Intervenciones para el tratamiento de la colitis colágena
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Randomized, double‐blind, placebo‐controlled. Duration of treatment was 8 weeks, plus an 8 week treatment‐free follow‐up, for a total of 16 weeks | |
| Participants | Patients (n = 28) aged > 18 years with clinically and histologically confirmed active collagenous colitis Clinical: minimum 3 semi‐loose or loose stools per day for at least 8 weeks, no other significant cause on history/physical, negative stool examination for pathogens, parasites, and C. difficile toxin and no macroscopic inflammation on colonoscopy (and no other endoscopic findings other than diverticulosis or diminutive polyps). Histological: subepithelial collagen band > 10 um thick and typical feathery appearance of the inferior border; increased mixed inflammatory cell infiltrate in lamina propria. Cases with overlapping features with lymphocytic colitis were allowed if the collagen band was a predominant finding Patients with significant gastrointestinal disease (except controlled gastroesophageal reflux disease and celiac disease on a long‐term gluten‐free diet) were excluded | |
| Interventions | Budesonide (Budenofalk) 9 mg/day (n = 14) versus placebo (n = 14) for 8 weeks | |
| Outcomes | Proportion of patients achieving clinical and/or histological response Clinical: reduction of stool frequency in last week of treatment by at least 50%. All patients kept a diary throughout the study period. Each patient underwent colonoscopy and standardized biopsy protocol pre‐ and post‐treatment | |
| Notes | Data from first 8 weeks of the study only were included in the analysis, as this was the duration of treatment with active drug or placebo. Five patients that failed to meet the inclusion criteria after being randomized into the trial (upon review of their stool diaries) were excluded from the analysis. Medications that could possibly affect stool frequency or the natural history of the disease were not allowed during the study and were discontinued (with an appropriate wash‐out period) before inclusion. Other chronic medications were allowed to be continued as long as the intake remained stable throughout the study period. 3 patients (2 placebo) dropped out of the study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of randomization was not described |
| Allocation concealment (selection bias) | Low risk | Randomization was done centrally by the company delivering the drugs and placebo |
| Blinding (performance bias and detection bias) | Unclear risk | Quote: "double‐blind" Quote: "All biopsies were randomly read by 2 blinded expert pathologists" |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "All calculations were made on an intention‐to‐treat basis" Quote: "Three patients dropped out of the study (2 placebo), one for noncompliance and 2 because of treatment failure" Intention‐to‐treat was followed for clinical response Intention‐to‐treat was not followed for histologic response (denominators of 13 and 12 for the treatment and placebo group respectively) |
| Selective reporting (reporting bias) | Low risk | All primary outcomes were reported. Time to clinical remission was not directly reported in text, but it was interpretable from one of their published figures (Figure 1) |
| Other bias | Low risk | Study appeared to be free of other forms of bias |
| Methods | Randomized, double‐blind, placebo‐controlled. Duration of study was 8 weeks. Stool frequency and stool weight was recorded pre‐ and immediately after stopping treatment. All patients underwent sigmoidoscopy with standardized biopsy protocol pre‐ and post‐treatment. Randomization was performed by the drug company. Medication and placebo were delivered prepackaged with consecutive randomized numbers | |
| Participants | Patients (n = 20, 16 females) aged > 18 years with clinically and histologically confirmed active collagenous colitis Clinical: > 4 stools/day and/or stool weight > 200 g/day averaged over 3 days pre‐treatment. Negative stool samples for pathogens, parasites, and ova. Histological: collagen layer > 10 um Inflammation was graded on a scale (0 to 3) independently by 2 pathologists Patients with other chronic gastrointestinal diseases were excluded, as were those with clinically significant renal or hepatic disease, those who had been treated with anti‐inflammatory drugs (aminosalicylates, corticosteroids, azathioprine) in the previous 3 months or were pregnant or breast feeding | |
| Interventions | Budesonide (9 mg/day for 4 weeks, 6 mg for 2 weeks and 3 mg for 2 weeks) versus placebo for 8 weeks | |
| Outcomes | Primary outcome was the proportion of patients that achieved a clinical or histological response Clinical: reduction of stool frequency and/or stool weight by > 50% | |
| Notes | No antiinflammatory drug treatment was allowed during the study period or for 3 months prior to inclusion. During the study antidiarrheal medications were allowed except during the periods of stool sampling. During these periods no other treatments with effects on the GI tract were allowed. NSAIDS were not permitted, but other chronic medications (e.g. ‐ antihypertensives) were allowed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described in published study |
| Allocation concealment (selection bias) | Low risk | Randomization was performed centrally by the drug company Medication and placebo were delivered prepackaged with consecutive randomized numbers |
| Blinding (performance bias and detection bias) | Low risk | Quote: "double‐blind" Quote: "The placebo medication was identical in appearance" Quote: "Histopathological evaluation was performed blindly by the two pathologists" |
| Incomplete outcome data (attrition bias) | Unclear risk | No description of dropouts or withdrawals |
| Selective reporting (reporting bias) | Low risk | The primary outcome of clinical remission was reported Histopathological changes were also described |
| Other bias | Low risk | Study appeared to be free of other forms of bias |
| Methods | Randomized, double‐blind, placebo‐controlled. Randomization was done with a computerized randomization program in blocks of 4 patients Induction: 6 weeks Maintenance: 24 weeks Treatment‐free follow‐up: 24 weeks | |
| Participants | Patients (n = 42) aged > 18 years with clinically (> 3 stools/day over 3 days registration) and histologically (subepithelial collagen layer with a thickness > 10 um, inflammation of the lamina propria, and a lymphocytic infiltrate of the epithelium) confirmed active collagenous colitis plus negative faecal cultures for intestinal pathogens Induction: n = 42 Maintenance: n = 34, 17 in each arm Follow‐up: n = 15, 13 in the budesonide arm and 2 in the placebo arm Patients were excluded if they had been treated with salazopyrine, 5‐aminosalicylic acid, budesonide or a systemic glucocorticoid within 3 months of trial enrolment or treated with ketoconazole during the 7 days before random selection. Other exclusionary criteria were other chronic gastrointestinal diseases (including celiac disease), clinically relevant impairment of kidney or liver function, previous intestinal resection or stoma | |
| Interventions | Induction: 6 weeks, open‐label 9 mg/day budesonide, randomized to maintenance or placebo therapy Maintenance: 24 weeks, budesonide 6 mg/day versus placebo Treatment‐free follow‐up: 24 weeks Patients who relapsed during the maintenance or follow‐up were offered treatment with open‐label budesonide (9 mg/day for 6 weeks, followed by budesonide 6 mg/day for 24 weeks) | |
| Outcomes | Induction: proportion entering clinical/histological remission, randomized to maintenance or placebo therapy after 6 weeks Maintenance: proportion maintaining clinical/histological remission after 24 weeks Treatment‐free follow‐up: proportion maintaining clinical/histological remission 24 weeks Clinical remission was defined as mean stool frequency of < 3 per day *Each patient underwent colonoscopy or sigmoidoscopy pre‐treatment. All were scheduled to undergo sigmoidoscopy at relapse or at the end of treatment, but this was only performed in 21 patients | |
| Notes | Data from the 24 weeks of the study only were included as the primary outcome measure, as this was the duration of active treatment with budesonide or placebo | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Computer‐generated block randomisation" |
| Allocation concealment (selection bias) | Low risk | Allocation sequence appears to be centrally generated |
| Blinding (performance bias and detection bias) | Low risk | Quote: "double‐blind" Quote: "budesonide 6 mg once a day (2 x 3 mg capsules) or matching placebo" Quote: "blinded follow‐up period (the randomisation code was unbroken until completion of follow‐up, such that neither patients nor physicians knew which treatment the patient had received during maintenance therapy)" |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "All analyses were completed on an intention‐to‐treat basis; premature discontinuation of treatment was considered as relapse in both treatment arms" Quote: "Two patients, one in each group, discontinued maintenance treatment because of adverse events" |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Low risk | Study appeared to be free of other forms of bias |
| Methods | Randomized, unblinded, open‐label study | |
| Participants | Patients (n = 819) who presented to clinic, underwent a colonoscopy because of chronic watery diarrhoea and were diagnosed with microscopic colitis (aged 19–68 years; n = 64; 23 with collagenous colitis and 41 with lymphocytic colitis) Clinical components of diagnosis: Chronic or recurrent non‐bloody diarrhea | |
| Interventions | Mesalazine 800 mg po tid (n = 20 with lymphocytic colitis and 11 with collagenous colitis) vs. mesalazine 800 mg po tid + cholestyramine 4 g po od (n = 21 with lymphocytic colitis and 12 with collagenous colitis) for 6 months A 24‐month treatment free follow was also performed A second round of 6 month‐therapy was offered if patients relapsed in follow‐up | |
| Outcomes | Primary outcomes: Clinical response: "Complete response was complete resolution of diarrhoea. Partial response was improvement but not resolution of diarrhoea Secondary outcomes: 24‐month follow‐up with coloscopies and biopsies, annually; adverse events; and days to remission or relapse, as well as various lab data (routine blood biochemistry and hematological counts, C‐reactive protein, antinuclear antibodies blood assay, serum T4 and thyroid stimulating hormone; IgA‐IgG antigliadin, antiendomysium, IgG anti tTG antibody blood assays; and parasitic‐bacterial, fecal‐stool, and hemo‐occult test | |
| Notes | "Relapse was defined as stool frequency greater than three soft or liquid stools per day" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization was performed with a computer generated list |
| Allocation concealment (selection bias) | Unclear risk | Not described in published study |
| Blinding (performance bias and detection bias) | High risk | Quote: "open‐label" Quote: "All biopsies were analyzed by a single experienced pathologist in a blinded fashion" |
| Incomplete outcome data (attrition bias) | Low risk | 3 of 23 patients with collagenous colitis were lost to follow‐up over a 24 month period The treatment groups and reasons for the missing data were not reported |
| Selective reporting (reporting bias) | Unclear risk | Outcomes were not pre‐specified in the methods section of the manuscript |
