Colecistectomía de incisión pequeña versus colecistectomía abierta para pacientes con colecistolitiasis sintomática
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias adicionales
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Single‐centre randomised trial. Generation of allocation: unclear. Intention‐to‐treat: not mentioned. | |
| Participants | Elective cholecystectomy for symptomatic cholelithiasis. In‐ and exclusion criteria: not mentioned. Comparability groups: well matched. | |
| Interventions | SIC versus OC. Minicholecystectomy: initial 5 cm (no preoperative ultrasound location), extended in stages each 1 cm long. Retrograde (fundus down) technique was performed. Open cholecystectomy: technique was left to the individual surgeon. Length of incision: offer comfortable exposure, however, not too generous. Antibiotic prophylaxis: yes. Intra‐operative cholangiography: selectively carried out according to clinical and laboratory indications. | |
| Outcomes | Primary and secondary outcome: not mentioned. Outcomes: difficulty of the procedure, operative time, degree of pain, total amount of analgesia, hospital stay, patient satisfaction, physical activity limitations. Duration of follow‐up: 2 weeks. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? | High risk | |
| Free of selective reporting? | High risk | |
| Free of other bias? | High risk | short follow‐up of 2 weeks |
| Methods | Single‐centre trial. Generation of allocation: adequate, by cards. (aleatoriamente = randomised). Intention‐to‐treat: not mentioned. | |
| Participants | Patients admitted for cholecystectomy. In‐ and exclusion criteria: not very well described. Comparability groups: well matched. | |
| Interventions | SIC versus OC. Both procedures not further specified. Antibiotic prophylaxis: not mentioned. Intra‐operative cholangiography: routinely performed in both groups. | |
| Outcomes | Primary and secondary outcome: not described. Outcome measures: clinical results. Duration of follow‐up: hospital stay. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? | High risk | |
| Free of selective reporting? | High risk | |
| Methods | Single‐centre trial. Generation of allocation: unclear. Patients randomly and prospectively divided into three groups. Intention‐to‐treat: not mentioned. | |
| Participants | Chronic calculous cholecystitis admitted for elective cholecystectomy. In‐ and exclusion criteria: not described. Comparability groups: well matched. | |
| Interventions | LC versus SIC versus OC. LC: four‐trocar technique, carbon dioxide insufflated. SIC: right upper quadrant transverse incision of 5 to 8 cm. OC: right upper quadrant subcostal incision of 15 to 20 cm. Antibiotic prophylaxis: not mentioned. Intra‐operative cholangiography: not mentioned. | |
| Outcomes | Primary and secondary outcome: not defined. Outcome measures: comparison of reduction in pulmonary function. Duration of follow‐up: not mentioned. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? | High risk | |
| Free of selective reporting? | High risk | |
| Free of other bias? | High risk | unclear duration of follow‐up |
| Methods | Two‐centre trial. Generation of allocation: unclear. Intention‐to‐treat: not mentioned. | |
| Participants | Patients having cholecystectomy for symptomatic gallstones. In‐ and exclusion criteria: well described. Comparability groups: well matched. | |
| Interventions | SIC versus OC. SIC: through 6 cm incision, rectus muscle divided. OC: not further described. Antibiotic prophylaxis: not mentioned. Routine operative cholangiography in all patients. | |
| Outcomes | Primary and secondary outcome: not specified. Outcome measures: pulmonary, function tests, analgesia requirements, hospital stay. Duration of follow‐up: hospital stay. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? | High risk | |
| Free of selective reporting? | High risk | |
| Free of other bias? | High risk | short follow‐up (hospital stay) |
| Methods | Randomised clinical single‐centre trial. Generation of allocation: unclear. Intention‐to‐treat: not mentioned. | |
| Participants | Patients for elective cholecystectomy. In‐ and exclusion criteria: not very well described. Comparability groups: well matched. | |
| Interventions | SIC versus OC. SIC: 6 cm subcostal transverse incision with diathermy transsection of the right rectus abdominis muscle. OC: a 13 cm subcostal incision with additional partial extension into the muscle spaces of the right lateral epigastric region. Antibiotic prophylaxis: not mentioned. Intra‐operative cholangiography: not mentioned. | |
| Outcomes | Primary and secondary outcome: not mentioned. Outcome measures: operating times, level of subjective pain, analgesic intake, complications. Duration of follow‐up: not mentioned. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? | High risk | |
| Incomplete outcome data addressed? | Low risk | |
| Free of selective reporting? | High risk | |
| Free of other bias? | High risk | unclear duration of follow‐up |
| Methods | Single‐centre randomised trial, operations performed by consultants and senior residents. Generation of allocation: unclear. Intention‐to‐treat: not mentioned. | |
| Participants | Patients undergoing elective cholecystectomy. In‐ and exclusion criteria: not very well described. Comparability groups: not very well described. | |
| Interventions | SIC versus OC. SIC: very well described, a 5 cm transverse incision in the right upper quadrant. OC: vertical midline incision. Antibiotic prophylaxis: not mentioned. Intra‐operative cholangiography: no, selective pre‐operative cholangiogram was performed when necessary. | |
| Outcomes | Primary and secondary outcome: not mentioned. Outcome measures: complications, operative time, hospital stay. Duration of follow‐up: 30 days. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? | High risk | |
| Free of selective reporting? | High risk | |
| Methods | Single‐centre trial. Randomised trial: prospective study with patients systematically divided. Generation of allocation: unclear. Intention‐to‐treat: not mentioned. | |
| Participants | Patients with chronic calculus cholecystitis. In‐ and exclusion criteria: not very well described. Comparability groups: well matched. | |
| Interventions | SIC versus OC. SIC: incision of 5 cm to 7 cm length with two well illuminated retractors, dissected either duct first or fundus first. OC: right subcostal incision of 10 cm to 15 cm. Antibiotic prophylaxis: not mentioned. Intra‐operative cholangiography: not mentioned | |
| Outcomes | Primary and secondary outcome: not mentioned. Outcome measures: pulmonary function. Duration of follow‐up: not mentioned (hospital stay). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? | High risk | |
| Free of selective reporting? | High risk | |
| Free of other bias? | Unclear risk | short follow‐up |
LC ‐ laparoscopic cholecystectomy,
SIC ‐ small‐incision cholecystectomy,
OC ‐ open cholecystectomy.
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Prospective study on three different types of small‐incision cholecystectomy, not randomised. | |
| Review on pain after laparoscopy; not a randomised trial. | |
| Comparison of costs of LC between ten surgeons; no comparison of operative procedures. | |
| Randomised clinical trial on conventional LC (two 10 mm and two 5 mm ports) and LC by small instruments (one 10 mm and three 2 mm ports); thus comparison of two types of LC. | |
| Editorial: discussion of other article. | |
| Randomised trial only including patients with acute cholecystitis. | |
| Correspondence with GD Bablekos on 11 October 2004: separating patients in triads with allocation according to registration sequence at the emergency ward: quasi‐randomised study of LC versus OC. | |
| Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. | |
| Comparison of three different time periods; not a randomised trial. | |
| Debate, consideration. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Economic evaluation. | |
| Review on indications and methods of cholecystectomy in treatment of gallstones. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Study on the frequency of incisional hernias after different types of conventional cholecystectomy; not a randomised trial. | |
| Quasi‐randomised trial: "... patients were randomised by alternate number to LC or OC ...". | |
| Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Prospective, not randomised study: " ... equipment was only made available on an intermittent basis ...". | |
| Prospective study on outpatient LC, comparing with historical (inpatient) LC; not a randomised trial. | |
| Study on costs and patient satisfaction before and after re‐engineering of a surgical service in LC patients and elective herniorrhaphy; no comparison of different types of cholecystectomy. | |
| One‐arm prospective study on costs; not a randomised trial (not two arms). | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Letter. | |
| Not a randomised trial; prospective study of small‐incision cholecystectomy. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Prospective study, not randomised: "... patients were not randomised as it was felt that it was unethical to do so ...". | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Not randomised; prospective study. | |
