Retention versus sacrifice of the posterior cruciate ligament in total knee arthroplasty for treating osteoarthritis
Abstract
Background
The functional and clinical basis on which to choose whether or not to retain the posterior cruciate ligament during total knee arthroplasty surgery remained unclear after a Cochrane systematic review and meta‐analysis in 2005, which contained eight clinical trials. Several new trials have been conducted since then. Hence, an update of the review was performed.
Objectives
Our aim was to assess the benefits and harms of retention compared to sacrifice of the posterior cruciate ligament in total knee arthroplasty in patients with osteoarthritis of the knee.
Search methods
An extensive search was conducted in CENTRAL, MEDLINE (PubMed), EMBASE, Web of Science, CINAHL, Academic Search Premier, Current Contents Connect and Science Direct. All databases were searched, without any limitations, up to 6 December 2012. References of the articles were checked and citation tracking was performed.
Selection criteria
Randomised and quasi‐randomised controlled trials comparing retention with sacrifice of the posterior cruciate ligament in primary total knee arthroplasty in patients with osteoarthritis of the knee.
Data collection and analysis
Data were collected with a pre‐developed form. Risk of bias was assessed independently by two authors (WV, LB). The level of evidence was graded using the GRADE approach. Meta‐analysis was performed by pooling the results of the selected studies, when possible. Subgroup analyses were performed for posterior cruciate ligament retention versus sacrifice using the same total knee arthroplasty design, and for studies using a posterior cruciate ligament retaining or posterior stabilised design, and when sufficient studies were available subgroup analyses were performed for the same brand.
Main results
Seventeen randomised controlled trials (with 1810 patients and 2206 knees) were found, described in 18 articles. Ten of these were new studies compared to the previous Cochrane Review. One study from the original Cochrane review was excluded. Most new studies compared a posterior cruciate ligament retaining design with a posterior stabilised design, in which the posterior cruciate ligament is sacrificed (a posterior stabilised design has an insert with a central post which can engage on a femoral cam during flexion).
The quality of evidence (graded with the GRADE approach) and the risk of bias were highly variable, ranging from moderate to low quality evidence and with unclear or low risk of bias for most domains, respectively.
The performance outcome 'range of motion' was 2.4 ° higher in favour of posterior cruciate ligament sacrifice (118.3 ° versus 115.9 °; 95% confidence interval (CI) of the difference 0.13 to 4.67; P = 0.04), however the results were heterogeneous. On the item 'knee pain' as experienced by patients, meta‐analysis could be performed on the Knee Society knee pain score; this score was 48.3 in both groups, yielding no difference between the groups. Implant survival rate could not be meta‐analysed adequately since randomised controlled trials lack the longer term follow‐up in order to evaluate implant survival. A total of four revisions in the cruciate‐retention and four revisions in the cruciate‐sacrifice group were found. The well‐validated Western Ontario and McMaster Universities osteoarthritis index (WOMAC) total score was not statistically significantly different between the groups (16.6 points for cruciate‐retention versus 15.0 points for cruciate‐sacrifice). One study reported a patient satisfaction grade (7.7 points for cruciate‐retention versus 7.9 points for cruciate‐sacrifice on a scale from 0 to 10, 10 being completely satisfied) which did not differ statistically significantly. Complications were distributed equally between both groups. Only one study reported several re‐operations other than revision surgery; that is patella luxations, surgical manipulation because of impaired flexion.
The mean functional Knee Society Score was 2.3 points higher (81.2 versus 79.0 points; 95% CI of the difference 0.37 to 4.26; P = 0.02) in the posterior cruciate ligament sacrificing group. Results from the outcome Knee Society functional score were homogeneous. All other outcome measures (extension angle, knee pain, adverse effects, clinical questionnaire scores, Knee Society clinical scores, radiological rollback, radiolucencies, femorotibial angle and tibial slope) showed no statistically significant differences between the groups. In the subgroup analyses that allowed pooling of the results of the different studies, no homogeneous statistically significant differences were identified.
Authors' conclusions
The methodological quality and the quality of reporting of the studies were highly variable. With respect to range of motion, pain, clinical, and radiological outcomes, no clinically relevant differences were found between total knee arthroplasty with retention or sacrifice of the posterior cruciate ligament. Two statistically significant differences were found; range of motion was 2.4 ° higher in the posterior cruciate ligament sacrificing group, however results were heterogeneous; and the mean functional Knee Society Score was 2.3 points higher in the posterior cruciate ligament sacrificing group. These differences are clinically not relevant.
PICO
Plain language summary
Retention versus sacrifice of the posterior cruciate ligament in total knee replacement for the treatment of osteoarthritis
Researchers in The Cochrane Collaboration have conducted a review of two types of knee replacement surgery for people with knee osteoarthritis. In one type, the posterior cruciate ligament is kept and in the other, it is removed. After searching for all relevant studies, they found 17 studies with up to 1810 patients.
The review shows that in people with osteoarthritis who have the posterior cruciate ligament preserved during total knee replacement surgery:
‐ this may not improve their range of motion, pain, function and patient satisfaction compared with removing the ligament.
We do not have precise information about side effects and complications, especially rare but serious side effects. Possible side effects may include infection, pain, and the need to have further surgery.
What is osteoarthritis and what is the posterior cruciate ligament?
Osteoarthritis (OA) is a disease of the joints, such as your knee or hip. When the joint loses cartilage, the bone may grow abnormally to try and repair the damage and make things worse. For example, it can make the joint painful and unstable. This can affect your physical function or ability to use your knee.
In some people, damage and pain in the knee from arthritis may be severe enough to require surgery. In total knee replacement surgery, a surgeon removes the damaged joint surface and replaces it with a metal and plastic implant.
The posterior cruciate ligament provides support and stable movement of the knee. In total knee replacement surgery, the posterior cruciate ligament can be kept in place or removed. This choice depends on the condition of the ligament, the type of total knee replacement selected or preference of the surgeon. When the ligament is removed, a special peg is used to provide stability and give your knee forward and backward movement with the tibia stabilised in relation to the femur.
What happens to people who have the posterior cruciate ligament preserved or removed during total knee replacement surgery
Range of motion (range of motion is the distance your knee can move from being bent to being fully extended. A lower range of motion is worse; you can’t bend or stretch your knee fully)
‐ People who had their posterior cruciate ligament preserved had 2 ° less range of motion compared to those who had it removed. This may be a result of chance
‐ People who had their posterior cruciate ligament removed had a range of motion of 118 ° of a possible 0 ° to 140 °
‐ People who had their posterior cruciate ligament preserved had a range of motion of 116 ° of a possible 0 ° to 140 °
Knee pain (lower score means worse pain)
‐ People who had their posterior cruciate ligament preserved rated their pain to be the same as those who had it removed. This may be a result of chance
‐ People who had their posterior cruciate ligament preserved or removed rated their pain to be 48 on a scale of 0 to 50
Health related quality of life and functional measures (higher means worse)
‐ People who had their posterior cruciate ligament preserved rated their quality of life to be 1 point worse than those who had it removed. This may be a result of chance
‐ People who had their posterior cruciate ligament preserved rated their quality of life to be 16 on a scale of 0 to 100
‐ People who had their posterior cruciate ligament removed rated their quality of life to be 15 on a scale of 0 to 100
Patient satisfaction (lower means worse)
‐ People who had their posterior cruciate ligament preserved rated their satisfaction the same as those who had it removed. This may be a result of chance
‐ People who had their posterior cruciate ligament preserved or removed rated their satisfaction to be 8 on a scale of 0 to 10
Complications and the need to have further surgery
‐ There were no differences in the number of revision surgeries, complications, or other further surgeries in people who had their posterior cruciate ligament preserved or removed.
Authors' conclusions
Summary of findings
| Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs) | |||||||
| Patient or population: Patients receiving total knee arthroplasty with or without posterior stabilised design for the treatment of osteoarthritis | |||||||
| Outcomes | Comparative risks | Relative effect | No. of patients (% of total) | No. of studies (% of total) | Quality of the evidence | Comments | |
| Cruciate‐sacrifice | Cruciate‐retention | ||||||
| Performance based measures ‐ Range of motion (possible range 0 (worst) to 140 (maximal) degrees) Follow‐up: 12‐78 months1 | The mean range of motion in the cruciate‐sacrifice group was 118.3 degrees (± SE 0.53) | The mean range of motion in the cruciate‐retaining group 2.40 lower (4.61 lower to 0.13 higher) | Total No. of patients: 1,119 (62%) Total No. of knees: 1,440 (65%) | 11 studies (65%) | ⊕⊕⊝⊝ | Absolute difference 2.40 lower (4.61 lower to 0.13 higher) Relative percent change: ‐2.0% (3.9% lower to 0.1% higher) Not statistically significant. | |
| Knee pain Knee Society Score, sub score pain (possible range of points 0 (severe pain) ‐ 50 (no pain)) Follow‐up: 24‐87 months years | The mean knee pain score in the cruciate‐sacrifice group was 48.3 points (± SE 0.54) | The mean knee pain score in the cruciate‐retention group was 0.01 higher (1.40 lower to 1.43 higher) | Total No. of patients: 656 (36%) Total No. of knees: 1,004 (46%) | 4 studies (24%) | ⊕⊕⊕⊝ | Absolute difference: 0.01 higher (1.40 lower to 1.43 higher) Relative percent change: 0.0% (2.9% lower to 3.0% higher) Not statistically significant. | |
| Survival rate of the implant (Revision surgery reported) Follow‐up: 17‐87 months | See comment | See comment | Not estimable | Total No. of patients: 926 (51%) Total No. of knees: 1,229 (56%) | 7 studies (41%) | See comment | Insufficient data provided. Incidental remarks on implant survival could be derived from 7 studies. One study Misra 2003 reported 2 revisions in de cruciate‐retention group, Chaudhary 2008 1 in the cruciate‐retention group, Harato 2008 1 in the cruciate‐retention group and 3 in the sacrifice group. Aglietti 2005 1 revision in the cruciate‐sacrifice group due to septic loosening Kim 2009, Yagishita 2012 and Tanzer 2002 specifically reported no revision surgery had occurred during follow‐up |
| Health related quality of life measures and functional measures with validated instruments (WOMAC, range 0‐100, higher scores indicate worse pain, stiffness and functional limitations) Follow‐up: 24‐87 months | The mean WOMAC total score in the cruciate‐sacrifice group was 15.0 points (± SE 1.2) | The mean WOMAC total score in the cruciate‐retention group was 0.78 higher (1.51 lower to 3.07 higher) | Total No. of patients: 501 (28%) Total No. of knees: 531 (24%) | 4 studies (24%) | ⊕⊕⊝⊝ | Absolute difference: 0.78 higher (1.51 lower to 3.07 higher) Relative percent change: 5.2% (10.0% lower to 20.5% higher) Not statistically significant. | |
| Global assessment (patient) Patient satisfaction on scale 0 (not at all satisfied) to 10 (completely satisfied) Follow‐up: 12‐83 months | The mean satisfaction score in the cruciate‐sacrifice group was 7.910 | The mean satisfaction score in the cruciate‐retention group was 0.2 lower10 | Total No. of patients: 103 (6%) Total No. of knees: 105 (5%) | 1 study (6%) | ⊕⊕⊝⊝ | Absolute difference: 0.2 lower 10 Relative percent change: ‐2.5% 10 Not statistically significant. | |
| Complications Follow‐up: 8‐87 months7 | See comment | See comment | Not estimable | Total No. of patients: 1,252 (69%) Total No. of knees: 1,635 (74%) | 11 studies (65%) | See comment | Due to the very diverse way of reporting and defining complications combining data for quantitative analysis was not possible8,9 |
| Re‐operation rate (not involving implant change, short and long term) Follow‐up: 24 months | See comment | See comment | Not estimable | Total No. of patients: 40 (2%) | 1 study (6%) | See comment | Catani 2004 reported 4 re‐operations; 3 patella luxations (2 in cruciate‐sacrificing, 1 in cruciate‐retention group) and 1 surgical manipulation due to lack of range of motion (in the cruciate‐retention group) |
| CI: Confidence interval; KSS: Knee Society Score, WOMAC: Western Ontario and McMasters Universities Osteoarthritis Index. NA: not applicable | |||||||
| GRADE Working Group grades of evidence | |||||||
| 1 Median follow‐up: 2 years 7 Some studies reported complications after several months. Mean follow‐up of other endpoints was > 1 year 8 Complications reported in the cruciate‐sacrifice group: 4 anterior knee pain, 4 limited range of motion, 1 deep venous thrombosis, 3 instability, 3 femoral notching, 3 aseptic loosening, 3 (deep) infection 9 Complications reported in the cruciate‐retention group: 6 anterior knee pain, 10 limited range of motion, 0 deep venous thrombosis, 3 instability, 2 femoral notching, 2 aseptic loosening, 3 (deep) infection, 2 ligament laxity, 1 ligament tightness 10 Not sufficient data reported to calculate standard error, range or confidence interval | |||||||
| Posterior cruciate ligament retention versus sacrifice (using the same arthroplasty design) | |||||||
| Patient or population: Patients receiving total knee arthroplasty with or without resection of the posterior cruciate ligament for the treatment of osteoarthritis | |||||||
| Outcomes | Comparative risks | Relative effect | No. of patients (% of total) | No of studies (% of total) | Quality of the evidence | Comments | |
| Cruciate‐sacrifice | Cruciate‐retention | ||||||
| Performance based measures ‐ Range of motion (possible range 0 (worst) to 140 (maximal) degrees) Follow‐up: 12‐78 months | The mean range of motion in the cruciate‐sacrifice group was 114.1 degrees (± SE 0.82) | The mean range of motion in the cruciate‐retention group was 2.7 degrees lower (8.71 lower to 3.32 higher) | Total No. of patients: 405 (22%) Total No. of knees: 414 (19%) | 4 studies (24%) | ⊕⊝⊝⊝ | Absolute difference: 2.7 degrees lower (8.71 lower to 3.32 higher) Relative percent change: ‐2.4% (7.6% lower to 2.9% higher) Not statistically significant. | |
| Knee pain Knee Society Score, sub score pain (possible range 0 (severe pain) ‐ 50 (no pain) points) | See comment | See comment | Not estimable | ‐ | ‐ | See comment | No data in studies comparing ligament resection and sacrifice using similar arthroplasty designs |
| Survival rate of the implant (Revision surgery reported) Follow‐up: 56‐60 months | See comment | See comment | Not estimable | Total No. of patients: 103 (6%) Total No. of knees: 105 (5%) | 1 study (6%) | See comment | Insufficient data provided. One study (Misra 2003) reported 2 revisions in the cruciate‐retention group. |
| Health related quality of life measures and functional measures with validated instruments (WOMAC, range 0‐100, higher scores indicate worse pain, stiffness and functional limitations) Follow‐up: 24‐37 months | The mean WOMAC total score in the cruciate‐sacrifice group was 17.0 points (± SE 1.1) | The mean WOMAC total score in the cruciate‐retention group was 1.10 lower (‐5.19 lower to 2.99 higher) | Total No. of patients: 86 (5%) Total No. of knees: 86 (4%) | 1 study (6%) | See comment | One study reported this outcome: Roh 2012 Absolute difference: 1.10 lower (‐5.19 lower to 2.99 higher) Relative percent change: ‐6.5% (30.5% lower to 17.6%higher) Not statisitically significant | |
| Global assessment (patient) Patient satisfaction on scale 0 (not at all satisfied) to 10 (completely satisfied)) Follow‐up: 12‐83 months | The mean satisfaction score in the cruciate‐sacrifice group was 7.97 | The mean satisfaction score in the cruciate‐retention group was 0.2 lower7 | Total No. of patients: 103 (6%) Total No. of knees: 105 (5%) | 1 study (6%) | ⊕⊕⊝⊝ | Absolute difference: 0.2 lower 7 Relative percent change: ‐2.5% 7 Not statistically significant. | |
| Complications Follow‐up: 12‐78 months | See comment | See comment | Not estimable | Total No. of patients: 405 (22%) Total No. of knees: 414 (19%) | 4 studies (24%) | See comment | Due to the very diverse way of reporting and defining complications combining data for quantitative analysis was not possible5,6 |
| Re‐operation rate (not involving implant change, short and long term) | See comment | See comment | Not estimable | ‐ | ‐ | See comment | No data in studies comparing ligament resection and sacrifice using similar arthroplasty designs |
| CI: Confidence interval. KSS: Knee Society Score, WOMAC: Western Ontaria and McMasters Universities Osteoarthritis Index. NA: not applicable | |||||||
| GRADE Working Group grades of evidence | |||||||
| 1 Risk of bias individual studies, see risk of bias tables 5 Complications reported in the cruciate‐sacrifice group: 3 instability, 3 aseptic loosening, 2 stiffness 6 Complications reported in the cruciate‐retention group: 3 instability, 1 infection (deep), 2 aseptic loosening, 2 stiffness, 2 ligament laxity, 1 ligament tightness 7 Not sufficient data reported to calculate standard error, range or confidence interval | |||||||
| Posterior cruciate ligament retention versus posterior stabilised sacrifice | |||||||
| Patient or population: Patients receiving total knee arthroplasty with or without posterior stabilised design for the treatment of osteoarthritis | |||||||
| Outcomes | Mean differences (95% CI) | Relative effect | No. of patients (% of total) | No. of studies (% of total) | Quality of the evidence | Comments | |
| Cruciate‐sacrifice (posterior stabilised) | Cruciate‐retention | ||||||
| Performance based measures ‐ Range of motion (possible range 0 (worst) to 140 (maximal) degrees) Follow‐up: 1‐6.5 years1 | The mean range of motion in the cruciate‐sacrifice group was 119.8 degrees (± SE 0.66) | The mean range of motion in the cruciate‐retention group was 3.4 degrees lower (6.32 to 0.54 lower) | Total No. of patients: 899 (50%) Total No. of knees: 1,193 (54%) | 8 studies (47%) | ⊕⊕⊕⊝ | Absolute difference: ‐3.4 degrees (6.32 to 0.54 lower) Relative percent change: ‐2.8% (5.3% lower to 0.45% higher) Statistically significant (P = 0.02) NNTB: 9 (5 to 51) | |
| Knee pain Knee Society Score, subscore pain (possible range 0 (severe pain) ‐ 50 (no pain) points) Follow‐up: 2‐7.3 years | The mean knee pain score in the cruciate‐sacrifice group was 48.3 points (± SE 0.68) | The mean knee pain score in the cruciate‐retention group was 0.60 higher (0.39 lower to 1.60 higher) | Total No. of patients: 471 (26%) Total No. of knees: 780 (35%) | 3 studies | ⊕⊕⊕⊝ | Absolute difference: 0.60 (0.39 lower to 1.60 higher) Relative percent change: 1.2% (0.81% lower to 3.3% higher) Not statistically significant. | |
| Survival rate of the implant (Revision surgery reported) | See comment | See comment | Not estimable | Total No. of patients: 802 (44%) Total No. of knees: 1,100 (50%) | 6 studies (35%) | See comment | Insufficient data provided. Incidental remarks on implant survival could be derived from 6 studies. Chaudhary 2008 1 in the cruciate‐retention group, Harato 2008 1 in the cruciate‐retention group and 3 in the sacrifice group. Aglietti 2005 1 revision in the cruciate‐sacrifice group due to septic loosening Kim 2009, Yagishita 2012 and Tanzer 2002 specifically reported no revision surgery had occurred during follow‐up |
| Health related quality of life measures and functional measures with validated instruments (WOMAC, range 0‐100, higher scores indicate worse pain, stiffness and functional limitations) Follow‐up: 24‐87 months | The mean WOMAC total score in the cruciate‐sacrifice group was 18.2 points(± SE 1.5) | The mean WOMAC total score in the cruciate‐retention group was 1.60 lower (1.32 lower to 4.50 higher) | Total No. of patients: 415 (23%) Total No. of knees: 445 (20%) | 3 studies (18%) | ⊕⊕⊝⊝ | Absolute difference: 1.60 lower (1.32 lower to 4.50 higher) Relative percent change: ‐8.8% (7.3% lower to 24.7% higher) Not statistically significant. | |
| Global assessment (patient) | See comment | See comment | Not estimable | ‐ | ‐ | See comment | No data in studies comparing ligament resection and sacrifice using similar arthroplasty designs |
| Complications Follow‐up: 8‐87 months5 | See comment | See comment | Not estimable | Total No. of patients: 878 (49%) Total No. of knees: 1,220 (55%) | 8 studies (47%) | See comment | Due to the very diverse way of reporting and defining complications combining data for quantitative analysis was not possible3,4 |
| Re‐operation rate (not involving implant change, short‐ and long‐term) Follow‐up: 24 months | See comment | See comment | Not estimable | Total No. of patients: 40 (2%) | 1 study (6%) | See comment | Catani 2004 reported 4 re‐operations; 3 patella luxations (2 in cruciate‐sacrificing, 1 in cruciate‐retention group) and 1 surgical manipulation due to lack of range of motion (in the cruciate‐retention group) |
| CI: Confidence interval. KSS: Knee Society Score, WOMAC: Western Ontaria and McMasters Universities Osteoarthritis Index. ROM range of motion NA: not applicable | |||||||
| GRADE Working Group grades of evidence | |||||||
| 1 Relatively many studies with 'unclear' risk of bias 2 < 400 arthroplasties in analysis 3 Complications reported in the cruciate‐sacrifice group: 2 anterior knee pain, 3 femoral notching, 1 superficial wound infection, 2 deep venous thrombosis, 1 septic loosening 4 Complications reported in the cruciate‐retention group: 1 anterior knee pain, 1 limited ROM, 2 femoral notching, 1 superficial wound infection 5 Some studies reported complications after several months. Mean follow‐up of other endpoints was > 1 year | |||||||
Background
Description of the condition
Osteoarthritis is a degenerative joint disease leading to degradation of articular cartilage and subchondral bone. Clinically, patients with knee osteoarthritis present in general with disabling knee pain and impaired knee function. At some point during the disease the only remaining treatment is surgery with a total knee arthroplasty.
Description of the intervention
A total knee arthroplasty is the resurfacing of the joint articulating surfaces. During total knee arthroplasty surgery several structures involved in the knee joint are either retained (for example the posterior cruciate ligament), replaced by artificial structures (for example patella resurfacing), or discarded (for example the anterior cruciate ligament and possibly the posterior cruciate ligament). The distal femur and proximal tibia are cut and replaced by a femoral and a tibial component. Between these components a polyethylene insert is placed. See Figure total knee arthroplasty components (Figure 1).

