Acupuntura para el accidente cerebrovascular agudo
Información
- DOI:
- https://doi.org/10.1002/14651858.CD003317.pub3Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 30 marzo 2018see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Accidentes cerebrovasculares
- Copyright:
-
- Copyright © 2018 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
Shihong Zhang and Ming Liu designed the protocol and the review. Shihong Zhang resolved disagreements about data collection and made critical suggestions on the manuscript. Mangmang Xu and Dan Li searched databases and extracted data. Mangmang Xu drafted this manuscript.
Sources of support
Internal sources
-
No sources of support supplied
External sources
-
Key Research and Development Program, Science & Technology Department of Sichuan Province (Grant No. 2017SZ0007), China.
Declarations of interest
Mangmang Xu: none known.
Dan Li: none known.
Shihong Zhang: none known.
Acknowledgements
We thank Hazel Fraser (Managing Editor, Cochrane Stroke Group) for the search of the Cochrane Stroke Group trials register, and Brenda Thomas (Trials Search Co‐ordinator) and Joshua Cheyne (Information Specialist) for the searches of CINAHL and AMED databases. We acknowledge with thanks the useful comments and the work of Prof Peter Langhorne, who spent time helping to revise this updated review. We also thank Valentina Assi, Joshua Cheyne, Maree Hackett, Hongmei Wu, Julie Gildie, Odie Geiger, and Heather Goodare for their many useful comments. We thank Prof Ming Liu for her contribution to previous versions of this review.
Version history
| Published | Title | Stage | Authors | Version |
| 2018 Mar 30 | Acupuncture for acute stroke | Review | Mangmang Xu, Dan Li, Shihong Zhang | |
| 2005 Apr 20 | Acupuncture for acute stroke | Review | Shihong Zhang, Ming Liu, Kjell Asplund, Lin Li | |
| 2001 Oct 23 | Acupuncture for acute stroke | Protocol | Ming Liu, Li He, Bo Wu, Shihong Zhang, Kjell Asplund | |
Differences between protocol and review
The previous version of this review included in the analysis truly unconfounded controlled clinical trials or quasi‐randomized trials, whereas only truly unconfounded controlled clinical trials were eligible for inclusion in this updated review.
In the protocol, we planned to use Embase (1980 to the search date) and MEDLINE (1966 to the search date). However, in the review, we used Embase Ovid (1974 to the search date) and MEDLINE Ovid (1946 to the search date), according to the Library of Sichuan University.
Mangmang Xu and Dan Li contributed equally to finishing this updated review and were co‐first authors.
Extensive revision of the structure and content of the review in December 2017 was in line with feedback from the Cochrane Stroke Group and the Cochrane Editorial Unit. Comparisons were restructured as (1) acupuncture versus any control (open control or sham acupuncture), and (2) acupuncture versus sham acupuncture.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Humans;
PICO

Funnel plot of comparison: 1 Acupuncture versus control, outcome: 1.1 Death or dependency at end of follow‐up.
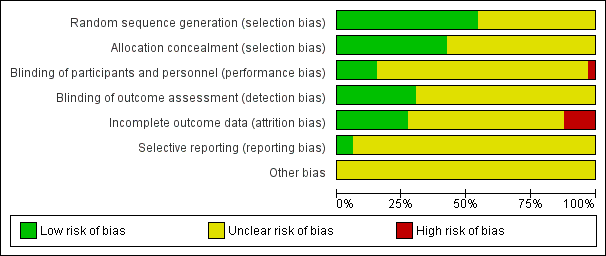
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Acupuncture versus control, Outcome 1 Death or dependency at end of follow‐up.

Comparison 1 Acupuncture versus control, Outcome 2 Death or dependency at end of follow‐up (> 3 months).