| Stress response in LC and OC patients, not randomised: "... 22 patients underwent OC and the other 24 had LC according to the availability of laparoscopic equipment ...". | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Not randomised; randomisation was not possible as most patients opted for the laparoscopic technique. | |
| Not a randomised trial: patients who were operated by LC or OC were analysed. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| No correct randomisation between two operative techniques: "... patients were randomly assigned to individual staff surgeons, as is our customary practice ...". | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Prospective study with control group, not randomised: "... because of the ethical problems associated with randomisation of LC and OC, we decided to conduct a prospective trial without randomisation, but with a control group ...". | |
| Retrospective study on cost‐effectiveness between extracorporeal shock‐wave lithotripsy, conventional cholecystectomy, and laparoscopic cholecystectomy. | |
| Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. | |
| Not randomised: the authors felt that randomisation was not possible on ethical grounds. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Randomised trial comparing performing cholecystectomy with or without a routine cholangiography. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Considerations on laparoscopic cholecystectomy, not a randomised trial. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Considerations on laparoscopic digestive surgery, not a randomised trial. | |
| Editorial. | |
| Not a randomised trial. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Considerations on laparoscopic surgery. | |
| Personal view: consideration on efficacy, safety and training; not a randomised trial. | |
| Letter. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Prospective study in patients having LC and OC, but no randomisation: "... twelve patients who had OC were recruited and served as the control group ...". | |
| Consideration of gallstone treatment modalities. | |
| Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. | |
| Randomised trial between LC and OC on acute cholecystitis. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Prospective study on patients who underwent LC: patients with uncomplicated LC were compared to patients who had conversion from LC to OC. | |
| Not a randomised trial: "the groups were not randomised". | |
| Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. | |
| Prospective study, but not randomised: "... patients were randomly allocated to either LC or OC, based on the availability of laparoscopic equipment ...". | |
| Survey in Scotland on cholecystectomy rate; not a randomised trial. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Cohort of patients treated by one technique; not a randomised trial. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. | |
| Only pilot phase of trial; in pilot phase no randomisation: SIC was performed when LC instruments were not available. | |
| Systematic review on different types of minimal access surgery; not a randomised trial. | |
| Patients with acute cholecystitis only. | |
| Comparison of two different types of anaesthesia in cholecystectomy. | |
| Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. | |
| Comparison of historical cohorts. | |
| Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. | |
| Letter, not a randomised trial. | |
| An unselected group of patients undergoing LC in one hospital was compared with a group undergoing OC in another hospital. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| No randomisation. | |
| Randomised controlled trial on two types of laparoscopic cholecystectomy (mini‐port LC (2 mm) versus conventional LC). | |
| Retrospective study on LC versus OC in patients with cardiac valve replacement. | |
| Review of literature from 1970 to 1992 on mini‐lap cholecystectomy: only articles in English were included and data on conventional and laparoscopic cholecystectomy were obtained from large series reported in literature. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Prospective not randomised study: "... allocation to either laparoscopic or conventional cholecystectomy depended on the availability of a laparoscopic set ...". | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Patients underwent conventional subcostal cholecystectomy whenever the instrumentation for laparoscopic surgery was not available; the laparoscopic group had on alternating basis general anaesthesia combined with epidural analgesia or general anaesthesia alone; not randomised. | |
| Study evaluating laparoscopic and small‐incision cholecystectomy. | |
| Not a randomised trial; comment on other article. | |
| Not randomised: "patients were divided into two groups". | |
| Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| No correct randomisation of surgical techniques: ".. patients were randomly assigned to one of four general surgical services; two of these used only the open cholecystectomy technique, and the other two used the laparoscopic approach ..". | |
| Not randomised; ".. procedure was determined by the attending physician ..". | |
| Randomised clinical trial on two types of conventional cholecystectomy (with nasogastric tube, iv infusion and subhepatic drain versus no tube, no infusion and no drain). | |
| Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. | |
| Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. | |
| Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. | |
| Trial on LC and OC patients, but no randomisation as the authors found that laparoscopic cholecystectomy was the method of first choice. | |
| Review on gallstones; not a randomised trial. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Prospective comparison between IL‐6 levels in LC and OC patients, but not randomised: " ... patients who underwent cholecystectomy, 12 each for OC and LC, were chosen as subjects in this study ...". | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Prospective study on LC and OC pulmonary function, but not randomised: "... selection for OC or LC depended upon surgeon ...". | |
| Prospective study in cirrhotic patients on laparoscopic versus open cholecystectomy; not randomised ( "... all cirrhotic patients were offered LC ..." ). | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. | |
| Randomised trial evaluating laparoscopic and open cholecystectomy. |
LC: laparoscopic cholecystectomy;
OC: open cholecystectomy.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intra‐operative complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| Analysis 1.1  Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 1 Intra‐operative complications. | ||||
| 1.1 High‐quality trials | 1 | 50 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.07, 0.07] |
| 1.2 Low‐quality trials | 6 | 521 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 2 Minor complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.03, 0.05] |
| Analysis 1.2  Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 2 Minor complications. | ||||
| 2.1 High‐quality trials | 1 | 50 | Risk Difference (M‐H, Random, 95% CI) | ‐0.04 [‐0.21, 0.13] |
| 2.2 Low‐quality trials | 6 | 521 | Risk Difference (M‐H, Random, 95% CI) | 0.02 [‐0.04, 0.07] |
| 3 Severe complications (without bile duct injuries) Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| Analysis 1.3  Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 3 Severe complications (without bile duct injuries). | ||||
| 3.1 High‐quality trials | 1 | 50 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.04 [‐0.14, 0.06] |
| 3.2 Low‐quality trials | 6 | 521 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| 4 Bile duct injuries Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| Analysis 1.4  Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 4 Bile duct injuries. | ||||
| 4.1 High‐quality trials | 1 | 50 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.07, 0.07] |
| 4.2 Low‐quality trials | 6 | 521 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 5 Total complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.00 [‐0.06, 0.07] |
| Analysis 1.5  Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 5 Total complications. | ||||
| 5.1 High‐quality trials | 1 | 50 | Risk Difference (M‐H, Random, 95% CI) | ‐0.08 [‐0.26, 0.10] |
| 5.2 Low‐quality trials | 6 | 521 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.06, 0.08] |
| 6 Operative time (minutes) Show forest plot | 3 | 210 | Mean Difference (IV, Fixed, 95% CI) | 1.94 [‐1.37, 5.25] |
| Analysis 1.6  Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 6 Operative time (minutes). | ||||
| 6.1 High‐quality trials | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Low‐quality trials | 3 | 210 | Mean Difference (IV, Fixed, 95% CI) | 1.94 [‐1.37, 5.25] |
| 7 Hospital stay (days) Show forest plot | 2 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.78 [‐4.94, ‐0.62] |
| Analysis 1.7  Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 7 Hospital stay (days). | ||||
| 7.1 High‐quality trials | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Low‐quality trials | 2 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.78 [‐4.94, ‐0.62] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intra‐operative complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| Analysis 2.1  Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 1 Intra‐operative complications. | ||||
| 1.1 High‐quality trials | 2 | 160 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.03, 0.03] |
| 1.2 Low‐quality trials | 5 | 411 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 2 Minor complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.03, 0.05] |
| Analysis 2.2  Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 2 Minor complications. | ||||
| 2.1 High‐quality trials | 2 | 160 | Risk Difference (M‐H, Random, 95% CI) | 0.11 [0.02, 0.21] |
| 2.2 Low‐quality trials | 5 | 411 | Risk Difference (M‐H, Random, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| 3 Severe complications (without bile duct injuries) Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| Analysis 2.3  Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 3 Severe complications (without bile duct injuries). | ||||
| 3.1 High‐quality trials | 2 | 160 | Risk Difference (M‐H, Fixed, 95% CI) | 0.02 [‐0.03, 0.08] |
| 3.2 Low‐quality trials | 5 | 411 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.02 [‐0.06, 0.01] |
| 4 Bile duct injuries Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| Analysis 2.4  Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 4 Bile duct injuries. | ||||
| 4.1 High‐quality trials | 2 | 160 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.03, 0.03] |
| 4.2 Low‐quality trials | 5 | 411 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 5 Total complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.00 [‐0.06, 0.07] |
| Analysis 2.5  Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 5 Total complications. | ||||
| 5.1 High‐quality trials | 2 | 160 | Risk Difference (M‐H, Random, 95% CI) | 0.14 [0.04, 0.24] |
| 5.2 Low‐quality trials | 5 | 411 | Risk Difference (M‐H, Random, 95% CI) | ‐0.03 [‐0.10, 0.03] |
| 6 Operative time (minutes) Show forest plot | 3 | 210 | Mean Difference (IV, Fixed, 95% CI) | 1.94 [‐1.37, 5.25] |
| Analysis 2.6  Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 6 Operative time (minutes). | ||||
| 6.1 High‐quality trials | 2 | 160 | Mean Difference (IV, Fixed, 95% CI) | 2.81 [‐1.78, 7.41] |
| 6.2 Low‐quality trials | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | 1.0 [‐3.77, 5.77] |
| 7 Hospital stay (days) Show forest plot | 2 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.78 [‐4.94, ‐0.62] |
| Analysis 2.7  Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 7 Hospital stay (days). | ||||
| 7.1 High‐quality trials | 1 | 130 | Mean Difference (IV, Random, 95% CI) | ‐3.9 [‐4.57, ‐3.23] |
| 7.2 Low‐quality trials | 1 | 50 | Mean Difference (IV, Random, 95% CI) | ‐1.70 [‐2.05, ‐1.35] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intra‐operative complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| Analysis 3.1  Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 1 Intra‐operative complications. | ||||
| 1.1 High‐quality trials | 0 | 0 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Low‐quality trials | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 2 Minor complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.03, 0.05] |
| Analysis 3.2  Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 2 Minor complications. | ||||
| 2.1 High‐quality trials | 0 | 0 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Low‐quality trials | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.03, 0.05] |
| 3 Severe complications (without bile duct injuries) Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| Analysis 3.3  Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 3 Severe complications (without bile duct injuries). | ||||
| 3.1 High‐quality trials | 0 | 0 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Low‐quality trials | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| 4 Bile duct injuries Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| Analysis 3.4  Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 4 Bile duct injuries. | ||||
| 4.1 High‐quality trials | 0 | 0 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Low‐quality trials | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 5 Total complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.00 [‐0.06, 0.07] |
| Analysis 3.5  Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 5 Total complications. | ||||
| 5.1 High‐quality trials | 0 | 0 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Low‐quality trials | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.00 [‐0.06, 0.07] |
| 6 Operative time (minutes) Show forest plot | 3 | 210 | Mean Difference (IV, Fixed, 95% CI) | 1.94 [‐1.37, 5.25] |
| Analysis 3.6  Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 6 Operative time (minutes). | ||||
| 6.1 High‐quality trials | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Low‐quality trials | 3 | 210 | Mean Difference (IV, Fixed, 95% CI) | 1.94 [‐1.37, 5.25] |
| 7 Hospital stay (days) Show forest plot | 2 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.78 [‐4.94, ‐0.62] |
| Analysis 3.7  Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 7 Hospital stay (days). | ||||
| 7.1 High‐quality trials | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Low‐quality trials | 2 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.78 [‐4.94, ‐0.62] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intra‐operative complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| Analysis 4.1  Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 1 Intra‐operative complications. | ||||
| 1.1 High‐quality trials | 1 | 130 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.03, 0.03] |
| 1.2 Low‐quality trials | 6 | 441 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 2 Minor complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.03, 0.05] |
| Analysis 4.2  Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 2 Minor complications. | ||||
| 2.1 High‐quality trials | 1 | 130 | Risk Difference (M‐H, Random, 95% CI) | 0.14 [0.03, 0.25] |
| 2.2 Low‐quality trials | 6 | 441 | Risk Difference (M‐H, Random, 95% CI) | ‐0.01 [‐0.04, 0.03] |
| 3 Severe complications (without bile duct injuries) Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| Analysis 4.3  Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 3 Severe complications (without bile duct injuries). | ||||
| 3.1 High‐quality trials | 1 | 130 | Risk Difference (M‐H, Fixed, 95% CI) | 0.03 [‐0.02, 0.08] |
| 3.2 Low‐quality trials | 6 | 441 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.02 [‐0.05, 0.01] |
| 4 Bile duct injuries Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| Analysis 4.4  Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 4 Bile duct injuries. | ||||
| 4.1 High‐quality trials | 1 | 130 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.03, 0.03] |
| 4.2 Low‐quality trials | 6 | 441 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 5 Total complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.00 [‐0.06, 0.07] |
| Analysis 4.5  Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 5 Total complications. | ||||
| 5.1 High‐quality trials | 1 | 130 | Risk Difference (M‐H, Random, 95% CI) | 0.17 [0.05, 0.29] |
| 5.2 Low‐quality trials | 6 | 441 | Risk Difference (M‐H, Random, 95% CI) | ‐0.02 [‐0.07, 0.03] |
| 6 Operative time (minutes) Show forest plot | 3 | 210 | Mean Difference (IV, Fixed, 95% CI) | 1.94 [‐1.37, 5.25] |
| Analysis 4.6  Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 6 Operative time (minutes). | ||||
| 6.1 High‐quality trials | 1 | 130 | Mean Difference (IV, Fixed, 95% CI) | 4.0 [‐0.86, 8.86] |
| 6.2 Low‐quality trials | 2 | 80 | Mean Difference (IV, Fixed, 95% CI) | 0.16 [‐4.35, 4.68] |
| 7 Hospital stay (days) Show forest plot | 2 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.78 [‐4.94, ‐0.62] |
| Analysis 4.7  Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 7 Hospital stay (days). | ||||
| 7.1 High‐quality trials | 1 | 130 | Mean Difference (IV, Random, 95% CI) | ‐3.9 [‐4.57, ‐3.23] |
| 7.2 Low‐quality trials | 1 | 50 | Mean Difference (IV, Random, 95% CI) | ‐1.70 [‐2.05, ‐1.35] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Sensitivity analysis 1: Operative time (minutes) Show forest plot | 7 | 571 | Mean Difference (IV, Random, 95% CI) | ‐2.98 [‐7.86, 1.90] |
| Analysis 5.1  Comparison 5 SIC versus OC ‐ sensitivity analysis imputing medians and standard deviations for missing data, Outcome 1 Sensitivity analysis 1: Operative time (minutes). | ||||
| 2 Sensitivity analysis 2: Hospital stay (days) Show forest plot | 7 | 571 | Mean Difference (IV, Random, 95% CI) | ‐1.97 [‐2.56, ‐1.39] |
| Analysis 5.2  Comparison 5 SIC versus OC ‐ sensitivity analysis imputing medians and standard deviations for missing data, Outcome 2 Sensitivity analysis 2: Hospital stay (days). | ||||
| 3 Sensitivity analysis 3: Omitting outlier Schmitz in total complications Show forest plot | 6 | 441 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.04 [‐0.09, 0.01] |
| Analysis 5.3  Comparison 5 SIC versus OC ‐ sensitivity analysis imputing medians and standard deviations for missing data, Outcome 3 Sensitivity analysis 3: Omitting outlier Schmitz in total complications. | ||||
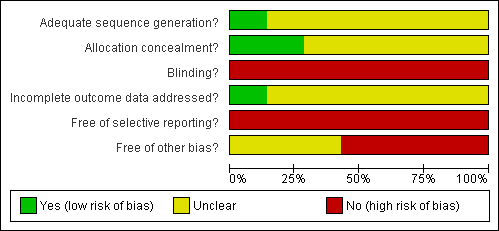
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
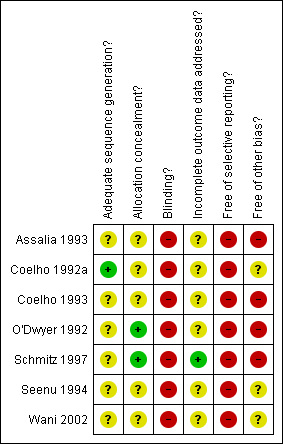
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.

