Incisión con bisturí versus incisión sin bisturí para la vasectomía
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Randomization by marking 102 sheets with one of the methods (51 for each arm), which were sealed in sequentially‐numbered envelopes. Blinding was not reported for outcome assessor or the participants. Two randomization envelopes were opened by mistake (both for no‐scalpel arm) and were not replaced. One post‐randomization exclusion was reported (no‐scalpel arm) due to inability to perform vasectomy under local anesthetic because of a high testis. Two men assigned to no‐scalpel were converted to bilateral incision during the procedure. High lost to follow‐up rate for the one‐month survey (7 men in the incisional group and 7 men in the no‐scalpel group; 13%) and for the 3‐month assessment for azoospermia (13 men in each group; 74%). | |
| Participants | 100 participants aged 31 to 44 years at one site in Denmark from July 1998 to January 2000. The inclusion and exclusion criteria were not stated. | |
| Interventions | Vasectomy with bilateral incision (N=51) versus vasectomy with no‐scalpel approach to the vas (N=49). The methods of vas occlusion and anesthesia were not stated. | |
| Outcomes | The outcome measures included vasectomy success as defined as azoospermia at 3 months, duration of procedure, pain and discomfort (measured with Visual Analog Scales immediately following the procedure), adverse events, need for assistance from another doctor and conversion to another type of procedure. Participants were sent a survey at 1 month regarding pain and wound problems. Participants were to return at 3 months for semen analysis to establish azoospermia. Postoperatively, the resected tissues were sent for microscopic evaluation of the vasectomy. Semen analysis methods were not described. | |
| Notes | The paper was reported in Danish and translated into English. None of the 8 operators (senior resident or fellow) had substantial experience in the no‐scalpel technique. Training was limited to a viewing of an instructional video and one supervised procedure. Only one surgeon performed more than 10 no‐scalpel vasectomies in the trial. Analysis was according to intent‐to‐treat principle exception for one post‐randomization exclusion (due to inability to perform either procedure). The authors reported a priori sample size calculation, but it was based on unrealistic numbers (i.e., 80% power to detect a 19% difference in effect rates between groups at the 5% alpha level). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Methods | Randomized controlled trial using randomly generated numbers. Allocation concealment by opaque, sealed envelopes. Outcome evaluator blinded. Participant blinding unclear. Few men lost to follow up or excluded following randomization. Participants with protocol violations, random allocation errors or technical failure were included in the primary analysis. | |
| Participants | 1429 participants at 8 sites in 5 countries (Brazil, Guatemala, Indonesia, Sri Lanka, Thailand) from March 1988 to August 1991. The age range was not stated. Inclusion criteria were men in good health requesting vasectomy who were 21 years of age or greater. Some local eligibility criteria applied, such as in the Brazil site men were 30 to 40 years of age, had 2 live children, an 8th grade education and minimum monthly income, while Sri Lanka participants had to have 2 or more living children. Exclusion criteria included a history of excessive pain or swelling, abnormality or congenital anomaly and previous injury to or operation on the scrotum or testes, including any previous sterilization. | |
| Interventions | Vasectomy (small segment of the vas excised and ligated both ends) using a no‐scalpel incision (N=715) versus vasectomy (same technique) with a single or double vertical incision (N=714). Method of anesthesia was not stated. | |
| Outcomes | The primary outcome measure was safety. Secondary measures were ease of use, duration of procedure and effectiveness (sterility). Participants were to return between 3 and 15 days for post‐operative evaluation and at 10 weeks for semen analysis. Absence of live spermatozoa was considered proof of sterility. Failures were determined at surgeon discretion and criteria were not standardized among centers. Participants were encouraged to return whenever they had a problem related to surgery and until semen analysis showed no live spermatozoa or sterilization was declared. | |
| Notes | All 8 operators (general surgeons and urologists) had experience with the standard vasectomy technique while 3 had experience with the no‐scalpel technique. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Not a randomized controlled trial. | |
| Not a randomized controlled trial since treatment group was based on patient preference for date of operation. | |
| Compared two no‐scalpel methods. | |
| Duplicate publication of Chen 2004; compared two no‐scalpel methods. | |
| Not a randomized controlled trial. | |
| Compared no‐scalpel method with intra‐vas device. |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Perioperative bleeding Show forest plot | 2 | 1534 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.59 [0.33, 1.04] |
| Analysis 1.1  Comparison 1 No‐scalpel versus standard incision, Outcome 1 Perioperative bleeding. | ||||
| 2 Hematoma during follow up Show forest plot | 2 | 1182 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.23 [0.15, 0.36] |
| Analysis 1.2  Comparison 1 No‐scalpel versus standard incision, Outcome 2 Hematoma during follow up. | ||||
| 3 Operating time <=6 minutes Show forest plot | 1 | 1428 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.37 [1.92, 2.91] |
| Analysis 1.3  Comparison 1 No‐scalpel versus standard incision, Outcome 3 Operating time <=6 minutes. | ||||
| 4 Operating time >=11 min Show forest plot | 1 | 1428 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.56 [0.43, 0.73] |
| Analysis 1.4  Comparison 1 No‐scalpel versus standard incision, Outcome 4 Operating time >=11 min. | ||||
| 5 Perioperative difficulty in identifying ductus Show forest plot | 1 | 99 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.54 [0.05, 5.30] |
| Analysis 1.5  Comparison 1 No‐scalpel versus standard incision, Outcome 5 Perioperative difficulty in identifying ductus. | ||||
| 6 Perioperative difficulty in isolating the vas Show forest plot | 1 | 1421 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.80 [1.18, 2.76] |
| Analysis 1.6  Comparison 1 No‐scalpel versus standard incision, Outcome 6 Perioperative difficulty in isolating the vas. | ||||
| 7 Perioperative equipment difficulties (unspecified) Show forest plot | 1 | 1456 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.28 [0.10, 0.77] |
| Analysis 1.7  Comparison 1 No‐scalpel versus standard incision, Outcome 7 Perioperative equipment difficulties (unspecified). | ||||
| 8 Perioperative need for assistance from second operator Show forest plot | 1 | 99 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.77 [0.67, 4.70] |
| Analysis 1.8  Comparison 1 No‐scalpel versus standard incision, Outcome 8 Perioperative need for assistance from second operator. | ||||
| 9 Perioperative pain Show forest plot | 1 | 1428 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.75 [0.61, 0.93] |
| Analysis 1.9  Comparison 1 No‐scalpel versus standard incision, Outcome 9 Perioperative pain. | ||||
| 10 Pain during follow up Show forest plot | 1 | 86 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.03 [0.43, 2.52] |
| Analysis 1.10  Comparison 1 No‐scalpel versus standard incision, Outcome 10 Pain during follow up. | ||||
| 11 Pain or tenderness during long‐term follow up Show forest plot | 1 | 1272 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.78 [0.46, 1.32] |
| Analysis 1.11  Comparison 1 No‐scalpel versus standard incision, Outcome 11 Pain or tenderness during long‐term follow up. | ||||
| 12 Scrotal pain during follow up Show forest plot | 2 | 1179 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.66 [0.52, 0.83] |
| Analysis 1.12  Comparison 1 No‐scalpel versus standard incision, Outcome 12 Scrotal pain during follow up. | ||||
| 13 Pain at ejaculation during follow up Show forest plot | 1 | 86 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.94 [0.49, 129.15] |
| Analysis 1.13  Comparison 1 No‐scalpel versus standard incision, Outcome 13 Pain at ejaculation during follow up. | ||||
| 14 Infection during follow up Show forest plot | 2 | 1182 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.34 [0.13, 0.90] |
| Analysis 1.14  Comparison 1 No‐scalpel versus standard incision, Outcome 14 Infection during follow up. | ||||
| 15 Wound problems during follow up Show forest plot | 1 | 86 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.51 [0.18, 1.47] |
| Analysis 1.15  Comparison 1 No‐scalpel versus standard incision, Outcome 15 Wound problems during follow up. | ||||
| 16 Sterility Show forest plot | 1 | 1239 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.94 [0.50, 1.76] |
| Analysis 1.16  Comparison 1 No‐scalpel versus standard incision, Outcome 16 Sterility. | ||||
| 17 Vasectomy failure Show forest plot | 1 | 1239 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.87 [0.37, 2.07] |
| Analysis 1.17  Comparison 1 No‐scalpel versus standard incision, Outcome 17 Vasectomy failure. | ||||

