Betamiméticos para la inhibición del trabajo de parto prematuro
Resumen
Antecedentes
El parto prematuro es una de las causas principales de mortalidad y morbilidad perinatal en todo el mundo. Los agentes tocolíticos son fármacos utilizados para inhibir las contracciones uterinas. Los betamiméticos son agentes tocolíticos utilizados ampliamente, especialmente en los países de escasos recursos.
Objetivos
Evaluar los efectos de la administración de betamiméticos a las pacientes con trabajo de parto prematuro.
Métodos de búsqueda
Se hicieron búsquedas en el registro de ensayos del Grupo Cochrane de Embarazo y Parto (Cochrane Pregnancy and Childbirth Group) (31 de diciembre de 2013) y en listas de referencias de los estudios recuperados.
Criterios de selección
Ensayos controlados aleatorios de betamiméticos, administrados por cualquier vía o a cualquier dosis, para el tratamiento de las pacientes en trabajo de parto prematuro y que compararon los betamiméticos con otros betamiméticos, placebo o ningún tratamiento.
Obtención y análisis de los datos
Dos revisores de forma independiente evaluaron el riesgo de sesgo y extrajeron los datos.
Resultados principales
Veintiocho ensayos se consideraron elegibles para inclusión en la revisión, pero ocho no informaron datos de resultados relevantes para la revisión. Los resultados se basan en los 20 ensayos que aportaron datos.
Doce ensayos con 1367 pacientes compararon betamiméticos con placebo. Los betamiméticos redujeron el número de pacientes en trabajo de parto prematuro que tuvieron un parto en el transcurso de 48 horas (cociente de riesgos [CR] promedio 0,68; intervalo de confianza [IC] del 95%: 0,53 a 0,88; diez ensayos, 1209 pacientes). Hubo una disminución en el número de partos en el transcurso de siete días (CR promedio 0,80; IC del 95%: 0,65 a 0,98; cinco ensayos, 911 pacientes) pero no hubo pruebas de una reducción en el parto prematuro (antes de las 37 semanas de gestación) (CR 0,95; IC del 95%: 0,88 a 1,03; diez ensayos, 1212 pacientes). No se demostraron efectos beneficiosos de los betamiméticos en la muerte perinatal (CR 0,84; IC del 95%: 0,46 a 1,55; 11 ensayos, 1332 neonatos), o la muerte neonatal (CR 0,90; IC del 95%: 0,27 a 3,00; seis ensayos, 1174 neonatos). No se demostraron efectos significativos en el síndrome de dificultad respiratoria (CR 0,87; IC del 95%: 0,71 a 1,08; ocho ensayos, 1239 neonatos). Algunos ensayos informaron sobre parálisis cerebral, mortalidad infantil y enterocolitis necrosante; no se identificaron diferencias significativas entre los grupos en ninguno de estos resultados. Los betamiméticos se asociaron de manera significativa con los siguientes resultados: retiro del tratamiento debido a efectos adversos; dolor torácico materno; disnea; palpitación; temblor; cefaleas; hipopotasemia; hiperglucemia; náuseas o vómitos; congestión nasal; y taquicardia fetal.
Nueve ensayos compararon diferentes tipos de betamiméticos. En cinco ensayos otros betamiméticos se compararon con ritodrina (n = 948). Otras comparaciones se examinaron en ensayos individuales: hexoprenalina comparada con salbutamol (n = 140), salbutamol de liberación lenta versus moderada (n = 52) y salbutamol comparado con terbutalina (n = 200). Los ensayos fueron pequeños, variados y no tuvieron calidad suficiente para delinear algún patrón consistente del efecto.
Conclusiones de los autores
Los betamiméticos ayudan a retrasar el parto, lo que puede proporcionar un tiempo que permita remitir a las pacientes a la atención terciaria o completar un ciclo de corticosteroides prenatales. Sin embargo, se deben considerar los efectos adversos múltiples. Los datos son demasiado escasos para apoyar la administración de cualquier betamimético en particular.
PICO
Resumen en términos sencillos
Betamiméticos para la inhibición del trabajo de parto prematuro
El trabajo de parto prematuro es cuando las pacientes comienzan el trabajo de parto antes de las 37 semanas de gestación. Los neonatos nacidos antes del término (nacimiento prematuro) tienen resultados más deficientes en comparación con los neonatos nacidos a término. Cuanto más temprano se produzca el nacimiento, más deficiente es el resultado. La mayoría de los partos prematuros ocurre en los países de bajos ingresos, donde se dispone de menos ayuda médica. El parto prematuro es una causa principal de mortalidad infantil y enfermedad grave en todo el mundo. El parto prematuro puede provocar síndrome de dificultad respiratoria y enfermedad pulmonar crónica, hemorragia en los espacios con líquido (ventrículos) dentro del cerebro (hemorragia intraventricular), infección generalizada o infección de la sangre (sepsis), parálisis cerebral y otras discapacidades del neurodesarrollo. Incluso retrasos cortos en el parto prematuro pueden permitir que las pacientes reciban atención especializada y se les administren fármacos "corticosteroides" antes del parto para mejorar la función pulmonar de los neonatos.
En ensayos controlados aleatorios se evaluaron los efectos beneficiosos de administrar betamiméticos (fármacos que inhiben las contracciones del útero) a las pacientes con trabajo de parto prematuro contra cualquier efecto adverso. Los betamiméticos se administraron por cualquier vía o a cualquier dosis y se compararon con placebo, ningún tratamiento u otros betamiméticos. Veinte ensayos que probaron el efecto de los betamiméticos para inhibir el trabajo de parto prematuro contribuyeron con datos. Los ensayos se publicaron durante un período de 44 años entre 1966 y 2010 y se realizaron en la atención terciaria o en hospitales universitarios en países de ingresos altos.
En los 12 ensayos que compararon un betamimético con placebo o ningún tratamiento participaron 1367 pacientes en trabajo de parto prematuro. Los betamiméticos redujeron el número de pacientes que tuvieron un parto en el transcurso de 48 horas y hubo una disminución en el número de partos en el transcurso de siete días.
El retraso en el momento del parto no se tradujo en cualquier mejoría en los resultados neonatales, pero la mayoría de las pacientes de los ensayos tenía 32 semanas o más de gestación. Los betamiméticos no mostraron reducir las muertes perinatales o el síndrome de dificultad respiratoria.
Los efectos secundarios en las pacientes fueron considerables. Estos efectos provocaron la interrupción del tratamiento y síntomas como palpitaciones, dolor torácico, cefalea, dificultad respiratoria, náuseas o vómitos.
A partir de los ensayos incluidos no hubo pruebas suficientes para indicar que un agente betamimético fue superior a otro.
Authors' conclusions
Background
Preterm birth is defined as birth occurring before 37 completed weeks of pregnancy (WHO 1977). Of the four million estimated neonatal deaths in the world each year, 99% occur in low‐income countries and around one‐third are directly attributable to premature (preterm) birth (Lawn 2005). Preterm birth is thus the leading cause of neonatal death (Liu 2012). There is considerable regional variation in the incidence of preterm birth; 6.2% in Europe, 10.6% in the US and higher rates in Africa (Beck 2010; Blencowe 2012). Accurate assessment of gestational age is challenging in low‐income countries but accurate ultrasound‐based assessments in Malawi found an incidence as high as 17% (van den Broek 2009). Preterm birth is also a leading cause of perinatal morbidity and of morbidities that persist into childhood. Preterm birth can cause respiratory distress syndrome, bronchopulmonary dysplasia (a chronic lung disease, which can follow respiratory distress syndrome), intraventricular haemorrhage (bleeding into the fluid spaces (ventricles) within the brain), sepsis (generalised infection or infection of the blood stream), cerebral palsy and other forms of neuro‐developmental impairment (Gladstone 2011), blindness and deafness. Preterm infants born in high‐income settings often require intensive care, which is costly (Petrou 2001) and stressful. Intensive care is largely unavailable in those parts of the world with the greatest burden of preterm births, namely Africa and South Asia.
The mechanisms or pathogenesis of preterm labour are not well understood. The causes of spontaneous preterm labour may involve genetic factors, stress, inflammatory response, infection, mechanical factors and haemorrhage (Goldenberg 2008). Antenatal strategies to try to prevent preterm birth have been largely disappointing, and the rate of preterm birth has not decreased (Chang 2013).
Tocolytic drugs (drugs that inhibit contractions of the uterus) have been used to try to prolong pregnancy when preterm labour is diagnosed. Theoretically, tocolysis could improve perinatal outcomes by (a) allowing the fetus to mature further in utero before being born, (b) enhancing lung maturation in the fetus by giving corticosteroid treatment to the mother (Roberts 2006), and (c) allowing time for in‐utero transfer to a tertiary care centre with better facilities for care of the premature newborn, including neonatal intensive care facilities.
Betamimetics (isoxsuprine, hexoprenaline, orciprenaline, ritodrine, terbutaline, and salbutamol) have been used extensively in the past. Beta‐adrenergic agonists activate adenyl cyclase to form cyclic adenosine 3',5' monophosphate (cAMP). The increased cellular levels of cAMP decrease myosin light‐chain kinase activity, both by phosphorylation of the myosin light‐chain kinase itself, and by reducing intracellular calcium through increasing calcium uptake by sarcoplasmic reticulum (Gabor 1982).
The ideal tocolytic agent is one which is effective in prolonging pregnancy but has no side effects for the woman or the baby. Betamimetics stimulate beta‐adrenergic receptors and may cause palpitations, tremor, nausea, vomiting, headaches, nervousness, anxiety, chest pain, shortness of breath, and a range of biochemical disturbances such as hyperglycaemia (high blood sugar level) and hypokalaemia (low serum potassium level). Moreover, pulmonary oedema (fluid accumulation in the lungs) may occur (Mabie 1983) and has even been associated with maternal death. The occurrence of side effects may necessitate some women stopping the medication. Betamimetics cross the placenta and may cause fetal tachycardia (increase fetal heart rate), and hypoglycaemia (low blood sugar level) and hyperinsulinism after birth. When considering whether or not to use tocolytic agents in preterm labour, consideration needs to be given to the risks and benefits for both mother and infant, including the side effects of any medication used.
Although the use of betamimetics to inhibit preterm labour has lost popularity in high‐income settings because of safety concerns, they are still used elsewhere, especially in resource‐poor countries. We aim to review the evidence for benefits and harms of betamimetics in this review. The use of betamimetics to try to reduce the risk of preterm birth in twin pregnancies (Yamasmit 2012) and as maintenance therapy after acute treatment of preterm labour (Dodd 2012) are addressed in other Cochrane reviews.
In addition to betamimetics, several alternative tocolytic agents (that use different physiological mechanisms to inhibit labour) have been examined in trials and used in clinical practice. These include calcium channel blockers, cyclo‐oxygenase (COX) inhibitors (prostaglandin inhibitors), magnesium sulphate, nitric oxide donors, progestational agents, relaxin and oxytocin receptor antagonists. The effectiveness and side effects of these agents have been examined in other Cochrane reviews (Bain 2013; Crowther 2002; Duckitt 2002; King 2003; King 2005; Nardin 2006; Papatsonis 2005; Su 2010), and their relative effects have been explored in a recent network meta‐analysis (Haas 2012).
Objectives
To assess the effects of betamimetics in the treatment of preterm labour.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (including cluster‐randomised trials) comparing outcomes for women and infants in which betamimetics were used, by any route or any dose, to inhibit preterm labour with outcomes in controls with betamimetics, placebo or no treatment. We did not include trials where the method of allocation to groups was not truly random (e.g. allocation by day of the week).
Types of participants
Pregnant women assessed as being in spontaneous preterm labour and considered suitable for tocolytic agents.
For the purpose of the review, preterm labour was defined by trial authors (with intact or ruptured membranes) unless they contradicted the gestational age criterion.
Types of interventions
Betamimetics, administered by any route or any dose, in the treatment of women in preterm labour where betamimetics were compared with other betamimetics, placebo or no treatment.
Types of outcome measures
Primary outcomes
Primary outcomes were chosen as being most representative of the clinically important measures of effectiveness.
-
Birth within 48 hours of treatment.
-
Perinatal death (at seven days).
-
Respiratory distress syndrome.
-
Chronic lung disease or bronchopulmonary dysplasia as defined by oxygen dependency at 28 days or 36 weeks postmenstrual age, or both.
-
Severe neuroradiological abnormality, for example, cystic periventricular leukomalacia (softening of the brain near the ventricles because brain tissue in this area has died) or grade III to IV periventricular haemorrhage, or both.
-
Abnormal long‐term neurodevelopmental status at more than 12 months corrected age (defined as moderate to severe developmental delay and/or cerebral palsy, and/or sensory impairment, for example, blind and deaf).
-
Neonatal length of hospital stay.
Secondary outcomes
-
Time to birth (interval between randomisation and the birth):
-
birth within seven days;
-
birth before 28 completed weeks;
-
birth before 34 completed weeks;
-
birth before 37 completed weeks.
-
-
Adverse events:
-
cessation of treatment due to adverse drug reaction;
-
serious maternal outcomes, for example, maternal death, cardiac arrest, respiratory arrest, admission to intensive care unit;
-
maternal adverse drug reactions (all), for example, palpitation, tachycardia, cardiac arrhythmias, pulmonary oedema, myocardial ischaemia, chest pain, dyspnoea, tremor, hypotension, hyperglycaemia, hypokalaemia, nausea, vomiting, nasal stuffiness, headaches, nervousness, anxiety;
-
fetal and neonatal side effects (all), for example, hypoglycaemia, fetal tachycardia.
-
-
Neonatal morbidity:
-
neonatal sepsis;
-
necrotising enterocolitis (an inflammation causing injury to the bowel);
-
retinopathy of prematurity (abnormal growth of blood vessels in the baby's eye).
-
-
Neonatal death (at 28 days).
-
Infant death (at 12 months of age).
Search methods for identification of studies
Electronic searches
We searched the Cochrane Pregnancy and Childbirth Group's Trials Register by contacting the Trials Search Co‐ordinator (31 December 2013).
The Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Trials Search Co‐ordinator and contains trials identified from:
-
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
-
weekly searches of MEDLINE;
-
weekly searches of Embase;
-
handsearches of 30 journals and the proceedings of major conferences;
-
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL, MEDLINE and Embase, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service can be found in the ‘Specialized Register’ section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
Trials identified through the searching activities described above are each assigned to a review topic (or topics). The Trials Search Co‐ordinator searches the register for each review using the topic list rather than keywords.
Searching other resources
We scanned the reference lists of all articles found.
We did not apply any language restrictions.
Data collection and analysis
For the methods used when assessing the trials identified in the previous version of this review, seeAppendix 1.
For this update, we used the following methods when assessing the reports identified by the updated searches.
Selection of studies
Two review authors (T Dowswell (TD) and H West (HW)) independently assessed eligibility for inclusion for studies identified by the search strategy. We resolved any disagreement through discussion or, if required, we consulted the third author (J Neilson (JPN)).
Data extraction and management
We designed a form to extract data. For eligible studies, two review authors (TD and HW) extracted data independently using the agreed form. We resolved discrepancies through discussion or, if required, we consulted the third review author (JPN) We entered data into Review Manager software (RevMan 2012) and checked for accuracy.
When information regarding any of the above was unclear, we attempted to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Two review authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved any disagreement by discussion or by involving a third assessor.
(1) Sequence generation (checking for possible selection bias)
We have described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
-
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
-
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
-
unclear.
(2) Allocation concealment (checking for possible selection bias)
We have described for each included study the method used to conceal the allocation sequence and determined whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
-
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
-
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
-
unclear.
(3) Blinding (checking for possible performance and detection bias)
We have described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that studies were at low risk of bias if they were blinded, or if we judged that the lack of blinding could not have affected the results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods as:
-
high, low or unclear risk of bias for participants;
-
high, low or unclear risk of bias for personnel;
-
high, low or unclear risk of bias for outcome assessors.
(4) Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, protocol deviations)
We have described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We have stated whether attrition and exclusions were reported, the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or supplied by the trial authors, we re‐included missing data in the analyses. We assessed methods as:
-
low risk of bias;
-
high risk of bias;
-
unclear.
Studies where more than 20% of the participants were lost to follow‐up have been excluded. We also excluded outcomes where there was more than 20% missing data. We considered that serious sample attrition meant that studies were at high risk of bias and results would be difficult to interpret.
