Éthosuximide, valproate de sodium ou lamotrigine dans le traitement de l'absence épileptique chez les enfants et adolescents
Résumé scientifique
Contexte
Ceci est une version mise à jour de la revue Cochrane originale publiée dans le numéro 3 en 2003.
L'absence épileptique se caractérise par des crises épileptiques de courte durée qui se manifestent pendant l'enfance et l'adolescence. Elles entraînent une perte soudaine de conscience, et l'électroencéphalogramme (EEG) montre généralement des décharges pointes‐ondes à raison de trois cycles par seconde. L'éthosuximide, le valproate et la lamotrigine sont actuellement utilisés dans le traitement de l'absence épileptique. L'objectif de cette revue était d'identifier l'anticonvulsivant le plus efficace chez l'enfant atteint d'absence épileptique typique.
Objectifs
Examiner les preuves d'effets de l'éthosuximide, du valproate et de la lamotrigine dans le traitement des enfants et adolescents atteints d'absence épileptique par rapport à un placebo ou les uns par rapport aux autres.
Stratégie de recherche documentaire
Nous avons consulté le registre spécialisé du groupe Cochrane sur l'épilepsie (novembre 2009), le registre Cochrane des essais contrôlés (CENTRAL) (Bibliothèque Cochrane, numéro 4, 2009), MEDLINE (de 1950 à la 3ème semaine de novembre 2009) et EMBASE (1988 à mars 2005). Aucune restriction de langue n'a été imposée. Nous avons également contacté Sanofi Winthrop, Glaxo Wellcome (aujourd'hui GlaxoSmithKline) et Parke Davis (aujourd'hui Pfizer), fabricants du valproate de sodium, de la lamotrigine et de l'éthosuximide, respectivement.
Critères de sélection
Les essais randomisés en groupes parallèles portant sur une monothérapie ou un traitement d'appoint et comparant n'importe lesquels des traitements suivants chez les enfants et les adolescents atteints d'absence épileptique : éthosuximide ; valproate de sodium ; lamotrigine ou placebo.
Recueil et analyse des données
Les mesures de résultats étaient les suivantes : (1) nombre de patients sans crise à 1, 3, 6, 12 et 18 mois post‐randomisation ; (2) nombre de patients présentant une réduction d'au moins 50 % de la fréquence des crises ; (3) normalisation de l'EEG et/ou test d'hyperventilation négatif et (4) effets indésirables. Les données ont été extraites par deux auteurs de revue de manière indépendante. Les résultats sont présentés sous forme de risques relatifs (RR) avec des intervalles de confiance à 95 % (IC à 95 %).
Résultats principaux
Cinq petits essais ont été identifiés, dont quatre étaient de faible qualité méthodologique. Un essai (29 participants) comparait de la lamotrigine à un placebo et utilisait un plan de type conditionné par la réponse. Dans cet essai de courte durée, les patients prenant de la lamotrigine étaient significativement plus susceptibles de ne plus présenter de crises par rapport aux participants recevant un placebo. Un autre essai comparait de la lamotrigine à du valproate de sodium mais sa puissance statistique était insuffisante pour détecter des différences en termes d'efficacité. Trois études examinaient de l'éthosuximide, mais nous avons décidé de ne pas combiner les résultats en une méta‐analyse en raison de la diversité des plans d'étude et des populations étudiées. Aucune de ces études ne rapportait de différence entre le valproate et l'éthosuximide en termes de contrôle des crises, mais les intervalles de confiance étaient larges et l'existence de différences importantes ne peut pas être exclue.
Conclusions des auteurs
Bien que l'éthosuximide, la lamotrigine et le valproate soient couramment utilisés dans le traitement des patients atteints d'absence épileptique, les preuves sont insuffisantes pour orienter la pratique clinique, et les quelques essais inclus dans cette revue étaient de faible qualité méthodologique et présentaient un effectif réduit. D'autres essais de meilleure qualité sont nécessaires.
PICO
Résumé simplifié
Éthosuximide, valproate de sodium ou lamotrigine dans le traitement de l'absence épileptique chez les enfants et adolescents
Les preuves sont insuffisantes pour identifier les médicaments les plus efficaces dans le traitement des crises épileptiques chez les enfants et adolescents atteints d'absence épileptique.
L'épilepsie est un trouble associé à des crises causées par des décharges électriques anormales dans le cerveau. L'absence épileptique se caractérise par des crises entraînant une perte soudaine de conscience. Elle se manifeste souvent dès l'enfance ou l'adolescence. Trois antiépileptiques sont souvent utilisés dans le traitement de l'absence épileptique : valproate; l'éthosuximide et la lamotrigine. Le valproate peut entraîner une prise de poids et pourrait provoquer des anomalies fœtales. Cette revue a identifié des preuves indiquant que les patients prenant de la lamotrigine étaient plus susceptibles de ne plus présenter de crises que ceux recevant un placebo. Aucune différence n'était observée entre le valproate et l'éthosuximide en termes d'efficacité, mais des recherches supplémentaires sont nécessaires.
Authors' conclusions
Background
This review is an update of a review originally published in the Cochrane Database of Systematic Reviews (2003, Issue 3; Posner 2003), and updated in 2005, Issue 4; Posner 2005b) on 'Ethosuximide, sodium valproate or lamotrigine for absence seizures in children and adolescents'.
Absence seizures (AS) are brief epileptic seizures characterised by sudden loss of awareness. Depending on clinical features and electroencephalogram (EEG) findings, they are divided into typical AS, atypical AS, and AS with special features (Berg 2010; Tenney 2013). About 10% of seizures in children with epilepsy are typical AS. Typical AS are associated with an EEG showing regular generalised and symmetrical spike and slow wave complexes at a frequency of three cycles per second at the same time as the absence. Childhood seizure disorders are classified into syndromes, which take into account seizure types, age and EEG changes. Typical AS may be the only seizure type experienced by a child and this then constitutes either an epileptic syndrome called childhood absence epilepsy or juvenile absence epilepsy. However, AS may also be only one of multiple types of seizures, for example in juvenile myoclonic epilepsy where myoclonic and tonic‐clonic seizures occur as well as AS. Atypical AS are characterised by less abrupt onset and offset, longer duration, changes in muscular tone, and variable impairment of consciousness; they are associated with interictal 1.5‐2.5 Hz irregular, asymmetrical spike and wave complexes on the EEG, and with diffuse, irregular slow spike and wave as ictal pattern. The 2010 revised International League Against Epilepsy (ILAE) Report on Terminology and Classification has recently recognised two additional types of AS, which are associated with special features: myoclonic AS and eyelid myoclonia with absence (EMA) (Berg 2010). Seizures occurring in EMA are clinically associated with jerkings of the eyelids with upward eye‐deviation, which are usually triggered by eye closure; the ictal EEG shows 3‐6 Hz generalised polyspike and wave complexes, sometimes associated with occipital paroxysmal discharges.