Comparison 1 No‐scalpel versus standard incision, Outcome 1 Perioperative bleeding.

Comparison 1 No‐scalpel versus standard incision, Outcome 2 Hematoma during follow up.

Comparison 1 No‐scalpel versus standard incision, Outcome 3 Operating time <=6 minutes.

Comparison 1 No‐scalpel versus standard incision, Outcome 4 Operating time >=11 min.

Comparison 1 No‐scalpel versus standard incision, Outcome 5 Perioperative difficulty in identifying ductus.

Comparison 1 No‐scalpel versus standard incision, Outcome 6 Perioperative difficulty in isolating the vas.

Comparison 1 No‐scalpel versus standard incision, Outcome 7 Perioperative equipment difficulties (unspecified).

Comparison 1 No‐scalpel versus standard incision, Outcome 8 Perioperative need for assistance from second operator.

Comparison 1 No‐scalpel versus standard incision, Outcome 9 Perioperative pain.

Comparison 1 No‐scalpel versus standard incision, Outcome 10 Pain during follow up.

Comparison 1 No‐scalpel versus standard incision, Outcome 11 Pain or tenderness during long‐term follow up.

Comparison 1 No‐scalpel versus standard incision, Outcome 12 Scrotal pain during follow up.

Comparison 1 No‐scalpel versus standard incision, Outcome 13 Pain at ejaculation during follow up.
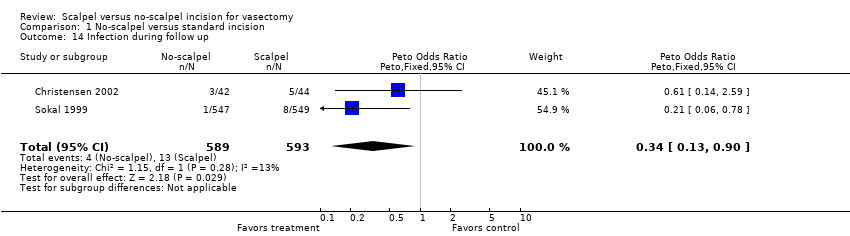
Comparison 1 No‐scalpel versus standard incision, Outcome 14 Infection during follow up.

Comparison 1 No‐scalpel versus standard incision, Outcome 15 Wound problems during follow up.
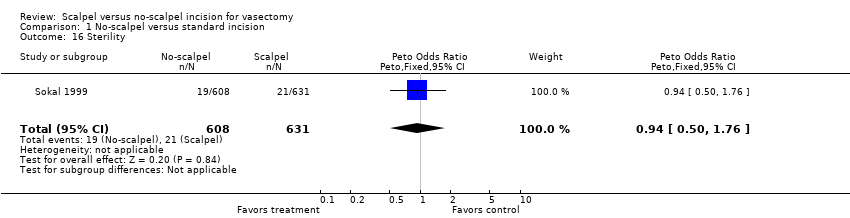
Comparison 1 No‐scalpel versus standard incision, Outcome 16 Sterility.
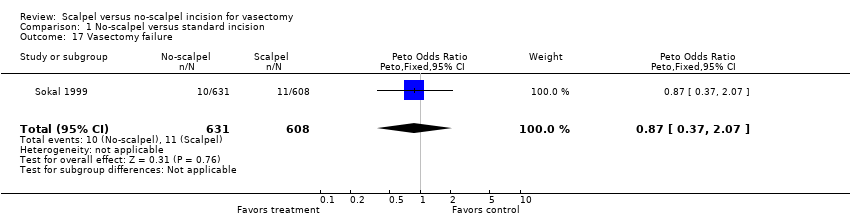
Comparison 1 No‐scalpel versus standard incision, Outcome 17 Vasectomy failure.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Perioperative bleeding Show forest plot | 2 | 1534 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.59 [0.33, 1.04] |
| 2 Hematoma during follow up Show forest plot | 2 | 1182 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.23 [0.15, 0.36] |
| 3 Operating time <=6 minutes Show forest plot | 1 | 1428 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.37 [1.92, 2.91] |
| 4 Operating time >=11 min Show forest plot | 1 | 1428 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.56 [0.43, 0.73] |
| 5 Perioperative difficulty in identifying ductus Show forest plot | 1 | 99 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.54 [0.05, 5.30] |
| 6 Perioperative difficulty in isolating the vas Show forest plot | 1 | 1421 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.80 [1.18, 2.76] |
| 7 Perioperative equipment difficulties (unspecified) Show forest plot | 1 | 1456 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.28 [0.10, 0.77] |
| 8 Perioperative need for assistance from second operator Show forest plot | 1 | 99 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.77 [0.67, 4.70] |
| 9 Perioperative pain Show forest plot | 1 | 1428 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.75 [0.61, 0.93] |
| 10 Pain during follow up Show forest plot | 1 | 86 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.03 [0.43, 2.52] |
| 11 Pain or tenderness during long‐term follow up Show forest plot | 1 | 1272 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.78 [0.46, 1.32] |
| 12 Scrotal pain during follow up Show forest plot | 2 | 1179 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.66 [0.52, 0.83] |
| 13 Pain at ejaculation during follow up Show forest plot | 1 | 86 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.94 [0.49, 129.15] |
| 14 Infection during follow up Show forest plot | 2 | 1182 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.34 [0.13, 0.90] |
| 15 Wound problems during follow up Show forest plot | 1 | 86 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.51 [0.18, 1.47] |
| 16 Sterility Show forest plot | 1 | 1239 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.94 [0.50, 1.76] |
| 17 Vasectomy failure Show forest plot | 1 | 1239 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.87 [0.37, 2.07] |

