Biorretroalimentación o ejercicios del esfínter para el tratamiento de la incontinencia fecal en adultos
Resumen
Antecedentes
La incontinencia fecal es una afección particularmente embarazosa y angustiante que tiene implicaciones médicas, sociales y económicas significativas. Los ejercicios del esfínter anal (entrenamiento muscular del suelo pelviano) y la terapia con biorretroalimentación se han utilizado para el tratamiento de los síntomas en pacientes con incontinencia fecal. Sin embargo, aún no existen estándares de tratamiento y todavía no se ha establecido la magnitud de sus supuestos efectos beneficiosos.
Objetivos
Determinar los efectos de la biorretroalimentación o los ejercicios del esfínter anal / entrenamiento de los músculos del suelo pelviano para el tratamiento de la incontinencia fecal en adultos.
Métodos de búsqueda
Se realizaron búsquedas en el Registro especializado de ensayos del Grupo Cochrane de Incontinencia (Cochrane Incontinence Group) (24 de enero de 2012) que contiene ensayos obtenidos a partir de búsquedas en CENTRAL, MEDLINE y búsquedas manuales de actas de congresos; y en las listas de referencias de artículos relevantes.
Criterios de selección
Todos los ensayos con asignación aleatoria o cuasialeatoria que evaluaran biorretroalimentación o ejercicios del esfínter anal en adultos con incontinencia fecal.
Obtención y análisis de los datos
Dos revisores evaluaron el riesgo de sesgo de los ensayos elegibles y dos revisores extrajeron de forma independiente los datos de los ensayos incluidos. Se consideró un amplio rango de medidas de resultado.
Resultados principales
Se identificaron 21 estudios elegibles con 1525 participantes. Cerca de la mitad de los ensayos tenían bajo riesgo de sesgo para la asignación al azar y la ocultación de la asignación.
Un ensayo pequeño mostró que biorretroalimentación más ejercicios fue mejor que los ejercicios solos (CR de no lograr la continencia total 0,70; IC del 95%: 0,52 a 0,94).
Un ensayo pequeño mostró que el agregado de biorretroalimentación a la estimulación eléctrica fue mejor que la estimulación eléctrica sola (CR de no lograr la continencia total 0,47; IC del 95%: 0,33 a 0,65).
Los datos combinados de dos ensayos mostraron que el número de pacientes que no lograron la continencia total fue significativamente menor cuando la estimulación eléctrica se agregó a la biorretroalimentación en comparación con la biorretroalimentación sola (CR 0,60; IC del 95%: 0,46 a 0,78).
La estimulación nerviosa del sacro fue mejor que el tratamiento conservador que incluyó biorretroalimentación y EMPP (a los 12 meses los episodios de incontinencia fueron significativamente menores con la estimulación nerviosa del sacro [DM 6,30; IC del 95%: 2,26 a 10,34]).
No hubo pruebas suficientes sobre si hubo una diferencia en el resultado entre cualquier método de biorretroalimentación o ejercicios. Hay indicaciones de que el entrenamiento de discriminación del volumen rectal mejora la continencia más que el entrenamiento simulado. A partir de los datos disponibles no se pueden establecer conclusiones adicionales.
Conclusiones de los autores
El número limitado de ensayos identificados, con defectos metodológicos en muchos casos, no permite una evaluación definitiva de la función de los ejercicios del esfínter anal ni de la terapia con biorretroalimentación en el tratamiento de los pacientes con incontinencia fecal. Se encontraron algunas pruebas de que la biorretroalimentación y la estimulación eléctrica pueden mejorar el resultado del tratamiento en comparación con la estimulación eléctrica sola o los ejercicios solos. Los ejercicios parecen ser menos eficaces que un estimulador nervioso implantado en el sacro. Existen indicaciones de que algunos elementos de la terapia con biorretroalimentación y los ejercicios del esfínter pueden tener un efecto terapéutico, pero no se ha podido confirmar. Se necesitan ensayos bien diseñados más grandes para poder establecer conclusiones seguras.
Resumen en términos sencillos
Ejercicios de los músculos alrededor del ano con o sin biorretroalimentación (ayuda para saber cuándo se contraen los músculos) para el tratamiento de la incontinencia fecal en adultos
La incontinencia fecal (incapacidad de controlar los movimientos intestinales o las pérdidas de heces) puede ser un problema muy embarazoso y socialmente limitante. Hay muchas causas posibles que incluyen el daño a los músculos que controlan los movimientos intestinales después del parto. Con frecuencia se recomiendan ejercicios para fortalecer estos músculos y "biorretroalimentación", donde se utiliza un equipo para mostrarles a los pacientes cómo utilizar los músculos adecuadamente. Hubo algunas pruebas de ensayos que indican que estos tratamientos son útiles. Si se seleccionan los pacientes que han probado y fracasado otros tratamientos más sencillos como el cambio en la dieta o el uso de fármacos, la biorretroalimentación con el uso de un equipo computarizado o balón rectal es más beneficiosa que el ejercicio solo. Los ejercicios y la estimulación eléctrica del ano pueden ser más útiles que los ejercicios vaginales para las mujeres con incontinencia fecal después del parto. Alrededor de la mitad de los 21 ensayos tuvieron un riesgo de sesgo bajo. Los ensayos compararon diferentes combinaciones de tratamientos y diferentes medidas de resultado, lo que dificulta la comparación entre ellos. Sin embargo, un escaso número de ensayos recientes más grandes proporcionan mejores pruebas.
Authors' conclusions
Background
Description of the condition
Faecal incontinence has been variously defined. An international consensus meeting has recommended: "Faecal incontinence is the involuntary loss of liquid or solid stool that is a social or hygienic problem" (Norton 2009).
Faecal incontinence is a common healthcare problem, affecting 5% to 10% of community‐dwelling adults (Macmillan 2004; Perry 2002; Whitehead 2009), with 1% to 2% experiencing significant impact on daily activities (Perry 2002). It becomes more common with advancing age and disability (Potter 2002). It is a symptom which is particularly embarrassing and socially unacceptable, and many sufferers do not seek professional help (Johanson 1996). Faecal incontinence has a major negative impact on physical and psychological health and lifestyle (Boreham 2005; Cotterill 2011; Wilson 2007), with severe social restrictions in many instances (Rockwood 1999; Rockwood 2000).
Faecal incontinence has many possible causes, including (among others) obstetric or other trauma, or a congenital abnormality of one or both of the anal sphincters or the pelvic floor muscles; loose stool or intestinal hurry; neurological disease or injury causing sensory or motor impairment to the continence mechanism; local anorectal pathology; rectal loading and subsequent 'overflow' leakage in frail or immobile individuals; and physical or mental disabilities affecting toilet habits. For many people, a combination of structural, physiological and psycho‐social factors (Norton 2004; Rao 2004; Tuteja 2004) combine to cause faecal incontinence.
It is generally recognised that symptoms may be of urgency with urge faecal incontinence, usually consequent upon external striated voluntary sphincter weakness or disruption, or loose stool or intestinal hurry; or of passive soiling in the absence of an urge to defecate, secondary to smooth muscle internal anal sphincter dysfunction, local pathology or incomplete evacuation. Recent advances in investigation techniques (notably ano‐rectal physiology studies and endo‐anal ultrasound) allow more accurate characterisation of the underlying cause for each patient. However, for many conditions the treatment options are limited, relying mainly on surgery and constipating drugs (Madoff 2009; Norton 2009; Whitehead 2001).
Description of the intervention and how it might work
Pelvic floor muscle training (PFMT) is a well‐established therapy for the treatment of urinary incontinence (Dumoulin 2010), but has been less commonly reported for faecal incontinence. The external anal sphincter is continuous with the puborectalis muscle and, as a striated muscle, is theoretically amenable to the same re‐educative and training techniques. The role of the ano‐rectal angle, maintained by the pubo‐rectalis muscle, is controversial but is believed to be important in faecal continence. It is not established whether pelvic floor muscle training can be distinguished from anal sphincter exercises in practice by patients, and the two will be considered together for the purposes of this review, with the use of vaginal or anal palpation, teaching, or biofeedback made explicit. The purpose of the exercises is stated variously as enhancing the strength, speed, or endurance of voluntary anal sphincter contraction. Some have also suggested that there could be an effect on resting closure pressure of the anus. Reported exercise regimens for faecal incontinence vary widely in terms of the type, number and intensity of exercises taught (for example maximal squeeze and how long to attempt to hold it; submaximal endurance squeeze; fast twitch squeezes), how many per day and in what pattern, and in length of time the exercises are suggested to be performed for. Some have reported a single regimen for all patients (for example 10 squeezes of 5 seconds each five times per day); others have individualised the exercise programme, depending on the initial muscle strength and endurance, on the principle of improving muscle performance by 'overload' (aiming to exercise at a level just above current ability). There is no consensus among professionals on the best exercise regimen for faecal incontinence.
Biofeedback uses equipment to record or amplify and then feed back to the patient activities of the body. Originally based on the principles of operant conditioning (Engel 1974), it is a very commonly reported clinical treatment for faecal incontinence in the colorectal and gastroenterology literature. Reviews of large numbers of case series, in the era before randomised controlled trials became the accepted method for evaluating the efficacy of treatment, have concluded that biofeedback is an effective treatment for the majority of people with faecal incontinence (Heymen 2001: Norton 2001). Many different therapies have been used with people with faecal incontinence under the label of 'biofeedback'. Early studies concentrated on operant conditioning to enhance what was presumed to be a reflex contraction of the external anal sphincter in response to the reflex inhibition of the internal anal sphincter when the rectum filled (recto‐anal inhibitory reflex). It has subsequently been suggested that this external sphincter reaction is in fact not a reflex but a voluntary response (Whitehead 1981). Other studies have focused on teaching the patient to discriminate progressively smaller volumes of distension of a rectal balloon, and to respond appropriately (by contracting the external sphincter) and as promptly as possible, abolishing any delay in sensation or reaction to it. Some have disregarded these elements and focused entirely on improving the strength or endurance of external anal sphincter contraction.
Three main modalities have been described