Non‐systematic reviews have suggested that ethosuximide and sodium valproate are equally effective (Duncan 1995). Valproate is considered the drug of choice in juvenile myoclonic epilepsy (Chadwick 1987; Christe 1989), although there is little in the way of evidence from randomised controlled trials to support this. Lamotrigine used to be considered a second‐line drug, reserved for intractable AS (Duncan 1995), but its use has increased with time. It is especially valued in situations where sodium valproate leads to weight gain and also for women of childbearing age. The latter is due to fears of a higher rate of fetal abnormalities in pregnancies exposed to valproate (Moore 2000). Preliminary studies suggested that lamotrigine may become the first‐line drug in AS (Buoni 1999). This review aims to determine the best choice of anticonvulsant for children and adolescents with AS by reviewing the information available from randomised controlled trials.
Objectives
To review the evidence for the effects of ethosuximide, valproate and lamotrigine as treatments for children and adolescents with typical absence seizures (AS), when compared with placebo or each other.
Methods
Criteria for considering studies for this review
Types of studies
-
Randomised parallel group monotherapy or add‐on trials which include a comparison of any of the following in children or adolescents with typical AS: ethosuximide; sodium valproate; lamotrigine and placebo.
-
The studies should have used either adequate or quasi‐randomised methods (e.g. allocation by day of week).
-
Blinded and unblinded studies.
Types of participants
Children or adolescents (up to 16 years of age) with typical AS.
Types of interventions
Sodium valproate, ethosuximide or lamotrigine as monotherapy or add‐on treatment. These drugs may be compared with placebo or with one another.
Types of outcome measures
-
Proportion of participants seizure free at one, three, six, 12 and 18 months after randomisation.
-
Fifty per cent or greater reduction in the frequency of seizures.
-
Normalisation of EEG and/or negative hyperventilation test.
-
Incidence of adverse effects.
Search methods for identification of studies
Electronic searches
Searches were run for the original review in March 2003 and subsequent searches were run in March 2005, July 2007, November 2009, August 2011, March 2014, and December 2015.
For the latest update we searched:
-
the Cochrane Epilepsy Group Specialized Register (1 September 2016) using the search strategy shown in Appendix 1;
-
(the Cochrane Central Register of Controlled Trials (CENTRAL) via the Cochrane Register of Studies Online (CRSO, 1 September 2016) using the search strategy shown in Appendix 2;
-
MEDLINE (Ovid, 1946 to 1 September 2016) using the search strategy shown in Appendix 3;
-
ClinicalTrials.gov (1 September 2016) using the search strategy shown in Appendix 4;
-
WHO International Clinical Trials Registry Platform ICTRP (1 September 2016) using the search strategy shown in Appendix 5.
Previously we searched Embase (1988 to March 2005). Subsequently, as we no longer had access to Embase, we searched SCOPUS (1823 to 31 March 2014) as a substitute using the search strategy shown in Appendix 6. These databases have not been searched again, because randomised and quasi‐randomised controlled trials in Embase are now included in CENTRAL
There were no language restrictions.
Searching other resources
We contacted Sanofi Winthrop, Glaxo Wellcome (now GlaxoSmithKline) and Parke Davis (now Pfizer), manufacturers of sodium valproate, lamotrigine and ethosuximide, respectively. We also reviewed any references of identified studies and retrieved any relevant studies.
Data collection and analysis
Two review authors (Francesco Brigo and Stanley Igwe) independently assessed trials for inclusion and disagreements were resolved by discussion. The same two review authors independently extracted data from trial reports.
We extracted the following data from the studies that met our inclusion criteria:
-
study design;
-
method of randomisation concealment;
-
method of blinding;
-
whether any participants had been excluded from reported analyses;
-
duration of treatment;
-
outcome measures;
-
participant data (total number of individuals allocated to each treatment group, age of participants, naive participants versus selected groups, individuals with other types of seizures co‐existing with typical absence seizures);
-
results (success rate and adverse effects).
Data analysis
The data for our chosen outcomes are dichotomous and our preferred outcome statistic was the risk ratio. We assessed clinical heterogeneity by comparing trial design, participant population and outcomes across trials. We assessed statistical heterogeneity using a Chi2 test for heterogeneity. Provided we thought it clinically appropriate, and no important heterogeneity was found, we planned to summarise results in a meta‐analysis. However, because of the methodological problems outlined below it was not possible to perform meta‐analysis of the data from the studies that fulfilled the inclusion criteria. The large difference in the length of follow‐up and timing of analysis was a particular problem. Further research could allow results to be pooled, leading to a quantitative rather than a qualitative summary of results.
Results
Description of studies
See Figure 1.
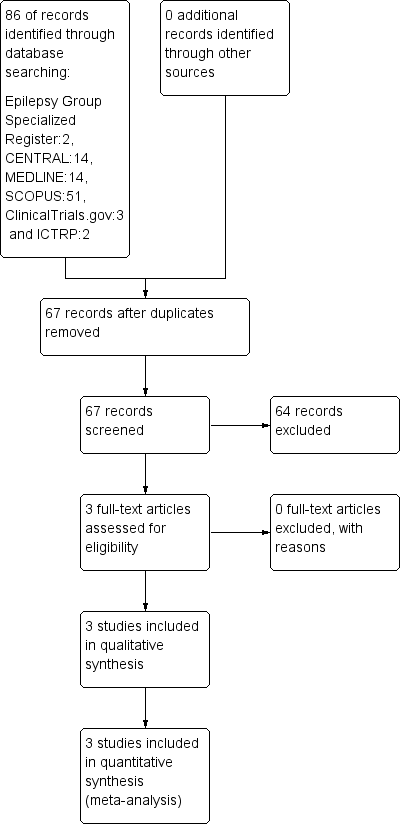
Study flow diagram (results refer only to the updated version of the review).
