Antibiotics for treating chronic osteomyelitis in adults
Abstract
Background
Chronic osteomyelitis is generally treated with antibiotics and surgical debridement but can persist intermittently for years with frequent therapeutic failure or relapse. Despite advances in both antibiotic and surgical treatment, the long‐term recurrence rate remains around 20%. This is an update of a Cochrane review first published in 2009.
Objectives
To determine the effects of different systemic antibiotic treatment regimens for treating chronic osteomyelitis in adults.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (October 2012), the Cochrane Central Register of Controlled Trials (The Cochrane Library 2012, Issue 9), MEDLINE (January 1948 to September Week 4 2012), EMBASE (January 1980 to 2012 Week 40), LILACS (October 2012), the WHO International Clinical Trials Registry Platform (June 2012) and reference lists of relevant articles.
Selection criteria
Randomised controlled trials (RCTs) or quasi‐RCTs addressing the effects of different antibiotic treatments given after surgical debridement for chronic osteomyelitis in adults.
Data collection and analysis
Two review authors independently screened papers for inclusion, extracted data and appraised risk of bias in the included trials. Where appropriate, we pooled data using the fixed‐effect model.
Main results
We included eight small trials involving a total of 282 participants with chronic osteomyelitis. Data were available from 248 participants. Most participants were male with post‐traumatic osteomyelitis, usually affecting the tibia and femur, where recorded. The antibiotic regimens, duration of treatment and follow‐up varied between trials. All trials mentioned surgical debridement before starting on antibiotic therapy as part of treatment, but it was unclear in four trials whether all participants underwent surgical debridement.
We found that study quality and reporting were often inadequate. In particular, we judged almost all trials to be at moderate to high risk of bias due to failure to conceal allocation and inadequate follow‐up.
Four trials compared oral versus parenteral route for administration of antibiotics. There was no statistically significant difference between the two groups in the remission at the end of treatment (70/80 versus 58/70; risk ratio (RR) 1.04, 95% confidence interval (CI) 0.92 to 1.18; four trials, 150 participants). There was no statistically significant difference between the two groups in the remission rate 12 or more months after treatment (49/64 versus 44/54; RR 0.94, 95% CI 0.78 to 1.13; three trials, 118 participants). There was also no significant difference between the two groups in the occurrence of mild adverse events (11/64 versus 8/54; RR 1.08, 95% CI 0.49 to 2.42; three trials, 118 participants) or moderate and severe adverse events (3/49 versus 4/42; RR 0.69, 95% CI 0.19 to 2.57; three trials, 91 participants). Superinfection occurred in participants of both groups (5/66 in the oral group versus 4/58 in the parenteral group; RR 1.08, 95% CI 0.33 to 3.60; three trials, 124 participants).
Single trials with few participants found no statistical significant differences for remission or adverse events for the following four comparisons: oral only versus parenteral plus oral administration; parenteral plus oral versus parenteral only administration; two different parenteral antibiotic regimens; and two different oral antibiotic regimens. No trials compared different durations of antibiotic treatment for chronic osteomyelitis, or adjusted the remission rate for bacteria species or severity of disease.
Authors' conclusions
Limited and low quality evidence suggests that the route of antibiotic administration (oral versus parenteral) does not affect the rate of disease remission if the bacteria are susceptible to the antibiotic used. However, this and the lack of statistically significant differences in adverse effects need confirmation. No or insufficient evidence exists for other aspects of antibiotic therapy for chronic osteomyelitis.
The majority of the included trials were conducted over 20 years ago and currently we are faced with a far higher prevalence of bacteria that are resistant to many of the available antibiotics used for healthcare. This continuously evolving bacterial resistance represents another challenge in the choice of antibiotics for treating chronic osteomyelitis.
PICO
Plain language summary
Antibiotics for treating chronic bone infection in adults
Osteomyelitis is an inflammation of the bone and bone marrow caused by pus‐forming bacteria, mycobacteria or fungi. All bone infection that is long‐standing is called chronic osteomyelitis. People with this condition are treated with systemic antibiotics, which can be given by mouth or parenterally (i.e. by injection into the muscle or vein). This review is an update of our previous 2009 publication.
We included eight small randomised trials involving 282 people. The trials presented results for a total of 248 people with chronic osteomyelitis. Post‐traumatic bone infections were the most frequent type. Surgical removal of the infected tissue (debridement) before starting on antibiotic therapy was mentioned as part of treatment in all trials, but in four trials it was unclear whether all participants underwent surgery. There were five comparisons of different treatments but we could only pool results for the comparison of antibiotic given by mouth with antibiotic given parenterally.
The pooled results (which included data from 150 people) did not show any difference between people given antibiotics by mouth or parenterally in terms of the number of people who did not have symptoms (in 'remission') at the end of treatment (four trials) or 12 months later (or more) (three trials); nor in the number of people that had negative side effects or had a superinfection (another infection that is not sensitive to antibiotic treatment). This evidence suggests that the way antibiotics are given does not impact on the disease remission rate if the bacteria causing the infection are sensitive to the antibiotic used. However, confirmation is needed. There was either no or insufficient evidence on which to base judgements about the optimum length of antibiotic treatment or the best antibiotics to use.
Authors' conclusions
Background
Description of the condition
Chronic osteomyelitis is a long‐lasting infection of the bone and bone marrow, caused by pyogenic bacteria, mycobacteria or fungi, which can progress to bone necrosis and sequestrum formation. Usually long‐lasting symptoms are vague and can include chronic pain, chills and low grade fever. Physical examination can reveal erythema, or swelling, sometimes in association with a draining sinus tract.
Osteomyelitis can be classified as either exogenous or hematogenous, based on its pathogenesis. Exogenous osteomyelitis results from a direct inoculation of bacteria into the bone at the time of trauma, during surgical reduction and internal fixation of fractures, or from an adjacent focus of infection (e.g. decubitus ulcer, soft tissue trauma) (Cunha 2002; Lew 2004; Mader 1997a; Mader 1999a; Mader 1999b; Waldvogel 1970; Walenkamp 1997). Thus, exogenous osteomyelitis includes post‐traumatic and post‐operative osteomyelitis, as well as osteomyelitis that is secondary to a contiguous focus (adjacent areas that are in contact) of infection or associated with peripheral vascular disease. In hematogenous osteomyelitis, blood‐borne bacteria reach bone from a remote portal of entry. This type is predominantly encountered in paediatric populations.