Bicondylar ligament cruciate retaining balancing total knee arthroplasty with rotating platform (balanSys®, Mathys Ltd., Bettlach, Switzerland) Hirschmann et al. BMC Musculoskeletal Disorders 2010 11:167 doi:10.1186/1471‐2474‐11‐167
Download authors' original image
For total knee arthroplasty it is desirable to reproduce the natural movements of the knee while maintaining stability from extension to flexion. In patients in whom the posterior cruciate ligament can be retained, this ligament can provide these requirements (Lombardi 2001; Mihalko 1999). Moreover, the posterior cruciate ligament is supposed to have different types of mechanoreceptors detecting joint position (proprioception) and joint motion (kinaesthesia) (Hogervorst 1998; Nelissen 2001; Swanik 2004). However, the structural integrity of the posterior cruciate ligament of an osteoarthritic knee may be lost due to mucoid degeneration (Nelissen 2001). When the posterior cruciate ligament is retained in total knee arthroplasty, some studies have shown a lack of posterior femoro‐tibial translation (for example the naturally occurring movement of the distal femur on the tibia, also known as rollback) with knee flexion (Dennis 1998; Mahoney 1994). This is thought to be attributable to inadequate balancing of the posterior cruciate ligament in flexion during surgery (Emodi 1999; Most 2003; Nozaki 2002). Balancing of the posterior cruciate ligament consists of choosing the insert thickness and component sizes in a way that the posterior cruciate ligament is adequately tensioned in flexion but relaxed in extension. When posterior cruciate ligament balancing has not been performed adequately, the patient might have a suboptimal total knee arthroplasty, which often produces pain (Pagnano 1998). If the posterior cruciate ligament is too loose, the patient might present with instability (Pagnano 1998; Waslewski 1998). If the posterior cruciate ligament is too tight, the patient suffers from limited flexion and the polyethylene insert is subjected to high stresses and wear (Migaud 2003; Pagnano 1998). A release of the posterior cruciate ligament can be used in cases with a tight ligament and difficulty to perform knee flexion during the procedure.
In many instances, however, the posterior cruciate ligament is sacrificed in the surgical procedure and another arthroplasty design is used. Sacrifice of the posterior cruciate ligament results in an increase in the flexion gap (the flexion gap is the gap between the cut posterior parts of the distal femur and the cut proximal tibia when the knee is flexed) (Baldini 2004; Mihalko 1999). This increase is generally compensated for with thicker polyethylene inserts or larger femoral components. Sacrificing the posterior cruciate ligament leads to an increase in the extension gap as well (the extension gap is the gap between the cut distal femur and the cut proximal tibia when the knee is in extension) (Baldini 2004). The size of these gaps has to be in such a way that the ligaments in and around the knee joint are balanced in order to achieve stability after placement of the arthroplasty. Several adjustments in total knee arthroplasty design exist to compensate for the absence of the posterior cruciate ligament. The posterior stabilised design is most commonly used. This design has a cam post mechanism to substitute for the function of the posterior cruciate ligament and permits rollback of the femoral component on the tibial component during flexion. Other knee systems use deep dish inserts with a high anterior rim as a brake against posterior subluxation of the tibia.
Factors influencing the choice of sacrifice or retention of the posterior cruciate ligament are the degenerative status of the ligament, knee deformities, the type of implant used, or the personal preference of the surgeon. Lombardi 2001 proposed a decision tree based upon the patient's history, the clinical examination, and the intraoperative findings (Lombardi 2001).
Why it is important to do this review
Randomised studies comparing posterior cruciate ligament retention with sacrifice have been conducted from the early 90s up to now (Seon 2011; Shoji 1994). In 2005, when the original Cochrane systematic review on this topic was published, these studies combined in a meta‐analysis could not find a clear difference between the two treatments. It was impossible to give clear advice on whether to retain or to sacrifice the posterior cruciate ligament (Jacobs 2005). In this extensive update the question remains whether the study results allow for pooling and whether the pooled results favour retention or sacrifice of the posterior cruciate ligament.
Objectives
To assess the range of motion, pain, clinical and radiological outcomes in patients with retention versus sacrifice of the posterior cruciate ligament in total knee arthroplasty for the treatment of osteoarthritis.
Methods
Criteria for considering studies for this review
Types of studies
Randomised and quasi‐randomised controlled trials were included. Quasi‐randomised studies use alternating sequences for randomisation (that is odd or even chart numbers, date of hospital admission, etc.) Non‐randomised clinical trials and historically controlled studies were excluded.
Types of participants
Studies were included when dealing with patients with osteoarthritis. Studies which included a wider range of indications were excluded if the proportion of patients with osteoarthritis was lower than 95% of the total group or when the subgroups were poorly described with separate results.
Types of interventions
Studies were included if total knee arthroplasty with retention of the posterior cruciate ligament was compared to sacrifice of the posterior cruciate ligament. Procedures with sacrifice of the posterior cruciate ligament were considered when the same arthroplasty design or when a posterior cruciate ligament substituting design was used.
Types of outcome measures
Major outcomes
-
Performance outcome: range of motion (flexion, extension)
-
Knee pain (i.e. as measured by a Visual Analogue Scale (VAS), Knee Society Score pain subscale, etc.)
-
Implant survival rate (revision surgery)
-
Validated clinical and functional questionnaire scores (i.e. Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC))
-
Patient satisfaction
-
Complications
-
Re‐operations other than revision surgery (e.g. manipulation because of impaired knee function)
Minor outcomes
-
Specific evaluation of daily tasks (i.e. walking or stair climbing ability, rising from a chair)
-
Less validated clinical and functional questionnaire scores (i.e. Knee Society score)
-
Radiological outcomes (i.e. Radio Stereotactic Analysis (RSA)
-
Gait analysis parameters
Search methods for identification of studies
Electronic searches
We conducted a sensitive search in order to retrieve all available literature. In consultation with an experienced librarian of the medical scientific library of the Leiden University Medical Center, we searched the following databases: the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE (PubMed), EMBASE, Web of Science, CINAHL, Academic Search Premier, Current Contents Connect and Science Direct. All databases were searched up to 6 December 2012 using an adopted syntax for every single database. The search syntax for the different databases is presented in Appendix 1. No restrictions or limits were formulated.
Searching other resources
A final check that no relevant articles were missed was carried out by screening the references from the articles and by performing citation tracking on the articles that were selected. To identify ongoing trials comparing retention with sacrifice of the posterior cruciate ligament we checked the online trial registries via the portal of the World Health Organization (www.who.int/trialsearch).
Data collection and analysis
Selection of studies
Articles were selected in two steps. Studies were excluded when it was apparent from the title or the abstract that the study did not meet all of the following criteria.
-
The intervention evaluated in the trials had to be primary total knee arthroplasty (excluding post‐patellectomy and post‐osteotomy studies), comparing one treatment in which the posterior cruciate ligament was retained against one in which it was sacrificed. Procedures with sacrifice of the posterior cruciate ligament were considered when the same prosthesis design was used as for the retention group, or when a posterior cruciate ligament substituting design was used (e.g. posterior stabilised or a deep dish insert).
-
The indication for total knee arthroplasty had to be osteoarthritis. Studies which included a wider range of indications were excluded if the proportion of patients with osteoarthritis was lower than 95% of the group.
-
Minimal follow‐up had to be 12 months.
-
Studies had to be randomised or quasi‐randomised controlled trials.
In the first step only the titles and abstracts were screened. In the second step, articles which passed the first step were retrieved in full and evaluated against the inclusion and exclusion criteria.
Data extraction and management
One review author (WV) conducted the literature search and retrieved the references to be evaluated. Two review authors (WV, LB) independently selected the trials to be included in the review. Disagreements were resolved by consensus. When no consensus could be reached, a third review author (WJ) was available for the decisive vote. A pre‐developed and tested data extraction form was used to extract data from the selected studies. Items collected were: study design features, population data, statistical analysis techniques, intervention characteristics, and all reported outcome parameters including results. All data was entered into Review Manager 5.1 (Review Manager 2011). When a selected article was written in a foreign language, the data extraction form was sent to a translator via the Cochrane Musculoskeletal group. A second form was used to assess the risk of bias (see below) and the clinical relevance of the selected studies.
Assessment of risk of bias in included studies
Selected studies were closely examined by two review authors working independently (WV, LB). Risk of bias was assessed according to the recommendations of The Cochrane Collaboration in risk of bias tables (Higgins 2011). To detect selection bias, performance bias and attrition bias, several items were evaluated in all selected studies. The risk of selection bias was judged by assessing how the randomisation sequence was generated and by assessing the way the allocation of treatment was concealed. Risk of performance and detection bias was judged by evaluating the blinding (of personnel, patients and outcome assessors) in the studies. The risk of attrition bias was assessed by judging the completeness of the data, including the follow‐up rates. Finally, the risk of reporting bias was assessed by judging if all (relevant) outcome measurements were reported. The possible judgments that could be made were low risk of bias, high risk of bias and unclear risk of bias.
Measures of treatment effect
Continuous data were entered as means and standard deviations, dichotomous outcomes as number of events. In the absence of significant heterogeneity, and given sufficient included trials, results were combined using mean differences for continuous data and risk ratios for dichotomous data.
Unit of analysis issues
Special issues in the analysis of studies with non‐standard (randomised controlled trial) designs (for example cluster‐randomised trials) were identified. A specific issue for studies on knee replacement surgery is the possibility to perform surgery bilaterally: allocating one knee to posterior cruciate ligament retention automatically allocates ligament sacrifice to the other contralateral knee.
Dealing with missing data
Standard deviations were used when available. When not provided, standard deviations were imputed from comparable studies or from the original scores (for example confidence intervals) when calculating change scores (Higgins 2011).
Assessment of heterogeneity
Heterogeneity was first assessed by visual inspection of the forest plots. Furthermore, it was investigated with the I2 statistic and if significant (P < 0.10 using the Chi2 statistic) the source of heterogeneity was investigated by doing a sensitivity analysis and considering clinical reasons for potential clinical heterogeneity. I2 values of 30% to 50% were considered to represent moderate heterogeneity; from 50% to 80% were considered to represent substantial heterogeneity and above 80% considerable heterogeneity (Higgins 2011).
Assessment of reporting biases
In order to evaluate the risk of publication bias we checked the online trial registries via the portal of the World Health Organization (www.who.int/trialsearch). When studies were tagged as 'stopped' (for example not ongoing) and were not published in an article, the investigator of the study was contacted and the reason why the study was not published was identified, when possible.
Data synthesis
Statistical analyses were conducted using RevMan 5.1. The outcomes specified in the protocol were included in the analysis. A random‐effects model was used for all analyses in this review (Fleiss 1993).
Subgroup analysis and investigation of heterogeneity
Besides the general comparison of total knee arthroplasties with and without sacrifice of the posterior cruciate ligament, several subgroup analyses were performed. First, as in the original Cochrane review, studies evaluating the effect of posterior cruciate ligament retention and sacrifice using the same design total knee arthroplasty (the posterior cruciate ligament retaining design) were considered in a subgroup analysis. Secondly, the studies evaluating the effect of posterior cruciate ligament retention and sacrifice comparing a posterior cruciate ligament retaining arthroplasty design with a posterior stabilised posterior ligament sacrificing design were considered in a subgroup analysis. When other design modifications than posterior stabilisation were studied, these were considered in separate subgroup analyses.
Sensitivity analysis
When it was unclear if findings in the meta‐analysis were robust to the decisions made in the process of obtaining them, this was tested in a sensitivity analysis. For example, when data for a specific outcome measure were not adequately reported the analysis was performed with and without inputed outcome values. Findings were considered 'robust' when they did not change significantly. Moreover, outcomes of the meta‐analyses were compared with the pooled outcomes from the studies with the lowest risk of bias.
Quality of evidence and summary of findings tables
For the outcome measures range of motion, flexion angle and knee pain, the primary outcome measures, beneficial effects were evaluated. To evaluate harmful effect differences between the two treatment groups we evaluated the occurrence of complications. Results were presented in 'summary of findings' tables. As prescribed by The Cochrane Collaboration, a quality of evidence assessment was performed using the GRADE approach (with GRADEpro software (version 3.6)).
The different grades of evidence according to the GRADE working group are as follows.
-
High quality: further research is very unlikely to change confidence in the estimate of effect.
-
Moderate quality: further research is likely to have an important impact on confidence in the estimate of the effect, and may change the effect.
-
Low quality: further research is very likely to have an important impact on confidence in the estimate of the effect, and is likely to change the effect.
-
Very low quality: the effect estimate is very uncertain.
Results
Description of studies
Results of the search
For this update, a total of 2129 unique references were identified (Figure 2, PRISMA flowchart). The search in MEDLINE (PubMed) resulted in 858 references. Furthermore, EMBASE yielded 543 unique references, Web of Science 299, Current Contents Connect 19, CENTRAL 72, CINAHL 215, Academic Search Premier 26 and Science Direct 97 unique references. After the first step of selection, 55 articles were selected for the second step. After applying the inclusion and exclusion criteria to the full text 18 papers remained. Citation tracking did not result in any extra references.

Study flow diagram (PRISMA).
The article of Victor 2005 described a population that was also part of the study population of Harato 2008. The data from both articles were used only once.
Included studies
Ultimately 17 studies (with 1810 patients and 2206 knees), described in 18 articles, were considered for analysis (Aglietti 2005; Catani 2004; Chaudhary 2008; Clark 2001; de Andrade 2009; Harato 2008; Kim 2009; Maruyama 2004; Matsumoto 2012; Misra 2003; Roh 2012; Seon 2011; Shoji 1994; Straw 2003; Tanzer 2002; Victor 2005; Wang 2004; Yagishita 2012). Ten studies were new compared to the original Cochrane review. The article of de Andrade et al (de Andrade 2009) was written in Portuguese and data were extracted by a translator from the Cochrane Musculoskeletal Group.
Interventions
In 12 studies the comparison between the two treatment arms was posterior cruciate retention with a cruciate retaining design versus sacrifice using a posterior stabilised design (Aglietti 2005: LPS/MBK; Catani 2004: Optetrak; Chaudhary 2008: SCORPIO; Clark 2001: AMK; de Andrade 2009: NexGen; Harato 2008: Genesis II; Kim 2009: NexGen; Maruyama 2004: PFC; Matsumoto 2012: NexGen; Seon 2011: NexGen; Tanzer 2002: NexGen; Yagishita 2012: NexGen). In three studies the same (cruciate‐retaining) arthroplasty design was used for both groups (Misra 2003: PFC; Roh 2012: E‐motion; Shoji 1994: Total Condylar Modifier). One study used all three treatments (that is cruciate‐retaining design with ligament retention and with ligament sacrifice and a posterior stabilised design (Straw 2003: Genesis I). Finally, one study did not clearly report the design of the arthroplasty (Wang 2004).
Duration of follow‐up in the included studies
Aglietti 2005 had a mean follow‐up of 36 months (range 30 to 48 months). Catani 2004 had a 24 months follow‐up; no range was reported. Chaudhary 2008 had a mean follow‐up of 22.7 months (± 5.2 months). Follow‐up in the study from Clark 2001 ranged from 12 to 36 months; no mean follow‐up was reported. de Andrade 2009 had a mean follow‐up of 15.8 months (± 3.8 months). Harato 2008 had a mean follow‐up of 64.8 months (range 60 to 87.6 months) for the cruciate‐retention group and a mean follow‐up of 67.2 months (range 60 to 87.6 months) for the cruciate‐sacrificing group. Kim 2009 had a mean follow‐up of 27.6 months (range 24 to 36 months). Maruyama 2004 had a mean follow‐up of 31.7 months (range 24 to 53 months) for the cruciate‐retention group and a mean follow‐up of 30.6 (range 24 to 38 months) for the cruciate‐sacrificing group. Matsumoto 2012 had a mean follow‐up of 71.9 months (range 61 to 83 months) for the cruciate‐retention group and a mean follow‐up of 70.2 months (range 63 to 87 months) for the cruciate‐sacrificing group. Misra 2003 had a mean follow‐up of 57 months; no range was reported. Roh 2012 had a mean follow‐up of 27.3 months (range 24 to 28 months) for the cruciate‐retention group and a mean follow‐up of 32.2 months (range 24 to 37 months) for the cruciate‐sacrificing group. Seon 2011 had a mean follow‐up of 26.1 months (± 1.7) for the cruciate‐retention group and a mean follow‐up of 28.4 months (± 2.1) for the cruciate‐sacrificing group. Shoji 1994 had a mean follow‐up of 38.4 months (range 30 to 54 months). Straw 2003 had a mean follow‐up of 42 months (range 12 to 78 months). Tanzer 2002 had a mean follow‐up of 24 months; no range was reported. Wang 2004 had a mean follow‐up of 42 months (range 24 to 66 months). Yagishita 2012 had a mean follow‐up of 60 months (range 36 to 73 months). See Characteristics of included studies.
Sex and age (patient characteristics)
The mean age in Aglietti 2005 et al was 71 years in the cruciate‐retention group (86% female patients) and 69.5 years in the cruciate‐sacrificing group (81% female patients). The mean age in Catani 2004 et al was 70 ± 6.0 years in the cruciate‐retention group (65% female patients) and 71 ± 7.0 years in the cruciate‐sacrificing group (75% female patients). The mean age in Chaudhary 2008 et al was 69.2 ± 9.1 years in the cruciate‐retention group (53% female patients) and 70.2 ± 8.4 years in the cruciate‐sacrificing group (45% female patients). The mean age in Clark 2001 et al was 71.8 ± 12.2 years in the cruciate‐retention group (sex of the patients not reported) and 71.2 ± 13.6 years in the cruciate‐sacrificing group. The mean age in de Andrade 2009 et al was 66.3 years (range 41 to 78 years) overall; 74% pf the patients were female. The mean age in Harato 2008 et al was 68.3 years (range 49 to 89 years) in the cruciate‐retention group (34% female patients) and 66.0 years (range 44 to 83 years) in the cruciate‐sacrificing group (34% female patients). The mean age in Kim 2009 et al was 71.6 ± 6.0 years overall; in the cruciate‐retention group (86% female patients) and 69.5 years in the cruciate‐sacrificing group (81% female patients). The mean age in Maruyama 2004 et al was 74.3 years (range 65 to 84 years) overall; 60% of the patients were female. The mean age in Matsumoto 2012 et al was 73.5 ± 1.3 years in the cruciate‐retention group (100% female patients) and 74.4 ± 0.9 years in the cruciate‐sacrificing group (100% female patients). The mean age in Misra 2003 et al was 66.8 years (range 55 to 83 years) in the cruciate‐retention group (67% female patients) and 67.2 years (range 59 to 82 years) in the cruciate‐sacrificing group (59% female patients). The mean age in Roh 2012 et al was 69.8 ± 4.7 years in the cruciate‐retention group (95% female patients) and 71 ± 4.9 years in the cruciate‐sacrificing group (93% female patients). The mean age in Seon 2011 et al was 68.2 ± 7.0 years in the cruciate‐retention group (91% female patients overall in the study) and 69.1 ± 6.7 years in the cruciate‐sacrificing group. The mean age in Shoji 1994 et al was not reported nor was the sex distribution of the patients. The mean age in Straw 2003 et al was 72.6 years in the cruciate‐retention group, 72.6 years in the posterior stabilised group and 74.1 years in the cruciate‐sacrificing group. The mean age in Tanzer 2002 et al was 68 years (range 51 to 86 years) in the cruciate‐retention group (75% female patients) and 66 years (range 52 to 77 years) in the cruciate‐sacrificing group (80% female patients). The mean age in Wang 2004 et al was 54.5 years (range 31 to 69 years) in the cruciate‐retention group (80% female patients) and 55 years (range 20 to 83 years) in the cruciate‐sacrificing group (80% female patients). The mean age in Yagishita 2012 et al was 74.3 ± 7.2 years overall; 86% of the patients were female. See Characteristics of included studies.
Categorisation
The comparisons made in the trials could be divided into several distinct comparisons based on the outcome of range of motion. One was posterior cruciate ligament retention versus sacrifice with a posterior stabilised total knee arthroplasty design. Another comparison was made between posterior cruciate ligament retention versus sacrifice using the same arthroplasty design (see analysis section).
Two studies (Misra 2003; Shoji 1994), identified in the original review, and one new study (Roh 2012) compared posterior cruciate ligament retention and sacrifice using the same arthroplasty design (for example a posterior cruciate retaining design without a substitution of the resected ligament). When a specific posterior cruciate ligament substituting design was used, a posterior cruciate ligament retaining design was compared with a posterior stabilised design in all selected studies.
For details of the included studies see the Characteristics of included studies table.
Outcomes
All studies used a clinical rating scale, either well validated (that is WOMAC) or less well validated (that is Knee Society score or Hospital for Special Surgery score), and reported range of motion or flexion measurements.
Sample size
Eight studies (Aglietti 2005; Clark 2001; Harato 2008; Kim 2009; Misra 2003; Seon 2011; Straw 2003; Wang 2004) had group sizes of more than 50. Chaudhary et al compared 51 patients in which the posterior cruciate ligament was retained to 49 patients in which it was sacrificed (Chaudhary 2008).
Excluded studies
One study from the original Cochrane review (Jacobs 2005) was excluded from this update (Swanik 2004). This study reported results with a mean follow‐up of 7.6 months. The protocol stated that follow‐up had to be at least 12 months.
Most excluded studies were classified as non‐randomised studies after reading the full text articles. Proceeding communications and abstracts of studies presented at international congresses were evaluated (Husain 1998; Matsuda 2003; MacDonald 2005; Surace 1997; Yamamoto 2003). Since methodological issues (for example randomisation technique) and outcome measures (for example mean with standard deviation) were not reported extensively enough, these studies were not included in the analyses. No additional publications were found for these studies. Ten studies were excluded for other different reasons.
For an overview of the excluded studies see the Characteristics of excluded studies table.
Risk of bias in included studies
Overall, the more recent publications had a lower risk of bias. Based on study characteristics and the risks of bias as described before, the studies of highest quality from the current selection of articles were Chaudhary (Chaudhary 2008), Kim (Kim 2009), Misra (Misra 2003) and Seon (Seon 2011).
Allocation
Four of the selected studies (24%) described how the randomisation sequence was generated (Chaudhary 2008: computer generated randomisation blocks; Harato 2008: randomisation blocks, stratified per centre; Misra 2003: random numbers table; Roh 2012: permuted block randomisation). The other 13 studies (76%) did not describe randomisation sequence generation (see Figure 3 and Figure 4). Concealment of allocation was performed using sealed or opaque envelopes, or both, as reported in five studies (29%) (Chaudhary 2008; Harato 2008; Kim 2009; Matsumoto 2012; Seon 2011). The other 12 studies (71%) did not mention concealment of allocation (see Figure 3 and Figure 4). Three studies used 'quasi‐randomisation': Aglietti 2005 based treatment choice on odd or even patient numbers; Maruyama 2004 used alternating sequences; and Wang 2004 used hospital admission moment to base treatment on (see Figure 3 and Figure 4).
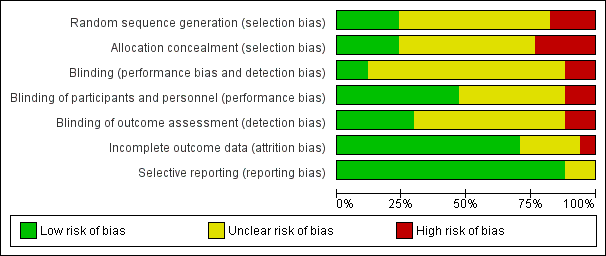
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
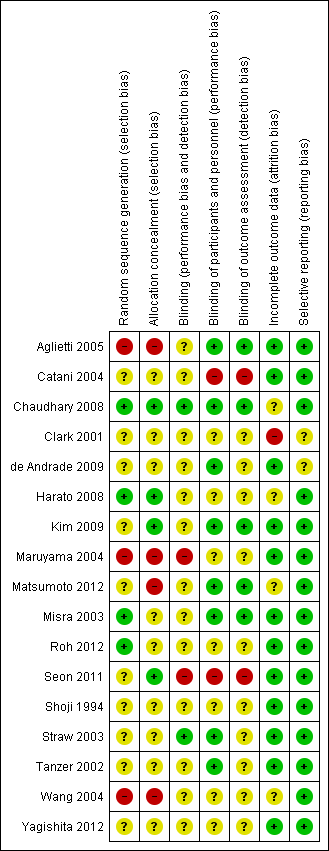
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Blinding
Blinding of participants and personnel was not described in eight studies (47%) (Catani 2004; Clark 2001; Harato 2008; Maruyama 2004; Roh 2012; Shoji 1994; Wang 2004; Yagishita 2012). Seon et al mentioned explicitly that no blinding was applied (Seon 2011). The other eight studies (47%) described only blinding of the outcome assessor (see Figure 3 and Figure 4).
Incomplete outcome data
The follow‐up rate was described by all studies, ranging from 0% lost to follow‐up (Catani 2004; de Andrade 2009; Maruyama 2004; Shoji 1994; Tanzer 2002; Yagishita 2012) to 22% lost to follow‐up (Chaudhary 2008) (see Figure 3 and Figure 4).
Selective reporting
It seemed that 15 studies (88%) reported all outcome measures that were studied. Of these, Kim 2009 reported some outcomes (WOMAC and radiological results) in a digital appendix. Clark 2001 and de Andrade 2009 reported only the total Knee Society Score. It is more usual to report the clinical and functional score separately because this gives more insight into the nature of the possible differences between groups.
No studies were identified from the trial registries that were not still ongoing.
Clinical relevance
Clinical relevance is assessed in the table 'Assessment of clinical relevance' (Table 1). Most notable is that effect sizes of both the posterior cruciate ligament retaining and posterior cruciate ligament sacrificing groups reported in the studies were clinically not relevant in almost all of the studies.
| Study | Description patients | Intervention described | Outcome measures | Effect size |
| Are the patients described in detail so that you can decide whether they are comparable to those that you see in your practice? | Are the interventions and treatment settings described well enough so that you can provide the same for your patients? | Were all clinically relevant outcomes measured and reported? | Is the size of the effect clinically important? | |
| Aglietti 2004 | No | Yes | Yes | No |
| Catani 2004 | No | No | No | Yes |
| Chaudhary 2008 | Yes | Yes | Yes | No |
| Clark 2001 | Unsure | Yes | No | No |
| de Andrade 2009 | Unsure | Unsure | No | No |
| Harato 2008 | Unsure | Yes | Yes | No |
| Kim 2009 | Yes | Yes | Yes | No |
| Maruyama 2004 | Yes | Yes | Yes | No |
| Matsumoto 2012 | Yes | Unsure | Yes | No |
| Misra 2003 | No | No | No | No |
| Roh 2012 | Yes | Yes | Yes | No |
| Seon 2011 | Yes | Unsure | Yes | Yes |
| Shoji 1994 | No | No | No | No |
| Straw 2003 | No | Unsure | No | No |
| Tanzer 2002 | Yes | Yes | No | No |
| Wang 2004 | Yes | No | Yes | No |
| Yagishita 2011 | Yes | Yes | Yes | No |
Effects of interventions
See: Summary of findings for the main comparison Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs); Summary of findings 2 Posterior cruciate ligament retention versus sacrifice (using the same arthroplasty design); Summary of findings 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice
Forest plots are displayed in the 'Data collection and analysis' section. Furthermore, an overview is given in summary of findings Table for the main comparison, summary of findings Table 2 and summary of findings Table 3.
Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs)
These analyses included posterior cruciate retaining implant designs (sometimes used where the posterior cruciate ligament was sacrificed as well) and posterior stabilised posterior cruciate sacrificing designs. These were all studied implants included in this review.
Performance based outcome: range of motion, flexion and extension angle
Range of motion (reported in 65% of the studies, analysed on 62% of all potential patients and 65% of all potential knees) showed a mean difference of 2.4 ° (95% CI 0.13 to 4.61; P = 0.04) favouring posterior cruciate ligament sacrifice (118.3 ° versus 115.9 °). The results were heterogeneous (I2 = 60%, P = 0.006). In particular, the results of Catani 2004 were very different compared to the other studies; these results indicated a large 17 ° higher flexion angle in favour of sacrifice of the posterior cruciate ligament.
The flexion angle showed a mean difference of 1.5 ° (119.8 ° versus 118.3 °) in favour of posterior cruciate ligament sacrifice (95% CI 0.24 to 3.15; P = 0.09). The results were homogeneous (I2 = 6%, P = 0.39).
Result for the extension angle were heterogeneous (I2 = 88%, P < 0.001) and showed a statistically non‐significant difference of 0.36 ° (95% CI ‐0.63 to 1.36).
Knee pain
Two studies reported outcomes on the VAS for pain (Aglietti 2005; Yagishita 2012). The mean difference was 1.50 points (95% CI ‐1.84 to 4.84; P = 0.38) in favour of ligament retention. This result was homogeneous (I2 = 0%, P = 0.58). There was also no difference between knee pain, as measured with the Knee Society pain score (zero is no pain, 50 is maximal pain). The mean difference was 0.02 points (95% CI ‐1.43 to 1.38; P = 0.97). However, this result was considered heterogeneous (I2 = 71%, P = 0.02). This result was based on 36% of all patients, 46% of all knees, and data were reported in 24% of all included studies.
Implant survival rate
Several studies reported the survival rate of the arthroplasties. Aglietti 2005 reported one case of revision due to septic loosening in the cruciate‐sacrificing group. Chaudhary 2008 reported one revision in the cruciate‐retention group, Harato 2008 reported one revision in the cruciate‐retention group and three in the sacrifice group. Misra 2003 reported two revisions in the cruciate‐retention group. Kim 2009, Yagishita 2012 and Tanzer 2002 specifically reported that no revision surgery had occurred during their follow‐up.
Validated clinical scoring systems
A validated scoring system, the WOMAC total score, was used in four studies (24% of included studies with data on 28% of all patients and 24% of all knees) (Clark 2001; Harato 2008; Roh 2012; Seon 2011). There was a 0.78 (95% CI ‐1.51 to 3.07; P = 0.50) points difference between posterior cruciate ligament retention and sacrifice in favour of the posterior cruciate sacrifice (sacrifice versus retention: 15.7 versus 16.4 points). This difference was not statistically significant (P = 0.57) and was homogeneous (I2 = 0, P = 0.69). No other validated scoring systems (that is Knee injury and Osteoarthritis Outcome Score (KOOS), Oxford Knee Score) were available for pooling.
Patient satisfaction
Only Misra 2003 (one study, 6% of all included studies) asked patients to grade their satisfaction, on a scale from 0 to 10 with 10 being completely satisfied: cruciate‐sacrifice scored 7.9 and cruciate‐retention 7.7. This difference was not statistically significant.
Complications
Complications were reported in 11 studies (65% of all included studies, reporting on 69% of all patients and 74% of all knees). Complications are listed in Table 2. Complications occurred with equal frequency in the two treatment groups. Reported complications ranged from anterior knee pain (10 patients) and limited range of motion (14 patients) a few weeks after surgery to septic or aseptic loosening (4 and 5 patients respectively). The latter is a serious complication, also occurring equally often in the two treatment groups.
| Study | Complications posterior cruciate ligament retention | Complications posterior cruciate ligament sacrifice |
| Aglietti 2004 | None | 1 Septic loosening after 2 years requiring 2‐stage revision surgery |
| Catani 2004 | 1 Anterior knee pain; treated: lateral release and patella resurfacing, 1 Limited range of motion; treated: surgical manipulation | 2 Anterior knee pain; treated: lateral release and patella resurfacing |
| Chaudhary 2008 | 1 Deep infection | 1 Limited range of motion (poor flexion); treated: surgical manipulation |
| Clark 2001 | Not reported | Not reported |
| de Andrade 2009 | Not reported | Not reported |
| Harato 2008 | 7 Stiff knee (<90 degrees flexion), 5 severe/moderate knee pain, 1 infection 2 Hemoarthrosis | 1 Deep venous thrombosis, 3 infection, 1 stiff knee (<90 degrees flexion) 2 Severe/moderate knee pain |
| Kim 2009 | 2 Femoral notching, 1 superficial wound infection | 3 Femoral notching, 1 superficial wound infection |
| Maruyama 2004 | None | None |
| Matsumoto 2012 | None | 1 Deep venous thrombosis |
| Misra 2003 | 3 Instability, 1 infection, 2 aseptic loosening, 2 stiffness (<30 degrees flexion) | 3 Instability, 3 aseptic loosening, 2 stiffness (<30 degrees flexion), 1 Reflex sympathetic dystrophy |
| Roh 2012 | 2 posterior cruciate laxity 1 posterior cruciate tightness | None |
| Seon 2011 | Not reported | Not reported |
| Shoji 1994 | Not reported | Not reported |
| Straw 2003 | Not reported | Not reported |
| Tanzer 2002 | Not reported | Not reported |
| Wang 2004 | Not specified per treatment group: 3 deaths unrelated to the knee surgery, 3 deep wound infections, 1 above the knee amputation due to diabetic gangrene, 1 cerebral vascular accident, 1 Parkinsons disease, 1 colon cancer | |
| Yagishita 2011 | None | 1 Deep venous thrombosis |
Other endpoints
The Knee Society functional score showed a statistically significant 2.3 points higher score (81.3 versus 79.0 points) in the posterior cruciate ligament sacrificed groups (95% CI of the difference 0.37 to 4.26; P = 0.02). Results were homogeneous (I2= 0%, P = 0.43). This result was clinically not relevant. This score ranges from 0 to 100, 100 being optimal function.
Meta‐analyses on the other outcomes, as displayed in the Data and analyses section, showed no statistically significant differences. These outcomes were: Knee Society clinical score, Hospital for Special Surgery score, Short Form (SF)‐12 mental score, radiological radiolucencies, radiological femorotibial angle, radiological rollback, and radiological tibial slope.
Posterior cruciate ligament retention versus sacrifice (using the same arthroplasty design)
Posterior cruciate ligament sacrifice versus retention with the same arthroplasty design (a posterior cruciate retaining design) did not show a statistically significant difference in range of motion (mean difference 2.7 °; 95% CI ‐8.7 to 3.32; P = 0.38). Data were heterogeneous (I2 = 88%, P < 0.001). Range of motion was the only endpoint available for meta‐analysis.
Posterior cruciate ligament retention versus posterior stabilised sacrifice
Posterior cruciate ligament sacrifice versus retention with a posterior stabilised design showed a statistically significant difference in range of motion of 3.47 ° (116.5 ° versus 120.0 °) in favour of the posterior stabilised design (95% CI 0.56 to 6.38; P = 0.02). However, data were heterogeneous (I2 = 60%, P = 0.01).
The flexion angle was 2.10 ° higher (95% CI ‐0.04 to 4.24; P = 0.05) in favour of the posterior stabilised design. This was a homogeneous result (I2 = 1%, P = 0.42).
The outcomes VAS pain, Knee Society pain score, WOMAC total score, Knee Society clinical and functional score, Hospital for Special Surgery score, Knee Society total score, the number of radiolucent lines, the femorotibial angles and tibial slope showed no statistically significant differences and these results were homogeneous.
The outcomes extension angle, SF‐12 mental score and radiological rollback showed no statistically significant differences and these results were heterogeneous.
Discussion
Summary of main results
By thoroughly updating the original review (Jacobs 2005) we were able to add 10 studies, described in 11 articles, to the analyses (Aglietti 2005; Chaudhary 2008; de Andrade 2009; Harato 2008; Kim 2009; Matsumoto 2012; Roh 2012; Seon 2011; Victor 2005; Wang 2004; Yagishita 2012). Only two outcomes differed statistically when all selected studies reporting similar outcomes were pooled. The range of motion was 2.4 ° higher and the functional Knee Society score was 2.3 points higher in the group with sacrifice of the posterior cruciate ligament. Complications were reported in 11 studies (Aglietti 2005; Catani 2004; Chaudhary 2008; Harato 2008; Kim 2009; Maruyama 2004; Matsumoto 2012; Misra 2003; Roh 2012; Wang 2004; Yagishita 2012). Complications varied from anterior knee pain and femoral notching to deep infection. Most complications occurred equally frequently in the posterior cruciate ligament sacrificing and retaining groups (Table 2). A remarkable finding in Harato 2008 was that the posterior cruciate ligament retaining group showed seven cases (6.3%) of a stiff knee, defined as < 90 ° of flexion, compared to one case (0.9%) in the posterior cruciate ligament sacrificing group.
The meta‐analyses showed statistically significant differences in range of motion and in the Knee Society functional score. Although the evidence originates from a meta‐analysis of more than one randomised controlled trial, one should be aware that the effect is still unstable and sensitive to the inclusion of new studies. Moreover, the mean difference in range of motion of 2.4 ° and in mean Knee Society functional score of 2.3 points are considered clinically not relevant (Pijls 2011). The table 'Assessment of clinical relevance' (Table 1) shows that most reported outcomes are not clinically relevant. The original review also showed a statistically significant mean difference in the Hospital for Special Surgery score of 1.6 points (P = 0.03) (Jacobs 2005) in favour of posterior cruciate ligament sacrifice arthroplasty. This difference, small and clinically not relevant, has disappeared in this review.
In order to have an impression of the difference in pain experienced between both groups we extracted data on pain from all studies. Four studies reported data on pain (Harato 2008; Kim 2009; Wang 2004; Yagishita 2012). All four presented the pain score as derived from the Knee Society Knee score. No study showed different scores per answer of the Knee score so it is not entirely clear how these pain scores were derived. Two studies used the VAS to evaluate the pain experienced by patients yielding no differences between retention or sacrifice of the posterior cruciate ligament (Aglietti 2005; Yagishita 2012).
The quality of the evidence, graded with the GRADE approach, ranged from moderate to low (summary of findings Table for the main comparison; summary of findings Table 2; summary of findings Table 3). No harmful outcomes were presented in the summary of findings tables in this review due to the absence of reporting of sufficient data.
Overall completeness and applicability of evidence
Because of our broad and thorough search we were able to find 10 additional studies to the previous review, increasing completeness of the evidence. Overall, outcome measures studied in the selected studies give solid indications on the clinical, functional and radiological features one might be interested in after total knee arthoplasty. Unfortunately, patient‐oriented outcomes such as patient satisfaction were hardly ever studied. An exception is Misra 2003, who asked patients to grade their satisfaction on a scale from one to 10.
Despite the fact that randomised controlled trials are described as providing the least biased evidence, the mean survival rate of total knee arthroplasty cannot be easily investigated by randomised controlled trials. Long term follow‐up evaluations in observational cohort studies are valuable alternatives. A survivorship analysis report on a large cohort of 11,606 total knee arthroplasties showed a mean survival rate at 10 years after surgery of 91% (95% CI 90 to 92) in the posterior cruciate ligament retention group and 76% (95% CI 62 to 86) in the posterior cruciate ligament sacrificing posterior stabilised group (Rand 2003). Abdel et al found similar results (Abdel 2011).
In the more recent years, the high demands in performance of total knee arthroplasty in certain ethnic (for example squatting position) and religious (for example prayer position) groups as well as in younger patients who require greater magnitudes of knee flexion has led to the development of newer implants. Together with the continuing process of optimising stability and kinematics in total knee arthroplasty, high flex posterior stabilised and bi‐cruciate stabilising designs were introduced. Long term follow‐up studies have yet to prove whether those implants indeed show improved results compared to the more established design types. In this review, Kim 2009, Seon 2011 and Yagishita 2012 studied high flexion total knee arthroplasties.
Quality of the evidence
In the original Cochrane review, the quality of the included studies was assessed using the van Tulder and Jadad checklist (Jacobs 2005). Catani (Catani 2004), Misra (Misra 2003) and Tanzer (Tanzer 2002) were regarded as high quality studies. However, The Cochrane Collaboration nowadays discourages the use of scales assessing the quality (Higgins 2011). To assess quality and risk of bias, risk of bias tables were used as advocated by The Cochrane Collaboration. Several items were evaluated, first the method of generation of randomisation sequence. This should be based on chance and should be reported clearly to avoid doubt about bias. Together with the method of concealment of treatment allocation these items indicate the risk of selection bias. Treatment allocation has to be completely at random; knowledge of the next allocation by the care provider could result in an 'awkward' patient either being at risk of being illegally excluded from the trial or of being assigned to the other treatment group. This will lead to an overestimation of the treatment effect (Wood 2008). A valid randomisation technique is applied just before the treatments are given, thus ensuring unpredictable allocation. There are several techniques to keep the allocation unpredictable, such as sealed envelopes or a telephone call to a research centre for the treatment allocations. It was chosen to include quasi‐randomised trials in the review as well. Quasi‐randomisation is randomisation based on odd or even chart numbers, dates of birth, alternating sequences, day of hospital admission etc. The risk of selection bias in this kind of randomisation is higher compared to pure randomisation. Another item is blinding. In most surgical trials blinding of the surgeon is impossible. However, the patients and the observers measuring the endpoints can be blinded for the studied intervention. Well‐blinded studies reduce risk of performance and detection bias. Furthermore, incomplete outcome data raise the possibility that the outcome is biased. When almost all anticipated outcome data are available the risk of attrition bias is low. Additionally, selection‐by‐indication bias was taken into account. This can only be corrected for if the degree of preoperative flexion contracture, valgus or varus deformity, is mentioned in the articles. Unfortunately the selected studies did not report these factors, except for one study that stated that a valgus or varus deformity in excess of 15 ° was an exclusion criterion (Chaudhary 2008).
The Cochrane Collaboration encourages the use of the GRADE approach (Atkins 2004). This GRADE approach defines "the quality of a body of evidence as the extent to which one can be confident that an estimate of effect or association is close to the quantity of specific interest" (Higgins 2011). Randomised controlled trials are considered as yielding high quality evidence. However, this grade can be downgraded to moderate, low or very low quality due to limitations in the design suggesting the likelihood of bias, indirectness of evidence, unexplained heterogeneity or inconsistency in the results, imprecision of the results, and a high probability of publication bias (Higgins 2011). Results were presented in the summary of findings tables. The Cochrane Collaboration encourages review authors to present the most important outcomes in these tables, including both beneficial and harmful outcomes. In this review serious adverse effects (for example serious complications) would be a harmful outcome, however the amount of data from the selected studies were not sufficient.
The quality of the evidence, graded with the GRADE approach, was low for range of motion, and moderate for the outcomes flexion angle and knee pain. In the subgroup analysis of posterior cruciate ligament retention and sacrifice with the same (cruciate‐retaining) arthroplasty design the evidence was graded ‘very low’ for the outcome range of motion. In the other subgroup analyses (cruciate‐retaining versus posterior stabilised) the evidence was moderate for the outcome range of motion (summary of findings Table for the main comparison; summary of findings Table 2; summary of findings Table 3).
The risk of bias estimations are displayed for all selected studies in the 'Characteristics of included studies' risk of bias tables. The studies regarded as having the least risk of bias from the current selection of articles are Chaudhary (Chaudhary 2008), Kim (Kim 2009), and Misra (Misra 2003). Except for Misra 2003 these are newly added studies. There seems to be a positive trend towards better methodologically performed and reported studies in the more recent years. However, because of the incomplete description of the methodology of the trials it was difficult to assess whether the methodology was inaccurate or the description of the methodology was just lacking information. None of the selected studies could be judged on all four items described above. Selection bias items were not described in 53% of the articles (9/17), performance bias in 41% (7/17), and attrition bias in 24% (4/17) of the studies. The summary of findings tables show the results of the quality appraisal by the GRADE approach. All outcomes were downgraded from high quality to moderate or even low quality.
Reporting of external funding could influence the likelihood of publication of the study. From the selected studies only one industry funded study was found (Chaudhary 2008). One study reported a non‐commercial grant from the National Council of Science (Wang 2004). Eight studies did not describe external funding (Aglietti 2005; Clark 2001; de Andrade 2009; Harato 2008; Maruyama 2004; Matsumoto 2012; Roh 2012; Shoji 1994). From the same study population described by Harato et al (Harato 2008) the report of Victor (Victor 2005) reported no external funding. The rest of the selected studies explicitly reported no external funding.
Potential biases in the review process
This review has several strengths and limitations. As mentioned before, randomised controlled trials are not the best studies to evaluate implant survival (for example 10 or 15 year survival) because follow‐up is usually too short in trials. Since implant survival is an important outcome after total knee arthroplasty this is a limitation. Furthermore, we could not present information on patient experience and satisfaction after total knee arthroplasty because these data were not presented in the selected studies. Even in a systematic review, publication bias can never be ruled out with certainty. We applied a relatively broad search strategy in multiple databases. Nevertheless, some references could not be indexed in the databases; therefore we also used citation tracking and we checked the reference lists of the included articles. Screening the international trials registers via the portal of the World Health Organization (www.who.int/trialsearch), four trials, tagged with an ongoing status, were found (ACTRN12609000960257; ISRCTN05635855; ISRCTN82612978; van den Boom 2009). For one of these studies, the study protocol was published ahead of starting the trial (van den Boom 2009). No clinically relevant differences and only two statistically significant differences were found comparing the two groups in our meta‐analyses, this might be due to a power problem. In the next update of the review these four studies can possibly overcome this problem.
This systematic review with meta‐analysis was composed in accordance with the criteria of the PRISMA statement (Preferred Reporting Items for Systematic reviews and Meta‐Analyses) (Liberati 2009). This is a revision and expansion of the QUORUM statement (QUality Of Reporting Of Meta‐analyses). Another strength is that we applied a broad and extensive search strategy.
Agreements and disagreements with other studies or reviews
Similar to the randomised and quasi‐randomised controlled trials selected in this review, other orthopaedic literature on this topic shows inconclusive results. Range of motion, for example, is the parameter most often measured. Only two randomised controlled trials (Catani 2004; Straw 2003) found a statistically significant difference, favouring posterior cruciate ligament sacrifice. One study (Stiehl 1997) found a superior range of motion for a posterior cruciate ligament retaining total knee arthroplasty and another study (Maloney 1992) for a posterior stabilised design. However, both studies showed a higher preoperative range of motion for the group with the superior results. Hirsch (Hirsch 1994) found a superior range of motion for a posterior stabilised design over posterior cruciate ligament sacrifice in a total knee arthroplasty without posterior stabilisation. Preoperative range of motion is believed to have a large influence on the postoperative results. Therefore, improvement of range of motion should be calculated and reported as well. The method of assessment of range of motion was not described in all reports. The measurement of range of motion is notoriously inaccurate if performed clinically (Kafer 2005).
Clinical rating scales are considered not very sensitive tools to evaluate the difference between two implant designs when only total scores are reported. WOMAC and KOOS scales are better validated and hence are preferred instruments for use in clinical trials. The studies in this review did not find any difference. Other non‐randomised studies show the same results; several studies found no difference on the Hospital for Special Surgery score between a posterior cruciate ligament retaining and a posterior stabilised design (Becker 1991; Pereira 1998; Vinciguerra 1994).
Technically relevant outcome measures are the outcomes anterior‐posterior stability and contact position. These measurements were not addressed in any of the studies. One laboratory study concludes that proper balancing is imperative to achieve proper rollback (Most 2003). De Jong et al found an average contact point between the femur and tibia at the posterior two‐thirds of the anteroposterior distance of the tibia and assumed that this is also the correct contact point for a replaced cruciate retaining knee implant and a correctly balanced posterior cruciate ligament (de Jong 2010). Balancing of the posterior cruciate ligament is technically more difficult due to the oblique orientation of the posterior cruciate ligament in flexion and a strong 3 to 5 mm anterior translation of the tibia with a 2 mm increase of the insert thickness (Christen 2007; Heesterbeek 2010).
Several studies using fluoroscopy suggest that participants having a posterior stabilised total knee arthroplasty have less abnormal knee kinematics in deeper flexion and greater flexion than participants having a posterior cruciate ligament retaining total knee arthroplasty (Dennis 1998; Garling 2005; Udomkiat 2000; Victor 2005; Wolterbeek 2009; Wolterbeek 2011). As mentioned before, the posterior cruciate ligament is reported to have proprioceptive properties (Hogervorst 1998; Nelissen 2001; Swanik 2004). Another study found no difference in proprioception between a posterior cruciate ligament retaining and a posterior stabilised design (Cash 1996). Simmons 1996 found no difference in proprioception in moderate grades of osteoarthritis, but in higher osteoarthritis grades the posterior cruciate ligament retaining group performed better than the sacrificing group.
Gait analysis could provide additional but generally unvalidated results. In this review we did not find any randomised controlled trials evaluating gait analysis. Dennis et al found in two (fluoroscopic) studies that posterior cruciate ligament retaining and posterior stabilised arthroplasties have similar kinematic patterns in early flexion activities such as gait (Dennis 2003; Dennis 2004). Bolanos et al performed gait analysis on posterior cruciate ligament retaining and posterior stabilised arthroplasties and found no statistically significant differences in range of motion or knee flexion moments during a level gait (Bolanos 1998). A recent study showed no differences in gait analysis parameters between posterior cruciate ligament retention and posterior stabilised total knee arthroplasty with the ligament resected in both treatment arms (Joglekar 2012). Ishii 1998 found increased abduction and adduction and increased proximal and distal translation during gait analysis for the posterior stabilised design, which may indicate decreased stability; however the results did not differ significantly.
There are other issues to be considered in total knee replacement surgery like the choice of what kind of bearing system is to be used. Jacobs 2004(2) performed a Cochrane systematic review to answer this question, this review is currently in update phase. Another question is whether or not to use cement on the implants, and Nakama 2012 has performed a Cochrane systematic review to answer this question. We refer to these reviews for more in‐depth information on these issues.

Bicondylar ligament cruciate retaining balancing total knee arthroplasty with rotating platform (balanSys®, Mathys Ltd., Bettlach, Switzerland) Hirschmann et al. BMC Musculoskeletal Disorders 2010 11:167 doi:10.1186/1471‐2474‐11‐167
Download authors' original image

Study flow diagram (PRISMA).

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
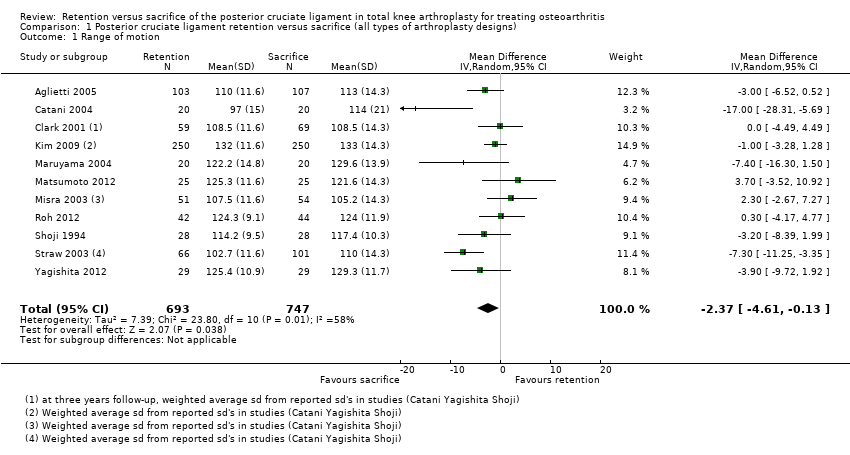
Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 1 Range of motion.
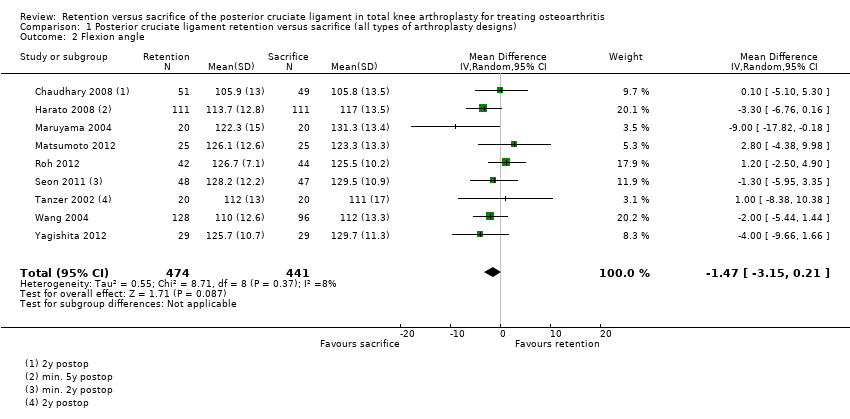
Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 2 Flexion angle.

Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 3 Extension angle.

Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 4 VAS pain.

Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 5 Knee pain (KSS pain).
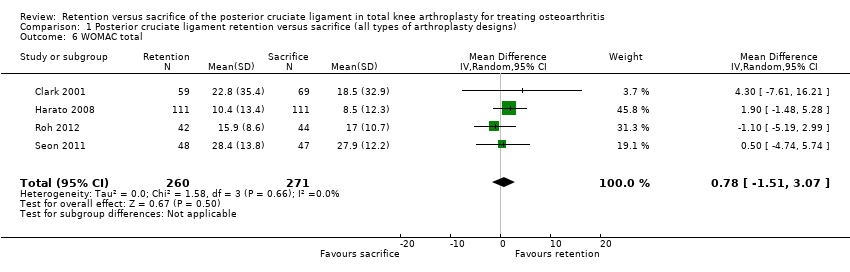
Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 6 WOMAC total.

Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 7 Knee Society Clinical score.
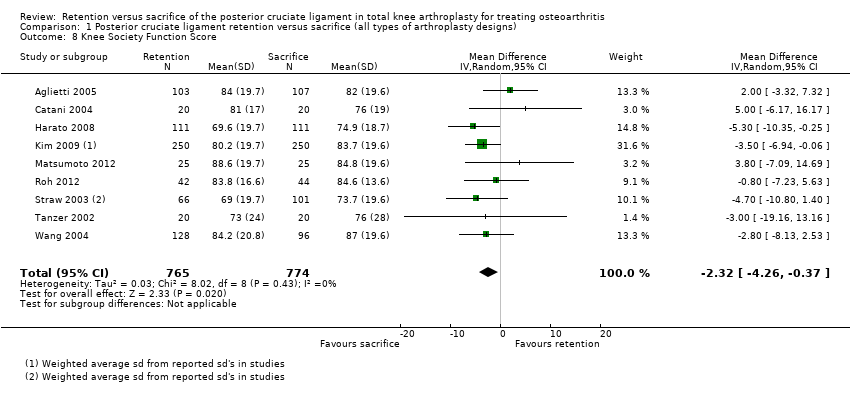
Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 8 Knee Society Function Score.

Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 9 Hospital Special Surgery Score.

Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 10 Knee Society Score overall.

Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 11 SF‐12 mental.

Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 12 Radiological: Radiolucent lines.
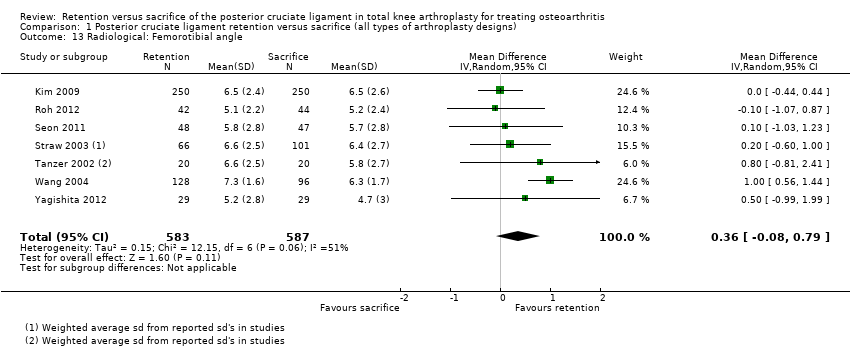
Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 13 Radiological: Femorotibial angle.

Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 14 Radiological: Rollback (in mm).

Comparison 1 Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs), Outcome 15 Radiological: Tibial slope.

Comparison 2 Posterior cruciate ligament retention versus sacrifice (using the same arthroplasty design), Outcome 1 Range of motion.

Comparison 2 Posterior cruciate ligament retention versus sacrifice (using the same arthroplasty design), Outcome 2 Improvement of range of motion.

Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 1 Range of motion.

Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 2 Flexion angle.
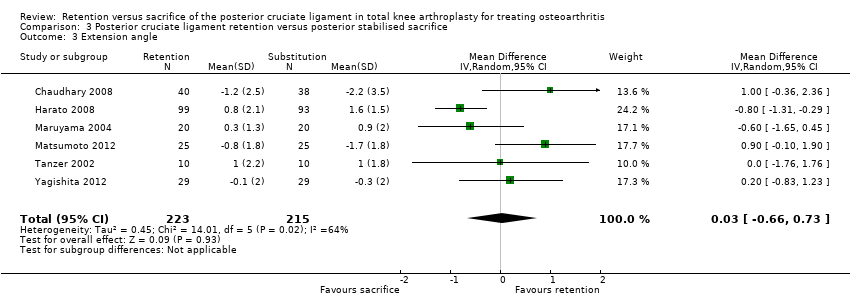
Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 3 Extension angle.

Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 4 VAS pain.

Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 5 Knee pain (KSS pain).
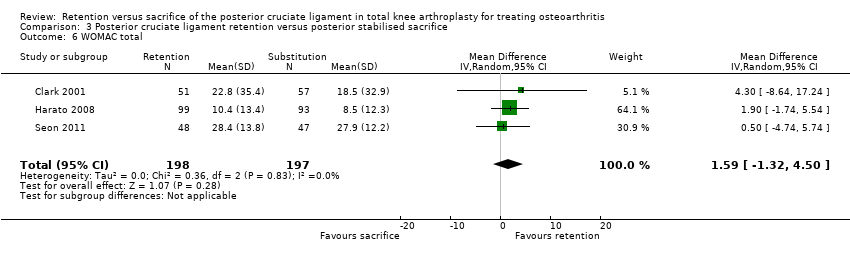
Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 6 WOMAC total.
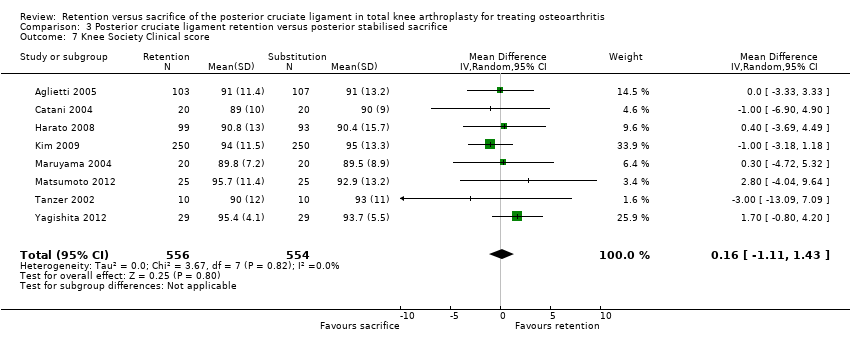
Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 7 Knee Society Clinical score.
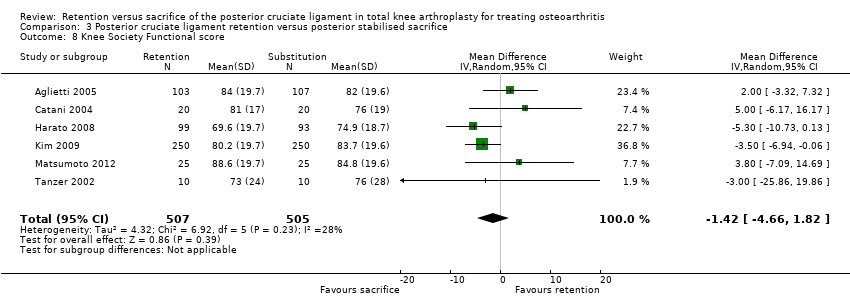
Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 8 Knee Society Functional score.

Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 9 Hospital Special Surgery score.
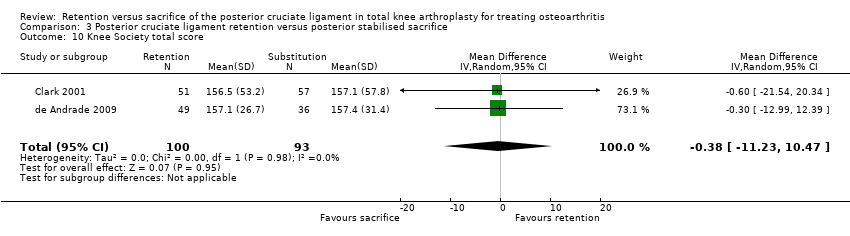
Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 10 Knee Society total score.

Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 11 SF‐12 mental.
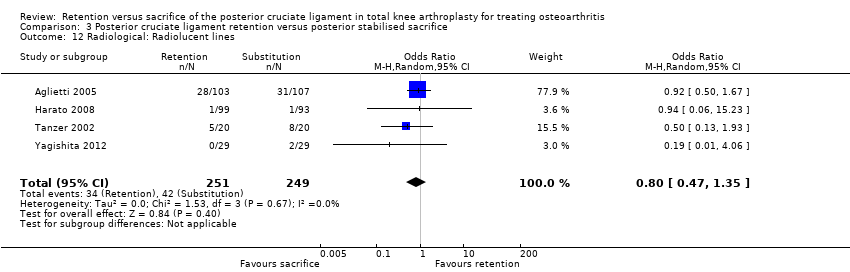
Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 12 Radiological: Radiolucent lines.
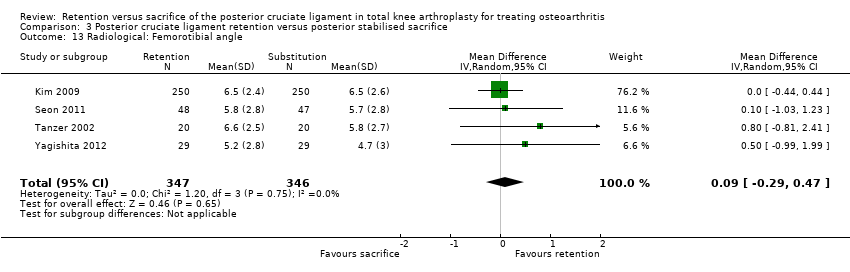
Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 13 Radiological: Femorotibial angle.

Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 14 Radiological: Rollback.
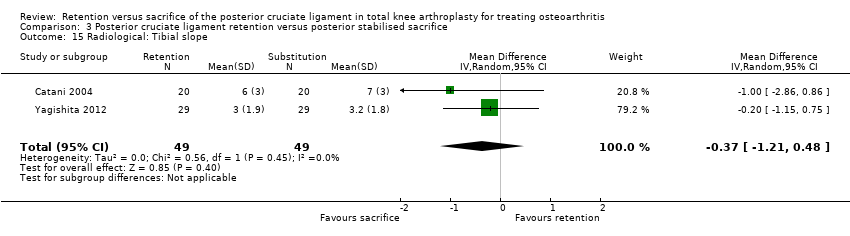
Comparison 3 Posterior cruciate ligament retention versus posterior stabilised sacrifice, Outcome 15 Radiological: Tibial slope.
| Posterior cruciate ligament retention versus sacrifice (all types of arthroplasty designs) | |||||||
| Patient or population: Patients receiving total knee arthroplasty with or without posterior stabilised design for the treatment of osteoarthritis | |||||||
| Outcomes | Comparative risks | Relative effect | No. of patients (% of total) | No. of studies (% of total) | Quality of the evidence | Comments | |
| Cruciate‐sacrifice | Cruciate‐retention | ||||||
| Performance based measures ‐ Range of motion (possible range 0 (worst) to 140 (maximal) degrees) Follow‐up: 12‐78 months1 | The mean range of motion in the cruciate‐sacrifice group was 118.3 degrees (± SE 0.53) | The mean range of motion in the cruciate‐retaining group 2.40 lower (4.61 lower to 0.13 higher) | Total No. of patients: 1,119 (62%) Total No. of knees: 1,440 (65%) | 11 studies (65%) | ⊕⊕⊝⊝ | Absolute difference 2.40 lower (4.61 lower to 0.13 higher) Relative percent change: ‐2.0% (3.9% lower to 0.1% higher) Not statistically significant. | |
| Knee pain Knee Society Score, sub score pain (possible range of points 0 (severe pain) ‐ 50 (no pain)) Follow‐up: 24‐87 months years | The mean knee pain score in the cruciate‐sacrifice group was 48.3 points (± SE 0.54) | The mean knee pain score in the cruciate‐retention group was 0.01 higher (1.40 lower to 1.43 higher) | Total No. of patients: 656 (36%) Total No. of knees: 1,004 (46%) | 4 studies (24%) | ⊕⊕⊕⊝ | Absolute difference: 0.01 higher (1.40 lower to 1.43 higher) Relative percent change: 0.0% (2.9% lower to 3.0% higher) Not statistically significant. | |
| Survival rate of the implant (Revision surgery reported) Follow‐up: 17‐87 months | See comment | See comment | Not estimable | Total No. of patients: 926 (51%) Total No. of knees: 1,229 (56%) | 7 studies (41%) | See comment | Insufficient data provided. Incidental remarks on implant survival could be derived from 7 studies. One study Misra 2003 reported 2 revisions in de cruciate‐retention group, Chaudhary 2008 1 in the cruciate‐retention group, Harato 2008 1 in the cruciate‐retention group and 3 in the sacrifice group. Aglietti 2005 1 revision in the cruciate‐sacrifice group due to septic loosening Kim 2009, Yagishita 2012 and Tanzer 2002 specifically reported no revision surgery had occurred during follow‐up |
| Health related quality of life measures and functional measures with validated instruments (WOMAC, range 0‐100, higher scores indicate worse pain, stiffness and functional limitations) Follow‐up: 24‐87 months | The mean WOMAC total score in the cruciate‐sacrifice group was 15.0 points (± SE 1.2) | The mean WOMAC total score in the cruciate‐retention group was 0.78 higher (1.51 lower to 3.07 higher) | Total No. of patients: 501 (28%) Total No. of knees: 531 (24%) | 4 studies (24%) | ⊕⊕⊝⊝ | Absolute difference: 0.78 higher (1.51 lower to 3.07 higher) Relative percent change: 5.2% (10.0% lower to 20.5% higher) Not statistically significant. | |
| Global assessment (patient) Patient satisfaction on scale 0 (not at all satisfied) to 10 (completely satisfied) Follow‐up: 12‐83 months | The mean satisfaction score in the cruciate‐sacrifice group was 7.910 | The mean satisfaction score in the cruciate‐retention group was 0.2 lower10 | Total No. of patients: 103 (6%) Total No. of knees: 105 (5%) | 1 study (6%) | ⊕⊕⊝⊝ | Absolute difference: 0.2 lower 10 Relative percent change: ‐2.5% 10 Not statistically significant. | |
| Complications Follow‐up: 8‐87 months7 | See comment | See comment | Not estimable | Total No. of patients: 1,252 (69%) Total No. of knees: 1,635 (74%) | 11 studies (65%) | See comment | Due to the very diverse way of reporting and defining complications combining data for quantitative analysis was not possible8,9 |
| Re‐operation rate (not involving implant change, short and long term) Follow‐up: 24 months | See comment | See comment | Not estimable | Total No. of patients: 40 (2%) | 1 study (6%) | See comment | Catani 2004 reported 4 re‐operations; 3 patella luxations (2 in cruciate‐sacrificing, 1 in cruciate‐retention group) and 1 surgical manipulation due to lack of range of motion (in the cruciate‐retention group) |
| CI: Confidence interval; KSS: Knee Society Score, WOMAC: Western Ontario and McMasters Universities Osteoarthritis Index. NA: not applicable | |||||||
| GRADE Working Group grades of evidence | |||||||
| 1 Median follow‐up: 2 years 7 Some studies reported complications after several months. Mean follow‐up of other endpoints was > 1 year 8 Complications reported in the cruciate‐sacrifice group: 4 anterior knee pain, 4 limited range of motion, 1 deep venous thrombosis, 3 instability, 3 femoral notching, 3 aseptic loosening, 3 (deep) infection 9 Complications reported in the cruciate‐retention group: 6 anterior knee pain, 10 limited range of motion, 0 deep venous thrombosis, 3 instability, 2 femoral notching, 2 aseptic loosening, 3 (deep) infection, 2 ligament laxity, 1 ligament tightness 10 Not sufficient data reported to calculate standard error, range or confidence interval | |||||||
| Posterior cruciate ligament retention versus sacrifice (using the same arthroplasty design) | |||||||
| Patient or population: Patients receiving total knee arthroplasty with or without resection of the posterior cruciate ligament for the treatment of osteoarthritis | |||||||
| Outcomes | Comparative risks | Relative effect | No. of patients (% of total) | No of studies (% of total) | Quality of the evidence | Comments | |
| Cruciate‐sacrifice | Cruciate‐retention | ||||||
| Performance based measures ‐ Range of motion (possible range 0 (worst) to 140 (maximal) degrees) Follow‐up: 12‐78 months | The mean range of motion in the cruciate‐sacrifice group was 114.1 degrees (± SE 0.82) | The mean range of motion in the cruciate‐retention group was 2.7 degrees lower (8.71 lower to 3.32 higher) | Total No. of patients: 405 (22%) Total No. of knees: 414 (19%) | 4 studies (24%) | ⊕⊝⊝⊝ | Absolute difference: 2.7 degrees lower (8.71 lower to 3.32 higher) Relative percent change: ‐2.4% (7.6% lower to 2.9% higher) Not statistically significant. | |
| Knee pain Knee Society Score, sub score pain (possible range 0 (severe pain) ‐ 50 (no pain) points) | See comment | See comment | Not estimable | ‐ | ‐ | See comment | No data in studies comparing ligament resection and sacrifice using similar arthroplasty designs |
| Survival rate of the implant (Revision surgery reported) Follow‐up: 56‐60 months | See comment | See comment | Not estimable | Total No. of patients: 103 (6%) Total No. of knees: 105 (5%) | 1 study (6%) | See comment | Insufficient data provided. One study (Misra 2003) reported 2 revisions in the cruciate‐retention group. |
| Health related quality of life measures and functional measures with validated instruments (WOMAC, range 0‐100, higher scores indicate worse pain, stiffness and functional limitations) Follow‐up: 24‐37 months | The mean WOMAC total score in the cruciate‐sacrifice group was 17.0 points (± SE 1.1) | The mean WOMAC total score in the cruciate‐retention group was 1.10 lower (‐5.19 lower to 2.99 higher) | Total No. of patients: 86 (5%) Total No. of knees: 86 (4%) | 1 study (6%) | See comment | One study reported this outcome: Roh 2012 Absolute difference: 1.10 lower (‐5.19 lower to 2.99 higher) Relative percent change: ‐6.5% (30.5% lower to 17.6%higher) Not statisitically significant | |
| Global assessment (patient) Patient satisfaction on scale 0 (not at all satisfied) to 10 (completely satisfied)) Follow‐up: 12‐83 months | The mean satisfaction score in the cruciate‐sacrifice group was 7.97 | The mean satisfaction score in the cruciate‐retention group was 0.2 lower7 | Total No. of patients: 103 (6%) Total No. of knees: 105 (5%) | 1 study (6%) | ⊕⊕⊝⊝ | Absolute difference: 0.2 lower 7 Relative percent change: ‐2.5% 7 Not statistically significant. | |
| Complications Follow‐up: 12‐78 months | See comment | See comment | Not estimable | Total No. of patients: 405 (22%) Total No. of knees: 414 (19%) | 4 studies (24%) | See comment | Due to the very diverse way of reporting and defining complications combining data for quantitative analysis was not possible5,6 |
| Re‐operation rate (not involving implant change, short and long term) | See comment | See comment | Not estimable | ‐ | ‐ | See comment | No data in studies comparing ligament resection and sacrifice using similar arthroplasty designs |
| CI: Confidence interval. KSS: Knee Society Score, WOMAC: Western Ontaria and McMasters Universities Osteoarthritis Index. NA: not applicable | |||||||
| GRADE Working Group grades of evidence | |||||||
| 1 Risk of bias individual studies, see risk of bias tables 5 Complications reported in the cruciate‐sacrifice group: 3 instability, 3 aseptic loosening, 2 stiffness 6 Complications reported in the cruciate‐retention group: 3 instability, 1 infection (deep), 2 aseptic loosening, 2 stiffness, 2 ligament laxity, 1 ligament tightness 7 Not sufficient data reported to calculate standard error, range or confidence interval | |||||||
| Posterior cruciate ligament retention versus posterior stabilised sacrifice | |||||||
| Patient or population: Patients receiving total knee arthroplasty with or without posterior stabilised design for the treatment of osteoarthritis | |||||||
| Outcomes | Mean differences (95% CI) | Relative effect | No. of patients (% of total) | No. of studies (% of total) | Quality of the evidence | Comments | |
| Cruciate‐sacrifice (posterior stabilised) | Cruciate‐retention | ||||||
| Performance based measures ‐ Range of motion (possible range 0 (worst) to 140 (maximal) degrees) Follow‐up: 1‐6.5 years1 | The mean range of motion in the cruciate‐sacrifice group was 119.8 degrees (± SE 0.66) | The mean range of motion in the cruciate‐retention group was 3.4 degrees lower (6.32 to 0.54 lower) | Total No. of patients: 899 (50%) Total No. of knees: 1,193 (54%) | 8 studies (47%) | ⊕⊕⊕⊝ | Absolute difference: ‐3.4 degrees (6.32 to 0.54 lower) Relative percent change: ‐2.8% (5.3% lower to 0.45% higher) Statistically significant (P = 0.02) NNTB: 9 (5 to 51) | |
| Knee pain Knee Society Score, subscore pain (possible range 0 (severe pain) ‐ 50 (no pain) points) Follow‐up: 2‐7.3 years | The mean knee pain score in the cruciate‐sacrifice group was 48.3 points (± SE 0.68) | The mean knee pain score in the cruciate‐retention group was 0.60 higher (0.39 lower to 1.60 higher) | Total No. of patients: 471 (26%) Total No. of knees: 780 (35%) | 3 studies | ⊕⊕⊕⊝ | Absolute difference: 0.60 (0.39 lower to 1.60 higher) Relative percent change: 1.2% (0.81% lower to 3.3% higher) Not statistically significant. | |
| Survival rate of the implant (Revision surgery reported) | See comment | See comment | Not estimable | Total No. of patients: 802 (44%) Total No. of knees: 1,100 (50%) | 6 studies (35%) | See comment | Insufficient data provided. Incidental remarks on implant survival could be derived from 6 studies. Chaudhary 2008 1 in the cruciate‐retention group, Harato 2008 1 in the cruciate‐retention group and 3 in the sacrifice group. Aglietti 2005 1 revision in the cruciate‐sacrifice group due to septic loosening Kim 2009, Yagishita 2012 and Tanzer 2002 specifically reported no revision surgery had occurred during follow‐up |
| Health related quality of life measures and functional measures with validated instruments (WOMAC, range 0‐100, higher scores indicate worse pain, stiffness and functional limitations) Follow‐up: 24‐87 months | The mean WOMAC total score in the cruciate‐sacrifice group was 18.2 points(± SE 1.5) | The mean WOMAC total score in the cruciate‐retention group was 1.60 lower (1.32 lower to 4.50 higher) | Total No. of patients: 415 (23%) Total No. of knees: 445 (20%) | 3 studies (18%) | ⊕⊕⊝⊝ | Absolute difference: 1.60 lower (1.32 lower to 4.50 higher) Relative percent change: ‐8.8% (7.3% lower to 24.7% higher) Not statistically significant. | |
| Global assessment (patient) | See comment | See comment | Not estimable | ‐ | ‐ | See comment | No data in studies comparing ligament resection and sacrifice using similar arthroplasty designs |
| Complications Follow‐up: 8‐87 months5 | See comment | See comment | Not estimable | Total No. of patients: 878 (49%) Total No. of knees: 1,220 (55%) | 8 studies (47%) | See comment | Due to the very diverse way of reporting and defining complications combining data for quantitative analysis was not possible3,4 |
| Re‐operation rate (not involving implant change, short‐ and long‐term) Follow‐up: 24 months | See comment | See comment | Not estimable | Total No. of patients: 40 (2%) | 1 study (6%) | See comment | Catani 2004 reported 4 re‐operations; 3 patella luxations (2 in cruciate‐sacrificing, 1 in cruciate‐retention group) and 1 surgical manipulation due to lack of range of motion (in the cruciate‐retention group) |
| CI: Confidence interval. KSS: Knee Society Score, WOMAC: Western Ontaria and McMasters Universities Osteoarthritis Index. ROM range of motion NA: not applicable | |||||||
| GRADE Working Group grades of evidence | |||||||
| 1 Relatively many studies with 'unclear' risk of bias 2 < 400 arthroplasties in analysis 3 Complications reported in the cruciate‐sacrifice group: 2 anterior knee pain, 3 femoral notching, 1 superficial wound infection, 2 deep venous thrombosis, 1 septic loosening 4 Complications reported in the cruciate‐retention group: 1 anterior knee pain, 1 limited ROM, 2 femoral notching, 1 superficial wound infection 5 Some studies reported complications after several months. Mean follow‐up of other endpoints was > 1 year | |||||||
| Study | Description patients | Intervention described | Outcome measures | Effect size |
| Are the patients described in detail so that you can decide whether they are comparable to those that you see in your practice? | Are the interventions and treatment settings described well enough so that you can provide the same for your patients? | Were all clinically relevant outcomes measured and reported? | Is the size of the effect clinically important? | |
| Aglietti 2004 | No | Yes | Yes | No |
| Catani 2004 | No | No | No | Yes |
| Chaudhary 2008 | Yes | Yes | Yes | No |
| Clark 2001 | Unsure | Yes | No | No |
| de Andrade 2009 | Unsure | Unsure | No | No |
| Harato 2008 | Unsure | Yes | Yes | No |
| Kim 2009 | Yes | Yes | Yes | No |
| Maruyama 2004 | Yes | Yes | Yes | No |
| Matsumoto 2012 | Yes | Unsure | Yes | No |
| Misra 2003 | No | No | No | No |
| Roh 2012 | Yes | Yes | Yes | No |
| Seon 2011 | Yes | Unsure | Yes | Yes |
| Shoji 1994 | No | No | No | No |
| Straw 2003 | No | Unsure | No | No |
| Tanzer 2002 | Yes | Yes | No | No |
| Wang 2004 | Yes | No | Yes | No |
| Yagishita 2011 | Yes | Yes | Yes | No |
| Study | Complications posterior cruciate ligament retention | Complications posterior cruciate ligament sacrifice |
| Aglietti 2004 | None | 1 Septic loosening after 2 years requiring 2‐stage revision surgery |
| Catani 2004 | 1 Anterior knee pain; treated: lateral release and patella resurfacing, 1 Limited range of motion; treated: surgical manipulation | 2 Anterior knee pain; treated: lateral release and patella resurfacing |
| Chaudhary 2008 | 1 Deep infection | 1 Limited range of motion (poor flexion); treated: surgical manipulation |
| Clark 2001 | Not reported | Not reported |
| de Andrade 2009 | Not reported | Not reported |
| Harato 2008 | 7 Stiff knee (<90 degrees flexion), 5 severe/moderate knee pain, 1 infection 2 Hemoarthrosis | 1 Deep venous thrombosis, 3 infection, 1 stiff knee (<90 degrees flexion) 2 Severe/moderate knee pain |
| Kim 2009 | 2 Femoral notching, 1 superficial wound infection | 3 Femoral notching, 1 superficial wound infection |
| Maruyama 2004 | None | None |
| Matsumoto 2012 | None | 1 Deep venous thrombosis |
| Misra 2003 | 3 Instability, 1 infection, 2 aseptic loosening, 2 stiffness (<30 degrees flexion) | 3 Instability, 3 aseptic loosening, 2 stiffness (<30 degrees flexion), 1 Reflex sympathetic dystrophy |
| Roh 2012 | 2 posterior cruciate laxity 1 posterior cruciate tightness | None |
| Seon 2011 | Not reported | Not reported |
| Shoji 1994 | Not reported | Not reported |
| Straw 2003 | Not reported | Not reported |
| Tanzer 2002 | Not reported | Not reported |
| Wang 2004 | Not specified per treatment group: 3 deaths unrelated to the knee surgery, 3 deep wound infections, 1 above the knee amputation due to diabetic gangrene, 1 cerebral vascular accident, 1 Parkinsons disease, 1 colon cancer | |
| Yagishita 2011 | None | 1 Deep venous thrombosis |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Range of motion Show forest plot | 11 | 1440 | Mean Difference (IV, Random, 95% CI) | ‐2.37 [‐4.61, ‐0.13] |
| 2 Flexion angle Show forest plot | 9 | 915 | Mean Difference (IV, Random, 95% CI) | ‐1.47 [‐3.15, 0.21] |
| 3 Extension angle Show forest plot | 7 | 734 | Mean Difference (IV, Random, 95% CI) | 0.36 [‐0.61, 1.32] |
| 4 VAS pain Show forest plot | 2 | 268 | Mean Difference (IV, Random, 95% CI) | 1.50 [‐1.84, 4.84] |
| 5 Knee pain (KSS pain) Show forest plot | 4 | 1004 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐1.40, 1.43] |
| 6 WOMAC total Show forest plot | 4 | 531 | Mean Difference (IV, Random, 95% CI) | 0.78 [‐1.51, 3.07] |
| 7 Knee Society Clinical score Show forest plot | 11 | 1637 | Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.93, 0.77] |
| 8 Knee Society Function Score Show forest plot | 9 | 1539 | Mean Difference (IV, Random, 95% CI) | ‐2.32 [‐4.26, ‐0.37] |
| 9 Hospital Special Surgery Score Show forest plot | 6 | 882 | Mean Difference (IV, Random, 95% CI) | ‐0.51 [‐1.55, 0.54] |
| 10 Knee Society Score overall Show forest plot | 2 | 213 | Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐10.80, 10.03] |
| 11 SF‐12 mental Show forest plot | 2 | 350 | Mean Difference (IV, Random, 95% CI) | 0.41 [‐5.08, 5.89] |
| 12 Radiological: Radiolucent lines Show forest plot | 5 | 754 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.68, 1.07] |
| 13 Radiological: Femorotibial angle Show forest plot | 7 | 1170 | Mean Difference (IV, Random, 95% CI) | 0.36 [‐0.08, 0.79] |
| 14 Radiological: Rollback (in mm) Show forest plot | 2 | 110 | Mean Difference (IV, Random, 95% CI) | 2.78 [‐9.57, 15.13] |
| 15 Radiological: Tibial slope Show forest plot | 2 | 98 | Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐1.21, 0.48] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Range of motion Show forest plot | 4 | 372 | Mean Difference (IV, Random, 95% CI) | ‐2.70 [‐8.71, 3.32] |
| 2 Improvement of range of motion Show forest plot | 2 | 161 | Mean Difference (IV, Random, 95% CI) | 1.92 [‐6.25, 10.08] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Range of motion Show forest plot | 8 | 1193 | Mean Difference (IV, Random, 95% CI) | ‐3.43 [‐6.32, ‐0.54] |
| 2 Flexion angle Show forest plot | 7 | 605 | Mean Difference (IV, Random, 95% CI) | ‐2.07 [‐4.17, 0.04] |
| 3 Extension angle Show forest plot | 6 | 438 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.66, 0.73] |
| 4 VAS pain Show forest plot | 2 | 268 | Mean Difference (IV, Random, 95% CI) | 1.50 [‐1.84, 4.84] |
| 5 Knee pain (KSS pain) Show forest plot | 3 | 750 | Mean Difference (IV, Random, 95% CI) | 0.60 [‐0.39, 1.60] |
| 6 WOMAC total Show forest plot | 3 | 395 | Mean Difference (IV, Random, 95% CI) | 1.59 [‐1.32, 4.50] |
| 7 Knee Society Clinical score Show forest plot | 8 | 1110 | Mean Difference (IV, Random, 95% CI) | 0.16 [‐1.11, 1.43] |
| 8 Knee Society Functional score Show forest plot | 6 | 1012 | Mean Difference (IV, Random, 95% CI) | ‐1.42 [‐4.66, 1.82] |
| 9 Hospital Special Surgery score Show forest plot | 3 | 635 | Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐2.11, 1.01] |
| 10 Knee Society total score Show forest plot | 2 | 193 | Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐11.23, 10.47] |
| 11 SF‐12 mental Show forest plot | 2 | 300 | Mean Difference (IV, Random, 95% CI) | 0.39 [‐5.10, 5.87] |
| 12 Radiological: Radiolucent lines Show forest plot | 4 | 500 | Odds Ratio (M‐H, Random, 95% CI) | 0.80 [0.47, 1.35] |
| 13 Radiological: Femorotibial angle Show forest plot | 4 | 693 | Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.29, 0.47] |
| 14 Radiological: Rollback Show forest plot | 2 | 110 | Mean Difference (IV, Random, 95% CI) | 2.78 [‐9.57, 15.13] |
| 15 Radiological: Tibial slope Show forest plot | 2 | 98 | Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐1.21, 0.48] |