(5) Selective reporting bias
We have described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
-
low risk of bias (where it was clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
-
high risk of bias (where not all the study’s pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest were reported incompletely and so could not be used; study failed to include results of a key outcome that would have been expected to have been reported);
-
unclear.
(6) Other sources of bias
We have described for each included study any important concerns we had about other possible sources of bias, such as baseline imbalance.
We assessed whether each study was free of other problems that could put it at risk of bias:
-
high risk of other bias;
-
low risk of other bias;
-
unclear.
(7) Overall risk of bias
We made explicit judgements about whether studies are at high risk of bias, according to the criteria given in the Handbook (Higgins 2011). With reference to (1) to (6) above, we assessed the likely magnitude and direction of the bias and whether we considered it was likely to impact on the findings. We explored the impact of the level of bias through undertaking sensitivity analyses ‐ seeSensitivity analysis.
Measures of treatment effect
Dichotomous data
For dichotomous data, we have presented results as summary risk ratio with 95% confidence intervals.
Continuous data
For continuous data, we used the mean difference if outcomes were measured in the same way between trials. Where appropriate, we planned to use the standardised mean difference to combine trials that measured the same outcome, but used different methods.
Unit of analysis issues
Cluster‐randomised trials
None of the trials in this version of the review randomised clusters. In future updates if such trials are identified we will include them in the analyses along with individually‐randomised trials. We will adjust their sample sizes using the methods described in the Handbook (Higgins 2011) using an estimate of the intra‐cluster correlation co‐efficient (ICC) derived from the trial (if possible), from a similar trial or from a study of a similar population. If we use ICCs from other sources, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC. If we identify both cluster‐randomised trials and individually‐randomised trials, we plan to synthesise the relevant information. We will consider it reasonable to combine the results from both if there is little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomisation unit is considered to be unlikely.
We will also acknowledge heterogeneity in the randomisation unit and perform subgroup analysis to investigate the effects of the randomisation unit.
Cross‐over trials
We have not included cross‐over trials; this type of study design was not considered suitable for this type of intervention.
Other unit of analysis issues
Where appropriate, in multi‐arm trials with more than one arm examining the same betamimetic (e.g. different doses), we combined results for the betamimetics group to form a single pair‐wise comparison.
If we had identified any multi‐arm studies where two different betamimetics were compared with a control group (placebo or no treatment), we planned to divide the control group between the two experimental arms (dividing control event rate and sample size by two for dichotomous outcomes, and dividing the sample size by two and assuming the same mean and standard deviation for continuous outcomes). No such trials were identified for inclusion in this version of the review.
Dealing with missing data
For included studies, we noted levels of attrition. We explored the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using sensitivity analysis.
For all outcomes, we carried out analyses, as far as possible, on an intention‐to‐treat basis, i.e. we attempted to include all participants randomised to each group in the analyses, and all participants were analysed in the group to which they were allocated, regardless of whether or not they received the allocated intervention. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta‐analysis using the Tau2, I2 and Chi2 statistics. We regarded heterogeneity as substantial if a Tau2 was greater than zero and either an I2 was greater than 30% or there was a low P value (less than 0.10) in the Chi2 test for heterogeneity.
Assessment of reporting biases
Where there were 10 or more studies in the meta‐analysis, we investigated reporting biases (such as publication bias) using funnel plots. We assessed funnel plot asymmetry visually, and if there was any obvious asymmetry identified we planned to use formal tests for funnel plot asymmetry (Higgins 2011).
Data synthesis
We carried out statistical analysis using the Review Manager software (RevMan 2012). We used fixed‐effect meta‐analysis for combining data where it was reasonable to assume that studies were estimating the same underlying treatment effect: i.e. where trials examined the same intervention, and the trials’ populations and methods were judged sufficiently similar. If there was clinical heterogeneity sufficient to expect that the underlying treatment effects differed between trials, or if substantial statistical heterogeneity was detected, we used random‐effects meta‐analysis to produce an overall summary, if an average treatment effect across trials was considered clinically meaningful. The random‐effects summary was treated as the average range of possible treatment effects and we have discussed the clinical implications of treatment effects differing between trials. If the average treatment effect was not considered clinically meaningful, we did not combine trials.
For random‐effects analyses, the results are presented as the average treatment effect with its 95% confidence interval, and the estimates of Tau2 and I2.
Subgroup analysis and investigation of heterogeneity
We planned to carry out subgroup analysis of trials where antenatal corticosteroids were given routinely to see if this had any impact on the treatment effect.
Studies that explicitly stated that both the intervention and control participants received corticosteroids concurrently with the betamimetics, placebo or no treatment compared with studies that did not mention the use of steroids routinely or where steroid administration rate was reported as 50% or less.
Subgroup analysis was restricted to the review’s primary outcomes.
We planned to assess differences between subgroups by interaction tests available in RevMan.
Sensitivity analysis
For primary outcomes we carried out sensitivity analysis by risk of bias, temporarily excluding trials with unclear or high risk of bias for allocation concealment from the analysis to examine the impact on results.
Results
Description of studies
One hundred and five reports were identified by the search strategy, equating to 93 separate studies (some trials resulted in multiple publications). Of these 93 studies, 28 were eligible for inclusion, although findings are based on 20 trials which contributed data. Eight trials that were otherwise eligible for inclusion did not report outcomes relevant to the review, and did not contribute data. Further information on these trials is set out in Characteristics of included studies tables but they are not otherwise discussed in the results below (Kovacs 1987; Kullander 1985; Pasargiklian 1983; Penney 1980; Philipsen 1981; Spellacy 1974; Spellacy 1978; Thoulon 1982).
Sixty‐four trials were excluded and one is awaiting classification pending further information from the trial authors.
Excluded studies
Trials were excluded for the following reasons: method of generation of allocation was not truly randomised or inadequate (Calder 1985; Caritis 1991; Castillo 1988; Castren 1975; Chhabra 1998; Csapo 1977; Das 1969; Gonik 1988; Gummerus 1981; Karlsson 1980; Kim 1983; Kosasa 1985; Lenz 1985; Park 1982; Ritcher 1975; Ryden 1977; Sciscione 1993; Sirohiwal 2001; Sivasamboo 1972; Spatling 1989; Weisbach 1986; Zeller 1986); it was not clear that all participants were in preterm labour (Dunlop 1986; Guinn 1997; Hallak 1992; Hallak 1993; Leake 1983; Levy 1985; Lipshitz 1976; Muller‐Holve 1987; Sanchez 1972; Tarnow‐Mordi 1988); the interventions were not consistent with the protocol (Ally 1992; Bedoya 1972; Besinger 1991; Bulgay‐Moerschel 2008; Caballero 1979; Cararach 2006; Dellenbach 1971; Ferguson 1987; Francioli 1988; Gamissans 1978; Gamissans 1982; Goel 2011; Hatjis 1987; Herzog 1995; Ieda 1991; Kanayama 1996; Katz 1983; Lyell 2005; Neri 2009; Raymajhi 2003; Reynolds 1978; Rios‐Anez 2001; Ritcher 1979; Ross 1983; Trabelsi 2008); some of the comparisons examined in these trials are examined in other Cochrane reviews. Loss to follow‐up exceeded 20% in one study (Beall 1985), and one paper reported results from a series of trials which were reported individually in included studies (Merkatz 1980).
In addition, some studies, which were included in the previous versions of the review, were excluded from this updated version due to several reasons: loss to follow‐up 20% or more (Garite 1987; Howard 1982; Larsen 1986); conducted in preterm premature rupture of membranes without preterm labour (Christensen 1980); and data were reported by episode of preterm labour (Wesselius‐De 1971).
Please see table of Characteristics of excluded studies for further details.
Included studies
Twenty randomised controlled trials examining the effect of betamimetics for inhibiting preterm labour contributed data to the review.
A total of 1367 women participated in the 12 included trials comparing betamimetics with placebo or no treatment (Adam 1966; Barden 1980; Cotton 1984; CPLG 1992; Hobel 1980; Ingemarsson 1976; Larsen 1980; Leveno 1986; Mariona 1980; Scommegna 1980; Spellacy 1979; Tohoku 1984). Data for four trials (Barden 1980; Hobel 1980; Mariona 1980; Scommegna 1980) were included in a previous version of the review (King 1988) and were extracted from personal communications from trial authors.
A further 948 women participated in the five trials of comparing other betamimetics with ritodrine (Caritis 1984; Essed 1978; Holleboom 1996; Lipshitz 1988; Von Oeyen 1990); in two of these trials results were reported in brief abstracts only (Lipshitz 1988; Von Oeyen 1990).
One trial with 140 women compared hexoprenaline and salbutamol (Gummerus 1983), Motazedian 2010 compared terbutaline with salbutamol in a trial with 200 women, and Crepin 1989 (60 women) examined slow versus normal release salbutamol.
(1) Study location and settings
Trials were published over a 44‐year period between 1966 (Adam 1966) and 2010 (Motazedian 2010). Included studies were conducted in tertiary care or University hospitals in high‐income settings: trials were conducted in the USA (Barden 1980; Caritis 1984; Cotton 1984; Hobel 1980; Leveno 1986; Lipshitz 1988; Mariona 1980; Scommegna 1980; Spellacy 1979; Von Oeyen 1990), Europe (Crepin 1989; Essed 1978; Gummerus 1983; Holleboom 1996; Ingemarsson 1976; Larsen 1980), Australia (Adam 1966), Canada (CPLG 1992), Iran (Motazedian 2010) and Japan (Tohoku 1984). Eight trials were multicentre studies.
(2) Participants
The participants included in these trials were reasonably homogeneous. The gestational age at inclusion ranged from 20 to up to 37 weeks. Preterm labour was reasonably consistently defined across the trials as the presence of uterine contractions documented by external tocography or cervical dilatation up to 4 to 5 cm, or both, except for three trials, which did not state the definition (Gummerus 1983; Lipshitz 1988; Von Oeyen 1990). Three trials included women admitted for preterm labour with preterm premature rupture of membranes (Caritis 1984; Cotton 1984; CPLG 1992) and three trials included twins (Adam 1966; Cotton 1984; CPLG 1992). Four trials did not state the exclusion criteria (Essed 1978; Gummerus 1983; Lipshitz 1988; Von Oeyen 1990). Most trials excluded those women with chorioamnionitis, pregnancy‐induced hypertension, vaginal bleeding, intrauterine compromise or fetal death, and contraindications to betamimetics.
(3) Interventions
Nine trials compared ritodrine with placebo (Barden 1980; CPLG 1992; Hobel 1980; Larsen 1980; Leveno 1986; Mariona 1980; Scommegna 1980; Spellacy 1979, Tohoku 1984). Intravenous ritodrine was used initially and maintained orally in all trials except one (Larsen 1980), which used intramuscular ritodrine initially. The dosage was consistent both intravenously and orally. Ritodrine was usually started at 100 mcg/minute and increased by 50 mcg/minute up to a maximum of 350 mcg/minute, or until contractions ceased, or there were intolerable adverse effects. Two trials compared terbutaline with placebo (Cotton 1984; Ingemarsson 1976); the same regimen for intravenous infusion was used but oral terbutaline was only given in one trial (Ingemarsson 1976). One trial compared isoxsuprine with placebo (Adam 1966). Two trials compared terbutaline with ritodrine (Caritis 1984; Von Oeyen 1990). Only one trial compared other betamimetics with ritodrine: fenoterol with ritodrine (Essed 1978); ritodrine loading dose with incremental dose (Holleboom 1996); and hexoprenaline with ritodrine (Lipshitz 1988). An additional study compared hexoprenaline with salbutamol (Gummerus 1983) while Motazedian 2010 compared terbutaline with salbutamol, and Crepin 1989 compared slow with normal release salbutamol.
(4) Outcomes
There was some inconsistency across the trials with regards to the way in which outcomes were reported. Only three common primary outcomes were consistently reported: birth within 48 hours, perinatal death, and respiratory distress syndrome. However, the definition of respiratory distress syndrome was not stated. Only the biggest trial reported neonatal outcomes both in the short‐ and long‐term (CPLG 1992). Secondary outcomes were less consistently reported and definitions were not stated. Mainly cardiovascular adverse effects from betamimetics were reported, particularly when treatment was stopped due to adverse reactions. Other adverse effects were less consistently reported.
Please see tables of Characteristics of included studies for further details.
Risk of bias in included studies
Summaries of 'Risk of bias' assessments for individual included studies, and for all studies are set out in Figure 1 and Figure 2.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
The method of generating the randomisation sequence was not described or was not clear in eight of these studies; 12 studies were assessed to be at low risk of bias for sequence generation. In these studies the sequence was determined by random number tables, by computer, or by an external randomisation service (Barden 1980; Caritis 1984; CPLG 1992; Hobel 1980; Kovacs 1987; Leveno 1986; Mariona 1980; Motazedian 2010; Scommegna 1980; Spellacy 1978; Spellacy 1979; Tohoku 1984).
Seven of the included trials reported adequate concealment of allocation (Caritis 1984; CPLG 1992; Holleboom 1996; Ingemarsson 1976; Leveno 1986; Motazedian 2010; Tohoku 1984). The method of concealment of allocation was unclear in the remaining trials (Adam 1966; Barden 1980; Cotton 1984; Crepin 1989; Essed 1978; Gummerus 1983; Hobel 1980; Kovacs 1987; Kullander 1985; Larsen 1980; Lipshitz 1988; Mariona 1980; Pasargiklian 1983; Penney 1980; Philipsen 1981; Scommegna 1980; Spellacy 1974; Spellacy 1978; Spellacy 1979; Thoulon 1982; Von Oeyen 1990). All these trials were conducted before 1990, the majority more than 25 years ago. More information on allocation of concealment could not be obtained from the authors. We decided to include these papers.
Blinding
Method of blinding (double‐blind and single‐bind) was reported in 15 trials (Adam 1966; Barden 1980; Caritis 1984; CPLG 1992; Crepin 1989; Hobel 1980; Ingemarsson 1976; Mariona 1980; Penney 1980; Philipsen 1981; Scommegna 1980; Spellacy 1974; Spellacy 1978; Spellacy 1979; Tohoku 1984), In some trials women were described as blinded, but it is unlikely that staff would have been unaware of treatment allocation as regimens in different arms of trials were not identical; other trials did not discuss blinding at all.
Incomplete outcome data
In this review, we have attempted to conduct an intention‐to‐treat analysis for all outcomes. All or most participants in 15 trials completed the study and most participants were accounted for in the analysis (Barden 1980; Caritis 1984; Cotton 1984; CPLG 1992; Hobel 1980; Holleboom 1996; Ingemarsson 1976; Leveno 1986; Mariona 1980; Motazedian 2010; Pasargiklian 1983; Philipsen 1981; Scommegna 1980; Spellacy 1979; Tohoku 1984). In two trials attrition may have related to treatment group and these trials were judged to be at high risk of bias for this domain (Crepin 1989; Essed 1978). In the remaining trials loss to follow‐up was not mentioned or not clear.
Selective reporting
Assessing selective reporting bias without access to trial protocols is difficult, and most studies were assessed as unclear. In the study by Motazedian 2010, outcomes for infants were only reported for those born after 37 weeks' gestation; data for infant outcomes were therefore at high risk of bias and have not been included in the data and analysis tables in the review.
Other potential sources of bias
In two studies there appeared to be baseline differences between groups (CPLG 1992; Essed 1978), and in one study there was considerable deviation from the protocol (Holleboom 1996).
Effects of interventions
1. Betamimetics compared with placebo (comparison 1)
Twelve trials compared betamimetics with placebo; trials included a total of 732 women in placebo groups and 635 women in betamimetics group. One trial (Larsen 1980) randomised the participants into four groups: long ritodrine infusion group, short ritodrine infusion group, intramuscular group and placebo. Data from all women on ritodrine regimens (three groups) were pooled together to compare with placebo‐treated women.
Primary outcomes
Birth within 48 hours of treatment
The use of betamimetics significantly decreased the number of women giving birth within 48 hours (average risk ratio (RR) 0.68; 95% confidence interval (CI) 0.53 to 0.88, 10 trials, 1209 women) (Analysis 1.1). There was moderate heterogeneity for this outcome (I2 = 32%) and we used a random‐effects model. The effect of betamimetics on reduction of birth within 48 hours was not changed after sensitivity analysis, retaining only studies with adequate allocation concealment (CPLG 1992; Ingemarsson 1976; Leveno 1986) (average RR 0.55; 95% CI 0.38 to 0.80) (data not shown). There was no obvious funnel plot asymmetry for this outcome (Figure 3).