The updated search strategy described above yielded 86 results (two Epilepsy Specialized Register, 14 CENTRAL, 14 MEDLINE, 51 SCOPUS, three ClinicalTrials.gov, and two ICTRP). After removing 19 duplicates, one publication already in review, and 26 obviously irrelevant items, we assessed 40 articles for possible inclusion. Two randomised controlled trials (Huang 2009; Glauser 2013a) identified in the updated search strategy were eventually included in this updated review. Two studies awaiting classification in the previous version of this review (Suzuki 1972; Basu 2005) were reconsidered for possible inclusion. The study by Basu (Basu 2005) was incorporated into the updated review as an included study, whereas the study by Suzuki (Suzuki 1972), was excluded as it was not randomised. Hence, three randomised controlled trials (Basu 2005; Huang 2009; Glauser 2013a) were eventually included in this updated review.
Callaghan 1982 (Callaghan 1982)
This was a randomised, parallel open study, which compared monotherapy with ethosuximide and sodium valproate. Ethosuximide was initially given at 250 mg/day and, whenever required, incremented by 250 mg to a maximum of 1500 mg/day. Valproate was started at 400 mg/day and, if deemed necessary, gradually incremented by 200 mg up to 2400 mg/day. Participants (total 28) had typical absence seizures, were between four and 15 years, and were previously untreated. Follow‐up ranged from 18 months to four years. The report acknowledged support from Warner‐Lambert Pharmaceuticals, manufacturers of ethosuximide.
Sato 1982 (Sato 1982)
This study used a complex response conditional design and recruited drug naive as well as participants already on treatment, with a total of 45 participants recruited. In the first phase of this trial, participants were randomised to receive either valproate (and placebo) or ethosuximide (and placebo) and followed up for six weeks. Participants responding to randomised treatment continued with the randomised drug for a further six weeks. Responders included previously untreated participants who became seizure free and participants who had been previously treated and had an 80% or greater reduction in AS frequency. Non‐responders and those with adverse effects were crossed over to the alternative treatment and followed up for a further six weeks. The age range of participants was three to 18 years. Apart from absence seizures some participants also had other types of seizures. The report does not specify if the absence seizures were typical or atypical. Some of the participants were drug naive and some drug resistant. Participants of the study were selected from those who attended epilepsy clinic at the Clinical Research Center, University of Virginia Hospital, USA. The work was supported by a contract from the Institute of Neurological and Communicative Disorders and Stroke (NINCDS).
Martinovic 1983 (Martinovic 1983)
This was a parallel, open design study comparing ethosuximide and sodium valproate. Participants were between five and eight years old with a recent (less than six weeks) onset of seizures. All participants (total 20) had 'simple absences' and were followed up for one to two years. Six individuals did not co‐operate and were therefore not included in the analysis. No information about sponsorship by a pharmaceutical company is given.
Frank 1999 (Frank 1999)
This was a double‐blind study using a 'responder enriched' design. Participants (total 29) had newly diagnosed typical absence seizures and were aged between three to 15 years. Prior to randomisation, all participants received treatment with lamotrigine. After four weeks or more of treatment, participants who were seizure free and had a negative 24‐hour EEG with hyperventilation, were randomised to either continue lamotrigine or to placebo and were followed up for four weeks. This study was sponsored by Glaxo Wellcome (now GlaxoSmithKline), makers of lamotrigine.
Coppola 2004 (Coppola 2004)
This was a randomised, parallel group unblinded study comparing lamotrigine and sodium valproate. All participants (n = 38) were drug naive, aged three to 13 years old with typical absence seizures. The follow‐up time was 12 months. The primary outcome measure was total seizure freedom, measured at one, three and 12 months. This study was not sponsored by any commercial organisation.
Basu 2005 (Basu 2005)
Results of this study were published as an abstract. We contacted the main author of this study via email three times (30 October and 4 November 2015, and 7 January 2016) asking for further information; we did not receive a reply. This was a randomised, open‐label, parallel group design comparing sodium valproate with lamotrigine used in monotherapy for treatment of typical absence seizures (diagnosed clinically and by EEG support). Thirty patients were included (males 16; females 14 – age between five and 14 years). Patients with other comorbidities were excluded. Fifteen patients were randomly allocated to receive valproate and 15 to receive lamotrigine. The follow‐up was 12 months. The primary outcome was seizure freedom and no EEG evidence of seizure. Drug dosages were not explicitly reported. The dosages were escalated according to the clinical response, starting from a low dose. Lamotrigine was titrated very slowly at two‐weekly intervals to avoid unwanted side effects (maximum 10 mg/kg/day). After one month of treatment nine patients (60%) receiving valproate and none (0%) receiving lamotrigine were seizure free. After three months, 11 patients (73.3%) in the sodium valproate and eight patients (53.3%) in the lamotrigine group receiving lamotrigine were seizure free. After 12 months, 12 patients (80%) receiving sodium valproate and 10 patients (66.6%) treated with lamotrigine were seizure free (P > 0.05). Minimal adverse events (not explicitly reported) were observed in 26.6% of patients treated with sodium valproate and in 20% of patients receiving lamotrigine. No dropouts were observed. No information on sponsorship by pharmaceutical company was available.
Huang 2009 (Huang 2009)
This study (Huang 2009), compared valproate with lamotrigine monotherapy in drug naive children (n = 48, six to 10 years) with newly diagnosed childhood AS (typical seizures). Included patients were 17 male and 31 female (no detailed descriptions in each group respectively). The follow‐up time was 12 months. The outcome measure was total seizure freedom, measured at one, three, six and 12 months. Complete normalisation of EEG with seizure freedom and occurrence of adverse effects were also considered. In the valproate group, sustained release tablets or oral solution were administered twice daily (totally 15 mg/kg per day); in case of persisting seizures after one week, the dose was increased to 20 mg/kg per day, twice daily (maximum dose daily 30 mg/kg). In case of persisting seizures despite a maximum dose of 30 mg/kg within a month, combination with lamotrigine 0.15 mg/kg daily to 2 mg to 5 mg/kg was administrated. In the lamotrigine group, patients received a starting dose of lamotrigine of 0.5 mg/kg daily, administered twice, increased to 0.15 mg/kg per two weeks. The daily maintenance dose was 2 mg to 5 mg/kg, and the maximum daily dose 10 mg/kg. In case of persisting seizures despite a maximum dose within a month, combination with valproate 10 mg/kg daily to 20 mg/kg was administrated. No information on sponsorship by pharmaceutical company was available.
