Posición y movilidad de la madre durante el período dilatante del trabajo de parto
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Randomised trial: using a convenience sample over a 3‐month period. | |
| Participants | 40 women, Cleveland, U.S.A.
Inclusion Criteria: Parity: nulliparous, Pluralty: single vertex fetus in an anterior position, Gestation: 38 to 42 weeks Onset of labour: spontaneous Other: medically uncomplicated pregnancies; adequate pelvic measurements; intact amniotic membranes at the beginning of the maximum slope in their labour (4 to 9 cm dilatation). | |
| Interventions | Study group:
15 women chose to lie down after receiving medication for rest: 5 of these women immediately returned to the upright position, stating that the contractions were more painful when they were lying down. The remaining 10 chose the lateral position to rest for up to 1 hour during the study period. Control group:
All women: ‐ position assumed when cervical dilatation was from 4 to 9 cm, ‐ were free to choose several variations within each position group. | |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes: Nil | |
| Notes | 1. The length of maximum slope in labour was recorded. This is a subdivision of the first stage of labour, during which rapid cervical dilatation takes place (from 4 to 9 cm). The duration of the first stage was determined by the first recorded time that cervical dilatation was assessed to be 4 cm and on the first recorded time that dilatation was assessed to be 9 cm. 2. The Maternal Comfort Assessment Tool was used. The tool estimates the level of maternal comfort by measuring focus of attention; eye contact during contractions; breathing pattern and vocal behaviour during contractions; muscle tension and activity during contractions; and verbalisations regarding ability to continue with labour. In addition, vital signs; degree of cervical dilatation; duration, frequency, and intensity of contractions; medications; and use of monitoring apparatus were recorded. When the scores for each category of observable behaviour in the tool are added, the highest possible comfort score for each contraction was 14 and the lowest was 0. Comfort scores for a series of 3 contractions were recorded on an hourly basis during the phase of maximum slope, and averaged for mean hourly comfort scores. Hourly comfort scores where then average to obtain an overall mean comfort score for each woman. 3. The amount of narcotic and other analgesia. The randomisation method is unclear. Women in the recumbent position were monitored externally more often (n = 13) than women in the upright position (n = 1), which may have been an additional source of discomfort for women in the recumbent group. Apgar scores were not included as outcome measures because only a mean Apgar at 1 minute for each group was provided. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as 'randomly assigned'. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No stated losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Unclear. |
| Methods | Randomised trial | |
| Participants | 200 women, Sousse, Tunisia.
Inclusion Criteria: Parity: nulliparous, Pluralty: singleton, Gestation: term, Onset of labour: spontaneous Other: less than 4 cm dilatation; cephalic presentation; no pathological antecedents; absence of fetal compromise; normal maternal examination; eligible for vaginal birth; consenting to participate. | |
| Interventions | Study group:
Control group:
| |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes:
| |
| Notes | 1. Duration of first stage of labour: no standard deviation reported. Standard deviation calculated using the weighted average standard deviation reported for nulliparous women. Unable to extract data for oxytocic use or Apgar scores ‐ only mean scores provided. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered sealed envelopes. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No stated losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Unclear. |
| Methods | Randomised trial: over a 12‐month period. | |
| Participants | 1067 women, Dallas, U.S.A.
Inclusion Criteria: Parity: mixed, Pluralty: not stated, Gestation: between 36 and 41 weeks, Onset of labour: spontaneous, Other: cervical dilatation of 3 to 5 cm; in active labour; fetuses in cephalic presentation; uncomplicated pregnancies. | |
| Interventions | Study group:
Women were encouraged to walk but were instructed to return to their beds when they needed intravenous or epidural analgesia or when the second stage of labour began. Nurses recorded the number of minutes spent walking. If continuous electronic fetal heart rate monitoring was required, further walking was prohibited. Of the 536 women assigned to the walking group: 380 actually walked; 30 had incomplete walking records; 8 had advanced cervical dilatation at the time of randomisation; and 2 had a fetus with unrecognised breech presentation. Control group:
Women were permitted to assume their choice of supine, lateral or sitting positions during labour. All women: ‐ routine surveillance using handheld a Doppler device was conducted every 30 mins. ‐ amniotomy was performed if the fetal membranes were intact, ‐ labour was augmented by intravenous oxytocin (initial dose 6 mU per min, increased every 40 mins by 6 mU per min to a maximum of 42 mU per min if a woman had hypotonic uterine contractions, and no further cervical dilatation after an additional 2‐3 hours. ‐ Dystocia was diagnosed if labour had not progressed in 2‐4 hours. ‐ all women wore pedometers | |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes:
| |
| Notes | Limitations of the protocol: inability to mask walking; inability to extrapolate results to women with pregnancy complications, higher rates of caesarean birth or epidural analgesia; lack of objective methods to gauge maternal satisfaction with either walking or lying down during labour. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as 'randomly assigned'. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No stated losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Methods | Randomisation was achieved by the use of sequentially numbered sealed envelopes. A computer‐generated random number sequence was used. | |
| Participants | 409 women, Hertfordshire, U.K.
Inclusion Criteria: Parity: mixed, Pluralty: not stated, Gestation: greater than 34 weeks, Onset of labour: spontaneous and induction of labour, Other: cervical dilatation of 3 to 5 cm; in active labour; fetuses in cephalic presentation; uncomplicated pregnancies; women who chose to use a CSE between August 1st 1999 to December 31st 2000. Exclusion Criteria: women who were physically unable to ambulate or could not understand English. | |
| Interventions | Study group:
Women in the experimental group were encouraged to ambulate for at least 15 mins in each hour. Midwives used a modified Bromage scale in order to assess maternal mobility after the CSE had been cited and prior to ambulation. The mean time of ambulation in the ambulant group was only 8.74 to 9.55 mins. 69 out of 199 women (34%) underwent induction of labour. Control group:
Women in the control group received normal care in labour. 51 out of 210 (24%) women underwent induction of labour. All women: ‐ pain was assessed with a visual analogue pain score. | |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes: Nil | |
| Notes | No durations of labour times, but author stated "there was no difference". Mode of birth data totals differ from demographic data totals. Apgar scores reported as means, therefore unable to be used. Pooled data used from nulliparous and multiparous total dose of analgesia. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number sequence. |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered sealed envelopes. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No stated losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Unclear. |
| Methods | Randomised trial of women undergoing induction of labour. | |
| Participants | 60 women, Goteborg, Sweden.
Inclusion Criteria: Parity: mixed, Pluralty: not stated, Gestation: not stated, Onset of labour: induced, Other: nil stated. | |
| Interventions | Study group:
20 women were assigned to receive telemetry and transcutaneous electrical nerve stimulation (TNS), and 20 women were assigned to receive telemetry without TNS. Control group:
All women: ‐ primary amniotomy, ‐ internal monitoring. | |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes: Nil | |
| Notes | Insufficient data to include total duration of labour (reported as 8 hours for primiparae and 4 hours for multipara in the study group; and 10 hours for primiparae and 6 hours for multipara in the control group). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as 'randomisation to three groups'. |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Unclear risk | No stated losses to follow‐up. |
| Selective reporting (reporting bias) | High risk | Claimed evidence of an outcome with little or no data to support it. |
| Methods | Quasi‐randomised trial. Patients were randomly allocated based on whether the final digit of their hospital number was odd or even. | |
| Participants | 200 women, Cardiff, U.K.
Inclusion Criteria: Parity: mixed, Pluralty: singleton, Gestation: term (at least 37 weeks' gestation), Onset of labour: spontaneous, Other: vertex presentation; uterine contractions occurring at least every 10 mins; cervix at least 2.5 cm dilated; no contraindication to vaginal birth. Exclusion criteria ‐ women who had previously suffered a stillbirth or neonatal death or who had undergone a caesarean birth. | |
| Interventions | Study group:
Women were advised that they could get of bed to walk, sit in an easy chair or use the day room. Only 45 women actually got out of bed. They remained out of bed between 3 mins, and 4 hours and 20 mins. The average time out of bed was 1 hour and 44 mins. 34 of those who left their beds initially, elected to stay in bed by the time they reached a cervical dilatation of 7 cm. Control group:
All patients in bed were nursed in the lateral position or with a lateral tilt. | |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes:
| |
| Notes | 3. Within 24 hours of birth all patients were asked to complete a questionnaire to express their experience of pain, anxiety, comfort and restriction of mobility during the first stage of labour and the degree of induced anxiety or reassurance attributed to the monitor. Assessment was based on linear analogue scales. A score of 0 indicated nil and the score 100 indicated the maximum imaginable. 5. Duration of second stage only given for those who delivered spontaneously. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Described as 'Final digit of hospital number (odd or even)'. |
| Allocation concealment (selection bias) | High risk | Described as 'Final digit of hospital number (odd or even)'. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No stated losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Unclear. |
| Methods | Quasi‐randomised trial. | |
| Participants | 200 women, Hong Kong.
Inclusion Criteria: Parity: primigravidae, Pluralty: not stated, Gestation: not stated, Onset of labour: not stated, Other: nil stated. Exclusion criteria ‐ planned elective caesarean birth. | |
| Interventions | Study group:
Control group:
| |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes:
| |
| Notes | 1. Duration of first stage of labour: no standard deviation or P values reported. Standard deviation calculated using the weighted average standard deviation reported for nulliparous women. Summary totals exclude number of L.S.C.S. cases. 2. Assisted breech births (2 upright, 4 recumbent) not included in spontaneous vaginal, operative vaginal or caesarean birth summary totals. 5. Duration of second stage of labour: no standard deviation or P values reported. Standard deviation calculated using the weighted average standard deviation reported. Summary totals exclude number of L.S.C.S. cases. 6. The summary total included one set of twins. 7. The summary total included one set of twins. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternate group allocation. |
| Allocation concealment (selection bias) | High risk | Not stated. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Unclear risk | No stated losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Unclear. |
| Methods | Quasi‐randomised trial: over a 2.5 year period. | |
| Participants | 185 women, Oita, Japan.
Inclusion Criteria: Parity: mixed, Pluralty: singleton, Gestation: full term, Onset of labour: spontaneous, Other: cephalic presentation; uneventful pregnancies. Exclusion criteria ‐ women received oxytocin augmentation; caesarean birth due to cephalo‐pelvic disproportion or fetal distress; women requested and received epidural anaesthesia; child with congenital anomalies; tococardiogram records were unsuitable for reading (n = 67 exclusions after group allocation). | |
| Interventions | Study group:
Most sat on a sofa (back of sofa at 65 degree angle from horizontal) with their knees flexed. When each woman's cervix became fully dilated, she was transferred to a birthing chair. There were 20 post‐randomisation exclusions from the study group. Reasons for exclusion included: oxytocin augmentation (n = 2); caesarean birth due to CPD (n = 2); caesarean birth due to fetal distress (n=3); epidural anaesthesia (n = 3); fetal anomaly (n = 1); unsatisfactory TCG record (n = 9). Control group:
There were 49 post‐randomisation exclusions from the control group: Reasons for exclusion included: oxytocin augmentation (n = 13); caesarean birth due to CPD (n = 8); caesarean birth due to fetal distress (n = 2); epidural anaesthesia (n = 9); fetal anomaly (n = 3); unsatisfactory TCG record (n = 14). All women: ‐ no analgesia or anaesthesia was used except for pudendal nerve block or perineal infiltration of xylocaine. ‐ amniotomy was performed when cervical dilatation reached 3 to 4 cm. | |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes:
| |
| Notes | 1. Duration recorded from 5 to 10 cm dilation only. Pooled data used from nulliparous and multiparous durations of first stage labour. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Described as 'Allocated following the order of their admission into the study'. |
| Allocation concealment (selection bias) | High risk | |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | High risk | 67 participants were excluded after group allocation (37%). Some of the reasons for exclusion are unlikely to have related to the intervention (e.g. children born with congenital abnormalities) but other reasons may have related to group allocation (e.g. oxytocin augmentation, caesarean for fetal distress). |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Methods | Randomised trial of women receiving a CSE | |
| Participants | 229 women, London, U.K.
Inclusion Criteria: Parity: nulliparous, Pluralty: singleton, Gestation: 36 to 42 weeks, Onset of labour: spontaneous or induced, Other: cephalic presentation; requested regional analgesia (given CSE); no other pregnancy complications. | |
| Interventions | Study group:
51 women achieved at least 30% of time out of bed, 15 women spent no time out of bed, 44 spent 1 to 29%, 32 spent 30% to 59% and 19 women spent > 60% of time out of bed. Reasons for not ambulating: 16 women developed motor block, 25 mothers were fatigued, 10 women were following instructions of the midwife. Control group:
16 women got out of bed: 15 between 1% to 29% of the time and 1 between 30% to 59% of the time. All women: ‐ continuous fetal monitoring, ‐ CSE ‐ 27‐G Becton‐Dickinson Whitacre 119 mm spinal needle and 16‐G Tuohy needle' ‐ long spinal needle inserted through Tuohy needle into cerebrospinal fluid (needle‐through‐needle CSE), ‐ Subarachnoid injection of 25 g fentanyl and 2.5 mg bupivacaine ‐ Labours were managed according to the department's standard practice (cervical dilatation was assessed every 3 hours and if dilatation had not increased by 2 cm, amniotomy was performed. If the membranes were intact, this was followed 2 hours later (if progress of labour was still inadequate) by augmentation of labour with oxytocin. If the membranes were ruptured and inadequate progress of labour was noted, then oxytocin was started without waiting for another 2 hours. ‐ The mothers were allowed up to 2 hours in the second stage of labour. If at the end of the second hour, birth was not imminent, instrumental birth was performed. | |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes:
| |
| Notes | Duration was recorded as the time between epidural insertion (highly variable) and birth (end of second stage). It was therefore not used as a comparable duration of first stage of labour. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Low risk | Described as 'sealed opaque numbered envelopes'. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Described as 'Obstetrician was not aware which group the mother was in'. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No stated losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Unclear. |
| Methods | Randomised trial of women receiving a CSE. | |
| Participants | 40 women, London, U.K.
Inclusion Criteria: Parity: nulliparous, Pluralty: not stated, Gestation: not stated, Onset of labour: not stated, Other: requesting regional analgesia. | |
| Interventions | Study group:
Control group:
All women: ‐ spinal injection of bupivacaine 2.5 mg and fentanyl 25 g using a 27 gauge, 1119 mm Becton‐Dickinson Whitacre spinal needle through a 16‐gauge Braun Tuohy needle, followed by epidural top ups of 10 mg bupivacaine in 10 mL with 2 g/mL of fentanyl. | |
| Outcomes | Maternal Outcomes: Nil Neonatal Outcomes:
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as 'randomly allocated'. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No stated losses to follow‐up. |
| Selective reporting (reporting bias) | High risk | No maternal outcomes reported. |
| Methods | Randomised trial of patients who expressed an interest in ambulation when they were admitted in labour. During the antenatal period they had been informed that a certain number of patients could walk around while being continuously monitored in labour. | |
| Participants | 68 women, Birmingham, U.K.
Inclusion Criteria: Parity: mixed, Pluralty: not stated, Gestation: not stated, Onset of labour: spontaneous, Other: expressing an interest in ambulation. | |
| Interventions | Study group:
When intravenous treatment was necessary (e.g. because of ketonuria or delay in labour) the women returned to bed. Control group:
All women: ‐ were nursed in bed during the second and third stages of labour. There was 33 cephalic and 1 breech presentation in each group. | |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes:
| |
| Notes | Assisted breech births (1 upright, 1 recumbent) not included as spontaneous vaginal, operative vaginal or caesarean births. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as 'randomised prospective'. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No stated losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Unclear. |
| Methods | Randomised trial of women requesting epidural anaesthesia. | |
| Participants | 61 women, Grenoble, France.
Inclusion Criteria: Parity: mixed, Pluralty: singleton, Gestation: 37 to 42 weeks, Onset of labour: spontaneous or admitted for elective induction, Other: fixed cephalic uncomplicated presentation; 3 to 5 cm cervical dilatation at the time of epidural insertion; uncomplicated pregnancy; a normal fetal heart rate pattern. Exclusion criteria ‐ unfixed cephalic presentation, cervical dilatation more than 5 cm, a contraindication to epidural analgesia, or a systolic arterial blood pressure < 100 mmHg before epidural insertion, twin pregnancy, history of caesarean birth, and any known complications of pregnancy including breech presentation. | |
| Interventions | Study group:
Women were asked to walk at least 15 mins of each hour or for 25% of the duration of the first stage of labour. Control group:
Confined to bed in dorsal or lateral recumbent position. | |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes:
| |
| Notes | Duration was recorded as the time between epidural insertion (highly variable) and complete cervical dilatation. It was therefore not used as a comparable duration of first stage of labour. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Low risk | Described as 'sealed numbered envelopes'. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No stated losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Unclear. |
| Methods | Randomised trial. | |
| Participants | 188 women, Taiwan, Republic of China.
Inclusion Criteria: Parity: mixed, Pluralty: singleton, Gestation: unclear, Onset of labour: spontaneous or admitted for elective induction, Other: older than 18 years of age; no major obstetric or medical pregnancy complications; normal extremities and ability to undertake activities; a partner who was to be present during labour; and the ability to speak; read and write Chinese. | |
| Interventions | Study group:
The birth ball exercise programme consisted of a 26 page booklet and a 19‐minute videotape, with periodic follow‐ups during prenatal checks. All women were asked to practise the exercises and positions at home for at least 20 mins three times a week for a period of 6‐8 weeks. During labour, women in the study group were given a birth ball for use during labour and encouraged every hour to choose the most comfortable positions, movements and exercises. There were 46 post‐randomisation exclusions from the study group: Reasons for exclusion included: did not follow protocol (n = 3); epidural anaesthesia (n = 16); emergency caesarean (n = 18); preterm labour (n = 6); delivery at other hospital (n = 3). Control group:
There were 55 post‐randomisation exclusions from the control group: Reasons for exclusion included: epidural anaesthesia (n = 25); emergency caesarean (n = 22); preterm labour (n = 6); delivery at other hospital (n = 2). | |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes:
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computer‐generated block randomisation list (with block‐sizes of four and eight varied randomly) was independently prepared by a statistician. |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, sealed opaque envelopes contained allocation to the appropriate group. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | High risk | There was an attrition rate of 53.7%. The reasons 101 women were removed from the study included: emergency caesarean; epidural anaesthesia; preterm labour; delivery at other hospital; not following the protocol. All outcome data for women excluded from the study were not included in the results. |
| Selective reporting (reporting bias) | High risk | Study analysis which included the participants who did not follow the study protocol was repeated as ITT analysis. The authors stated there was no significant differences in effects based on ITT, but the outcome data for those and other excluded participants were not reported. |
| Methods | Quasi‐randomised trial. | |
| Participants | 60 women, Helsinki, Finland.
Inclusion Criteria: Parity: mixed, Pluralty: not stated, Gestation: between 38 and 42 weeks, Onset of labour: not stated, Other: healthy, uneventful pregnancy. | |
| Interventions | Study group:
Telemetry women were encouraged to sit or walk during the opening phase of labour. Control group:
All women: ‐ nitrous oxide‐oxygen, pethidine (usual dose 75 mg given once or twice) or epidural block were used for analgesia when needed. | |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes:
| |
| Notes | Pooled data used from nulliparous and multiparous durations of first stage labour. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as matched pairs 'allocated at random' to one of two groups. Patients were matched for age, parity and duration of pregnancy. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No stated losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Unclear. |
| Methods | Randomised trial. | |
| Participants | 221 women, Evry, France
Inclusion Criteria: Parity: mixed, Pluralty: singleton, Gestation: between 36 and 42 weeks, Onset of labour: spontaneous or scheduled for induced labour, Other: uncomplicated pregnancies. Exclusion criteria ‐ women with pre‐eclampsia or previous caesarean. | |
| Interventions | Study group:
Women could walk, sit in a chair or reclined in a semi‐supine position (n = 141), as long as they demonstrated: acceptable analgesia; acceptable systolic blood pressure and ability to stand on one leg. 3 women in this group were excluded because they had a fast birth. Control group:
Women were not allowed to sit, walk or go to the toilet, they had to remain in the supine position or to lie in a semi‐supine or lateral position (n = 74). 2 women in this group were excluded because they had a fast birth, and another 1 woman was excluded because of inadvertent dural puncture. All women: ‐ Study conducted in daytime only (as women in labour at night are less inclined to walk). ‐ Received intermittent epidural injection of 0.1% ropivacaine with 0.6 µg/mL sufentanil. ‐ Repeat injections were given when the women requested additional pain relief. | |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes: Nil | |
| Notes | Duration was recorded as the time between epidural insertion (highly variable) and birth (end of second stage). It was therefore not used as a comparable duration of first stage of labour. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'Randomly divided' in a 2:1 ratio. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | High risk | 6 women were excluded after randomisation. |
| Selective reporting (reporting bias) | Unclear risk | Unclear. |
| Methods | Randomised trial. | |
| Participants | 196 women, Adelaide, Australia.
Inclusion Criteria: Parity: mixed, Pluralty: singleton, Gestation: between 37 and 42 weeks, Onset of labour: spontaneous, Other: cephalic presentation; in established labour (presence of regular contractions less than 10 mins apart and cervical dilatation of 3 cm or more); able to ambulate in labour. Exclusion criteria: women undergoing intravenous therapy, with hypertension (> 90 mmHg diastolic blood pressure), epidural or narcotic analgesia at or before entry to trial, evidence of possible fetal distress, previous prostaglandin treatment, induced labour and a physical inability to ambulate. | |
| Interventions | Study group:
Women were encouraged to ambulate but were also given the option of sitting or lying down when they wished. Only 37 women actually chose to ambulate for half an hour or more. The mean time they spent upright was 1.8 hrs, and the mean time they spent recumbent was 4.5 hrs. Control group:
Most women chose a semi‐recumbent posture with the head end of the bed at 45 degrees but they could also be on their side with lower elevation of the head. All women: After entry to the trial, all women had an artificial rupture of the membranes if they had not already spontaneously ruptured. | |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes:
| |
| Notes | Duration was recorded as the time between entry (highly variable) and birth (end of second stage). It was therefore not used as a comparable duration of first stage of labour. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Described as 'Balanced variable blocks with stratification by parity'. |
| Allocation concealment (selection bias) | Low risk | Opaque, sealed envelopes. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No stated losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Unclear. |
| Methods | Randomised controlled trial approach with post test control group design. | |
| Participants | 60 women, Magalore, India.
Inclusion Criteria: Parity: nulliparous, Pluralty: not stated, Gestation: not stated, Onset of labour: not stated, Other: Nil stated. | |
| Interventions | Study group:
Control group:
| |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes: Nil. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Purposive sampling technique was used for the selection of samples. |
| Allocation concealment (selection bias) | Unclear risk | Random allocation of 20 samples to each of the three groups was achieved using a lottery method. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | High risk | There was missing data for the duration for 1st and 2nd stage labour: ambulation (n = 2), control (n = 4), but no missing data from the birthing ball group. There was no explanation to explain the missing data. In one table, 2 out of 24 women in the ambulation group are reported as having had a caesarean birth, but this is contradictory to the other reported data of zero caesarean births from 20 participants in the ambulation group. |
| Selective reporting (reporting bias) | High risk | All methods of birth outcome data were reported, but not all durations of birth data were reported. |
| Methods | Randomised trial of women undergoing induction of labour. | |
| Participants | 40 women, Glasgow, U.K.
Inclusion Criteria: Parity: mixed, Pluralty: singleton, Gestation: 38 weeks or more, Onset of labour: induced, Other: cervical score 6 or greater. Exclusion criteria ‐ multiple pregnancies or breech presentations. | |
| Interventions | Study group:
Women were encouraged to "be up and about". If woman wished to go to bed, she was nursed in a sitting position with the aid of pillows. Control group:
Women were nursed in the lateral position. All women: Labour was induced by forewater amniotomy and 0.5 mg PGE2 immediately after amniotomy and hourly thereafter until labour was considered to be established. | |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes:
| |
| Notes | Duration was recorded as the time between induction (highly variable) and birth (end of second stage). It was therefore not used as a comparable duration of first stage of labour. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as 'randomised prospective study'. |
| Allocation concealment (selection bias) | Low risk | Described as 'randomly allocated according to the contents of a plain envelope'. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No stated losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Unclear. |
| Methods | Randomised trial. | |
| Participants | 107 women, Campinas, Brazil
Inclusion Criteria: Parity: nulliparous, Pluralty: singleton, Gestation: term, Onset of labour: spontaneous, Other: cephalic presentation; cervical dilation between 3 cm and 5 cm; in labour; low risk; aged 16 to 40 years. Exclusion criteria ‐ contraindications to upright position or booked for elective caesarean birth. | |
| Interventions | Study group:
Women received written information/education involving the use of models on the benefits of maintaining an upright position and encouraged to stand, walk, sit, crouch or kneel. If women remained supine for more than 30 mins they were encouraged to return to an upright position. Women remained upright for 57% of the time. Control group:
Women remained upright for 28% of the time. Women were not encouraged to adopt upright positions but were allowed to move around and adopt any position they chose. | |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes:
| |
| Notes | 1. Duration of first stage labour only reported as median and P value. Symmetrical distribution assumed. Median value used as a mean to calculate standard deviation and utilise data. 2. No data for numbers of operative vaginal birth or caesarean births. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated. |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes opened sequentially. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Unclear risk | Few women lost to follow‐up but no data for numbers of operative vaginal birth or caesarean births. |
| Selective reporting (reporting bias) | High risk | Reported data for the number of women having spontaneous vaginal birth, but not for operative births or caesarean births. |
| Methods | Randomised trial. | |
| Participants | 100 women, Terre Haute, U.S.A.
Inclusion Criteria: Parity: nulliparous, Pluralty: not stated, Gestation: term, Onset of labour: spontaneous, Other: cephalic presentation; latent phase of labour or the active phase with the cervix between 1 cm and 3 cm; admitted to the labour room; no evidence of cephalopelvic disproportion; no history of surgery or trauma to the cervix; normal prenatal course. | |
| Interventions | Study group:
All women were allowed to sit up after the amniotomy had been performed and the presenting part was engaged. The women were allowed to lie down from time to time, if they desired. Control group:
Women were placed in the supine position and allowed to turn on their sides. | |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes: Nil | |
| Notes | 1. SD's from the mean time in active labour (time to birth) used for the active 'phase' of labour duration times. Apgar scores only provided as a mean value. It is not clear if all women in both groups had routine amniotomy. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as 'divided randomly into two groups'. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No stated losses to follow‐up. |
| Selective reporting (reporting bias) | High risk | Claimed evidence of an outcome with little or no data to support it. |
| Methods | Randomised trial. | |
| Participants | 761 women, California, U.S.A.
Inclusion Criteria: Parity: nulliparous, Pluralty: not stated, Gestation: 36 weeks or more, Onset of labour: spontaneous or induced for spontaneous rupture of membranes at 36 weeks or more, Other: fetus in the vertex position; requesting epidural analgesia. | |
| Interventions | Study group:
Ambulation was defined as a minimum of five mins of walking per hour. Control group:
All women: ‐ had CSE. | |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes:
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as 'randomly assigned'. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No stated losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Unclear. |
| Methods | Randomised trial. Randomised in blocks. | |
| Participants | 204 women, Southern Thailand.
Inclusion Criteria: Parity: nulliparous, Pluralty: singleton, Gestation: 38 ‐ 42 weeks, Onset of labour: spontaneous, Other: cephalic presentation; in latent phase for > 10 hours; married; aged 18 ‐ 35 years; fetal weight 2500 ‐ 4000 g. Exclusion criteria: had analgesia before recruitment; induced labour; membrane rupture > 20 hours previously; psychiatric problem; infection; asthma or objection to intervention. 5 separate intervention groups (described below). In this review we have included data from two groups: | |
| Interventions | Study group:
Control group:
| |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes: Nil. | |
| Notes | Complicated study design with five study groups: In this review we have used data for groups 2 and 5 in the analyses. (It was not clear what 'CAT' signified) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information. |
| Allocation concealment (selection bias) | Unclear risk | Described as 'random block design'. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | Three women were lost to follow‐up as they had caesarean births during the first stage of labour. It was not clear whether this was before randomisation. No other loss to follow‐up was apparent. |
| Selective reporting (reporting bias) | Unclear risk | Unclear. |
| Methods | Randomised trial. | |
| Participants | 62 women, Tehran, Iran.
Inclusion Criteria: Parity: nulliparous, Pluralty: singleton, Gestation: 38 ‐ 40 weeks, Onset of labour: spontaneous, Other: cephalic presentation; cervical dilatation between 4 to 8 cm; anticipation of a normal birth; no history of infertility; aged 18 to 25 years. | |
| Interventions | Study group:
There were two post randomisation exclusions from the study group. Reasons included: dissatisfied with sitting on the ball during birth ball movements (n = 1); caesarean birth because of lack of descent of the fetal head (n = 1). Control group:
Routine care consists of the parturient lying on the bed without ambulating or any intervention. | |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes: Nil. | |
| Notes | 1. Duration of first stage labour reported as duration of active phase. 2. No mode of birth outcomes for vaginal birth or operative vaginal birth were given. If there was a need for analgesic medication, or if obstetric complications occurred, the participant was immediately referred to an obstetrician and other professionals as needed, then excluded from the study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | 60 volunteer women (convenience sample) were randomly allocated using a table of random numbers. |
| Allocation concealment (selection bias) | High risk | If the number was even, women were assigned to the birth ball group, if the number was odd, women were assigned to control group. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Low risk | The individual responsible for data analysis was masked to the study purposes to minimise any bias that might arise from knowledge about the participants. |
| Incomplete outcome data (attrition bias) | Unclear risk | There were two post randomisation exclusions reported: dissatisfied with sitting on the ball during birth ball movements (n = 1); caesarean birth because of lack of descent of the fetal head (n = 1). The total number of participants included for duration of labour and maternal pain data is not clearly stated. It is unclear if the number includes totals before or after exclusions. It is also not clear if the group numbers were even before or after the exclusions. |
| Selective reporting (reporting bias) | Unclear risk | Unclear. |
| Methods | Randomised trial. | |
| Participants | 160 women, Pennsylvania, U.S.A.
Inclusion Criteria: Parity: nulliparous, Pluralty: singleton, Gestation: 36 ‐ 42 weeks, Onset of labour: spontaneous or induction of labour, Other: vertex position; 3‐5 cm cervical dilatation at the time of epidural insertion; uncomplicated pregnancies. Exclusion criteria ‐ pre‐eclampsia, diabetes mellitus, preterm gestation (< 36 weeks) and post‐term gestation (> 42 weeks). | |
| Interventions | Study group:
After 1 hour, women with a modified Bromage score of 5 who could stand on one foot (right and left) without assistance (all women in this group were able to do this) and without hypotension (systolic blood pressure < 100 mmHg or a decrease of 20 mmHg), were encouraged to ambulate with a support person (spouse or friend). If the woman could not comply with ambulation, she was encouraged to sit in a chair. Control group:
Women were confined to bed, encouraged to stay recumbent in a lateral position, and were not allowed to raise the head of the bed more than 45 degrees from horizontal. All women: ‐ AEA blocks initiated with 15 to 25 mL ropivacaine (0.07%) plus 100 g/mL fentanyl, no test dose, to achieve a T10 dermatome sensory level. After achieving adequate pain relief, a continuous infusion of 0.07% ropivacaine plus 2 g/mL fentanyl at 15 to 20 mL/hour was administered. | |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes:
| |
| Notes | Duration was recorded as the time between epidural insertion (highly variable) and complete cervical dilatation. It was therefore not used as a comparable duration of first stage of labour. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Described as 'random number computer‐generated program'. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | High risk | 9 women were excluded. |
| Selective reporting (reporting bias) | Unclear risk | Unclear. |
| Methods | Quasi‐randomised trial. | |
| Participants | 300 women, London, U.K.
Inclusion Criteria: Parity: mixed, Pluralty: singleton, Gestation: 36‐42 weeks, Onset of labour: spontaneous, Other: nil stated. | |
| Interventions | Study group:
Women were informed about the possible benefits of ambulation and were encouraged to walk about during the first stage of labour Control group:
| |
| Outcomes | Maternal Outcomes:
Neonatal Outcomes:
| |
| Notes | Pooled data used from nulliparous and multiparous durations of first stage labour. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Described as 'divided into two groups according to their hospital number'. |
| Allocation concealment (selection bias) | High risk | See above. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | High risk | Not feasible. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No stated losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Unclear. |
AEA: ambulatory epidural analgesia
CPD: cephalopelvic disproportion
CSE: combined spinal epidural
G: gauge
ITT: intention‐to‐treat
L.S.C.S.:lower segment caesarian section
mins: minutes
mU: milli‐units
NICU: neonatal intensive care unit
PCE2: prostaglandin E2
SD: standard deviation
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Brief abstract, data for the single result presented were not in a form we were able use in the review. | |
| Not clear that this was an RCT. States that 'patients were selected at random' but it was not clear that allocation to experimental and control groups was random. All primigravidae in the control group were subjected to prophylactic episiotomies, not all primigravidae in the intervention group were subjected to prophylactic episiotomies. | |
| Not randomised. | |
| 1. Observational ‐ Not RCT. | |
| Intervention not relevant. Study examining lying on side versus lying on back. | |
| The study group received a different amount of ropivacaine compared to the control group. No outcomes relevant to the review were reported. | |
| The trial compared low‐dose combined spinal epidural and low‐dose infusion techniques and traditional epidural techniques. Therefore the study group received a different epidural type compared with the control group. | |
| The purpose of this study was to compare cardiac output after epidural analgesia in both left lateral and supine positions, which are both regarded as recumbent positions for the purposes of this review. | |
| The study compared using exercise ball or not using an exercise ball. It did not compare upright positions with recumbent positions. Control group was allowed freedom of movement. | |
| This study uses quasi‐randomised group allocation, but more than a third of the experimental group were excluded from the analysis; women that did not comply with the protocol were excluded post randomisation. | |
| No data were presented. No outcomes relevant to the review were reported. Outcomes ‐ BP, uterine work and beat‐to‐beat variability. | |
| The purpose of the study was to compare epidural spread for supine compared with 3 hip‐flexed postures. No outcomes relevant to the review were reported | |
| In this study the comparison was between two management policies rather than two different treatments. One group was nursed in bed and one group was encouraged to mobilise but there were also other differences in the treatment the two groups received which may have had an effect on outcomes. Women nursed in bed had routine amniotomy, women in the ambulant group did not; monitoring was also different in the two groups. These differences in management mean that it is not possible to assess the effect of position on outcomes. | |
| Compared ambulation with immediate oxytocin. | |
| All bed‐care patients had an epidural and not all ambulant patients did. | |
| Women were allocated to the treatment or control group according to personal preference. No other randomisation details were described. | |
| Compares semi‐upright position with lying flat position, which are both recumbent positions for the purposes of this review. | |
| Study not completed ‐ no results reported. | |
| Cross‐over design ‐ women alternated between vertical and horizontal positions, then rated their level of pain at the end of each 20‐minute period. | |
| Cross‐over design ‐ women alternated between vertical and horizontal positions, then rated their level of pain at the end of each 15‐minute period. | |
| Study position, squatting, assumed in second stage of labour only. | |
| Comparing ambulation with oxytocin. | |
| Cross‐over design ‐ women alternated between sitting and lateral recumbence positions, every 30 minutes. | |
| Cross‐over design ‐ measures fetal oxygen saturations for different and successive maternal birth positions. | |
| No quantitative outcome data presented. | |
| The study participants were not in labour. | |
| Not randomised. | |
| Compares positions used in the 2nd stage of labour. | |
| The study did not compare upright positions with recumbent positions. | |
| Study compares walking to the toilet to void with using a bed pan in bed. No relevant outcomes are reported. | |
| The trial compared low‐dose combined spinal epidural and low‐dose infusion techniques and traditional epidural techniques. Therefore the study group received a different epidural type compared with the control group. | |
| Intervention not relevant to review outcomes. Study examining lying on one side rather than the other to correct fetal malpresentation. |
BP: blood pressure
RCT: randomised controlled trial
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Duration of first stage labour (hours) Show forest plot | 15 | 2503 | Mean Difference (IV, Random, 95% CI) | ‐1.36 [‐2.22, ‐0.51] |
| Analysis 1.1 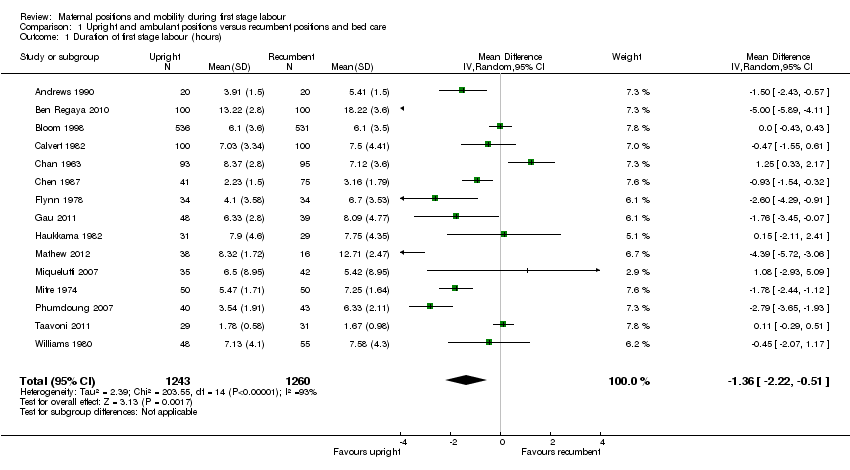 Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 1 Duration of first stage labour (hours). | ||||
| 2 Duration of first stage labour (hours): subgroup analysis: parity Show forest plot | 12 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.2  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 2 Duration of first stage labour (hours): subgroup analysis: parity. | ||||
| 2.1 Nulliparous women | 12 | 1486 | Mean Difference (IV, Random, 95% CI) | ‐1.21 [‐2.35, ‐0.07] |
| 2.2 Multiparous women | 4 | 662 | Mean Difference (IV, Random, 95% CI) | ‐0.56 [‐1.19, 0.06] |
| 3 Duration of first stage labour (hours): subgroup analysis: onset of labour Show forest plot | 11 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.3  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 3 Duration of first stage labour (hours): subgroup analysis: onset of labour. | ||||
| 3.1 Spontaneous labour: all women | 11 | 2114 | Mean Difference (IV, Random, 95% CI) | ‐1.43 [‐2.35, ‐0.50] |
| 3.2 Induction of labour: all women | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Duration of first stage labour (hours): subgroup analysis: position types Show forest plot | 15 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.4  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 4 Duration of first stage labour (hours): subgroup analysis: position types. | ||||
| 4.1 Sitting vs Recumbent / supine / lateral | 3 | 252 | Mean Difference (IV, Random, 95% CI) | ‐2.39 [‐4.06, ‐0.72] |
| 4.2 Walking vs Recumbent / supine / lateral | 3 | 302 | Mean Difference (IV, Random, 95% CI) | ‐3.96 [‐5.36, ‐2.57] |
| 4.3 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 3 | 311 | Mean Difference (IV, Random, 95% CI) | ‐1.02 [‐3.36, 1.33] |
| 4.4 Sitting vs Bed care | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.29, 0.51] |
| 4.5 Walking vs Bed care | 2 | 1170 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.44, 0.38] |
| 4.6 Sitting, standing, squatting, kneeling or walking vs Bed care | 4 | 424 | Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐1.49, 0.45] |
| 5 Duration of first stage labour (hours): subgroup analysis: position types Show forest plot | 15 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.5  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 5 Duration of first stage labour (hours): subgroup analysis: position types. | ||||
| 5.1 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 8 | 849 | Mean Difference (IV, Random, 95% CI) | ‐2.19 [‐3.49, ‐0.89] |
| 5.2 Sitting, standing, squatting, kneeling or walking vs Bed care | 7 | 1654 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.30, 0.25] |
| 6 Duration of first stage labour (hours): subgroup analysis: position types Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.6  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 6 Duration of first stage labour (hours): subgroup analysis: position types. | ||||
| 6.1 Sitting, standing, squatting, kneeling or walking vs supine only | 2 | 183 | Mean Difference (IV, Random, 95% CI) | ‐2.24 [‐3.23, ‐1.26] |
| 7 Duration of first stage labour (hours): sensitivity analysis ‐ positions Show forest plot | 3 | 364 | Mean Difference (IV, Fixed, 95% CI) | ‐3.86 [‐4.73, ‐2.99] |
| Analysis 1.7  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 7 Duration of first stage labour (hours): sensitivity analysis ‐ positions. | ||||
| 7.1 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 1 | 200 | Mean Difference (IV, Fixed, 95% CI) | ‐3.00 [‐6.05, ‐3.95] |
| 7.2 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Bed care | 2 | 164 | Mean Difference (IV, Fixed, 95% CI) | ‐1.33 [‐2.89, 0.23] |
| 8 Mode of birth: spontaneous vaginal Show forest plot | 14 | 2626 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.99, 1.11] |
| Analysis 1.8  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 8 Mode of birth: spontaneous vaginal. | ||||
| 9 Mode of birth: spontaneous vaginal: subgroup analysis: parity Show forest plot | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.9 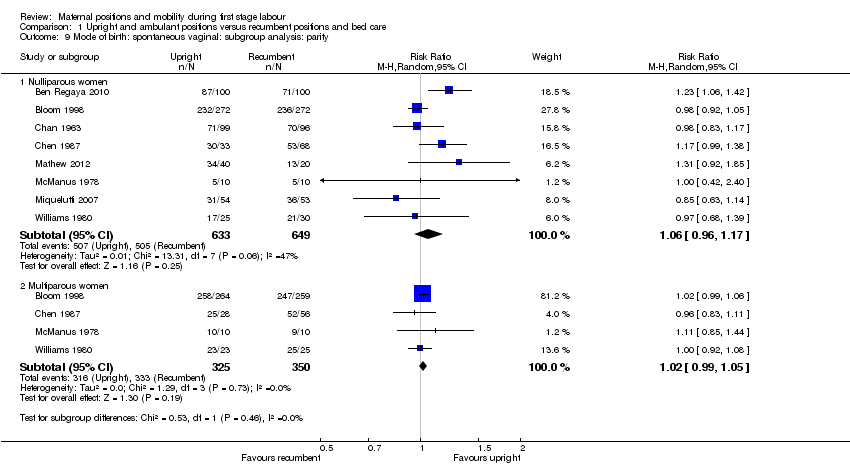 Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 9 Mode of birth: spontaneous vaginal: subgroup analysis: parity. | ||||
| 9.1 Nulliparous women | 8 | 1282 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.96, 1.17] |
| 9.2 Multiparous women | 4 | 675 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.99, 1.05] |
| 10 Mode of birth: spontaneous vaginal: subgroup analysis: onset of labour Show forest plot | 10 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.10  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 10 Mode of birth: spontaneous vaginal: subgroup analysis: onset of labour. | ||||
| 10.1 Spontaneous labour: all women | 8 | 2124 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.97, 1.12] |
| 10.2 Induction of labour: all women | 2 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.98, 1.57] |
| 11 Mode of birth: spontaneous vaginal: subgroup analysis: position types Show forest plot | 14 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.11  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 11 Mode of birth: spontaneous vaginal: subgroup analysis: position types. | ||||
| 11.1 Sitting vs Recumbent / supine / lateral | 2 | 225 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.88, 1.64] |
| 11.2 Walking vs Recumbent / supine / lateral | 3 | 306 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [1.11, 1.42] |
| 11.3 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 2 | 235 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.85, 1.17] |
| 11.4 Sitting vs Bed care | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.5 Walking vs Bed care | 4 | 1426 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.93, 1.11] |
| 11.6 Sitting, standing, squatting, kneeling or walking vs Bed care | 4 | 454 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.92, 1.08] |
| 12 Mode of birth: spontaneous vaginal: subgroup analysis: position types Show forest plot | 14 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.12 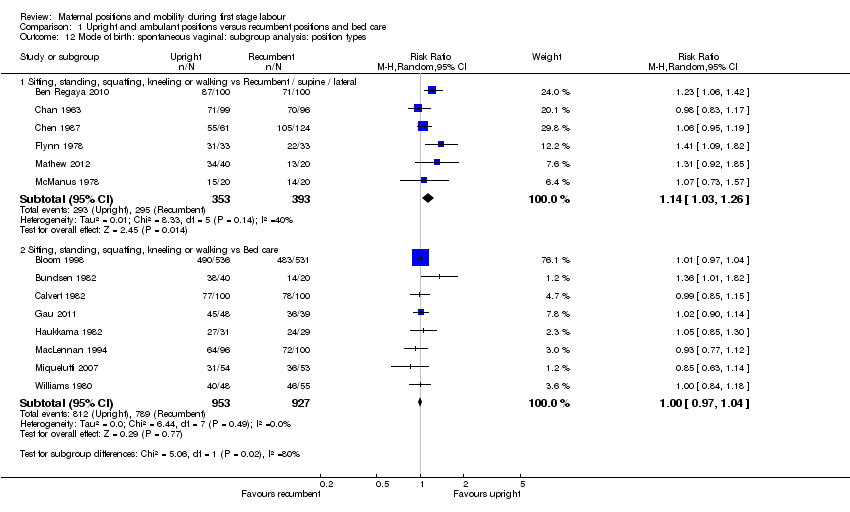 Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 12 Mode of birth: spontaneous vaginal: subgroup analysis: position types. | ||||
| 12.1 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 6 | 746 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [1.03, 1.26] |
| 12.2 Sitting, standing, squatting, kneeling or walking vs Bed care | 8 | 1880 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.97, 1.04] |
| 13 Mode of birth: spontaneous vaginal: subgroup analysis: position types | 0 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 13.1 Sitting, standing, squatting, kneeling or walking vs supine only | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Mode of birth: spontaneous vaginal: sensitivity analysis ‐ positions Show forest plot | 5 | 630 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.94, 1.13] |
| Analysis 1.14  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 14 Mode of birth: spontaneous vaginal: sensitivity analysis ‐ positions. | ||||
| 14.1 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.2 [1.05, 1.38] |
| 14.2 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Bed care | 3 | 390 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.83, 1.05] |
| 15 Mode of birth: operative vaginal: all women Show forest plot | 13 | 2519 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.73, 1.14] |
| Analysis 1.15  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 15 Mode of birth: operative vaginal: all women. | ||||
| 16 Mode of birth: operative vaginal: subgroup analysis: parity Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.16 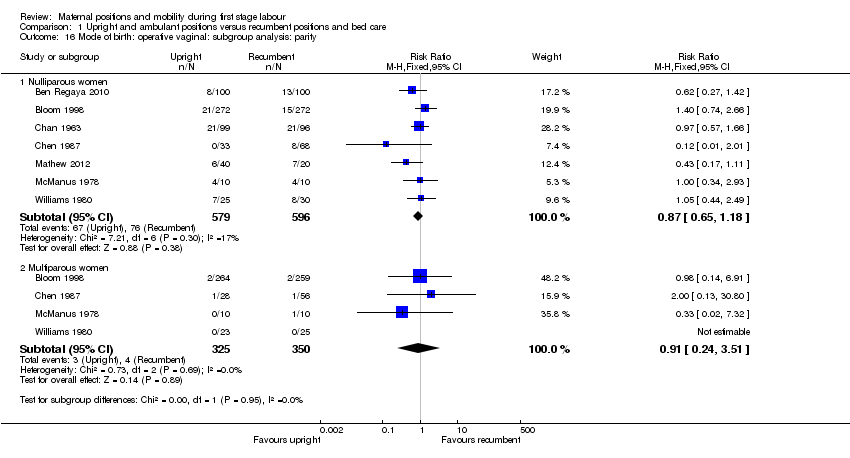 Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 16 Mode of birth: operative vaginal: subgroup analysis: parity. | ||||
| 16.1 Nulliparous women | 7 | 1175 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.65, 1.18] |
| 16.2 Multiparous women | 4 | 675 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.24, 3.51] |
| 17 Mode of birth: operative vaginal: subgroup analysis: onset of labour Show forest plot | 9 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.17  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 17 Mode of birth: operative vaginal: subgroup analysis: onset of labour. | ||||
| 17.1 Spontaneous labour: all women | 7 | 2017 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.62, 1.39] |
| 17.2 Induction of labour: all women | 2 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.23, 1.58] |
| 18 Mode of birth: operative vaginal: subgroup analysis: position types Show forest plot | 13 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.18 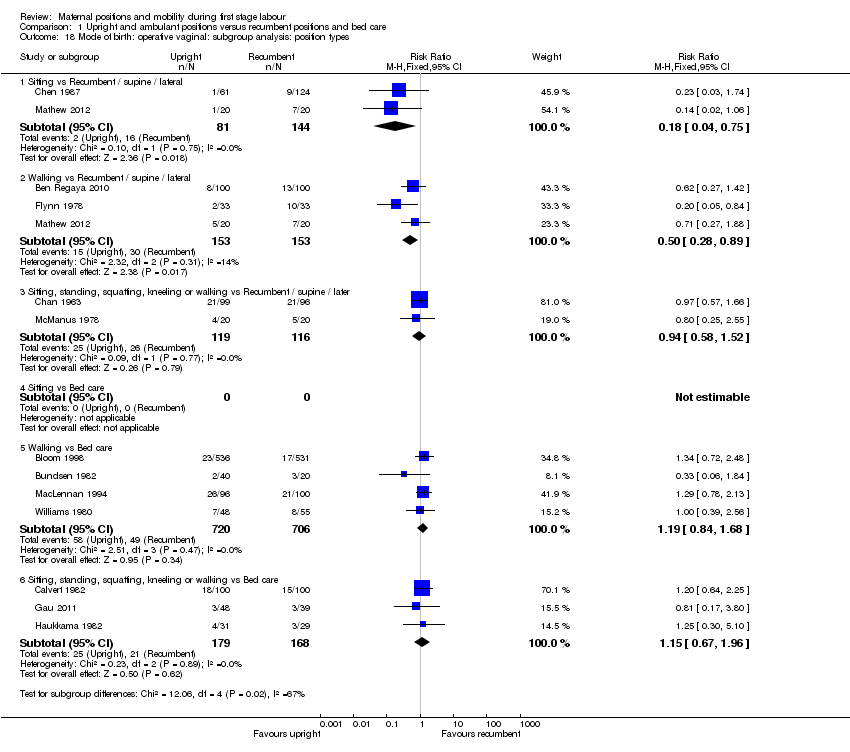 Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 18 Mode of birth: operative vaginal: subgroup analysis: position types. | ||||
| 18.1 Sitting vs Recumbent / supine / lateral | 2 | 225 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.18 [0.04, 0.75] |
| 18.2 Walking vs Recumbent / supine / lateral | 3 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.28, 0.89] |
| 18.3 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / later | 2 | 235 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.58, 1.52] |
| 18.4 Sitting vs Bed care | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18.5 Walking vs Bed care | 4 | 1426 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.84, 1.68] |
| 18.6 Sitting, standing, squatting, kneeling or walking vs Bed care | 3 | 347 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.67, 1.96] |
| 19 Mode of birth: operative vaginal: subgroup analysis: position types Show forest plot | 13 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.19 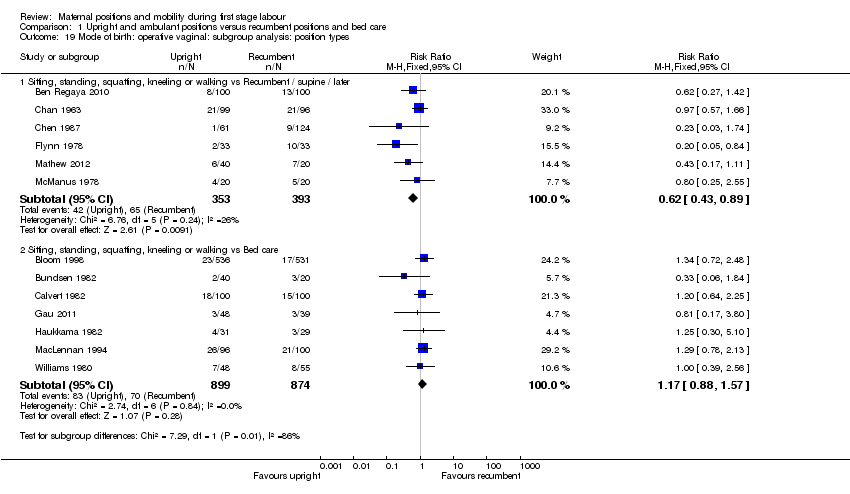 Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 19 Mode of birth: operative vaginal: subgroup analysis: position types. | ||||
| 19.1 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / later | 6 | 746 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.43, 0.89] |
| 19.2 Sitting, standing, squatting, kneeling or walking vs Bed care | 7 | 1773 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.88, 1.57] |
| 20 Mode of birth: operative vaginal: subgroup analysis: position types | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 20.1 Sitting, standing, squatting, kneeling or walking vs supine only | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Mode of birth: operative vaginal: sensitivity analysis ‐ positions Show forest plot | 4 | 523 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.67, 1.45] |
| Analysis 1.21  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 21 Mode of birth: operative vaginal: sensitivity analysis ‐ positions. | ||||
| 21.1 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.34, 1.31] |
| 21.2 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Bed care | 2 | 283 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.76, 1.97] |
| 22 Mode of birth: caesarean birth Show forest plot | 14 | 2682 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.54, 0.94] |
| Analysis 1.22 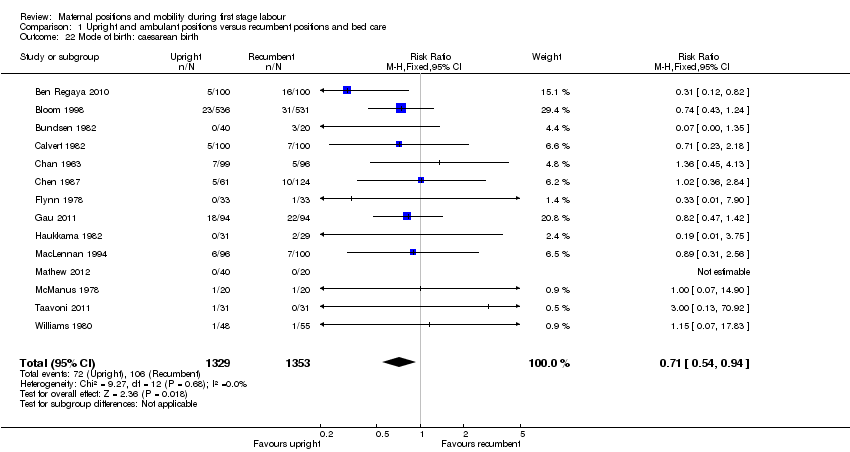 Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 22 Mode of birth: caesarean birth. | ||||
| 23 Mode of birth: caesarean birth: subgroup analysis: parity Show forest plot | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.23 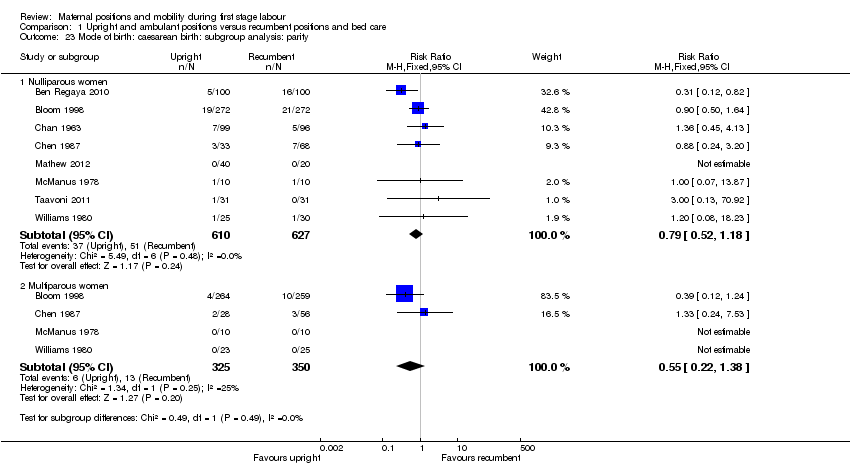 Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 23 Mode of birth: caesarean birth: subgroup analysis: parity. | ||||
| 23.1 Nulliparous women | 8 | 1237 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.52, 1.18] |
| 23.2 Multiparous women | 4 | 675 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.22, 1.38] |
| 24 Mode of birth: caesarean birth: subgroup analysis: onset of labour Show forest plot | 10 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.24  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 24 Mode of birth: caesarean birth: subgroup analysis: onset of labour. | ||||
| 24.1 Spontaneous labour: all women | 8 | 2079 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.49, 1.01] |
| 24.2 Induction of labour: all women | 2 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 0.29 [0.02, 3.86] |
| 25 Mode of birth: caesarean birth: subgroup analysis: position types Show forest plot | 14 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.25 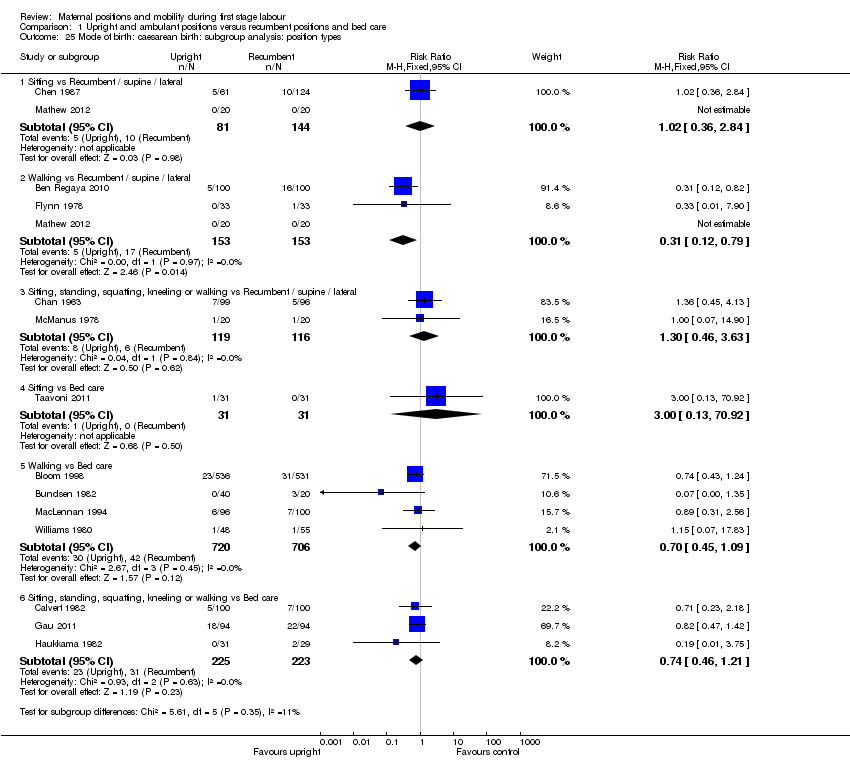 Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 25 Mode of birth: caesarean birth: subgroup analysis: position types. | ||||
| 25.1 Sitting vs Recumbent / supine / lateral | 2 | 225 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.36, 2.84] |
| 25.2 Walking vs Recumbent / supine / lateral | 3 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.12, 0.79] |
| 25.3 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 2 | 235 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.46, 3.63] |
| 25.4 Sitting vs Bed care | 1 | 62 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 70.92] |
| 25.5 Walking vs Bed care | 4 | 1426 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.45, 1.09] |
| 25.6 Sitting, standing, squatting, kneeling or walking vs Bed care | 3 | 448 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.46, 1.21] |
| 26 Mode of birth: caesarean birth: subgroup analysis: position types Show forest plot | 14 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.26  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 26 Mode of birth: caesarean birth: subgroup analysis: position types. | ||||
| 26.1 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 6 | 746 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.39, 1.15] |
| 26.2 Sitting, standing, squatting, kneeling or walking vs Bed care | 8 | 1936 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.53, 1.02] |
| 27 Mode of birth: caesarean birth: subgroup analysis: position types | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 27.1 Sitting, standing, squatting, kneeling or walking vs supine only | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 28 Mode of birth: caesarean birth: sensitivity analysis ‐ positions Show forest plot | 4 | 624 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.48, 1.09] |
| Analysis 1.28 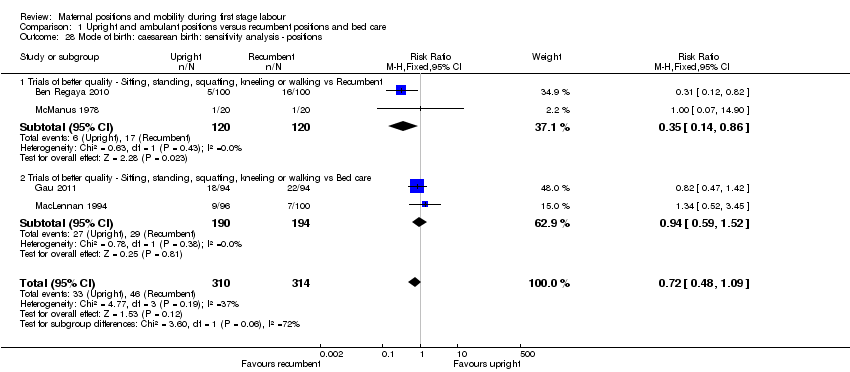 Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 28 Mode of birth: caesarean birth: sensitivity analysis ‐ positions. | ||||
| 28.1 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Recumbent | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.14, 0.86] |
| 28.2 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Bed care | 2 | 384 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.59, 1.52] |
| 29 Analgesia type Show forest plot | 10 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.29 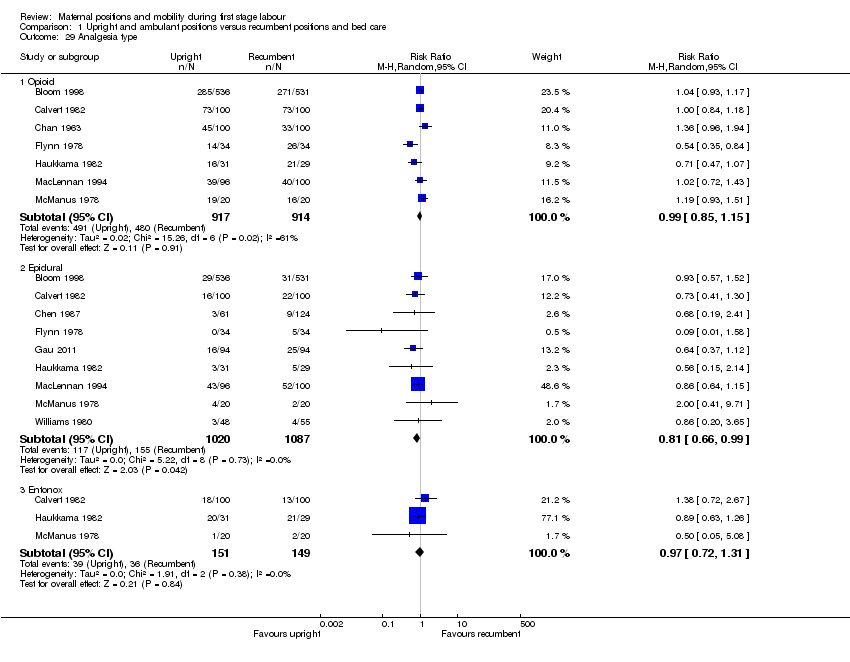 Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 29 Analgesia type. | ||||
| 29.1 Opioid | 7 | 1831 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.85, 1.15] |
| 29.2 Epidural | 9 | 2107 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.66, 0.99] |
| 29.3 Entonox | 3 | 300 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.72, 1.31] |
| 30 Maternal satisfaction Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.30  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 30 Maternal satisfaction. | ||||
| 30.1 Satisfaction with position reported at 6 cm | 1 | 107 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [0.60, 2.85] |
| 30.2 Preferred upright position | 1 | 107 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.97, 1.61] |
| 31 Maternal comfort Show forest plot | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | 0.74 [‐0.27, 1.75] |
| Analysis 1.31  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 31 Maternal comfort. | ||||
| 31.1 Comfort score | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | 0.74 [‐0.27, 1.75] |
| 32 Maternal pain Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.32 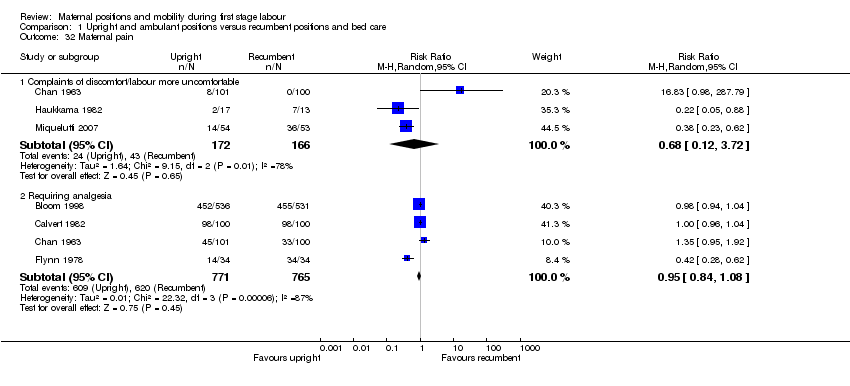 Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 32 Maternal pain. | ||||
| 32.1 Complaints of discomfort/labour more uncomfortable | 3 | 338 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.12, 3.72] |
| 32.2 Requiring analgesia | 4 | 1536 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.84, 1.08] |
| 33 Maternal pain Show forest plot | 2 | 400 | Mean Difference (IV, Fixed, 95% CI) | 6.36 [‐0.31, 13.03] |
| Analysis 1.33 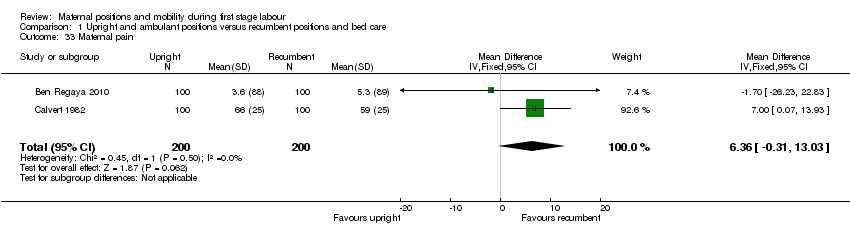 Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 33 Maternal pain. | ||||
| 34 Maternal pain Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.34  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 34 Maternal pain. | ||||
| 34.1 Visual Analogue Scale (VAS) Score | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐1.74 [‐2.51, ‐0.97] |
| 34.2 Visual Analogue Scale (VAS) Score @ 4 cm | 1 | 87 | Mean Difference (IV, Fixed, 95% CI) | ‐2.0 [‐2.70, ‐1.30] |
| 34.3 Visual Analogue Scale (VAS) Score @ 8 cm | 1 | 87 | Mean Difference (IV, Fixed, 95% CI) | ‐1.70 [‐2.20, ‐1.20] |
| 34.4 Verbal Response Scale (VRS) Score @ 4 cm | 1 | 87 | Mean Difference (IV, Fixed, 95% CI) | ‐10.40 [‐13.27, ‐7.53] |
| 34.5 Verbal Response Scale (VRS) Score@ 8 cm | 1 | 87 | Mean Difference (IV, Fixed, 95% CI) | ‐5.00 [‐11.33, ‐2.67] |
| 34.6 Present Pain Intensity Scale (PPI) @ 4 cm | 1 | 87 | Mean Difference (IV, Fixed, 95% CI) | ‐1.40 [‐3.61, 0.81] |
| 34.7 Present Pain Intensity Scale (PPI) @ 8 cm | 1 | 87 | Mean Difference (IV, Fixed, 95% CI) | ‐0.80 [‐3.76, 2.16] |
| 35 Maternal anxiety Show forest plot | 1 | 200 | Mean Difference (IV, Fixed, 95% CI) | 8.0 [‐0.19, 16.19] |
| Analysis 1.35  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 35 Maternal anxiety. | ||||
| 36 Analgesia amount Show forest plot | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐17.5 [‐36.89, 1.89] |
| Analysis 1.36  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 36 Analgesia amount. | ||||
| 36.1 Narcotics and other analgesia | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐17.5 [‐36.89, 1.89] |
| 37 Duration of second stage of labour (minutes) Show forest plot | 9 | 2077 | Mean Difference (IV, Random, 95% CI) | ‐3.71 [‐9.37, 1.94] |
| Analysis 1.37 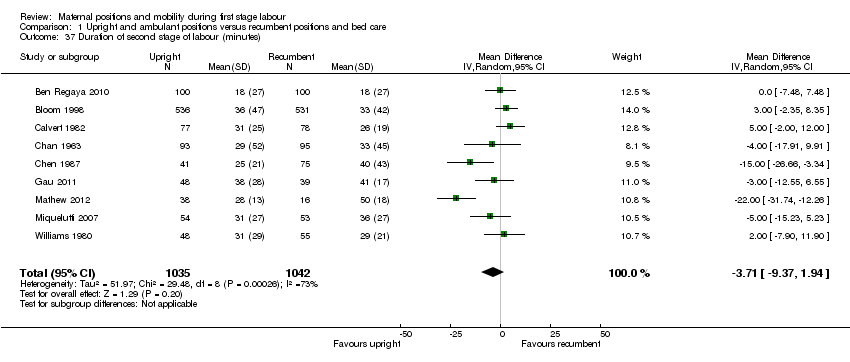 Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 37 Duration of second stage of labour (minutes). | ||||
| 38 Augmentation of labour using oxytocin Show forest plot | 8 | 1826 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.76, 1.05] |
| Analysis 1.38  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 38 Augmentation of labour using oxytocin. | ||||
| 39 Artificial rupture of membranes Show forest plot | 4 | 276 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.95, 1.10] |
| Analysis 1.39  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 39 Artificial rupture of membranes. | ||||
| 40 Hypotension requiring intervention | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 41 Estimated blood loss > 500 mL Show forest plot | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.14, 3.55] |
| Analysis 1.41 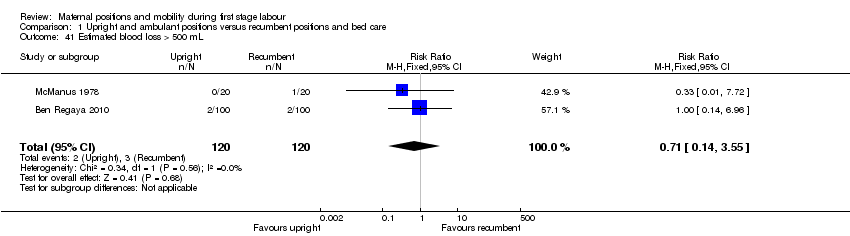 Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 41 Estimated blood loss > 500 mL. | ||||
| 42 Perineal trauma Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.42 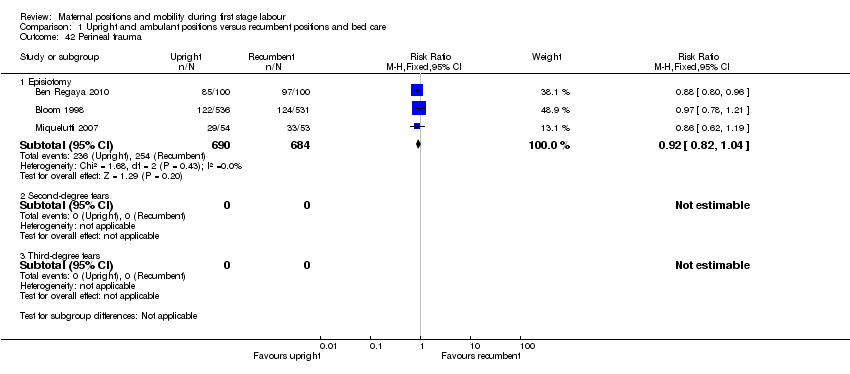 Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 42 Perineal trauma. | ||||
| 42.1 Episiotomy | 3 | 1374 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.82, 1.04] |
| 42.2 Second‐degree tears | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 42.3 Third‐degree tears | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 43 Fetal distress (requiring immediate delivery) Show forest plot | 6 | 1757 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.35, 1.33] |
| Analysis 1.43  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 43 Fetal distress (requiring immediate delivery). | ||||
| 44 Use of neonatal mechanical ventilation Show forest plot | 2 | 1107 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.19, 3.10] |
| Analysis 1.44  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 44 Use of neonatal mechanical ventilation. | ||||
| 44.1 Intubation in delivery room | 2 | 1107 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.19, 3.10] |
| 45 Apgar scores Show forest plot | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.45  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 45 Apgar scores. | ||||
| 45.1 Apgar < 4 at birth | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.92] |
| 45.2 Apgar < 7 at 1 min | 6 | 706 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.54, 1.31] |
| 45.3 Apgar < 7 at 5 mins | 4 | 466 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.27 [0.34, 31.05] |
| 45.4 Apgar < 3 at 5 mins | 1 | 1067 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 45.5 Apgar < 8 at 5 mins | 1 | 87 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.01, 2.19] |
| 46 Admission to NICU Show forest plot | 2 | 396 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.25, 1.36] |
| Analysis 1.46  Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 46 Admission to NICU. | ||||
| 46.1 Admission to NICU | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.04, 0.89] |
| 46.2 Admission to Level I or II nursery | 1 | 196 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.56 [0.45, 5.37] |
| 47 Perinatal mortality Show forest plot | 5 | 1564 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.05, 5.37] |
| Analysis 1.47 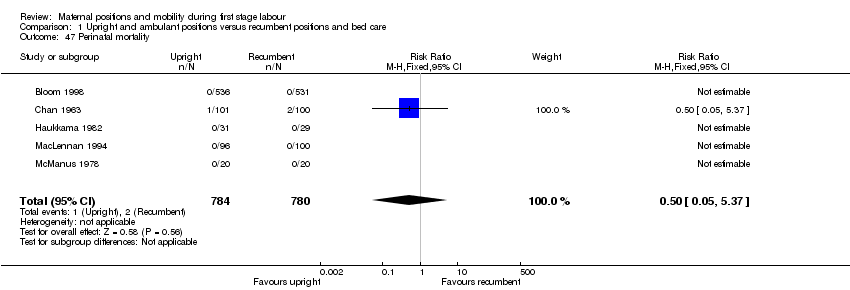 Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 47 Perinatal mortality. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Duration of first stage labour: (minutes) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Mode of birth: spontaneous vaginal Show forest plot | 6 | 1566 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.89, 1.05] |
| Analysis 2.2  Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 2 Mode of birth: spontaneous vaginal. | ||||
| 3 Mode of birth: spontaneous vaginal: subgroup analysis: parity Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.3  Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 3 Mode of birth: spontaneous vaginal: subgroup analysis: parity. | ||||
| 3.1 Nulliparous women | 4 | 1179 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.84, 1.04] |
| 3.2 Multiparous women | 1 | 111 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.81, 1.27] |
| 4 Mode of birth: spontaneous vaginal: subgroup analysis: onset of labour Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 2.4 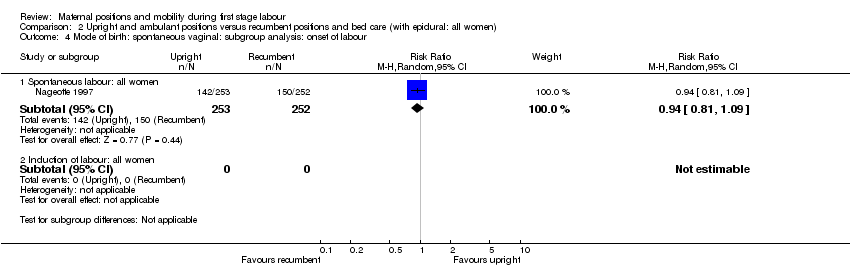 Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 4 Mode of birth: spontaneous vaginal: subgroup analysis: onset of labour. | ||||
| 4.1 Spontaneous labour: all women | 1 | 505 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.81, 1.09] |
| 4.2 Induction of labour: all women | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Mode of birth: spontaneous vaginal: subgroup analysis: position types Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 2.5 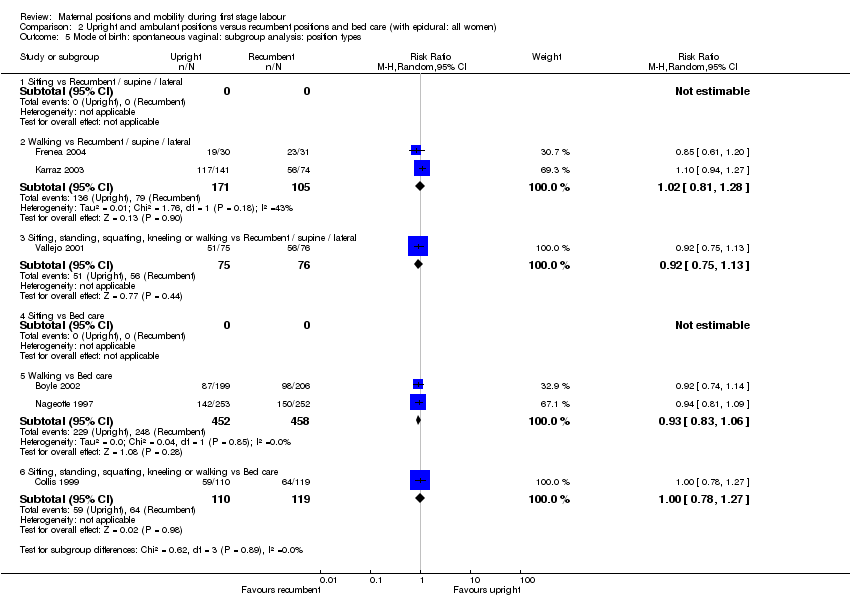 Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 5 Mode of birth: spontaneous vaginal: subgroup analysis: position types. | ||||
| 5.1 Sitting vs Recumbent / supine / lateral | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Walking vs Recumbent / supine / lateral | 2 | 276 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.81, 1.28] |
| 5.3 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 1 | 151 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.75, 1.13] |
| 5.4 Sitting vs Bed care | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.5 Walking vs Bed care | 2 | 910 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.83, 1.06] |
| 5.6 Sitting, standing, squatting, kneeling or walking vs Bed care | 1 | 229 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.78, 1.27] |
| 6 Mode of birth: spontaneous vaginal: subgroup analysis: position types Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 2.6  Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 6 Mode of birth: spontaneous vaginal: subgroup analysis: position types. | ||||
| 6.1 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 3 | 427 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.86, 1.15] |
| 6.2 Sitting, standing, squatting, kneeling or walking vs Bed care | 3 | 1139 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.85, 1.06] |
| 7 Mode of birth: spontaneous vaginal: sensitivity analysis Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.7 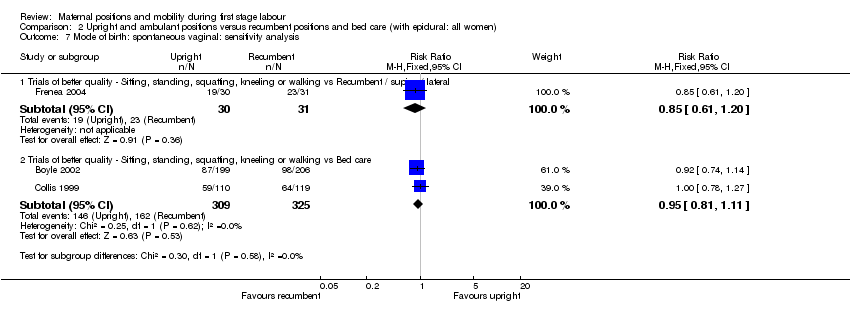 Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 7 Mode of birth: spontaneous vaginal: sensitivity analysis. | ||||
| 7.1 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 1 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.61, 1.20] |
| 7.2 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Bed care | 2 | 634 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.81, 1.11] |
| 8 Mode of birth: operative vaginal Show forest plot | 6 | 1566 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.90, 1.25] |
| Analysis 2.8 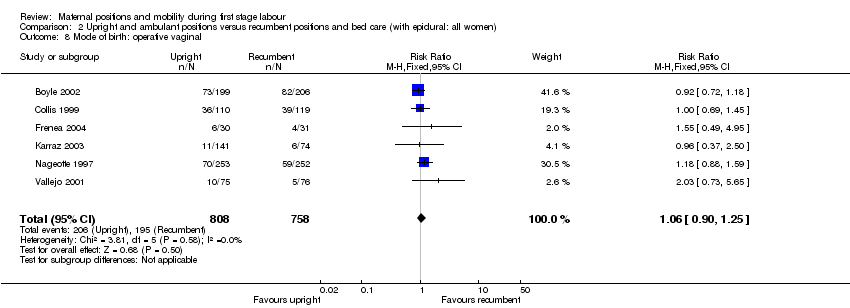 Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 8 Mode of birth: operative vaginal. | ||||
| 9 Mode of birth: operative vaginal: subgroup analysis: parity Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 2.9  Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 9 Mode of birth: operative vaginal: subgroup analysis: parity. | ||||
| 9.1 Nulliparous women | 4 | 1084 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [0.95, 1.94] |
| 9.2 Multiparous women | 1 | 111 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.49, 2.42] |
| 10 Mode of birth: operative vaginal: subgroup analysis: onset of labour Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.10  Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 10 Mode of birth: operative vaginal: subgroup analysis: onset of labour. | ||||
| 10.1 Spontaneous labour: all women | 1 | 505 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.88, 1.59] |
| 10.2 Induction of labour: all women | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Mode of birth: operative vaginal: subgroup analysis: position types Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 2.11  Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 11 Mode of birth: operative vaginal: subgroup analysis: position types. | ||||
| 11.1 Sitting vs Recumbent / supine / lateral | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Walking vs Recumbent / supine / lateral | 2 | 276 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [0.56, 2.44] |
| 11.3 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 1 | 151 | Risk Ratio (M‐H, Random, 95% CI) | 2.03 [0.73, 5.65] |
| 11.4 Sitting vs Bed care | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.5 Walking vs Bed care | 2 | 910 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.81, 1.31] |
| 11.6 Sitting, standing, squatting, kneeling or walking vs Bed care | 1 | 229 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.69, 1.45] |
| 12 Mode of birth: operative vaginal: subgroup analysis: position types Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 2.12 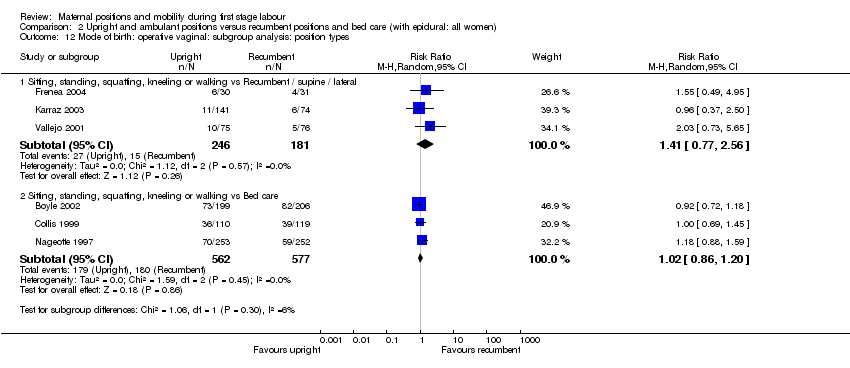 Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 12 Mode of birth: operative vaginal: subgroup analysis: position types. | ||||
| 12.1 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 3 | 427 | Risk Ratio (M‐H, Random, 95% CI) | 1.41 [0.77, 2.56] |
| 12.2 Sitting, standing, squatting, kneeling or walking vs Bed care | 3 | 1139 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.86, 1.20] |
| 13 Mode of birth: operative vaginal: sensitivity analysis Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.13 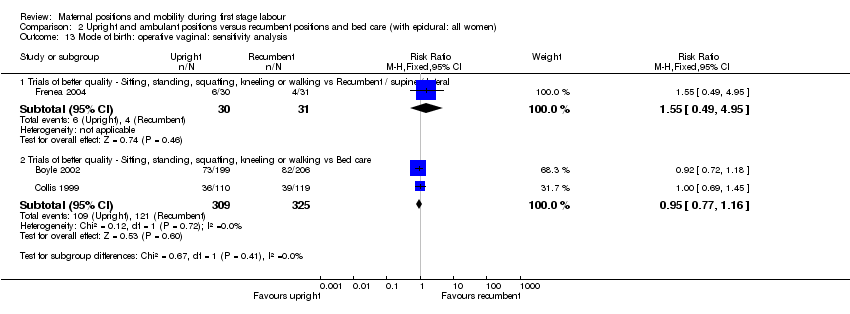 Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 13 Mode of birth: operative vaginal: sensitivity analysis. | ||||
| 13.1 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 1 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.55 [0.49, 4.95] |
| 13.2 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Bed care | 2 | 634 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.77, 1.16] |
| 14 Mode of birth: caesarean birth Show forest plot | 6 | 1566 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.83, 1.32] |
| Analysis 2.14  Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 14 Mode of birth: caesarean birth. | ||||
| 15 Mode of birth: caesarean birth: subgroup analysis: parity Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 2.15  Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 15 Mode of birth: caesarean birth: subgroup analysis: parity. | ||||
| 15.1 Nulliparous women | 4 | 1084 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.75, 1.73] |
| 15.2 Multiparous women | 1 | 206 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [0.55, 3.09] |
| 16 Mode of birth: caesarean birth: subgroup analysis: onset of labour Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.16  Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 16 Mode of birth: caesarean birth: subgroup analysis: onset of labour. | ||||
| 16.1 Spontaneous labour: all women | 1 | 505 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.64, 1.40] |
| 16.2 Induction of labour: all women | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Mode of birth: caesarean birth: subgroup analysis: position types Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 2.17  Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 17 Mode of birth: caesarean birth: subgroup analysis: position types. | ||||
| 17.1 Sitting vs Recumbent / supine / lateral | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Walking vs Recumbent / supine / lateral | 2 | 276 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.35, 1.56] |
| 17.3 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 1 | 151 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.49, 1.82] |
| 17.4 Sitting vs Bed care | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.5 Walking vs Bed care | 2 | 910 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.74, 1.94] |
| 17.6 Sitting, standing, squatting, kneeling or walking vs Bed care | 1 | 229 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.53, 1.95] |
| 18 Mode of birth: caesarean birth: subgroup analysis: position types Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 2.18 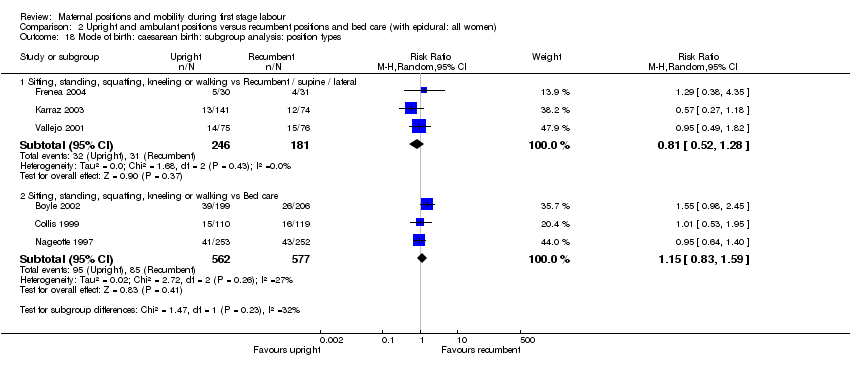 Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 18 Mode of birth: caesarean birth: subgroup analysis: position types. | ||||
| 18.1 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 3 | 427 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.52, 1.28] |
| 18.2 Sitting, standing, squatting, kneeling or walking vs Bed care | 3 | 1139 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.83, 1.59] |
| 19 Mode of birth: caesarean birth: sensitivity analysis Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.19 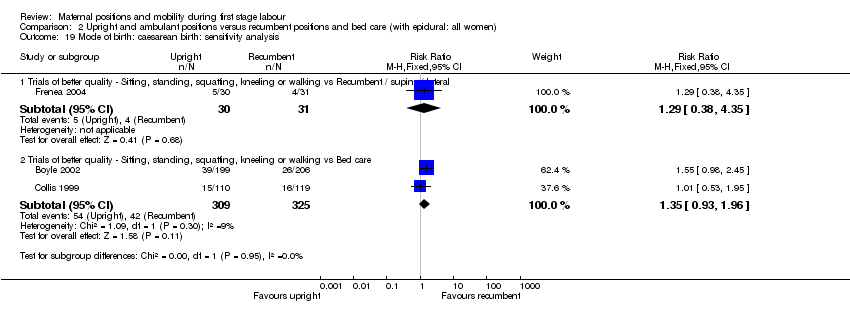 Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 19 Mode of birth: caesarean birth: sensitivity analysis. | ||||
| 19.1 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 1 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.38, 4.35] |
| 19.2 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Bed care | 2 | 634 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.35 [0.93, 1.96] |
| 20 Maternal satisfaction | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Maternal pain Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 2.21  Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 21 Maternal pain. | ||||
| 21.1 Requiring additional Bupivocaine bolus doses | 2 | 720 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.22, 1.48] |
| 22 Analgesia amount Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.22  Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 22 Analgesia amount. | ||||
| 22.1 Bupivocaine | 3 | 463 | Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐2.32, 1.84] |
| 22.2 Ropivacaine | 1 | 151 | Mean Difference (IV, Random, 95% CI) | 19.70 [0.77, 38.63] |
| 22.3 Fentanyl | 1 | 229 | Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐1.99, 1.23] |
| 22.4 Bupivocaine & Fentanyl | 1 | 409 | Mean Difference (IV, Random, 95% CI) | ‐1.37 [‐7.59, 4.85] |
| 23 Duration of second stage of labour (minutes) Show forest plot | 2 | 204 | Mean Difference (IV, Fixed, 95% CI) | 2.35 [‐15.22, 19.91] |
| Analysis 2.23  Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 23 Duration of second stage of labour (minutes). | ||||
| 24 Augmentation of labour using oxytocin Show forest plot | 5 | 1161 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.90, 1.07] |
| Analysis 2.24  Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 24 Augmentation of labour using oxytocin. | ||||
| 25 Artificial rupture of membranes | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 26 Hypotension requiring intervention Show forest plot | 3 | 781 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.52, 2.45] |
| Analysis 2.26 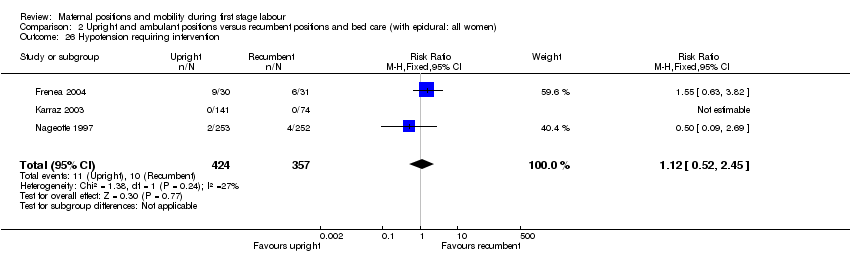 Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 26 Hypotension requiring intervention. | ||||
| 27 Estimated blood loss > 500 mL | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 28 Perineal trauma | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 28.1 Episiotomy | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 28.2 Second‐degree tears | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 28.3 Third‐degree tears | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 29 Fetal distress (requiring immediate delivery) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 30 Use of neonatal mechanical ventilation | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 31 Apgar scores Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.31 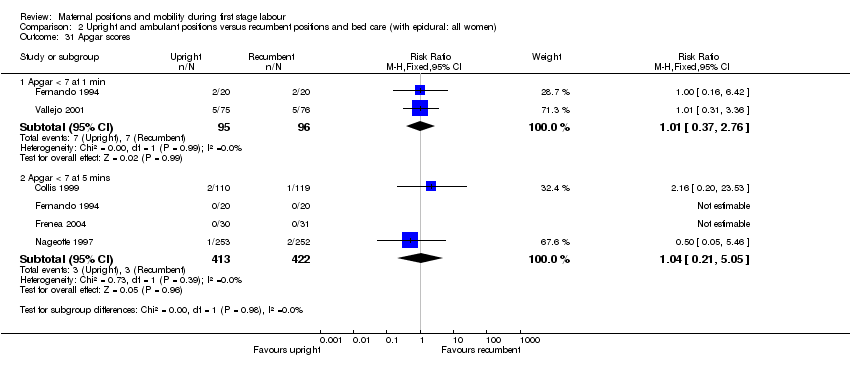 Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 31 Apgar scores. | ||||
| 31.1 Apgar < 7 at 1 min | 2 | 191 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.37, 2.76] |
| 31.2 Apgar < 7 at 5 mins | 4 | 835 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.21, 5.05] |
| 32 Admission to NICU | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 33 Perinatal mortality | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |

Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.

Funnel plot of comparison: 1 Upright and ambulant positions versus recumbent positions and bed care, outcome: 1.1 Duration of first stage labour (hours).
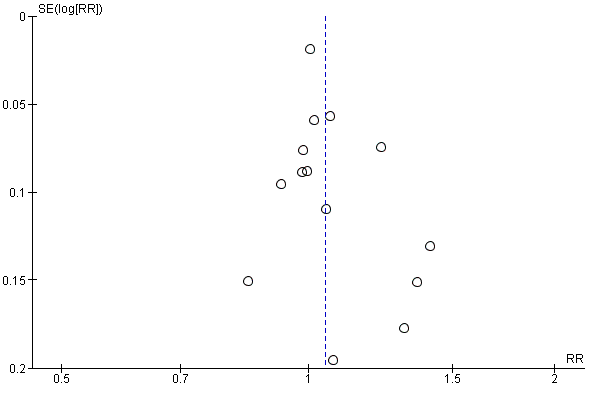
Funnel plot of comparison: 1 Upright and ambulant positions versus recumbent positions and bed care, outcome: 1.8 Mode of birth: spontaneous vaginal.
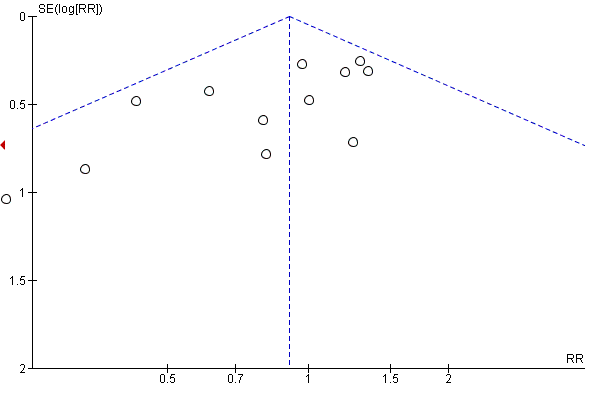
Funnel plot of comparison: 1 Upright and ambulant positions versus recumbent positions and bed care, outcome: 1.15 Mode of birth: operative vaginal: all women.

