Entrenamiento de integración auditiva y otras terapias de sonido para trastornos del espectro autista (TEA)
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Randomised controlled trial. Randomisation by random numbers table | |
| Participants | Diagnosis: autism or Asperger syndrome diagnosed by an independent agency | |
| Interventions | 1. AIT: 2 30min sessions for 10 consecutive days | |
| Outcomes | Standardised tests assessing behaviour, sensory measures and cognitive ability (see outcomes table) | |
| Notes | No loss to follow‐up | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Personal communication with study author (Bettison 2002): "a table of random numbers was used to allocate each child to either condition A or B." |
| Allocation concealment (selection bias) | High risk | Inadequate following communication with study author (Bettison 2002) |
| Incomplete outcome data (attrition bias) | Low risk | No participant withdrawal |
| Selective reporting (reporting bias) | Low risk | Study protocol not available. Pre‐specified outcomes described in methods are reported in results |
| Other bias | Unclear risk | Financial support from the Commonwealth Department of Health, Housing and Community Services, an Apex Trust for Autism Grant and the Autistic Association of New South Wales |
| Blinding of participants and personnel (performance bias) | Low risk | Investigators not blinded. Personal communication with study author (Bettison 2002): blinding not possible as they needed to set and administer treatment. Parents and teachers unaware of which treatment each child was receiving |
| Blinding of outcome assessment (detection bias) | Low risk | Outcomes assessors blinded |
| Methods | Randomised controlled trial (cross‐over) | |
| Participants | Diagnosis: autistic disorder based on DSM‐IV criteria, Autism Diagnostic Observation Schedule‐Generic (ADOS‐G) and clinical judgement Age: 3‐7 years n=11 | |
| Interventions | 1. Tomatis Method: filtered music, "Electronic Ear" headphone, auditory feedback, specially produced compact discs of Mozart and Gregorian chants 4 three‐week treatment blocks, total duration: 18 weeks 2. Placebo: commercially produced Mozart and Gregorian chant compact discs, no active microphone or "Electronic Ear", schedule as for treatment group | |
| Outcomes | Standardised tests assessing core features of autism, cognitive ability and language | |
| Notes | No loss to follow‐up | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation table provided by a independent statistician (personal communication with study author) |
| Allocation concealment (selection bias) | Low risk | Sequence table held in a sealed envelope in locked filing cabinet until study completion |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | The outcomes listed in the methods are reported in the results |
| Other bias | High risk | The authors report that "although the participants were randomly assigned to the groups, the developmental level appeared to be different for each in that the placebo/treatment group was higher functioning than the treatment/placebo group." The study was a crossover design and it is unclear whether there was sufficient washout between each treatment period |
| Blinding of participants and personnel (performance bias) | Low risk | Parents blinded until conclusion of the study. Individuals administering the music were not blinded but were not affiliated with the M.I.N.D. institute (Corbett 2011) |
| Blinding of outcome assessment (detection bias) | Low risk | M.I.N.D. institute researchers remained blind until the conclusion of the study |
| Methods | Randomised controlled trial. Randomisation based on telephone number | |
| Participants | Diagnosis: autism | |
| Interventions | 1. AIT 2 30‐min sessions for 10 consecutive days | |
| Outcomes | Standardised tests assessing behaviour, auditory problems, electrophysiological recordings (P300 ERP) | |
| Notes | Data from 1 control participant excluded due to no match in the AIT group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation based on telephone number |
