Mosquiteros tratados con insecticida para la prevención del paludismo en el embarazo
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Cluster randomized controlled trial: 96 clusters, 48 per group Generation of allocation sequence and allocation concealment: determined by "open ballot of community leaders" Blinding: open Inclusion of randomized participants in analysis: 1806/1961 (92%) had blood taken in the third trimester for malaria and haemoglobin outcomes; 847/1961 (43%) had pregnancy outcomes reported | |
| Participants | 1961 pregnant women (1033 intervention and 928 control) of any parity who had attended the study clinic at least once | |
| Interventions | 1. ITNs 2. No nets | |
| Outcomes | 1. Malaria infection | |
| Notes | Location: living compounds in Kassena‐Nankana district, Ghana Date: June 1994 to April 1995 Malaria transmission: hyperendemic and perennial with peaks in the rainy season Trial assessed the impact of ITN use on malaria and anaemia in pregnancy as a supplementary study in a major cluster randomized trial of bed nets supported by WHO/TDR Active surveillance was used to track all deliveries of the recruited women, but this had to be abandoned in favour of passive surveillance after 6 months because of resource constraints | |
| Methods | Browne 2001 results for women in first pregnancy during the dry season | |
| Participants | — | |
| Interventions | — | |
| Outcomes | — | |
| Notes | — | |
| Methods | Browne 2001 results for women in first pregnancy during the wet season | |
| Participants | — | |
| Interventions | — | |
| Outcomes | — | |
| Notes | — | |
| Methods | Browne 2001 results for women in second pregnancy during the dry season | |
| Participants | — | |
| Interventions | — | |
| Outcomes | — | |
| Notes | — | |
| Methods | Browne 2001 results for women in second pregnancy during the wet season | |
| Participants | — | |
| Interventions | — | |
| Outcomes | — | |
| Notes | — | |
| Methods | Browne 2001 results for women in third or greater pregnancy during the dry season | |
| Participants | — | |
| Interventions | — | |
| Outcomes | — | |
| Notes | — | |
| Methods | Browne 2001 results for in third or greater pregnancy during the wet season | |
| Participants | — | |
| Interventions | — | |
| Outcomes | — | |
| Notes | — | |
| Methods | Individual randomized controlled trial Generation of allocation sequence and allocation concealment: states "randomized", but the methods not described Blinding: ITNs versus untreated nets comparison double blind (participants, antenatal clinic staff, and supervising physician) Inclusion of randomized participants in analysis: of 223 enrolled into ITN and untreated groups 203 (91%) completed | |
| Participants | Pregnant women of all parity 341 women enrolled; 34 were excluded from the analysis because they either delivered within 2 weeks of enrolment or were lost to follow up | |
| Interventions | 1. ITNs 2. Untreated nets 3. No study nets, but some women in this group had their own family‐size untreated nets supplied by the Consortium of Christian Relief Organizations and Interaid Additional interventions: women with uncomplicated Plasmodium falciparum were treated with quinine sulphate (30 mg salt/kg/d in 3 divided doses for 7 d), and Plasmodium vivax infections with chloroquine (25 mg/kg base over 3 d); severe cases of P. falciparum were treated with intravenous quinine in a local hospital | |
| Outcomes | 1. Malaria infection during pregnancy | |
| Notes | Location: 3 camps (Shoklo, Bonoklo, and Maesalit) for displaced people of the Karen ethnic minority, Thailand Date: recruitment between October 1990 and September 1992 Malaria transmission: mesoendemic with estimated attack rates of 1.0/year in the under 10 years age group and 0.8/year in older children and adults In the published results the 'no study nets group' was split into those who had no nets and those who had received nets from the charity: we felt the validity of the no study nets control group was compromised and decided to use data only on the treated versus untreated nets comparison | |
| Methods | Individual randomized controlled trial Generation of allocation sequence: enrolled women randomized into the 4 arms in blocks of 12 using computer‐generated random numbers; randomization numbers were prepared before the trial started and kept at each recruitment centre until the end of the trial Allocation concealment: method not described Blinding: open for ITNs versus no nets comparison; double blind for sulfadoxine‐pyrimethamine versus sulfadoxine‐pyrimethamine placebo comparison Inclusion of randomized participants in analysis: 963 women were recruited, out of which 752 (78%) were followed up to completion | |
| Participants | Women in their first or second pregnancy | |
| Interventions | 1. ITNs plus sulfadoxine‐pyrimethamine Net size (cm): 190 wide by 180 long by 150 high | |
| Outcomes | 1. Malaria infection | |
| Notes | Location: Bondo District Nyanza province, Kenya Date: July 1997 to September 1999 Malaria transmission: perennial with 2 peaks coinciding with the rainy seasons with 90 to 400 infective bites per person annually | |
| Methods | Njagi 2002 results for ITNs nets plus sulfadoxine‐pyrimethamine versus no nets plus sulfadoxine‐pyrimethamine | |
| Participants | — | |
| Interventions | — | |
| Outcomes | — | |
| Notes | — | |
| Methods | Njagi 2002 results for ITNs plus placebo versus placebo | |
| Participants | ||
| Interventions | — | |
| Outcomes | — | |
| Notes | — | |
| Methods | Cluster randomized controlled trial: 56 clusters (28:28) each of approximately 1000 individuals Generation of allocation sequence and allocation concealment: determined by "open ballot "; information received via personal communication from Christian Lengeler Blinding: open Inclusion of randomized participants in analysis: of 503 recruited 462 (91.8%) had third trimester blood sample, 130 (25.8%) delivered in hospital, and 497 (98.8%) followed up at least 4 weeks after delivery | |
| Participants | 503 women pregnant for the first time with singleton pregnancies or history of previous pregnancy that did not go beyond 12 weeks | |
| Interventions | 1. ITNs 2. No nets Additional interventions: all women with haemoglobin < 10 g/dL were given haematins and those with a positive slide for malaria were treated with sulfadoxine‐pyrimethamine; all women with severe anaemia also given sulfadoxine‐pyrimethamine irrespective of the results of their malaria smear, based on the assumption that those with negative smear would be likely to have placental parasitaemia Sufficient nets provided for all members of randomized households | |
| Outcomes | 1. Malaria infection | |
| Notes | Location: resident in rural populations Kilifi District, Kenya Date: September 1994 to November 1995 Malaria transmission: endemic and perennial with peaks in the 2 rainy seasons with individuals on average receiving 10 infective bites per person per year (ranging from 1 every 2 years to nearly 60 per person per year) The trial recruited pregnant women who came from a rural population that had already been randomized to receiving or not receiving nets treated with permethrin (500 g/m2) as part of a trial assessing the effect of ITNs on childhood mortality and severe malaria in children; randomization and distribution of nets had been finished by August 1993, and this study was conducted between September 1994 and November 1995 | |
| Methods | Cluster randomized controlled trial 79 villages: 60 villages described as 'non cohort' with delivery data only, and 19 villages described as 'cohort' with outcomes collected prior to delivery and at delivery Generation of allocation sequence and allocation concealment: "open lottery" Blinding: open Inclusion of randomized participants in analysis: birth outcomes for 2754/2991 (92%); minimum of 764/780 (98%) included in analysis of outcomes assessing the impact of nets during pregnancy | |
| Participants | 2991 pregnant women of all parity | |
| Interventions | 1. ITNs 2. No nets | |
| Outcomes | 1. Malaria infection | |
| Notes | Location: Rarieda Division (Asebo), Siaya district, Kenya Malarial transmission: intense perennial transmission with 60 to 300 infected bites per person annually with peaks in the 3 rainy seasons Conducted within the context of a large community‐based randomized controlled trial designed to assess the impact of ITNs on mortality in children < 5 years of age. The mortality in children trial consisted of two main sites, Asebo and Gem, but the study on the impact of ITNs in pregnancy was conducted in Asebo area only (200 km2). The trial involved randomizing villages to the intervention group, in which all households received ITNs during the fourth quarter of 1996 or control group which received ITNs in April 1999 after the trial was completed | |
| Methods | ter Kuile 2003 results for women in their first to fourth pregnancy | |
| Participants | — | |
| Interventions | — | |
| Outcomes | — | |
| Notes | — | |
| Methods | ter Kuile 2003 results for women in their fifth or greater pregnancy | |
| Participants | — | |
| Interventions | — | |
| Outcomes | — | |
| Notes | — | |
ITN: insecticide‐treated net; WHO/TDR: World Health Organization/United Nations Development Programme (UNDP)/World Bank/WHO Special Programme for Research and Training in Tropical Diseases.
