Retention versus sacrifice of the posterior cruciate ligament in total knee arthroplasty for treating osteoarthritis
Información
- DOI:
- https://doi.org/10.1002/14651858.CD004803.pub3Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 11 octubre 2013see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Salud musculoesquelética
- Copyright:
-
- Copyright © 2013 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
Original review
W Jacobs and D Clement: writing the protocol, selecting the studies, extracting data, and writing the manuscript
A Wymenga: clinical interpretation of the results
Update review
W Verra, L vd Boom and W Jacobs: updating the protocol, selecting studies, extracting data, writing manuscript
R Nelissen: writing manuscript, interpretation of results
A Wymenga, D Clement: correcting the manuscript
Declarations of interest
None known
Acknowledgements
We would like to thank JW Schoones, librarian (Walaeus Library, Leiden University Medical Center, Leiden, the Netherlands) for assisting in the searches and arranging reprints, as well as the Cochrane Musculoskeletal Group, especially Ms E Ghogomu for her help in the development of the review.
Version history
| Published | Title | Stage | Authors | Version |
| 2013 Oct 11 | Retention versus sacrifice of the posterior cruciate ligament in total knee arthroplasty for treating osteoarthritis | Review | Wiebe C Verra, Lennard GH van den Boom, Wilco Jacobs, Darren J Clement, Ate AB Wymenga, Rob GHH Nelissen | |
| 2005 Oct 19 | Retention versus sacrifice of the posterior cruciate ligament in total knee replacement for treatment of osteoarthritis and rheumatoid arthritis | Review | Wilco Jacobs, Darren J Clement, Ate AB Wymenga | |
| 2004 Jan 26 | Retention vs sacrifice of the posterior cruciate ligament in total knee replacement for treatment of osteoarthritis and rheumatoid arthritis | Protocol | Wilco CH Jacobs, Patricia G Anderson, Darren J Clement, Ate AB Wymenga | |
Differences between protocol and review
Compared to the protocol, some deviations occurred during the process of developing the review.
First, the decision was made, as requested by the reviewer and editor, to included quasi‐randomised trials.
Furthermore, in accordance with the reviewers and editor, the definitions of the major and minor outcomes changed slightly.
The seven major outcomes now are, 1. performance based: range of motion, 2. patients' experience: knee pain, 3. implant survival rate, 4. validated questionnaires on quality of life or function (that is WOMAC), 5. patient satisfaction, 6. complication rate, 7. re‐operations other than revision surgery.
The 'rheumatoid arthritis' is removed from the title because we felt it did not add anything to the rest of the title.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Humans;
PICO

Bicondylar ligament cruciate retaining balancing total knee arthroplasty with rotating platform (balanSys®, Mathys Ltd., Bettlach, Switzerland) Hirschmann et al. BMC Musculoskeletal Disorders 2010 11:167 doi:10.1186/1471‐2474‐11‐167
Download authors' original image

Study flow diagram (PRISMA).

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
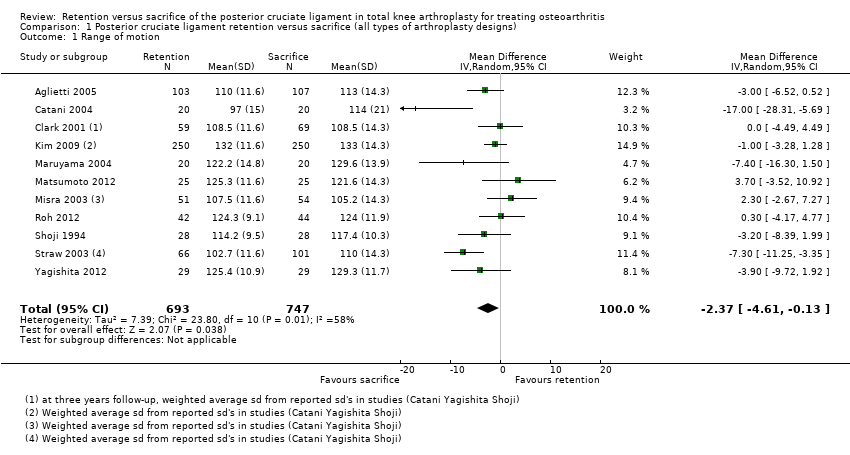
Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 1 Range of motion.
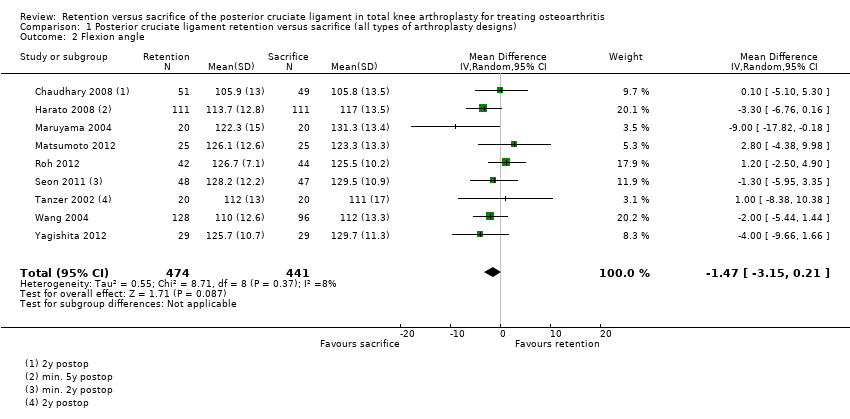
Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 2 Flexion angle.

Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 3 Extension angle.

Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 4 VAS pain.

Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 5 Knee pain (KSS pain).
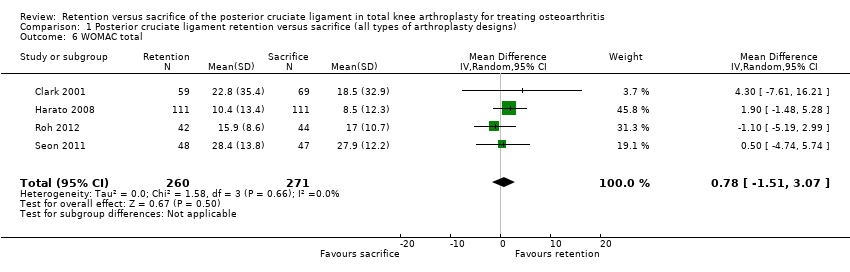
Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 6 WOMAC total.

Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 7 Knee Society Clinical score.
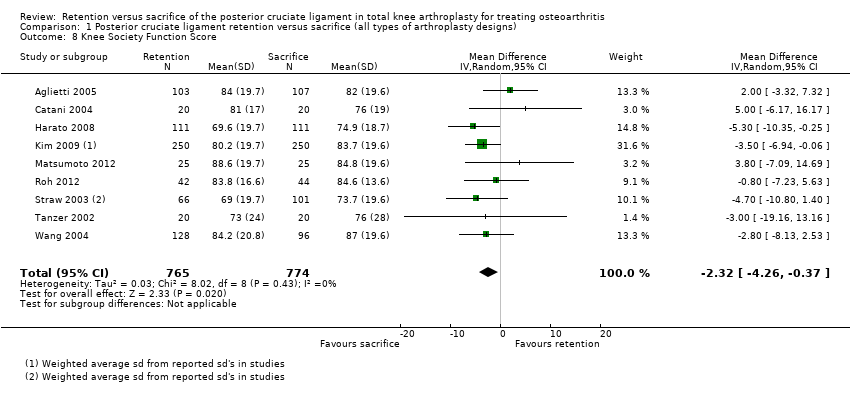
Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 8 Knee Society Function Score.

Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 9 Hospital Special Surgery Score.

Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 10 Knee Society Score overall.

Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 11 SF‐12 mental.

Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 12 Radiological: Radiolucent lines.
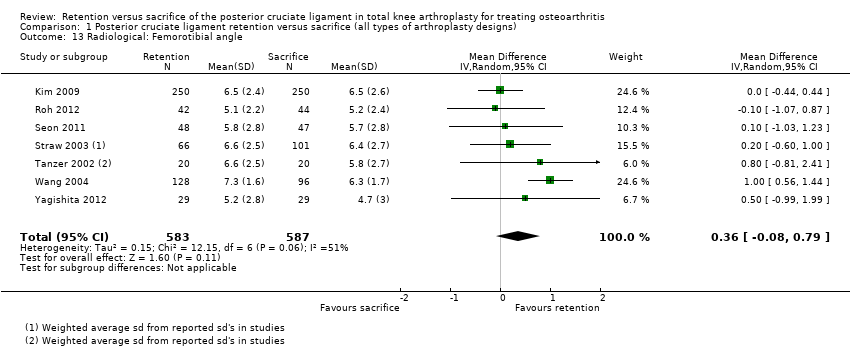
Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 13 Radiological: Femorotibial angle.

Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 14 Radiological: Rollback (in mm).

Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 15 Radiological: Tibial slope.

Comparison 2 Posterior cruciate ligament retention versus sacrifice (using the same arthroplasty design), Outcome 1 Range of motion.

Comparison 2 Posterior cruciate ligament retention versus sacrifice (using the same arthroplasty design), Outcome 2 Improvement of range of motion.

Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 1 Range of motion.

Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 2 Flexion angle.
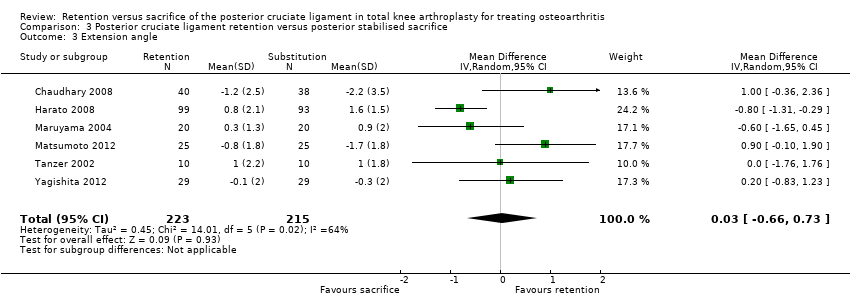
Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 3 Extension angle.

Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 4 VAS pain.

Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 5 Knee pain (KSS pain).
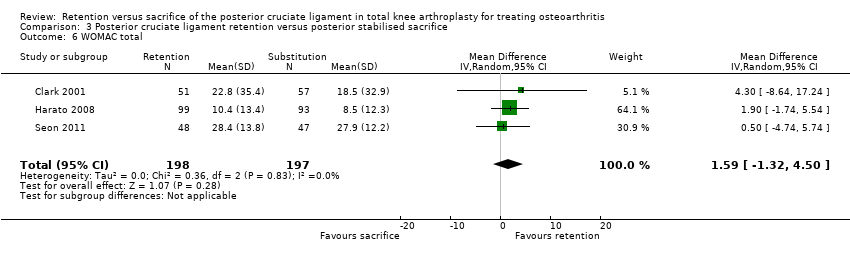
Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 6 WOMAC total.
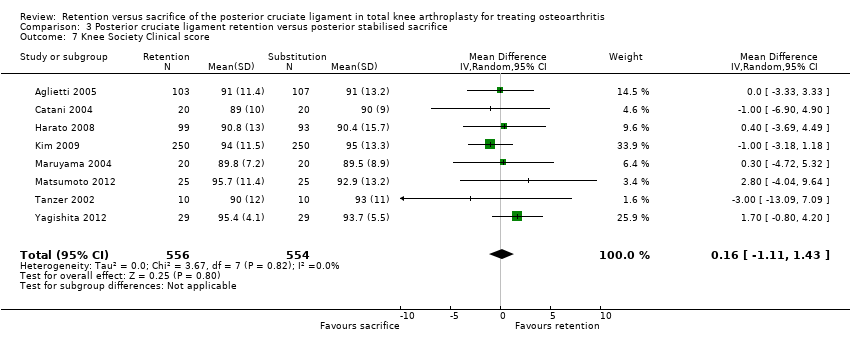
Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 7 Knee Society Clinical score.
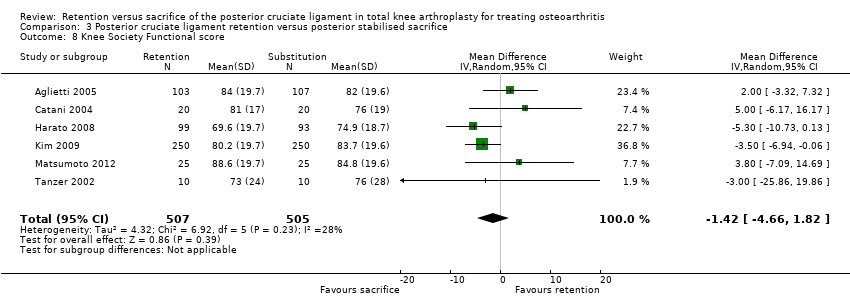
Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 8 Knee Society Functional score.

Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 9 Hospital Special Surgery score.
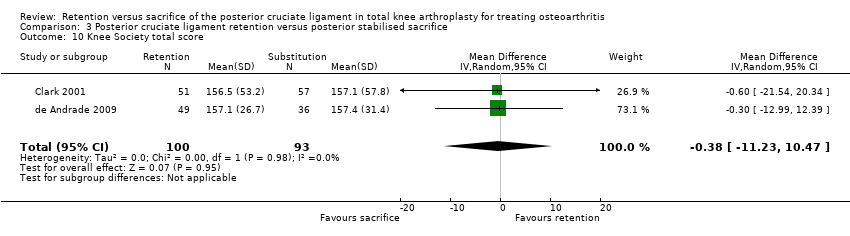
Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 10 Knee Society total score.

Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 11 SF‐12 mental.
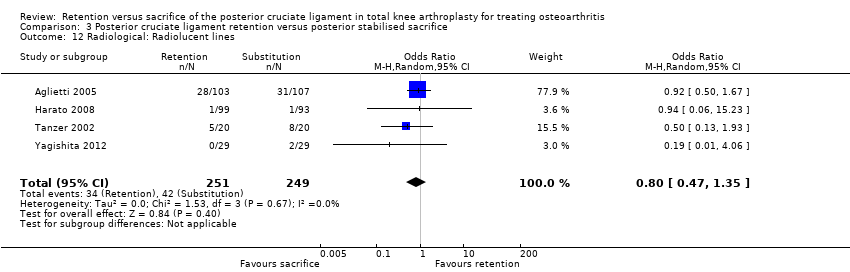
Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 12 Radiological: Radiolucent lines.
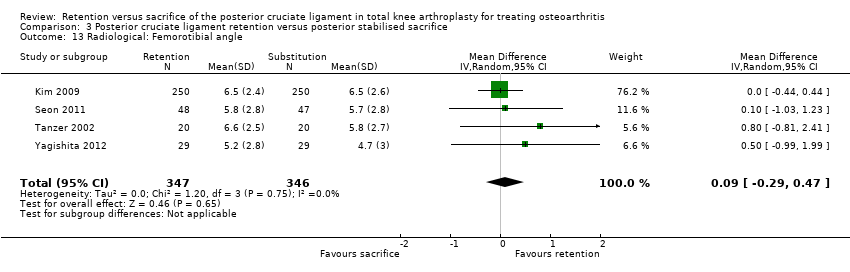
Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 13 Radiological: Femorotibial angle.

Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 14 Radiological: Rollback.
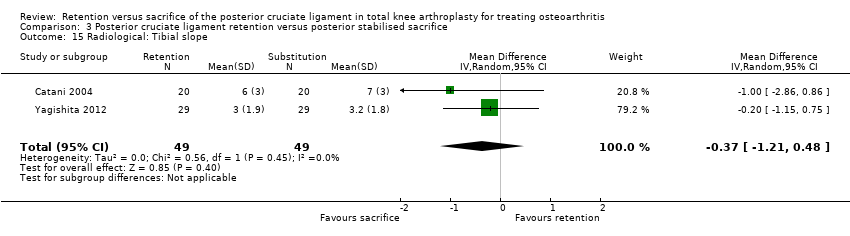
Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 15 Radiological: Tibial slope.
| Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs) | |||||||
| Patient or population: Patients receiving total knee arthroplasty with or without posterior stabilised design for the treatment of osteoarthritis | |||||||
| Outcomes | Comparative risks | Relative effect | No. of patients (% of total) | No. of studies (% of total) | Quality of the evidence | Comments | |
| Cruciate‐sacrifice | Cruciate‐retention | ||||||
| Performance based measures ‐ Range of motion (possible range 0 (worst) to 140 (maximal) degrees) Follow‐up: 12‐78 months1 | The mean range of motion in the cruciate‐sacrifice group was 118.3 degrees (± SE 0.53) | The mean range of motion in the cruciate‐retaining group 2.40 lower (4.61 lower to 0.13 higher) | Total No. of patients: 1,119 (62%) Total No. of knees: 1,440 (65%) | 11 studies (65%) | ⊕⊕⊝⊝ | Absolute difference 2.40 lower (4.61 lower to 0.13 higher) Relative percent change: ‐2.0% (3.9% lower to 0.1% higher) Not statistically significant. | |
| Knee pain Knee Society Score, sub score pain (possible range of points 0 (severe pain) ‐ 50 (no pain)) Follow‐up: 24‐87 months years | The mean knee pain score in the cruciate‐sacrifice group was 48.3 points (± SE 0.54) | The mean knee pain score in the cruciate‐retention group was 0.01 higher (1.40 lower to 1.43 higher) | Total No. of patients: 656 (36%) Total No. of knees: 1,004 (46%) | 4 studies (24%) | ⊕⊕⊕⊝ | Absolute difference: 0.01 higher (1.40 lower to 1.43 higher) Relative percent change: 0.0% (2.9% lower to 3.0% higher) Not statistically significant. | |
| Survival rate of the implant (Revision surgery reported) Follow‐up: 17‐87 months | See comment | See comment | Not estimable | Total No. of patients: 926 (51%) Total No. of knees: 1,229 (56%) | 7 studies (41%) | See comment | Insufficient data provided. Incidental remarks on implant survival could be derived from 7 studies. One study Misra 2003 reported 2 revisions in de cruciate‐retention group, Chaudhary 2008 1 in the cruciate‐retention group, Harato 2008 1 in the cruciate‐retention group and 3 in the sacrifice group. Aglietti 2005 1 revision in the cruciate‐sacrifice group due to septic loosening Kim 2009, Yagishita 2012 and Tanzer 2002 specifically reported no revision surgery had occurred during follow‐up |
| Health related quality of life measures and functional measures with validated instruments (WOMAC, range 0‐100, higher scores indicate worse pain, stiffness and functional limitations) Follow‐up: 24‐87 months | The mean WOMAC total score in the cruciate‐sacrifice group was 15.0 points (± SE 1.2) | The mean WOMAC total score in the cruciate‐retention group was 0.78 higher (1.51 lower to 3.07 higher) | Total No. of patients: 501 (28%) Total No. of knees: 531 (24%) | 4 studies (24%) | ⊕⊕⊝⊝ | Absolute difference: 0.78 higher (1.51 lower to 3.07 higher) Relative percent change: 5.2% (10.0% lower to 20.5% higher) Not statistically significant. | |
| Global assessment (patient) Patient satisfaction on scale 0 (not at all satisfied) to 10 (completely satisfied) Follow‐up: 12‐83 months | The mean satisfaction score in the cruciate‐sacrifice group was 7.910 | The mean satisfaction score in the cruciate‐retention group was 0.2 lower10 | Total No. of patients: 103 (6%) Total No. of knees: 105 (5%) | 1 study (6%) | ⊕⊕⊝⊝ | Absolute difference: 0.2 lower 10 Relative percent change: ‐2.5% 10 Not statistically significant. | |
| Complications Follow‐up: 8‐87 months7 | See comment | See comment | Not estimable | Total No. of patients: 1,252 (69%) Total No. of knees: 1,635 (74%) | 11 studies (65%) | See comment | Due to the very diverse way of reporting and defining complications combining data for quantitative analysis was not possible8,9 |
| Re‐operation rate (not involving implant change, short and long term) Follow‐up: 24 months | See comment | See comment | Not estimable | Total No. of patients: 40 (2%) | 1 study (6%) | See comment | Catani 2004 reported 4 re‐operations; 3 patella luxations (2 in cruciate‐sacrificing, 1 in cruciate‐retention group) and 1 surgical manipulation due to lack of range of motion (in the cruciate‐retention group) |
| CI: Confidence interval; KSS: Knee Society Score, WOMAC: Western Ontario and McMasters Universities Osteoarthritis Index. NA: not applicable | |||||||
| GRADE Working Group grades of evidence | |||||||
| 1 Median follow‐up: 2 years 7 Some studies reported complications after several months. Mean follow‐up of other endpoints was > 1 year 8 Complications reported in the cruciate‐sacrifice group: 4 anterior knee pain, 4 limited range of motion, 1 deep venous thrombosis, 3 instability, 3 femoral notching, 3 aseptic loosening, 3 (deep) infection 9 Complications reported in the cruciate‐retention group: 6 anterior knee pain, 10 limited range of motion, 0 deep venous thrombosis, 3 instability, 2 femoral notching, 2 aseptic loosening, 3 (deep) infection, 2 ligament laxity, 1 ligament tightness 10 Not sufficient data reported to calculate standard error, range or confidence interval | |||||||
| Posterior cruciate ligament retention versus sacrifice (using the same arthroplasty design) | |||||||
| Patient or population: Patients receiving total knee arthroplasty with or without resection of the posterior cruciate ligament for the treatment of osteoarthritis | |||||||
| Outcomes | Comparative risks | Relative effect | No. of patients (% of total) | No of studies (% of total) | Quality of the evidence | Comments | |
| Cruciate‐sacrifice | Cruciate‐retention | ||||||
| Performance based measures ‐ Range of motion (possible range 0 (worst) to 140 (maximal) degrees) Follow‐up: 12‐78 months | The mean range of motion in the cruciate‐sacrifice group was 114.1 degrees (± SE 0.82) | The mean range of motion in the cruciate‐retention group was 2.7 degrees lower (8.71 lower to 3.32 higher) | Total No. of patients: 405 (22%) Total No. of knees: 414 (19%) | 4 studies (24%) | ⊕⊝⊝⊝ | Absolute difference: 2.7 degrees lower (8.71 lower to 3.32 higher) Relative percent change: ‐2.4% (7.6% lower to 2.9% higher) Not statistically significant. | |
| Knee pain Knee Society Score, sub score pain (possible range 0 (severe pain) ‐ 50 (no pain) points) | See comment | See comment | Not estimable | ‐ | ‐ | See comment | No data in studies comparing ligament resection and sacrifice using similar arthroplasty designs |
| Survival rate of the implant (Revision surgery reported) Follow‐up: 56‐60 months | See comment | See comment | Not estimable | Total No. of patients: 103 (6%) Total No. of knees: 105 (5%) | 1 study (6%) | See comment | Insufficient data provided. One study (Misra 2003) reported 2 revisions in the cruciate‐retention group. |
| Health related quality of life measures and functional measures with validated instruments (WOMAC, range 0‐100, higher scores indicate worse pain, stiffness and functional limitations) Follow‐up: 24‐37 months | The mean WOMAC total score in the cruciate‐sacrifice group was 17.0 points (± SE 1.1) | The mean WOMAC total score in the cruciate‐retention group was 1.10 lower (‐5.19 lower to 2.99 higher) | Total No. of patients: 86 (5%) Total No. of knees: 86 (4%) | 1 study (6%) | See comment | One study reported this outcome: Roh 2012 Absolute difference: 1.10 lower (‐5.19 lower to 2.99 higher) Relative percent change: ‐6.5% (30.5% lower to 17.6%higher) Not statisitically significant | |
| Global assessment (patient) Patient satisfaction on scale 0 (not at all satisfied) to 10 (completely satisfied)) Follow‐up: 12‐83 months | The mean satisfaction score in the cruciate‐sacrifice group was 7.97 | The mean satisfaction score in the cruciate‐retention group was 0.2 lower7 | Total No. of patients: 103 (6%) Total No. of knees: 105 (5%) | 1 study (6%) | ⊕⊕⊝⊝ | Absolute difference: 0.2 lower 7 Relative percent change: ‐2.5% 7 Not statistically significant. | |
| Complications Follow‐up: 12‐78 months | See comment | See comment | Not estimable | Total No. of patients: 405 (22%) Total No. of knees: 414 (19%) | 4 studies (24%) | See comment | Due to the very diverse way of reporting and defining complications combining data for quantitative analysis was not possible5,6 |
| Re‐operation rate (not involving implant change, short and long term) | See comment | See comment | Not estimable | ‐ | ‐ | See comment | No data in studies comparing ligament resection and sacrifice using similar arthroplasty designs |
| CI: Confidence interval. KSS: Knee Society Score, WOMAC: Western Ontaria and McMasters Universities Osteoarthritis Index. NA: not applicable | |||||||
| GRADE Working Group grades of evidence | |||||||
| 1 Risk of bias individual studies, see risk of bias tables 5 Complications reported in the cruciate‐sacrifice group: 3 instability, 3 aseptic loosening, 2 stiffness 6 Complications reported in the cruciate‐retention group: 3 instability, 1 infection (deep), 2 aseptic loosening, 2 stiffness, 2 ligament laxity, 1 ligament tightness 7 Not sufficient data reported to calculate standard error, range or confidence interval | |||||||
| Posterior cruciate ligament retention versus posterior stabilised sacrifice | |||||||
| Patient or population: Patients receiving total knee arthroplasty with or without posterior stabilised design for the treatment of osteoarthritis | |||||||
| Outcomes | Mean differences (95% CI) | Relative effect | No. of patients (% of total) | No. of studies (% of total) | Quality of the evidence | Comments | |
| Cruciate‐sacrifice (posterior stabilised) | Cruciate‐retention | ||||||
| Performance based measures ‐ Range of motion (possible range 0 (worst) to 140 (maximal) degrees) Follow‐up: 1‐6.5 years1 | The mean range of motion in the cruciate‐sacrifice group was 119.8 degrees (± SE 0.66) | The mean range of motion in the cruciate‐retention group was 3.4 degrees lower (6.32 to 0.54 lower) | Total No. of patients: 899 (50%) Total No. of knees: 1,193 (54%) | 8 studies (47%) | ⊕⊕⊕⊝ | Absolute difference: ‐3.4 degrees (6.32 to 0.54 lower) Relative percent change: ‐2.8% (5.3% lower to 0.45% higher) Statistically significant (P = 0.02) NNTB: 9 (5 to 51) | |
| Knee pain Knee Society Score, subscore pain (possible range 0 (severe pain) ‐ 50 (no pain) points) Follow‐up: 2‐7.3 years | The mean knee pain score in the cruciate‐sacrifice group was 48.3 points (± SE 0.68) | The mean knee pain score in the cruciate‐retention group was 0.60 higher (0.39 lower to 1.60 higher) | Total No. of patients: 471 (26%) Total No. of knees: 780 (35%) | 3 studies | ⊕⊕⊕⊝ | Absolute difference: 0.60 (0.39 lower to 1.60 higher) Relative percent change: 1.2% (0.81% lower to 3.3% higher) Not statistically significant. | |
| Survival rate of the implant (Revision surgery reported) | See comment | See comment | Not estimable | Total No. of patients: 802 (44%) Total No. of knees: 1,100 (50%) | 6 studies (35%) | See comment | Insufficient data provided. Incidental remarks on implant survival could be derived from 6 studies. Chaudhary 2008 1 in the cruciate‐retention group, Harato 2008 1 in the cruciate‐retention group and 3 in the sacrifice group. Aglietti 2005 1 revision in the cruciate‐sacrifice group due to septic loosening Kim 2009, Yagishita 2012 and Tanzer 2002 specifically reported no revision surgery had occurred during follow‐up |
| Health related quality of life measures and functional measures with validated instruments (WOMAC, range 0‐100, higher scores indicate worse pain, stiffness and functional limitations) Follow‐up: 24‐87 months | The mean WOMAC total score in the cruciate‐sacrifice group was 18.2 points(± SE 1.5) | The mean WOMAC total score in the cruciate‐retention group was 1.60 lower (1.32 lower to 4.50 higher) | Total No. of patients: 415 (23%) Total No. of knees: 445 (20%) | 3 studies (18%) | ⊕⊕⊝⊝ | Absolute difference: 1.60 lower (1.32 lower to 4.50 higher) Relative percent change: ‐8.8% (7.3% lower to 24.7% higher) Not statistically significant. | |
| Global assessment (patient) | See comment | See comment | Not estimable | ‐ | ‐ | See comment | No data in studies comparing ligament resection and sacrifice using similar arthroplasty designs |
| Complications Follow‐up: 8‐87 months5 | See comment | See comment | Not estimable | Total No. of patients: 878 (49%) Total No. of knees: 1,220 (55%) | 8 studies (47%) | See comment | Due to the very diverse way of reporting and defining complications combining data for quantitative analysis was not possible3,4 |
| Re‐operation rate (not involving implant change, short‐ and long‐term) Follow‐up: 24 months | See comment | See comment | Not estimable | Total No. of patients: 40 (2%) | 1 study (6%) | See comment | Catani 2004 reported 4 re‐operations; 3 patella luxations (2 in cruciate‐sacrificing, 1 in cruciate‐retention group) and 1 surgical manipulation due to lack of range of motion (in the cruciate‐retention group) |
| CI: Confidence interval. KSS: Knee Society Score, WOMAC: Western Ontaria and McMasters Universities Osteoarthritis Index. ROM range of motion NA: not applicable | |||||||
| GRADE Working Group grades of evidence | |||||||
| 1 Relatively many studies with 'unclear' risk of bias 2 < 400 arthroplasties in analysis 3 Complications reported in the cruciate‐sacrifice group: 2 anterior knee pain, 3 femoral notching, 1 superficial wound infection, 2 deep venous thrombosis, 1 septic loosening 4 Complications reported in the cruciate‐retention group: 1 anterior knee pain, 1 limited ROM, 2 femoral notching, 1 superficial wound infection 5 Some studies reported complications after several months. Mean follow‐up of other endpoints was > 1 year | |||||||
| Study | Description patients | Intervention described | Outcome measures | Effect size |
| Are the patients described in detail so that you can decide whether they are comparable to those that you see in your practice? | Are the interventions and treatment settings described well enough so that you can provide the same for your patients? | Were all clinically relevant outcomes measured and reported? | Is the size of the effect clinically important? | |
| Aglietti 2004 | No | Yes | Yes | No |
| Catani 2004 | No | No | No | Yes |
| Chaudhary 2008 | Yes | Yes | Yes | No |
| Clark 2001 | Unsure | Yes | No | No |
| de Andrade 2009 | Unsure | Unsure | No | No |
| Harato 2008 | Unsure | Yes | Yes | No |
| Kim 2009 | Yes | Yes | Yes | No |
| Maruyama 2004 | Yes | Yes | Yes | No |
| Matsumoto 2012 | Yes | Unsure | Yes | No |
| Misra 2003 | No | No | No | No |
| Roh 2012 | Yes | Yes | Yes | No |
| Seon 2011 | Yes | Unsure | Yes | Yes |
| Shoji 1994 | No | No | No | No |
| Straw 2003 | No | Unsure | No | No |
| Tanzer 2002 | Yes | Yes | No | No |
| Wang 2004 | Yes | No | Yes | No |
| Yagishita 2011 | Yes | Yes | Yes | No |
| Study | Complications posterior cruciate ligament retention | Complications posterior cruciate ligament sacrifice |
| Aglietti 2004 | None | 1 Septic loosening after 2 years requiring 2‐stage revision surgery |
| Catani 2004 | 1 Anterior knee pain; treated: lateral release and patella resurfacing, 1 Limited range of motion; treated: surgical manipulation | 2 Anterior knee pain; treated: lateral release and patella resurfacing |
| Chaudhary 2008 | 1 Deep infection | 1 Limited range of motion (poor flexion); treated: surgical manipulation |
| Clark 2001 | Not reported | Not reported |
| de Andrade 2009 | Not reported | Not reported |
| Harato 2008 | 7 Stiff knee (<90 degrees flexion), 5 severe/moderate knee pain, 1 infection 2 Hemoarthrosis | 1 Deep venous thrombosis, 3 infection, 1 stiff knee (<90 degrees flexion) 2 Severe/moderate knee pain |
| Kim 2009 | 2 Femoral notching, 1 superficial wound infection | 3 Femoral notching, 1 superficial wound infection |
| Maruyama 2004 | None | None |
| Matsumoto 2012 | None | 1 Deep venous thrombosis |
| Misra 2003 | 3 Instability, 1 infection, 2 aseptic loosening, 2 stiffness (<30 degrees flexion) | 3 Instability, 3 aseptic loosening, 2 stiffness (<30 degrees flexion), 1 Reflex sympathetic dystrophy |
| Roh 2012 | 2 posterior cruciate laxity 1 posterior cruciate tightness | None |
| Seon 2011 | Not reported | Not reported |
| Shoji 1994 | Not reported | Not reported |
| Straw 2003 | Not reported | Not reported |
| Tanzer 2002 | Not reported | Not reported |
| Wang 2004 | Not specified per treatment group: 3 deaths unrelated to the knee surgery, 3 deep wound infections, 1 above the knee amputation due to diabetic gangrene, 1 cerebral vascular accident, 1 Parkinsons disease, 1 colon cancer | |
| Yagishita 2011 | None | 1 Deep venous thrombosis |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Range of motion Show forest plot | 11 | 1440 | Mean Difference (IV, Random, 95% CI) | ‐2.37 [‐4.61, ‐0.13] |
| 2 Flexion angle Show forest plot | 9 | 915 | Mean Difference (IV, Random, 95% CI) | ‐1.47 [‐3.15, 0.21] |
| 3 Extension angle Show forest plot | 7 | 734 | Mean Difference (IV, Random, 95% CI) | 0.36 [‐0.61, 1.32] |
| 4 VAS pain Show forest plot | 2 | 268 | Mean Difference (IV, Random, 95% CI) | 1.50 [‐1.84, 4.84] |
| 5 Knee pain (KSS pain) Show forest plot | 4 | 1004 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐1.40, 1.43] |
| 6 WOMAC total Show forest plot | 4 | 531 | Mean Difference (IV, Random, 95% CI) | 0.78 [‐1.51, 3.07] |
| 7 Knee Society Clinical score Show forest plot | 11 | 1637 | Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.93, 0.77] |
| 8 Knee Society Function Score Show forest plot | 9 | 1539 | Mean Difference (IV, Random, 95% CI) | ‐2.32 [‐4.26, ‐0.37] |
| 9 Hospital Special Surgery Score Show forest plot | 6 | 882 | Mean Difference (IV, Random, 95% CI) | ‐0.51 [‐1.55, 0.54] |
| 10 Knee Society Score overall Show forest plot | 2 | 213 | Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐10.80, 10.03] |
| 11 SF‐12 mental Show forest plot | 2 | 350 | Mean Difference (IV, Random, 95% CI) | 0.41 [‐5.08, 5.89] |
| 12 Radiological: Radiolucent lines Show forest plot | 5 | 754 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.68, 1.07] |
| 13 Radiological: Femorotibial angle Show forest plot | 7 | 1170 | Mean Difference (IV, Random, 95% CI) | 0.36 [‐0.08, 0.79] |
| 14 Radiological: Rollback (in mm) Show forest plot | 2 | 110 | Mean Difference (IV, Random, 95% CI) | 2.78 [‐9.57, 15.13] |
| 15 Radiological: Tibial slope Show forest plot | 2 | 98 | Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐1.21, 0.48] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Range of motion Show forest plot | 4 | 372 | Mean Difference (IV, Random, 95% CI) | ‐2.70 [‐8.71, 3.32] |
| 2 Improvement of range of motion Show forest plot | 2 | 161 | Mean Difference (IV, Random, 95% CI) | 1.92 [‐6.25, 10.08] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Range of motion Show forest plot | 8 | 1193 | Mean Difference (IV, Random, 95% CI) | ‐3.43 [‐6.32, ‐0.54] |
| 2 Flexion angle Show forest plot | 7 | 605 | Mean Difference (IV, Random, 95% CI) | ‐2.07 [‐4.17, 0.04] |
| 3 Extension angle Show forest plot | 6 | 438 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.66, 0.73] |
| 4 VAS pain Show forest plot | 2 | 268 | Mean Difference (IV, Random, 95% CI) | 1.50 [‐1.84, 4.84] |
| 5 Knee pain (KSS pain) Show forest plot | 3 | 750 | Mean Difference (IV, Random, 95% CI) | 0.60 [‐0.39, 1.60] |
| 6 WOMAC total Show forest plot | 3 | 395 | Mean Difference (IV, Random, 95% CI) | 1.59 [‐1.32, 4.50] |
| 7 Knee Society Clinical score Show forest plot | 8 | 1110 | Mean Difference (IV, Random, 95% CI) | 0.16 [‐1.11, 1.43] |
| 8 Knee Society Functional score Show forest plot | 6 | 1012 | Mean Difference (IV, Random, 95% CI) | ‐1.42 [‐4.66, 1.82] |
| 9 Hospital Special Surgery score Show forest plot | 3 | 635 | Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐2.11, 1.01] |
| 10 Knee Society total score Show forest plot | 2 | 193 | Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐11.23, 10.47] |
| 11 SF‐12 mental Show forest plot | 2 | 300 | Mean Difference (IV, Random, 95% CI) | 0.39 [‐5.10, 5.87] |
| 12 Radiological: Radiolucent lines Show forest plot | 4 | 500 | Odds Ratio (M‐H, Random, 95% CI) | 0.80 [0.47, 1.35] |
| 13 Radiological: Femorotibial angle Show forest plot | 4 | 693 | Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.29, 0.47] |
| 14 Radiological: Rollback Show forest plot | 2 | 110 | Mean Difference (IV, Random, 95% CI) | 2.78 [‐9.57, 15.13] |
| 15 Radiological: Tibial slope Show forest plot | 2 | 98 | Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐1.21, 0.48] |