| Allocation concealment (selection bias) | High risk | Inadequate, following communication with the author (Edelson 2002 (pers comm)) |
| Incomplete outcome data (attrition bias) | Unclear risk | Nil loss to follow‐up but results for one patient in the control group were not used as analyses were based on matched pairs. Only 5 participants able to complete electrophysiological tasks and audiometric assessments due to poor language and attention skills |
| Selective reporting (reporting bias) | High risk | Total scores presented for Aberrant Behaviour Checklist only |
| Other bias | Unclear risk | "A comparison of the pre‐assessment total scores (reflecting the number of behavioural or auditory problems) was conducted for all three questionnaires and indicated no a priori significant differences between the experimnetal (AIT) and the placebo groups)" however no raw data is provided Partial funding support provided by the Nancy Lurie Marks Charitable Trust |
| Blinding of participants and personnel (performance bias) | Low risk | Investigator provided processed or unprocessed music to each participant but "did not interact with parents, guardians or participants after group assignment was determined". Parents and guardians unaware of the group to which participants were assigned |
| Blinding of outcome assessment (detection bias) | Low risk | Evaluators unaware of group assignment for participants |
| Methods | Randomised controlled trial (cross‐over) Methods: geographically divided into groups, then into subgroups alphabetically by the first letter of their name | |
| Participants | Diagnosis: autism (DSM4 or ICD10) | |
| Interventions | 1. AIT: 2 30min sessions for 10 consecutive days | |
| Outcomes | Standardised tests assessing behaviour, language and cognitive ability, parental reports, observations by investigators | |
| Notes | 5 lost to follow‐up due to lack of cooperation, safety issues, transport problems | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Participants geographically divided into groups, then into subgroups alphabetically by the first letter of their name |
| Allocation concealment (selection bias) | High risk | Inadequate, following communication with the author (Mudford 2002 (pers comm)) |
| Incomplete outcome data (attrition bias) | High risk | 5 of 21 participants (24%) lost to follow‐up due to lack of cooperation, safety issues, transport problems |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes described in methods are reported in results |
| Other bias | Low risk | Funded by a research grant from National Health Service Research and Development Programme for People with Physical and Complex Disabilities. Treatment providers (who assisted with the study) from Honormead Schools have ceased to provide auditory integration training |
| Blinding of participants and personnel (performance bias) | Low risk | Investigators blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Outcomes assessors blinded |
| Methods | Randomised controlled trial. Randomised by last 2 digits of their telephone number | |
| Participants | Diagnosis: autism | |
| Interventions | 1. AIT: 2 30 min sessions for 10 consecutive days | |
| Outcomes | Standardised tests of behaviour, auditory problems | |
| Notes | 1 lost to follow‐up due to transport problems | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation sequence based on last 2 digits of telephone number |
| Allocation concealment (selection bias) | High risk | Inadequate, following communication with the author (Edelson 2002 (pers comm)) |
| Incomplete outcome data (attrition bias) | Low risk | 1 lost to follow‐up due to transport problems |
| Selective reporting (reporting bias) | Low risk | The outcomes listed in the methods are reported in the results |
| Other bias | Unclear risk | "Funding was provided in part by the Adriana Foundation and the Alex Kunin Fund." |
| Blinding of participants and personnel (performance bias) | Low risk | Parents were blinded. Investigators not blinded as they were required to set and administer treatment. Investigators did not conduct pre‐ or post‐assessments |
| Blinding of outcome assessment (detection bias) | Low risk | Outcomes assessors blinded |
| Methods | Randomised controlled trial. Randomised by last 2 digits of their telephone number | |
| Participants | Diagnosis: autism | |
| Interventions | 1. AIT 2 30min sessions for 10 consecutive days | |
| Outcomes | Standardised tests of behaviour, auditory problems | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation sequence based on last 2 digits of telephone number |
| Allocation concealment (selection bias) | High risk | Inadequate |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | High risk | Total scores presented for Aberrant Behaviour Checklist only |
| Other bias | Unclear risk | Funding source for study not stated. Subjects were matched for age, sex and language level however raw data were not provided |
| Blinding of participants and personnel (performance bias) | Low risk | Parents unaware of treatment assignment of their child until completion of study. The investigator assigned children to groups and administered the therapy but did not conduct evaluations |
| Blinding of outcome assessment (detection bias) | Low risk | Outcomes assessors blinded |
| Methods | Randomised controlled trial. Randomised using a random numbers table | |
| Participants | Diagnosis: cognitive impairment including autism spectrum disorder. Age: 7‐24 years | |
| Interventions | 1. AIT 2 30 min sessions for 10 consecutive days 2. Control: as above but music unmodified | |
| Outcomes | Standardised tests of behaviour, sound sensitivity, measurement of pure tone thresholds | |
| Notes | 28 analysed for ABC at 9mths | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table |
| Allocation concealment (selection bias) | High risk | Inadequate, following communication with study author (Zollweg 2002 (pers comm)) |
| Incomplete outcome data (attrition bias) | Unclear risk | 2 patients lost to follow‐up (1 from each group) prior to completion of study. There were fewer participants for audiological and sound sensitivity data due to illness or poor cooperation |
| Selective reporting (reporting bias) | Low risk | The outcomes listed in the methods are reported in the results |
| Other bias | Unclear risk | Treatment group included 9 cognitively impaired and 6 autistic patients, control group included 12 cognitively impaired and 3 autistic patients. Correspondence with author confirmed that all participants had been diagnosed with autism |
| Blinding of participants and personnel (performance bias) | Low risk | Investigators blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Outcomes assessors blinded |
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Not a randomised controlled trial (RCT). | |
| Not a randomised controlled trial (RCT). | |
| Not RCT. | |
| A controlled trial involving measurement of event‐related brain potentials elicited by auditory stimuli (ie not AIT or sound therapy). Control group involved normal participants. | |
| A controlled trial involving "reduced auditory input" for autistic children rather than AIT or sound therapy. | |
| Individuals with autistic disorder received AIT, however there was no control group. | |
| A controlled trial which did not involve AIT or sound therapy. Participants in control group were not autistic. | |
| A controlled trial involving 'Virtual Reality' technologies rather than AIT or sound therapy. Control group were non‐autistic children. | |
| A controlled trial which did not involve AIT or sound therapy. Participants in control group were not autistic. | |
| A study that did not involve AIT or sound therapy and was not a RCT. | |
| AIT administered to individuals with autism, however there was no control group. Control group data from a previous study were used. | |
| A RCT involving an 'auditory trainer' for autistic children rather than AIT or sound therapy. | |
| A controlled trial which did not involve AIT or sound therapy. Participants in control group were not autistic. | |
| A randomised controlled trial involving AIT administered to children with central auditory processing disorders. Children with autism spectrum disorders were excluded. |
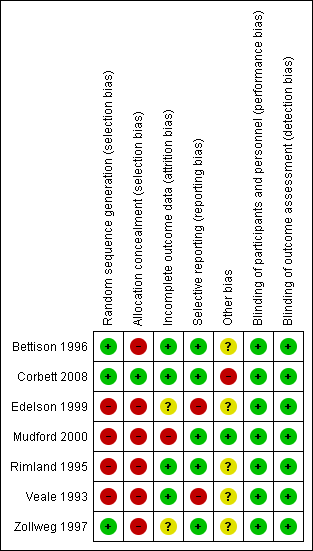
