Entrenamiento de fuerza con resistencia progresiva para mejorar la función física en adultos mayores
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | RCT (randomised controlled trial) | |
| Participants | Location: USA | |
| Interventions | PRT (progressive resistance strength training) versus control | |
| Outcomes | Strength (1 repetition maximum) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Primary: WOMAC pain and physical function subscales, SF‐36 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Muscle strength (1RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus aerobic | |
| Outcomes | Strength (1RM) | |
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Australia | |
| Interventions | PRT versus control (flexibility training) | |
| Outcomes | Primary: SF‐36 | |
| Notes | Data from PRT and flexibility training group were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Primary: FIM, physical performance test | |
| Notes | Means and SDs at 12 months were not reported. Portion results at 6 months could be estimated from baseline score and change score. Because of small sample size, the precision is questionable. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Primary: Short Physical Performance Battery (including chair rise) | |
| Notes | Post mean = baseline + change score; baseline SD was used | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 4 groups: low intensity, medium intensity and high intensity and control group | |
| Participants | Location: Greece | |
| Interventions | PRT (low intensity, medium intensity, and high intensity) versus control | |
| Outcomes | Muscle strength | |
| Notes | Results from males were extracted | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: France | |
| Interventions | PRT versus control | |
| Outcomes | Strength (1RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Netherlands | |
| Interventions | PRT Group (high‐guidance) versus control | |
| Outcomes | Primary: disability measure (Groningen Activity Restriction Scale) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Strength (1RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Muscle strength (1RM/body weight) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Primary: CS physical performance test , SF‐36 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Demark | |
| Interventions | PRT versus control | |
| Outcomes | Muscle strength (1 RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT: with four groups: strength training alone, endurance training alone, strength and endurance training and control group | |
| Participants | Location: USA | |
| Interventions | PRT versus control Adherence: 95% excluding drop‐outs; 81% including drop‐outs | |
| Outcomes | Aerobic capacity | |
| Notes | Data from PRT and control group were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Muscle strength | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT both groups were also on a low‐protein diet (run‐in period for 6 weeks to evaluate this); comparison was between low‐protein diet alone or low‐protein diet plus resistance training | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Strength (1RM), | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Muscle strength (1 RM) | |
| Notes | Reported whole body muscle strength (data were not pooled) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | HRQoL (SF‐36) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Strength (1RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 4 groups: PRT, control, functional training, and combined training | |
| Participants | Location: Netherlands | |
| Interventions | PRT versus control, versus functional training, and versus combined training | |
| Outcomes | Primary: physical activities/ADL disability | |
| Notes | Comparisons: PRT versus control, PRT versus functional training | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Strength (number of reps at % of body weight) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | HRQoL (SF‐36) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 4 groups: high intensity, medium intensity, and low intensity, and control | |
| Participants | Location: Australia | |
| Interventions | PRT (high intensity, medium intensity, and low intensity) versus control | |
| Outcomes | Dynamic muscle strength | |
| Notes | Involved power training | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: PRT, control, and functional task exercise group | |
| Participants | Location: Netherlands | |
| Interventions | PRT versus control and versus functional task exercise | |
| Outcomes | Primary: SF‐36 | |
| Notes | Data of SF‐36 were provided by the trial authors | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT (fixed repetition and periodised repetition) versus control | |
| Outcomes | Muscle strength (1 RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT (once a week versus twice a week) | |
| Outcomes | Strength (1RM) | |
| Notes | Date from 2 times a week and one time a week were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT, factorial design (comparison of floor surface types not included here) | |
| Participants | Location: UK | |
| Interventions | PRT versus control | |
| Outcomes | Falls (during hospital stay) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | RCT, PRT vs moderate aerobic exercise | |
| Participants | Location: USA | |
| Interventions | PRT versus aerobic | |
| Outcomes | Short physical performance battery (SPPB) | |
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B‐ Unclear |
| Methods | RCT with 3 groups: PRT, aerobic training and health education (attention control) | |
| Participants | Location: USA | |
| Interventions | PRT versus control and versus aerobic | |
| Outcomes | Primary: self‐report physical disability (23 item scale developed for use in this trial) | |
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: PRT, control, and aerobic group | |
| Participants | Location: USA | |
| Interventions | PRT versus control and aerobic | |
| Outcomes | Muscle strength (1RM) | |
| Notes | Comparisions: PRT versus control, and PRT versus aerobic | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: PRT, control, and aerobic group | |
| Participants | Location: Greece | |
| Interventions | PRT versus control and versus aerobic (cardiovascular training) | |
| Outcomes | Muscle strength (1 RM) | |
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: high intensity PRT, low intensity PRT, and control | |
| Participants | Location: Greece | |
| Interventions | PRT (high intensity and low intensity) versus control | |
| Outcomes | Muscle strength | |
| Notes | Data from high intensity and low intensity PRT group were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT, factorial design (comparison of nutritional supplements versus placebo not considered here) | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Strength (1RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Strength | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT (high velocity versus low velocity) | |
| Outcomes | Muscle strength | |
| Notes | No reported results can be pooled (missing M and SD for each group) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Strength (1RM ‐ ? data collected for controls) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Australia | |
| Interventions | PRT versus control | |
| Outcomes | Primary: SF‐12, Adelaide Activities profile, WOMAC | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Muscle strength (1RM, isokinetic strength of knee extension) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Australia | |
| Interventions | PRT (3‐set versus 1‐set) | |
| Outcomes | Muscle strength (1 RM) | |
| Notes | 3‐set PRT versus 1‐set PRT | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Strength (1RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT (high intensity versus low intensity) | |
| Outcomes | Muscle strength | |
| Notes | No numerical results for the control group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Canada | |
| Interventions | PRT versus control | |
| Outcomes | Strength (1RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: PRT, control, and aerobic group | |
| Participants | Location: Canada | |
| Interventions | PRT versus control and versus aerobic | |
| Outcomes | Muscle strength | |
| Notes | sample size for each group was not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT trial with 4 groups: PRT alone, growth hormone treatment alone, PRT and growth hormone treatment and control. Only PRT alone and control are included in this review | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Strength (isokinetic dynamometry) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Canada | |
| Interventions | PRT versus control and versus aerobic | |
| Outcomes | Peak VO2 | |
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: PRT, walking (aerobic training) and control | |
| Participants | Location: USA | |
| Interventions | PRT versus control and versus aerobic | |
| Outcomes | Strength (Cybex dynamometer) | |
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: High‐intensity PRT, Low‐intensity PRT and Control | |
| Participants | Location: USA | |
| Interventions | PRT (high intensity and low intensity) versus control | |
| Outcomes | Force accuracy and steadiness | |
| Notes | Date from high intensity PRT and low intensity PRT were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Canada | |
| Interventions | PRT versus control | |
| Outcomes | TUAG | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with people randomised to variable intensity resistance training and high‐intensity resistance training NOTE: control group participants were not randomly assigned, and are not included in this review | |
| Participants | Location: USA | |
| Interventions | PRT (high versus variable resistance) versus control | |
| Outcomes | Strength (1RM and isometric) | |
| Notes | Date from high intensity PRT and variable intensity PRT were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Spain | |
| Interventions | PRT versus endurance training (aerobic) | |
| Outcomes | Muscle strength (1RM‐half squat) | |
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Strength (Cybex isokinetic dynamometer) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Strength (hand‐held dynamometer) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | RCT: (note: data reported by dominant and non‐dominant leg. Data for dominant leg used in analyses) | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Strength and muscular endurance (isokinetic dynamometer) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: PRT, aerobic training and control | |
| Participants | Location: USA | |
| Interventions | PRT versus control and versus aerobic | |
| Outcomes | Muscle size | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with factorial design: PRT alone, balance training alone, PRT and balance, control | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Strength (isokinetic dynamometer) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Greece | |
| Interventions | PRT (high intensity and moderate intensity) versus control | |
| Outcomes | Muscle strength (1‐RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: PRT, control, and aerobic group | |
| Participants | Location: Finland | |
| Interventions | PRT versus control and versus aerobic (Note: participants in all groups were given 600mg calcium per day) | |
| Outcomes | PeakVO2 | |
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | SF‐36 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Denmark | |
| Interventions | PRT versus control | |
| Outcomes | Primary: simple ADL (interview) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus functional training | |
| Outcomes | Primary: SF‐36 | |
| Notes | Numerical results of means and SDs were not reported. Reported/figured % difference | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Australia | |
| Interventions | PRT versus control | |
| Outcomes | Muscle strength | |
| Notes | Final muscle strength outcome was not available | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: New Zealand | |
| Interventions | PRT versus control | |
| Outcomes | Strength (1RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | RCT with a factorial design (only information about PRT vs control reported, 3‐ month outcomes reported) | |
| Participants | Location: New Zealand and Australia | |
| Interventions | PRT versus control | |
| Outcomes | Primary: falls over 6 months, HRQoL (SF‐36) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | RCT | |
| Participants | Location: Canada | |
| Interventions | PRT versus control | |
| Outcomes | Primary: health related quality of life, general physical function | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: UK | |
| Interventions | PRT (speed versus strength) | |
| Outcomes | Strength measure | |
| Notes | Involved power training, no control group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: PRT, control, and endurance (aerobic) group | |
| Participants | Location: USA | |
| Interventions | PRT versus control and versus endurance (aerobic) | |
| Outcomes | VO2max | |
| Notes | Baseline + relative change score | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Australia | |
| Interventions | PRT versus control | |
| Outcomes | Strength (1RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: PRT, functional training, and PRT with functional training group | |
| Participants | Location: Greece | |
| Interventions | PRT versus control and versus aerobic | |
| Outcomes | Strength measure | |
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: PRT, control, and aerobic group | |
| Participants | Location: USA | |
| Interventions | PRT versus control and versus aerobic | |
| Outcomes | Primary: SF‐36 | |
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: PRT, functional training, and PRT with functional training | |
| Participants | Location: USA | |
| Interventions | PRT versus functional training and versus PRT with functional training | |
| Outcomes | Muscle strength | |
| Notes | Data from PRT and functional training group were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Primary: WOMAC, SF‐36 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT. All results broken down into four groups by sex and age (60‐70 or 70‐80, only results for women aged 70‐80 ‐ the largest group ‐ used for pooled comparisons in review) | |
| Participants | Location: Canada | |
| Interventions | PRT versus control | |
| Outcomes | Strength (1RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Australia | |
| Interventions | PRT versus control | |
| Outcomes | Strength (10 RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with three groups, PRT, mobility exercise programme and attention control | |
| Participants | Location: UK | |
| Interventions | PRT versus control and versus mobility | |
| Outcomes | TUAG | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | RCT cluster randomised by residence | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | ADL performance (modified version of Lawton and Brody's IADL scale) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus flexibility (control) | |
| Outcomes | Primary: SF‐36 (at the 30 month), WOMAC | |
| Notes | SF‐36 was not pooled because it was not measured right after the training | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Australia | |
| Interventions | PRT versus control | |
| Outcomes | Primary: SF‐12 | |
| Notes | Reported Median & 95%CI. Data from participants who took nutrition supplementation were not extracted. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: PRE, control, and power exercise | |
| Participants | Location: USA | |
| Interventions | PRT versus control and versus power exercise | |
| Outcomes | Primary: Continuous Scale Physical Functional Performance | |
| Notes | Involved power training | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Canada | |
| Interventions | PRT versus control | |
| Outcomes | Primary: Chedoke‐McMaster Stroke Assessment | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Strength (1RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Canada | |
| Interventions | PRT versus control | |
| Outcomes | Strength (1RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Strength (1RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Primary: Late‐Life Function and Disability Instrument, sickness impact profile | |
| Notes | SD is obtained from SE for LLFD 1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Canada | |
| Interventions | PRT versus control | |
| Outcomes | Strength (1RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: PRT, control, and aerobic training group | |
| Participants | Location: USA | |
| Interventions | PRT versus control and versus aerobic | |
| Outcomes | Strength | |
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Exercise capacity (6‐minute walk) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT: (groups of healthy young people and middle‐aged people with RA not included in this review) | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Strength (1RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: UK | |
| Interventions | PRT versus control | |
| Outcomes | Muscle strength | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Canada | |
| Interventions | PRT versus control | |
| Outcomes | Muscle strength (1RM, hand grip) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Strength (isokinetic dynamometer) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Muscle strength (1 RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Canada | |
| Interventions | PRT versus control | |
| Outcomes | Primary: Health‐related quality of life | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Australia | |
| Interventions | PRT versus control | |
| Outcomes | Muscle strength | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: high intensity, low intensity, and control | |
| Participants | Location: France | |
| Interventions | PRT (high intensity and low intensity) versus control | |
| Outcomes | Primary: self‐reported disability | |
| Notes | SD was calculated from SEM | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: France | |
| Interventions | PRT versus control | |
| Outcomes | Muscle strength (Torques) | |
| Notes | Training at ankle joints | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Muscle strength (1RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Canada | |
| Interventions | PRT versus control | |
| Outcomes | Strength (1RM) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Australia | |
| Interventions | PRT versus control | |
| Outcomes | Human Activity Profile WHO‐QOL | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Sickness Impact Profile | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: high intensity, low intensity, and control | |
| Participants | Location: Australia | |
| Interventions | PRT (high intensity versus low intensity) versus control | |
| Outcomes | Primary: SF‐36 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: PRT, control and aerobic training group | |
| Participants | Location: Finland | |
| Interventions | PRT versus control and versus endurance (aerobic) | |
| Outcomes | Strength | |
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: UK | |
| Interventions | PRT versus control | |
| Outcomes | Human Activity Profile | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: UK | |
| Interventions | PRT versus control | |
| Outcomes | Human Activity Profile | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Portugal | |
| Interventions | PRT versus control | |
| Outcomes | Primary: self‐reported disability | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Denmark | |
| Interventions | PRT versus control | |
| Outcomes | Muscle strength | |
| Notes | SD was calculated from SE | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT (High intensity versus low intensity) | |
| Outcomes | Muscle strength | |
| Notes | Reported absolute change. High‐intensity leg exercise led to greater leg strength, No significance in aggregate physical performance score change between any intervention groups. Final score = baseline + change score. Final SD = baseline SD | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | RCT | |
| Participants | Location: Canada | |
| Interventions | PRT (isokinet concentric versus excentric) | |
| Outcomes | Muscle strength | |
| Notes | Eccentric versus concentric | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: high intensity training, low intensity and control (high‐intensity only used for main comparisons) | |
| Participants | Location: USA | |
| Interventions | PRT (high intensity and low intensity) versus control | |
| Outcomes | Strength (1RM), | |
| Notes | Date from high intensity PRT and low intensity PRT were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 4 groups, PRT once per week, twice per week, 3 times per week and control (main analyses with 3 times per week and control) | |
| Participants | Location: USA | |
| Interventions | PRT (at different frequencies) versus control | |
| Outcomes | Strength (1RM) | |
| Notes | Data from 3 times per week and one time per week group were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT (note: results extrapolated from graph) | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Gait speed | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Strength | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | WOMAC | |
| Notes | Calculated SDs from reported SEMs | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: PRT, control, and aerobic groups | |
| Participants | Location: USA | |
| Interventions | PRT versus control and versus aerobic | |
| Outcomes | Arm curls (repetitions) | |
| Notes | Numerical results of SDs were not reported. Data were not pooled. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Primary: physical function tests (including gait speed, chair rise, stair ascent/descent) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: High‐intensity PRT, low‐intensity PRT, and control | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Strength (1RM) | |
| Notes | Date from high intensity PRT and low intensity PRT were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Sweden | |
| Interventions | PRT versus control | |
| Outcomes | Aerobic capacity ( Peak VO2 and 6 minute walk test) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 3 groups: High‐intensity PRT, low‐intensity PRT and control | |
| Participants | Location: USA | |
| Interventions | PRT versus control | |
| Outcomes | Strength (1RM) | |
| Notes | Added results from more recent publications | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B‐ Unclear |
| Methods | RCT | |
| Participants | Location: The Netherlands | |
| Interventions | PRT versus control and versus aerobic | |
| Outcomes | Strength (maximum torque measured by the Quadriso‐tester) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | Location: Austria | |
| Interventions | PRT versus control | |
| Outcomes | VO2max | |
| Notes | Numerical results of muscle strength were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT with 4 groups: PRT alone, aerobic training alone, combined PRT and aerobic training and control | |
| Participants | Location: USA | |
| Interventions | PRT versus control and versus aerobic | |
| Outcomes | Strength (5RM) | |
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
ADL: activities of daily living
Age: overall age of all groups. If this is not available age for progressive resistance training group alone is reported
CHF: congestive heart failure
CHD:coronary heart disease
COPD: chronic obstructive pulmonary disease
Ex: exercise
Ex1: exercise once per week
Ex2: exercise twice per week
Ex3: exercise three times per week
HI: high intensity
MI: Medium intensity
LI: low intensity
LL: lower limb
METs: maximum metabolic equivalents
MMSE: the Mini‐Mental State Examination