1. Rectal sensitivity training. A rectal balloon is gradually distended with air or water and the patient is asked to report the first sensation of rectal filling. Once this threshold volume is determined, repeated re‐inflations of the balloon are performed with the objective being to teach the patient to feel the distension at progressively lower volumes. The rationale is that some patients are found to have high threshold volumes and if the patient detects stool arriving sooner there is more possibility to either find a toilet or use an anal squeeze, or both. Conversely, the same technique can also be used to teach the patient to tolerate progressively larger volumes, in those with urgency and a hypersensitive rectum.
2. Strength training. Biofeedback techniques have been used to demonstrate to the patient anal sphincter pressures or activity, thereby enabling teaching of anal sphincter exercises and giving feedback on performance and progress. This can be achieved by using electromyography (EMG) skin electrodes, manometric pressures, intra‐anal EMG, or anal ultrasound. The patient is encouraged by seeing or hearing the signal to enhance squeeze strength and endurance. There is no consensus on an optimum exercise regimen for use at home between sessions, nor on the number of squeezes, the frequency of exercises or treatment duration, with different authors describing very different programmes.
3. Co‐ordination training. Some authors have described a three‐balloon system for biofeedback for faecal incontinence. One distension balloon is situated in the rectum, the second and third smaller pressure‐recording balloons are situated in the upper and lower anal canal. Rectal distension triggers the rectal‐anal inhibitory reflex. This momentary anal relaxation is a point of vulnerability for people with faecal incontinence and incontinence can occur at this time. By distending the rectal balloon and showing the patient this consequent pressure drop, the aim is to teach the patient to counteract this by a voluntary anal squeeze that is hard enough and for long enough for resting pressure to return to its baseline level.
The three methods are not mutually exclusive, and many protocols combine two or three elements together. There has been considerable variation in protocols, such as the number or frequency of sessions, intensity and duration of exercises and instructions for practice at home. Some studies have included other elements, such as patient teaching, diet and fluid advice and titration of medication, although many fail to mention these other elements or give details. Some have used additional surface electrode electrical stimulation of the anal sphincter muscles, which is the subject of a separate Cochrane review (Hosker 2007). There is widespread agreement on the crucial role of patient motivation and the patient‐therapist interaction.
Why it is important to do this review
There are numerous case series reporting on biofeedback for faecal incontinence, nearly all of which have reported positive results (Heymen 2001; Norton 2001). Only one published study has reported negative results (van Tets 1996). It would be easy to conclude from case series that biofeedback or exercises are an effective intervention. However, it is known that there is a publication bias in favour of publishing positive results and that there is an effect of intervention per se, especially in many functional gastrointestinal disorders (Thompson 1999). Delivering a programme of biofeedback or anal sphincter exercises, or both, inevitably involves a complex combination of patient‐therapist interaction, patient education and formal or informal advice on a range of related issues. Randomised controlled trials provide the best evidence of the efficacy of health care interventions. More complex interventions are likely to involve more clinic attendances for the patients and more costs. Patients who fail to respond to conservative treatments are often referred for costly surgical treatments such as sacral nerve stimulation. If they have not tried the most effective available conservative interventions, they may undergo surgery unnecessarily or alternatively decide to live with distressing symptoms which might have responded to the best available treatment.
The aim of the present review is to systematically search for and combine evidence from all relevant randomised controlled trials on the effects of biofeedback or sphincter exercises, or both, for the treatment of faecal incontinence in order to provide the best evidence currently available on which to base recommendations for clinical practice and for future research.
Objectives
To determine the effectiveness of anal sphincter exercises/pelvic floor muscle training (PFMT) with or without biofeedback in the treatment of the symptoms of faecal incontinence in adults. The following comparisons were considered:
1. Anal sphincter exercises/PFMT with or without biofeedback versus no treatment
2. Anal sphincter exercises/PFMT with or without biofeedback versus any other treatment alone
3. Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone
4. Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus exercises with or without biofeedback
5. Anal sphincter exercises/PFMT and biofeedback versus anal sphincter exercises/PFMT alone
6. One type of biofeedback versus another type of biofeedback
7. One type of anal sphincter exercises/PFMT versus another type of anal sphincter exercises/ PFMT
Methods
Criteria for considering studies for this review
Types of studies
All randomised or quasi‐randomised controlled trials of patients with faecal incontinence receiving anal sphincter exercises or biofeedback, or both as treatment.
Types of participants
Adults (18 years and older or as defined by the trialists) suffering from faecal incontinence.
Types of interventions
Anal sphincter exercises and/or biofeedback.
Under the term 'anal sphincter exercises' we included: anal sphincter exercises, 'Kegel exercises' (Kegel 1948), pelvic floor exercises, or pelvic floor muscle training.
All types of visual, sensory (usually with a rectal balloon) or auditory biofeedback were considered. As the specific techniques used for biofeedback might have differed among studies, a clear description of the modality used was made explicit in each instance (see table 'Characteristics of included studies').
Types of outcome measures
1. Patient symptoms
Incontinence status
Frequency of incontinence
Number of pads changes
Incontinence score.
Occurrence of adverse events
Diary
2. Patient satisfaction with outcome
Self‐report
3. Ano‐rectal physiology measurements
Resting anal pressure (pressure or EMG)
Pressure rise and squeeze increment on voluntary contraction (pressure or EMG)
Duration of pressure rise on voluntary contraction (pressure or EMG)
Vector Symmetry Index
Rectal sensation assessment (by balloon distention or electrical means, or both)
4. Health status measures
Psychological health measures (e.g. Hospital Anxiety and Depression Scale, HADS) (Zigmond 1983)
Health‐related quality of life measures (e.g. Short Form‐36) (Ware 1993) or condition‐specific measures
Activities of daily living measures (e.g. Barthel activities of daily living (ADL) Index) (Wade 1988)
5. Health economics
Costs of interventions
Resource implications
Cost effectiveness or cost utility evaluation (e.g. cost per QALY) (Weinstein 1977)
6. Other outcomes
Other outcome measures given by authors and judged to be important when undertaking the review
Search methods for identification of studies
We did not impose any language or other limits on any of the searches.
Electronic searches
This review has drawn on the search strategy developed by the Cochrane Incontinence Group. Relevant trials were identified from the Incontinence Group Specialised Trials Register, which is described under the Incontinence Group's module in The Cochrane Library. The register contains trials identified from MEDLINE, CINAHL, the Cochrane Central Register of Controlled Trials (CENTRAL) and handsearching of journals and conference proceedings. The date of the most recent search of the register was 24 January 2012.
The trials in the Incontinence Group Specialised Trials Register are also contained in CENTRAL. The Incontinence Group Trials Register was searched using the Group's own keyword system. The search terms used were:
({design.rct* or design.cct*})
AND
({TOPIC.FAECAL.INCON* or TOPIC.FAECAL.NEUROGENIC*})
AND
({INTVENT.PHYS.PFMT* or INTVENT.PHYS.BIOFEED* or INTVENT.PHYS.SphincterExercise* or INTVENT.PHYS.exercise*})
(All searches were of the keyword field of Reference Manager 12, ISI ResearchSoft).
Searching other resources
We checked all reference lists of identified trials.
Data collection and analysis
Trials selection
Two review authors (CN, JC) examined all the citations and abstracts derived from the electronic search strategy. Reports of potentially relevant trials were retrieved in full. Both review authors independently applied the selection criteria to trials reports. They were not blind to the names of trials' authors, institutions or journals. Any disagreements were resolved by discussion.
Risk of bias
The risk of bias of identified trials was assessed independently by the two review authors using the Cochrane Collaboration 'Risk of bias' tool (Higgins 2011a). This takes into account the quality of random sequence generation, allocation concealment, the description of dropouts and withdrawals, whether data were analysed on an intention‐to‐treat basis, and whether therapists, participants or outcome assessors were blind to the treatments provided.
Where the method of allocation concealment was not clearly reported the authors were contacted, if possible, for clarification.
Any disagreements were resolved by discussion. Studies were excluded if they not meet the pre‐specified inclusion criteria. The list of excluded studies and the reasons for their exclusion are summarised in the table 'Characteristics of excluded studies'.
Data extraction
Data extraction from the included studies was undertaken independently by the review authors. Only published data have been used for the purposes of this review. Data were processed as described in the Cochrane Collaboration Handbook (Higgins 2011b). Any difference of opinion was resolved by discussion.
Missing information was sought from trialists, if necessary.
Analysis
Data were analysed using Review Manager (RevMan) software.
For each trial, risk ratios and 95% confidence intervals were calculated for dichotomous outcomes using a fixed‐effect model. Continuous variables were processed using mean and standard deviation values. Where the results were reported in terms of the mean and standard error of the mean (SEM), the standard deviation (SD) was calculated using the standard statistical equation: SD = SEM x square root (sample size). Differences between groups were presented as weighted mean differences (WMD) with accompanying 95% confidence intervals.
All outcomes were reported in terms of unfavourable events. This implied that risk ratios less than one or a WMD less than zero indicated a reduction in unfavourable events (that is a beneficial treatment effect). Therefore, the benefits of the experimental treatment were all displayed on the same side of the line of no effect.
Results
Description of studies
Results of the search
Three hundred and ten possible studies were identified by the search of which 21 are included in the review. The flow of literature through the assessment process is shown in the PRISMA flowchart (Figure 1).