Funnel plot on small‐incision versus open cholecystectomy regarding concealment of allocation considering total complications, including 95% confidence interval lines. No arguments for bias.
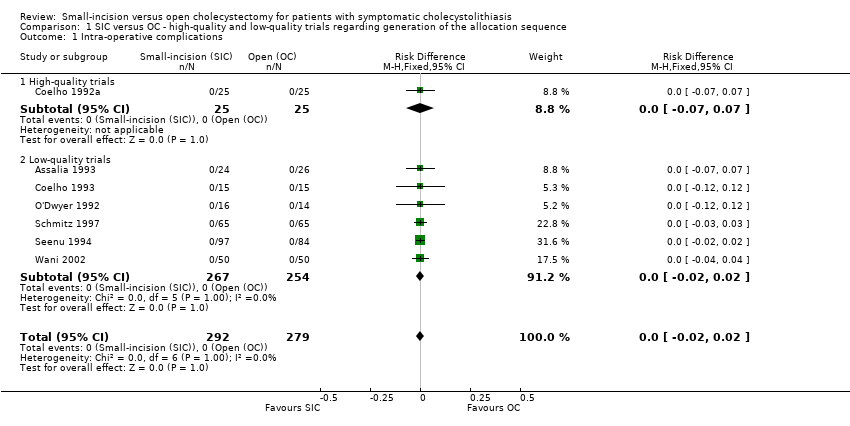
Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 1 Intra‐operative complications.
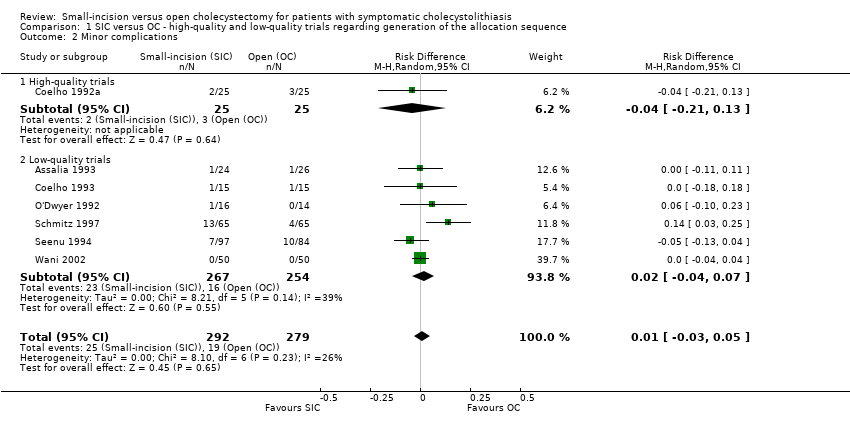
Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 2 Minor complications.

Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 3 Severe complications (without bile duct injuries).

Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 4 Bile duct injuries.

Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 5 Total complications.

Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 6 Operative time (minutes).
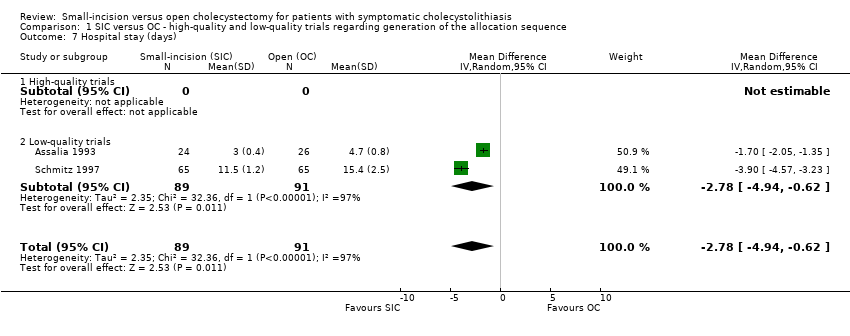
Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 7 Hospital stay (days).

Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 1 Intra‐operative complications.
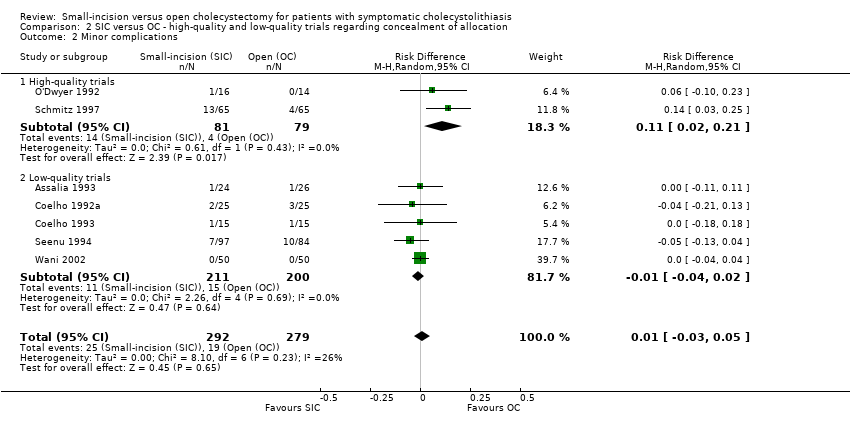
Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 2 Minor complications.

Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 3 Severe complications (without bile duct injuries).

Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 4 Bile duct injuries.
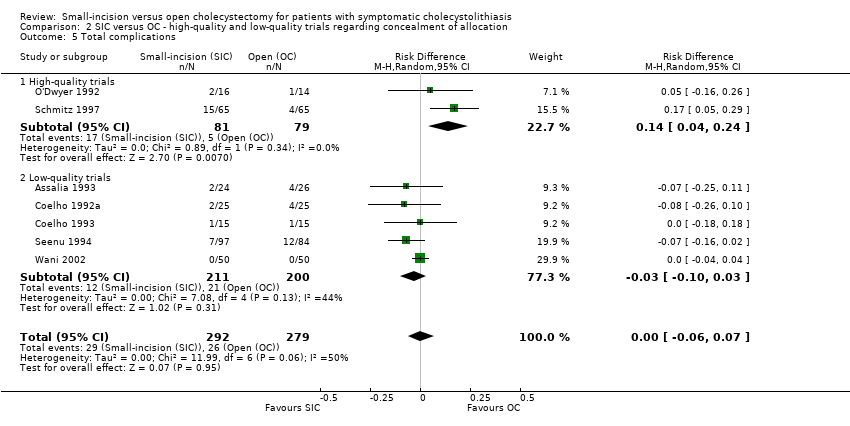
Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 5 Total complications.
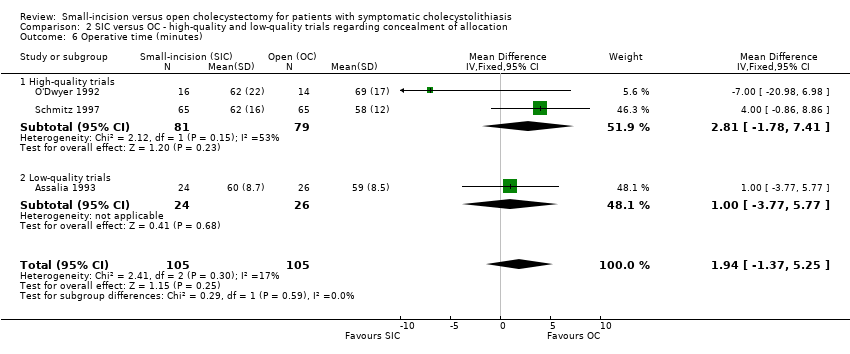
Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 6 Operative time (minutes).
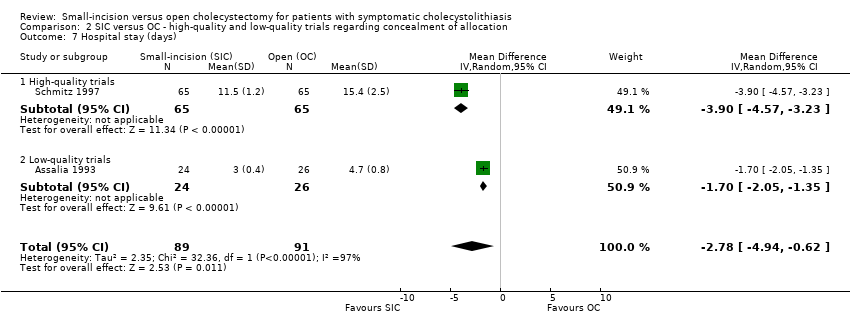
Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 7 Hospital stay (days).

Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 1 Intra‐operative complications.

Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 2 Minor complications.
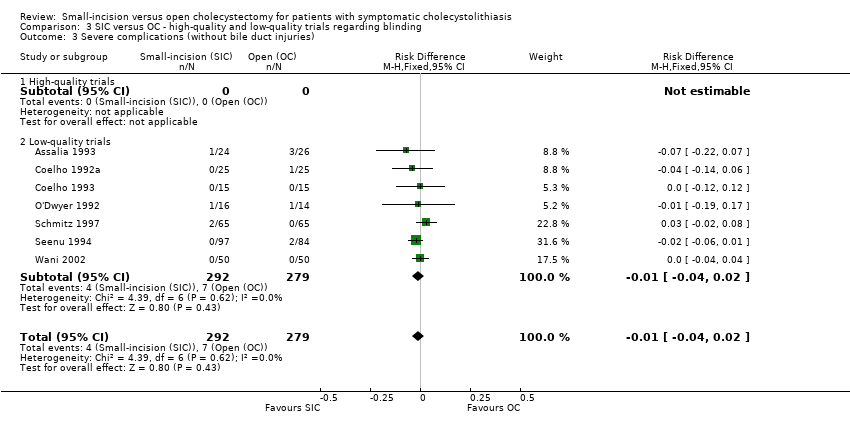
Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 3 Severe complications (without bile duct injuries).

Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 4 Bile duct injuries.

Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 5 Total complications.

Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 6 Operative time (minutes).
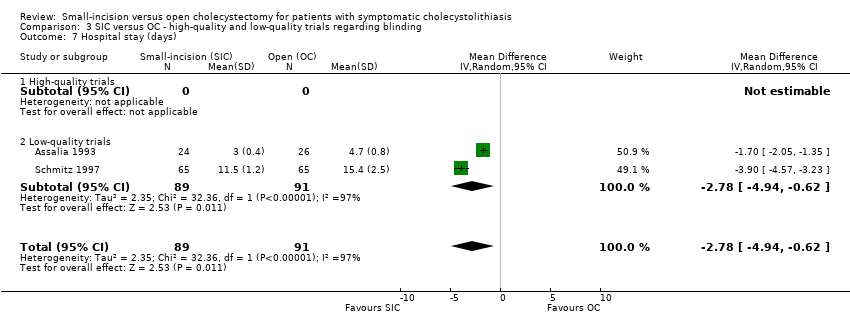
Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 7 Hospital stay (days).
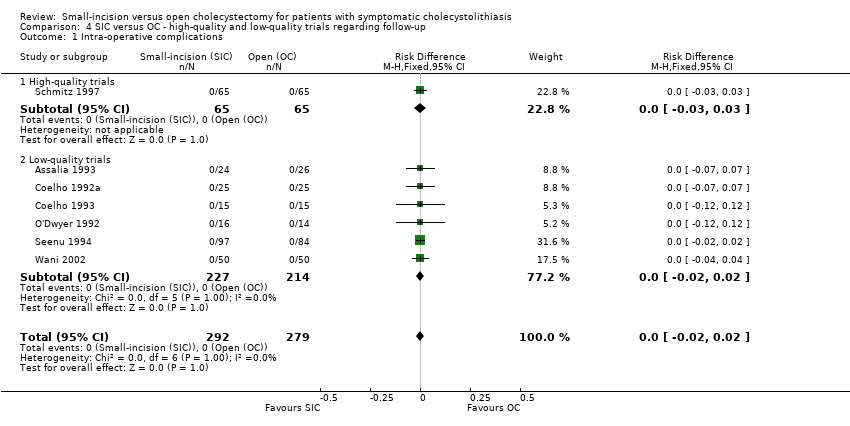
Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 1 Intra‐operative complications.

Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 2 Minor complications.

Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 3 Severe complications (without bile duct injuries).
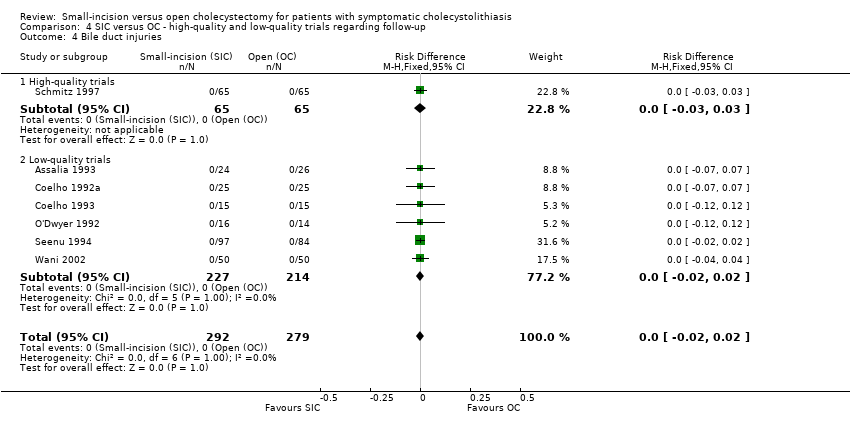
Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 4 Bile duct injuries.

Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 5 Total complications.
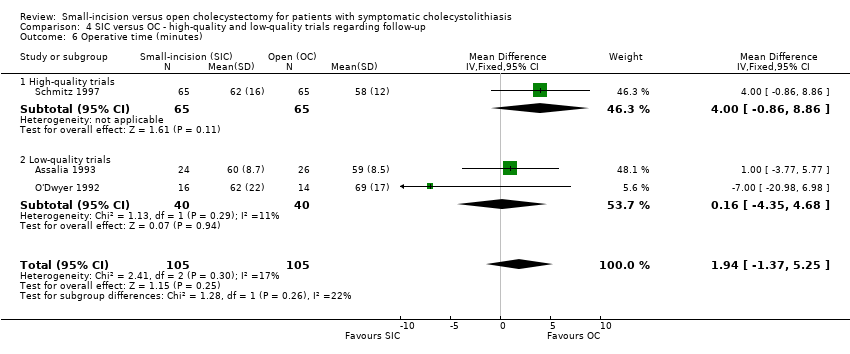
Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 6 Operative time (minutes).
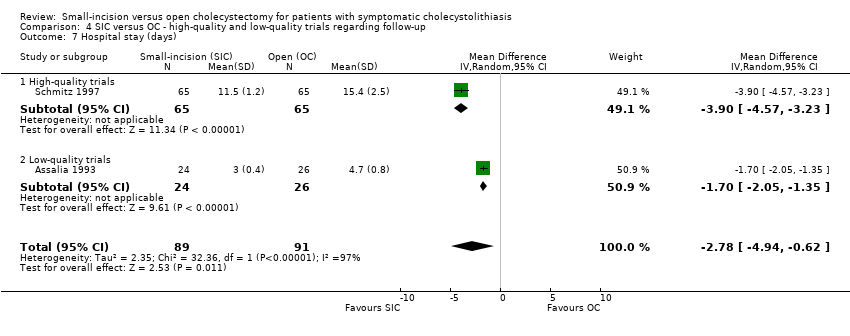
Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 7 Hospital stay (days).

Comparison 5 SIC versus OC ‐ sensitivity analysis imputing medians and standard deviations for missing data, Outcome 1 Sensitivity analysis 1: Operative time (minutes).

Comparison 5 SIC versus OC ‐ sensitivity analysis imputing medians and standard deviations for missing data, Outcome 2 Sensitivity analysis 2: Hospital stay (days).
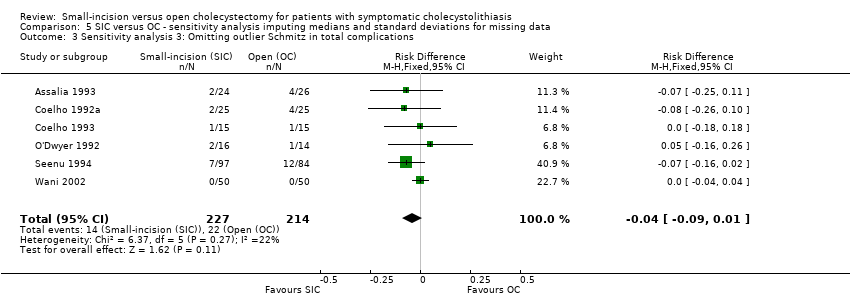
Comparison 5 SIC versus OC ‐ sensitivity analysis imputing medians and standard deviations for missing data, Outcome 3 Sensitivity analysis 3: Omitting outlier Schmitz in total complications.
| Trial | Randomised | Excluded | Included SIC | Included OC | Cholangiography | Antibiotics | Surgical expertise |
| Assalia 1993 | 50 | 0 | 24 | 26 | N | Y | S |
| Coelho 1992a | 50 | 0 | 25 | 25 | Y | U | U |
| Coelho 1993 | 45* | 0 | 15 | 15 | U | U | U |
| O'Dwyer 1992a | 30 | 0 | 16 | 14 | Y | U | R |
| Schmitz 1997a | 130 | 0 | 65 | 65 | U | U | U |
| Seenu 1994 | 181 | 0 | 97 | 84 | U | U | R |
| Wani 2002 | 100 | 0 | 50 | 50 | U | U | U |
| Total | 586 | 0 | 292 | 279 | |||
| * three‐arm trial, patients in the LC group not listed in this table. | N = no | Y = yes | U = unknown | S = one surgeon | R = also registrars |
| Trial | N | Age | Age | Sex (m/f) | Sex (m/f) | BMI | BMI | ASA (I‐II‐III‐IV) | ASA (I‐II‐III‐IV) |
| SIC vs OC | randomised | SIC | OC | SIC | OC | SIC | OC | SIC | OC |
| Assalia 1993 | 24 / 26 | 60.3 (12.1) | 59.2 (13.4) | 5 / 19 | 7 / 19 | ‐ | ‐ | ‐ | ‐ |
| Coelho 1992a | 25 / 25 | 46 ( ‐ ) | 45 ( ‐ ) | 2 / 23 | 4 / 21 | ‐ | ‐ | ‐ | ‐ |
| Coelho 1993 | 15 / 15 | 42.5 (25‐66) | 45.4 (18‐73) | 2 / 13 | 3 / 12 | ‐ | ‐ | ‐ | ‐ |
| O'Dwyer 1992a | 16 / 14 | 46 (27‐74) | 51 (38‐73) | 3 / 13 | 4 / 10 | ‐ | ‐ | 16 ‐ 0 ‐ 0 ‐ 0 | 14 ‐ 0 ‐ 0 ‐ 0 |
| Schmitz 1997a | 65 / 65 | 52.6 (14.6) | 54.1 (12.2) | 20 / 45 | 23 / 42 | ‐ | ‐ | ‐ | ‐ |
| Seenu 1994 | 97 / 84 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Wani 2002 | 50 / 50 | 34.8 (5.6) | 37.4 (6.2) | 5 / 45 | 5 / 45 | 21.5 (1.9) | 21.6 (1.8) | ‐ | ‐ |
| mean (standard deviation / range) |
| Complications | SIC | OC |
| INTRA‐OPERATIVE | (0) | (0) |
| POSTOPERATIVE ‐ MINOR | (25 / 8.6%) | (19 / 6.8%) |
| wound hematoma | 12 | 4 |
| wound infection | 12 | 15 |
| urinary retention | 1 | 0 |
| POSTOPERATIVE ‐ SEVERE | (4 / 1.4%) | (7 / 2.5%) |
| stone left in cystic duct (re‐operation) | 1 | 0 |
| pneumonia | 1 | 5 |
| atelectasis | 1 | 0 |
| cardiovascular | 1 | 0 |
| upper GI bleeding (endoscopy / conservative) | 0 | 2 |
| BILE DUCT INJURY | (0) | (0) |
| TOTAL COMPLICATIONS | 29 (9.9%) | 26 (9.3%) |
| RE‐OPERATIONS (all complications) | 2 (0.7%) | 0 |
| TOTAL NUMBER OF PATIENTS INCLUDED (all trials) | 292 | 279 |
| Trial | Generation of alloc | Concealment of alloc | Blinding | Follow‐up |
| Assalia 1993 | U | U | N | U |
| Coelho 1992a | A | U | N | U |
| Coelho 1993 | U | U | N | U |
| O'Dwyer 1992a | U | A | N | U |
| Schmitz 1997a | U | A | N | A |
| Seenu 1994 | U | U | N | U |
| Wani 2002 | U | U | N | U |
| A: Adequate | U: Unclear | I: Inadequate | N: Not performed |
| Outcome | RD/WMD | HQ/LQ/AT | Fixed | Random | Discrepancy | Emphasize | HQ‐LQ difference | Significant |
| Minor complications | RD | HQ | 0.12 (0.03, 0.22) * | 0.11 (0.02, 0.21) * | no | |||
| LQ | ‐0.03 (‐0.07, 0.02) | ‐0.01 (‐0.04, 0.02) | no | |||||
| AT | 0.02 (‐0.03, 0.06) | 0.01 (‐0.03, 0.05) | no | random | yes | yes/no | ||
| Total complications | RD | HQ | 0.15 (0.04, 0.25) * | 0.14 (0.04, 0.24) * | no | |||
| LQ | ‐0.05 (‐0.10, 0.00) | ‐0.03 (‐0.10, 0.03) | no | |||||
| AT | 0.01 (‐0.04, 0.05) | 0.00 (‐0.06, 0.07) | no | random | yes | yes/no | ||
| Hospital stay | WMD | HQ | ‐3.90 (‐4.57, ‐3.23) * | ‐3.90 (‐4.57, ‐3.23) * | no | |||
| LQ | ‐1.70 (‐2.05, ‐1.35) * | ‐1.70 (‐2.05, ‐1.35) * | no | |||||
| AT | ‐2.16 (‐2.47, ‐1.85) * | ‐2.78 (‐4.94, ‐0.62) * | no | random | no | yes | ||
| * significant result | HQ: high‐quality trials | LQ: low‐quality trials | AT: all trials | RD: risk difference | WMD: weighted mean difference | random: random‐effects model |
| Trial | Type of data | SIC ‐ mean/median | SIC ‐ SD/range | OC ‐ mean/median | OC ‐ SD/range | Skewness SIC | Skewness OC |
| Assalia 1993 | A ‐ SD | 60 | 8.7 | 59 | 8.5 | 6.90 | 6.94 |
| Coelho 1992a | A ‐ | 86 | ‐ | 99 | ‐ | ‐ | ‐ |
| Coelho 1993 | A ‐ range | 74 | 40 ‐ 125 | 86 | 40 ‐ 140 | ‐ | ‐ |
| O'Dwyer 1992a | A ‐ SD | 62 | 22 | 69 | 17 | 2.82 | 4.06 |
| Schmitz 1997a | A ‐ SD | 62 | 16 | 58 | 12 | 3.88 | 4.83 |
| Seenu 1994 | A ‐ range | 60 | 30 ‐ 100 | 65 | 20 ‐ 90 | ‐ | ‐ |
| Wani 2002 | A ‐ range | 74 | 40 ‐ 125 | 70 | 50 ‐ 125 | ‐ | ‐ |
| A: Average / mean | SD: standard deviation |
| Trial | Type of data | SIC ‐ mean/median | SIC ‐ SD/range | OC ‐ mean/median | OC ‐ SD/range | Skewness SIC | Skewness OC |
| Assalia 1993 | A ‐ SD | 3 | 0.4 | 4.7 | 0.8 | 7.5 | 5.88 |
| Coelho 1992a | A ‐ | 1,7 | ‐ | 3,5 | ‐ | ‐ | ‐ |
| Coelho 1993 | A ‐ range | 1 | 1 ‐ 1 | 2 | 2 ‐ 3 | ‐ | ‐ |
| O'Dwyer 1992a | M ‐ range | 3 | 1 ‐ 10 | 5 | 3 ‐ 8 | ‐ | ‐ |
| Schmitz 1997a | A ‐ SD | 11.5 | 1.2 | 15.4 | 2.5 | 9.58 | 6.16 |
| Seenu 1994 | A ‐ range | 2.6 | 1 ‐ 4 | 4 | 3 ‐ 8 | ‐ | ‐ |
| Wani 2002 | A ‐ | 3 | ‐ | 5 | ‐ | ‐ | ‐ |
| A: Average / mean | SD: standard deviation | M: median |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intra‐operative complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 1.1 High‐quality trials | 1 | 50 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.07, 0.07] |
| 1.2 Low‐quality trials | 6 | 521 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 2 Minor complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.03, 0.05] |
| 2.1 High‐quality trials | 1 | 50 | Risk Difference (M‐H, Random, 95% CI) | ‐0.04 [‐0.21, 0.13] |
| 2.2 Low‐quality trials | 6 | 521 | Risk Difference (M‐H, Random, 95% CI) | 0.02 [‐0.04, 0.07] |
| 3 Severe complications (without bile duct injuries) Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| 3.1 High‐quality trials | 1 | 50 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.04 [‐0.14, 0.06] |
| 3.2 Low‐quality trials | 6 | 521 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| 4 Bile duct injuries Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 4.1 High‐quality trials | 1 | 50 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.07, 0.07] |
| 4.2 Low‐quality trials | 6 | 521 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 5 Total complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.00 [‐0.06, 0.07] |
| 5.1 High‐quality trials | 1 | 50 | Risk Difference (M‐H, Random, 95% CI) | ‐0.08 [‐0.26, 0.10] |
| 5.2 Low‐quality trials | 6 | 521 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.06, 0.08] |
| 6 Operative time (minutes) Show forest plot | 3 | 210 | Mean Difference (IV, Fixed, 95% CI) | 1.94 [‐1.37, 5.25] |
| 6.1 High‐quality trials | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Low‐quality trials | 3 | 210 | Mean Difference (IV, Fixed, 95% CI) | 1.94 [‐1.37, 5.25] |
| 7 Hospital stay (days) Show forest plot | 2 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.78 [‐4.94, ‐0.62] |
| 7.1 High‐quality trials | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Low‐quality trials | 2 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.78 [‐4.94, ‐0.62] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intra‐operative complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 1.1 High‐quality trials | 2 | 160 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.03, 0.03] |
| 1.2 Low‐quality trials | 5 | 411 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 2 Minor complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.03, 0.05] |
| 2.1 High‐quality trials | 2 | 160 | Risk Difference (M‐H, Random, 95% CI) | 0.11 [0.02, 0.21] |
| 2.2 Low‐quality trials | 5 | 411 | Risk Difference (M‐H, Random, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| 3 Severe complications (without bile duct injuries) Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| 3.1 High‐quality trials | 2 | 160 | Risk Difference (M‐H, Fixed, 95% CI) | 0.02 [‐0.03, 0.08] |
| 3.2 Low‐quality trials | 5 | 411 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.02 [‐0.06, 0.01] |
| 4 Bile duct injuries Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 4.1 High‐quality trials | 2 | 160 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.03, 0.03] |
| 4.2 Low‐quality trials | 5 | 411 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 5 Total complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.00 [‐0.06, 0.07] |
| 5.1 High‐quality trials | 2 | 160 | Risk Difference (M‐H, Random, 95% CI) | 0.14 [0.04, 0.24] |
| 5.2 Low‐quality trials | 5 | 411 | Risk Difference (M‐H, Random, 95% CI) | ‐0.03 [‐0.10, 0.03] |
| 6 Operative time (minutes) Show forest plot | 3 | 210 | Mean Difference (IV, Fixed, 95% CI) | 1.94 [‐1.37, 5.25] |
| 6.1 High‐quality trials | 2 | 160 | Mean Difference (IV, Fixed, 95% CI) | 2.81 [‐1.78, 7.41] |
| 6.2 Low‐quality trials | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | 1.0 [‐3.77, 5.77] |
| 7 Hospital stay (days) Show forest plot | 2 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.78 [‐4.94, ‐0.62] |
| 7.1 High‐quality trials | 1 | 130 | Mean Difference (IV, Random, 95% CI) | ‐3.9 [‐4.57, ‐3.23] |
| 7.2 Low‐quality trials | 1 | 50 | Mean Difference (IV, Random, 95% CI) | ‐1.70 [‐2.05, ‐1.35] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intra‐operative complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 1.1 High‐quality trials | 0 | 0 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Low‐quality trials | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 2 Minor complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.03, 0.05] |
| 2.1 High‐quality trials | 0 | 0 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Low‐quality trials | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.03, 0.05] |
| 3 Severe complications (without bile duct injuries) Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| 3.1 High‐quality trials | 0 | 0 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Low‐quality trials | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| 4 Bile duct injuries Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 4.1 High‐quality trials | 0 | 0 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Low‐quality trials | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 5 Total complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.00 [‐0.06, 0.07] |
| 5.1 High‐quality trials | 0 | 0 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Low‐quality trials | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.00 [‐0.06, 0.07] |
| 6 Operative time (minutes) Show forest plot | 3 | 210 | Mean Difference (IV, Fixed, 95% CI) | 1.94 [‐1.37, 5.25] |
| 6.1 High‐quality trials | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Low‐quality trials | 3 | 210 | Mean Difference (IV, Fixed, 95% CI) | 1.94 [‐1.37, 5.25] |
| 7 Hospital stay (days) Show forest plot | 2 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.78 [‐4.94, ‐0.62] |
| 7.1 High‐quality trials | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Low‐quality trials | 2 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.78 [‐4.94, ‐0.62] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intra‐operative complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 1.1 High‐quality trials | 1 | 130 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.03, 0.03] |
| 1.2 Low‐quality trials | 6 | 441 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 2 Minor complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.03, 0.05] |
| 2.1 High‐quality trials | 1 | 130 | Risk Difference (M‐H, Random, 95% CI) | 0.14 [0.03, 0.25] |
| 2.2 Low‐quality trials | 6 | 441 | Risk Difference (M‐H, Random, 95% CI) | ‐0.01 [‐0.04, 0.03] |
| 3 Severe complications (without bile duct injuries) Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| 3.1 High‐quality trials | 1 | 130 | Risk Difference (M‐H, Fixed, 95% CI) | 0.03 [‐0.02, 0.08] |
| 3.2 Low‐quality trials | 6 | 441 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.02 [‐0.05, 0.01] |
| 4 Bile duct injuries Show forest plot | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 4.1 High‐quality trials | 1 | 130 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.03, 0.03] |
| 4.2 Low‐quality trials | 6 | 441 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 5 Total complications Show forest plot | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.00 [‐0.06, 0.07] |
| 5.1 High‐quality trials | 1 | 130 | Risk Difference (M‐H, Random, 95% CI) | 0.17 [0.05, 0.29] |
| 5.2 Low‐quality trials | 6 | 441 | Risk Difference (M‐H, Random, 95% CI) | ‐0.02 [‐0.07, 0.03] |
| 6 Operative time (minutes) Show forest plot | 3 | 210 | Mean Difference (IV, Fixed, 95% CI) | 1.94 [‐1.37, 5.25] |
| 6.1 High‐quality trials | 1 | 130 | Mean Difference (IV, Fixed, 95% CI) | 4.0 [‐0.86, 8.86] |
| 6.2 Low‐quality trials | 2 | 80 | Mean Difference (IV, Fixed, 95% CI) | 0.16 [‐4.35, 4.68] |
| 7 Hospital stay (days) Show forest plot | 2 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.78 [‐4.94, ‐0.62] |
| 7.1 High‐quality trials | 1 | 130 | Mean Difference (IV, Random, 95% CI) | ‐3.9 [‐4.57, ‐3.23] |
| 7.2 Low‐quality trials | 1 | 50 | Mean Difference (IV, Random, 95% CI) | ‐1.70 [‐2.05, ‐1.35] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Sensitivity analysis 1: Operative time (minutes) Show forest plot | 7 | 571 | Mean Difference (IV, Random, 95% CI) | ‐2.98 [‐7.86, 1.90] |
| 2 Sensitivity analysis 2: Hospital stay (days) Show forest plot | 7 | 571 | Mean Difference (IV, Random, 95% CI) | ‐1.97 [‐2.56, ‐1.39] |
| 3 Sensitivity analysis 3: Omitting outlier Schmitz in total complications Show forest plot | 6 | 441 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.04 [‐0.09, 0.01] |