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| 1. Cluster randomized trial that did not adjust for clustering in the analysis |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe anaemia Show forest plot | 4 | Various (Fixed, 95% CI) | Subtotals only | |
| Analysis 1.1  Comparison 1 Insecticide‐treated nets versus no nets, Outcome 1 Severe anaemia. | ||||
| 1.1 Odds ratio (third trimester) | 2 | Various (Fixed, 95% CI) | 0.77 [0.56, 1.08] | |
| 1.2 Risk ratio (at delivery) | 2 | Various (Fixed, 95% CI) | 0.98 [0.63, 1.52] | |
| 1.3 Hazard ratio | 2 | Various (Fixed, 95% CI) | 0.89 [0.61, 1.31] | |
| 2 Any anaemia Show forest plot | 5 | Various (Random, 95% CI) | Subtotals only | |
| Analysis 1.2  Comparison 1 Insecticide‐treated nets versus no nets, Outcome 2 Any anaemia. | ||||
| 2.1 Odds ratio (third trimester) | 1 | Various (Random, 95% CI) | 0.88 [0.71, 1.10] | |
| 2.2 Odds ratio (at delivery) | 2 | Various (Random, 95% CI) | 0.95 [0.50, 1.79] | |
| 2.3 Hazard ratio | 2 | Various (Random, 95% CI) | 0.90 [0.71, 1.13] | |
| 3 Haemoglobin (g/L) Show forest plot | 11 | Mean difference (Random, 95% CI) | Subtotals only | |
| Analysis 1.3  Comparison 1 Insecticide‐treated nets versus no nets, Outcome 3 Haemoglobin (g/L). | ||||
| 3.1 Third trimester: first or second pregnancy | 5 | Mean difference (Random, 95% CI) | ‐0.04 [‐2.41, 2.33] | |
| 3.2 Third trimester: third or greater pregnancy | 3 | Mean difference (Random, 95% CI) | 0.30 [‐3.38, 3.97] | |
| 3.3 At delivery: first or second pregnancy | 3 | Mean difference (Random, 95% CI) | 1.95 [‐2.61, 6.51] | |
| 4 Low birthweight Show forest plot | 4 | Various (Fixed, 95% CI) | 0.80 [0.64, 1.00] | |
| Analysis 1.4  Comparison 1 Insecticide‐treated nets versus no nets, Outcome 4 Low birthweight. | ||||
| 4.1 Risk ratio: first or second pregnancy | 3 | Various (Fixed, 95% CI) | 0.77 [0.61, 0.98] | |
| 4.2 Risk ratio: fifth or greater pregnancy | 1 | Various (Fixed, 95% CI) | 1.12 [0.56, 2.24] | |
| 5 Birthweight (kg) Show forest plot | 10 | Mean difference (Fixed, 95% CI) | 0.06 [0.02, 0.09] | |
| Analysis 1.5  Comparison 1 Insecticide‐treated nets versus no nets, Outcome 5 Birthweight (kg). | ||||
| 5.1 First or second pregnancy | 8 | Mean difference (Fixed, 95% CI) | 0.05 [0.02, 0.09] | |
| 5.2 Third or greater pregnancy | 2 | Mean difference (Fixed, 95% CI) | 0.08 [‐0.13, 0.28] | |
| 6 Clinical malaria illness during pregnancy Show forest plot | 2 | Various (Fixed, 95% CI) | Totals not selected | |
| Analysis 1.6  Comparison 1 Insecticide‐treated nets versus no nets, Outcome 6 Clinical malaria illness during pregnancy. | ||||
| 6.1 Odds ratio | 1 | Various (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Hazard ratio | 1 | Various (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Peripheral parasitaemia Show forest plot | 6 | Various (Fixed, 95% CI) | Subtotals only | |
| Analysis 1.7  Comparison 1 Insecticide‐treated nets versus no nets, Outcome 7 Peripheral parasitaemia. | ||||
| 7.1 Odds ratio: third trimester | 2 | Various (Fixed, 95% CI) | 0.88 [0.73, 1.06] | |
| 7.2 Risk ratio: at delivery | 4 | Various (Fixed, 95% CI) | 0.76 [0.67, 0.86] | |
| 7.3 Hazard ratio | 2 | Various (Fixed, 95% CI) | 0.67 [0.52, 0.86] | |
| 8 Parasite density Show forest plot | 8 | Geometric mean ratio (Fixed, 95% CI) | 0.93 [0.77, 1.11] | |
| Analysis 1.8  Comparison 1 Insecticide‐treated nets versus no nets, Outcome 8 Parasite density. | ||||
| 8.1 First or second pregnancy | 6 | Geometric mean ratio (Fixed, 95% CI) | 0.82 [0.66, 1.02] | |
| 8.2 Third or greater pregnancy | 2 | Geometric mean ratio (Fixed, 95% CI) | 1.28 [0.90, 1.82] | |
| 9 Placental parasitaemia Show forest plot | 5 | Risk Ratio (Random, 95% CI) | 0.79 [0.63, 0.98] | |
| Analysis 1.9  Comparison 1 Insecticide‐treated nets versus no nets, Outcome 9 Placental parasitaemia. | ||||
| 9.1 First or second pregnancy | 4 | Risk Ratio (Random, 95% CI) | 0.82 [0.61, 1.11] | |
| 9.2 Fifth or greater pregnancy | 1 | Risk Ratio (Random, 95% CI) | 0.72 [0.48, 1.08] | |
| 10 Fetal loss Show forest plot | 5 | Risk Ratio (Fixed, 95% CI) | 0.68 [0.48, 0.98] | |
| Analysis 1.10  Comparison 1 Insecticide‐treated nets versus no nets, Outcome 10 Fetal loss. | ||||
| 10.1 First or second pregnancy | 4 | Risk Ratio (Fixed, 95% CI) | 0.67 [0.47, 0.97] | |
| 10.2 Fifth or greater pregnancy | 1 | Risk Ratio (Fixed, 95% CI) | 1.02 [0.17, 6.23] | |

Comparison 1 Insecticide‐treated nets versus no nets, Outcome 1 Severe anaemia.

Comparison 1 Insecticide‐treated nets versus no nets, Outcome 2 Any anaemia.
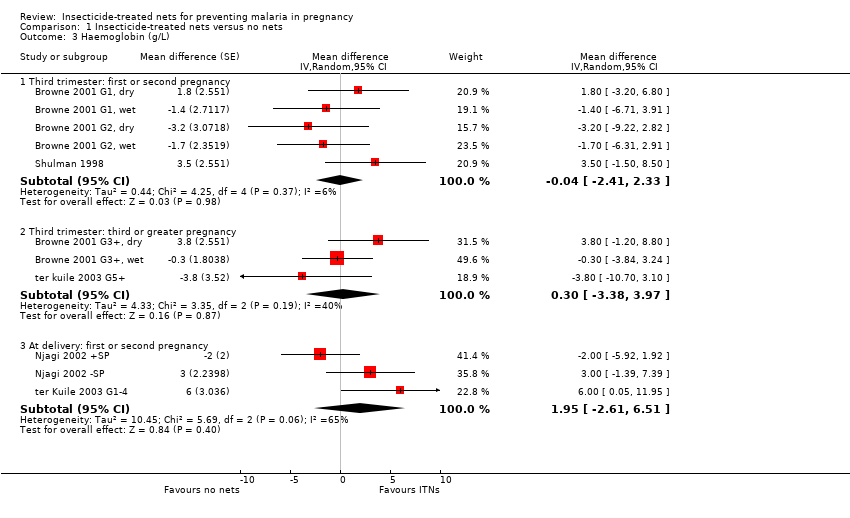
Comparison 1 Insecticide‐treated nets versus no nets, Outcome 3 Haemoglobin (g/L).