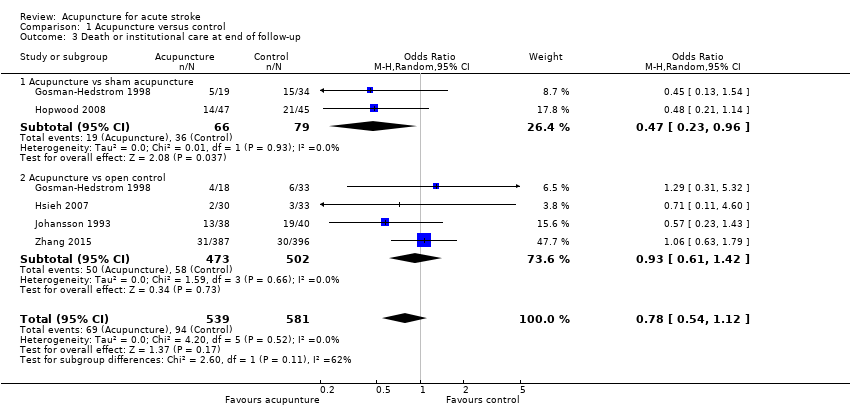
Comparison 1 Acupuncture versus control, Outcome 3 Death or institutional care at end of follow‐up.

Comparison 1 Acupuncture versus control, Outcome 4 Change in global neurological deficit score at end of treatment period.
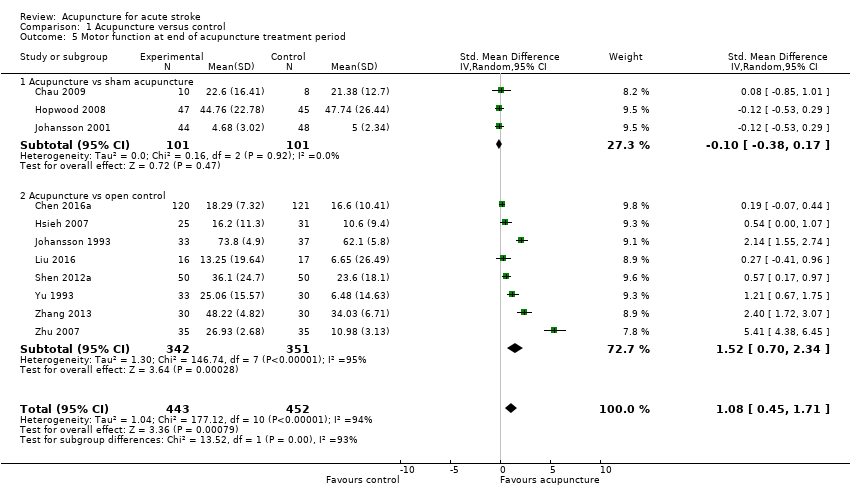
Comparison 1 Acupuncture versus control, Outcome 5 Motor function at end of acupuncture treatment period.

Comparison 1 Acupuncture versus control, Outcome 6 Motor function at end of follow‐up (> 3 months).

Comparison 1 Acupuncture versus control, Outcome 7 Death within first 2 weeks.
