Profilaxis con antibióticos para prevenir la endocarditis bacteriana tras intervenciones dentales
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Study characteristics | ||
| Methods | Case‐control study | |
| Participants | All 349 people who developed definite native‐valve endocarditis in the Netherlands over a 2‐year period (1 November 1986 to 1 November 1988) were collected. | |
| Interventions | Cases and controls had to have undergone a medical or dental procedure that required antibiotic prophylaxis within 180 days prior to the onset of symptoms of endocarditis (cases) or their interview (controls). Of the participants who underwent a dental procedure with definite indication for prophylaxis:
Median time from dental procedure to onset of endocarditis in cases was 10 days, range 0 to 175, and for the 7 who received antibiotics median time to onset was 18 days, range 7 to 60. Median time from dental procedure to interview in controls was 71 days, range 0 to 179 (12 missing values ignored), and for the controls who received antibiotics the median was 83 days, range 5 to 151 (1 missing value ignored). For both groups, all information about invasive procedures and use of prophylaxis was checked with medical or dental specialists and pharmacists. | |
| Outcomes | Of the 349 people with definite native‐valve endocarditis, 197 had previous heart disease (10 proxy responders). Of these, 54 had undergone a medical or dental procedure with an indication for prophylaxis within the past 180 days. A causal relationship was ruled out in 6 of these 54 potential cases as the agent isolated from the blood was unlikely to have originated in the area of the procedure. Of the remaining 48 people with endocarditis, 44 had undergone a dental procedure with a definite (24) or possible (20) indication for prophylaxis (none of these cases had used a proxy responder). Of 889 potential controls who were sent an introductory letter, 689 were ineligible (53 had died, 29 had a prosthetic heart valve, 62 could not be located, 102 could not be contacted by phone and 418 had not undergone an invasive dental or medical procedure within the past 180 days) and the remaining 200 were interviewed by phone 2 to 5 days later. 181 of these controls had undergone a dental procedure with definite (79) or possible (102) indication for prophylaxis. The authors ensured that controls had not developed endocarditis, as defined by the diagnostic criteria of Von Reyn 1981. They also checked the appropriateness of antibiotic prophylaxis with medical, dental and pharmacy staff and against the Netherlands Heart Foundation recommendations, finding that 7 of 24 cases and 16 of 79 controls had had appropriate prophylaxis for a dental procedure requiring definite prophylaxis within the previous 180 days. | |
| Notes | The published paper provided data on participants who had both medical and dental invasive procedures. The author kindly separated out those who had had invasive dental interventions. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not undertaken (case‐control study). It is possible that, as dentists decide whether to give prophylaxis or not on the basis of the information about the patient in front of them, those patients appearing more frail may have been more likely to receive prophylaxis. |
| Allocation concealment (selection bias) | High risk | Not undertaken (case‐control study) |
| Blinding of outcome assessment (detection bias) | High risk | Not undertaken |
| Incomplete outcome data (attrition bias) | Unclear risk | Having died was an exclusion criterion for controls but not for cases, who could be included through a proxy. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes and exposure reported |
| Confounding | Unclear risk | Participant sex and cardiac risk factor type was not described for the subgroup who had had a dental procedure, and the type of dental intervention appeared to be different in the cases and controls, although cases and controls were matched for age. Both groups were required to have undergone invasive dental techniques within 180 days prior to onset of symptoms/interview and data were split by time period for both groups. |
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Retrospective analysis of cumulative exposure to bacteraemia following various dental procedures in children with severe congenital heart disease but no cases of endocarditis | |
| Economic analysis of the cost‐effectiveness of using prophylactic antibiotics using same data as Bonhomme 1992 | |
| 2 case studies of high risk patients developing endocarditis after dental treatment with antibiotic prophylaxis | |
| Not all cases at risk and no controls | |
| No control group | |
| Retrospective analysis of 28 cases of endocarditis, no controls | |
| Case report | |
| Economic analysis of the cost‐effectiveness of using prophylactic antibiotics based on published data | |
| No control group | |
| Assessment of the effect of mitral valve prolapse on risk of endocarditis (rather than assessment of the effect of prophylaxis), case‐control design | |
| Participants not at high risk of endocarditis | |
| Cohort study, but it was not stated how many patients had preceding dental treatment, only two cases with preceding dental treatment and no prophylaxis | |
| Case report (German) | |
| All children with cardiac disease received antibiotic prophylaxis before dental extraction, no controls | |
| Retrospective study of a group of people at high risk of endocarditis who had had appropriate prophylaxis for medical and dental interventions, and a group of people at similar risk who did not have appropriate prophylaxis for such interventions. It was not possible to ascertain how many of the cases or controls had had dental interventions, and the source of the 2 groups is unclear. | |
| Case‐control study: people with endocarditis (cases) who died were excluded, although the mortality rate in the cases was much higher (20%) than was likely in the control group, thus making the 2 groups incomparable. | |
| CCT, but participants not at high risk of endocarditis and no relevant outcomes measured | |
| Case‐control study: people with endocarditis (cases) who died were excluded, although the mortality rate in the cases was much higher (20%) than was likely in the control group, thus making the 2 groups incomparable. | |
| Case reports | |
| Cohort study of patients having dental extractions but all patients received antibiotics | |
| Letter on failures of prophylaxis on a case by case basis, not RCT, CCT, cohort or case‐control design | |
| Case reports | |
| Retrospective study of cases of endocarditis but no controls | |
| Serological study of bacteraemia following penicillin versus administration and tooth extraction | |
| Not an assessment of antibiotic prophylaxis (concerned with adjunctive use of antiseptic solution) | |
| Case series | |
| No at‐risk patients; examined serum levels of amoxicillin in healthy volunteers | |
| Case‐control study based in the USA of 273 hospital patients with endocarditis. Not all the cases (38%) or controls (6%) had a previously known risk of endocarditis. | |
| No dental interventions, and participants not at high risk of endocarditis | |
| Same group of patients as Tzukert 1986 | |
| Epidemiological study of endocarditis in the Netherlands, no controls | |
| Basic science research paper | |
| Cohort study of 17 patients undergoing dental extractions; all received antibiotics |
CCT: controlled clinical trial; RCT: randomised controlled trial
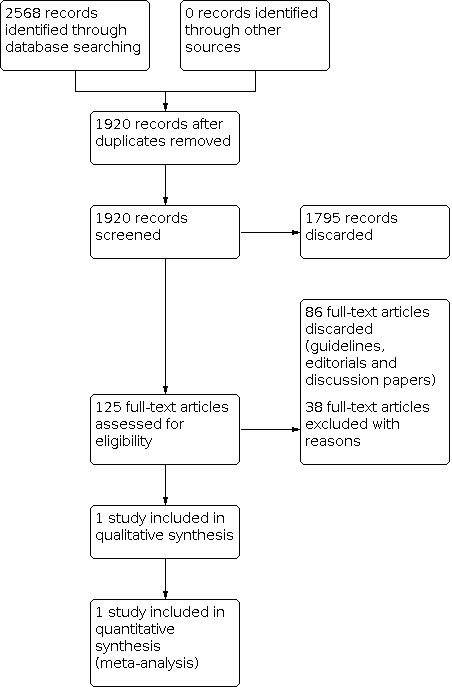
Study flow diagram

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
| Antibiotic prophylaxis compared with no antibiotic prophylaxis for the prevention of bacterial endocarditis in dentistry | ||||
| Population: adults or children at risk of endocarditis Setting: dental setting Intervention: antibiotic prophylaxis Comparison: no antibiotic prophylaxis | ||||
| Outcome | Results | No of participants | Certainty of the evidence | Comments |
|---|---|---|---|---|
| Mortality or serious adverse events requiring hospitalisation | No data reported | 248 (1 study) | ‐ | ‐ |
| Development of endocarditis (in those with definite indication for prophylaxis) | There was no difference in the number of people (with a definitive indication for prophylaxis) who developed endocarditis between those receiving prophylaxis and those not receiving prophylaxis (OR 1.62; 95% CI 0.57 to 4.57). | 248 (1 study) | ⊕⊝⊝⊝ | ‐ |
| Adverse effects of antibiotics | No data reported | 248 (1 study) | ‐ | ‐ |
| CI: confidence interval; OR: odds ratio | ||||
| GRADE Working Group grades of evidence | ||||
| aDowngraded 3 levels for high risk of bias and serious imprecision. | ||||