| Other bias | Low risk | Study appeared to be free of other forms of bias |
| Methods | Randomized, double‐blind, placebo‐controlled. Duration of study was 8 weeks. After 8 weeks, placebo group remained blinded and crossed over to active treatment with bismuth salicylate | |
| Participants | Patients (n = 14, split evenly) with microscopic colitis (11F, 3M; aged 35‐78 years; 9 with thickened subepithelial collagen, 5 without) Clinical: 8 weeks of non bloody watery diarrhea (without steatorrhea) and normal endoscopic appearance of the colonic mucosa. | |
| Interventions | Bismuth subsalicylate (nine 262 mg/day chewable tablets in 3 divided doses) versus placebo (identically coloured and flavoured sucrose tablets) for 8 weeks. | |
| Outcomes | "48 hour fecal weight and consistency, and distal colonic histology (from 16 biopsies obtained by flexible sigmoidoscopy)" were assessed pre and post therapy Clinical: improvement of diarrhea to passage of 2 or less formed or semi‐formed stools/day | |
| Notes | Only patients with a thickened subepithelial collagen band on biopsy were included (scored as normal, focally thickened, or diffusely thickened). 4 patients with normal thickness of the subepithelial collagen band were excluded from the analysis. Patients were not to take antibiotics or anti‐inflammatory agents for minimum 6 weeks, and not to take antidiarrheals for minimum 2 weeks prior to the beginning of the study Abstract publication For the histological outcome analysis, a histopathology score from 0 to 10 was based on the following parameters: surface epithelium assessed for micro‐ulceration, cell flattening, and mucin depletion (scored: 0 ‐ normal, 1 ‐ moderate, 2 ‐ severe); crypts (scored: 0 ‐ normal, 1 ‐ distorted architecture and/or cryptitis with neutrophils, 2 ‐ containing crypt abscesses); lamina propria cellularity (scored: 0 ‐ normal, 1 ‐ focally increased with neutrophils, mononuclear inflammatory cells, or both, 2 ‐ diffusely increased with neutrophils, mononuclear inflammatory cells, or both); number of intraepithelial lymphocytes within surface epithelium (scored 0 ‐ normal, 1 ‐ moderately increased, 2 ‐ significantly increased); number of intraepithelial lymphocytes within crypt epithelium (scored 0 ‐ normal, 1 ‐ moderately increased, 2 ‐ significantly increased) Additional information provided by author | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomization was performed by pulling pieces of paper out of a sealed box" |
| Allocation concealment (selection bias) | Unclear risk | Not described in abstract publication |
| Blinding (performance bias and detection bias) | Low risk | Quote: "double‐blind" Quote: "identically coloured and favoured sucrose‐placebo tablets" Quote: "Blind histologic analysis" |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "All patients taking BSS completed the study; one patient receiving placebo dropped out of the study after 4 weeks" |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Low risk | Study appeared to be free of other forms of bias |
| Methods | Randomized, double‐blind, placebo‐controlled trial performed at multiple German centres. Duration of study was 6 weeks. Study had potential crossover for the non‐responders in the placebo group | |
| Participants | Patients (n = 31) aged 18‐80 years with clinically and histologically confirmed collagenous colitis ("at least five liquid or soft stools per day on average per week, and a complete colonoscopy performed within the last 4 weeks before randomization") Histological diagnosis made with colonoscopy with biopsy: main criteria was collagen band > 10 um thick Other analyzed criteria included inflammation of lamina propria (semi‐quantitative definition) and degeneration of surface epithelium (qualitative definition) | |
| Interventions | Boswellia serrata extract (three 400 mg/day capsules) versus placebo for 6 weeks Cross‐over therapy offered to non‐responders after 6 weeks, open‐labelled BSE 400 mg po t.i.d | |
| Outcomes | Primary endpoint was clinical remission after 6 weeks (stool frequency of < 3 per day) stool frequency of less than 3 per day Histological (via colonoscopy with biopsy): improvement in baseline parameters "Stool frequency and consistency, intake of study medication, adverse events, and any intake of allowed concomitant medication were assessed by standardized questionnaire" "Patients who did not respond to treatment after 6 weeks were individually unblinded. If they were in the active treatment group, they were judged as treatment failure. If they were in the placebo group, crossover therapy with open‐labelled BSE 400 mg, given orally three times daily was offered" | |
| Notes | During the first three weeks of treatment loperamide was allowed as rescue medication. "Patients were allowed to use butylscopolamine in case of abdominal pain" Steroids, anti‐inflammatory drugs, immunosuppressives, antibiotics, prokinetics and bismuth compounds were not allowed during the study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization was via a central computer generated randomization list in groups of four patients |
| Allocation concealment (selection bias) | Low risk | Quote: "central computer‐generated randomization list" |
| Blinding (performance bias and detection bias) | Low risk | Quote: "double‐blind" Quote: "Physicians, patients, and pathologist were blinded to the treatment group. Study medication was provided in identical‐ looking white boxes labelled with consecutive numbers corresponding to the randomization list. In addition, the placebo containers were prepared from the inside to mimic the typical scent of incense to prevent unblinding by the typical odour of BSE." |
| Incomplete outcome data (attrition bias) | Low risk | 5/31 patients discontinued (4 patients, reasons described) the trial or were lost to follow‐up (1 patient). All 31 patients were included in the intention‐to‐treat analysis, 26 patients were included in the per‐protocol analysis |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Low risk | Study appeared to be free of other forms of bias |
| Methods | Randomized, double‐blind, placebo‐controlled performed at 35 centres in Germany (hospitals and private clinics), which used a centrally‐removed pathologist. Duration of study was 6 weeks | |
| Participants | Patients (n = 51) aged 18‐80 years with clinically and histologically confirmed collagenous colitis ("at least five liquid or soft stools per day on average per week, and a complete colonoscopy performed within the last 4 weeks before randomization"). Female patients must also be using appropriate contraception Histological diagnosis made with colonoscopy with biopsy: main criteria was collagen band > 10 um thick by Van Giesen staining. Other analyzed criteria included inflammation of lamina propria (semi‐quantitative definition) and degeneration of surface epithelium (qualitative definition) Patients were excluded if they had evidence of infectious diarrhea (from culture or biopsy), any other endoscopic or histologic findings (polyps 2 cm, tumors, Crohn’s disease, ulcerative colitis, ischemic colitis) which may have caused diarrhea, known intolerance to budesonide, pregnancy, lactation, or prior partial colonic resection, or if they had received treatment with budesonide, salicylates, steroids, prokinetics, antibiotics, ketoconazole, or non‐steroidal anti‐inflammatory drugs within 4 weeks before randomization | |
| Interventions | Budesonide 9 mg/day (three 3 mg/day tablets once in the morning) versus identically‐matched placebo for 6 weeks Cross‐over therapy offered to non‐responders after 6 weeks, open‐label budesonide, 9 mg/day po for another 6 weeks | |
| Outcomes | Proportion of patients achieving clinical remission or histological improvement after 6 weeks Clinical remission defined as: average of < 3 soft stools per day during the last week of treatment Patients who did not respond to treatment after 6 weeks were unblinded. If they were in the active treatment group, they were judged as treatment failure. If they were in the placebo group, crossover therapy with open‐label budesonide, 9 mg/day po for another 6 weeks | |
| Notes | Other therapies for collagenous colitis were discontinued for at least 3 weeks prior to enrolment in the trial. Loperamide was allowed for the first 4 weeks of the trial (used by 4 patients in the placebo group and 2 in the budesonide group), but no anti‐diarrhoeals allowed in the last two weeks. Patients were allowed to use butylscopolamine for abdominal pain | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Eligible patients were randomized by groups of 4 patients according to a central computer‐generated randomization list" |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) | Low risk | Quote: "double‐blind" Quote: "Active and placebo capsules were identical in appearance" |
| Incomplete outcome data (attrition bias) | Low risk | 6/51 patients withdrew (3 from placebo and 3 from budesonide) from the trial (reasons described) Both per‐protocol and intention‐to‐treat analysis available For endoscopic investigations per‐protocol analysis used |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Low risk | Study appeared to be free of other forms of bias |
| Methods | Randomized, double‐blind, placebo‐controlled performed at 38 centres in Germany | |
| Participants | Patients aged >18 years with symptomatic and histologically proven collagenous colitis Clinically active defined as ">3 watery/loose stools per day on ≥ 4 of the previous 7 days and had a history of diarrhoea for ≥ 4 weeks" Histological requirements: Subepithelial collagen band > 10 um; inflammatory infiltrate in the lamina propria Exclusion criteria: infectious causes for diarrhea; other inflammatory bowel diseases; history of colonic surgery; celiac disease; malignancies; severe concomitant (organ) diseases that would interfere with the study; at time of inclusion, were being treated 5‐aminosalicylates, salicylates (except in doses ≤165 mg for cardiovascular prophylaxis), systemic steroids, antibiotics, or NSAIDs (including selective cyclo‐oxygenase‐2 inhibitors); used of budesonide within the 2 weeks prior to enrolment, known intolerance to budesonide; pregnancy, lactation, drug and/or alcohol abuse Induction phase: n = 48 Maintenance phase: n = 46, split equally to budesonide and placebo | |
| Interventions | Induction phase: open‐label budesonide 9 mg/day (3 x 3 mg capsules [Entocort CIR capsules]) once/day for 6 weeks (all included patients) Maintenance phase: budesonide 6 mg/day or placebo for 6 months | |
| Outcomes | Primary endpoint was cumulative rate of relapse at the end of 6 months (maintenance phase); remission had been induced during the 6 week induction phase. Relapse was defined as > 3 stools per day on ≥ 4 consecutive days. Relapse rates were determined from daily patient diaries Secondary outcomes were time to relapse during maintenance therapy; the proportions of patients with clinical remission after 6 weeks’ induction therapy and after 2 and 4 months of maintenance therapy; HRQOL outcomes; and changes in histologic variables after 6 months’ maintenance therapy ("thickness of the collagen band (>10 or <10 µm); inflammation of the lamina propria (infiltration with lymphocytes and plasma cells; absent, mild, moderate, or severe); and degeneration of the surface epithelium (absent, or present)"). Histologic improvement defined as improvement in ≥ 2 variables versus baseline Safety and tolerability assessments were also performed | |