Funnel plot of comparison: 1 All betamimetics versus placebo, outcome: 1.1 Birth within 48 hours of treatment.
Perinatal death (up to seven days) and serious neonatal morbidity
Betamimetics were not shown to reduce perinatal deaths (RR 0.84; 95% CI 0.46 to 1.55, 11 trials, 1332 infants) (Analysis 1.2), respiratory distress syndrome (RR 0.87; 95% CI 0.71 to 1.08, eight trials, 1239 infants) (Analysis 1.3), or cerebral palsy (RR 0.19; 95% CI 0.02 to 1.63, one trial, 246 infants) (Analysis 1.4), Differences between groups remained non‐significant when we carried out sensitivity analysis retaining only those studies at low risk of bias for allocation concealment (data not shown).Visual assessment suggested no obvious funnel plot asymmetry for perinatal death (Figure 4).

Funnel plot of comparison: 1 All betamimetics versus placebo, outcome: 1.2 Perinatal death (7 days).
Neonatal length of hospital stay
Only one trial reported the mean neonatal length of hospital stay (Leveno 1986) with the total length of hospital stay being 24.5 days in the ritodrine group and 24.8 days in the placebo group. The mean neonatal length of intensive care stay was 14.3 days in the ritodrine group and 12.4 days in the placebo group. (Standard deviations were not provided in the trial report and data for these outcomes are not shown in data and analyses tables.)
Maternal secondary outcomes
Betamimetics decreased the frequency of birth within seven days (average RR 0.80; 95% CI 0.65 to 0.98, five trials, 911 women) (Analysis 1.5), but did not significantly reduce the risk of delivering prior to 37 weeks' gestation (RR 0.95; 95% CI 0.88 to 1.03, 10 trials, 1212 women) (Analysis 1.6).
No subgroup data based on birth before 28 and before 34 completed weeks were reported because most participants were 32 weeks' gestation or more.
No maternal deaths were reported in two trials that explicitly reported this (CPLG 1992; Larsen 1980). Other serious maternal outcomes, for example, cardiac arrest, respiratory arrest and admission to intensive care unit, were not reported in any trial. Maternal pulmonary oedema was reported in three trials; only one case was identified (Cotton 1984; CPLG 1992; Leveno 1986) (RR 3.03; 95% CI 0.12 to 74.23) (Analysis 1.8). There were no significant differences between groups for maternal cardiac arrhythmias (RR 3.54; 95% CI 0.74 to 16.92, one trial, 708 women) (Analysis 1.9); myocardial ischaemia (RR 12.53; 95% CI 0.72 to 216.91, one trial, 106 women) (Analysis 1.10), or maternal hypotension (average RR 1.56; 95% 0.12 to 20.86, two trials, 136 women) (Analysis 1.11).
The frequency of other maternal adverse effects varied in different trials but overall, were significantly increased with betamimetics compared to placebo: cessation of treatment due to adverse drug reaction (RR 11.38; 95% CI 5.21 to 24.86, five trials, 1081 women) (Analysis 1.12); chest pain (RR 11.29; 95% CI 3.81 to 33.46, two trials, 814 women) (Analysis 1.15); dyspnoea (RR 3.86; 95% CI 2.21 to 6.77, two trials, 814 women) (Analysis 1.16); palpitation (RR 9.91; 95% CI 6.46 to 15.20, five trials, 1089 women) (Analysis 1.13); tremor (RR 10.74; 95% CI 6.20 to 18.59, one trial 708 women) (Analysis 1.17); headaches (RR 4.07; 95% CI 2.60 to 6.35, three trials, 936 women) (Analysis 1.22); hypokalaemia (RR 6.07; 95% CI 4.00 to 9.20, one trial, 708 women) (Analysis 1.19); hyperglycaemia (RR 2.90; 95% CI 2.05 to 4.09, one trial, 708 women) (Analysis 1.18); nausea or vomiting (RR 1.76; 95% CI 1.29 to 2.42, three trials, 932 women) (Analysis 1.20); and nasal stuffiness (RR 2.90; 95% CI 1.64 to 5.12, one trial, 708 women) (Analysis 1.21). Two trials reported tachycardia; in one trial there was a significant difference between groups, while in the second trial, similar numbers of women in both groups reported this side effect and we have not pooled results for this outcome (Analysis 1.14).
Neonatal secondary outcomes
There were no statistically significant differences between groups for neonatal death (average RR 0.90; 95% CI 0.27 to 3.00, six trials, 1174 infants) (Analysis 1.23), infant death (RR 0.51; 95% CI 0.05 to 5.64, one trial, 750 women) (Analysis 1.24) and necrotising enterocolitis (RR 0.42; 95% CI 0.06 to 2.78, two trials, 149 infants) (Analysis 1.25). Significant heterogeneity was identified for two outcomes: sepsis and fetal hypoglycaemia, and results were not pooled for these outcomes (Analysis 1.26; Analysis 1.27).Fetal tachycardia associated with betamimetics was significantly increased compared with placebo in one trial with data for 30 infants (RR 2.40; 95% CI 1.12 to 5.13) (Ingemarsson 1976) (Analysis 1.28).
No data on chronic lung disease, bronchopulmonary dysplasia, severe neuroradiological abnormality, and retinopathy of prematurity were reported. Only one trial reported abnormal long‐term neurodevelopmental status after follow‐up of 246 infants at 18 months (CPLG 1992). There was no significant difference between groups on the Bayley Psychomotor Development Index (mean difference (MD) 1.30; 95% CI ‐2.74 to 5.34) (Analysis 1.29). The average score on the Bayley Mental Developmental Index was slightly higher in the ritodrine group (MD 5.20; 95% CI 0.56 to 9.84) (Analysis 1.30).
2. Other betamimetics compared with ritodrine
Terbutaline compared with ritodrine (comparison 2)
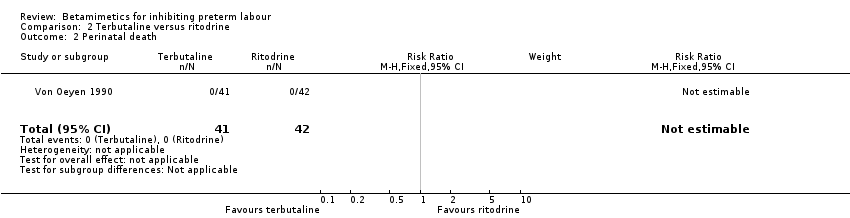
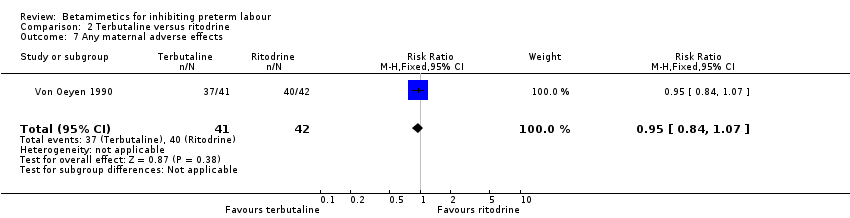
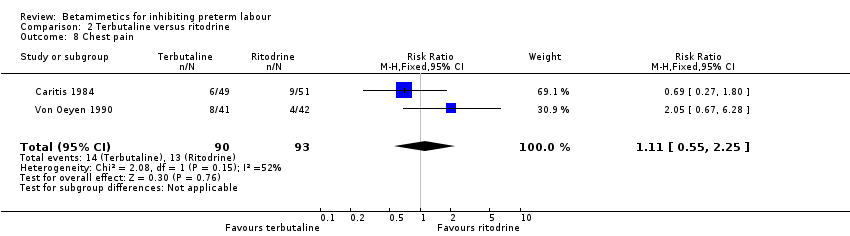
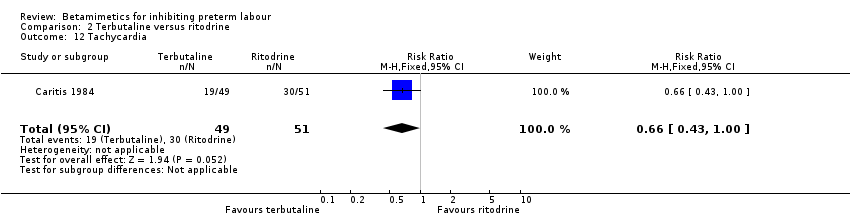
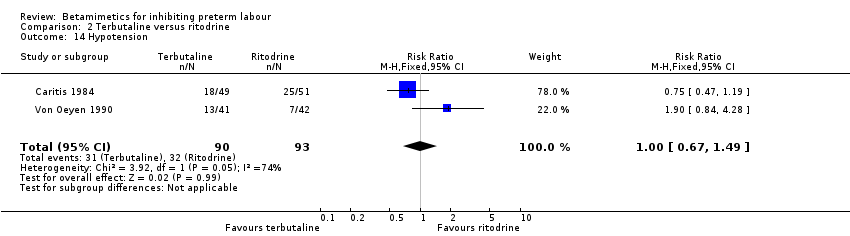
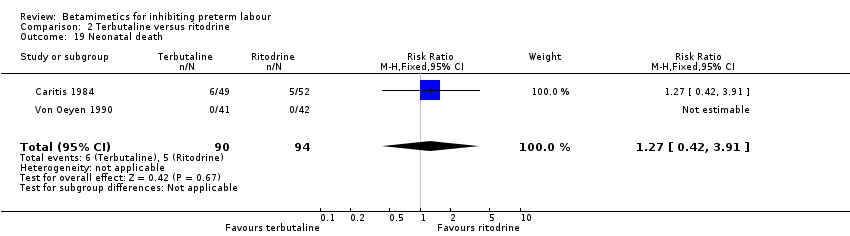
There were only two trials in this group involving 183 women: 90 in the terbutaline group and 93 in the ritodrine group (Caritis 1984; Von Oeyen 1990). Only 19 outcomes were reported.
Primary outcomes
Birth within 48 hours of treatment
There was no significant difference between terbutaline and ritodrine for the number of women giving birth within 48 hours in one trial with 83 women (RR 2.05; 95% confidence interval (CI) 0.77 to 5.48, one trial) (Analysis 2.1).
Perinatal death (up to seven days) and serious neonatal morbidity
There were no significant differences between the two betamimetics for perinatal deaths (no deaths in one trial with 83 infants) (Analysis 2.2) or respiratory distress syndrome (RR 1.99; 95% CI 0.93 to 4.27, one trial, 101 infants) (Analysis 2.3). Cerebral palsy was not reported.
Neonatal length of hospital stay
Length of hospital stay was not reported in either trial contributing data to this comparison.
Secondary outcomes
Most of our secondary maternal and infant outcomes were not reported.
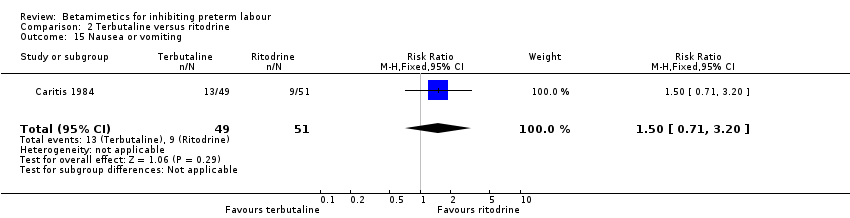
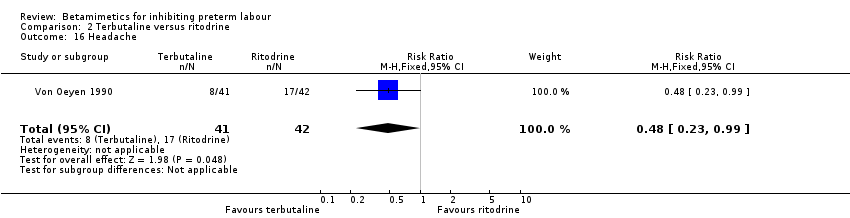
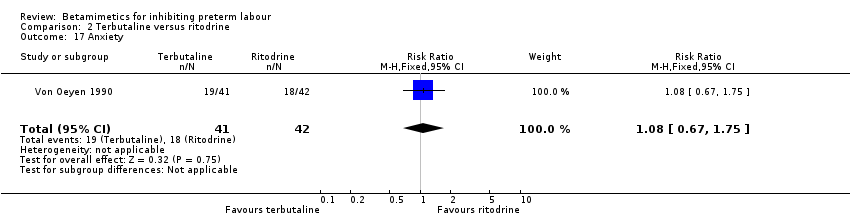
Hyperglycaemia was statistically significantly increased in the terbutaline group (RR 1.78; 95% CI 1.05 to 3.03) (Analysis 2.10). However, this outcome was reported in one trial with 100 women only (Caritis 1984). Other maternal and neonatal outcomes (measured in only one trial) were not statistically significantly different between the two groups: birth within seven days (RR 0.80; 95% CI 0.57 to 1.10) (Analysis 2.4); birth before 28 completed weeks (RR 2.08; 95% CI 0.55 to 7.87) (Analysis 2.5); or cessation of treatment due to adverse drug reactions (RR 0.83; 95% CI 0.24 to 2.92) (Analysis 2.6). Both trials reported chest pain, shortness of breath and hypotension; there were no significant differences between groups for any of these outcomes (RR 1.11; 95% CI 0.55 to 2.25; RR 0.83; 95% CI 0.41 to 1.67, and RR 1.00; 95% CI 0.67 to 1.49 respectively). Dyspnoea, arrhythmia, tachycardia, palpitation, and headache were reported in only one trial and there were no clear differences between terbutaline and ritodrine for these side effects.
Fenoterol compared with ritodrine (comparison 3)
There was only one trial in this group, involving 48 women in each group (Essed 1978). Only six outcomes were reported.
Maternal and neonatal outcomes
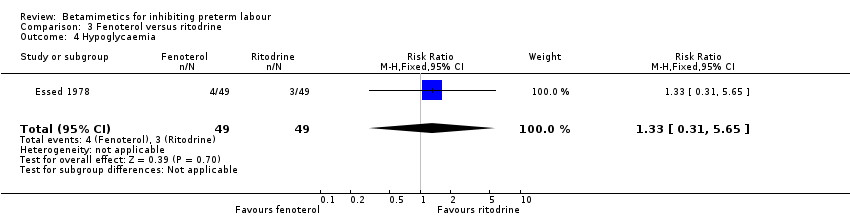
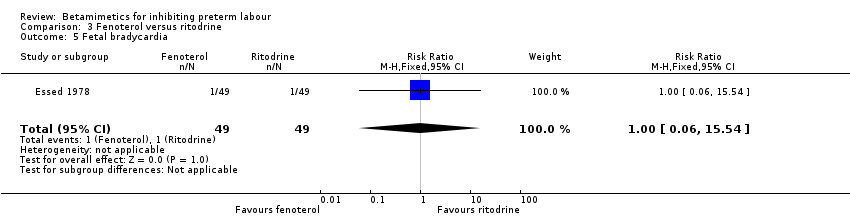
Neonatal death was statistically significantly decreased in the fenoterol group (RR 0.13; 95% CI 0.02 to 0.96) (Analysis 3.6). However, the sample size was small and the methodological quality of the single study reporting this outcome was poor. There were no statistically significant differences between the groups for other maternal and neonatal outcomes reported: perinatal death; respiratory distress syndrome; tachycardia; fetal bradycardia; and hypoglycaemia.
Ritodrine loading dose with conventional incremental dose (comparison 4)
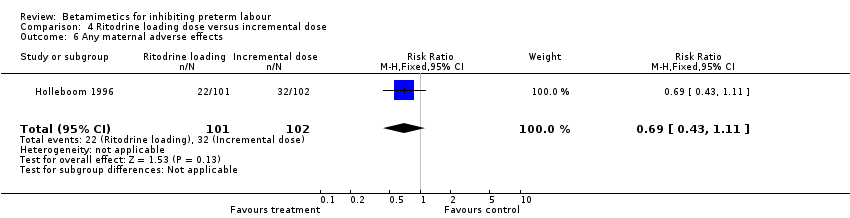
