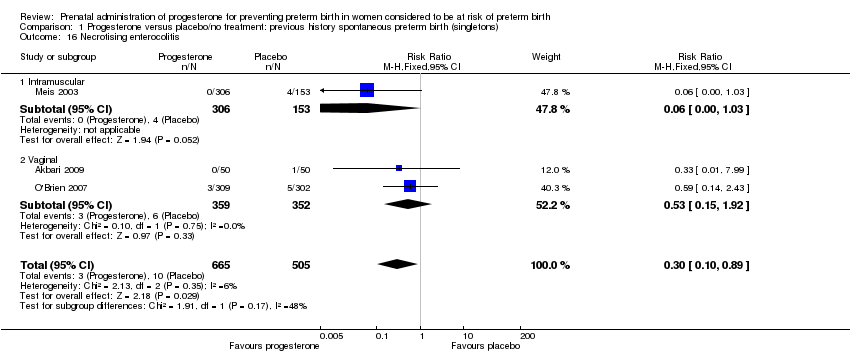
| 22 Necrotising enterocolitis Show forest plot | 6 | 5059 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.50, 1.75] |
|
| 22.1 Intramuscular | 5 | 3726 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.52, 1.88] |
| 22.2 Vaginal | 1 | 1333 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.05, 5.63] |
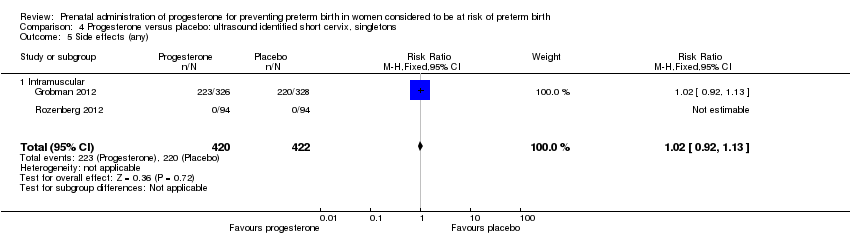
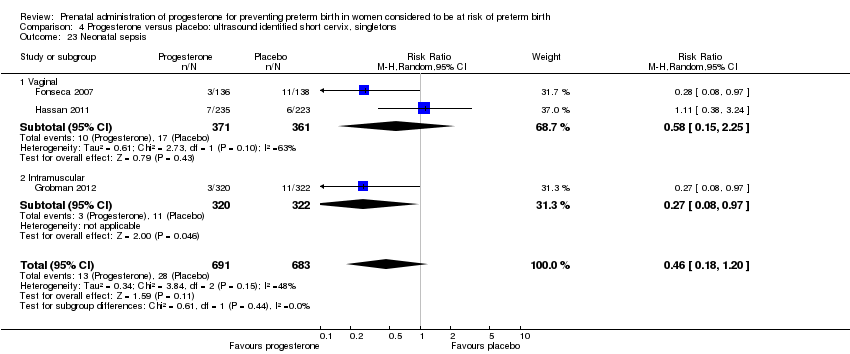
| 23 Neonatal sepsis Show forest plot | 6 | 5065 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.89, 1.62] |
|
| 23.1 Intramuscular | 5 | 3732 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.87, 1.72] |
| 23.2 Vaginal | 1 | 1333 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.61, 2.13] |
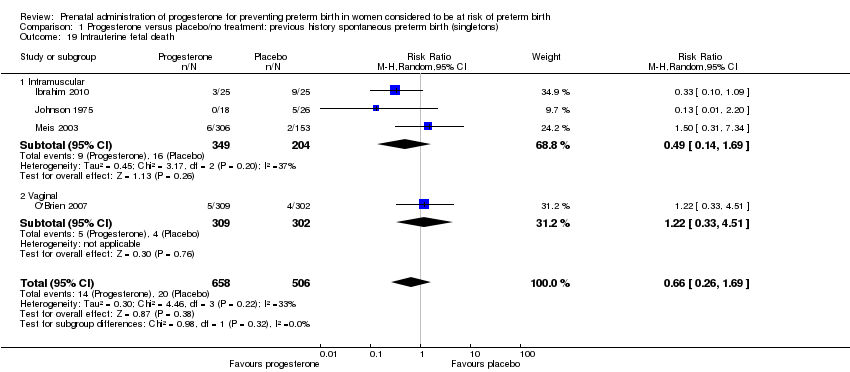
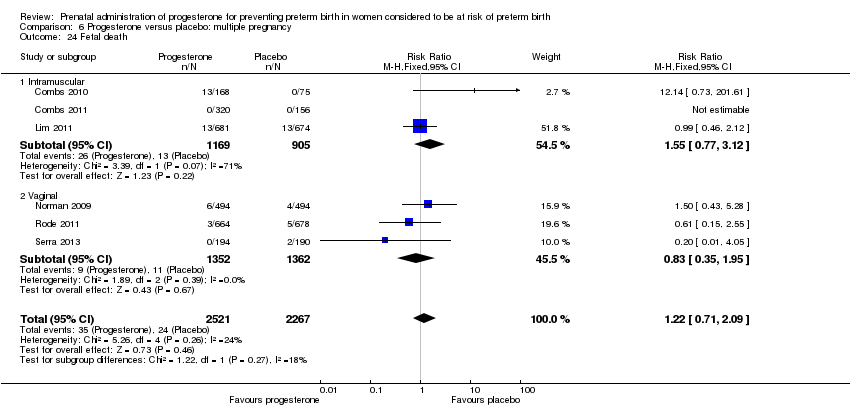
| 24 Fetal death Show forest plot | 6 | 4788 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.71, 2.09] |
|
| 24.1 Intramuscular | 3 | 2074 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.55 [0.77, 3.12] |
| 24.2 Vaginal | 3 | 2714 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.35, 1.95] |
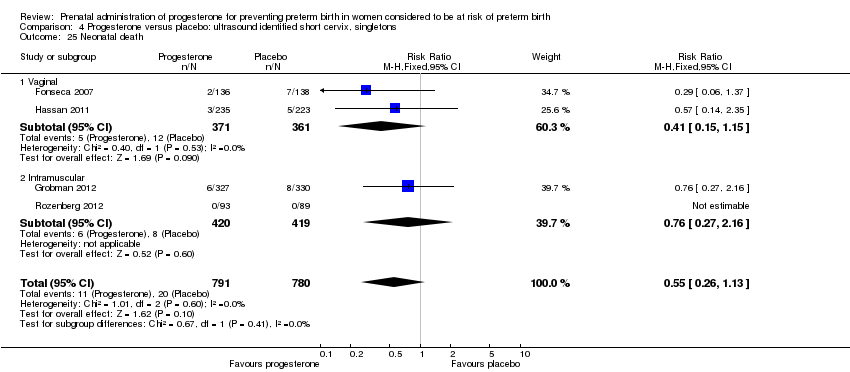
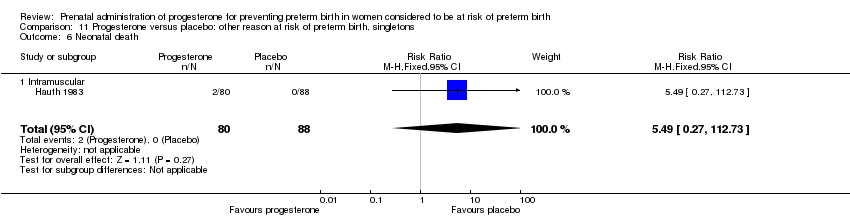
| 25 Neonatal death Show forest plot | 7 | 5170 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.48, 2.10] |
|
| 25.1 Intramuscular | 4 | 2456 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.31, 2.10] |