N: number of participants allocated to strength training group and control group; or number of participants allocated to additional intervention group
NA: not applicable
OA: osteoarthritis
PAD: peripheral arterial disease RCT: Randomised controlled trial
PRT: progressive resistance strength training Reps: repetitions
RM: repetition maximum
SF‐36: Medical Outcome Studies 36 Item Short Form questionnaire
Tr: trunk
TUAG: timed "up‐and‐go" test
UL: upper limb
WOMAC: Western Ontario/McMaster Universities Arthritis Index
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Not a RCT | |
| Participants too young (mean age <60) | |
| Not a RCT | |
| Combined program ‐ not PRT alone | |
| Not a RCT | |
| Combined intervention program ‐ not PRT alone | |
| Not a RCT | |
| Combined program ‐ not PRT alone | |
| Not a RCT | |
| Does not meet criteria for PRT | |
| Does not meet criteria for PRT | |
| Not a RCT | |
| Participants too young (mean age <60) | |
| Participants too young (mean age <60) | |
| Not a RCT | |
| Combined program ‐ not PRT alone | |
| Participants too young (mean age <60) | |
| Does not meet for criteria for PRT | |
| Combined program ‐ not PRT alone | |
| No relevant outcomes to the review | |
| No relevant outcomes to the review | |
| Does not meet the criteria for PRT ‐ not progressive | |
| Combined program ‐ not PRT alone | |
| Not a RCT | |
| Combined program ‐ not PRT alone | |
| Not a RCT | |
| Combined program ‐ not PRT alone | |
| Combined program ‐ not PRT alone | |
| Combined program ‐ not PRT alone | |
| No relevant outcomes to the review | |
| No relevant outcomes to the review | |
| Article cannot be located. | |
| Combined program (with supplement) ‐ not PRT alone | |
| Not a RCT | |
| Does not meet the criteria for PRT | |
| Included participants younger than 60 | |
| No relevant outcomes to the review | |
| No relevant outcomes to the review | |
| Included young participants (younger than 60 years old) | |
| Participants too young (mean age <60) | |
| Included young participants (younger than 60 years old) | |
| Not a RCT | |
| Does not meet the criteria for PRT | |
| Not a RCT | |
| Not a RCT | |
| Not a RCT | |
| Not a RCT | |
| Combined program ‐ not PRT alone | |
| Does not meet the criteria for PRT | |
| Combined program ‐ not PRT alone | |
| No relevant comparisons to the review | |
| Combined program ‐ not PRT alone | |
| Included young participants (younger than 60 years old) | |
| Combined program ‐ not PRT alone | |
| Combined program ‐ not PRT alone | |
| Combined program ‐ not PRT alone | |
| Not a RCT | |
| Not a RCT | |
| Not PRT alone ‐ with eating plan | |
| Not PRT alone ‐ with eating plan | |
| Not a RCT | |
| Combined program ‐ not PRT alone | |
| Not a RCT | |
| Not a RCT | |
| Not a RCT | |
| Not a RCT | |
| Not a RCT | |
| Not a RCT | |
| Not a RCT | |
| Not a RCT | |
| Not a RCT | |
| Included young participants (younger than 60 years old) | |
| Not a RCT | |
| Participants too young (mean age <60) | |
| Combined program (with hormone intervention) | |
| Not a RCT | |
| Combined program (protein) ‐ not PRT alone | |
| No relevant outcomes to the review | |
| Does not meet the criteria for PRT ‐ not progressive | |
| Not a RCT | |
| Not a RCT | |
| Combined program ‐ not PRT alone | |
| Combined program ‐ not PRT alone | |
| No relevant outcomes to the review | |
| Combined program ‐ not PRT alone | |
| Participants too young (mean age <60) | |
| Does not meet the criteria for PRT | |
| Not a RCT | |
| Not a RCT | |
| Not a RCT | |
| Not a RCT | |
| Included young participants (younger than 60 years old) | |
| Participants too young (mean age <60) | |
| No relevant outcomes to the review | |
| Not a RCT | |
| No relevant outcomes to the review | |
| Not a RCT | |
| Participants too young (mean age <60) | |
| No relevant outcomes to the review | |
| Training did not meet criteria for PRT | |
| No relevant outcomes to the review | |
| Combined program (with hormone) ‐ not PRT alone | |
| No relevant outcomes to the review | |
| Included young participants (younger than 60 years old) | |
| Not a RCT | |
| Not a RCT (not clearly stated that patients were randomised) | |
| Combined program ‐ not PRT alone | |
| Training did not meet criteria for PRT ‐ not progressive | |
| No relevant outcomes to the review | |
| Does not meet the criteria for PRT | |
| Participants too young (mean age <60) | |
| Participants too young (mean age <60) | |
| Participants too young (mean age <60) | |
| Not a RCT | |
| No relevant comparisons to the review | |
| Not a RCT | |
| Training did not meet criteria for PRT | |
| Not a RCT | |
| Combined program ‐ not PRT alone | |
| Combined program ‐ not PRT alone | |
| Combined program ‐ not PRT alone | |
| Participants too young (mean age <60) | |
| Combined program ‐ not PRT alone | |
| Training did not meet criteria for PRT | |
| Training did not meet criteria for PRT ‐ not progressive/included young participants | |
| Combined program ‐ not PRT alone | |
| Included younger participants (middle age) | |
| Combined program ‐ not PRT alone | |
| Combined program ‐ not PRT alone | |
| Not a RCT | |
| Training did not meet criteria for PRT | |
| Training did not meet criteria for PRT | |
| No relevant outcomes to the review | |
| Training did not meet criteria for PRT | |
| Not a RCT | |
| Serious threats to internal validity ‐ participants allowed to move from exercise to control group‐Not a RCT | |
| Training did not meet criteria for PRT ‐ not progressive | |
| Combined program ‐ not PRT alone | |
| Does not meet the criteria for PRT | |
| Not a RCT | |
| Does not meet the criteria for PRT | |
| Not a RCT | |
| Not a RCT | |
| Training did not meet criteria for PRT | |
| Training did not meet criteria for PRT ‐ not progressive | |
| Combined program (with diet) ‐ not PRT alone | |
| Not a RCT | |
| No relevant outcomes to the review | |
| Combined program ‐ not PRT alone | |
| Not a RCT | |
| Combined program (with supplement) ‐ not PRT alone | |
| Not a RCT | |
| Not a RCT | |
| Training did not meet criteria for PRT | |
| Does not meet the criteria for PRT ‐ not progressive | |
| Participants too young (mean age <60) | |
| Not a RCT | |
| Combined program ‐ not PRT alone | |
| Not a RCT | |
| Not a RCT | |
| Does not meet the criteria for PRT | |
| Included young participants (younger than 60 years old) | |
| Combined program ‐ not PRT alone | |
| No relevant outcomes to the review | |
| Combined program ‐ not PRT alone | |
| Training did not meet criteria for PRT ‐ The resistance was not progressively increased | |
| Combined program ‐ not PRT alone | |
| Combined program ‐ not PRT alone | |
| Combined program ‐ not PRT alone | |
| Combined program ‐ not PRT alone | |
| Not a RCT | |
| Combined program ‐ not PRT alone | |
| Combined program ‐ not PRT alone | |
| Combined program ‐ not PRT alone | |
| Article cannot be identified | |
| Participants too young (mean age of the control group < 60) | |
| Combined program ‐ not PRT alone | |
| Included young participants (younger than 60 years old) | |
| Does not meet the criteria for PRT | |
| Combined program ‐ not PRT alone | |
| Combined program (with hormone)‐not PRT alone | |
| Combined program ‐ not PRT alone | |
| No relevant outcomes to the review | |
| No relevant outcomes to the review | |
| Included young participants (younger than 60 years old) | |
| Training did not meet criteria for PRT. The resistance was not progressively increased | |
| Does not meet the criteria for PRT | |
| Not a RCT |
RCT = randomised controlled trial; PRT = progressive resistance strength training
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Main function measure (higher score = better function) Show forest plot | 33 | 2172 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.14 [0.05, 0.22] |
| Analysis 1.1  Comparison 1 PRT versus control, Outcome 1 Main function measure (higher score = better function). | ||||
| 2 Physical function domain of SF‐36/SF‐12 (Higher score = better function) Show forest plot | 14 | 778 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.08, 0.21] |
| Analysis 1.2  Comparison 1 PRT versus control, Outcome 2 Physical function domain of SF‐36/SF‐12 (Higher score = better function). | ||||
| 3 Activities of daily living measure (higher score = better function) Show forest plot | 3 | 330 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.04 [‐0.18, 0.26] |
| Analysis 1.3  Comparison 1 PRT versus control, Outcome 3 Activities of daily living measure (higher score = better function). | ||||
| 4 Activity level measure (kJ/week) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.4  Comparison 1 PRT versus control, Outcome 4 Activity level measure (kJ/week). | ||||
| 5 Main lower limb (LL) strength measure Show forest plot | 73 | 3059 | Std. Mean Difference (IV, Random, 95% CI) | 0.84 [0.67, 1.00] |
| Analysis 1.5  Comparison 1 PRT versus control, Outcome 5 Main lower limb (LL) strength measure. | ||||
| 6 Main measure of aerobic function Show forest plot | 29 | 1138 | Std. Mean Difference (IV, Random, 95% CI) | 0.31 [0.09, 0.53] |
| Analysis 1.6  Comparison 1 PRT versus control, Outcome 6 Main measure of aerobic function. | ||||
| 7 VO2 or peak oxygen uptake Show forest plot | 19 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.7  Comparison 1 PRT versus control, Outcome 7 VO2 or peak oxygen uptake. | ||||
| 7.1 VO2max‐ml/kg.min | 18 | 710 | Mean Difference (IV, Random, 95% CI) | 1.50 [0.49, 2.51] |
| 7.2 Peak oxygen uptake‐L/min | 2 | 47 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.04, 0.24] |
| 8 Six‐minute walk test (meters) Show forest plot | 11 | 325 | Mean Difference (IV, Random, 95% CI) | 52.37 [17.38, 87.37] |
| Analysis 1.8  Comparison 1 PRT versus control, Outcome 8 Six‐minute walk test (meters). | ||||
| 9 Balance measures (higher = better balance) Show forest plot | 17 | 996 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.12 [‐0.00, 0.25] |
| Analysis 1.9  Comparison 1 PRT versus control, Outcome 9 Balance measures (higher = better balance). | ||||
| 10 Balance measures (Low = better balance) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.10  Comparison 1 PRT versus control, Outcome 10 Balance measures (Low = better balance). | ||||
| 10.1 PRT (high intensity) versus control | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 PRT (low intensity) versus control | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Gait speed (m/s) Show forest plot | 24 | 1179 | Mean Difference (IV, Random, 95% CI) | 0.08 [0.04, 0.12] |
| Analysis 1.11  Comparison 1 PRT versus control, Outcome 11 Gait speed (m/s). | ||||
| 12 Timed walk (seconds) Show forest plot | 8 | 204 | Mean Difference (IV, Fixed, 95% CI) | ‐0.23 [‐1.07, 0.62] |
| Analysis 1.12  Comparison 1 PRT versus control, Outcome 12 Timed walk (seconds). | ||||
| 13 Timed "Up‐and‐Go" (seconds) Show forest plot | 12 | 691 | Mean Difference (IV, Fixed, 95% CI) | ‐0.69 [‐1.11, ‐0.27] |
| Analysis 1.13  Comparison 1 PRT versus control, Outcome 13 Timed "Up‐and‐Go" (seconds). | ||||
| 14 Time to stand from a chair Show forest plot | 11 | 384 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.94 [‐1.49, ‐0.38] |
| Analysis 1.14  Comparison 1 PRT versus control, Outcome 14 Time to stand from a chair. | ||||
| 15 Stair climbing (seconds) Show forest plot | 8 | 268 | Mean Difference (IV, Random, 95% CI) | ‐1.44 [‐2.51, ‐0.37] |
| Analysis 1.15  Comparison 1 PRT versus control, Outcome 15 Stair climbing (seconds). | ||||
| 16 Chair stand within time limit (number of times) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.16  Comparison 1 PRT versus control, Outcome 16 Chair stand within time limit (number of times). | ||||
| 17 Vitality (SF‐36/Vitality plus scale, higher = more vitality) Show forest plot | 10 | 611 | Mean Difference (IV, Fixed, 95% CI) | 1.33 [‐0.89, 3.55] |
| Analysis 1.17  Comparison 1 PRT versus control, Outcome 17 Vitality (SF‐36/Vitality plus scale, higher = more vitality). | ||||
| 18 Pain (higher = less pain, Bodily pain on SF‐36) Show forest plot | 10 | 587 | Mean Difference (IV, Fixed, 95% CI) | 0.34 [‐3.44, 4.12] |
| Analysis 1.18  Comparison 1 PRT versus control, Outcome 18 Pain (higher = less pain, Bodily pain on SF‐36). | ||||
| 19 Pain (lower score = less pain) Show forest plot | 6 | 503 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.30 [‐0.48, ‐0.13] |
| Analysis 1.19  Comparison 1 PRT versus control, Outcome 19 Pain (lower score = less pain). | ||||
| 20 Death Show forest plot | 13 | 1125 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.52, 1.54] |
| Analysis 1.20  Comparison 1 PRT versus control, Outcome 20 Death. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Main function measure (higher score = better function) Show forest plot | 2 | 62 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.17 [‐0.67, 0.33] |
| Analysis 2.1  Comparison 2 High versus low intensity PRT, Outcome 1 Main function measure (higher score = better function). | ||||
| 2 Main lower limb (LL) strength measure Show forest plot | 9 | 219 | Std. Mean Difference (IV, Random, 95% CI) | 0.48 [0.03, 0.93] |
| Analysis 2.2  Comparison 2 High versus low intensity PRT, Outcome 2 Main lower limb (LL) strength measure. | ||||
| 3 VO2 Max (ml/kg/min) Show forest plot | 3 | 101 | Mean Difference (IV, Random, 95% CI) | 1.82 [‐0.79, 4.43] |
| Analysis 2.3  Comparison 2 High versus low intensity PRT, Outcome 3 VO2 Max (ml/kg/min). | ||||
| 4 Pain (higher score = less pain) Show forest plot | 2 | 62 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.55, 0.45] |
| Analysis 2.4  Comparison 2 High versus low intensity PRT, Outcome 4 Pain (higher score = less pain). | ||||
| 5 Vitality (SF‐36, higher score = more vitality) Show forest plot | 2 | 62 | Mean Difference (IV, Fixed, 95% CI) | 6.54 [0.69, 12.39] |
| Analysis 2.5  Comparison 2 High versus low intensity PRT, Outcome 5 Vitality (SF‐36, higher score = more vitality). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Main lower limb (LL) strength measure Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 3.1  Comparison 3 High versus variable intensity PRT, Outcome 1 Main lower limb (LL) strength measure. | ||||
| 2 VO2 Max (ml/kg/min) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.2  Comparison 3 High versus variable intensity PRT, Outcome 2 VO2 Max (ml/kg/min). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Main LL strength measure Show forest plot | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.1  Comparison 4 PRT frequency, Outcome 1 Main LL strength measure. | ||||
| 1.1 Three times versus once per week | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Twice versus once per week | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Main lower limb (LL) strength measure Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.1  Comparison 5 PRT: 3‐sets versus 1‐sets, Outcome 1 Main lower limb (LL) strength measure. | ||||
| 2 Six‐minute walk test (meters) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.2  Comparison 5 PRT: 3‐sets versus 1‐sets, Outcome 2 Six‐minute walk test (meters). | ||||
| 3 Timed walk (seconds) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.3  Comparison 5 PRT: 3‐sets versus 1‐sets, Outcome 3 Timed walk (seconds). | ||||
| 4 Time to stand from a chair (seconds) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.4  Comparison 5 PRT: 3‐sets versus 1‐sets, Outcome 4 Time to stand from a chair (seconds). | ||||
| 5 Stair climbing (seconds) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.5  Comparison 5 PRT: 3‐sets versus 1‐sets, Outcome 5 Stair climbing (seconds). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Main function measure (higher score = better function) Show forest plot | 4 | 125 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.21 [‐0.56, 0.15] |
| Analysis 6.1  Comparison 6 PRT versus aerobic training, Outcome 1 Main function measure (higher score = better function). | ||||
| 2 Main function measure (lower score = better function) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.2  Comparison 6 PRT versus aerobic training, Outcome 2 Main function measure (lower score = better function). | ||||
| 3 Main lower limb strength measure Show forest plot | 10 | 487 | Std. Mean Difference (IV, Random, 95% CI) | 0.44 [0.08, 0.80] |
| Analysis 6.3  Comparison 6 PRT versus aerobic training, Outcome 3 Main lower limb strength measure. | ||||
| 4 VO2 max (ml/kg.min) Show forest plot | 8 | 423 | Mean Difference (IV, Random, 95% CI) | ‐1.13 [‐2.63, 0.38] |
| Analysis 6.4  Comparison 6 PRT versus aerobic training, Outcome 4 VO2 max (ml/kg.min). | ||||
| 5 Six minute walk test (meters) Show forest plot | 2 | 63 | Mean Difference (IV, Fixed, 95% CI) | ‐4.28 [‐48.24, 39.67] |
| Analysis 6.5  Comparison 6 PRT versus aerobic training, Outcome 5 Six minute walk test (meters). | ||||
| 6 Gait speed (m/s) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.6  Comparison 6 PRT versus aerobic training, Outcome 6 Gait speed (m/s). | ||||
| 7 Pain (lower score = less pain) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.7  Comparison 6 PRT versus aerobic training, Outcome 7 Pain (lower score = less pain). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Main function measure (higher score = better function) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 7.1  Comparison 7 PRT versus functional exercise, Outcome 1 Main function measure (higher score = better function). | ||||
| 2 Main lower limb strength measure Show forest plot | 3 | 158 | Mean Difference (IV, Fixed, 95% CI) | ‐6.51 [‐21.05, 8.04] |
| Analysis 7.2  Comparison 7 PRT versus functional exercise, Outcome 2 Main lower limb strength measure. | ||||
| 3 Timed "Up‐and‐Go" (seconds) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 7.3  Comparison 7 PRT versus functional exercise, Outcome 3 Timed "Up‐and‐Go" (seconds). | ||||
| 4 Vitality (SF‐36/Vitality plus scale, higher = more vitality) Show forest plot | 2 | 147 | Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐2.68, 2.54] |
| Analysis 7.4  Comparison 7 PRT versus functional exercise, Outcome 4 Vitality (SF‐36/Vitality plus scale, higher = more vitality). | ||||
| 5 Pain (higher = less pain, Bodily pain on SF‐36) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 7.5  Comparison 7 PRT versus functional exercise, Outcome 5 Pain (higher = less pain, Bodily pain on SF‐36). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 SF36 (higher score = better function) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.1  Comparison 8 PRT versus flexibility training, Outcome 1 SF36 (higher score = better function). | ||||
| 2 Main lower limb (LL) strength measure Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.2  Comparison 8 PRT versus flexibility training, Outcome 2 Main lower limb (LL) strength measure. | ||||
| 3 Timed walk (seconds) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.3  Comparison 8 PRT versus flexibility training, Outcome 3 Timed walk (seconds). | ||||
| 4 Time to stand from a chair (seconds) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.4  Comparison 8 PRT versus flexibility training, Outcome 4 Time to stand from a chair (seconds). | ||||
| 5 Vitality (SF‐36/Vitality plus scale, higher = more vitality) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.5  Comparison 8 PRT versus flexibility training, Outcome 5 Vitality (SF‐36/Vitality plus scale, higher = more vitality). | ||||
| 6 Pain (higher = less pain, Bodily pain on SF‐ 36) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.6  Comparison 8 PRT versus flexibility training, Outcome 6 Pain (higher = less pain, Bodily pain on SF‐ 36). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Main lower limb strength measure Show forest plot | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 9.1  Comparison 9 Power training, Outcome 1 Main lower limb strength measure. | ||||
| 1.1 High intensity (power treatment) versus control (control) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 High intensity (treatment) versus low intensity (control) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Strength (grouped by allocation concealment) Show forest plot | 73 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 10.1  Comparison 10 PRT versus control supplementary analyses, Outcome 1 Strength (grouped by allocation concealment). | ||||
| 1.1 Allocation concealed | 6 | 607 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.12 [‐0.04, 0.28] |
| 1.2 Concealment unknown | 67 | 2452 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.65 [0.56, 0.73] |
| 2 Strength (grouped by assessor blinding) Show forest plot | 73 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 10.2  Comparison 10 PRT versus control supplementary analyses, Outcome 2 Strength (grouped by assessor blinding). | ||||
| 2.1 Blinded assessors | 19 | 1523 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.23 [0.13, 0.34] |
| 2.2 Assessors were not blinded | 54 | 1536 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.88 [0.77, 0.99] |
| 3 Strength (grouped by intention‐to‐treat) Show forest plot | 73 | 3059 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.53 [0.46, 0.61] |
| Analysis 10.3  Comparison 10 PRT versus control supplementary analyses, Outcome 3 Strength (grouped by intention‐to‐treat). | ||||
| 3.1 Intention‐to‐treat was used | 12 | 1041 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.18 [0.06, 0.30] |
| 3.2 Intention‐to‐treat was not used | 61 | 2018 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.74 [0.64, 0.83] |
| 4 Strength (grouped by attention control) Show forest plot | 73 | 3059 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.53 [0.46, 0.61] |
| Analysis 10.4  Comparison 10 PRT versus control supplementary analyses, Outcome 4 Strength (grouped by attention control). | ||||
| 4.1 Attention control | 24 | 1408 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.34 [0.23, 0.44] |
| 4.2 No attention control | 49 | 1651 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.72 [0.61, 0.82] |
| 5 Strength (grouped by exercise intensity) Show forest plot | 72 | 3052 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.53 [0.45, 0.60] |
| Analysis 10.5  Comparison 10 PRT versus control supplementary analyses, Outcome 5 Strength (grouped by exercise intensity). | ||||
| 5.1 High intensity | 54 | 2026 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.60 [0.51, 0.70] |
| 5.2 Low‐to‐moderate intensity | 19 | 1026 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.39 [0.26, 0.51] |
| 6 Strength (grouped by exercise duration) Show forest plot | 56 | 2564 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.53 [0.45, 0.61] |
| Analysis 10.6  Comparison 10 PRT versus control supplementary analyses, Outcome 6 Strength (grouped by exercise duration). | ||||
| 6.1 Less than 12 weeks | 20 | 828 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.52 [0.37, 0.66] |
| 6.2 Longer than 12 weeks | 36 | 1736 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.53 [0.43, 0.63] |
| 7 Strength (grouped by health status) Show forest plot | 65 | 2428 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.60 [0.52, 0.69] |
| Analysis 10.7  Comparison 10 PRT versus control supplementary analyses, Outcome 7 Strength (grouped by health status). | ||||
| 7.1 Healthy participants | 46 | 1502 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.77 [0.66, 0.88] |
| 7.2 Older adults with a specific health problem | 19 | 926 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.37 [0.24, 0.51] |
| 8 Strength (grouped by functional limitations) Show forest plot | 54 | 2133 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.60 [0.51, 0.70] |
| Analysis 10.8  Comparison 10 PRT versus control supplementary analyses, Outcome 8 Strength (grouped by functional limitations). | ||||
| 8.1 No functional limitations | 41 | 1349 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.81 [0.69, 0.93] |
| 8.2 With functional limitations | 13 | 784 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.30 [0.16, 0.44] |
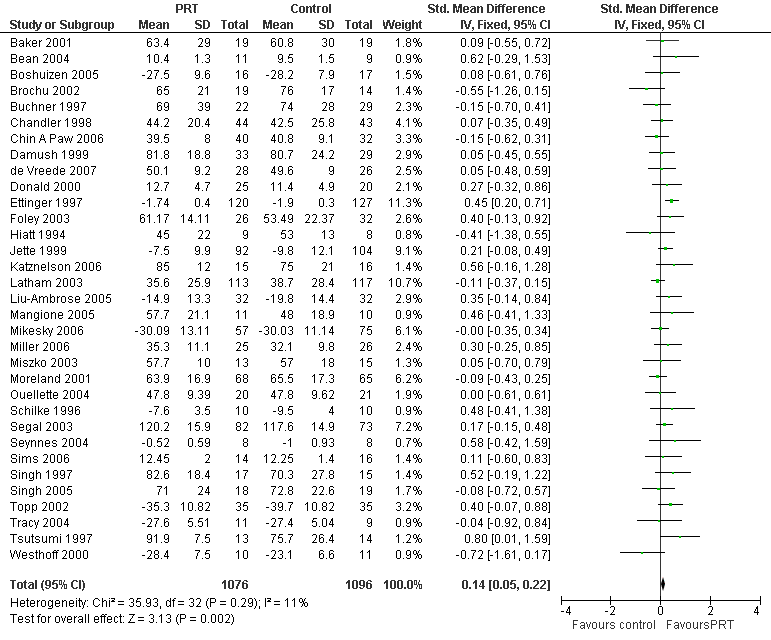
Forest plot of comparison: 1 PRT versus control, outcome: 1.1 Main function measure (higher score = better function).