There was only one trial in this group involving 203 women: 101 in the ritodrine loading dose group and 102 in the incremental dose group (Holleboom 1996). Only 12 outcomes were reported.
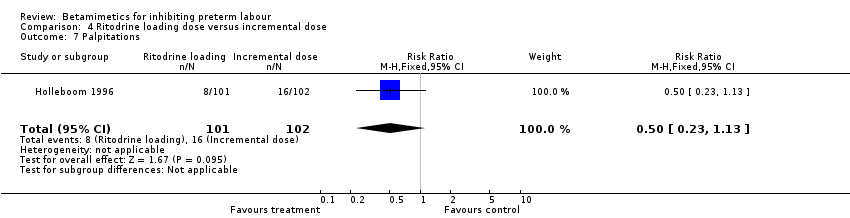
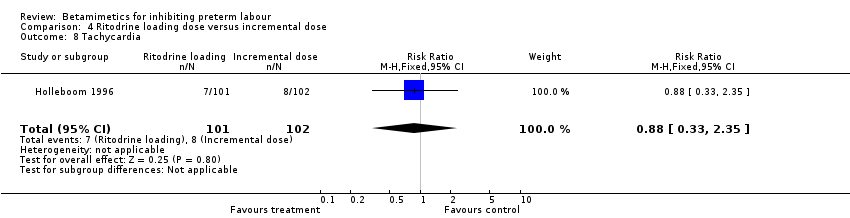
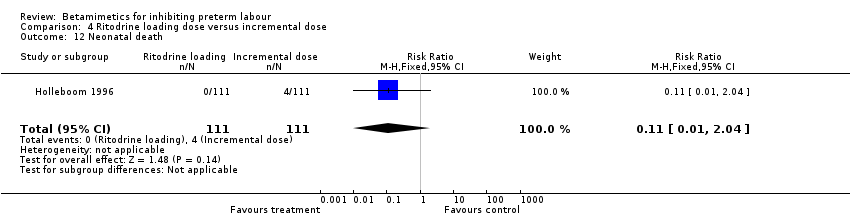
There were no statistically significant differences between the groups for maternal and neonatal outcomes: birth within 48 hours; birth before 34 completed weeks; birth before 37 completed weeks; respiratory distress syndrome; any maternal adverse effects; tachycardia; nausea or vomiting; palpitation; headache; neonatal death; periventricular haemorrhage grade three to four; and sepsis.
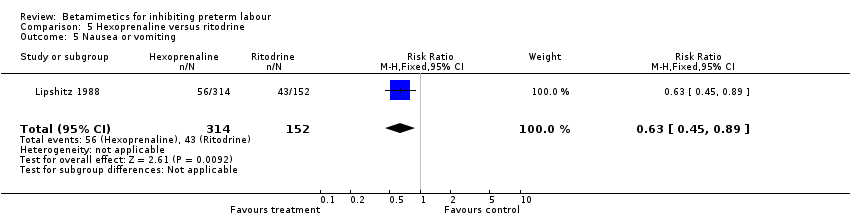
Hexoprenaline compared with ritodrine (comparison 5)
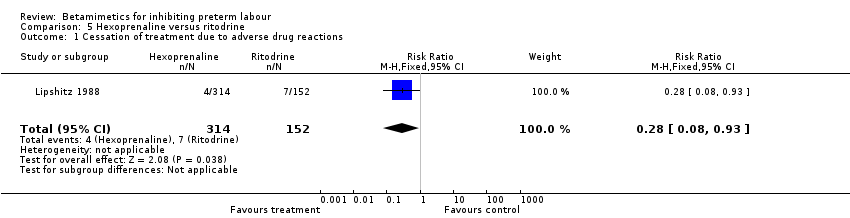
There was only one trial in this group involving 466 women: 314 in the hexoprenaline group and 152 in the ritodrine group (Lipshitz 1988). Only six outcomes were reported.
Maternal and neonatal adverse effects were statistically significantly decreased in the hexoprenaline group: cessation of treatment due to adverse reaction (RR 0.28; 95% CI 0.08 to 0.93) (Analysis 5.1); any maternal adverse effects (RR 0.83; 95% CI 0.76 to 0.91) (Analysis 5.2); nausea or vomiting (RR 0.63; 95% CI 0.45 to 0.89) (Analysis 5.5); palpitation (RR 0.75; 95% CI 0.60 to 0.94) (Analysis 5.3); hypotension (RR 0.77; 95% CI 0.61 to 0.96) (Analysis 5.4); increased fetal heart rate (RR 0.74; 95% CI 0.56 to 0.98) (Analysis 5.6). However, the quality of this trial was poor (abstract only).
Hexoprenaline compared with salbutamol (comparison 6)
There was only one trial in this group involving 140 women: 70 in the hexoprenaline group and 70 in the salbutamol group (Gummerus 1983). Only six outcomes were reported.
Maternal adverse effects were statistically significantly decreased in the hexoprenaline group: any maternal adverse effects (RR 0.38; 95% CI 0.18 to 0.80) ( Analysis 6.3) and tachycardia (RR 0.11; 95% CI 0.01 to 0.85) (Analysis 6.4). However, the methodological quality of this trial was poor. There were no statistically significant differences between the groups for respiratory distress syndrome, cessation of treatment due to adverse reactions, nausea or vomiting, headache, and tremor.
Subgroup analysis based on adjunctive steroid treatment was not done because of the low incidence of corticosteroid usage in all trials.
Terbutaline compared with salbutamol (comparison 7)
Only one trial with 200 women contributed data to this comparison (Motazedian 2010) and few of our primary and secondary outcomes were reported.
There was no significant difference between women receiving terbutaline and salbutamol for birth within 48 hours (RR 0.63; 95% CI 0.21 to 1.84).
Side effects were more likely in the salbutamol group. Women in the terbutaline group were at reduced risk of side effects overall (RR 0.54; 95% CI 0.42 to 0.70) (Analysis 7.2); and of tachycardia (RR 0.48; 95% CI 0.30 to 0.75) (Analysis 7.3); anxiety (RR 0.48; 95% CI 0.28 to 0.84) (Analysis 7.6); and chills (RR 0.48; 95% CI 0.34 to 0.69) (Analysis 7.7). There were no statistically significant differences between groups for dyspnoea (RR 0.42; 95% CI 0.15 to 1.14) (Analysis 7.4), nausea (RR 0.66; 95% CI 0.39 to 1.09) (Analysis 7.5), or oedema (RR 0.75; 95% CI 0.17 to 3.27) (Analysis 7.8).
The length of maternal hospital stay was reduced in the terbutaline group (MD ‐0.80 days; 95% CI ‐1.19 to ‐0.41) (Analysis 7.9).
Women who delivered during the treatment period, whose contractions did not cease within 48 hours, or who developed complications were not included in analysis for pregnancy outcomes or complications (44/200 – 22%) data for these outcomes have not been included in the review because of high risk of bias.
Comparison 8: Slow release salbutamol compared with normal release salbutamol
A single trial with data for 56 women was included in this comparison (Crepin 1989). None of our primary outcomes were reported.
For maternal secondary outcomes, there was no difference between the two types of salbutamol for preterm birth (before 37 weeks) (RR 2.57; 95% CI 0.29 to 23.13) (Analysis 8.1) or caesarean birth (RR 1.29; 95% CI 0.23 to 7.07) (Analysis 8.2). None of the women in either group had severe side effects leading to discontinuation of treatment, and there was no evidence of difference in the frequency of nausea (RR 0.86; 95% CI 0.06 to 12.98) (Analysis 8.4). For infant Apgar score, no infants (in either group) were reported to have a score less than seven at five minutes. Other outcomes were not reported.
Discussion
Summary of main results
Betamimetics were shown to be effective in delaying birth for 48 hours and up to seven days. This is sufficient time to allow transfer of a woman to a tertiary care unit or to complete a course of antenatal corticosteroid. However, there was no evidence that this delay in the timing of birth translated into any improvements in neonatal outcomes, and the side effects for the woman are considerable.
It may be that health gains have not been demonstrated for several reasons.
-
Time gain in‐utero: most participants were 32 weeks' gestation or more. Therefore, increased gestational age might have little or no effect on perinatal outcomes leading to no statistical significance in the pooled estimate of important outcomes such as respiratory distress syndrome, perinatal death, neonatal death and infant death. Also, prolongation of pregnancy itself may be disadvantage to the baby. If the eligibility criteria had been restricted to lower gestation groups, and had the number of participants been greater, an effect on clinical outcomes might have been detected.
-
Referral to higher care level: all trials in this review took place in tertiary care or University hospitals, that were likely to have neonatal intensive care facilities. If the trials had involved women who needed to be transferred to distant referral hospitals, again a difference in outcome might have been seen.
-
Antenatal corticosteroids administration: the majority of trials were conducted before 1990, when antenatal corticosteroids were not widely used. Even in CPLG 1992, antenatal corticosteroids were prescribed only to one third of all women in each arm. Therefore, subgroup analysis to evaluate the effect of betamimetics to allow a complete course of antenatal corticosteroids (betamimetics alone and betamimetics combined with corticosteroids) on neonatal outcomes could not be assessed.
There is not enough evidence to suggest that one betamimetic agent is superior to another.
Agreements and disagreements with other studies or reviews
Betamimetics have been used for primary tocolysis and maintenance therapy for many years, and continue to be used throughout the world. However, alternative agents have been shown to be more effective in terms of pregnancy prolongation and have been associated with fewer and less severe side effects compared with betamimetics. The effects of different classes of tocolytics compared with placebo, and with each other (where different types of tocolytics have been compared directly in trials) have been set out in a series of Cochrane Reviews (Bain 2013; Crowther 2002; Duckitt 2002; King 2003; King 2005; Papatsonis 2005; Su 2010), and the effects of combinations of different tocolytic drugs to treat preterm labour is the subject of a review currently in development (Nardin 2006). A recent review, which included both network and pair‐wise meta‐analysis, incorporated evidence from 95 trials examining a range of tocolytics (betamimetics, magnesium sulphate, calcium channel blockers, COX inhibitors, oxytocin receptor antagonists, nitric oxide donors and other drugs) (Haas 2012). The results of this review suggest that all types of tocolytics were better than placebo in terms of prolonging pregnancy beyond 48 hours, but that betamimetics performed less well than other types of tocolytics (e.g. COX inhibitors, and calcium channel blockers). It was not clear that any class of tocolytic was effective in reducing respiratory distress syndrome compared with placebo. The evidence regarding side effects suggested that COX inhibitors and oxytocin receptor antagonists were associated with fewer maternal side effects compared with other types of tocolytics including betamimetics.
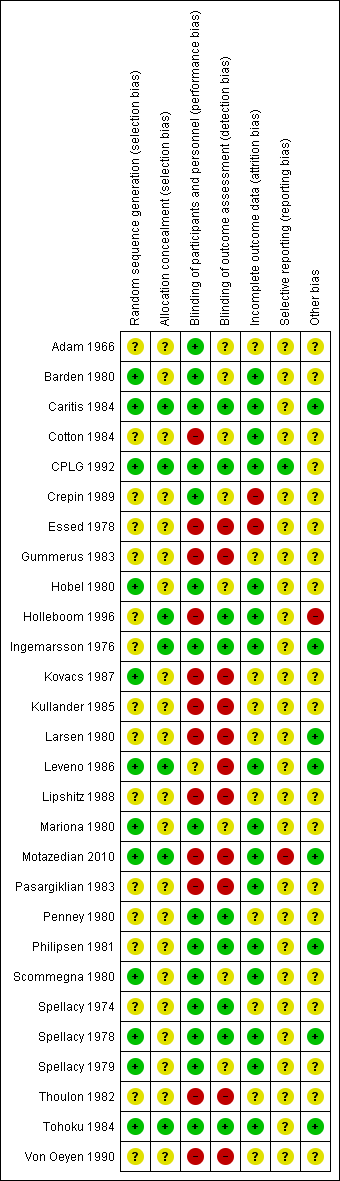
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
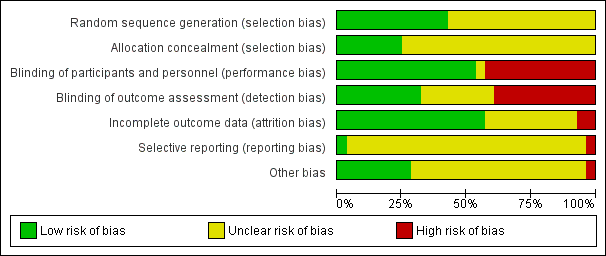
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
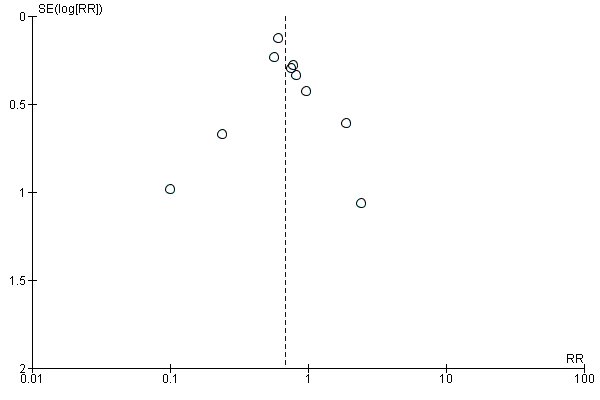
Funnel plot of comparison: 1 All betamimetics versus placebo, outcome: 1.1 Birth within 48 hours of treatment.

Funnel plot of comparison: 1 All betamimetics versus placebo, outcome: 1.2 Perinatal death (7 days).
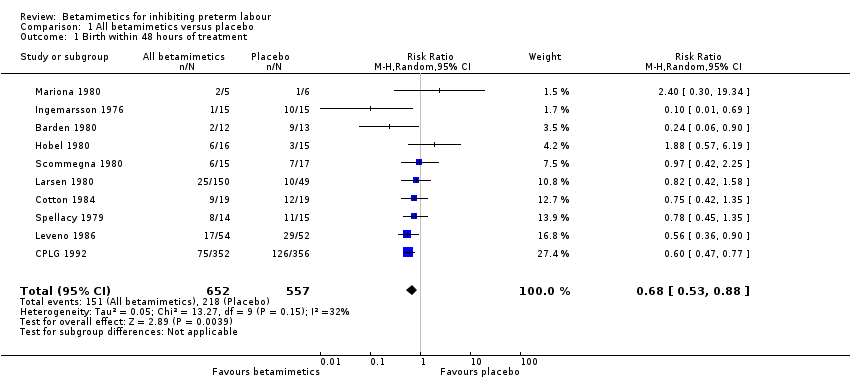
Comparison 1 All betamimetics versus placebo, Outcome 1 Birth within 48 hours of treatment.
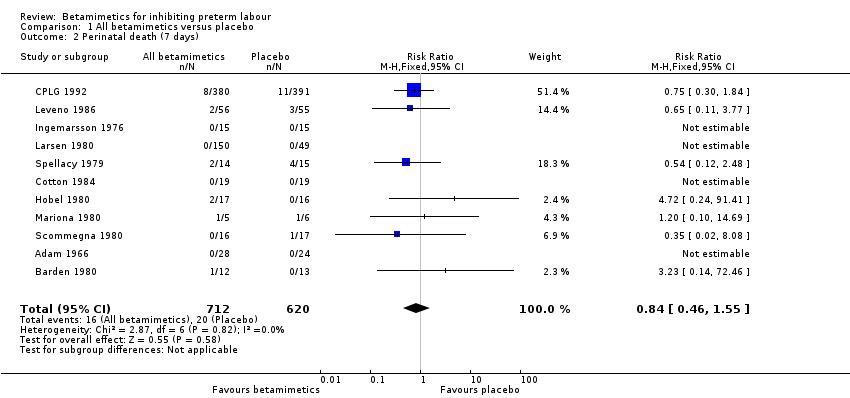
Comparison 1 All betamimetics versus placebo, Outcome 2 Perinatal death (7 days).
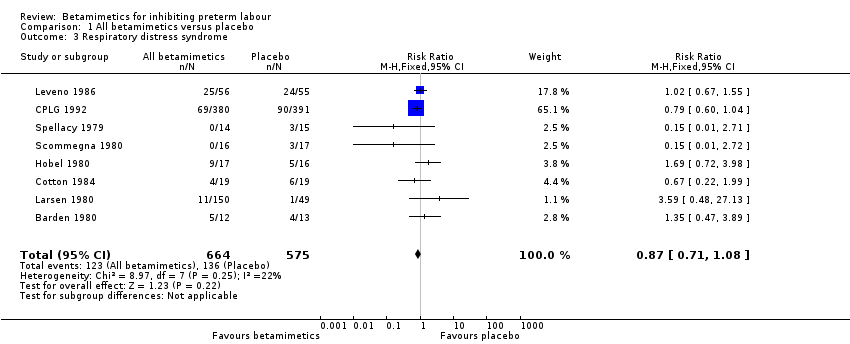
Comparison 1 All betamimetics versus placebo, Outcome 3 Respiratory distress syndrome.
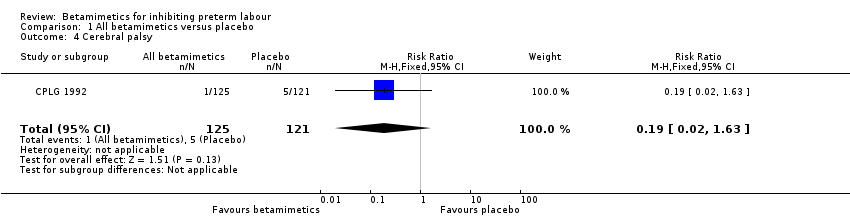
Comparison 1 All betamimetics versus placebo, Outcome 4 Cerebral palsy.