| 25.2 Vaginal | 3 | 2714 | Risk Ratio (M‐H, Random, 95% CI) | 1.34 [0.36, 4.95] |
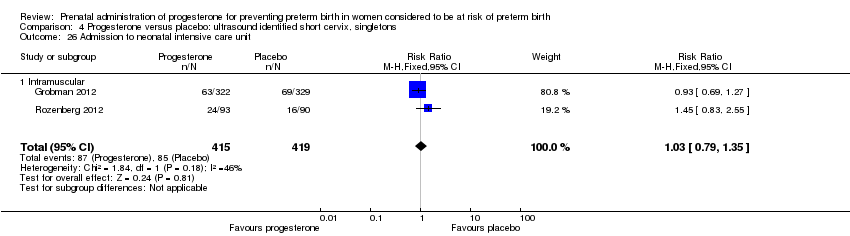
| 26 Admission to NICU Show forest plot | 5 | 4251 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.76, 1.18] |
|
| 26.1 Vaginal | 4 | 2896 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.71, 1.07] |
| 26.2 Intramuscular | 1 | 1355 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [1.05, 1.62] |
| 27 Perinatal death Show forest plot | 7 | 4133 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.61, 2.08] |
|
| 27.1 Intramuscular | 4 | 2228 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.30, 3.71] |
| 27.2 Vaginal | 3 | 1905 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.67, 2.35] |
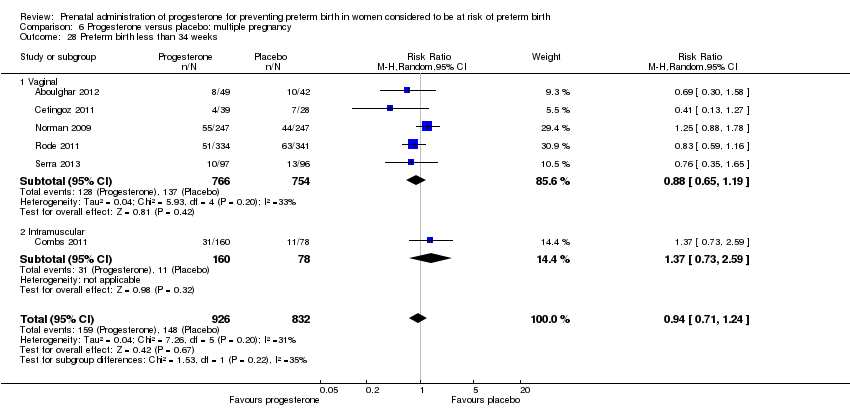
| 28 Preterm birth less than 34 weeks Show forest plot | 6 | 1758 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.71, 1.24] |
|
| 28.1 Vaginal | 5 | 1520 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.65, 1.19] |
| 28.2 Intramuscular | 1 | 238 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [0.73, 2.59] |
| 29 Preterm PROM Show forest plot | 3 | 995 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.69, 1.60] |
|
| 29.1 Intramuscular | 2 | 802 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.72, 1.71] |
| 29.2 Vaginal | 1 | 193 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.03, 3.12] |
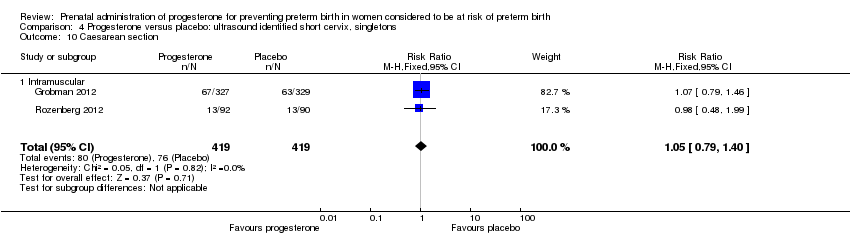
| 30 Caesarean section Show forest plot | 8 | 3136 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.91, 1.01] |
|
| 30.1 Intramuscular | 5 | 1773 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.94, 1.09] |
| 30.2 Vaginal | 3 | 1363 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.84, 0.98] |
| 31 Antenatal tocolysis Show forest plot | 7 | 2642 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.80, 1.10] |
|
| 31.1 Intramuscular | 5 | 1775 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.82, 1.17] |
| 31.2 Vaginal | 2 | 867 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.56, 1.05] |
| 32 Antenatal corticosteroids Show forest plot | 2 | 847 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.76, 1.24] |
|
| 32.1 Intramuscular | 1 | 654 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.70, 1.17] |
| 32.2 Vaginal | 1 | 193 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.58 [0.76, 3.31] |
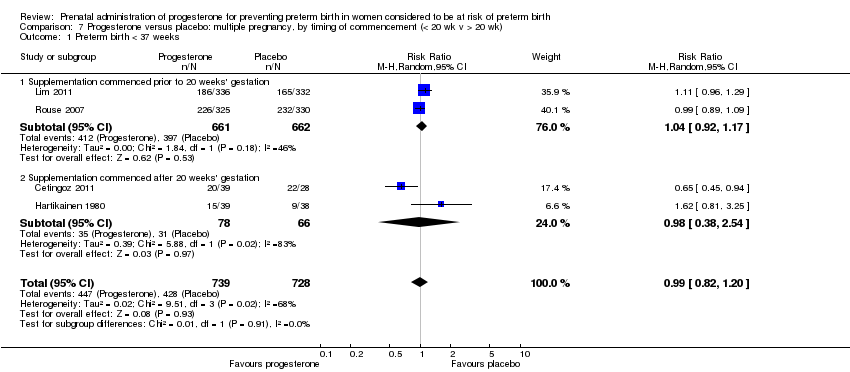
| 33 Preterm birth less than 37 weeks Show forest plot | 8 | 2674 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.95, 1.13] |
|
| 33.1 Intramuscular | 4 | 1638 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.96, 1.22] |
| 33.2 Vaginal | 4 | 1036 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.84, 1.11] |
| 34 Preterm birth less than 28 weeks Show forest plot | 5 | 1855 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.80, 2.04] |
|
| 34.1 Intramuscular | 3 | 987 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.68, 2.07] |