PRISMA study flow diagram.
Included studies
Twenty one studies are included in this review ( Bartlett 2011; Bols 2011; Davis 2004; Fynes 1999; Healy 2006; Heymen 2000; Heymen 2009; Hinninghofen 2003; Ilnyckyj 2005; Latimer 1984; Mahony 2004; Markwell 2006; McHugh 1986; Miner 1990; Naimy 2007; Norton 2003; Schwandner 2010; Schwandner 2011; Solomon 2003; Tjandra 2008; Whitehead 1985). A total of 1525 participants were randomised.
Further details can be found in the Table of Characteristics of included studies.
Design
One study (Whitehead 1985) allocated alternate patients to exercises or a control group.
Seventeen studies prospectively randomised patients to one of two (Bartlett 2011; Bols 2011; Davis 2004; Fynes 1999; Healy 2006; Heymen 2009; Ilnyckyj 2005; Mahony 2004; Markwell 2006; Naimy 2007; Schwandner 2010; Schwandner 2011; Tjandra 2008), three (Hinninghofen 2003; Solomon 2003) or four groups (Heymen 2000; Norton 2003).
Two trials (Latimer 1984; Miner 1990) which attempted to evaluate different components of biofeedback therapy had a complex design. One trial (Latimer 1984) reported the results of single case experiments employed with eight incontinent patients randomly allocated to different components of biofeedback (A, B, C or D). The single case designs were A B A C A D A or A C A B A D A. For each patient, results of the pre‐treatment phase were compared to those of the last follow‐up. Results at the end of each treatment phase were either not reported or provided in a form unsuitable for statistical analyses, rendering the interpretation of trial findings difficult. The other trial (Miner 1990), which investigated some of the factors thought to be responsible for the improvement of patients undergoing biofeedback therapy, was a 'two‐phase randomised trial'. Patients were initially randomised to one of two groups for sensory retraining (phase II); before and after treatment results were reported for both intervention groups. At the end of phase I all patients were again randomly assigned to one of two groups for either strength or coordination training. After a month they were crossed over. Results of the cross‐over phases were not clearly reported. Only results of the final assessment were given for phase II.
One trial randomised patients to two groups using a cross‐over design (McHugh 1986).
Sample sizes
The sample sizes of included trials ranged from eight (Latimer 1984) to 171 (Norton 2003) participants.
Setting
Each of the trials, except two (Schwandner 2010; Schwandner 2011), were carried out in a single hospital centre; these were in a variety of countries. Schwandner 2010 was a multi centre trial which involved eight centres in Germany (Schwandner 2010).
Participants
In all studies where information on gender was reported, the majority of participants were female. Most studies enrolled patients with mixed aetiologies. Four studies included women with obstetric trauma only (Davis 2004; Fynes 1999; Mahony 2004; Naimy 2007). One study included older patients only (Whitehead 1985). One study included only patients undergoing surgical anal sphincter repair (Davis 2004). Some investigators only included patients who had failed previous dietary and medication interventions (Bols 2011; Heymen 2009). In some studies patients with specific diagnoses such as rectal prolapse were excluded, inflammatory bowel disease, and irritable bowel syndrome (see table 'Characteristics of included studies' for details of the inclusion and exclusion criteria in each study).
Interventions
One study used a dual‐balloon system with visual or auditory feedback of anal pressure. Patients were encouraged to contract the anal sphincter in response to rectal distension. Exercises during the session (one hour per week for six weeks, commenced three months following anal sphincter repair surgery) and home practice included maximal, submaximal and fast‐twitch contractions practised at least twice daily. The control group had no therapist contact, biofeedback or exercises (Davis 2004). Another study compared rectal balloon therapy with PFMT against PFMT alone (Bols 2011).
Two other studies included a no biofeedback or exercises group. In one of these studies the control group received one‐to‐one time and advice (Norton 2003); in the other study the control group received no intervention (Whitehead 1985). Three studies included a no‐biofeedback exercise group which involved exercises taught digitally (Norton 2003; Solomon 2003) or verbally (Ilnyckyj 2005).
Heyman 2009 compared manometric biofeedback and pelvic floor exercises against exercises alone.
Bartlett compared a standard clinical protocol (sustained submaximal anal and pelvic floor exercises versus an alternative group (rapid squeeze plus sustained submaximal exercises) with biofeedback in both arms of the study. There were five outpatient sessions over eight weeks. The first four sessions were weekly; participants then practised techniques for four weeks before returning for their final session (Bartlett 2011).
Markwell (Markwell 2006) compared dietary modification, stool bulking agents, specific pelvic floor muscle action using abdominal muscles and defecation training compared with dietary modification, stool bulking agents and conventional pelvic floor exercises.
Tjandra (Tjandra 2008) compared optimum medical therapy, including pelvic floor exercises, bulking agents, dietary management of fluid and fibres, with a team of physiotherapists and dietitians. Attendance varied with need, usually monthly for six months then two‐monthly. This group was compared against two phase sacral nerve stimulation: peripheral nerve evaluation for at least seven days; patients with a 50% reduction or more in incontinence episodes were surgically implanted with a permanent sacral nerve stimulator.
Two studies compared biofeedback and exercises against biofeedback, exercises and electrical stimulation (Fynes 1999; Mahony 2004). The Fynes study (Fynes 1999) randomised women with post‐natal faecal incontinence to either vaginal pressure non‐computer biofeedback (Peritron) with a nurse (weekly 30 minute sessions for 12 weeks) with fast and slow twitch exercises, or to computer‐assisted anal probe EMG biofeedback (fast and slow twitch exercises) with a physiotherapist plus anal electrical stimulation at 20 Hz and 50 Hz. The Mahoney study (Mahony 2004) likewise recruited women with post‐natal incontinence, randomised to have anal EMG biofeedback to perform fast and slow twitch contractions (10 minutes), with or without additional anal electrical stimulation at 35 Hz (20 minutes) at weekly sessions for 12 weeks. The Mahony study randomised women to intra‐anal EMG biofeedback with or without anal electrical stimulation.
Schwandner 2010 (Schwandner 2010) compared "Triple target training" where amplitude‐modulated middle‐frequency electrical stimulation was combined with electromyography biofeedback and compared against electromyography biofeedback carried out at home daily for 20 minutes for a duration of nine months.
Schwandner 2011 (Schwandner 2011) compared "Triple target training" where amplitude‐modulated middle‐frequency electrical stimulation was combined with electromyography biofeedback and compared against low frequency electrostimulation.
Healy (Healy 2006) compared endo‐anal pudendal nerve stimulation daily at home against attending a physiotherapy department for endo‐anal electrical stimulation under supervision. They alternated biofeedback and electrical stimulation using augmented biofeedback.
Hinninghofen (Hinninghofen 2003) included three different groups, sphincter training compared with electrical stimulation, sphincter training with biofeedback and pelvic floor training without support; the intervention lasted three months.
Naimy (Naimy 2007) compared biofeedback with electrical stimulation. Biofeedback consisted of Neuro Trac ETS: using an Anuform anal probe. Quick 3 second squeeze; 10 second squeeze; squeeze for as long as it kept 50% of 3 second amplitude. Each squeeze was repeated five times with equal rest time between. The initial session was for 30 minutes with a 30 minute follow‐up session one week later; then daily 30 minute sessions at home for eight weeks. Electrical stimulation consisted of Neuro Trac ETS: 30 or 40 Hz at alternate sessions; pulse width 200 µsec; upper limit 80 mAmp using Anuform anal probe. Patients turned up the stimulation to the maximum voltage which caused no discomfort: 3 seconds on then 3 seconds rest for 20 minutes twice daily at home. The initial session was 30 minutes with a 30 minute follow‐up session one week later. Both interventions were carried out two times daily for eight weeks.
Four studies compared different methods of delivering biofeedback (Heymen 2000; McHugh 1986; Norton 2003; Solomon 2003). Heymen randomised patients to one of four groups:
1. anal EMG biofeedback plus home exercise;
2. anal EMG biofeedback plus rectal balloon distension sensory training to perceive lower rectal volumes and hold larger rectal volumes;
3. anal EMG biofeedback plus home exercise using a home biofeedback machine;
4. anal EMG biofeedback plus rectal balloon distension sensory training plus home exercise using a home biofeedback machine.
Norton (Norton 2003) randomised patients to one of four groups (all monthly 45 to 60 minute sessions for up to six sessions):
1. education, advice, urge resistance training, medication titration, diet and fluid adjustment (no biofeedback or exercise);
2. as 1, plus anal sphincter exercises taught by digital examination and a leaflet, with instruction to practise maximal, submaximal and fast‐twitch exercises 10 times daily at home;
3. as 2. plus computer‐assisted anal sphincter pressure biofeedback at each session;
4. as 3. plus a home anal EMG biofeedback machine for home practice.
Solomon (Solomon 2003) randomised patients to exercises taught digitally, via anal ultrasound biofeedback or via anal manometry biofeedback (five 30 minute sessions over four months).
One study compared clinic biofeedback with a home biofeedback device (McHugh 1986).
The design of the remaining two trials (Latimer 1984; Miner 1990), which attempted to evaluate different components of biofeedback therapy, have been described above.
Outcomes
Trials included a variety of outcome measures, many of which have not been validated.
Five trials reported patient evaluation of the outcome as a primary outcome measure (Bols 2011; Davis 2004; Naimy 2007; Norton 2003; Solomon 2003).
Eight studies used a patient‐completed diary. One study took no episodes of faecal incontinence in a one week diary at the end of treatment as a 'complete response' (Ilnyckyj 2005).
Nine studies reported results of a variety of continence scores.
Eleven trials reported quality of life evaluation (Bartlett 2011; Bols 2011; Davis 2004; Healy 2006; Heymen 2009; Hinninghofen 2003; Mahony 2004; Naimy 2007; Norton 2003; Schwandner 2010; Tjandra 2008). One study used the SF‐36 tool (Norton 2003).
Eight trials reported changes in manometric data as a proxy for patient outcome.
No attempts were made to include economic data in any trial.
See the Characteristics of included studies table for details of outcome measures used in each study.
Excluded studies
Of the excluded studies, some included children only, others were not randomised controlled trials (RCTs) or did not include the target interventions. Two were abstract reports of subsequently published full papers. See the table 'Characteristics of excluded studies' for details.
Risk of bias in included studies
Allocation
Thirteen trials (Bartlett 2011; Bols 2011; Davis 2004; Fynes 1999; Heymen 2000; Heymen 2009; Mahony 2004; Markwell 2006; Naimy 2007; Norton 2003; Schwandner 2010; Schwandner 2011; Solomon 2003) were judged to be at low risk of bias for random sequence generation, where an independent method such as a computer‐generated list was used to produce the allocation of groups.
The quality of allocation concealment was judged to be adequate in 10 trials (Bartlett 2011; Bols 2011; Heymen 2009; Mahony 2004; Markwell 2006; Norton 2003; Schwandner 2010; Schwandner 2011; Solomon 2003; Tjandra 2008), unclear in 10 trials (Davis 2004; Fynes 1999; Healy 2006; Heymen 2000; Hinninghofen 2003; Ilnyckyj 2005; Latimer 1984; McHugh 1986; Miner 1990; Naimy 2007) and inadequate in one trial (Whitehead 1985). Most of the 'unclear' allocations mentioned computer‐generated random numbers but did not explicitly state that allocation was concealed.
Blinding
In the Bartlett trial (Bartlett 2011) participants were blinded. Markwell (Markwell 2006) was described as 'single blind study' but information on who was actually blinded was not clearly reported.
In four trials (Bols 2011; Fynes 1999; Schwandner 2011; Solomon 2003) the outcome assessor was blind to patients' treatment protocol; in two trials outcome assessors were blinded for some of the outcomes (Norton 2003; Schwandner 2010).
In Heyman 2009 (Heymen 2009) the therapist telephoned to ask if participants had experienced 'adequate relief', which could be considered a violation of the trial protocol.
Incomplete outcome data
Most studies reported overall withdrawals with no indication of which groups patients were originally enrolled. Five trials (Bols 2011; Heymen 2009; Latimer 1984; Norton 2003; Schwandner 2010) that analysed data on an intention‐to‐treat basis and (Fynes 1999) had no or comparable drop outs from each group, were considered to be at low risk of bias.
In two trials (Latimer 1984; Miner 1990) data of the cross‐over phases were not reported separately and it was not possible to analyse them as parallel group data.
Effects of interventions
Twenty one trials with a total of 1525 participants were included in this review.
Only nine trials (Davis 2004; Fynes 1999; Healy 2006; Heymen 2009; Miner 1990; Naimy 2007; Schwandner 2010; Schwandner 2011; Tjandra 2008) provided data in a form suitable for statistical analyses in RevMan.
Follow‐up
Most studies reported results at the end of treatment or within a few weeks of completion only. Two studies reported results nine months after starting biofeedback (Davis 2004; Schwandner 2010) and five studies reported results one year after completing treatment (Bartlett 2011; Markwell 2006; Miner 1990; Norton 2003; Tjandra 2008).
1. Anal sphincter exercises/PFMT with or without biofeedback versus no treatment
One small cross‐over trial with 25 participants was found (Miner 1990). Data suitable to be analysed were presented for the first phase of the trial only. In the experimental group active sensory retraining was employed to teach the patient to discriminate progressively smaller volumes of rectal balloon distension with decreasing delay. Controls received the same procedure but with no feedback on performance. Miner reported that sensory biofeedback produced better results than strength training alone. There was a significant difference between groups in incontinence episodes per week (MD ‐1.40, 95% CI ‐1.51 to ‐1.29) (Analysis 1.3) and rectal sensory threshold (WMD ‐12.90, 95% CI ‐14.10 to ‐11.70) (Analysis 1.8) favouring treatment. However, there was no statistically significant result for people failing to achieve full continence (RR 0.71, 95% CI 0.48 to 1.03) (Analysis 1.1) or no improvement in incontinence status (RR 0.26, 95% CI 0.07 to 1.03) (Analysis 1.2). Controls were said to achieve similar benefits when crossed over to active training but these data were not given.
2. Anal sphincter exercises/PFMT with or without biofeedback versus any other treatment alone
Biofeedback versus electrical stimulation
One trial (Naimy 2007) compared biofeedback with electrical stimulation alone, with no mention of exercises between treatments in either group. There was no statistically significant difference for numbers of people dissatisfied with treatment although the confidence interval was wide (Analysis 2.7).
3. Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone
Seven trials were found (Davis 2004; Healy 2006; Ilnyckyj 2005; Norton 2003; Schwandner 2011; Tjandra 2008; Whitehead 1985).
Exercises plus medical therapy versus sacral nerve stimulation
Tjandra compared optimal medical therapy, which consisted of pelvic floor exercises (biofeedback provided with digital guidance), bulking agents, dietary management of fluid and fibres versus two phase sacral nerve stimulation (peripheral nerve evaluation for at least 7 days; patients with a 50% reduction or more in incontinence episodes were implanted with a permanent sacral nerve stimulator). At 12 months the number of incontinence episodes per week was significantly lower in the sacral nerve stimulation group (MD 6.30, 95% CI 2.26 to 10.34) (Analysis 3.4). However the difference in the number of pad changes per week was not statistically significant (Analysis 3.5). Both the Incontinence score and condition‐specific quality of life (fecal incontinence quality of life index, FIQL) showed a statistically significant result favouring sacral nerve stimulation (MD 12.90, 95% CI 12.22 to 13.58, Analysis 3.6; MD 1.00, 95% CI 0.70 to 1.30, Analysis 3.16, respectively).
Exercises plus biofeedback plus surgery versus surgery alone
Davis (Davis 2004) compared anal sphincter repair with or without subsequent biofeedback commenced three months post‐operatively in 38 women with obstetric‐related anal sphincter injuries. There was no difference between the groups as regards continence score at nine months (Analysis 3.6) or patient satisfaction measured by visual analogue score (Analysis 3.19). Davis (Davis 2004) used a validated faecal incontinence quality of life questionnaire at nine months and there were no statistically significant differences between the groups in mean score changes for lifestyle, depression and embarrassment measurements.
Exercises plus biofeedback plus electrical stimulation versus electrical stimulation alone
Schwandner (Schwandner 2011) compared medium frequency electrical stimulation and electromyographic (EMG) biofeedback (known as triple target treatment) versus low frequency electrostimulation. electrostimulation. The number of people who failed to achieve full continence was significantly lower in the triple target group (RR 0.47, 95% CI 0.33 to 0.65, Analysis 3.1). The Wexner incontinence score was statistically significant favouring triple target training (MD ‐8.80, 95% CI ‐10.70 to ‐6.90) (Analysis 3.6).
Healy (Healy 2006) compared endo‐anal pudendal nerve electrical stimulation daily at home versus endo‐anal electrical stimulation plus augmented biofeedback under supervision and reported that low frequency endo‐anal electrical stimulation significantly improves continence scores and quality of life. The data could not be analysed in RevMan.
Exercises plus biofeedback plus education versus exercises plus education
Ilnyckyj (Ilnyckyj 2005) compared anal sphincter exercises plus biofeedback plus education versus exercises and education in 23 women, the data were not suitable for further analyses in RevMan as no measures of variance were reported. Ilnyckyj reported that resting and squeeze manometric pressures were not significantly different between the groups, but there was a trend in favour of biofeedback. Squeeze duration was better in the biofeedback group (P = 0.019). On the outcome measure of no incontinence in a one week diary, 86% (six out of seven) of biofeedback patients and 45% (five of 11) of education without biofeedback participants were "complete responders" (Analysis 3.20).
Norton (Norton 2003) compared education and advice, with or without exercises, with or without biofeedback (clinic and home or clinic alone) in 171 patients. No significant differences between the groups were reported on manometric parameters, continence scores, quality of life, anxiety and depression, diary data and self‐rating.This study consisted of four groups and consequently fits with comparison 3 and 6 below. No data were given in a format suitable for statistical analysis in RevMan.
Group 1: education (advice and information on bowel re‐training).
Group 2: education and sphincter exercises.
Group 3: education, sphincter exercises and clinic biofeedback.
Group 4: education, sphincter exercises, clinic biofeedback and home biofeedback daily.
Education plus exercises versus education alone
In the groups comparing education plus sphincter exercises (43 patients) with education alone (37 patients) there were no reported difference between the groups for any of multiple outcomes on an intention‐to‐treat analysis immediately after and at one year follow‐up.
Education, sphincter exercises and clinic biofeedback versus education alone
In the groups comparing education plus sphincter exercises versus sphincter exercises plus clinic biofeedback versus sphincter exercises plus clinic and home biofeedback there were no statistically significant differences reported between the groups in the outcomes of manometry, scores, quality of life, diary, visual analogue scale, or anxiety and depression at the end of treatment nor at one year follow‐up.
Education, sphincter exercises, clinic biofeedback and home biofeedback daily versus education alone
In the groups comparing education plus sphincter exercises versus sphincter exercises plus clinic biofeedback versus sphincter exercises plus clinic and home biofeedback there were no statistically significant differences reported between the groups in the outcomes of manometry, scores, quality of life, diary, visual analogue scale, or anxiety and depression at the end of treatment nor at one year follow‐up.
Exercises plus habit re‐training versus habit re‐training alone
Whitehead included 18 participants. The data were not suitable for analysis in RevMan. After four weeks of exercises the median number of incontinent episodes per week was 0.70 for the exercise group and 0.54 for the no‐exercise group. Measures of variation were not reported and it was not possible to perform any statistical analyses on these data. All patients underwent habit training. Alternate patients were initially assigned to sphincter exercises or no exercises. The main focus of the trial was, however, biofeedback therapy. All patients who failed to respond to the exercise phase were treated subsequently with biofeedback. Most of the results presented in the paper referred to this non‐randomised phase and consequently were not analysed. No further data were available from the authors (Whitehead 1985).
4. Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus exercises with or without biofeedback
Four trials were included in this comparison (Fynes 1999; Hinninghofen 2003; Mahony 2004; Schwandner 2010).
Exercises plus biofeedback plus electrical stimulation versus exercises plus biofeedback
The combined result of Fynes and Schwandner showed a statistically significant result favouring the addition of electrical stimulation to biofeedback over biofeedback alone for numbers failing to achieve full continence (RR 0.60, 95% CI 0.46 to 0.78) (Analysis 4.1). Participants were on average 40% more likely to achieve full continence in the electrical stimulation group compared with control.
Schwandner (Schwandner 2010) compared 'Triple target training' where amplitude‐modulated middle‐frequency electrical stimulation was combined with electromyography (EMG) biofeedback versus EMG biofeedback carried out at home daily for 20 minutes for a duration of nine months. Schwandner also showed a statistically significant result for the incontinence score favouring the addition of electrical stimulation (Analysis 4.6).
Fynes (Fynes 1999) compared vaginal pelvic floor manometric pressure biofeedback and home exercises taught by a continence nurse versus anal EMG biofeedback and home exercises in combination with anal electrical stimulation taught by a physiotherapist. The number of people with no improvement in their faecal incontinence symptoms was significantly lower in the electrical stimulation group (RR 0.06, 95% CI 0.00 to 0.91) (Analysis 4.2). Other outcomes were presented as median values and range (continence score) or as mean values and range (resting pressure, squeeze pressure, squeeze increment and vector symmetry). The estimation of the standard deviation could not be computed from the range since this would result in an over‐estimation of the standard deviation.
Mahony (Mahony 2004) compared exercises plus biofeedback plus anal electrical stimulation versus exercises and biofeedback in 54 women with obstetric‐related faecal incontinence. However, most results given were intra‐group rather than inter‐group comparisons. The authors stated that there were no differences between the groups in continence scores, resting or squeeze pressures or quality of life.
Hinninghofen (Hinninghofen 2003) compared sphincter training with electrostimulation versus sphincter training with biofeedback. The data could not be analysed in RevMan.
5. Anal sphincter exercises/PFMT and biofeedback versus anal sphincter exercises/PFMT alone
Three trials were included in this comparison (Bols 2011; Heymen 2009; Hinninghofen 2003).
Bols (Bols 2011) evaluated rectal balloon therapy in addition to PFMT versus PFMT alone and reported that adding rectal balloon therapy was equally effective as PFMT alone in modifying the continence score of 5 points or more, and that added rectal balloon therapy was better than exercises alone on quality of life, manometric and global perceived effect measurements. The data were not suitable for statistical analyses in RevMan.
Heyman (Heymen 2009) compared manometric biofeedback and pelvic floor exercises with exercises alone. The number of people who failed to achieve full continence was significantly lower in the biofeedback and PFMT group (RR 0.70, 95% CI 0.52 to 0.94, Analysis 5.1). The number of people satisfied with the treatment (Analysis 5.3) was not significantly different between intervention groups.
Hinninghofen (Hinninghofen 2003) compared sphincter training with biofeedback versus pelvic floor training without support. The data could not be analysed in RevMan, only a brief abstract in German was available.
6. One type of biofeedback versus another type of biofeedback
Three trials were included in this comparison (Heymen 2000; Norton 2003; Solomon 2003).
Heyman (Heymen 2000) compared four different types of biofeedback: clinic EMG; clinic EMG plus rectal distension; clinic EMG plus home biofeedback; or clinic EMG plus rectal distension and home biofeedback. This trial reported no differences between the groups allocated to the different interventions. The data could not be analysed in RevMan.
Solomon (Solomon 2003) compared anal sphincter exercises (taught verbally and on digital examination) alone versus sphincter exercises plus ultrasound or EMG biofeedback in 120 patients. The data could not be analysed in RevMan. Solomon reported that there were no differences between the three groups in manometric measurements, continence scores, incontinence symptoms or quality of life at the end of treatment. The data for continence scores and manometric parameters are presented in 'Other data' tables (Analysis 6.7; Analysis 6.13).
Norton (Norton 2003) compared education, sphincter exercises and clinic biofeedback versus education, sphincter exercises, clinic biofeedback and home biofeedback. The data could not be analysed in RevMan. Norton stated that the addition of home biofeedback did not result in any statistically significant difference in incontinence scores, manometric measurements, quality of life, diary, or anxiety and depression measurements both at the end of treatment and at one year follow‐up.
7. One type of anal sphincter exercises/PFMT versus another type of anal sphincter exercises/ PFMT
Two trials were included in this comparison (Bartlett 2011; Markwell 2006).
Bartlett compared a standard clinical protocol (sustained submaximal anal and pelvic floor exercises versus an alternative group (rapid squeeze plus sustained submaximal exercises) with biofeedback in both arms of the study (Bartlett 2011) and reported no difference in objective manometric measurements, Cleveland Clinic (Wexner) Fecal Incontinence score or the Fecal Incontinence Quality of Life Scale survey tool.
Markwell (Markwell 2006) compared one type of exercise versus another type of exercise, however there were no useable data for this review. One group (Group A) were taught a specific pelvic floor muscle action, abdominal muscle action, toilet dynamics and dietary advice; the other group (Group B) were taught a standard pelvic floor muscle exercise and were provided with the same dietary advice. Markwell (Markwell 2006) reported that those in Group A were significantly more happy with their symptoms than those in Group B, at three months.
One trial with a complex cross‐over design with only eight patients did not report data in sufficient details to be analysed in RevMan (Latimer 1984).
Discussion
Summary of main results
Some studies have suggested that there is no difference between different conservative interventions and that adding exercises or biofeedback, or both, does not enhance the outcomes of conservative management (Norton 2003). However, subsequent studies have used a step‐wise protocol, trying the simpler interventions first and then only recruiting those who fail to respond to simpler measures such as diet and education (Bols 2011: Heymen 2009). These later studies have found a difference between exercise alone and exercise with the addition of rectal balloon (Bols 2011) or EMG biofeedback (Heymen 2009) in favour of adding biofeedback.
There was not enough evidence to say whether different methods of providing feedback made a difference (Heymen 2000; Norton 2003; Solomon 2003) because the trials were small.
Addition of electrical stimulation to biofeedback and exercises may also enhance results (RR 0.60, 95% CI 0.46 to 0.78) (Fynes 1999; Schwandner 2010). A single trial in this review suggests that anal biofeedback is superior to vaginal, and that electrical stimulation might enhance the results of exercises (Fynes 1999). However, the trial focused on the use of electrical stimulation as an adjunct to biofeedback and compared two very different types of interventions (vaginal pelvic floor manometric pressure biofeedback and home exercise with anal EMG biofeedback and home exercises in combination with anal electrical stimulation) and did not single out just the effects of electrical stimulation or biofeedback. Moreover, it is difficult to know how much of this improvement is a consequence of the natural history of faecal incontinence following childbirth as a no‐treatment group was not included.
In one small trial (Tjandra 2008) showed that sacral nerve stimulation was better than conservative management which consisted of biofeedback and PFMT.
One small trial (Schwandner 2011) showed that adding biofeedback to electrical stimulation was better than electrical stimulation alone (RR for failing to achieve full continence 0.47, 95% CI 0.33 to 0.65).
One small trial (Heymen 2009) comparing manometric biofeedback and pelvic floor exercises with exercises alone showed a statistically significant result for number of people failing to achieve full continence favouring biofeedback (RR 0.70, 95% CI 0.52 to 0.94).
It appears also that training to enhance rectal discrimination of sensation may be helpful in reducing faecal incontinence (Bols 2011; Miner 1990). It may be that adding this technique to the more commonly available pelvic floor muscle training (PFMT) would enhance results, but this cannot be a strong recommendation in view of the small numbers and lack of follow‐up data (Bols 2011).
Further conclusions are not warranted from the available data.
Overall completeness and applicability of evidence
There was a wide variation among trial reports in terms of characteristics of participants, characteristics of interventions, choice of outcome measures, duration of treatment and length of follow‐up. Most of the trials were small and probably of insufficient power to detect any differences between intervention groups. The outcome measures used were often insufficiently reported to enable further statistical analyses. Length of follow‐up was not clearly reported or was inadequate in many of the trials. The way in which data were reported in many of the trials (by not reporting measures of variance) made a quantitative synthesis of results (meta‐analysis) impossible.
Quality of the evidence
Randomised controlled trials are thought to provide sound evidence on the effects of healthcare interventions mainly because they can eliminate selection bias. Methodological weaknesses in some studies included in this review are likely to have compromised this assumption. About half of the trials had low risk of bias for randomisation and allocation concealment.
Potential biases in the review process
It should be noted that pressure and EMG measurements may not be comparable between different studies because of equipment and technique variations. Within‐study changes should be more reliable. There are no direct 'objective' measures of faecal incontinence. Changes in anorectal physiology measurements are proxy outcome measures and need not mean changes in the patient's symptoms, which should be seen as the primary end‐point.
Agreements and disagreements with other studies or reviews
There are over 60 uncontrolled trial reports in the literature on the use of biofeedback for the management of faecal incontinence in adults (Norton 2009). Some authors maintain that biofeedback is the treatment of choice for faecal incontinence on the basis of the findings of these observational studies. The results of this review show that there is some evidence from randomised controlled trials to support the effectiveness of biofeedback therapy for the management of people with faecal incontinence. All studies reviewed showed improved symptoms in all groups, and some difference between groups are reported in the latest studies in favour of adding biofeedback or electrical stimulation.
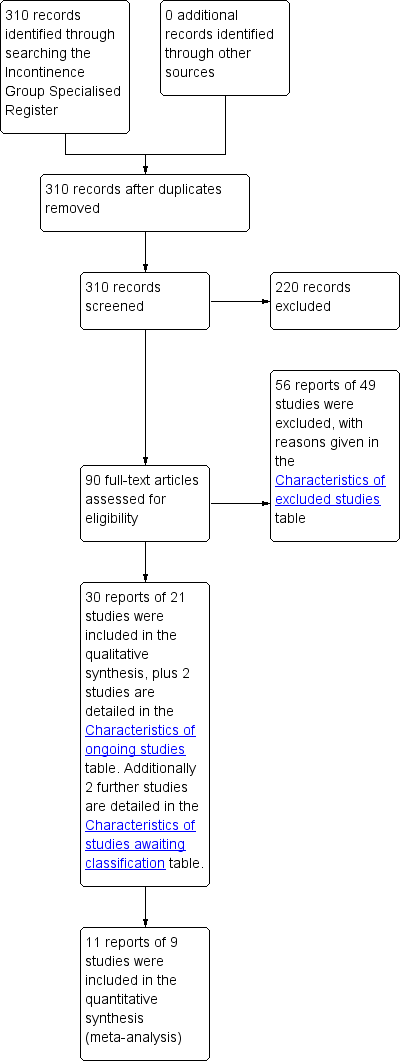
PRISMA study flow diagram.
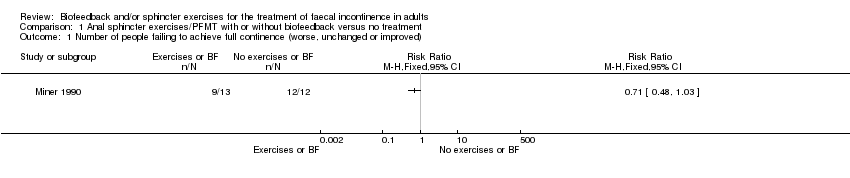
Comparison 1 Anal sphincter exercises/PFMT with or without biofeedback versus no treatment, Outcome 1 Number of people failing to achieve full continence (worse, unchanged or improved).
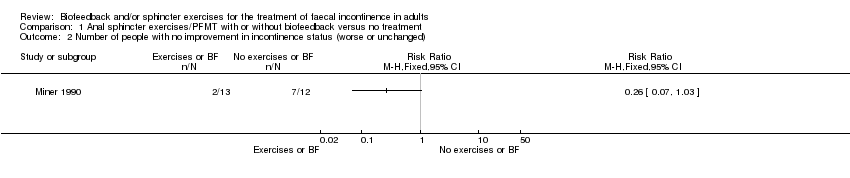
Comparison 1 Anal sphincter exercises/PFMT with or without biofeedback versus no treatment, Outcome 2 Number of people with no improvement in incontinence status (worse or unchanged).

Comparison 1 Anal sphincter exercises/PFMT with or without biofeedback versus no treatment, Outcome 3 Number of incontinence episodes per week.

Comparison 1 Anal sphincter exercises/PFMT with or without biofeedback versus no treatment, Outcome 8 Sensory threshold (rectal balloon distension ‐ ml).

Comparison 2 Anal sphincter exercises/PFMT with or without biofeedback versus any other treatment alone, Outcome 7 Number of people dissatisfied with the treatment.

Comparison 3 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone, Outcome 1 Number of people failing to achieve full continence (worse, unchanged or improved).

Comparison 3 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone, Outcome 4 Number of incontinence episodes per week.
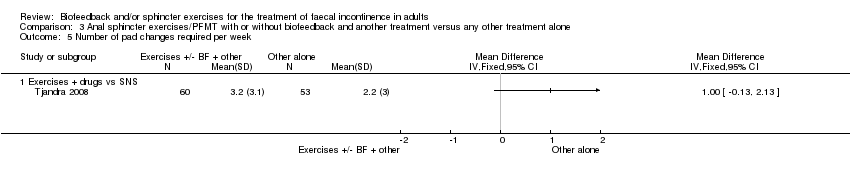
Comparison 3 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone, Outcome 5 Number of pad changes required per week.

Comparison 3 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone, Outcome 6 Incontinence score.

Comparison 3 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone, Outcome 15 General health measures.

Comparison 3 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone, Outcome 16 Condition specific quality of life measures.
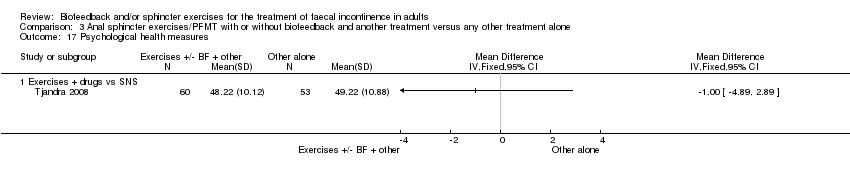
Comparison 3 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone, Outcome 17 Psychological health measures.

Comparison 3 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone, Outcome 19 Satisfaction with treatment (VAS).
| Study | Resting pressure | Squeeze pressure | Fatigue time | ||
| Exercises + BF + education vs exercises + education | |||||
| Ilnyckyj 2005 | Education plus = 51.6 (mm [H2O]) | Education plus BF = 91.7 (mm [H2O]) | Treatment = 19.4 | ||
Comparison 3 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone, Outcome 20 Manometric pressures (medians).

Comparison 4 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus exercises with or without biofeedback, Outcome 1 Number of people failing to achieve full continence (worse, unchanged or improved).

Comparison 4 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus exercises with or without biofeedback, Outcome 2 Number of people with no improvement in incontinence status (worse or unchanged).

Comparison 4 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus exercises with or without biofeedback, Outcome 6 Incontinence score.

Comparison 5 Anal sphincter exercises/PFMT and biofeedback versus anal sphincter exercises/PFMT alone, Outcome 1 Number of people failing to achieve full continence (worse, unchanged or improved).

Comparison 5 Anal sphincter exercises/PFMT and biofeedback versus anal sphincter exercises/PFMT alone, Outcome 3 Number of people dissatisfied with the treatment.
| Study | St Marks Vaizey 0‐13 | Pescatori (0‐6) | Self‐rating (0‐10) |
| Solomon 2003 | Ultrasound BFB = 7 | Ultrasound BFB = 4 | Ultrasound BFB = 3.6 |
Comparison 6 One type of biofeedback versus another type of biofeedback, Outcome 7 Incontinence score (median).
| Study | Resting pressure | Squeeze pressure | Fatigue time |
| Solomon 2003 | Ultrasound BFB = 44 (mm Hg) | Ultrasound BFB = 95 (mm Hg) | Ultrasound BFB = 27 (sec) |
Comparison 6 One type of biofeedback versus another type of biofeedback, Outcome 13 Manometric pressures (medians).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of people failing to achieve full continence (worse, unchanged or improved) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Number of people with no improvement in incontinence status (worse or unchanged) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Number of incontinence episodes per week Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Number of pad changes required per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Incontinence score | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Number of people with adverse effects | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Number of people dissatisfied with the treatment | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Sensory threshold (rectal balloon distension ‐ ml) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9 Manometric resting pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Manometric squeeze pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Manometric squeeze increment (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Duration of squeeze (seconds) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 General health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Condition specific quality of life measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Psychological health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Activities of daily living measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of people failing to achieve full continence (worse, unchanged or improved) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Number of people with no improvement in incontinence status (worse or unchanged) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Number of incontinence episodes per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Number of pad changes required per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Incontinence score | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Number of people with adverse effects | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Number of people dissatisfied with the treatment Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1 Biofeedback vs electrical stimulation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Sensory threshold (rectal balloon distension ‐ ml) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Manometric resting pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Manometric squeeze pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Manometric squeeze increment (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Duration of squeeze (seconds) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 General health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Condition specific quality of life measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Psychological health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Activities of daily living measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of people failing to achieve full continence (worse, unchanged or improved) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Exercises +BF+ ES vs ES alone | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Number of people with no improvement in incontinence status (worse or unchanged) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Satisfaction with the treatment | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Number of incontinence episodes per week Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Exercises + drugs vs SNS | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Number of pad changes required per week Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 Exercises + drugs vs SNS | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Incontinence score Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 Exercises + BF + surgery vs surgery alone | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Exercises + drugs vs SNS | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 Exercises + BF + ES vs ES alone | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Number of people with adverse effects | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Sensory threshold (rectal balloon distension ‐ ml) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Manometric resting pressure | 0 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.1 Exercises + BF + ES vs ES alone | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Manometric squeeze pressure (cm of water) | 0 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 Exercises + BF + ES vs ES alone | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Manometric squeeze increment (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Duration of squeeze (seconds) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Vector symmetry index | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Saline retention test (ml) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 General health measures Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.1 Exercises + drugs vs SNS | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Condition specific quality of life measures Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16.1 Exercises + drugs vs SNS | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Psychological health measures Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 17.1 Exercises + drugs vs SNS | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 Activities of daily living measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Satisfaction with treatment (VAS) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 19.1 Exercises + BF + surgery vs surgery alone | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 Manometric pressures (medians) Show forest plot | Other data | No numeric data | ||
| 20.1 Exercises + BF + education vs exercises + education | Other data | No numeric data | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of people failing to achieve full continence (worse, unchanged or improved) Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Exercises + BF + ES vs exercises + BF alone | 2 | 167 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.46, 0.78] |
| 2 Number of people with no improvement in incontinence status (worse or unchanged) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Exercises + BF + ES vs exercises + BF alone | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Number of people dissatisfied with the treatment | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Number of incontinence episodes per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Number of pad changes required per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Incontinence score Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Exercises + BF + ES vs exercises + BF alone | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Number of people with adverse effects | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Sensory threshold (rectal balloon distension ‐ ml) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Manometric resting pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Manometric squeeze pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Manometric squeeze increment (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Duration of squeeze (seconds) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Vector symmetry index | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Saline retention test (ml) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 General health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Condition specific quality of life measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Psychological health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of people failing to achieve full continence (worse, unchanged or improved) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Number of people with no improvement in incontinence status (worse or unchanged) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Number of people dissatisfied with the treatment Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Number of incontinence episodes per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Number of pad changes required per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Incontinence score | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Number of people with adverse effects | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Sensory threshold (rectal balloon distension ‐ ml) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Manometric resting pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Manometric squeeze pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Manometric squeeze increment (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Duration of squeeze (seconds) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Vector symmetry index | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Saline retention test (ml) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 General health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Condition specific quality of life measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Psychological health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Activities of daily living measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of people failing to achieve full continence (worse, unchanged or improved) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Number of people with no improvement in incontinence status (worse or unchanged) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Number of people dissatisfied with the treatment | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Number of incontinence episodes per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Number of pad changes required per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Incontinence score | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Incontinence score (median) Show forest plot | Other data | No numeric data | ||
| 8 Number of people with adverse effects | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Sensory threshold (rectal balloon distension ‐ ml) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Manometric resting pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Manometric squeeze pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Manometric squeeze increment (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Manometric pressures (medians) Show forest plot | Other data | No numeric data | ||
| 14 Duration of squeeze (seconds) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Vector symmetry index | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Saline retention test (ml) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17 General health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Condition specific quality of life measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Psychological health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Activities of daily living measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Activities of daily living measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of people failing to achieve full continence (worse, unchanged or improved) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Number of people with no improvement in incontinence status (worse or unchanged) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Number of incontinence episodes per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Number of pad changes required per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Incontinence score | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Number of people with adverse effects | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Number of people dissatisfied with the treatment | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Sensory threshold (rectal balloon distension ‐ ml) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Manometric resting pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Manometric squeeze pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Manometric squeeze increment (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Duration of squeeze (seconds) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 General health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Condition specific quality of life measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Psychological health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Activities of daily living measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |

