Incisión con bisturí versus incisión sin bisturí para la vasectomía
Información
- DOI:
- https://doi.org/10.1002/14651858.CD004112.pub4Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 30 marzo 2014see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Regulación de la fertilidad
- Copyright:
-
- Copyright © 2017 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
A Pun and L Cook did the data abstraction. L Lopez reviewed the literature searches for the initial review, and updated the review from 2009 to 2014. All authors were involved in the review development and edited the initial manuscript.
Sources of support
Internal sources
-
No sources of support supplied
External sources
-
U.S. Agency for International Development, USA.
Support for conducting the review and updates at FHI 360 (through 2011)
-
National Institute of Child Health and Human Development, USA.
Support for conducting the review and updates at FHI 360 (through 2014)
Declarations of interest
L Lopez is employed at FHI 360 (formerly known as Family Health International) where one of the included trials was conducted (Sokal 1999). She was not involved in that trial.
Acknowledgements
From FHI 360:
-
Carol Manion assisted with the literature searches.
-
David Grimes and David Sokal reviewed the initial manuscript.
-
Florence Carayon helped with the searches and reviewed the search results in 2014.
Thanks to Dr Hugo Andreini, for advising us of an error in the text in the Effects of interventions section. The error was corrected and the amended review was republished in February 2017.
Version history
| Published | Title | Stage | Authors | Version |
| 2014 Mar 30 | Scalpel versus no‐scalpel incision for vasectomy | Review | Lynley A Cook, Asha Pun, Maria F Gallo, Laureen M Lopez, Huib AAM Van Vliet | |
| 2007 Apr 18 | Scalpel versus no‐scalpel incision for vasectomy | Review | Lynley A Cook, Asha Pun, Maria F Gallo, Laureen M Lopez, Huib AAM Van Vliet | |
| 2006 Oct 18 | Scalpel versus no‐scalpel incision for vasectomy | Review | Lynley A Cook, Asha Pun, H van Vliet, Maria M.F. Gallo, Laureen M Lopez, Huib HAAM Van Vliet | |
| 2003 Apr 22 | Scalpel versus no scalpel incision for vasectomy | Protocol | Lynley A L.A. Cook, Asha Pun, Huib HAAM Van Vliet, Maria M.F. Gallo | |
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Humans; Male;
PICO

Comparison 1 No‐scalpel versus standard incision, Outcome 1 Perioperative bleeding.

Comparison 1 No‐scalpel versus standard incision, Outcome 2 Hematoma during follow up.

Comparison 1 No‐scalpel versus standard incision, Outcome 3 Operating time <=6 minutes.

Comparison 1 No‐scalpel versus standard incision, Outcome 4 Operating time >=11 min.

Comparison 1 No‐scalpel versus standard incision, Outcome 5 Perioperative difficulty in identifying ductus.

Comparison 1 No‐scalpel versus standard incision, Outcome 6 Perioperative difficulty in isolating the vas.

Comparison 1 No‐scalpel versus standard incision, Outcome 7 Perioperative equipment difficulties (unspecified).

Comparison 1 No‐scalpel versus standard incision, Outcome 8 Perioperative need for assistance from second operator.

Comparison 1 No‐scalpel versus standard incision, Outcome 9 Perioperative pain.

Comparison 1 No‐scalpel versus standard incision, Outcome 10 Pain during follow up.

Comparison 1 No‐scalpel versus standard incision, Outcome 11 Pain or tenderness during long‐term follow up.

Comparison 1 No‐scalpel versus standard incision, Outcome 12 Scrotal pain during follow up.

Comparison 1 No‐scalpel versus standard incision, Outcome 13 Pain at ejaculation during follow up.
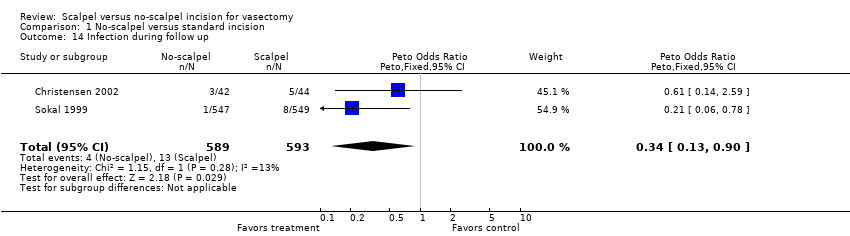
Comparison 1 No‐scalpel versus standard incision, Outcome 14 Infection during follow up.

Comparison 1 No‐scalpel versus standard incision, Outcome 15 Wound problems during follow up.
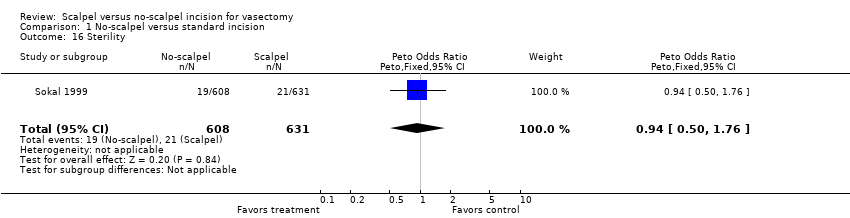
Comparison 1 No‐scalpel versus standard incision, Outcome 16 Sterility.
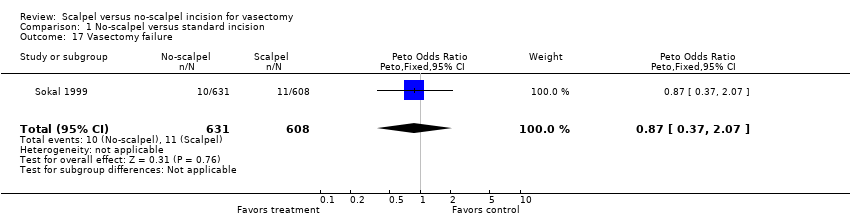
Comparison 1 No‐scalpel versus standard incision, Outcome 17 Vasectomy failure.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Perioperative bleeding Show forest plot | 2 | 1534 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.59 [0.33, 1.04] |
| 2 Hematoma during follow up Show forest plot | 2 | 1182 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.23 [0.15, 0.36] |
| 3 Operating time <=6 minutes Show forest plot | 1 | 1428 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.37 [1.92, 2.91] |
| 4 Operating time >=11 min Show forest plot | 1 | 1428 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.56 [0.43, 0.73] |
| 5 Perioperative difficulty in identifying ductus Show forest plot | 1 | 99 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.54 [0.05, 5.30] |
| 6 Perioperative difficulty in isolating the vas Show forest plot | 1 | 1421 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.80 [1.18, 2.76] |
| 7 Perioperative equipment difficulties (unspecified) Show forest plot | 1 | 1456 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.28 [0.10, 0.77] |
| 8 Perioperative need for assistance from second operator Show forest plot | 1 | 99 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.77 [0.67, 4.70] |
| 9 Perioperative pain Show forest plot | 1 | 1428 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.75 [0.61, 0.93] |
| 10 Pain during follow up Show forest plot | 1 | 86 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.03 [0.43, 2.52] |
| 11 Pain or tenderness during long‐term follow up Show forest plot | 1 | 1272 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.78 [0.46, 1.32] |
| 12 Scrotal pain during follow up Show forest plot | 2 | 1179 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.66 [0.52, 0.83] |
| 13 Pain at ejaculation during follow up Show forest plot | 1 | 86 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.94 [0.49, 129.15] |
| 14 Infection during follow up Show forest plot | 2 | 1182 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.34 [0.13, 0.90] |
| 15 Wound problems during follow up Show forest plot | 1 | 86 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.51 [0.18, 1.47] |
| 16 Sterility Show forest plot | 1 | 1239 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.94 [0.50, 1.76] |
| 17 Vasectomy failure Show forest plot | 1 | 1239 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.87 [0.37, 2.07] |