| Notes | HRQOL was assessed using the validated Medical Outcome Short Form (SF)‐36 questionnaire26 and the Short Inflammatory Bowel Disease Questionnaire (sIBDQ) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomization not described |
| Allocation concealment (selection bias) | Unclear risk | Method of allocation not described in published study |
| Blinding (performance bias and detection bias) | Low risk | Quote: "double‐blind" Quote: "budesonide and placebo capsules appeared identical and were packaged in identical bottles" |
| Incomplete outcome data (attrition bias) | Low risk | 21/46 patients withdrew during the maintenance phase, 17 due to relapse (14 taking placebo and 3 taking budesonide), 4 due to adverse events (1 taking placebo and 3 taking budesonide) Quote: "for the purposes of intention‐to‐treat analysis, patients who withdrew because of adverse events during maintenance therapy were counted as relapses" |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Low risk | Study appeared to be free of other forms of bias |
| Methods | Randomized, double‐blind, double‐dummy, placebo‐controlled, comparative phase‐3 trial performed at 31 European centres (hospitals and private clinics) ‐ Germany, Denmark, Lithuania, Spain, and the United Kingdom. Duration of study was 8 weeks | |
| Participants | N = 92 (budesonide n = 30; mesalamine n = 25, placebo n = 37) Inclusion criteria: Clinical: Patients between 18 and 80 years of age with >4 watery or soft stools on ≥4 days and >3 stools/day in the week prior to baseline. Patients must have also had chronic diarrhoea for ≥3 months prior to baseline and have had a colonoscopy within 4 months of baseline Histological: confirmed collagenous colitis with subepithelial collagenous band > 10 um and degeneration of the surface epithelium Exclusion criteria: "other significant colonic diseases (i.e. polyps >2 cm, tumors, Crohn’s disease, ulcerative colitis, ischemic colitis), partial colonic resection, infectious diarrhea, celiac disease (blood tests and/or duodenal histology required), diarrhea caused by other organic diseases of the gastrointestinal tract, treatment with budesonide, Boswellia serrata extract, salicylates, steroids, antibiotics, cholestyramine, nonsteroidal anti‐inflammatory, or other immunosuppressant drugs within the last 4 weeks before baseline, malignant disease, severe comorbidity, abnormal hepatic function or liver cirrhosis, renal insufficiency, active peptic ulcer disease, known intolerance or resistance to study drugs, pregnancy, or breast‐feeding" | |
| Interventions | Budesonide 9 mg/day ["(3x3 mg pH‐modified release capsules, Budenofalk) 30 minutes before breakfast"] Mesalamine 3 g/day [morning dosage of "sachets each containing 1.5 g mesalamine presented as a granule formulation, Salofalk"] Placebo All medications take for 8 weeks if responsive. If unresponsive after 4 weeks, or relapsed in the 16 week treatment‐free follow‐up, patient's removed from study arm and received 9 mg/day of budesonide for the remaining 4 weeks. | |
| Outcomes | Measured at each interim visit: 2, 4, 6, 8 weeks; 8 and 16 weeks Primary Outcomes: Clinical: remission defined as ≤3 stools/day in the week before the visit. Histological: measured collagen band thickness (≤10um or 50% reduction), lamina propria inflammation (by scoring), intraepithelial lymphocytes (by scoring) and whether the surface epithelium was degenerated. Improvement was defined as improvement of two of the parameters. Histological remission was defined as "collagen band thickness 10 mm and no inflammation of the lamina propria with neutrophilic and eosinophilic granulocytes." Secondary Outcome: Clinical remission was also evaluated according to Hjortswang‐Criteria of disease activity ("mean <3 stools per day, with <1 watery stool per day)" Also, "time to remission, number of watery and solid stools per week, abdominal pain, histopathology, | |
| Notes | Relapse was defined as: ">4 watery/soft stools on at least 4 days in the week before the visit and >3 stools per day within the last 7 days before the visit" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated random numbers assigning at a 1:1:1 ratio between the 3 arms of the study |
| Allocation concealment (selection bias) | Low risk | Computer generated, random numbers list prepared by a contract research organization that had no clinical involvement with the trial Used medication packed in boxes with consecutive numbers according to the randomization list |
| Blinding (performance bias and detection bias) | Low risk | "double‐blind, double‐dummy" Identical placebo capsules and sachets Single pathologist was blinded |
| Incomplete outcome data (attrition bias) | Low risk | 21/92 patients withdrew from the trial prematurely (before 8 weeks). Two taking budesonide, 9 taking mesalamine and 10 taking placebo. Reasons described. 64/92 entered follow up, 16 entered open‐label budesonide. Intention‐to‐treat was followed |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | Study appeared to be free of other forms of bias |
| Methods | An initial 8‐week open‐label induction phase with budesonide therapy to achieve clinical remission was followed by a double‐blind, randomized, placebo‐controlled, parallel‐group, multicentre, 12‐month phase for maintenance of clinical remission. After this there was 6 months of treatment‐free follow‐up | |
| Participants | A total of 148 patients were screened, all age ≥ 18 years Inclusion criteria: 1. Histologically established diagnosis of collagenous 2. Prescreening history of non‐bloody, watery diarrhea for ≥2 weeks in patients with newly diagnosed collagenous colitis, or a prescreening history of clinical relapse for ≥1 week in patients with previously established collagenous colitis 3. A mean of ≥3 stools/day, including a mean of ≥1 watery stool/day, during the week prior to baseline Exclusion criteria: 1. Diabetes mellitus, infection, glaucoma, tuberculosis, peptic ulcer disease or hypertension if careful medical monitoring was not ensured 2. Established cataract 3. Known hereditary problems of galactose or fructose intolerance, lactase deficiency, increased levels of anti‐transglutaminase 2 antibodies 4. Established osteoporosis with T‐score <−2.5 As per Figure 2: 110 met eligibility criteria and started the open‐label phase. 92 patients had achieved remission during the open‐label phase and were randomized for treatment in the double‐blind phase (44 budesonide, 48 placebo). 43 completed the 12‐month study visit (32 budesonide, 11 placebo). 36 patients at the end of the double‐blind phase (28 budesonide, 8 placebo) entered the follow‐up phase | |
| Interventions | During the open‐label induction phase, all patients received once‐daily budesonide (Budenofalk 3 mg capsules) at a dose of 9 mg/day for 4 weeks, then 6 mg/day for 2 weeks, followed by alternate daily doses of 6 and 3 mg/day (mean 4.5 mg/day) for the final 2 weeks During the double‐blind phase, the active treatment group received once‐daily budesonide 6 and 3 mg/day on alternate days (mean 4.5 mg/day). The placebo group received two placebo capsules and one placebo capsule on alternate days, administered once daily After the final visit of the double‐blind phase (month 12), there was a 2‐week tapering‐off period, during which patients in the active treatment group received 3 mg/day budesonide for 1 week followed by 3 mg/day budesonide every second day for 1 week. Patients in the placebo group received one placebo capsule on the corresponding days Patients who remained in clinical remission at the end of the double‐blind phase received no further study drug after the 2‐week tapering‐off period During the treatment‐free follow‐up, no intervention was given | |
| Outcomes | The primary endpoint was the proportion of patients remaining in clinical remission during the 12‐month double‐blind phase, with clinical remission defined as a mean of <3 stools/day, including a mean of <1 watery stool/day over 1 week The main secondary endpoints during the double‐label phase included health‐related quality of life using the Short Health Scale (SHS) and the Psychological General Well‐Being Index (PGWBI) Further secondary endpoints during the double‐blind phase were achievement of histological remission or histological improvement | |
| Notes | During the entire study period, loperamide, anti‐inflammatory or immunosuppressant drugs were not permitted | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Method of randomization was described as "a computer‐generated randomisation list using randomly permuted blocks" |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not described |
| Blinding (performance bias and detection bias) | Low risk | Double‐blinding is mentioned, but not described in more detail. Placebo capsules were used |
| Incomplete outcome data (attrition bias) | Low risk | Well described patient disposition in Figure 2 and had intention‐to‐treat analysis described. They accounted for attrition/exclusions with reasons given |
| Selective reporting (reporting bias) | Low risk | All primary outcomes were reported. Most secondary outcomes were reported with exception of histological outcomes Safety and adverse‐effect data was also presented, but not described as part of methods section |
| Other bias | Low risk | Study appeared to be free of other forms of bias |
| Methods | Randomized, double‐blind, placebo‐controlled, multi‐centred trial | |
| Participants | Patients (n = 12, 11 with collagenous colitis and 1 with lymphocytic colitis) aged >18 years reporting at least 3 months with diarrhoea without blood or pus and with a stool volume ≥350 g/day or ≥200 g/day and a stool frequency ≥5/day and a histological diagnosis of microscopic colitis. Female patients also needed to use appropriate contraceptive techniques Patients were diagnosed histologically using a macroscopic normal colonoscopy or sigmoidoscopy plus a normal barium enema and confirmed by an independent pathologist with either lymphocytic colitis or collagenous colitis using the following criteria: “chronic inflammatory infiltrate in the lamina propria and either a lymphocytic infiltration of at least 20% of epithelial crypt cells (lymphocytic colitis) and/or a subepithelial collagen bond >10 µm in a well‐oriented biopsy (collagenous colitis)” Excluded patients: tested positive for pathogenic bacteria or parasites; failed a normal lactose absorption test and vitamin B12 absorption test, or a normal barium follow through; had celiac disease (confirmed with IgG and IgA antigliadin antibodies and antiendomysium antibodies and/or abnormal histology in duodenal biopsies); had bile acid malabsorption and/or no response to cholestyramine, and/or steatorrhoea; had other gastrointestinal diseases or previous gastrointestinal surgery (exception: cholecystectomy); had other serious diseases, abnormal laboratory tests (haematology, renal function, liver enzymes, urinalysis); had been treated with immunosuppressives within 3 months of randomization; or used medicines with known effects on gastrointestinal functioning including anti‐ulcer medication, antacids, antibiotics and NSAIDs | |
| Interventions | Prednisolone, n = 9 (50 mg/dayfor 2 weeks, tapered to 37.5 mg/day in third week) versus placebo, n = 3, for 2 weeks. All patients also received Ca 500 mg + vitamin D 5 ug/day | |
| Outcomes | Proportion of patients achieving clinical remission after 2 weeks Clinical remission was defined as stool weight ≤ 200 g/day or frequency ≤ 2/day; effect was defined as >50% reduction of either stool frequency or weight. | |
| Notes | Inclusion of patients was stopped when planned monitoring indicated that prednisone did not induce remission. Protocol also included a 48‐week azathioprine continuation phase which was closed when it became clear that the calculated number of patients could not be recruited Medications with immunosuppressive effects, antidiarrhoeals or those with known effects on gastrointestinal function were not allowed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomization not described |
| Allocation concealment (selection bias) | Unclear risk | Method of allocation not described in published study |
| Blinding (performance bias and detection bias) | Low risk | Quote: "double‐blind" Quote: "identical placebo tablets" |
| Incomplete outcome data (attrition bias) | Low risk | No missing data Quote: "All patients complied with and completed the treatment protocol" |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Low risk | Study appeared to be free of other forms of bias |
| Methods | Randomized, double‐blind, placebo‐controlled trial at 4 Danish centres. Randomization was in a 2:1 fashion (probiotic:placebo) | |
| Participants | Patients (n = 36*, therefore n = 29, 2 men) aged ≥18 years with confirmed histological diagnosis of collagenous colitis that is active and untreated for at least 4 weeks prior to study inclusion. Clinically active disease is defined as > 21 liquid or soft stools per week or stool weight of > 200 g/day for at least 4 weeks | |
| Interventions | Probiotic (AB‐Cap‐10; two capsules twice daily) or placebo (2 capsules twice daily) for 12 weeks. Loperamide and opioids were allowed during the study | |
| Outcomes | Primary outcome was the proportion of patients with a at least a 50% reduction in the number of stools per week at 12 weeks Histological scores from: significant change in three parameters: reduction of thickness of the collagen band; improvement in the degree of inflammation of the lamina propria; improvement of degeneration of surface epithelium The study period was 17 weeks (12 weeks treatment + 5 weeks follow up) with patients being assessed at weeks ‐1, 0, 4, 6, 12, and 16. All patients kept a diary throughout the study period | |
| Notes | AB‐Cap‐10 is a mixture of L. acidophilus strain LA‐5 and B. animalis subsp. lactis strain BB‐12. Each capsule contained 0.5 x 10^10 colony‐forming units of each bacterium, leading to a total delivery of 1 x 10^10 CFU per capsule SIBDQ; a 10‐item questionnaire measuring health‐related quality of life [HRQOL] intended for patients with Crohn’s disease and ulcerative colitis *Seven patients that failed to meet the inclusion criteria after being randomized into the trial (six patients had lymphocytic colitis and one had a subepithelial collagen band < 10 um thick) are excluded from the analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization was completed in blocks of 9 using a table of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Method of randomization not described in study |
| Blinding (performance bias and detection bias) | Low risk | Quote: "double‐blind" Quote: "Placebo medication (Chr. Hansen A/S) was identical in appearance, size, and taste" |
| Incomplete outcome data (attrition bias) | Low risk | 3 probiotic treatment patients dropped out because of lack of response Quote: "When data at week 12 were missing because of withdrawals, the last observation was carried forward" |
| Selective reporting (reporting bias) | Low risk | All outcome reported. One post hoc analysis noted |
| Other bias | Low risk | Study appeared to be free of other forms of bias |
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Not a randomized trial. It was a cohort extension trial of another randomized controlled trial | |
| Not a randomized trial. It is a case report | |
| Not a randomized trial. It also included microscopic colitis patients without specifying for collagenous colitis | |
| Not a randomized trial. It also included microscopic colitis patients without specifying for collagenous colitis | |
| Withdrawal of short‐term budesonide therapy. Examines different outcomes | |
| No study data |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical response Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.1 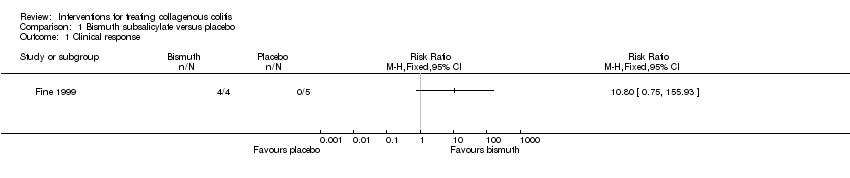 Comparison 1 Bismuth subsalicylate versus placebo, Outcome 1 Clinical response. | ||||
| 2 Histological response Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.2 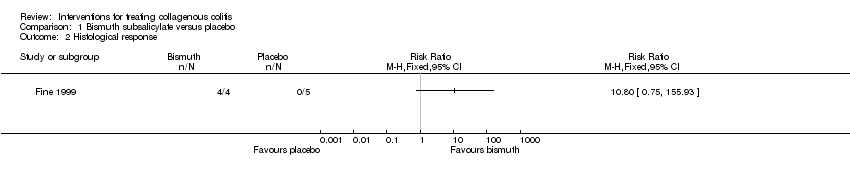 Comparison 1 Bismuth subsalicylate versus placebo, Outcome 2 Histological response. | ||||
| 3 Adverse events Show forest plot | 1 | 9 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 1.3 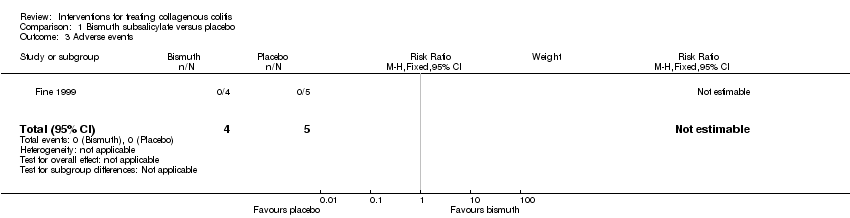 Comparison 1 Bismuth subsalicylate versus placebo, Outcome 3 Adverse events. | ||||
| 4 Withdrawals due to adverse events Show forest plot | 1 | 9 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 1.4 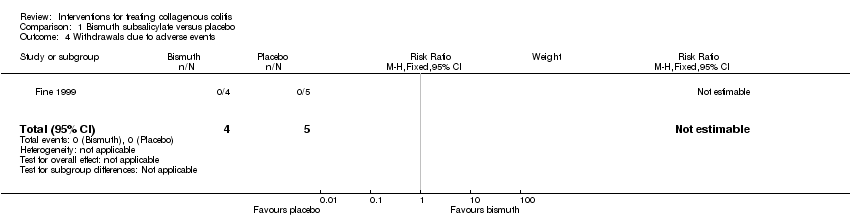 Comparison 1 Bismuth subsalicylate versus placebo, Outcome 4 Withdrawals due to adverse events. | ||||
| 5 Serious adverse events Show forest plot | 1 | 9 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 1.5  Comparison 1 Bismuth subsalicylate versus placebo, Outcome 5 Serious adverse events. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical response Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.1 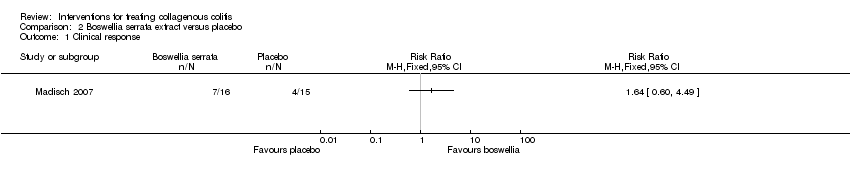 Comparison 2 Boswellia serrata extract versus placebo, Outcome 1 Clinical response. | ||||
| 2 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.2  Comparison 2 Boswellia serrata extract versus placebo, Outcome 2 Adverse events. | ||||
| 3 Withdrawals due to adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.3 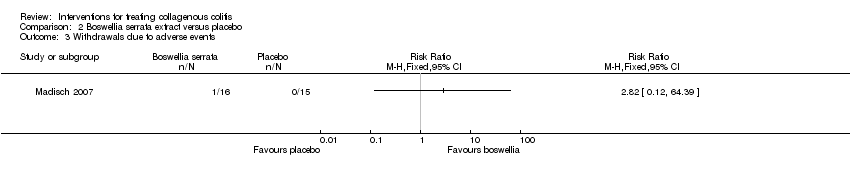 Comparison 2 Boswellia serrata extract versus placebo, Outcome 3 Withdrawals due to adverse events. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical response Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.1  Comparison 3 Budesonide versus mesalazine, Outcome 1 Clinical response. | ||||
| 2 Histological response Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.2  Comparison 3 Budesonide versus mesalazine, Outcome 2 Histological response. | ||||
| 3 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.3  Comparison 3 Budesonide versus mesalazine, Outcome 3 Adverse events. | ||||
| 4 Withdrawals due to adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.4 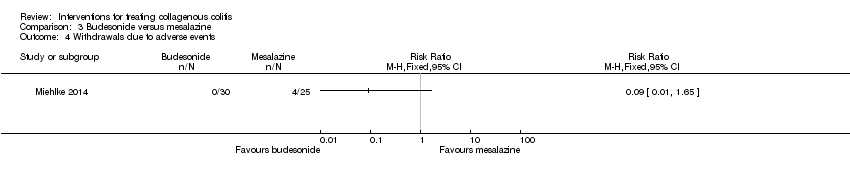 Comparison 3 Budesonide versus mesalazine, Outcome 4 Withdrawals due to adverse events. | ||||
| 5 Serious adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.5  Comparison 3 Budesonide versus mesalazine, Outcome 5 Serious adverse events. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical response Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.1  Comparison 4 Mesalamine versus placebo, Outcome 1 Clinical response. | ||||
| 2 Histological response Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.2 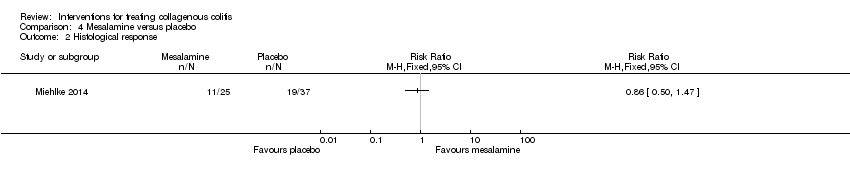 Comparison 4 Mesalamine versus placebo, Outcome 2 Histological response. | ||||
| 3 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.3  Comparison 4 Mesalamine versus placebo, Outcome 3 Adverse events. | ||||
| 4 Withdrawals due to adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.4 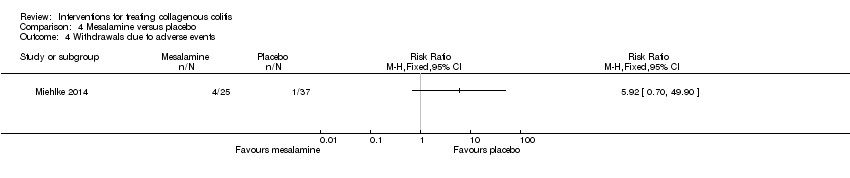 Comparison 4 Mesalamine versus placebo, Outcome 4 Withdrawals due to adverse events. | ||||
| 5 Serious adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.5  Comparison 4 Mesalamine versus placebo, Outcome 5 Serious adverse events. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical response Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.1 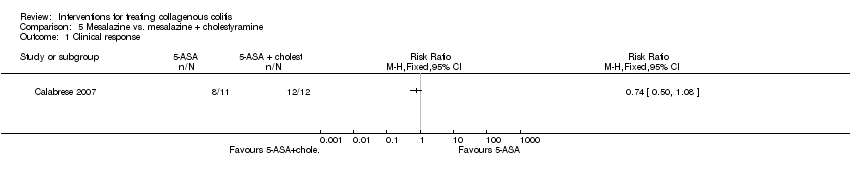 Comparison 5 Mesalazine vs. mesalazine + cholestyramine, Outcome 1 Clinical response. | ||||
| 2 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.2 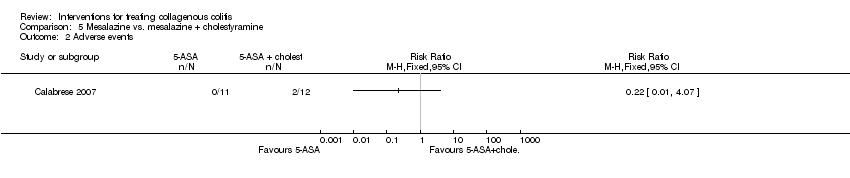 Comparison 5 Mesalazine vs. mesalazine + cholestyramine, Outcome 2 Adverse events. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical response Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.1  Comparison 6 Prednisolone versus placebo, Outcome 1 Clinical response. | ||||
| 2 Withdrawals due to adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.2 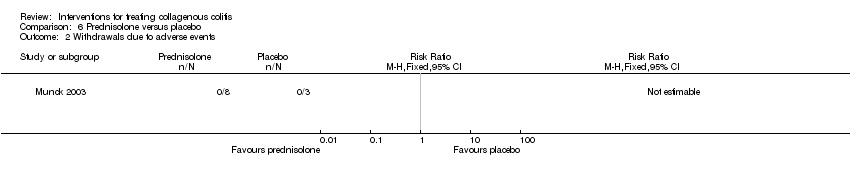 Comparison 6 Prednisolone versus placebo, Outcome 2 Withdrawals due to adverse events. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical response Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 7.1  Comparison 7 Probiotics versus placebo, Outcome 1 Clinical response. | ||||
| 2 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 7.2  Comparison 7 Probiotics versus placebo, Outcome 2 Adverse events. | ||||
| 3 Withdrawals due to adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 7.3  Comparison 7 Probiotics versus placebo, Outcome 3 Withdrawals due to adverse events. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical response Show forest plot | 4 | 161 | Risk Ratio (M‐H, Random, 95% CI) | 2.98 [1.14, 7.75] |
| Analysis 8.1 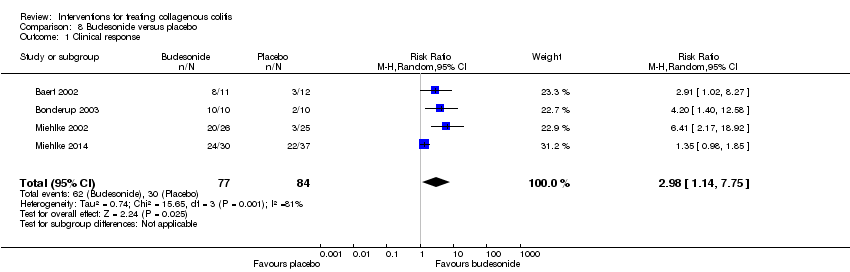 Comparison 8 Budesonide versus placebo, Outcome 1 Clinical response. | ||||
| 2 Clinical response sensitivity analysis excluding Miehlke 2014 Show forest plot | 3 | 94 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.56 [2.43, 8.55] |
| Analysis 8.2  Comparison 8 Budesonide versus placebo, Outcome 2 Clinical response sensitivity analysis excluding Miehlke 2014. | ||||
| 3 Histological response Show forest plot | 4 | 161 | Risk Ratio (M‐H, Random, 95% CI) | 2.68 [1.37, 5.24] |
| Analysis 8.3  Comparison 8 Budesonide versus placebo, Outcome 3 Histological response. | ||||
| 4 Histological response sensitivity analysis excluding Miehlke 2014 Show forest plot | 3 | 94 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.15 [2.25, 7.66] |
| Analysis 8.4  Comparison 8 Budesonide versus placebo, Outcome 4 Histological response sensitivity analysis excluding Miehlke 2014. | ||||
| 5 Maintenance of clinical response Show forest plot | 3 | 172 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.30 [2.13, 5.09] |
| Analysis 8.5  Comparison 8 Budesonide versus placebo, Outcome 5 Maintenance of clinical response. | ||||
| 6 Maintenance of histological response Show forest plot | 2 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.17 [1.44, 6.95] |
| Analysis 8.6  Comparison 8 Budesonide versus placebo, Outcome 6 Maintenance of histological response. | ||||
| 7 Adverse events Show forest plot | 5 | 290 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.92, 1.51] |
| Analysis 8.7 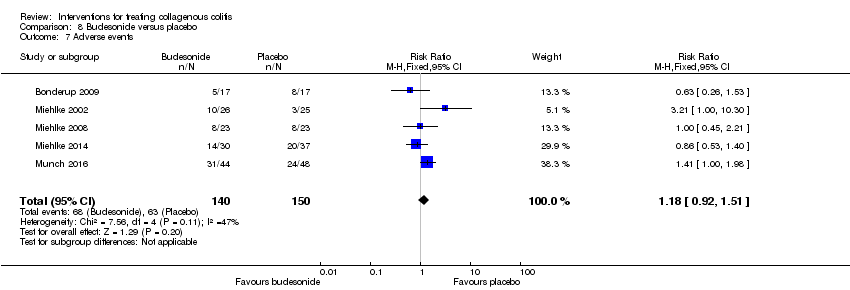 Comparison 8 Budesonide versus placebo, Outcome 7 Adverse events. | ||||
| 8 Withdrawals due to adverse events Show forest plot | 5 | 290 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.43, 2.17] |
| Analysis 8.8  Comparison 8 Budesonide versus placebo, Outcome 8 Withdrawals due to adverse events. | ||||
| 9 Serious adverse events Show forest plot | 4 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.15, 8.01] |
| Analysis 8.9  Comparison 8 Budesonide versus placebo, Outcome 9 Serious adverse events. | ||||

Study flow diagram.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Bismuth subsalicylate versus placebo, Outcome 1 Clinical response.
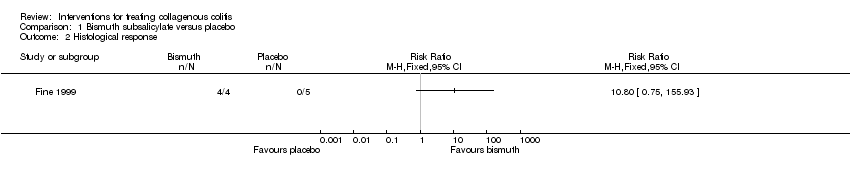
Comparison 1 Bismuth subsalicylate versus placebo, Outcome 2 Histological response.

Comparison 1 Bismuth subsalicylate versus placebo, Outcome 3 Adverse events.

Comparison 1 Bismuth subsalicylate versus placebo, Outcome 4 Withdrawals due to adverse events.
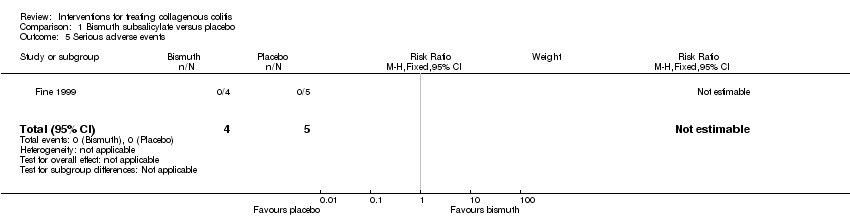
Comparison 1 Bismuth subsalicylate versus placebo, Outcome 5 Serious adverse events.

Comparison 2 Boswellia serrata extract versus placebo, Outcome 1 Clinical response.

Comparison 2 Boswellia serrata extract versus placebo, Outcome 2 Adverse events.

Comparison 2 Boswellia serrata extract versus placebo, Outcome 3 Withdrawals due to adverse events.

Comparison 3 Budesonide versus mesalazine, Outcome 1 Clinical response.
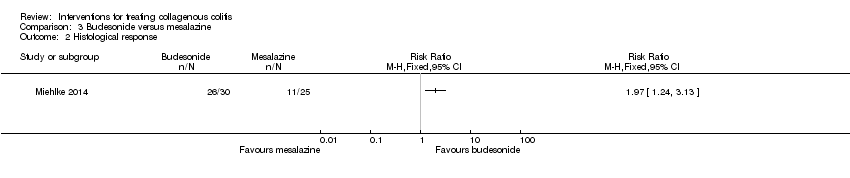
Comparison 3 Budesonide versus mesalazine, Outcome 2 Histological response.
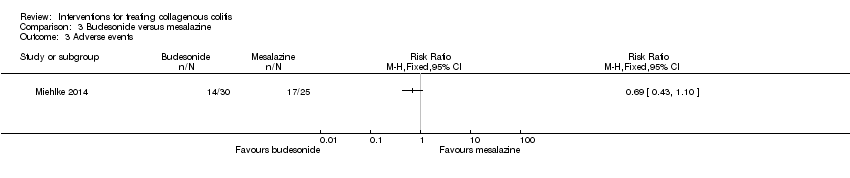
Comparison 3 Budesonide versus mesalazine, Outcome 3 Adverse events.

Comparison 3 Budesonide versus mesalazine, Outcome 4 Withdrawals due to adverse events.

Comparison 3 Budesonide versus mesalazine, Outcome 5 Serious adverse events.

Comparison 4 Mesalamine versus placebo, Outcome 1 Clinical response.
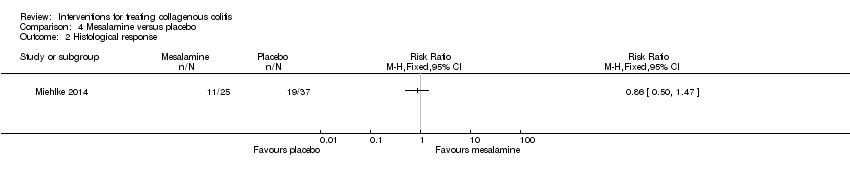
Comparison 4 Mesalamine versus placebo, Outcome 2 Histological response.

Comparison 4 Mesalamine versus placebo, Outcome 3 Adverse events.
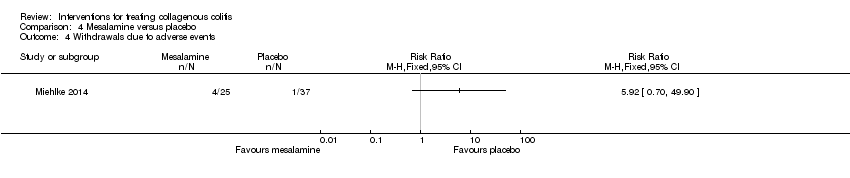
Comparison 4 Mesalamine versus placebo, Outcome 4 Withdrawals due to adverse events.

Comparison 4 Mesalamine versus placebo, Outcome 5 Serious adverse events.

Comparison 5 Mesalazine vs. mesalazine + cholestyramine, Outcome 1 Clinical response.
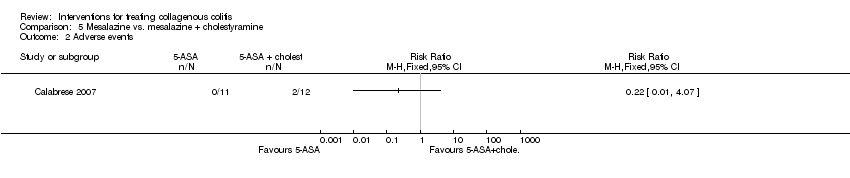
Comparison 5 Mesalazine vs. mesalazine + cholestyramine, Outcome 2 Adverse events.

Comparison 6 Prednisolone versus placebo, Outcome 1 Clinical response.

Comparison 6 Prednisolone versus placebo, Outcome 2 Withdrawals due to adverse events.

Comparison 7 Probiotics versus placebo, Outcome 1 Clinical response.

Comparison 7 Probiotics versus placebo, Outcome 2 Adverse events.

Comparison 7 Probiotics versus placebo, Outcome 3 Withdrawals due to adverse events.
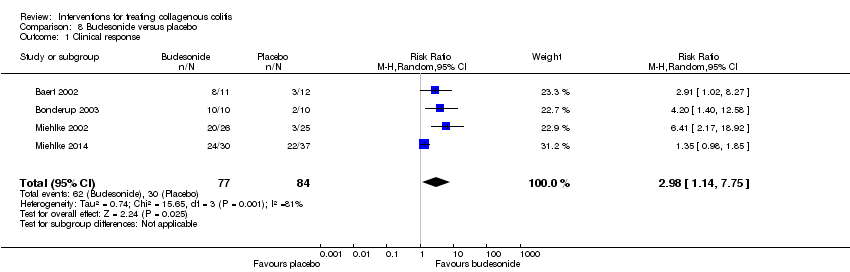
Comparison 8 Budesonide versus placebo, Outcome 1 Clinical response.

Comparison 8 Budesonide versus placebo, Outcome 2 Clinical response sensitivity analysis excluding Miehlke 2014.

Comparison 8 Budesonide versus placebo, Outcome 3 Histological response.

Comparison 8 Budesonide versus placebo, Outcome 4 Histological response sensitivity analysis excluding Miehlke 2014.

Comparison 8 Budesonide versus placebo, Outcome 5 Maintenance of clinical response.
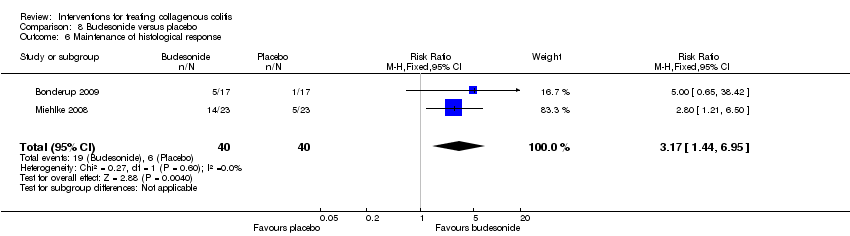
Comparison 8 Budesonide versus placebo, Outcome 6 Maintenance of histological response.

Comparison 8 Budesonide versus placebo, Outcome 7 Adverse events.
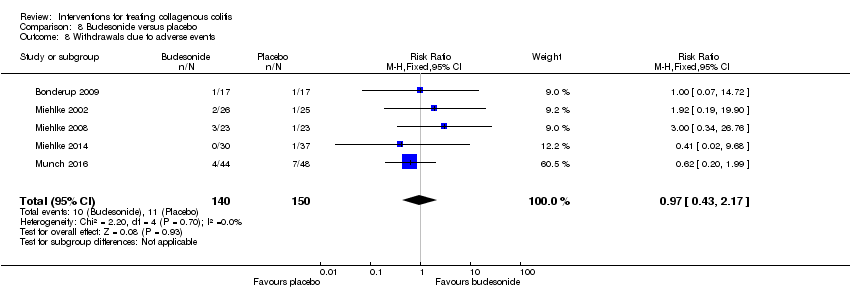
Comparison 8 Budesonide versus placebo, Outcome 8 Withdrawals due to adverse events.

Comparison 8 Budesonide versus placebo, Outcome 9 Serious adverse events.
| Bismuth subsalicylate versus placebo for treating collagenous colitis | ||||||
| Patient or population: Patients with collagenous colitis | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with placebo | Risk with Bismuth subsalicylate | |||||
| Clinical response | 0 per 10001 | 0 per 1000 | RR 10.80 | 9 | ⊕⊝⊝⊝ | |
| Histological response | 0 per 10001 | 0 per 1000 | RR 10.80 | 9 | ⊕⊝⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Control group risk comes from control arm of the included study. | ||||||
| Boswellia serrata extract versus placebo for treating collagenous colitis | ||||||
| Patient or population: Patients with collagenous colitis | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with placebo | Risk with Boswellia serrata extract | |||||
| Clinical response | 267 per 10001 | 437 per 1000 | RR 1.64 | 31 | ⊕⊕⊝⊝ | |
| Adverse events | 67 per 10001 | 125 per 1000 | RR 1.88 | 31 | ⊕⊕⊝⊝ | |
| Withdrawals due to adverse events | 0 per 10001 | 0 per 1000 | RR 2.82 | 31 | ⊕⊕⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Control group risk comes from control arm of the included study. | ||||||
| Budesonide versus mesalazine for treating collagenous colitis | ||||||
| Patient or population: Patients with collagenous colitis | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with mesalazine | Risk with Budesonide | |||||
| Clinical response | 440 per 10001 | 801 per 1000 | RR 1.82 | 55 | ⊕⊕⊝⊝ | |
| Histological response | 440 per 10001 | 867 per 1000 | RR 1.97 | 55 | ⊕⊕⊝⊝ | |
| Adverse events | 680 per 10001 | 469 per 1000 | RR 0.69 | 55 | ⊕⊕⊝⊝ | |
| Withdrawals due to adverse events | 160 per 10001 | 14 per 1000 | RR 0.09 | 55 | ⊕⊕⊝⊝ | |
| Serious adverse events | 120 per 10001 | 14 per 1000 | RR 0.12 | 55 | ⊕⊕⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Control group risk comes from control arm of the included study. | ||||||
| Mesalamine versus placebo for treating collagenous colitis | ||||||
| Patient or population: Patients with collagenous colitis | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with placebo | Risk with Mesalamine | |||||
| Clinical response | 595 per 10001 | 440 per 1000 | RR 0.74 | 62 | ⊕⊕⊝⊝ | |
| Histological response | 514 per 10001 | 442 per 1000 | RR 0.86 | 62 | ⊕⊕⊝⊝ | |
| Adverse events | 541 per 10001 | 681 per 1000 | RR 1.26 | 62 | ⊕⊕⊝⊝ | |
| Withdrawals due to adverse events | 27 per 10001 | 160 per 1000 | RR 5.92 | 62 | ⊕⊕⊝⊝ | |
| Serious adverse events | 27 per 10001 | 120 per 1000 | RR 4.44 | 62 | ⊕⊕⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Control group risk comes from control arm of the included study. | ||||||
| Mesalazine vs. mesalazine + cholestyramine for treating collagenous colitis | ||||||
| Patient or population: Patients with collagenous colitis | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with mesalazine + cholestyramine | Risk with Mesalazine | |||||
| Clinical response | 167 per 10001 | 123 per 1000 | RR 0.74 | 23 | ⊕⊝⊝⊝ | |
| Adverse events | 0 per 10001 | 0 per 1000 | RR 0.22 | 23 | ⊕⊝⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Control group risk comes from control arm of the included study. | ||||||
| Prednisolone versus placebo for treating collagenous colitis | ||||||
| Patient or population: Patients with collagenous colitis | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with placebo | Risk with Prednisolone | |||||
| Clinical response | 0 per 10001 | 0 per 1000 | RR 4.89 | 11 | ⊕⊝⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Control group risk comes from control arm of the included study. | ||||||
| Probiotics versus placebo for treating collagenous colitis | ||||||
| Patient or population: Patients with collagenous colitis | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with placebo | Risk with Probiotics | |||||
| Clinical response | 125 per 10001 | 286 per 1000 | RR 2.29 | 29 | ⊕⊝⊝⊝ | |
| Adverse events | 500 per 10001 | 285 per 1000 | RR 0.57 | 29 | ⊕⊝⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Control group risk comes from control arm of the included study. | ||||||
| Budesonide versus placebo for treating collagenous colitis | ||||||
| Patient or population: Patients with collagenous colitis | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with placebo | Risk with Budesonide | |||||
| Clinical response sensitivity analysis excluding Miehlke 2014 | 170 per 10001 | 722 per 1000 | RR 4.56 (2.43 to 8.55) | 94 | ⊕⊕⊝⊝ | |
| Histological response sensitivity analysis excluding Miehlke 2014 | 170 per 10001 | 706 per 1000 | RR 4.15 (2.25 to 7.66) | 94 | ⊕⊕⊝⊝ | |
| Maintenance of clinical response | 205 per 10001 | 675 per 1000 | RR 3.30 | 172 | ⊕⊕⊝⊝ | |
| Maintenance of histological response | 150 per 10001 | 476 per 1000 | RR 3.17 | 80 | ⊕⊝⊝⊝ | |
| Adverse events | 420 per 10001 | 496 per 1000 | RR 1.18 | 290 | ⊕⊕⊕⊝ | |
| Withdrawals due to adverse events | 73 per 10001 | 71 per 1000 | RR 0.97 | 290 | ⊕⊕⊝⊝ | |
| Serious adverse events | 11 per 10001 | 12 per 1000 | RR 1.11 | 175 | ⊕⊕⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Control group risk comes from control arm of meta‐analysis, based on included trials. | ||||||
| Therapy | References |
| 5‐ASA compounds | Weidner 1984, Farah 1985, Giardiello 1987, Wang 1987, Jessurun 1987, Eckstein 1988, Mason 1988, Rokkas 1988, O'Mahony 1990, Gubbins 1991, Giardiello 1991, Carpenter 1992, Fasoli 1994, Katanuma 1995, Bohr 1996, Goff 1997, Mullhaupt 1998, Wang 1999, Bonner 2000, Fielder 2001, Pardi 2001, Kimble 2001, Bozdech 2001, Abdo 2002, Fernandez 2003, Honkoop 2003, Randall 2003, Buchman 2004, Mowat 2005, Fekih 2006, Roe 2006, Madisch 2006, Narvaez 2006, de la Iglesia 2007, Ekiz 2007, Freeman 2007, Koch 2007, Halsey 2007, Rubio‐Tapia 2007 |
| Antibiotics | Mogensen 1984, Wang 1987, Puri 1994, Pimental 1995, Bohr 1996, Mullhaupt 1998, Swensson 1999, Honkoop 2001, Madisch 2006 |
| Antihistamine | Benchimol 2007 |
| Azathioprine/6‐mercaptopurine | Goff 1997, Pardi 2001, Roe 2006, Wickbom 2006 |
| Bismuth subsalicylate | Girard 1987, Fine 1998, Bohr 1999, Bozdech 2001, Buchman 2004, Madisch 2006, Chande 2007, Rubio‐Tapia 2007 |
| Budesonide | Van Gossum 1998, Delarive 1998, Lanyi 1999, Tromm 1999, Bohr 1999, Mueller‐Wittlic 2000, Bajor 2003, Fernandez 2003, Honkoop 2003, Buchman 2004, Hawkins 2004, Barta 2005, Bajor 2006, Roe 2006, Wickbom 2006, Freeman 2006, Hilmer 2006, Chopra 2006, Kiesslich 2006, de la Iglesia 2007, Freeman 2007, Brar 2007 |
| Cholestyramine/colestipol | Andersen 1993, Bohr 1996, Ung 2000, Fernandez 2003, Baert 2004, Mahmoud 2005, Hilmer 2006 |
| Cyclosporine | Eijsbouts 1995, Roe 2006 |
| Dietary modification | Fekih 2006 |
| Elemental diet | Teahon 1994 |
| Ketotifen | Marshall 1998, Benchimol 2007 |
| Methotrexate | Bhullar 1996, Hillman 2001, Riddell 2007 |
| Octreotide | Fisher 1996, Goff 1997 |
| Pentoxifylline | Peterson 1996, Williams 1998 |
| Probiotics | Tromm 2004 |
| Steroids, intravenous | Pardi 2001, Buchman 2004 |
| Steroids, oral | Palmer 1986, Hamilton 1986, Giardiello 1987, Wang 1987, Jessurun 1987, O'Mahony 1990, Sloth 1991, Giardiello 1991, Carpenter 1992, Fasoli 1994, Pimental 1995, Katanuma 1995, Bohr 1996, Goff 1997, Duncan 1997, Wang 1999, Castellano 1999, Swensson 1999, Bonner 2000, Fielder 2001, Persoz 2001, Honkoop 2001, Abdo 2002, Fernandez 2003, Honkoop 2003, Buchman 2004, Mowat 2005, O'Beirne 2005, Taha 2006, Madisch 2006, Narvaez 2006, Rubio‐Tapia 2007 |
| Steroids, topical | Wang 1987, Mason 1988 |
| Surgery | Jarnerot 1995, Alikhan 1997, Munch 2005, Shen 2006, Davis 2007 |
| Symptomatic therapy: antidiarrheal agents, bulking agents, spasmolytics | Bamford 1982, Eaves 1983, Giardiello 1987, Wang 1987, Gubbins 1991, Pimental 1995, Katanuma 1995, Bohr 1996, Goff 1997, Mullhaupt 1998, Wang 1999, Fielder 2001, Abdo 2002, Honkoop 2003, Mowat 2005, Smith 2005, Fekih 2006, Hilmer 2006, Madisch 2006, Ekiz 2007, Khawaja 2007, Halsey 2007 |
| Verapamil | Scheidler 2001 |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical response Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Histological response Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Adverse events Show forest plot | 1 | 9 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Withdrawals due to adverse events Show forest plot | 1 | 9 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Serious adverse events Show forest plot | 1 | 9 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical response Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Withdrawals due to adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical response Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Histological response Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Withdrawals due to adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Serious adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical response Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Histological response Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Withdrawals due to adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Serious adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical response Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical response Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Withdrawals due to adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical response Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Withdrawals due to adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical response Show forest plot | 4 | 161 | Risk Ratio (M‐H, Random, 95% CI) | 2.98 [1.14, 7.75] |
| 2 Clinical response sensitivity analysis excluding Miehlke 2014 Show forest plot | 3 | 94 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.56 [2.43, 8.55] |
| 3 Histological response Show forest plot | 4 | 161 | Risk Ratio (M‐H, Random, 95% CI) | 2.68 [1.37, 5.24] |
| 4 Histological response sensitivity analysis excluding Miehlke 2014 Show forest plot | 3 | 94 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.15 [2.25, 7.66] |
| 5 Maintenance of clinical response Show forest plot | 3 | 172 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.30 [2.13, 5.09] |
| 6 Maintenance of histological response Show forest plot | 2 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.17 [1.44, 6.95] |
| 7 Adverse events Show forest plot | 5 | 290 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.92, 1.51] |
| 8 Withdrawals due to adverse events Show forest plot | 5 | 290 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.43, 2.17] |
| 9 Serious adverse events Show forest plot | 4 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.15, 8.01] |