Glauser 2013 (Glauser 2013a)
This was a randomised, parallel double‐blind controlled trial comparing ethosuximide, lamotrigine and sodium valproate in children with newly diagnosed childhood absence epilepsy. The study designed included also a partial cross‐over to open‐label (at treatment failure only) with subsequent follow‐up: participants reaching a treatment failure criterion in the double‐blind treatment phase were given the opportunity to enter into the open‐label phase, during which participants were randomised to one of the two other antiepileptic drugs. Participants (total 453 enrolled) had typical absence seizure, were between seven months and 12 years 11 months, and were previously untreated. Among the 453 patients enrolled, seven were withdrawn, hence 446 participants were included in subsequent effectiveness analyses and 451 participants included in the safety analyses. Follow‐up was up to 12 months. Study drugs were titrated as tolerated in predetermined increments every one to two weeks over 16 weeks. Ethosuximide and valproic acid doses were incremented of 5 mg to 10 mg/kg/day at intervals of two weeks, whilst lamotrigine doses were incremented of 0.3 mg to 0.6 mg/kg/day at intervals of two weeks. The maximal target doses were ethosuximide 60 mg/kg/day or 2000 mg/day (whichever was lower), valproic acid 60 mg/kg/day or 3000 mg/day (whichever was lower), and lamotrigine 12 mg/kg/day or 600 mg/day (whichever was lower). The main effectiveness outcome was the freedom from treatment failure assessed 12 months after randomisation. Freedom from treatment failure was also assessed at 16 to 20 weeks. Treatment failure was defined as failure either due to lack of seizure control, or meeting safety exit criteria, or withdrawal from the study for any other reason. This study was not sponsored by any commercial organisation.
Risk of bias in included studies
See Figure 2; Figure 3; Characteristics of included studies.

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Results of one study (Basu 2005) were published as an abstract. Despite several attempts to contact the research authors to obtain more information on methodological issues and risk of bias, we received no reply. Thus, for this study there is an unclear risk of bias.
Three of the included studies (Callaghan 1982; Sato 1982; Martinovic 1983) date back 30 years and there was an obvious difference in the quality of the reporting in comparison with the newer studies (Frank 1999; Coppola 2004; Huang 2009; Glauser 2013a). Only two of the studies described explicitly the methods of allocation concealment (Coppola 2004; Glauser 2013a). The studies reported by Sato (Sato 1982), Frank (Frank 1999), and Glauser (Glauser 2013a) were double‐blinded, whilst the studies reported by Martinovic (Martinovic 1983), Callaghan (Callaghan 1982), Coppola (Coppola 2004), and Huang (Huang 2009) were unblinded. In two out of the three double‐blinded studies, placebo and active drugs were indistinguishable (Frank 1999; Glauser 2013a). Five studies described losses to follow‐up or exclusions from analyses. Frank 1999 reports that one participant withdrew consent before treatment but after randomisation and that one participant did not comply but was included in the analysis. Martinovic 1983 reports that six of the initially recruited participants did not co‐operate and were not included in the analysis. Coppola 2004 reports loss of nine patients overall, all due to lack of efficacy, these patients exited the study at three months follow‐up; all randomised patients were included in the analysis. Huang 2009 reports that one patient in the valproate group was lost to follow‐up (no further specifications), whereas two patients in the lamotrigine group were withdrawn due to severe adverse effects (systemic anaphylaxis rash). Glauser 2013a reports that among the 453 patients enrolled, seven were withdrawn due to ineligibility at baseline, so that 446 participants were included in subsequent effectiveness analyses and 451 participants in safety analyses. Two reports (Callaghan 1982; Sato 1982) did not make an explicit statement that participants were not lost to follow‐up or excluded from analyses. Whilst most studies are specified as being funded by a pharmaceutical company or not, two studies (Basu 2005; Huang 2009) did not explicitly report such information.
Effects of interventions
Lamotrigine versus placebo
We found one study (Frank 1999) comparing lamotrigine with placebo which recruited 29 participants. As outlined in Description of studies above, this trial used a responder‐enriched design where participants responding to lamotrigine during a pre‐randomisation baseline phase were randomised to continue lamotrigine or have it withdrawn. This trial therefore compares the effect of continuing versus withdrawing lamotrigine. The results were as follows: in the initial open‐label dose‐escalation phase, 71% of the participants became seizure free on lamotrigine using a 24‐hour EEG/video telemetry recording; in the placebo controlled phase 64% of the participants on lamotrigine remained seizure free versus 21% receiving placebo (P < 0.03).
Valproate versus placebo
We found no trials comparing valproate versus placebo.
Ethosuximide versus placebo
We found no trials comparing ethosuximide versus placebo.
Valproate versus ethosuximide
We found four studies comparing valproate with ethosuximide (Callaghan 1982; Sato 1982; Martinovic 1983; Glauser 2013a). Due to differences in study design, participants and length of follow‐up we did not think it appropriate to pool results in a meta‐analysis. For our chosen outcome 'seizure freedom', we were unable to extract data for this outcome at the time points we had specified (one, six and 18 months). Rather than not present any data for this outcome, we have summarised results for individual trials, where the proportion of participants seizures free during follow‐up was reported. Results for individual studies are presented below as well as in meta‐view tables.
(1) Seizure freedom
The risk ratio (RR) estimates with 95% confidence intervals (CI) for seizure freedom (RR < 1 favours ethosuximide) are:
(a) Callaghan 1982: RR 0.70 (95% CI 0.32 to 1.51); seizure freedom was observed in six out of 15 patients receiving valproate and in eight out of 14 patients receiving ethosuximide.
(b) Sato 1982: RR 1.93 (95% CI 0.87 to 4.25); the proportion of patients achieving seizure freedom in both groups is not explicitly reported.
(c) Martinovic 1983: RR 0.88 (95% CI 0.53 to 1.46); seizure freedom was observed in seven out of 10 patients receiving valproate and in eight out of 10 patients receiving ethosuximide.
(d) Glauser 2013a: RR 0.96 (95% CI 0.75 to 1.24); seizure freedom was observed in 64 out of 146 patients receiving valproate and in 70 out of 154 patients receiving ethosuximide.
Hence, none of these trials found a difference for this outcome. However, confidence intervals are all wide and the possibility of important differences has not been excluded and equivalence cannot be inferred.
(2) 80% or greater reduction in seizure frequency
This outcome was only reported by Sato 1982, and the RR was 0.70 (95% CI 0.19 to 2.59); the proportion of patients achieving 80% or greater reduction in seizure frequency in both groups was not explicitly reported. Again, no difference was found, but the confidence interval is wide and equivalence cannot be inferred.
(3) 50% or greater reduction in seizure frequency
This was reported for two trials. In one trial (Martinovic 1983) all participants achieved this outcome (10/10 in the valproate and 10/10 in the ethosuximide group). For the other trial (Callaghan 1982) the RR was 1.02 (95% CI 0.70 to 1.48); 12 out of 15 patients receiving valproate and 11 out of 14 patients receiving ethosuximide experienced 50% or greater reduction in seizure frequency. Again, no difference is found, but the confidence interval is wide and equivalence cannot be inferred.