Comparison 1 PRT versus control, Outcome 1 Main function measure (higher score = better function).

Comparison 1 PRT versus control, Outcome 2 Physical function domain of SF‐36/SF‐12 (Higher score = better function).

Comparison 1 PRT versus control, Outcome 3 Activities of daily living measure (higher score = better function).

Comparison 1 PRT versus control, Outcome 4 Activity level measure (kJ/week).

Comparison 1 PRT versus control, Outcome 5 Main lower limb (LL) strength measure.

Comparison 1 PRT versus control, Outcome 6 Main measure of aerobic function.

Comparison 1 PRT versus control, Outcome 7 VO2 or peak oxygen uptake.
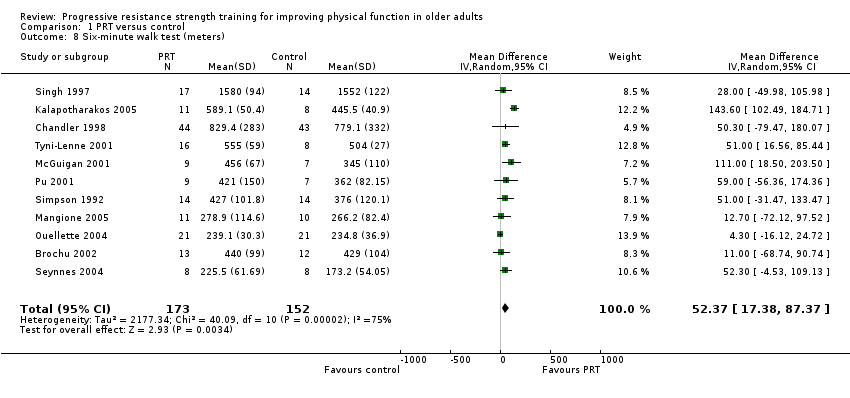
Comparison 1 PRT versus control, Outcome 8 Six‐minute walk test (meters).

Comparison 1 PRT versus control, Outcome 9 Balance measures (higher = better balance).

