Akupunktur untuk kemurungan
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Single‐blind randomised controlled trial of acupuncture, non‐specific acupuncture, and a wait‐list control | |
| Participants | Diagnosis: major depressive disorder Method of diagnosis: DSM‐IV Age: 18 to 45 years Participant information: 38 women Location: United States (community) Inclusion/Exclusion: Exclusion criteria: dysthymia or chronic depression, history of psychosis or mania, substance abuse, current treatment, endocrine abnormalities, history of central nervous system lesions or any medical condition causing depression, pregnancy, suicide potential | |
| Interventions | (1) Duration: 8 weeks (12 sessions) Frequency of treatment: The intervention involved 2 sessions a week for the first 4 weeks, followed by 1 session a week thereafter. Treatment protocol: Acupuncture ‐ no details provided (2) Duration: 8 weeks (12 sessions) Frequency of treatment: The intervention involved 2 sessions a week for the first 4 weeks, followed by 1 session a week thereafter. Treatment protocol: Non‐specific acupuncture ‐ no details provided (3) Duration: 8 weeks Frequency of treatment: N/A Treatment protocol: The wait list control received acupuncture at 8 weeks. | |
| Outcomes | Time points for assessment: baseline, 8 and 16 weeks Outcomes: Hamilton Depression Rating Scale (HAMD) Beck Depression Inventory (BDI) | |
| Notes | A power calculation was not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was computer generated. |
| Allocation concealment (selection bias) | Low risk | Randomisation was undertaken centrally. |
| Blinding of participants and personnel (performance bias) | Low risk | Participants in the 2 acupuncture groups and the therapist were blind. It remains possible that the acupuncture therapists developed some awareness between treatments. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The assessing clinician was blind. It was unclear whether the analyst was blind. |
| Incomplete outcome data (attrition bias) | Low risk | Five women dropped out (13%) ‐ 2 from the acupuncture group, 2 from non‐specific acupuncture, and 1 from wait‐list control. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Unclear risk | Insufficient information was presented to examine other sources of bias, for example, imbalance at randomisation. |
| Methods | Single‐blind randomised controlled trial of acupuncture, non‐specific acupuncture, and a wait‐list control | |
| Participants | Diagnosis: major depressive disorder (MDD) Method of diagnosis: DSM‐IV criteria and HAMD score > 14 Age: 18 to 65 years Participant information: 157 males and females Location: community setting, USA Inclusion/Exclusion: Exclusion criteria: dysthymia or a chronic MDD over longer than 2 years, seasonal pattern; current Axis I diagnosis besides MDD or Axis II cluster B disorder; history of psychosis or mania, substance abuse, or dependence within past 4 months; current relevant treatment; endocrine abnormalities; history of CNS involvement (seizures); medical condition believed to cause depression; active suicidal risk; pregnancy | |
| Interventions | Acupuncture practitioners were NCCAOM board‐certified acupuncturists with a minimum of 4 years and in practice for 5 years. (1) Duration: 8 weeks (12 sessions) Frequency of treatment: Treatment was administered twice a week for 4 weeks, followed by once a week for 4 weeks. Treatment protocol: The acupuncture group received individualised TCM treatment. Point selection used unilateral and bilateral points and 10 to 16 needles; the depth of needle insertion was based on TCM principles; de qi sensation was obtained, and needles were retained for 20 minutes. No co‐interventions were allowed. (2) Duration: 8 weeks (12 sessions) Frequency of treatment: Treatment was administered twice a week for 4 weeks, followed by once a week for 4 weeks. Treatment protocol: The control group consisted of an active comparator involving non‐specific acupuncture. Valid acupuncture points were used but were not designed to treat depression. Points were needled as above. (3) Duration: 8 weeks Frequency of treatment: N/A Treatment protocol: Wait‐list control | |
| Outcomes | Time points for assessment: All patients completed the Beck Depression Inventory at weekly intervals. Blinded outcome assessors used the Hamilton Depression Rating Scale at 4‐weekly intervals. Outcomes: Hamilton Depression Rating Scale (HAMD) Beck Depression Inventory (BDI) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of generating randomisation schedule was not reported. |
| Allocation concealment (selection bias) | Low risk | The schedule was devised by the first trial author and was made available only on completion of assessments. |
| Blinding of participants and personnel (performance bias) | Low risk | Participants and treating acupuncturists were blind to the study hypothesis. The non‐specific intervention involved valid acupuncture points, and therapists administering acupuncture in this group would perceive that they were providing a valid treatment. Therapist expectations were assessed; the blinding strategy suggests that acupuncturists may have developed some awareness, but no evidence suggested that this influenced the clinical outcome. |
| Blinding of outcome assessment (detection bias) | Low risk | Assessing clinicians were blind to study groups. |
| Incomplete outcome data (attrition bias) | High risk | Six participants (3.8%) were post‐randomisation exclusions. Valid intention‐to‐treat sample acupuncture n = 50, non‐specific acupuncture n = 49, wait‐list control n = 52. Twenty (13%) participants terminated treatment before completion of the intervention, but this was not different between groups. A further 42 (28%) participants terminated treatment before 16 weeks. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | No imbalances were evident at randomisation. The study appears free of other sources of bias. |
| Methods | Acupuncture vs control acupuncture | |
| Participants | Diagnosis: major depressive disorder Method of diagnosis: DSM‐IV and SCID with score > 14, mild to moderate depression Age: not stated Participant information: 53 participants Location: University of Pittsburgh Medical Center (UPMC) Shadyside, Center for Complementary Medicine, Pittsburgh, Pennsylvania, USA Inclusion/Exclusion: Exclusion criteria: severe MDD, suicidal, seizure disorder, psychosis, bipolar disorder, chronic MDD (i.e. duration > 2 years), treatment‐resistant MDD, history of substance abuse within past 6 months | |
| Interventions | All medication was tapered before randomisation and participants remained free of psychotropic medication during the study. No other interventions were used. (1) Duration: 6 weeks (12 sessions) Frequency of treatment: 2/week Treatment protocol: Each session was administered over 30 minutes. Points Du 20 and Yingtang were needled. Electro‐acupuncture (EA) was administered. 0.22 × 30 mm needles were inserted. Electro‐stimulator 4C connected current 3 to 5 mA had a frequency of 2 Hz. Treatment was administered by a practitioner with 4 years of training who had completed Masters of Acupuncture and TCM and was certified by NCCAOM, had been in practice for 5 years, and had clinical practice with treatment of patients with anxiety and depression. (2) Duration: 6 weeks (12 sessions) Frequency of treatment: 2/week Treatment protocol: Control group: non‐scalp points with sham EA. Needles were inserted at 2 points away from classical points near channels, and no current was applied to the needle. Needles were inserted obliquely to 1 cm. | |
| Outcomes | Time points for assessment: unclear for HAMD, weekly for side effects rating scale; SF‐36 2 weeks post intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Comparison of responders in each group defined as a score ≤ 10 with relative decrease of 50% from baseline Side effects rating scale SF‐36 | |
| Notes | ITT was undertaken. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence was used. |
| Allocation concealment (selection bias) | Low risk | Envelopes were sealed/opaque. |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding of participants and key study personnel was ensured; it is unlikely that blinding could have been broken. |
| Blinding of outcome assessment (detection bias) | Low risk | The trained research associate undertaking measurement was blind. |
| Incomplete outcome data (attrition bias) | Low risk | Reasons for missing outcome data were unlikely to be related to true outcomes (for survival data, censoring was unlikely to introduce bias). Treatment group: 4 were attrition, 1 could not be contacted, 2 preferred a different treatment regimen, 1 withdrew owing to physical health. Control group: All 3 could not be contacted. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | The study appears free of other sources of bias. |
| Methods | Randomised controlled trial of 50 participants comparing manual acupuncture vs wait‐list control | |
| Participants | Diagnosis: depression Method of diagnosis: ICD F33.2 Age: 48.68 years (experimental), 46.32 years (control) Participant information: 3 males, 22 females (experimental), 2 males 23 females (control) Location: Germany (psychiatric clinic) Inclusion/Exclusion: Inclusion criteria: not specified, apart from the diagnosis of depression Exclusion criteria: addiction (other than nicotine), epilepsy or other neurological disorders, other co‐morbid psychiatric disorders | |
| Interventions | (1) Duration: 12 weeks (12 sessions) Frequency of treatment: 1/week Treatment protocol: TCM‐style acupuncture/manual acupuncture. Needles were retained for 60 minutes. Point selection was individualised with the following points being most common (% of all treatments): Hegu (LI4) (96%), Sanyinjiao (SP6) (96%), Yinlingquan (SP9) (96%), Shenmen (HT7) (95%), Taixi (KI3) (95%), Sishencong (EX‐HN1) (92%), Zusanli (ST36) (91%), Taichong (LR3) (78%), Quchi (LI11) (53%), Zhaohai (KI6) (53%), Guanyuan (CV4) (46%), Yanglingquan (GB34) (36%), Gongsun (SP4) (34%), Xuehai (SP10) (34%), and Lieque (LU7) (32%). All acupuncture was performed by a licensed Oriental medical practitioner with more than 5 years of clinical experience. (2) Duration: 12 weeks Frequency of treatment: N/A Treatment protocol: Wait‐list control | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Beck Depression Inventory (BDI) | |
| Notes | ITT not undertaken | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Patient‐reported outcomes were used; therefore blinding was not applicable. |
| Incomplete outcome data (attrition bias) | High risk | Dropout rate was high (> 20%). |
| Selective reporting (reporting bias) | Unclear risk | Insufficient details were provided. |
| Other bias | Unclear risk | Insufficient details were provided. |
| Methods | Randomised controlled trial of abdominal acupuncture vs electro‐acupuncture and standard care | |
| Participants | Diagnosis: major depressive disorder Method of diagnosis: depression diagnosed by CCMD and DSM‐II Age: 60 to 85 years Participant information: 60 participants Location: inpatients at the Department of Neurology at the First Hospital Affiliated to Changchun China Inclusion/Exclusion: Inclusion criteria: cerebral infarction or cerebral haemorrhage; no history of depression or abuse of medication or alcohol and no known allergies to medications; no severe heart, lung, liver, or kidney disease; no loss of speech Exclusion criteria: history of mental disorders; taking antidepressants in past 2 weeks; severe depression; HAMD > 35; allergic to alcohol or medications; cardiovascular, cerebral, liver, kidney, or blood pathology conditions; do no meet inclusion criteria; not taking medication as advised or dropped out halfway; fainting during acupuncture; infection at acupuncture points | |
| Interventions | (1) Duration: 6 weeks (21 treatments) Frequency of treatment: every second day Treatment protocol: The treatment group received abdominal acupuncture, with stimulation to acupuncture points CV12 Zhong Wan, CV10 Xia Wan, CV6 Qi Hai, CV4 Guan Yuan, ST24 Hua Rou Men (on both sides), ST26 Wai Ling, and Tai Heng. Acupuncture needles were inserted perpendicular to a depth before the muscle layer. Needles were inserted quickly ‐ only twirling no lifting, and de qi sensation was not obtained. Needles were left in for 30 minutes. Needles used were of the Hwato brand and were manufactured at Suzhouby Tai xin san lI medical product company, H model, 0.35 mm × 40 mm, 0.30 mm × 25 mm, 0.30 mm × 50 mm. (2) Duration: 6 weeks (21 treatments) Frequency of treatment: every second day Treatment protocol: Electro‐acupuncture to points DU 20 Baihui, DU24 Shen Ting, M‐HN‐3 Yintang, M‐NH‐1 Shishenchong, LIV 3 Taichong, and HT 7 Shenmen. Baihui was needled 1 cun parallel to the skin, Shenting was needled 0.5 cun parallel to the skin, Yintang was needled 0.5 cun parallel to the skin, Shishenchong was needled parallel to the skin, Taichong was needled perpendicular 0.5 to 1 cun, Shenmen was needled perpendicular 0.5 cun. The electro‐acupuncture machine was connected to needles administered at a frequent pulse frequency at 4 Hz and intermittent pulse at 20 Hz. Positive pulse amplitude at 50 V and negative pulse amplitude at 35 V. During treatment, patients should feel an achey numbness, a sensation of fullness, or twitching of muscle. Needles were left in for 30 minutes. Electro‐machine model GD6805X, manufactured by Xia xi san yuan medical equipment company, was used. (3) Duration: 6 weeks Frequency of treatment: treatment administered every second day. Treatment protocol: The control was standard care for stroke rehabilitation. | |
| Outcomes | Time points for assessment: 2, 4, and 6 weeks after the start of the study Outcomes: Hamilton Depression Rating Scale (HAMD) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details of randomisation were provided. |
| Allocation concealment (selection bias) | Unclear risk | No information could be obtained from trial authors. |
| Blinding of participants and personnel (performance bias) | High risk | The participant and the therapist were not blind. |
| Blinding of outcome assessment (detection bias) | Unclear risk | It was unclear whether analysts and assessing clinicians were blind to group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | No losses to follow‐up were reported. Data on all participants were analysed. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Data show no imbalance in randomisation at baseline between groups. The study appears free of other sources of bias. |
| Methods | Electro‐acupuncture vs minimal acupuncture vs control acupuncture controlled trial | |
| Participants | Diagnosis: major depressive disorder Method of diagnosis: DSM‐IV and clinician assessment via structured interview Age: not stated Participant information: 150 participants Location: 4 regional psychiatric outpatient clinics in Hong Kong Inclusion/Exclusion: Inclusion criteria: age 18‐70 years, insomnia >3 nights /week for last 3 months, Insomnia severity index score >15, fixed dose of antidepressants in last 3 months Exclusion criteria: HAMD score > 18, apnoea hypopnoea index ≥ 10 or periodic limb movement disorder ≥ 15, significant suicidal risk, previous diagnosis of schizophrenia, psychotic disorder, bipolar disorder, alcoholism, substance abuse, pregnancy or breastfeeding, infection close to acupuncture points, serious illness, acupuncture in previous 12 months, CHM within 2 weeks before baseline measurements, increased dose of hypnotics within 4 weeks of baseline measures | |
| Interventions | Acupuncture experience of person administering treatment: registered acupuncturist with at least 3 years' experience (1) Duration: 3 weeks (9 sessions) Frequency of treatment: 3/week Treatment protocol: TCM‐style acupuncture. Choice of points used: bilateral ear shenmen, Sishencong Anmian, PC6, Ht7, SP6 Yintang GV20 Mode of stimulation:depth of insertion 2 to 25 mm. De qi obtained if possible. Electro‐stimulator attached to all needles, current 0.4 ms at 4 Hz needles left for 30 minutes (2) Duration: 3 weeks (9 sessions) Frequency of treatment: 3/week Treatment protocol: Minimal: at points thought to have no effect and avoidance of de qi. Points on forearm 1 inch lateral to HE3 and HE7, I inch lateral to Lu3, and 0.5 inch dorsal to GB29, pony forehead, and ear. Electro‐stimulator the same (3) Duration: 3 weeks (9 sessions) Frequency of treatment: 3/week Treatment protocol: Placebo: Streitberger placebo needle placed at 1 inch beside acupuncture points used in acupuncture group connected to electro‐stimulator with no current | |
| Outcomes | Time points for assessment: Outcome assessment at 1 and 5 weeks post treatment Adverse events assessed after 3rd, 6th, and 9th treatments Outcomes: Hamilton Depression Rating Scale (HAMD) Secondary outcomes: quality of life based on SF‐36 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated assignment was used. |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes were used. |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding of participants and key study personnel was ensured, and it is unlikely that the blinding could have been broken. Credibility and blinding of treatment were assessed. |
| Blinding of outcome assessment (detection bias) | Low risk | Study personnel were blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Missing outcome data were balanced in numbers across intervention groups, with similar reasons provided for missing data across groups; 16 (10%) dropped out during treatment, and 18 (12%) withdrew at 5 weeks. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | The study appears free of other sources of bias. |
| Methods | Acupuncture vs medication (fluoxetine) | |
| Participants | Diagnosis: post‐stroke depression Method of diagnosis: Diagnoses were based on DSM‐II‐R and HAMD scales. Age: not stated Participant information: 62 participants Location: Beijing Hospital of Integration of Chinese and Western Medicine, China Inclusion/Exclusion: Exclusion criteria: none specified | |
| Interventions | (1) Duration: unclear (40 sessions) Frequency of treatment: daily for 10 days, then 2‐ to 3‐day break Treatment protocol: Acupuncture points on the Du meridian were needles including DU 20 Baihui, DU 24 Shenting, DU 16 Feng fu. Additional points were used including PC6 Neiguan (both sides), LI4 Hegu (both sides), GB20 Feng chi (both sides). Needles of 30 gauge 1 to 1.5 cun (Chinese unit of measurement) long were used, needled to a depth of 0.5 to 1 cun. Needles were manipulation using reinforcing reducing method. Once de qi was obtained, needles were left in for 30 minutes. (2) Duration: 60 days Frequency of treatment: daily Treatment protocol: The control group received medication including fluoxetine 20 mg/d for 60 days. | |
| Outcomes | Time points for assessment: before treatment, 30 days into treatment, 60 days into treatment Outcomes: Hamilton Depression Rating Scale (HAMD) | |
| Notes | Two participants dropped out owing to adverse effects. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation schedule was computer generated. |
| Allocation concealment (selection bias) | Unclear risk | No information could be obtained from the trial author. |
| Blinding of participants and personnel (performance bias) | High risk | The study participant and the therapist were not blind. |
| Blinding of outcome assessment (detection bias) | Unclear risk | It was unclear whether the assessing clinician(s) and the analyst were blind to the study group. |
| Incomplete outcome data (attrition bias) | Low risk | Two participants (1 from each group) were excluded post randomisation with no details reported. Data on primary outcome were available for 60 participants. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Unclear risk | It was unclear whether baseline characteristics were comparable. |
| Methods | Three‐arm randomised controlled trial of electro‐acupuncture vs acupuncture vs medication (fluoxetine) among participants with post‐stroke depression | |
| Participants | Diagnosis: post‐stroke depression Method of diagnosis: depression according to DSM‐IV, CCMD‐3, and HAMD score > 20 Age: not stated Participant information: 108 participants Location: inpatients or day patients from the Heilongjiang Provincial Academy of TCM Hospitial, China Inclusion/Exclusion: Exclusion criteria: a severe health condition, pregnancy or breastfeeding, long‐term medication, plasma 5‐HT and SSRI‐type medications taken together in the past 2 weeks, lack of willingness or suitability to be participants in this clinical trial, severe suicidal ideation or behaviour not suitable for patient to be medicated, organic mental disorder, depression caused by psychoactive substances or non‐addictive medications | |
| Interventions | (1) Duration: 30 days (30 sessions) Frequency of treatment: daily Treatment protocol: Electro‐acupuncture. Points stimulated include GB5 Xuan Lu, DU17 Nao Hu, GV18 Qiang Jian, GB15 Tou lin qi, GB14 Yang Bai, GB 8 Shuai Gu, GB 7 Qu Bin, GV24 Shen Ting, M‐HN‐3 Yin Tang. Each acupuncture needle was inserted to a depth of 40 to 50 mm, stimulation used a fast but small angled twirling manipulation method, at 200 twirls per minute, with each needle manipulated for 1 minute. Needles were then connected to an electro‐acupuncture device, model G6805‐I. A continuous pulse was used, with frequency set at 120 to 250 pulse per minute. Intensity was set at a level tolerable to the participant. Stimulation was given over 30 minutes, with needles retained for 1 hour. (2) Duration: 30 days (30 sessions) Frequency of treatment: daily Treatment protocol: Manual acupuncture of non‐point‐through‐point (NON). Acupuncture was administered to points GV20 Baihui, M‐HN‐3 Yintang, M‐HN‐1 Shishencong, PC6 Neiguan, HT7 Shenmen, SP6 Sanyinjiao, LI4 Hegu, and LIV3 Taichong. Needles were inserted and de qi obtained, needles were manipulated using either lifting twirling reinforcing‐dispersing method or reinforcing‐dispersing manipulation methods. Needles were retained for 1 hour. Hwato acupuncture needles, manufactured by Suzhou medical product company, with dimensions 0.38 mm × 40 mm to 40 mm were used. (3) Duration: 30 days Frequency of treatment: daily Treatment protocol: The medication group received fluoxetine. Participants initially were given a 20‐mg/d dose; after 2 weeks with no severe side effects observed, the dose was increase to 80 mg/d. | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details on randomisation were reported. |
| Allocation concealment (selection bias) | Unclear risk | No communication was received from trial authors in response to a letter requesting further details on study methods. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and therapists were not blind to their group allocation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No details on the blinding status of the assessing clinician(s) and analyst were reported. |
| Incomplete outcome data (attrition bias) | Unclear risk | Exclusions and loss of data were not explained. Data on one primary outcome are complete. Data on secondary outcomes are incomplete. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Groups were comparable at baseline. The study appears free of other sources of bias. |
| Methods | Randomised controlled trial comparing 2 types of manual acupuncture with medication (fluoxetine) | |
| Participants | Diagnosis: clinical depression Method of diagnosis: CCMD‐3, HAMD score ≥ 20 Age: not stated Participant information: 103 women Location: outpatient setting, China Inclusion/Exclusion: Exclusion criteria: schizophrenia; interstitial disease; physical illness that can cause symptoms of depression; schizophrenia and other psychotic disorders; heart, liver, and kidney system diseases; glaucoma | |
| Interventions | (1) Duration: 6 weeks (42 sessions) Frequency of treatment: daily Treatment protocol: Harmonize spirit soothe liver acupuncture group Points needled: Baihui (DU20); Fengfu (DU16); Shuigou (DU26); Yintang (EX‐HN 3); Sishencong (EX‐HN 1);Taichong (LR 3); Ganshu (BL18) (2) Duration: 6 weeks (42 sessions) Frequency of treatment: daily Treatment protocol: Regular acupuncture group Points needled: Qimen (LV14); Taichong (LR 3); Yanglingquan (GB34); Zhigou (SJ6); Neiguan (PC6); Zusanli (ST36) (3) Duration: 6 weeks Frequency of treatment: daily treatment. Treatment protocol: Control group: fluoxetine 20 mg/d for 6 weeks | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) SDS SCL‐90 Cured rate based on HAMD score | |
| Notes | No ITT | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not stated. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) | High risk | Reason for missing outcome data is likely to be related to true outcomes, with imbalance in numbers or reasons for missing data across intervention groups. |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient. |
| Other bias | High risk | Sample size calculation was not provided. |
| Methods | Randomised controlled trial of electro‐acupuncture, medication (fluoxetine), and electro‐acupuncture plus medication | |
| Participants | Diagnosis: clinical depression Method of diagnosis: CCMD‐3 and HAMD score of 20 to 35 Age: 18 to 60 years Participant information: 75 participants Location: inpatients or day patients at the Department of Neurology, PLA General Hospital, Beijing, China Inclusion/Exclusion: Inclusion criteria: history of severe neurological or physical disease, no history of mental illness; willingness to participate in this study Exclusion criteria: schizophrenia and other mental disorders; central nervous system organic disease; pregnancy or breastfeeding, or planning pregnancy during treatment; severe depression with HAMD score of 35; suicidal tendencies; known allergies to fluoxetine | |
| Interventions | (1) Duration: 6 weeks (36 sessions) Frequency of treatment: 6/week Treatment protocol: Electro‐acupuncture plus medication. Acupuncture points Baihui DU 20, M‐HN‐3 Yintang were stimulated. Additional points were added based on differential patterns: Liver qi stagnation type add LIV3 Taichong, LI4 Hegu; Fire due to qi stagnation type add LIV2 Xing jian; Melancholy injuring the spirit type add Anmian, Shenmen HT7, Neiguan PC6; heart and spleen deficiency add SP6 Sanyinjiao, Zhusanl ST36; Yin deficiency with excess fire type add KD3 Taixi and KD6 Zhaohai. GV20 Baihu and DU24 Shen ting were connected to electro‐acupuncture machine model G 6805‐1, using continuous pulse, frequency set at 120 to 250 times per minute. Strength was set at a comfort level for the participant. Electro‐acupuncture was administered over 30 minutes, and needles were retained for 1 hour. Medication consisted of fluoxetine 20 mg per day, administered over 6 weeks. (2) Duration: 6 weeks (36 sessions) Frequency of treatment: 6/week Treatment protocol: Electro‐acupuncture only. Acupuncture points Baihui DU 20, M‐HN‐3 Yintang were stimulated. Additional points were added based on differential patterns: Liver qi stagnation type add LIV3 Taichong, LI4 Hegu; Fire due to qi stagnation type add LIV2 Xing jian; Melancholy injuring the spirit type add Anmian, Shenmen HT7, Neiguan PC6; heart and spleen deficiency add SP6 Sanyinjiao, Zhusanl ST36; Yin deficiency with excess fire type add KD3 Taixi and KD6 Zhaohai. GV20 Baihu and DU24 Shen ting were connected to electro‐acupuncture machine model G 6805‐1, using continuous pulse, frequency set at 120 to 250 times per minute. Strength was set at a comfort level for the participant. Electro‐acupuncture was administered over 30 minutes, and needles were retained for 1 hour. (3) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: Medication only, fluoxetine 20 mg per day | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation sequence was computer generated. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment was unclear. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and therapists were not blind to group allocation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Assessing clinicians were blind, but it was unclear whether analysts were blind to group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | Five (6%) participants dropped out from the trial ‐ 2 in the medication group owing to side effects, 2 in the electro‐acupuncture group owing to work commitments and a family member death, and 1 in the acupuncture plus medication group owing to side effects attributed to the medication. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | No imbalances in randomisation were evident at baseline. The study appears free of other sources of bias. |
| Methods | Randomised controlled trial of electro‐acupuncture plus medication (fluoxetine) or medication only | |
| Participants | Diagnosis: depression Method of diagnosis: ICD‐10 and HAMD score 18 to 30 Age: 18 to 50 years Participant information: 75 participants Location: outpatient setting recruited at the Chinese PLA General Hospital, The General Hospital of the People's Liberation Army, China Inclusion/Exclusion: Inclusion criteria: first onset, no serious cerebral organic disease, no other mental health history Exclusion criteria: schizophrenia or other mental disorders; organic diseases such as tumours and central nervous system diseases; pregnancy or lactation, or may be pregnant during treatment; severe depression or relapsed depression, or HAMD score 35 points or with suicidal tendencies; intolerant or hypersensitive to fluoxetine | |
| Interventions | (1) Duration: 6 weeks (36 sessions) Frequency of treatment: 6/week Treatment protocol: Acupuncture points: GV20 and Yintang. For insomnia, add Sishencong (Extra‐HN), Anmian Ⅰ (Extra 8), Sanyinjiao (SP6), Taixi (KI3), and Zhaohai (KI6), etc.; for headache or dizziness, Shenting (DU24), Benshen (GB13), and Fengchi (GB20), etc.; for digestion syndromes, Zhongwan (ZH12), Tianshu (ST25), Liangqiu (ST34), Fenglong (ST40), Zusanli (ST36), and Neiting (ST44), etc.; for cardio syndromes, Shenmen (H7), Neiguan (P6), and Sanyinjiao (SP6), etc.; for chronic pain, Back‐shu points for general malaise, Wushu points, etc. A good needle sensation was administered and described by participants as soreness, numbness, heaviness, or distension; was achieved when needling each point. After achieving the needling sensation, compulsory points were connected to a type G68052‐Ⅰ electro‐acupuncture apparatus. The output wave was continuous, with a frequency of 2 Hz; the output power was regulated according to each participant's tolerance. An electric stimulator was connected for 30 to 40 minutes, and needles were taken off after 1 hour. Participants were administered fluoxetine 20 mg per day in the morning (trade names: fluoxetine; common name: fluoxetine hydrochloride capsule, produced by the Eli Lilly Company (Suzhou) of the United States; specification: 20 mg for each pill) for a total of 6 weeks. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: Participants were administered fluoxetine 20 mg per day in the morning (trade names: fluoxetine; common name: fluoxetine hydrochloride capsule, produced by the Eli Lilly Company (Suzhou) of the United States, specification: 20 mg for each pill) for a total of 6 weeks. | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Symptom severity reduction rate and remission | |
| Notes | ITT was not stated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and study personnel were not blinded. |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessment was blinded. HAMD scores of participants were assessed by 2 separate doctors in psychology who were blinded from grouping information; they were required to reach consistency at a level of at least 98%. |
| Incomplete outcome data (attrition bias) | Low risk | Missing outcome data were balanced in numbers across intervention groups, with similar reasons provided for missing data across groups; 5 cases of attrition. 3 in control: 1 quit owing to dizziness and postural hypotension occurring after 2 weeks of treatment, another owing to panic and pyknosphygmia detected by EKG after 4 weeks of treatment, and the third for dysuria. Two in the EA group quit. The condition of 1 participant deteriorated and participant was hospitalised for combined therapy owing to the death of his mother; the other quit because of a heart attack. Statistical analysis was not performed for these 5 individuals |
| Selective reporting (reporting bias) | Unclear risk | Study protocol was not available. |
| Other bias | Unclear risk | Reporting in the manuscript was insufficient. |
| Methods | Randomised placebo‐controlled trial of acupuncture vs control acupuncture | |
| Participants | Diagnosis: minor depression Method of diagnosis: ICD‐10 F32.0, 32.1 Age: unclear Participant information: 56 participants with depression Location: inpatient and outpatient clinic setting in Germany Inclusion/Exclusion: Exclusion criteria: compulsory detained, alcohol or drug intoxication, subcutaneous long‐acting medication taken in the previous 30 days, mania, bipolar disorder, schizophrenia, blood clot disorder, impaired wound healing, organic disease, seizures, pregnancy or breastfeeding, study participation in the past 30 days, knowledge of acupuncture | |
| Interventions | Before the intervention was commenced, a 2‐week washout was undertaken. A total of 11 points was used for both groups. (1) Duration: 2 weeks (14 sessions) Frequency of treatment: daily Treatment protocol: Participants were administered body acupuncture via acupuncture points known from the literature to have a regulating effect. These included Du20 Baihui, Bl62 Shenmai, PC6 Naiguan, HT 7 Shenman, and EX‐HN1 Sishencong. (2) Duration: 2 weeks (14 sessions) Frequency of treatment: daily Treatment protocol: The control group used sham points at non‐specific points with minimal insertion, located on the hand, head, and foot. | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Global Clinical Improvement Scale | |
| Notes | Reported results may have been limited because data were presented for depression combined with general anxiety. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details of the randomisation schedule were reported. |
| Allocation concealment (selection bias) | Unclear risk | No details of the randomisation schedule were reported. |
| Blinding of participants and personnel (performance bias) | Low risk | Participants were blind to group allocation, and therapists were aware of group allocation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Assessing clinicians were blinded. It is unclear whether analysts were blind to group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up was reported. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | No differences in baseline characteristics were evident. The study appears free of other sources of bias. |
| Methods | Randomised controlled trial of acupuncture, medication (Prozac), and control acupuncture | |
| Participants | Diagnosis: depressive neurosis Method of diagnosis: CCMD‐2 Age: 18 to 65 years Participant information: 81 participants Location: Guangdong Hospital, Guangdong, China Inclusion/Exclusion: Inclusion criteria: needed not to have taken medication in the previous 2 weeks Exclusion criteria: liver, kidney, blood, gastrointestinal disorders; infectious diseases; current pregnancy or breastfeeding | |
| Interventions | (1) Duration: 3 months Frequency of treatment: unclear Treatment protocol: Acupuncture was administered to 4 acupuncture points, Baihi Du 20, M‐HN‐3 Yintang, 4 gates, ear seeds to auricular points liver and heart. These points were rotated between the left and right ear twice a week. Other points were retained for 30 minutes. (2) Duration: 3 months Frequency of treatment: daily Treatment protocol: The first control group received 20 mg of fluoxetine daily for 3 months. (3) Duration: 3 months Frequency of treatment: unclear Treatment protocol: The second control group received sham acupuncture at non‐acupuncture points; the ear points were administered. | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation sequence was computer generated. |
| Allocation concealment (selection bias) | Low risk | Randomisation was concealed by the use of opaque envelopes. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and therapists were not blind to group allocation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Assessing clinicians were blind, and it is unclear whether analysts were blind to group allocation. |
| Incomplete outcome data (attrition bias) | High risk | Four participants (5%) from the medication group withdrew from the study owing to side effects. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Unclear risk | Reported information was insufficient for assessment of other sources of bias. |
| Methods | Randomised parallel controlled trial of acupuncture vs acupuncture with shallow needling vs acupuncture vs control | |
| Participants | Diagnosis: depression Method of diagnosis: CCMD‐3 Age: not stated Participant information: 163 participants Location: outpatient at Guangdong Provincial Hospital of TCM, China Inclusion/Exclusion: Inclusion criteria: HAMD score < 20, meeting TCM criteria for stagnation of liver qi, qi depression transforming into fire, aged 18 to 70 years, not taking antidepressant medication in the past 2 weeks Exclusion criteria: organic somatic disease, e.g. psychosis, schizophrenia; HAMD score > 35; other TCM diagnostic criteria met; epilepsy; serious cerebro‐cardiovascular hepatic, renal gastrointestinal disease | |
| Interventions | (1) Duration: 12 weeks (24 sessions) Frequency of treatment: 2/week Treatment protocol: Acupuncture delivered with the aim of soothing the liver and regulating the mind Acupuncture points: LI4 and LR3, GV20 and Yintang, GV29 Mode of stimulation: 0.35 mm × 25 mm needles, insertion 10 to 12 mm, even lifting, thrusting and rotating manipulation until arrival of de qi. Moxa on Bl17, Bl19, 5 cones/point interdermal needling Bl15, Bl18 (2) Duration: 12 weeks (24 sessions) Frequency of treatment: 2/week Treatment protocol: Control group: non‐acupuncture points with invasive shallow needling 10 mm away from Li4, LR3, GV20 Gv29; shallow but same needling techniques Moxa 10 mm away from points; intradermal needles 10 mm away from points | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Symptom Checklist‐90 Adverse events Dropout from treatment | |
| Notes | ITT not undertaken Groups 1 and 2 combined | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and some key study personnel were not blinded; non‐blinding of others was likely to introduce bias. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Patient‐reported outcomes were reported; therefore blinding was not applicable. |
| Incomplete outcome data (attrition bias) | Low risk | Six dropped out from acupuncture, 8 from shallow needling, 6 from control. Reasons for missing outcome data were unlikely to be related to true outcomes. |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient, but no adverse events were reported. |
| Other bias | Unclear risk | No differences were evident between baseline characteristics. |
| Methods | Parallel randomised controlled trial of acupuncture vs medication (fluoxetine) | |
| Participants | Diagnosis: depression Method of diagnosis: SDS (Self‐rating Depression Scale) score > 50, Hamilton Depression Rating Scale (HAMD) score > 7, PSQI score ≥ 8 Age: 18 to 75 years Participant information: 80 participants Location: outpatient and inpatient ward of Traditional Chinese Medicine (TCM) Department or Acupuncture Department of Chinese PLA General Hospital, China, from October 2008 to October 2010 Inclusion/Exclusion: Inclusion criteria: no intellectual or mental disorders, ability to self‐judge the sleep condition and other common conditions, ability to accomplish the scale independently, expected survival time longer than 3 months Exclusion criteria: taking antidepressant drugs at the present time, Karnofsky score < 30 | |
| Interventions | (1) Duration: 30 days Frequency of treatment: daily Treatment protocol: In treatment group, participants were treated with acupuncture on the acupoints of Fenglong (ST 40), Yinlingquan (SP 9), Xuehai (SP 10), Sanyinjiao (SP 6), Yintang (EX‐HN3), Baihui (DU 20), Sishencong (EX‐HN1), Neiguan (PC 6), and Shenmen (TF 4). When needling, method of neutral supplementation and drainage was used. Participants were treated for 20 to 30 minutes, and the acupuncturist performed needling manipulation at intervals of 5 to 10 minutes. (2) Duration: 30 days Frequency of treatment: daily Treatment protocol: Participants in the control group received fluoxetine hydrochloride capsules (trade name: Prozac, produced by Patheon, in France) 20 mg per day. | |
| Outcomes | Time points for assessment: end of intervention Outcomes: HAMD reduced rate (%) = (score before treatment - score after treatment)/score before treatment × 100% Cure rate (reduced rate > 75%), effective rate (reduced rate 50% to 75%), improved rate (reduced rate 25% to 49%), invalid rate (reduced rate < 25%) | |
| Notes | ITT was not mentioned. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Blinding status was not reported. |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts were reported. |
| Selective reporting (reporting bias) | Unclear risk | No protocol was available and reporting was insufficient. |
| Other bias | Unclear risk | Reporting was insufficient. |
| Methods | Three‐armed randomised controlled trial comparing acupuncture, medication, and control acupuncture for treatment of individuals with depression | |
| Participants | Diagnosis: depression Method of diagnosis: CCMD‐2‐R Age: not stated Participant information: 201 participants were randomised into acupuncture group (n = 78), medication (Prozac) group (n = 82), and sham‐acupuncture group (n = 41). Location: outpatient, China Inclusion/Exclusion: Exclusion criteria: schizophrenia; physical diseases or organic diseases that can cause similar symptoms of depression; age > 65; severe cardiovascular, liver, kidney, haematopoietic system diseases; pregnancy; haematic disease; antidepressant drugs taken within the past 2 weeks | |
| Interventions | (1) Duration: 12 weeks (24 sessions) Frequency of treatment: twice per week Treatment protocol: TCM style of acupuncture. Acupoints used were Taichong (LR 3), Hegu (LI 4), Baihui (GV 20), Yintang (EX‐HN 3), to point Liver and Heart. For sham acupuncture group, punctured spots were those 0.5 cm to LR 3 and LI4 on the radial side, 0.5 cm to GV 20 on the left side, 0.5 cm to EX‐HN 3 on the left side. Manual acupuncture treatment lasted 30 minutes. (2) Duration: 12 weeks Frequency of treatment: daily Treatment protocol: Participants in medication group were ordered to take Prozac 20 mg/d, continuously for 12 weeks. | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Self‐rating Depression Scale (SDS) | |
| Notes | ITT was not stated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence was used. |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes were used. |
| Blinding of participants and personnel (performance bias) | Low risk | Acupuncture and sham participants were blinded. |
| Blinding of outcome assessment (detection bias) | Unclear risk | It was unclear whether assessing clinicians and analysts were blinded. |
| Incomplete outcome data (attrition bias) | Unclear risk | Details were insufficient; 28 were lost to follow‐up, but no details of group allocation were provided. |
| Selective reporting (reporting bias) | Unclear risk | Information presented was insufficient. |
| Other bias | Unclear risk | Information presented was insufficient. |
| Methods | Multi‐centred randomised controlled trial of acupuncture vs control acupuncture vs medication (fluoxetine) | |
| Participants | Diagnosis: depression Method of diagnosis: CCMD‐2 and score > 20 on the HAMD Age: 18 to 65 years Participant information: 440 participants Location: mixed inpatients and outpatients from 4 different hospitals between October 2004 and December 2006, in China Inclusion/Exclusion: Inclusion criteria: conscious, no loss of speech, preserved intelligence, minimum primary education level, TCM diagnostic criteria of ‘yu bing’ depressive disease due to liver qi stagnation or qi stagnation causing fire, no antidepressant medication taken in the previous 2 weeks Exclusion criteria: schizophrenia; organic or somatic disease that can trigger depression; < 18 years or > 65 years of age; severe cardiovascular, neurological, liver, kidney, or blood function disease; pregnancy; non‐co‐operative during needling; not taking medication on time; antidepressants taken in the past 2 weeks | |
| Interventions | (1) Duration: 12 weeks (24 sessions) Frequency of treatment: twice per week Treatment protocol: Treatment group received acupuncture administered to LIV3 Taichong, LI 4 Hegu, DU 20 Baihui, and M‐HN‐3 Yin tang. The 4 gates were needled first, to a depth of 15 mm; the needle was stimulated by lifting twirling manipulation until de qi was obtained. Bai hui was needled at a 30º angle in a quick motion. Yintang was needled by pinching the skin, then inserting to a depth of 15 mm parallel to the skin surface. Baihui and Yintang were twirled until de qi was obtained. The needles were left in for 30 minutes. Two auricular acupuncture points were used ‐ liver and heart points. Ear press tacks were placed on points and secured with small strips of bandage. These points were left in for 3 days, then were repeated in alternate ears. (2) Duration: 12 weeks Frequency of treatment: daily Treatment protocol: The control group received fluoxetine 20 mg/d (Prozac capsule, manufactured by Eli Lilly and Company). These were taken orally once in the morning after meals for a total of 12 weeks. (3) Duration: 12 weeks (24 sessions) Frequency of treatment: twice per week Treatment protocol: The sham acupuncture group involved needling of points in the region of Taichong, Baihui, Yintang, but roughly 0.5 cun away from actual points. The needle was inserted and manipulated in the same way as for the acupuncture group. The auricular acupuncture points were used in the same way as in the active group. | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Assessment of cure and marked effect > 75% change from baseline Reports of adverse events | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation allocation sequence was computer generated. |
| Allocation concealment (selection bias) | Low risk | The allocation sequence was concealed with the use of opaque envelopes. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Blinding of participants in acupuncture and sham groups was unclear, and no testing was reported. The therapist was not blind to group allocation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Assessing clinicians were blind, and the blinding status of analysts was unclear. |
| Incomplete outcome data (attrition bias) | High risk | A total of 64 (15%) participants did not complete the trial. No further details were reported. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | High risk | Potential bias was evident with imbalance in characteristics at randomisation, including previous psychiatric medication use and history of psychiatric care, for which no adjustments were made in the analysis. |
| Methods | Acupuncture vs standard medication (maprotiline) | |
| Participants | Diagnosis: depression Method of diagnosis: ICD‐10 and score > 20 on the Hamilton Depression Rating Scale Age: 18 to 55 years Participant information: 66 men and women Location: outpatients from the Beijing University Mental Health Institute, China Inclusion/Exclusion: Exclusion criteria: none specified. | |
| Interventions | (1) Duration: 6 weeks (36 sessions) Frequency of treatment: 6/week Treatment protocol: Electro‐acupuncture was administered for 45 minutes, 6 times a week, over 6 weeks, through unspecified numerous standardised points. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The medicated group received daily maprotiline at doses ranging from 75 to 250 mg for 6 weeks. | |
| Outcomes | Time points for assessment: baseline and 14, 28, and 42 days from trial entry Outcomes: Hamilton Depression Rating Scale (HAMD) Clinical Global Impression Scale Ashberg Rating Scale for side effects | |
| Notes | ITT was performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details on how the allocation sequence was generated could be obtained from the trial author. |
| Allocation concealment (selection bias) | Unclear risk | No details on the method of concealment used could be obtained from the trial author. |
| Blinding of participants and personnel (performance bias) | High risk | The study participant and the therapist were not blind. |
| Blinding of outcome assessment (detection bias) | Unclear risk | It was unclear whether assessing clinicians and analysts were blinded to the study group. |
| Incomplete outcome data (attrition bias) | Low risk | Complete follow‐up was obtained. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Baseline characteristics show no imbalance between groups. Intention‐to‐treat analysis was performed. The study appears free of other sources of bias. |
| Methods | Manual acupuncture vs medication (fluoxetine) | |
| Participants | Diagnosis: post‐stroke depression Method of diagnosis: Chinese Neuroscience Society diagnostic guidelines Age: not stated Participant information: 170 participants Location: inpatients from Zhongshan Chinese Medicine Hospital, China Inclusion/Exclusion: Exclusion criteria: serious heart, liver, kidney conditions; glaucoma | |
| Interventions | (1) Duration: 8 weeks (48 sessions) Frequency of treatment: 6/week Treatment protocol: The acupuncture intervention consisted of stimulation of the acupuncture points DU26 Ren Zhong, PC6 Neiguan, LIV3 Taichong, HT7 Shenmen, with xing nao kai qiao needling method, with dispersal and regulation of liver qi and calming shen. Additional acupuncture points were added according to the diagnosis. If liver stagnation, diagnosed points TH6 Zhi Gou, LIV 14 Qi men were added. Qi stagnation with stagnation fire, diagnosed points LIV 2 Xing Jian, GB43 Jai xi were used to clear liver and purge fire. Heart and spleen deficiency was diagnosed; points UB15 Xing Shu, UB20 Pi Shu, ST36 Zusanli, SP6 Sanyinjiao were used to strengthen the spleen and nourish the heart. If the spirit was depressed affecting shen, additional points ST36 Zusanli, SP6 Sanyinjiao, and tong li HT5 were used to nourish the heart and calm the shen. Ren zhong was needled towards the nose 5 fen deep using the pecking dispersing method. Zhigou and Neiguan were needled perpendicular 1 cun, via the lifting twirling dispersing method. Xing jian, Jaixi, and Taichong were needled perpendicular 0.5 cun via the twirling dispersing method. Tong li, Shenmen were needled perpendicular via the reinforcing‐reducing manipulation method. Qimen was needled perpendicular 1 cun with the twirling dispersing method. Xingshu and Pishu were needled towards the spine 1 cun, after de qi use of the twirling dispersing method. Zusanli and Sanyinjiao were needle perpendicular 1 cun via the lifting twirling reinforcing method. Needles were retained for 30 minutes. (2) Duration: 8 weeks Frequency of treatment: daily Treatment protocol: The control group received fluoxetine 20 mg/d, taken in the morning. | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Rates of recovery reported as "cured" and "marked" effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation schedule was computer generated. |
| Allocation concealment (selection bias) | Unclear risk | No additional details could be obtained from the trial author. |
| Blinding of participants and personnel (performance bias) | High risk | The study participant and the therapist were not blind. |
| Blinding of outcome assessment (detection bias) | Unclear risk | It was unclear whether assessing clinicians and analysts were blind to study groups. |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up was reported. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Data show no imbalance at randomisation. The study appears free of other sources of bias. |
| Methods | Randomised controlled trial of acupuncture vs medication (amitriptyline) | |
| Participants | Diagnosis: post‐stroke depression Method of diagnosis: CCMD‐3 Age: not stated Participant information: 256 participants Location: inpatients from The First Affiliated Hospital of Tianjin University of Chinese Medicine, China Inclusion/Exclusion: Inclusion criteria: dysphoria as the predominant symptom lasting a minimum of 2 weeks at the same time exhibiting at least 4 of the following symptoms: loss of interest, no feelings of pleasure; reduced concentration and feeling fatigued; slow psychomotor activity; low self‐evaluation or self‐blame or feelings of guilt; cognitive difficulties or self‐aware impairment of association; repetitive thoughts of suicide or inflicting injury to oneself; dyssomnia, e.g. insomnia, waking early, or oversleeping; reduction in appetite or obvious drop in body weight; hyposexuality Exclusion criteria: none stated | |
| Interventions | (1) Duration: 1 month (approximately 60 sessions) Frequency of treatment: twice daily Treatment protocol: Acupuncture points PC6 Neiguan, DU26 Shui guo, DU20 Baihui, M‐HN‐3 Yintang, SP6 Sanyinjiao were selected. Nei guan on both sides was needled perpendicular to a depth of 0.5 to 1 cun, manipulated via the lifting twirling dispersing method for 1 minute. For the first 3 days, needling of Shui guo was towards the mid of the nose to a depth of 5 fen, via the pecking manipulation method. After the first 3 days, Baihui and Yintang were used. Baihui was needled towards the posterior side, to a depth of 5 fen, by a quick twirling tonifying method for 1 minute. Yin tang was needled with the skin pinched, to a depth of 5 fen, via a quick twirling tonifying method, for 1 minute. Sanyinjiao was needled perpendicular to a depth of 0.5 to 1.2 cun by a lifting twirling tonifying method for 1 minute. Each needle was kept in for 20 minutes. (2) Duration: 1 month Frequency of treatment: daily Treatment protocol: The control group received amitriptyline. For the first day, amitriptyline 50 mg was taken orally at night. Subsequently, 1 tablet (25 mg per tablet) was added per day until 200 mg per day was reached. | |
| Outcomes | Time points for assessment: baseline and at 4 weeks Outcomes: Self‐rating Scale of Depression Hamilton Depression Rating Scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No response was received from the trial author in reply to communication sent to request further information on randomisation. |
| Allocation concealment (selection bias) | Unclear risk | No response was received from the trial author in reply to communication sent to request further information on randomisation. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and therapists were not blind to study groups. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The blinding status of assessing clinicians and analysts was unclear. |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up was reported. All participants were included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Data show no imbalance at randomisation. The study appears free of other sources of bias. |
| Methods | Randomised trial of acupuncture or medication (fluoxetine) | |
| Participants | Diagnosis: depression Method of diagnosis: CCMD‐3 Age: not stated Participant information: 80 participants Location: outpatient clinic of Rehabilitation Department at Fosan Shunde Jun’an Hospital, China, from August 2010 to June 2011 Inclusion/Exclusion: Inclusion criteria: aged 18 to 65 years, no schizophrenia; no history and family history of mental disorders. | |
| Interventions | (1) Duration: 6 weeks (45 sessions) Frequency of treatment: daily with a 2‐day interval every 15 days Treatment protocol: Acupuncture group received points: Bihui GV20, YinTang, Sanyinjaio SP6, Taichong LIV3, Neiguan PC6, and Hegu LI4. Acupuncture was given once per day; needles remained for 30 minutes. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: Control received fluoxetine once per day, 20 mg/time. | |
| Outcomes | Time points for assessment: end of intervention Outcomes: HAMD Cured: reduced rate ≥ 75%; remarkably effective: reduced rate ≥ 50% and < 75%; improved: reduced rate ≥ 25% and < 50%; failed: reduced rate < 25% HAMD was classified into 7 categories of factor structures. Of them, a score < 8 indicated normal, in the range from 8 to 18 indicated mild depression, from 18 to 24 indicated moderate depression, and > 24 indicated serious depression. | |
| Notes | ITT was not stated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | High risk | Participants were divided into an acupuncture group (40 cases) and a western medicine group (40 cases). |
| Blinding of participants and personnel (performance bias) | High risk | Participants were not blind. |
| Blinding of outcome assessment (detection bias) | High risk | Assessing clinicians undertook measurements by observation and communication, and therefore were unlikely to be blinded. |
| Incomplete outcome data (attrition bias) | Unclear risk | Six cases: 2 in the acupuncture group, 4 in the control group |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient. |
| Other bias | Unclear risk | Reporting was insufficient. |
| Methods | 60 patients with depression were randomly assigned to the medication group (30 cases) and to the treatment plus medication group (30 cases). | |
| Participants | Diagnosis: clinical depression Method of diagnosis: CCMD‐3 Age: not stated Participant information: 60 men and women Location: inpatients in China Inclusion/Exclusion: Exclusion criteria: depression with psychotic symptoms and organic psychosis; depression caused by mental activity substance and non‐addiction substance; serious physical ailments, organic brain disorder, drug‐ and alcohol‐dependent individuals, and those with allergies | |
| Interventions | (1) Duration: 6 weeks (18 sessions) Frequency of treatment: once every other day, 3 out of 7 days Treatment protocol: Manual acupuncture was administered. Acupuncture points Baihui (GV 20), Yintang (EX‐HN 3), Fengfu (GV16), Dazhui (GV 14), Fengchi (GB 20), Neiguan (PC 6), and Sanyinjiao (SP 6) were administered. (3) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: Control group: paroxetine hydrochloride 20 to 40 mg/d | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD), Self‐rating Depression Scale (SDS), Eisenberg Antidepressant Side Effects Scale (Asberg) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts were reported. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient details were reported. |
| Other bias | Unclear risk | Insufficient details were reported. |
| Methods | Single‐blind randomised controlled trial of acupuncture vs medication (fluoxetine) | |
| Participants | Diagnosis: depression Method of diagnosis: CCMD‐3 and Hamilton Depression Rating Scale with score > 20 Age: not stated Participant information: 110 participants Location: inpatients at hospitals in the Tianjin District, China Inclusion/Exclusion: Exclusion criteria: a history of organic mental disorder; taking psychoactive drugs; schizophrenia and other mental disorders; any heart, liver, kidney, and glaucoma condition | |
| Interventions | (1) Duration: 6 weeks (30 sessions) Frequency of treatment: 5/week Treatment protocol: The aim of treatment was to regulate mental activity and sooth the liver. Acupuncture points DU 20 Baihui, DU16 Fengfu, DU 26 Renzhong, M‐HN‐3 Yintang, M‐HN‐1 Shishengcong, LIV3 Taichong, and UB18 Ganshu were used. Baihui was needled towards anterior, until 1.67 to 2.66 cm of the needle was inserted. Fengfu was needled perpendicular to a depth of 1.67 to 3.33 cm. A reinforcing‐reducing method of needle manipulation was applied for 1 to 2 minutes. Renzhong was needled towards the nose to a depth of 1 to 1.67 cm via a twirling reducing needling method for 1 to 2 minutes. Shishengcong was needled towards Baihui 1.67 to 2.66 cm via twirling reinforcing method. Taichong was needled perpendicular to a depth of 1.67 to 3.33 cm, and Ganshu was needled to a depth of 1.67 to 2.66 cm and was stimulated via a twirling reducing method for 1 to 3 minutes. Needles were retained for 30 minutes each time. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The medication group received fluoxetine 20 mg/d, administered in the morning after meals. Details were not reported on the active control acupuncture group because this form of control did not meet eligibility criteria of the protocol. | |
| Outcomes | Time points for assessment: end of the intervention Outcomes: Hamilton Depression Rating Scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The allocation sequence was computer generated. |
| Allocation concealment (selection bias) | Unclear risk | No details on concealment of the allocation were reported. No response was received from a letter sent to the trial author. |
| Blinding of participants and personnel (performance bias) | High risk | Study participants and therapists were not blind. |
| Blinding of outcome assessment (detection bias) | Unclear risk | It was unclear whether assessing clinicians and analysts were blind to the study group. |
| Incomplete outcome data (attrition bias) | Unclear risk | Seven (6.3%) participants dropped out of the trial. Acupuncture group ‐ 1 participant dropped out owing to work commitments. Second acupuncture group ‐ 1 participant was hospitalised owing to worsening of symptoms. Medication groups ‐ 5 participants dropped out owing to side effects of medication, high cost of treatment, and, in 1 case, for no stated reason. Participants were excluded from the analysis. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Group characteristics were similar at baseline. The study appears free of other sources of bias. |
| Methods | Electro‐acupuncture vs standard medication (fluoxetine or paroxetine) | |
| Participants | Diagnosis: mild, moderate, or severe depression Method of diagnosis: CCMD‐3, HAMD, BDI Age: not stated Participant information: 56 participants Location: inpatients at The First Teaching Hospital of Tianjin Traditional Chinese Medicine College, China Inclusion/Exclusion: Exclusion criteria: none specified | |
| Interventions | (1) Duration: variable ‐ from 2 to 6 weeks Frequency of treatment: daily Treatment protocol: Particpants were randomly allocated to receive electro‐acupuncture or fluoxetine or paroxetine (adequate dose defined). The following acupuncture points were used: GB20 Feng chi, Anmien, M‐HN‐1 Shishencong, M‐HN‐3 Yintang, DU20 Baihui, Ht 7 Shenmen, PC5 Jian Shi, LI4 Hegu, LIV3 Taichong, SP6 Sanyinjiao, GB40 Quixu, GB 8 Shuaigu, and ST36 Zhusanli. All needles were manipulated by a twirling method, with gentle insertion applied on Shenmen. Zhong wan used as a breathing purging method, and electro‐acupuncture was applied to Yintang and Baihui, with the level of stimulation determined by the participant. Needles were left in for 30 minutes, and participants were needled once a day. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The control group received oral fluoxetine or paroxetine 20 mg once a day in the morning. | |
| Outcomes | Time points for assessment: 18 weeks Outcomes: Hamilton Depression Rating Scale Rates of recovery reported as "cured" and "marked" effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information could be obtained from the trial author on how the allocation sequence was generated. |
| Allocation concealment (selection bias) | Unclear risk | The trial author did not respond to letters sent. |
| Blinding of participants and personnel (performance bias) | High risk | Study participants and therapists were not blind. |
| Blinding of outcome assessment (detection bias) | Unclear risk | It was unclear whether assessing clinicians and analysts were blind to the study group. |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up was reported, and all participants were included in the analysis. |
| Selective reporting (reporting bias) | High risk | Data from the Hamilton Depression Rating Scale ‐ but not the Beck Depression Inventory ‐ were reported. |
| Other bias | Low risk | Data show no imbalance in participant characteristics at baseline. The study appears free of other sources of bias. |
| Methods | Randomised controlled trial of TCM manual acupuncture (30 participants) vs control acupuncture (30 participants) via 'off channel' points | |
| Participants | Diagnosis: depression Method of diagnosis: CCMD‐2‐R Age: not stated Participant information: 60 participants Location: unclear setting, China Inclusion/Exclusion: Exclusion criteria: organic cause for depression including schizophrenia, psychosis, or reactive depression; epilepsy; cardiovascular, liver, kidney, circulatory, or gastrointestinal disorders; pregnancy or lactation; any ear infection or damage to the ear; long‐term use of benzodiazepines for insomnia | |
| Interventions | (1) Duration: 12 weeks (24 sessions) Frequency of treatment: 2/week Treatment protocol: Verum acupuncture was performed at Taichong (LR3), Hegu (LI4), Baihui (GV20), and Yintang (EX‐HN3). Ear acupuncture was performed on liver and heart auricular points. Manual stimulation was used for all points and was retained for 30 minutes. (2) Duration: 12 weeks (24 sessions) Frequency of treatment: 2/week Treatment protocol: Sham acupuncture was performed at 'off channel' points, 1 cm to the side of LR3, LI4, GV20, and EX‐HN3, and was retained for 30 minutes. Ear acupuncture was performed on liver and heart auricular points. | |
| Outcomes | Time points for assessment: end of the intervention Outcomes: Hamilton Depression Rating Scale (HAMD) "Cured" rate measured by HAMD reduction > 75% | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random number table was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding of participants and key study personnel was ensured; it is unlikely that the blinding could have been broken. |
| Blinding of outcome assessment (detection bias) | Unclear risk | It was unclear whether assessing clinicians and analysts were blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Missing outcome data were balanced in numbers across intervention groups, and reasons for missing data were similar across groups. |
| Selective reporting (reporting bias) | Unclear risk | Reporting in the paper was insufficient. |
| Other bias | Unclear risk | Reporting in the paper was insufficient. |
| Methods | Acupuncture vs control acupuncture in a double‐blind controlled trial | |
| Participants | Diagnosis: depression Method of diagnosis: DSM‐IV Age: not stated Participant information: 43 men and women (23 to acupuncture and 20 to sham acupuncture) Location: unclear setting, China Inclusion/Exclusion: Exclusion criteria: stroke patients with aphasia, language barrier, cognitive impairment, previous history of depression, needle phobia | |
| Interventions | Both groups were able to continue taking fluoxetine. (1) Duration: 6 weeks (30 sessions) Frequency of treatment: 5 out of 7 days Treatment protocol: Acupuncture: TCM acupuncture. Each treatment lasted 30 minutes. Points Baihui (GV 20), Yintang (EX‐HN 3), Sishencong (EX‐HN 1), Taichong (LR 3), Shenmen (HT7), Neiguan (PC 6), Sanyinjiao (SP 6), Taixi (K 3), and Xinshu (BL 15) were administered. (2) Duration: 6 weeks (30 sessions) Frequency of treatment: 5 out of 7 days Treatment protocol: Sham acupuncture: applied to non‐acupoint points (5 mm lateral to acupoints) via shallow needling technique | |
| Outcomes | Time points for assessment: end of the intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Asberg Antidepressant Side Effect Scale | |
| Notes | ITT was not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) | Low risk | Participants were blind to group allocation. |
| Blinding of outcome assessment (detection bias) | Low risk | Assessing clinicians were blinded; it is unlikely that blinding would have been broken. |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts were reported. |
| Selective reporting (reporting bias) | Unclear risk | Reporting of details was insufficient. |
| Other bias | Unclear risk | Reporting of details was insufficient. |
| Methods | Randomised controlled trial of medication, manual acupuncture plus medication, and electro‐acupuncture plus medication | |
| Participants | Diagnosis: depression Method of diagnosis: ICD‐10 plus a score ≥ 17 on the Hamilton Depression Rating Scale Age: not stated Participant information: 102 men and women (34 cases allocated to each group) Location: China, unclear setting. Inclusion/Exclusion: Exclusion criteria: previous enrolment in other clinical studies within 4 weeks, currently using antidepressants or anxiolytics, suicidal behaviour, cognitive disorders, serious cerebrovascular disease, liver and kidney disease, pregnancy or lactation, inability to comply with research data requirements during intervention or follow‐up phases | |
| Interventions | Both acupuncture groups received the medication. (1) Duration: 6 weeks (18 sessions) Frequency of treatment: once every other day, 3 out of 7 days Treatment protocol: TCM‐style acupuncture was administered. Manual acupuncture to points Baihui (GV 20), Yintang (EX‐HN 3), Fengfu (GV16), Fengchi (GB 20), Dazhui (GV 14), Neiguan (PC 6), and Sanyinjiao (SP 6). Supplementary acupoints were combined according to syndrome differentiation. (2) Duration: 6 weeks (18 sessions) Frequency of treatment: once every other day, 3 out of 7 days Treatment protocol: Electro‐acupuncture stimulation to points Baihui (GV 20) and Yintang (EX‐HN 3) No other needling details were reported. (3) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: Medication group: Seroxat was prescribed for oral administration once per day. | |
| Outcomes | Time points for assessment: end of the intervention Outcomes: Clinical Global Impression Scale (CGI) Quality of life assessed by the WHOQOL | |
| Notes | ITT was not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) | Low risk | 10 participants dropped out, numbers were balanced across groups, reasons were not reported. |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient to allow assessment. |
| Other bias | Unclear risk | Reporting was insufficient to allow assessment. |
| Methods | Randomised controlled trial of acupuncture vs medication (fluoxetine) | |
| Participants | Diagnosis: clinical depression Method of diagnosis: CCMD‐2‐R Age: not stated Participant information: 246 men and women (101 randomised to acupuncture, 145 randomised to control) Location: inpatient, China Inclusion/Exclusion: Exclusion criteria: dementia, deafness, cognitive disorders, communication disorders, family history of mental health disorders | |
| Interventions | (1) Duration: 6 weeks (30 sessions) Frequency of treatment: every other day, 5 out of 7 days Treatment protocol: TCM acupuncture was administered. Manual acupuncture to the following points: Sishengcong (EX‐HN1), Anmian (Extra 8), Neiguan (PC 6), Shenmen (H7), Zusanli (ST36), Sanyinjiao (SP 6), Taichong (Liv3), Zhaohai (K6), Shenmai (B 62) (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: Control group received medication: Prozac 20 mg/d for 6 weeks | |
| Outcomes | Time points for assessment: end of the intervention Outcomes: Hamilton Depression Rating Scale (HAMD) | |
| Notes | ITT was not stated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) | High risk | No other blinding was undertaken. |
| Incomplete outcome data (attrition bias) | Unclear risk | None were reported. |
| Selective reporting (reporting bias) | Unclear risk | Reporting in the paper was insufficient. |
| Other bias | Unclear risk | Reporting in the paper was insufficient. |
| Methods | Randomised controlled trial of acupuncture plus medication vs medication alone | |
| Participants | Diagnosis: clinical depression Method of diagnosis: CCMD‐3, HAMD score ≥ 17 Age: not stated Participant information: 90 men and women (45 in each group) Location: unclear, China Inclusion/Exclusion: Exclusion criteria: physical ailments, organic brain disorder, drug and alcohol addiction, pregnancy or lactation, serious adverse reactions and allergies to medication | |
| Interventions | (1) Duration: 4 weeks (14 sessions) Frequency of treatment: once every other day Treatment protocol: Treatment group comprised medication plus TCM‐style manual acupuncture to Baihui (GV20), Yintang (GV29), Shenting (Bl24), Sishencong (EX‐HN1), and Fengchi (GB20). Each session lasted 30 minutes. (2) Duration: 4 weeks Frequency of treatment: daily Treatment protocol: Control group comprised SSRIs, with use of fluoxetine and paroxetine. | |
| Outcomes | Time points for assessment: end of 1st, 2nd, and 4th weeks of treatment Outcomes: Hamilton Depression Rating Scale (HAMD) VAS for pain assessment Adverse events | |
| Notes | ITT was not stated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts were reported. |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient for assessment. |
| Other bias | Unclear risk | Reporting was insufficient for assessment. |
| Methods | Randomised controlled trial comparing manual acupuncture with SSRI vs SSRI alone | |
| Participants | Diagnosis: clinical depression Method of diagnosis: CCMD‐3 Age: not stated Participant information: 90 male and female participants Location: inpatient setting in China Inclusion/Exclusion: Exclusion criteria: serious body disease, organic brain disease, alcohol or drug dependence, women in gestation or lactation period, inability to tolerate adverse drug reactions, allergic constitution, psychotic symptoms | |
| Interventions | (1) Duration: 4 weeks (14 sessions) Frequency of treatment: once every 2 days Treatment protocol: Manual acupuncture with an SSRI All participants received TCM‐style manual acupuncture for 30 minutes each session. Primary acupuncture points were Baihui (DU20), Yintang (EX‐HN3), Shenting (GV 24), Fengchi (G 20), Dazhui (GV 14), and Sishencong (EX‐HN 1). Supplementary acupoints were combined according to syndrome differentiation. All participants in group 1 also received SSRI treatment in the same fashion as the control group. (2) Duration: 4 weeks Frequency of treatment: daily Treatment protocol: Control group: Participants randomly used 1 type of 5 medicines. Fluoxetine hydrochloride, first day 20 mg/d, other days 20 to 60 mg/d for 4 weeks Paroxetine hydrochloride, first day 20 mg/d, other days 20 to 60 mg/d for 4 weeks Citalopram hydrobromide, first day 20 mg/d, other days 20 to 60 mg/d for 4 weeks Sertraline hydrochloride, first day 20 mg/d, other days 50 to 200 mg/d for 4 weeks Fluvoxamine maleate, first day 20 mg/d, other days 50 to 300 mg/d for 4 weeks | |
| Outcomes | Time points for assessment: 1 week, 2 weeks, 4 weeks (end of treatment) Outcomes: Hamilton Depression Rating Scale (HAMD) | |
| Notes | ITT was not mentioned. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random number table was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not stated. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was reported. |
| Blinding of outcome assessment (detection bias) | High risk | No blinding was reported. |
| Incomplete outcome data (attrition bias) | Unclear risk | Reporting was insufficient. |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient. |
| Other bias | High risk | Sample size calculation was lacking. |
| Methods | Electro‐acupuncture vs amitriptyline | |
| Participants | Diagnosis: clinical depression Method of diagnosis: ≥ 20 on the Hamilton Depression Rating Scale Age: not stated Participant information: 47 men and women Location: unclear setting, China Inclusion/Exclusion: Exclusion criteria: not specified | |
| Interventions | (1) Duration: 5 weeks (30 sessions) Frequency of treatment: 6/week Treatment protocol: Electro‐acupuncture: Two acupuncture points were stimulated: DU20 Baihui and M‐HN‐3 Yintang. Needles were stimulated via electro‐acupuncture. (2) Duration: 5 weeks Frequency of treatment: daily Treatment protocol: Medication (amitriptyline): initial dose 25 mg 3 times a day for 1 week; treatment dose then increased to average dose of 142 mg | |
| Outcomes | Time points for assessment: baseline and end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Clinical Global Impression Chart Asberg Antidepressant Side Effect Scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details on randomisation were provided. |
| Allocation concealment (selection bias) | Unclear risk | No details on randomisation were provided. |
| Blinding of participants and personnel (performance bias) | High risk | Participants were not blind to group allocation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No other details were reported. |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up was reported; all participants were included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Baseline characteristics were similar between groups. The study appears free of other sources of bias. |
| Methods | Electro‐acupuncture vs amitriptyline | |
| Participants | Diagnosis: clinical depression Method of diagnosis: ≥ 20 on the Hamilton Depression Rating Scale Age: 32 to 64 years Participant information: 241 men and women Location: inpatients from 3 psychiatric hospitals in China Inclusion/Exclusion: Exclusion criteria: none specified | |
| Interventions | (1) Duration: 6 weeks (36 sessions) Frequency of treatment: 6/week Treatment protocol: Electro‐acupuncture: Two acupuncture points were stimulated: DU20 Baihui and M‐HN‐3 Yintang. Needles were stimulated via electro‐acupuncture. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: Medication (amitriptyline): initial dose 25 mg 3 times a day for 1 week; treatment dose then increased to 50 mg 3 times a day | |
| Outcomes | Time points for assessment: baseline and end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Clinical Global Impression Chart Asberg Antidepressant Side Effect Scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details on randomisation were provided. |
| Allocation concealment (selection bias) | Unclear risk | No details on randomisation were provided. |
| Blinding of participants and personnel (performance bias) | High risk | Participants were not blind to group allocation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No other details were reported. |
| Incomplete outcome data (attrition bias) | Unclear risk | No loss to follow‐up was reported. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Unclear risk | It is unclear whether the study was free of other sources of bias. |
| Methods | Electro‐acupuncture plus placebo tablets vs amitriptyline versus electro‐acupuncture and amitriptyline | |
| Participants | Diagnosis: clinical depression Method of diagnosis: ≥ 20 on the Hamilton Depression Rating Scale Age: not stated Participant information: 29 men and women Location: closed ward at Beijing Medical University Hospital Inclusion/Exclusion: Inclusion criteria: drug free the week before start of the trial Exclusion criteria: none specified | |
| Interventions | (1) Duration: 6 weeks (36 sessions) Frequency of treatment: 6/week Treatment protocol: Electro‐acupuncture group: Two acupuncture points were stimulated: DU20 Baihui and M‐HN‐3 Yintang. Needles were stimulated via electro‐acupuncture for 45 minutes; the current was 3 to 5 mA at a frequency of 2 Hz. (2) Duration: 6 weeks (36 sessions) Frequency of treatment: daily Treatment protocol: Amitriptyline group: Participants taking medication received an average dose of 161 mg per day. | |
| Outcomes | Time points for assessment: baseline and end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Clinical Global Impression Chart Asberg Antidepressant Side Effect Scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details on randomisation were provided. |
| Allocation concealment (selection bias) | Unclear risk | No details on randomisation were provided. |
| Blinding of participants and personnel (performance bias) | High risk | Participants were not blind to group allocation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Assessing clinicians were blind to study groups; no other details were provided. |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up was reported; all participants were included in the analyses. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Unclear risk | It was unclear whether the study was free of other sources of bias. |
| Methods | Three‐armed randomised controlled trial comparing auricular acupuncture vs auricular acupuncture with TCM psychotherapy vs Deanxit | |
| Participants | Diagnosis: depression after breast cancer surgery Method of diagnosis: CCMD‐3 and SDS score ≥ 53 Age: not stated Participant information: 90 participants Location: inpatient setting, China Inclusion/Exclusion: Exclusion criteria: patient major life events affected by mood change over recent 5 years; severe mental illness with self‐injury and recent suicidal behaviour; a history of alcohol or drug abuse within 3 months; severe heart, brain, vascular, liver, kidney, haematopoietic system diseases; breast cancer metastasis | |
| Interventions | (1) Duration: 4 weeks Frequency of treatment: unclear Treatment protocol: Auricular acupuncture with indwelling needles for 4 weeks. These were changed once a week, alternating between each ear. Each day, participants were instructed to press and stimulate the indwelling needles for 3 to 5 minutes each time, 3 to 5 times per day. Auricular points used were Xin (CO15), Shen (CO10), Gan (CO12), Shenmen (TF4), Pizhixia (AT4), and Neifenmi (CO18). In addition to auricular therapy, group 1 received a TCM emotion intervention, which was poorly described. (2) Duration: 4 weeks Frequency of treatment: unclear Treatment protocol: Group 2 received the same treatment as Group 1 without the additional emotion intervention. (3) Duration: 4 weeks Frequency of treatment: unclear Treatment protocol: Control group: Deanxit (flupentixol 0.5 mg and melitracen 10 mg): 1 tablet per day for 4 weeks Comparisons were made between group 2 and the control group. | |
| Outcomes | Time points for assessment: end of treatment and 4 weeks after end of treatment Outcomes: SDS score Cured rate based on changes in SDS score | |
| Notes | ITT was not discussed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not stated. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was reported. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Patient‐reported outcomes were included; therefore blinding was not applicable. |
| Incomplete outcome data (attrition bias) | Unclear risk | Reporting was insufficient. |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient. |
| Other bias | High risk | Sample size calculation was lacking. |
| Methods | Randomised controlled trial of acupuncture vs medication (fluoxetine) | |
| Participants | Diagnosis: clinical depression Method of diagnosis: CCMD‐3 Age: not stated Participant information: 60 participants (acupuncture ‐ 31, fluoxetine ‐ 29) Location: unclear setting, China Inclusion/Exclusion: Exclusion criteria: depression from an organic cause, "depression caused by mental activity substance" | |
| Interventions | (1) Duration: 6 weeks (30 sessions) Frequency of treatment: 5 out of 7 days Treatment protocol: TCM‐style manual acupuncture was delivered for 30 minutes. Acupuncture points used on all participants included BL13, BL14, BL15, BL17, BL18, BL19, and BL20. LR3 and SP6 or HT7 and SP6 could be added based on TCM pattern differentiation. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The control group received fluoxetine hydrochloride capsules, 20 mg per day for 6 weeks. | |
| Outcomes | Time points for assessment: 2, 4, and 6 weeks Outcomes: Hamilton Depression Rating Scale (HAMD) Recovered vs not recovered based on Hamilton Depression Rating Scale Adverse event reporting | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) | Unclear risk | Reporting in the paper was insufficient. |
| Selective reporting (reporting bias) | Unclear risk | Reporting in the paper was insufficient. |
| Other bias | Unclear risk | Reporting in the paper was insufficient. |
| Methods | Randomised controlled trial of paroxetine, verum acupuncture + paroxetine, and electroacupuncture + paroxetine | |
| Participants | Diagnosis: clinical depression Method of diagnosis: ICD‐10 and score ≥ 17 on the Hamilton Depression Rating Scale Age: 18 to 60 years Participant information: 157 participants (drug control (paroxetine, n = 48), verum acupuncture (verum acupuncture + paroxetine, n = 53), and electro‐acupuncture (electro‐acupuncture + paroxetine, n = 56)) Location: inpatient setting, China Inclusion/Exclusion: Exclusion criteria: bipolar depression, other clinical trial participation within last 4 weeks, taking or coming off antidepressant drugs, pregnant, lactating, planned suicide. | |
| Interventions | The verum acupuncture and electro‐acupuncture groups were treated with paroxetine combined with acupuncture. (1) Duration: 6 weeks (18 sessions) Frequency of treatment: every second day, 3/week Treatment protocol: Electro‐acupuncture group Baihui, Yintang, and bilateral Fengchi were stimulated with Han's acupoint nerve stimulator (LH202H; Beijing, China). The positive electrode of 1 set of electric wires was connected to Baihui, and the negative electrode was connected to Yintang; the other set of wires was connected to bilateral Fengchi, with positive and negative electrodes alternated between left and right sides at each treatment. A disperse‐dense wave ‐ 2/15 Hz ‐ was used, and the current was controlled within tolerance (skin micromovement). Each electro acupuncture lasted for 30 minutes. (2) Duration: 6 weeks (18 sessions) Frequency of treatment: every second day, 3/week Treatment protocol: Verum acupuncture group: The needle was left in place for 30 minutes at the other acupoints, with needling once after 15 minutes for 5 to 10 seconds. The principal points ‐ acupoints of co‐ordination, needles, acupuncture methods, and duration of treatment ‐ were the same as for both groups. Acupoints: Baihui and Yintang were the principal points; Fengfu (GV16), bilateral Fengchi (GB20), Dazhui (GV14), bilateral Neiguan (PC6), and bilateral Sanyinjiao (SP6) were the acupoints of co‐ordination, selected according to current data on acupoints for treatment of individuals with clinical depression. (3) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: Control: Participants in the drug control group were treated with paroxetine. The drug dose was 10 mg/d for the first 2 days, then 20 mg/d until the end of treatment, administered orally once per day after breakfast. | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) WHOQOL Scale | |
| Notes | ITT was not stated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The sequence was computer generated. |
| Allocation concealment (selection bias) | Low risk | Central randomisation was performed. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding of participants was reported. |
| Blinding of outcome assessment (detection bias) | High risk | No blinding of assessing clinicians was reported. |
| Incomplete outcome data (attrition bias) | Unclear risk | Thirty participants withdrew from the study, leaving 127 cases (38 drug control, 45 verum acupuncture, and 44 electro‐acupuncture) in the final analysis. “Subjects who withdrew from the study were excluded”. “Treatment was terminated in subjects with poor compliance, who did not undergo acupuncture according to regulations, who experienced physiopathological changes, who was intolerant of or hypersensitive to paroxetine, who developed adverse effects or who may have become pregnant during the treatment". |
| Selective reporting (reporting bias) | Unclear risk | Insufficient details were reported. |
| Other bias | Unclear risk | Insufficient details were reported. |
| Methods | Randomised controlled 3‐arm parallel study of acupuncture plus usual care, counselling plus usual care, or usual care alone | |
| Participants | Diagnosis: depression Method of diagnosis: Beck Depression Inventory scoring ≥ 20, diagnosed by the GP Age: over 18 years Participant information: 755 participants Location: community, United Kingdom Inclusion/Exclusion: Excluson criteria: receiving acupuncture or counselling at the time; terminal illness; significant learning disabilities; haemophilia; hepatitis; HIV; pregnancy; confounding psychiatric conditions (bipolar disorder, postpartum depression, adjustment disorder, psychosis, dementia, or personality disorder). Patients who had suffered a close personal bereavement or given birth during the previous 12 months were also excluded. | |
| Interventions | (1) Duration: 3 months (12 sessions) Frequency of treatment: approximately once per week Treatment protocol: Acupuncture: Traditional Chinese Medicine (TCM) style. On average, 13 needles were inserted per session (range 3 to 26). Average number of sessions per week, 0.74. Average number of weeks between sessions, 1.36. Average duration of session, 53 minutes (range 28 to 95 minutes). 246 different points were used. Common points were SP‐6, LIV‐3, ST‐36, and LI‐4, which were used within a course of treatment for 91%, 89%, 83%, and 74% of participants, respectively. Manual methods: tonifying (68%), reducing (43%), even method (55%). The response sought varied, most commonly, de qi by 96% of acupuncturists. Acupuncturist: British Acupuncture Council members, with more than 3 years' post‐qualification experience (2) Duration: 3 months Frequency of treatment: approximately once per week Treatment protocol: Counselling: Counseling will be provided by members of the British Association of Counseling and Psychotherapy, who used primarily a non‐directive approach. Counsellors (3) Duration: 3 months Frequency of treatment: N/A Treatment protocol: Usual care: Usual GP care was available to all participants according to need. | |
| Outcomes | Time points for assessment: baseline and 3, 6, 9, and 12 months Outcomes: PHQ‐9 BDI‐II SF‐36 bodily pain subscale EQ‐5D Texted mood scores were collected weekly over the first 15 weeks. Medication and health service were used. | |
| Notes | ITT was reported and performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer randomisation was provided by the York Trials Unit. |
| Allocation concealment (selection bias) | Low risk | Central randomisation was performed. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding of participants was reported. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Patient‐reported outcomes were measured; therefore blinding was not applicable. Analysts were blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Missing data have been imputed by appropriate methods. At 3 months, 3 withdrew from acupuncture, 21 from counselling, and 3 from usual care. |
| Selective reporting (reporting bias) | Low risk | Protocol was available. |
| Other bias | Low risk | The study appears free of other sources of bias. |
| Methods | Randomised controlled trial of TCM‐style acupuncture vs medication (fluoxetine hydrochloride) | |
| Participants | Diagnosis: clinical depression Method of diagnosis: CCMD‐3‐R, HAMD score ≥ 18 Age: not stated Participant information: 120 participants (acupuncture ‐ 62, fluoxetine hydrochloride ‐ 58) Location: unclear setting, China Inclusion/Exclusion: Exclusion criteria: cardiovascular, liver, or kidney disease or falling sickness (as per Chinese translation); pregnancy or lactation; drug dependence; severe mental disorder | |
| Interventions | (1) Duration: 6 weeks (30 sessions) Frequency of treatment: 5/week Treatment protocol: TCM‐style manual acupuncture was delivered for 30 minutes. Acupuncture points used on all participants were BL13, BL14, BL15, BL17, BL18, BL19,and BL20. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The control group received fluoxetine hydrochloride capsules, 20 mg per day. | |
| Outcomes | Time points for assessment: baseline and 2, 4, and 6 weeks Outcomes: Hamilton Depression Rating Scale (HAMD) Effectiveness rates based on changes in HAMD scores | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random number table was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) | Unclear risk | Study did not address this outcome. |
| Selective reporting (reporting bias) | Unclear risk | Reporting in paper was insufficient. |
| Other bias | Unclear risk | Reporting in paper was insufficient. |
| Methods | Randomised controlled trial of manual acupuncture compared with fluoxetine (Prozac) | |
| Participants | Diagnosis: clinical depression Method of diagnosis: CCMD‐3 Age: not stated Participant information: 40 men and women Location: mixed inpatient and outpatient setting, China Inclusion/Exclusion: Exclusion criteria: none stated | |
| Interventions | (1) Duration: 60 sessions Frequency of treatment: unclear Treatment protocol: TCM acupuncture: Each session lasted 45 minutes. Manual acupuncture was administered with stimulation to points Baihui (GV20) and Shenmen (H7). Other auxiliary acupuncture points were used according to differentiation, although this was not stated. Method of stimulation included a technique of reinforcing deficiency and reducing excess. (1) Duration: unclear Frequency of treatment: daily Treatment protocol: Control: Prozac 20 mg/d over the course of the intervention | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) | |
| Notes | ITT was not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts were reported, |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient. |
| Other bias | Unclear risk | Reporting was insufficient. |
| Methods | Randomsied controlled group of electro‐acupuncture, manual acupuncture, or medication (paroxetine) | |
| Participants | Diagnosis: clinical depression Method of diagnosis: ICD‐10 diagnosis for depression with moderate to severe symptoms with score ≥ 17 on the Hamilton Depression Rating Scale Age: not stated Participant information: 160 participants Location: outpatient acupuncture clinic of Southern Medical University, First Affliated Hospital of Jinan University, and Guangdong 999 Brain Hospital, China Inclusion/Exclusion: Exclusion criteria: unstable medical condition; a history of brain injury or surgery; suicidal attempts or aggressive behaviour; a history of manic, hypomanic, or mixed episode illness; comorbidity with other neuropsychiatric disorders; a family history of mental illness; investigational drug treatment within the previous 6 months; a history of alcohol or drug abuse within the previous 12 months; pregnancy or lactation; current cognitive‐behavioural therapy or other behavioural therapies | |
| Interventions | All groups received paroxetine. Acupuncture procedure was performed in the treatment room by experienced acupuncturists (JQC and GLL) who had received 5 years of undergraduate training in Chinese medicine and had practiced Chinese medicine over 3 years. To ensure consistency in the acupuncture procedure, acupuncturists attended a training workshop to establish the acupuncture protocol before the study began. (1) Duration: 6 weeks (18 sessions) Frequency of treatment: 3/week Treatment protocol: Manual acupuncture: Manual manipulation was conducted and needling sensation was generally achieved within 2 minutes after the manipulation. After the needling sensation was achieved, needles were retained for 30 minutes and were manipulated once again during retaining to maintain needling sensation. Point selection: Baihui (GV20), Yintang (EXHN3), Fengfu (GV16), Dazhui (GV14), bilateral Fengchi (GB20), bilateral Neiguan (PC6), and bilateral Sanyinjiao (SP6) (2) Duration: 6 weeks (18 sessions) Frequency of treatment: 3/week Treatment protocol: Electro‐acupuncture: Electrical stimulation was delivered between Baihui (Du20) and Yintang (EX‐HN3) and bilateral Fengchi (GB20), with continuous waves at alternating low (2 Hz) and high (100 Hz) frequency via Han’s Acupuncture Nerve Stimulator (H.A.N.S., mode code: LH202H). Point selection: Baihui (GV20), Yintang (EXHN3), Fengfu (GV16), Dazhui (GV14), bilateral Fengchi (GB20), bilateral Neiguan (PC6), and bilateral Sanyinjiao (SP6) (3) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: Paroxetine: The PRX dose was initiated at 10 mg/d and was escalated to 20 mg/d within 1 week based on individual participant response. The PRX dose would be further increased if psychiatrists believed that participants' symptoms were aggravated. The maximum dose was set at 40 mg/d. | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) BDI Self‐reported depression Adverse events. | |
| Notes | ITT was undertaken and reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Non‐sequential random numbers were generated in advance by a computer programme (SPSS version II). |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes were used. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and acupuncturists were not blind. |
| Blinding of outcome assessment (detection bias) | Low risk | The principal investigator, the data collector, and the analysts were blind. |
| Incomplete outcome data (attrition bias) | Low risk | Missing data have been imputed by appropriate methods. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Unclear risk | Reporting was insufficient. |
| Methods | Single‐blind randomised controlled trial of laser acupuncture vs control laser acupuncture | |
| Participants | Diagnosis: clinical depression Method of diagnosis: clinical assessment of depression and BDI score of 12 to 30 Age: not stated Participant information: 30 men and women Location: community setting, Australia Inclusion/Exclusion: Exclusion criteria: chronic depression over 2 years; hypomania; psychosis or drug abuse; taking psychotropic drugs over the previous 3 months; pregnancy; a history of endocrine disorders; suicidal disorder | |
| Interventions | Acupuncture was performed by a fellow of the Australian Medical Acupuncture College. A low‐level laser unit was used. A flick switch was installed ‐ numbered 1 and 2 by the manufacturer. The laser unit beeped and flashed for both groups. (1) Duration: 8 weeks (12 sessions) Frequency of treatment: twice weekly for first 4 weeks, then weekly Treatment protocol: Acupuncture treatment was administered on the basis of TCM diagnosis and was individualised and based on syndrome. Most common diagnosis pattern liver qi stagnation or liver qi deficiency. Treatment was individualised. Classical alarm points were used: Qi Men Liv 14 (on the right), CV14 Ju Que,15, HT 7 Shenmen, and LIV 8 Qu Quan Other points included Kd10 Yin Gu, LI4 Hegu, SP6 San Yin Jao, and GV20 Baihu. No co‐interventions were allowed. The laser was applied to each point for 5 seconds, delivering 0.5 J. Total delivered: 3 to 4 J per session (2) Duration: 8 weeks (12 sessions) Frequency of treatment: twice weekly for first 4 weeks, then weekly Treatment protocol: The control group received inactive laser. | |
| Outcomes | Time points for assessment: 4 and 8 weeks, with follow‐up BDI through a mail‐out at 12 and 20 weeks following randomisation Outcomes: BDI Hamilton Depression Rating Scale (HAMD) Adverse events questionnaire | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was generated from "lot drawing" based on equal numbers of red and green beans placed in a closed jar with a small hole in the lid. The research assistant randomly selected 1 bean to determine group allocation. |
| Allocation concealment (selection bias) | Low risk | Coding of group allocation was determined by a flip of the coin and was known only by the manufacturer until the data had been analysed. |
| Blinding of participants and personnel (performance bias) | Low risk | Participants and the acupuncturist were blind to group allocation. |
| Blinding of outcome assessment (detection bias) | Low risk | The research assistant and the analyst were blind to group allocation. |
| Incomplete outcome data (attrition bias) | High risk | Four (13%) participants discontinued the intervention ‐ 2 in each group ‐ owing to illness, decreased mood, and relocation. One participant in the control group was lost to follow‐up. Data analysed: 14/16 treatment, 12/14 control |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Data show no imbalances at randomisation. The study had no other sources of bias. |
| Methods | Randomised double‐blind RCT of laser acupuncture vs control laser | |
| Participants | Diagnosis: major depressive disorder Method of diagnosis: DSM‐IV Age: 18 to 50 years Participant information: 47 participants Location: community setting, Sydney, Australia Inclusion/Exclusion: Inclusion criteria: need to be free of herbal medication and psychotropic drugs in the last 4 weeks. Exclusion criteria: duration of depression greater than 2 tears; a history of hypomania or mania, substance abuse disorders; known central nervous system lesions; known uncontrolled endocrine disorders; pregnancy or potential pregnancy; active suicidal tendencies. | |
| Interventions | Both laser units had a concealed section with a flick switch numbered by the manufacturer as‘A’ and ‘B’ ‐ 1 of which was the placebo option, known only to the project manager (JAH) and the manufacturer. The control panel of the laser units beeped and a red light flashed when the laser probe button appeared on either A or B. Each unit was separately set up for placebo or laser options. (1) Duration: 8 weeks (12 sessions) Frequency of treatment: 2/week for 4 weeks, once a week for another 4 weeks Treatment protocol: Laser acupuncture: Laser acupuncture 100 Mw low‐intensity infrared (808 nm) units were produced and followed the Moxla protocol. The laser probe was fully in contact (perpendicular to the skin surface) to avoid scatter of the laser beam. Points used were LR14, CV14, LR8, HT7, and KI3. (2) Duration: 8 weeks (12 sessions) Frequency of treatment: 2/week for 4 weeks, once a week for another 4 weeks Treatment protocol: Control laser acupuncture: The placebo group received inactive laser. Points used were LR14, CV14, LR8, HT7, and KI3. | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Remission defined as score ≤ 7 on HAMD or ≤ 5 on QIDS | |
| Notes | ITT analysis was undertaken and reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computer‐generated sequence was used. |
| Allocation concealment (selection bias) | Low risk | Sealed and opaque envelopes were used. |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding of participants and key study personnel was ensured, and it is unlikely that the blinding could have been broken. Blinding of participants: The percentages of participants in the active group that offered guess ‘active’, ‘placebo’, and ‘unsure’ were 65.2%, 30.4%, and 4.3%. In the placebo group, corresponding percentages were 60.0%, 30.0%, and 10.0%. These differences between groups were not statistically significant. |
| Blinding of outcome assessment (detection bias) | Low risk | Assessing clinicians and analysts were blind to treatment allocation. |
| Incomplete outcome data (attrition bias) | Low risk | Three in the treatment group and 1 in the control group discontinued. Missing outcome data were balanced in numbers across intervention groups, and reasons for missing data were similar across groups; plausible effect size (difference in means or standardised difference in means) among missing outcomes was not enough to have a clinically relevant impact on observed effect size. |
| Selective reporting (reporting bias) | Low risk | Study protocol was available. |
| Other bias | Unclear risk | Available information was insufficient for assessment. |
| Methods | Single‐blind placebo‐controlled trial of medication vs acupuncture plus medication vs medication plus control acupuncture | |
| Participants | Diagnosis: clinical depression Method of diagnosis: DSM‐IV, score > 18 on the Hamilton Depression Rating Scale Age: 20 to 70 years Participant information: 70 participants Location: inpatient setting, Germany Inclusion/Exclusion: Exclusion criteria: suicidal behaviour, diagnosis of schizophrenia or bipolar affective disorder or delusions; coagulation disease; wound healing disease; emphysematous thorax; abnormal blood cell count; serious liver and kidney disease; epilepsy | |
| Interventions | Up to 20 mg/d diazepam was allowed if required in all groups. (1) Duration: 4 weeks Frequency of treatment: daily Treatment protocol: Mianserin (90 to 120 mg/d) (2) Duration: 4 weeks Frequency of treatment: daily medication, 3/week acupuncture Treatment protocol: Mianserin (90 to 120 mg/d) plus verum acupuncture. A standardised acupuncture treatment was applied 3 times a week over 4 weeks. Points included were U.B.15, U.B.17, BL.18, H7, P6, St40, Sp5, Sp6, and Lu1. Needles were retained for 30 minutes. (3) Duration: 4 weeks Frequency of treatment: daily medication, 3/week acupuncture Treatment protocol: Mianserin (90 to 120 mg/d) plus control acupuncture | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Global Assessment Scale Melancholia Scale Clinical Global Impressions Scale Mean dosage of medication collected Self‐reported improvement | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details on how the allocation sequence was generated could be obtained from the trial author. |
| Allocation concealment (selection bias) | Unclear risk | No details could be obtained from the trial author. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Study participants may have been blinded. No data were provided to verify whether participants were blind to being allocated to acupuncture or placebo acupuncture. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Assessing clinicians were blind, and it is unclear whether the analyst was blind. |
| Incomplete outcome data (attrition bias) | Low risk | No losses to follow‐up were reported. All participants were included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Data show no imbalance in baseline characteristics between groups. The study appears free of other sources of bias. |
| Methods | Single‐blind randomised controlled trial of manual acupuncture vs medication (amitriptyline) | |
| Participants | Diagnosis: post‐stroke depression Method of diagnosis: CCMD Age: not stated Participant information: 256 participants Location: inpatients from a hospital setting in Tian jin, China Inclusion/Exclusion: Exclusion criteria: impaired speech, impaired consciousness, history of organic metal illness | |
| Interventions | (1) Duration: 30 days (30 sessions) Frequency of treatment: daily Treatment protocol: The intervention of manual acupuncture points used points PC6 Nei guan, GV26 Shui guo, DU20 Baihui, M‐Hn‐3 Yintang, and SP6 Sanyinjiao. The form of needling stimulation was described as locating Neiguan on both sides, perpendicular insertion of the needle to a depth of 13 to 25 mm; the needles were manipulated with twirling lifting method for 1 minute. For the first 3 days, the acupuncture point Shui Gou was used, with needling towards the nose, via a pecking method of needle manipulation. The following 3 days, the acupuncture points Yintang and Baihui were stimulated. These points were needled towards the posterior side to a depth of 13 mm. Manipulation of the needle used the frequent twirling reinforcing method for 1 minute. Sanyinjiao was needled to a depth of 13 to 44 mm with a twirling reinforcing method for 1 minute. Needles were left in for 20 minutes. (1) Duration: 30 days Frequency of treatment: daily Treatment protocol: The control group received amitriptyline. A dose of 50 mg/d was taken orally at night; 3 days later, the dose was increased by 25 mg every day until a dose of 200 mg was administered. | |
| Outcomes | Time points for assessment: 8 weeks Outcomes: Improvement was assessed as cured, marked effect, improved, or no effect. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The allocation sequence was computer generated. |
| Allocation concealment (selection bias) | Unclear risk | The trial author did not respond to a letter sent to request further details on trial methods. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and the therapist were not blind |
| Blinding of outcome assessment (detection bias) | Unclear risk | It was unclear whether assessing clinicians and analysts were blind to study group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up was reported. |
| Selective reporting (reporting bias) | Unclear risk | No protocol was available. Data on study outcomes were reported; however the instrument used was unclear. |
| Other bias | Low risk | Baseline characteristics were similar. The study had no other major sources of bias. |
| Methods | Randomised controlled trial comparing 2 different types of electro‐acupuncture vs medication (fluoxetine hydrochloride) | |
| Participants | Diagnosis: clinical depression Method of diagnosis: CCMD‐2, HAMD score ≥ 17 Age: not stated Participant information: 90 participants Location: unclear setting, China Inclusion/Exclusion: Exclusion criteria: diagnosis of depression, with HAMD scores < 17; other serious primary diseases, such as heart disease, hepatic disease, renal disease, and haematopoietic system disease; psychiatric patients; pregnancy or lactation; non‐co‐operative patients; definitive diagnosis of infectious disease | |
| Interventions | (1) Duration: 6 weeks (30 sessions) Frequency of treatment: 5/week Treatment protocol: Group 1 received TCM‐style electro‐acupuncture. Acupuncture points used were Baihui (DU20) and Sanyinjiao (SP6). (2) Duration: 6 weeks (30 sessions) Frequency of treatment: 5/week Treatment protocol: Group 2 also received TCM‐style electro‐acupuncture in a similar manner to group 1 but using Taichong (LR 3),Sanyinjiao (SP 6), Neiguan (PC 6), and Shenmen (HT 7). (3) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The control group received Prozac (fluoxetine) 20 mg/d. | |
| Outcomes | Time points for assessment: 2, 4, and 6 weeks Outcomes: Hamilton Depression Rating Scale (HAMD) Recovered vs not recovered scores calculated on the basis of changes in HAMD | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) | Low risk | Missing outcome data were balanced in numbers across intervention groups, and reasons for missing data were similar across groups. |
| Selective reporting (reporting bias) | Unclear risk | Reporting in the paper was insufficient. |
| Other bias | Unclear risk | Reporting in the paper was insufficient. |
| Methods | Propective randomised controlled trial of acupuncture vs medication (fluoxetine) | |
| Participants | Diagnosis: clinical depression Method of diagnosis: DSM‐IV via a standard clinical interview and score ≥ 20 on the Hamilton Depression Rating Scale Age: 18 to 70 years Participant information: 75 participants Location: outpatients in the Department of Acupuncture, Beijing Hospital of Traditional Chinese Medicine, China Inclusion/Exclusion: Exclusion criteria: psychiatric illness, mental retardation, alcohol or drug abuse, severe somatic illness, positive medical history for cerebral disease, obesity, history of infection, known autoimmune disease, electroconvulsive therapy, immunosuppressive agents or immunostimulants used within 6 months, pregnancy or breastfeeding | |
| Interventions | Acupuncture interventions for treatment and control groups were manipulated by the same acupuncturists, who had 5 years of training in acupuncture and TCM and more than 2 years of clinical experience. For both groups 1 and 2, the needles at Baihui (DU20) and Zusanli (ST36) or of Taichong (LR3) and Sanyinjiao (SP6) were connected to an electro‐acupuncture apparatus (KWD‐808 II Acupuncture Stimulator; Great Wall brand, Shanghai, China), with a frequency of 3 Hz and continuous waves based on patient tolerance. EA was applied for 30 minutes at a time. (1) Duration: 6 weeks (30 sessions) Frequency of treatment: 5/week Treatment protocol: Electro‐acupuncture at the acupoints of Baihui (DU20) and Zusanli (ST36) (2) Duration: 6 weeks (30 sessions) Frequency of treatment: 5/week Treatment protocol: Electro‐acupuncture control group at the acupoints of Taichong (LR3), Sanyinjiao (SP6), Neiguan (PC6), and Shenmen (HT7) (3) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: Fluoxetine (20 mg/d) for 6 weeks | |
| Outcomes | Time points for assessment: 0 (baseline) and 2, 4, and 6 weeks after treatment Outcomes: Hamilton Depression Rating Scale (HAMD) Treatment response was defined as ≥ 50% reduction in HAMC score, and great improvement was defined as final HAMD score ≤ 15. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computer‐generated list was used. |
| Allocation concealment (selection bias) | Low risk | Opaque envelopes with information describing group allocation were transferred to another nurse, who was not involved in the study; these were sequentially numbered. |
| Blinding of participants and personnel (performance bias) | High risk | Participants were not blind; no other details were provided. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No other details were provided. |
| Incomplete outcome data (attrition bias) | High risk | 14 participants dropped out: 5 from the EA treatment group and 9 from the EA control group. Among the 5 dropouts from the EA treatment group, 4 had no reason for refusing to participate in the study, and 1 refused because she was scared of having blood drawn. Among 9 dropouts from the EA control group, 4 had no reason for refusing to participate in the study, and the other 5 refused owing to fear of drawing blood for testing. |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient. |
| Other bias | Unclear risk | Reporting was insufficient. |
| Methods | Randomised controlled trial examining effects of manual acupuncture plus medication (fluoxetine) vs medication alone for treatment of individuals with post‐stroke depression | |
| Participants | Diagnosis: post‐stroke depression Method of diagnosis: CCMD‐3, HAMD ≥ 8 Age: not stated Participant information: 63 men and women Location: inpatient setting, China Inclusion/Exclusion: Exclusion criteria: serious disuse; aphasia; memory loss; impaired hearing or understanding or cognitive issues; cerebral hernia or severe heart, liver, kidney, or haematopoietic system disease; depression, anxiety, and a history of mental illness or suicidal disorder before stroke; taking all kinds of calming, psychotropic drugs; a history of alcohol dependence; obvious cognitive impairment by MMSE | |
| Interventions | (1) Duration: 4 weeks (24 sessions) Frequency of treatment: 6/week Treatment protocol: TCM‐style manual acupuncture for 40 minutes each session. Acupuncture points used were primary point: Baihui (DU20); Fengfu (DU16); Shenting (GV 24); Shuigou (DU26); Dazhui (DU14); and Shendao (DU11). Supplementary acupoints were combined according to syndrome differentiation. All participants in group 1 received the same medication as the control group. (2) Duration: 4 weeks Frequency of treatment: daily Treatment protocol: Control group: fluoxetine 20 mg/d for 4 weeks | |
| Outcomes | Time points for assessment: 2 weeks and at end of treatment Outcomes: Hamilton Depression Rating Scale (HAMD) Cured rate based on HAMD scores | |
| Notes | ITT was not mentioned. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random number generator was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not stated. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was reported. |
| Blinding of outcome assessment (detection bias) | High risk | No blinding was reported. |
| Incomplete outcome data (attrition bias) | Unclear risk | Reporting was insufficient. |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient. |
| Other bias | High risk | Sample size calculation was lacking. |
| Methods | Randomised controlled trial comparing manual TCM acupuncture vs medication (Deanxit (Flupentixol + Melitracen)) | |
| Participants | Diagnosis: clinical depression Method of diagnosis: CCMD‐3, HAMD score ≥ 20 Age: not stated Participant information: 41 participants Location: unclear setting, China Inclusion/Exclusion: Exclusion criteria: not reported in the paper | |
| Interventions | (1) Duration: 20 days (20 sessions) Frequency of treatment: daily Treatment protocol: TCM‐style manual acupuncture was delivered for 20 minutes. Acupuncture points used were Baihui (GV20), Yintang (EX‐HN3), Taiyang (EX‐HN5), Shuaigu (GB8), Fengchi (GB20), Fengfu (GV16), Shuigou (DU26), Hegu (LI4), Neiguan (PC6), Quchi (LI11), Sanyinjiao (SP6), Taichong (LR3), and Zusanli (ST36). (2) Duration: 20 days Frequency of treatment: daily Treatment protocol: The medication control group received Deanxit (Flupentixol + Melitracen) 1 tablet twice per day for 10 days, then 1 tablet daily for another 10 days. | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Cured rates also reported, but source of these unclear | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Drawing of lots was described. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) | Unclear risk | The study did not address this outcome. |
| Selective reporting (reporting bias) | Unclear risk | Reporting in the paper was insufficient. |
| Other bias | Unclear risk | Reporting in the paper was insufficient. |
| Methods | Randomised controlled trial comparing manual acupuncture plus medication (SSRI) vs an SSRI alone | |
| Participants | Diagnosis: major depressive disorder Method of diagnosis: ICD‐9, HAMD score ≥ 18 Age: not stated Participant information: 76 participants Location: inpatient department of medical psychology at Nanjing Brain Hospital between April and November 2006 Inclusion/Exclusion: Exclusion criteria: SSRI or acupuncture treatment for depression in the past 3 months; severe medical disease; a history of brain stroke or other mental health disorders; pregnancy or breastfeeding | |
| Interventions | Both acupuncture and medication control groups received an SSRI ‐ fluoxetine (20 mg once per day), paroxetine (20 mg once per day), or duloxetine (40 mg twice daily). (1) Duration: 6 weeks (30 sessions) Frequency of treatment: 5/week Treatment protocol: Acupuncture treatment: Acupuncture points used for all participants were GV24 (Shenting), GV20 (Baihui), GV14 (Dazhui), and GV4 (Mingmen). Additional points were used according (TCM) differentiation for depression with the 4 diagnostic methods including tongue and pulse once a week, and additional points were changed accordingly: Liver depression and Spleen deficiency, add LR3 (Taichong), SP9 (Yinlingquan); Liver Qi stagnation, add LR3, LR14 (Qimen); Heart and Spleen deficiency, add HT7 (Shenmen) and ST36 (Zusanli); Liver and Kidney Yin deficiency, add KI3 (Taixi) and LR3; Spleen and Kidney Yang deficiency, add CV4 and CV6. In addition, according to individual symptoms, extra points could be applied: insomnia and forgetfulness, add HT7 and An’mian (Ext); palpitations and chest tightness, add PC6 (Neiguan); constipation, add ST25 (Tianshu) and ST37 (Shangjuxu). After achieving de qi needling sensation, the Dao qi technique was used. Acupuncture was applied at the 4 key acupuncture points. This manipulation involved lifting‐thrusting and rotating the needle with light and smooth stimulation. The amplitude was 1 to 2 mm; the needle rotation angle was < 90°, and frequency was 60 to 100 times per minute for 1 to 2 minutes. GV14 and GV4 were needled in a sitting position, with 5 minutes of retention before the needles were removed. All acupuncture treatments were delivered by a senior acupuncturist (TW) with 15 years’ clinical experience and certified by the China Association of Acupuncture and Moxibustion. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The medication control group received the SSRI alone. | |
| Outcomes | Time points for assessment: 1, 2, 4, and 6 weeks after the start of the intervention Outcomes: Hamilton Depression Rating Scale (HAMD) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | Low risk | Randomisation was conducted via sequentially numbered and sealed opaque envelopes, prepared in advance. |
| Blinding of participants and personnel (performance bias) | Low risk | Healthcare staff, apart from the acupuncturist, were blinded to group allocation before each participant was enrolled. |
| Blinding of outcome assessment (detection bias) | Low risk | All assessments were carried out by trained psychiatrists who were blinded to group allocation. |
| Incomplete outcome data (attrition bias) | Unclear risk | Reporting was insufficient. |
| Selective reporting (reporting bias) | High risk | The study report fails to include results for a key outcome that would be expected to have been reported for such a study. |
| Other bias | Low risk | The study appears free of other sources of bias. |
| Methods | Randomised controlled trial comparing manual acupuncture vs psychological intervention and health education | |
| Participants | Diagnosis: clinical depression Method of diagnosis: SDS score between 50 and 70 Age: not stated Participant information: 44 participants Location: outpatient setting, China Inclusion/Exclusion: Exclusion criteria: severe heart, lung, liver, or kidney disease; osteoarthritis; rheumatoid arthritis; gouty arthritis; a cardiac pacemaker; stroke followed by haemorrhagic infarction, moyamoya disease, subarachnoid haemorrhage, cerebral haemorrhage, brain tumour, brain trauma, etc.; not completing the self‐rating depression scale; low compliance with treatment | |
| Interventions | (1) Duration: 8 weeks (16 sessions) Frequency of treatment: 2/week Treatment protocol: Group 1 received TCM‐style manual acupuncture and moxibustion. Treatment was given for 30 minutes per session. Acupuncture points used were Baihui (DU20); Shenting (GV 24); Sishencong (EX‐HN 1); Hegu (LI4); Zusanli (ST36); Taichong (LR3); Guanyuan(CV4); Zhongwan(CV12); and Shenque(CV8). Indirect moxibustion was used above Guanyuan (CV4); Zhongwan (CV12); and Shenque (CV8) for 5 minutes. (2) Duration: 8 weeks Frequency of treatment: unclear Treatment protocol: Group 2 was given unspecified health maintenance education and psychological intervention. | |
| Outcomes | Time points for assessment: end of intervention Outcomes: SDS score | |
| Notes | ITT was not stated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The sequence was computer generated. |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes were used. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was reported. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Patient‐reported outcomes were reported; therefore blinding was not applicable. |
| Incomplete outcome data (attrition bias) | Unclear risk | Reporting was insufficient. |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient. |
| Other bias | Low risk | The study appears free of other sources of bias. |
| Methods | Randomised controlled trial of acupuncture vs medication (fluoxetine hydrochloride) | |
| Participants | Diagnosis: clinical depression Method of diagnosis: CCMD‐2‐R, HAMD score > 17 Age: 19 to 51 years Participant information: 62 participants with duration of depression ranging from 6 months to 6½ years Location: inpatient and outpatient departments of the Second Clinical Medical College of Guanzhou University of TCM, China Inclusion/Exclusion: Exclusion criteria: severe organic disease | |
| Interventions | (1) Duration: 8 weeks (56 sessions) Frequency of treatment: daily Treatment protocol: Acupuncture based on TCM syndrome differentiation. The main syndromes were Heart and Spleen deficiency, Spleen and Kidney Yang deficiency, and a disorder of the Chong and Ren meridians. The main acupuncture points were Hegu LI4, Taichong LR 3, Baihui GV 20, and Yintang EX‐HN‐3. Other adjunct points included Xinshu (Bl15) or Jueyinshu BL14 (implanted intradermal needle). Ear points were Xin (MA‐IC), Dannang (EX‐LE 6), and Ershenmen (MA‐TF 1) implanted ring headed thumbtack needle for insomnia. Shenmen HT7, Sanyinjiao (SP6) was added for Heart and Spleen deficiency. Shenmen (HT 7) and Qiuxu (GB 40) was used for timidity due to heart qi deficiency. Sanyinjiao (SP 6) was added for liver qi stagnation and spleen deficiency. Taixi (KI 3), Daling (PC7), and Yinbai (SP1) were used for a disturbance of the mind by accumulated phlegm. Gongsun (SP4) and Lieque (LU7) supplemented a disorder of the Chong and Ren meridians. Qi was obtained. Needles were retained for 30 minutes. (2) Duration: 8 weeks Frequency of treatment: daily Treatment protocol: The control group was administered fluoxetine hydrochloride 20 mg per day. | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) A score of cured was defined as greater than 75% improvement. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation sequence was generated by the study statistician, who produced a computer‐generated list. |
| Allocation concealment (selection bias) | Unclear risk | No details on allocation were reported. |
| Blinding of participants and personnel (performance bias) | High risk | It was not feasible to blind participants and therapists. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No details were provided on the blinding status of assessing clinicians and analysts. |
| Incomplete outcome data (attrition bias) | Low risk | No participants were lost to follow‐up; all participants were analysed. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Data show no imbalance in baseline characteristics. The study appears free of other sources of bias. |
| Methods | Pilot randomised controlled trial of acupuncture vs control acupuncture | |
| Participants | Diagnosis: mixed anxiety and depression Method of diagnosis: clinical interview schedule revised Age: > 18 years Participant information: 19 participants Location: 7 general practices in the UK Inclusion/Exclusion: Exclusion criteria: a history of substance abuse, brain damage, other psychiatric disorder preceding the onset of depression, in receipt of concurrent alternative treatment, talking therapy for repression, pharmacological treatments for more than 3 months in the past year | |
| Interventions | (1) Duration: 12 sessions Frequency of treatment: unclear Treatment protocol: Manual acupuncture: delivered by a TCM practitioner with 10 years' clinical experience. A formula of points plus 2 discretionary points was used. Choice of points and needle depth were individualised according to TCM principles and body mass of the participant. Needles were retained for 20 minutes. (2) Duration: 12 sessions Frequency of treatment: unclear Treatment protocol: The control group received sham acupuncture. Sham acupuncture involved actual shallow needling but at sites unrelated to depression. Points were reported on the Web appendix. No needle stimulation was provided, and de qi was avoided. Needles were retained for 20 minutes. | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Beck Depression Inventory Rand 36‐Item Survey | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | It is unclear how the randomisation sequence was generated. |
| Allocation concealment (selection bias) | Low risk | The allocation sequence was concealed via off‐site central randomisation. |
| Blinding of participants and personnel (performance bias) | Low risk | Participants and researchers were blind to group allocation. Participants were asked about their perception of the group to which they were allocated. Blinding was maintained. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Assessing clinicians were blind to group allocation. It is unclear whether analysts were blind to group allocation. |
| Incomplete outcome data (attrition bias) | High risk | Five (26%) participants did not complete all acupuncture sessions. Three (50%) participants in the sham group did not comply with treatment. Two participants in the sham group were lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | High risk | Data show imbalances between groups at randomisation with regard to age and BDI. No other sources of bias are evident. |
| Methods | Randomised controlled trial of TCM‐style manual acupuncture vs medication (paroxetine) | |
| Participants | Diagnosis: breast cancer with comorbid depression Method of diagnosis: CCMD‐3, SDS score between 50 and 69 Age: not stated Participant information: 60 women Location: mixed inpatient and outpatient setting, China Inclusion/Exclusion: Exclusion criteria: pregnancy or breastfeeding, organic cause for depression such as schizophrenia, severe infection, or abuse of/dependence on psychoactive substances | |
| Interventions | (1) Duration: 8 weeks (40 sessions) Frequency of treatment: 5/week Treatment protocol: TCM‐style manual acupuncture was delivered for 30 minutes. Acupuncture points used included Taichong (LIV3), Hegu (LI4), and Baihui (DU20) with the even‐reinforcing method, and Zusanli (ST36) and Qihai (REN6) with the twirling reinforcing method. Auricular acupressure with Semen Vaccariae was also applied to liver, spleen, and endocrine points unilaterally, alternating sides every 4 days. (2) Duration: 8 weeks Frequency of treatment: daily Treatment protocol: The medication control group received paroxetine hydrochloride capsules, 20 mg per day. | |
| Outcomes | Time points for assessment: 4 and 8 weeks Outcomes: Hamilton Depression Rating Scale (HAMD) Reported effectiveness rates based on changes in HAMD scores | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) | Unclear risk | The study did not address this outcome. |
| Selective reporting (reporting bias) | Unclear risk | Reporting in the paper was insufficient. |
| Other bias | Unclear risk | Reporting in the paper was insufficient. |
| Methods | Single‐blind randomised controlled trial of acupuncture vs medication (amitriptyline) | |
| Participants | Diagnosis: clinical depression Method of diagnosis: Hamilton Depression Rating Scale (HAMD) Age: not stated Participant information: 41 participants Location: inpatient and outpatient clinics at Beijing Medical University, China Inclusion/Exclusion: Exclusion criteria: none reported | |
| Interventions | (1) Duration: 6 weeks (36 sessions) Frequency of treatment: 6/week Treatment protocol: Mixed manual acupuncture and electro‐acupuncture: Acupuncture points DU 24 Shenting, DU20 Baihui, DU14 Dazhui, DU12 Shenzhu, Conception Vessel 17 Shanzong, CV14 Juque Ren, GB 20 Fengchi, and PC6 Neiguan. Additional acupuncture points were used depending on the Chinese medical diagnosis. For stagnation of Liver Qi ST23 Taiyi, SP6 Sanyinjiao and LIV3 Taichong were used. For Stagnation of Liver Blood LI4 Hegu, LIV3 Taichong and SP10 Xuehai were used. For Spleen and Heart Deficiency, HT7 Shenmen, PC7 Daling, SP6 Sanyinjiao, and ST36 Zusanli were used. For Spleen and Kidney Yang Deficiency, KD3 Taixi, SP6 Sanyinjiao, ST36 Zusanli, and CV4 Guanyuan were used. Needles were inserted bilaterally and were stimulated manually, except for DU 24 and DU 20, which were stimulated by electro‐acupuncture (frequency 80 to 100/s). (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The control group received 25 mg of amitriptyline on the first day; the dose was increased by 25 to 50 mg each day up to 150 mg. In the second week, the dose was adjusted according to response and side effects but ranged from 150 mg to 300 mg daily. | |
| Outcomes | Time points for assessment: weekly until the end of the intervention Outcomes: Hamilton Depression Rating Scale (HAMD) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | It is unclear how the allocation sequence was generated. |
| Allocation concealment (selection bias) | Unclear risk | It is unclear whether concealment of the randomisation schedule was adequate. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and therapists were not blind to group allocation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | It is unclear whether assessing clinicians and analysts were blind to group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | Follow‐up was complete; all participants were included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Unclear risk | Information was insufficient for judgement. |
| Methods | Randomised controlled trial comparing manual acupuncture and electro‐acupuncture in combination with medication (SSRI) vs SSRI alone | |
| Participants | Diagnosis: clinical depression Method of diagnosis: CCMD‐3, HAMD score ≥ 17 Age: not stated Participant information: 75 participants Location: unclear setting, China Inclusion/Exclusion: Exclusion criteria: physical ailments, organic brain disorders, substance dependence, had taken hormones, nerve blockers or immunomodulating drugs in the past month | |
| Interventions | All groups received an SSRI such as citalopram, paroxetine, or fluoxetine at the standard daily oral dose. (1) Duration: 6 weeks (18 sessions) Frequency of treatment: 3/week Treatment protocol: A manual TCM‐style acupuncture intervention was delivered for 30 minutes. Acupuncture points included Baihui (GV20), Yintang (EX‐HN3), Shenting (GV24), Fengchi (GB20), Dazhui (GV14), Shengdao (GV11), and Zhiyang (GV9). (2) Duration: 6 weeks (18 sessions) Frequency of treatment: 3/week Treatment protocol: The electro‐acupuncture intervention was identical to the manual acupuncture intervention except that electro‐acupuncture was performed between GV20 and EX‐HN‐3. (3) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The control medication group received only the SSRI. | |
| Outcomes | Time points for assessment: 1, 2, 4, and 6 weeks Outcomes: Hamilton Depression Rating Scale (HAMD) Reported effectiveness scores based on changes in HAMD | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random number table was used. |
| Allocation concealment (selection bias) | Low risk | Central randomisation was used. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) | Unclear risk | The study did not address this outcome. |
| Selective reporting (reporting bias) | Unclear risk | Reporting in the paper was insufficient. |
| Other bias | Unclear risk | Reporting in the paper was insufficient. |
| Methods | Single‐blind randomised controlled trial of electro‐acupuncture vs medication (amitriptyline) | |
| Participants | Diagnosis: clinical depression Method of diagnosis: CCMD, HAMD score > 20 Age: not stated Participant information: 30 participants Location: inpatients at Anning Hospital, Tianjin, China Inclusion/Exclusion: Exclusion criteria: none reported | |
| Interventions | (1) Duration: 30 days (30 sessions) Frequency of treatment: daily Treatment protocol: Electro‐acupuncture: administered to 2 acupuncture points: DU20, Baihui, and M‐NH‐3 Yingtang. Needles were Inserted to a depth of 1 cun and were connected to the electro‐acupuncture machine, Model G605. A strong current was delivered to generate visible observation of muscle pulsation, with a threshold of frequency of 80 to 90 times/min. Needles were retained for 1 hour. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The control group received amitriptyline. For the first week, 250 mg per day was administered, medication was taken 3 times a day according to severity and side effects reported by the participant, and dosage was adjusted accordingly. The. average dose was 130 mg a day (suboptimal dose). | |
| Outcomes | Time points for assessment: 6 weeks post trial entry Outcomes: Hamilton Depression Rating Scale (HAMD) Improvement in depression measured subjectively by reporting on the number of participants cured | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | It is unclear how the randomisation sequence was generated. |
| Allocation concealment (selection bias) | Unclear risk | No response was received from the trial author when further details of randomisation were requested. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and therapists were not blind. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Assessing clinicians were blind to group allocation; it is unclear whether analysts were blind to study group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up was reported. All participants were included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Groups were comparable at baseline. No other sources of bias were apparent. |
| Methods | Randomised controlled trial comparing electro‐acupuncture, minimal acupuncture, and control acupuncture | |
| Participants | Diagnosis: major depressive disorder Method of diagnosis: DSM‐IV, HAMD score ≤ 18 Age: not stated Participant information: 78 Chinese participants recruited through referrals from psychiatrists and advertisements at the clinic Location: outpatient clinic of the Department of Psychiatry at Queen Mary Hospital, a regional teaching hospital in Hong Kong Inclusion/Exclusion: Inclusion criteria: (1) ethnic Chinese; (2) age 18 to 65 years; (3) chief complaint of insomnia; (4) previous diagnosis of MDD based on DSM‐IV criteria, as assessed by a clinician; (5) 17‐item Hamilton Depression Rating Scale (HAMD17) score ≤ 18 at screening and baseline; (6) taking the same antidepressants at a fixed dose for 12 weeks before baseline Exclusion criteria: (1) symptoms suggestive of specific sleep disorders, as assessed by the Insomnia Interview Schedule, a semistructured face‐to‐face interview; (2) significant risk of suicide; (3) previous diagnosis of schizophrenia, other psychotic disorders, bipolar disorder, or alcohol or substance use disorder; (4) pregnancy or breastfeeding, or woman of childbearing potential not using adequate contraception; (5) valvular heart defects or bleeding disorders or taking anticoagulant drugs; (6) infection or abscess close to the site of selected acupoints; (7) any serious physical illness; (8) taking Chinese herbal medicine or over‐the‐counter drugs intended for insomnia. Also, an apnoea‐hypopnoea index ≥ 10 or a periodic limb movement disorder index with arousal ≥ 15, as assessed by overnight polysomnography in a subgroup of participants who consented to the investigation | |
| Interventions | Participants were advised to continue the same type and dosage of antidepressants throughout the study period. Sedatives, anxiolytics, and hypnotics could be continued during the study period, but dose escalation was disallowed. All acupuncture treatments were performed in a quiet treatment room by the same acupuncturist. (1) Duration: 3 weeks (9 sessions) Frequency of treatment: 3/week Treatment protocol: Electroacupuncture group: needled for 30 minutes at Yintang (EX‐HN3) and Baihui (GV20), and bilateral Ear Shenmen, Sishencong (EX‐HN1), and Anmian (EX), with disposable acupuncture needles. De qi was achieved if possible. Needles were held in place with surgical tape or hair pins. Electro‐acupuncture was delivered via a constant‐current, 0.45‐ms square wave pulse at 4 Hz. (2) Duration: 3 weeks (9 sessions) Frequency of treatment: 3/week Treatment protocol: Minimal acupuncture group: needled superficially at bilateral “Deltoideus” (in the middle of the line of insertion of Binao LI14 and acromion), “Forearm” (1 inch lateral to the middle point between Shaohai HE3 and Shenmen HE7), “Upper arm” (1 inch lateral to Tianfu LU3), and “Lower leg” (0.5 inch dorsal to Xuanzhong GB39) De qi was avoided during needling. Acupuncturist, setting, number of points needled, electrostimulation, treatment frequency, and duration of treatment were the same as in the electro‐acupuncture group. (3) Duration: 3 weeks (9 sessions) Frequency of treatment: 3/week Treatment protocol: Placebo acupuncture group: treated at the same acupoints as the electro‐acupuncture group with placebo needles. Placebo needles were placed 1 inch beside the acupoints to avoid acupressure effect. The needles were then connected to the electric stimulator, but with zero frequency and amplitude. Treatment frequency and duration of treatment were the same as in the electro‐acupuncture group. | |
| Outcomes | Time points for assessment: 1 and 4 weeks post treatment Outcomes: Hamilton Depression Rating Scale (HAMD) Recorded changes in quality of life and adverse events from acupuncture | |
| Notes | ITT analysis was used. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence was used. |
| Allocation concealment (selection bias) | Low risk | Central randomisation was used. |
| Blinding of participants and personnel (performance bias) | High risk | Participants were blinded to group allocation, but no data on the success of blinding were collected; therefore it is possible that blinding was not successful. |
| Blinding of outcome assessment (detection bias) | Low risk | Assessment of depressive symptoms, past psychiatric history, and antidepressant treatment history was conducted by a clinician. Analysis of questionnaires, sleep diaries, and actigraphy results was conducted by independent investigators, who were blinded to participants' group allocation. The HAMD was administered by an experienced psychiatrist (KCT), who was blind to treatment allocation. |
| Incomplete outcome data (attrition bias) | Low risk | Missing outcome data were balanced in numbers across intervention groups, and reasons for missing data were similar across groups; 7 participants (9.0%) dropped out during the treatment period, and 3 participants (3.8%) withdrew from the study at 4‐week follow‐up. Data show no difference in attrition rates among groups at 1‐week and 4‐week follow‐up (P > 0.05; Fisher exact test). |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Data show no significant between‐group differences in sociodemographic and clinical features, nor in pharmacotherapy. |
| Methods | Randomised trial of electro‐acupuncture or medication (amitriptyline) | |
| Participants | Diagnosis: clinical depression Method of diagnosis: CCMD‐2, HAMD score > 20 Age: 12 to 50 years Participant information: 460 participants. The duration of depression ranged from 6 months to 4 years. Location: inpatients and outpatients from Sichuan Province, China Inclusion/Exclusion: Exclusion criteria: none reported | |
| Interventions | (1) Duration: 3 weeks (unclear) Frequency of treatment: 6/week Treatment protocol: Two primary groups of acupuncture points were administered to participants. First, Baihui DU20, Laogong PC8, and Yongquan KI 1. Other points included Shuugou DU26, Hegu LI 4, and Taichong LIV3. Additional combined points were administered. For participants with palpitations, insomnia, and vexation, Xinshu Bl15, Fengchi GB20, Neiguan PC6, and Shenmen HT7 were added. For participants with stomach ache, poor appetite, and abdominal distension, Zusanli ST36, Pishu BL20, and Weishu BL21 were added. The 2 groups of acupuncture points were used alternatively. Acupuncture needles were inserted to a depth 0.5 to 1.0 cun. An ML8804 electro‐acupuncture unit was applied with output of 50 to 100 Hz, wave width 200 micros, and a current of 2 to 3 mA. The needles were stimulated until muscles trembled slightly, then were manipulated by a reinforcing‐reducing technique for 30 to 60 minutes. (2) Duration: 3 weeks Frequency of treatment: daily Treatment protocol: For the medication group, amitriptyline was given at 25 mg 3 times a day in the first week. Subsequent doses were modified after the first week, with an average dose of 150 mg per day administered over 3 weeks. All participants received psychological treatment for 3 weeks. | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) The following outcomes were also described. Cured clinical symptoms disappeared with no sign of relapse after 2 to 3 weeks. Marked effect: Clinical symptoms were eased with occasional emotional fluctuation. Improvement: Clinical symptoms improved with some mental fluctuation. Failure: no improvement was seen. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details on the method of randomisation were reported. |
| Allocation concealment (selection bias) | Unclear risk | Details on randomisation were not confirmed by the trial author. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and therapists were not blind to group allocation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | It was unclear whether assessing clinicians and analysts were blind to group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up was reported, and all participants were included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Groups were comparable at baseline. The study appears free of other sources of bias. |
| Methods | Randomised controlled trial of TCM‐style acupuncture vs medication (paroxetine) | |
| Participants | Diagnosis: clinical depression Method of diagnosis: CCMD‐2‐R, HAMD score ≥ 17 Age: not stated Participant information: 86 participants Location: outpatient setting, China Inclusion/Exclusion: Exclusion criteria: depression due to organic causes | |
| Interventions | (1) Duration: 30 to 40 days (30 to 40 sessions) Frequency of treatment: daily Treatment protocol: TCM‐style manual acupuncture was delivered for 20 to 30 minutes. Acupuncture points included Baihui (GV20), Yintang (EX‐HN3), Shenmen (HT7), Neiguan (PC6), and Taichong (LR3). Other points were added on the basis of syndrome differentiation. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The control medication group received paroxetine at 20 mg once per day for 6 weeks. | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Reported effectiveness scores based on changes in HAMD | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random number table was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) | Low risk | No data were missing. |
| Selective reporting (reporting bias) | Unclear risk | Reporting in the paper was insufficient. |
| Other bias | Unclear risk | Reporting in the paper was insufficient. |
| Methods | Single‐blind randomised controlled trial of electro‐acupuncture plus medication (paroxetine) vs medication for participants with clinical depression | |
| Participants | Diagnosis: clinical depression Method of diagnosis: CCMD‐3, HAMD score > 17 Age: not stated Participant information: 42 participants Location: inpatients at hospital in Hubei, China Inclusion/Exclusion: Exclusion criteria: previous suicide attempts, pregnancy or breastfeeding, dependence on drugs or alcohol | |
| Interventions | Both groups received medication. (1) Duration: 6 weeks (36 sessions) Frequency of treatment: 6/week Treatment protocol: Electro‐acupuncture group: Dominant acupoints were Baihui (DU20) and Yintang (EXHN3). Bilateral auxiliary points were Neiguan (PC6), Waiguan (SJ5), Shenmen (HT7), Hegu (LI4), Taichong (LR3), Zusanli (ST36), Fenglong (ST40), Sanyinjiao(SP6), Taiyuan (LU9), etc. (sic). Needles were connected to the electro‐acupuncture machine ‐ type g6805 ‐ and needle stimulation was administered at 2 Hz frequency, with sparse‐dense wave, 6 volts, applied to produce stimulation within the participant's comfort level. EA was applied for 30 minutes. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The control group received paroxetine 10 to 40 mg daily. | |
| Outcomes | Time points for assessment: 2, 4, and 6 weeks Outcomes: Hamilton Depression Rating Scale (HAMD) Side effects ratings | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | It is unclear how the randomisation sequence was generated. |
| Allocation concealment (selection bias) | Unclear risk | It was not reported whether concealment of the allocation sequence was adequate. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and therapists were not blind. |
| Blinding of outcome assessment (detection bias) | Unclear risk | It is unclear whether assessing clinicians and analysts were blind to study group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | No losses to follow‐up were reported. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Data show no differences between groups at baseline. The study appears free of other sources of bias. |
| Methods | Randomised controlled trial comparing TCM‐style manual acupuncture vs medication (amitriptyline) | |
| Participants | Diagnosis: clinical depression Method of diagnosis: CCMD‐2‐R, HAMD ≥ 20 Age: not stated Participant information: 100 participants Location: China, outpatient setting. Inclusion/Exclusion: Exclusion criteria: immune modulators or hormone preparations within the past 6 months, acute or chronic infection, trauma, recent inflammation or fever, known food or drug allergy | |
| Interventions | (1) Duration: 28 sessions Frequency of treatment: not stated Treatment protocol: TCM‐style manual acupuncture was delivered for 20 minutes. Acupuncture points used were Neiguan (PC6), Fengchi (GB20), Sanyinjiao (SP6), and Baihui (GV20). (2) Duration: not stated Frequency of treatment: daily Treatment protocol: The control medication group received amitriptyline 25 mg 3 times per day for 7 days. The dosage was then altered based on symptoms and adverse reactions. The average dosage was 150 mg per day. | |
| Outcomes | Time points for assessment: 2 and 4 weeks of treatment Outcomes: Hamilton Depression Rating Scale (HAMD) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | High risk | An open allocation sequence was used. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) | Unclear risk | The study does not address this outcome. |
| Selective reporting (reporting bias) | Unclear risk | Reporting in the paper was insufficient. |
| Other bias | Unclear risk | Reporting in the paper was insufficient. |
| Methods | Randomised controlled trial of acupuncture plus medication (fluoxetine) vs control acupuncture plus medication | |
| Participants | Diagnosis: major depressive disorder Method of diagnosis: DSM‐IV, HAMD score > 14 Age: 18 and 60 years Participant information: 80 men and women Location: outpatient recruitment from psychiatric hospital and general hospital, China Inclusion/Exclusion: Exclusion criteria: acute suicidality; substance abuse or dependence; receiving electroconvulsive treatment; previous acupuncture experience; diagnosis of schizoaffective or bipolar affective disorder, coagulation disease, abnormal blood cell count, pregnancy, serious liver or kidney disease; epilepsy history | |
| Interventions | Before administration of fluoxetine, a minimum 1‐week placebo washout was required, with 3 weeks for patients receiving monoamine oxidase inhibitors; then all patients were reevaluated, with HRSD as the baseline depressive score. Two licensed acupuncturists with 3 months of formal research training, in practice 3 to 5 years, delivered the intervention. Fluoxetine and placebo (sugar) tablets were identical in appearance and taste, and were administered as a morning dose. During the 6‐week randomised phase, the dose regimen guideline was 1 fluoxetine pill (10 mg) plus 1 placebo pill a day in group 1, or 2 fluoxetine pills (20 mg) a day in group 2, for the first 2 weeks, followed by 1 fluoxetine pill (10 mg) plus 2 placebo pills a day in group 1, or 3 fluoxetine pills (30 mg) a day in group 2, for the next 4 weeks. Zolpidem (up to 10 mg prn at bedtime) for insomnia was permitted during the trial. (1) Duration: 6 weeks (30 sessions) Frequency of treatment: 5/week Treatment protocol: Acupuncture treatment based on TCM standardised protocol via published books/relevant literature: Acupuncture points were GV20, ExHN1 Sishencong, Yintang Ex HN3, GV26 Shuogou, PC6 Neiguan, H7 Shen men, Liv3, and LI4. 15 needles were inserted. Needle manipulation included manual reinforcing reducing, de qi with needling of each point retained for 30 minutes. (2) Duration: 6 weeks (30 sessions) Frequency of treatment: 5/week Treatment protocol: Sham: needled at non‐specific locations in the neighbourhood (1 to 3 cm, not recognised as true acupoints or meridians) of the loci cited above, merely pricking the skin superficially (1 to 4 mm deep). The same sham points were used during each treatment session. Shallow superficial insertion of the needle along with a minimum of needle sensation was emphasized. Minimum manual stimulation was applied to the needles. | |
| Outcomes | Time points for assessment: baseline and 2, 4, and 6 weeks of treatment Outcomes: Hamilton Depression Rating Scale (HAMD) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified randomisation schedule was based on severity of depression (HRSD score < 21 or ≥ 21). Random number tables were used. |
| Allocation concealment (selection bias) | Unclear risk | These assignments were generated from a closed list of random numbers by a biostatistician not involved in conducting the trial, and were transmitted to a psychiatric nurse not otherwise involved in the clinical trial |
| Blinding of participants and personnel (performance bias) | Low risk | All participants were informed that they would receive 2 indistinguishable but different‐style acupuncture treatments for depression. Although the 2 interventions were described to participants as ‘‘traditional acupuncture’’ or ‘‘non‐traditional acupuncture’’ on informed consent forms, participants were not told to which group they were assigned. For the sake of blinding, each participant was required to lie in bed completely relaxed, with eyes closed during the treatment process. |
| Blinding of outcome assessment (detection bias) | Low risk | The treatment group was concealed from psychiatrists, other care providers, and research raters. |
| Incomplete outcome data (attrition bias) | Low risk | Missing data were balanced between groups. Treatment: 1 physical disease, 1 lack of response. Sham: 1 given herbs, 2 lack of response, 1 arrhythmia. |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient. |
| Other bias | Low risk | No differences in baseline or power analysis were reported. |
| Methods | Parallel RCT of acupuncture vs acupuncture control | |
| Participants | Diagnosis: major depressive disorder Method of diagnosis: DSM‐IV, HAMD score > 18 and Clinical Global Impression‐Severity (CGI‐S) score > 4 Age: 25 to 65 years Participant information: 70 participants Location: outpatient setting, Hong Kong Inclusion/Exclusion: Exclusion criteria: (1) unstable medical conditions; (2) suicide attempts or aggressive behaviours; (3) history of manic, hypomanic, or mixed episode; (4) family history of bipolar or psychotic disorder; (5) a history of substance abuse within the previous 12 months; (6) investigational drug treatment in the previous 6 months; (7) current psychotropic treatment exceeding 1 week; (8) needle phobia | |
| Interventions | Unmedicated participants in both groups received orally administered fluoxetine for 3 weeks in an open manner. The dose was initiated at 10 mg/d and was escalated to an optimal dose within 1 week on the basis of individual participants' responses, with a maximum dose of 40 mg/d. Those currently treated with fluoxetine for no longer than 1 week continued their medication at the same dose. Those currently treated with other psychotropic medications for no longer than 1 week were required to be switched to the fluoxetine regimen by gradual withdrawal of drugs within 1 week to wash out potential ‘‘carryover’’ effects. Concomitant use of other psychotropic drugs was not allowed. To ensure consistency in acupuncture procedures, the principal investigator (Z.J.Z.) provided a training workshop on the acupuncture protocol. Acupuncture intervention was performed by registered acupuncturists (W.W. and S.C.M.) who had received 5‐year undergraduate training in Chinese medicine and had practiced Chinese medicine over 3 years. (1) Duration: 3 weeks (9 sessions) Frequency of treatment: 3/week Treatment protocol: Dense cranial electro‐acupuncture stimulation (DCEAS) is a novel stimulation mode by which electrical stimulation is delivered through dense acupoints located on the forehead mainly innervated by the trigeminal nerve, efficiently modulating multiple central transmitter systems via the trigeminal sensory‐brainstem NA and 5‐HT neuronal pathways. For DCEAS, the following 6 matches of forehead acupoints innervated by the trigeminal nerve via inserted or non‐inserted needles were used: Baihui (Du‐20) and Yintang (EXHN3), left Sishencong (EX‐HN1) and Toulinqi (GB15), right Sishencong (EX‐HN1) and Toulinqi (GB15), bilateral Shuaigu (GB8), bilateralTaiyang (EX‐HN5), and bilateral Touwei (ST8). Electrical stimulation was delivered to the 6 points. Electrical stimulation with continuous waves at 2 Hz and constant current and voltage (9 V) was delivered via an acupuncture stimulation instrument (Hwarto, SDZ‐II) for 30 minutes (pulse width could not be determined by this model instrument). Selection of this stimulation mode was based on the fact that low frequency could exert broader effects on central neurochemical systems compared with high frequency; this mode has been widely introduced into treatment for those with neuropsychiatric disorders. The intensity of stimulation was adjusted to a level at which participants felt most comfortable. (2) Duration: 3 weeks (9 sessions) Frequency of treatment: 3/week Treatment protocol: Non‐invasive electro‐acupuncture (n‐EA) control procedure with Streitberger’s non‐invasive needle was used. The needles with blunt tips were quickly put onto the same acupoints used in DCEAS without insertion into the skin. These needles were then affixed with plastic O‐rings and adhesive tapes. Electrical stimulation was delivered based on the same parameters as were used in DCEAS. Participants felt the stimulation via blunt tips touched on the skin. | |
| Outcomes | Time points for assessment: baseline and days 3, 7, 14, and 21 Outcomes: Hamilton Depression Rating Scale (HAMD) Clinical Global Impression Scale (CGI) Safety assessed by the TESS | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly assigned to n‐EA or DCEAS treatment at a ratio of 1:1, via a random block scheme from an automatic computer programme (SPSS version 2). |
| Allocation concealment (selection bias) | Unclear risk | Assignment was done in a single‐blind manner, by which random codes were known only by the acupuncturists. |
| Blinding of participants and personnel (performance bias) | Low risk | The validity of the participant‐blind design was ensured by a sham acupuncture procedure performed at the forehead acupoints, which were outside the visual field of participants. To minimise expected effects, participants were not told during random assignment about potential responses to control and DCEAS procedures. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Raters were blind to treatment allocation; it is unclear whether analysts were blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Missing outcome data were balanced in numbers across intervention groups, and reasons for missing data were similar across groups. Three withdrew from the control group ‐ 1 medical emergency, 1 loss to follow‐up, and 1 severe headache. Seven withdrew from treatment ‐ 2 losses to follow‐up, 3 medical emergencies, and 2 intolerance to acupuncture. |
| Selective reporting (reporting bias) | Low risk | The 3 primary measures from the protocol were reported. |
| Other bias | Low risk | The study appears free of other sources of bias. |
| Methods | Single‐blind randomised controlled trial of acupuncture plus massage vs medication | |
| Participants | Diagnosis: post‐stroke depression Method of diagnosis: CCMD‐R, HAMD > 8 Age: not stated Participant information: 62 participants with post‐stroke depression for longer than 1 year Location: day patients and inpatients at the Guangzhou Hospital, China Inclusion/Exclusion: Exclusion criteria: serious cardiovascular disease, allergy to a sedative named “Dai an shen” containing flupentixol and melitracen | |
| Interventions | (1) Duration: 4 weeks (15 sessions) Frequency of treatment: every second day Treatment protocol: “ZhisanZhen” included a combination of points such as GB13 Ben Shen, DU24 Shenting, PC6 Neiguan, and SP4 Gongsun. The “Zhisanzhen” was needled with 25‐mm needles. PC6 was needled with 50‐mm needles, with deep needling. SP4 was needled towards SP3 Taibai, with de qi obtained and the sensation of qi sensation moving towards the chest. Needles were retained for 30 minutes. In addition, the group received finger point pressure and massage, which consisted of head massage, that is, massage on Tianmen points press Yingtang and stroke towards Shenting, repeated 5 times. Pressure was applied to acupuncture points DU20 Baihui, M‐NH‐3 Yingtang, DU26 Shuigou, and M‐HN‐9 Taiyang 5 times. Points GB20 Fengchi and DU16 Feng fu were pressed 3 times. Abdominal massage: In a circular clockwise motion, massage was applied to the abdomen 10 times. Pressure massage was applied to acupuncture points CV8 Shenque, CV4 Guanyuan, CV6 Qihai, and CV17 Shanzhong 3 to 5 times. Tendon separating pressure was applied to acupuncture points ST36 Zhusanli, SP6 Sanyinjiao 3 times. Massage via a kneading technique was applied to KD3 Taixi, LIV3 Taichong, SP6 Sanyinjiao, and PC6 Neiguan 3 times. Massage was applied once every second day for 15 treatments. (2) Duration: 4 weeks Frequency of treatment: daily Treatment protocol: The control group received medication consisting of Dai an shen (contains flupenthixol and melitracen). Two tablets were taken once a day in the morning for 1 month continuously. Note: Flupenthixol is a antipsychotic drug, and melitracen is a tricyclic antidepressant. | |
| Outcomes | Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Data on participants cured, or showing a marked effect | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random table was used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | No response was received from the trial author when further details of randomisation were requested. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and therapists were not blind. |
| Blinding of outcome assessment (detection bias) | Unclear risk | It is unclear whether assessing clinicians and analysts were blind to study group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | No attrition or exclusions were reported; no data are missing; all participants were included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | The study appears free of other sources of bias. |
BDI: Beck Depression Inventory.
CCMD: Chinese Classification of Mental DIsorders.
CGI: Clinical Global Impression Scale.
CGI‐S: Clinical Global Impression‐Severity Scale.
CHM: Chinese herbal medicine.
CNS: central nervous system.
DCEAS: dense cranial electro‐acupuncture stimulation.
DSM: Diagnostic and Statistical Manual of Mental Disorders.
EA: electro‐acupuncture.
EQ‐5D: EuroQoL quality of life questionnaire based on five dimensions.
GP: general practitioner.
HAMD: Hamilton Depression Rating Scale.
ICD: International Statistical Classification of Diseases and Related Health Problems.
ITT: intention‐to‐treat.
MDD: major depressive disorder.
MMSE: Mini‐Mental State Examination.
N/A: not applicable.
NCCAOM: National Certification Commission for Acupuncture and Oriental Medicine.
n‐EA: non‐invasive electro‐acupuncture.
PHQ: Patient Health Questionnaire.
QIDS: Quick Inventory for Depression Self Reporting.
RCT: randomised controlled trial.
SCID: Structured Clinical Interview for DSM.
SCL‐90: Symptom Checklist‐90.
SDS: Self‐rating Depression Scale.
SF‐36: Short Form Health Survey.
SPSS: Statistical Package for the Social Sciences.
SSRI: selective serotonin reuptake inhibitor.
TCM: Traditional Chinese Medicine.
TESS: Toxic Exposure Surveillance System.
UPMC: University of Pittsburgh Medical Center.
VAS: visual analogue scale.
WHOQOL: World Health Organization quality of life questionnaire.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| This trial of depression and anxiety aimed to evaluate the effect of acupuncture on cardiac autonomic nervous system function. Thirty‐six participants were randomly allocated to acupuncture or control sham acupuncture. No clinically meaningful data were reported. Data on cardiovascular outcomes (e.g. heart rate variability) were reported. | |
| Inability to confirm clinical diagnosis of depression | |
| Clinical diagnosis of depression not made | |
| Clinical diagnosis of depression not made | |
| Inability to confirm clinical diagnosis | |
| Clinical diagnosis of depression not made | |
| Inability to establish clinical diagnosis of depression | |
| Study intervention involved use of TENS stimulation. | |
| In this trial of acupuncture, participants had experienced a stroke and reported post‐stroke depression. Depression was diagnosed as per our protocol and did not meet trial criteria. Details on randomisation could not be confirmed. Participants were allocated into 3 groups: Xingnao acupuncture method, routine acupuncture plus medication (doxepin), and routine acupuncture. No other details were reported. The outcome measure was unclear. | |
| Observational study | |
| Clinical diagnosis of depression not made | |
| The intervention focussed primarily on reducing menopausal ‐ not depressive ‐ symptoms. | |
| Duplicate publication of Duan 2011 | |
| Duplicate publication of Fan 2013 | |
| Study population, intervention, and outcomes are the same as those reported in Allen 1998. This study reported follow‐up data at 12 months for an earlier trial (Allen 1998). However data reported separately by group cannot be obtained. | |
| Clinical diagnosis of depression not made | |
| Sixty‐one participants from China were given a diagnosis of depression based on the CCMD. Participants were given acupuncture or Chinese herbal medicine. The control group was administered Chinese herbs that did not meet our definition of standard care. Details on randomisation were unclear. The outcome measure was assessed by the Hamilton Depression Rating Scale. | |
| The comparator group did not meet inclusion criteria. | |
| Clinical diagnosis of depression not made | |
| Clinical diagnosis of depression not made | |
| The intervention did not meet the inclusion criteria because electro‐acupuncture was compared with manual acupuncture. | |
| The intervention did not meet the inclusion criteria because acupuncture and Chinese herbal medicine were combined. | |
| Acupuncture plus electro‐acupuncture vs manual acupuncture did not meet inclusion criteria for comparator groups. | |
| Eighty‐five participants with post‐stroke depression were recruited in China. Participants were allocated to acupuncture and point injection groups every second day for 12 days. The control group received amitriptyline 25 to 50 mg 2 to 3 times per day. Outcome assessment was based on the Hamilton Depression Rating Scale. The study evaluated point injection therapy with a parental solution of breviscapine, and this did not our criteria for inclusion. | |
| Ninety inpatients from a hospital in China were recruited to the trial. Participants met DSM‐II‐R diagnostic criteria for depression and were randomly allocated to scalp acupuncture or routine acupuncture, administered 6 days a week for 6 weeks.The Hamilton Depression Rating Scale was used to measure outcomes. This study was excluded owing to use of acupuncture as the control. | |
| Clinical diagnosis of depression not made | |
| Participants quasi‐randomised by day of admission | |
| Clinical diagnosis of depression not made | |
| Clinical diagnosis of depression not made | |
| The intervention did not meet inclusion criteria because acupuncture and Chinese herbal medicine were combined. | |
| Sixty‐six participants with a diagnosis of depression based on CCMD‐3. Participants were inpatients from a hospital in China and were randomised to acupuncture plus medication or medication only. Electro‐acupuncture was administered 5 times a week for 6 weeks. Details on the dose of medication were insufficient as reported in the manuscript. We were unable to confirm details despite extensive efforts to reach trial authors. Outcome assessment was based on the Hamilton Depression Rating Scale. | |
| Clinical diagnosis of depression not made | |
| Study not randomised | |
| The intervention did not meet inclusion criteria because acupuncture and Chinese herbal medicine were combined. | |
| The study compared tongue acupuncture vs body acupuncture. | |
| 142 participants with stroke and depression (score > 7 on HAMD). Intervention group received scalp acupuncture once a day for 30 days ‐ Prozac 0.5 mg administered once per day. Outcome measures were based on HAMD. A suboptimal dose of medication was administered in the control group ‐ 0.5 mg once a day. Clarification was sought from the trial author but no response was received after extensive efforts. | |
| The intervention did not meet inclusion criteria because acupuncture and Chinese herbal medicine were combined. | |
| Clinical diagnosis of depression not made | |
| Clinical diagnosis of depression not made | |
| Clinical diagnosis of depression not made | |
| Participants had depression following a stroke, and depression was diagnosed by the Hamilton Depression Rating Scale. Participants in the intervention group received acupuncture 5 times a week for 4 weeks. Participants in the control group received diazepam 2.5 mg once a day, or clozapine 25 mg once a day, for 4 weeks. Neither medication was prescribed for the control group to treat depression. Outcomes were measured on the Hamilton Depression Rating Scale. | |
| Thirty‐four participants were recruited as inpatients from a hospital in Malta. Diagnosis for depression did not meet our criteria. This study compared acupuncture vs standard medication for depression. Participants received electro‐acupuncture twice a week for 5 weeks. The control group received Deanxit; during the first 3 weeks, 2 tablets a day were given, and during the past 2 weeks, 1 tablet a day was given. No details on dosage are available. However, we were unable to confirm through correspondence with the trial author whether this was a randomised controlled trial. | |
| Participants were quasi‐randomised via case number. | |
| Clinical diagnosis of depression not made | |
| Inability to establish method of randomisation despite efforts to contact trial author | |
| The intervention did not meet inclusion criteria because acupuncture and blood letting were combined. | |
| This was a non‐randomised observational study. | |
| The intervention did not meet inclusion criteria because acupuncture and control acupuncture were combined. | |
| This was a non‐randomised study. | |
| Participants were quasi‐randomised ‐ allocated by case number. | |
| Participants had depression associated with menopause. This trial did not provide a clear definition and used the HAMD to classify depression. This study defined a subcategory of depression in post‐menopausal women ‐ a group not recognised in the West. The intervention consisted of acupuncture given once per day 6 days a week for 6 weeks. The control group received fluoxetine 20 mg once per day for 6 weeks. Outcomes were measure by the HAMD. | |
| The intervention did not meet the inclusion criteria because acupuncture and moxibustion were combined. |
CCMD: Chinese Classification of Mental Disorders.
DSM‐II‐R: Diagnostic and Statistical Manual of Mental Disorders, Second Edition, Revised.
HAMD: Hamilton Depression Rating Scale.
TENS: transcutaneous electrical nerve stimulation.
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Randomised study of acupuncture vs fluoxetine |
| Participants | 62 participants with depression diagnosed by the CCMD‐2R |
| Interventions | Fluoxetine 20 mg daily for 8 weeks Acupuncture LV 3, LI 4, GV20, Yintang, with adjunctive points BL15, BL14, ear points, HT7, GB 40, once daily twice a week |
| Outcomes | Recovery HAMD > 75% |
| Notes | Awaiting response from trial authors on details of randomisation |
| Methods | Acupuncture plus paroxetine vs medication only |
| Participants | 72 inpatients and outpatients with major depression |
| Interventions | Acupuncture plus paroxetine, electro‐acupuncture, and paroxetine vs paroxetine only |
| Outcomes | HAMD, SDS |
| Notes | Paper presented at conference, manuscript in preparation |
| Methods | Evaluation of therapeutic effects of early interventions and comparison of advantages of electro‐acupuncture (EA), cognitive‐behaviour therapy (CBT), and their combination in ameliorating depressive symptoms |
| Participants | 33 patients in depressive status included via the Hamilton Depression Rating Scale‐17 (HAMD‐17) and the Mini International Neuropsychiatric Interview (MINI) |
| Interventions | Electro‐acupuncture vs cognitive‐behavioural therapy (CBT) vs a combination of CBT and electro‐acupuncture vs observation only |
| Outcomes | HAMD |
| Notes | Conference paper (ICCMR 2015). Manuscript requested from trial author |
| Methods | Investigation of the change in signal transduction system among patients with major depressive disorder and the effect on signal transduction of electro‐acupuncture for treatment of individuals with depression |
| Participants | Patients with DSM‐IV or ICD‐10 major depressive disorder (MDD) recruited |
| Interventions | Under a double‐blind, acupuncture‐controlled, randomised pattern, participants were divided into 3 groups and were given different treatments for 6 weeks: electro‐acupuncture (n = 20), fluoxetine (n = 21), and needle punching (n = 21). |
| Outcomes | For each participant, blood samples were collected before and after treatment. |
| Notes | Unable to establish details of randomisation and any other outcome measures assessed |
| Methods | Randomised study of the effect of electrical acupuncture on serum cytokines in depressive patients |
| Participants | 61 patients with depression, 30 healthy controls |
| Interventions | Electro‐acupuncture, medication |
| Outcomes | Depression, anxiety, IL‐6, IL‐1ß, TNF‐alpha |
| Notes | Unable to determine method of randomisation and details of clinical diagnosis |
| Methods | Randomised trial of electro‐acupuncture compared with medication (no details on randomisation reported) |
| Participants | 61 participants with depression meeting criteria for ICD‐10 |
| Interventions | Electro‐acupuncture 6 sessions per week for 6 weeks, or 174 mg of medication per day |
| Outcomes | Hamilton Depression Rating Scale, self‐rating scale for depression, self‐rating scale for anxiety, Clinical Global Impression scale |
| Notes | Wrote to trial authors seeking clarification of randomisation |
| Methods | Randomised controlled trial of acupuncture vs fluoxetine |
| Participants | 69 patients with depression diagnosed by CCMD‐2‐R |
| Interventions | Manual acupuncture plus fluoxetine vs fluoxetine |
| Outcomes | Hamilton Depression Rating Scale (HAMD) and CGI used to evaluate efficacy |
| Notes | Unable to establish method of randomisation |
| Methods | Acupuncture vs medication |
| Participants | Patients with diagnosis of depression based on CCMD‐3 |
| Interventions | Manual acupuncture plus paroxetine vs paroxetine |
| Outcomes | HAMD scores |
| Notes | Unable to establish whether the trial was randomised |
| Methods | Acupuncture compared with medication, parallel design |
| Participants | 53 patients with depression diagnosed by CCMD‐3 |
| Interventions | Manual acupuncture vs paroxetine |
| Outcomes | HAMD and adverse events |
| Notes | Wrote to trial author seeking clarification of randomisation details |
| Methods | Controlled trial of electro‐acupuncture vs fluoxetine |
| Participants | 41 participants met diagnostic criteria for depression according to the Chinese Classification and Diagnostic Criteria for Mental Diseases, and scored > 17 on the Hamilton |
| Interventions | Electro‐acupuncture administered to points Baihui (GV 20), Shenting (GV 24), and Yintang (EX‐HN3). Additional points given based on Traditional Chinese Medicine diagnosis |
| Outcomes | Treatment Emergent Symptom Scale after 1 week, 2 weeks, 4 weeks, and 6 weeks of treatment |
| Notes | Unable to establish whether the trial was randomised |
| Methods | Randomised controlled trial (RCT) divided into 3 groups treated with fluoxetine, EA, and control EA, respectively |
| Participants | 90 patients with MDD meeting DSM‐IV criteria |
| Interventions | Participants in the fluoxetine treatment group received 20 mg fluoxetine per day and sham EA (a needle punctured under the skin at the side of 1 cm far from Yintang, Baihui points without electrical current). Participants in the EA treatment group received the real EA (a needle punctured in the Yintang, Baihui point with electrical current of 10 to 40 mA) for 45 minutes in the morning of every weekday and 20 mg placebo. Sham EA treatment group received sham EA and 20 mg placebo. |
| Outcomes | HAMD |
| Notes | Wrote to trial author seeking clarification of randomisation details |
| Methods | Depressed patients were randomly and blindly assigned to 3 groups of treatment: (1) EA and placebo capsules; (2) fluoxetine and control EA; or (3) control EA and placebo capsules. |
| Participants | 95 patients were recruited from outpatient clinics of the Beijing Mental Health Institute. Patients were assessed via the Structured Clinical Interview for DSM‐IV (SCID) and met DSM‐IV (Diagnostic and Statistical Manual of Mental Disorders) criteria for major depressive disorder. |
| Interventions | EA treatment was performed by placing needles at Bai Hui and at Yin Tang acupuncture points on the forehead. The acupuncture needles (0.30 mm × 33 mm) were then connected to an electro‐acupuncture machine with an antidepression sequence of waves for 45 minutes 3 times a week. Sham acupuncture was performed by placing the needles at non‐therapeutic points: 1 cm beside the Bai Hiu and Yin Tang acupoints. The needles were connected via the same EA machine that simulated the same oscillation waves as the active EA. The treatment procedure was the same as for the EA group. Fluoxetine (20 mg) or matched placebo capsules (supplied by Eli Lilly Pharmaceutical Company, USA) were taken after breakfast, 1 per day for 6 weeks. |
| Outcomes | Hamilton Depression Rating Scale (HAMD) 21 item scores (15) and Clinical Global Impression Scale (CGI) |
| Notes | Trial author did not confirm that the study was randomised. |
| Methods | Acupuncture vs Prozac vs acupuncture plus Prozac |
| Participants | 93 participants with post‐stroke depression |
| Interventions | Four‐week intervention |
| Outcomes | HAMD |
| Notes | Unable to confirm whether participants had received a clinical diagnosis of depression |
| Methods | Double‐blind control acupuncture vs real acupuncture clinical trial |
| Participants | Major depression as diagnosed by DSM‐IV. A total of 42 participants were recruited from the university primary care centre in Mexico. |
| Interventions | Electro‐acupuncture vs sham control |
| Outcomes | Carroll Rating Scale for Depression |
| Notes | Trial author did not confirm that the study was randomised. |
| Methods | Control study of laser acupuncture vs medication. Method of randomisation unclear |
| Participants | 62 patients with depressive neurosis based on Chinese criteria of diagnosis |
| Interventions | Laser acupuncture or doxepin administered over 21 days |
| Outcomes | HAMD, CGI |
| Notes | Wrote to trial author seeking clarification of the method of randomisation |
| Methods | Randomised trial with no details reported (divided into 2 groups) |
| Participants | 90 patients |
| Interventions | Acupuncture vs medication ‐ fluoxetine |
| Outcomes | HAMD scale |
| Notes | Contacted trial authors; no response received |
| Methods | Acupuncture vs fluoxetine |
| Participants | 60 patients with HAMD score ≥ 20 |
| Interventions | Acupuncture administered once daily for 30 days. Fluoxetine administered 2 tablets for first 10 days, then 2 tablets for 20 days |
| Outcomes | HAMD scale |
| Notes | Unable to establish whether study was truly randomised |
CBT: cognitive‐behavioural therapy.
CCMD: Chinese Classification of Mental Disorders.
CGI: Clinical Global Impression Scale.
DSM‐IV: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.
EA: electro‐acupuncture.
HAMD: Hamilton Depression Rating Scale.
ICCMR: International Congress of Complementary Medicine Research.
ICD‐10: International Statistical Classification of Diseases and Related Health Problems, Tenth Edition.
IL: interleukin.
MDD: major depressive disorder.
MINI: Mini International Neuropsychiatric Interview.
RCT: randomised controlled trial.
SCID: Structured Clinical Interview for DSM.
SDS: Self‐rating Depression Scale.
TNF: tumour necrosis factor.
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Effect of acupuncture on the DMN of brain in patients with major depressive disorder: a resting‐state fMRI study |
| Methods | Case control study |
| Participants | 60 patients with depression as diagnosed by DSM‐IV. Patients are included if they are having their first depressive episode, are drug naive, are aged between 18 and 60 years, are right handed, and have an HAMD score ≥ 18 |
| Interventions | Acupuncture at Baihui (GV20) for 20 minutes |
| Outcomes | Activity in brain regions (ALFF, ReHo) |
| Starting date | January 2011 |
| Contact information | Study leader: Demao Deng ([email protected]) |
| Notes | Recruitment is complete. |
| Trial name or title | Clinical study of acupuncture for mild and moderate depressive episodes |
| Methods | Randomised controlled trial comparing a comprehensive intervention vs drug treatment |
| Participants | 200 patients aged 18 to 75 with diagnosis of mild to moderate depression according to CCMD‐3. Patients are excluded if they have an organic mental disorder or psychoactive substances and non‐addictive substance‐induced depression; are younger than 18 years of age or older than 75 years; cannot comprehend the meaning of self‐report of patients; are pregnant women; have epilepsy or serious disorders of the heart and brain blood vessels, liver, kidney, haematopoietic system, or gastrointestinal system; or cannot follow through with treatment. |
| Interventions | Comprehensive intervention programme plus placebo acupuncture Drug treatment plus sham acupuncture |
| Outcomes | Hamilton Depression Rating Scale, SF‐36 |
| Starting date | February 2015 |
| Contact information | Study leader: Ling Fan ([email protected]) |
| Notes | Currently recruiting |
| Trial name or title | Clinical study on acupuncture treating insomnia with depression |
| Methods | Randomised controlled trial of 2 styles of acupuncture |
| Participants | 140 patients aged between 18 and 65 with depression diagnosed according to CCMD‐3 with a chief complaint of insomnia. HAMD scores between 20 and 35. Patients able to give informed consent. Patients are excluded if depression is a result of mental disease, active substances, or non‐addiction medicine, as are pregnant or lactating women; patients with serious heart, brain, or kidney disease or other major medical disorder; patients with cancer; and patients unable to co‐operate with their doctor |
| Interventions | Conventional acupuncture treatment: Hegu (LI4), Tai Chong (LIV3), Yintang (EX‐HN‐3), Bai hui (GV20). Needles retained 30 minutes. While needles are inserted, patients are advised to take 6 deep breaths, then rest and repeat this every minute until the needles are removed. Optimised acupuncture treatment: Same as the conventional group but with Lie Qie (LU7) and Zhao Hai (KID6) added. Embedded needles (2 to 3 mm long) are used for 2 alternating groups of points: Xin Shu (BL‐15) and Shen Shu (Bl‐23) or Dan Shu (Bl19) and An Mian (N‐HN‐54). These embedded needles are retained until the start of subsequent treatment. |
| Outcomes | PSQI and HAMD are the primary outcome measures. |
| Starting date | September 2011 |
| Contact information | Trial leader: Wenbin Fu ([email protected]) |
| Notes |
| Trial name or title | Acupuncture for ischemic post‐stroke depression |
| Methods | Multi‐centre, single‐blind, randomised controlled clinical trial in patients with ischaemic post‐stroke depression comparing verum acupuncture plus placebo medication vs control acupuncture plus true medication |
| Participants | 208 patients aged 45 to 80 years with a diagnosis of ischaemic stroke per International Classification of Diseases‐10 163 (ICD‐10 163: diagnosis of a major depressive episode according to the depression module of the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM‐IV), or the Chinese Classification and Diagnostic Criteria of Mental Disorders‐3 (CCMD‐3)). Onset of ischaemic post‐stroke depression is recent (< 6 months); patient is conscious, co‐operative, and without aphasia and has severe cognitive impairment; and has the capacity to provide written consent for both research assessment and treatment. |
| Interventions | Experimental: Traditional acupuncture and placebo: Participants will be treated at Renzhong (Du26), Yintang (EX‐HN3), acupuncture Shangxing (DU23), penetrate to Baihui (DU20), Sishencong (EX‐HN1), Neiguan (PC6), Sibai (ST2), Fengchi (GB20), and Sanyinjiao (SP6) in bilateral; Jianyu (LI15), Quchi (LI11), Shousanli (LI10), Hegu (LI 4), Fengshi (GB31), Xuehai (SP10), Zusanli (ST36), and Taichong (LR 3) on the hemiplegia side. Another 6 groups use acupoints in bilateral. The acupuncturist will choose 1 group of acupoints according to the participant's syndrome: Zhigou (SJ6), Qimen (LR14), Xingjian (LR2), Xiaxi (GB43), Fenglong (ST40), Lianquan (RN23), Tongli (HT5), Xinshu (BL15), Xinshu (BL15), Pishu (BL20), Shenshu (BL23), and Taixi (KI3). Sham‐acupoint acupuncture and fluoxetine: Participants will be treated at Jianliao (SJ14), Tianquan (PC2), Xiabai (LU4), Xiaoluo (SJ12), Shouwuli (LI13), Sidu (SJ9), Huizong (SJ7), Wenliu (LI7), Zhouliao (LI12), Quze (PC3), Kongzui (LI6), Zhigou (SJ6), Zhongzhu (SJ3), Futu (ST32), Jimen (SP11), Yinshi (ST33), Liangqiu (ST34), Shangjuxu (ST37), Xiajuxu (ST39), Xiyangguan (GB33), Ligou (LR5), Pucan (BL61), Jinggu (BL64), Rangu (KI2), Ligou (LR5), and Neiting (ST44) on the hemiplegia side. |
| Outcomes | HAMD‐17 |
| Starting date | March 2016 |
| Contact information | Menghan Li, State Administration of Traditional Chinese Medicine of the People's Republic of China, The First Affiliated Hospital of Tianjin University of Traditional Chinese Medicine |
| Notes | Not yet recruiting |
| Trial name or title | Adjunctive treatment of major depression utilizing auricular acupuncture |
| Methods | Randomised, single‐blind study of 6 weeks' duration involving the use of auricular acupuncture or control acupuncture for adjunctive treatment of college students with depression |
| Participants | 40 college students presenting for care at Counseling and Psychological Services who meet Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM‐V) criteria for major depression single episode or recurrent will be included in the trial. Patients must have been symptomatic with depression for 2 months or longer or less than 18 months. Participants will be randomised into a sham auricular acupuncture group or a treatment acupuncture group. All patients who meet inclusion criteria will be treated with the selective serotonin reuptake inhibitor (SSRI) Lexapro 10 mg daily, which will be increased to 20 mg daily at week 2. Some participants will be treated twice weekly during their follow‐up visits with sham auricular acupuncture, others in the auricular acupuncture group will be treated with microcurrents of electricity. Trial duration will be 6 weeks. |
| Interventions | Experimental: Auricular acupuncture + Lexipro: Participants will be treated with the SSRI Lexapro 10 mg daily, which will be increased to 20 mg daily at week 2. Participants in this group will be treated twice weekly during their follow‐up visits with microcurrents of electricity through auricular acupuncture. Sham comparator: Sham auricular acupuncture + Lexapro: Participants will be treated with the SSRI Lexapro 10 mg daily, which will be increased to 20 mg daily at week 2. Participants will be treated twice weekly during their follow‐up visits with sham auricular acupuncture (no microcurrent). |
| Outcomes | Change from baseline score of the Behavioral Health Measure‐20 through 6 weeks |
| Starting date | August 2015 |
| Contact information | Principal investigator: John Prater ([email protected]) |
| Notes | Currently recruiting |
| Trial name or title | Acupuncture based on five elements of body characteristics in the treatment of patients with post‐stroke depression |
| Methods | Randomised control trial comparing body acupuncture, 5‐element body acupuncture, and western medicine for post‐stroke depression |
| Participants | 150 patients aged 30 to 70 years who meet both Chinese medicine and conventional medicine diagnostic criteria for post‐stroke depression, who are able to understand and complete the depression scale, whose lesion is confirmed by head CT or MRI examination, and whose lesions are located in the anterior cerebral circulation |
| Interventions | Observation group: 5 pedestrian body dialectical acupuncture Acupuncture group: conventional acupuncture Western medicine control group: no acupuncture |
| Outcomes | Changes in HAMD scale score |
| Starting date | July 2013 |
| Contact information | Study leader: Liu Tai ([email protected]) |
| Notes | Recruitment complete |
| Trial name or title | Abdominal acupuncture on moderate and severe depression female patients: a randomised controlled blind clinical trial |
| Methods | Randomised controlled trial comparing a combination of acupuncture and fluoxetine vs another combination of acupuncture and fluoxetine |
| Participants | 40 female patients aged 23 to 60 years with depression, able to understand and read Chinese, with SDS < 53 or MADRE score > 14 |
| Interventions | Acupuncture and fluoxetine treatment group Acupuncture and fluoxetine control group |
| Outcomes | Self‐Rating Depression Scale (SDS), Montgomery‐Asberg Depression Rating Scale (MADRS) |
| Starting date | September 2014 |
| Contact information | Study leader: Xiaoyun Wang ([email protected]) |
| Notes | Currently recruiting |
| Trial name or title | Clinical evaluation of depression treated by disease and syndrome combined method |
| Methods | Randomised parallel controlled trial comparing low‐resistance‐state thought induction psychotherapy vs cognitive‐behavioural therapy vs low‐resistance‐state thought induction psychotherapy and acupuncture and herbs |
| Participants | 225 patients aged 18 to 60 with depression diagnosed by SCID and HAMD score of 25 to 36, with education level higher than junior high school and no suicidal ideation. Patients would be excluded if they had schizophrenia and substance addiction; had organic brain disease or endocrine disease; were pregnant or lactating women; had had a manic attack; or had serious physical disease. |
| Interventions | TIP group: low‐resistance‐state thought induction psychotherapy CBT group: cognitive‐behavioural treatment Comprehensive group: low‐resistance‐state thought induction psychotherapy and acupuncture and herbs |
| Outcomes | Hamilton Depression Rating Scale, Beck Depression Inventory |
| Starting date | May 2015 |
| Contact information | |
| Notes | Recruitment pending |
| Trial name or title | A clinical evaluation research for the treatment of major depression by integrated disease with Zheng of TCM method |
| Methods | Randomised parallel controlled trial of acupuncture, herbal medicine, and escitalopram vs escitalopram alone |
| Participants | 160 patients aged 18 to 45 with depression diagnosed in accordance with conventional disease diagnosis and TCM treatment in Shanghai (second edition) and DSM‐IV psychiatric diagnostic standard in the United States, and Hamilton Depression Rating Scale score ≥ 20 points, namely, the clinical‐severe type; who at least 1 week before treatment have not used antidepressant drugs (including western medicine and TCM) or other psychiatric drugs or have used them with cleaning at least 1 week; after 2 different types of antidepressants or at least more than 6 weeks, nearly 1 week is invalid, can maintain the original drug dosage into the group; has a cultural degree for junior high school above; available for the course of more than 2 weeks; right‐handed; has no contraindications to MRI scanning; with the approval of the hospital ethics committee, volunteer to participate in, and sign the informed consent. |
| Interventions | Acupuncture, liver depression resolving particles, and escitalopram vs escitalopram alone |
| Outcomes | HAMD |
| Starting date | April 2016 |
| Contact information | Study leader: Wang Weidong ([email protected]) |
| Notes | Currently recruiting |
| Trial name or title | Effectiveness and safety of electro‐acupuncture for mild to moderate perimenopausal depression |
| Methods | Randomised controlled trial to compare effects of electro‐acupuncture and escitalopram oxalate tablets on mild to moderate perimenopausal depression, and to evaluate the safety of electro‐acupuncture stimulation |
| Participants | 252 women aged 45 to 55 years, meeting the diagnostic standard of STRAW‐10 for perimenopause, conforming to the diagnostic standard of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM‐5), for depression, and conforming to the diagnostic standard of the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD‐10) F32.0 (mild depression) or F32.1 (moderate depression), with HAMD‐17 score > 7 and < 23, with first episode of depression during the perimenopausal period, not on hormone replacement therapy (HRT), and taking no antidepressant 3 months before the study begins |
| Interventions | Experimental: Electro‐acupuncture: Baihui, Yintang, Guanyuan (dual), Zigong (dual), Sanyinjiao (dual), Hegu (dual), and Taichong (dual). Insert needles to the acupoints mentioned above after sterilised. Needle handles of Baihui and Yintang are connected with the electro‐acupuncture instrument wire. Needle handles of bilateral Zigong are connected with the electro‐acupuncture instrument wire. Needle handles of bilateral Tianshu are connected with the electro‐acupuncture instrument wire. Density wave, frequency of 10/50 Hz, and current intensity of 0.5˜1.0 mA for 30 minutes. 3 times per week. Each treatment interval > 24 hours, continuous treatment for 12 weeks. Active comparator: escitalopram oxalate tablets 0.5 hour after breakfast, oral 10 mg escitalopram oxalate tablets, continuous treatment for 12 weeks |
| Outcomes | Change from baseline in scores of the 17‐item Hamilton Depression Rating Scale (HAMD‐17) at 4th week, 8th week, 12th week, 16th week, and 24th week |
| Starting date | September 2013 |
| Contact information | Study leader: Wenben Fu ([email protected]) |
| Notes | Estimated completion: December 2015 |
| Trial name or title | The clinical study of the best treatment option in acupuncture on depression |
| Methods | Randomised controlled trial comparing manual acupuncture, electro‐acupuncture, and medication (paroxetine HCL) |
| Participants | 480 patients aged 18 to 60 with depression diagnosed by ICD‐10 (excluding bipolar disorder), HAMD score ≥ 17 who are able to give informed consent. Patients are excluded if they have joined another clinical examination within 4 weeks of starting the trial, are taking antidepressants, are pregnant or lactating women, have other serious diseases, have caught brain disease, or have suicidal ideation. |
| Interventions | Manual acupuncture group: Baihui, Yintang, Fengfu, Fengchi, Da Zhui, Neiguan, Sanyinjiao Electro‐acupuncture group: Baihui, Yintang, Fengfu, Fengchi, Da Zhui, Neiguan, Sanyinjiao Medication control group: paroxetine HCL, 10 mg/d for the first 2 days, then 20 mg/d |
| Outcomes | SDS, HAMD, CGI |
| Starting date | October 2007 |
| Contact information | Study leader: Tu Ya ([email protected]) |
| Notes | Recruitment complete |
| Trial name or title | The clinical curative effect of acupuncture treatment in depression |
| Methods | Randomised parallel controlled trial of electro‐acupuncture vs SSRI antidepressants |
| Participants | 80 patients aged 18 to 65 with mild and moderate depression as diagnosed by ICD‐10 and HAMD score ≥ 17 and ≤ 22, diagnosed for the first time, without current systemic treatment, with depression starting within the past 2 weeks to 1 year. Patients are excluded if 4 weeks before the start of this study they participated in other clinical trials; |
| Interventions | Electro‐acupuncture: Yintang and Baihui, Taichong, Neiguan, Zusanli, Shenmen, Sanyinjiao. Treatment 2 times a week, 30 minutes per session. Electro‐acupuncture frequency 20 Hz Medication: SSRIs, antidepressants including fluoxetine, paroxetine, fluvoxamine, sertraline, and citalopram. Dosage was based on physician advice. |
| Outcomes | fMRI; ACTH; CORT; IL‐6; TNF‐alpha; IL‐1; HAMD scale |
| Starting date | July 2015 |
| Contact information | Study leader: Tu Ya ([email protected]) |
| Notes | Recruitment status unknown |
| Trial name or title | Comparison of treatment effect of Chinese medicine and western medicine on depression in China and America |
| Methods | Randomised controlled trial comparing Chinese medicine, acupuncture, traditional Chinese medicine psychology and physical treatment for treatment of individuals with depression |
| Participants | 160 patients aged 16 to 70 with depression diagnosed by ICD‐10 criteria; antidepressants and other psychiatric drugs were not taken 2 weeks before the trial, or the drugs above were used but have a cleaning period of 2 weeks; level of education is higher than junior middle school; course of disease is longer than 2 weeks, and informed consent is given. |
| Interventions | Experimental: Chinese herb: Chinese herbs special for depression Experimental: Acupuncture: acupuncture at DU20, EX HN3, EX HN1, PC6, HT7, SP6, special point for depression Experimental: Psychotherapy: thought imprint psychotherapy under lower resistance state Physiotherapy: transcranial magnetic stimulation on the head |
| Outcomes | Psychological questionnaires at 1 week, 2 weeks, 4 weeks, 6 weeks, and 12 weeks post treatment |
| Starting date | March 2012 |
| Contact information | Study leader: Xue Yan ([email protected]) |
| Notes | Estimated completion date: March 2014 |
| Trial name or title | Wrist‐ankle acupuncture combined with Prozac in the treatment of post‐stroke depression |
| Methods | Randomised controlled trial comparing 3 different styles of wrist‐ankle needling in conjunction with fluoxetine |
| Participants | 105 patients aged 30 to 75 years with a diagnosis of post‐stroke depression according to TCM syndrome diagnostic criteria, with HAMD score ≥ 18 in the post‐acute phase (2 weeks after stroke), with vital signs that are stable. Patient is conscious, has certain expression and communication skills, and is able to sign informed consent or has immediate family members who will sign informed consent. |
| Interventions | Group 1: Thick needle+Prozac Group 2: Fine needle+Prozac Group 3: Sham needle+Prozac |
| Outcomes | Hamilton Depression Rating Scale (HAMD), Self‐rating Depression Scale (SDS) |
| Starting date | June 2015 |
| Contact information | Study leader: You Yanli ([email protected]) |
| Notes | Recruitment pending |
ACTH: adrenocorticotropic hormone.
ALFF: amplitude of spontaneous low‐frequency fluctuation.
CBT: cognitive‐behavioural therapy.
CCMD: Chinese Classification of Mental DIsorders.
CGI: Clinical Global Impression Scale.
CORT: Cortisol.
CT: computed tomography.
DMN: default mode network.
DSM‐5: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
DSM‐IV: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.
fMRI: functional magnetic resonance imaging.
HAMD: Hamilton Depression Rating Scale.
HRT: hormone replacement therapy.
ICD‐10: International Statistical Classification of Diseases and Related Health Problems, Tenth Edition.
IL: interleukin.
MADRS: Montgomery‐Asberg Depression Rating Scale.
MRI: magnetic resonance imaging.
PSQI: Pittsburg Sleep Quality Index.
ReHo: regional homogeneity.
SCID: Structured Clinical Interview for DSM.
SDS: Self‐rating Depression Scale.
SF‐36: Short Form Health Survey.
SSRI: selective serotonin reuptake inhibitor.
STRAW‐10: Stages of Reproductive Aging Workshop.
TCM: Traditional Chinese Medicine.
TNF: tumour necrosis factor.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severity of depression at the end of treatment Show forest plot | 5 | 488 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.66 [‐1.06, ‐0.25] |
| Analysis 1.1  Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 1 Severity of depression at the end of treatment. | ||||
| 1.1 Manual acupuncture | 5 | 458 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.56 [‐0.98, ‐0.15] |
| 1.2 Electro‐acupuncture | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.26 [‐2.10, ‐0.43] |
| 2 Adverse events Show forest plot | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.35, 2.24] |
| Analysis 1.2  Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 2 Adverse events. | ||||
| 2.1 Manual acupuncture | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.35, 2.24] |
| 3 Severity of depression during treatment Show forest plot | 2 | 137 | Mean Difference (IV, Random, 95% CI) | ‐6.75 [‐9.12, ‐4.38] |
| Analysis 1.3  Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 3 Severity of depression during treatment. | ||||
| 3.1 Manual acupuncture | 2 | 107 | Mean Difference (IV, Random, 95% CI) | ‐7.04 [‐11.08, ‐3.00] |
| 3.2 Electro‐acupuncture | 1 | 30 | Mean Difference (IV, Random, 95% CI) | ‐6.24 [‐9.86, ‐2.62] |
| 4 Severity of depression 0‐6 months after treatment Show forest plot | 1 | 237 | Mean Difference (IV, Random, 95% CI) | ‐1.90 [‐3.01, ‐0.79] |
| Analysis 1.4 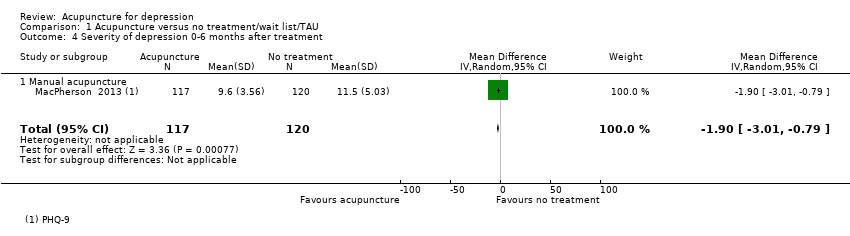 Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 4 Severity of depression 0‐6 months after treatment. | ||||
| 4.1 Manual acupuncture | 1 | 237 | Mean Difference (IV, Random, 95% CI) | ‐1.90 [‐3.01, ‐0.79] |
| 5 Severity of depression 6‐12 months after treatment Show forest plot | 1 | 235 | Mean Difference (IV, Random, 95% CI) | ‐1.0 [‐2.53, 0.53] |
| Analysis 1.5  Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 5 Severity of depression 6‐12 months after treatment. | ||||
| 5.1 Manual acupuncture | 1 | 235 | Mean Difference (IV, Random, 95% CI) | ‐1.0 [‐2.53, 0.53] |
| 6 Remission of depression Show forest plot | 2 | 94 | Risk Ratio (M‐H, Random, 95% CI) | 1.67 [0.77, 3.65] |
| Analysis 1.6 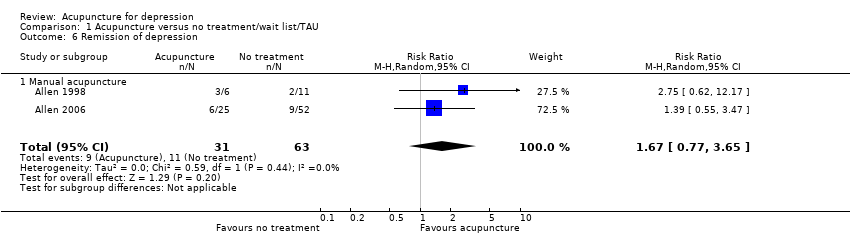 Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 6 Remission of depression. | ||||
| 6.1 Manual acupuncture | 2 | 94 | Risk Ratio (M‐H, Random, 95% CI) | 1.67 [0.77, 3.65] |
| 7 Change in use of medication at the end of treatment Show forest plot | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.73, 1.14] |
| Analysis 1.7  Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 7 Change in use of medication at the end of treatment. | ||||
| 7.1 Manual acupuncture | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.73, 1.14] |
| 8 Dropout from treatment Show forest plot | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.21, 4.88] |
| Analysis 1.8  Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 8 Dropout from treatment. | ||||
| 8.1 Manual acupuncture | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.21, 4.88] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severity of depression at the end of the intervention Show forest plot | 14 | 841 | Mean Difference (IV, Random, 95% CI) | ‐1.69 [‐3.33, ‐0.05] |
| Analysis 2.1  Comparison 2 Acupuncture versus control acupuncture, Outcome 1 Severity of depression at the end of the intervention. | ||||
| 1.1 Manual acupuncture vs invasive control | 7 | 418 | Mean Difference (IV, Random, 95% CI) | ‐2.97 [‐6.26, 0.31] |
| 1.2 Electro‐acupuncture vs invasive control | 5 | 251 | Mean Difference (IV, Random, 95% CI) | 0.43 [‐0.54, 1.40] |
| 1.3 Electro‐acupuncture vs non‐invasive electro‐control | 2 | 99 | Mean Difference (IV, Random, 95% CI) | 0.17 [‐2.14, 2.48] |
| 1.4 Laser acupuncture vs non‐invasive control | 2 | 73 | Mean Difference (IV, Random, 95% CI) | ‐5.51 [‐8.30, ‐2.73] |
| 2 Adverse events Show forest plot | 5 | 300 | Risk Ratio (M‐H, Random, 95% CI) | 1.63 [0.93, 2.86] |
| Analysis 2.2 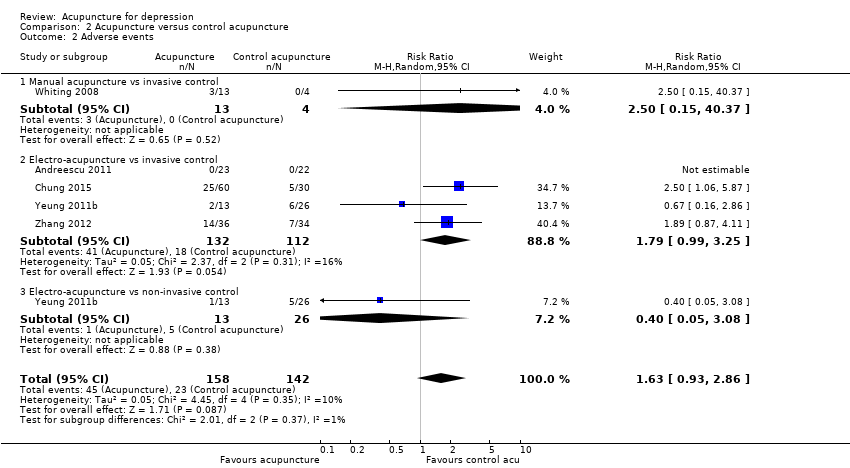 Comparison 2 Acupuncture versus control acupuncture, Outcome 2 Adverse events. | ||||
| 2.1 Manual acupuncture vs invasive control | 1 | 17 | Risk Ratio (M‐H, Random, 95% CI) | 2.5 [0.15, 40.37] |
| 2.2 Electro‐acupuncture vs invasive control | 4 | 244 | Risk Ratio (M‐H, Random, 95% CI) | 1.79 [0.99, 3.25] |
| 2.3 Electro‐acupuncture vs non‐invasive control | 1 | 39 | Risk Ratio (M‐H, Random, 95% CI) | 0.4 [0.05, 3.08] |
| 3 Severity of depression during treatment Show forest plot | 6 | 413 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.81, 0.90] |
| Analysis 2.3  Comparison 2 Acupuncture versus control acupuncture, Outcome 3 Severity of depression during treatment. | ||||
| 3.1 Manual acupuncture vs invasive control | 2 | 117 | Mean Difference (IV, Random, 95% CI) | 0.09 [‐2.55, 2.74] |
| 3.2 Electro‐acupuncture vs invasive control | 4 | 197 | Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.92, 1.24] |
| 3.3 Electro‐acupuncture vs non‐invasive control | 2 | 99 | Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐2.71, 1.80] |
| 4 Severity of depression at 0‐6 months' follow‐up Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.4  Comparison 2 Acupuncture versus control acupuncture, Outcome 4 Severity of depression at 0‐6 months' follow‐up. | ||||
| 4.1 Manual acupuncture vs invasive control | 1 | 95 | Mean Difference (IV, Random, 95% CI) | ‐0.85 [‐0.98, ‐0.72] |
| 5 Remission of depression Show forest plot | 10 | 601 | Risk Ratio (M‐H, Random, 95% CI) | 1.91 [1.14, 3.21] |
| Analysis 2.5  Comparison 2 Acupuncture versus control acupuncture, Outcome 5 Remission of depression. | ||||
| 5.1 Manual acupuncture vs invasive control | 5 | 368 | Risk Ratio (M‐H, Random, 95% CI) | 1.89 [0.75, 4.75] |
| 5.2 Electro‐acupuncture vs invasive control | 2 | 87 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.35, 4.29] |
| 5.3 Electro‐acupuncture vs non‐invasive electro‐control | 1 | 73 | Risk Ratio (M‐H, Random, 95% CI) | 2.15 [0.60, 7.67] |
| 5.4 Laser acupuncture vs non‐invasive control | 2 | 73 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [1.48, 6.09] |
| 6 Quality of life (emotional) during treatment Show forest plot | 1 | 150 | Mean Difference (IV, Random, 95% CI) | ‐1.98 [‐5.41, 1.45] |
| Analysis 2.6  Comparison 2 Acupuncture versus control acupuncture, Outcome 6 Quality of life (emotional) during treatment. | ||||
| 6.1 Electro‐acupuncture vs invasive control | 1 | 90 | Mean Difference (IV, Random, 95% CI) | ‐2.09 [‐6.54, 2.36] |
| 6.2 Electro‐acupuncture vs non‐invasive control | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐1.81 [‐7.18, 3.56] |
| 7 Quality of life (emotional) at the end of treatment Show forest plot | 2 | 167 | Mean Difference (IV, Random, 95% CI) | ‐2.25 [‐5.89, 1.39] |
| Analysis 2.7 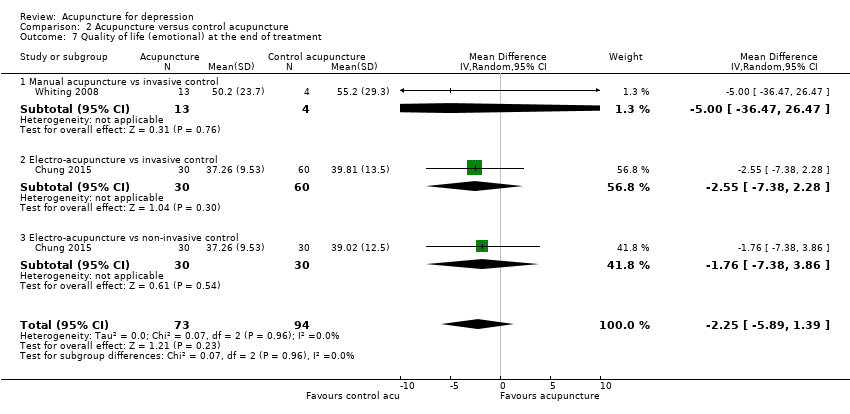 Comparison 2 Acupuncture versus control acupuncture, Outcome 7 Quality of life (emotional) at the end of treatment. | ||||
| 7.1 Manual acupuncture vs invasive control | 1 | 17 | Mean Difference (IV, Random, 95% CI) | ‐5.0 [‐36.47, 26.47] |
| 7.2 Electro‐acupuncture vs invasive control | 1 | 90 | Mean Difference (IV, Random, 95% CI) | ‐2.55 [‐7.38, 2.28] |
| 7.3 Electro‐acupuncture vs non‐invasive control | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐1.76 [‐7.38, 3.86] |
| 8 Quality of life (physical) during treatment Show forest plot | 1 | 150 | Mean Difference (IV, Random, 95% CI) | ‐0.99 [‐4.74, 2.77] |
| Analysis 2.8 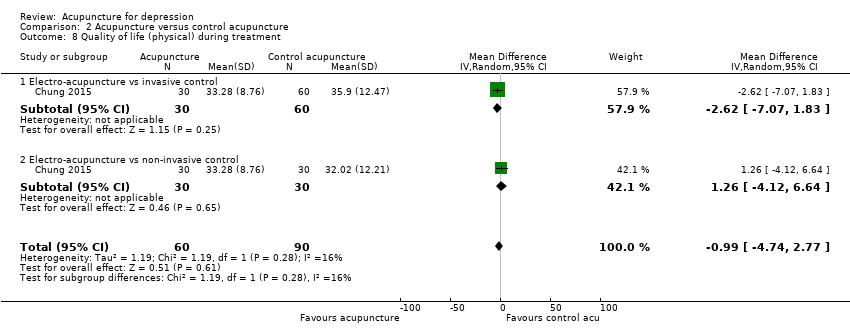 Comparison 2 Acupuncture versus control acupuncture, Outcome 8 Quality of life (physical) during treatment. | ||||
| 8.1 Electro‐acupuncture vs invasive control | 1 | 90 | Mean Difference (IV, Random, 95% CI) | ‐2.62 [‐7.07, 1.83] |
| 8.2 Electro‐acupuncture vs non‐invasive control | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 1.26 [‐4.12, 6.64] |
| 9 Quality of life (physical) at the end of treatment Show forest plot | 1 | 150 | Mean Difference (IV, Random, 95% CI) | ‐5.12 [‐10.38, 0.13] |
| Analysis 2.9  Comparison 2 Acupuncture versus control acupuncture, Outcome 9 Quality of life (physical) at the end of treatment. | ||||
| 9.1 Electro‐acupuncture vs invasive control | 1 | 90 | Mean Difference (IV, Random, 95% CI) | ‐7.61 [‐12.38, ‐2.84] |
| 9.2 Electro‐acupuncture vs non‐invasive control | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐2.23 [‐7.81, 3.35] |
| 10 Change in medication Show forest plot | 1 | 70 | Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐1.71, 0.93] |
| Analysis 2.10 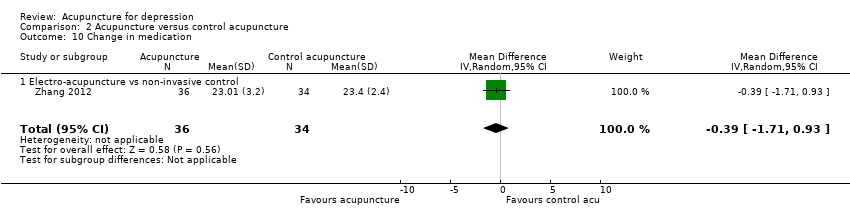 Comparison 2 Acupuncture versus control acupuncture, Outcome 10 Change in medication. | ||||
| 10.1 Electro‐acupuncture vs non‐invasive control | 1 | 70 | Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐1.71, 0.93] |
| 11 Dropout from treatment Show forest plot | 7 | 501 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.62, 1.75] |
| Analysis 2.11  Comparison 2 Acupuncture versus control acupuncture, Outcome 11 Dropout from treatment. | ||||
| 11.1 Manual acupuncture vs invasive control | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.6 [0.16, 2.29] |
| 11.2 Electro‐acupuncture vs invasive control | 4 | 224 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.51, 2.02] |
| 11.3 Electro‐acupuncture vs non‐invasive control | 4 | 217 | Risk Ratio (M‐H, Random, 95% CI) | 1.48 [0.56, 3.91] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severity of depression at the end of treatment Show forest plot | 31 | 3127 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.40, ‐0.05] |
| Analysis 3.1  Comparison 3 Acupuncture versus medication, Outcome 1 Severity of depression at the end of treatment. | ||||
| 1.1 Manual acupuncture vs SSRI | 16 | 1570 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.50, 0.04] |
| 1.2 Electro‐acupuncture vs SSRI | 5 | 197 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.47 [‐0.85, ‐0.10] |
| 1.3 Manual acupuncture vs TCAs | 3 | 397 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐1.25, 0.69] |
| 1.4 Electro‐acupuncture vs TCAs | 5 | 801 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.42, 0.01] |
| 1.5 Manual acupuncture vs other antidepressant | 1 | 60 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.73, 0.29] |
| 1.6 Electro‐acupuncture vs heterocyclic antidepressants | 1 | 61 | Std. Mean Difference (IV, Random, 95% CI) | 0.30 [‐0.21, 0.80] |
| 1.7 Electro‐acupuncture vs other antidepressant | 1 | 41 | Std. Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.52, 0.70] |
| 2 Adverse events Show forest plot | 3 | 481 | Mean Difference (IV, Random, 95% CI) | ‐4.32 [‐7.41, ‐1.23] |
| Analysis 3.2 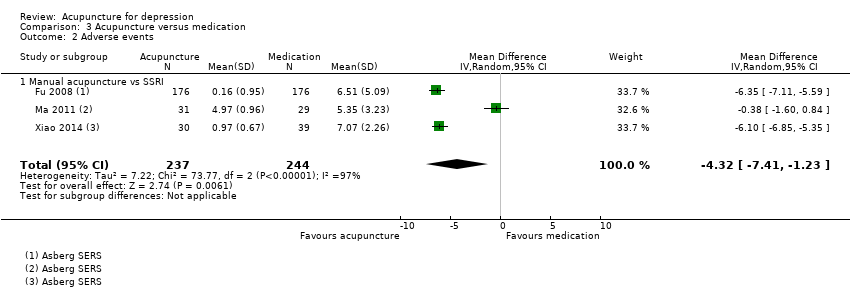 Comparison 3 Acupuncture versus medication, Outcome 2 Adverse events. | ||||
| 2.1 Manual acupuncture vs SSRI | 3 | 481 | Mean Difference (IV, Random, 95% CI) | ‐4.32 [‐7.41, ‐1.23] |
| 3 Severity of depression during treatment Show forest plot | 9 | 552 | Mean Difference (IV, Random, 95% CI) | ‐1.67 [‐2.91, ‐0.43] |
| Analysis 3.3  Comparison 3 Acupuncture versus medication, Outcome 3 Severity of depression during treatment. | ||||
| 3.1 Manual acupuncture vs SSRI | 5 | 340 | Mean Difference (IV, Random, 95% CI) | ‐1.38 [‐3.20, 0.45] |
| 3.2 Electro‐acupuncture vs SSRI | 3 | 112 | Mean Difference (IV, Random, 95% CI) | ‐2.58 [‐4.38, ‐0.78] |
| 3.3 Manual acupuncture vs TCAs | 1 | 100 | Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐3.65, 2.05] |
| 4 Severity of depression 0‐6 months after treatment Show forest plot | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐5.60 [‐7.60, ‐3.60] |
| Analysis 3.4  Comparison 3 Acupuncture versus medication, Outcome 4 Severity of depression 0‐6 months after treatment. | ||||
| 4.1 Manual acupuncture vs other antidepressant medication | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐5.60 [‐7.60, ‐3.60] |
| 5 Remission of depression Show forest plot | 25 | 2918 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [1.05, 1.29] |
| Analysis 3.5  Comparison 3 Acupuncture versus medication, Outcome 5 Remission of depression. | ||||
| 5.1 Manual acupuncture vs SSRI | 14 | 1332 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.98, 1.37] |
| 5.2 Electro‐acupuncture vs SSRI | 4 | 188 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [0.94, 1.75] |
| 5.3 Manual acupuncture vs TCAs | 4 | 620 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [1.03, 1.69] |
| 5.4 Electro‐acupuncture vs TCAs | 4 | 778 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.88, 1.21] |
| 6 Dropout from treatment Show forest plot | 5 | 246 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.20, 3.71] |
| Analysis 3.6  Comparison 3 Acupuncture versus medication, Outcome 6 Dropout from treatment. | ||||
| 6.1 Manual acupuncture vs SSRI | 2 | 134 | Risk Ratio (M‐H, Random, 95% CI) | 0.27 [0.03, 2.47] |
| 6.2 Electro‐acupuncture vs SSRI | 3 | 112 | Risk Ratio (M‐H, Random, 95% CI) | 1.82 [0.43, 7.79] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severity of depression at the end of treatment Show forest plot | 11 | 813 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.15 [‐1.63, ‐0.66] |
| Analysis 4.1  Comparison 4 Acupuncture plus medication versus medication, Outcome 1 Severity of depression at the end of treatment. | ||||
| 1.1 Manual acupuncture plus SSRI vs SSRI | 8 | 539 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.32 [‐2.09, ‐0.55] |
| 1.2 Electro‐acupuncture plus SSRI vs SSRI | 5 | 274 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.84 [‐1.16, ‐0.51] |
| 2 Adverse events Show forest plot | 3 | 200 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.32 [‐2.86, 0.23] |
| Analysis 4.2 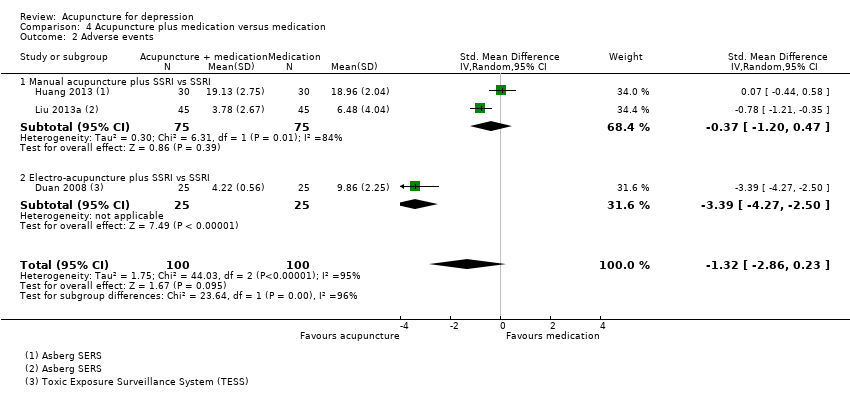 Comparison 4 Acupuncture plus medication versus medication, Outcome 2 Adverse events. | ||||
| 2.1 Manual acupuncture plus SSRI vs SSRI | 2 | 150 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐1.20, 0.47] |
| 2.2 Electro‐acupuncture plus SSRI vs SSRI | 1 | 50 | Std. Mean Difference (IV, Random, 95% CI) | ‐3.39 [‐4.27, ‐2.50] |
| 3 Severity of depression during treatment Show forest plot | 6 | 514 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.60 [‐2.45, ‐0.76] |
| Analysis 4.3 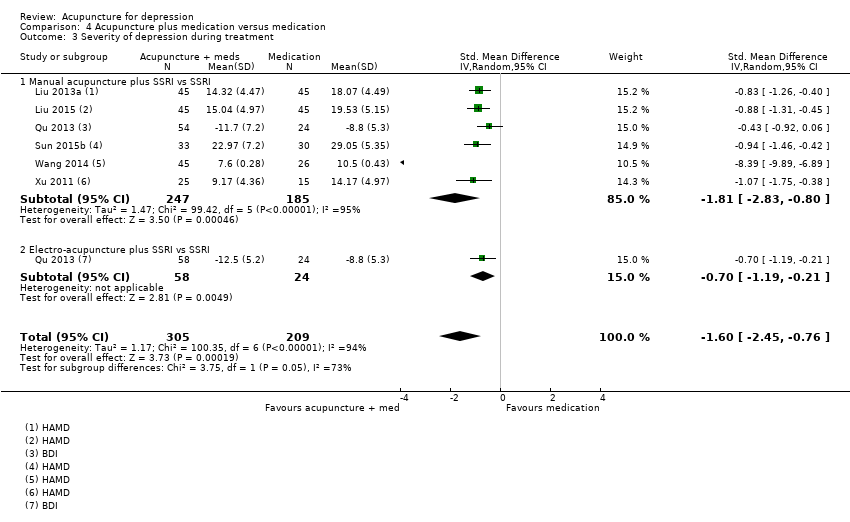 Comparison 4 Acupuncture plus medication versus medication, Outcome 3 Severity of depression during treatment. | ||||
| 3.1 Manual acupuncture plus SSRI vs SSRI | 6 | 432 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.81 [‐2.83, ‐0.80] |
| 3.2 Electro‐acupuncture plus SSRI vs SSRI | 1 | 82 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐1.19, ‐0.21] |
| 4 Remission of depression Show forest plot | 9 | 618 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.85, 1.73] |
| Analysis 4.4 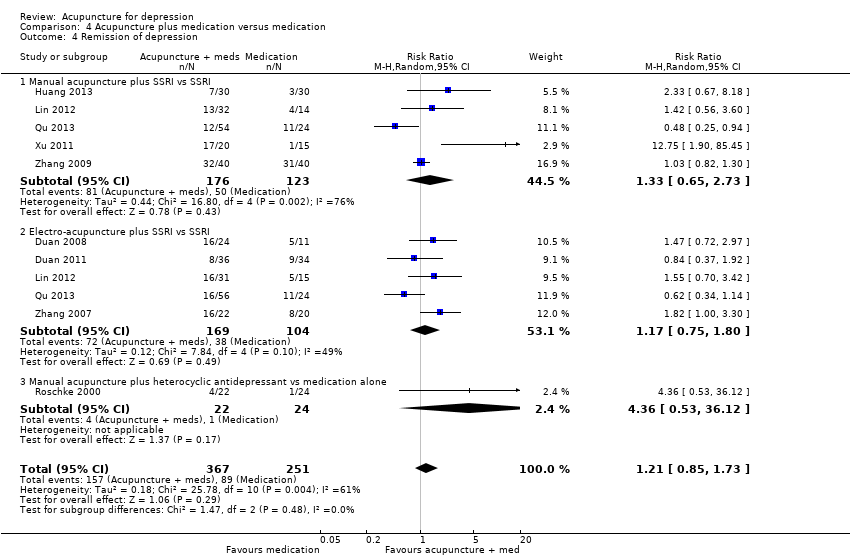 Comparison 4 Acupuncture plus medication versus medication, Outcome 4 Remission of depression. | ||||
| 4.1 Manual acupuncture plus SSRI vs SSRI | 5 | 299 | Risk Ratio (M‐H, Random, 95% CI) | 1.33 [0.65, 2.73] |
| 4.2 Electro‐acupuncture plus SSRI vs SSRI | 5 | 273 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [0.75, 1.80] |
| 4.3 Manual acupuncture plus heterocyclic antidepressant vs medication alone | 1 | 46 | Risk Ratio (M‐H, Random, 95% CI) | 4.36 [0.53, 36.12] |
| 5 Quality of life (physical) Show forest plot | 1 | 127 | Mean Difference (IV, Fixed, 95% CI) | 1.19 [0.33, 2.05] |
| Analysis 4.5 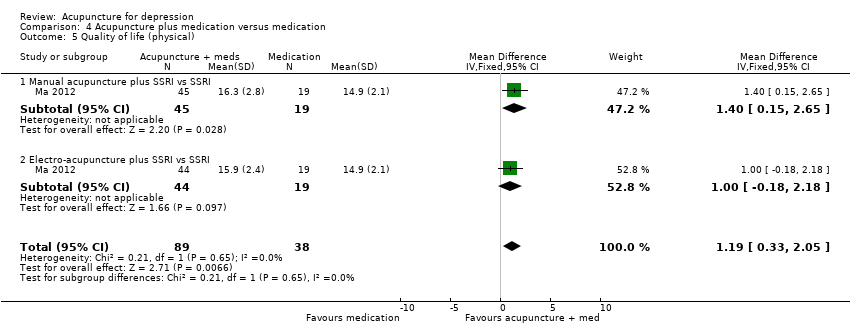 Comparison 4 Acupuncture plus medication versus medication, Outcome 5 Quality of life (physical). | ||||
| 5.1 Manual acupuncture plus SSRI vs SSRI | 1 | 64 | Mean Difference (IV, Fixed, 95% CI) | 1.40 [0.15, 2.65] |
| 5.2 Electro‐acupuncture plus SSRI vs SSRI | 1 | 63 | Mean Difference (IV, Fixed, 95% CI) | 1.0 [‐0.18, 2.18] |
| 6 Quality of life (emotional) Show forest plot | 2 | 219 | Mean Difference (IV, Random, 95% CI) | 0.25 [‐0.90, 1.40] |
| Analysis 4.6  Comparison 4 Acupuncture plus medication versus medication, Outcome 6 Quality of life (emotional). | ||||
| 6.1 Manual acupuncture plus SSRI vs SSRI | 2 | 111 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐1.46, 1.65] |
| 6.2 Electro‐acupuncture plus SSRI vs SSRI | 2 | 108 | Mean Difference (IV, Random, 95% CI) | 0.35 [‐2.00, 2.70] |
| 7 Change in use of medication Show forest plot | 2 | 236 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.22, 0.67] |
| Analysis 4.7  Comparison 4 Acupuncture plus medication versus medication, Outcome 7 Change in use of medication. | ||||
| 7.1 Manual acupuncture plus SSRI vs SSRI | 2 | 154 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.20, 0.72] |
| 7.2 Electro‐acupuncture plus SSRI vs SSRI | 1 | 82 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.13, 1.30] |
| 8 Dropout from treatment Show forest plot | 5 | 426 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.35, 1.42] |
| Analysis 4.8  Comparison 4 Acupuncture plus medication versus medication, Outcome 8 Dropout from treatment. | ||||
| 8.1 Manual acupuncture plus SSRI vs SSRI | 3 | 234 | Risk Ratio (M‐H, Random, 95% CI) | 0.45 [0.18, 1.15] |
| 8.2 Electro‐acupuncture plus SSRI vs SSRI | 3 | 192 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.43, 3.51] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severity of depression at the end of treatment Show forest plot | 2 | 497 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐1.33, 0.33] |
| Analysis 5.1  Comparison 5 Acupuncture versus psychological therapy, Outcome 1 Severity of depression at the end of treatment. | ||||
| 1.1 Manual acupuncture | 2 | 497 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐1.33, 0.33] |
| 2 Adverse events Show forest plot | 1 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.29, 1.33] |
| Analysis 5.2 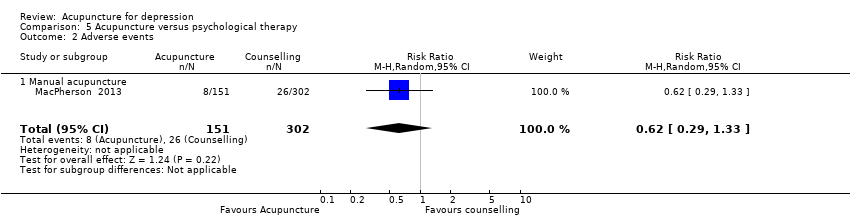 Comparison 5 Acupuncture versus psychological therapy, Outcome 2 Adverse events. | ||||
| 2.1 Manual acupuncture | 1 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.29, 1.33] |
| 3 Severity of depression 0‐6 months after treatment Show forest plot | 1 | 453 | Mean Difference (IV, Random, 95% CI) | 0.5 [‐0.51, 1.51] |
| Analysis 5.3  Comparison 5 Acupuncture versus psychological therapy, Outcome 3 Severity of depression 0‐6 months after treatment. | ||||
| 3.1 Manual acupuncture | 1 | 453 | Mean Difference (IV, Random, 95% CI) | 0.5 [‐0.51, 1.51] |
| 4 Severity of depression 6‐12 months Show forest plot | 1 | 453 | Mean Difference (IV, Random, 95% CI) | 0.60 [‐0.80, 2.00] |
| Analysis 5.4  Comparison 5 Acupuncture versus psychological therapy, Outcome 4 Severity of depression 6‐12 months. | ||||
| 4.1 Manual acupuncture | 1 | 453 | Mean Difference (IV, Random, 95% CI) | 0.60 [‐0.80, 2.00] |
| 5 Remission of depression | 0 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 Manual acupuncture | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Change in use of medication Show forest plot | 1 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.61, 1.10] |
| Analysis 5.6  Comparison 5 Acupuncture versus psychological therapy, Outcome 6 Change in use of medication. | ||||
| 6.1 Manual acupuncture | 1 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.61, 1.10] |
| 7 Dropout from treatment Show forest plot | 1 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 0.27 [0.08, 0.90] |
| Analysis 5.7  Comparison 5 Acupuncture versus psychological therapy, Outcome 7 Dropout from treatment. | ||||
| 7.1 Manual acupuncture | 1 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 0.27 [0.08, 0.90] |
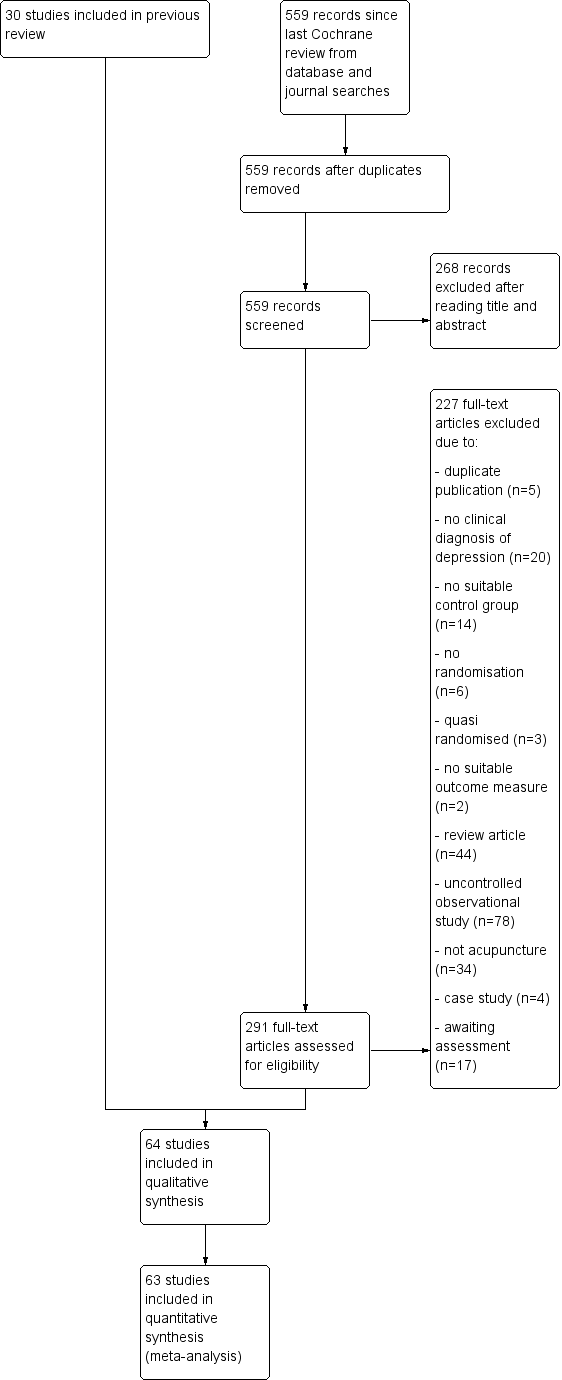
Study flow diagram.

Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
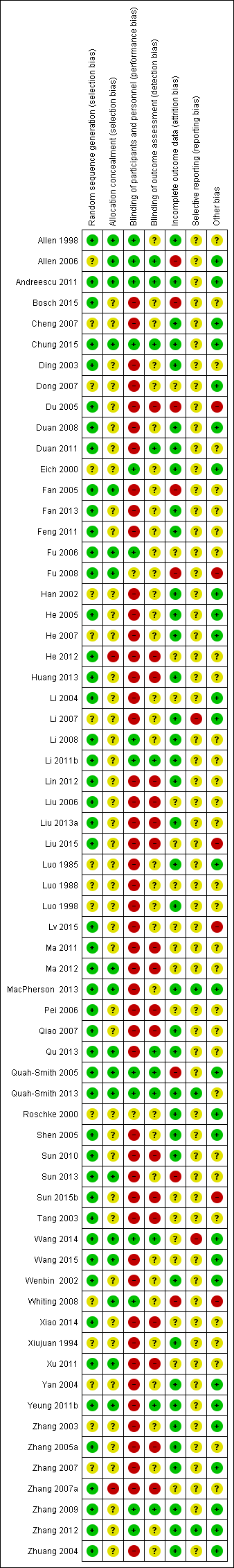
Review authors' judgements about each 'risk of bias' domain for each included study.

Forest plot of comparison: 1 Acupuncture versus no treatment/wait list/TAU, outcome: 1.1 Severity of depression at the end of treatment.

Forest plot of comparison: 2 Acupuncture versus control acupuncture, outcome: 2.1 Severity of depression at the end of the intervention.

Forest plot of comparison: 3 Acupuncture versus medication, outcome: 3.1 Severity of depression at the end of treatment.

Forest plot of comparison: 4 Acupuncture plus medication vs medication, outcome: 4.1 Severity of depression at the end of treatment.
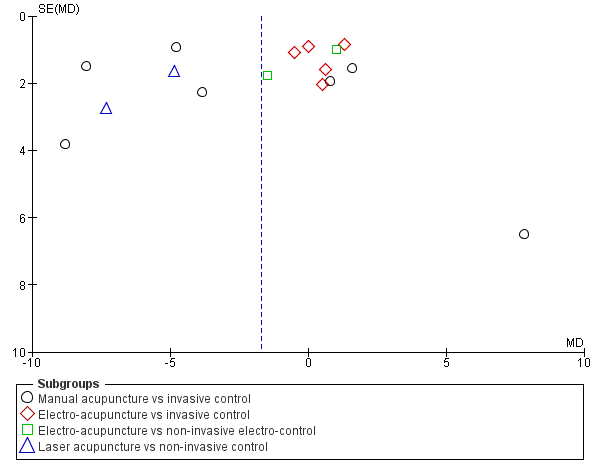
Funnel plot of comparison: 2 Acupuncture versus control acupuncture, outcome: 2.1 Severity of depression at the end of the intervention.

Funnel plot of comparison: 3 Acupuncture versus medication, outcome: 3.1 Severity of depression at the end of treatment.
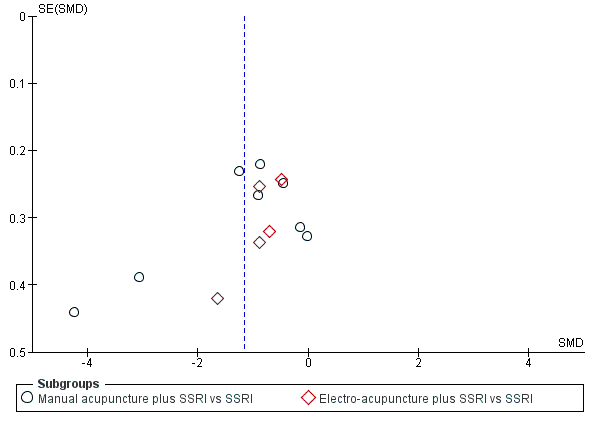
Funnel plot of comparison: 4 Acupuncture plus medication vs medication, outcome: 4.1 Severity of depression at the end of treatment.

Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 1 Severity of depression at the end of treatment.

Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 2 Adverse events.
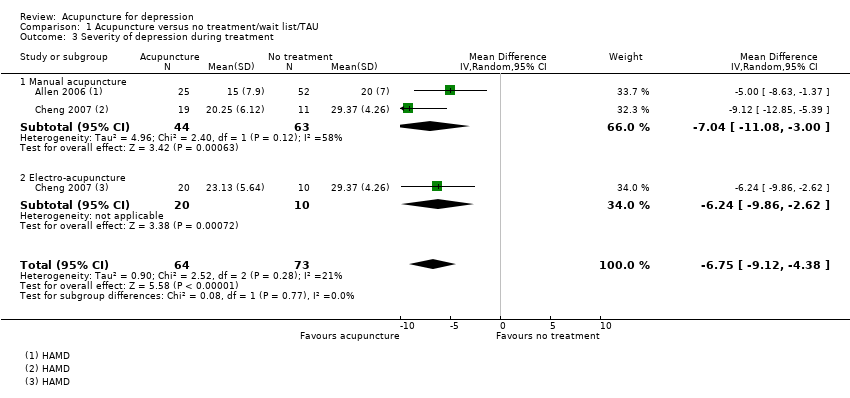
Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 3 Severity of depression during treatment.

Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 4 Severity of depression 0‐6 months after treatment.
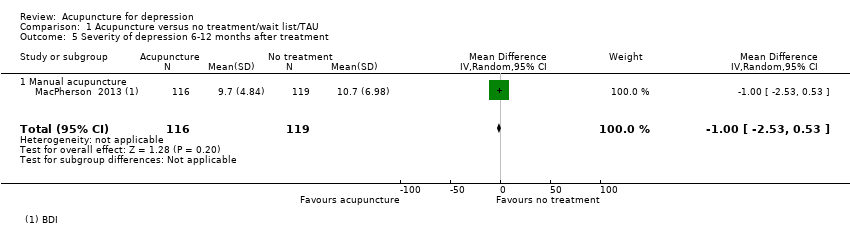
Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 5 Severity of depression 6‐12 months after treatment.
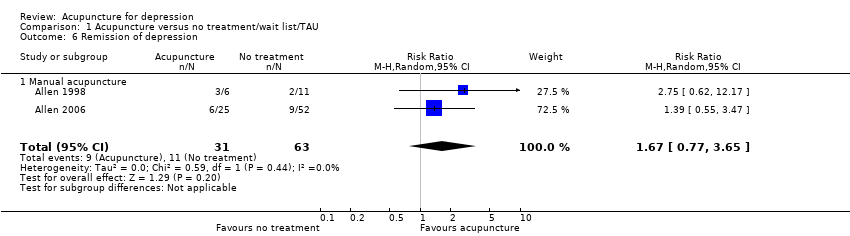
Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 6 Remission of depression.
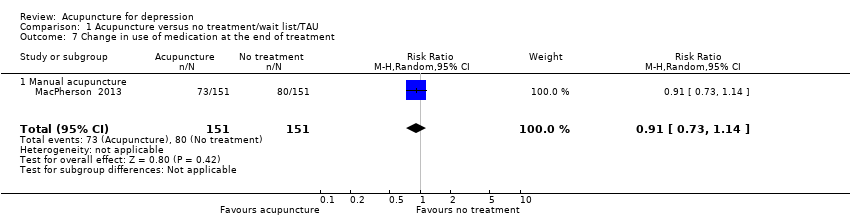
Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 7 Change in use of medication at the end of treatment.

Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 8 Dropout from treatment.

Comparison 2 Acupuncture versus control acupuncture, Outcome 1 Severity of depression at the end of the intervention.

Comparison 2 Acupuncture versus control acupuncture, Outcome 2 Adverse events.
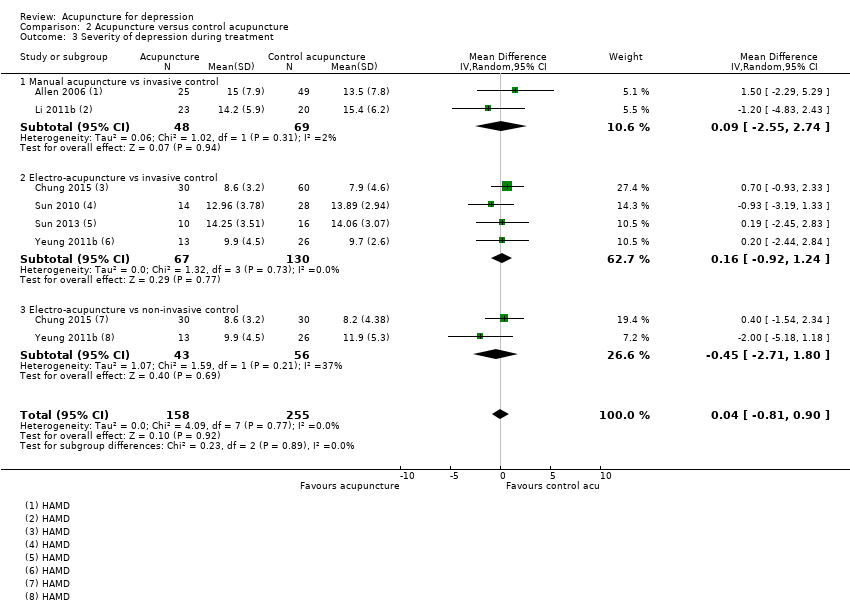
Comparison 2 Acupuncture versus control acupuncture, Outcome 3 Severity of depression during treatment.
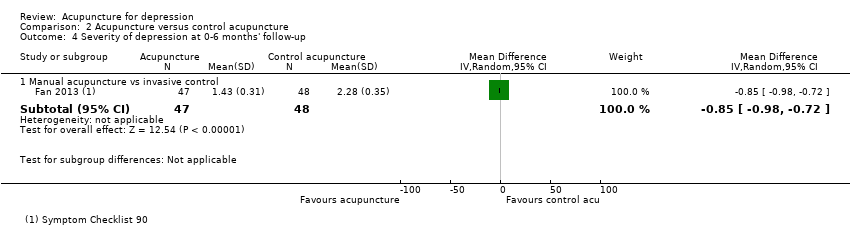
Comparison 2 Acupuncture versus control acupuncture, Outcome 4 Severity of depression at 0‐6 months' follow‐up.
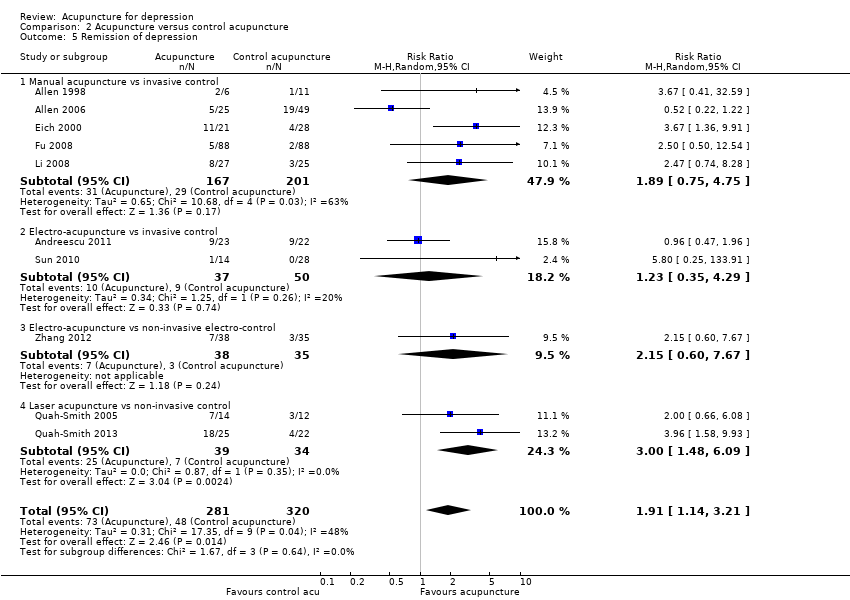
Comparison 2 Acupuncture versus control acupuncture, Outcome 5 Remission of depression.

Comparison 2 Acupuncture versus control acupuncture, Outcome 6 Quality of life (emotional) during treatment.
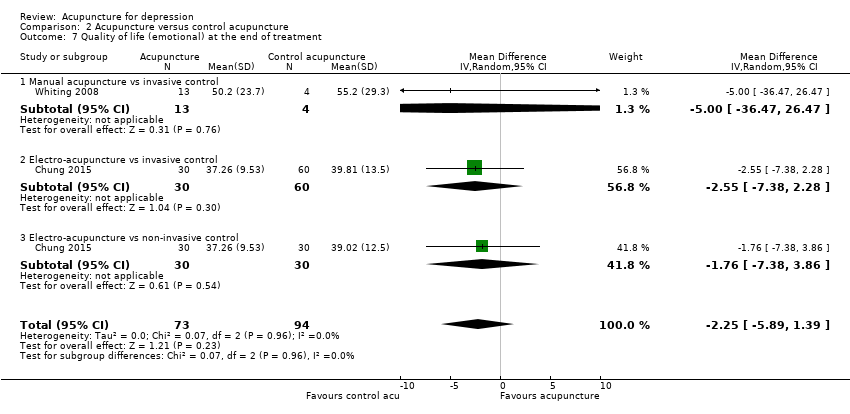
Comparison 2 Acupuncture versus control acupuncture, Outcome 7 Quality of life (emotional) at the end of treatment.

Comparison 2 Acupuncture versus control acupuncture, Outcome 8 Quality of life (physical) during treatment.
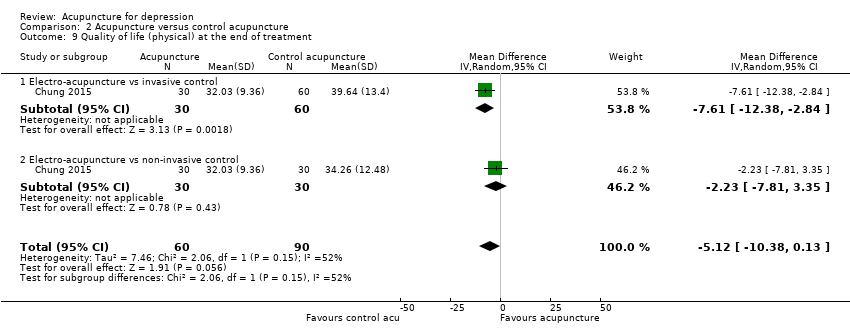
Comparison 2 Acupuncture versus control acupuncture, Outcome 9 Quality of life (physical) at the end of treatment.

Comparison 2 Acupuncture versus control acupuncture, Outcome 10 Change in medication.

Comparison 2 Acupuncture versus control acupuncture, Outcome 11 Dropout from treatment.
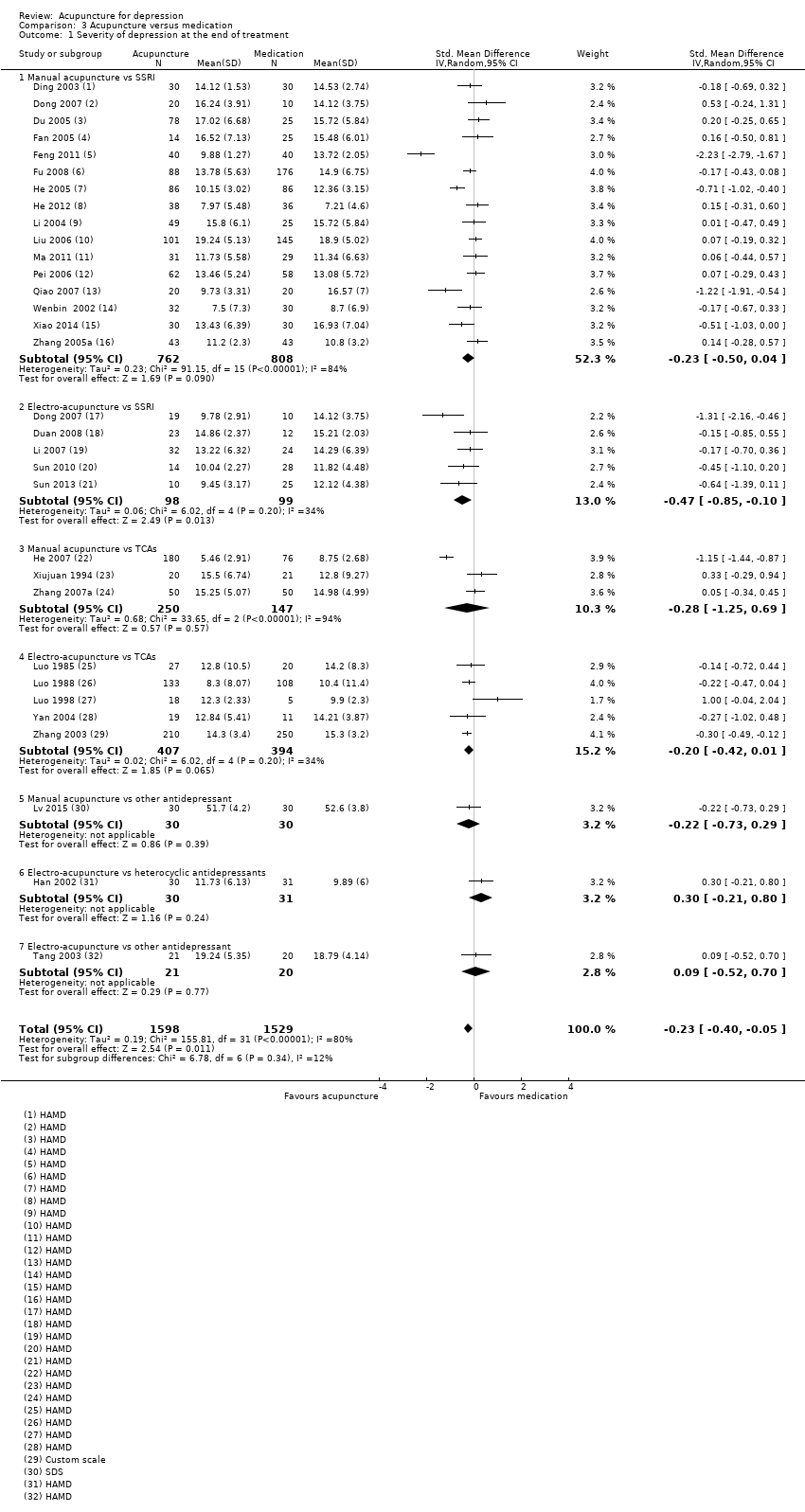
Comparison 3 Acupuncture versus medication, Outcome 1 Severity of depression at the end of treatment.

Comparison 3 Acupuncture versus medication, Outcome 2 Adverse events.

Comparison 3 Acupuncture versus medication, Outcome 3 Severity of depression during treatment.

Comparison 3 Acupuncture versus medication, Outcome 4 Severity of depression 0‐6 months after treatment.

Comparison 3 Acupuncture versus medication, Outcome 5 Remission of depression.
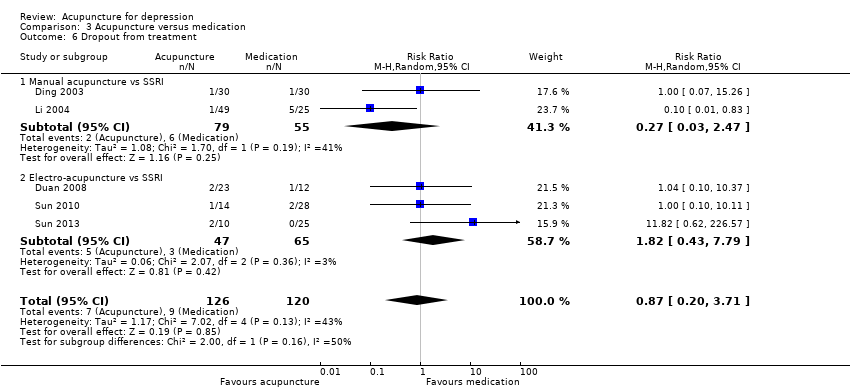
Comparison 3 Acupuncture versus medication, Outcome 6 Dropout from treatment.

Comparison 4 Acupuncture plus medication versus medication, Outcome 1 Severity of depression at the end of treatment.
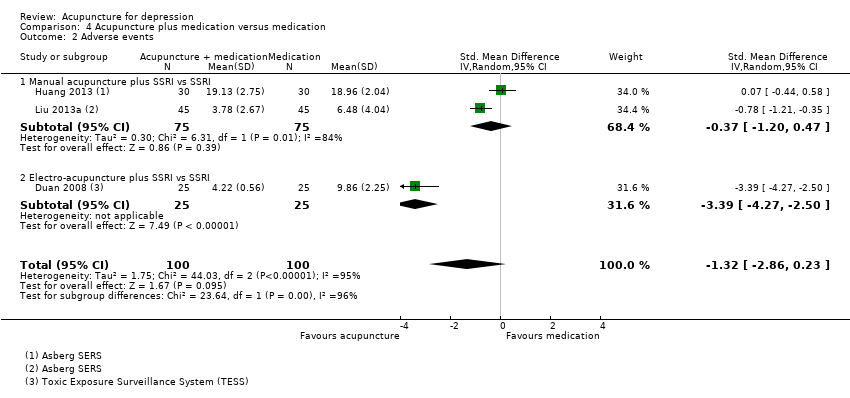
Comparison 4 Acupuncture plus medication versus medication, Outcome 2 Adverse events.
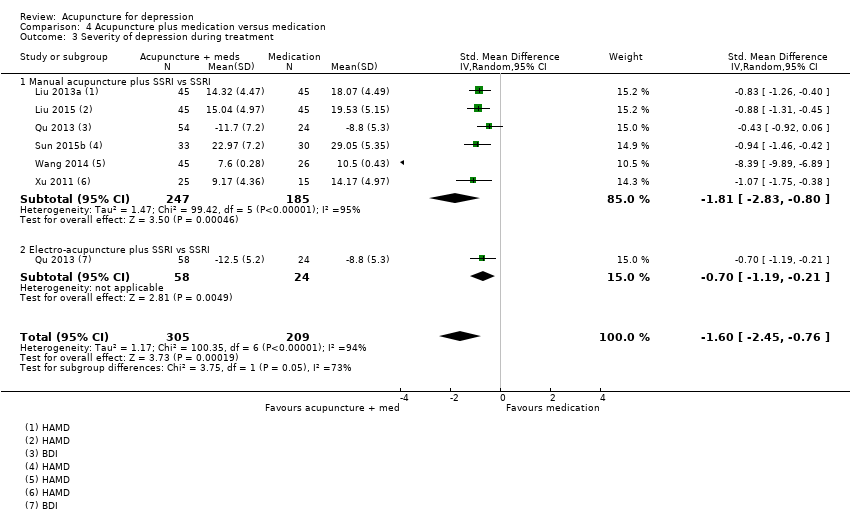
Comparison 4 Acupuncture plus medication versus medication, Outcome 3 Severity of depression during treatment.

Comparison 4 Acupuncture plus medication versus medication, Outcome 4 Remission of depression.
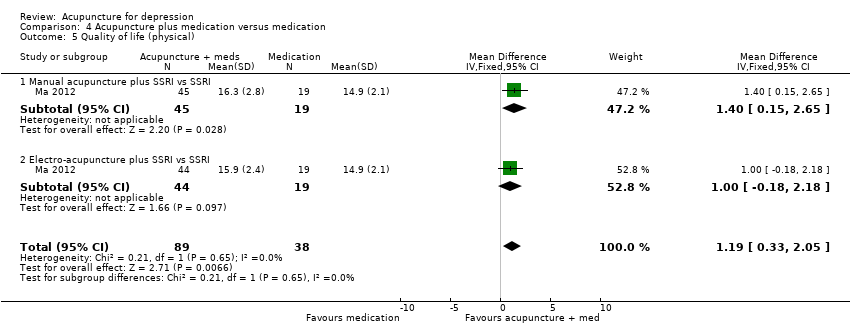
Comparison 4 Acupuncture plus medication versus medication, Outcome 5 Quality of life (physical).

Comparison 4 Acupuncture plus medication versus medication, Outcome 6 Quality of life (emotional).
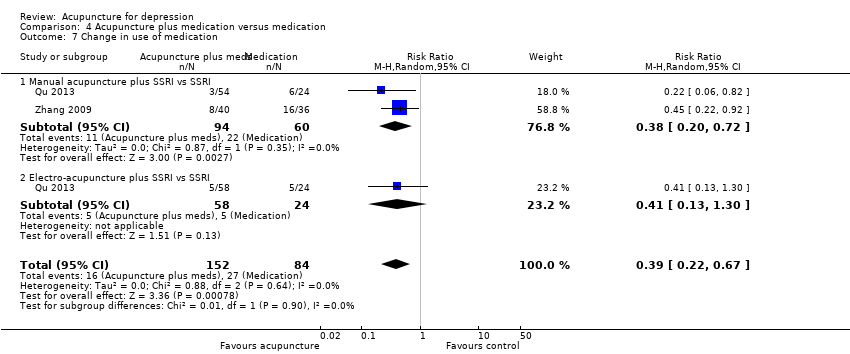
Comparison 4 Acupuncture plus medication versus medication, Outcome 7 Change in use of medication.
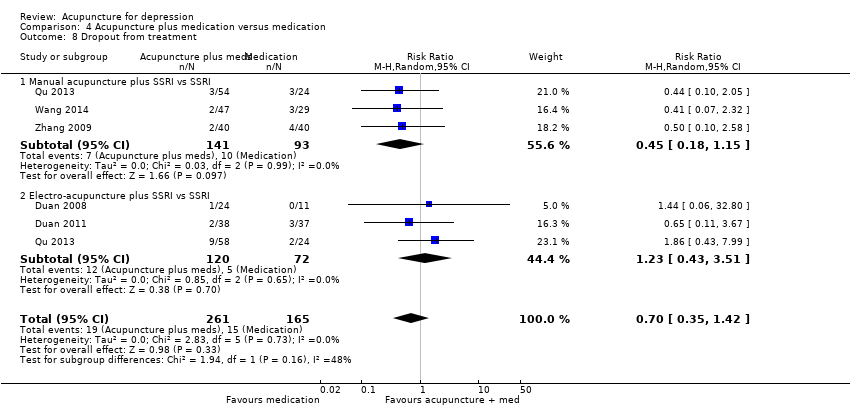
Comparison 4 Acupuncture plus medication versus medication, Outcome 8 Dropout from treatment.

Comparison 5 Acupuncture versus psychological therapy, Outcome 1 Severity of depression at the end of treatment.

Comparison 5 Acupuncture versus psychological therapy, Outcome 2 Adverse events.

Comparison 5 Acupuncture versus psychological therapy, Outcome 3 Severity of depression 0‐6 months after treatment.

Comparison 5 Acupuncture versus psychological therapy, Outcome 4 Severity of depression 6‐12 months.

Comparison 5 Acupuncture versus psychological therapy, Outcome 6 Change in use of medication.

Comparison 5 Acupuncture versus psychological therapy, Outcome 7 Dropout from treatment.
| Acupuncture compared with no treatment/wait list/treatment as usual for depression | ||||||
| Patient or population: clinical diagnosis of depression | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with no treatment/wait list/treatment as usual | Risk with acupuncture | |||||
| Severity of depression at the end of treatment | SMD 0.66 lower | ‐ | 488 | ⊕⊕⊝⊝ | As a rule of thumb, 0.2 SMD represents a small difference, 0.5 moderate, and 0.8 large. | |
| Adverse events | Study population | RR 0.89 | 302 | ⊕⊕⊝⊝ | ||
| 60 per 1000 | 53 per 1000 | |||||
| Quality of life (physical) | ‐ | ‐ | ‐ | ‐ | ‐ | Cannot estimate the effect of acupuncture as no studies reported on this outcome |
| Quality of life (emotional) | ‐ | ‐ | ‐ | ‐ | ‐ | Cannot estimate the effect of acupuncture as no studies reported on this outcome |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level owing to high risk of performance bias across most included studies. bDowngraded one level owing to substantial heterogeneity (I2 = 64%, Tau2 = 0.14, P = 0.02). cDowngraded one level owing to high risk of performance bias. dDowngraded one level owing to small sample size for detecting relatively rare events. | ||||||
| Acupuncture compared with control acupuncture for depression | ||||||
| Patient or population: clinical diagnosis of depression | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with control acupuncture | Risk with acupuncture | |||||
| Severity of depression at the end of the intervention as measured by the Hamilton Depression Rating Scale (HAMD) scored from 0 to 54 (lower score indicates less severe depression) | In the study population, average severity of depression at the end of treatment was 11.4 in clinician‐rated HAMD scores. | MD 1.69 lower | ‐ | 841 | ⊕⊕⊝⊝ | |
| Adverse events | Study population | RR 1.63 | 300 | ⊕⊕⊕⊝ | ||
| 162 per 1000 | 264 per 1000 | |||||
| Quality of life (physical) at the end of treatment (higher scores indicate greater quality of life) | Mean quality of life (physical) at the end of treatment was 37. | MD 5.12 lower | ‐ | 150 | ⊕⊕⊝⊝ | |
| Quality of life (emotional) at the end of treatment (higher scores indicate greater quality of life) | Mean quality of life (emotional) at the end of treatment was 44.6. | MD 2.25 lower | ‐ | 167 | ⊕⊕⊕⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level owing to high risk of bias in performance bias in five of the included studies and high risk of bias in at least one domain in most studies. bDowngraded one level owing to substantial heterogeneity (I2 = 80%, Tau2 = 7.80, P < 0.001). cDowngraded one level owing to small sample size for relatively rare events. dDowngraded one level because only one small study contributed to this outcome. eDowngraded one level for imprecision due to small sample size. | ||||||
| Acupuncture compared with medication for depression | ||||||
| Patient or population: clinical diagnosis of depression | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with medication | Risk with acupuncture | |||||
| Severity of depression at the end of treatment | SMD 0.23 lower | ‐ | 3127 | ⊕⊝⊝⊝ | As a rule of thumb, 0.2 SMD represents a small difference, 0.5 moderate, and 0.8 large. | |
| Adverse events (measured with Asberg Antidepressant Side Effect Scale) | Mean number of adverse events was 6.2. | MD 4.32 lower | ‐ | 481 | ⊕⊝⊝⊝ | |
| Quality of life (physical) | ‐ | ‐ | No studies reported on this outcome. | ‐ | Cannot estimate the effect of acupuncture as no studies reported on this outcome | |
| Quality of life (emotional) | ‐ | ‐ | No studies reported on this outcome. | ‐ | Cannot estimate the effect of acupuncture as no studies reported on this outcome | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded two levels owing to very serious risk of bias. Of 31 trials, 30 were at high risk of bias owing to lack of blinding of participants, and 12 were at high risk of bias owing to lack of blinding of outcome assessors. bDowngraded one level owing to substantial heterogeneity (I2 = 80%, Tau2 = 0.19, P < 0.0001). cDowngraded two levels owing to very serious risk of bias in all three studies. dDowngraded two levels owing to considerable heterogeneity (I2 = 97%, Tau2 = 7.22, P < 0.001). | ||||||
| Acupuncture plus medication compared with medication for depression | ||||||
| Patient or population: clinical diagnosis of depression | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with medication | Risk with acupuncture plus medication | |||||
| Severity of depression at the end of treatment | SMD 1.15 lower | ‐ | 813 | ⊕⊝⊝⊝ | As a rule of thumb, 0.2 SMD represents a small difference, 0.5 moderate, and 0.8 large. | |
| Adverse events (measured with Asberg Antidepressant Side Effect Scale and Toxic Exposure Surveillance System) | SMD 1.32 lower | ‐ | 200 | ⊕⊝⊝⊝ | As a rule of thumb, 0.2 SMD represents a small difference, 0.5 moderate, and 0.8 large. | |
| Quality of life (physical) at the end of treatment (higher scores indicate greater quality of life) | Quality of life (physical) score in the single included study was 14.9. | MD 1.19 higher | ‐ | 127 | ⊕⊝⊝⊝ | |
| Quality of life (emotional) at the end of treatment (higher scores indicate greater quality of life) | Mean quality of life (emotional) score was 17.2. | MD 0.25 higher | ‐ | 219 | ⊕⊝⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded two levels owing to very serious risk of bias. Of 11 trials, nine were at high risk of bias owing to lack of blinding of participants, and 6 were at high risk of bias owing to lack of blinding of outcome assessors. bDowngraded two levels owing to considerable heterogeneity (I2 = 89%, Tau2 = 0.70, P < 0.001). fDowngraded two levels owing to very serious risk of bias. | ||||||
| Acupuncture compared with psychological therapy for depression | ||||||
| Patient or population: clinical diagnosis of depression | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with psychological therapy | Risk with acupuncture | |||||
| Severity of depression at the end of treatment as measured by self‐rated depression scores (lower score indicates less severe depression) | SMD 0.5 lower | ‐ | 497 | ⊕⊕⊝⊝ | As a rule of thumb, 0.2 SMD represents a small difference, 0.5 moderate, and 0.8 large. | |
| Adverse events measured during study treatment | Study population | RR 0.62 | 453 | ⊕⊕⊝⊝ | ||
| 86 per 1000 | 53 per 1000 | |||||
| Quality of life (physical) | ‐ | ‐ | ‐ | No studies reported on this outcome. | ‐ | Cannot estimate the effect of acupuncture as no studies reported on this outcome |
| Quality of life (emotional) | ‐ | ‐ | ‐ | No studies reported on this outcome. | ‐ | Cannot estimate the effect of acupuncture as no studies reported on this outcome |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level for serious risk of bias; both included trials have high risk of performance bias. dDowngraded one level owing to high risk of performance bias. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severity of depression at the end of treatment Show forest plot | 5 | 488 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.66 [‐1.06, ‐0.25] |
| 1.1 Manual acupuncture | 5 | 458 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.56 [‐0.98, ‐0.15] |
| 1.2 Electro‐acupuncture | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.26 [‐2.10, ‐0.43] |
| 2 Adverse events Show forest plot | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.35, 2.24] |
| 2.1 Manual acupuncture | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.35, 2.24] |
| 3 Severity of depression during treatment Show forest plot | 2 | 137 | Mean Difference (IV, Random, 95% CI) | ‐6.75 [‐9.12, ‐4.38] |
| 3.1 Manual acupuncture | 2 | 107 | Mean Difference (IV, Random, 95% CI) | ‐7.04 [‐11.08, ‐3.00] |
| 3.2 Electro‐acupuncture | 1 | 30 | Mean Difference (IV, Random, 95% CI) | ‐6.24 [‐9.86, ‐2.62] |
| 4 Severity of depression 0‐6 months after treatment Show forest plot | 1 | 237 | Mean Difference (IV, Random, 95% CI) | ‐1.90 [‐3.01, ‐0.79] |
| 4.1 Manual acupuncture | 1 | 237 | Mean Difference (IV, Random, 95% CI) | ‐1.90 [‐3.01, ‐0.79] |
| 5 Severity of depression 6‐12 months after treatment Show forest plot | 1 | 235 | Mean Difference (IV, Random, 95% CI) | ‐1.0 [‐2.53, 0.53] |
| 5.1 Manual acupuncture | 1 | 235 | Mean Difference (IV, Random, 95% CI) | ‐1.0 [‐2.53, 0.53] |
| 6 Remission of depression Show forest plot | 2 | 94 | Risk Ratio (M‐H, Random, 95% CI) | 1.67 [0.77, 3.65] |
| 6.1 Manual acupuncture | 2 | 94 | Risk Ratio (M‐H, Random, 95% CI) | 1.67 [0.77, 3.65] |
| 7 Change in use of medication at the end of treatment Show forest plot | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.73, 1.14] |
| 7.1 Manual acupuncture | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.73, 1.14] |
| 8 Dropout from treatment Show forest plot | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.21, 4.88] |
| 8.1 Manual acupuncture | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.21, 4.88] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severity of depression at the end of the intervention Show forest plot | 14 | 841 | Mean Difference (IV, Random, 95% CI) | ‐1.69 [‐3.33, ‐0.05] |
| 1.1 Manual acupuncture vs invasive control | 7 | 418 | Mean Difference (IV, Random, 95% CI) | ‐2.97 [‐6.26, 0.31] |
| 1.2 Electro‐acupuncture vs invasive control | 5 | 251 | Mean Difference (IV, Random, 95% CI) | 0.43 [‐0.54, 1.40] |
| 1.3 Electro‐acupuncture vs non‐invasive electro‐control | 2 | 99 | Mean Difference (IV, Random, 95% CI) | 0.17 [‐2.14, 2.48] |
| 1.4 Laser acupuncture vs non‐invasive control | 2 | 73 | Mean Difference (IV, Random, 95% CI) | ‐5.51 [‐8.30, ‐2.73] |
| 2 Adverse events Show forest plot | 5 | 300 | Risk Ratio (M‐H, Random, 95% CI) | 1.63 [0.93, 2.86] |
| 2.1 Manual acupuncture vs invasive control | 1 | 17 | Risk Ratio (M‐H, Random, 95% CI) | 2.5 [0.15, 40.37] |
| 2.2 Electro‐acupuncture vs invasive control | 4 | 244 | Risk Ratio (M‐H, Random, 95% CI) | 1.79 [0.99, 3.25] |
| 2.3 Electro‐acupuncture vs non‐invasive control | 1 | 39 | Risk Ratio (M‐H, Random, 95% CI) | 0.4 [0.05, 3.08] |
| 3 Severity of depression during treatment Show forest plot | 6 | 413 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.81, 0.90] |
| 3.1 Manual acupuncture vs invasive control | 2 | 117 | Mean Difference (IV, Random, 95% CI) | 0.09 [‐2.55, 2.74] |
| 3.2 Electro‐acupuncture vs invasive control | 4 | 197 | Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.92, 1.24] |
| 3.3 Electro‐acupuncture vs non‐invasive control | 2 | 99 | Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐2.71, 1.80] |
| 4 Severity of depression at 0‐6 months' follow‐up Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Manual acupuncture vs invasive control | 1 | 95 | Mean Difference (IV, Random, 95% CI) | ‐0.85 [‐0.98, ‐0.72] |
| 5 Remission of depression Show forest plot | 10 | 601 | Risk Ratio (M‐H, Random, 95% CI) | 1.91 [1.14, 3.21] |
| 5.1 Manual acupuncture vs invasive control | 5 | 368 | Risk Ratio (M‐H, Random, 95% CI) | 1.89 [0.75, 4.75] |
| 5.2 Electro‐acupuncture vs invasive control | 2 | 87 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.35, 4.29] |
| 5.3 Electro‐acupuncture vs non‐invasive electro‐control | 1 | 73 | Risk Ratio (M‐H, Random, 95% CI) | 2.15 [0.60, 7.67] |
| 5.4 Laser acupuncture vs non‐invasive control | 2 | 73 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [1.48, 6.09] |
| 6 Quality of life (emotional) during treatment Show forest plot | 1 | 150 | Mean Difference (IV, Random, 95% CI) | ‐1.98 [‐5.41, 1.45] |
| 6.1 Electro‐acupuncture vs invasive control | 1 | 90 | Mean Difference (IV, Random, 95% CI) | ‐2.09 [‐6.54, 2.36] |
| 6.2 Electro‐acupuncture vs non‐invasive control | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐1.81 [‐7.18, 3.56] |
| 7 Quality of life (emotional) at the end of treatment Show forest plot | 2 | 167 | Mean Difference (IV, Random, 95% CI) | ‐2.25 [‐5.89, 1.39] |
| 7.1 Manual acupuncture vs invasive control | 1 | 17 | Mean Difference (IV, Random, 95% CI) | ‐5.0 [‐36.47, 26.47] |
| 7.2 Electro‐acupuncture vs invasive control | 1 | 90 | Mean Difference (IV, Random, 95% CI) | ‐2.55 [‐7.38, 2.28] |
| 7.3 Electro‐acupuncture vs non‐invasive control | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐1.76 [‐7.38, 3.86] |
| 8 Quality of life (physical) during treatment Show forest plot | 1 | 150 | Mean Difference (IV, Random, 95% CI) | ‐0.99 [‐4.74, 2.77] |
| 8.1 Electro‐acupuncture vs invasive control | 1 | 90 | Mean Difference (IV, Random, 95% CI) | ‐2.62 [‐7.07, 1.83] |
| 8.2 Electro‐acupuncture vs non‐invasive control | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 1.26 [‐4.12, 6.64] |
| 9 Quality of life (physical) at the end of treatment Show forest plot | 1 | 150 | Mean Difference (IV, Random, 95% CI) | ‐5.12 [‐10.38, 0.13] |
| 9.1 Electro‐acupuncture vs invasive control | 1 | 90 | Mean Difference (IV, Random, 95% CI) | ‐7.61 [‐12.38, ‐2.84] |
| 9.2 Electro‐acupuncture vs non‐invasive control | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐2.23 [‐7.81, 3.35] |
| 10 Change in medication Show forest plot | 1 | 70 | Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐1.71, 0.93] |
| 10.1 Electro‐acupuncture vs non‐invasive control | 1 | 70 | Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐1.71, 0.93] |
| 11 Dropout from treatment Show forest plot | 7 | 501 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.62, 1.75] |
| 11.1 Manual acupuncture vs invasive control | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.6 [0.16, 2.29] |
| 11.2 Electro‐acupuncture vs invasive control | 4 | 224 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.51, 2.02] |
| 11.3 Electro‐acupuncture vs non‐invasive control | 4 | 217 | Risk Ratio (M‐H, Random, 95% CI) | 1.48 [0.56, 3.91] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severity of depression at the end of treatment Show forest plot | 31 | 3127 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.40, ‐0.05] |
| 1.1 Manual acupuncture vs SSRI | 16 | 1570 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.50, 0.04] |
| 1.2 Electro‐acupuncture vs SSRI | 5 | 197 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.47 [‐0.85, ‐0.10] |
| 1.3 Manual acupuncture vs TCAs | 3 | 397 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐1.25, 0.69] |
| 1.4 Electro‐acupuncture vs TCAs | 5 | 801 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.42, 0.01] |
| 1.5 Manual acupuncture vs other antidepressant | 1 | 60 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.73, 0.29] |
| 1.6 Electro‐acupuncture vs heterocyclic antidepressants | 1 | 61 | Std. Mean Difference (IV, Random, 95% CI) | 0.30 [‐0.21, 0.80] |
| 1.7 Electro‐acupuncture vs other antidepressant | 1 | 41 | Std. Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.52, 0.70] |
| 2 Adverse events Show forest plot | 3 | 481 | Mean Difference (IV, Random, 95% CI) | ‐4.32 [‐7.41, ‐1.23] |
| 2.1 Manual acupuncture vs SSRI | 3 | 481 | Mean Difference (IV, Random, 95% CI) | ‐4.32 [‐7.41, ‐1.23] |
| 3 Severity of depression during treatment Show forest plot | 9 | 552 | Mean Difference (IV, Random, 95% CI) | ‐1.67 [‐2.91, ‐0.43] |
| 3.1 Manual acupuncture vs SSRI | 5 | 340 | Mean Difference (IV, Random, 95% CI) | ‐1.38 [‐3.20, 0.45] |
| 3.2 Electro‐acupuncture vs SSRI | 3 | 112 | Mean Difference (IV, Random, 95% CI) | ‐2.58 [‐4.38, ‐0.78] |
| 3.3 Manual acupuncture vs TCAs | 1 | 100 | Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐3.65, 2.05] |
| 4 Severity of depression 0‐6 months after treatment Show forest plot | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐5.60 [‐7.60, ‐3.60] |
| 4.1 Manual acupuncture vs other antidepressant medication | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐5.60 [‐7.60, ‐3.60] |
| 5 Remission of depression Show forest plot | 25 | 2918 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [1.05, 1.29] |
| 5.1 Manual acupuncture vs SSRI | 14 | 1332 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.98, 1.37] |
| 5.2 Electro‐acupuncture vs SSRI | 4 | 188 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [0.94, 1.75] |
| 5.3 Manual acupuncture vs TCAs | 4 | 620 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [1.03, 1.69] |
| 5.4 Electro‐acupuncture vs TCAs | 4 | 778 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.88, 1.21] |
| 6 Dropout from treatment Show forest plot | 5 | 246 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.20, 3.71] |
| 6.1 Manual acupuncture vs SSRI | 2 | 134 | Risk Ratio (M‐H, Random, 95% CI) | 0.27 [0.03, 2.47] |
| 6.2 Electro‐acupuncture vs SSRI | 3 | 112 | Risk Ratio (M‐H, Random, 95% CI) | 1.82 [0.43, 7.79] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severity of depression at the end of treatment Show forest plot | 11 | 813 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.15 [‐1.63, ‐0.66] |
| 1.1 Manual acupuncture plus SSRI vs SSRI | 8 | 539 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.32 [‐2.09, ‐0.55] |
| 1.2 Electro‐acupuncture plus SSRI vs SSRI | 5 | 274 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.84 [‐1.16, ‐0.51] |
| 2 Adverse events Show forest plot | 3 | 200 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.32 [‐2.86, 0.23] |
| 2.1 Manual acupuncture plus SSRI vs SSRI | 2 | 150 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐1.20, 0.47] |
| 2.2 Electro‐acupuncture plus SSRI vs SSRI | 1 | 50 | Std. Mean Difference (IV, Random, 95% CI) | ‐3.39 [‐4.27, ‐2.50] |
| 3 Severity of depression during treatment Show forest plot | 6 | 514 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.60 [‐2.45, ‐0.76] |
| 3.1 Manual acupuncture plus SSRI vs SSRI | 6 | 432 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.81 [‐2.83, ‐0.80] |
| 3.2 Electro‐acupuncture plus SSRI vs SSRI | 1 | 82 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐1.19, ‐0.21] |
| 4 Remission of depression Show forest plot | 9 | 618 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.85, 1.73] |
| 4.1 Manual acupuncture plus SSRI vs SSRI | 5 | 299 | Risk Ratio (M‐H, Random, 95% CI) | 1.33 [0.65, 2.73] |
| 4.2 Electro‐acupuncture plus SSRI vs SSRI | 5 | 273 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [0.75, 1.80] |
| 4.3 Manual acupuncture plus heterocyclic antidepressant vs medication alone | 1 | 46 | Risk Ratio (M‐H, Random, 95% CI) | 4.36 [0.53, 36.12] |
| 5 Quality of life (physical) Show forest plot | 1 | 127 | Mean Difference (IV, Fixed, 95% CI) | 1.19 [0.33, 2.05] |
| 5.1 Manual acupuncture plus SSRI vs SSRI | 1 | 64 | Mean Difference (IV, Fixed, 95% CI) | 1.40 [0.15, 2.65] |
| 5.2 Electro‐acupuncture plus SSRI vs SSRI | 1 | 63 | Mean Difference (IV, Fixed, 95% CI) | 1.0 [‐0.18, 2.18] |
| 6 Quality of life (emotional) Show forest plot | 2 | 219 | Mean Difference (IV, Random, 95% CI) | 0.25 [‐0.90, 1.40] |
| 6.1 Manual acupuncture plus SSRI vs SSRI | 2 | 111 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐1.46, 1.65] |
| 6.2 Electro‐acupuncture plus SSRI vs SSRI | 2 | 108 | Mean Difference (IV, Random, 95% CI) | 0.35 [‐2.00, 2.70] |
| 7 Change in use of medication Show forest plot | 2 | 236 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.22, 0.67] |
| 7.1 Manual acupuncture plus SSRI vs SSRI | 2 | 154 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.20, 0.72] |
| 7.2 Electro‐acupuncture plus SSRI vs SSRI | 1 | 82 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.13, 1.30] |
| 8 Dropout from treatment Show forest plot | 5 | 426 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.35, 1.42] |
| 8.1 Manual acupuncture plus SSRI vs SSRI | 3 | 234 | Risk Ratio (M‐H, Random, 95% CI) | 0.45 [0.18, 1.15] |
| 8.2 Electro‐acupuncture plus SSRI vs SSRI | 3 | 192 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.43, 3.51] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severity of depression at the end of treatment Show forest plot | 2 | 497 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐1.33, 0.33] |
| 1.1 Manual acupuncture | 2 | 497 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐1.33, 0.33] |
| 2 Adverse events Show forest plot | 1 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.29, 1.33] |
| 2.1 Manual acupuncture | 1 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.29, 1.33] |
| 3 Severity of depression 0‐6 months after treatment Show forest plot | 1 | 453 | Mean Difference (IV, Random, 95% CI) | 0.5 [‐0.51, 1.51] |
| 3.1 Manual acupuncture | 1 | 453 | Mean Difference (IV, Random, 95% CI) | 0.5 [‐0.51, 1.51] |
| 4 Severity of depression 6‐12 months Show forest plot | 1 | 453 | Mean Difference (IV, Random, 95% CI) | 0.60 [‐0.80, 2.00] |
| 4.1 Manual acupuncture | 1 | 453 | Mean Difference (IV, Random, 95% CI) | 0.60 [‐0.80, 2.00] |
| 5 Remission of depression | 0 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 Manual acupuncture | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Change in use of medication Show forest plot | 1 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.61, 1.10] |
| 6.1 Manual acupuncture | 1 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.61, 1.10] |
| 7 Dropout from treatment Show forest plot | 1 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 0.27 [0.08, 0.90] |
| 7.1 Manual acupuncture | 1 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 0.27 [0.08, 0.90] |