Comparison 1 All betamimetics versus placebo, Outcome 5 Birth within 7 days.

Comparison 1 All betamimetics versus placebo, Outcome 6 Birth less than 37 weeks' gestation.
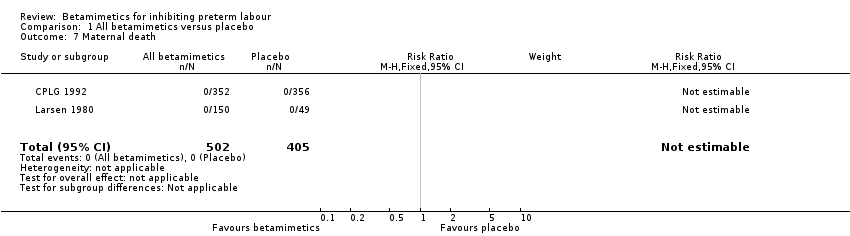
Comparison 1 All betamimetics versus placebo, Outcome 7 Maternal death.

Comparison 1 All betamimetics versus placebo, Outcome 8 Pulmonary oedema.
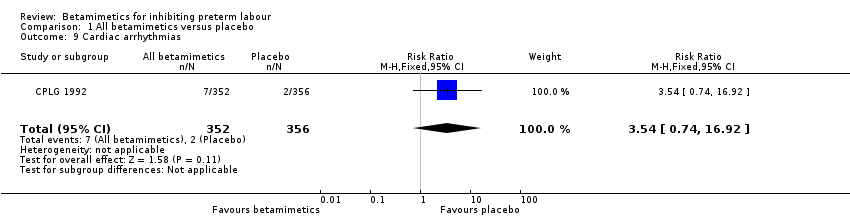
Comparison 1 All betamimetics versus placebo, Outcome 9 Cardiac arrhythmias.

Comparison 1 All betamimetics versus placebo, Outcome 10 Myocardial ischemia.
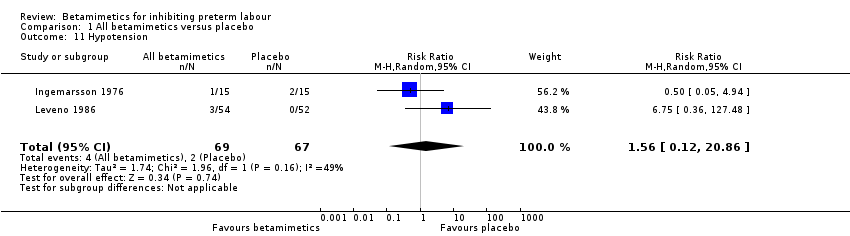
Comparison 1 All betamimetics versus placebo, Outcome 11 Hypotension.

Comparison 1 All betamimetics versus placebo, Outcome 12 Cessation of treatment due to adverse drug reaction.
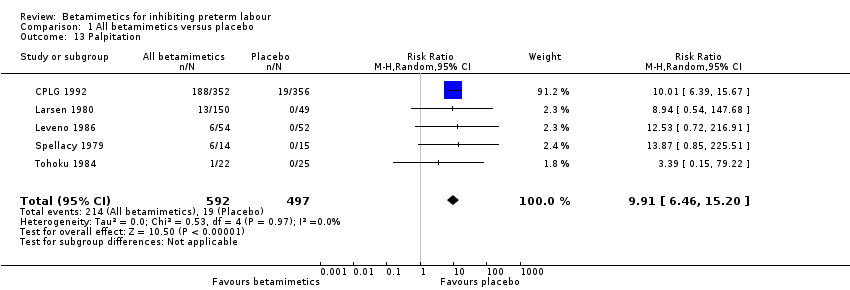
Comparison 1 All betamimetics versus placebo, Outcome 13 Palpitation.
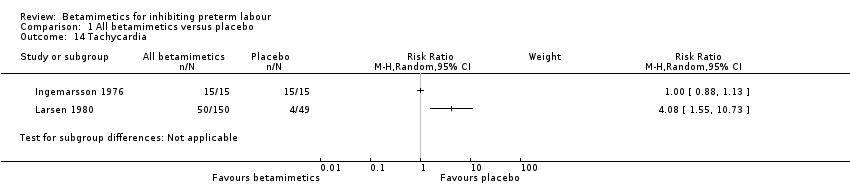
Comparison 1 All betamimetics versus placebo, Outcome 14 Tachycardia.

Comparison 1 All betamimetics versus placebo, Outcome 15 Chest pain.

Comparison 1 All betamimetics versus placebo, Outcome 16 Dyspnoea.
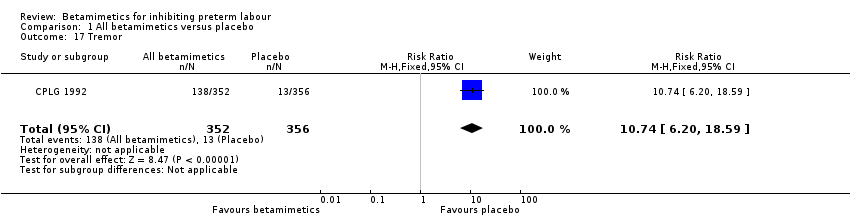
Comparison 1 All betamimetics versus placebo, Outcome 17 Tremor.
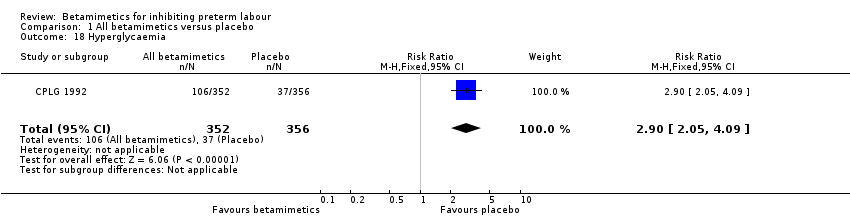
Comparison 1 All betamimetics versus placebo, Outcome 18 Hyperglycaemia.

Comparison 1 All betamimetics versus placebo, Outcome 19 Hypokalaemia.

Comparison 1 All betamimetics versus placebo, Outcome 20 Nausea or vomiting.
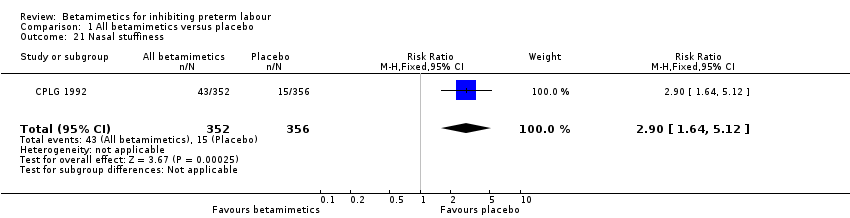
Comparison 1 All betamimetics versus placebo, Outcome 21 Nasal stuffiness.

Comparison 1 All betamimetics versus placebo, Outcome 22 Headaches.

Comparison 1 All betamimetics versus placebo, Outcome 23 Neonatal death.

Comparison 1 All betamimetics versus placebo, Outcome 24 Infant death.

Comparison 1 All betamimetics versus placebo, Outcome 25 Necrotising enterocolitis.

Comparison 1 All betamimetics versus placebo, Outcome 26 Sepsis or infection.
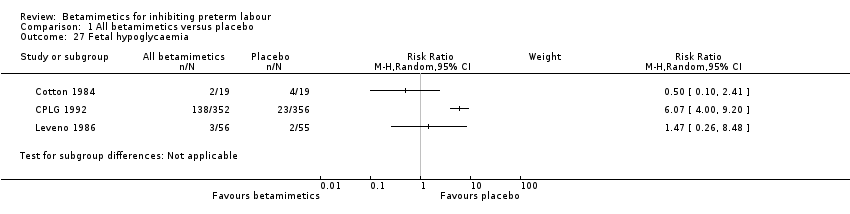
Comparison 1 All betamimetics versus placebo, Outcome 27 Fetal hypoglycaemia.

Comparison 1 All betamimetics versus placebo, Outcome 28 Fetal tachycardia.

Comparison 1 All betamimetics versus placebo, Outcome 29 Infant long‐term neurological development (Bayley score: Psychomotor development).
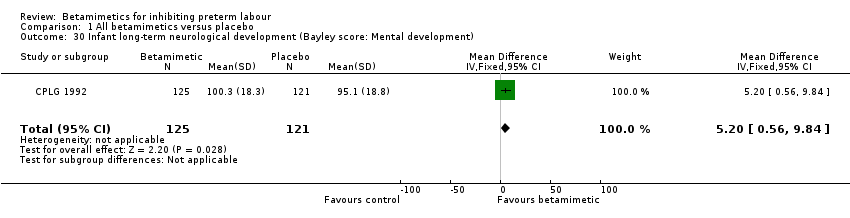
Comparison 1 All betamimetics versus placebo, Outcome 30 Infant long‐term neurological development (Bayley score: Mental development).

Comparison 2 Terbutaline versus ritodrine, Outcome 1 Birth within 48 hours.
Comparison 2 Terbutaline versus ritodrine, Outcome 2 Perinatal death.
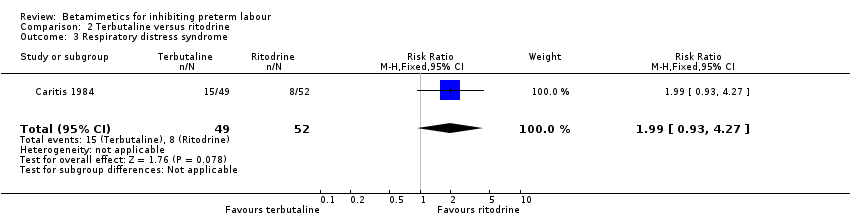
Comparison 2 Terbutaline versus ritodrine, Outcome 3 Respiratory distress syndrome.

Comparison 2 Terbutaline versus ritodrine, Outcome 4 Birth within 7 days.
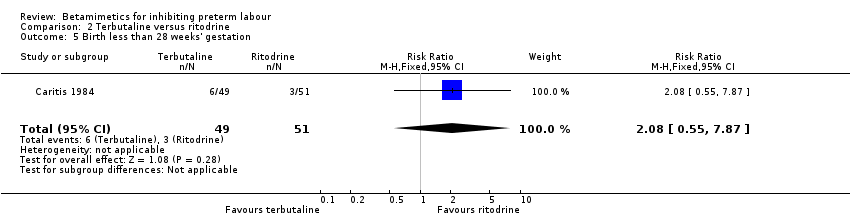
Comparison 2 Terbutaline versus ritodrine, Outcome 5 Birth less than 28 weeks' gestation.

Comparison 2 Terbutaline versus ritodrine, Outcome 6 Cessation of treatment due to adverse drug reactions.
Comparison 2 Terbutaline versus ritodrine, Outcome 7 Any maternal adverse effects.
Comparison 2 Terbutaline versus ritodrine, Outcome 8 Chest pain.

Comparison 2 Terbutaline versus ritodrine, Outcome 9 Shortness of breath or dyspnea.

Comparison 2 Terbutaline versus ritodrine, Outcome 10 Hyperglycaemia or abnormal glucose tolerance test.

Comparison 2 Terbutaline versus ritodrine, Outcome 11 Palpitations.
Comparison 2 Terbutaline versus ritodrine, Outcome 12 Tachycardia.

Comparison 2 Terbutaline versus ritodrine, Outcome 13 Arrhythmia.
Comparison 2 Terbutaline versus ritodrine, Outcome 14 Hypotension.
Comparison 2 Terbutaline versus ritodrine, Outcome 15 Nausea or vomiting.
Comparison 2 Terbutaline versus ritodrine, Outcome 16 Headache.
Comparison 2 Terbutaline versus ritodrine, Outcome 17 Anxiety.

Comparison 2 Terbutaline versus ritodrine, Outcome 18 Necrotising enterocolitis.
Comparison 2 Terbutaline versus ritodrine, Outcome 19 Neonatal death.
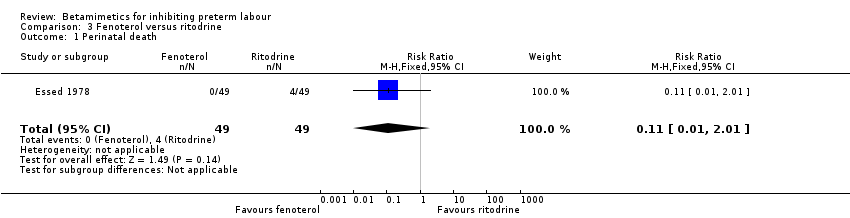
Comparison 3 Fenoterol versus ritodrine, Outcome 1 Perinatal death.

Comparison 3 Fenoterol versus ritodrine, Outcome 2 Respiratory distress syndrome.

Comparison 3 Fenoterol versus ritodrine, Outcome 3 Tachycardia.
Comparison 3 Fenoterol versus ritodrine, Outcome 4 Hypoglycaemia.
Comparison 3 Fenoterol versus ritodrine, Outcome 5 Fetal bradycardia.

Comparison 3 Fenoterol versus ritodrine, Outcome 6 Neonatal death.

Comparison 4 Ritodrine loading dose versus incremental dose, Outcome 1 Birth within 48 hours.

Comparison 4 Ritodrine loading dose versus incremental dose, Outcome 2 Respiratory distress syndrome.

Comparison 4 Ritodrine loading dose versus incremental dose, Outcome 3 Periventricular haemorrhage grade 3‐4.

Comparison 4 Ritodrine loading dose versus incremental dose, Outcome 4 Birth less than 34 weeks.

Comparison 4 Ritodrine loading dose versus incremental dose, Outcome 5 Birth less than 37 weeks.
Comparison 4 Ritodrine loading dose versus incremental dose, Outcome 6 Any maternal adverse effects.
Comparison 4 Ritodrine loading dose versus incremental dose, Outcome 7 Palpitations.
Comparison 4 Ritodrine loading dose versus incremental dose, Outcome 8 Tachycardia.

Comparison 4 Ritodrine loading dose versus incremental dose, Outcome 9 Nausea or vomiting.

Comparison 4 Ritodrine loading dose versus incremental dose, Outcome 10 Headache.

Comparison 4 Ritodrine loading dose versus incremental dose, Outcome 11 Sepsis.
Comparison 4 Ritodrine loading dose versus incremental dose, Outcome 12 Neonatal death.
Comparison 5 Hexoprenaline versus ritodrine, Outcome 1 Cessation of treatment due to adverse drug reactions.
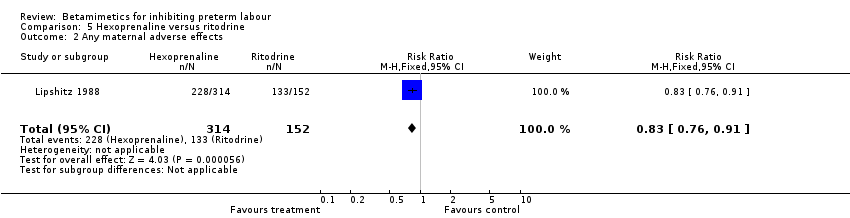
Comparison 5 Hexoprenaline versus ritodrine, Outcome 2 Any maternal adverse effects.

Comparison 5 Hexoprenaline versus ritodrine, Outcome 3 Palpitations.

Comparison 5 Hexoprenaline versus ritodrine, Outcome 4 Hypotension.
Comparison 5 Hexoprenaline versus ritodrine, Outcome 5 Nausea or vomiting.
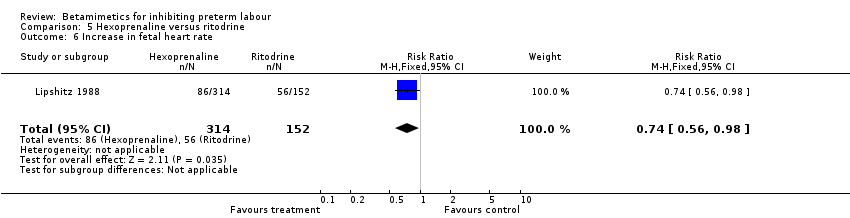
Comparison 5 Hexoprenaline versus ritodrine, Outcome 6 Increase in fetal heart rate.

Comparison 6 Hexoprenaline versus salbutamol, Outcome 1 Respiratory distress syndrome.
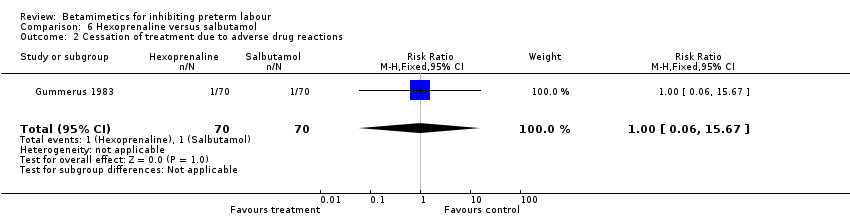
Comparison 6 Hexoprenaline versus salbutamol, Outcome 2 Cessation of treatment due to adverse drug reactions.
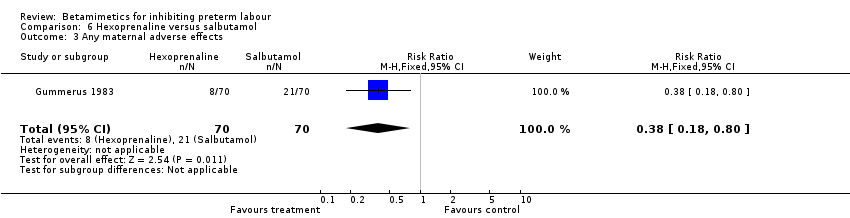
Comparison 6 Hexoprenaline versus salbutamol, Outcome 3 Any maternal adverse effects.
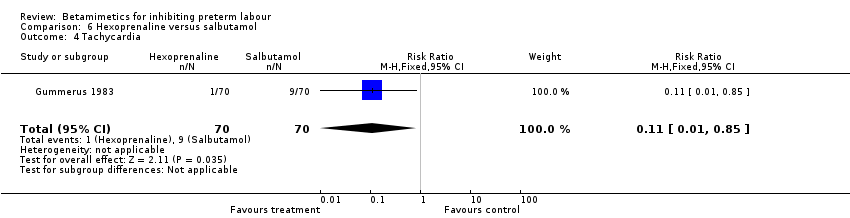
Comparison 6 Hexoprenaline versus salbutamol, Outcome 4 Tachycardia.

Comparison 6 Hexoprenaline versus salbutamol, Outcome 5 Nausea or vomiting.
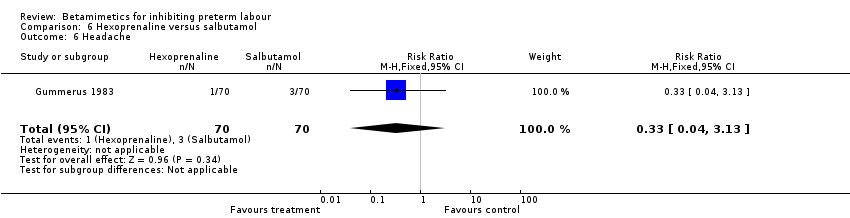
Comparison 6 Hexoprenaline versus salbutamol, Outcome 6 Headache.
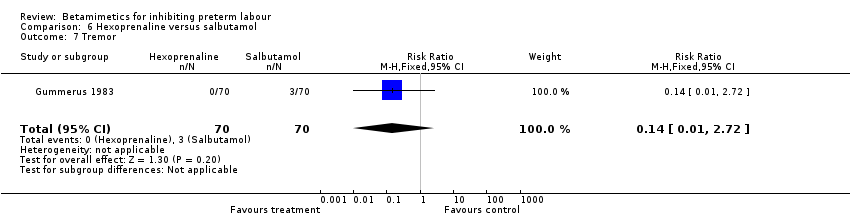
Comparison 6 Hexoprenaline versus salbutamol, Outcome 7 Tremor.

Comparison 7 Terbutaline versus salbutamol, Outcome 1 BIrth within 48 hours.
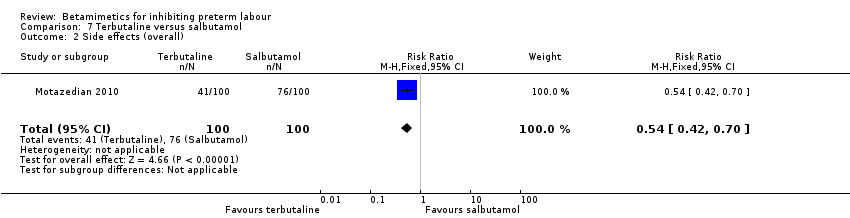
Comparison 7 Terbutaline versus salbutamol, Outcome 2 Side effects (overall).

Comparison 7 Terbutaline versus salbutamol, Outcome 3 Tachycardia.

Comparison 7 Terbutaline versus salbutamol, Outcome 4 Dyspnea.

Comparison 7 Terbutaline versus salbutamol, Outcome 5 Nausea.
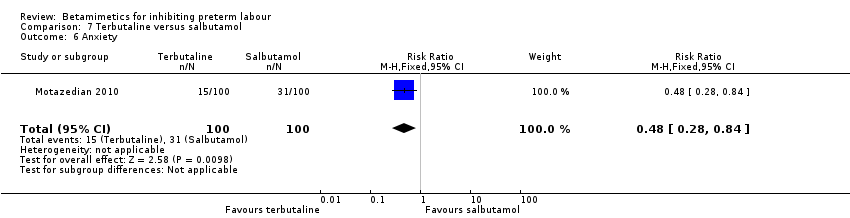
Comparison 7 Terbutaline versus salbutamol, Outcome 6 Anxiety.

Comparison 7 Terbutaline versus salbutamol, Outcome 7 Chills.

Comparison 7 Terbutaline versus salbutamol, Outcome 8 Oedema.
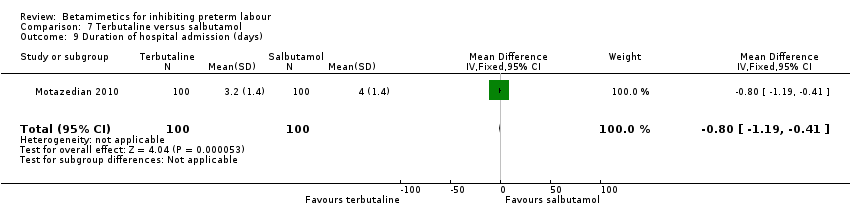
Comparison 7 Terbutaline versus salbutamol, Outcome 9 Duration of hospital admission (days).
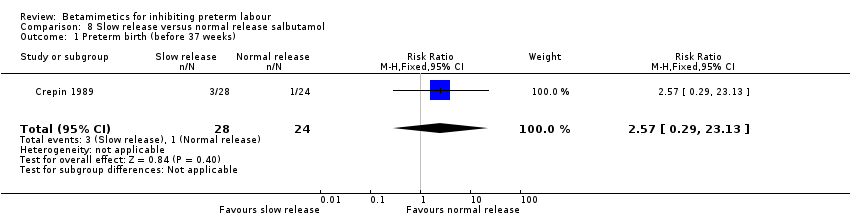
Comparison 8 Slow release versus normal release salbutamol, Outcome 1 Preterm birth (before 37 weeks).

Comparison 8 Slow release versus normal release salbutamol, Outcome 2 Caesarean section.

Comparison 8 Slow release versus normal release salbutamol, Outcome 3 Side effects leading to discontinuation of treatment.

Comparison 8 Slow release versus normal release salbutamol, Outcome 4 Nausea.

Comparison 8 Slow release versus normal release salbutamol, Outcome 5 Apgar score less than 7 at 5 minutes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Birth within 48 hours of treatment Show forest plot | 10 | 1209 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.53, 0.88] |
| 2 Perinatal death (7 days) Show forest plot | 11 | 1332 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.46, 1.55] |
| 3 Respiratory distress syndrome Show forest plot | 8 | 1239 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.71, 1.08] |
| 4 Cerebral palsy Show forest plot | 1 | 246 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.02, 1.63] |
| 5 Birth within 7 days Show forest plot | 5 | 911 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.65, 0.98] |
| 6 Birth less than 37 weeks' gestation Show forest plot | 10 | 1212 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.88, 1.03] |
| 7 Maternal death Show forest plot | 2 | 907 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Pulmonary oedema Show forest plot | 3 | 852 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.03 [0.12, 74.23] |
| 9 Cardiac arrhythmias Show forest plot | 1 | 708 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.54 [0.74, 16.92] |
| 10 Myocardial ischemia Show forest plot | 1 | 106 | Risk Ratio (M‐H, Fixed, 95% CI) | 12.53 [0.72, 216.91] |
| 11 Hypotension Show forest plot | 2 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 1.56 [0.12, 20.86] |
| 12 Cessation of treatment due to adverse drug reaction Show forest plot | 5 | 1081 | Risk Ratio (M‐H, Fixed, 95% CI) | 11.38 [5.21, 24.86] |
| 13 Palpitation Show forest plot | 5 | 1089 | Risk Ratio (M‐H, Random, 95% CI) | 9.91 [6.46, 15.20] |
| 14 Tachycardia Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 15 Chest pain Show forest plot | 2 | 814 | Risk Ratio (M‐H, Fixed, 95% CI) | 11.29 [3.81, 33.46] |
| 16 Dyspnoea Show forest plot | 2 | 814 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.86 [2.21, 6.77] |
| 17 Tremor Show forest plot | 1 | 708 | Risk Ratio (M‐H, Fixed, 95% CI) | 10.74 [6.20, 18.59] |
| 18 Hyperglycaemia Show forest plot | 1 | 708 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.90 [2.05, 4.09] |
| 19 Hypokalaemia Show forest plot | 1 | 708 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.07 [4.00, 9.20] |
| 20 Nausea or vomiting Show forest plot | 3 | 932 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.76 [1.29, 2.42] |
| 21 Nasal stuffiness Show forest plot | 1 | 708 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.90 [1.64, 5.12] |
| 22 Headaches Show forest plot | 3 | 936 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.07 [2.60, 6.35] |
| 23 Neonatal death Show forest plot | 6 | 1174 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.27, 3.00] |
| 24 Infant death Show forest plot | 1 | 750 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.05, 5.64] |
| 25 Necrotising enterocolitis Show forest plot | 2 | 149 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.06, 2.78] |
| 26 Sepsis or infection Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 27 Fetal hypoglycaemia Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 28 Fetal tachycardia Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.4 [1.12, 5.13] |
| 29 Infant long‐term neurological development (Bayley score: Psychomotor development) Show forest plot | 1 | 246 | Mean Difference (IV, Fixed, 95% CI) | 1.30 [‐2.74, 5.34] |
| 30 Infant long‐term neurological development (Bayley score: Mental development) Show forest plot | 1 | 246 | Mean Difference (IV, Fixed, 95% CI) | 5.20 [0.56, 9.84] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Birth within 48 hours Show forest plot | 1 | 83 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.05 [0.77, 5.48] |
| 2 Perinatal death Show forest plot | 1 | 83 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Respiratory distress syndrome Show forest plot | 1 | 101 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.99 [0.93, 4.27] |
| 4 Birth within 7 days Show forest plot | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.57, 1.10] |
| 5 Birth less than 28 weeks' gestation Show forest plot | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.08 [0.55, 7.87] |
| 6 Cessation of treatment due to adverse drug reactions Show forest plot | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.24, 2.92] |
| 7 Any maternal adverse effects Show forest plot | 1 | 83 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.84, 1.07] |
| 8 Chest pain Show forest plot | 2 | 183 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.55, 2.25] |
| 9 Shortness of breath or dyspnea Show forest plot | 2 | 183 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.41, 1.67] |
| 10 Hyperglycaemia or abnormal glucose tolerance test Show forest plot | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.78 [1.05, 3.03] |
| 11 Palpitations Show forest plot | 1 | 83 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.78, 1.79] |
| 12 Tachycardia Show forest plot | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.43, 1.00] |
| 13 Arrhythmia Show forest plot | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.04, 3.22] |
| 14 Hypotension Show forest plot | 2 | 183 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.67, 1.49] |
| 15 Nausea or vomiting Show forest plot | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.50 [0.71, 3.20] |
| 16 Headache Show forest plot | 1 | 83 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.23, 0.99] |
| 17 Anxiety Show forest plot | 1 | 83 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.67, 1.75] |
| 18 Necrotising enterocolitis Show forest plot | 1 | 101 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.05, 5.67] |
| 19 Neonatal death Show forest plot | 2 | 184 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.42, 3.91] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Perinatal death Show forest plot | 1 | 98 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.11 [0.01, 2.01] |
| 2 Respiratory distress syndrome Show forest plot | 1 | 98 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.38, 10.42] |
| 3 Tachycardia Show forest plot | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.35, 1.45] |
| 4 Hypoglycaemia Show forest plot | 1 | 98 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.31, 5.65] |
| 5 Fetal bradycardia Show forest plot | 1 | 98 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.06, 15.54] |
| 6 Neonatal death Show forest plot | 1 | 98 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.02, 0.96] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Birth within 48 hours Show forest plot | 1 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.60, 1.91] |
| 2 Respiratory distress syndrome Show forest plot | 1 | 222 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.35, 1.41] |
| 3 Periventricular haemorrhage grade 3‐4 Show forest plot | 1 | 222 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.01, 2.73] |
| 4 Birth less than 34 weeks Show forest plot | 1 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.70, 1.45] |
| 5 Birth less than 37 weeks Show forest plot | 1 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.60, 1.13] |
| 6 Any maternal adverse effects Show forest plot | 1 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.43, 1.11] |
| 7 Palpitations Show forest plot | 1 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.23, 1.13] |
| 8 Tachycardia Show forest plot | 1 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.33, 2.35] |
| 9 Nausea or vomiting Show forest plot | 1 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.38, 3.84] |
| 10 Headache Show forest plot | 1 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.06, 15.93] |
| 11 Sepsis Show forest plot | 1 | 222 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.23, 2.18] |
| 12 Neonatal death Show forest plot | 1 | 222 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.11 [0.01, 2.04] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Cessation of treatment due to adverse drug reactions Show forest plot | 1 | 466 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.28 [0.08, 0.93] |
| 2 Any maternal adverse effects Show forest plot | 1 | 466 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.76, 0.91] |
| 3 Palpitations Show forest plot | 1 | 466 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.60, 0.94] |
| 4 Hypotension Show forest plot | 1 | 466 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.61, 0.96] |
| 5 Nausea or vomiting Show forest plot | 1 | 466 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.45, 0.89] |
| 6 Increase in fetal heart rate Show forest plot | 1 | 466 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.56, 0.98] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Respiratory distress syndrome Show forest plot | 1 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.75 [0.54, 5.71] |
| 2 Cessation of treatment due to adverse drug reactions Show forest plot | 1 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.06, 15.67] |
| 3 Any maternal adverse effects Show forest plot | 1 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.18, 0.80] |
| 4 Tachycardia Show forest plot | 1 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.11 [0.01, 0.85] |
| 5 Nausea or vomiting Show forest plot | 1 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.34, 2.95] |
| 6 Headache Show forest plot | 1 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.04, 3.13] |
| 7 Tremor Show forest plot | 1 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.01, 2.72] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 BIrth within 48 hours Show forest plot | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.21, 1.84] |
| 2 Side effects (overall) Show forest plot | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.42, 0.70] |
| 3 Tachycardia Show forest plot | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.30, 0.75] |
| 4 Dyspnea Show forest plot | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.15, 1.14] |
| 5 Nausea Show forest plot | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.39, 1.09] |
| 6 Anxiety Show forest plot | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.28, 0.84] |
| 7 Chills Show forest plot | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.34, 0.69] |
| 8 Oedema Show forest plot | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.17, 3.27] |
| 9 Duration of hospital admission (days) Show forest plot | 1 | 200 | Mean Difference (IV, Fixed, 95% CI) | ‐0.80 [‐1.19, ‐0.41] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Preterm birth (before 37 weeks) Show forest plot | 1 | 52 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.57 [0.29, 23.13] |
| 2 Caesarean section Show forest plot | 1 | 52 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.23, 7.07] |
| 3 Side effects leading to discontinuation of treatment Show forest plot | 1 | 52 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Nausea Show forest plot | 1 | 52 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.06, 12.98] |
| 5 Apgar score less than 7 at 5 minutes Show forest plot | 1 | 52 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |