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
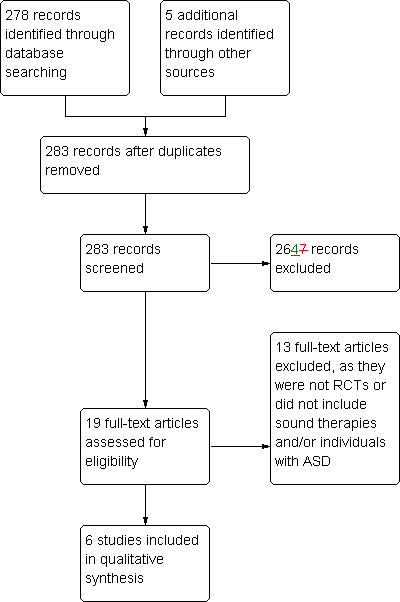
Study flow diagram: original search 2002
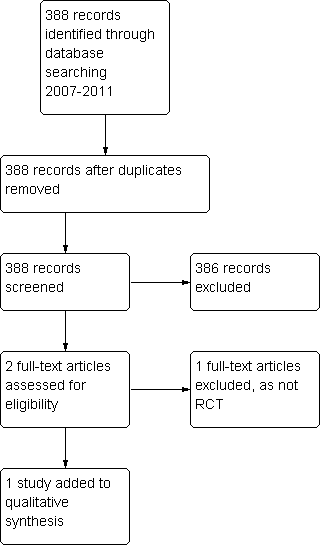
Study flow diagram for 2011 review update
| Outcome measure | Veale 1993 | Rimland 1995 | Bettison 1996 | Zollweg 1997 | Edelson 1999 | Mudford 2000 | Corbett 2008 |
| Aberrant Behaviour Checklist | ✔* | ✔* |
| ✔*** | ✔* | ✔*,** |
|
| Developmental Behaviour Checklist: parent, teacher (Einfeld 1995) |
|
| ✔ |
|
|
|
|
| Autism Behaviour Checklist |
|
| ✔ |
|
|
|
|
| Conners' Rating Scales ‐ Parent | ✔ |
|
|
| ✔ |
|
|
| Nisonger Child Behaviour Rating Form ‐ Parent |
|
|
|
|
| ✔ |
|
| Fisher's Auditory Problems Checklist ‐ Parent | ✔ | ✔ |
|
| ✔ |
|
|
| Leiter International Performance Scale |
|
| ✔ |
|
| ✔ |
|
| Peabody Picture Vocabulary test |
|
| ✔† |
|
|
| ✔‡ |
| Vineland Adaptive Behaviour Scores |
|
|
|
|
| ✔ |
|
| Reynell Language Developmental Scales III: a) expressive language b) comprehension |
|
|
|
|
| ✔ |
|
| Sensory problems checklist |
|
| ✔ |
|
|
|
|
| Hearing sensitivity questionnaire (HSQ) |
| ✔ |
|
|
|
|
|
| Sound sensitivity questionnaire (version of HSQ) |
|
| ✔ |
|
|
|
|
| Pure tone discomfort test |
| ✔ |
| ✔ |
|
|
|
| Ear occlusion |
|
|
|
|
| ✔ |
|
| P300 event‐related brain potentials |
|
|
|
| ✔ |
|
|
| Loudness discomfort levels |
|
|
| ✔ |
|
|
|
| Autism Diagnostic Observation Schedule‐Generic |
|
|
|
|
|
| ✔ |
| Stanford‐Binet Intelligence Scale‐Fourth Edition |
|
|
|
|
|
| ✔ |
| Expressive One Word Vocabulary Test |
|
|
|
|
|
| ✔ |
| * parent, ** teacher, *** other, † L, M forms, ‡third edition | |||||||
| Outcome | Trial | Tool(s) | Duration of follow‐up | Between group difference |
| Behaviour problems | Bettison 1996 | Autism Behaviour Checklist, Developmental Behaviour Checklist | 12 months | Improved both groups Not significant |
| Edelson 1999 | Aberrant Behaviour Checklist ABC)†, Fisher's Auditory Problems Checklist (FAPC), Conners' Rating Scales ‐ Parent | 3 months | Not significant for FAPC and Conners' Rating Scales, significant improvement for ABC for AIT group | |
| Mudford 2000 | Aberrant Behaviour Checklist‡, Nisonger Child Behaviour Rating Form ‐ Parent, observations from parents | 14 months | No significant improvement for combined behavioural data | |
| Rimland 1995 | Aberrant Behaviour Checklist‡, Fisher's Auditory Problems Checklist | 3 months | Significant improvement for AIT group for both tools (including 4 of 5 subscales of ABC) | |
| Veale 1993 | Fisher's Auditory Problems Checklist, Conners' Rating Scales ‐ Parent, Aberrant Behaviour Checklist† | 3 months | Not significant for all tools. | |
| Zollweg 1997 | Aberrant Behaviour Checklist‡ | 9 months | Improved both groups (including each ABC subscale) Not significant | |
| Cognitive ability | Mudford 2000 | Leiter International Performance Scale and Vineland Adaptive Behaviour Scores | 14 months | Neither group improved for all tools |
| Bettison 1996 | Leiter International Performance Scale | 12 months | Both groups improved | |
| Corbett 2008 | Stanford‐Binet Intelligence Scale ‐ Fourth Edition | 9 months | Not applicable | |
| Sound sensitivity | Zollweg 1997 | "Loudness discomfort levels" | 9 months | Not significant |
| Bettison 1996 | Sound sensitivity questionnaire | 12 months | Not significant. Improved both groups | |
| Rimland 1995 | Hearing sensitivity questionnaire and a "Pure Tone Discomfort test" | 3 months | Neither group improved | |
| Listening and comprehension | Rimland 1995 | Subgroup of Fisher's Auditory Problems Checklist | 3 months | Significant improvement for AIT group |
| Language | Corbett 2008 | Peabody Picture Vocabulary test, Expressive One Word Vocabulary Test | 9 months | Not significant for both tools |
| Bettison 1996 | Peabody Picture Vocabulary test | 12 months | Not significant | |
| Adverse events | Bettison 1996 | Parental questionnaire (non‐standardised) | 12 months | Not significant |
| Rimland 1995 | Parental questionnaire | 3 months | Not significant | |
| † Total scores presented for Aberrant Behaviour Checklist only, ‡ Total and subgroup scores for Aberrant Behaviour Checklist presented | ||||