Regardless of the route of access, the microorganism (for example Staphylococcus aureus) adheres to fibronectin receptors or other membrane proteins of the bone marrow to establish an infection. Subsequently, biofilm development occurs whereby bacteria are covered by a layer of fibrinogen (slimy coat) and protected from host defence mechanism and antibiotics. The local inflammation elicited by the bacteria or by trauma contributes to destruction of bone trabeculae and bone matrix. The devitalised bone and tissue provide an inert matrix upon which microorganisms thrive. This biofilm can act as a barrier that retards the penetration of nutrients and antimicrobial agents, and together with impaired vascularisation, favours infection persistence. In the biofilm, the bacteria hide intracellularly and achieve a slow metabolic rate. The metabolically‐inactive bacteria are largely insensitive to antibiotics. Fragments of dead bone (sequestra) or metal implants can perpetuate the infection by exposing sites to which pathogenic bacteria can bind (Ciampolini 2000; Gristina 1990; Haas 1996; Lew 2004; Mader 1997a; Waldvogel 1970; Walter 2012).
Another classification of osteomyelitis is based on the anatomical stage of disease and is related to prognosis: medullary (confined to medullary cavity), superficial (involves just cortical bone), localised (involves both the cortical and medullary bone, but not the entire bone diameter) or diffuse (involves the entire thickness of the bone). Under this classification system, patients are classified as A, B or C according to the presence and severity of underlying diseases (Cierny 1985; Cierny 2003).
All aetiological classes of osteomyelitis may progress to a chronic process and it is not possible to define a time threshold after which an acute infection becomes chronic. The infection can persist intermittently for years with frequent therapeutic failure (Huber 2002; Mader 1993).
In recent years, chronic osteomyelitis incidence has apparently increased probably due to population aging, increasing prevalence of diabetes and trauma, and diagnosis improvement (Pollard 2006; Trampuz 2006). Osteomyelitis usually occurs in adults, secondary to an open injury to the bone, or after surgery for reconstruction of the bone (Darouiche 2004; Holtom 1999; Lazzarini 2002; Mader 1999b). Infections associated with prostheses are also common (Carek 2001; Haas 1996; Lew 2004). Chronic osteomyelitis may present as a recurrent or intermittent disease, with periods of quiescence of variable duration. These tend to relapse, after apparently successful therapy, with a major impact on the quality of life and a substantial financial burden to health system (Huber 2002).
Based on bacterial cultures of operative specimens, S. aureus is the main causative agent of chronic osteomyelitis. However, gram negative bacilli (Pseudomonas spp and Enterobacteriaceae) have been more frequently reported, as well as a high proportion of polymicrobial aetiology cases (Carek 2001; Mader 1992; Sheehy 2010; Waldvogel 1980).
The microbiological aetiology of chronic osteomyelitis can be difficult to establish. Bone culture should guide the antimicrobial choice. Superficial samples or swabs from fistulas should not be used for pathogen identification since they present low accuracy when compared with bone biopsy culture (Senneville 2006;Zuluaga 2002)
Non‐specific blood tests, such as erythrocyte sedimentation rate, C‐reactive protein and alpha‐1 acid glycoprotein, are widely employed in assessing chronic osteomyelitis. They are usually elevated but have low sensitivity and specificity. Some authors suggest that they can be helpful to assist the early diagnosis of postoperative bone infection, and to assess the effectiveness during the course of antibiotic therapy (Bourguignat 1996; Ferard 2002).
Description of the intervention
In general, chronic osteomyelitis is treated with antibiotics and surgical debridement to remove all the dead bone tissue (Parsons 2004). Microorganisms residing in the dead bone, if not removed along with sequestra (dead bone), can cause flare‐ups many years after the initial attack. The goal of debridement is to reach healthy, viable tissue and to remove the biofilm. Adequate debridement may leave a large bone defect known as dead space. The dead space is usually filled with local tissue flaps, or free flaps, bone graft, calcium hydroxyapatite implants or temporarily with polymethylmethacrylate beads with or without antibiotic. The goal of dead space management is to replace dead bone and scar tissue with durable vascularised tissue. If necessary, measures must be taken to achieve permanent stability of the bone. Skin grafting is used to cover wound sites involving bone that has undergone surgery, or to cover muscle flaps or graft of cancellous bone (bone that has a spongy structure) (Ciampolini 2000; Eckardt 1994; Haidar 2010; Lew 2004; Mader 1997a; Mader 1999b; Parsons 2004; Waldvogel 1980; Walter 2012).
Given the importance of biofilm in the pathophysiology and relapses of chronic osteomyelitis, some experts suggest the use of an antibiotic (e.g. rifampin) with activity against micro‐organisms in biofilm as a combination drug in both parenteral and oral regimens. However, there is insufficient evidence for choosing antibiotics based on biofilm antimicrobial susceptibility testing rather than the conventional antimicrobial susceptibility test (Saginur 2006; Walter 2012).
Four to six weeks of parenteral (non‐oral administration such as an intravenous injection) antibiotic therapy after surgery has become the standard treatment for chronic osteomyelitis. The rationale for this regimen is that three to four weeks are required for the bone to revascularise, and is based on experience of treating children with acute osteomyelitis (Carek 2001; Gentry 1990; Lazzarini 2002; Lazarini 2005; Mader 1992; Mader 1999a). However, different centres can vary regarding antibiotic use and duration of treatment, depending on the disease stage, pathogen identified or surgical intervention performed (Walter 2012; Spellberg 2012).
How the intervention might work
Despite advances in both antibiotics and surgical treatment, the long‐term recurrence rate of chronic osteomyelitis remains at around 20% (Gentry 1990; Mader 1990; Spellberg 2012; Rissing 1997). Evaluating the success of treatment is difficult as many studies show promising initial results but frequently lack long‐term follow‐up data (Mader 1992).
The optimal duration of antibiotic therapy has not been well‐defined. Due to failure rates in clinical studies, some authors advocate longer treatment with six to eight weeks of high doses of intravenous therapy followed by a course of three months or longer of oral therapy (Johnston 2007; Spellberg 2012). Apart from the doubts related to the duration of chronic osteomyelitis treatment, there are some controversies about the best route of antibiotic administration. Some reports suggest that short‐term parenteral therapy followed by oral antibiotic therapy for six weeks or oral antibiotic alone may be an effective strategy with more economic benefits than parenteral therapy alone (Gentry 1990; Mader 2001; Rissing 1997; Spellberg 2012; Swiontkowski 1999).
Short‐term oral antibiotics for treating chronic osteomyelitis, if as effective as the parenteral route, would be more convenient for patients, with no risk of vascular line infection, and would probably cost less.
Why it is important to do this review
The epidemiology of chronic osteomyelitis has changed in recent years. There has been a significant increase in post‐traumatic and post surgical osteomyelitis, especially in developed countries (Trampuz 2006).