Comparison 1 PRT versus control, Outcome 10 Balance measures (Low = better balance).

Comparison 1 PRT versus control, Outcome 11 Gait speed (m/s).

Comparison 1 PRT versus control, Outcome 12 Timed walk (seconds).
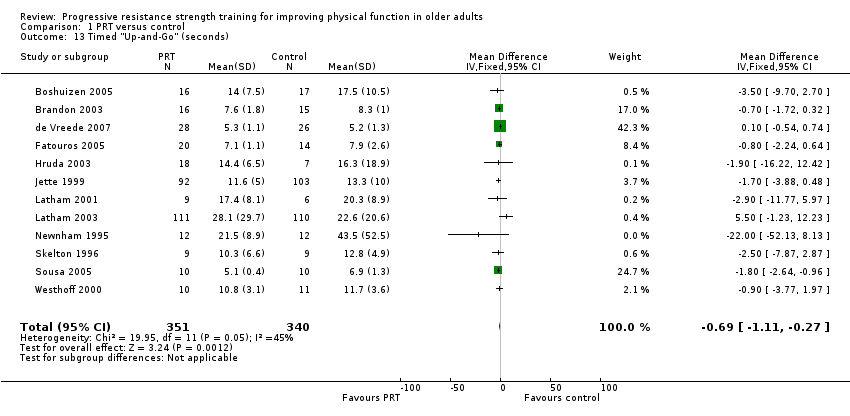
Comparison 1 PRT versus control, Outcome 13 Timed "Up‐and‐Go" (seconds).

Comparison 1 PRT versus control, Outcome 14 Time to stand from a chair.
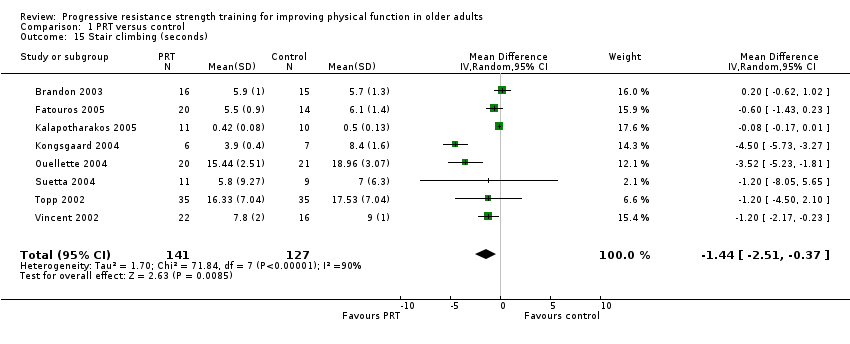
Comparison 1 PRT versus control, Outcome 15 Stair climbing (seconds).

Comparison 1 PRT versus control, Outcome 16 Chair stand within time limit (number of times).

Comparison 1 PRT versus control, Outcome 17 Vitality (SF‐36/Vitality plus scale, higher = more vitality).

Comparison 1 PRT versus control, Outcome 18 Pain (higher = less pain, Bodily pain on SF‐36).
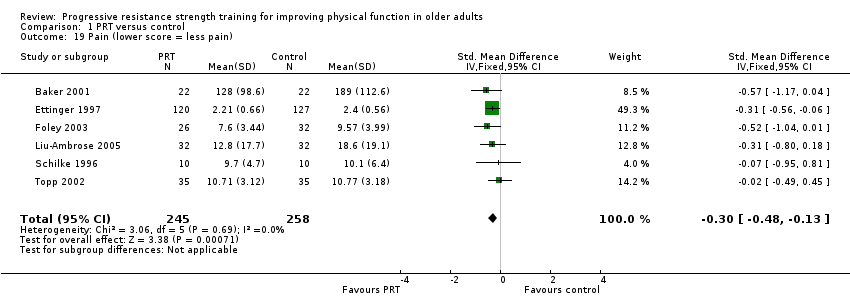
Comparison 1 PRT versus control, Outcome 19 Pain (lower score = less pain).

Comparison 1 PRT versus control, Outcome 20 Death.
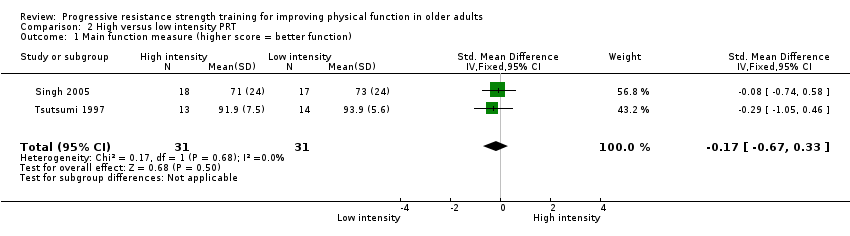
Comparison 2 High versus low intensity PRT, Outcome 1 Main function measure (higher score = better function).

Comparison 2 High versus low intensity PRT, Outcome 2 Main lower limb (LL) strength measure.
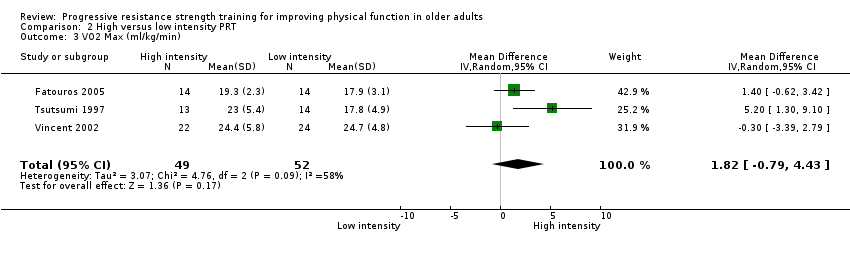
Comparison 2 High versus low intensity PRT, Outcome 3 VO2 Max (ml/kg/min).

Comparison 2 High versus low intensity PRT, Outcome 4 Pain (higher score = less pain).

Comparison 2 High versus low intensity PRT, Outcome 5 Vitality (SF‐36, higher score = more vitality).
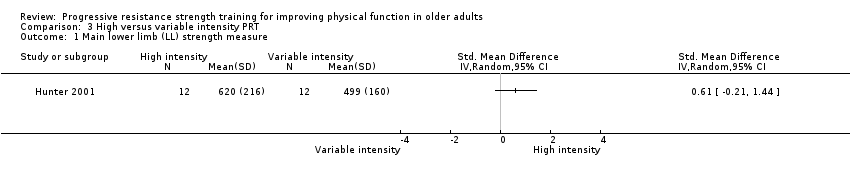
Comparison 3 High versus variable intensity PRT, Outcome 1 Main lower limb (LL) strength measure.
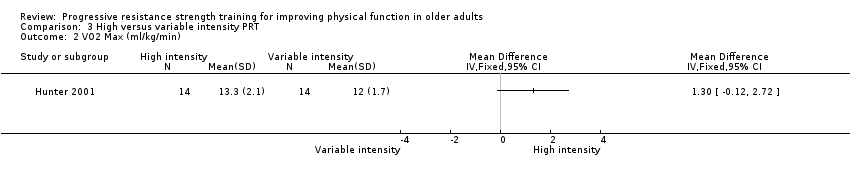
Comparison 3 High versus variable intensity PRT, Outcome 2 VO2 Max (ml/kg/min).
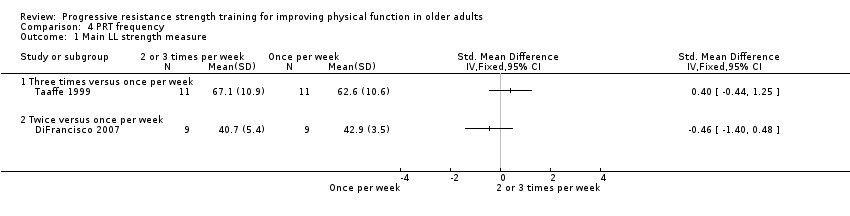
Comparison 4 PRT frequency, Outcome 1 Main LL strength measure.
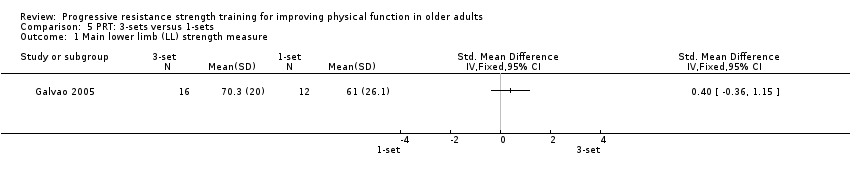
Comparison 5 PRT: 3‐sets versus 1‐sets, Outcome 1 Main lower limb (LL) strength measure.

Comparison 5 PRT: 3‐sets versus 1‐sets, Outcome 2 Six‐minute walk test (meters).
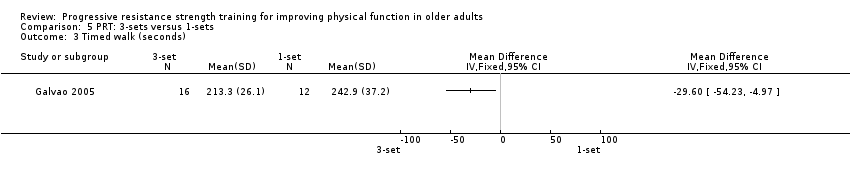
Comparison 5 PRT: 3‐sets versus 1‐sets, Outcome 3 Timed walk (seconds).
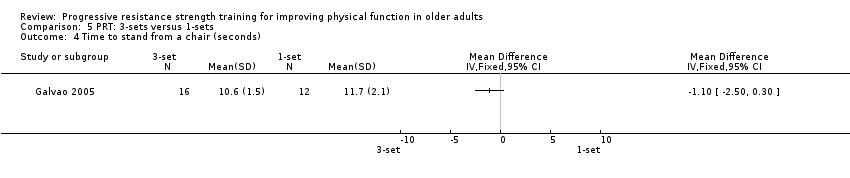
Comparison 5 PRT: 3‐sets versus 1‐sets, Outcome 4 Time to stand from a chair (seconds).
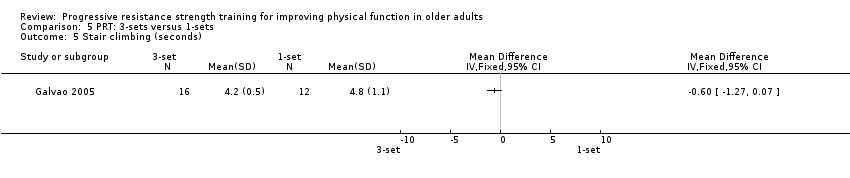
Comparison 5 PRT: 3‐sets versus 1‐sets, Outcome 5 Stair climbing (seconds).

Comparison 6 PRT versus aerobic training, Outcome 1 Main function measure (higher score = better function).

Comparison 6 PRT versus aerobic training, Outcome 2 Main function measure (lower score = better function).

Comparison 6 PRT versus aerobic training, Outcome 3 Main lower limb strength measure.
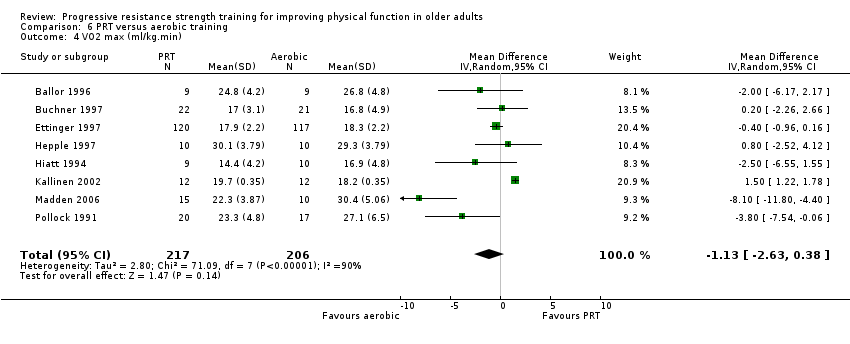
Comparison 6 PRT versus aerobic training, Outcome 4 VO2 max (ml/kg.min).
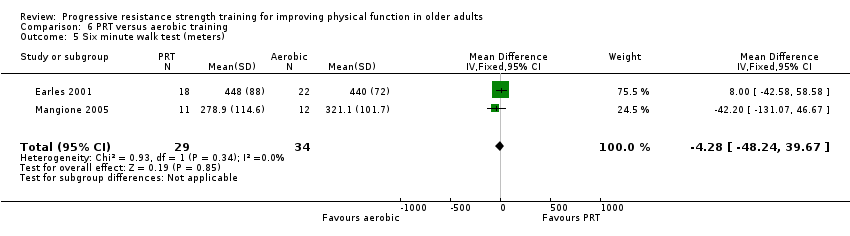
Comparison 6 PRT versus aerobic training, Outcome 5 Six minute walk test (meters).
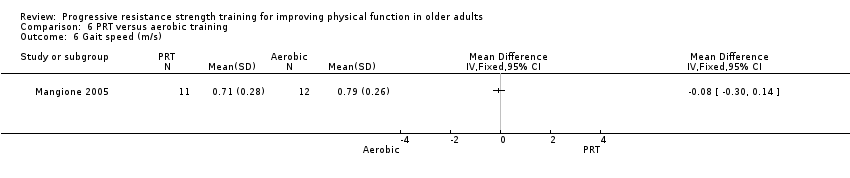
Comparison 6 PRT versus aerobic training, Outcome 6 Gait speed (m/s).

Comparison 6 PRT versus aerobic training, Outcome 7 Pain (lower score = less pain).

Comparison 7 PRT versus functional exercise, Outcome 1 Main function measure (higher score = better function).
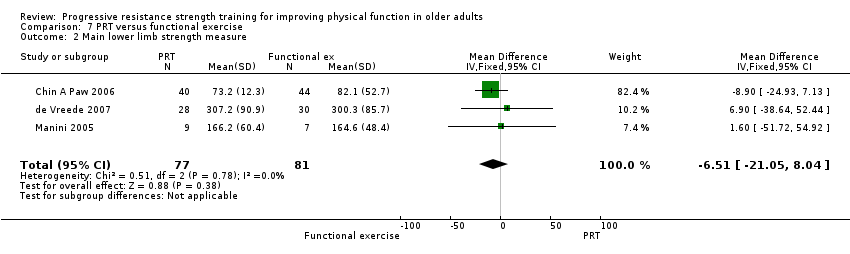
Comparison 7 PRT versus functional exercise, Outcome 2 Main lower limb strength measure.

Comparison 7 PRT versus functional exercise, Outcome 3 Timed "Up‐and‐Go" (seconds).

Comparison 7 PRT versus functional exercise, Outcome 4 Vitality (SF‐36/Vitality plus scale, higher = more vitality).

Comparison 7 PRT versus functional exercise, Outcome 5 Pain (higher = less pain, Bodily pain on SF‐36).

Comparison 8 PRT versus flexibility training, Outcome 1 SF36 (higher score = better function).

Comparison 8 PRT versus flexibility training, Outcome 2 Main lower limb (LL) strength measure.

Comparison 8 PRT versus flexibility training, Outcome 3 Timed walk (seconds).

Comparison 8 PRT versus flexibility training, Outcome 4 Time to stand from a chair (seconds).

Comparison 8 PRT versus flexibility training, Outcome 5 Vitality (SF‐36/Vitality plus scale, higher = more vitality).
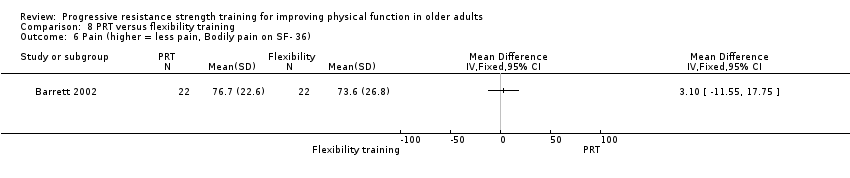
Comparison 8 PRT versus flexibility training, Outcome 6 Pain (higher = less pain, Bodily pain on SF‐ 36).

Comparison 9 Power training, Outcome 1 Main lower limb strength measure.
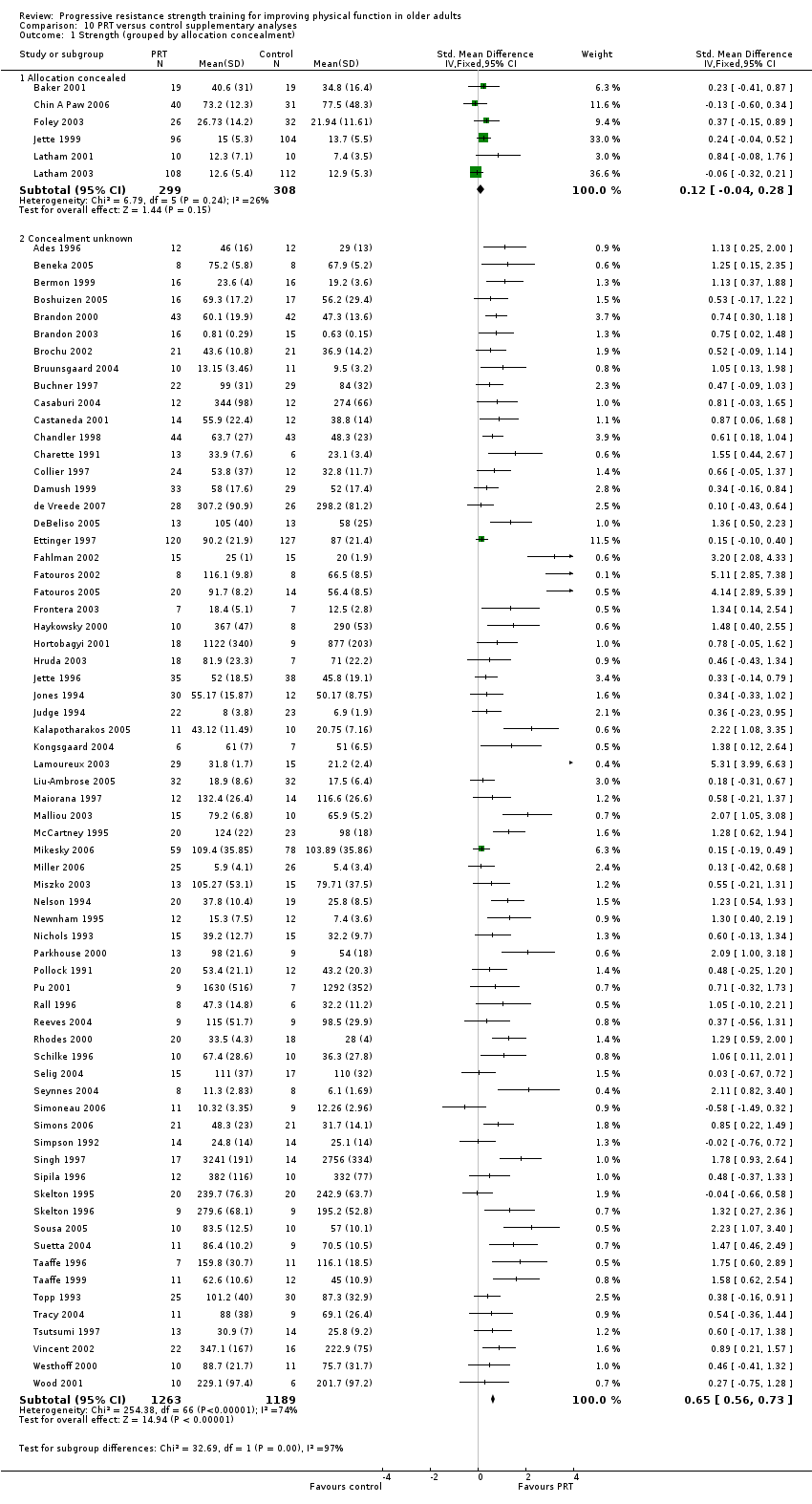
Comparison 10 PRT versus control supplementary analyses, Outcome 1 Strength (grouped by allocation concealment).

Comparison 10 PRT versus control supplementary analyses, Outcome 2 Strength (grouped by assessor blinding).

Comparison 10 PRT versus control supplementary analyses, Outcome 3 Strength (grouped by intention‐to‐treat).
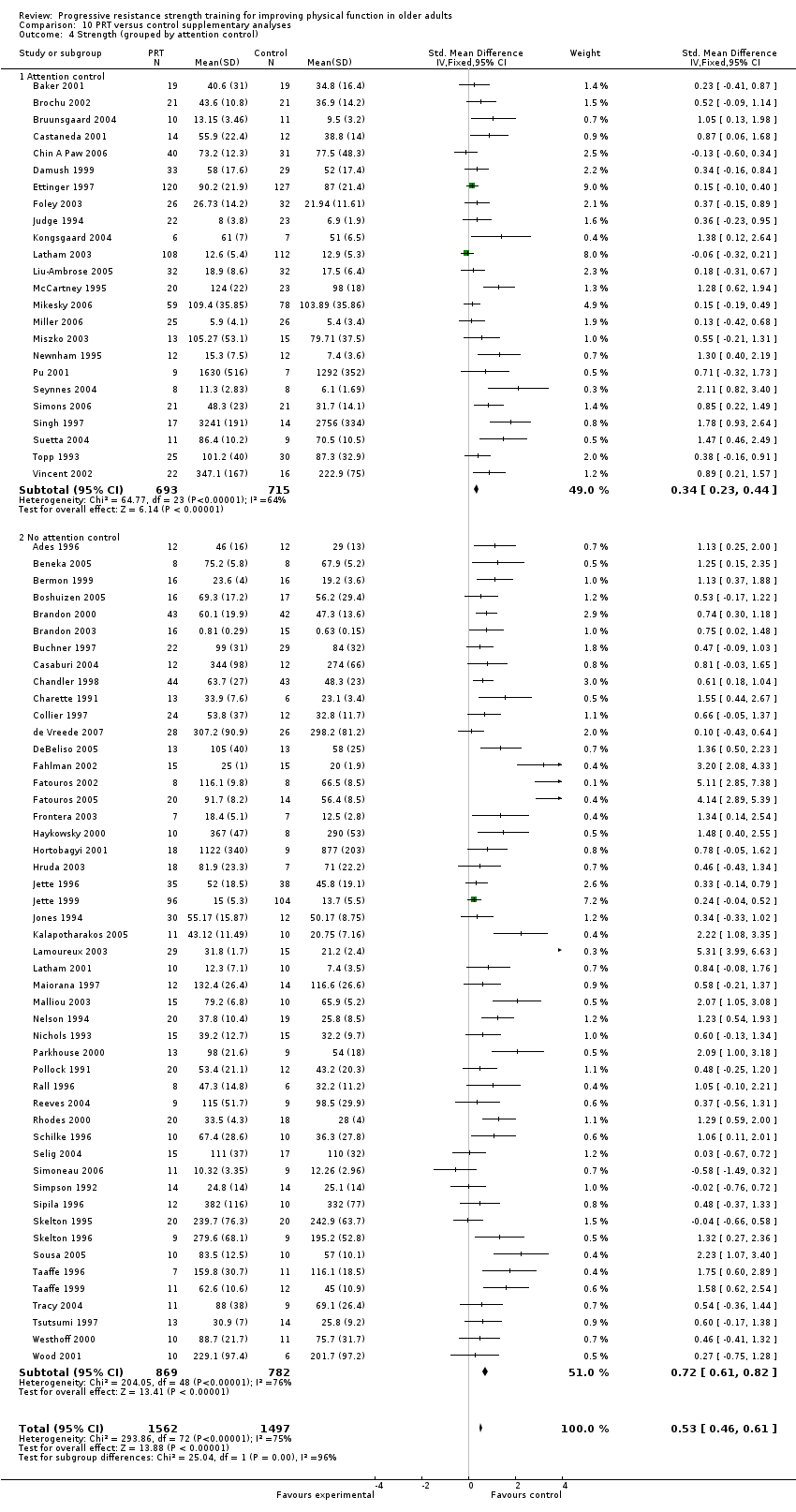
Comparison 10 PRT versus control supplementary analyses, Outcome 4 Strength (grouped by attention control).
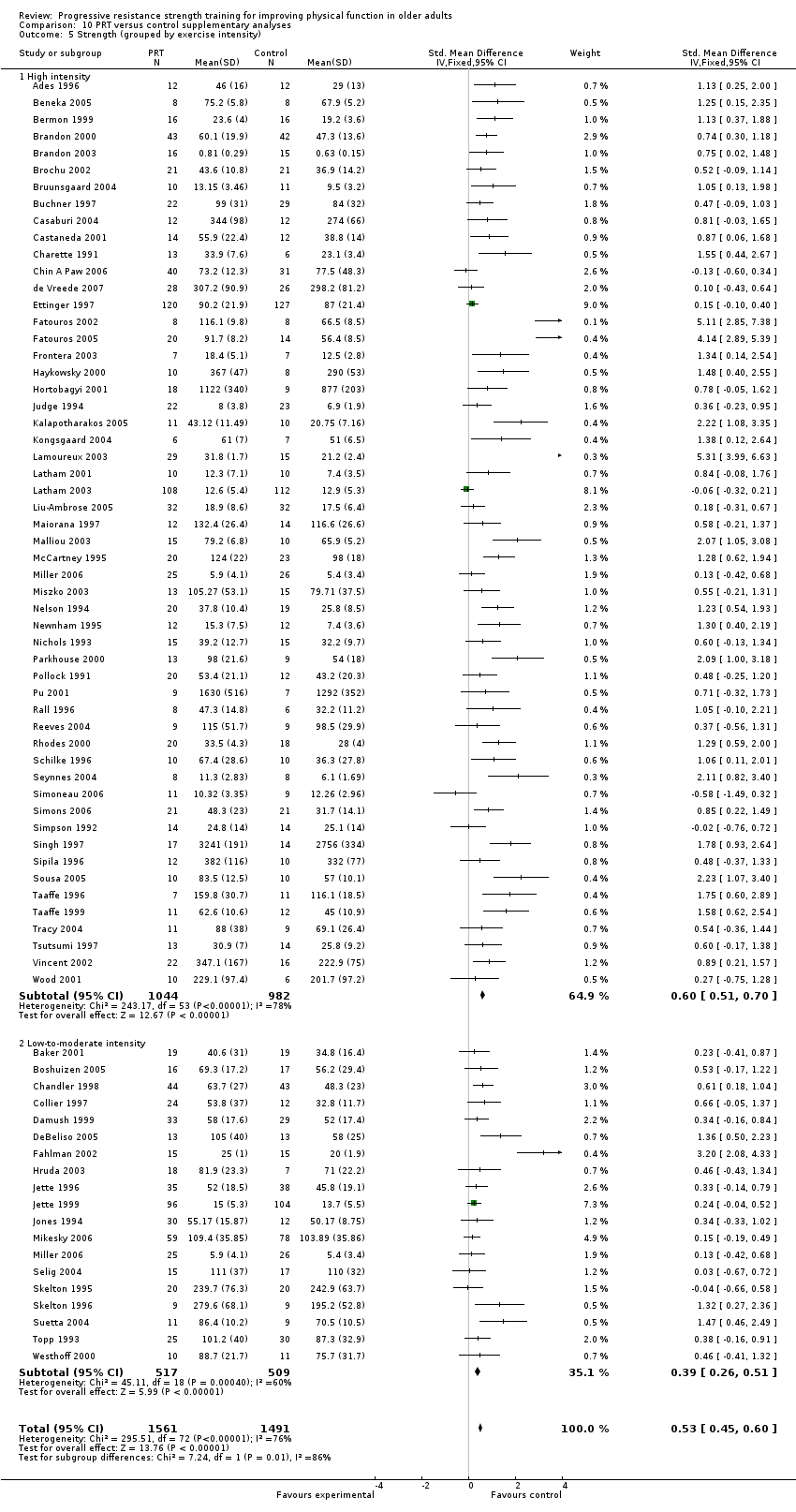
Comparison 10 PRT versus control supplementary analyses, Outcome 5 Strength (grouped by exercise intensity).
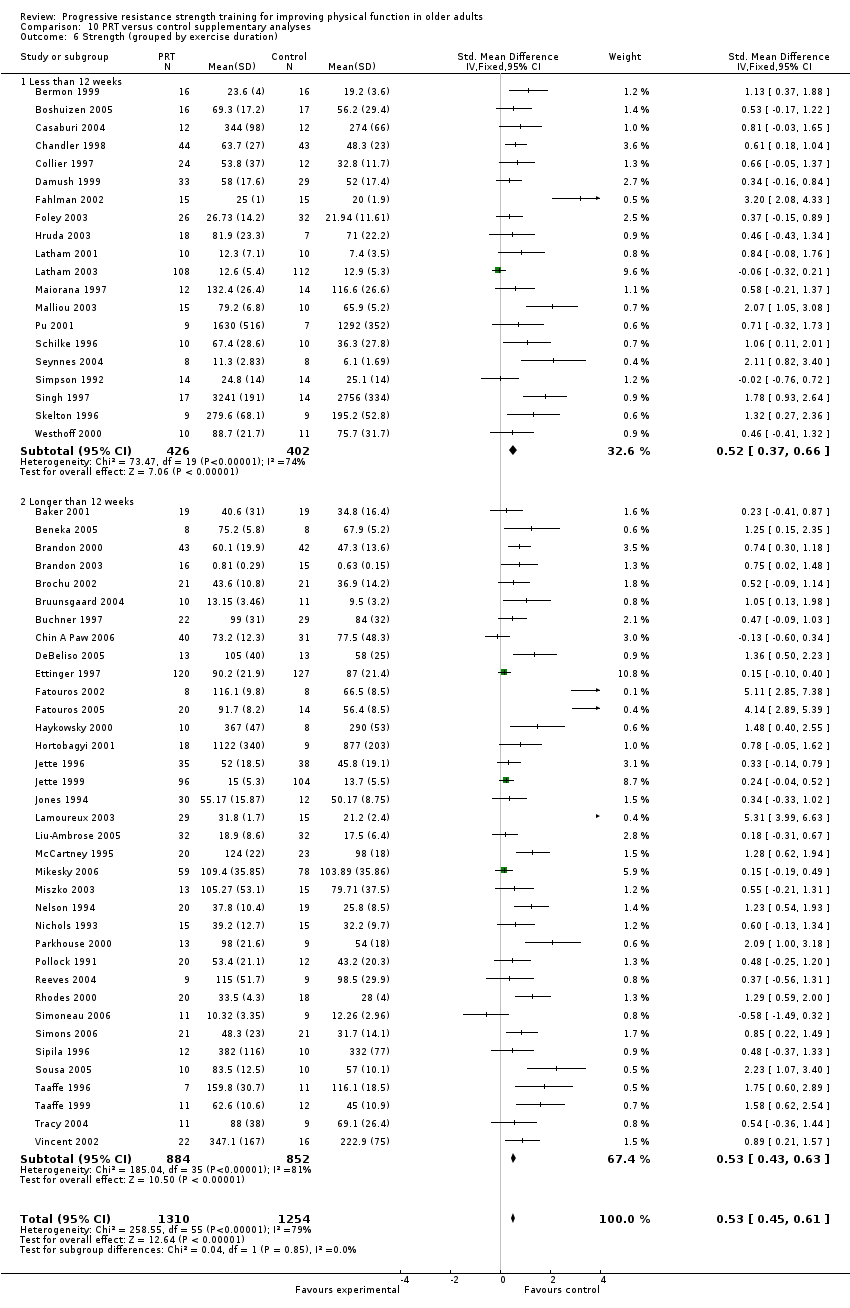
Comparison 10 PRT versus control supplementary analyses, Outcome 6 Strength (grouped by exercise duration).
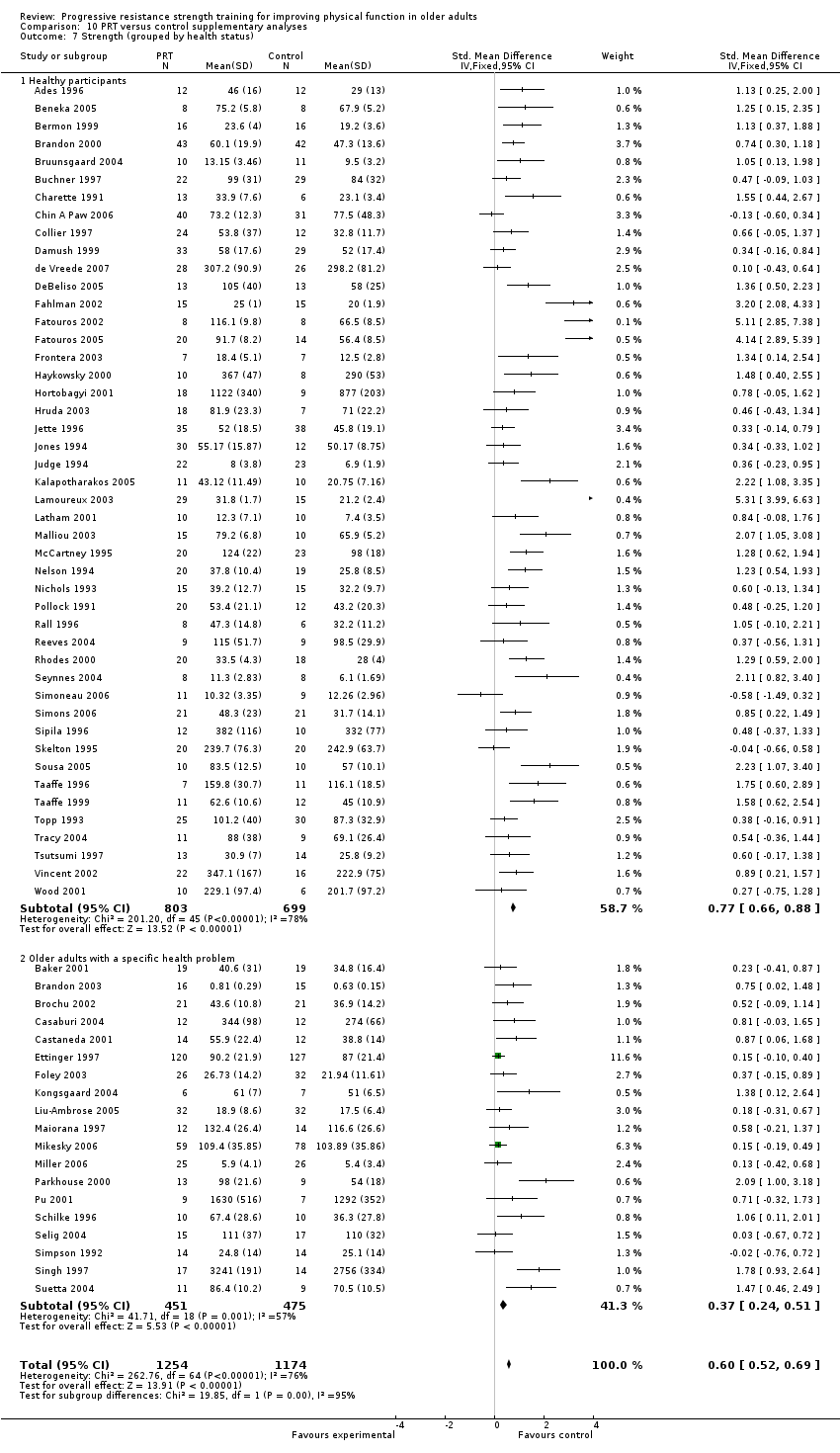
Comparison 10 PRT versus control supplementary analyses, Outcome 7 Strength (grouped by health status).
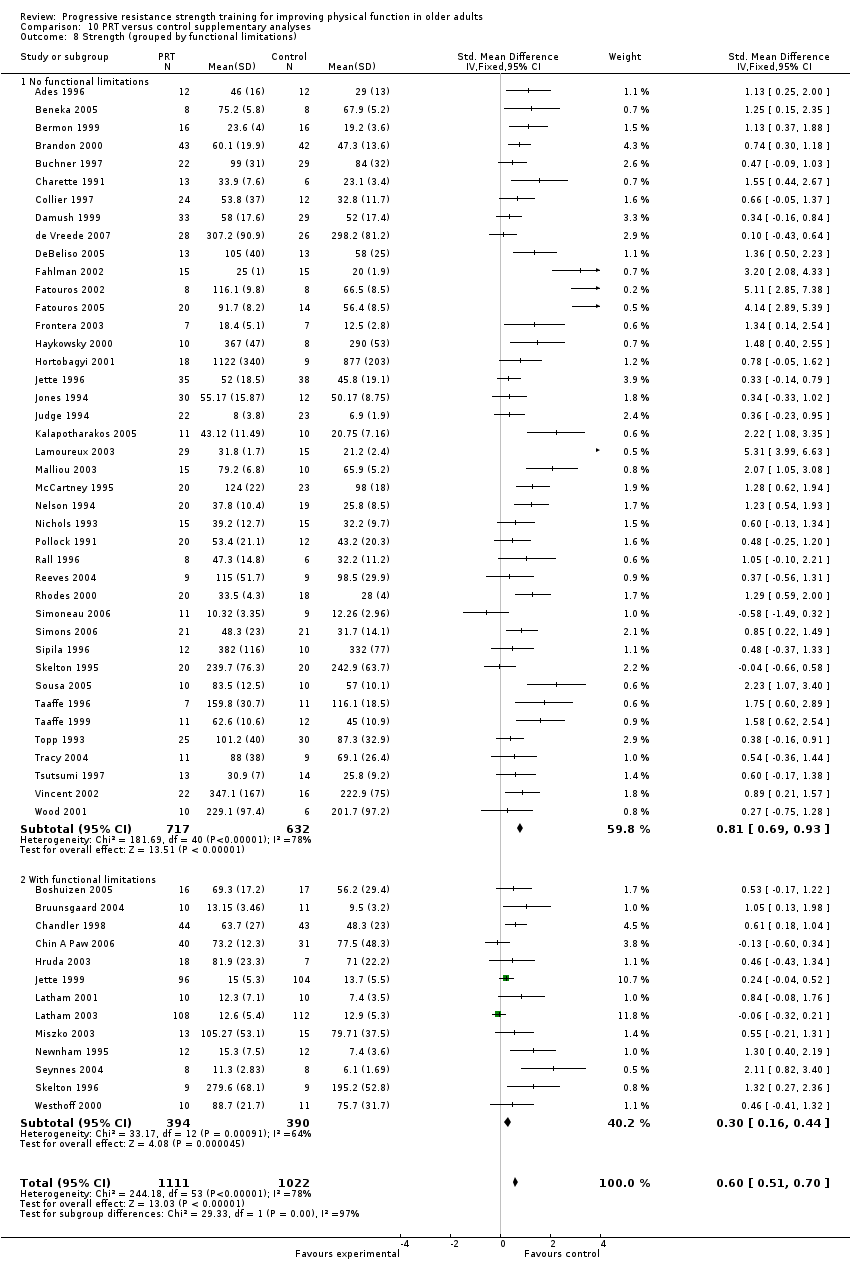
Comparison 10 PRT versus control supplementary analyses, Outcome 8 Strength (grouped by functional limitations).
| Items | Scores | Notes |
| A. Was the assigned treatment adequately concealed prior to allocation? | 2 = method did not allow disclosure of assignment. | |
| B. Were the outcomes of patients/participants who withdrew described and included in the analysis (intention‐to‐treat)? | 2 = withdrawals well described and accounted for in analysis. | |
| C. Were the outcome assessors blind to treatment status? | 2 = effective action taken to blind assessors. | |
| D. Were the participants blinded to the treatment status? | 2 = effective action taken to blind assessors. | |
| E. Were the treatment and control group comparable at entry? Specifically, were the groups comparable with respect to age, medical co‐morbidities (one or more of history of coronary artery disease, stroke, hypertension, diabetes, chronic lung disease), pre‐entry physical dependency (independent vs dependent in self‐care ADL) and mental status (clinical evidence of cognitive impairment, yes or no)? | 2 = good comparability of groups, or confounding adjusted for in analysis. | |
| F. Were care programmes, other than the trial options, identical? | 2 = care programmes clearly identical. | |
| G. Were the inclusion and exclusion criteria clearly defined? | 2 = clearly defined. | |
| H. Were the interventions clearly defined? | 2 = clearly defined interventions are applied with a standardised protocol. | |
| I. Were the outcome measures used clearly defined? | 2 = clearly defined measures and the method of data collection and scoring are clearly described | For our primary outcome, physical disability in terms of self‐report measures of physical function, we considered the outcome clearly defined if a validated and standardised scale was used and the method of data collection was clearly described. |
| J. Was the surveillance active and of clinically appropriate duration (i.e. at least 3 months)? | 2 = active and appropriate duration (three months follow‐up or greater). |
| Study | Concealed allocation | ITT | Assessor blind | Participants blind | Compable at entry | Identical care | Inclusion/ exclusion | Interventions defined | Outcomes defined |
| 1 | 0 | 0 | 0 | 2 | 2 | 0 | 2 | 1 | |
| 2 | 2/0 | 2/0 | 2 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 1 | 1 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 2 | 2 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 1 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 1 | 0 | 2 | 2 | |
| 1 | 1 | 2 | 0 | 1 | 2 | 2 | 2 | 2 | |
| 0 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 1 | 0 | 0 | 2 | 0 | 1 | 2 | 2 | |
| 1 | 1 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 1 | 0 | 0 | 2 | 2 | 1 | 2 | 1 | |
| 1 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 1 | 2 | 0 | 2 | 2 | 2 | 2 | 1 | |
| 1 | 1 | 2/0 | 2 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 2 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 1 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 1 | 2 | 0 | 2 | 2 | |
| 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 1 | 2 | 1 | 1 | 2 | |
| 1 | 0 | 0 | 1 | 2 | 2 | 1 | 1 | 2 | |
| 1 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 1 | 2 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 1 | 0 | 0 | 2 | 0 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 1 | 2 | 1 | 2 | 2 | |
| 2 | 0 | 0 | 0 | 2 | 2 | 0 | 0 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 1 | 2 | 1 | 2 | 2 | |
| 1 | 1 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 1 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 2 | 2/0 | 1 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 0 | 1 | 0 | 2 | 0 | 2 | 2 | |
| 1 | 1 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 0 | 1 | 2 | 2 | |
| 1 | 1 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 0 | 2 | 2 | |
| 1 | 1 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 1 | 2 | 0 | 0 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 1 | 1 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 1 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 0 | 2 | 1 | |
| 1 | 1 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 2 | 0 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 2 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 1 | 2 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 1 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 1 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 1 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | |
| 1 | 1 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 2 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 2 | 0 | 0 | 0 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 1 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 1 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 1 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 2 | 1 | 1 | 2 | 2 | 1 | 2 | |
| 1 | 0 | 0 | 1 | 2 | 2 | 2 | 2 | 1 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 1 | |
| 2 | 0 | 2 | 1 | 2 | 2 | 2 | 1 | 2 | |
| 1 | 0 | 0 | 1 | 1 | 2 | 0 | 1 | 1 | |
| 1 | 2 | 2 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 1 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 2 | 2 | 2 | 1 | 2 | 2 | 0 | 0 | 0 | |
| 1 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 1 | |
| 1 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 1 | 2 | 2 | 1 | 1 | |
| 1 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 2 | 2/0 | 2 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 1 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 0 | 1 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 1 | |
| 1 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 1 | 0 | 2 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 1 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 2 | 1 | 1 | |
| 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 2/0 | 1 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 1 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 1 | |
| 1 | 0 | 0 | 0 | 2 | 0 | 1 | 2 | 2 | |
| 1 | 1 | 1 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 2 | 2 | 2 | 0/2 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 1 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 1 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 1 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 1 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 1 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 1 | 2 | 1 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 0 | 2 | 0 | 2 | 2 | 1 | 2 | 2 | |
| 1 | 1 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| Note: 2/0 indicates that different standards used to assess different outcomes in the same study | |||||||||
| Study | Outcome Measure | Treatment Group | Control Group |
| Physical performance test at 6 month. Mean = baseline score + change score. SD was not reported. | 9.2 | 8.1 | |
| mean change in number of independent IADL's | mean 0.1 (SD 0.7) | mean 0.2 (SD 0.7) | |
| Barthel Index (actual data not in paper) | no significant difference | ||
| ankle activity monitors (counts/day) | mean change 3412 (SD 1700) | mean change ‐1230 (SD 1670) | |
| overall self‐reported activity level (measure not specified) | significant improvement (p<0.05) in exercise group | NR | |
| SF‐36‐PF | No significant differences between high intensity and low intensity groups | ||
| SF‐36 ‐ PF (actual data not reported) | no significant difference between groups (data not reported) | ||
| three ADLs of a questionnaire developed by the Danish Institute of Clinical Epidemiology | Actual data not reported. The author stated that the self‐reported ADL level was significantly higher in the Ex group than in the control group | ||
| SF‐36. 7 people (2 in PRT, 5 in Functional training) reported improvement in the SF‐36 items | |||
| Physical Activity Questionnaire (no reference) self report | mean 209.8 (SD 142.9) kJ/kg | mean 250.1 (SD 225) kJ/kg | |
| SF‐36 PF (no SD/SE reported) | mean 50.3 | mean 49.2 | |
| WOMAC section C (no SD/SE reported) | 464.4 | 606.6 | |
| Aims Mobility (no SD/SE reported) | 1.28 | 1.21 | |
| Barthel Index (medians reported) | median change 0 (range ‐1 to 2) | median change control 0 (range ‐1 to 1) | |
| adapted version of Lawton and Brody's IADL scale (higher = better, not pooled because study was cluster randomised) | mean 105 (SD 12) | mean 68 (SD 25) | |
| SF‐36 physical function at 30 month (the intervention was 1 ‐ year) | n =81, mean = 65.37 (SD = 25.05) | n = 79, mean = 63.88 (SD = 25.48) | |
| Blair Seven‐day recall Caloric Expenditure (KCalories) | not significantly altered | not significantly altered | |
| AIMS mobility score (actual data not reported) | "no significant differences between or within groups" | ||
| IADL (Lawton Brody Scale) | mean 23.4 (SD 0.4) | mean 23.9 (SD 0.1) | |
| Human Activity Profile ‐ (only reported training groups % change and the P‐value of the change) | 3.9% change3.9% change | NR | |
| Human Activity Profile ‐ Max Activity Score | 0% change | NR | |
| Human Activity Profile | no difference from baseline | no difference from baseline | |
| Rivermead Motor Assessment | Significant improvement was found for people in the control group with low‐level function | ||
| Minnesota Living with Heart Failure Questionnaire (lower score = better QOL, medians reported) | median 19 (range 0‐61) | median 44 (range 3‐103) |
| Study | Fall Statistic | PRT | Control |
| 1) Cox regression analysis, time to first fall, 0.53, 95% CI 0.3‐0.91 for exercise group (including endurance exercise groups) | |||
| 2) proportion of people who fell in one year | all exercise groups: 42% | 60% | |
| 3) fall rate (falls/year) | all exercise: 0.81 falls/year | 0.49 falls/year | |
| 1) number of falls | 7 (n = 32) | 4 (n = 27) | |
| 2) number of people who fell | 6 (n = 32) | 2 (n = 27) | |
| 1) average falls/subject | 2.32 | 2.77 | |
| 2) covariance adjusted treatment incidence ratio (PRT vs control) | 0.95 (95% CI 0.64, 1.41) | ||
| falls | no difference between groups (no data provided) | ||
| 1) Average falls/subject | 0.82 | 1.22 | |
| 2) Co‐variate adjusted treatment incidence ratio (PRT vs control) | 0.61 (95%CI 0.34,1.09) | ||
| 1) Average falls/subject | 0.68 | 1.6 | |
| 2) Co‐variate adjusted treatment incidence ratio (PRT vs control) | 0.91 (95%CI 0.48,1.74) | ||
| 1 in the PRT group sustained an unrelated fall halfway through the 6‐week intervention, resulting in injury of her dominate shoulder. Exercise was modified for her. | 1 | 0 | |
| total falls | 164 | 149 | |
| 1) number of people who fell | 60 | 64 | |
| 2) fall‐rate, person years | 1.02 | 1.07 | |
| the frequency of falls (excluded falls occurred in exercise classes) | 18 (1 subject fell 7 times) | 0 | |
| Reported the number of participants fell during post‐training examination (n = 1 ‐ group was not reported) | |||
| Report number of people | 5 | 1 | |
| Numbers per person, no statistical difference between groups | .15 (.37) | 0 | |
| Note: Data marked with * were obtained from Province 1995 | |||
| Study | Any Comment re: AE | AE Occurred (y/n/nr) | Description | Dropout Pathologies | Pain | Medical Care | Deaths |
| No |
|
| None reported |
|
|
| |
| Yes | No | NR | Yes, 2 in treatment group (neck arthritis, prior back injury), 2 in control (illness, psoriatic arthritis) | Treatment group decreased in WOMAC, SF‐36 BP no change | NR |
| |
| No |
|
| NR |
|
|
| |
| No |
|
| NR |
|
|
| |
| Yes | Yes | 2 in PRT group, aggravation of OA | 2 in PRT group, aggravation of OA |
|
|
| |
| Yes | Yes |
| The number of illness was not reported. 13% of repeated measurements after baseline were missing because of death or patient inability to perform the test because of acute illness. |
|
| 1 in the PRT group | |
| Yes | no | No significant adverse events occurred |
|
|
|
| |
| No | NR |
|
|
|
|
| |
| No |
|
| No |
|
|
| |
| Yes | yes |
| 9 dropout due to illness of participant or partner | 4 reported pain during or after the exercise |
| 1 in control | |
| No |
|
|
| NR | NR |
| |
| Yes | 8 members of exercise group had BP raised to over 200 mmHg systolic or 100 mmHg diastolic at some point during the exercises during 24 months; and had to stop exercising that day |
| Participant's disease (diabetics) got worse; specific number was not reported |
|
|
| |
| Yes | Yes | 2 experienced occasional significant exacerbation of arthritic conditions during the training. 1 experienced significant dizziness in a supine position. | Yes, 3 due to medical problems that are not related to the training | 2 individuals experienced occasional significant exacerbation of arthritic conditions during the training | NR | NR | |
| No | NR |
|
|
|
|
| |
| Yes | Yes | 6 Injuries in strength training or in strength/endurance training group (not reported separately, n = 50) | Not described | no significant change in BP of SF‐36 | For all exercise groups (i.e. including endurance exercise groups): stable outpatient visits in exercise group/ control increased, no difference in hospitalisation rates |
| |
| Yes | No |
| 5 (group?)‐non protocol related health problems | NR |
|
| |
| Yes | No |
| No |
|
|
| |
| Yes | Yes |
| The authors did not report the number and group of the dropouts. The statement is "reasons for early termination of the study included loss of greater than 20% of initial body weight, need for dialysis therapy or transplantation, development of a serious condition requiring hospitalization or precluding exercise and signs of malnutrition" |
|
|
| |
| No |
|
| 9 drop‐outs due to illness, 1 due to increased hip pain, 1 refused further strength testing (not given by group) | NR | NR |
| |
| No |
|
| 1 discomfort after initial strength testing, 3 intercurrent illness not related to training | NR | NR |
| |
| Yes | Yes | None withdrew because of adverse effects | 9 illness in PRT; 9 illness in functional training group; 10 illness in combined training group; 6 illness in control group |
|
| 1 in PRT; 4 in functional training; 1 in combined training; 2 in control group | |
| No |
|
| No |
|
|
| |
| No |
|
| 6 exercise drop‐outs due to illness |
|
|
| |
| Yes | Yes | 20 AEs reported in 17 participants. 16 were related to strength testing and 4 were related to power training. 8 were in high intensity group, 7 in medium, 4 in low, and 1 in control. AEs included minor strains, tendonities, and exacerbation of osteoarthritis. | 4 (1 in each group) dropout‐joint pain | Joint pain (see dropout pathologies) |
|
| |
| Yes | Yes | PRT: 1 had muscle strained. 10 reported muscle pain, 5 osteoarthritic joint pain, 3 prosthetic joint pain, and 4 lower back pain | PRT group: 1 hip fracture, 1 pneumonia, & 1 eye operation. Control: 1 wrist fracture | PRT: 10 reported muscle pain, 5 osteoarthritic joint pain, 3 prosthetic joint pain, and 4 lower back pain |
|
| |
| Yes | no | no injuries occurred during the training |
|
|
|
| |
| Yes | No | Occasionally complaints of muscle soreness for 2 days after exercise, but it did not affect participants' daily routine or training |
|
|
|
| |
| No |
|
| not clear |
|
|
| |
| Yes (a priori outcome) | Yes | 4 reported discomfort, 2 stopped program ‐ 1 due to back pain, 1 due to lumbar disc herniation, possibly due to study intervention | Yes |
|
|
| |
| Yes | Yes | PRT: 2 falls, one weight dropped on foot; Aerobic: 2 falls; Control: 1 sudden death (defined AE as death or injury requiring medical care) | NR | less for PRT group vs control | NR | NR | |
| No | NR |
|
|
|
|
| |
| No | NR |
|
|
|
|
| |
| Yes | Yes |
| 3 men stopped within the 1st week due to injury |
|
|
| |
| No |
|
| 1 exercise drop‐out due to increased musculoskeletal pain | NR | no difference in health care visits between groups | NR | |
| Yes | Yes | PRT: 2 reports of joint pain, program was altered No control info No cardiovascular events | 2 exercise drop outs, 1 due to musculoskeletal pain, 1 due to pneumonia | not measured | NR | 0 PRT and 1 control | |
| Yes | yes | see the dropout pathologies | 4 (2 in each group) discontinued secondary to exacerbation of preexist OA. 1 in the high velocity group withdrew secondary to recurrence of chronic plantar fasciicis |
|
|
| |
| No |
|
| NR | NR | NR | NR | |
| Yes | Yes | Gym‐based exercise group: 2 had increased pain and 1 had increased blood pressure. 1 ‐Dr. advised to cease program | Gym‐based exercise group: 2 with increased pain, 1 with unrelated surgery, 1 with increased blood pressure, and 1 had joint replacement surgery. Control group: 2 with joint replacement surgery and 1 with illness. | 2 reported increased pain the gym‐based exercise group. |
|
| |
| No | NR |
|
|
|
|
| |
| Yes | No | 1 in 1‐set group withdrew due to illness, 1 due to injury sustained during part‐time work, and 1 due to aggravation of a preexisting hip injury |
|
|
|
| |
| No |
|
| 3 PRT and 1 control withdrew because of minor injuries or previous medical problems exacerbated by testing/training | "no complaints of excess or intolerable muscle soreness or fatigue" | NR | NR | |
| Yes | No |
|
|
|
|
| |
| Yes | Yes |
| 1 in PRT withdrew because of shoulder discomfort and migraines. 1 in the combination training suffered a lower extremity injury not related to the study |
|
|
| |
| Yes | No (completed without complications) |
| NR |
|
|
| |
| No |
|
| NR |
|
|
| |
| No |
|
| No |
|
|
| |
| No |
|
| No |
|
|
| |
| No (not identified as such) | Yes | Pain and bruising of shoulder from machine ‐ dropped out | Yes | Yes | NR | NR | |
| Yes | Yes? |
| 5 (2 in the PRT group and 3 in the control group) dropped out due to health reasons |
|
|
| |
| No |
|
| NR |
|
|
| |
| No | NR |
|
|
|
|
| |
| No (not identified as such) |
|
| Yes ‐ 2 drop‐outs because of the exercises, 1 due to back pain, 1 due to shortness of breath during exercise, |
|
|
| |
| Yes | No |
| Reasons not described | NR, but fatigue significantly worse in exercise group | NR | NR | |
| Yes | No |
| NR |
|
|
| |
| Yes | No |
| NR |
|
|
| |
| Yes (a priori outcome of study) | Yes | 10/55 people in RT or combined balance and RT developed musculoskeletal complaints, (specific details given), only 1 complaint in balance group, no control report, no serious injuries in any group | NR | NR |
|
| |
| NR | NR |
|
|
|
|
| |
| Yes | Yes | 1‐PRT, died of myocardial infarction at 8 weeks; 1‐PRT, unstable angina at 4 weeks; 1 in PRT, began to have occasional angina and dyspnoea at 8 weeks; 1‐endurance, brainstem infarction at week 9, 1‐endurance, abnormal aortic aneurysm happened after the program | See the description |
|
| 1 in PRT, died of myocardial infarction | |
| Yes | Yes |
| 5 were due to events unrelated to study drug, including bruised ribs, need for knee replacement, angina prior to the baseline visit, nausea during the first week of the study, and excessive i e commitments. Another subject in the placebo arm withdrew because of depression. |
|
|
| |
| No |
|
| Yes ‐ 3 in FITNESS group, including wrist and back injury |
|
|
| |
| No | NR |
|
|
|
|
| |
| Yes | Yes | 1 in the PRT group sustained an unrelated fall halfway through the 6‐week intervention, resulting in injury of her dominate shoulder. Exercise was modified for her. |
|
|
|
| |
| No | NR |
|
|
|
|
| |
| Yes | No |
| No |
|
|
| |
| Yes (a priori outcome) | Yes | 18 musculoskeletal adverse events in PRT group vs 5 in control group | No |
|
| 6 in PRT versus 8 in control | |
| Yes | Yes | 10 in PRT group and 2 in stretching control group had minor musculoskeletal complains but resolved or diminished within 3 weeks | Yes, 1 in PRT and 1 in control drop out due to illness |
|
|
| |
| Yes | Yes | 1 back pain and 1 spur on the heel | 1 back pain and 1 spur on the heel | 1 back pain |
|
| |
| No | NR |
|
|
|
|
| |
| Yes (safety an aim of study) | Yes | In ex group: MI (before exercises began),1 vasovagal episode, 1 musculoskeletal pain. Control: 2 people stop testing because of aggravation of psoriatic arthritis(1) and atrial fibrilation (1) | Yes, as reported | NR | NR ‐ ischaemic symptoms/ECG changes during training |
| |
| No | NR |
|
|
|
|
| |
| Yes | Yes | several participants reported muscle soreness or fatigue in the PRT group. 1 fell during post‐training examination, 4 in the PRT were hospitalized | in the PRT group, 1‐illness (progressive neuromuscular disorder), 4 were hospitalized. | 1 in aerobic training group was unable to perform exercise at recommended intensity level |
| 2 (among those who were hospitalized) in the PRT group | |
| Yes | Yes | 11 were excluded from the steadiness experiment because of discomfort from knee OA during the testing protocol. 14 dropout for a variety of medical personal reasons | 11 were excluded from the steadiness experiment because of discomfort from knee OA during the testing protocol. 14 others dropped out for a variety of medical and personal reasons. |
|
|
| |
| Yes | No |
| Yes, 4 drop‐outs due to increased pain "but neither subjects nor investigators attributed pain to the treatment" | WOMAC pain, 143.8 in PRT vs 167.1 control | NR | NR | |
| Yes | No |
| 9 exercise drop‐outs due to "illness", 3 controls due to medical problems. Stated "no injuries as a result of training" |
|
|
| |
| No |
|
| NR |
|
|
| |
| Yes | No |
| see hosp admissions |
| 3 hospital admissions in PRT, 2 in control, 3 in home mobility ‐ reported not related to exercise | 2 in home mobility group, no others ‐ not related to exercise | |
| No |
|
| NR |
|
|
| |
| Yes | Yes | 1 discontinued in the PRT group because of increased knee pain | 1 discontinued in the PRT group because of increased knee pain | 1 discontinued in the PRT group because of increased knee pain |
|
| |
| No | NR |
|
|
| Discharge destination ‐ on discharge from acute care, 52 participants were discharged to a rehabilitation programme, 12 were transferred to a community hospital, 16 were discharged to higher level care and 20 returned directly to their pre‐injury admission accommodation. | 2 in PRT, 1 in attention control | |
| Yes | Yes | 6 women fell (5 in PRT, 1 in control) | some (the number is not specified) due to personal medical reasons or injuries |
|
|
| |
| Yes (a priori outcome) | Yes | yes to pain or stiffness = 14 in PRT vs 8 in control; other adverse: 8 in PRT vs 3 in control | 5 withdrew due to medical complications in PRT vs 3 in control |
|
|
| |
| Yes | Yes | 7/20 in PRT group experienced transient musculoskeletal pain; 3 musculoskeletal injuries (2 fractures and 1 sprain) in the control group | No ‐ MI in PRT group occurred while patient was on vacation |
|
|
| |
| No |
|
| No |
|
| 3 in each group | |
| Yes (safety a priori objective) | Yes | control subject contused sternum during baseline testing, mild to moderate delayed onset muscle soreness | PRT ‐ 1 injury unrelated to program |
|
|
| |
| Yes | Yes, 4 events | 1 in the PRT group was withdrawn after coronary artery stent placement unrelated to study participation. 2 subjects did not undergo week‐12 strength testing due to recurrence of an inguinal hernia (PRT group) and ECG abnormalities (control group). A fourth subject experienced anginal symptoms consistent with coronary artery disease but returned to the study after medical clearance. | Please see the description |
|
|
| |
| No |
|
| NR |
|
|
| |
| Yes (a‐priori outcome, well‐defined) | Yes | 11/57 subjects sustained an injury during 1RM testing; 2/23 sustained an injury during training. In aerobic group, no injuries during testing but 9/21 had an injury during training | NR by group |
|
|
| |
| Yes | Yes | 1 control patient developed trochanteric bursitis from 1RM testing, 4 people had mild musculoskeletal soreness, no cardiac complications, deaths or hospitalisations occurred | No |
|
|
| |
| Yes | No |
|
|
|
|
| |
| No | NR |
|
|
|
|
| |
| No |
|
| NR |
|
|
| |
| Sartario 2001 | No |
|
| NR |
|
|
|
| No |
|
| No | decreased in OASI, no difference between groups on AIMS |
|
| |
| Yes | No |
| No |
|
|
| |
| No | NR |
|
|
|
|
| |
| Yes | yes | 1 illness (noncardiac) and 1 died at home in the exercise group |
|
|
| 1 in exercise group | |
| Yes | No | No injuries, medical complications, or study‐related AE | 3 dropouts because of medical reasons not related to the study |
|
|
| |
| Yes | NR | 2 dropouts for non‐study related illnesses |
|
|
|
| |
| No | NR |
|
|
|
|
| |
| No |
|
| No |
|
|
| |
| No | No |
| 1 acquired a health problem that prohibited from driving |
|
|
| |
| Yes (a priori outcome) | No |
| No | weeks of pain reported‐: mean 5.4 (SD=0.7) in PRT, mean 5.6 (SD 0.7) in control | health prof visits mean 2.1 (SD 0.4) for PRT; mean 2.0 (SD 0.5) for control; hospital stays mean 0.24 (SD 0.2) for PRT, mean 0.53 (SD 0.4) for control |
| |
| Yes | Yes | visits to a health professional, minor illness, pain, injuries requiring training adjustment, hospital days, falls | 2 drop out in low intensity group due to pain. I in the control due to hospitalisation | Muscular pain (number of weeks reported per person): High intensity group‐4.1 (2.7); low intensity group‐2.9 (2.6); control group‐3.6 (2.5) | Visits to a health professional over the study (numbers per person): high intensity group ‐ 2 (2); low intensity group ‐ 2 (1.8); controls ‐ 5 (1.8) |
| |
| No |
|
| 3 drop‐outs due to illness "not related to exercise" |
|
|
| |
| Yes | No |
| 4 exercise and control participants dropped out because of ill‐health "not related to exercise" |
|
|
| |
| Yes | yes | patient fainted due to an arythmia during exercise | NR |
|
|
| |
| No | NR |
|
|
|
|
| |
| yes | No |
| 2 became ill (1 in PRT) for reasons unrelated to the study |
|
|
| |
| Yes | Yes | 7 withdrew, developed an exacerbation of an underlying medical problem | 7 withdrew, developed an exacerbation of an underlying medical problem |
|
|
| |
| Yes | Yes | 5 knee discomfort; 1 bruising | 5 knee discomfort; 1 bruising |
|
|
| |
| No |
|
| 5 drop‐outs from exercise groups for medical problems "not related to the exercise program" |
|
|
| |
| No |
|
| NR |
|
|
| |
| No |
|
| 1 exercise drop‐out due to worsening emphysema, 1 due to a stroke |
|
|
| |
| No |
|
| NR |
|
|
| |
| No | NR |
|
|
|
|
| |
| No | NR |
|
|
|
|
| |
| No | NR |
|
|
|
|
| |
| No |
|
| NR |
|
|
| |
| Yes | Maybe | increased oedema in exercise patient | No |
|
|
| |
| Yes | Yes | 6 participants stopped exercise for 6 weeks due to hip/knee pain | few (the number is not specified) dropped out for surgery/injury not related to the study protocol. |
|
|
| |
| Yes (asked about complaints during exercise) | Yes | increased knee pain in person with OA, 1 person had pain from elastic band | 2 drop outs because of medica problems (1 had increased epileptic attacks, 1 was often ill) |
|
|
| |
| No | NR |
|
|
|
|
| |
| No | NR | stated none of the dropouts left the program as a result of adverse responses to treatment ‐ not information about adverse events overall | No |
|
|
|
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Main function measure (higher score = better function) Show forest plot | 33 | 2172 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.14 [0.05, 0.22] |
| 2 Physical function domain of SF‐36/SF‐12 (Higher score = better function) Show forest plot | 14 | 778 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.08, 0.21] |
| 3 Activities of daily living measure (higher score = better function) Show forest plot | 3 | 330 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.04 [‐0.18, 0.26] |
| 4 Activity level measure (kJ/week) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5 Main lower limb (LL) strength measure Show forest plot | 73 | 3059 | Std. Mean Difference (IV, Random, 95% CI) | 0.84 [0.67, 1.00] |
| 6 Main measure of aerobic function Show forest plot | 29 | 1138 | Std. Mean Difference (IV, Random, 95% CI) | 0.31 [0.09, 0.53] |
| 7 VO2 or peak oxygen uptake Show forest plot | 19 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 VO2max‐ml/kg.min | 18 | 710 | Mean Difference (IV, Random, 95% CI) | 1.50 [0.49, 2.51] |
| 7.2 Peak oxygen uptake‐L/min | 2 | 47 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.04, 0.24] |
| 8 Six‐minute walk test (meters) Show forest plot | 11 | 325 | Mean Difference (IV, Random, 95% CI) | 52.37 [17.38, 87.37] |
| 9 Balance measures (higher = better balance) Show forest plot | 17 | 996 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.12 [‐0.00, 0.25] |
| 10 Balance measures (Low = better balance) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 PRT (high intensity) versus control | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 PRT (low intensity) versus control | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Gait speed (m/s) Show forest plot | 24 | 1179 | Mean Difference (IV, Random, 95% CI) | 0.08 [0.04, 0.12] |
| 12 Timed walk (seconds) Show forest plot | 8 | 204 | Mean Difference (IV, Fixed, 95% CI) | ‐0.23 [‐1.07, 0.62] |
| 13 Timed "Up‐and‐Go" (seconds) Show forest plot | 12 | 691 | Mean Difference (IV, Fixed, 95% CI) | ‐0.69 [‐1.11, ‐0.27] |
| 14 Time to stand from a chair Show forest plot | 11 | 384 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.94 [‐1.49, ‐0.38] |
| 15 Stair climbing (seconds) Show forest plot | 8 | 268 | Mean Difference (IV, Random, 95% CI) | ‐1.44 [‐2.51, ‐0.37] |
| 16 Chair stand within time limit (number of times) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 17 Vitality (SF‐36/Vitality plus scale, higher = more vitality) Show forest plot | 10 | 611 | Mean Difference (IV, Fixed, 95% CI) | 1.33 [‐0.89, 3.55] |
| 18 Pain (higher = less pain, Bodily pain on SF‐36) Show forest plot | 10 | 587 | Mean Difference (IV, Fixed, 95% CI) | 0.34 [‐3.44, 4.12] |
| 19 Pain (lower score = less pain) Show forest plot | 6 | 503 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.30 [‐0.48, ‐0.13] |
| 20 Death Show forest plot | 13 | 1125 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.52, 1.54] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Main function measure (higher score = better function) Show forest plot | 2 | 62 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.17 [‐0.67, 0.33] |
| 2 Main lower limb (LL) strength measure Show forest plot | 9 | 219 | Std. Mean Difference (IV, Random, 95% CI) | 0.48 [0.03, 0.93] |
| 3 VO2 Max (ml/kg/min) Show forest plot | 3 | 101 | Mean Difference (IV, Random, 95% CI) | 1.82 [‐0.79, 4.43] |
| 4 Pain (higher score = less pain) Show forest plot | 2 | 62 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.55, 0.45] |
| 5 Vitality (SF‐36, higher score = more vitality) Show forest plot | 2 | 62 | Mean Difference (IV, Fixed, 95% CI) | 6.54 [0.69, 12.39] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Main lower limb (LL) strength measure Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 VO2 Max (ml/kg/min) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Main LL strength measure Show forest plot | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Three times versus once per week | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Twice versus once per week | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Main lower limb (LL) strength measure Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Six‐minute walk test (meters) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Timed walk (seconds) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Time to stand from a chair (seconds) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Stair climbing (seconds) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Main function measure (higher score = better function) Show forest plot | 4 | 125 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.21 [‐0.56, 0.15] |
| 2 Main function measure (lower score = better function) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Main lower limb strength measure Show forest plot | 10 | 487 | Std. Mean Difference (IV, Random, 95% CI) | 0.44 [0.08, 0.80] |
| 4 VO2 max (ml/kg.min) Show forest plot | 8 | 423 | Mean Difference (IV, Random, 95% CI) | ‐1.13 [‐2.63, 0.38] |
| 5 Six minute walk test (meters) Show forest plot | 2 | 63 | Mean Difference (IV, Fixed, 95% CI) | ‐4.28 [‐48.24, 39.67] |
| 6 Gait speed (m/s) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7 Pain (lower score = less pain) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Main function measure (higher score = better function) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Main lower limb strength measure Show forest plot | 3 | 158 | Mean Difference (IV, Fixed, 95% CI) | ‐6.51 [‐21.05, 8.04] |
| 3 Timed "Up‐and‐Go" (seconds) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Vitality (SF‐36/Vitality plus scale, higher = more vitality) Show forest plot | 2 | 147 | Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐2.68, 2.54] |
| 5 Pain (higher = less pain, Bodily pain on SF‐36) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 SF36 (higher score = better function) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Main lower limb (LL) strength measure Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Timed walk (seconds) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Time to stand from a chair (seconds) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Vitality (SF‐36/Vitality plus scale, higher = more vitality) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 Pain (higher = less pain, Bodily pain on SF‐ 36) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Main lower limb strength measure Show forest plot | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 High intensity (power treatment) versus control (control) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 High intensity (treatment) versus low intensity (control) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Strength (grouped by allocation concealment) Show forest plot | 73 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Allocation concealed | 6 | 607 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.12 [‐0.04, 0.28] |
| 1.2 Concealment unknown | 67 | 2452 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.65 [0.56, 0.73] |
| 2 Strength (grouped by assessor blinding) Show forest plot | 73 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Blinded assessors | 19 | 1523 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.23 [0.13, 0.34] |
| 2.2 Assessors were not blinded | 54 | 1536 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.88 [0.77, 0.99] |
| 3 Strength (grouped by intention‐to‐treat) Show forest plot | 73 | 3059 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.53 [0.46, 0.61] |
| 3.1 Intention‐to‐treat was used | 12 | 1041 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.18 [0.06, 0.30] |
| 3.2 Intention‐to‐treat was not used | 61 | 2018 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.74 [0.64, 0.83] |
| 4 Strength (grouped by attention control) Show forest plot | 73 | 3059 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.53 [0.46, 0.61] |
| 4.1 Attention control | 24 | 1408 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.34 [0.23, 0.44] |
| 4.2 No attention control | 49 | 1651 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.72 [0.61, 0.82] |
| 5 Strength (grouped by exercise intensity) Show forest plot | 72 | 3052 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.53 [0.45, 0.60] |
| 5.1 High intensity | 54 | 2026 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.60 [0.51, 0.70] |
| 5.2 Low‐to‐moderate intensity | 19 | 1026 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.39 [0.26, 0.51] |
| 6 Strength (grouped by exercise duration) Show forest plot | 56 | 2564 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.53 [0.45, 0.61] |
| 6.1 Less than 12 weeks | 20 | 828 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.52 [0.37, 0.66] |
| 6.2 Longer than 12 weeks | 36 | 1736 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.53 [0.43, 0.63] |
| 7 Strength (grouped by health status) Show forest plot | 65 | 2428 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.60 [0.52, 0.69] |
| 7.1 Healthy participants | 46 | 1502 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.77 [0.66, 0.88] |
| 7.2 Older adults with a specific health problem | 19 | 926 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.37 [0.24, 0.51] |
| 8 Strength (grouped by functional limitations) Show forest plot | 54 | 2133 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.60 [0.51, 0.70] |
| 8.1 No functional limitations | 41 | 1349 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.81 [0.69, 0.93] |
| 8.2 With functional limitations | 13 | 784 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.30 [0.16, 0.44] |