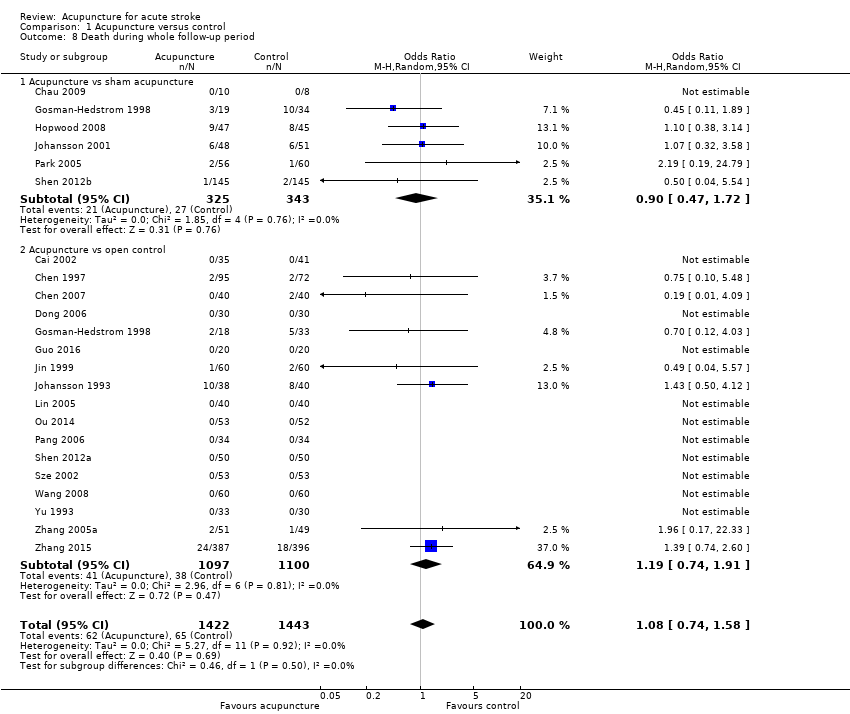
Comparison 1 Acupuncture versus control, Outcome 8 Death during whole follow‐up period.
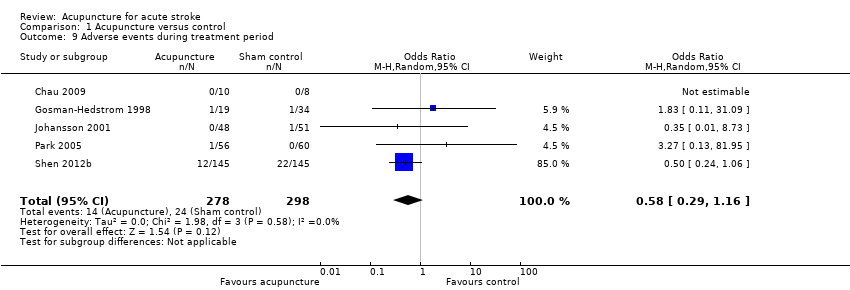
Comparison 1 Acupuncture versus control, Outcome 9 Adverse events during treatment period.
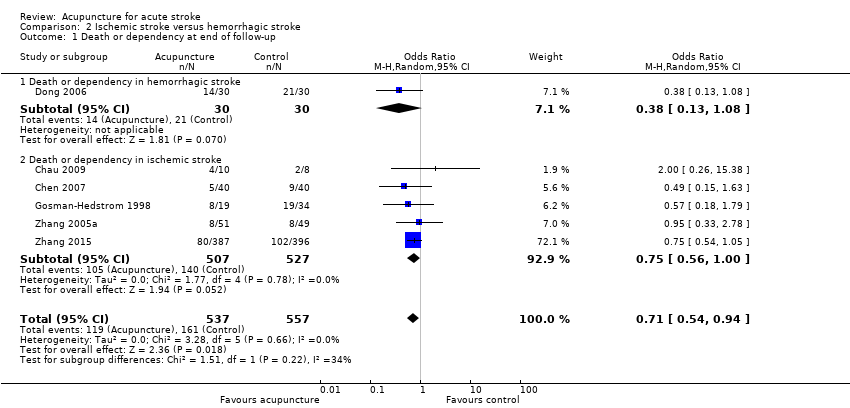
Comparison 2 Ischemic stroke versus hemorrhagic stroke, Outcome 1 Death or dependency at end of follow‐up.
| Acupuncture compared with all control for patients with acute stroke | ||||||
| Patient or population: patients with acute stroke | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Acupuncture | |||||
| Death or dependency at end of follow‐up | Study population | OR 0.61 | 1582 | ⊕⊝⊝⊝ | Dependency was defined as BI ≤ 60 (of a potential total of 100), BI ≤ 70 (of a potential total of 100), or BI ≤ 12 (of a potential total of 20). One trial used the trialists' own definition. | |
| 347 per 1000 | 245 per 1000 | |||||
| Death or dependency at end of follow‐up (> 3 months) | Study population | OR 0.67 | 1436 | ⊕⊝⊝⊝ | Dependency was defined as BI ≤ 60 (of a potential total of 100), BI ≤ 70 (of a potential total of 100), or BI ≤ 12 (of a potential total of 20). One trial used the trialists' own definition. | |
| 325 per 1000 | 244 per 1000 | |||||
| Moderate | ||||||
| 444 per 1000 | 349 per 1000 | |||||
| Death or institutional care at end of follow‐up | Study population | OR 0.78 | 1120 | ⊕⊕⊝⊝ | ||
| 162 per 1000 | 131 per 1000 | |||||
| Changes in global neurological deficit score at end of treatment period | Mean change in global neurological deficit score at end of treatment period in intervention groups was | 1086 | ⊕⊝⊝⊝ | Global neurological function was measured via modified Edinburgh‐Scandinavian Stroke Scale in 9 trials, NIHSS in 2, and SSS in 1. | ||
| Motor function at end of acupuncture treatment period | Mean motor function at end of acupuncture treatment period in intervention groups was | 895 | ⊕⊝⊝⊝ | Motor function was measured via Fugl‐Meyer Assessment in 7 trials, Motricity Index in 1, motor function score in 1, Rivermead Mobility Index in 1, and mobility index in 1. | ||
| Death within first 2 weeks | Study population | OR 0.91 | 1612 | ⊕⊕⊝⊝ | ||
| 10 per 1000 | 9 per 1000 | |||||
| Death during whole follow‐up period | Study population | OR 1.08 | 2865 | ⊕⊕⊝⊝ | ||
| 45 per 1000 | 48 per 1000 | |||||
| Adverse events related to acupuncture | See comments. | See comments. | See comments. | (13 studies) | ⊕⊕⊝⊝ | The incidence of adverse events directly related to acupuncture (such as pain, dizziness, faint) was approximately 6.17% (64/1037 participants) in the acupuncture group, and 1.35% (14/1037 participants) discontinued acupuncture. AEs related to sham acupuncture occurred in 8.0% (24/298) of participants. |
| *The basis for the assumed risk (eg, the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aOf the 33 included RCTs, the acupuncture treatment type and period were heterogeneous. The acupuncture treatment period ranged from one to three months. The acupoints varied across trials. The needling sensation could be provoked by manual stimulation or electrical stimulation. bDowngraded one level for serious inconsistency: variation in the definition of dependency and acupuncture treatment type and duration. cDowngraded two levels for very serious risk of bias: Among the 11 included trials, eight had risk of performance bias and seven had risk of detection bias; the result was not consistent with the sensitivity analysis using only sham controls. dDowngraded two levels for very serious risk of bias: Among the eight included trials, six had risk of performance bias and four had risk of detection bias; the result was not consistent with the sensitivity analysis using only sham controls. eDowngraded two levels for very serious risk of bias: Among the five included trials, four had risk of performance bias; the result was not consistent with the sensitivity analysis using only sham controls. fDowngraded two levels for very serious inconsistency: considerable statistical heterogeneity (I2 > 50%) and variation in acupuncture treatment type and duration. gDowngraded two levels for very serious risk of bias: Among the 13 included trials, at least eight trials had risk of allocation bias, performance bias, or detection bias; the result was not consistent with the sensitivity analysis using only sham controls. hDowngraded two levels for very serious risk of bias: Among the 11 included trials, at least six had risk of allocation bias, performance bias, or detection bias; the result was not consistent with the sensitivity analysis using only sham controls. iDowngraded two levels for very serious risk of bias: Among the 18 included trials, at least 10 trials had risk of allocation bias, performance bias, or detection bias; the result was not consistent with the sensitivity analysis using only sham controls. jDowngraded two levels for very serious risk of bias: Among the 22 included trials, at least 11 trials had risk of allocation bias, performance bias, or detection bias; the result was not consistent with the sensitivity analysis using only sham controls. kDowngraded two levels for very serious inconsistency: variation between trials in reporting of adverse events and in acupuncture treatment type and duration. | ||||||
| Acupuncture compared with sham control for patients with acute stroke | ||||||
| Patient or population: patients with acute stroke | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Acupuncture | |||||
| Death or dependency at end of follow‐up | Study population | OR 0.71 | 262 | ⊕⊕⊝⊝ | ||
| 464 per 1000 | 384 per 1000 | |||||
| Death or dependency at end of follow‐up (> 3 months) | Study population | OR 0.67 | 244 | ⊕⊕⊝⊝ | ||
| 476 per 1000 | 376 per 1000 | |||||
| Death or institutional care at end of follow‐up | Study population | OR 0.47 | 145 | ⊕⊕⊝⊝ | ||
| 456 per 1000 | 286 per 1000 | |||||
| Changes in global neurological deficit score at end of treatment period | Mean change in global neurological deficit score at end of treatment period in intervention groups was | 53 | ⊕⊕⊝⊝ | |||
| Motor function at end of acupuncture treatment period | Mean motor function at end of acupuncture treatment period in intervention groups was | 202 | ⊕⊕⊝⊝ | |||
| Death within first 2 weeks | Study population | OR 1.20 | 378 | ⊕⊕⊝⊝ | ||
| 15 per 1000 | 4 per 1000 | |||||
| Death during whole follow‐up period | Study population | OR 0.90 | 668 | ⊕⊕⊝⊝ | ||
| 79 per 1000 | 79 per 1000 | |||||
| Adverse events related to acupuncture | See comments. | See comments. | OR 0.58 (0.29 to 1.16) | 576 (5 studies) | ⊕⊕⊝⊝ | The incidence of adverse events directly related to acupuncture (such as pain, dizziness, faint) was approximately 8.0% (24/298) in sham acupuncture patients. |
| *The basis for the assumed risk (eg, the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aOf the 33 included RCTs, the acupuncture treatment type and period were heterogeneous. The treatment period for acupuncture ranged from one to three months. Acupoints varied across trials. The needling sensation could be provoked by manual stimulation or electrical stimulation. bDowngraded one level for serious imprecision: small number of studies and wide confidence intervals. cDowngraded one level for serious risk of bias: Among the four included trials, two trials had risk of performance bias or attrition bias. dDowngraded one level for serious risk of bias: Among the three included trials, one trial had risk of performance bias. eDowngraded one level for serious risk of bias: Among the two included trials, one trial had risk of performance bias. fDowngraded two levels for very serious imprecision: single study and very wide confidence intervals. gDowngraded one level for serious risk of bias: Among the three included trials, at least two trials had risk of performance bias or attrition bias. hDowngraded one level for serious risk of bias: Among the five included trials, at least two trials had risk of performance bias or attrition bias. iDowngraded one level for serious risk of bias: Among the six included trials, at least two trials had risk of performance bias or attrition bias. jDowngraded one level for serious inconsistency: Reporting of adverse events varied between trials. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Death or dependency at end of follow‐up Show forest plot | 11 | 1582 | Odds Ratio (M‐H, Random, 95% CI) | 0.61 [0.46, 0.79] |
| 1.1 Acupuncture vs sham acupuncture | 4 | 262 | Odds Ratio (M‐H, Random, 95% CI) | 0.71 [0.43, 1.18] |
| 1.2 Acupuncture vs open control | 8 | 1320 | Odds Ratio (M‐H, Random, 95% CI) | 0.55 [0.37, 0.80] |
| 2 Death or dependency at end of follow‐up (> 3 months) Show forest plot | 8 | 1436 | Odds Ratio (M‐H, Random, 95% CI) | 0.67 [0.53, 0.85] |
| 2.1 Acupuncture vs sham acupuncture | 3 | 244 | Odds Ratio (M‐H, Random, 95% CI) | 0.67 [0.40, 1.12] |
| 2.2 Acupuncture vs open control | 6 | 1192 | Odds Ratio (M‐H, Random, 95% CI) | 0.62 [0.42, 0.93] |
| 3 Death or institutional care at end of follow‐up Show forest plot | 5 | 1120 | Odds Ratio (M‐H, Random, 95% CI) | 0.78 [0.54, 1.12] |
| 3.1 Acupuncture vs sham acupuncture | 2 | 145 | Odds Ratio (M‐H, Random, 95% CI) | 0.47 [0.23, 0.96] |
| 3.2 Acupuncture vs open control | 4 | 975 | Odds Ratio (M‐H, Random, 95% CI) | 0.93 [0.61, 1.42] |
| 4 Change in global neurological deficit score at end of treatment period Show forest plot | 12 | 1086 | Std. Mean Difference (IV, Random, 95% CI) | 0.84 [0.36, 1.32] |
| 4.1 Acupuncture vs sham acupuncture | 1 | 53 | Std. Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.55, 0.57] |
| 4.2 Acupuncture vs open control | 12 | 1033 | Std. Mean Difference (IV, Random, 95% CI) | 0.91 [0.41, 1.41] |
| 5 Motor function at end of acupuncture treatment period Show forest plot | 11 | 895 | Std. Mean Difference (IV, Random, 95% CI) | 1.08 [0.45, 1.71] |
| 5.1 Acupuncture vs sham acupuncture | 3 | 202 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.38, 0.17] |
| 5.2 Acupuncture vs open control | 8 | 693 | Std. Mean Difference (IV, Random, 95% CI) | 1.52 [0.70, 2.34] |
| 6 Motor function at end of follow‐up (> 3 months) Show forest plot | 3 | 186 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.21, 0.37] |
| 6.1 Acupuncture vs sham acupuncture | 2 | 144 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.35, 0.31] |
| 6.2 Acupuncture vs open control | 1 | 42 | Std. Mean Difference (IV, Random, 95% CI) | 0.44 [‐0.18, 1.05] |
| 7 Death within first 2 weeks Show forest plot | 18 | 1612 | Odds Ratio (M‐H, Random, 95% CI) | 0.91 [0.33, 2.55] |
| 7.1 Acupuncture vs sham acupuncture | 5 | 378 | Odds Ratio (M‐H, Random, 95% CI) | 1.20 [0.27, 5.26] |
| 7.2 Acupuncture vs open control | 14 | 1234 | Odds Ratio (M‐H, Random, 95% CI) | 0.71 [0.17, 2.96] |
| 8 Death during whole follow‐up period Show forest plot | 22 | 2865 | Odds Ratio (M‐H, Random, 95% CI) | 1.08 [0.74, 1.58] |
| 8.1 Acupuncture vs sham acupuncture | 6 | 668 | Odds Ratio (M‐H, Random, 95% CI) | 0.90 [0.47, 1.72] |
| 8.2 Acupuncture vs open control | 17 | 2197 | Odds Ratio (M‐H, Random, 95% CI) | 1.19 [0.74, 1.91] |
| 9 Adverse events during treatment period Show forest plot | 5 | 576 | Odds Ratio (M‐H, Random, 95% CI) | 0.58 [0.29, 1.16] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Death or dependency at end of follow‐up Show forest plot | 6 | 1094 | Odds Ratio (M‐H, Random, 95% CI) | 0.71 [0.54, 0.94] |
| 1.1 Death or dependency in hemorrhagic stroke | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 0.38 [0.13, 1.08] |
| 1.2 Death or dependency in ischemic stroke | 5 | 1034 | Odds Ratio (M‐H, Random, 95% CI) | 0.75 [0.56, 1.00] |