Surgical debridement is a mainstay of chronic osteomyelitis treatment (Parsons 2004). However, in current practice, additional treatment with antibiotics is frequently recommended for infection eradication (Spellberg 2012; Walter 2012). Various antibiotic regimens are in use (Lazarini 2005; Walter 2012) and there are many questions regarding the ideal route of antibiotic administration (oral or parenteral). If oral therapy is proven to be similarly or more effective for treating chronic osteomyelitis, it will be preferred because it is generally more comfortable for the patient and less expensive (Johnston 2007; Spellberg 2012; Stengel 2001; Walter 2012).
Currently, increasing antibiotic resistance, due in part to the inappropriate use of antimicrobials, is of great concern worldwide. Many S. aureus acquired infections in the community or in hospital are now resistant to beta‐lactamic antibiotics, and the gram negative bacilli have become resistant to beta‐lactamic and fluoroquinolones (Lew 2004; Murphy 2011; Sheehy 2010). Therefore, the duration and type of antibiotic regimen to treat chronic osteomyelitis needs to be defined based on good quality research. This is an update of a Cochrane review first published in 2009 (Conterno 2009).
Objectives
To determine the effects of systemic antibiotics for treating chronic osteomyelitis in adults.
We aimed to compare different antimicrobial regimens, in terms of choice of drug and route of administration, to treat bacterial chronic osteomyelitis in adults.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) and quasi‐RCTs (i.e. a method of allocation that is not strictly speaking random, such as date of birth or alternation) irrespective of publication status or blinding.
Types of participants
We included adults with chronic osteomyelitis.
The diagnosis of chronic osteomyelitis could be defined in the included studies as: clinical pattern evolved over months or years and characterised by low‐grade inflammation, presence of pus, microorganisms or presence of dead bone (sequestra), demonstrated by plain film, computed tomography or magnetic resonance imaging, or isolation of bacteria from the bone lesion (Lew 2004). Trial participants should have undergone surgical management of infection with the debridement of necrotic tissue. However, we did not exclude studies based on failure to describe prior treatment.
We excluded trials that focused specifically on the treatment of diabetic foot osteomyelitis, implant‐associated osteomyelitis, sternal or vertebral osteomyelitis. We included mixed population trials primarily focusing on chronic osteomyelitis only if the proportion of participants with otherwise excluded conditions was low or separate data were available.
Types of interventions
Comparative studies of systemic antibiotic treatment of chronic osteomyelitis. We included trials comparing different antibiotics, different antibiotic routes of administration (oral, parenteral or a combination of parenteral and oral) or different treatment durations.
We defined parenteral route of administration as any route other than the mouth or bowel. We did not include studies addressing local antibiotic treatment. The bacteria should have had documented sensitivity to the antibiotics used. Participants should have had surgical management of infection with debridement of all necrotic tissue and obliteration of dead space; stabilisation of the bone and adequate soft tissue coverage should have been done if necessary.
Types of outcome measures
Primary outcomes
-
Remission of infection, where we defined remission as the resolution of all signs and symptoms of active infection at the end of therapy and after a minimal post‐treatment observation period of one year (Carek 2001; Gentry 1990; Mader 1992).
-
Number of participants who presented remission of infection at the end of therapy.
-
Number of participants who presented remission of infection at least one year after therapy.
Secondary outcomes
-
Number of participants with failure (defined as a lack of apparent response to therapy as evidenced by one or more of the following: persistence of drainage, recurrence of sinus tract or failure of sinus tract to close, persistence of systemic signs of infection (chills, fever, weight loss, bone pain), or progression of bone infection shown by imaging methods) (Gentry 1990; Mader 1992). Treatment failure also included early interruption of treatment, such as for adverse effects or disease complications such as amputation.
-
Number of participants with early relapse (defined as recurrence of signs and symptoms plus isolation of the same pathogen(s) within four to six weeks after discontinuation of antibacterial therapy) (Gentry 1990; Mader 1992).
-
Number of participants with late relapse (defined as recurrence occurring after six weeks and up to 12 months after the end of therapy) (Gentry 1990; Mader 1992).
-
Adverse events:
-
Adverse events related to antibiotic use
-
Orthopaedic sequels such as residual pain and non‐union
-
Superinfection (defined as the isolation of new pathogens from infected bone during therapy)
-
Number of amputations
-
Death
-
Resource use (all settings)
Such as:
-
Cost of antibiotics
-
Days of hospitalisation
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (October 2012), the Cochrane Central Register of Controlled Trials (The Cochrane Library 2012, Issue 9), MEDLINE (January 1948 to September Week 4 2012), EMBASE (January 1980 to 2012 Week 40) and LILACS (Latin America and Caribbean Health Sciences ‐ October 2012). We also searched the World Health Organization International Clinical Trials Registry platform (June 2012) for ongoing trials. We did not apply any language restrictions.
In MEDLINE (OVID WEB), we combined the search strategy with the revised optimal trial search strategy (Higgins 2006). We modified the strategy for use in the other databases (see Appendix 1).
Searching other resources
We searched reference lists of relevant articles.
Data collection and analysis
Selection of studies
Two review authors (LOC and MDT) independently inspected each reference produced by the search and identified potentially eligible studies, for which we obtained full text articles where possible. The same two authors independently performed study selection. We resolved any disagreements by consensus.
Data extraction and management
Two review authors (LOC and MDT) independently extracted the data from trial reports. We used a tool based on the generic data extraction tool developed by the Cochrane Bone, Joint and Muscle Trauma Group. We resolved any disagreements by consensus.
Assessment of risk of bias in included studies
In this review update, two authors independently assessed the risk of bias in newly included trials, without masking the source and authorship of the trial reports. At least one author assessed risk of bias in trials that we included in previous versions of the review. We performed a pilot trial of the assessment form using two trials. One author checked data extraction consistency between review authors and between review versions. We resolved any differences through discussion. We used the risk of bias tool outlined in the Cochrane Handbook for Systematic Reviews of Interventions to assess bias in included studies (Higgins 2011). This tool incorporates assessment of randomisation (sequence generation and allocation concealment), blinding (of participants, treatment providers and outcome assessment), completeness of outcome data, selection of outcomes reported and other sources of bias. We assessed three additional sources of bias: major imbalances in baseline characteristics; lack of comparability of care programmes other than the interventions under test; and inadequate duration of follow‐up.
Measures of treatment effect
We calculated risk ratios (RR) and 95% confidence intervals (CIs) for dichotomous outcomes.
If future updates of this review include studies with continuous outcomes, we will calculate mean differences and 95% CIs.
Unit of analysis issues
We did not have any unit of analysis issues, in particular those relating to cluster‐RCTs, cross‐over trials or trials with multiple treatment groups.
Dealing with missing data
As all the studies (except Euba 2009) were conducted more than 10 years ago, we therefore chose not request to additional information from the trial authors.
Whenever possible, we performed intention‐to‐treat analyses to include all randomised participants. However, when we identified drop‐outs, we used the actual denominators of participants contributing data at the relevant outcome assessment. Should continuous outcome data be available in future, we will be alert to the potential mislabelling or non‐identification of standard errors and standard deviations. Unless missing standard deviations can be derived from CIs or standard errors, we will not assume values in order to present these in the analyses.
Assessment of heterogeneity
We assessed heterogeneity by visual inspection of the forest plot and using the Chi² statistic (with significance set at P < 0.10) in conjunction with the I² statistic, which describes the percentage of the variability in effect estimates that are due to heterogeneity rather than sampling error (chance) (Higgins 2003). We considered an I² value > 50% as evidence of substantial heterogeneity.
Assessment of reporting biases
As an insufficient number of trials met our inclusion criteria (fewer than 10 trials), we did not generate funnel plots to explore the potential for publication bias.
Data synthesis
Where appropriate, we pooled data using the fixed‐effect model and presented 95% CI values.
Subgroup analysis and investigation of heterogeneity
In future updates, if appropriate, we will investigate possible causes of heterogeneity by subgrouping according to different bacteria groups (gram‐negative, gram‐positive or polymicrobial infection), severity of the disease (medullary, superficial, localised or diffuse) (Cierny 2003), treatment duration (more or less than six weeks) and classification (post‐traumatic, post‐surgical).
We will investigate whether the results of subgroups are significantly different by inspecting the overlap of confidence intervals and performing the test for subgroup differences available in Review Manager (RevMan)RevMan.
Sensitivity analysis
In future updates, if appropriate, we will perform sensitivity analyses to examine various aspects of trial and review methodology, including the effects of missing data, the selection of statistical model (fixed‐effect versus random‐effects) for pooling, and the effects of excluding trials at high or unclear risk of bias, such as high risk of selection bias arising from the lack of allocation concealment.
Results
Description of studies
Results of the search
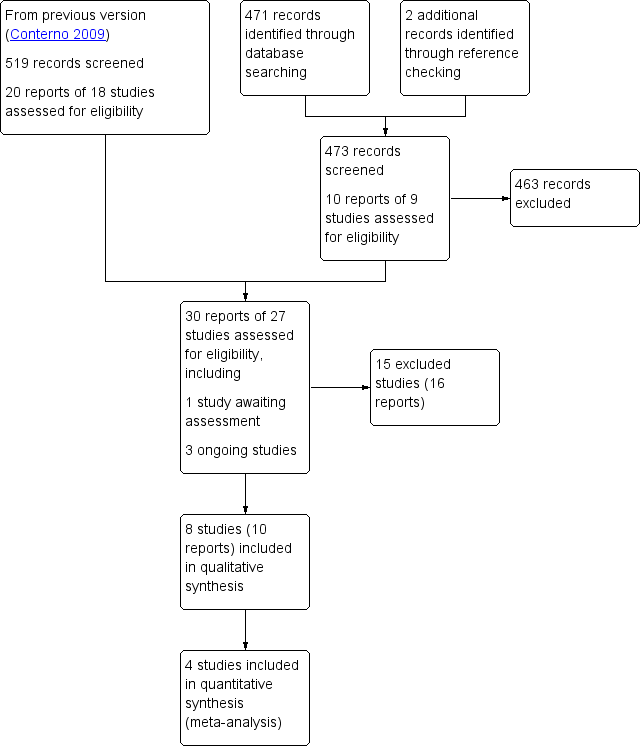
In the previous search conducted up to October 2008, we screened 519 studies. For this review update (search completed October 2012), we screened a total of 471 records from the following databases: Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (5 records); Cochrane Central Register of Controlled Trials (31), MEDLINE (96), EMBASE (227), LILACS (45) and WHO International Clinical Trials Registry Platform (67). We also identified two potentially eligible studies from other sources (reference lists of included studies and reviews on the subject). For details, see the PRISMA study flowchart (Figure 1)

Study flow diagram.
From the search update, we identified 10 citations of potentially eligible records, for which we obtained full reports where possible. We included one additional trial (two references) in this update (Euba 2009), we excluded four trials (Ingianni 2007; Marriott 2008; Nguyen 2009; Tascini 2009), and three trials are ongoing (CTRI/2008/091/000060; EUCTR2009‐015744‐42‐GB; NCT00324922). A further study (Barberán 2000) is awaiting classification.
We excluded one of the studies included in the previous version (Greenberg 1987) from this update.
Overall, we have included eight trials, excluded 15 studies, and identified three ongoing trials and one study awaiting classification.
Included studies
We have listed the details of the individual trials in the Characteristics of included studies.
Design
Of the eight included trials, seven RCTs and one quasi‐RCT (Mader 1990). Three trials (Gentry 1990; Gentry 1991; Norden 1986) were multicentre trials and five trials were likely to have been conducted at a single site (Euba 2009; Gomis 1999; Greenberg 2000; Mader 1990; Sheftel 1986).
Sample sizes
The eight included trials comprised a total of 282 participants, with data available from 248. The number of participants enrolled in the individual studies ranged from 12 (Greenberg 2000) to 67 (Gentry 1990), and in individual intervention groups ranged from five (Greenberg 2000) to 31 (Gentry 1990). Only one trial reported a sample‐size calculation, but even in this trial the trial authors did not achieve the desired sample size (Norden 1986).
Setting
All eight trials were conducted in the tertiary care (hospital) setting. Six trials were conducted in the USA; two of these (Gentry 1990; Gentry 1991) were also carried out in Costa Rica. Two trials were conducted in Spain (Euba 2009; Gomis 1999). Three trials were funded by the pharmaceutical industry (Gentry 1991; Mader 1990; Norden 1986).
Participants
All trials had at least twice as many male as female participants. Whenever reported, the mean age of participants ranged from 33 years (Mader 1990) to 59 years (Gomis 1999).
According to the trial reports, all participants had a diagnosis of chronic osteomyelitis, but with variable duration of symptoms pretreatment. Three trials reported the duration of chronic osteomyelitis (Euba 2009; Mader 1990; Norden 1986) and ranged from one month (Euba 2009) to 28 years (Norden 1986).
Two studies described the classification of osteomyelitis using the Cierny‐Mader System (Mader 1990; Sheftel 1986) and Gomis 1999 used the classification based on aetiology. Post‐traumatic osteomyelitis was the most frequent type. Where reported, the location of the infection was mainly the tibia and femur.
In all trials, trial authors obtained the bacteria sample for microbiological diagnosis by open biopsy or aspiration from infected bone, and the isolated bacteria were sensitive to the antibiotic used.
In four trials, S. aureus was the most frequent bacterial species isolated (Gentry 1990; Gentry 1991; Gomis 1999; Mader 1990), but polymicrobial infections and infections caused by Pseudomonas aeruginosa were common among the trials. Two trials included only chronic osteomyelitis caused by S. aureus (Euba 2009; Norden 1986) and another trial reported only infection caused by gram‐negative bacteria (Sheftel 1986).
All trials mentioned debridement as part of treatment. Only three trials gave details about the surgical proceedings (Euba 2009; Mader 1990; Norden 1986). Gentry 1991 and Gomis 1999 reported that the surgical debridement was performed as indicated; Mader 1990 and Greenberg 2000 did not report whether the surgical debridement was done in all participants; and Norden 1986 reported that all participants but two had surgical debridement.
Interventions
The included trials evaluated five different comparisons:
-
Oral antibiotics versus parenteral antibiotics (Gentry 1990; Gentry 1991; Gomis 1999; Mader 1990)
-
Oral antibiotics versus parental plus oral antibiotics (Euba 2009)
-
Parenteral antibiotics plus oral antibiotics versus parenteral antibiotic (Norden 1986)
-
Parenteral antibiotics versus another parenteral antibiotics (Sheftel 1986)
-
Oral antibiotics versus another oral antibiotics (Greenberg 2000)
No trial specifically compared different durations of antibiotic treatment for chronic osteomyelitis.
Regarding oral antibiotics used, five trials used quinolones (Gentry 1990; Gentry 1991; Gomis 1999; Greenberg 2000; Mader 1990), two trials used rifampin (Euba 2009; Norden 1986), one trial used cloxacillin (Euba 2009) and one trial used cotrimoxazole (Euba 2009).
Trials used several different parenteral antibiotics. Four trials used ceftazidime or cefazolin (Gentry 1990; Gentry 1991; Norden 1986; Sheftel 1986), three trials used nafcillin (Gentry 1990; Mader 1990; Norden 1986), one trial used imipenem (Gomis 1999), three trials used aminoglycoside (Gentry 1990; Mader 1990; Sheftel 1986), one trial used cloxacillin (Euba 2009) and one trial used ticarcillin (Sheftel 1986).
The antibiotic regimens varied among the trials in terms of drugs used; even within the same trial, there were many different combinations of antibiotics. We could not make comparisons between the included trials to determine the best antibiotic for treating chronic osteomyelitis in adults.
The duration of treatment in the included studies varied within and between trials and ranged from less than seven days (Gomis 1999) to 110 days (Greenberg 2000).
Outcomes
Across the trials, authors did not uniformly report the definitions of the outcome measures. Also, the reported definition of the outcomes varied between trials but we considered these definitions to be clinically consistent enough to permit pooling in some cases.
The outcomes were clinically and microbiologically based in two trials (Gentry 1990; Sheftel 1986) and clinically based in the remaining six trials.
Eight trials reported the complete resolution of disease symptoms at the end of treatment, and seven trials after follow‐up of at least 12 months (Euba 2009; Gentry 1990; Gentry 1990; Greenberg 2000; Mader 1990; Norden 1986; Sheftel 1986). The length of follow‐up for individual trial participants, which varied between and within trials, ranged from less than one month (Greenberg 2000) to more than 13 years (Euba 2009).
All eight trials reported adverse events related to antibiotic therapy. Five trials reported the adverse events as severe. Four trials reported the occurrence of superinfection during the treatment (Gentry 1990; Gentry 1991; Gomis 1999; Sheftel 1986).
Only one trial (Euba 2009) reported data on the length of hospital stay. No trial reported on the costs related to treatment.
Excluded studies
We excluded 15 studies (see the Characteristics of excluded studies for details). The main reasons for exclusion were lack of separate data for participants with chronic osteomyelitis (seven studies), lack of details of the antibiotic used and the diagnosis criteria (three studies), lack of surgical debridement (three studies) and retrospective study design (two studies). We excluded a previously included trial (Greenberg 1987) from this update because the trial authors did not perform surgical debridement.
Ongoing studies
Three RCTs are ongoing but each have uncertain recruitment status. One study (CTRI/2008/091/000060), which includes adults with mild or severe infection, including bone and joint infections, compares treatment with vancomycin plus ceftriaxone versus vancomycin alone. EUCTR2009‐015744‐42‐GB, which includes adults with bone and joint infection, compares treatment with oral antibiotics versus parenteral antibiotics. NCT00324922, which includes adults with bone and joint infection by methicillin‐resistant S. aureus, compares treatment with trimethoprim‐sulphamethoxazole versus vancomycin.
Risk of bias in included studies
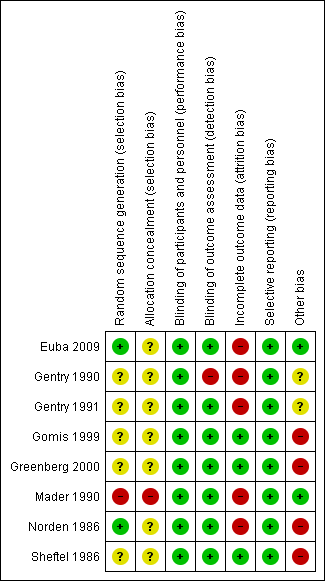
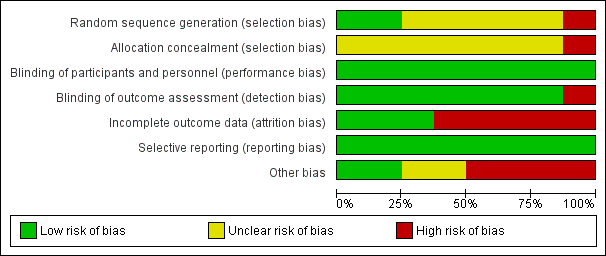
We have summarised the risk of bias judgements for the individual trials in Figure 2 and Figure 3. We described them in the 'Risk of bias' tables in the Characteristics of included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
Allocation
We judged the two studies that provided details of random sequence generation (computer‐generated randomisation list and random numbers table, respectively) to be at low risk of selection bias related to sequence generation (Euba 2009; Norden 1986). Both of these studies and five other studies failed to provide sufficient information to permit judgement regarding allocation concealment and had unclear risk of bias. In Mader 1990, the trial authors "sequentially assigned" participants to the two treatment groups and this trial was therefore considered at high risk of selection bias.
Blinding
Seven studies did not blind the participants, personnel or assessors to the treatment (Euba 2009; Gentry 1990; Gentry 1991; Gomis 1999; Greenberg 2000; Norden 1986; Sheftel 1986). However, we classified these studies as low risk of bias because we judged that the outcomes (remission after the treatment) were not influenced by lack of blinding. We considered Gentry 1990 at high risk of detection bias because participants reported the return of the symptoms either via the telephone or a letter.
Incomplete outcome data
Three studies reported the number of withdrawals and they undertook intention‐to‐treat analysis whenever possible (Gomis 1999; Greenberg 2000; Sheftel 1986). Five studies stated the numbers and reasons for withdrawal but they were unable to undertake intention‐to‐treat analysis (Euba 2009; Gentry 1990; Gentry 1991; Mader 1990; Norden 1986). We judged these five studies at high risk of attrition bias.
Selective reporting
All studies reported the outcomes described in the methods section, including adverse events, and had no evidence of selective reporting.
Other potential sources of bias
In general, studies described the baseline characteristics of participant age, gender and site of infection. Three trials mentioned duration of disease (Euba 2009; Mader 1990; Norden 1986), and only two trials gave the classification of disease using the Cierny‐Mader System (Mader 1990; Sheftel 1986). We considered there was baseline comparability in four trials (Euba 2009; Gomis 1999; Mader 1990; Norden 1986).
In all trials, participants received apparently identical care programmes. However, no study gave details for individual treatment groups of medical history, physical examination or laboratory investigations carried out during the study.
There was some variation between trials in the definition of inclusion criteria, outcome measures and outcome assessment, but all trials gave sufficient information and were clinically consistent.
Trials reported active follow‐up. However, the length of follow‐up was different for each participant within the trials and was not long enough in four trials, where some participants were followed up for nine months (Norden 1986), six months (Gomis 1999), two months (Sheftel 1986) or less than one month (Greenberg 2000).
Overall, we judged two trials (Euba 2009; Mader 1990) at low risk of other bias; two trials (Gentry 1990; Gentry 1991) at unclear risk; and the other four trials at high risk.
Effects of interventions
We report the results for the five comparisons made by the included trials below. None addressed the impact of different bacteria species (e.g. S. aureus, Enterobacteriaceae, Pseudomonas spp) on the rate of remission, or the impact of different duration of antibiotic use on the rate of remission. Only Euba 2009 reported on length of hospital stay. None of the included trials reported on cost.
Oral versus parenteral route of administration of antibiotics
Four trials, presenting data from a total of 150 participants, compared oral quinolones with various parenteral antibiotics regimens (Gentry 1990; Gentry 1991; Gomis 1999; Mader 1990).
The remission rates at the end of treatment with oral versus parenteral antibiotic were 88% (70/80) with oral antibiotic and 83% (58/70) with parenteral antibiotic, with no statistically significant difference between the two groups (RR 1.04, 95% CI 0.92 to 1.18; four trials, 150 participants; Analysis 1.1). We did not observe any statistical heterogeneity between trials.
Remission rates at 12 or more months after the end of treatment were 77% (49/64) with oral antibiotic and 81% (44/54) with parenteral antibiotics (Gentry 1990; Gentry 1991; Mader 1990). We did not detect any statistically significant difference between groups (RR 0.94, 95% CI 0.78 to 1.13; three trials, 118 participants; Analysis 1.2) or any statistical heterogeneity between trials.
Three trials reported a variety of mild adverse events relating to the antibiotic used (Gentry 1990; Gentry 1991; Mader 1990); 17% (11/64) in the oral antibiotic groups and 15% (8/54) in the parenteral groups. We did not observe any statistically significant difference between the two groups in the pooled results (RR 1.08, 95% CI 0.49 to 2.42; three trials, 118 participants; Analysis 1.3). Moderate or severe adverse events, such as those requiring termination of treatment, occurred in 6.1% (3/49) of participants in the oral antibiotic group and 9.5% (4/42) in the parenteral groups but this was nota statistically significant difference (RR 0.69, 95% CI 0.19 to 2.57; three trials, 91 participants; Analysis 1.4).
Superinfection occurred in participants of both groups (7.6% (5/66) in the oral group versus 6.9% (4/58) in the parenteral group) (RR 1.08, 95% CI 0.33 to 3.60; three trials, 124 participants; Analysis 1.5).
Oral antibiotics versus parenteral plus oral antibiotics
One trial (Euba 2009) included 55 participants with chronic osteomyelitis by S. aureus and compared oral antibiotics (cotrimoxazole and rifampicin) versus parenteral (cloxacillin) plus oral antibiotic (cloxacillin). The remission rates at 12 months after the end of treatment were 80% (24/30) in the group that received oral antibiotics and 76% (19/25) in the group that received parenteral plus oral antibiotic. We did not observe any statistically significant difference between the two groups (RR 1.05, 95% CI 0.79 to 1.40; one trial, 55 participants; Analysis 2.1).
In total there were eight adverse events: three cases of rash, one case of bronchospasm and one case of nausea in the oral antibiotic group; and three cases of phlebitis in the parenteral plus oral antibiotic group (RR 1.39, 95% CI 0.37 to 5.25; one trial, 55 participants; Analysis 2.2).
The median number of days in hospital stay (interquartile range) was significantly shorter in the group who received oral antibiotics only compared with the group who received parental plus oral antibiotic: 31 days (21 to 49 days) versus 51 days (43 to 67), P = 0.002.
Parenteral plus oral antibiotics versus parenteral antibiotics
Remission rate at least 12 months after the end of treatment was reported in only one trial with 19 participants (data available from 18) with chronic osteomyelitis caused by Staphylococcus aureus (Norden 1986). The remission rates were 80% (8/10) in the parenteral plus oral antibiotic group and 50% (4/8) in the parenteral antibiotic group. We did not observe any statistically significant difference (RR 1.60, 95% CI 0.75 to 3.42; one trial, 18 participants; Analysis 3.1).
Trial authors reported significant neutropenia in one participant of the parenteral plus oral antibiotic group and three participants of the parenteral antibiotic group, all with spontaneous recovery (RR 0.27, 95% CI 0.03 to 2.10; one trial, 18 participants; Analysis 3.2).
Parenteral antibiotics
Sheftel 1986 compared regimens of parenteral antibiotics (ceftazidime versus ticarcillin plus tobramycin) in 18 participants with chronic osteomyelitis caused by gram‐negative bacilli. P. aeruginosa and Enterobacter cloacae were the most common organisms isolated. The remission rates at 12 months after the end of treatment were 67% (6/9) in the group that received ceftazidime and 89% (8/9) in the group that received ticarcillin (RR 0.75, 95% 0.45 to 1.26; one trial, 18 participants; Analysis 4.1).
The trial author reported one adverse event, a case of mild increase in serum hepatic enzyme level in the ceftazidime group, and none in the other group (RR 3.00, 95% 0.14 to 65.16; one trial, 18 participants; Analysis 4.2).
Trial authors reported superinfection in two participants of the ceftazidime group and none in the ticarcillin plus tobramycin group (RR 5.00, 95% CI 0.27 to 91.52; one trial, 18 participants; Analysis 4.3).
Oral antibiotics
One trial (Greenberg 2000) compared two different oral quinolones (ciprofloxacin and lomefloxacin) and included five and seven participants with chronic osteomyelitis respectively in the two groups. We did not observe any statistically significant difference in the remission rates after 12 months follow‐up between the groups (two in each group; RR 1.40, 95% CI 0.29 to 6.86; one trial, 12 participants; Analysis 5.1).
Trial authors reported adverse events in three participants of the lomefloxacin group and in none of the ciprofloxacin group but this difference was not statistically significant (RR 0.19, 95% CI 0.01 to 3.03; one trial, 12 participants; Analysis 5.2).
Discussion
Summary of main results
In this review update, we included eight small and heterogeneous studies that involved 282 adults with biopsy‐proven chronic osteomyelitis caused by bacteria with confirmed sensitivity to the antibiotics used. Results data were available for 248 participants. The main finding of this review is the lack of evidence to guide practice. The route of antibiotic administration was the only outcome that was evaluated by more than one trial.
We found no evidence of a difference between oral antibiotics (all quinolones in four trials) compared with parenteral antibiotic in the rate of remission at the end of therapy (RR 1.04, 95% CI 0.92 to 1.18; four trials, 150 participants) and after 12 months or more follow‐up (RR 0.94, 95% CI 0.78 to 1.13; three trials, 118 participants). These results were statistically homogeneous. Separately pooled results for mild and more serious adverse events again showed no statistical differences between the two routes of administration. We did not observe any difference between the two groups in the incidence of superinfection.
Single trials with few participants found no statistical significant differences for remission or adverse events for the following four comparisons: oral antibiotic versus parenteral plus oral (one trial, 55 participants); parenteral plus oral versus parenteral only administration (one trial, 18 participants); two parenteral antibiotic regimens (one trial, 18 participants); two oral antibiotic regimens (one trial, 12 participants).
Overall completeness and applicability of evidence
Due to the lack of data, we were unable to draw robust conclusions. In the comparison of oral versus parenteral antibiotics, the data suggest that provided the infective bacteria show sensitivity to the antibiotic used, the method of administration does not affect rate of disease remission. However, the number of participants in the included trials and pooled results may be insufficient to detect a difference between different routes of antibiotic administration to treat chronic osteomyelitis.
Other considerations include length of follow‐up, the relative importance of surgical debridement and currency of the trial evidence.
Chronic osteomyelitis in adults generally occurs secondary to an open injury to the bone or after surgery for reconstruction of the bone (Holtom 1999; Lazzarini 2002; Mader 1999b; Trampuz 2006). It may present as a recurrent or intermittent disease, with periods of quiescence of variable duration. Because of this aspect, the term 'remission' is preferable to 'cure' and the time of post‐treatment follow‐up should be at least 12 months to assume a sustained remission of disease. While we have applied the 12‐month definition here, some authors suggest a follow‐up of five years as ideal (Mader 1990). Others recommend survival analysis to provide information about the length of time free of relapse (Simpson 2001; Walenkamp 1997). In one trial, the authors planned a survival analysis but this was not presented (Euba 2009).
The current practice for treating chronic osteomyelitis includes complete surgical debridement of necrotic bone and antibiotic therapy. The contribution of each component to clinical success in the treatment of osteomyelitis is not known. Some researchers argue that the surgical intervention is the most important and that insufficient debridement is correlated with a high recurrence rate (Eckardt 1994; Gentry 1990; Haidar 2010; Simpson 2001; Stengel 2001). The requirement of surgical debridement is unquestionable, but we do not know whether surgical debridement is enough for the sustained remission of chronic osteomyelitis. Given that antibiotics could contribute to the control of chronic bone infection, it remains important to know if the class of antimicrobial used, the route of drug administration and the duration of therapy could influence the rate of sustained remission of infection.
The only aspect of the antibiotic regimen that was evaluated by more than one trial included in this review was the route of administration. The trial participants were treated with many different antibiotics and surgical debridement. Since the trials did not give details about the surgical intervention, we do not know if this aspect of treatment was adequate and comparable among the trials. However, some trials did attribute some treatment failures to inadequate debridement (e.g. Gentry 1990). Nonetheless, the available data preclude any conclusion about the exact contribution of surgery to the rate of remission.
If oral antibiotics have the same success rates as parenteral antibiotics, with similar risks of adverse adverse effects, then these have the attraction of being easier to administer, being less expensive and avoiding the inconvenience of prolonged hospital stays and medical treatment associated with parenteral administration. However, we were not able to demonstrate this in this review due to the variability in the trial characteristics and lack of evidence for aspects of administration such as duration of treatment.
Currently, chronic osteomyelitis is increasing and is often associated with trauma, such as car accidents and orthopedic surgeries, and affects patients with diabetes mellitus or decubitus ulcers. This heterogeneous population is not adequately represented in this review because we excluded people with diabetic foot osteomyelitis, implant‐associated osteomyelitis, sternal or vertebral osteomyelitis.
Finally, the majority of the included trials are over 20 years old. Nowadays there are higher prevalences of bacteria resistant to one or more available antibiotics, particularly when the infections are associated with healthcare procedures (Murphy 2011; Sheehy 2010). For example, methicillin‐resistant S. aureus prevalence is much higher now compared to the past two decades. We have a very limited number of antibiotics to treat this bacterial infection (Liu 2011). Continuously evolving bacterial resistance represents another challenge to the choice of antibiotics to treat chronic osteomyelitis.
Quality of the evidence
We judged almost all of the included trials to be at moderate to high risk of bias due to trial design and reporting. These factors included failure to conceal allocation, lack of blinding, poor or unknown comparability of baseline characteristics, inadequate follow‐up and post‐randomisation exclusions in some trials. Overall, we did not detect statistically significant differences for the pooled results of trials comparing oral versus parenteral antibiotics. Exaggerated effects that may be associated with these biases were therefore not apparent.
Overall, we consider the quality of the evidence for the main comparison (oral versus parenteral antibiotics) to below. This reflects, in particular, the high likelihood of bias, the questions over applicability of the evidence and the small sample size. Further research may change the results and conclusions for this comparison.
Potential biases in the review process
The key potential bias in our review is that we may have not included all the evidence from randomised trials. Although our database search was comprehensive, we may have missed trials reported in conference proceedings. However, such reports are likely to be unavailable if these were contemporaneous with most of the studies in this review. As most of the trials and trial reports were over 10 years old, we decided not to request information from trial authors, including separate data for patients with chronic osteomyelitis in several excluded trials with mixed populations.
Agreements and disagreements with other studies or reviews
We located five published systematic reviews on the clinical efficacy of antibiotics for treating bone and joint infection including chronic osteomyelitis (Haidar 2010; Karamanis 2008; Lazarini 2005; Spellberg 2012; Stengel 2001). These differ from our review in terms of participants' characteristics, types of infections and study designs included. In this review, we included RCTs and quasi‐RCTs of adult patients with chronic osteomyelitis treated with systemic antibiotics.
Stengel 2001 included RCTs and quasi‐RCTs only and covered local antibiotic therapy and joint infection. They concluded that no reliable inferences could be made from the available data on antibiotic therapy for osteomyelitis and septic arthritis.
Lazarini 2005 evaluated antibiotic treatment for acute and chronic osteomyelitis in children and adults and included uncontrolled studies. The authors concluded that the optimal duration of antibiotic therapy remains undefined and they could not determine the best agent, route or duration of antibiotic therapy from the available data.
Karamanis 2008 included seven RCTs and compared fluoroquinolones versus B‐lactamic antibiotic to treat osteomyelitis. We did not include three studies described in Karamanis 2008 in our review: one trial (Lipsky 1997) included participants with osteomyelitis secondary to diabetic foot infection and two trials (Giamarellou 1989; Greenberg 1987) did not report whether bone debridement was done.
Haidar 2010 searched the medical literature for evidence in animal and human studies to support the use of short courses of antibiotics for treating chronic osteomyelitis. The review authors only included studies that used short courses of antibiotics (three to 14 days). Haidar 2010 did not report their criteria for study inclusion nor the length of follow‐up. The authors suggested that shortened duration of antimicrobial treatment with emphasis on debridement, and well‐vascularised flap coverage might be a possible alternative for treating chronic osteomyelitis in the lower extremities. They concluded that properly designed studies are needed to determine the optimal duration of antibiotics.
The most recent review included 13 RCTs and 63 non‐RCTs (Spellberg 2012). The authors concluded that oral and parenteral therapies achieve similar cure rates and that there is no evidence that antibiotic therapy for greater than four to six weeks improves outcomes compared with shorter regimens. However, the review included RCTs and non‐RCTs and heterogeneous populations in terms of the type of osteomyelitis (osteomyelitis secondary to diabetes foot infection and orthopaedic implants).
Study flow diagram.
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

Comparison 1 Oral antibiotic versus parenteral antibiotic (AB), Outcome 1 Remission at the end of treatment.

Comparison 1 Oral antibiotic versus parenteral antibiotic (AB), Outcome 2 Remission at least 12 months after the end of treatment.

Comparison 1 Oral antibiotic versus parenteral antibiotic (AB), Outcome 3 Mild adverse events.

Comparison 1 Oral antibiotic versus parenteral antibiotic (AB), Outcome 4 Moderate or severe adverse events.

Comparison 1 Oral antibiotic versus parenteral antibiotic (AB), Outcome 5 Superinfection.

Comparison 2 Oral antibiotic versus parenteral plus oral antibiotic, Outcome 1 Remission at least 12 months after the end of the treatment.

Comparison 2 Oral antibiotic versus parenteral plus oral antibiotic, Outcome 2 Adverse events.
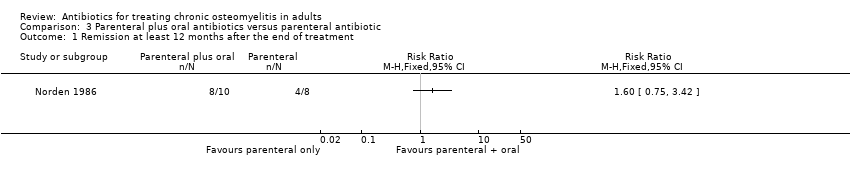
Comparison 3 Parenteral plus oral antibiotics versus parenteral antibiotic, Outcome 1 Remission at least 12 months after the end of treatment.

Comparison 3 Parenteral plus oral antibiotics versus parenteral antibiotic, Outcome 2 Adverse events.
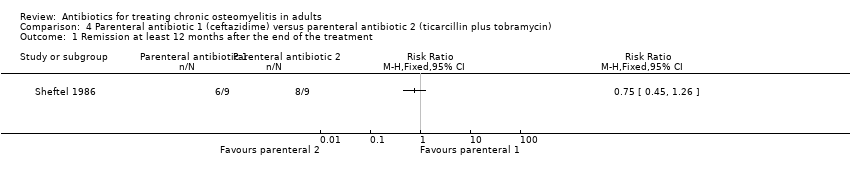
Comparison 4 Parenteral antibiotic 1 (ceftazidime) versus parenteral antibiotic 2 (ticarcillin plus tobramycin), Outcome 1 Remission at least 12 months after the end of the treatment.
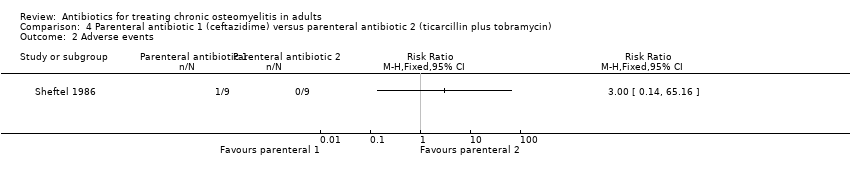
Comparison 4 Parenteral antibiotic 1 (ceftazidime) versus parenteral antibiotic 2 (ticarcillin plus tobramycin), Outcome 2 Adverse events.

Comparison 4 Parenteral antibiotic 1 (ceftazidime) versus parenteral antibiotic 2 (ticarcillin plus tobramycin), Outcome 3 Superinfection.

Comparison 5 Oral antibiotic 1 (ciprofloxacin) versus oral antibiotic 2 (lomefloxacin), Outcome 1 Remission at least 12 months after the end of treatment.

Comparison 5 Oral antibiotic 1 (ciprofloxacin) versus oral antibiotic 2 (lomefloxacin), Outcome 2 Adverse events.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Remission at the end of treatment Show forest plot | 4 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.92, 1.18] |
| 2 Remission at least 12 months after the end of treatment Show forest plot | 3 | 118 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.78, 1.13] |
| 3 Mild adverse events Show forest plot | 3 | 118 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.49, 2.42] |
| 4 Moderate or severe adverse events Show forest plot | 3 | 91 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.19, 2.57] |
| 5 Superinfection Show forest plot | 3 | 124 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.33, 3.60] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Remission at least 12 months after the end of the treatment Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Remission at least 12 months after the end of treatment Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Remission at least 12 months after the end of the treatment Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Superinfection Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Remission at least 12 months after the end of treatment Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |

