Ventilación de alta frecuencia versus ventilación convencional para el tratamiento de las lesiones pulmonares agudas y el síndrome de dificultad respiratoria aguda
Información
- DOI:
- https://doi.org/10.1002/14651858.CD004085.pub3Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 28 febrero 2013see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Anestesia
- Copyright:
-
- Copyright © 2013 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
All authors contributed to the study concept and design, revised the manuscript for important intellectual content, and approved the final version. SS conceived the study, acquired data, analysed and interpreted data, and drafted the manuscript. MS, JOF, and NKJA acquired, analysed and interpreted the data. MOM, NDF, and HW interpreted the data. NKJA and JOF contributed equally to this study. SS, JOF, NKJA are guarantors.
Declarations of interest
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare that all authors had:
-
no financial support for the submitted work from anyone other than their employer;
-
no financial relationships with commercial entities that might have an interest in the submitted work;
-
no spouses, partners, or children with relationships with commercial entities that might have an interest in the submitted work;
-
the following non‐financial interests relevant to the submitted work: Drs Meade and Ferguson are primary investigators and Drs Friedrich and Adhikari are co‐investigators for the ongoing Canadian Institutes of Health Research (CIHR) funded OSCILLATE study. CareFusion (formerly SensorMedics) is providing study oscillators to some of the hospitals involved in the OSCILLATE study for the duration of the study.
Acknowledgements
We thank all primary investigators who provided additional data for this review: Steven Derdak and Tom Bachman; Casper Bollen; Spyros Mentzelopoulos; Rujipat Samransamruajkit; and Sanjoy Shah.
We would like to acknowledge James Mapstone for contributions made to earlier versions of this systematic review (Wunsch 2004).
We would like to thank Mathew Zacharias (content editor), Marialena Trivella (statistical editor), Rodrigo Cavallazzi, Hansjoerg Waibel, Arash Afshari (peer reviewers) and Janet Wale (consumer Editor) for their help and editorial advice during the preparation of this updated systematic review.
Version history
| Published | Title | Stage | Authors | Version |
| 2016 Apr 04 | High‐frequency oscillatory ventilation versus conventional ventilation for acute respiratory distress syndrome | Review | Sachin Sud, Maneesh Sud, Jan O Friedrich, Hannah Wunsch, Maureen O Meade, Niall D Ferguson, Neill KJ Adhikari | |
| 2013 Feb 28 | High‐frequency ventilation versus conventional ventilation for treatment of acute lung injury and acute respiratory distress syndrome | Review | Sachin Sud, Maneesh Sud, Jan O Friedrich, Hannah Wunsch, Maureen O Meade, Niall D Ferguson, Neill KJ Adhikari | |
| 2004 Jan 26 | High‐frequency ventilation versus conventional ventilation for treatment of acute lung injury and acute respiratory distress syndrome | Review | Hannah Wunsch, James Mapstone | |
| 2002 Jun 26 | High‐frequency ventilation versus conventional ventilation for treatment of acute lung injury and acute respiratory distress syndrome | Protocol | Hannah Wunsch, James Mapstone | |
Differences between protocol and review
| Original Protocol | Amended Protocol (03 27 2009) | Reason (outcome #) |
| Primary: mortality (Intensive care unit (ICU), hospital, 30 days, 60 plus days). | Primary outcomes: 1. hospital or 30‐day mortality.
| Hospital mortality is the most common endpoint in critical care studies. ICU mortality is not a patient centred outcome. Hospital mortality and 30‐day mortality are considered equivalent. Longer term mortality was included as a secondary outcome. |
| Secondary: 1. total length of mechanical ventilation (high‐frequency and conventional combined), 2. length of stay in the intensive care unit, 3. length of hospital stay, 4. any long‐term quality of life measurements, 5. any long‐term cognitive measurements, 6. cost effectiveness. | Secondary outcomes: 1. 6‐month mortality, 2. duration of mechanical ventilation (in days, as stated by the authors), 3. ventilator‐free days to day 28 or 30 (in days, as stated by the authors), 4. health‐related quality of life at one year, 5. treatment failure, leading to crossover to the other arm or discontinuation of the study protocol. We accepted authors’ definitions of treatment failure, which could include severe oxygenation failure, ventilation failure, hypotension, or barotrauma (pneumothorax, pneumomediastinum, subcutaneous emphysema), 6. the ratio of partial pressure of arterial oxygen (PaO2) to inspired fraction of oxygen (FiO2) (PaO2/FiO2 ratio) at 24, 48, and 72 hours after randomization, 7. oxygenation index (OI, defined as 100 x mean airway pressure/PaO2/FiO2 ratio) measured at 24, 48, and 72 hours after randomization, 8. ventilation, measured by partial pressure of carbon dioxide (PaCO2) at 24, 48, and 72 hours after randomization, 9. mean airway pressure 24, 48, and 72 hours after randomization, 10. barotrauma (as stated by the authors), 11. hypotension (as stated by the authors), 12. endotracheal tube obstruction due to secretions, 13. technical complications and equipment failure in patients treated with HFO (including unintentional system air leaks, and problems with the oscillatory diaphragm, humidifier, and alarm systems).
| Total duration of mechanical ventilation (1) is ambiguous may be measured in two ways in critical care trials: days of mechanical ventilation or ventilator free days. Since these endpoints cannot be combined we analysed them separately. We did not analyse length of ICU stay or hospital length of stay (2, 3) as these were likely to be confounded by mortality (an intervention that improves survival will also increase ICU or hospital length of stay). Long term quality of life measurements (4) and long term cognitive measurements (5) was not precisely defined and unlikely to be reported in studies to date. We chose to analyse health‐related quality of life at one year, if reported.
We did not analyse cost‐effectiveness (6) because it is unlikely cost‐effectiveness studies would be performed since this intervention has not been yet proven to be effective.
We included several physiologic endpoints not in the original review in order to assess the effect of HFO on oxygenation (6,7) and ventilation (8,9).
We included several additional safety endpoints prior to undertaking this update in order to assess potential complications of HFO (10‐13). |
| Subgroup analyses: none. | Subgroup analyses: (see Subgroup analysis and investigation of heterogeneity; Sensitivity analysis). | (See text) |
| Search strategy:
(see previous version: Wunsch 2004).
| Search strategy:
(see Appendix 1).
| A more sensitive (but less specific) search strategy was designed using published sensitive strategies for retrieving randomized trials (Haynes 2005; Wong 2006). We also improved sensitivity of the search strategy by searching conference proceedings and contacting primary investigators. |
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Adolescent; Adult; Child; Child, Preschool; Humans; Infant;
PICO
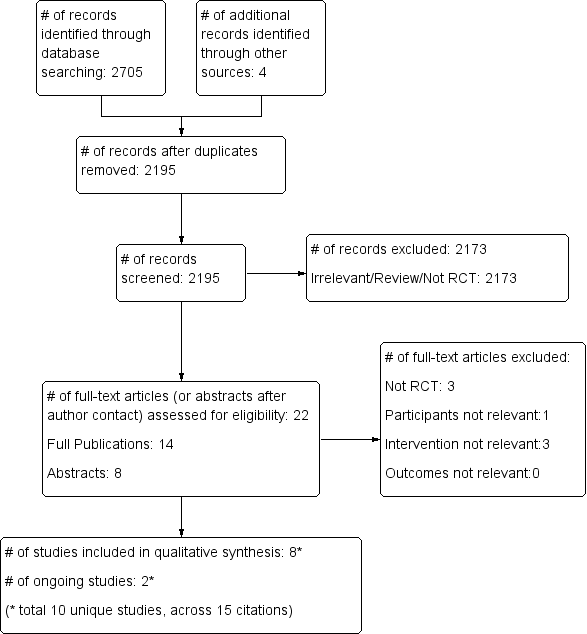
Study flow diagram.
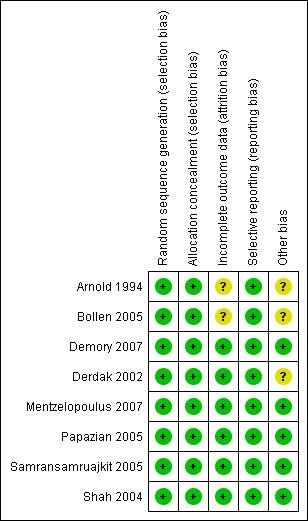
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
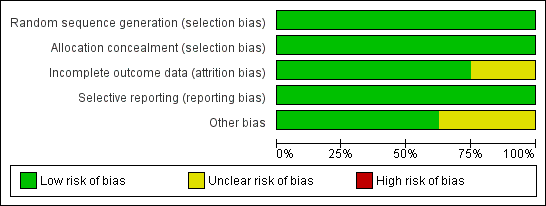
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
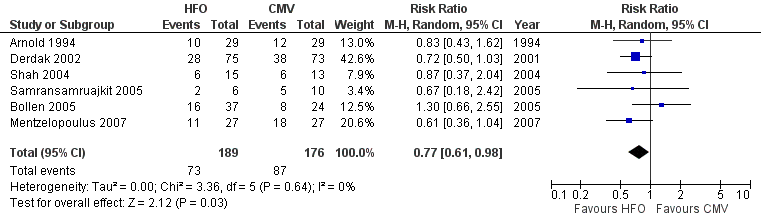
Forest plot of comparison: 1 Mortality, outcome: 1.1 Hospital or 30‐day mortality.

Forest plot of comparison: 2 Adverse events, outcome: 2.1 Treatment failure (intractable hypoxia, hypotension, acidosis, hypercapnoea requiring discontinuation of study intervention).

Comparison 1 Mortality, Outcome 1 Hospital or 30‐day Mortality.

Comparison 1 Mortality, Outcome 2 Hospital or 30‐day Mortality (Bollen 2005 patients lost to follow‐up excluded).

Comparison 1 Mortality, Outcome 3 Hospital or 30‐day mortality: Adult versus paediatric trials.

Comparison 1 Mortality, Outcome 4 Hospital or 30‐day Mortality: Low risk of bias versus unclear risk of bias.
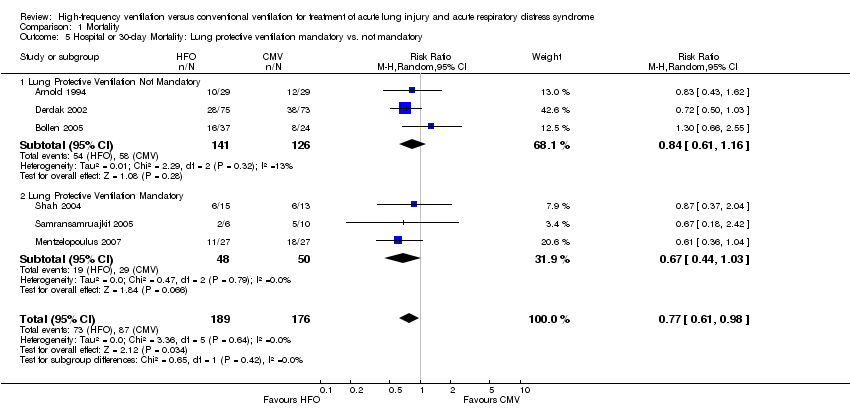
Comparison 1 Mortality, Outcome 5 Hospital or 30‐day Mortality: Lung protective ventilation mandatory vs. not mandatory.
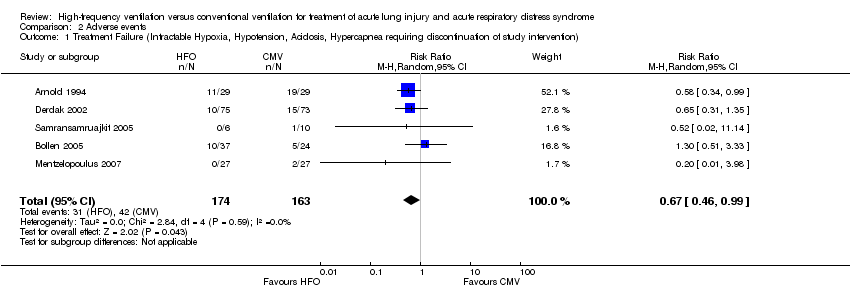
Comparison 2 Adverse events, Outcome 1 Treatment Failure (Intractable Hypoxia, Hypotension, Acidosis, Hypercapnea requiring discontinuation of study intervention).

Comparison 2 Adverse events, Outcome 2 Barotrauma.
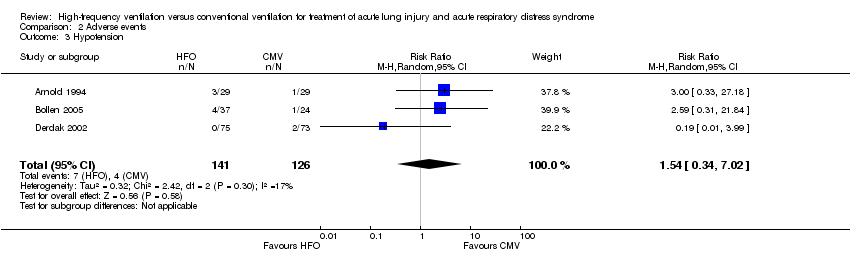
Comparison 2 Adverse events, Outcome 3 Hypotension.

Comparison 2 Adverse events, Outcome 4 Hypotension (Shah and Mentzelopoulos included).

Comparison 2 Adverse events, Outcome 5 ETT Obstruction.
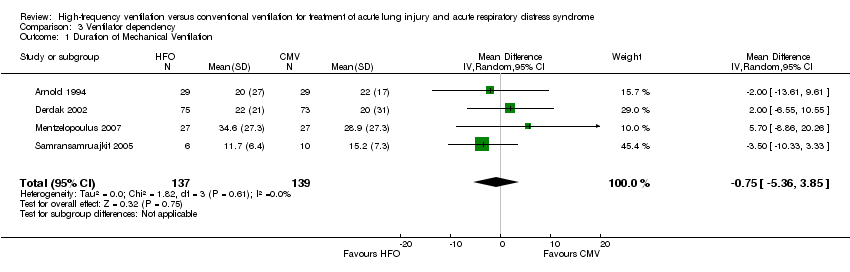
Comparison 3 Ventilator dependency, Outcome 1 Duration of Mechanical Ventilation.
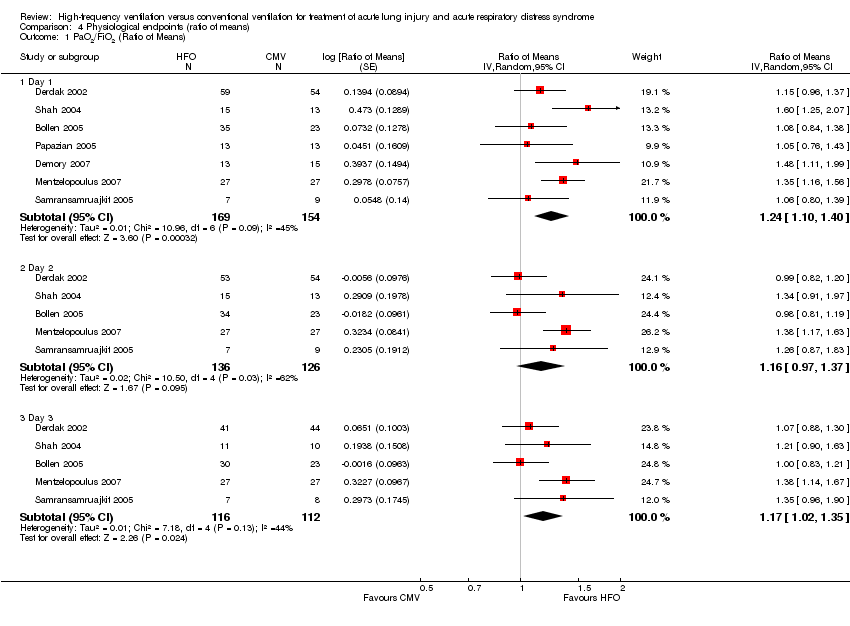
Comparison 4 Physiological endpoints (ratio of means), Outcome 1 PaO2/FiO2 (Ratio of Means).

Comparison 4 Physiological endpoints (ratio of means), Outcome 2 Oxygenation Index (Ratio of Means).

Comparison 4 Physiological endpoints (ratio of means), Outcome 3 PaCO2 (Ratio of Means).

Comparison 4 Physiological endpoints (ratio of means), Outcome 4 Mean Airway Pressure (Ratio of Means).
| HFO compared to conventional mechanical ventilation for ALI and ARDS | ||||||
| Patient or population: patients with ALI and ARDS | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Conventional mechanical ventilation | High Frequency Oscillation | |||||
| Hospital (or 30 day) mortality | Typical risk1 | RR 0.77 | 365 | ⊕⊕⊕⊝ | ||
| 443 per 1000 | 341 per 1000 | |||||
| 6 month mortality | 589 per 10004 | 465 per 1000 | RR 0.79 | 148 | ⊕⊕⊝⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 The basis of the assumed risk is a systematic review and meta‐analysis of the mortality in patients with ARDS (Phua 2009). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Hospital or 30‐day Mortality Show forest plot | 6 | 365 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.61, 0.98] |
| 2 Hospital or 30‐day Mortality (Bollen 2005 patients lost to follow‐up excluded) Show forest plot | 6 | 362 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.61, 0.98] |
| 3 Hospital or 30‐day mortality: Adult versus paediatric trials Show forest plot | 6 | 365 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.61, 0.98] |
| 3.1 Adult Trials | 4 | 291 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.58, 1.02] |
| 3.2 Paediatric Trials | 2 | 74 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.44, 1.43] |
| 4 Hospital or 30‐day Mortality: Low risk of bias versus unclear risk of bias Show forest plot | 6 | 365 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.61, 0.98] |
| 4.1 Low Risk of Bias Trials (free of selection, reporting, and attrition bias) | 4 | 246 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.53, 0.92] |
| 4.2 Unclear Risk of Bias Trials (possible selection, reporting or attrition bias) | 2 | 119 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.65, 1.66] |
| 5 Hospital or 30‐day Mortality: Lung protective ventilation mandatory vs. not mandatory Show forest plot | 6 | 365 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.61, 0.98] |
| 5.1 Lung Protective Ventilation Not Mandatory | 3 | 267 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.61, 1.16] |
| 5.2 Lung Protective Ventilation Mandatory | 3 | 98 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.44, 1.03] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Treatment Failure (Intractable Hypoxia, Hypotension, Acidosis, Hypercapnea requiring discontinuation of study intervention) Show forest plot | 5 | 337 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.46, 0.99] |
| 2 Barotrauma Show forest plot | 6 | 365 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.37, 1.22] |
| 3 Hypotension Show forest plot | 3 | 267 | Risk Ratio (M‐H, Random, 95% CI) | 1.54 [0.34, 7.02] |
| 4 Hypotension (Shah and Mentzelopoulos included) Show forest plot | 5 | 349 | Risk Ratio (M‐H, Random, 95% CI) | 1.46 [0.77, 2.76] |
| 5 ETT Obstruction Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Duration of Mechanical Ventilation Show forest plot | 4 | 276 | Mean Difference (IV, Random, 95% CI) | ‐0.75 [‐5.36, 3.85] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PaO2/FiO2 (Ratio of Means) Show forest plot | 7 | Ratio of Means (Random, 95% CI) | Subtotals only | |
| 1.1 Day 1 | 7 | 323 | Ratio of Means (Random, 95% CI) | 1.24 [1.10, 1.40] |
| 1.2 Day 2 | 5 | 262 | Ratio of Means (Random, 95% CI) | 1.16 [0.97, 1.37] |
| 1.3 Day 3 | 5 | 228 | Ratio of Means (Random, 95% CI) | 1.17 [1.02, 1.35] |
| 2 Oxygenation Index (Ratio of Means) Show forest plot | 7 | Ratio of Means (Random, 95% CI) | Subtotals only | |
| 2.1 Day 1 | 7 | 352 | Ratio of Means (Random, 95% CI) | 1.11 [0.97, 1.26] |
| 2.2 Day 2 | 6 | 306 | Ratio of Means (Random, 95% CI) | 1.07 [0.92, 1.24] |
| 2.3 Day 3 | 6 | 266 | Ratio of Means (Random, 95% CI) | 1.07 [0.88, 1.29] |
| 3 PaCO2 (Ratio of Means) Show forest plot | 8 | Ratio of Means (Random, 95% CI) | Subtotals only | |
| 3.1 Day 1 | 8 | 386 | Ratio of Means (Random, 95% CI) | 0.91 [0.78, 1.07] |
| 3.2 Day 2 | 6 | 310 | Ratio of Means (Random, 95% CI) | 0.87 [0.72, 1.06] |
| 3.3 Day 3 | 6 | 267 | Ratio of Means (Random, 95% CI) | 0.98 [0.84, 1.14] |
| 4 Mean Airway Pressure (Ratio of Means) Show forest plot | 8 | Ratio of Means (Random, 95% CI) | Subtotals only | |
| 4.1 Day 1 | 8 | 389 | Ratio of Means (Random, 95% CI) | 1.33 [1.27, 1.40] |
| 4.2 Day 2 | 6 | 309 | Ratio of Means (Random, 95% CI) | 1.26 [1.16, 1.37] |
| 4.3 Day 3 | 6 | 274 | Ratio of Means (Random, 95% CI) | 1.22 [1.07, 1.39] |