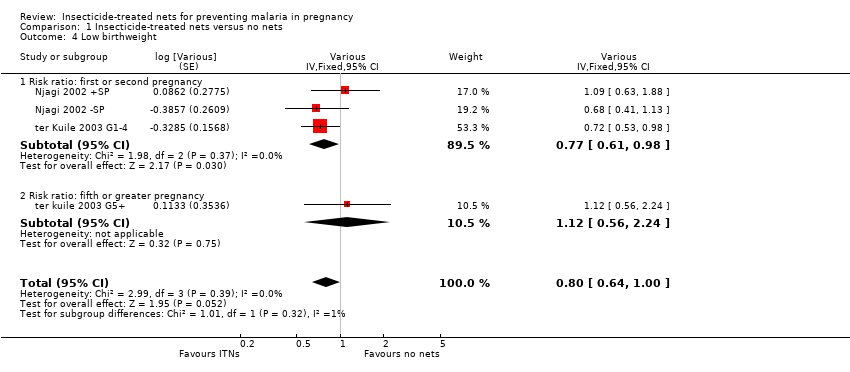
Comparison 1 Insecticide‐treated nets versus no nets, Outcome 4 Low birthweight.
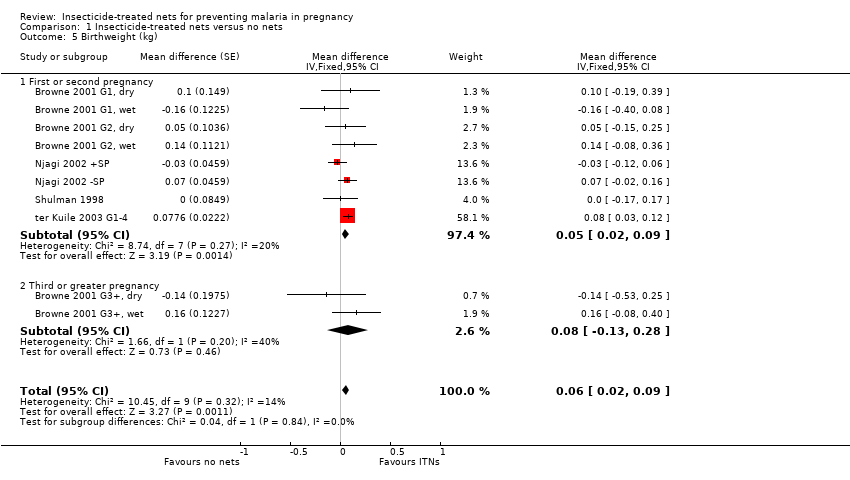
Comparison 1 Insecticide‐treated nets versus no nets, Outcome 5 Birthweight (kg).

Comparison 1 Insecticide‐treated nets versus no nets, Outcome 6 Clinical malaria illness during pregnancy.
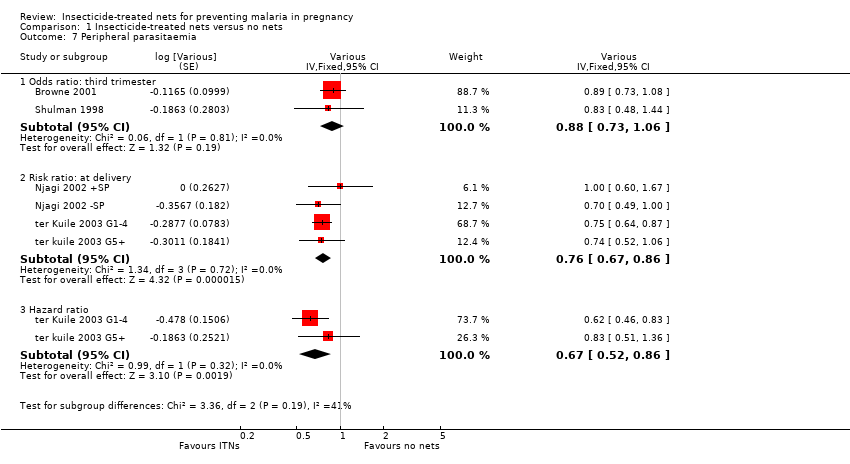
Comparison 1 Insecticide‐treated nets versus no nets, Outcome 7 Peripheral parasitaemia.

Comparison 1 Insecticide‐treated nets versus no nets, Outcome 8 Parasite density.

Comparison 1 Insecticide‐treated nets versus no nets, Outcome 9 Placental parasitaemia.

Comparison 1 Insecticide‐treated nets versus no nets, Outcome 10 Fetal loss.
| Search set | CIDG SRa | CENTRAL | MEDLINEb | EMBASEb | LILACSb |
| 1 | malaria | malaria | malaria | malaria | malaria |
| 2 | pregnan* | pregnan* | pregnan* | pregnan* | pregnan* |
| 3 | woman | woman | woman | woman | woman |
| 4 | women | women | women | women | women |
| 5 | 3 or 4 | 3 or 4 | 3 or 4 | 3 or 4 | 3 or 4 |
| 6 | 1 and 2 and 5 | 1 and 2 and 5 | 1 and 2 and 5 | 1 and 2 and 5 | 1 and 2 and 5 |
| 7 | net* | net* | net* | net* | net* |
| 8 | ITN* | ITN* | ITN* | ITN* | 6 and 7 |
| 9 | ITM* | ITM* | ITM* | ITM* | — |
| 10 | 7 or 8 or 9 | 7 or 8 or 9 | 7 or 8 or 9 | 7 or 8 or 9 | — |
| 11 | 6 and 10 | 6 and 10 | 6 and 10 | 6 and 10 | — |
| aCochrane Infectious Diseases Group Specialized Register. | |||||
| Trial | Generation of allocation sequence | Allocation concealment | Blinding | Inclusion of all randomized participants in the analysis |
| Method not described | Not described | Double blind (participants, antenatal clinic staff, and supervising physician) for ITNs versus untreated nets comparison | Adequate | |
| Adequate | Adequate | Open | Adequate for number with a third trimester blood sample Inadequate for number women who delivered in hospital Adequate for number followed up at least 4 weeks after delivery Adequate for number with a third trimester blood sample Inadequate for number women who delivered in hospital Adequate for number followed up at least 4 weeks after delivery | |
| Adequate | Adequate | Open | Adequate for number with blood taken in third trimester for malaria and haemoglobin Inadequate for number with pregnancy outcomes reported | |
| Adequate | Not described | Open for ITNs versus no nets comparison Double blind for sulfadoxine‐pyrimethamine (SP) versus SP placebo comparison Open for ITNs versus no nets comparison Double blind for sulfadoxine‐pyrimethamine (SP) versus SP placebo comparison | Inadequate for number evaluated at delivery | |
| Adequate | Adequate | Open | Adequate number for birth outcomes and analysis of outcomes assessing the impact of nets during pregnancy | |
| aDetails of methods used in individual trials are in the 'Characteristics of included studies'. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe anaemia Show forest plot | 4 | Various (Fixed, 95% CI) | Subtotals only | |
| 1.1 Odds ratio (third trimester) | 2 | Various (Fixed, 95% CI) | 0.77 [0.56, 1.08] | |
| 1.2 Risk ratio (at delivery) | 2 | Various (Fixed, 95% CI) | 0.98 [0.63, 1.52] | |
| 1.3 Hazard ratio | 2 | Various (Fixed, 95% CI) | 0.89 [0.61, 1.31] | |
| 2 Any anaemia Show forest plot | 5 | Various (Random, 95% CI) | Subtotals only | |
| 2.1 Odds ratio (third trimester) | 1 | Various (Random, 95% CI) | 0.88 [0.71, 1.10] | |
| 2.2 Odds ratio (at delivery) | 2 | Various (Random, 95% CI) | 0.95 [0.50, 1.79] | |
| 2.3 Hazard ratio | 2 | Various (Random, 95% CI) | 0.90 [0.71, 1.13] | |
| 3 Haemoglobin (g/L) Show forest plot | 11 | Mean difference (Random, 95% CI) | Subtotals only | |
| 3.1 Third trimester: first or second pregnancy | 5 | Mean difference (Random, 95% CI) | ‐0.04 [‐2.41, 2.33] | |
| 3.2 Third trimester: third or greater pregnancy | 3 | Mean difference (Random, 95% CI) | 0.30 [‐3.38, 3.97] | |
| 3.3 At delivery: first or second pregnancy | 3 | Mean difference (Random, 95% CI) | 1.95 [‐2.61, 6.51] | |
| 4 Low birthweight Show forest plot | 4 | Various (Fixed, 95% CI) | 0.80 [0.64, 1.00] | |
| 4.1 Risk ratio: first or second pregnancy | 3 | Various (Fixed, 95% CI) | 0.77 [0.61, 0.98] | |
| 4.2 Risk ratio: fifth or greater pregnancy | 1 | Various (Fixed, 95% CI) | 1.12 [0.56, 2.24] | |
| 5 Birthweight (kg) Show forest plot | 10 | Mean difference (Fixed, 95% CI) | 0.06 [0.02, 0.09] | |
| 5.1 First or second pregnancy | 8 | Mean difference (Fixed, 95% CI) | 0.05 [0.02, 0.09] | |
| 5.2 Third or greater pregnancy | 2 | Mean difference (Fixed, 95% CI) | 0.08 [‐0.13, 0.28] | |
| 6 Clinical malaria illness during pregnancy Show forest plot | 2 | Various (Fixed, 95% CI) | Totals not selected | |
| 6.1 Odds ratio | 1 | Various (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Hazard ratio | 1 | Various (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Peripheral parasitaemia Show forest plot | 6 | Various (Fixed, 95% CI) | Subtotals only | |
| 7.1 Odds ratio: third trimester | 2 | Various (Fixed, 95% CI) | 0.88 [0.73, 1.06] | |
| 7.2 Risk ratio: at delivery | 4 | Various (Fixed, 95% CI) | 0.76 [0.67, 0.86] | |
| 7.3 Hazard ratio | 2 | Various (Fixed, 95% CI) | 0.67 [0.52, 0.86] | |
| 8 Parasite density Show forest plot | 8 | Geometric mean ratio (Fixed, 95% CI) | 0.93 [0.77, 1.11] | |
| 8.1 First or second pregnancy | 6 | Geometric mean ratio (Fixed, 95% CI) | 0.82 [0.66, 1.02] | |
| 8.2 Third or greater pregnancy | 2 | Geometric mean ratio (Fixed, 95% CI) | 1.28 [0.90, 1.82] | |
| 9 Placental parasitaemia Show forest plot | 5 | Risk Ratio (Random, 95% CI) | 0.79 [0.63, 0.98] | |
| 9.1 First or second pregnancy | 4 | Risk Ratio (Random, 95% CI) | 0.82 [0.61, 1.11] | |
| 9.2 Fifth or greater pregnancy | 1 | Risk Ratio (Random, 95% CI) | 0.72 [0.48, 1.08] | |
| 10 Fetal loss Show forest plot | 5 | Risk Ratio (Fixed, 95% CI) | 0.68 [0.48, 0.98] | |
| 10.1 First or second pregnancy | 4 | Risk Ratio (Fixed, 95% CI) | 0.67 [0.47, 0.97] | |
| 10.2 Fifth or greater pregnancy | 1 | Risk Ratio (Fixed, 95% CI) | 1.02 [0.17, 6.23] | |