Valproate versus lamotrigine
We found four studies comparing valproate with lamotrigine (Coppola 2004; Basu 2005; Huang 2009; Glauser 2013a). Due to differences in study design, participants and length of follow‐up we did not think it appropriate to pool results in a meta‐analysis. For our chosen outcome 'seizure freedom', we were unable to extract data for this outcome at the time points we had specified (one, six and 18 months). Rather than not present any data for this outcome, we have summarised results for individual trials, where the proportion of participants seizures free during follow‐up was reported. Results for individual studies are presented below as well as in meta‐view tables.
(1) Seizure freedom at 12 months
This outcome was reported for four trials (Coppola 2004; Basu 2005; Huang 2009; Glauser 2013a). The relative risk (RR) estimates with 95% confidence intervals (CI) for seizure freedom (RR < 1 favours lamotrigine) at 12 months are:
(a) Coppola 2004: 1.30 (95% CI 0.77 to 2.20);
(b) Basu 2005: 1.20 (95% CI 0.77 to 1.86);
(b) Huang 2009: 1.36 (95% CI 0.86 to 2.13);
(b) Glauser 2013a: 2.06 (95% CI 1.44 to 2.97)
Hence, none of these trials found a difference for this outcome. However, confidence intervals are all wide and the possibility of important differences has not been excluded and equivalence cannot be inferred.
One study (Coppola 2004) comparing valproate and lamotrigine head‐to‐head, recruited drug naive children with typical absence seizures. The primary outcome measure was total seizure freedom and was assessed at one, three and 12 months. At one month follow‐up 52.6% of patients taking valproate (10 out of 19) were seizure free compared to only 5.3% of patients taking lamotrigine (1 out of 19) (P = 0.004). With the passage of time increasingly more patients responded to lamotrigine. At three months seizure freedom was observed in 12 out of 19 (63.1%) patients taking sodium valproate and in seven out of 19 (36.8%) patients taking lamotrigine (P = 0.19). At the last observation at 12 months follow‐up, 13/19 (68.4%) patients taking sodium valproate and 10(19 (52.6%) taking lamotrigine were seizure free (P = 0.51).
One study (Basu 2005) compared sodium valproate with lamotrigine in patients with typical absence in a randomised, open‐label, parallel group design. After one month of treatment nine patients (60%) receiving valproate and none (0%) receiving lamotrigine were seizure free. After three months, 11 patients out of 15 (73.3%) in the sodium valproate and eight patients out of 15 (53.3%) in the lamotrigine group receiving lamotrigine were seizure free. After 12 months 12 patients out of 15 (80%) receiving sodium valproate and 10 patients out of 15 (66.6%) treated with lamotrigine were seizure free (P > 0.05).
One study (Huang 2009) compared valproate with lamotrigine monotherapy in drug naive children with newly diagnosed childhood absence seizures (typical seizures). At 12 months, 17 patients out of 24 (71%) in the valproate group and 12 out of 24 patients (50%) in the lamotrigine group achieved seizure freedom. Detailed data on seizure freedom at one, three, six and 12 months are reported in meta‐view tables.
One study (Glauser 2013a) compared valproate and lamotrigine in drug naive patients with childhood absence seizures. The main effectiveness outcome was the freedom from treatment failure assessed 12 months after randomisation. Freedom from treatment failure was also assessed at 16 to 20 weeks, and in between 16 and 20 weeks and month 12. Treatment failure was defined as failure either due to lack of seizure control, or meeting safety exit criteria, or withdrawal from the study for any other reason. Freedom from treatment failure at 12 months after randomisation was higher in patients taking sodium valproate (64/146, 44%) than in patients taking lamotrigine (31/146, 21%; P < 0.001). At 16 to 20 weeks, freedom from treatment failure was observed in 85/146 (58%) patients taking valproate and 43/146 (29%) patients taking lamotrigine.
(2) Normalisation of the EEG
Only one study (Huang 2009) explicitly reported data on this outcome. The proportion showing normal EEG at 12 months in the lamotrigine group (6/22, 27.3%) was significantly lower than that in the valproic acid group (15/23, 65.2%) (P < 0.05).
Ethosuximide versus lamotrigine
One study (Glauser 2013a), compared ethosuximide and lamotrigine in drug naive patients with childhood absence seizures. The main effectiveness outcome was the freedom from treatment failure assessed 12 months after randomisation. Freedom from treatment failure was also assessed at 16 to 20 weeks, and in between 16 and 20 weeks and month 12. Treatment failure was defined as failure either due to lack of seizure control, or meeting safety exit criteria, or withdrawal from the study for any other reason. Freedom from treatment failure at 12 months after randomisation was higher in patients taking ethosuximide (70/154, 45%) than in patients taking lamotrigine (31/146, 21%; P < 0.001). At 16 to 20 weeks, freedom from treatment failure was observed in 81/154 (53%) patients taking ethosuximide and 43/146 (29%) patients taking lamotrigine.
Adverse effects
The most common adverse effects of treatment with valproate reported by the studies assessing this drug (Callaghan 1982; Martinovic 1983; Sato 1982; Huang 2009; Glauser 2013a) were fatigue, nausea, vomiting, increased appetite with weight gain, behavioural/psychiatric changes (decreased concentration, personality change, hyperactivity, attention problems, hostility), and thrombocytopenia (Table 1). This is similar to the general adverse effects profile of valproate. Adverse effects often seen with valproate treatment are dyspepsia, weight gain, tremor, transient hair loss and haematological abnormalities (Panayiotopoulos 2001).
| Event | Callaghan 1982 | Sato 1982 | Martinovic 1983 | Coppola 2004 | Huang 2009 | Glauser 2013 |
| Acute pancreatitis | 1 | |||||
| Obesity/Weight gain | 1 | 1 | 14 | |||
| Drowsiness | 4 | |||||
| Nausea | 5 | 3 | 12* | |||
| Vomiting | 1 | 2 | 12* | |||
| Decreased platelet numbers | 2 | 4 | ||||
| Increased appetite | 15 | |||||
| Poor appetite | 1 | 8 | ||||
| Diarrhoea | 1 | 7 | ||||
| Dizziness | 1 | 2 | ||||
| Hyperactivity | 23 | |||||
| Attention problems | 24 | |||||
| Hostility | 22 | |||||
| Concentration decreased | 18 | |||||
| Personality change | 17 | |||||
| Sleep problem | 17 | |||||
| Depression | 11 | |||||
| Slow process speed | 11 | |||||
| Memory problem | 10 | |||||
| Apathy | 9 | |||||
| Fatigue | 27 | |||||
| Headache | 1 | 18 | ||||
| Leukopenia | 2 | |||||
| Elevated liver function tests | 1 | 7 | ||||
| Elevated LDH | 1 | |||||
| Rash | 2 |
* Nausea, vomiting, or both
LDH: lactate dehydrogenase
Numbers of individuals within each study undertaking valproate: 14 (Callaghan 1982), 22 (Sato 1982), 10 (Martinovic 1983), 19 (Coppola 2004), 23 (Huang 2009), 146 (Glauser 2013a).
Ethosuximide treatment was mostly associated with nausea, vomiting, and behavioural/psychiatric changes (Table 2).
| Event | Callaghan 1982 | Sato 1982 | Martinovic 1983 | Glauser 2013 |
| Drowsiness | 1 | 5 | ||
| Tiredness | 2 | |||
| Nausea | 3 | 2 | 29* | |
| Vomiting | 3 | 29* | ||
| Increased appetite | 6 | |||
| Poor appetite | 1 | 10 | ||
| Diarrhoea | 9 | |||
| Dizziness | 1 | 10 | ||
| Headache | 2 | 23 | ||
| Leukopenia | 3 | |||
| Hiccups | 1 | |||
| Moodiness | 1 | |||
| Hyperactivity | 13 | |||
| Attention problems | 8 | |||
| Hostility | 4 | |||
| Concentration decreased | 6 | |||
| Personality change | 6 | |||
| Sleep problem | 11 | |||
| Depression | 4 | |||
| Slow process speed | 3 | |||
| Memory problem | 0 | |||
| Apathy | 4 | |||
| Fatigue | 26 | |||
| Rash | 6 |
* Nausea, vomiting, or both
Numbers of individuals within each study undertaking ethosuximide: 14 (Callaghan 1982), 23 (Sato 1982), 10 (Martinovic 1983), 154 (Glauser 2013a).
The most common adverse effects of treatment with lamotrigine were fatigue, and behavioural/psychiatric changes (Table 3). In one lamotrigine study (Frank 1999), the most commonly reported adverse event was rash (reported on 11 occasions in 10 patients). However, only in one of the individuals was this thought to be related to lamotrigine. There were two serious adverse events during the treatment, but they were judged to be unrelated to treatment. In one study (Huang 2009), systemic anaphylaxis rash during lamotrigine treatment led to patients´ withdrawal from the study. In the Glauser 2013a study, no side effects (including rash, reported in two patients taking valproate, six patients taking ethosuximide, and six patients taking lamotrigine) occurred more frequently in the lamotrigine cohort compared to the other treatment groups (valproate and ethosuximide). The occurrence of rash in patients receiving lamotrigine is a well‐known adverse events of this drug and its risk may be reduced by slow titration (Wang 2015).
| Event | Frank 1999 | Coppola 2004 | Huang 2009 | Glauser 2013 |
| Abdominal pain | 5 | |||
| Headache | 2 | 2 | 14 | |
| Nausea | 3 | 2* | ||
| Vomiting | 2* | |||
| Poor appetite | 2 | 9 | ||
| Increased appetite | 1 | 10 | ||
| Diarrhoea | 2 | |||
| Dizziness | 3 | 5 | 5 | |
| Hyperkinesia | 2 | |||
| Hyperactivity | 12 | |||
| Attention problems | 11 | |||
| Hostility | 11 | |||
| Concentration decreased | 9 | |||
| Personality change | 10 | |||
| Sleep problem | 5 | |||
| Depression | 11 | |||
| Slow process speed | 7 | |||
| Memory problem | 8 | |||
| Apathy | 3 | |||
| Fatigue | 1 | 18 | ||
| Rash | 10 | 1 | 2 | 6 |
| Nervousness | 1 | |||
| Diplopia | 1 |
* Nausea, vomiting, or both
Numbers of individuals within each study undertaking lamotrigine: 15 (Frank 1999), 19 (Coppola 2004), 24 (Huang 2009), 146 (Glauser 2013a).
Discussion
Despite absence seizures being a relatively common seizure type in children, we found only eight randomised controlled trials, seven of them recruiting 20 to 48 participants. Only the study of Glauser 2013a included a much larger sample.
One trial compared lamotrigine with placebo (Frank 1999), three compared ethosuximide with valproate (Callaghan 1982; Sato 1982; Martinovic 1983), three compared lamotrigine with valproate (Coppola 2004; Basu 2005; Huang 2009), and one compared ethosuximide, valproate, and lamotrigine (Glauser 2013a). The description of important methodology was sometimes poor, and only two studies (Coppola 2004; Glauser 2013a) gave a description of allocation concealment. Three of the trials were explicitly reported as double‐blind (Sato 1982; Frank 1999; Glauser 2013a). In three of the trials there was no mention of losses to follow‐up or exclusions from analyses. The trials used a variety of methodologies; six were parallel trials (Callaghan 1982; Martinovic 1983; Coppola 2004; Basu 2005; Huang 2009; Glauser 2013a) and two used response conditional designs (Sato 1982; Martinovic 1983). The length of follow‐up ranged from four weeks to four years.
The trial comparing lamotrigine with placebo (Frank 1999), found that individuals becoming seizure free on lamotrigine, were more likely to remain seizure free if they were randomised to stay on lamotrigine rather than placebo. In essence, this trial assessed the effect of lamotrigine withdrawal. Although this trial finds evidence of an effect of lamotrigine on absence seizures, it was of only four weeks duration, and the design is inadequate to inform clinical practice. Also, clinicians and people living with epilepsy are likely more concerned with how drugs compare with each other rather than with placebo.
Three studies (Coppola 2004; Basu 2005; Huang 2009) directly compared lamotrigine with the long‐established treatment for typical absence seizures, sodium valproate. All these three studies found both valproate and lamotrigine to be efficacious in the treatment of typical absence seizures in children. However, in these studies (Coppola 2004; Basu 2005; Huang 2009) the study sample size was small (38, 30 and 48 patients, respectively), and estimates are therefore imprecise. Most robust results are provided by the much larger study including three groups: valproic acid, lamotrigine and ethosuximide (Glauser 2013a). This study found that at 12 months, the freedom‐from‐failure rates for ethosuximide and valproic acid were similar and were higher than the rate for lamotrigine. The frequency of treatment failures due to lack of seizure control (P < 0.001) and intolerable adverse events (P < 0.037) was significantly different among the treatment groups. Almost two thirds of the 125 participants with treatment failure due to lack of seizure control were in the lamotrigine cohort. The largest subgroup (42%) of the 115 participants discontinuing due to adverse events was in the valproic acid group. Overall, this study demonstrates the superior effectiveness of ethosuximide and valproic acid compared to lamotrigine as initial monotherapy aimed to control seizures without intolerable adverse events in children with childhood absence epilepsy. Because of the higher rate of adverse events leading to drug discontinuation and the significant negative effects on attentional measures seen in the valproate cohort, the authors concluded that ethosuximide represents the optimal initial empirical monotherapy for childhood absence epilepsy. Notably, this study was the very first randomised controlled trial to meet the International League Against Epilepsy (ILAE) criteria for class I evidence for childhood absence epilepsy (or for any type of generalised seizure in adults or children) (Glauser 2006). Consequently, ethosuximide and valproate were designed/designated as treatments with level A evidence in children with childhood absence epilepsy in the recent ILAE treatment guidelines (Glauser 2013b).
The good efficacy profile of ethosuximide for the treatment of absence seizures as shown in Glauser 2013a confirms results of three other smaller studies that compared ethosuximide with valproate (Callaghan 1982; Sato 1982; Martinovic 1983); all these three smaller studies reported a superior efficacy profile for ethosuximide over valproate with regards to seizure freedom (Callaghan 1982; Sato 1982; Martinovic 1983), although with wide confidence intervals due to small sample size. However, it is noteworthy to consider that ethosuximide does not suppress tonic‐clonic seizures (Berkovic 1993), and it has even been suggested that it can transform absences into grand mal seizures (Glauser 2002), although with contrasting data (Schmitt 2007). Hence, ethosuximide should probably be avoided in patients with absence seizures and co‐existing generalised tonic‐clonic seizures
Significance
There are no placebo‐controlled trials for ethosuximide or valproate, and hence no evidence from randomised controlled trials to support a specific effect on absence seizures for either of these two drugs. Due to the differing methodologies used in the trials comparing ethosuximide, lamotrigine and valproate, we thought it inappropriate to undertake a meta‐analysis. Hence, recommendations for practice from this review are based on a qualitative comparison. Further trials with larger size than many of the studies currently included in this review are required. Further research could allow results to be pooled, leading to a quantitative rather than a qualitative summary of results. In summary, ethosuximide, lamotrigine and valproate are commonly used to treat children and adolescents with absence seizures. We now have evidence from a recently conducted, high‐quality, large trial that ethosuximide and valproate have higher efficacy than lamotrigine as initial monotherapy in children and adolescents with absence seizures. This study showed a higher rate of adverse events leading to drug discontinuation and significant negative effects on attentional measures in the valproate group. Consequently, with regards to both efficacy and tolerability, ethosuximide represents the optimal initial empirical monotherapy for children and adolescents with absence seizures. However, the use of ethosuximide should be avoided in patients with absence seizures and generalised tonic‐clonic seizures, as this drug is probably inefficacious on tonic‐clonic seizures.
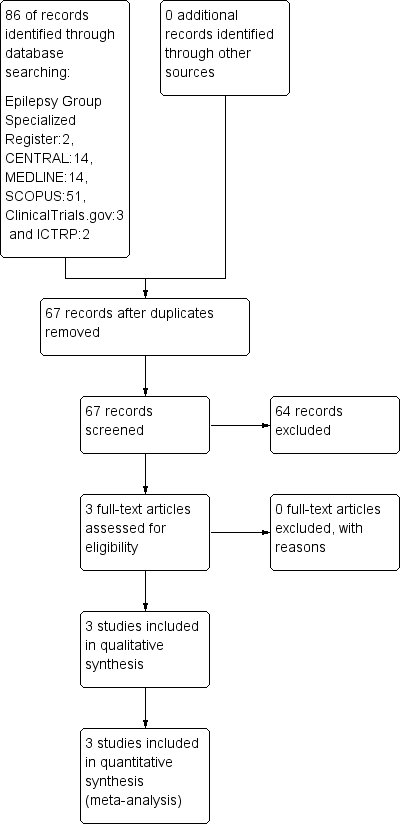
Study flow diagram (results refer only to the updated version of the review).
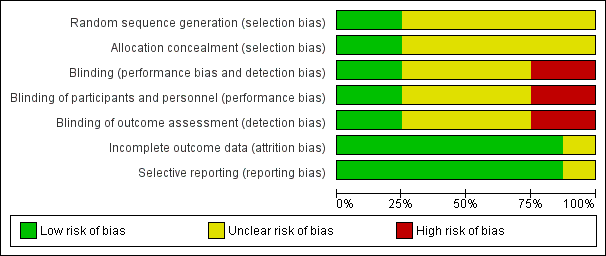
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
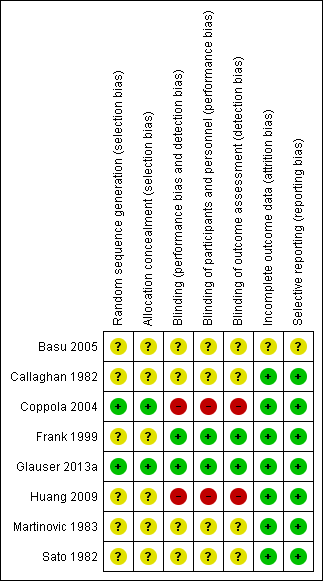
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
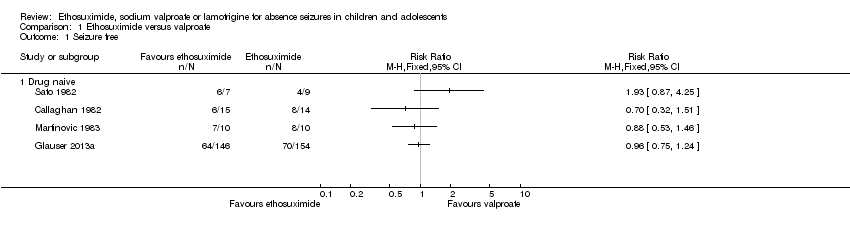
Comparison 1 Ethosuximide versus valproate, Outcome 1 Seizure free.