| 34.2 Vaginal | 2 | 868 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [0.63, 3.69] |
| 35 Infant birthweight less than 2500 g Show forest plot | 7 | 5401 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.89, 1.04] |
|
| 35.1 Intramuscular | 4 | 3502 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.91, 1.14] |
| 35.2 Vaginal | 3 | 1899 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.82, 0.96] |
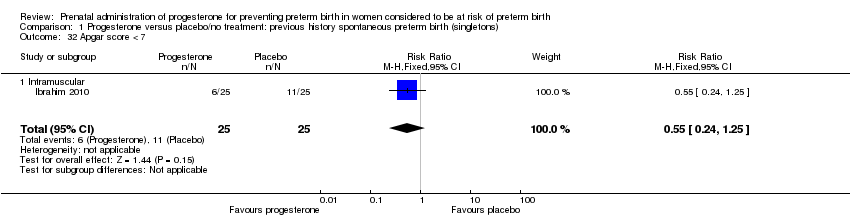
| 36 Apgar score < 7 at 5 minutes Show forest plot | 4 | 3448 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.70, 1.27] |
|
| 36.1 Intramuscular | 2 | 1750 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.70, 1.38] |
| 36.2 Vaginal | 2 | 1698 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.41, 1.58] |
| 37 Use of assisted ventilation Show forest plot | 4 | 3389 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.81, 1.19] |
|
| 37.1 Intramuscular | 2 | 1675 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.80, 1.22] |
| 37.2 Vaginal | 2 | 1714 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.55, 1.59] |
| 38 Fetal death Show forest plot | 6 | 4785 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.35 [0.79, 2.29] |
|
| 38.1 Intramuscular | 3 | 2074 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.55 [0.77, 3.12] |
| 38.2 Vaginal | 3 | 2711 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.49, 2.48] |
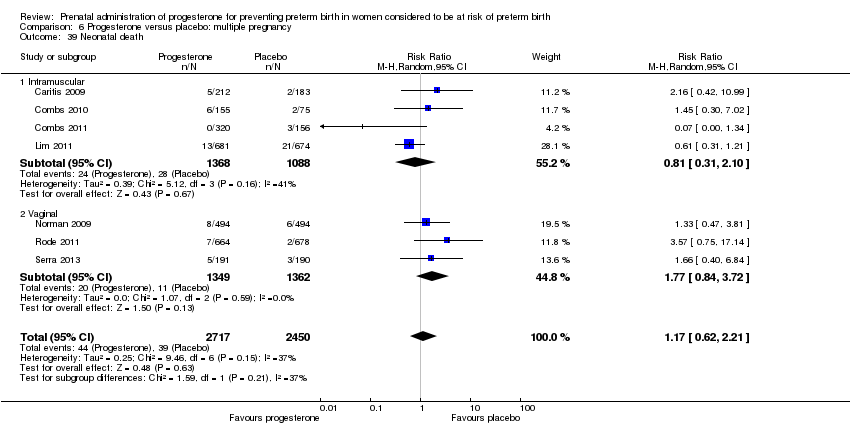