Funnel plot of comparison: 1 Upright and ambulant positions versus recumbent positions and bed care, outcome: 1.22 Mode of birth: caesarean birth.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 1 Duration of first stage labour (hours).

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 2 Duration of first stage labour (hours): subgroup analysis: parity.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 3 Duration of first stage labour (hours): subgroup analysis: onset of labour.
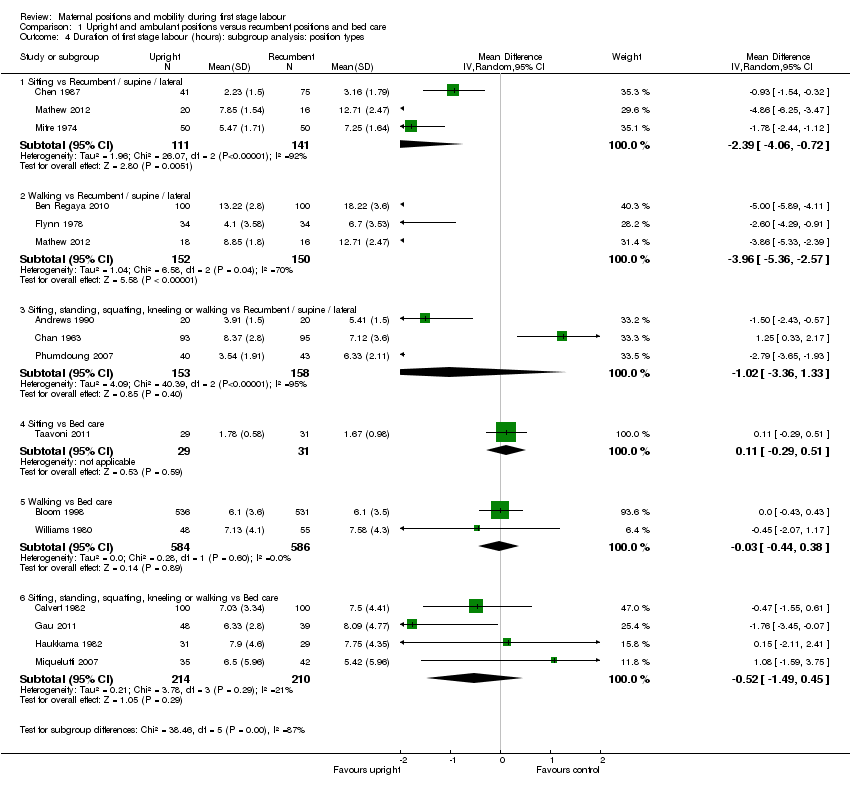
Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 4 Duration of first stage labour (hours): subgroup analysis: position types.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 5 Duration of first stage labour (hours): subgroup analysis: position types.
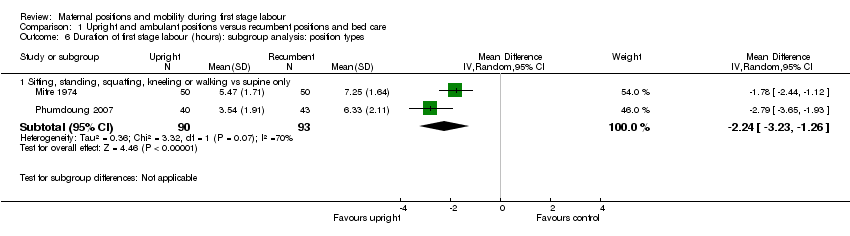
Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 6 Duration of first stage labour (hours): subgroup analysis: position types.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 7 Duration of first stage labour (hours): sensitivity analysis ‐ positions.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 8 Mode of birth: spontaneous vaginal.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 9 Mode of birth: spontaneous vaginal: subgroup analysis: parity.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 10 Mode of birth: spontaneous vaginal: subgroup analysis: onset of labour.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 11 Mode of birth: spontaneous vaginal: subgroup analysis: position types.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 12 Mode of birth: spontaneous vaginal: subgroup analysis: position types.
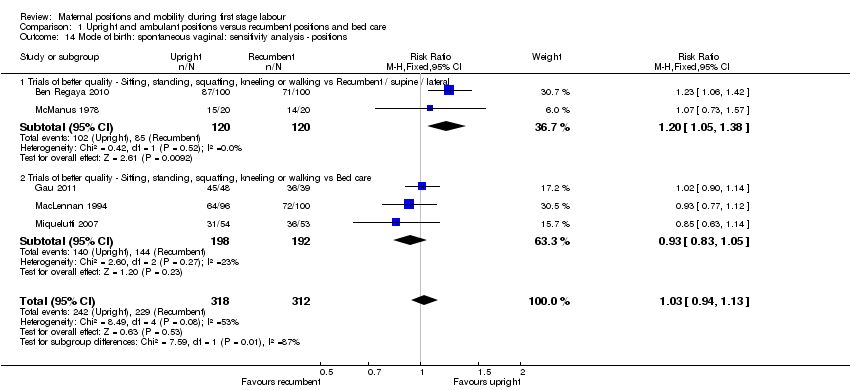
Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 14 Mode of birth: spontaneous vaginal: sensitivity analysis ‐ positions.
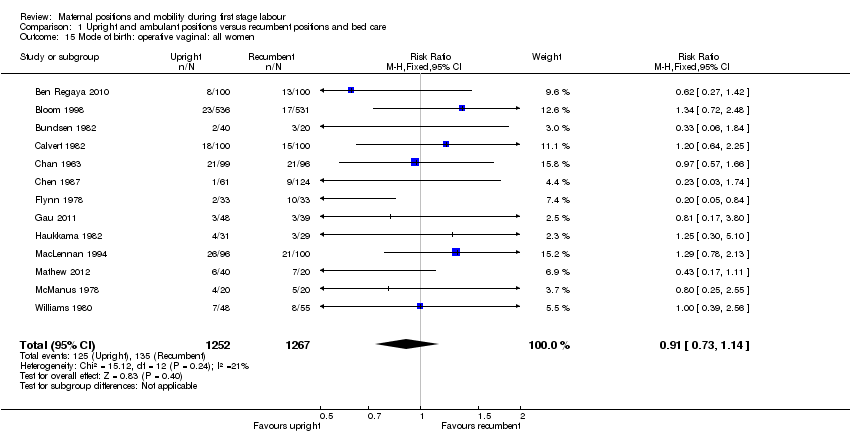
Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 15 Mode of birth: operative vaginal: all women.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 16 Mode of birth: operative vaginal: subgroup analysis: parity.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 17 Mode of birth: operative vaginal: subgroup analysis: onset of labour.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 18 Mode of birth: operative vaginal: subgroup analysis: position types.
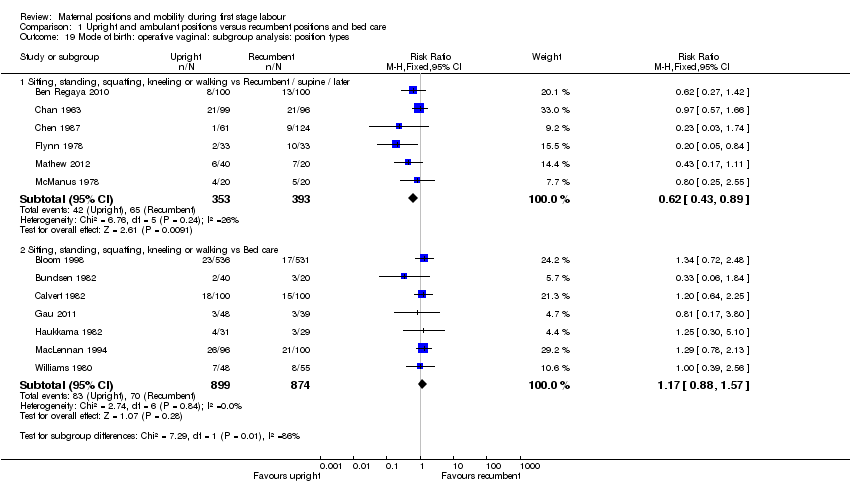
Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 19 Mode of birth: operative vaginal: subgroup analysis: position types.
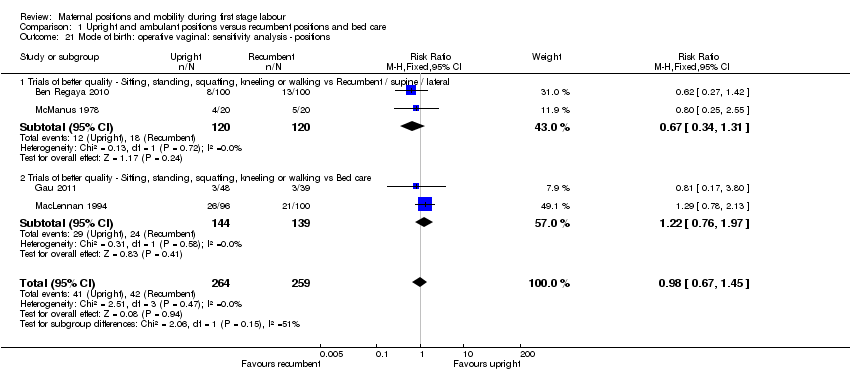
Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 21 Mode of birth: operative vaginal: sensitivity analysis ‐ positions.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 22 Mode of birth: caesarean birth.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 23 Mode of birth: caesarean birth: subgroup analysis: parity.
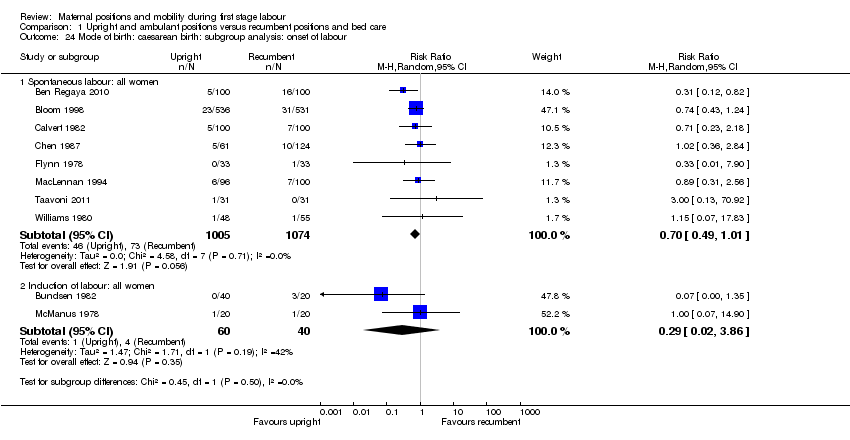
Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 24 Mode of birth: caesarean birth: subgroup analysis: onset of labour.
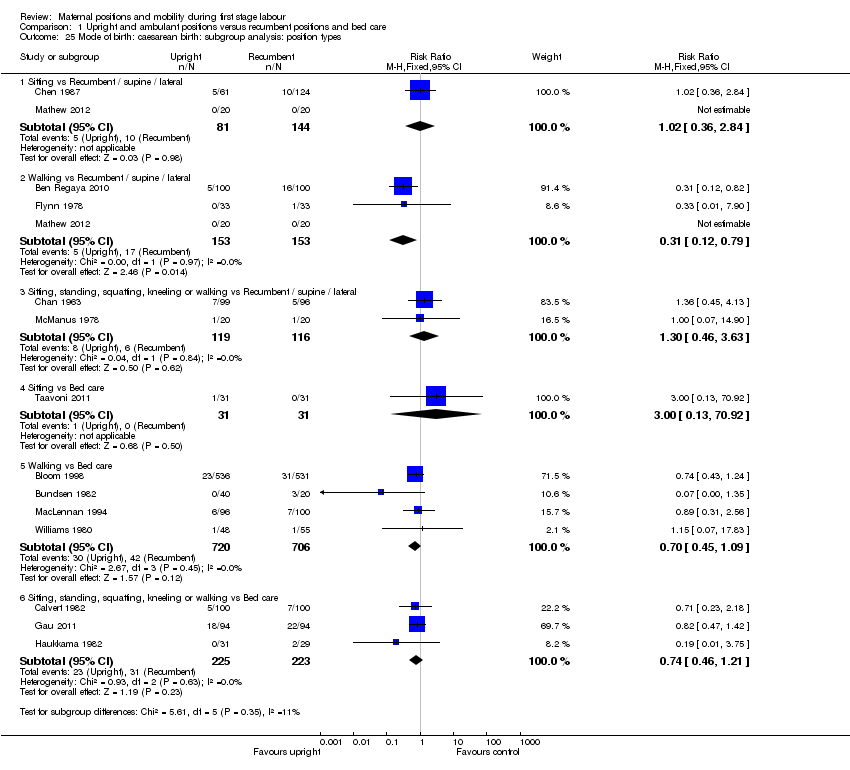
Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 25 Mode of birth: caesarean birth: subgroup analysis: position types.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 26 Mode of birth: caesarean birth: subgroup analysis: position types.
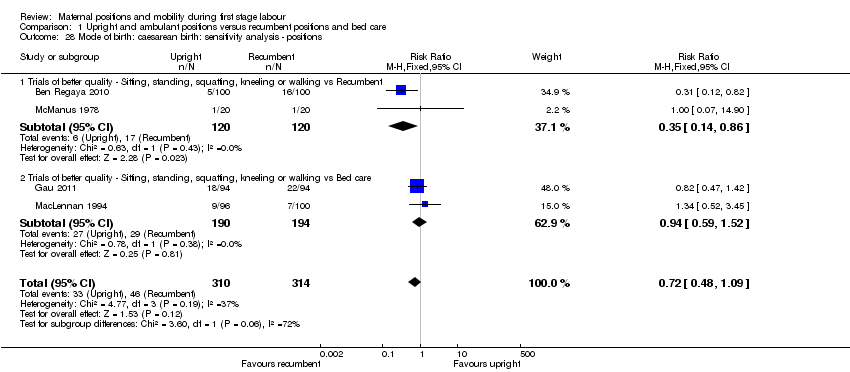
Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 28 Mode of birth: caesarean birth: sensitivity analysis ‐ positions.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 29 Analgesia type.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 30 Maternal satisfaction.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 31 Maternal comfort.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 32 Maternal pain.
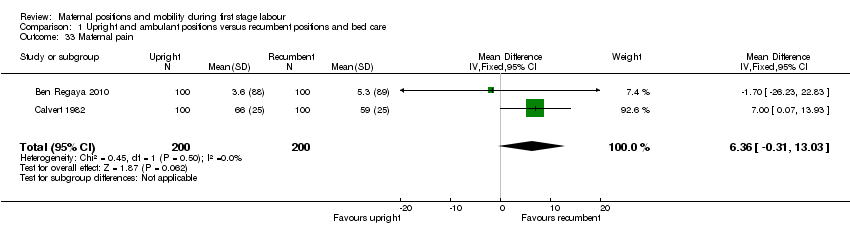
Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 33 Maternal pain.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 34 Maternal pain.
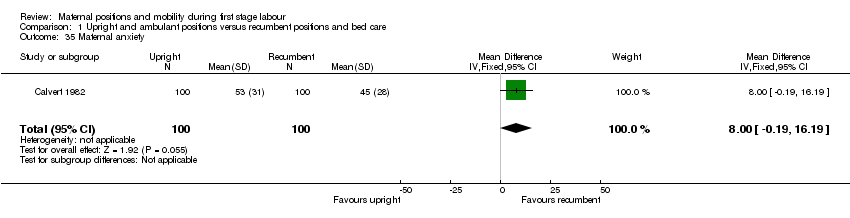
Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 35 Maternal anxiety.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 36 Analgesia amount.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 37 Duration of second stage of labour (minutes).