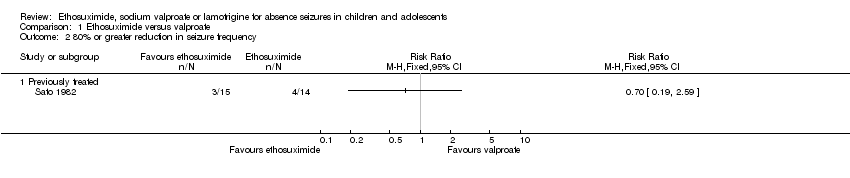
Comparison 1 Ethosuximide versus valproate, Outcome 2 80% or greater reduction in seizure frequency.

Comparison 1 Ethosuximide versus valproate, Outcome 3 50% or greater reduction in seizure frequency.

Comparison 2 Lamotrigine versus valproate, Outcome 1 Seizure free.
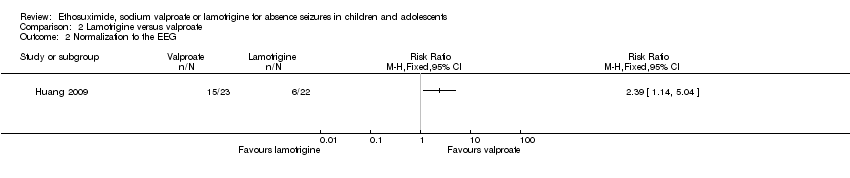
Comparison 2 Lamotrigine versus valproate, Outcome 2 Normalization fo the EEG.
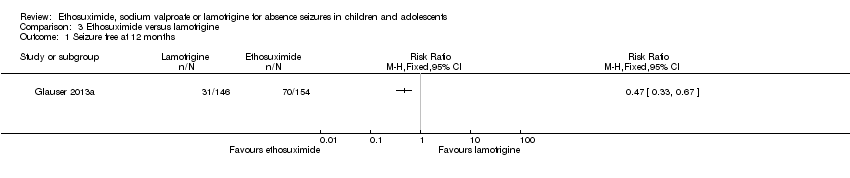
Comparison 3 Ethosuximide versus lamotrigine, Outcome 1 Seizure free at 12 months.
| Event | Callaghan 1982 | Sato 1982 | Martinovic 1983 | Coppola 2004 | Huang 2009 | Glauser 2013 |
| Acute pancreatitis | 1 | |||||
| Obesity/Weight gain | 1 | 1 | 14 | |||
| Drowsiness | 4 | |||||
| Nausea | 5 | 3 | 12* | |||
| Vomiting | 1 | 2 | 12* | |||
| Decreased platelet numbers | 2 | 4 | ||||
| Increased appetite | 15 | |||||
| Poor appetite | 1 | 8 | ||||
| Diarrhoea | 1 | 7 | ||||
| Dizziness | 1 | 2 | ||||
| Hyperactivity | 23 | |||||
| Attention problems | 24 | |||||
| Hostility | 22 | |||||
| Concentration decreased | 18 | |||||
| Personality change | 17 | |||||
| Sleep problem | 17 | |||||
| Depression | 11 | |||||
| Slow process speed | 11 | |||||
| Memory problem | 10 | |||||
| Apathy | 9 | |||||
| Fatigue | 27 | |||||
| Headache | 1 | 18 | ||||
| Leukopenia | 2 | |||||
| Elevated liver function tests | 1 | 7 | ||||
| Elevated LDH | 1 | |||||
| Rash | 2 | |||||
| * Nausea, vomiting, or both Numbers of individuals within each study undertaking valproate: 14 (Callaghan 1982), 22 (Sato 1982), 10 (Martinovic 1983), 19 (Coppola 2004), 23 (Huang 2009), 146 (Glauser 2013a). | ||||||
| Event | Callaghan 1982 | Sato 1982 | Martinovic 1983 | Glauser 2013 |
| Drowsiness | 1 | 5 | ||
| Tiredness | 2 | |||
| Nausea | 3 | 2 | 29* | |
| Vomiting | 3 | 29* | ||
| Increased appetite | 6 | |||
| Poor appetite | 1 | 10 | ||
| Diarrhoea | 9 | |||
| Dizziness | 1 | 10 | ||
| Headache | 2 | 23 | ||
| Leukopenia | 3 | |||
| Hiccups | 1 | |||
| Moodiness | 1 | |||
| Hyperactivity | 13 | |||
| Attention problems | 8 | |||
| Hostility | 4 | |||
| Concentration decreased | 6 | |||
| Personality change | 6 | |||
| Sleep problem | 11 | |||
| Depression | 4 | |||
| Slow process speed | 3 | |||
| Memory problem | 0 | |||
| Apathy | 4 | |||
| Fatigue | 26 | |||
| Rash | 6 | |||
| * Nausea, vomiting, or both Numbers of individuals within each study undertaking ethosuximide: 14 (Callaghan 1982), 23 (Sato 1982), 10 (Martinovic 1983), 154 (Glauser 2013a). | ||||
| Event | Frank 1999 | Coppola 2004 | Huang 2009 | Glauser 2013 |
| Abdominal pain | 5 | |||
| Headache | 2 | 2 | 14 | |
| Nausea | 3 | 2* | ||
| Vomiting | 2* | |||
| Poor appetite | 2 | 9 | ||
| Increased appetite | 1 | 10 | ||
| Diarrhoea | 2 | |||
| Dizziness | 3 | 5 | 5 | |
| Hyperkinesia | 2 | |||
| Hyperactivity | 12 | |||
| Attention problems | 11 | |||
| Hostility | 11 | |||
| Concentration decreased | 9 | |||
| Personality change | 10 | |||
| Sleep problem | 5 | |||
| Depression | 11 | |||
| Slow process speed | 7 | |||
| Memory problem | 8 | |||
| Apathy | 3 | |||
| Fatigue | 1 | 18 | ||
| Rash | 10 | 1 | 2 | 6 |
| Nervousness | 1 | |||
| Diplopia | 1 | |||
| * Nausea, vomiting, or both Numbers of individuals within each study undertaking lamotrigine: 15 (Frank 1999), 19 (Coppola 2004), 24 (Huang 2009), 146 (Glauser 2013a). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Seizure free Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Drug naive | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 80% or greater reduction in seizure frequency Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Previously treated | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 50% or greater reduction in seizure frequency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Seizure free Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Seizure free at 1 month | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.42 [2.77, 25.59] | |
| 1.2 Seizure free at 3 months | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [1.16, 2.31] | |
| 1.3 Seizure freedom at 6 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.42 [0.88, 2.28] | |
| 1.4 Seizure free at 12 months | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [1.32, 2.11] | |
| 2 Normalization fo the EEG Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Seizure free at 12 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |