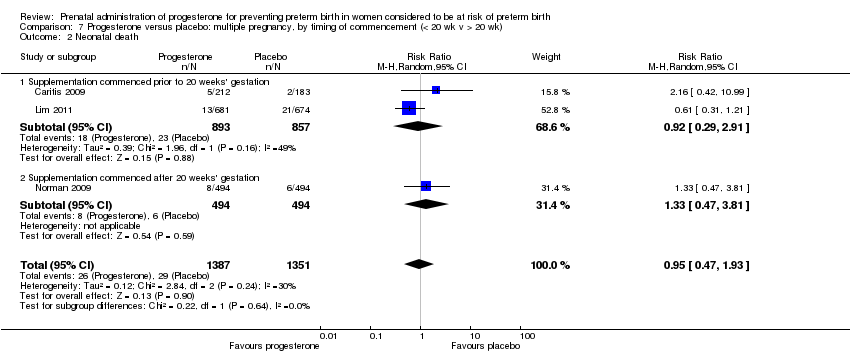
| 39 Neonatal death Show forest plot | 7 | 5167 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [0.62, 2.21] |
|
| 39.1 Intramuscular | 4 | 2456 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.31, 2.10] |
| 39.2 Vaginal | 3 | 2711 | Risk Ratio (M‐H, Random, 95% CI) | 1.77 [0.84, 3.72] |
| 40 Admission to NICU Show forest plot | 5 | 4248 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.75, 1.17] |
|
| 40.1 Vaginal | 4 | 2893 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.70, 1.07] |
| 40.2 Intramuscular | 1 | 1355 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [1.05, 1.62] |
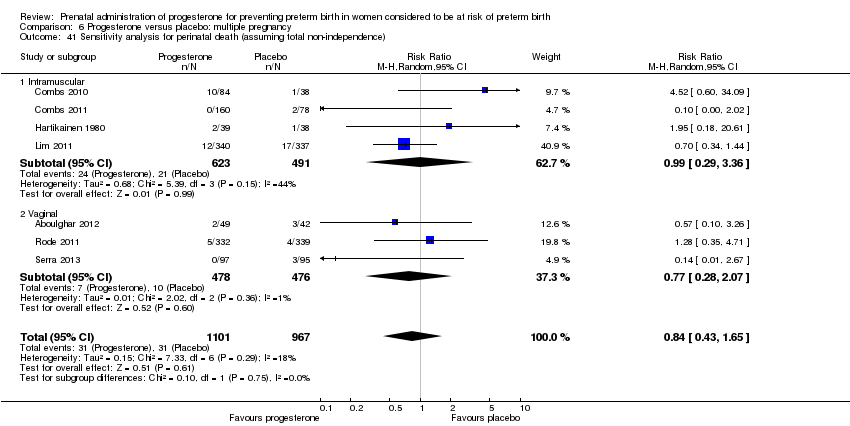
| 41 Sensitivity analysis for perinatal death (assuming total non‐independence) Show forest plot | 7 | 2068 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.43, 1.65] |
|
| 41.1 Intramuscular | 4 | 1114 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.29, 3.36] |
| 41.2 Vaginal | 3 | 954 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.28, 2.07] |
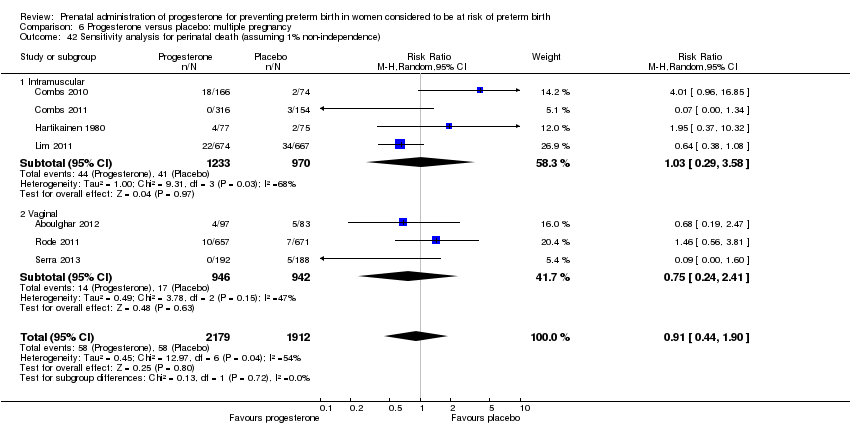
| 42 Sensitivity analysis for perinatal death (assuming 1% non‐independence) Show forest plot | 7 | 4091 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.44, 1.90] |
|
| 42.1 Intramuscular | 4 | 2203 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.29, 3.58] |
| 42.2 Vaginal | 3 | 1888 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.24, 2.41] |