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 38 Augmentation of labour using oxytocin.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 39 Artificial rupture of membranes.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 41 Estimated blood loss > 500 mL.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 42 Perineal trauma.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 43 Fetal distress (requiring immediate delivery).
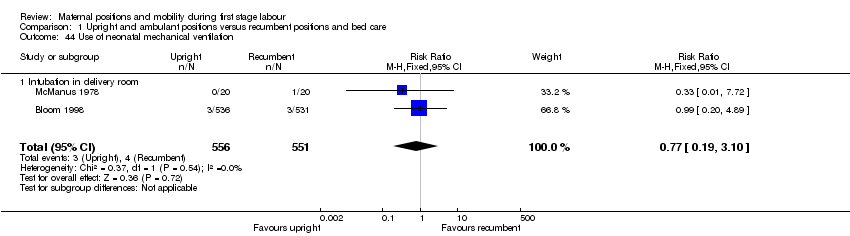
Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 44 Use of neonatal mechanical ventilation.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 45 Apgar scores.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 46 Admission to NICU.

Comparison 1 Upright and ambulant positions versus recumbent positions and bed care, Outcome 47 Perinatal mortality.

Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 2 Mode of birth: spontaneous vaginal.

Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 3 Mode of birth: spontaneous vaginal: subgroup analysis: parity.
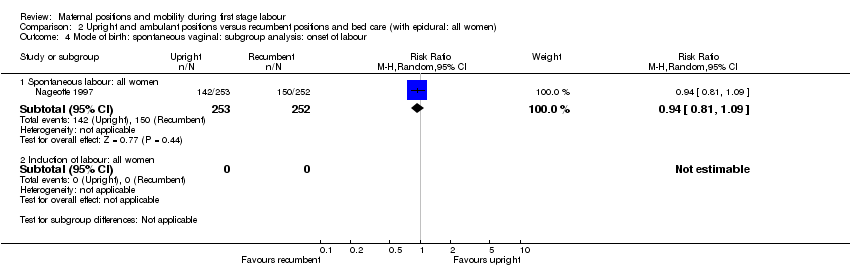
Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 4 Mode of birth: spontaneous vaginal: subgroup analysis: onset of labour.

Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 5 Mode of birth: spontaneous vaginal: subgroup analysis: position types.

Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 6 Mode of birth: spontaneous vaginal: subgroup analysis: position types.

Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 7 Mode of birth: spontaneous vaginal: sensitivity analysis.

Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 8 Mode of birth: operative vaginal.

Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 9 Mode of birth: operative vaginal: subgroup analysis: parity.
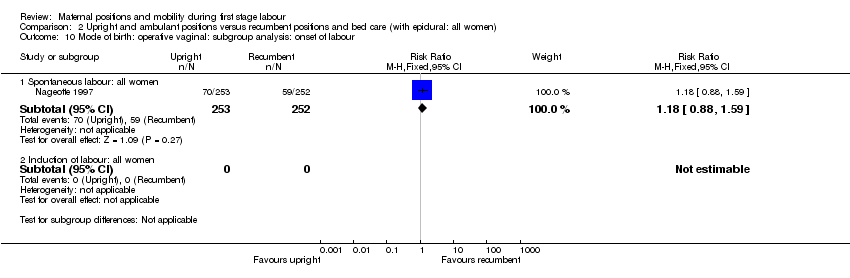
Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 10 Mode of birth: operative vaginal: subgroup analysis: onset of labour.

Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 11 Mode of birth: operative vaginal: subgroup analysis: position types.

Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 12 Mode of birth: operative vaginal: subgroup analysis: position types.

Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 13 Mode of birth: operative vaginal: sensitivity analysis.

Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 14 Mode of birth: caesarean birth.

Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 15 Mode of birth: caesarean birth: subgroup analysis: parity.

Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 16 Mode of birth: caesarean birth: subgroup analysis: onset of labour.
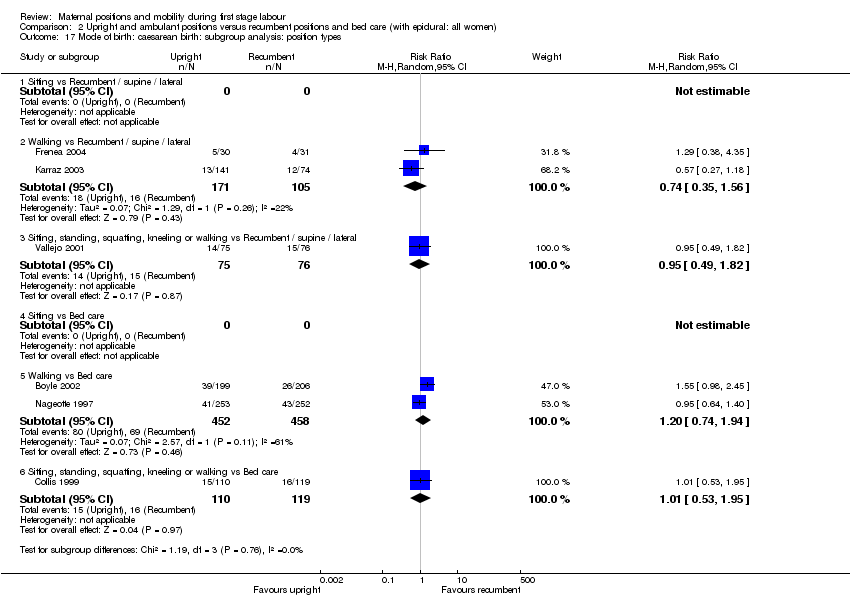
Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 17 Mode of birth: caesarean birth: subgroup analysis: position types.

Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 18 Mode of birth: caesarean birth: subgroup analysis: position types.

Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 19 Mode of birth: caesarean birth: sensitivity analysis.
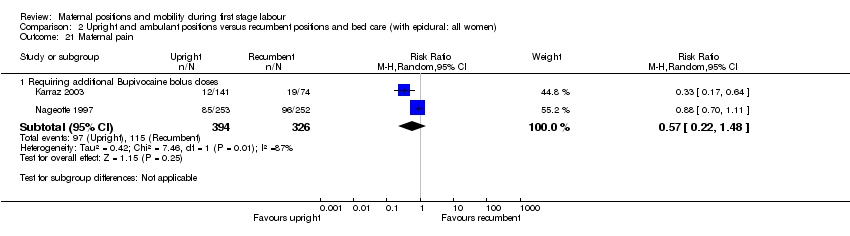
Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 21 Maternal pain.
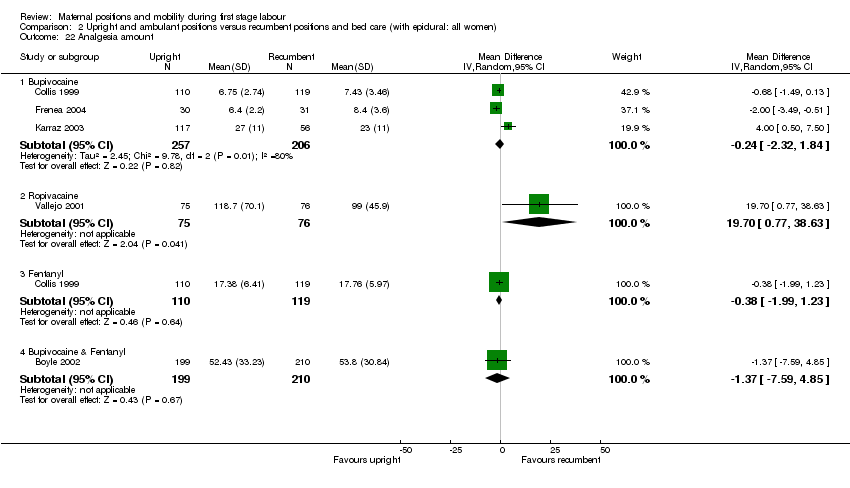
Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 22 Analgesia amount.

Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 23 Duration of second stage of labour (minutes).

Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 24 Augmentation of labour using oxytocin.

Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 26 Hypotension requiring intervention.
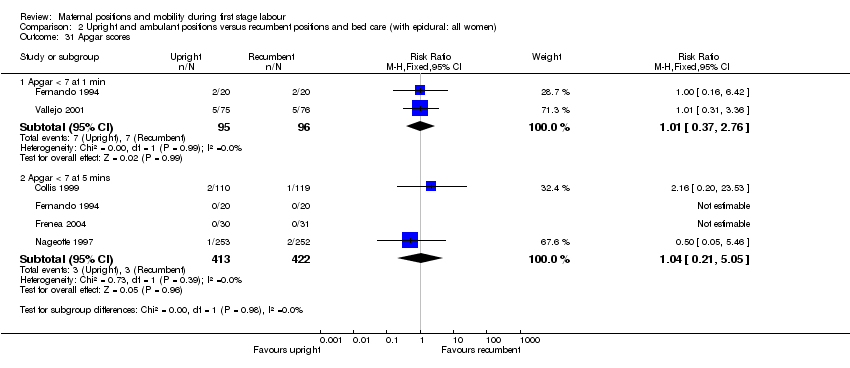
Comparison 2 Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women), Outcome 31 Apgar scores.
| Comparison 1: Upright and ambulant positions versus recumbent positions and bed care Outcomes showing significance | ||
|
| Primary Outcomes | Secondary Outcomes |
| Maternal | 1. Shorter duration of labour if upright. Subgroup analysis demonstrated this when:
Sensitivity analysis, which excluded lower quality trials, comparing sitting, standing, squatting, kneeling or walking with recumbent/supine/lateral did confirm this result.
2. More likely to have a vaginal birth if upright. Subgroup analysis demonstrated this when:
Sensitivity analysis, which excluded lower quality trials, comparing sitting, standing, squatting, kneeling or walking with recumbent/supine/lateral did confirm this result. 3. Less likely to have operative birth if upright. Subgroup analysis demonstrated this when:
Sensitivity analysis, which excluded lower quality trials, did confirm this result.
3. Less likely to have caesarean birth if upright. Subgroup analysis demonstrated this when:
Sensitivity analysis, which excluded lower quality trials, comparing sitting, standing, squatting, kneeling or walking with recumbent/supine/lateral did confirm this result. | 1. Less likely to have an epidural if upright. 2. Lower pain scores if upright. 3. BUT More anxiety for nulliparous women if upright. However this outcome is only from 1 study of 206 women.
Note: there were no data for: spontaneous rupture of membranes or hypotension requiring intervention. |
| Fetal / Neonatal |
| 1. Less likely to have admission to NICU if mother is upright. |
|
| ||
| Comparison 2: Upright and ambulant positions versus recumbent positions and bed care (all women: epidural) Outcomes showing significance | ||
|
| Primary Outcomes | Secondary Outcomes |
| Maternal | 1. More likely to have operative vaginal birth if multiparous and upright (subgroup analysis: parity only). Note: there were no data for: duration of first stage labour; maternal satisfaction. |
Note: there was no data for: artificial rupture of membranes; spontaneous rupture of membranes; estimated blood loss > 500 mL; perineal trauma. |
| Fetal / Neonatal | Note: there were no data for: fetal distress requiring immediate birth or use of neonatal mechanical ventilation. | Note: there were no data for: admission to the NICU. |
| NICU: neonatal intensive care unit | ||
| Trial and participant numbers, grouped by comparison and sorted alphabetically | ||||||||
| Comparison 1: Upright and ambulant positions versus recumbent positions and bed care | Comparison 2: Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women) | |||||||
| No. of studies | Author | Year | No. | No. of studies | Author | Year | No. | |
| 1 | Andrews | 1990 | 40 | 1 | Boyle | 2002 | 409 | |
| 2 | Ben Regaya | 2010 | 200 | 2 | Collis | 1999 | 229 | |
| 3 | Bloom | 1998 | 1067 | 3 | Fernando | 1994 | 40 | |
| 4 | Bundsen | 1982 | 60 | 4 | Frenea | 2004 | 61 | |
| 5 | Calvert | 1982 | 200 | 5 | Karraz | 2003 | 221 | |
| 6 | Chan | 1963 | 200 | 6 | Nageotte | 1997 | 761 | |
| 7 | Chen | 1987 | 185 | 7 | Vallejo | 2001 | 160 | |
| 8 | Flynn | 1978 | 68 | |||||
| 9 | Gau | 2011 | 188 | |||||
| 10 | Haukkama | 1982 | 60 | |||||
| 11 | MacLennan | 1994 | 196 | |||||
| 12 | Mathew | 2012 | 60 | |||||
| 13 | McManus | 1978 | 40 | |||||
| 14 | Miquelutti | 2007 | 107 | |||||
| 15 | Mitre | 1974 | 100 | |||||
| 16 | Phumduong | 2007 | 204 | |||||
| 17 | Taavoni | 2011 | 62 | |||||
| 18 | Williams | 1980 | 300 | |||||
| 18 | 3337 | 7 | 1881 | |||||
| Total number of studies for comparisons 1&2: | 25 | |||||||
| Total number of participants for comparisons 1&2: | 5218 | |||||||
| Method of birth outcomes, grouped by comparison | ||||||||||||||
|
| Comparison 1: Upright and ambulant positions versus recumbent positions and bed care | Comparison 2: Upright and ambulant positions versus recumbent positions and bed care (with epidural: all women) | ||||||||||||
|
| Upright | Recumbent | Comp. 1 | Upright | Recumbent | Comp. 2 | ||||||||
|
| n | total | % | n | total | % | Total | n | total | % | n | total | % | Total |
| Vaginal Birth | 1105 | 1306 | 85% | 1084 | 1320 | 82% | 83% | 475 | 808 | 59% | 447 | 758 | 59% | 59% |
| Operative Vaginal Birth | 125 | 1252 | 10% | 135 | 1267 | 11% | 10% | 206 | 808 | 25% | 195 | 758 | 26% | 26% |
| Caesarean Birth | 72 | 1329 | 5% | 106 | 1353 | 8% | 7% | 127 | 808 | 16% | 116 | 758 | 15% | 16% |
| Characteristics of all studies, sorted by year of publication | |||||||||
| Author | Year | Upright | Recumbent | Country | Parity | No. | All women: epidural | All women: other | |
| 1 | Chan | 1963 | sit or walk | supine or lateral | Hong Kong | nulliparous | 200 | ||
| 2 | Mitre | 1974 | sit | supine | U.S.A. | nulliparous | 100 | ||
| 3 | Flynn | 1978 | walk | lateral | U.K. | mixed | 68 | External monitoring | |
| 4 | McManus | 1978 | walk or sit | lateral | U.K. | mixed | 40 | Induction; Amniotomy | |
| 5 | Williams | 1980 | walk | bed care | U.K. | mixed | 300 | ||
| 6 | Bundsen | 1982 | walking | bed care | Sweden | mixed | 60 | Induction; Amniotomy; Internal Monitoring | |
| 7 | Calvert | 1982 | walk or sit | bed care | U.K. | mixed | 200 | External monitoring | |
| 8 | Haukkama | 1982 | sit or walk | bed care | Finland | mixed | 60 | External monitoring | |
| 9 | Chen | 1987 | sit | dorsal or lateral | Japan | mixed | 185 | Amniotomy | |
| 10 | Andrews | 1990 | standing, walking, sitting, squatting, kneeling | supine, lateral, prone | U.S.A. | nulliparous | 40 | ||
| 11 | Fernando | 1994 | walking, standing, sitting | bed care | U.K. | nulliparous | 40 | Epidural | |
| 12 | MacLennan | 1994 | walk | bed care | Australia | mixed | 196 | External monitoring | |
| 13 | Nageotte | 1997 | walk | bed care | U.S.A. | nulliparous | 761 | Epidural | |
| 14 | Bloom | 1998 | walking as desired | bed care | U.S.A. | mixed | 1067 | ||
| 15 | Collis | 1999 | walking, standing, sitting | bed care | U.K. | nulliparous | 229 | Epidural | External Monitoring |
| 16 | Vallejo | 2001 | walk or sit | lateral | U.S.A. | nulliparous | 160 | Epidural | Induction; External Monitoring |
| 17 | Boyle | 2002 | walk | bed care | U.K. | mixed | 409 | Epidural | |
| 18 | Karraz | 2003 | walk | supine, semi supine or lateral | France | mixed | 221 | Epidural | Induction |
| 19 | Frenea | 2004 | ambulation | dorsal or lateral | France | mixed | 61 | Epidural | External Monitoring |
| 20 | Miquelutti | 2007 | stand, walk, sit, crouch, kneel | bed care | Brazil | nulliparous | 107 | ||
| 21 | Phumduong | 2007 | kneeling | supine | Thailand | nulliparous | 204 | ||
| 22 | Ben Regaya | 2010 | ambulation | dorsal or lateral | Tunisia, North Africa | nulliparous | 200 | ||
| 23 | Gau | 2011 | sitting, standing, kneeling, squatting | bed care | Taiwan | mixed | 188 | External Monitoring | |
| 24 | Taavoni | 2011 | sitting | bed care | Iran | nulliparous | 62 | ||
| 25 | Mathew | 2012 | walk or sit | dorsal or lateral | India | nulliparous | 60 | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Duration of first stage labour (hours) Show forest plot | 15 | 2503 | Mean Difference (IV, Random, 95% CI) | ‐1.36 [‐2.22, ‐0.51] |
| 2 Duration of first stage labour (hours): subgroup analysis: parity Show forest plot | 12 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Nulliparous women | 12 | 1486 | Mean Difference (IV, Random, 95% CI) | ‐1.21 [‐2.35, ‐0.07] |
| 2.2 Multiparous women | 4 | 662 | Mean Difference (IV, Random, 95% CI) | ‐0.56 [‐1.19, 0.06] |
| 3 Duration of first stage labour (hours): subgroup analysis: onset of labour Show forest plot | 11 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Spontaneous labour: all women | 11 | 2114 | Mean Difference (IV, Random, 95% CI) | ‐1.43 [‐2.35, ‐0.50] |
| 3.2 Induction of labour: all women | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Duration of first stage labour (hours): subgroup analysis: position types Show forest plot | 15 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Sitting vs Recumbent / supine / lateral | 3 | 252 | Mean Difference (IV, Random, 95% CI) | ‐2.39 [‐4.06, ‐0.72] |
| 4.2 Walking vs Recumbent / supine / lateral | 3 | 302 | Mean Difference (IV, Random, 95% CI) | ‐3.96 [‐5.36, ‐2.57] |
| 4.3 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 3 | 311 | Mean Difference (IV, Random, 95% CI) | ‐1.02 [‐3.36, 1.33] |
| 4.4 Sitting vs Bed care | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.29, 0.51] |
| 4.5 Walking vs Bed care | 2 | 1170 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.44, 0.38] |
| 4.6 Sitting, standing, squatting, kneeling or walking vs Bed care | 4 | 424 | Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐1.49, 0.45] |
| 5 Duration of first stage labour (hours): subgroup analysis: position types Show forest plot | 15 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 8 | 849 | Mean Difference (IV, Random, 95% CI) | ‐2.19 [‐3.49, ‐0.89] |
| 5.2 Sitting, standing, squatting, kneeling or walking vs Bed care | 7 | 1654 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.30, 0.25] |
| 6 Duration of first stage labour (hours): subgroup analysis: position types Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 Sitting, standing, squatting, kneeling or walking vs supine only | 2 | 183 | Mean Difference (IV, Random, 95% CI) | ‐2.24 [‐3.23, ‐1.26] |
| 7 Duration of first stage labour (hours): sensitivity analysis ‐ positions Show forest plot | 3 | 364 | Mean Difference (IV, Fixed, 95% CI) | ‐3.86 [‐4.73, ‐2.99] |
| 7.1 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 1 | 200 | Mean Difference (IV, Fixed, 95% CI) | ‐3.00 [‐6.05, ‐3.95] |
| 7.2 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Bed care | 2 | 164 | Mean Difference (IV, Fixed, 95% CI) | ‐1.33 [‐2.89, 0.23] |
| 8 Mode of birth: spontaneous vaginal Show forest plot | 14 | 2626 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.99, 1.11] |
| 9 Mode of birth: spontaneous vaginal: subgroup analysis: parity Show forest plot | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 9.1 Nulliparous women | 8 | 1282 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.96, 1.17] |
| 9.2 Multiparous women | 4 | 675 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.99, 1.05] |
| 10 Mode of birth: spontaneous vaginal: subgroup analysis: onset of labour Show forest plot | 10 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 10.1 Spontaneous labour: all women | 8 | 2124 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.97, 1.12] |
| 10.2 Induction of labour: all women | 2 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.98, 1.57] |
| 11 Mode of birth: spontaneous vaginal: subgroup analysis: position types Show forest plot | 14 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 11.1 Sitting vs Recumbent / supine / lateral | 2 | 225 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.88, 1.64] |
| 11.2 Walking vs Recumbent / supine / lateral | 3 | 306 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [1.11, 1.42] |
| 11.3 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 2 | 235 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.85, 1.17] |
| 11.4 Sitting vs Bed care | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.5 Walking vs Bed care | 4 | 1426 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.93, 1.11] |
| 11.6 Sitting, standing, squatting, kneeling or walking vs Bed care | 4 | 454 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.92, 1.08] |
| 12 Mode of birth: spontaneous vaginal: subgroup analysis: position types Show forest plot | 14 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 12.1 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 6 | 746 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [1.03, 1.26] |
| 12.2 Sitting, standing, squatting, kneeling or walking vs Bed care | 8 | 1880 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.97, 1.04] |
| 13 Mode of birth: spontaneous vaginal: subgroup analysis: position types | 0 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 13.1 Sitting, standing, squatting, kneeling or walking vs supine only | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Mode of birth: spontaneous vaginal: sensitivity analysis ‐ positions Show forest plot | 5 | 630 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.94, 1.13] |
| 14.1 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.2 [1.05, 1.38] |
| 14.2 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Bed care | 3 | 390 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.83, 1.05] |
| 15 Mode of birth: operative vaginal: all women Show forest plot | 13 | 2519 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.73, 1.14] |
| 16 Mode of birth: operative vaginal: subgroup analysis: parity Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 16.1 Nulliparous women | 7 | 1175 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.65, 1.18] |
| 16.2 Multiparous women | 4 | 675 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.24, 3.51] |
| 17 Mode of birth: operative vaginal: subgroup analysis: onset of labour Show forest plot | 9 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 17.1 Spontaneous labour: all women | 7 | 2017 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.62, 1.39] |
| 17.2 Induction of labour: all women | 2 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.23, 1.58] |
| 18 Mode of birth: operative vaginal: subgroup analysis: position types Show forest plot | 13 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 18.1 Sitting vs Recumbent / supine / lateral | 2 | 225 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.18 [0.04, 0.75] |
| 18.2 Walking vs Recumbent / supine / lateral | 3 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.28, 0.89] |
| 18.3 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / later | 2 | 235 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.58, 1.52] |
| 18.4 Sitting vs Bed care | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18.5 Walking vs Bed care | 4 | 1426 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.84, 1.68] |
| 18.6 Sitting, standing, squatting, kneeling or walking vs Bed care | 3 | 347 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.67, 1.96] |
| 19 Mode of birth: operative vaginal: subgroup analysis: position types Show forest plot | 13 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 19.1 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / later | 6 | 746 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.43, 0.89] |
| 19.2 Sitting, standing, squatting, kneeling or walking vs Bed care | 7 | 1773 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.88, 1.57] |
| 20 Mode of birth: operative vaginal: subgroup analysis: position types | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 20.1 Sitting, standing, squatting, kneeling or walking vs supine only | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Mode of birth: operative vaginal: sensitivity analysis ‐ positions Show forest plot | 4 | 523 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.67, 1.45] |
| 21.1 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.34, 1.31] |
| 21.2 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Bed care | 2 | 283 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.76, 1.97] |
| 22 Mode of birth: caesarean birth Show forest plot | 14 | 2682 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.54, 0.94] |
| 23 Mode of birth: caesarean birth: subgroup analysis: parity Show forest plot | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 23.1 Nulliparous women | 8 | 1237 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.52, 1.18] |
| 23.2 Multiparous women | 4 | 675 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.22, 1.38] |
| 24 Mode of birth: caesarean birth: subgroup analysis: onset of labour Show forest plot | 10 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 24.1 Spontaneous labour: all women | 8 | 2079 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.49, 1.01] |
| 24.2 Induction of labour: all women | 2 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 0.29 [0.02, 3.86] |
| 25 Mode of birth: caesarean birth: subgroup analysis: position types Show forest plot | 14 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 25.1 Sitting vs Recumbent / supine / lateral | 2 | 225 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.36, 2.84] |
| 25.2 Walking vs Recumbent / supine / lateral | 3 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.12, 0.79] |
| 25.3 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 2 | 235 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.46, 3.63] |
| 25.4 Sitting vs Bed care | 1 | 62 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 70.92] |
| 25.5 Walking vs Bed care | 4 | 1426 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.45, 1.09] |
| 25.6 Sitting, standing, squatting, kneeling or walking vs Bed care | 3 | 448 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.46, 1.21] |
| 26 Mode of birth: caesarean birth: subgroup analysis: position types Show forest plot | 14 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 26.1 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 6 | 746 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.39, 1.15] |
| 26.2 Sitting, standing, squatting, kneeling or walking vs Bed care | 8 | 1936 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.53, 1.02] |
| 27 Mode of birth: caesarean birth: subgroup analysis: position types | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 27.1 Sitting, standing, squatting, kneeling or walking vs supine only | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 28 Mode of birth: caesarean birth: sensitivity analysis ‐ positions Show forest plot | 4 | 624 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.48, 1.09] |
| 28.1 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Recumbent | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.14, 0.86] |
| 28.2 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Bed care | 2 | 384 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.59, 1.52] |
| 29 Analgesia type Show forest plot | 10 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 29.1 Opioid | 7 | 1831 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.85, 1.15] |
| 29.2 Epidural | 9 | 2107 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.66, 0.99] |
| 29.3 Entonox | 3 | 300 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.72, 1.31] |
| 30 Maternal satisfaction Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 30.1 Satisfaction with position reported at 6 cm | 1 | 107 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [0.60, 2.85] |
| 30.2 Preferred upright position | 1 | 107 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.97, 1.61] |
| 31 Maternal comfort Show forest plot | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | 0.74 [‐0.27, 1.75] |
| 31.1 Comfort score | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | 0.74 [‐0.27, 1.75] |
| 32 Maternal pain Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 32.1 Complaints of discomfort/labour more uncomfortable | 3 | 338 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.12, 3.72] |
| 32.2 Requiring analgesia | 4 | 1536 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.84, 1.08] |
| 33 Maternal pain Show forest plot | 2 | 400 | Mean Difference (IV, Fixed, 95% CI) | 6.36 [‐0.31, 13.03] |
| 34 Maternal pain Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 34.1 Visual Analogue Scale (VAS) Score | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐1.74 [‐2.51, ‐0.97] |
| 34.2 Visual Analogue Scale (VAS) Score @ 4 cm | 1 | 87 | Mean Difference (IV, Fixed, 95% CI) | ‐2.0 [‐2.70, ‐1.30] |
| 34.3 Visual Analogue Scale (VAS) Score @ 8 cm | 1 | 87 | Mean Difference (IV, Fixed, 95% CI) | ‐1.70 [‐2.20, ‐1.20] |
| 34.4 Verbal Response Scale (VRS) Score @ 4 cm | 1 | 87 | Mean Difference (IV, Fixed, 95% CI) | ‐10.40 [‐13.27, ‐7.53] |
| 34.5 Verbal Response Scale (VRS) Score@ 8 cm | 1 | 87 | Mean Difference (IV, Fixed, 95% CI) | ‐5.00 [‐11.33, ‐2.67] |
| 34.6 Present Pain Intensity Scale (PPI) @ 4 cm | 1 | 87 | Mean Difference (IV, Fixed, 95% CI) | ‐1.40 [‐3.61, 0.81] |
| 34.7 Present Pain Intensity Scale (PPI) @ 8 cm | 1 | 87 | Mean Difference (IV, Fixed, 95% CI) | ‐0.80 [‐3.76, 2.16] |
| 35 Maternal anxiety Show forest plot | 1 | 200 | Mean Difference (IV, Fixed, 95% CI) | 8.0 [‐0.19, 16.19] |
| 36 Analgesia amount Show forest plot | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐17.5 [‐36.89, 1.89] |
| 36.1 Narcotics and other analgesia | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐17.5 [‐36.89, 1.89] |
| 37 Duration of second stage of labour (minutes) Show forest plot | 9 | 2077 | Mean Difference (IV, Random, 95% CI) | ‐3.71 [‐9.37, 1.94] |
| 38 Augmentation of labour using oxytocin Show forest plot | 8 | 1826 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.76, 1.05] |
| 39 Artificial rupture of membranes Show forest plot | 4 | 276 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.95, 1.10] |
| 40 Hypotension requiring intervention | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 41 Estimated blood loss > 500 mL Show forest plot | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.14, 3.55] |
| 42 Perineal trauma Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 42.1 Episiotomy | 3 | 1374 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.82, 1.04] |
| 42.2 Second‐degree tears | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 42.3 Third‐degree tears | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 43 Fetal distress (requiring immediate delivery) Show forest plot | 6 | 1757 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.35, 1.33] |
| 44 Use of neonatal mechanical ventilation Show forest plot | 2 | 1107 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.19, 3.10] |
| 44.1 Intubation in delivery room | 2 | 1107 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.19, 3.10] |
| 45 Apgar scores Show forest plot | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 45.1 Apgar < 4 at birth | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.92] |
| 45.2 Apgar < 7 at 1 min | 6 | 706 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.54, 1.31] |
| 45.3 Apgar < 7 at 5 mins | 4 | 466 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.27 [0.34, 31.05] |
| 45.4 Apgar < 3 at 5 mins | 1 | 1067 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 45.5 Apgar < 8 at 5 mins | 1 | 87 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.01, 2.19] |
| 46 Admission to NICU Show forest plot | 2 | 396 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.25, 1.36] |
| 46.1 Admission to NICU | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.04, 0.89] |
| 46.2 Admission to Level I or II nursery | 1 | 196 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.56 [0.45, 5.37] |
| 47 Perinatal mortality Show forest plot | 5 | 1564 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.05, 5.37] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Duration of first stage labour: (minutes) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Mode of birth: spontaneous vaginal Show forest plot | 6 | 1566 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.89, 1.05] |
| 3 Mode of birth: spontaneous vaginal: subgroup analysis: parity Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Nulliparous women | 4 | 1179 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.84, 1.04] |
| 3.2 Multiparous women | 1 | 111 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.81, 1.27] |
| 4 Mode of birth: spontaneous vaginal: subgroup analysis: onset of labour Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 Spontaneous labour: all women | 1 | 505 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.81, 1.09] |
| 4.2 Induction of labour: all women | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Mode of birth: spontaneous vaginal: subgroup analysis: position types Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 Sitting vs Recumbent / supine / lateral | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Walking vs Recumbent / supine / lateral | 2 | 276 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.81, 1.28] |
| 5.3 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 1 | 151 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.75, 1.13] |
| 5.4 Sitting vs Bed care | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.5 Walking vs Bed care | 2 | 910 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.83, 1.06] |
| 5.6 Sitting, standing, squatting, kneeling or walking vs Bed care | 1 | 229 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.78, 1.27] |
| 6 Mode of birth: spontaneous vaginal: subgroup analysis: position types Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 3 | 427 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.86, 1.15] |
| 6.2 Sitting, standing, squatting, kneeling or walking vs Bed care | 3 | 1139 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.85, 1.06] |
| 7 Mode of birth: spontaneous vaginal: sensitivity analysis Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 1 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.61, 1.20] |
| 7.2 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Bed care | 2 | 634 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.81, 1.11] |
| 8 Mode of birth: operative vaginal Show forest plot | 6 | 1566 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.90, 1.25] |
| 9 Mode of birth: operative vaginal: subgroup analysis: parity Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 9.1 Nulliparous women | 4 | 1084 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [0.95, 1.94] |
| 9.2 Multiparous women | 1 | 111 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.49, 2.42] |
| 10 Mode of birth: operative vaginal: subgroup analysis: onset of labour Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 Spontaneous labour: all women | 1 | 505 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.88, 1.59] |
| 10.2 Induction of labour: all women | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Mode of birth: operative vaginal: subgroup analysis: position types Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 11.1 Sitting vs Recumbent / supine / lateral | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Walking vs Recumbent / supine / lateral | 2 | 276 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [0.56, 2.44] |
| 11.3 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 1 | 151 | Risk Ratio (M‐H, Random, 95% CI) | 2.03 [0.73, 5.65] |
| 11.4 Sitting vs Bed care | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.5 Walking vs Bed care | 2 | 910 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.81, 1.31] |
| 11.6 Sitting, standing, squatting, kneeling or walking vs Bed care | 1 | 229 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.69, 1.45] |
| 12 Mode of birth: operative vaginal: subgroup analysis: position types Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 12.1 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 3 | 427 | Risk Ratio (M‐H, Random, 95% CI) | 1.41 [0.77, 2.56] |
| 12.2 Sitting, standing, squatting, kneeling or walking vs Bed care | 3 | 1139 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.86, 1.20] |
| 13 Mode of birth: operative vaginal: sensitivity analysis Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 13.1 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 1 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.55 [0.49, 4.95] |
| 13.2 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Bed care | 2 | 634 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.77, 1.16] |
| 14 Mode of birth: caesarean birth Show forest plot | 6 | 1566 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.83, 1.32] |
| 15 Mode of birth: caesarean birth: subgroup analysis: parity Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 15.1 Nulliparous women | 4 | 1084 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.75, 1.73] |
| 15.2 Multiparous women | 1 | 206 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [0.55, 3.09] |
| 16 Mode of birth: caesarean birth: subgroup analysis: onset of labour Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 16.1 Spontaneous labour: all women | 1 | 505 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.64, 1.40] |
| 16.2 Induction of labour: all women | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Mode of birth: caesarean birth: subgroup analysis: position types Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 17.1 Sitting vs Recumbent / supine / lateral | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Walking vs Recumbent / supine / lateral | 2 | 276 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.35, 1.56] |
| 17.3 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 1 | 151 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.49, 1.82] |
| 17.4 Sitting vs Bed care | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.5 Walking vs Bed care | 2 | 910 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.74, 1.94] |
| 17.6 Sitting, standing, squatting, kneeling or walking vs Bed care | 1 | 229 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.53, 1.95] |
| 18 Mode of birth: caesarean birth: subgroup analysis: position types Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 18.1 Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 3 | 427 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.52, 1.28] |
| 18.2 Sitting, standing, squatting, kneeling or walking vs Bed care | 3 | 1139 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.83, 1.59] |
| 19 Mode of birth: caesarean birth: sensitivity analysis Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 19.1 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Recumbent / supine / lateral | 1 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.38, 4.35] |
| 19.2 Trials of better quality ‐ Sitting, standing, squatting, kneeling or walking vs Bed care | 2 | 634 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.35 [0.93, 1.96] |
| 20 Maternal satisfaction | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Maternal pain Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 21.1 Requiring additional Bupivocaine bolus doses | 2 | 720 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.22, 1.48] |
| 22 Analgesia amount Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 22.1 Bupivocaine | 3 | 463 | Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐2.32, 1.84] |
| 22.2 Ropivacaine | 1 | 151 | Mean Difference (IV, Random, 95% CI) | 19.70 [0.77, 38.63] |
| 22.3 Fentanyl | 1 | 229 | Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐1.99, 1.23] |
| 22.4 Bupivocaine & Fentanyl | 1 | 409 | Mean Difference (IV, Random, 95% CI) | ‐1.37 [‐7.59, 4.85] |
| 23 Duration of second stage of labour (minutes) Show forest plot | 2 | 204 | Mean Difference (IV, Fixed, 95% CI) | 2.35 [‐15.22, 19.91] |
| 24 Augmentation of labour using oxytocin Show forest plot | 5 | 1161 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.90, 1.07] |
| 25 Artificial rupture of membranes | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 26 Hypotension requiring intervention Show forest plot | 3 | 781 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.52, 2.45] |
| 27 Estimated blood loss > 500 mL | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 28 Perineal trauma | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 28.1 Episiotomy | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 28.2 Second‐degree tears | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 28.3 Third‐degree tears | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 29 Fetal distress (requiring immediate delivery) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 30 Use of neonatal mechanical ventilation | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 31 Apgar scores Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 31.1 Apgar < 7 at 1 min | 2 | 191 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.37, 2.76] |
| 31.2 Apgar < 7 at 5 mins | 4 | 835 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.21, 5.05] |
| 32 Admission to NICU | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 33 Perinatal mortality | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |

